medical-surgical flowsheet guidelines - Department of Nursing ...
medical-surgical flowsheet guidelines - Department of Nursing ...
medical-surgical flowsheet guidelines - Department of Nursing ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
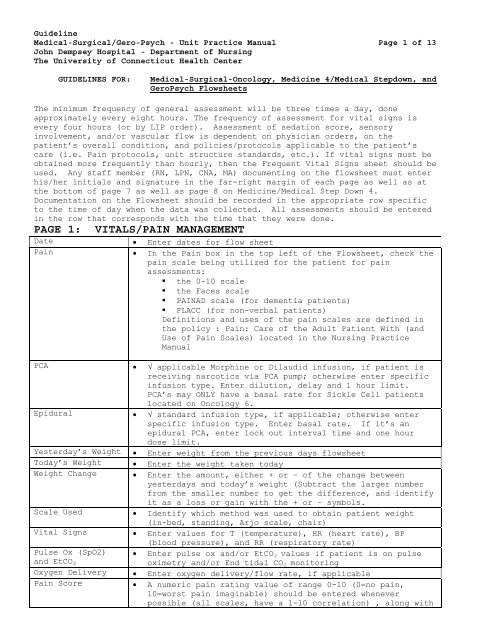
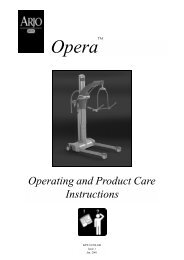
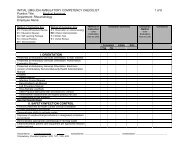
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 1 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsThe minimum frequency <strong>of</strong> general assessment will be three times a day, doneapproximately every eight hours. The frequency <strong>of</strong> assessment for vital signs isevery four hours (or by LIP order). Assessment <strong>of</strong> sedation score, sensoryinvolvement, and/or vascular flow is dependent on physician orders, on thepatient’s overall condition, and policies/protocols applicable to the patient’scare (i.e. Pain protocols, unit structure standards, etc.). If vital signs must beobtained more frequently than hourly, then the Frequent Vital Signs sheet should beused. Any staff member (RN, LPN, CNA, MA) documenting on the <strong>flowsheet</strong> must enterhis/her initials and signature in the far-right margin <strong>of</strong> each page as well as atthe bottom <strong>of</strong> page 7 as well as page 8 on Medicine/Medical Step Down 4.Documentation on the Flowsheet should be recorded in the appropriate row specificto the time <strong>of</strong> day when the data was collected. All assessments should be enteredin the row that corresponds with the time that they were done.PAGE 1: VITALS/PAIN MANAGEMENTDate Enter dates for flow sheetPain In the Pain box in the top left <strong>of</strong> the Flowsheet, check thepain scale being utilized for the patient for painassessments:• the 0-10 scale• the Faces scale• PAINAD scale (for dementia patients)• FLACC (for non-verbal patients)Definitions and uses <strong>of</strong> the pain scales are defined inthe policy : Pain: Care <strong>of</strong> the Adult Patient With (andUse <strong>of</strong> Pain Scales) located in the <strong>Nursing</strong> PracticeManualPCA √ applicable Morphine or Dilaudid infusion, if patient isreceiving narcotics via PCA pump; otherwise enter specificinfusion type. Enter dilution, delay and 1 hour limit.PCA’s may ONLY have a basal rate for Sickle Cell patientslocated on Oncology 6.Epidural √ standard infusion type, if applicable; otherwise enterspecific infusion type. Enter basal rate. If it’s anepidural PCA, enter lock out interval time and one hourdose limit.Yesterday’s Weight Enter weight from the previous days <strong>flowsheet</strong>Today’s Weight Enter the weight taken todayWeight Change Enter the amount, either + or – <strong>of</strong> the change betweenyesterdays and today’s weight (Subtract the larger numberfrom the smaller number to get the difference, and identifyit as a loss or gain with the + or – symbols.Scale Used Identify which method was used to obtain patient weight(in-bed, standing, Arjo scale, chair)Vital Signs Enter values for T (temperature), HR (heart rate), BP(blood pressure), and RR (respiratory rate)Pulse Ox (SpO2) Enter pulse ox and/or EtCO 2 values if patient is on pulseand EtCO 2 oximetry and/or End tidal CO 2 monitoringOxygen Delivery Enter oxygen delivery/flow rate, if applicablePain Score A numeric pain rating value <strong>of</strong> range 0-10 (0=no pain,10=worst pain imaginable) should be entered wheneverpossible (all scales, have a 1-10 correlation) , along with
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 2 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych Flowsheetsa Y (yes) or N (no) indicating whether or not the patientfinds the pain level acceptable to him/herPCA Document the number <strong>of</strong> injected doses <strong>of</strong> medication and thenumber <strong>of</strong> attempts for patients on a PCA pumpSedation Score,Sensory Check, Enter values using the legend at top <strong>of</strong> page.Motor CheckEpidural Rate/Site Enter the rate that the epidural is running at. RateCheckchanges are captured here Epidural site check must be performed every 12 hours. Thesite should be assessed for redness, bruising, swelling andleakage. The check mark indicates the check was done, ifany <strong>of</strong> the above are present (redness, bruising,swelling,leakage), document in the nursing note and notifyanesthesia.Pulses Document strength <strong>of</strong> blood flow <strong>of</strong> the RRAD (right radial),LRAD (left radial), RDP (right dorsalis pedis) and LDP(left dorsalis pedis) by indicating if the palpable pulsesor Doppler pulse is 0 (absent), 1 (diminished/weak), 2 (asexpected), 3 (full/increased), or 4 (bounding), or if thedoppler measurement is audible (DA) or inaudible(DI)Comments/Meds Use this column for any medications you want to include onthe Flowsheet (perhaps in response to an elevated VS or FSGor pain) or any other comments that may be helpful. ReferFingerstickglucose (FSG)to MAR for documentation <strong>of</strong> any medications administeredEnter any decentralized lab testing values and slidingscale insulin coverage if applicable; refer to MAR fordocumentation <strong>of</strong> all drugs administered in response to thevalue** A significant deterioration in any vital sign or other objective measure <strong>of</strong>patient status indicates the need to report the condition to the LicensedIndependent Practitioner (LIP).PAGE 2: 24 HOUR FLUID INTAKEIV Sites Document the location(s) <strong>of</strong> each IV site. There is space toinclude 3(three) IV sites as well as 1 (one) central line.Be sure to specify insertion date. If the dressing isintact, changed or the IV is discontinued, check theappropriate box.For Portacaths, identify the date <strong>of</strong> the needle change, aswell is when the dressing change was done and whether theneedle was discontinues.Infusions A column is provided for up to 5 (Five) separate infusions.Each infusion should have the intravenous fluid (IVF) beingadministered identified along with the corresponding sitenumber (#).Solutions infused must be documented with the correspondingcolumn/IV site, as well as the hourly ratePhlebitis and infiltration scores should be documentedevery 8 hours under the corresponding IV site
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 3 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsIV document the volume <strong>of</strong> intermittent medicationsMedications/Flush administered, when applicableTube Feeds Document the type <strong>of</strong> tube feeding product being used, aswell as the hourly infusion rateResidual/Placement Document the volume <strong>of</strong> residual aspirated as well as theplacement <strong>of</strong> the tube (+ for positive placement – fornegative placement, if placement is negative, nothingshould be placed in the tube, and the LIP contactedPO Fluid All oral fluids must be included in the cumulative 24-hourintake CalculationPO Solid (%)DietDocument the percentage <strong>of</strong> each meal consumed, especiallyfor patients on calorie counts. Document the patientscurrent diet orderIntake Hourly If needed, this column can be used to keep track <strong>of</strong> allCumulativeintake on an hourly basis8 Hour Total At eight hour intervals, record the 8-hour intake for eachcolumn24 Hour Total At the bottom <strong>of</strong> the page, record the 24-hour intake foreach columnPAGE 3: 24 HOUR FLUID OUTPUTTop Left BoxTop Right BoxTubes 1-5CBI: Continuousbladder irrigationCheck the appropriate box to indicate how the patient voids,and if they have a colostomy or ileostomy. If they do have anappliance, indicate when the change was done and the dateHemodialysis- check the box if they are a hemodylasis patientCAPD- check the box if the patient is a CAPD patient- thiswill indicate a separate CAPD <strong>flowsheet</strong>Due to Void (DTV): check the box and enter the time that thepatient is due to void in this space.EBL: enter the estimated blood loss in this column.Enter type <strong>of</strong> tube at top <strong>of</strong> column, and the hourly output,if applicableMake certain that each tube is clearly labeled on the<strong>flowsheet</strong> and correspond to the same tube on the patient.Enter the type <strong>of</strong> continuous bladder irrigation fluid beingused.Record amounts for solution hung, amount infused each hour,and amount <strong>of</strong> output each hour. Then calculate the true urineoutput by subtracting amount infused from the output.Urine OutputEnter volume <strong>of</strong> output corresponding to the appropriate time<strong>of</strong> dayPost Void Residual Enter volume <strong>of</strong> urine obtained after patient voids(PVR):Stool/Heme LBM = last bowel movement; enter the date <strong>of</strong> the last bowelmovement Indicate the volume <strong>of</strong> stool produced, as appropriate. Forhemacult testing use + if positive or – if negativestickermay be used.Emesis Enter amount produced, as appropriate
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 4 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych Flowsheets8 Hour Total At three, 8 hour intervals, record the 8-hour output foreach column24 Hour Total At the bottom <strong>of</strong> the page, record the 24-hour output foreach columnCumulative Values At bottom <strong>of</strong> page 3, record the 24-hour cumulative totalintake from the previous page and the total output from thecurrent page in the dark-outlined boxSubtract the two values to determine the 24-hour netbalance, and record on the FlowsheetPAGE 4: NURSING ASSESSMENTEye Opening Using the legend at the top <strong>of</strong> the page, document thepatients eye opening response:• 4 – spontaneously• 3 - to speech• 2 – to pain• 1 – no openingMotor Response Using the legend at the top <strong>of</strong> the page, document thepatients motor response:• 6 – observes commands• 5 – localizes pain• 4 – withdraws from pain• 3 – flexion to pain• 2 – extension to painRespiratoryAssessmentVerbalResponse• 1 – noneUsing the legend at the top <strong>of</strong> the page, document verbalresponse:• 5 – oriented• 4 – confused• 3 – inappropriate• 2 – incomprehensible• 1 - noneMotor Function Assess motor function <strong>of</strong> the left and right upper and lowerextremities as:5-full strength4-less than normal strength3-can raise extremity, but not against resistance2-can move extremity, but not lift it1-slight movement0-no movementPupils Document size and reaction for left and right eyeaccordinglySuctionIncentiveSpirometerTrach Care Place a check mark in the appropriate box corresponding tothe time that each <strong>of</strong> these tasks was performed by thenurse or patientBreath Sounds Document auscultated breath sounds according to the legend atthe top <strong>of</strong> the page, corresponding to the time <strong>of</strong> theassessmentBoxes are labeled as LUL (left upper lobe), LLL (left lowerlobe), RUL (right upper lobe) and RLL (right lower lobe)Breath sounds are identified as N (normal), W (wheeze), C
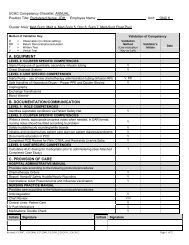
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 5 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsGI AssessmentSputumBowel SoundsFlatusEdema(crackles), A (absent), or (decreased)The color (clear, white, tan, yellow, green, hemoptysis) andamount <strong>of</strong> sputum (small, medium, large/copious) is documentedin the corresponding boxes and under the appropriate timeframeUsing the legend at the top <strong>of</strong> page 4, document the patients’abdominal exam. Bowel sounds are assessed in each <strong>of</strong> the fourquadrants: RUQ (right upper quadrant), RLQ (right lowerquadrant), LUQ (left upper quadrant), and LLQ (left lowerquadrant) as positive, negative hypoactive or hyperactive.Flatus is documented as either positive or negativeEdema is documented according to the legend at the top <strong>of</strong> thepage for right and left, upper and lower extremities (RUE,RLE, LUE, LLE)PAGE 5: FALL PREVENTION TREATMENT PLANFALL PREVENTION TREATMENT PLANFall Prevention Treatment Plan is incorporated into the <strong>medical</strong> 4/ Med Stepdown andMed/Surg/Onc Flowsheet as its own form. It now incorporates both the fall score aswell as various potential or actual interventions put into place for a givenpatient.The Fall Risk Assessment Screening Tool is located on the left side <strong>of</strong> thedocument, and is divided into 5 categories – fall history;confusion/disorientation; mobility impaired/change <strong>of</strong> position; elimination,altered; and medications.The next column provides an overview <strong>of</strong> the patient descriptors (i.e. indicatorsfor point values) for each fall risk category.The Shift/Time boxes should be filled in for the shift/time that the fall riskscreening was completed. The number <strong>of</strong> points the patient scores for each givencategory (from 4 points to 2 points) should be filled in for each category. Thefall risk score should be totaled at the bottom <strong>of</strong> this column.The Interventions/Guidelines column provides the nurse the opportunity to documentinterventions put into place for a given shift/time <strong>of</strong> day. The Shift/Time boxneeds to completed at the time <strong>of</strong> documenting interventions. Universal Risk islocated at the top <strong>of</strong> the form and includes pre-determined interventions tomaintain the safety <strong>of</strong> all patients regardless <strong>of</strong> what their fall score isdetermined to be. They should be implemented and signed <strong>of</strong>f for all patients by allnurses in the appropriate column corresponding to the shift/time.The Fall risk assessment screening categories are scored according to whether thepatient meets any <strong>of</strong> the patient descriptors in the second column. The point value(2 or 4 pts) should be written in the column corresponding the shift/time <strong>of</strong>screening. If the patient scores any points for any given fall risk, then anyinterventions put into place for that given risk should be signed <strong>of</strong>f. Please notethat some interventions are required interventions (noted with an asterisk [*]) fora given fall risk. For example, if a patient earns 2 or 4 points for the fallhistory category, then the required interventions that should be
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 6 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych Flowsheetsinitiated/implemented and signed <strong>of</strong>f include “PT consult ordered” and “encouragepatient to call for assistance.” Other interventions listed next to fall historyare optional and should be based on additional patient factors.PAGE 6:SKIN AND WOUND ASSESSMENTSScoring <strong>of</strong> the Braden Scale Pressure Ulcer Risk Reduction Tool, interventions, anddocumentation <strong>of</strong> skin or wound breakdown documentation is located page 6, in thesection called Skin and Wound Assessments.There are 3 outlined areas to complete in this form:I. Outlined area 1: Braden ScaleAll adult inpatients should have this form completed using the following<strong>guidelines</strong>:The Braden Scale will be performed:o On hospital admissiono Every 24 hourso Upon patient transfer (by the nurse accepting the patient on the new unit)o With any change <strong>of</strong> conditionTimeInitialsSensoryPerceptionEnter the military time the Braden Scale is donePlace your initials in the boxPlace a numerical score in the subset box (from 1-4).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. completely limited sensory perception2. very limited sensory perception3. slightly limited sensory perception4. no impairmentMoisture Place a numerical score in the subset box (from 1-4).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. constantly moist2. very moist3. occasionally moist4. rarely moistActivity Place a numerical score in the subset box (from 1-4).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. bedfast2. chairfast3. walks occasionally4. walks frequentlyMobility Place a numerical score in the subset box (from 1-4).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. completely immobile2. very limited mobility3. slightly limited mobility4. no mobility limitationNutrition Place a numerical score in the subset box (from 1-4).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. very poor nutritional status
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 7 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsFriction &ShearTotalIdentifiedRisk2. probably inadequate nutrition status3. adequate nutrition4. excellent nutritionPlace a numerical score in the subset box (from 1-3).The score is based on the nurse’s patient assessment <strong>of</strong>the following:1. problem identified for patient “at risk” forfriction and shear skin injuries2. potential problem identified for patient3. no apparent problem identifiedAdd scores <strong>of</strong> all the subset boxes for a total compositescorePlace a checkmark in the box to indicate that the patientis identified as “At Risk” if the total score equals/oris less than the number 18 OR equals/or is less than thenumber 2 in any subset.Interventions A permanent “X” is placed in the box to remind the nurseto implement interventions based on the Procedure For:Pressure Ulcer Prevention and Management: Care <strong>of</strong> theAdult Inpatient.II. Outlined area 2: Broken into 5 boxes which consist <strong>of</strong>Outline <strong>of</strong> Body, General Reminders, Pressure Ulcer PreventionInterventionsBox 1Braden & SkinAssessmentcompleted:Box 2WoundAssessmentcompleted:Box 3InterventionsTriggers reminders when to complete – hospital admission every 24 hours upon transfer with change in conditionTriggers reminders when to complete – within 24 hours <strong>of</strong> hospital admission weekly (Wednesday) with change in condition <strong>of</strong> patient or woundEvery patient must have interventions appropriatelychecked <strong>of</strong>f to indicate care given. Special attentionmust be given to match appropriate interventions when apatient is found at risk in a particular subset (equalto/or less than 2).Interventions will include: Nutritional i.e. dietary consult, supplemental tubefeeding, TPN, calorie count, etc. Float heels i.e. positioning lower extremitiesusing pillows to <strong>of</strong>fload heels Chair cushion i.e. use <strong>of</strong> a pressure reductioncushion in the chair Head <strong>of</strong> bed less than 30 degrees Use <strong>of</strong> a moisture barrier cream to dry skin toreduce surface tension & risk <strong>of</strong> shear Use <strong>of</strong> a pressure reduction mattress i.e.versacare, total care sport
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 8 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsBox 4Outline <strong>of</strong>body (frontand back)Outline <strong>of</strong>plantarsurface <strong>of</strong>feetOutline <strong>of</strong>dorsalsurface <strong>of</strong>feetBox 5Is this theAdmissionAssessment? Turn/reposition plan Other ____________Fill in i.e. use <strong>of</strong> hovermat fortransferring patientCircle and number any areas <strong>of</strong> skin breakdown on theanatomical outline to correspond to the descriptorslocated below in Outline Area #3.Question is posed to prompt nurse to check <strong>of</strong>f either“yes” or “no” :Yes – this is done only one time at the initial hospitaladmissionNo – this is checked every time after the hospitaladmissionIII. Outlined area 3: Skin or Wound Breakdown Areas DocumentationWhen the nurse determines that the patient does not have any areas <strong>of</strong>skin breakdown following the performance a skin assessment, the nursechecks <strong>of</strong>f the box “No Skin Breakdown”. No further documentation isneeded on this form.However, when a patient has skin breakdown or wounds, this spacedocuments wound descriptors for pressure ulcer wounds or non-pressureulcer wounds (arterial ulcers, venous stasis ulcers, skin tears,presence <strong>of</strong> a rash, wound dehiscence, fistulas, an open postop <strong>surgical</strong>incision, etc.) using these parameters:oooWithin 24 hours <strong>of</strong> hospital admissionWeekly (every Wednesday)With change in patient or wound conditionPage 6 supplements the overall Skin Assessment Section located on page7 <strong>of</strong> the Med/Surg/Onc Flowsheet The one exception to completion <strong>of</strong>this part <strong>of</strong> the wounds flow sheet for wounds is a <strong>surgical</strong> incisionthat is well-approximated and closed, and the patient has no additionalskin or wound breakdowns to describe. In that case, the documentationon page 7 is sufficient, and notes the <strong>surgical</strong> incision’s location,and whether it is clean ©, dry (D), dressing intact (I), andapproximated (A).
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 9 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsLocation Columns #1, #2, #,3,#41. List each location <strong>of</strong> skin breakdown or woundlocation, up to 4 sites.2. Should correspond to circled and number areas <strong>of</strong>the body outline.3. If there are additional columns needed foradditional areas, please use a second flow sheetand label “second sheet”.Wound Type Under appropriate column, fill in the wound type usingthe abbreviations:NPU non-pressure ulcer (such as arterial, venous,diabetic)OSI open <strong>surgical</strong> wound (dehisced, post-op)ST skin tearPU pressure ulcerR rashPressureUlcer Stageor NALengthWidthDepthTunnelingUnderminingWoundAppearanceDrainageTypeO other (purpura, hematoma, etc.)Pressure ulcer (skin breakdown over bony prominence frompressure, friction, shear)Stage 1Stage 2Stage 3Stage 4DTI Deep Tissue InjuryUS UnstageableN/A No Applicable - not a pressure ulcerMeasurement <strong>of</strong> length <strong>of</strong> wound in centimeters (head totoe)Measurement <strong>of</strong> width <strong>of</strong> wound in centimeters (hip to hip)Measurement <strong>of</strong> depth <strong>of</strong> wound in centimeters (deepestarea0In presence <strong>of</strong> wound tunneling, describe in centimeterslocation using clock method, such as“1.5 cm at 9 oclock”Leave blank or draw line through box if tunneling is notpresent.In presence <strong>of</strong> wound undermining, describe in centimeterslocation using clock method, such as “2.5 cm at 2 to 4 oclock”Leave blank or draw line through box if undermining isnot present.In percentages, describe wound bed, based on appearance.R= red wound bed, represents granulationY = yellow wound bed, represents sloughB = Black or brown wound bed, represents necrotic tissueUnder appropriate column for each corresponding wound,document drainage type:N= none (no drainage)S= serousSA= sanguinousP= purulent
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 10 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsDrainageAmountSurroundingTissueOdorTreatmentcodeTXUnder appropriate column for each corresponding wound,document drainage amount:N= none (no drainage)M= minimal (scant)MO= moderateL=largeDescribe surrounding wound tissue (periwound):I= intactP=purpleEX= excoriatedM=maceratedR= red or erythemaO=otherDoes the wound have an odor?Y= yesN= noAllows documentation <strong>of</strong> up to three daily dressingchanges for each wound with time <strong>of</strong> change and initialsunder the appropriate wound column using treatment codes: Category I = Place I in column for dressingchanged, wound unchanged Category II= Place II in column for a dressingchanged, wound appears changed furtherdocumentation to support change is written in thecolumns above Category III= Place III in column when dressingremains intact, and is not changed or not due to bechangedDocumentation <strong>of</strong> treatment or dressings with time andinitials under the corresponding columns matched tosequence <strong>of</strong> dressing changes (1,2, or 3):H= hydrocolloid (duoderm)DSD= dry sterile dressingVac= wound vacBS= barrier spray ( i.e. cavilon spray)HB= hydr<strong>of</strong>era blueHG= hydrogelWD= wet to dryHF= hydr<strong>of</strong>iber (Aquacel)HFAG= hydr<strong>of</strong>iber with silver (aquacel AG)OTA= open to airO= other Describe _____________ (examples – Dakin’ssolution, mepilex, mesalt)
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 11 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsPAGE 7: CARE GIVENThe nurse performing the nursing assessment and/or collecting data must enterthe shift that the identified nursing care is given. Care needs are divided intotwo different columns and categorized on the left hand side <strong>of</strong> each column.Categories are hygiene, activity, skin assessment, safety, cardiac and chest tubes.Next to each category are various check boxes and/or interventions with boldedcodes. When care is provided to a patient, the nurse writes his/her initials or thecode next to the nursing care under his/her corresponding shift column.Hygiene Initial one or more boxes appropriate for the care whichwas provided:• Shower (S), Sponge bath (SB)• Self/Assist/Total (S, A or T)• Pericare/Foley care (P or F)• Bedside Commode• Oral Care• OtherActivity Initial and/or check the appropriate box(es) applicable tothe patient’s activity level:• Bedrest• Out <strong>of</strong> Bed (OOB): with assist or without assist• Ambulate: with assist or without assist• Turn/Reposition q ____ hours• Bed: Versacare, Advanta or Other• H.O.B. ______degrees• Traction and/or CPM and/or Foot pumps and/or Legpumps as well as bilateral, right limb or left limb• Immobilizer: Identify type <strong>of</strong> immoblizer used andwhich side (left, right or bilateral) it is beingused on as appropriate.• OtherSkin Assessment Document whether the patient has no skin breakdown. Document weather the patient’s skin is pink (P), warm (W),dusky(D) and/or Jaundice (J). If other- describe (such aspale) If there is a <strong>surgical</strong> incision, document the location, andif it is clean (C), dry (D), dressing intact (I) andapproximated (A). There is space for two <strong>surgical</strong>incisions. Other wounds or Skin breakdown: initial to indicate thatthe skin and wound assessment page has been utilizedSafety Initial appropriate boxes for:• side rails up (2-3 rails may be up, 4 side rails upare considered a restraint).• call light in reach• ID bracelet (white) is on• Correct colored snap(s) applied to ID bracelet Allergy – red snap Fall risk – yellow snap
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 12 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych Flowsheets Latex – green Limb Alert – pink snap DNR – purple snap• Bed Alarm (B) or Chair Alarm (C) is on• Restraints• Constant observation/1:1• Seizure precautions• Aspiration precautions• Other (such as radiation)• Visual impairment or deaf/hard <strong>of</strong> hearing• If interpreter services are needed, and if so whatlanguageCardiac Indicate type <strong>of</strong> monitoring used (if any): Telemetry,Hardwire or continuous pulse oximetry Permanent Pacemaker AICD (automated implantable cardioverter-defibrillator)Chest Tubes Indicate if the patient has a pleural chest tube (right orleft) Indicate if chest tube is on continuous low wall suction(S) or to water seal (W) by placing a S or W in thecorresponding time column. Presence <strong>of</strong> an air leak: Y= Yes N= No, enter Y or N incolumn Presence <strong>of</strong> crepitus : Y= Yes N= No, enter Y or N in columnInitials/Signature EVERY person documenting on the Flowsheet must have theirinitials, signature and title documented on the bottom <strong>of</strong>page 7~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~PAGES 8 and 9 are for Medicine 4 and Medical Stepdown ONLY:Page 8: Arrhythmia StripsArrhythmia StripsPage 8 <strong>of</strong> the <strong>flowsheet</strong> includes space for four differentarrhythmia strips. It is important that the strip does notexceed the space <strong>of</strong> the box outlined on the page. To the leftthe date and time should be recorded along with the rate, PRI,QRS, QT and interpretation. A signature should accompany eachstrip. The person recording the strip must also sign, initialand title the bottom <strong>of</strong> page 7 on the <strong>flowsheet</strong>. Thefrequency <strong>of</strong> obtaining and interpreting strips is outlined inthe policy: Cardiac Monitoring: Care <strong>of</strong> the Patient onCardiac Monitoring.
GuidelineMedical-Surgical/Gero-Psych - Unit Practice Manual Page 13 <strong>of</strong> 13John Dempsey Hospital - <strong>Department</strong> <strong>of</strong> <strong>Nursing</strong>The University <strong>of</strong> Connecticut Health CenterGUIDELINES FOR:Medical-Surgical-Oncology, Medicine 4/Medical Stepdown, andGeroPsych FlowsheetsPage 9: Frequent Vital SignsFrequent VitalSignsFor vitals signs that are obtained more frequently that oncean hour, record the following: Date, time, temperature, heartrate/rhythm, respiratory rate, blood pressure, SpO2 (pulseoximetry), any applicable comments and initials. Initialsmust have corresponding signature, initials and title on page7 <strong>of</strong> the flow sheet.Important Documentation Reminders:1. A progress note is required a minimum <strong>of</strong> every 24 hours, and in accordancewith the “Documentation: Progress Notes” procedure located in the <strong>Nursing</strong>Practice Manual.2. All nursing progress notes will be written using DAR (focus) format, andlabeled using a nursing diagnosis, an event or symptom, a variance, or anactive problem on the patient care plan.D (Data): Subjective and/or objective information, which supports theproblem or describes observations at the time <strong>of</strong> a significant event intherapyA (Action): Past, present or future actions based on theassessment/evaluation <strong>of</strong> the patient’s condition. The action alsoincludes evaluation <strong>of</strong> the present care plan, any changes required, andthe plan for future careR (Response): Description <strong>of</strong> patient responses/outcomes to care3. All med/surg patients will have an individualized patient care plan initiatedby the nurse. This will be kept either in the <strong>medical</strong> record or in the binderwith the <strong>flowsheet</strong> outside the patient’s room. The patient care plan willserve as a communication and documentation tool for clinical staff as theywork with the patient, family and interdisciplinary team to:a. plan the patient’s care based on clinical, psychosocial,teaching/learning, spiritual and cultural needsb. set outcomes based goalsc. identify interventions to be implemented for attaining goals4. Problems on the patient care plan will be reviewed and prioritized at leastonce daily by the nurse. Data supporting the patient’s specificfocus/problem, interventions (including assessments and monitoring), andpatient response will be reflected through the use <strong>of</strong> unit-specific<strong>flowsheet</strong>s, and focus/DAR notes in the <strong>medical</strong> record.5. All patient and family teaching must be documented on the appropriate Patientand Family Teaching Record.Effective Date: 11/03Revised: 12/08, 6/09, 9/09, 9/2010