TAYLOR SPATIAL FRAME: Butt Frame Configuration and Application
TAYLOR SPATIAL FRAME: Butt Frame Configuration and Application
TAYLOR SPATIAL FRAME: Butt Frame Configuration and Application
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
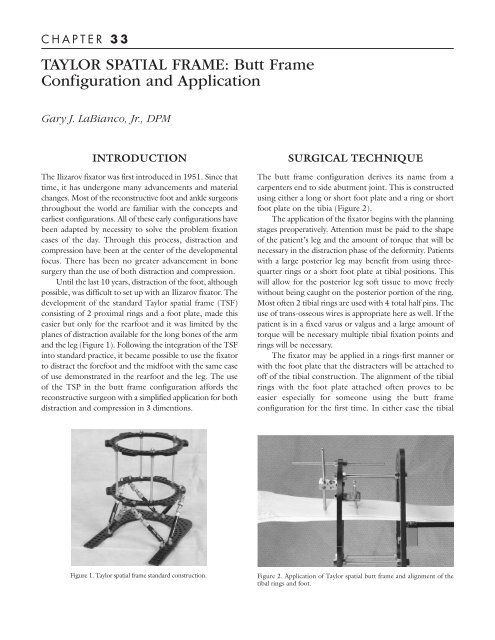
C H A P T E R 3 3<strong>TAYLOR</strong> <strong>SPATIAL</strong> <strong>FRAME</strong>: <strong>Butt</strong> <strong>Frame</strong><strong>Configuration</strong> <strong>and</strong> <strong>Application</strong>Gary J. LaBianco, Jr., DPMINTRODUCTIONThe Ilizarov fixator was first introduced in 1951. Since thattime, it has undergone many advancements <strong>and</strong> materialchanges. Most of the reconstructive foot <strong>and</strong> ankle surgeonsthroughout the world are familiar with the concepts <strong>and</strong>earliest configurations. All of these early configurations havebeen adapted by necessity to solve the problem fixationcases of the day. Through this process, distraction <strong>and</strong>compression have been at the center of the developmentalfocus. There has been no greater advancement in bonesurgery than the use of both distraction <strong>and</strong> compression.Until the last 10 years, distraction of the foot, althoughpossible, was difficult to set up with an Ilizarov fixator. Thedevelopment of the st<strong>and</strong>ard Taylor spatial frame (TSF)consisting of 2 proximal rings <strong>and</strong> a foot plate, made thiseasier but only for the rearfoot <strong>and</strong> it was limited by theplanes of distraction available for the long bones of the arm<strong>and</strong> the leg (Figure 1). Following the integration of the TSFinto st<strong>and</strong>ard practice, it became possible to use the fixatorto distract the forefoot <strong>and</strong> the midfoot with the same easeof use demonstrated in the rearfoot <strong>and</strong> the leg. The useof the TSP in the butt frame configuration affords thereconstructive surgeon with a simplified application for bothdistraction <strong>and</strong> compression in 3 dimentions.SURGICAL TECHNIQUEThe butt frame configuration derives its name from acarpenters end to side abutment joint. This is constructedusing either a long or short foot plate <strong>and</strong> a ring or shortfoot plate on the tibia (Figure 2).The application of the fixator begins with the planningstages preoperatively. Attention must be paid to the shapeof the patient’s leg <strong>and</strong> the amount of torque that will benecessary in the distraction phase of the deformity. Patientswith a large posterior leg may benefit from using threequarterrings or a short foot plate at tibial positions. Thiswill allow for the posterior leg soft tissue to move freelywithout being caught on the posterior portion of the ring.Most often 2 tibial rings are used with 4 total half pins. Theuse of trans-osseous wires is appropriate here as well. If thepatient is in a fixed varus or valgus <strong>and</strong> a large amount oftorque will be necessary multiple tibial fixation points <strong>and</strong>rings will be necessary.The fixator may be applied in a rings-first manner orwith the foot plate that the distracters will be attached tooff of the tibial construction. The alignment of the tibialrings with the foot plate attached often proves to beeasier especially for someone using the butt frameconfiguration for the first time. In either case the tibialFigure 1. Taylor spatial frame st<strong>and</strong>ard construction.Figure 2. <strong>Application</strong> of Taylor spatial butt frame <strong>and</strong> alignment of thetibal rings <strong>and</strong> foot.
200CHAPTER 33rings are applied to the tibia allowing for enough space forthe posterior leg <strong>and</strong> the ability to potentially convert thebutt frame configuration to a st<strong>and</strong>ard TSF is desired laterduring the postoperative process. Care must be taken toallow enough room for the placement of the foot plate <strong>and</strong>the distal distraction ring with the distracters in place onthe foot. Once the foot plate is in place <strong>and</strong> attached to thetibial rings, the distal distraction plate is fixated thoughthe distal foot area using trans-osseous wires. In some casesit may be possible to use half pins depending on the sizeof the bones to be distracted or compressed.However, trans-osseous wires allow better control ofthe foot during three dimensional distractions althoughthey lack the stiffness characteristics of half pins.Following the application of the distal ring thedistracters are attached. The surgeon may now manuallydistract the foot in the desired direction <strong>and</strong> set the clampson the distracters. The application process is shown inFigures 3-8. At this time the numbers on the distractersare recorded <strong>and</strong> the data entered into the computerprogram. The computer program will provide a printoutfor the patient <strong>and</strong> the surgeon for the daily distractionprocess. It is important that the surgeon underst<strong>and</strong> therotation <strong>and</strong> the length of distraction that will be necessaryfor the numbers to take the deformity in the direction it issupposed to go. When placing the trans-osseous wiresthrough the forefoot, the surgeon must be cautious thatthe attachment sites for the distracters are not used for thewires. There is a limited amount of connection holesbetween the distracter connection holes. Good underst<strong>and</strong>ingof the spatial relationship of the wires <strong>and</strong> thedistracters will help avoid impingement of the two duringthe distraction or compression phase of treatment.INTRAOPERATIVE CAREThe patient <strong>and</strong> the surgeon will distract or compress thedeformity on a daily basis in most cases. Soft tissuedeformities can be distracted at a rate of 1 mm per day ata minimum. It may be possible to distract larger amountsdepending on the patient’s tolerance to pain. Cautionshould be taken to keep from fracturing bone due toexcessive or quick distraction. If an osteotomy has beenmade <strong>and</strong> the distraction is performed to grow bone whilecorrecting the deformity, then the usual rate of 1 mm perday is recommended beginning at approximately 7 dayspostoperative. Soft tissue distraction does not require apostoperative waiting period. Daily pin care is required asis normal with all external fixators. Drainage should beexpected from the distal foot wires as there is a significantamount of tension on the skin during distraction.Distraction will often cause the skin to cut as the wiresmove distally. This area can become irritated <strong>and</strong> needs tobe addressed with daily wound care. Radiographs takenthroughout the postoperative process will allow thesurgeon to check the progress <strong>and</strong> assess any neededcorrections in distraction planes.Following the adequate distraction of the deformitymultiple options become available. In some cases anosteotomy may be used with or without bone grafting.There are instances when the deformity can be pinned inthe new position <strong>and</strong> then compressed with the samefixation intact. The fixator may be reconfigured with thereplacement of the distracters with threaded rods or to ast<strong>and</strong>ard TSF configuration.Figure 3. Dorsal alignment view with the footcentered on the tibial rings.Figure 4. Plantar view showing alignment of the leg <strong>and</strong> foot with theTaylor spatial butt frame.
CHAPTER 33 201Figure 5. Lateral alignment with the foot centered for distraction.Figure 6. Final lateral view with distracters <strong>and</strong> distal foot ring in place.Figure 7. Final plantar view with distracters <strong>and</strong>foot ring.Figure 8. Final dorsal view of Taylor spatial buttframe.DISCUSSIONSince the early 1990s there has been debate about the useof external fixation in foot <strong>and</strong> ankle surgery. Often, thisdebate is centered between those staunchly in favor ofinternal fixation versus external fixation. To add to thisdebate are those practitioners who consider themselves tooold to learn about this at this point in their careers <strong>and</strong> thosewho were not taught the proper technique during theirresidencies. This has been debated in the literature for manyyears <strong>and</strong> extreme statements have been made on the partof both sides. So what is the truth in this old debate?There is a middle ground. In the h<strong>and</strong>s of a properlytrained surgeon there is no more powerful tool fordeformity reduction than external fixation. However,patient deformity characteristics <strong>and</strong> selection are the keyto good postoperative results. The TSF <strong>and</strong> the butt frameconfiguration are excellent tools to be used in thecorrection <strong>and</strong> fixation of deformities. Contrary topopular belief by both sides of the debate there is mostdefinitely room for strategies involving both internal <strong>and</strong>external fixation.The strategy for the use of the TSF butt frame must becentered on the deformity, the patient, <strong>and</strong> the possibilityof gaining a satisfactory result. Distraction may not alwayslead to the complete reduction of the deformity. In manycases the distraction of the deformity allows for reductionof the overall deformity followed by bone grafting <strong>and</strong>further stabilization. Multiple revisions may be necessaryduring the postoperative process. However, distractiondoes allow for the correction of deformities not possiblewithout excessive soft tissue dissection <strong>and</strong> risk. It isalways important for the physician <strong>and</strong> the patient tounderst<strong>and</strong> that not all deformities are “exfixable” <strong>and</strong> notall deformities are fixable.