QOF Plus Year 1 - Imperial College London
QOF Plus Year 1 - Imperial College London
QOF Plus Year 1 - Imperial College London
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Towards world class healthcare for all
<strong>QOF</strong>+ report on alcohol ............................................................................................................ 27Proposed indicators ........................................................................................................................... 27Background ........................................................................................................................................ 27Priority and relevance to national policy ........................................................................................... 28Prevalence of condition ..................................................................................................................... 28Associated morbidity and mortality .................................................................................................. 28Local context ...................................................................................................................................... 29Review of evidence to support the proposed indicators ................................................................... 29Degree of perceived professional consensus .................................................................................... 30Degree of perceived support from patients and carers .................................................................... 30Impact on health inequalities ............................................................................................................ 30Health impact .................................................................................................................................... 30Workload and training implications .................................................................................................. 31References ......................................................................................................................................... 31<strong>QOF</strong>+ report on smoking .......................................................................................................... 33Proposed indicators ........................................................................................................................... 33Background ........................................................................................................................................ 33Priority and relevance to national policy ........................................................................................... 34Prevalence of condition ..................................................................................................................... 34Associated morbidity and mortality .................................................................................................. 34Local context ...................................................................................................................................... 35Review of evidence to support proposed indicators ......................................................................... 35Degree of perceived support from professionals .............................................................................. 35Degree of perceived support from patients and carers .................................................................... 35Impact on health inequalities ............................................................................................................ 35Health impact .................................................................................................................................... 36Workload and training implications .................................................................................................. 36References ......................................................................................................................................... 37<strong>QOF</strong>+ report on smoking in pregnancy .................................................................................... 39Proposed Indicators ........................................................................................................................... 39Background ........................................................................................................................................ 39Priority and relevance to national policy ........................................................................................... 39Prevalence of condition ..................................................................................................................... 40Associated morbidity and mortality .................................................................................................. 40Local context ...................................................................................................................................... 40Evidence to support the proposed indicators ................................................................................... 41Degree of perceived professional consensus .................................................................................... 41Degree of perceived support from patients and carers .................................................................... 41Impact on health inequalities ............................................................................................................ 41Health impact .................................................................................................................................... 42Workload and training implications .................................................................................................. 42References ......................................................................................................................................... 43
<strong>QOF</strong>+ report on breastfeeding ................................................................................................. 45Proposed Indicators ........................................................................................................................... 45Background ........................................................................................................................................ 45Priority and relevance to national policy ........................................................................................... 46Prevalence of condition ..................................................................................................................... 46Associated morbidity and mortality .................................................................................................. 46Local context ...................................................................................................................................... 47Review of evidence to support the proposed indicator .................................................................... 47Degree of perceived professional consensus .................................................................................... 49Degree of perceived support from patients and carers .................................................................... 49Impact on health inequalities ............................................................................................................ 49Health Impact .................................................................................................................................... 49Workload and training implications .................................................................................................. 49References ......................................................................................................................................... 50<strong>QOF</strong>+ report on ethnicity.......................................................................................................... 51Proposed Indicators ........................................................................................................................... 51Background ........................................................................................................................................ 51Priority and relevance to national policy ........................................................................................... 52Demography ...................................................................................................................................... 52Associated Morbidity and Mortality .................................................................................................. 53Local context ...................................................................................................................................... 53Review of evidence to support proposed indicators ......................................................................... 53Degree of perceived support from professionals .............................................................................. 54Degree of perceived support from patients and carers .................................................................... 54Impact on health inequalities ............................................................................................................ 54Health impact .................................................................................................................................... 54Workload and training implications .................................................................................................. 55References ......................................................................................................................................... 55<strong>QOF</strong>+ report on records ........................................................................................................... 57Proposed indicators ........................................................................................................................... 57Background ........................................................................................................................................ 57Priority and relevance to national policy ........................................................................................... 58Prevalence of conditions ................................................................................................................... 58Local context ...................................................................................................................................... 59Review of evidence to support the proposed indicators ................................................................... 60Degree of perceived professional consensus .................................................................................... 61Degree of perceived support from patients and carers .................................................................... 61Impact on health inequalities ............................................................................................................ 61Health impact .................................................................................................................................... 61Workload and training implications .................................................................................................. 62References ......................................................................................................................................... 63
<strong>QOF</strong>+ report on new patient screening .................................................................................... 65Proposed indicator ............................................................................................................................ 65Background ........................................................................................................................................ 65Priority and relevance to national policy ........................................................................................... 66Prevalence of condition ..................................................................................................................... 66Associated morbidity and mortality .................................................................................................. 66Local context ...................................................................................................................................... 66Review of evidence to support the proposed indicators ................................................................... 67Degree of perceived professional consensus .................................................................................... 67Degree of perceived support from patients and carers .................................................................... 67Impact on health inequalities ............................................................................................................ 67Health impact .................................................................................................................................... 67Workload and training implications .................................................................................................. 68References ......................................................................................................................................... 68<strong>QOF</strong>+ report on patient information ........................................................................................ 69Proposed indicators ........................................................................................................................... 69Background ........................................................................................................................................ 69Priority and relevance to national policy ........................................................................................... 71Local context ...................................................................................................................................... 71Review of evidence to support the proposed indicators ................................................................... 72Degree of perceived professional consensus .................................................................................... 72Degree of perceived support from patients and carers .................................................................... 73Impact on health inequalities ............................................................................................................ 73Health impact .................................................................................................................................... 73Workload and training implications .................................................................................................. 74References ......................................................................................................................................... 75<strong>QOF</strong>+ report on patient experience ......................................................................................... 77Proposed indicators ........................................................................................................................... 77Background ........................................................................................................................................ 78Priority and relevance to national policy ........................................................................................... 79Local context ...................................................................................................................................... 79Review of evidence to support the proposed indicators ................................................................... 80Degree of perceived professional consensus .................................................................................... 82Degree of perceived support from patients and carers .................................................................... 82Impact on health inequalities ............................................................................................................ 82Health impact .................................................................................................................................... 82Workload and training implications .................................................................................................. 82References ......................................................................................................................................... 83
<strong>QOF</strong>+ report on patient safety ................................................................................................. 85Proposed indicators ........................................................................................................................... 85Background ........................................................................................................................................ 86Priority and relevance to national policy ........................................................................................... 87Local context ...................................................................................................................................... 87Review of evidence to support the proposed indicators ................................................................... 88Degree of perceived professional consensus .................................................................................... 89Degree of perceived support from patients and carers .................................................................... 89Impact on health inequalities ............................................................................................................ 90Health impact .................................................................................................................................... 90Workload and training implications .................................................................................................. 90References ......................................................................................................................................... 90Training and support requirements for <strong>QOF</strong>+ .......................................................................... 91Introduction ....................................................................................................................................... 91Training and support requirements for selected existing <strong>QOF</strong> indicators ......................................... 91Training and support requirements for new <strong>QOF</strong>+ indicators .......................................................... 92
Appendix 1 – Background to the <strong>QOF</strong>+ development process ..................................................... 100Composition of the <strong>QOF</strong>+ development group ............................................................................... 100Process employed by the <strong>QOF</strong>+ development group ...................................................................... 100Approach to development of the scheme ....................................................................................... 100Appendix 2 – Methodology for the extension of existing clinical <strong>QOF</strong> targets .............................. 102Selection of candidate existing indicators for revised upper thresholds ......................................... 102Methodology for revised target setting for existing clinical indicators ........................................... 103Methodology for point allocation for existing clinical indicators .................................................... 106Minimum attainment thresholds .................................................................................................... 109Exception reporting ......................................................................................................................... 110List turnover ..................................................................................................................................... 115References ....................................................................................................................................... 115Appendix 3 – Current levels of attainment and exception reporting for existing clinical indicators 116Purpose of these data ...................................................................................................................... 116Data sources .................................................................................................................................... 116Using the graphs .............................................................................................................................. 117Asthma 6 .......................................................................................................................................... 118BP 5 .................................................................................................................................................. 119CHD 6 ............................................................................................................................................... 120CHD 8 ............................................................................................................................................... 121CHD 10 ............................................................................................................................................. 122CS 1 .................................................................................................................................................. 123DM 12 .............................................................................................................................................. 124DM 17 .............................................................................................................................................. 125DM 20 .............................................................................................................................................. 126MH 6 ................................................................................................................................................ 127Stroke 6 ............................................................................................................................................ 128Stroke 8 ............................................................................................................................................ 129Appendix 4 – Methodology for the design and development of the new indicators for <strong>QOF</strong>+ ...... 130Methodology for the creation of new indicator areas long list ....................................................... 130Consultation with local stakeholders to select priority areas for the development of <strong>QOF</strong>+indicators ......................................................................................................................................... 132Methodology for the development of new indicators .................................................................... 134Consultation with local practices ..................................................................................................... 135Assessment of new indicators ......................................................................................................... 135Response to feedback on proposed new indicators ........................................................................ 136Final consultation with local practices ............................................................................................. 137Methodology for point allocation for the new <strong>QOF</strong>+ indicators ..................................................... 137Communication with the PCT’s health informatics team ................................................................ 138Appendix 5 – Methodology for the development of the training and support package ................. 140Development of the training and support package ......................................................................... 140Results of data analysis of practice achievement for selected existing <strong>QOF</strong> indicators .................. 141Results of practice training and support needs assessment ........................................................... 141Appendix 6 – Summary of the <strong>QOF</strong>+ scheme ............................................................................. 142
CreditsProject boardJosip CarMiles FreemanYvonne OdegbamiAzeem MajeedArti MainiBecky WellburnChristopher HuckvaleSian ClaptonHakan AkozekXavier YiboweiProject Executive, Academic & Clinical leadjosip.car@hf-pct.nhs.ukProject Executive, Management leadmiles.freeman@hf-pct.nhs.ukProject ManagerAcademic and Clinical AdvisorClinical <strong>QOF</strong>+ CoordinatorNon-clinical <strong>QOF</strong>+ Coordinator<strong>QOF</strong>+ AnalyticsProject Finance OfficerChief Information OfficerHead of InformaticsProject governanceHakan AkozekJosip CarFrances DonellyMiles FreemanChristopher MillettAlison WilliamsDagmar ZeunerDeputy Director of Informatics and QualityPEC Chair & Medical DirectorProject Director for Primary Care QualityDirector of Primary Care and CommissioningConsultant in Public HealthDirector of FinanceDirector of Public HealthContributorsRiyadh Alshamsan (Doctoral researcher in health economics)Josip Car (PEC Chair & Medical Director, GP and Director of e·Health Unit)Miles Freeman (Interim Director of Primary Care)Christopher Huckvale (Honorary research associate in e·Health)Elizabeth Koshy (Academic GP & honorary clinical research fellow)Arti Maini (Academic GP & honorary clinical research fellow)Azeem Majeed (Head of Department and Professor of Primary Care)Christopher Millett (Academic Consultant in Public Health)David Morley (Health informatics team)Sam Nemonique (GP on clinical leadership training)Shanker Vijayadeva (GP & honorary clinical research fellow)Jill Waddingham (<strong>QOF</strong>+ Resource Pack Co-ordinator)Becky Wellburn (Head of Primary Care Commissioning)Xavier Yibowei (Health informatics team)Dominik Zenner (GP and Specialist Registrar in Public Health)Dagmar Zeuner (Director of Public Health)
Delphi local stakeholder consultation groupJosip Car, Miles Freeman, Sheraz Khan, Paul Skinner, Tony Willis, Dagmar ZeunerHealth informatics teamHakan Akozek, Christopher Huckvale, David Morley, Richard McSharry, Xavier Yibowei
AcknowledgementsWe are indebted to the valuable contribution made by the following individuals and groups.Dr Ike AnyaDr Mark AshworthProfessor Richard BakerPatricia CaddenChristopher CorfieldGloria-Anne CoxDr Tim DoranProfessor Colin DrummondRachel HaffendenLynne JonesProfessor Helen LesterChristine McCruddenProfessor Martin RolandProfessor Aziz SheikhDr Michael SoljakTom StevensonDr Richard WilliamsConsultant in Public Health, NHS Hammersmith and FulhamKings <strong>College</strong> <strong>London</strong>University of LeicesterSenior Substance Misuse Commissioning Manager<strong>London</strong> Borough of Hammersmith and FulhamChief Pharmacist, NHS Hammersmith and FulhamHammersmith and Fulham TB Action GroupUniversity of ManchesterKings <strong>College</strong> <strong>London</strong>Hammersmith and Fulham TB Action GroupDesignated Nurse for Child ProtectionHammersmith and FulhamUniversity of ManchesterHammersmith and Fulham TB Action GroupUniversity of ManchesterUniversity of Edinburgh<strong>Imperial</strong> <strong>College</strong>, <strong>London</strong>Head of Communications, NHS Hammersmith and FulhamLambeth PCTThe NHS Information CentreGPRD Group, Medicines and Healthcare Products Regulatory AgencyProfessional Executive Committee (PEC), NHS Hammersmith and FulhamPlanning and Strategy Group, NHS Hammersmith and FulhamWe would like to thank all the general practices of Hammersmith and Fulham who participated in the<strong>QOF</strong>+ consultation process.In addition, we would like to acknowledge the work of the <strong>QOF</strong> Review; a collaboration between theUniversities of Birmingham and Manchester, the Society of Academic Primary Care and the Royal <strong>College</strong>of General Practitioners which is led by co-directors Professors Richard Hobbs (UoB) and Helen Lester(UoM). We based the structure of the <strong>QOF</strong>+ reports on that used in the reports produced through the<strong>QOF</strong> Review.
Foreword<strong>QOF</strong> <strong>Plus</strong> has high ambition - to deliver world class healthcare. It focuses on helping peoplelive healthier and longer lives, and above all aims to dramatically reduce health inequalities.To achieve this vision of better care for all <strong>QOF</strong> <strong>Plus</strong> builds on existing systems for quality in primary careand uses the best international evidence to extend these. We know that improving quality is not easy. Yetwe also know that it is possible when priorities and the approach to change are right. With <strong>QOF</strong> <strong>Plus</strong> wehave focused on what matters and makes a difference for both patients and clinicians. We have built intothe implementation the best evidence on support for quality improvement. In particular, we want toensure that individual practices and clinicians are enabled in transforming their clinical practice to make itof consistently high quality.This publication is accompanied by a support resource pack, guidance on business and financial rules,EMIS and Vision templates for health monitoring, details of a series of training events, visits andworkshops. Most importantly, <strong>QOF</strong> <strong>Plus</strong> is supported by a committed clinical, academic and managementteam which aims to provide a range of multimodal supportive strategies to address, in real time, areas ofchallenge. This is the most significant investment into quality improvement in primary care since theintroduction of <strong>QOF</strong>.This innovative scheme, developed jointly with experts in our local Department of Primary Care and SocialMedicine at <strong>Imperial</strong> <strong>College</strong>, combines a strong evidence-based approach with meaningful engagementand consultation with local practices and stakeholders. <strong>QOF</strong> <strong>Plus</strong> has been designed in line with nationalguidance and addresses a range of important national and local health service priorities. It builds on theanalysis of the public health needs of Hammersmith and Fulham, and on what local people have told usthey want.Advice offered by national and international experts in health care quality improvement has played asignificant role in helping determine the vision and implementation strategy for <strong>QOF</strong> <strong>Plus</strong>, ensuring thatwe learn from past experience in the field. The key individuals involved in designing and developing <strong>QOF</strong><strong>Plus</strong> believe passionately in – and are fully committed to – the principles embodied by the scheme,namely achieving excellence in healthcare for all people and reducing health inequalities; ensuring thehealthcare needs of those most vulnerable are addressed. This team is championing the scheme and will,in partnership with patients and colleagues in primary care, work to make it a success.I am sincerely grateful to all that have contributed to this important project that brings new dynamism toprimary care embodying some of the key principles of Lord Darzi’s Next Stage Review. I believe <strong>QOF</strong> <strong>Plus</strong>will make a real difference to the people of Hammersmith and Fulham. I also hope that this work willmake a valuable contribution to the current national debate about the future direction of <strong>QOF</strong>, and serveas a model for other PCTs wishing to initiate similar schemes.Sarah WhitingCEO, NHS Hammersmith and Fulham, December 2008
Executive summaryIntroductionPrevious work has highlighted several limitations of the national Quality and Outcomes Framework (<strong>QOF</strong>)including insufficient focus on health outcomes, primary prevention, prioritised local health needs andbenefits. <strong>QOF</strong> may not encourage practices in reaching the more challenging patients, as practices do notreceive further incentives once they have received the upper payment threshold. It is anticipated thatintroduction of a local <strong>QOF</strong> will help address these limitations.AimsThis document describes a joint venture by NHS Hammersmith and Fulham and the Department ofPrimary Care and Social Medicine at <strong>Imperial</strong> <strong>College</strong> <strong>London</strong> to design and develop a local <strong>QOF</strong> forHammersmith and Fulham (<strong>QOF</strong>+) which is in line with current national guidance, developed through theprocess of effective clinical engagement and which aims to have a greater emphasis on prevention,address local needs, accelerate improvement and reduce inequity.MethodologyEngagement with local practices and other local provider services, feedback from patients and discussionswith national and international experts in health care quality improvement provided insights whichinformed the development of the scheme.A number of existing <strong>QOF</strong> indicators were identified as candidates that might benefit from additionalincentivisation through the provision of revised upper targets. Indicator selection was weighted towardsthose whose attainment confers significant potential health benefits at a population level and wherecurrent attainment in Hammersmith and Fulham is below that seen nationally.Potential sources for new indicator areas were identified and prioritised on the basis of being both localand national priorities. These were subjected to a structured consultation with local stakeholders to selectareas for indicator development for the first year of the scheme through a consensus process.Literature reviews of the evidence base were undertaken for each selected indicator area to informdevelopment of indicators.Proposed new indicators were assessed using the Organisation for Economic Cooperation andDevelopment (OECD) criteria of importance, scientific soundness and feasibility. Each indicator was alsoassessed for clarity. This assessment was informed by the views of local practices, a local stakeholderpanel (through a structured consultation with the aim of achieving consensus for the clinical and recordsdomains), local provider services and national and international experts in the proposed indicator areas.
Like <strong>QOF</strong>, <strong>QOF</strong>+ includes a combination of all-or-northing and payment stage indicators, re-uses theconcept of exception reporting and determines remuneration using a system of population andprevalence-weighted point allocation. The PCT Health Informatics Team was consulted to ensure thatproposed indicators would work within primary care IT systems.The development of a training and support package to support <strong>QOF</strong>+ was informed by consultation withlocal and national experts, analysis of data on achievement for existing <strong>QOF</strong> for individual practices, and atraining and support needs assessment conducted among all local practices.OutcomesThrough <strong>QOF</strong>+, practices will be rewarded with <strong>QOF</strong>+ points for achievement of higher thresholds for aselected number of existing national <strong>QOF</strong> indicators including the following:Asthma 6, BP 5, CHD 6, CHD 8, CHD 10, CS 1, DM 12, DM 17, DM 20, MH 6, Stroke 6, Stroke 8.Additionally, practices will be rewarded for achievement of new <strong>QOF</strong>+ indicators which have beendeveloped in clinical and non-clinical domains covering the following areas: Cardiovascular DiseasePrimary Prevention, Alcohol, Smoking Cessation (including Smoking in Pregnancy) Breastfeeding,Ethnicity, Records, New Entrant Screening (for Tuberculosis), Patient Information, Patient Experience andPatient Safety.Anonymised medical records of all registered patients will be stored centrally by the PCT through the useof the APOLLO IT system by practices. This will enable analysis of performance, improved practiceprofiling, equity assessment using patient-level data, and provision of monthly feedback of performanceto practices, as part of a wider training and support package which has been developed to support <strong>QOF</strong>+.© Copyright NHS Hammersmith and Fulham 2008© Copyright eHealth unit, Department of Primary Care and Social Medicine, <strong>Imperial</strong> <strong>College</strong> 2008
Support with <strong>QOF</strong>+If you have a problem with any of the IT aspects of <strong>QOF</strong>+, please contact:This service is available to NHS Hammersmith and Fulham practices only.Additional <strong>QOF</strong>+ resources and content are available to download from:requires N3 connectionFor all other enquiries:For general help and support with any aspect of <strong>QOF</strong>+, there is a dedicated email address:Hammersmith and Fulham practices can also contact their commissioning manager.
Introduction to <strong>QOF</strong>+Improving the quality of primary care services inHammersmith and FulhamContextThe purpose of this paper is to provide the rationale and describe the process for implementing amajor quality improvement initiative for primary care services in Hammersmith and Fulham,called <strong>QOF</strong>+. The initiative has been developed by NHS Hammersmith and Fulham in partnershipwith the eHealth unit of the Department of Primary Care & Social Medicine at <strong>Imperial</strong> <strong>College</strong><strong>London</strong>.NHS Hammersmith and Fulham has identified quality improvement in primary care as a key localpriority. The PCT has earmarked over £2 million annual funding to implement a comprehensivelocal financial incentive scheme (<strong>QOF</strong>+) over the next three years (2008/09, 2009/10, 2010/11).The aims of this scheme are to achieve a step-change in quality and address local priorities.Subject to a positive evaluation, this funding is likely to be extended beyond this period.Defining and measuring the quality of healthcareThere are currently no internationally agreed definitions of healthcare quality. Maxwell (1983)offers six dimensions of quality in healthcare including appropriateness, equity, accessibility,effectiveness, acceptability and efficiency. One of the most widely adopted definitions of qualityis provided by the Institute of Medicine: "The degree to which health services for individuals andpopulations increase the likelihood of desired health outcomes and are consistent with currentprofessional knowledge” (Institute of Medicine, 2001). Performance indicators are designed tomeasure the extent to which health services meet this goal (Majeed, 1995).There has been an increased interest in measuring the quality of care over the past decade. Inparallel, there have been significant developments in databases, both administrative and clinical,which have enabled collection of routine information on quality. These factors have significantlyinfluenced the development and implementation of performance indicators (Majeed et al., 2007).International evidence underlines the importance of high quality primary care in achieving aneffective and efficient health care system and in improving population health (Starfield, 2001).Whilst recent investment in quality initiatives in the UK has led to considerable improvements inprimary care, the quality of service provision remains variable in many areas (Gray et al., 2007;Hippisley-Cox et al., 2004).1
The quality and outcomes framework (<strong>QOF</strong>)April 2004 saw the introduction of the Quality and Outcomes Framework (<strong>QOF</strong>) as part of theNew Contract for General Practitioners where pay was linked to performance with the purpose ofdriving up standards for primary care. The framework includes quality and performanceindicators in a number of domains, including clinical, organisational and patient experience, aswell as additional areas such as cervical screening (Roland et al., 2004). The quality measures in2004 were largely drawn from existing national guidelines, and were designed to reflect widelyaccepted standards of clinical care. The contract was significantly revised in 2006 following arenegotiation, with the addition of nine areas, changes in indicators and increased thresholds forpayment.Impact of the quality and outcomes frameworkGPs have achieved high scores in the <strong>QOF</strong> in each of the first three years of the scheme. In 2006-07 practices in England achieved an average of 954.5 points, (95.5 percent of the 1,000 available).This compares with an average achievement of 96.2 per cent in 2005-06 and 91.3 percent in2004-05 against the 1,050 points then available (National Audit Office, 2008).Early data suggests the introduction of the <strong>QOF</strong> has shown moderate improvements in outcomesfor patient care in some long term conditions such as asthma and diabetes, but not for otherssuch as coronary heart disease (Campbell et al., 2007).Future changes to the quality and outcomes frameworkBuilt into the new GMS contract is the expectation that <strong>QOF</strong> will evolve over time. The focus inthe first few years of <strong>QOF</strong> has been on process measures as a first step towards achieving goodoutcomes. Lester (2008) further comments that “In future, perhaps pay for performance schemesshould be actively designed with health inequalities in mind.”As part of the NHS Next Stage Review, the Department of Health announced proposals for furtherdeveloping the Quality and Outcomes Framework (<strong>QOF</strong>) including an independent andtransparent process for developing and reviewing indicators. The Review outlined plans to discusswith the National Institute for Health and Clinical Excellence (NICE) and with professional andpatient groups how this new process should work, and to explore the possibility of allowing PCTsgreater flexibility to select indicators (from a national menu) that reflect local healthimprovement priorities (Darzi, 2008).The National Audit Office (NAO) report on GP contract modernisation (National Audit Office2008) recommended that the Department of Health should:develop a long term strategy to support yearly negotiations on <strong>QOF</strong>, anddevelop <strong>QOF</strong> based on patients’ needs and in a transparent way,base the strategy more on outcomes and cost effectiveness, andagree to allocate a proportion of <strong>QOF</strong> indicators for local negotiation at Strategic HealthAuthority (SHA) or PCT level.2
The Department of Health is currently consulting on the proposal to ask NICE to oversee a newindependent, transparent and objective process for developing and reviewing <strong>QOF</strong> clinical andhealth Improvement indicators for England from 1 April 2009 (DoH, 2008).The Department of Health is also consulting on the proposal that Primary Care Trusts (PCTs)should have flexibility to select additional indicators from the NICE menu to reflect localpriorities.The Royal <strong>College</strong> of General Practitioners is planning to develop and roll out nationally by 2010an accreditation scheme for GP practices. It is proposed that this scheme will serve as a vehicle todrive organisational quality improvement, and this is likely to have a significant impact on thearrangements for incentivising organisational quality through the Quality and OutcomesFramework (National Primary Care Research and Development Centre, 2008).Limitations of the quality and outcomes frameworkThe National Audit Office (2008) and Fleetcroft el al. (2006) have highlighted a number oflimitations of the national <strong>QOF</strong>: incentivised clinical areas in <strong>QOF</strong> may not reflect local populationhealth needs, indicators are insufficiently focused on health outcomes, and rewards areinsufficiently aligned with prioritised health need or health benefit.Payment thresholds have arguably been set too low, so that standards recommended in nationalclinical guidelines are not being achieved for most patients (Fleetcroft et al., 2008). There is someevidence that improvements in care associated with <strong>QOF</strong> have not occurred in all groups, e.g.ethnic minorities, thereby potentially worsening health inequalities (Gray et al., 2007). Qualityindicators in <strong>QOF</strong> have not been sufficiently weighted towards primary prevention (Darzi, 2008).In addition, Short (2007) notes discrepancies between <strong>QOF</strong> and NICE guidance in certain areasand comments that “there needs to be some clarity and stream-lining of guidance betweenprimary care and major clinical governing bodies.” NICE is currently examining the fit between<strong>QOF</strong> and the evidence-based NICE guidelines (Leech, 2008).The role of healthcare in addressing health inequalitiesThe principle of social justice incorporated into the Physician’s Charter (Medical ProfessionalismProject: ABIM Foundation 2002) states that “the medical profession must promote justice in thehealthcare system” and that physicians should “work actively to eliminate discrimination inhealthcare, whether based on race, gender, socio-economic status, ethnicity, religion or anyother social category.” One of the professional responsibilities included in the Physician’s Charterinvolves improving access to care. This requires that physicians must “individually and collectivelystrive to reduce barriers to equitable health care.”3
Effect of measurement on health inequalityMant (2008) comments that “in everyday clinical practice, variability in usual care matters mostat the tail-end of the distribution where poor care can lead to adverse outcomes includingavoidable death.” Evidence from epidemiological studies suggest that while effective regularmechanisms for dealing with poor care are essential, a more effective approach is to developstrategies for raising average performance, and therefore shifting the whole distribution (Rose etal., 1990). An example of this is the introduction of cervical smear targets for UK general practicesin 1990. The highest targets were achieved rapidly by practices in affluent areas, and this resultedin an initial widening of the health inequality gap. However, practices in more deprived areascaught up over the next few years, thereby reducing inequality (Baker et al., 2003; Middleton etal., 2003). This phenomenon has been termed the inverse equity hypothesis (Victora et al., 2000).This hypothesis predicts that the benefits of new public health interventions are initiallyexperienced by the wealthier sector of the population and later by the poor, increasing theinequity ratio. However, once the poor have experienced benefits and a ceiling effect is reachedin the richer population, the inequity ratio which initially increases, then decreases.Although the Quality and Outcomes Framework was not designed to tackle health inequalities(Roland, 2004), there is evidence of the inverse equity hypothesis being relevant to <strong>QOF</strong>. Data isnow emerging which suggests that from a longer term perspective, more equitable healthcare isbeing generated following the introduction of <strong>QOF</strong> (Lester, 2008). Ashworth et al. (2008) assessedthe effects of social deprivation on levels of BP monitoring and control using data from over 97%of practices in England over the first three years of the <strong>QOF</strong>. They found that:“Since the reporting of performance indicators for primary care and the incorporation ofpay for performance in 2004, blood pressure monitoring and control have improvedsubstantially. Improvements in achievement have been accompanied by the neardisappearance of the achievement gap between least and most deprived areas.”Doran et al. (2008) looked at overall achievement in 48 of the clinical indicators in <strong>QOF</strong> and foundthat median achievement score increased across the board, with the gap in median achievementbetween practices in the most and least deprived areas reducing considerably.The evidence suggests that “low scoring practices in deprived areas also seem just as able toimprove the quality of their care (as measured by the Framework) as low scoring practices inmore affluent areas” (Lester, 2008). Lester (2008) further comments that:“Overall, the financial incentives seem to have reached areas of high need relativelyeffectively for most targets. An important subsidiary message is the need to take a longterm view when interpreting the effects of quality measures on health inequalities.”However, there remains concern that <strong>QOF</strong> may not encourage practices in reaching the morechallenging, hard-to-reach patients, as practices do not receive further incentives once they haveachieved the 90% upper threshold for payment (National Audit Office, 2008). This meanspractices can receive maximum points and payment for every clinical indicator before all eligiblepatients receive indicated care. Fleetcroft et al. (2008) comment that this can result in an‘incentive ceiling effect’ with associated reductions in health gains, and state that “there may beno rationale for maximum target thresholds to be set below 100% as there are comprehensivereasons for exception reporting any patient who would not theoretically benefit from theindicated care”. Setting and rewarding achievement of higher thresholds for selected existing4
<strong>QOF</strong> indicators may therefore help to address this issue, with the aim of achieving additionalhealth gains in a more challenging group of patients.Why have a local <strong>QOF</strong>?Local Enhanced Services (LES) already provide scope for local development within the GMScontract. The purpose of these is to allow PCTs to tackle local problems not addressed in thenational <strong>QOF</strong>. These may include a greater emphasis on prevention and strategies designed toreduce inequity. It is anticipated that introduction of a local <strong>QOF</strong> would confer a number ofadvantages, including more robust performance reporting, mainstreaming quality throughtemplates and coverage of a greater number of areas.The concept of developing a local <strong>QOF</strong> has recently received backing from the National AuditOffice (2008) and the NHS Next Stage Review (Darzi, 2008).Development and implementation of a local <strong>QOF</strong> may also contribute to PCTs fulfilling theirfunctions as World Class Commissioners. The Department of Health describes World ClassCommissioners as being “central to a self-improving NHS. They will operate as learningorganisations, seeking and sharing knowledge and skills. World class commissioners will also bestimulating provider and clinical innovation through improvements in experienced quality, accessand outcomes” (DoH, 2008). As part of this commissioning process, PCTs are required to “investlocally to achieve the greatest health gains and reductions in health inequalities, at best value forcurrent and future service users”.The World Class Commissioning programme (DoH, 2008) outlines a series of competencies whichcommissioners will need to reach world class status. These are:locally lead the NHSwork with community partnersengage with public and patientscollaborate with cliniciansmanage knowledge and assess needsprioritise investmentstimulate the marketpromote improvement and innovationsecure procurement skillsmanage the local health systemmake sound financial investments5
How might a local <strong>QOF</strong> operate in practice?There is ongoing debate about how a local <strong>QOF</strong> could work in practice. The Department of Healthhas proposed that to help address local health needs more effectively, PCTs should be able toselect local indicators from a national menu of indicators, for use in local voluntary incentiveschemes (DoH, 2008).An alternative is for indicators to be developed locally by PCTs. However, there are practicallimitations associated with this approach including:the need for technical expertise in the development of evidence-based indicators andbusiness rules for extraction of clinical data from GP systems;the IM&T support required to extract data from clinical systems and to link this withpayment calculations (DoH, 2008).Why have a local <strong>QOF</strong> for Hammersmith and Fulham?Evaluations of recently introduced LES and local Shared Care schemes (including CVD PrimaryPrevention, Smoking Cessation and Alcohol) in Hammersmith and Fulham highlighted a numberof problems with these schemes, in terms of their complexity and design and the level of uptakeby practices. These highlight a need for widespread implementation in a way that is easilyunderstood. There is also a need to reduce health inequalities and recognition that <strong>QOF</strong> may be avehicle to achieve this. Although it has been proposed that PCTs should have flexibility to selectlocal indicators from a national menu published by NICE, the infrastructure required to supportdevelopment of local <strong>QOF</strong>s through this approach is not anticipated to be in place until 2011/12at the earliest (DoH, 2008). It was therefore proposed that NHS Hammersmith and Fulham woulddevelop a local <strong>QOF</strong> scheme to run initially for 3 years from 2008/9-2010/11, with technicalexpertise in indicator development being provided by the Department of Primary Care and SocialMedicine at <strong>Imperial</strong> <strong>College</strong> <strong>London</strong> in conjunction with national and international experts in thisfield, and IM&T support being provided by the PCT’s Health Informatics Team.The need for clinical engagementEffective local clinical engagement is crucial to the success of service improvement initiatives andits integral role has been highlighted in the competencies of World Class Commissioning (DoH,2008) and by The NHS Alliance (2003) which states that “front-line clinical staff should beeffectively involved in redesign, service provision and in ensuring services are used costeffectively.”The NHS Alliance further highlights that the engagement of front-line professionalsat a strategic level would allow PCTs to draw on a bank of untapped knowledge resulting from thewider experiences of primary care. The involvement of local practices in helping shape <strong>QOF</strong>+ wastherefore seen as a central element of the design and development of the scheme.6
AimsThis paper describes the design and development of a local <strong>QOF</strong> for Hammersmith and Fulhamwhich is in line with current national guidance, developed through the process of effective clinicalengagement and which aims to have a greater emphasis on prevention, address local needs,accelerate improvement and reduce inequity.ReferencesAshworth M, Medina J, Morgan M (2008). Effect of social deprivation on blood pressure monitoringand control in England: a survey of data from the "quality and outcomes framework." British MedicalJournal 337:a2030Baker D, Middleton E (2003) Cervical screening and health inequality in England in the 1990s.Epidemiological Community Health 57:417-23.Campbell S, Reeves D, Kontopantelis E, Middleton E, Sibbald B, Roland M. Quality of Primary Care inEngland with the Introduction of Pay for Performance (2007). New England Journal of Medicine357:181-90.Darzi A (2008) High Quality Care for All, the final report of the NHS Next Stage Review Final Report byLord Darzi The Stationary Office. <strong>London</strong>Department of Health (2008) Developing the Quality and Outcomes Framework: Proposals for a new,independent process. [Online, Accessed November 03 2008] Available at:http://www.dh.gov.uk/en/Consultations/Liveconsultations/DH_089778Department of Health (2008) World Class Commissioning. [Online, Accessed August 10 2008] Availableat:http://www.dh.gov.uk/en/Managingyourorganisation/Commissioning/Worldclasscommissioning/index.htm7
Doran T, Fullwood C, Kontopantelis E, Reeves D (2008). Effect of financial incentives on inequalities inthe delivery of primary clinical care in England: analysis of clinical activity indicators for the quality andoutcomes framework. Lancet 372:728-36Fleetcroft, R and Cookson, R (2006) Do the incentive payments in the new NHS contract for primarycare reflect likely population health gains? Journal of Health Care Research and Policy 11:27–31.Fleetcroft R, Steel N, Cookson R, Howe A (2008) “Mind the gap!" Evaluation of the performance gapattributable to exception reporting and target thresholds in the new GMS contract: National databaseanalysis. BMC Health Services Research 8: 131Gray J, Millett C, Saxena S, Netuveli G, Khunti K, Majeed A (2007) Ethnicity and Quality of DiabetesCare in a Health System with Universal Coverage: Population-Based Cross-sectional Survey in PrimaryCare. Journal of General Internal Medicine 22:1317-20.Hippisley-Cox J, O'Hanlon S, Coupland C (2004). Association of deprivation, ethnicity, and sex withquality indicators for diabetes: population based survey of 53 000 patients in primary care. BritishMedical Journal 329:1267-9.Institute of Medicine (2001). Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC: National Academy PressLeech P (2008) <strong>QOF</strong>; Key benefits and challenges in long term conditions management.[Online, Accessed August 10 2008] Available at:www.pcc.nhs.uk/events/uploads/dr_philip_leech_17th_october.pptLester H (2008) The UK Quality and outcomes framework. British Medical Journal 337:a2095Mant D (2008) The problem with usual care. British Journal of General Practice 58:755-6Majeed FA, Voss S (1995). Performance indicators for general practice. British Medical Journal311:209-10Majeed FA, Lester H, Bindman AB (2007) Measuring Quality through Performance: Improving thequality of care with performance indicators. British Medical Journal 335: 916-8Maxwell R (1983) Seeking quality. Lancet 8314-5:45–8Medical Professionalism Project: ABIM Foundation (2002): Medical Professionalism in the NewMillennium: A Physician Charter. Annals of Internal Medicine 136:243-46Middleton E, Baker J (2003) Comparison of social distribution of immunisation with measles, mumps,and rubella vaccine, England, 1991-2001. British Medical Journal 326:854National Audit Office (2008) NHS Pay Modernisation: New Contracts for General Practice Services inEngland. The Stationary Office. <strong>London</strong>Roland M (2004). Linking physician pay to quality of care—a major experiment in the United Kingdom.New England Journal of Medicine 351:1448-54Rose G, Day S (1990). The population mean predicts the number of deviant individuals. British MedicalJournal 301:1031–34.Short K (2007) <strong>QOF</strong> vs NICE. British Journal of General Practice 57:748Starfield B (2001). New paradigms for quality in primary care. British Journal of General Practice51:303-9.Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E (2000). Explaining trends in inequities: evidencefrom Brazilian child health studies. Lancet 356:1093-88
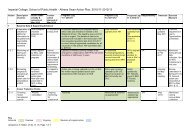
Summary of indicatorsHigher thresholds for existing Clinical <strong>QOF</strong> indicatorsPractices will receive a fixed number of <strong>QOF</strong>+ points for reaching or exceeding a revised upperthreshold for the indicators detailed below. Point awards will be in addition to those allocatedunder <strong>QOF</strong> and based on attainment at close of business on March 31 2010.<strong>QOF</strong><strong>QOF</strong>+IndicatorUpperThresholdThreshold& (Tolerance) †PointsASTHMA 6. The percentage of patients withasthma who have had an asthma review in theprevious 15mthsBP 5. The percentage of patients withhypertension in whom the last blood pressure(measured in the previous 9 months) is ≤150/90CHD 6. The percentage of patients withcoronary heart disease in whom the last bloodpressure reading (measured in the previous 15months) is ≤150/90CHD 8. The percentage of patients withcoronary heart disease whose last measuredtotal cholesterol (measured in the previous 15months) is ≤5mmol/lCHD 10. The percentage of patients withcoronary heart disease who are currentlytreated with a beta blocker (unless acontraindication or side-effects are recorded)CS 1. The percentage of patients aged from 25to 64 whose notes record that a cervical smearhas been performed in the last five yearsDM 12. The percentage of patients withdiabetes in whom the last blood pressure is≤145/8570% 95% (3%) 1070% 90% (2%) 2970% 98% (1%) 670% 87% (2%) 760% 87% (1%) 1480% 88% (7%) 3560% 86% (1%) 5Continues overleaf9
Continued…<strong>QOF</strong><strong>QOF</strong>+IndicatorUpperThresholdThreshold& (Tolerance) †PointsDM 17. The percentage of patients withdiabetes whose last measured total cholesterolwithin the previous 15 months is ≤5mmol/lDM 20. The percentage of patients withdiabetes in whom the last HBA1c is 7.5 or less inthe previous 15 monthsMH 6. The percentage of patients on theregister who have a comprehensive care plandocumented in the records agreed betweenindividuals, their family and/or carers asappropriateSTROKE 6. The percentage of patients with ahistory of TIA or stroke in whom the last bloodpressure reading (measured in the previous 15months) is ≤150/90 in the previous 15 monthsSTROKE 8. The percentage of patients with ahistory of TIA or stroke in whom the last totalcholesterol (measured in the previous 15months) is 5 mmol/l or less70% 88% (1%) 950% 77% (1%) 2050% 97% (1%) 370% 96% (1%) 660% 85% (1%) 5Under the current <strong>QOF</strong> 2009/10 proposal, DM20 will be replaced by DM23, which lowersthe target for HbA1c to ≤7.0. We recognise that attaining this more aggressive target willrequire significant effort involving potentially large numbers of patients. To rewardpractices as they progress towards the revised goal, we propose to retain DM20 within<strong>QOF</strong>+ until the end of March 2010. Since DM20 attainment status will no longer beavailable through QMAS, feedback will instead be provided through the same mechanismof monthly reporting used for the new <strong>QOF</strong>+ clinical indicators.† During consultation with practices concern was raised about the possibility, with an ‘allor-nothing’payment mechanism, of receiving no remuneration where the revised targetwas missed through accidental failures involving small numbers of patients. A range ofsolutions were considered to address this – including the use of payment ranges, similarto those of <strong>QOF</strong> – but all were felt to distract from a key aim of the revised targets, whichis to drive performance towards the best seen at a national level. It was decided to retainthe single upper threshold but to introduce a tolerance (bracketed figures in the tableabove) which lowers the threshold by the specified amount. Attainment lying at or abovethis lower figure will be remunerated by receiving half the available points. Where thepoint number is odd, the points will be divided unequally with the balance in favour ofthe tolerance payment. The existing 3-month exemption for newly registered patientswill be respected across these and the newly introduced indicators.10
New clinical <strong>QOF</strong>+ indicatorsNew indicators are distinguished from existing <strong>QOF</strong> targets by the plus (+) prefix. Blanketminimum attainment thresholds will no longer be included in year 1 of the <strong>QOF</strong>+ scheme (for more information see Appendix 2, Section A2.4). Point awards will be based on attainment atclose of business on November 30 2009.Cardiovascular disease prevention Chapter 3 (p19)Indicator<strong>QOF</strong>+pointsPaymentstages+ CVD PREVENT 1. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a Blood Pressurerecorded in the previous 17 months+ CVD PREVENT 2. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of BMImeasured in the previous 17 months+ CVD PREVENT 3. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a baseline record oftotal and HDL cholesterol recorded in the previous 17 months+ CVD PREVENT 4. The percentage of patients on the PracticeCVD At-Risk Register for whom there is a record of a fastingblood glucose in the previous 17 months+ CVD PREVENT 5. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of familyhistory of CHD in first degree relatives (parents, brothers,sisters, or children of a patient)+ CVD PREVENT 6. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of familyhistory of diabetes in first degree relatives (parents, siblings,or children of a patient)+ CVD PREVENT 7. The percentage of patients on the PracticeCVD At-Risk Register who have been offered lifestyle advice onexercise, and appropriate dietary changes within the previous17 months+ CVD PREVENT 8. The percentage of patients on the PracticeCVD At-Risk Register who have been offered statin therapy (inline with 2008 NICE guidance on Lipid Modification) as part oftheir primary prevention management strategy8 40-90%8 40-90%8 40-90%8 40-90%8 40-90%8 40-90%10 40-90%10 40-90%It is prerequisite that in order to receive payment for + CVD PREVENT 1, practices have achievedthe existing <strong>QOF</strong> RECORDS 11 Indicator (The BP of patients aged 45 and over is recorded in thepreceding 5 years for at least 65% of patients.)11
Alcohol Chapter 4 (p27)Indicator<strong>QOF</strong>+pointsPaymentstages+ ALCOHOL 1. The percentage of patients on one or morepractice registers for CVD At-Risk, Diabetes, Stroke and TIA,Hypertension and CHD who have had AUDIT-C or FASTrecorded on the practice system within the previous 17months+ ALCOHOL 2. The proportion of patients who screen positiveusing either AUDIT-C or FAST within the previous 17 monthswho are subsequently recorded as having a brief interventionfor alcohol misuse15 20-70%30 40-90%It is prerequisite that in order to receive payment for + ALCOHOL 2, practices shall have reachedthe lower threshold for + ALCOHOL 1.Smoking Chapter 5 (p33)Indicator<strong>QOF</strong>+pointsPaymentstages+ SMOKING 1. The percentage of patients aged 15 years orolder whose notes record smoking status in the past 17months, or whose most recent recorded smoking status,recorded over the age of 25, indicates that they had neversmoked+ SMOKING 2. The percentage of patients aged 15 years orolder who smoke whose notes contain a record that smokingcessation advice or referral to a local smoking cessationservice has been offered within the previous 17 months20 40-90%10 40-90%Smoking in pregnancy Chapter 6 (p39)Indicator<strong>QOF</strong>+pointsPaymentstages+ SMOKING IN PREG 1. The percentage of pregnant womenwhose notes record their smoking status at the time of theirfirst booking appointment in primary care+ SMOKING IN PREG 2. The percentage of pregnant womenwho smoke whose notes contain a record that at the time oftheir first antenatal booking appointment in primary care theyhave been given smoking cessation advice and details of thelocal NHS Stop Smoking Services and the NHS pregnancysmoking helpline (0800 169 9 169)3 70-90%5 70-90%12
BreastfeedingIndicator+ BREASTFEEDING 1. The percentage of women who arerecorded as being pregnant on or after December 01 2008,and who at their antenatal booking appointment in primarycare have been given specific information on breastfeeding,including information on breastfeeding workshops+ BREASTFEEDING 2. The percentage of babies born on orafter December 01 2008 and breast fed at 6-8 weeks whoserecord indicates that breastfeeding support contact has beenoffered to the babies’ mother at the time of the 6-8 weekcheck+ BREASTFEEDING 3. At least 80% of babies born on or afterDecember 01 2008 have a record of feeding method at thetime of the 6-8 week check<strong>QOF</strong>+points Chapter 7 (p45)Paymentstages4 70-90%6 70-90%3 -EthnicityIndicator+ ETHNICITY 1. The percentage of patients on one or morepractice registers for: CVD At-Risk, Hypertension, CHD,Diabetes, Mental Health and Stroke and TIA whose notesrecord their ethnicity and first language+ ETHNICITY 2. The percentage of patients who have newlyregistered with the practice on or after December 01 2008whose notes record their ethnicity and first language<strong>QOF</strong>+points Chapter 8 (p51)Paymentstages30 60-90%20 90-100%13
RecordsIndicator+ PRESCRIPTION 1. The percentage of individual repeatmedications issued which have a diagnosis or symptom in theelectronic medical record relating to that medication+ REFERRALS 1. The percentage of outpatient referrals madeon or after December 01 2008 where both the referred-tospeciality and diagnosis/symptom triggering referral are codedon the clinical system+ CARERS 1. Carer status is recorded for 100% of individualsnewly registered on or after December 01 2008+ OSTEOARTHRITIS 1. The practice is able to produce aregister of patients who have osteoarthritis+ RHEUMATOID ARTHRITIS 1. The practice is able to producea register of patients who have rheumatoid arthritis+ ECZEMA 1. The practice is able to produce a register ofpatients who have eczema+ PSORIASIS 1. The practice is able to produce a register ofpatients who have psoriasis<strong>QOF</strong>+points Chapter 9 (p57)Paymentstages45 40-90%50 70-90%6 -1 -1 -1 -1 -14
New non-clinical <strong>QOF</strong>+ indicatorsNew indicators are distinguished from existing <strong>QOF</strong> targets by the plus (+) prefix.New patient screening Chapter 10 (p65)Indicator+ PATIENT REGISTRATION 1. The practice is trained in and implements thePCT TB Early Referral Protocol to identify and refer patients who are newlyregistered at the Practice and who are new entrants to the UK fromcountries with a high TB prevalence<strong>QOF</strong>+points5Patient information Chapter 11 (p69)Indicator+ PATIENT INFORMATION 1. The practice uses the PCT practice informationleaflet template for patients which is designed to include information onthe following: Preventative services such as stop smoking, immunization andscreening Choice / Choose & Book PCT’s Patient Advice & Liaison Service and complaints team Walk-in and urgent care centres Practice opening times including extended hours Information for patients in a range of languages informing them oftheir right to interpreting services during appointments+ PATIENT INFORMATION 2. The practice takes responsibility for regularlyupdating practice information on the NHS choices website+ PATIENT INFORMATION 3. The practice has up to date patientinformation about local training and support for self-management (in theform of posters and leaflets) and that these are clearly displayed forpatients in waiting areas.<strong>QOF</strong>+points37315
Patient experience Chapter 12 (p77)Indicator+ PATIENT EXPERIENCE 1. The practice takes part in a PCT-led local versionof the Picker Institute patient satisfaction survey+ PATIENT EXPERIENCE 2. The practice takes part in a PCT-led feedbacksession based on the results of the local version of the Picker Institutepatient satisfaction survey and agrees an action plan including explicit andappropriate targets that can be used in the following 2 years to assess theextent to which the action plan is implemented+ PATIENT EXPERIENCE 3. The practice shares with patients the results andaction plan from the local version of the Picker Institute patient satisfactionsurvey. This should be through information leaflets and poster(s) in thepractice’s waiting and reception area, and through the Practice’s PatientParticipation Group where this exists+ PATIENT EXPERIENCE 4. The practice can show satisfactory objectiveevidence of implementing and achieving the action plan agreed with thePCT following the PCT-led feedback session based on the results of the localversion of the Picker Institute patient satisfaction survey. Deviations fromthe action plan must be described and explained+ PATIENT EXPERIENCE 5. The practice has a register of patients who needsigning and interpreting support for appointments, including a record offirst language spoken+ PATIENT EXPERIENCE 6. The practice offers double length appointmentsto patients identified as needing interpreting and signing support and to allpatients on the learning disabilities register+ PATIENT EXPERIENCE 7. 100% of carers who are newly registered with thePractice on or after December 01 2008 have a record of being advised bythe Practice that they can ask Social Services for an assessment of their ownneeds+ PATIENT EXPERIENCE 8. The practice has a system in place for taking thespecial needs of carers into account, including when allocatingappointments and issuing prescriptions+ PATIENT EXPERIENCE 9. A named carer is recorded for at least 90% ofpatients on the learning disability register+ PATIENT EXPERIENCE 10. The practice scores better than the nationalaverage on the local Picker survey response to the statement “I waitedmore than 2 working days for a GP appointment”+ PATIENT EXPERIENCE 11. The practice scores better than the nationalaverage on the local Picker survey response to the question “Have you hada problem getting through to your GP practice/health centre on thephone?”<strong>QOF</strong>+points35103057555202016
Patient safety Chapter 13 (p85)Indicator+ PATIENT SAFETY 1. The practice submits significant event analysis (SEA)summaries to an annual PCT audit+ PATIENT SAFETY 2. The practice can show evidence of reporting incidentsor near misses involving harm/potential harm to patients via the nationalreporting and learning system (NRLS) using the standard e-reporting form+ PATIENT SAFETY 3. The practice has a system for ensuring that all practicestaff have had CRB checks within the last three years+ PATIENT SAFETY 4. The practice has a system in place to assist, whereappropriate, with the multi-agency referral process for investigationsrelating to the protection of children and vulnerable adults, includingacknowledging any referrals or requests for information within 2 workingdays+ PATIENT SAFETY 5. The practice has a system in place for identifyingvulnerable children, and this includes cases where a parent is known to be asubstance misuser, has a severe mental health problem, or where there isdomestic violence+ PATIENT SAFETY 6. The case conference notes of all children who are thesubject of a Child Protection Plan are scanned into the child’s medicalrecords+ PATIENT SAFETY 7. The practice has a system in place for ensuring thatwhere a child has been the subject of a child protection plan, this isrecorded as a Significant Active problem in the records of the child, theparents and other members of the household, and that this leads toeffective flagging of records<strong>QOF</strong>+points445785517
C3<strong>QOF</strong>+ report on cardiovasculardisease preventionProposed indicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ CVD PREVENT 1. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a Blood Pressurerecorded in the previous 17 months+ CVD PREVENT 2. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of BMImeasured in the previous 17 months+ CVD PREVENT 3. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a baseline record oftotal and HDL cholesterol recorded in the previous 17 months+ CVD PREVENT 4. The percentage of patients on the PracticeCVD At-Risk Register for whom there is a record of a fastingblood glucose in the previous 17 months+ CVD PREVENT 5. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of familyhistory of CHD in first degree relatives (parents, brothers,sisters, or children of a patient)+ CVD PREVENT 6. The percentage of patients on the PracticeCVD At-Risk Register whose notes have a record of familyhistory of diabetes in first degree relatives (parents, siblings,or children of a patient)+ CVD PREVENT 7. The percentage of patients on the PracticeCVD At-Risk Register who have been offered lifestyle advice onexercise, and appropriate dietary changes within the previous17 months+ CVD PREVENT 8. The percentage of patients on the PracticeCVD At-Risk Register who have been offered statin therapy (inline with 2008 NICE guidance on Lipid Modification) as part oftheir primary prevention management strategy8 40-90%8 40-90%8 40-90%8 40-90%8 40-90%8 40-90%10 40-90%10 40-90%The proposed indicators are in line with the recently published NICE Guidance on LipidModification (2008) and derived from NHS Hammersmith and Fulham’s LES on CVD PrimaryPrevention.19
It is prerequisite that in order to receive payment for + CVD PREVENT 1, practices have achievedthe existing <strong>QOF</strong> RECORDS 11 Indicator (The BP of patients aged 45 and over is recorded in thepreceding 5 years for at least 65% of patients.)For + CVD PREVENT 8, practices will be expected to follow the NICE Guidance on LipidModification (2008), which states that:“People should be offered information about their absolute risk of CVD and about theabsolute benefits and harms of an intervention over a 10-year period. This informationshould be in a form that:presents individualised risk and benefit scenarios-presents the absolute risk ofevents numerically, anduses appropriate diagrams and text.Before offering lipid modification therapy for primary prevention, all other modifiableCVD risk factors should be considered and their management optimised if possible.Baseline blood tests and clinical assessment should be performed, and comorbidities andsecondary causes of dyslipidaemia should be treated.Treatment for the primary prevention of CVD should be initiated with simvastatin 40 mg.If there are potential drug interactions, or simvastatin 40 mg is contraindicated, a lowerdose or alternative preparation such as pravastatin may be chosen.”Further guidance relating to CVD risk assessment, communication of risk and patient informationon CVD primary prevention can be found in the <strong>QOF</strong>+ Resource Pack. Prescribing patterns will beanalysed further by the PCT.It is proposed that these indicators will replace the existing NHS Hammersmith and Fulham LESfor CVD Primary Prevention. The outcome indicators below are included in the current LES forCVD Primary Prevention.The percentage of patients who had a multifactorial CVD risk assessment of ≥ 20% over10 years whose most recent BMI recorded in the previous 12 months is below 30 kg/m2The percentage of patients who had a multifactorial CVD risk assessment of ≥ 20% over10 years whose most recent BMI recorded in the previous 12 months is below 25 kg/m2The percentage of patients who had a multifactorial CVD risk assessment of ≥ 20% over10 years whose most recent blood pressure recorded in the previous 12 months is below150/90 mmHgIt is proposed that these outcome indicators are not included within <strong>QOF</strong>+ at this stage as thefirst priority for this area is to achieve comprehensive vascular screening of the population agedbetween 32-74. Subsequent years/phases of <strong>QOF</strong>+ could then include outcome-based indicators.20
Creation of practice CVD at-risk registerPractices will use a systematic strategy to identify individuals between the ages of 32-74 withoutdiabetes or CVD (who should be on their respective disease registers) with a record of a 20% orgreater 10-year risk of developing CVD (formally estimated through computerized Framingham1991 10-year risk equations, using CVD risk factors already documented in their primary caremedical records, and recorded using an appropriate Read code.) Central support for this processwill be provided by the PCT’s Health Informatics team. This process will generate a CVD At-RiskRegister for each practice.The term ‘Practice CVD At-Risk Register’ used in the indicators below will refer to this register.BackgroundThere is international consensus that for the management of hypertension, it is important toaddress cardiovascular risk for the purposes of primary prevention (Cooper et al., 2008). It is nowpossible to calculate cardiovascular risk for people not known to suffer from cardiovasculardisease, through the use of equations that take into account risk factors. These equations includethose derived through the Framingham data, as well as newer risk equations such as ASSIGN andQRISK. The recently issued NICE Guideline on Lipid Modification recommended the continued useof the Framingham equations at present to calculate risk (Cooper et al., 2008).Priority and relevance to national policyThere is national recognition of the need for a shift in the paradigm of cardiovascular prevention.Primary prevention of CVD is highlighted in the National Service Framework for Coronary HeartDisease (DoH, 2000) and for Older People (DoH, 2001) and in national guidelines of professionalbodies including the Joint British Societies and the British Hypertension Society. The targetsrecommended are reflected in indicators in the new GMS contract. The NSF specifies that“every practice should have a systematically developed and maintained practice-basedregister of people with clinical evidence of coronary heart disease (CHD), occlusivevascular disease and of people whose risk of [cardiovascular] events is [>20%] over 10years in place and actively used to provide structured care to those at high risk of CHD,”and that“every practice should have a protocol describing the systematic assessment, treatmentand follow-up of people at high risk of CHD, including those without evidence of existingarterial disease but whose risk of [cardiovascular] events is [>20%] over 10 years, agreedlocally and being used to provide structured care…”In addition, plans for implementing a national vascular screening programme have recently beenannounced by the Government, and the NICE Guideline on Lipid Modification has been published(Cooper et al., 2008) which includes information on primary prevention of CVD.21
Prevalence of conditionThe number of people in the England and Wales suffering with CVD (Coronary Heart Disease andStroke) amounts to over 3 million (Cooper et al., 2008). Lloyd-Jones et al. (1999) estimated thelifetime risk of developing CHD after the age of 40 to be 49% for men and 32% for women.Associated morbidity and mortalityCVD is the most common cause of death in the England and Wales. In 2005, CVD accounted for124000 deaths (1 in 3 deaths) in England and Wales (Cooper et al., 2008). CVD is an increasingcause of morbidity, resulting in ill-health and disability.Local contextCirculatory diseases are a major cause of hospital admissions in Hammersmith and Fulham.During 2006, 37% of deaths in Hammersmith and Fulham were caused by circulatory diseases(Zeuner D, 2008). Within Hammersmith and Fulham, the premature mortality rate fromcirculatory disease increases as deprivation increases, and 79% of the difference in rates can beexplained by deprivation (Zeuner D, 2008).NHS Hammersmith and Fulham has recently introduced a Local Enhanced Service (LES) toencourage practices to identify all patients on the practice list who are asymptomatic withoutdiabetes and without CVD whose 10-year risk of developing CVD (formally estimated usingcomputerised Framingham 1991 10-year risk equations) is 20% or greater, and to manage themin line with recommendations from NICE. Practices have already had Oberoi software installedwhich helps create a CVD at-risk register for patients aged 32 – 74 (age range is fixed bysoftware).It is proposed that this LES would be replaced by including indicators relating to CVD primaryprevention in <strong>QOF</strong>+. These indicators have been designed to reflect the recommendations madeby the recently updated 2008 NICE Guideline on Lipid Modification.The costing template accompanying the 2008 NICE Guideline on Lipid Modification estimates thatfor Hammersmith and Fulham, the number of adults without CVD aged 40 to 74 with a greaterthan 20% 10-year risk of CVD (using Framingham with adjustments as per NICE guideline) andwithout diabetes totals 7541.Review of evidence to support the proposed indicatorsThere is evidence for the effectiveness of statins in both primary and secondary prevention ofCHD events, strokes and combined major and vascular endpoints. (Cholesterol TreatmentTrialists’ Collaborators, Lancet, 2005). In the West of Scotland Coronary Prevention Study(WOSCOPS), a major primary prevention trial, statin therapy significantly reduced coronarymortality and relative risk for major coronary events (Shepherd J et al., 1995).There is also evidence that aspirin and angiotensin-converting enzyme (ACE) inhibitors reduce riskin asymptomatic patients at high risk of CVD (Hennekens, 1999; Yusuf et al., 2000). The NICEGuideline on Lipid Modification describes clear evidence that reduction in CVD risk can be22
achieved through primary prevention strategies to reduce blood pressure and cholesterol levels,such as lifestyle change and use of pharmaceutical agents including statins, and there is goodevidence of the cost-effectiveness of statins in primary prevention (Cooper et al., 2008).The NICE Guideline on Lipid Modification (Cooper et al., 2008) issues the followingrecommendations:For the primary prevention of CVD in primary care, a systematic strategy should be usedto identify people aged between 40 and 74 who are likely to be at high risk.People should be prioritised on the basis of an estimate of their CVD risk before a fullformal risk assessment.Their CVD risk should be estimated using CVD risk factors already recorded in primarycare electronic medical records.People older than 40 should have their estimate of CVD risk reviewed on an ongoingbasis.People should be prioritised for a full formal risk assessment if their estimated 10-yearrisk of CVD is 20% or more.Healthcare professionals should discuss the process of risk assessment with the personidentified as being at risk, including the option of declining any formal risk assessment.Opportunistic assessment should not be the main strategy used in primary care toidentify CVD risk in unselected people.Many of the current CVD risk assessment tools are based on data from the Framingham study,and other tools are currently in development. The Framingham data uses factors including age,gender, smoking status, diabetic status, blood pressure and cholesterol levels, and presence ofleft ventricular hypertrophy to estimate risk. The Framingham equations were derived from workon a mainly white, middle-class American cohort, and may therefore not be accurate in UKpopulations, including people from ethnic minorities. The Framingham equations have also beenshown to underestimate risk in people with a family history of coronary heart disease, and inlower socio-economic groups. Other risk equations are also being developed and these includeASSIGN (developed using a Scottish cohort) and QRISK (developed with data from UK generalpractice databases). These have the advantage of taking into account factors such as familyhistory and social deprivation. The NICE Guideline on Lipid Modification (Cooper et al., 2008)recommend the continued use of the Framingham equations at present to calculate risk, buthighlight “an urgent need to establish which score is most acceptable for use in the population ofEngland and Wales.”Evidence from economic modelling in an English primary care population shows that prioritisingpatients based upon a prior estimate of their CVD risk using data already held in generalpractitioners’ electronic medical records is the most efficient strategy for identifying people athigh risk of developing CVD.The current JBS 2 guidelines recommend that risk assessment should include ethnicity, smokinghabit history, family history of CVD, and measurements of weight, waist circumference, bloodpressure, non-fasting lipids (total cholesterol and HDL-cholesterol) and non-fasting glucose (JointBritish Societies, 2005). These recommendations are reflected in the SIGN guidelines whichsuggest gathering of additional information on age, gender, socio-economic status and renalfunction (SIGN, 2007).23
Degree of perceived professional consensusCVD risk assessment is supported by professional organisations including the British HeartFoundation, the Joint British Societies and the National Obesity Forum, and by guidelinesincluding JBS-2, SIGN and NICE.A consultation with local stakeholders, including representatives from primary care and publichealth, showed overall consensus for the scientific soundness, importance and feasibility of theseindicators in <strong>QOF</strong>+.Degree of perceived support from patients and carersThere is support for the principles of primary prevention of CVD from a number of patientorganisations including Diabetes UK, the Stroke Association and the British Heart Foundation.Impact on health inequalitiesThose in economically and socially disadvantaged groups and certain ethnic minority groups areat increased risk of CVD. Focussing on primary prevention of CVD in high-risk patients may help toreduce this inequality (Cooper et al., 2008).Health impactPatients may benefit through reduced cardiovascular risk leading to improved life expectancy.Potential harms to patients include iatrogenic effects such as medication side-effects andmedicalisation, leading to negative psychological consequences of having a medical label.24
Workload and training implicationsIncreased workload for primary care teams will be a key issue. This workload will result from theinformation gathering process and the increased contact between primary care practitioners andpatients identified at increased CVD risk. In the long term, there may be a possible reduction inworkload as the identification and management of patients at increased CVD risk may lead toreduced presentation of problems at a later stage.General practice records are now universally computerised and are likely to contain much of theinformation necessary to generate a prior estimate of cardiovascular risk based on existing data(e.g. smoking status, blood pressure and serum lipid profiles) in a high proportion of people(Hobbs et al., 2007). Missing data can be estimated from age- and sex-specific values drawn frompopulation surveys (Marshall, 2006), and automated computer-based risk calculators could beintroduced.The NICE Guideline on Lipid Modification (Cooper et al., 2008) suggests that “using therecommended CVD risk equations, a prior estimate of CVD risk based on pre-existing informationcan be obtained and the practice population can be ranked from highest to lowest risk.” It isproposed that Oberoi software is used to generate a CVD At-Risk Register, using a systematicstrategy to identify asymptomatic people between the ages of 32-74 without diabetes andwithout CVD but who are likely to have a high (20% or greater) 10-year risk of developing CVD(formally estimated through computerized Framingham 1991 10-year risk equations, using CVDrisk factors already documented in their primary care medical records). Starting with those athighest risk, the practice would then invite people to attend for a formal clinical assessment andrisk factor estimation based on the measurement of blood pressure, lipids and current smokingstatus and taking account of other relevant factors such as family history, ethnicity and social orclinical circumstances. Training will be required for primary care staff in cardiovascular riskassessment and communication of risk. The practice will retain responsibility for the creation ofthe CVD at-risk register, which will be dynamic and will require continual updating. However,additional PCT support for this process will be available.In order to evaluate the inclusion in <strong>QOF</strong>+ of indicators relating to CVD primary prevention, it isimportant for practices to submit anonymised data for this purpose (e.g. uptake of screening byage group, sex, ethnic group, deprivation etc; distribution of risk factors by patient group;changes in risk factors over time; economic appraisal). For details of the proposed training package see section 14.3.1 (p92).25
ReferencesCholesterol Treatment Trialists' (CTT) Collaborators (2005) Efficacy and safety of cholesterol-loweringtreatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials ofstatins. Lancet 366:1267-78Cooper A, Nherera L, Calvert N, O’Flynn N, Turnbull N, Robson J, Camosso-Stefinovic J, Rule C, BrowneN, Ritchie G, Stokes T, Mannan R, Bath P, Brindle P, Gill P, Gujral R, Hogg M, Marshall T, Minhas R,Pavitt L, Reckless J, Rutherford A, Thorogood M, Wood D (2008) Clinical Guidelines and EvidenceReview for Lipid Modification: cardiovascular risk assessment and the primary and secondaryprevention of cardiovascular disease <strong>London</strong>: National Collaborating Centre for Primary Care andRoyal <strong>College</strong> of General Practitioners.Department of Health (2000) National Service Framework for Coronary Heart Disease. The StationaryOffice: <strong>London</strong>Department of Health (2001) National Service Framework for Older People. The Stationary Office:<strong>London</strong>Hennekens CH (1999) Update on aspirin in the treatment and prevention of cardiovascular disease.American Heart Journal 137:S9-S13Joint British Societies (2005). JBS 2: Joint British Societies' guidelines on prevention of cardiovasculardisease in clinical practice. Heart 91S5:v1-52Lloyd-Jones DM, Larson MG, Beiser A, Levy D (1999) Lifetime risk of developing coronary heartdisease. Lancet 353:89-92Marshall T, Rouse A (2002). Resource implications and health benefits of primary prevention strategiesfor cardiovascular disease in people aged 30 to 74: mathematical modelling study. British MedicalJournal 325:197-9Marshall T (2006). Estimating the value of information in strategies for identifying patients at high riskof cardiovascular disease. Informatics in Primary Care 14:85-98NICE (2008) Lipid Modification: Costing Template. NICEScottish Intercollegiate Guidelines Network (2007). Risk estimation and the prevention ofcardiovascular disease. A national clinical guideline. [Online, Accessed November 01 2008] Available athttp://www.sign.ac.uk/pdf/sign97.pdf.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, et al. (1995). Prevention ofcoronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland CoronaryPrevention Study Group. New England Joirnal of Medicine 333:1301-7Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effects of an angiotensin-convertingenzymeinhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart OutcomesPrevention Evaluation Study Investigators. New England Journal of Medicine 342:145-53Zeuner, D (2008) Annual Report of the Director of Public Health 2007-2008. Hammersmith and FulhamPCT26
<strong>QOF</strong>+ report on alcoholProposed indicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ ALCOHOL 1. The percentage of patients on one or morepractice registers for CVD At-Risk, Diabetes, Stroke and TIA,Hypertension and CHD who have had AUDIT-C or FASTrecorded on the practice system within the previous 17months+ ALCOHOL 2. The proportion of patients who screen positiveusing either AUDIT-C or FAST within the previous 17 monthswho are subsequently recorded as having a brief interventionfor alcohol misuse15 20-70%30 40-90%It is prerequisite that in order to receive payment for + ALCOHOL 2, practices have reached thelower threshold for + ALCOHOL 1.Practices may also wish to consider participating in the Directed Enhanced Service (DES) forAlcohol 2009/10 which provides additional incentives for screening newly registered patients inprimary care settings.BackgroundResearch by Kaner et al. (1999a) suggests that up to 98 percent of hazardous and harmfuldrinkers may be missed in primary care due to a reliance on clinical history and signs. Themajority of patients in primary care do not object to being asked about their alcohol consumptionif there are good reasons to do so (Wallace and Haines, 1984; Richmond et al., 1996). Primarycare is an ideal setting within which to deliver brief interventions for alcohol misuse in view of itsaccess to the majority of the population, the absence of stigma attached to attending primarycare settings, the presence of ‘teachable moments’ in consultations about alcohol-relatedillnesses, and the generally high credibility in the community of GPs and other primary careprofessionals (Babor, Ritson and Hodgson, 1986).27
Priority and relevance to national policyAddressing alcohol misuse is a key priority for the Government. The Government’s Alcohol HarmReduction Strategy for England was published in 2004. In 2007, the Government followed thiswith a new publication: ‘Safe. Sensible. Social. The Next Steps in the National Alcohol Strategy’.The Review of the Effectiveness of Treatment for Alcohol Problems published by the NationalTreatment Agency (Raistrick et al., 2006) provides a comprehensive review of the researchsurrounding identification and management of alcohol problems. In his final report of the NHSNext Stage Review (2008), Lord Darzi listed the reduction of alcohol harm as one of the key goalsfor primary care trusts to address when commissioning comprehensive well-being and preventionservices, in partnership with local authorities…” The Department of Health and GeneralPractitioner Committee (GPC) have very recently released details of a new Directed EnhancedService (DES) for Alcohol, incorporating screening and brief interventions.Prevalence of conditionIn 2004 an estimated 8.2 million people in England aged 16-64 (26 percent of the totalpopulation) had an alcohol use disorder in England. 38 percent of these were men and 16 percentwere women (Drummond et al., 2004).Associated morbidity and mortalityExcess alcohol consumption is responsible for significant amounts of morbidity and mortality andcosts the health service £1.7bn per annum (Hutchings et al., 2006). Alcohol misuse is associatedwith up to 22,000 premature deaths in England and Wales annually, and a significant proportionof these are due to alcohol-related liver disease (Prime Minister’s Strategy Unit, 2004). Alcoholmisuse is responsible for over 30,000 hospital admissions per year for alcohol dependencesyndrome, and up to 70% of all admissions to accident and emergency departments at peak times(Leon et al., 2006). Annually, alcohol misuse is associated with approximately 14 percent ofdeaths from injuries, which involves about 1700 individuals. Alcohol misuse may be linked to 38-45 percent of deaths in fires, 7-25 percent deaths at work and 23-38 percent of deaths fromdrowning (Leon et al., 2006). Alcohol misuse may be a causal factor in up to 41 percent ofsuicides. Of those presenting to hospital with self harm, 50 percent were found to be regulardrinkers and 23 percent were dependent (Leon et al., 2006). 1.2 million violent incidents (aroundhalf of all violent crimes), 360,000 incidents of domestic violence (around a third), increased antisocialbehaviour and fear of crime, up to 17 million lost working days, between 780,000 and 1.3million children affected by parental alcohol problems, and an increased divorce rate have beenattributed to alcohol use (Cabinet Office, 2004). Alcohol is responsible for 3.5 percent of deathsfrom cancer in the UK, or 5000 deaths per year (Prime Minister’s Strategy Unit, 2003). Alcoholmisuse is also a risk factor for cardiovascular disease (Royal <strong>College</strong> of Physicians, 2001).28
Local contextThe Hammersmith and Fulham Public Health Report 2007/8 (Zeuner, 2008) states that:“It is estimated that 5.7% of adults aged 15-64 in Hammersmith and Fulham (7,300people) have an alcohol dependency, which is the highest prevalence in <strong>London</strong>.Hammersmith and Fulham has a particularly high prevalence of hazardous and harmfuldrinking. It is estimated that around 36,000 adults (25%) in Hammersmith and Fulhamconsume hazardous amounts of alcohol, and a further 10,000 adults (7%) consumeharmful amounts of alcohol. Given the socio - demographic characteristics of thepopulation, it is expected that approximately 16.4% (CI: 13.8% - 19.3%) of adults bingedrink (around 24,000 adults). Hospital admission rates for alcohol-specific and alcoholattributableconditions are high in Hammersmith and Fulham, particularly among males.Mortality rates for alcohol-specific and alcohol-attributable conditions are high inHammersmith and Fulham, particularly among males. The alcohol-specific mortality rateamong males is one of the highest in England. The mortality rate from chronic liverdisease among males in Hammersmith and Fulham is also one of the highest in England”.Review of evidence to support the proposed indicatorsThere is a significant amount of evidence supporting the effectiveness of opportunistic casefindingfor alcohol misuse and the delivery of brief interventions (Moyer et al., 2002). The resultsof many of the large-scale systematic reviews and meta-analyses are summarised in an evidencebriefing by the Health Development Agency (2005) and in the Scottish Intercollegiate GuidelinesNetwork (SIGN) guidelines. Strong evidence for the effectiveness of brief alcohol interventions inprimary care populations is also provided by a recent Cochrane Collaboration review (Kaner et al.,2007).The CAGE screening questionnaire was validated in 1974 and is the most widely used test inclinical practice (Smart et al., 1991). However, research by Aertgeerts et al. (2001) found that itwas not sufficient as a screening instrument for detecting alcohol misuse or dependence amongprimary care patients.The AUDIT was developed by the World Health Organisation (WHO) as a simple method ofscreening for excessive drinking (Saunders et al., 2003). AUDIT takes 5 minutes to complete, canbe administered through a brief, structured interview or a self-report questionnaire, and has asensitivity of 92% a specificity of 94% (Saunders et al., 2003).Abbreviated versions of the WHO Alcohol Use Disorders Identification Test (AUDIT)questionnaire, include the AUDIT-FAST (developed for use in A and E and other hospital settingsby Hodgson et al. in 2002, and now validated for use in primary care), the AUDIT-C and theAUDIT-PC (developed by Bush et al. in 1998 for use in primary care).29
Degree of perceived professional consensusThe RCGP supports inclusion of alcohol misuse in the <strong>QOF</strong> and regards a selective screeningapproach to adult patients in routine care as realistic for clinicians.A consultation with local stakeholders, including representatives from primary care and publichealth, showed overall consensus for the scientific soundness, importance and feasibility of theseindicators in <strong>QOF</strong>+.Degree of perceived support from patients and carersThere is evidence that patients are supportive of advice on alcohol-related issues (Hutchings etal., 2006).Impact on health inequalitiesThe Independent Inquiry into Inequalities in Health (Acheson, 1998) concluded that:“Deaths from diseases caused by alcohol show a clear gradient with socio-economicposition, with an almost fourfold higher rate in unskilled working men compared to thosefrom professional groups. In addition, alcohol is a contributory factor to deaths fromaccidents, which also show a pronounced socio-economic gradient.”Disadvantaged communities have higher levels of alcohol-related mortality, hospital admission,crime, absence from work, school exclusions, teenage pregnancy and road traffic accidentsassociated with greater levels of alcohol consumption. Within localities, the most disadvantagedindividuals have four to fifteen times greater alcohol-specific mortality and four to ten timesgreater alcohol-specific admission to hospital than the most affluent (North West Public HealthObservatory, 2007, Department of Health, 2008).Health impactEvidence by Wallace et al. (1988) suggests that the consistent implementation of simple alcoholadvice, across the UK, would result in the reduction from hazardous and harmful to low-riskdrinking levels in 250,000 men and 67,500 women each year.There is some limited evidence from a meta-analysis that brief interventions reduce alcoholrelatedmortality (Cuijpers, Riper and Lemmens, 2004).30
Workload and training implicationsResearch by Kaner et al. (1999b) identified a number of barriers to implementation of briefintervention in primary care. These include lack of time, lack of training, a belief that patients willnot take advice to change drinking behaviour, a lack of suitable screening and counsellingmaterials, lack of reimbursement from government health schemes, negative attitudes towardspatients with drinking problems and fear of offending patients by raising the topic of drinking.In their review of the effectiveness of treatment for alcohol problems, Raistrick et al. (2006)describe ways in which many of these barriers can be easily overcome, such as providingappropriate training in screening and brief interventions for alcohol misuse, but acknowledgethat “the most difficult obstacles are those to do with lack of time and of reimbursement for thiswork”.Incorporation into <strong>QOF</strong>+ of indicators relating to screening and brief intervention for alcoholmisuse in primary care could help address the issue of reimbursement. With respect to training, itis proposed that this will take place through an e-module offered by the Department of Health(due to launch in November 2008) and will be supplemented by training to individual practicesdelivered by the Hammersmith and Fulham Drug and Alcohol Team. For details of the proposed training package see section 14.3.2 (p92).ReferencesAcheson D (1998) Inequalities in health: report of an independent inquiry. <strong>London</strong>: HMSOAertgeerts B, Buntix F, Ansoms S & Fevery J (2001) Screening properties of questionnaires andlaboratory tests for the detection of alcohol abuse or dependence in a general practice population.British Journal o0f General Practice 51:206-217Babor TF, Ritson EB & Hodgson RJ (1986). Alcohol-related problems in the primary health care setting:A review of early intervention strategies. British Journal of Addiction 81:23–46Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA (1998). The AUDIT alcohol consumptionquestions (AUDIT-C): An effective brief screening test for problem drinking. Archives of InternalMedicine 158:1789–1795Carpenter A and Mayers A (2006) Hammersmith and Fulham PCT Public Health Report 2006.Cuijpers P, Riper H, Lemmens L (2004). The effects on mortality of brief interventions for problemdrinking: A meta-analysis. Addiction 99:839–845Darzi A (2008) High Quality Care for All, the final report of the NHS Next Stage Review Final Report byLord Darzi The Stationary Office. <strong>London</strong>Department of Health (2008) Health inequalities: progress and next steps. <strong>London</strong>: Department ofHealthDepartment of Health, Home Office, Department for Education and Skills, Department for Culture,Media and Sport (2007) Safe. Sensible. Social. The next steps in the national alcohol strategyDrummond C, Oyefeso A, Phillips T, Cheeta S, Deluca P, Perryman K, et al. (2004) Alcohol needsassessment research project (ANARP): the 2004 national alcohol needs assessment for England.<strong>London</strong>: Department of Health31
Hodgson R, Alwyn T, John B, Thom B, Smith A (2002) The FAST Alcohol Screening Test. Alcohol andAlcoholism 37:61–6Hutchings D, Cassidy P, Dallolio E, Pearson P, Heather N, Kaner E (2006) Primary Health Care Research& Development 7:221-229 Cambridge University PressKaner E, Haighton C, McAvoy B, Heather N, Gilvarry E (1999a) A RCT of three training and supportstrategies to encourage implementation of screening and brief alcohol intervention by generalpractitioners. British Journal of General Practice 49:699–703Kaner E, Heather N, McAvoy B, Lock C, Gilvarry E (1999b) Intervention for excessive alcoholconsumption in primary health care: Attitudes and practices of English general practitioners. Alcoholand Alcoholism 34:559–566Kaner EF, Beyer F, Dickinson HO et al. (2007) Effectiveness of brief alcohol interventions in primarycare populations. Cochrane Database of Systematic Reviews 2:CD004148Leon D, McCambridge J (2006) Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysisof routine data. Lancet 367:52-6Mulvihill et al. (2005) Prevention and Reduction of Alcohol Misuse: Evidence Briefing 2 nd Ed HealthDevelopment AgencyMoyer A, Finney J, Swearingen E, Vergun P (2002) Brief interventions for alcohol problems: a metaanalyticreview of controlled investigations in treatment-seeking and non-treatment-seekingpopulations. Addiction 97:279-92Prime Minister’s Strategy Unit (2004), Alcohol Harm Reduction Strategy for England, Cabinet Office,<strong>London</strong>North West Public Health Observatory (2007) Indicators of Public Health in the English Regions 8.Alcohol. Centre for Public Health, Liverpool John Moores UniversityPrime Minister’s Strategy Unit (2203). Interim analytical report. Strategy unit, alcohol harm reductionproject. <strong>London</strong>: Cabinet OfficeRaistrick D, Heather N, Godfrey C (2006) Review of the effectiveness of treatment for alcoholproblems. National Treatment Agency for Substance Misuse.Richmond R, Kehoe L, Heather N, Wodak A, Webster I (1996) General practitioners’ promotion ofhealthy life styles: What patients think. Australian and New Zealand Journal of Public Health 20:195–200.Royal <strong>College</strong> of Physicians (2001). Alcohol—can the NHS afford it? Recommendations for a coherentalcohol strategy for hospitals. <strong>London</strong>: Royal <strong>College</strong> of PhysiciansSaunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M (1993) Development of the Alcohol UseDisorders Identification Test (AUDIT): WHO collaborative project on early detection of persons withharmful alcohol consumption – II. Addiction 88:791–804Scottish Intercollegiate Guidelines Network (SIGN).(2003). Guideline on the Management of HarmfulDrinking and Alcohol Dependence in Primary Care – a National Clinical Guideline (74). Edinburgh:SIGN.Seppä K, Lepistö J, Sillanaukee P (1998) Five-shot questionnaire on heavy drinking. Alcoholism: Clinicaland Experimental Research 22:1788-1791Wallace P, Cutler S, Haines A (1988) Randomised control trial of general practitioner intervention withexcessive alcohol consumption. British Medical Journal 297:663-68Wallace PG, Haines AP (1984) General practitioner and health promotion: What patients think. BritishMedical Journal 289:534–6Williams RH, Vinson DC (2001) Validation of a single question screen for problem drinking. Journal ofFamily Practice 50:307–312Zeuner D (2008) Annual Report of the Director of Public Health 2007-2008. Hammersmith and FulhamPCT32
<strong>QOF</strong>+ report on smokingProposed indicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ SMOKING 1. The percentage of patients aged 15 years orolder whose notes record smoking status in the past 17months, or whose most recent recorded smoking status,recorded over the age of 25, indicates that they had neversmoked+ SMOKING 2. The percentage of patients aged 15 years orolder who smoke whose notes contain a record that smokingcessation advice or referral to a local smoking cessationservice has been offered within the previous 17 months20 40-90%10 40-90%These indicators have been adapted from those in the existing <strong>QOF</strong> and from NHS Hammersmithand Fulham’s Local Enhanced Service for CVD Primary Prevention.BackgroundThe aims of incorporating additional indicators for smoking cessation within <strong>QOF</strong>+ include:reducing smoking prevalence in practice-registered populations, andoffering those wishing to stop smoking appropriate help either through practice-basedsupport or referrals to specialist services outside the practice.The proposed indicators are additional to the NHS Hammersmith and Fulham Local EnhancedService (LES) for Smoking Cessation and existing <strong>QOF</strong> indicators. This LES aims to increase thenumber of patients who receive multi-session stop smoking support through practice-basedadvisors and/or referral to specialist services outside the practice.33
Priority and relevance to national policyThere is a considerable body of national policy documentation related to smoking, reflecting itsimportance as a key priority area for the Government and for the NHS. This includes the tobaccowhite paper ‘Smoking Kills’, the public health white paper, ‘Choosing Health’ and the white paper‘Our Health, Our Care, Our Say’. Since 2004, the General Medical Services contract for generalpractice (the Quality and Outcomes Framework) has awarded points for recording patients’smoking status and providing cessation advice or referrals. In his final report of the NHS NextStage Review (2008), Lord Darzi listed the reduction of smoking rates as one of the key goals forprimary care trusts to address when “commissioning comprehensive well-being and preventionservices, in partnership with local authorities…” The government’s Public Service Agreement forSmoking states a goal of reducing adult smoking rates (from 26% in 2002) to 21% or less by 2010,with a reduction in prevalence among routine and manual groups (from 31% in 2002) to 26% orless (DoH, 2004). Key performance indicators related to smoking are incorporated into theHealthcare Commission targets for acute trusts and for PCTs.Prevalence of conditionIn 2006, 24% of people aged 16 and over in England smoked (Lader, 2007). Among those inroutine or manual occupations, the prevalence in 2005 was 29% (Goddard, 2006). Smokingprevalence is also high among some minority ethnic groups (Erens et al. 2000).Associated morbidity and mortalitySmoking remains the main cause of preventable morbidity and premature death in England,leading to an estimated annual average of 86,500 deaths between 1998 and 2002 (Twigg et al.2004). It is estimated to cost the NHS £1.5 billion a year (Parrott et al. 1998). Smoking has beenidentified as a causal factor in cancers, respiratory diseases, coronary heart and other circulatorydiseases, stomach and duodenal ulcers, erectile dysfunction and infertility, osteoporosis,cataracts, age-related macular degeneration and periodontitis (US Department of Health andHuman Services 2004). Following surgery, smoking contributes to lower survival rates, delayedwound healing and post-operative respiratory complications (US Department of Health andHuman Services 2004). Smoking during pregnancy incurs specific risks to both mother and foetusand is the focus of a separate indicator set ( see Smoking in Pregnancy, Chapter 6, page 39).Passive smoking is also associated with risks including exacerbation of respiratory symptoms andtriggering asthma attacks as well as increasing the risk of lung cancer, respiratory illnesses(especially asthma), heart disease and stroke (NICE, 2008; International Agency for Research onCancer 2002; Scientific Committee on Tobacco and Health 2004; US Environmental ProtectionAgency 1993).34
Local context24% of adults (35,000) within Hammersmith and Fulham are estimated to be current smokers,and around 7% of mothers in Hammersmith and Fulham and in <strong>London</strong> smoke during pregnancy.Although smoking cessation targets have been achieved by the PCT over recent years, last yearonly approximately 5.4% of smokers had quit for at least 4 weeks using the smoking cessationservice in Hammersmith and Fulham. During 2006 there were 820 deaths of residents. 37% ofthese deaths were caused by circulatory diseases, 30% by cancer and 13% by respiratory disease,and these conditions are known to be associated with smoking. The main cancers causing deathsin Hammersmith and Fulham are lung, breast, colon, bladder and stomach cancer – togetheraccounting for almost half of all cancer deaths. Smoking is known to be a risk factor in all thesecancers (Zeuner, 2008).Review of evidence to support proposed indicatorsFollowing a review of smoking cessation services, recently published NICE public health guidancestates that evidence directly applicable to UK health care settings supports the efficacy and costeffectivenessof physician advice as a brief intervention for smoking cessation and the efficacyand cost-effectiveness of nicotine replacement therapy (NRT) as part of a brief intervention forsmokers wishing to make a quit attempt (NICE, 2008). This guidance also states that there isevidence that additional specialist clinic input increase quit rates and pharmacologicalinterventions including bupropion and varenicline are effective and recommended within theirproduct licenses. (NICE, 2008)Degree of perceived support from professionalsThere is good professional consensus with respect to the appropriateness of smoking cessation(NICE, 2008; BMA, 2004). A consultation with local stakeholders, including representatives fromprimary care and public health, showed overall consensus for the scientific soundness,importance and feasibility of these indicators in <strong>QOF</strong>+.Degree of perceived support from patients and carersThe programme development group of the recently published NICE guidance on smokingcessation services included members of the public (NICE, 2008).Impact on health inequalitiesSmoking is the primary reason for the gap in healthy life expectancy between rich and poor.Among men, smoking is responsible for over half the excess risk of premature death between thesocial classes (NICE, 2008; Jarvis and Wardle 1999). There is evidence that NHS stop smokingservices are making a modest contribution to reducing smoking-related inequalities in health inEngland (NICE, 2008).35
Health impactThe further incentivisation of efforts to increase smoking cessation will contribute to thereduction of smoking-related morbidity and mortality.Workload and training implicationsWorkload is significant in that smokers and ex-smokers require annual documentation.It is proposed that to qualify for payment for achievement of smoking-related indicators in <strong>QOF</strong>+,practices will be required to sign up to the LES for Smoking Cessation. This LES stipulates thatpractices must:1 Nominate a lead for smoking cessation who will attend level 1 and 2 training in smokingcessation.2 Identify the people who will deliver smoking cessation advice and support to quitters andensure that the named staff attend level 2 training and annual update training.3 Ensure level 2 advisors are up to date in cessation interventions and maintain contactwith the Stop Smoking Service.4 Agree to work within the Department of Health Guidelines on Stop smoking servicesNICE guidance recommends that all frontline healthcare staff should be trained to offer briefadvice on smoking cessation and to make referrals, where necessary and possible, to NHS StopSmoking Services and other publicly funded smoking cessation services (NICE, 2006). For details of the proposed training package see section 14.3.3 (p93).36
ReferencesBritish Medical Association (2004) Smoking and reproductive life: the impact of smoking on sexual,reproductive and child health. <strong>London</strong>: British Medical Association.Department of Health (2004) Spending review 2004: public service agreement. <strong>London</strong>: The StationeryOffice.Department of Health (2004) Choosing Health: Making healthy choices easier. The Stationary Office.<strong>London</strong>Darzi A (2008) High Quality Care for All, the final report of the NHS Next Stage Review Final Report byLord Darzi The Stationary Office. <strong>London</strong>Erens B, Primatesta P, Prior G, editors (2000) Health survey for England 1999: the health of minorityethnic groups. <strong>London</strong>: The Stationery Office.Goddard E (2006) Smoking and drinking among adults, 2005: General household survey 2005. <strong>London</strong>:Office for National Statistics.Innes KE, Byers TE. (2001) Smoking during pregnancy and breast cancer risk in very young women(United States). Cancer Causes Control 12: 179−185.International Agency for Research on Cancer (2002) Tobacco smoke and involuntary smoking. IARCMonographs vol 83. Lyon: World Health Organisation.Jarvis M, Wardle J (1999) Social patterning of individual health behaviours: the case of cigarettesmoking. In: Marmot M, Wilkinson R, editors. Social determinants of health. Oxford: Oxford UniversityPress.Lader D (2007) Smoking related behaviours and attitudes 2006. <strong>London</strong>: Office for National Statistics.NICE (2006) Brief interventions and referral for smoking cessation in primary care and other settings.NICE public health intervention guidance 1. National Institute for Health and Clinical ExcellenceNICE (2008) Smoking cessation services in primary care, pharmacies, local authorities and workplaces,particularly for manual working groups, pregnant women and hard to reach communities. Nice PublicHealth Guidance 10. National Institute for Health and Clinical ExcellenceParrott S, Godfrey C, Raw M et al. (1998) Guidance for commissioners on the cost effectiveness ofsmoking cessation interventions. Thorax 53: 2–37.Scientific Committee on Tobacco and Health, Department of Health (2004) Secondhand smoke: reviewof the evidence since 1998. <strong>London</strong>: The Stationery Office.Secretary of State for Health (2006). Our health, our care, our say: a new direction for communityservices. The Stationery Office. <strong>London</strong>Secretary of State for Health (1998). Smoking Kills: a white paper on tobacco. The Stationary Office<strong>London</strong>Twigg L, Moon G, Walker S (2004) The smoking epidemic in England. <strong>London</strong>: Health DevelopmentAgency.US Department of Health and Human Services (2004) The health consequences of smoking: a report ofthe Surgeon General. Washington DC: USA.US Environmental Protection Agency (1993) Respiratory health effects of passive smoking: lung cancerand other disorders. Washington DC: US Environmental Protection Agency.West, 2002 R. West, Smoking cessation and pregnancy, Foetal and Maternal Medicine Review 3(2002), pp. 181–194.Zeuner, D (2008) Annual Report of the Director of Public Health 2007-2008 Hammersmith and FulhamPCT37
<strong>QOF</strong>+ report onsmoking in pregnancyProposed IndicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ SMOKING IN PREG 1. The percentage of pregnant womenwhose notes record their smoking status at the time of theirfirst booking appointment in primary care+ SMOKING IN PREG 2. The percentage of pregnant womenwho smoke whose notes contain a record that at the time oftheir first antenatal booking appointment in primary care theyhave been given smoking cessation advice and details of thelocal NHS Stop Smoking Services and the NHS pregnancysmoking helpline (0800 169 9 169)3 70-90%5 70-90%These indicators have been adapted from current smoking-related indicators in <strong>QOF</strong> and from the2008 NICE clinical guideline on antenatal care.BackgroundThe association between smoking and adverse outcomes of pregnancy for both infant andmother is well established. These adverse outcomes are described further below. Smoking inpregnancy is a potentially preventable activity, and therefore has important public healthimplications.Priority and relevance to national policyThe NHS Stop Smoking Services were initiated in 1999, and local services have had a particularfocus on reducing the number of pregnant women who smoke (DoH, 1998). The Department ofHealth’s white paper ‘Smoking Kills’ (DoH, 1998) set a national target to reduce the number ofwomen who smoke during pregnancy from 23% to 15% by 2010 and this target is reflected in theKey Performance Indicators of the Healthcare Commission. Additionally, the NHS Priorities andPlanning Framework (DoH, 2002) contains a target of delivering a one percentage point reductionper year in the proportion of women continuing to smoke throughout pregnancy. The frameworkfocuses especially on smokers from disadvantaged groups as a contribution to the national targetto reduce by at least 10% the gap in mortality between ‘routine and manual’ groups and thepopulation as a whole by 2010, starting with children under one year.39
The NICE Clinical Guideline on Antenatal Care (NICE, 2008) include recommendations for smokingin pregnancy. These include:“At the first contact with the woman, discuss her smoking status, provide informationabout the risks of smoking to the unborn child and the hazards of exposure tosecondhand smoke. Address any concerns she and her partner or family may have aboutstopping smoking. Pregnant women should be informed about the specific risks ofsmoking during pregnancy (such as the risks of having a baby with low birthweight andpreterm birth). The benefits of quitting at any stage should be emphasized,”and:“Offer personalised information, advice and support on how to stop smoking. Encouragepregnant women to use local NHS Stop Smoking Services and the NHS pregnancysmoking helpline, by providing details on when, where and how to access them. Monitorsmoking status and offer smoking cessation advice, encouragement and supportthroughout the pregnancy and beyond.”Prevalence of conditionSurvey data found that 27% of women in the UK declared themselves to be current smokers atthe birth of their baby (Owen, 1998). When interpreting these figures, it is important to recognizethat this is likely to be an underestimate, as a proportion of women deny their smoking (West,2002).Associated morbidity and mortalityIt is now well recognized that cigarette smoking during pregnancy is associated with harm to bothfoetus and mother (West, 2002). Risks to the foetus include miscarriage, stillbirth, Sudden InfantDeath Syndrome (SIDS) and respiratory problems in the young child. Longer term problemsinclude intellectual impairment, problem behaviour, infertility, high blood pressure andcardiovascular disease. Potential harms to the mother include increased risk from pregnancycomplications such as abruption and possibly an increased risk of early onset breast cancer (West,2002; Innes et al., 2001). A study by DiFranza et al. (1995) estimated that tobacco use in the USdetermines between 19,000 to 141,000 spontaneous abortions annually, 32,000 to 61,000 casesof low birthweight and up to 26,000 admissions to neonatal intensive care. The same workestimated 1,900 to 4,800 cases of tobacco-related perinatal mortality and 1,200 to 2,200 cases ofSIDS. In pregnancy, passive smoking can reduce foetal growth and increase the risk of pretermbirth (British Medical Association, 2004).Local contextAround 7% of mothers in Hammersmith and Fulham and in <strong>London</strong> smoke during pregnancy. Lowbirth weight is strongly associated with infant mortality and smoking in pregnancy is a risk factorfor low birth weight. Although the low birth weight rate is not particularly high (9% inHammersmith and Fulham, 8% in England), it is strongly related to deprivation (Zeuner, 2008).40
Evidence to support the proposed indicatorsA Cochrane review by Silagy (2000) found that a single episode of brief physician advice given tosmoking patients can increase the proportion who stop smoking long-term by 1±2%. West (2002)comments that “while this is a small effect, the fact that the advice takes only a few minutes andso is inexpensive and the health gains from cessation are so great, makes this an extremelyimportant and cost-effective life-preserving intervention”. There is some evidence to suggest thatthe effect of this advice on pregnant smokers is similar to that for other smokers (Haug et al.,1994; Senore et al., 1998).A Cochrane systematic review by Lumley et al. (2001) found a significant reduction in smoking inlate pregnancy among women who attended smoking cessation programmes compared with noprogramme. Another systematic review by Law et al. (1995) included a trial of physician advice, atrial of advice from a health educator, a trial of group sessions, and seven trials on behaviouraltherapy based on self-help manuals. This review found that cessation programmes significantlyincreased the rate of quitting.The NICE Clinical Guideline on Antenatal Care (2008) concludes that “there is good-qualityevidence to show that smoking cessation interventions help women reduce smoking anddecrease adverse neonatal outcomes.”Degree of perceived professional consensusEvidence suggests that health professionals recognize the dangers of smoking during pregnancyand support the idea that pregnant women should stop smoking (West, 2002). A consultationwith local stakeholders, including representatives from primary care and public health, showedoverall consensus for the scientific soundness, importance and feasibility of these indicators in<strong>QOF</strong>+.Degree of perceived support from patients and carersSurveys suggest that, even among women who continue to smoke during pregnancy, almost twothirds say they would like to stop (Hughes et al., 1982; Haslam et al., 1997). The NICE ClinicalGuideline on Antenatal Care (2008) conclude that “most women preferred information to beprovided on a face-to-face basis” and that women required a wide range of informationantenatally including advice on smoking cessation.Impact on health inequalitiesResearch has identified a number of factors associated with continuation of smoking inpregnancy. These include younger age, deprived socio-economic backgrounds and lowereducational level (Cnattingius et al., 1992; Mas et al., 1996). Therefore including an indicator in<strong>QOF</strong>+ relating to smoking in pregnancy may help to address health inequalities.41
Health impactThere are significant health gains to both foetus and mother associated with cessation of smokingin pregnancy. Walsh et al. (1996) estimated that that if all pregnant women stopped smoking, a10% reduction in infant and foetal deaths would be seen.Workload and training implicationsCollecting the data required for the indicators proposed should be a routine part of communityantenatal care. A survey by Bishop et al. (1998) found that time constraints meant thatprofessionals felt they did not have sufficient time to consider smoking cessation, and reportedthat health professionals felt under-resourced in terms of finances and numbers of staff. Trainingfor primary care staff in offering brief interventional advice would support delivery of theseindicators. For details of the proposed training package see section 14.3.3 (p93).42
ReferencesBritish Medical Association (2004) Smoking and reproductive life: the impact of smoking on sexual,reproductive and child health. <strong>London</strong>: British Medical Association.Cnattingius S, Lindmark G, Meirik O (1992). Who continues to smoke while pregnant? Journal ofEpidemiology and Community Health 46: 218-21.Department of Health. (2002) Improvement, expansion and reform: the next three years. Prioritiesand planning framework 2003 to 2006. The Stationary Office: <strong>London</strong>.Department of Health. (1998) Smoking kills: a white paper on tobacco. The Stationary Office: <strong>London</strong>.DiFranza JR, Lew RA (1995). Effect of maternal cigarette smoking on pregnancy complications andsudden infant death syndrome. Journal of Family Practice 40: 385-94.Mas R, Escriba V, Colomer C (1996). Who quits smoking during pregnancy? Scandinavian Journal ofSocial Medicine 24: 102-106Haslam C, Draper ES, Goyder E (1997) The pregnant smoker: a preliminary investigation of the socialand psychological influences. Journal of Public Health Medicine 1997; 19: 187-92.Haug K, Fugelli P, Aaro LE, Foss OP (1994). Is smoking intervention in general practice more successfulamong pregnant than non-pregnant women? Family Practice 11: 111-16.Hughes JR, Epstein LH, Andrasik F, Neff DF, Thompson DS (1982). Smoking and carbon monoxidelevels during pregnancy. Addictive Behaviour 7: 271-76.Innes KE, Byers TE (2001). Smoking during pregnancy and breast cancer risk in very young women(United States). Cancer Causes Control 12: 179-85.Law M, Tang JL (1995). An analysis of the effectiveness of interventions intended to help people stopsmoking. Archives of Internal Medicine 155:1933–41.Lumley J, Oliver S, Waters E (2001). Interventions for promoting smoking cessation during pregnancy.Cochrane Database of Systematic Reviews (2). 2001.NICE Clinical Guideline (2008) Antenatal Care. National Institute for Health and Clinical ExcellenceOwen L, McNeill A, Callum C (1998). Trends in smoking during pregnancy in England, 1992-97: quotasampling surveys British Medical Journal 317: 728.Senore C, Battista RN, Shapiro SH, Segnan N, Ponti A, Rosso S, et al. (1998). Predictors of smokingcessation following physicians' counselling. Preventative Medicine 27: 412-21Silagy C (2000). Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2:CD000165.West R (2002) Smoking cessation in pregnancy. Foetal and Maternal Medicine Review 13:3 181-194Zeuner, D (2008) Annual Report of the Director of Public Health 2007-2008 Hammersmith and FulhamPCT43
<strong>QOF</strong>+ report on breastfeedingProposed IndicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ BREASTFEEDING 1. The percentage of women who arerecorded as being pregnant on or after December 01 2008,and who at their antenatal booking appointment in primarycare have been given specific information on breastfeeding,including information on breastfeeding workshops+ BREASTFEEDING 2. The percentage of babies born on orafter December 01 2008 and breast fed at 6-8 weeks whoserecord indicates that breastfeeding support contact has beenoffered to the babies’ mother at the time of the 6-8 weekcheck+ BREASTFEEDING 3. At least 80% of babies born on or afterDecember 01 2008 have a record of feeding method at thetime of the 6-8 week check4 70-90%6 70-90%3 -BackgroundBreastfeeding is associated with a range of important health advantages and in view of this, theWorld Health Organisation recommends breastfeeding for a minimum of six months andcontinued breastfeeding up to two years of age or beyond (World Health Organisation, 2003).However, current patterns of infant feeding show that many women in the UK who commencebreastfeeding will change to formula feeding, often within the first few weeks of giving birth, andrates of exclusive breastfeeding remain low, especially amongst younger women and womenfrom low-income groups (Hamlyn et al., 2002). Inclusion of a breastfeeding indicator in <strong>QOF</strong>+ hasbeen identified as a way to address this.45
Priority and relevance to national policyThe importance of breastfeeding is highlighted in national policy including Choosing Health;Making Healthy Choices Easier (DoH, 2004) and the National Service Framework for Children andMaternity Services (DoH, 2004). Breastfeeding contributes to several Public Service Agreement(PSA) targets and NICE guidance on postnatal care (2006) has made recommendations that topromote breastfeeding, the UNICEF Baby Friendly Initiative should be implemented as routinepractice, the minimal standard across NHS Trusts in England. NICE has also published publichealth guidance on improving the nutrition of pregnant and breastfeeding mothers and childrenin low-income households (NICE, 2008).Prevalence of conditionUK breastfeeding rates are amongst the lowest in Europe. In the Office of Population CensusSurvey (Hamlyn et al., 2002) 71% of mothers across the UK initiated breastfeeding, and 86% ofmothers were from managerial and professional occupations compared to 60% of mothers fromroutine and manual occupations.The UK Infant Feeding Survey 2005 (2007) also found that 48% of all mothers in the UnitedKingdom were breastfeeding at six weeks, while 25% were still breastfeeding at six months. At sixweeks the rate of exclusive breastfeeding was 22% in England. In this survey, 84% of mothers saidthey were aware of the health benefits of breastfeeding. Three quarters of these mothers hadalso given their baby milk; which was not breast milk by the age of six weeks, an this percentagerose to 92% by six months.Associated morbidity and mortalityLow rates of breastfeeding are associated with increased incidence in the infant ofgastrointestinal, urinary, respiratory and middle ear infection (Aniansson et al. 1994; Howie et al.1990; Pisacane et al. 1992) and atopic disease, especially if there is a family history of this (Burr etal. 1989; Oddy et al. 1999). Breastfeeding may be protective against cardiovascular disease(Wilson et al. 1998}. Women who do not breastfeed may be at increase risk of certain forms ofcancer, including breast cancer (DoH, 1996).46
Local contextIn 2006/7, the percentage of mothers initiating breastfeeding within 48 hours was 79% (Zeuner,2008). The Food & Health Strategy developed by NHS Hammersmith and Fulham, in collaborationwith the <strong>London</strong> Borough of Hammersmith and Fulham, includes the following recommendationsfor infant care services:1 Promoting breastfeeding, especially to vulnerable young mothers, through Health Visitorante-natal support.2 Community breastfeeding support groups, run in conjunction with Children’s Centres byHealth Visitors, Midwives, Childcare Advisors and Family Support Workers.3 Breastfeeding advice and support given in child health clinics, post-natal/baby massagegroups, parenting groups, home visits and by telephone.4 Healthy weaning advice groups provided by Childcare Advisors to all parents and carersof babies from 17 weeks of age. Sessions also included in six-weekly parenting groupprogrammes. Support and information provided in Child Health Clinics, individual homevisits and by telephone.5 Training sessions on practical nutritional guidelines for people working with infants andyoung children.Review of evidence to support the proposed indicatorThe National Institute for Health and Clinical Excellence’s Public Health Briefing ‘Promotion ofBreastfeeding Initiation and Duration’ (2006) includes a comprehensive review of the currentevidence base for supporting the initiation and continuation of breastfeeding in the UK. ThePublic Health Briefing recommends that there should be provision of a ‘best package’ to suit localneeds that is informed by practitioners and service users and that targets areas where rates arelowest. It also recommends implementation of the UNICEF Baby Friendly Initiative in hospital andcommunity settings.The introduction of the Baby Friendly Initiative in the UK was launched in 1994. It provides aframework for both implementation and audit of best evidence based practice. It includes aSeven Point Community Plan which aims to promotes, protect and support breastfeeding incommunity health care settings. Facilities that meet the required standards can apply foraccreditation as Baby Friendly.47
The Seven Point Plan for the Protection, Promotion and Support of Breastfeeding in CommunityHealth Care Settings recommends:1 A written breastfeeding policy that is routinely communicated to all health care staff.2 Training all staff involved in the care of mothers and babies in the skills necessary toimplement the policy.3 Informing all pregnant women about the benefits and management of breastfeeding.4 Supporting mothers to initiate and maintain breastfeeding.5 Encouraging exclusive and continued breastfeeding, with appropriately timedintroduction of complementary foods.6 Providing a welcoming atmosphere for breastfeeding families.7 Promoting co-operation between healthcare staff, breastfeeding support groups and thelocal communityThe NICE Clinical Postnatal Guidelines (Demott, 2006) recommends that “all healthcare providers(hospital and community) should implement an externally evaluated structured programme thatencourages breastfeeding using the Baby Friendly Initiative as a minimum standard” andconcludes that “it is highly likely that the initiative is cost-effective.” The document also highlightsthat Trusts that have achieved the accreditation have increased the breastfeeding initiation ratesby more than 10% average, over a four-year period, with evidence of sustainability. Dyson et al.(2006) found high quality evidence that both health professional support and peer support can beeffective in supporting both exclusive and any breastfeeding.Incorporating the proposed indicators within <strong>QOF</strong>+ would contribute to practices addressingpoints 3 and 4 of the Baby Friendly Initiative’s Seven Point Community Plan.There is evidence from a Cochrane systematic review (Dyson, 2007) that antenatal breastfeedingeducation has a significant effect on increasing initiation rates of breastfeeding compared withroutine care.Recently published NICE guidance on improving the nutrition of pregnant and breastfeedingmothers and children in low-income households recommends that:“during individual antenatal consultations GPs, obstetricians and midwives shouldencourage breastfeeding. They should pay particular attention to the needs of womenwho are least likely to breastfeed (for example, young women, those who have loweducational achievement and those from disadvantaged groups).” (NICE, 2008)48
Degree of perceived professional consensusA Seven Point Plan for the Protection, Promotion and Support of Breastfeeding in CommunityHealth Care Settings was developed in consultation with UK health and medical professionals(UNICEF UK, 2004).A consultation with local stakeholders, including representatives from primary care and publichealth, showed overall consensus for the scientific soundness, importance and feasibility of theseindicators in <strong>QOF</strong>+.Degree of perceived support from patients and carersThe development of the UK Baby Friendly Initiative has been informed by the views of keystakeholders, including mothers (UNICEF UK, 2004).Impact on health inequalitiesThere is a strong inverse association between breastfeeding rates, social class and ethnicity(Bolling et al., 2007). Department of Health Public Service Agreements (PSA) direct organisationsto “reduce health inequalities by 10% as measured by infant mortality and life expectancy atbirth.” This includes a target to “deliver an increase of two percentage points a year inbreastfeeding initiation rates, focusing on women from disadvantaged groups”Health ImpactBreastfeeding provides many short and long-term health advantages for a woman and her baby.Benefits of breastfeeding for the infant include protection against gastrointestinal, urinary,respiratory and middle ear infection (Aniansson et al. 1994; Howie et al. 1990; Pisacane et al.1992) and atopic disease, especially if there is a family history of this (Burr et al. 1989; Oddy et al.1999). There is also increasing evidence of long-term protection against cardiovascular disease(Wilson et al., 1998}. For the woman, breastfeeding can reduce the risk of certain forms ofcancer, including breast cancer (DoH, 1996). Other advantages associated with breastfeedinginclude promotion of attachment between the mother and her infant, and ready availability ofnourishment for the baby (Bick et al., 2002)Workload and training implicationsThere will be a need for staff involved in the care of mothers and babies to be trained in the skillsnecessary to work towards implementing the Baby Friendly Initiative. For details of the proposed training package see section 14.3.4 (p93).49
ReferencesAniansson, G., Alm, B., Andersson, B., Hakansson, A., Larsson, P., Nylen, O., Peterson, H., Rigner, P.,Svanborg, M., Sabharwal, H (1994) A prospective cohort study on breast-feeding and otitis media inSwedish infants Pediatric Infectious Disease Journal; 13 (3) 183-188.Bick, D., MacArthur, C., Knowles, H., Winter, H. (2002), Postnatal Care. Evidence and Guidelines forManagement. Edinburgh: Churchill Livingstone.Bolling K, Grant C, Hamlyn B, Thornton A. (2007) Infant Feeding Survey 2005. The Information Centre.Burr, M. L., Miskelly, F. G., Butland, B. K., Merrett, T. G., & Vaughan-Williams, E. (1989) Environmentalfactors and symptoms in infants at high risk of allergy Journal of Epidemiology and Community Health43 (2) 125-132.Demott K, Bick D, Norman R, Ritchie G, Turnbull N, Adams C, Barry C, Byrom S, Elliman D, Marchant S,Mccandlish R, Mellows H, Neale C, Parkar M, Tait P, Taylor C, (2006) Clinical Guidelines And EvidenceReview For Post Natal Care: Routine Post Natal Care Of Recently Delivered Women And Their Babies<strong>London</strong>: National Collaborating Centre For Primary Care And Royal <strong>College</strong> Of General Practitioners.Department of Health. (1996), Breastfeeding: good practice guidance to the NHS Department ofHealth.Department of Health (2004), National Service Framework for Children, Young People and MaternityServices: Core Standards. <strong>London</strong>: Department of Health.Department of Health (2004) Choosing Health: Making healthy choices easier. The Stationary Office.<strong>London</strong>Dyson L, Renfrew M, McFadden A, et al. (2006) Promotion of breastfeeding initiation and duration:Evidence into practice briefing. National Institute for Health and Clinical Excellence.Dyson L, McCormick F, Renfrew MJ (2007). Interventions for promoting the initiation of breastfeeding.(Cochrane Review). In: Cochrane Database of Systematic Reviews, Issue 2, Chichester: WileyInterscience.Hamlyn, B., Brooker, S, Oleinikova, K. (2002) Infant Feeding 2000: a survey conducted on behalf of theDepartment of Health, the Scottish Executive, the National Assembly for Wales and the Department ofHealth Social Services and Public Health in Northern Ireland. <strong>London</strong>: Stationary Office.HM Treasury (2007) PSA Delivery Agreement 12: Improve the health and wellbeing of children andyoung people. The Stationary Office: <strong>London</strong>Howie, P. W., Forsyth, J. S., Ogston, S. A., Clark, A., & Florey, C. D.(1990) Protective effect of breastfeeding against infection British Medical Journal; 300(6716) 11-16.NICE Clinical Guideline (2008) Antenatal Care. National Institute for Health and Clinical ExcellenceNICE public health guidance 11 (2008) Improving the nutrition of pregnant and breastfeeding mothersand children in low-income households. National Institute for Health and Clinical Excellence.Oddy, W. H., Holt, P. G., Sly, P. D., Read, A. W., Landau, L. I., Stanley, F. J., Kendall, G. E., & Burton, P. R.(1999) Association between breast feeding and asthma in 6 year old children: findings of aprospective birth cohort study British Medical Journal; 319(7213) 815-819.Pisacane, A., Graziano, L., Mazzarella, G., Scarpellino, B., & Zona, G. (1992) Breast-feeding and urinarytract infection Journal of Pediatrics; 120 (1). 87-89.UNICEF UK. UNICEF UK baby friendly initiative: seven point plan. 2004 [Accessed 30.7.08]; Availablefrom URL:www.babyfriendly.org.uk/commun.aspWilson, A. C., Forsyth, J. S., Greene, S. A., Irvine, L., Hau, C., & Howie, P. W. (1998) Relation of infantdiet to childhood health: seven year follow up of cohort of children in Dundee infant feeding studyBritish Medical Journal 316 (7124) 21-25.World Health Organisation (2003) Global strategy for infant and young child feeding. Geneva: WorldHealth Organisation.Zeuner, D (2008) Annual Report of the Director of Public Health 2007-2008 Hammersmith and FulhamPCT50
<strong>QOF</strong>+ report on ethnicityProposed IndicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ ETHNICITY 1. The percentage of patients on one or morepractice registers for: CVD At-Risk, Hypertension, CHD,Diabetes, Mental Health and Stroke and TIA whose notesrecord their ethnicity and first language+ ETHNICITY 2. The percentage of patients who have newlyregistered with the practice on or after December 01 2008whose notes record their ethnicity and first language30 60-90%20 90-100%It is recognised that this indicator set partly overlaps with the existing RECORDS 21 <strong>QOF</strong> Indicatorand also partly overlaps with the recently announced Directed Enhanced Service (DES) forEthnicity for 2009/10 (which provides incentives for collection of data on ethnicity and religion).BackgroundIt is now recognised that health-seeking behaviour, use of health services, and differential accessto health services among different ethnic groups in the UK may explain patterns of ill-health(Hargreaves, 2007).The cultural appropriateness of health-care provision in the UK has been questioned, and there isevidence of inequity in access to services, both at the referral level from GPs and in the quality ofcare offered, which may differ both within individual ethnic groups and between ethnic groupsand the White population (Arai et al., 2002).Through the use of good and robust ethnic group data on patients and service users, the NHS andcouncils will be in a better position to address health inequalities, difficulties in access anddiscrimination experienced by some black and minority ethnic individuals and communities. As aresult, the NHS will be better placed to contribute to national targets and meet local corestandards (DoH, 2007b).51
The Department of Health states that the 16 code national standard should be used as aminimum for collecting and reporting on the ethnic group of patients, service users and staff. Thisis as follows:White British Indian CaribbeanIrish Pakistani AfricanOther White Bangladeshi Other BlackWhite and Black Caribbean Other Asian ChineseWhite and AsianWhite and Black AfricanOther Ethnic GroupNot stated / refusedOther MixedPriority and relevance to national policyThe Government white paper ‘Saving Lives: Our Healthier Nation’ highlighted the need for moreresearch into the needs of ethnic minority groups and the aim of improving the health of themost marginalised members of society (DoH, 1999).The Race Relations Act 1976 and The Race Relations (Amendment) Act 2000 place a generalstatutory duty on public authorities to promote race equality and monitor policy and servicedelivery for different ethnic groups. Specific duties have also been placed on listed authorities(including the Department of Health, NHS trusts, primary care trusts, special health authoritiesand strategic health authorities) to assist them in meeting the general statutory duty. The specificduties include a requirement to collect and publish a specific set of information relating to theethnicity of employees and to assess, consult on and monitor the impact of policies and serviceson the promotion of race equality.The Operating Framework for the NHS in England 2008-09 lists reducing inequalities as an explicitpriority (DoH, 2007a).DemographyAccording to Census 2001 data (ONS, 2002) from a population of 165,242 in Hammersmith andFulham, 22.2% of the population reported a non-white ethnic group, which included 5% blackCaribbean, 5% black African, with various other ethnicities (including Indian, Pakistani, Banglaeshiand Chinese) making up the remaining 11%. There are also sizable Polish and Irish communities.33.6% of the population reported being born outside the UK.There are also known to be significant numbers of refugees and asylum seekers in Hammersmithand Fulham, and a study by Lukes et al. (2002) found that 6.3%-7.2% of the population inHammersmith and Fulham were asylum seekers or refugees (9,800-11,300).The ethnic composition of wards in Hammersmith and Fulham is strongly associated withdeprivation levels. The four most deprived wards in Hammersmith and Fulham have the largestBlack and Minority Ethnic (BME) populations (Zeuner, 2008).52
Associated Morbidity and MortalityThe incidence, prevalence, and mortality of many diseases are known to vary by ethnic group,and those in certain ethnic groups experience inequities in access to prevention, treatment, andpalliative health and social care services. There are also differences in the quality of services andoutcomes of treatment and care for different ethnic groups (<strong>London</strong> Health Observatory, 2006).Local contextHammersmith and Fulham ranks 59 (out of 354) for deprivation in local authorities in England,and 28% of the population live within the most deprived fifth of areas nationally. The deprivationlevel has not substantially changed since 2004. The north of the borough is particularly deprived,although deprivation and wealth often occur in close proximity. The borough has a particularlyhigh level of income deprivation that affects children, and almost 10,000 children live in lowincomehouseholds. High proportions of school pupils speak English as an additional languageand are eligible for free school meals (Zeuner, 2008)In the last few years, NHS Hammersmith and Fulham has made significant progress in ethnicityreporting. However, the quality of ethnic recording in community services and general practiceremains relatively poor.Review of evidence to support proposed indicatorsThe current <strong>QOF</strong> includes an indicator relating to recording of ethnicity for newly registeredpatients.Soljak et al. (2007) suggest that “it is clearly feasible to extend the recording of ethnicity at thetime of new patient registration to all patients with <strong>QOF</strong> diseases across the UK as a next step,”and the findings of their study suggest that “lack of recording is a proxy for overall poor quality ofrecording and of clinical care.”Senior (1994) has highlighted that collection of routine data on ethnicity alone masks a number ofimportant factors influencing service use or health needs, including significant differencesbetween patient groups in the same ethnic category. Gerrish (2000) suggests that a wider rangeof variables including language may be more appropriate from the perspective of both researchand planning.Research shows that language and communication issues are important barriers to care,influencing many aspects of service use (Hargreaves, 2007; Levy, 2005). There is evidence thatpoor communication with GPs due to language barriers is associated with confusion regardingadvice and the medicines prescribed (Free et al., 1999) and is a key factor associated with delayeddiagnosis and misunderstood treatment regimens (Green et al., 2002). Research suggests that useof services such as Language Line, community interpreting services and health advocates byservice providers remains patchy, and in many areas, interpreting services are considered to beinadequate and of poor quality, costly, and with many service providers lacking adequate training(Gerrish, 2004; Murphy et al., 2002).53
Degree of perceived support from professionalsThere is strong professional consensus from the BMA, RCGP and GMC for the principles of codingethnicity and first language. Soljak et al. (2007) comment that “there is a high level of awarenessof the importance of ethnicity as a disease risk factor, and many practices appear to be usingethnicity as an indicator of risk for clinical management purposes already”.Degree of perceived support from patients and carersThere is support from a number of patient organisations including Diabetes UK for the principlesof coding of ethnicity and first language.It is important to note that ethnic monitoring still arouses suspicion for some people who maysee the process as a means of further discriminating against them. The reasons for ethnicmonitoring should, therefore, be carefully explained, and analyses and decisions, based on theresults of ethnic monitoring, should be openly shared (DoH, 2007).Impact on health inequalitiesCollecting, analysing and using data on ethnic group will enable comparison of “uptake of servicesbetween different groups to ensure fairness in allocation of resources and delivery of servicesaccording to needs and, where appropriate, to address health inequalities experienced byparticular ethnic groups” (DoH, 2007). This process will be enhanced further by the collection andanalysis of data on first language.Ethnic monitoring and data collection of ethnicity and first language are essential steps towardsensuring that the NHS provides equity of access, delivery and outcomes for all service users.Health impactEthnic monitoring and data collection on ethnicity and first language will“…contribute to assessments of individuals' needs and circumstances, thereby ensuringthat access to services and service delivery can be as personalised and appropriate aspossible. For example, insights into a person's ethnic background - or the ethnicbackground of their family - may assist with diagnosis. Information about a person's mainspoken language and competency in English could indicate a need for translation andinterpreting services.” (DoH, 2007)The process will also “assist with the clinical management of patients as the prevalence andcourse of many conditions varies by ethnicity” (DoH, 2007).54
Workload and training implicationsPrimary care staff should already be familiar with the process of ethnic monitoring as it is in thecurrent national <strong>QOF</strong>. However, the existing <strong>QOF</strong> indicator refers to coding for new registrations,and practices will need to put in place a system for collecting data on ethnicity and first languagefor those on the specified chronic disease registers. This process can be facilitated through theuse of templates.Training will be required for primary care staff with respect to the importance of and rationale forethnicity monitoring. Training is critical to the success of collecting ethnic group data, and shouldbe tailored to local circumstances and experiences of ethnic monitoring (DoH, 2007). For details of the proposed training package see section 14.3.5 (p93).ReferencesArai L, Harding S (2002). Health and social care services for minority ethnic communities in the UnitedKingdom: a review of the literature on access and use. Glasgow: MRC Social and Public Health SciencesUnit, University of GlasgowAspinall P and Jacobson B (2006) How to analyse ethnic differences in health, Health care and theworkforce: a toolkit for the NHS. <strong>London</strong> Health Observatory. <strong>London</strong>Department of Health (2007a) The NHS in England; The Operating Framework for 2008/9 Departmentof Health. <strong>London</strong>Department of Health (2007b) A practical guide to ethnic monitoring in the NHS and social care.Department of Health. <strong>London</strong>Department of Health (1999) Saving Lives: Our Healthier Nation. <strong>London</strong>: HMSOGreen G, Bradby H, Chan A, Lee M, Eldridge K (2002). Is the English National Health Service meetingthe needs of mentally distressed Chinese women? J Health Services Research Policy 7:216-21.Free C, White P, Shipman C, Dale J (1999). Access to and use of out-of-hours services by members ofVietnamese community groups in South <strong>London</strong>: a focus group study. Family Practice ;16:369-74.Gerrish K (2000). Researching ethnic diversity in the British NHS: methodological and practicalconcerns. Journal of Advanced Nursing 31:918-25.Gerrish K, Chau R, Sobowale A, Birks E (2004). Bridging the language barrier: the use of interpreters inprimary care nursing. Health and Social Care Community 12:407-13.Hargreaves S (2007) The impact on and use of the UK’s National Health Service by new migrants . PhDThesis. The International Health Unit, <strong>Imperial</strong> <strong>College</strong> <strong>London</strong>. University of <strong>London</strong>Levi S (2005) Barriers to health care and experiences for asylum seekers and recently settled refugeesin East Kent. <strong>London</strong>: University of <strong>London</strong>Lukes S, Bell M. (2002) Renewing West <strong>London</strong>. Refugee communities: their hopes and needs. Abaseline study for Renewal. <strong>London</strong>: Michael Bell AssociatesMurphy D, Ndegwa D, Kanani A, C R-J, Webster A (2002) Mental health of refugees in inner-<strong>London</strong>.Psychiatric Bulletin 26:222-224.ONS. Census 2001 (2002) <strong>London</strong>: HMSO/UK Office for National StatisticsSenior P, Bopal R(1994)Ethnicity as a variable in epidemiological research.British Medical Journal309:327-330Soljak, M, Majeed A, Eliahoo J, Dornhorst A (2007) Ethnic inequalities in the treatment and outcome ofdiabetes in three English Primary Care Trusts International Journal for Equity in Health 6:8Zeuner, D (2008) Annual Report of the Director of Public Health 2007-2008 Hammersmith and FulhamPCT55
<strong>QOF</strong>+ report on recordsProposed indicatorsIndicator<strong>QOF</strong>+pointsPaymentstages+ PRESCRIPTION 1. The percentage of individual repeatmedications issued which have a diagnosis or symptom in theelectronic medical record relating to that medication+ REFERRALS 1. The percentage of outpatient referrals madeon or after December 01 2008 where both the referred-tospeciality and diagnosis/symptom triggering referral are codedon the clinical system+ CARERS 1. Carer status is recorded for 100% of individualsnewly registered on or after December 01 2008+ OSTEOARTHRITIS 1. The practice is able to produce aregister of patients who have osteoarthritis+ RHEUMATOID ARTHRITIS 1. The practice is able to producea register of patients who have rheumatoid arthritis+ ECZEMA 1. The practice is able to produce a register ofpatients who have eczema+ PSORIASIS 1. The practice is able to produce a register ofpatients who have psoriasis45 40-90%50 70-90%6 -1 -1 -1 -1 -It is recognised that + PRESCRIPTION 1 overlaps with the existing RECORDS 9 <strong>QOF</strong> Indicator.BackgroundGeneral practitioners are responsible for providing primary care services and for organisingreferrals for specialist care. These records are increasingly held in electronic format and canprovide excellent information on morbidity, risk factor and health care utilisation patterns on thelocal population. The medical records held by general practitioners are therefore a key resourcein improving quality of care and promoting public health.The quality of data recording in general practice has been variable and this incentive scheme willencourage improvement in data quality locally (Jordan et al., 2004).57
Priority and relevance to national policyThere are a number of existing frameworks which describe best practice with regards dataquality; perhaps the best example is the guideline for data recording for practices contributing tothe General Practice Research Database (GPRD). More recently, the drive to deliver the NationalProgramme for IT for the NHS led to the introduction of a national directed enhanced service forinformation management and technology (IM&T DES) aimed at improving data quality.Improvement in data quality by promoting diagnosis recording for repeat prescriptions is a goodway of improving data quality across the board in chronic disease management. The suggestedindicator is generally perceived to be best practice amongst the profession, but in this instanceattracts a potentially significant reward. This is for a number of reasons, but mainly because ofthe possible clinical improvement that this may drive.Firstly, practices will provide much improved disease register data, which will have many uses at alocal and wider public health level. Secondly, as a consequence, there is the potential foridentifying additional patients who will fall under <strong>QOF</strong> domains; this in turn will increaseworkload. Thirdly, there is a significant patient safety issue with repeat prescriptions issuedwithout a clear diagnosis. It is expected that this indicator will lead to a transformation in dataquality in year 1 and therefore may attract fewer points in future years.Prevalence of conditionsNew disease registers for carers, chronic musculoskeletal conditions and chronic skin conditionshave been included due to the high prevalence and morbidity that these can cause.The 2001 census suggests that there are 6 million carers in the UK (10% of the total population)whilst the General Household Survey (and the Northern Ireland equivalent the Health and SocialWell-being Survey) estimates the figure to be over 7 million. The Department of Health iscurrently piloting schemes to improve the mental and physical health of carers, but implementingthis requires identification of those in need.In England musculoskeletal conditions have an estimated prevalence of 9.5 million (16% of thepopulation) according to the 2008 Burden of Disease scoping study commissioned by theDepartment of Health. From the same study, skin and subcutaneous conditions have anestimated prevalence of 7.9 million (9% of the population).Associated morbidity and mortalityOsteoarthritis (OA), a degenerative joint disease, is the most prevalent form of arthritis, affecting25% of UK adults over 50 years old and can result in disabling symptoms in an estimated 10%(McCormick et al., 1995). OA is one of the most commonly diagnosed conditions amongst olderpatients in general practice, third only behind acute bronchitis and essential hypertension(McCormick et al, 1995). Disability secondary to knee OA is reported to be comparable to thatcaused by cardiac disease and greater than any other medical condition in the elderly population(Guccione AA et al., 1994).58
Rheumatoid Arthritis (RA) is an autoimmune condition characterised by pain, swelling andprogressive destruction of peripheral joints. Although less common than OA (1% of UKpopulation), there is a significant burden of morbidity that can profoundly affect the quality of lifeof those living with the condition. While progression can be variable, up to 40% of affectedindividuals will no longer be able to work five years post-diagnosis, while overall life expectancy isreduced by 5-10 years (NICE, 2007). Prompt diagnosis and aggressive early treatment withdisease modifying agents (DMARDS) are important in limiting joint damage (Grigor, 2004) andthis is contingent on effective management in primary care. A multidisciplinary approach isimportant in responding early to changes in disease activity, controlling pain and in providingsupport where there is increased physical and financial dependence (SIGN, 2000).Eczema is used as an umbrella term for a range of chronic, episodic skin conditions where signs ofinflammation predominate (e.g. redness, itching, scaling and cracking). Symptoms often presentin early childhood (affecting up to 20%) and approximately half will persist into adulthood(PCSD/BAD, 2003; Williams, 2006). However, the variation in the severity and course of thecondition and the broadness with which the diagnostic term is applied makes this a heterogenouspatient group. There are concerns that the stepwise approach to care advocated in best practiceguidance (NICE, 2007a), although consensus-based rather than evidentiary (National PrescribingCentre, 2003), is not being followed in primary care and that strategies around prevention(trigger avoidance in Atopic disease), routine emollient use (even when disease is quiescent) andthe appropriate, tailored prescribing of corticosteroids are not being applied in a systematic way.Visible skin changes can be stigmatising, particularly for children, while the need for intensivetreatment in some patients can interfere with normal activities.Psoriasis affects 1.5% of the UK population (Gelfand et al., 2005) and is a skin disorder thatcharacterised by the formation of scaly plaques. There is increasing interest in its association withother systemic conditions (for example arthritis, diabetes and CVD), particularly in more severeforms of the disease (Hanseler and Christophers, 1995). Pharmacotherapy is evolving rapidly andnow includes novel biological agents. Primary care practioners need to be aware of this changinglandscape to select appropriate topical agents (British Association of Dermatologists, 2006). Thepsychosocial impact of the condition is typically underestimated, and a role for activeidentification of anxiety and depression symptoms in primary care is advocated (Griffiths andBarker, 2007).Local contextThe aims are to make the use of electronic patient record systems ubiquitous in general practicesin Hammersmith and Fulham and to ensure that the quality of the data stored on these systemsis amongst the highest in the UK.Achievement of high standards of data quality will allow the development of better identificationand management of people with chronic diseases and risk factors for poor-health. We expectthese high quality records to be used to drive improvements in health care quality, efficiency andin public health (Gnani and Majeed, 2006). The minimum standards in this framework have beenselected for these reasons, whilst ensuring the broader aims of the <strong>QOF</strong>+ scheme are met.59
Specific reasons for this framework are:1 A minimum data quality standard is required to accurately validate work done for <strong>QOF</strong>+.2 Incentives for specific disease areas may have a detrimental effect on other areas ofclinical management that are not covered by these incentives. Minimum standards indata quality can be applied across a wider range of health domains, which will encouragemore standardisation of care in areas not incentivised by current the <strong>QOF</strong> or <strong>QOF</strong>+schemes.3 There are a number of disease areas, with a high burden of disease, which are notrewarded through <strong>QOF</strong> or <strong>QOF</strong>+. Improving data standards will raise the profile of theseareas.4 Improving existing data quality will allow practices and the PCT to be more effective atpro-actively finding ‘at-risk’ patient groups and so aid health promotion and prevent illhealth.Specific examples are recording details of exercise habits and dietary status (inthe future).5 High quality data will also allow better monitoring of health inequalities across the PCTthat is known to have a diverse ethnic and socio-economic population mix.6 High quality primary care data across Hammersmith and Fulham will enable audit thataccurately describes current clinical practice and the population being served. This will inturn allow better service planning and commissioning, and identification of educationand training needs.High quality electronic data from general practices is an essential element for the Hammersmithand Fulham <strong>QOF</strong>+ financial incentive scheme. This proposed framework requires all practices tohave electronic patient records and to use them as their default medical record system. Anelectronic record allows relatively easy and accurate searching for the purposes of audit andverification, as well as being used as a tool to identify at risk groups quickly. Without an electronicrecord the intended outcomes of the <strong>QOF</strong>+ incentive scheme are less likely to be achieved.Data standards matching or exceeding the requirements of each indicator in this framework willlead to a payment. Each indicator is an ‘all or nothing’ payment according to whether a practicereaches a certain standard, and so they are not designed to be unattainable since this maydiscourage the transformational improvement in practice that the <strong>QOF</strong>+ scheme will require. Infact, full attainment of year 1 targets is ultimately desirable, both to drive up data standards andto achieve ‘buy-in’ to the scheme from general practices on the understanding that targets willrise in future years in a continual drive for improvement.Review of evidence to support the proposed indicatorsThe standards set for each indicator of quality are designed to be challenging, with the aim ofincrementally raising the bar in each successive year of the scheme. This process of tangiblefinancial reward and feedback of results has been described as best practice in any effectiveprimary care data quality programme (De Lusignan and Teasdale, 2004).60
Degree of perceived professional consensusThere is strong support for the principle of improving data quality from professional organisationsincluding the BMA and the RCGP.Degree of perceived support from patients and carersThis is strong support from a range of patient and carer organisations locally and nationally.Impact on health inequalitiesHigh quality data will allow better monitoring of health inequalities across a PCT that is known tohave a diverse ethnic and socio-economic population mix, and will allow better service planningand commissioning, and identification of education and training needs.Health impactThe provision of high standard care can only be measured if the data is recorded accurately, andconversely high quality data can be used to improve clinical care, particularly with respect tohealth promotion and disease prevention.61
Workload and training implicationsThere may be significant administrative workload implications and additional training for practiceadministrative staff may be required. NHS Hammersmith and Fulham will be able to provideadditional support and training for this process if necessary.The assessment and verification process for these indicators will be developed and refined duringthe course of the scheme. Payment will be based on a practice declaration of attainment, and anyverification will occur post-payment.For the + PRESCRIPTION 1 indicator it is expected that all repeat medicines issued fromcommencement of the scheme will have a diagnosis or symptom related to that prescription inthe patient’s active problem list. This includes any prescriptions that may only be issuedinfrequently or as required, such as prescriptions for gout medications or analgesia. It will not benecessary for an individual medication to be ‘linked’ to a symptom or diagnosis, but simply forthe symptom or diagnosis to be recorded in the active problem list. The workload for GPs isexpected to be in the form of a brief review and update of the active problem list wheneverrepeat medications are prescribed. This will significantly improve monitoring of chronicconditions and subsequently the quality of care for these patients.For the + REFERRALS 1 indicator, each practice will be expected to ensure a record has beenmade of referrals to secondary care outpatient clinics with diagnosis and symptom referred for,and specialty of referral. Emergency referrals to A&E will not be subject to this indicator. It isexpected that this will increase workload for GPs or administrative staff as they will be requiredto ensure that a proper record has been made.The identification of carers from new registrations for the + CARERS 1 indicator is unlikely to addmuch workload to the processes already required for new registrants. An additional question onexisting new patient questionnaires may be required if one is not already included, andadministrative staff may need to ensure that this question is answered by the new registrant.A consequence of the + PRESCRIPTION 1 indicator is that the final 4 indicators regarding practiceregisters for arthritis and eczema/psoriasis should naturally be populated. This should requireminimal additional work by the practice on top of that already undertaken, save to verify that theregisters are a true reflection of the practice’s populations with these conditions. For details of the proposed training package see section 14.3.6 (p95).62
References2001 Census web site: http://www.statistics.gov.uk/census2001/profiles, National Statistics Office,2003.British Association of Dermatologists (2006). Psoriasis guideline 2006. [Available online, Accessed27/11/2008]http://www.bad.org.uk/healthcare/guidelines/psoriasis_guideline_(Final_update)_280906.pdfDe Lusignan S & Teasdale S. The features of an effective primary care data quality programme.Healthcare Computing 2004; 95-102.Department of Health. Carers at the heart of 21 st century families and communities. <strong>London</strong>: HMGovernment; 2008.Department of Health, Social Services and Public Safety. Informal Carers Report, A report from theHealth and Social Wellbeing Survey 1997, Northern Ireland; 2001.Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. (2005) Prevalence andtreatment of psoriasis in the United Kingdom. Arch Dermatol 141:1537-41General Practice Research Database Group. GPRD recording guidelines for Vision users. <strong>London</strong>:MRHA; 2004.Gnani S & Majeed A. A user’s guide to data collected in primary care in England. Eastern Region PublicHealth Observatory; 2006.Green G, Bradby H, Chan A, Lee M, Eldridge K (2002). Is the English National Health Service meetingthe needs of mentally distressed Chinese women? J Health Services Research Policy 7:216-21.Griffiths CE and Barker JNWN (2007). Pathogenesis and clinical features of psoriasis. Lancet 370:263-71Grigor C, Capell H, Stirling A, McMahon AD, Lock P, Vallance R, et al. (2004) Effect of a treatmentstrategy of tight control for rheumatoid arthritis (the TICORA study): a single-blind randomisedcontrolled trial. Lancet 364:263–9Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. (1994) The effects ofspecific medical conditions on the functional limitations of elders in the Framingham Study. Am JPublic Health 84:351-8Jordan K, Porcheret M and Croft P. Quality of morbidity coding in general practice computerizedmedical records: a systematic review. Family Practice 2004; 21: 396-412.Lukes S, Bell M. (2002) Renewing West <strong>London</strong>. Refugee communities: their hopes and needs. Abaseline study for Renewal. <strong>London</strong>: Michael Bell AssociatesMaher J & Green H. Carers 2000 Office for National Statistics, The Stationery Office: <strong>London</strong>; 2002.McCormick A, Fleming D, Charlton J. (1995) Morbidity Statistics from General Practice. Fourth NationalStudy 1991-1992. HMSONational Institute for Clinical Excellence (NICE) (2007) Rheumatoid arthritis: the management andtreatment of rheumatoid arthritis in adults, final scope. [Available online, Accessed 27/11/2008]http://www.nice.org.uk/nicemedia/pdf/RAScope.pdfNational Institute for Clinical Excellence (NICE) (2007a) Clinical guideline: atopic eczema in children[Available online, Accessed 27/11/2008]http://www.gserve.nice.org.uk/Guidance/CG57/Guidance/pdf/EnglishNational Prescribing Centre. (2006) MeReC bulletin - atopic eczema in primary care. [Available online,Accessed 27/11/2008] http://www.npc.co.uk/MeReC_Bulletins/2003Volumes/Vol14no1.pdfPrimary Care Dermatology Society & British Association of Dermatologists. (2005) Guidelines on themanagement of atopic eczema. [Available online, Accessed 27/11/2008]http://www.bad.org.uk/healthcare/guidelines/PCDSBAD-Eczema.pdfScottish Intercollegiate Guidelines Network (SIGN) (2000) Management of early rheumatoid arthritis.[Available online, Accessed 27/11/2008] http://www.sign.ac.uk/pdf/sign48.pdf63
<strong>QOF</strong>+ report on newpatient screeningProposed indicatorIndicator+ PATIENT REGISTRATION 1. The practice is trained in and implements thePCT TB Early Referral Protocol to identify and refer patients who are newlyregistered at the Practice and who are new entrants to the UK fromcountries with a high TB prevalence<strong>QOF</strong>+points5The proposed indicator is designed to help implement a TB early referral and screening scheme inHammersmith and Fulham. Early referral for TB new entrant screening has been successfullypiloted in four local practices and it is planned to roll this scheme out in all GP practices in theborough.The PCT Protocol for TB Early Referral states that “New entrants to the UK from countries with ahigh TB prevalence should be identified at the point of registration with their GP practice”. Theterm ‘New entrants’ refers to people who entered the UK within the last 5 years from a foreigncountry with a TB prevalence of >40/100,000; i.e. most countries outside of the European Union,North America, Australia or New Zealand (a detailed list is included in Section R8 of the ResourcePack). The protocol also states that patients who are new entrants who came from one of thesecountries within the last 5 years via a third country should also be referred.A minimum of one key person from each participating practice should have attended a brieftraining session organised through the TB Service, and this person would be responsible forcascading this information to the relevant personnel in the practice.BackgroundTuberculosis (TB) is the leading cause of death among treatable infectious diseases globally,causing an estimated 9 million new infections and 2 million deaths per year globally. Rates havedecreased in Britain throughout the 20th century mainly due to improved living standards,vaccination and the introduction of antibiotics. However TB rates started to increase again fromthe 1980s. 40% of all the new cases in the UK occur in <strong>London</strong> and the rates are highest amongstparticular risk groups, such as those living in overcrowding and socioeconomic deprivation, aswell as those who recently entered the UK from other countries, where TB is much moreprevalent.65
In 2007 the North West <strong>London</strong> Sector had one of the highest TB rates in the country (59.8 per100.000), and rates for Hammersmith and Fulham were reported to be 40.3 per 100,000 (Zeuner,2008). 87.5% of all new notifications in the UK were from residents born outside of the UK, and48.6% of cases where year of entry was recorded entered the UK within the last 5 years. (NW<strong>London</strong> TB Network, 2008). Inclusion of an indicator in <strong>QOF</strong>+ relating to early referral for TB newentrant screening and early referral has been locally identified as a way to address this.Priority and relevance to national policyThe Chief Medical Officer (CMO) identified TB as “new threat which needs concerted action todeal with it”. He laid out the government’s commitment and recommended next steps to tacklethis new epidemic in an action plan (DoH, 2004). This action plan was accompanied by a nationaltoolkit (DoH, 2007).The CMO’s action plan recommends in action 7 to “transform practices for improving casefinding, including targeted screening among high risk groups, in particular: *…+ disseminatemodels of good practice for screening new entrants to this country *…+” (DoH, 2004). Theproposed referral scheme is in line with national policies.Prevalence of conditionThere were 69 TB cases in Hammersmith and Fulham during 2007 (40.3 per 100,000) and thenotification rate of residents born outside of the UK was more than 2½ times higher than in UKbornresidents in 2006 (Zeuner, 2008).Associated morbidity and mortalityApproximately 10% of those infected will develop active TB disease (more, ifimmunocompromised or living in adverse living conditions). Untreated TB disease has a very highmorbidity and an almost 50% mortality rate. In addition, those with untreated pulmonary TB willtransmit their infection to approximately 10-15 others per year. However, appropriately treatedTB is curable and patients can resume a normal life with no or very few sequelae from this illness.Local contextTackling Tuberculosis locally was seen as a key priority for Hammersmith and Fulham and the2007/08 PCT Operating Plan includes speeding up access to treatment for suspected TB as a keypriority target (H&F, 2007). A local action plan has been agreed, based on best practicerecommended by NICE (2006). One of the three key areas is to “increase the percentage of newentrants who are screened for active and latent TB in line with NICE’s clinical guideline.”Identifying individuals at risk for TB at the point of GP registration was recognised as animportant area to support this key area.The proposed referral system was piloted in four local GP practices and the feedback from boththe practices as well as the TB service in Hammersmith Hospital was very positive. A more formalfinal evaluation of this pilot will follow.66
Review of evidence to support the proposed indicatorsCurrent NICE guidance recommends that “New entrants should be identified for TB screeningfrom *…+ new registrations with primary care” amongst others (NICE, 2006), where “new entrantsare defined as people who have recently arrived in or returned to the UK from high-incidencecountries, with an incidence of more than 40 per 100,000 per year.” This NICE recommendation isbased on grade B evidence, i.e. there have been at least some very good quality observationalstudies in support of this. Schwartzman and Menzies (2000) found new entrant screening withchest X-rays and tuberculin tests cost effective to prevent active TB cases in a Canadian modellingstudy.Based on best evidence and cost-effectiveness, NICE recommends different types of screening fordifferent new entrant populations varying mainly by age group and home country TB prevalence.Because of this and the fact that the expected case load per practice is expected to be too low forassuring high TB testing quality it was locally agreed that TB screening would be best placedwithin the TB service and that GP practices should refer these patients for screening.Degree of perceived professional consensusThe proposed approach is in line with current NICE guidelines.Degree of perceived support from patients and carersThe degree of support from patients and the public will depend on careful informationdissemination and a strict avoidance of stigmatisation. This can only be achieved in closecollaboration with practice staff and it is expected that practice staff will require training towardshandling this information. To support this process an explanatory leaflet for patients has beendeveloped. In addition, CITAS (the main interpreter agency) has been briefed about this referralsystem.Impact on health inequalitiesTB affects deprived communities disproportionally more. Ensuring detection and adequatetreatment is expected to help narrow the health inequalities gap.Health impactEarly detection and treatment of TB is lifesaving and prevents further spread of the illness.Improving access to recognition and treatment would therefore yield benefits not only for theindividual, but also for the community as a whole.67
Workload and training implicationsThe proposed referral system was piloted in four local GP practices. Once trained, the staff feltthat the workload was minimal. However there is a need for trained staff, particularlyreceptionists, in order to ensure the appropriateness of referrals. For details of the proposed training package see section 14.3.7 (p96).ReferencesZeuner, D (2008). Annual Report of the Director of Public Health 2007-2008. Hammersmith andFulham PCTDepartment of Health (2004). Stopping Tuberculosis in England. An Action Plan from the Chief MedicalOfficer. <strong>London</strong>: Department of HealthHealth Protection Agency (2007). Tuberculosis in the UK. Annual report on tuberculosis surveillanceand control in the UK 2007. <strong>London</strong>: Health Protection Agency.Department of Health (2007). Tuberculosis prevention and treatment: a toolkit for planning,commissioning and delivering high-quality services in England. <strong>London</strong>: Department of HealthHammersmith and Fulham PCT (2007). Hammersmith and Fulham PCT Operating Plan 2007/08.68
<strong>QOF</strong>+ report onpatient informationProposed indicatorsIndicator+ PATIENT INFORMATION 1. The practice uses the PCT practice informationleaflet template for patients which is designed to include information onthe following: Preventative services such as stop smoking, immunization andscreening Choice / Choose & Book PCT’s Patient Advice & Liaison Service and complaints team Walk-in and urgent care centres Practice opening times including extended hours Information for patients in a range of languages informing them oftheir right to interpreting services during appointments+ PATIENT INFORMATION 2. The practice takes responsibility for regularlyupdating practice information on the NHS choices website+ PATIENT INFORMATION 3. The practice has up to date patientinformation about local training and support for self-management (in theform of posters and leaflets) and that these are clearly displayed forpatients in waiting areas.<strong>QOF</strong>+points373BackgroundThe 2002 Wanless report ‘Securing our Future Health: Taking a Long-term View’ stated that thefuture costs to the NHS depended on how well “people become fully engaged with their ownhealth.” The 2004 Wanless report suggested that it is “the aggregate actions of individuals, whichwill ultimately be responsible for whether of not the fully engaged scenario unfolds.” The needfor better self care is also highlighted in the subsequent NHS Improvement Plan and the NationalService Frameworks, and self-care and self-management are key approaches to meeting theincreasing challenge of caring for people with long-term conditions within the NHS.69
Self care has been defined as “the actions people take for themselves, their children and theirfamilies to stay fit and maintain good physical and mental health; meet social and psychologicalneeds; prevent illness or accidents; care for minor ailments and long-termconditions; and maintain health and well-being after an acute illness or discharge from hospital.”(DoH, 2005), Self care encompasses a range of methods enabling people to manage their ownhealth, including self monitoring, self help and support groups, self management educationprogrammes, patient access to personal medical information, easy access to high qualityinformation on conditions and services and patient-centred telecare.Figure 11.1Self-care encompasses both minor and long term illness. Specific training can help mitigate the impacton lifestyle by providing individuals with skills to manage their illness.The proposed indicators will help ensure that core information on health and well-being, selfcare,and access to appropriate NHS services is provided for all patients. This will support peopleto adopt healthy choices and take responsibility for their own health.It is proposed that the core content of the PCT Practice leaflet template will include informationin a range of languages informing people of their right to interpreting services duringappointments. Content of the leaflets will also be designed to support increasing uptake ofpreventative services, the appropriate use of services, and identification of undiagnosed chronicconditions.70
Priority and relevance to national policyImproving self care for people, including those who live with a long-term condition, is a majorpolicy goal in health in the UK. It is estimated that more than 15 million people in the UK live witha long term condition (DoH, 2006), and long term conditions account for a high proportion of NHStime and resources. Approximately 80% of GP consultations are thought to relate to chronicdisease and patients with chronic disease or complications account for 60% of hospital bed days(DoH, 2004). Health professionals have a vital role in ensuring that patients understand theircondition, and supporting them to self-manage it.Self care includes both self care and self management and was highlighted in the NHS Plan (DoH,2000) as one of the key building blocks for a person-centred health service. The white paper ‘OurHealth, Our Care, Our Say’ (DoHh 2006) also emphasises supporting self care. Supporting Peoplewith Long Term Conditions to Self Care (DoH, 2006) highlights the importance of changing theunderlying culture of health and social care to promote individuals’ empowerment and self care.The Department of Health has recently issued the Common Core Principles to Support Self Carefor the health and social care workforce. Other national policies highlighting the role of self carein the management of long term conditions include the Expert Patients Programme (EPP), theNHS in England: the operating framework 2008/09 (DoH, 2007), and the introduction ofinformation prescriptions following a commitment from Our Health, Our Care, Our Say. Theprinciples of self-care and self-management are strongly emphasised in the recently publishedHigh Quality Care for All, the final report of the NHS Next Stage Review by Lord Darzi (2008). Thisreview is clear in its message that improved patient information is central to enabling patients tomake more choices in accessing healthcare and this is also seen as a means of addressing currentvariation in the quality of services. Achievement of these indicators would provide practiceassurance of the following Healthcare Commission core standards: C7e and C16.Local contextLocal patient consultation exercises have consistently shown that patients want improvedinformation about their GP practice and healthcare services available in the local area.According to Hammersmith and Fulham’s PCT’s Public Health Report 2006 (Carpenter andMayers, 2006), approximately 15% of residents state they have a limiting long-term illness. Theburden of long-term conditions in Hammersmith and Fulham is likely to increase as a result of theageing local population. It is therefore crucial to develop projects and strategies addressing selfmanagementof their conditions, which includes provision of high quality patient information,ensuring that patients are aware of the range of services and support available locally.All GP practices are required under the GMS contract to make information available to theirregistered population through a practice leaflet. In August 2008 the Primary Care Trust’sPerformance Monitoring Group reviewed the current leaflets provided by each of the 30 localsurgeries in Hammersmith and Fulham. The group found wide variation in quality both in terms ofthe content and format of leaflets. Leaflets vary greatly in quality of production and the amountof information that they contain. Some are simply a black and white photocopy, or printed-offsheet. Some are folded pull-outs; some are A5 brochures in colour, with additional informationabout self treatment for common conditions, and advice on the content of a family medical chest.71
Some refer to a practice website; many do not. The majority of local leaflets currently carry littleor no information on:Preventative services such as stop smoking, immunization, screeningChoice / Choose & BookThe PCT’s Patient Advice & Liaison Service and complaints teamCopying letters to patientsWalk-in and urgent care centresThe PCT’s Performance Monitoring Group found that the three most comprehensive localpractice leaflets were all produced by Neighbourhood Direct Ltd (ND). They produce them forpractices all over the country. They are a commercial organisation, but there is no cost to thepractices. The booklets are financed by local advertising. Often, advertisers are private providersof health services. Some are complementary health providers.Practices will need to update their practice leaflets and inform all patients of new opening timesrelating to extended hours, and this would therefore be an opportunistic time to promoteimproved quality of practice information leaflets.Review of evidence to support the proposed indicatorsThere is evidence that effective self-management can reduce hospitalisation and accident andemergency attendances (Gibson et al., 2004). The research evidence on the effectiveness of selfcare support provides an evidence base on the effectiveness of self care support, such asinformation, self care support devices, self care skills training and self care support networks inthe care of people with long term health conditions, short term ailments and among those takinginitiatives to stay healthy (DoH, 2007). The evidence base includes systematic reviews, primaryresearch studies, and surveys covering the different types of self care support interventions for arange of health problems.Tower Hamlets PCT has funded the introduction of template based leaflets for their GP surgeries.The Performance Monitoring Group has recommended that The PCT adopts a similar approach toTower Hamlets in order to significantly improve the quality of some local surgery leaflets andensure consistency across local surgeries, while removing the need for commercial advertising.Degree of perceived professional consensusThere is support for the provision of high quality patient information from professionalassociations including the RCGP and the BMA and from national guidance produced by NICE andthe Scottish Intercollegiate Guidelines Network (SIGN).The proposal relating to use of a PCT practice leaflet template has the support of the PEC Chairand the Director of Public Health. It is proposed that one of the PCT’s Public Health Consultantsand number of local GPs will be involved in developing the core content for the leaflet.72
Degree of perceived support from patients and carersA MORI baseline survey was commissioned by the Department of Health to explore publicattitudes towards self care and their self care behaviours (DoH, 2008). This survey describessupport from patients and carers for the principles of self care, including self management of longterm conditions and provision of information for patients.Strategies promoting self-care and self-management are strongly supported by a wide range ofpatient organisations including the British Lung Foundation, Asthma UK, Diabetes UK and ArthritisCare.During local public engagement events held in 2007 and 2008, a consistent theme has been thatproviding good information on local services is an issue local people feel is important – and needsimproving.Impact on health inequalitiesPatients with low health literacy have poorer health status, higher rates of hospital admission, areless likely to adhere to prescribed treatments and self care plans, experience more drug andtreatment errors, and make less use of preventive services. Achieving greater health literacy inthe population is integral to improving the health of disadvantaged populations and to tacklinghealth inequalities (Coulter et al., 2006).Health impactOverall the evidence suggests that self care support including provision of information forpatients can result in beneficial health outcomes for people and more appropriate use of healthand social care services (DoH, 2007). Coulter et al. (2006) further states that “health literacy isfundamental to patient engagement. If people cannot obtain, process, and understand basichealth information, they will not be able to look after themselves well or make good decisions onhealth.”73
Workload and training implicationsIf effective, the promotion of self care and provision of high quality information for patients mayreduce later workload.Recording the provision of self-management education would be a routine part of a reviewconsultation. For written information, different language versions or picture-based informationmay also be needed.Delivery of these indicators should ideally be supported by training for health professionals whichequips them to empower people with long term conditions and their carers in self management(e.g. motivational interviewing, behaviour change training and the use of self-management tools).The requirement for practices to have available sources of information (written, internet) couldbe verified through inspection. Additionally, it would be possible to electronically record whetherpatients have received written patient information material.It is proposed that the PCT commission a design and print company to develop and produce astandard practice leaflet template. This could be used by practices to help achieve the indicatorrelating to producing a practice leaflet, at no extra cost to the practice.A significant number of practices may need access to training for at least one member of thepractice team to be able to update the NHS choices website. For details of the proposed training package see section 14.3.8 (p97).74
ReferencesCarpenter A and Mayers A (2006) Hammersmith and Fulham PCT Public Health Report 2006.Coulter A, Ellins J (2006) Patient-focused interventions: a review of the evidence. <strong>London</strong>, The HealthFoundation.Darzi A (2008) High Quality Care for All, the final report of the NHS Next Stage Review Final Report byLord Darzi The Stationary Office. <strong>London</strong>Department of Health (2007) Research Evidence for the Effectiveness of Self Care Support <strong>London</strong>:Department of HealthDepartment of Health (2008) Self Care: A National View in 2007 compared with 2004—2005 <strong>London</strong>:Department of HealthDepartment of Health (2005) Supporting people with long-term conditions. <strong>London</strong>: Department ofHealth.Department of Health (2004) The NHS improvement plan: putting people at the heart of publicservices. <strong>London</strong>: Department of Health.Department of Health (2007) The NHS in England: The Operating Framework for 2008-9. <strong>London</strong>:Department of HealthDepartment of Health (2001) The Expert Patient: a new approach to chronic disease management forthe 21 st century. <strong>London</strong>: Department of HealthDepartment of Health (2004) Chronic disease management: A compendium of information. <strong>London</strong>:Department of HealthDonaldson GC, Hurst JR, Seemungal TA, Wedzicha JA. (2004) Early therapy improves outcomes ofexacerbations of chronic obstructive pulmonary disease. American Journal of Respiratory and CriticalCare Medicine ;169:1298-303.Gibson PG, et al. (2002) Self-management education and regular practitioner review for adults withasthma. The Cochrane Database of Systematic Reviews 2002, Issue 3. Art. No.: CD001117. DOI:10.1002/14651858.CD001117.Gibson, PG. et al. (2004). Written action plans for asthma: an evidence-based review of the keycomponents. Thorax; 59: 94-9Griffiths C, et al. (2004). Specialist nurse intervention to reduce unscheduled asthma care in a deprivedmultiethnic area: the east <strong>London</strong> randomised control trial for high risk asthma. British MedicalJournal;328: 144-7Loveman, E., Frampton, G.K., and Clegg, A.J. (2008) The clinical effectiveness of diabetes educationmodels for type 2 diabetes: a systematic review. Health Technology Assessment 12(9), 1-136.McCormick A, Fleming D, Charlton J (1995). Morbidity statistics from general practice. 4th Nationalstudy 1991-1992. <strong>London</strong>, HMSOMonninkhof E, van der Valk P, van der Palen J, van Herwaarden C, Partridge MR, Zielhuis G. Selfmanagement education for patients with chronic obstructive pulmonary disease: a systematic review.Thorax 2003;58:394-8.Moudgil H, et al. Asthma education and quality of life in the community: a randomised controlledstudy to evaluate the impact on white European and Indian subcontinent ethnic groups from socioeconomicallydeprived areas in Birmingham, UK Thorax 2000; 55: 177-183NICE (2008) Type 2 diabetes: the management of type 2 diabetes (NICE guideline). National Institutefor Health and Clinical Excellence.Secretary of State for Health (2006). Our health, our care, our say: a new direction for communityservices. The Stationery Office. <strong>London</strong>Secretary of State for Health. The NHS plan. The Stationery Office. <strong>London</strong> 2000.Skills for care, skills for health (2008). Common core principles to support self-care: a guide to supportimplementation. <strong>London</strong>: Department of HealthSprangers MA, deREgt EB, Andries F, van Agt HM, BijlRV, de Boer JB, Foets M, Hoeymans N, Jacobs AE,Kempen GI, Miedema HS, Tijhuis M A, and de Haes HC (2000). Which chronic conditions are associatedwith better or poorer quality of life? Journal of Clinical Epidemiology. 53(9): 895 – 90775
The British Thoracic Society / Scottish Intercollegiate Guideline Network. British Guideline on themanagement of asthma. Thorax 2003; 58 (S1): i1-i94. 2004 updateWanless D (2004) Securing good health for the whole population: final reportWanless D (2002) Securing our future health: taking a long-term view: final reportWatson PB, Town GI, Holbrook N, Dwan C, Toop LJ, Drennan CJ (1997). Evaluation of a selfmanagementplan for chronic obstructive pulmonary disease. European.Respiratory Journal 10:1267-71.76
<strong>QOF</strong>+ report onpatient experienceProposed indicatorsIndicator+ PATIENT EXPERIENCE 1. The practice takes part in the national patientsatisfaction survey+ PATIENT EXPERIENCE 2. The practice takes part in a PCT-led feedbacksession based on the results of the national patient satisfaction survey andagrees an action plan including explicit and appropriate targets that can beused in the following 2 years to assess the extent to which the action plan isimplemented+ PATIENT EXPERIENCE 3. The practice shares with patients the results andaction plan from the national patient satisfaction survey. This should bethrough information leaflets and poster(s) in the practice’s waiting andreception area, and through the Practice’s Patient Participation Groupwhere this exists+ PATIENT EXPERIENCE 4. The practice can show satisfactory objectiveevidence of implementing and achieving the action plan agreed with thePCT following the PCT-led feedback session based on the results of thenational patient satisfaction survey. Deviations from the action plan must bedescribed and explained+ PATIENT EXPERIENCE 5. The practice has a register of patients who needsigning and interpreting support for appointments, including a record offirst language spoken+ PATIENT EXPERIENCE 6. The practice offers double length appointmentsto patients identified as needing interpreting and signing support and to allpatients on the learning disabilities register+ PATIENT EXPERIENCE 7. 100% of carers who are newly registered with thePractice on or after December 01 2008 have a record of being advised bythe Practice that they can ask Social Services for an assessment of their ownneeds<strong>QOF</strong>+points351030575Continues overleaf77
Continued…Indicator+ PATIENT EXPERIENCE 8. The practice has a system in place for taking thespecial needs of carers into account, including when allocatingappointments and issuing prescriptions+ PATIENT EXPERIENCE 9. A named carer is recorded for at least 90% ofpatients on the learning disability register+ PATIENT EXPERIENCE 10. The practice scores better than the nationalaverage on the local response to the statement “I waited more than 2working days for a GP appointment” posed as part of the national patientsatisfaction survey+ PATIENT EXPERIENCE 11. The practice scores better than the nationalaverage on the local response to the question “Have you had a problemgetting through to your GP practice/health centre on the phone?” posed aspart of the national patient satisfaction survey<strong>QOF</strong>+points552020BackgroundA recent comprehensive review by Coulter and Ellins (2006) highlights that “measurement ofpatients’ experience is a useful component of a broader quality improvement strategy” and that“there is an association between poor quality experience and worse health outcomes.” Theproposed patient experience indicators therefore form an integral part of the Hammersmith andFulham primary care quality improvement strategy.The ‘inverse care law’ refers to the reduced availability and utilisation of services by those withthe greatest need (Hart, 1971). This has serious consequences for both individual and society,reducing the effectiveness and outcomes of healthcare while costs increase. Given this, there is astrong imperative to find ways of facilitating and broadening access (Coulter and Ellins, 2006).Chapman et al. 2004 describe four dimensions of healthcare access: availability, utilisation,relevance and effectiveness, and equity. These are:Availability describes the supply side of health services; whether resources are suppliedadequately and in proportion to need.Utilisation refers to the use of health services, indicating the degree of fit between userand the healthcare system. Measures the extent to which the health serviceaccommodates the patient and community served, and includes dimensions of usability,acceptability and affordability.Relevance and acceptability measure whether the right service is provided to adequatelyaddress the health needs of the target population and whether it has been developed totake into account the local socio-cultural setting.Equity is a social justice dimension indicating the extent to which resources are mobilisedto reflect need in a given population.78
Rosen et al. (2001) categorised initiatives to improve access to healthcare in terms of absoluteand relative strategies. The aim of absolute strategies is to increase the overall availability ofservices. Relative strategies aim to reduce inequalities and improve fairness. The relativestrategies adopted through the proposed indicators specifically target groups including ethnicminority groups and people with learning or physical disabilities) for whom services are known tobe inadequate, inappropriate or difficult to make use of.The recently published results for the 2007/8 Picker Institute Patient Survey identified twoparticular areas where performance in Hammersmith and Fulham is poor compared to theaverage performance of the 69 Picker Institute Trusts participating in the Patient Survey. Theseareas are ‘Making an Appointment’ and ‘Seeing a Doctor’. The proposed indicators have beendesigned to support practices in focussing on these areas.Priority and relevance to national policyThe concepts of patient experience and patient-centredness in healthcare have becomeincreasing prominent over the last decade and this has been increasingly reflected in nationalDepartment of Health national policy and national guidance. Correspondingly, the measurementof aspects of patient experience, including patient experience of access, has featured in the KeyPerformance Indicators of the Healthcare Commission and there are indicators relating to patientexperience in the national Quality and Outcomes Framework.Local contextA high proportion of children speak English as an additional language in Hammersmith andFulham – 45% at primary school (ranging from 6% to 67% between schools) and 39% atsecondary school (ranging from 7% to 56% between schools). 158 languages are spoken bychildren who attend local schools. After English, the main languages are Somali and Arabic(Zeuner, 2008).A relatively high percentage of residents in Hammersmith and Fulham (22%) are from non-whiteethnic groups. The largest non-white ethnic groups are Black Caribbean and Black African (both4.4%) (Zeuner, 2008).There are a total of 10,850 residents on disability registers in Hammersmith and Fulham. Ofthese, 350 are registered as deaf or hard of hearing and 470 are registered with a learningdisability. In terms of health deprivation and disability, around 17% of the population live withinthe most deprived fifth of areas nationally (Zeuner, 2008).Seven percent of people (11,600 people) in Hammersmith and Fulham provide unpaid care. Ofthese, almost 2,000 people provide care for at least 50 hours per week. The profile of carers inHammersmith and Fulham is similar to that in England. Adults in their fifties are most likely to beproviding care, with more than 20% doing so. A greater proportion of women than men arecarers providing care to a partner or relative (Zeuner, 2008).79
The recently published national Picker Institute survey of patient satisfaction with GP serviceshighlighted the many positive aspects of the patient experience. The majority of Hammersmithand Fulham patients reported that:69% could pre-plan or get an appointment within 2 working days,60% were seen within 15 minutes of their appointment time,76% thought the doctor listened carefully to what they had to say,66% thought they had enough time with the doctor,56% thought they were involved as much as they wanted to be in decision about theircare and treatment,66% had confidence and trust in their doctor and 89% felt they were treated with respectand dignity,71% thought the doctor knew enough about their condition/treatment, and58% thought that the main reason for their visit to a practice had been dealt with to theirsatisfaction.Most patients are highly appreciative of the care they receive. However, the survey resultshighlight that there is also room for improving the patient experience. The Picker Institute uses asimple summary score to show where patients think there is a problem or room for improvementregarding a specific aspect of care. Hammersmith and Fulham scored worse than the nationalaverage in 2 particular categories: ‘Making an Appointment’ and ‘Seeing a Doctor’. While thenational survey is a useful high level tool it does not allow analysis of individual practiceperformance and for this reason the plan is to carry out a local version of this survey. It isproposed that the PCT involves practices in innovative interactive feedback sessions resulting inindividual plans for addressing areas of concern.Review of evidence to support the proposed indicatorsPatient surveysA review by Coulter et al. (2006) concludes that direct and indirect feedback from patients is seenas a means of stimulating quality improvements, and that one of the main ways in whichfeedback can be obtained is through patient surveys.Patient surveys generally show relatively high levels of satisfaction with primary care. However, areview by Coulter (2006) of findings of patient surveys in six countries has shown that patientengagement tends to be lower in the United Kingdom (the comparison countries were the UnitedStates (US), Australia, Canada, New Zealand and Germany). This review found that doctors in theUK were reported as less likely than doctors in other countries to involve patients in decisionmaking,to give information on self-help or self-management, or to give information about theside-effects of medication.The two currently approved patient survey instruments (IPQ and GPAQ) have several limitationsand have not been designed to address important areas such as engagement and continuity.80
The National 2007 Quality and Outcomes Framework (<strong>QOF</strong>) Report on Patient Experiencehighlights that “having undertaken an annual survey for several years with the same instruments,many practices have stopped learning anything new about the experience of their patients. Theprocess has therefore become, for at least some practices, a relatively sterile and routine processwith little or no benefit for patients” (Baker, 2007).The report further states that“If the goal is to promote improvement in patient experience through rewardingpractices according to patient survey results, or by creating competition throughpublication of comparative performance data, the development of a standard nationalsurvey that enables comparison between practices would be needed. Evidence wouldalso be needed to show how patient characteristics influence ratings.”This evidence is currently lacking, and an appropriate national survey has not yet been developedsuitable for use as part of <strong>QOF</strong>.In view of this, the proposed indicators are designed instead to promote genuine patientengagement within practices enabling practices to better understand and respond to patientexperiences of care.The Picker General Practice questionnaire is based on the Primary Care Trust (PCT) questionnaire,developed by Picker Institute Europe for use in the NHS Patient Survey Programme. The localversion of the Picker Institute survey has been selected in order to take account of the concernsof local patients.It is proposed that practices should make the survey results available to practice patients, andalso to discus the findings with the PCT in order to produce an action plan. This approach issupported by the conclusions and recommendations of the Department of Health’s recentlypublished report, ‘No Patient Left Behind’ (Lakhani, 2008).Availability of long appointment slots for patients who require interpreting or signingsupport or for those with learning disabilitiesFor patients with particular needs or problems, e.g. those whose first language is not English orthose who need signing support or who have a learning disability, the availability of longerappointments can improve the quality of clinical care provided for patients in these groups. Theproposed patient experience indicators are designed to help address issues raised in the ‘Nopatient left behind’ report (Lakhani, 2008) which highlighted particularly how communicationdifficulties impact on the overall quality of care received by Black and Minority Ethnic (BME)patients, and also has implications for patient safety.Carers of people with learning disabilitiesPeople with learning disabilities typically do not seek out health care. They also experiencebarriers in accessing appropriate services and support for their health needs, health promotionneeds and lifestyle choices. Carers therefore play a potentially crucial role in the lives andexperiences of these patients. Carers are unpaid for their caring role, and they may havesignificant health and financial consequences as a result of their role. These consequences maybe further compounded if the carer is from a disadvantaged group.81
Degree of perceived professional consensusThe importance of taking account of patient experience as a marker of quality is highlighted by awide range of professional associations including the RCGP and the BMA. There is debatesurrounding the value of providing incentives for the results of patient surveys. The PCT’sapproach has been adopted following consultation with local stakeholders and national experts inpatient experience.Degree of perceived support from patients and carersThere is strong support from patients and carers for the inclusion of indicators relating to patientexperience.Impact on health inequalitiesThe introduction of the proposed <strong>QOF</strong> indicators for patient experience could potentially result ina reduction in the barriers accessing primary health care services for vulnerable anddisadvantaged groups, and improvements in the quality of clinical care provided to these groups,as well as raising the standards of care for all patients.Health impactIn view of the association between patient experience and health outcomes (Coulter et al., 2006),it is anticipated that the introduction of the proposed <strong>QOF</strong>+ patient indicators will contribute toimproved health outcomesWorkload and training implicationsFurther training in Learning disabilities awareness, carers awareness, cultural awareness,customer care and communication skills will further support delivery of these indicators. Therewill be some administrative workload implications associated with these indicators. For details of the proposed training package see section 14.3.9 (p98).82
ReferencesBaker, R (2007) Quality and Outcomes Framework Patient Experience National Primary Care Researchand Development CentreChapman, J.L. et al. (2004) 'Systematic review of recent innovations in serviceprovision to improve access to primary care'. British Journal of General Practice, 54:374-381.Coulter A, Ellins J (2006) Patient-focussed interventions-a review of the evidence Oxford: PickerInstitute EuropeCoulter A (2006). Engaging Patients in their Healthcare. How is the UK doing relative to othercountries? Oxford: Picker Institute EuropeHart, J.T. (1971) 'The inverse care law'. Lancet, i: 405-411.Lakhani M (2008) No patient left behind: how can we ensure world class primary care for black andethnic minority people? Department of HealthRosen, R. et al. (2001) 'Improving access, maintaining fairness: will the NHS Plan meet the challenge?'.Health Care UK, Winter: 19-33.Zeuner, D (2008). Annual Report of the Director of Public Health 2007-2008. Hammersmith andFulham PCT83
<strong>QOF</strong>+ report onpatient safetyProposed indicatorsIndicator+ PATIENT SAFETY 1. The practice submits significant event analysis (SEA)summaries to an annual PCT audit+ PATIENT SAFETY 2. The practice can show evidence of reporting incidentsor near misses involving harm/potential harm to patients via the nationalreporting and learning system (NRLS) using the standard e-reporting form+ PATIENT SAFETY 3. The practice has a system for ensuring that all practicestaff have had CRB checks within the last three years+ PATIENT SAFETY 4. The practice has a system in place to assist, whereappropriate, with the multi-agency referral process for investigationsrelating to the protection of children and vulnerable adults, includingacknowledging any referrals or requests for information within 2 workingdays+ PATIENT SAFETY 5. The practice has a system in place for identifyingvulnerable children, and this includes cases where a parent is known to be asubstance misuser, has a severe mental health problem, or where there isdomestic violence+ PATIENT SAFETY 6. The case conference notes of all children who are thesubject of a Child Protection Plan are scanned into the child’s medicalrecords+ PATIENT SAFETY 7. The practice has a system in place for ensuring thatwhere a child has been the subject of a child protection plan, this isrecorded as a Significant Active problem in the records of the child, theparents and other members of the household, and that this leads toeffective flagging of records<strong>QOF</strong>+points445785585
BackgroundThe United Nations Convention on the Rights of the Child (UNCRC) states that all children have aright to be protected from “physical or mental violence, injury or abuse, neglect, maltreatment orexploitation including sexual abuse, while in the care of parent(s), legal guardian(s) or any otherperson who has the care of the child” (Article 19).The proposed indicators relating to child protection have been derived from SafeguardingChildren and Young People in General Practice: A Toolkit, which aims to equip practices with theknowledge and tools to integrate safeguarding children and young people into practice systemsand processes.Child protection is the term used to refer to the activity taken to protect children who aresuffering or at risk of suffering significant harm.A vulnerable adult is a person aged 18 years or over “who is or may be in need of community careservices by reason of mental or other disability, age or illness; and who is or may be unable totake care of him or herself, or unable to protect him or herself against significant harm orexploitation” (DoH, 2000).The publication ‘No Secrets’ (DoH, 2000) states that “in recent years several serious incidentshave demonstrated the need for immediate action to ensure that vulnerable adults, who are atrisk of abuse, receive protection and support.” The publication highlights the need for thecreation of“…a framework for action within which all responsible agencies work together to ensurea coherent policy for the protection of vulnerable adults at risk of abuse and a consistentand effective response to any circumstances giving ground for concern or formalcomplaints or expressions of anxiety. The agencies’ primary aim should be to preventabuse where possible but, if the preventive strategy fails, agencies should ensure thatrobust procedures are in place for dealing with incidents of abuse.”Within existing <strong>QOF</strong> practices are expected to carry out a minimum number of significant eventaudits (SEA) each year. The purpose of this is to support reflective practice and to ensurechanges are made were necessary to reduce the likelihood of problems recurring.PCTs and hospital trusts now routinely report patient safety incidents via the National Reportingand Learning System (NRLS). This system saves anonymised data from incident reports with theaim of recognising recurrent patterns and feedback learning nationally. The system relies on acritical mass of incident reports being received.86
Priority and relevance to national policyExamples of national legislation and policy relating to safeguarding children, young people andvulnerable adults (including partnership working) include: Children Act 1989United Nations Convention on the Rights of the Child(ratified by UK Government in 1991) Human Rights Act 1998 Protection of Children Act 1999 Health and Social Care Act 2001 Adoption and Children Act 2002 Sexual Offences Act 2003 Children Act 2004Working Together to Safeguard Children 2006/Working Together under the Children Act2004 (2006)/Protecting Children- a shared responsibility (1998) Safeguarding Vulnerable Groups Act 2006Recent guidance produced by the National Patient Safety Agency (Bowie and Pringle, 2008)addresses the importance of Significant Event Analyses, including those relating to near missesinvolving potential harm to patients, and of sharing this information with Primary Care Trusts andthe NPSA in order to enable lessons to be shared with others.Achievement of these indicators would provide practice assurance of the following HealthcareCommission core standards: C1a, C2, C5d, C7a, C7c, C11a and C20a.Local contextThe number of children on the child protection register in Hammersmith and Fulham rose from70 in February 2006 to 139 by March 2007. The main reasons for registration continue to beneglect and emotional abuse. Information is collated at case conferences regarding family issues.For the period December 2006 – February 2007 there were 133 conferences. Domestic Violencewas a factor in 42% of all cases. Other factors that are significant are substance misuse andmental health issues (Hammersmith and Fulham Child Protection Annual Report 2006/7).The proposed indicators relating to child protection are in concordance with therecommendations of Hammersmith and Fulham Child Protection Annual Report 2006/7. They aredesigned to strengthen record-keeping and cross-organisational communication in relation tochild protection, which have been identified locally as an area for action, and to embed a systemof regular CRB checks for practice staff.A multi-agency policy and related procedures for the protection of vulnerable adults has beenproduced by the the local social services department and partner agencies to protect vulnerableadults in the borough (LBHF Social Services Department, 2006).87
In March 2008, a PCT audit of significant event audits was carried out and this highlighted asignificant range in the quality and quantity of reports across the patch. The practices are beingrequired to take part in an annual audit of SEAs to monitor quality and share learning acrosspractices.Review of evidence to support the proposed indicatorsThe role of primary care in protecting children from abuse and neglect is highlighted within theposition paper for the RCGP (2002). This was re-affirmed within the Keep Me Safe, Strategy forChild Protection (2005).A toolkit produced jointly by the RCGP and the NSPCC, ‘Safeguarding Children and Young Peoplein General Practice’ states that:“Children and young people are part of the general population and it is unusual for achild not to be registered with a general practitioner (GP); it is important that childrenare registered whenever possible. GPs remain the first point of contact for most healthproblems. This sometimes includes families who are not registered but seek medicalattention. A GP may be the first to recognise parental and/ or carer health problems, orsomeone whose behaviour may pose a risk to children and young people. The primaryhealth care team may be the only professionals to have contact with infants and preschoolchildren.”The toolkit further states that:“The long-term effects of abuse are widely documented and include a range ofpsychological, emotional and social effects. In order to achieve the optimum life chancesfor children and young people, early detection and intervention is paramount.Depending on the circumstances of a particular case, intervention may be an assessmentof further support needed for the child and family (for example, a child or family in needof services), or a child in need of protection. It is important to stress that we must notstereotype families or adults who do have health problems, such as mental health orsubstance misuse, although it is crucial that a holistic approach is taken with families sothat the needs of young children are assessed when treating parents with mental healthproblems or addictions.”The Department of Health publication ‘No Secrets’ gives guidance to local agencies who have aresponsibility to investigate and take action when a vulnerable adult is believed to be sufferingabuse. It offers a structure and content for the development of local inter-agency policies,procedures and joint protocols which draw on good practice nationally and locally, and highlightsthe role and importance of information-sharing in the context of this.The National Patient Safety Agency (NPSA) has recently produced guidance for Primary CareTeams on Significant Event Audit. This guidance states that:“Reporting when things go wrong is essential in general practice. The practice will berequired to report a proportion of significant events, particularly those where the safetyof a patient has been compromised. When this has happened it is tempting to explain itas the product of negligence, incompetence or carelessness on the part of staff, or as arare misfortune that is neither predictable nor preventable. However, experience from88
other complex high-technology settings, such as the aviation industry, has shown thatsafety incidents are not simply the result of human mistakes, such as inattention orforgetfulness, nor are they random or rare – in fact certain organisational and culturalfactors can make them more likely to happen. Also, where such a mechanism exists,confidential SEA reports should be passed to local clinical governance leads so there maybe an opportunity for lessons learned to be shared with others.” (Bowie and Pringle,2008)The NPSA encourages the:“confidential and anonymous reporting of incidents that caused no harm to patients, orwhere harm was averted, as well as events with a serious outcome which are more likelyto be flagged up in existing clinical governance and reporting systems. It is theseprevented patient safety incidents (known as near misses) that can provide the mostvaluable learning for the NHS because they can highlight problem areas where there isthe potential for things to go wrong in the future. They can also highlight ways in whichstaff have prevented the incident harming the patient (or have minimised the actualharm caused to the patient), and the NPSA is looking to learn from these actions toencourage the spread of best practice. All NHS organisations in the UK should have localarrangements in place to enable primary care staff to report patient safety incidents.”(Bowie and Pringle, 2008)To date, few reports on patient safety incidents are received by the National Patient SafetyAgency (NPSA) from general practice, and the NPSA is looking at ways to improve the level ofreporting. It is proposed that practices will be incentivised, through <strong>QOF</strong>+, to make use of thenational reporting e-form. In addition incentives will be provided for submission of SEAsummaries to an annual PCT audit in order to enable lessons to be shared with others andencourage the spread of best practice.Degree of perceived professional consensusThere is professional consensus from the RCGP and the BMA on the principles relating to theproposed indicators. In addition, the proposed indicators which relate to child protection havebeen derived from a toolkit produced by the NSPCC and the RCGP on Safeguarding Children andYoung People in General Practice.Degree of perceived support from patients and carersThere is strong support from patients and carers for the inclusion of indicators on patient safety.In addition, the proposed indicators which relate to child protection have been derived from atoolkit produced by the NSPCC and the RCGP on ‘Safeguarding Children and Young People inGeneral Practice’.89
Impact on health inequalitiesPoverty is the most frequently and persistently noted risk factor for child abuse, and is has alsobeen identified as a risk factor for abuse of vulnerable adults. Including indicators relating toprotection of children and vulnerable adults will contribute to safeguarding of children andvulnerable adults from disadvantaged backgrounds.Health impactPatient safety is integral to achieving positive health outcomes.Workload and training implicationsChild protection training will be an integral aspect of delivery of these indicators. Training relatingto vulnerable adults will also support indicator delivery.Some practices will need PCT health informatics support to implement a child protection flaggingsystem.There will be administrative workload implications associated with these indicators.Significant event analysis training may be required by some practices to move toward a moreuniform standard of practice across the PCT. For details of the proposed training package see section 14.3.10 (p99).ReferencesBowie P, Pringle M (2008) Significant Event Analysis Guidance for Primary Care Teams. NationalPatient Safety AgencyDepartment of Health and Home Office (2000) No secrets: guidance on developing and implementingmulti-agency policies and procedures to protect vulnerable adults from abuse. <strong>London</strong>Luce, R (2007) Safeguarding children and young people in general practice: A toolkit NSPCC and RCGPChild Protection Annual Report 2006/7 (2007) Hammersmith and Fulham PCTSocial Services Department, <strong>London</strong> Borough of Hammersmith and Fulham (2006) Inter-agency policyand procedures for the protection of vulnerable adults. <strong>London</strong>90
Training and supportrequirements for <strong>QOF</strong>+IntroductionFinancial incentives delivered in isolation are unlikely to lead to optimal quality improvement(Oxman et al., 1995). For this reason, it is proposed that a range of interventions will bedeveloped to support practices participating in <strong>QOF</strong>+ to improve the quality of care delivered totheir patients. These interventions include additional educational and training activities, audit,peer support and enhanced IT support. These interventions will incorporate both face-to-faceand e·learning components through a blended learning approach.A detailed practice training and support needs analysis is currently in progress and will be used toinform further development of the <strong>QOF</strong>+ training and support package.Training and support requirements for selected existing <strong>QOF</strong> indicatorsAnalysis of data on <strong>QOF</strong> achievement by individual practices suggests possible generaltraining/support needs (for most practices) in the areas of Mental Health and Cervical Screening.The data also highlight a small number of poorer performing practices which may need moreglobal (rather than specific) support. This support may need to be more administrative andmanagerial than clinical.Analysis of data from a preliminary training and support needs assessment of local primary carepractitioners (GPs, practice nurses and practice managers) shows that the majority of practiceswould value increased administrative support, including additional training for administrativestaff. A number of practices felt that additional clinical training and support for practice nurseswould be beneficial.Practices described a range of methods for delivery of training that they would find useful,including online modules, educational meetings and individual practice trainer visits. It isenvisaged that the <strong>QOF</strong>+ training and support package will incorporate all these mechanisms toencompass a wide range of learning styles and preferences.A number of practices highlighted the importance of tailoring training to individual practiceneeds. To this end, it is proposed that those practices signing up to <strong>QOF</strong>+ will receive anadditional training bursary which will allow them to determine how best their training needs maybe met.One practice felt that it would be useful if the PCT hosted regular <strong>QOF</strong>+ meetings for practices tofacilitate sharing of ideas between practices. If other practices also feel this would be helpful,then this idea will be developed further.91
Training and support requirements for new <strong>QOF</strong>+ indicatorsThe PCT will need to provide training and resources for primary care staff in the use of IT forcreating and maintaining the Practice CVD at Risk Register.Proposed training resource(s)PCT Health Informatics TeamTraining and resources will also be required for cardiovascular risk assessment andcommunication of risk.Proposed training resource(s)Provision of relevant guidelines1 2008 NICE Guideline on Lipid Modificationhttp://www.nice.org.uk/nicemedia/pdf/CG67NICEguideline.pdf2 MeReC Bulletin:Assessing and Communicating the Risk of Cardiovascular Diseasehttp://www.npc.co.uk/MeReC_Bulletins/MeReC_Bulletin_Vol19_No1_main.pdfInformation on self-directed online training resources e.g. the section on cardiovascularrisk assessment in theNational Prescribing Centre Website. This section is veryinteractive, and includes case studies, quizzes and key slides.http://www.npci.org.uk/therapeutics/cardio/cdrisk/room_cdrisk.phpFunding for GPs and Practice nurses to complete a diploma level module oncardiovascular disease risk assessment offered by Education for Health. Module deliveryis through comprehensive written material supported by 2 study days. It is possible forthis module to be delivered locally to 10 or more people.http://www.educationforhealth.org.uk/pages/heartsave/cardiovascular_disease.aspTraining will be required for primary care staff in the delivery of brief interventions for alcoholmisuse.Proposed training resource(s)The Department of Health is planning to roll out in November 2008 an e•learningmodule on screening and brief interventions for alcohol misuse. This e-module is aimedat primary care practitioners. It is proposed that this forms part of the training requiredin this area for primary care practitioners in Hammersmith and Fulham. Additionally, theHammersmith and Fulham Drug and Alcohol Team would be able to provide individualpractice-based training for primary care teams on screening and brief interventions forprimary care, and is proposed to take place during the first few months following launchof the <strong>QOF</strong>+ scheme in November 2008. This will enable the provision of local expertiseon linkage to local services as part of the training.92
As per NICE guidance, all frontline healthcare staff should be trained to offer brief advice onsmoking cessation and to make referrals, where necessary and possible, to NHS Stop SmokingServices and other publicly funded smoking cessation services (NICE, 2006).Proposed training resource(s)The existing LES for Smoking Cessation already includes provision of relevant trainingand this could be extended to those practices participating in <strong>QOF</strong>+.It is recommended that staff involved in the care of mothers and babies are trained in the skillsnecessary to work towards implementing the Baby Friendly Initiative. The PCT may wish toconsider working towards becoming accredited through the Baby Friendly Initiative, and thiswould further support the introduction of indicators relating to breastfeeding into <strong>QOF</strong>+.Proposed training resource(s)The Baby Friendly Initiative has produced a training pack aimed at GPs.http://www.babyfriendly.org.uk/pdfs/infosheets/doctor_packs_infosheet.pdfEthnicity and first languageTraining will be required for primary care staff with respect to the importance of and rationale forethnicity monitoring. Training is critical to the success of collecting ethnic group data, and shouldbe tailored to local circumstances and experiences of ethnic monitoring. Cultural awarenesstraining for primary care staff will also support delivery of the proposed indicators. Hammersmithand Fulham also has a high number of refugees and asylum seekers and these groups haveadditional needs and face additional challenges. <strong>QOF</strong>+ should also incorporate training on howbest to work with these populations to meet their health needs, and what resources are availablein primary care.Proposed training resource(s)Cultural awareness training sessionsCurrently, training in equality and diversity is mandatory for all NHS Hammersmith andFulham staff members. The PCT also provides on-going training for staff on:• Equality and diversity awareness• The PCT’s equality legislative obligations• Screening and EIA processes• Performance managementTraining is provided by both internal and external providers. This training could beexpanded to enable primary care workers to participate.93
Information on self-directed online training resources1 As part of its e-GP project, The RCGP will shortly be making available for GPs ane·learning module on equality and diversity. GPs who are members of the RCGPcould be directed to this, if they are not already aware of its existence.http://www.rcgp-curriculum.org.uk/information__resources/elearning_project.aspx2 The ‘multiethnic teaching and learning in nursing project’ on the MarySeacole Centre for Nursing Practice website is an online educationalresource on raising awareness in relation to ethnicity, culture and health care.It addresses cultural diversity, models of transcultural care, essential aspects ofcare and the lifespan approach, including scenarios.http://www.health.tvu.ac.uk/maryseacole/melting/validated.asp3 The Health for Asylum Seekers and Refugee portal (HARPWEB) providesinformation and practical tools written by people with expert knowledge ofworking with asylum seekers and refugees, both in the UK and other countriesto enable health care practitioners to develop a culturally sensitive and informedapproach to their practice. Materials are provided on general health, mentalhealth and multilingual information.http://www.harpweb.org/index.php4 The refugee health team for Lambeth PCT have produced a resource pack tohelp primary healthcare professionals in their work with refugees and asylumseekers. This could be adapted for use in Hammersmith and Fulham.5 The NHS Core Learning Unit has produced an e-learning module on Equalityand Diversity. This course is freely available to those working in the NHS.Automatically generated certificates of completion are awarded for eachcompleted module. The courses can be accessed through the website of theNHS Core Learning Unit.http://www.corelearningunit.comIndividual practice training sessionsThis could include training relating to the above areas, tailored to the needs of individualpractice teams. The training should address how best to work with on how best to workwith diverse populations, including refugees and asylum seekers, to meet their healthneeds.94
RecordsIt is proposed that the PCT provides additional administrative support and training for practiceswith respect to administration. This process will be greatly facilitated by IT support.A data warehouse held centrally securely within the NHS net by the PCT will host all generalpractice data for reporting purposes. The following data will be extracted from general practicessystems for the data warehouse, subject to the practices’ agreement, for all patients from April01 2003 onwards:A data warehouse held centrally securely within the NHS net by the PCT will host all generalpractice data for reporting purposes. The following data will be extracted from general practicessystems for the data warehouse, subject to the practices’ agreement, for all patients from April01 2003 onwards:1 Patient detailsPractice patient IDAgeSexEthnicityLanguageCountry of birthLSOA code for the patient’s main address postcodeMosaic code for the patient’s main address postcode2 Registration details (including status and associated dates)3 Patient recordAll coded data (without any free text information)All appointment data (without any free text information)These data will enable us to analyse and monitor <strong>QOF</strong>+ achievements for all practices centrallyand feed back to practices their achievement. The process will be with time automated butinitially will involve semi-automated processes.The data will enable the <strong>QOF</strong>+ support team to centrally systematically search for each practicetheir patient records and identify patients at highest risk and in need for CVD primary prevention.Data will also enable central monitoring and pro-active approach in a number of other diseaseareas. This will represent significant support to practices.Proposed training resource(s)General practice research database recording guidelinesThis is a support document for reference and training. The guidelines are intended toprovide a more detailed explanation of the requirements. It clarifies the patientinformation that needs to be recorded and how to appropriately enter it.http://www.gprd.com/_docs/recordingguidelines.pdf95
New patient screeningProposed training resource(s)TB Target Training DayScheduled for February 2009 (further details will be available shortly.)In-House Practice TrainingThis will be provided by the PCT TB Service based at Charing Cross Hospital. Forinformation on arranging training, practices can contact:Gloria-Anne Cox, TB Nurse SpecialistTel 0208 383 8805 Fax 0208 308 8816 tbnurses@imperial.nhs.ukfurtherProvision of relevant guidelinesThe proposed indicators are in line with the 2006 NICE guidelines relating to TB.http://www.nice.org.uk/download.aspx?o=CG033quickrefguideInformation on self-directed online training resourcesThe following website provides generic resources relating to TB for non-clinicians(including receptionists).http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1195733780018?p=1191942150139Diagnosis and Management of TB in Primary Care is an interactive online learningmodule about TB epidemiology, diagnosis prevention and control, and is based on the2006 NICE Guidance on TB. It is available through the Health Protection Agency (HPA)website.http://www.hpa.org.uk/webw/HPAweb&HPAwebStandard/HPAweb_C/1200055722753?p=1191942150139#resourcesFor nurses, this module is also available throughhttp://www.uknursing.netFor doctors, this module is also available throughhttp://www.doctors.net.uk/TB96
Patient informationDelivery of these indicators should ideally be supported by training for health professionals whichequips them to empower people with long term conditions and their carers in self management(e.g. motivational interviewing, behaviour change training).A significant number of practices may need access to training for at least one member of thepractice team to be able to update the NHS choices websiteProposed training resource(s)Training CoursesIt is proposed that primary care practitioners have access to training in enhancedcommunication skills. This may include training in motivational interviewing skills andbehaviour change and in approaches such as neuro-linguistic programming (NLP) and thecognitive behavioural model (an approach based on cognitive behaviour therapy andadapted for use in primary care.)Guidelines for updating information on NHS ChoicesThese guidelines provide step by step information and instructions for practices formaintaining and updating their practice profile on the NHS choices website.http://www.iscms.nhs.uk/pbe/GPGuidance.pdf97
Patient experienceLearning disabilities awareness training, carers awareness training, cultural awareness trainingand training in communication skills and customer care skills will further support delivery of theseindicators.Proposed training resource(s)Training in communication skillsIt is proposed that primary care practitioners have access to training in enhancedcommunication skills. This may include training in motivational interviewing skills and inapproaches such as neuro-linguistic programming (NLP) and the cognitive behaviouralmodel (an approach based on cognitive behaviour therapy and adapted for use inprimary care.)Information on self-directed online training resources1 Training in Cultural Awareness - see section on Ethnicity and First Language Section 14.3.5, p93.2 The self assessment toolkit ‘Good Practice Guide: to Highlight the Needs ofCarers’ enables practices to assess themselves against criteria for the servicesthey provide for patients and their carers.http://www.carers.org/data/files/a-good-practice-guide-to-highlight-the-needsof-carers-2865.pdf3 The NHS Core Learning Unit provides a curriculum of online work-based trainingcourses. The courses address a range of topics including The courses aretransferable, accredited, nationally endorsed, as well as being mapped to theKnowledge and Skills Framework (KSF), NHS Litigation Authority (NHSLA),Healthcare Commission (HCC) and sector skills competencies. E-learning andwork-based training modules for Equality and Diversity, Disability Awareness andCustomer Care are freely available to those working in the NHS. Automaticallygenerated certificates of completion are awarded for each completed module.The courses can be accessed through the website of the NHS Core Learning Unit.Relevant modules include Equality and Diversity, Disability Awareness andCustomer Care.http://www.corelearningunit.com98
Patient safetyTraining relating to patient safety generally (including reporting mechanisms and SignificantEvent Analysis) and for protection of children and vulnerable adults will be an integral aspect ofdelivery of these indicators.Proposed training resource(s)Provision of relevant guidelines1 The guidance “Significant Event Audit: Guidance for Primary Care Teams”provides a tool for practices to help conduct an effective Significant Event Audit(SEA).http://www.npsa.nhs.uk/nrls/improvingpatientsafety/primarycare/significantevent-audit/2 The toolkit “Safeguarding Children and Young People in General Practice: AToolkit” has been produced jointly by the Royal <strong>College</strong> of General Practitionersand by the NSPCC. It provides guidance notes, templates of child protectionpolicies, procedures and a good practice code. The document also containsfurther guidance related to caring for children and young people in generalpractice.http://www.rcgp.org.uk/PDF/CIR_Toolkit%20document%20final%20edit.pdfSelf-directed online training resourcesThe NHS Core Learning Unit provides a free E-learning training module on Patient Safety.This is transferable, accredited, nationally endorsed, as well as being mapped to theKnowledge and Skills Framework (KSF), NHS Litigation Authority (NHSLA), HealthcareCommission (HCC) and sector skills competencies.These can be accessed through the website of the NHS Core Learning Unit.http://www.corelearningunit.comAn automatically generated certificate of completion is awarded on completion of themodule. The Core Learning Unit will shortly be making available e-learning modulesrelating to the protection of children and vulnerable adults.14.6 ReferencesOxman AD TMDDHRB (1995) No magic bullets: a systematic review of 102 trials of interventions toimprove professional practice. Canadian Medical Association Journal 153(10):1423-31.99
Appendix 1Background to the <strong>QOF</strong>+ development processComposition of the <strong>QOF</strong>+ development groupThe <strong>QOF</strong>+ Development Group was based at NHS Hammersmith and Fulham and at the eHealthunit of the Department of Primary Care and Social Medicine at <strong>Imperial</strong> <strong>College</strong> <strong>London</strong>.Members were drawn from the PCT, primary care, public health and the field of healtheconomics, and included the Local Director of Public Health, PCT Head of Primary Care, PCTInterim Director of Primary Care, Medical Director and Professional Executive Committee (PEC)Chair, and members of the academic Department of Primary Care and Social Medicine at <strong>Imperial</strong><strong>College</strong> <strong>London</strong> (including local General Practitioners and Consultants in Public Health).Process employed by the <strong>QOF</strong>+ development groupCommunication within the group took place through weekly face-to-face meetings, through emailand through telephone contact throughout the development process from June 2008 toNovember 2008. Throughout this process, frequent contact was made with local stakeholdersdrawn for the PCT and from primary care.Approach to development of the schemeDiscussions with national and international experts in health care quality improvement took placethroughout the development of the scheme, including two teleconferences with Professor HelenLester and Professor Richard Baker. A number of issues were considered further during theseteleconferences, which provided valuable insights which helped inform further development of<strong>QOF</strong>+ indicators and the training and support package, as well as the development of theconsultation process with local stakeholders including those from primary care. These issues aresummarised below:The approach for further incentivising existing <strong>QOF</strong> indicators was discussed includingwhether to raise the upper threshold or reward any improvement. HL felt that rewardingimprovement may not be such an important objective in the context of recent researchwhich suggests that following the introduction of <strong>QOF</strong>, health inequalities have narrowedamong the practices serving more deprived patients. RB suggested the possibility ofhaving both schemes within <strong>QOF</strong>+, which could be tailored to individual practices, as‘one size does not fit all.’ The <strong>QOF</strong>+ Development Team highlighted that if only theachievement of raised upper thresholds was rewarded, less well performing practiceswould be provided with additional support by the PCT in terms of training etc whichwould be free to the practice. RB then brought up the question of “How do you getchange to happen?”, and raised concerns that if targets were set too high, poorlyperforming practices would have low motivation to change. However as out ofapproximately 30 local practices, only a small proportion were performing less well (andwould be provided with further support by the PCT through other means) RBacknowledged that the approach of rewarding improvement through <strong>QOF</strong>+ may not beas important.100
The proposed methodology for selecting priority areas for development of indicators andthe methodology for indicator development was discussed. Both HL and RB supportedthe <strong>QOF</strong>+ Development team’s proposed approach of using a structure consultationprocess to select priority areas and applying evidence based criteria to select indicators.Advice was also sought from HL on the proposed membership of the local stakeholderpanel, and she agreed with the group’s proposals for this.The need for all LES schemes currently offered by the PCT to be incorporated into <strong>QOF</strong>+was discussed. HL and RB felt that the concepts underlying <strong>QOF</strong> were different in manyways from those underlying LES, and that the two schemes had different butcomplementary functions. It therefore may not be appropriate to combine all the LESinto <strong>QOF</strong>+.The need for strong IT support was emphasized to ensure indicators were workablewithin practice systems.The collection of good quality quantitative data would enable evaluation of the schemeto see whether a ‘step-change’ effect had occurred. HL also felt a qualitative componentwould be appropriate and helpful. RB mentioned that an evaluation would probablyrequire more than just <strong>QOF</strong> data. GPED data could be used and he highlighted thepossibility of finding a local comparator group.The need for engagement with all local practices was emphasized, as well as the need toprovide education and training support in addition to financial incentives.The relevance of the findings of the NHS Next Stage Review in terms of helping shape thedirection of the scheme.In terms of additional quality initiatives, the <strong>QOF</strong>+ Development team highlighted thatfinancial incentives in themselves don’t improve care, and that there were plans to put inplace a robust IT system and local support. RB mentioned the importance of tailoringadditional initiatives to take into account the stages that practices are at. e.g. leadingedge practices were likely to be able to work on their own initiative with minimumsupport. Practices in the mid-range may benefit from education, training and theopportunity to learn from colleagues. The tail end of practices may need other forms ofsupport, e.g. development of teamwork, leadership and management skills. He alsomade the point that in some cases, levels of practice achievement would be related tothe nature of the practice’s patient population. The <strong>QOF</strong>+ Development Teamhighlighted that within <strong>QOF</strong>+, there would be flexibility to add associated features e.g.GP peer support, management support etc.A1.4 ReferencesDarzi A (2008) High Quality Care for All, the final report of the NHS Next Stage Review Final Report byLord Darzi The Stationary Office. <strong>London</strong>101
Appendix 2Methodology for the extension ofexisting clinical <strong>QOF</strong> targetsSelection of candidate existing indicators for revised upper thresholdsBecause the initial remit of the <strong>QOF</strong>+ Development Group concerned improving aspects of clinicalcare, it was decided that only indicators in the <strong>QOF</strong> clinical domain be considered for furtherincentivisation through <strong>QOF</strong>+. The additional services indicator for cervical screening wassubsequently appended to that list as it had been identified through the local Public Healthreport and by the PCT as a key priority area for Hammersmith and Fulham ( see Graph A3.3.6.1,p123).Analysis of data compiled by the group on local practice achievement for existing <strong>QOF</strong> indicatorsin 2006/7 found that most practices in Hammersmith and Fulham were achieving well on processindicators. It was therefore decided to reward achievement of revised upper thresholds for aselected number of outcome and process indicators where there was scope for furtherimprovement.The list of candidate indicators was refined following consultation with local practices andresulted in the removal of EP 8 and COPD 10 in view of the limited evidence base and thepotential for these indicators to exacerbate health inequalities. Following a series of face-to-faceand email discussions, the list was reduced to 12 indicators, spanning key areas of morbidity forHammersmith and Fulham:ASTHMA 6, BP 5, CHD 6, CHD 8, CHD 10, CS 1, DM 12, DM 17, DM 20, MH 6, STROKE 6and STROKE 8 (see also Table A2.1, below).Data compiled by the group on individual practice attainment in <strong>QOF</strong> 06/07 and 07/08 were usedto inform this process. While there was continued general improvement between <strong>QOF</strong> 06/07 and<strong>QOF</strong> 07/08, the selected indicators still represent the 12 worst-performing areas forHammersmith and Fulham.102
Lower Upper PointsPractices ≥UpperASTHMA 6 40% 70% 20 28BP 5 40% 70% 57 25CHD 6 40% 70% 19 29CHD 8 40% 70% 17 24CHD 10 40% 60% 7 24CS 1 40% 80% 11 4DM 12 40% 60% 18 26DM 17 40% 70% 6 23DM 20 40% 50% 17 27MH 6 25% 50% 6 28STROKE 6 40% 70% 5 27STROKE 8 40% 60% 5 22Table A2.1Summary of current <strong>QOF</strong> targets and point allocations for the 12 indicators selected for target revisionin <strong>QOF</strong>+. The number of Hammersmith and Fulham practices already exceeding the <strong>QOF</strong> upper boundis shown (calculated from QMAS data as at June 2008).Methodology for revised target setting for existing clinical indicatorsAn early principle established by the <strong>QOF</strong>+ Development Group was that revised targets be set ina way that drives standards towards the best seen at a national level. The original plan was for asingle ‘all-or-nothing’ target set at the 90 th national centile of attainment or 90%, whichever waslower, for a given indicator.A number of problems became apparent with this approach, notably the uneven distribution ofperformance for the 12 selected indicators when local and national statistics were compared(using <strong>QOF</strong> 07/08 data, see Appendix 3, p116). For some indicators (particularly CHD 8 andSTROKE 6) this meant that significant numbers of practices already displayed attainment thatbrought them close to the 90% threshold, while for others (e.g. CS 1) the desired improvementwas unrealistic (in a single year).To explore this issue further, the group introduced the concept of median distance ̃ , calculatedas the median of the differences between any proposed target and the current level ofattainment for each Hammersmith and Fulham practice, :{ } , ̃ (1)This was converted into a figure representing the number of patients that the medianHammersmith and Fulham practice (of 4975 patients, prevalence figures in Table A2.2) wouldhave to treat to reach the target:⌈ ̃ ⌉ (2)103
PrevalenceRegistersizeAsthma 5.75% 287Hypertension 12.79% 637Cancer 1.08% 54CHD 3.50% 175COPD 1.48% 74CS Eligible 25.00% 1244Diabetes 3.87% 193Epilepsy 0.60% 30LVD 0.75% 38Mental Health 0.73% 37Stroke and TIA 1.63% 82Thyroid 2.71% 135Table A2.2Adjusted prevalence figures and expected register size (absolute number of patients) for the medianHammersmith and Fulham practice of 4975 patients. Data sourced from <strong>QOF</strong> 07/08.The sigmoid nature of many of the attainment distributions seen ( see Appendix 3, p116)results in a tension between the desire to set a target that motivates even the best performingpractices (argues for a high target) but without discouraging those poorer participating practicesfrom participation at all in the scheme (argues towards a lower target). The possibility of basingthresholds on the performance of below-median practices (for example, restricting analysis topractices lying in the lower IQR for attainment) was considered but rejected because it uniformlyresults in large numbers of better-performing practices already attaining the revised target. Theissue of providing additional rewards to practices who have not needed to make anyperformance gain is sensitive from both a financial governance and political point of view. Thiswas ultimately addressed by capping the number of NHS Hammersmith and Fulham practiceswho already exceed the <strong>QOF</strong>+ revised thresholds at four (i.e. whenever more than 4 practicesmet a candidate threshold, it was discounted.) To address the needs of poorer performingpractices for whom the thresholds may represent large jumps in attainment, it was decided thatspecific resources be made available to support them, instead of trying to revise the targetdownward.The target-setting scheme for the revised <strong>QOF</strong>+ threshold was ultimately based on an iterativeapproach that started from the 75 th national centile for <strong>QOF</strong> 07/08 (selected after analysis of themedian distances for each indicator) and revised up in 5 centile increments whenever the cappingrule described above was violated. The thresholds set by this scheme and the centiles on whichthey are based, together with the median distance and expected patient numbers aresummarised in Table A2.4. Consultation with local practices raised concerns about theconsequence of ‘all-or-nothing’ rewards on marginal errors (i.e. accidentally missing a singlepatient). To address this, an indicator-specific tolerance was introduced to provide a ‘cushion’against these errors.The tolerance is the difference between the original <strong>QOF</strong>+ threshold and a new lower thresholdcalculated using the original capping method but removing the 75 th national centile floor and the104
5-centile step. This lower value is termed the Tolerance threshold. Details of these and theoriginal <strong>QOF</strong>+ thresholds are summarised below:ToleranceThreshold Based on PointsMediandistanceExpected# PatientsPractices ≥ThresholdASTHMA 6 92% 90th 5 11.5% 33 2BP 5 88% 91st 15 10.1% 65 2CHD 6 97% 92nd 3 7.6% 14 1CHD 8 85% 61st 4 5.3% 10 2CHD 10 86% 82nd 7 18.1% 32 3CS 1 81% 31st 18 9.6% 119 3DM 12 85% 73rd 3 4.2% 9 4DM 17 87% 71st 5 7.8% 16 3DM 20 76% 83rd 10 10.4% 20 3MH 6 96% 77th 2 8.8% 4 3STROKE 6 95% 87th 3 6.1% 6 3STROKE 8 84% 77th 3 9.0% 8 3Table A2.3Lower (Tolerance) <strong>QOF</strong>+ thresholds for the 12 clinical indicators taken from <strong>QOF</strong>. The medianimprovement that a practice would have to make to reach the target is shown as well as the number ofpatients that this improved would involve for the median Hammersmith and Fulham practices. Thenumber of practices already exceeding Tolerance thresholds is shown.<strong>QOF</strong>+Threshold Based on PointsMediandistanceExpected# PatientsPractices ≥ThresholdASTHMA 6 95% 95th 5 14.5% 42 0BP 5 90% 95th 14 12.1% 78 0CHD 6 98% 95th 3 8.6% 16 0CHD 8 87% 75th 3 7.3% 13 1CHD 10 87% 85th 7 19.1% 34 3CS 1 88% 75th 17 16.6% 206 0DM 12 86% 75th 2 5.2% 11 3DM 17 88% 75th 4 8.8% 17 3DM 20 77% 85th 10 11.4% 22 2MH 6 97% 80th 1 9.8% 4 2STROKE 6 96% 90th 3 7.1% 6 2STROKE 8 85% 80th 2 10.0% 9 3Table A2.4Default <strong>QOF</strong>+ thresholds for the 12 clinical indicators taken from <strong>QOF</strong>. The median improvement that apractice would have to make to reach the target is shown as well as the number of patients that thisimproved would involve for the median Hammersmith and Fulham practices. The number of practicesalready exceeding these thresholds is shown.105
While both threshold types are remunerated as all-or-nothing targets, there is ongoing debatewithin the <strong>QOF</strong>+ Development Group as to how these might perform against scaled (as in existing<strong>QOF</strong>) or other reward schemes in terms of motivating improvement. A key effect of an all-ornorthingtarget is likely to be greater influence over the pattern of attainment seen inparticipating practices. Scaled rewards free practices to decide what represents an adequate levelof reward versus attainment for them. Notwithstanding the cushion effect of the Tolerancethreshold, this choice is effectively removed under the current scheme. Part of the reason for thisis a genuine desire to drive a ‘step-change’ in quality by the commissioners of the <strong>QOF</strong>+ project.However, there are still concerns that, despite efforts to set thresholds with reference to currentlevels of attainment, the all-or-nothing scheme may discourage engagement by poorerperforming practices. Evaluation over the next twelve months will aim to explore this issue with aview to considering possible alternative approaches for <strong>QOF</strong>+ 09/10. Schemes that wereconsidered during <strong>QOF</strong>+ development include per-practice target setting, multiple tierremuneration and non-linear scaled rewards (where the fraction of points awarded accelerates aspractices approach the upper threshold). The administrative burden associated with per-practicetarget setting is a significant concern, while it proved difficult to reconcile multiple tier paymentwith the capping requirements.A separate argument which requires further consideration is that, since exception reportingprovides recourse for all legitimate reasons for non-treatment of patients, there is no reason whyupper targets not be set at 100% (Fleetcroft et al. 2008).Methodology for point allocation for existing clinical indicatorsPayment under <strong>QOF</strong> is based on a points system. For the average practice in England (beforecorrection for list size and disease-specific prevalence), each point is currently worth £124.60.Each indicator has a fixed number of points allocated, a whole-numbered fraction of which areawarded in linear proportion to practice attainment. Achievement below the lower <strong>QOF</strong>threshold for each indicator results in no points being awarded, while practices who exceed theupper threshold do not receive additional points beyond the maximum available for the indicator.While the stated purpose of the point system is to reward “GPs and their staff for the volume andquantity of work done” (BMA NHS Confederation, 2003), information about how this process wasconducted – particularly for the first year of <strong>QOF</strong> (2004/05) – is limited. Roland (2004) describeshow point allocation was determined “partly by the academic advisory group *of the original <strong>QOF</strong>negotiation process] and partly by a formal scoring process undertaken by groups of familypractitioners in England and Scotland.” Fleetcroft and Cookson (2006) present a slightly differentaccount of “two small groups of GPs estimating the work required to achieve the different qualitycriteria,” but this must be viewed within the context of their argument that there is a disparitybetween point allocation and health outcomes. By contrast, guidance from the NHS Primary CareContracting Website states that:“there is no set workload represented by a <strong>QOF</strong> point… any local frameworks used byPMS contractors should be comparable to the National <strong>QOF</strong> in terms of the work neededto earn the same amount of money..”It is interesting to note that subsequent revisions of <strong>QOF</strong> have typically raised thresholds withminimal or no alterations to point allocation.106
There is, therefore, an outstanding question as to whether point allocation under <strong>QOF</strong> was – andcontinues to be – systematic and appropriate (either on workload- and outcome-weightedgrounds). Data-driven exploration by the group underlines this point. For each indicator i, it ispossible to derive the points awarded per percentage improvement, ppp i, by diving the totalnumber of <strong>QOF</strong> points by the percentage difference between the qof upper and lower bounds:(3)A related concept is the pounds awarded per patient-treated for the average practice (in thiscase, the median practice for NHS Hammersmith and Fulham) £pp i, calculated by dividing thetotal amount of money available for an indicator (the maximum number of points multiplied by£124.60) by the expected number of patients that would need to be treated to move fromattainment at the <strong>QOF</strong> lower threshold to the upper threshold (equation 4). The expectednumber of patients is based on prevalence for each indicator area for the median practice.⌈⌉(4)While this measure of per-patient remuneration is not perfect (for example, becauseimplementation costs do not simply scale linearly with register size) our view is that it provides auseful handle on remuneration that is directly comparable between indicators. Table A2.5 showsthe results of the analysis. The large discrepancy in per-patient remuneration was a surprise,particularly between indicators that are ostensibly addressing the same problem (but in differentpatient groups), for example £40.35 per patient for cholesterol control in CHD patients versus£12.91 in diabetics.Pointsper %£ perpatientScalingfactorRevised pointsper %Revised £ perpatient<strong>QOF</strong>+pointsASTHMA 6 0.67 £28.94 1.00 0.67 £28.94 10BP 5 1.90 £37.16 1.25 2.38 £46.46 29CHD 6 0.63 £45.09 1.00 0.63 £45.09 6CHD 8 0.57 £40.35 1.50 0.85 £60.52 7CHD 10 0.35 £24.92 2.00 0.70 £49.84 14CS 1 0.28 £2.75 7.50 2.06 £20.66 35DM 12 0.90 £58.10 1.00 0.90 £58.10 5DM 17 0.20 £12.91 5.00 1.00 £64.56 9DM 20 1.70 £109.75 1.00 1.70 £109.75 20MH 6 0.24 £80.82 1.00 0.24 £80.82 3STROKE 6 0.17 £25.33 5.00 0.83 £126.63 6STROKE 8 0.25 £37.99 2.00 0.50 £75.98 5Table A2.5Comparison of points-per-percent and pounds-per-patient (for the median NHS Hammersmith andFulham practice) between current <strong>QOF</strong> and <strong>QOF</strong>+. Data sourced from <strong>QOF</strong> 07/08.107
The low level of remuneration for cervical screening (£2.75 per patient) was also a significantconcern, given the consistently poor performance of Hammersmith and Fulham practicescompared to national levels of attainment ( see Graph A3.3.6.1, p123).Point allocation for the revised <strong>QOF</strong>+ target aimed to tackle this discrepancy by introducing ascaling factor to normalise like-for-like indicators (CHD 8 and DM 17 now reward at ~£60 perpatient). An element of empirical judgement must also be acknowledged, reflecting experiencefrom practising GPs with the group and their perceptions around the difficulty of attaining eachindicator. Revision was performed through the use of an indicator-specific scaling factor ,applied to the original points-per-percent allocation (equation 5). The concept of a uniformscaling factor , was discussed, reflecting the idea that higher attainment becomesdisproportionately more difficult in a uniform way, but ultimately discounted (so = 1).(5)Table A2.5 shows the adjusted £-per-patient after application of the correction in equation 5.It was originally planned that the number of <strong>QOF</strong>+ points Qp i, would reflect the distance betweenthe <strong>QOF</strong>+ threshold and the upper <strong>QOF</strong> thresholds :(6)However, given the large numbers of practices exceeding the existing <strong>QOF</strong> upper threshold foreach indicator (see Table A2.1) it was felt that this approach would not adequately reflect thetrue workload to practices. A revised formula was used instead, which is based on the mediandistance to the <strong>QOF</strong>+ threshold, introduced above:̃ (7)When the lower Tolerance threshold was introduced after consultation with practices, the pointsallocated under this method were divided evenly across the two thresholds (except for non-evenpoint allocations, where the Tolerance threshold receives the remainder).108
Minimum attainment thresholdsIt was initially proposed that there be a set of minimum attainment thresholds, applicable to allexisting <strong>QOF</strong> and <strong>QOF</strong>+ indicators, that a practice must reach in order to receive anyremuneration under the <strong>QOF</strong>+ scheme. Beyond concerns that incentive schemes per se mayencourage neglect of non-incentivised areas of care (Roland, 2004; Chaix-Couturier et al., 2000),it is recognised that there may be competing interests within such schemes that lead to someindicator areas being systematically under-prioritised. Evidence from a US cancer screeningprogramme suggests that competition between incentive areas can compromise theeffectiveness of each to cause change (Hillman et al., 1998). Fleetcroft and Cookson (2006) notethe important distinction between cost-effectiveness in terms of workload and cost-effectivenessin terms of health outcomes, arguing that the former is more likely to shape clinical practice.Minimum attainment thresholds aim to stimulate a systematic approach to patient care;discouraging practices from ‘cherry-picking’ indicators that might be easy for them to attain whilepotentially neglecting other areas of patient care (including those areas of <strong>QOF</strong> not covered bythe <strong>QOF</strong>+ scheme.) Despite this goal, it proved difficult to peg thresholds that were meaningful(i.e. their attainment would represent true clinical merit) but did not penalise (and deterparticipation by) poorly performing practices.Because of this, and because significant negative feedback was elicited when the issue waspresented to practices, it has been decided to defer the introduction of minimum attainmentthresholds in <strong>QOF</strong>+ 08/09. The <strong>QOF</strong>+ Development Group remains committed to ensuring thatthe introduction of <strong>QOF</strong>+ in Hammersmith and Fulham does not come at the cost of progressmade in other clinical areas. Monitoring over the first 12 months will facilitate discussion aboutwhether this policy requires review in <strong>QOF</strong>+ 09/10.109
Exception reportingMany <strong>QOF</strong> (and a significant number of the new <strong>QOF</strong>+) indicators reward based on a percentagecalculation where the numerator represents all the patients who meet the given criteria and thedenominator all the patients to whom the indicator should apply.(8)The denominator for a given indicator at a given practice , is constituted by applying a seriesof rules to the relevant disease register , which itself is a subset of the practice population .These rules are of two forms: Exclusions , which capture the specific criteria of each indicator. Not all indicators willapply to every patient on the disease register and there may be diagnostic anddemographic restrictions (for example, an indicator applicable to those within a certainage range.) These are applied in a systematic way to select a subpopulation of thedisease register. Exceptions , which are the dynamic mechanism by which practices can omit certainpatients from inclusion in the denominator. Exceptions provide practices with amechanism to ensure that inappropriate treatment is not pursued and that they are notpenalised for issues out of their control (for example uncooperative patients). Table A2.6details the current list of valid exceptions. Most exceptions are time-limited (typicallywith a period equivalent to that of the testing/review-cycle for a given indicator) whichmeans that there is an ongoing workload associated with managing exception reporting.ABCDEFGHIPatient recorded as refusing to attend review who have been invited on at least threedifferent occasions during the preceding 12 monthsPatients for whom it is not appropriate to review the chronic disease parameters becauseof particular circumstances, for example terminal illness or extreme frailtyPatients newly diagnosed within the practice or who have recently registered with thepractice, who should have measurements made within 3 months and delivery of clinicalstandards within 9 monthsPatients who are on maximum tolerated doses of medication whose levels remain suboptimalPatients for whom prescribing a medication is not clinically appropriate, for example thosewho have an allergy, another contraindication or who have experienced an adversereactionWhere a patient has not tolerated medicationWhere a patient does not agree to investigation or treatment (informed dissent) and thishas been recorded in the medical recordsWhere the patient has a supervening condition which makes treatment of the targetcondition inappropriate, for example cholesterol reduction in a patient with liver diseaseWhere an investigative service or secondary care service is unavailableTable A2.6Current list of valid reasons for exception reporting. Sourced from the GMS Contractdocumentation (DoH, 2003)110
Percentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingException reporting patterns in Hammersmith and FulhamThe metric used to report exception reporting here is that published by the NHS InformationCentre: the effective exception rate, . The for a given practice or group of practices iscalculated by summing all the exception counts across all numeric indicators , and dividing thisinto the sum of the [denominator + exception counts]:∑ ∑(9)∑ (∑ ( ))While dealing with absolute numbers of exceptions rather than averaging reported ratesminimises the skew caused by practices with small numbers of patients, it also disproportionatelyweights large-denominator indicators (e.g. CS 1), and this should be kept in mind while reviewingthe figures. Those quoted here are derived from <strong>QOF</strong> 07/08 data. They differ slightly from thosepublished by the Information Centre because we disagree with their practice of assuming thatunreported data should be equivalent to an exception rate of zero for a given practice-indicator.Our view is more conservative (practice-indicators without a stated exception rate are simplyomitted) and yields a pessimistic upper bound on exception reporting.100%90%80%National <strong>QOF</strong> 07/08H&F June 083028262470%60%50%40%30%20%10%2220181614121086420%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMediansFigure A2.7Cumulative distribution plot comparing rates of exception reporting in NHS Hammersmith and Fulham(June 2008 data, solid red line) with national rates (<strong>QOF</strong> 07/08 data, dotted purple line) for the 12 <strong>QOF</strong>indicators subject to <strong>QOF</strong>+ incentivisation. Data sourced from QMAS and the NHS Information Centre.The EER in national <strong>QOF</strong> 07/08 was 6.08% for all indicators and 7.50% when the 12 clinicalindicators included in <strong>QOF</strong>+ are considered in isolation. Hammersmith and Fulham’s rates are6.01% and 6.12%, respectively, ranking it 75 th and 9 th lowest for exception reporting by PCTnationally. Compared to <strong>London</strong> PCTs (EER 6.43% and 7.81%) Hammersmith and Fulham currentlyranks 8 th and 2 nd lowest. The cumulative distribution of exception reporting for the 12 clinical111
indicators compared to national rates is shown in Figure A2.7 (for explanation of how to interpretthe graph, see Section A3.2, p117). No practices in NHS Hammersmith and Fulham have EER’sexceeding 15% and only two exceed 10%.While Hammersmith and Fulham currently displays relatively low rates of exception reporting, itshould be noted that the absolute numbers involved are small and that these figures masksituations where – for individual indicators – local rates are higher than the national average (e.g.DM 20).Exception reporting and <strong>QOF</strong>+The exception reporting criteria used in <strong>QOF</strong>+ will remain the same as those in national <strong>QOF</strong>.An early proposal was that, for existing <strong>QOF</strong> indicators with revised upper thresholds, practiceswould need to keep below the 50 th centile of national rates of exception reporting in order toqualify for payment. Motivating this was a concern that, as targets were raised, the temptation toinappropriately exclude patients increases. It has been suggested, however, that the current[denominator - numerator] group contains disproportionate numbers of patients who mightultimately be legitimately excluded. Under this view, the fact that national levels of exceptionreporting have remained relatively static (Doran et al., 2006; Doran et al., 2008; The InformationCentre, 2008) reflects only the fact that current <strong>QOF</strong> targets are not yet high enough to force theissue.Negative feedback from practices consulted early in the <strong>QOF</strong>+ development process promptedfurther consultation on this issue from Professor Martin Roland and Dr Tim Doran who arerecognised experts in this field. They raised a specific concern about the validity of comparingexception reporting at even a local level because of the significant effect that inter-practicepopulation characteristics appear to have on rates of exception reporting. The nature of thesefactors is not well understood; early suggestions that exception reporting might be related tolevels of deprivation (Sigfrid et al., 2006) have recently been disputed by others (Doran et al.,2008). It is known that the uncertainty associated with a given rate of exception reportingincreases dramatically when disease register size drops below a certain level, which raises issuesfor validating exception reporting rates in small practices (The Information Centre, 2008). Withthese issues in mind, it was decided to abandon attempts to cap or control rates of exceptionreporting in <strong>QOF</strong>+ 08/09.Figure A2.8 is a scatter plot which relates mean exception reporting rate with attainment for the12 <strong>QOF</strong> clinical indicators for 28 practices in Hammersmith and Fulham. Diamonds outlined in redrepresent practices with below mean disease register sizes (normalised for practice list size) whilegreen filled diamonds represent those with above average register sizes. There is a clearassociation between increased attainment and higher rates of exception reporting (trend line isshown, calculated with circled outliers omitted the correlation coefficient is 0.72) and alsobetween higher rates of exception reporting and small register (not denominator) sizes. Althoughevidence collected to date suggests that gaming is a not a significant problem in the NHS as whole(Doran et al., 2008), the group is concerned about the possibility that high attainment locallymight be resulting from practices shaping their denominator profile in ways not consistent withthe spirit of <strong>QOF</strong>. There will be careful examination of how exception reporting rates change ofthe next twelve months.112
Exception Reporting Rate (Percentage of Eligible Patients)25%20%r=0.72 (outliers removed)15%10%5%0%70% 75% 80% 85% 90%AttainmentOutliersFigure A2.8Scatter plot relating aggregate attainment and exception reporting rates for 28 (out of 30)Hammersmith and Fulham practices across the 12 <strong>QOF</strong> indicators used in <strong>QOF</strong>+. Data were sourcedfrom QMAS in June 2008 and were incomplete for 1 practice (omitted) and 1 outlier is not shown(attainment 51.9%, exception reporting grate 5.1%). Practices with above average disease registersizes (adjusted for list size) are shaded in green while those with below average register sizes areoutlined in red. There is a strong correlation between increased attainment and exception reportingrates in Hammersmith and Fulham (r=0.72, circled outliers not included). The exception rates shownare not EER but the means of the individual rates for each practice, attainment was determined in thesame way.A somewhat counterintuitive mathematical feature of exception reporting is that it sometimesrewards considerably less than if excepted patients were treated to meet the indicator criteriainstead. For simplicity, consider a situation where there is a patient population of 4, two of whommeet target criteria (i.e. current attainment of 50%). If both patients are either excepted ortreated then attainment increases to 100% in both instances. If, however, one patient remainsunmanaged (not treated and not excepted) and we consider only the treatment or exception of asingle patient, the situation is different. Excepting that patient reduces the denominator by 1 andresults in an attainment of 66.7%. By contrast, treating that patient increases the numerator by 1and results in an attainment of 75% (8.3% more). In general, it can be said that excepting isalways less profitable than treating while there are unmanaged patients in the denominatorgroup (8.3% is the maximal difference). This issue is relevant to both indicator design (as towhether particular actions should be considered as numerator qualifiers or exceptions) and tothe way exception reporting is promoted or otherwise to GPs.113
114
List turnoverConsultation with practices has identified a concern that higher thresholds will bedisproportionately more difficult for high-turnover practices (e.g. those based in areas withsignificant migrant or student populations) to attain. In addition to an increased equilibriumworkload (the number of cases that must be processed simply to maintain current attainment),there may be specific issues around identifying and contacting members of such transientpopulations.While regression modelling of <strong>QOF</strong> 04/05 did not identify list turnover as a factor contributory tolower <strong>QOF</strong> attainment (Ashworth and Armstrong, 2006), the effect of raised thresholds has notbeen explored. Data around turnover and attainment will be collated during the first months of<strong>QOF</strong>+ 08/09 with the aim of determining the scope of the issue and evaluating whether thisshould be taken into account in calculating remuneration. In the meantime, we would valuefeedback from practices about their practical experience of any issues relating to turnover andmeeting the revised thresholds.ReferencesAsthworth M, Armstrong D (2006) The relationship between general practice characteristics andquality of care: a national survey of quality indicators used in the UK quality and outcomesframework, 2004-5. BMC Family Practice 7:68Chaix-Couturier C, Durand-Zaleski I, Jolly D, Durieux P (2000) Effects of financial incentives on medicalpractice: results from a systematic review of the literature and methodological issues. InternationalJournal for Quality in Health Care 12:133-42Department of Health (2003) New GMS contract 2003: investing in general practice. NHSConfederation and the BMA. <strong>London</strong>.Doran T, Fullwood C, Gravelle H, Kontopantelis E, Hiroeh U, Roland M (2006) Pay-for-performanceprograms in family practices in the United Kingdom. New England Journal of Medicine 355:375-84Doran T, Fullwood C, Reeves D, Gravelle H, Roland M (2008) Exclusion of patients from pay-forperformancetargets by English physicians. New England Journal of Medicine 359:274-84Fleetcroft, R and Cookson, R (2006) Do the incentive payments in the new NHS contract for primarycare reflect likely population health gains? Journal of Health Care Research and Policy 11:27–31Fleetcroft R, Steel N, Cookson R, Howe A (2008) “Mind the gap!" Evaluation of the performance gapattributable to exception reporting and target thresholds in the new GMS contract: National databaseanalysis. BMC Health Services Research 8: 131Hillman AL, Ripley K, Goldfarb N, et al. (1998) Physician financial incentives and feedback: failure toincrease cancer screening in Medicaid managed care. American Journal of Public Health 88:1699-1701Primary Care Contracting (2008) What is the workload associated with 1 <strong>QOF</strong> point? [Online, AccessedSeptember 01 2008] Available at: http://www.pcc.nhs.uk/qanda.php?article_request=133Roland M (2004). Linking physician pay to quality of care—a major experiment in the United Kingdom.New England Journal of Medicine 351:1448-54Sigfrid LA, Turner C, Crook D, Ray S (2006) Using the UK primary care quality and outcomes frameworkto audit health care equity: preliminary data on diabetes management. Journal of Public Health28:221-25The Information Centre (2008) National quality and outcomes framework exception reportingstatistics for England 2007/8 bulletin. [Online, Accessed November 01 2008] Available at:http://www.ic.nhs.uk/cmsincludes/_process_document.asp?sPublicationID=1225147131677&sDocID=4317115
Appendix 3Current levels of attainment and exception reporting forexisting clinical indicatorsPurpose of these dataThe following pages display graphs summarising the distribution of attainment and exceptionreporting within Hammersmith and Fulham and comparison with national patterns for the 12existing <strong>QOF</strong> indicators that have revised upper thresholds in <strong>QOF</strong>+.Visualisation and exploration of these played a key role in the target setting and point allocationprocess for these indicators.They are included so that practices can see how their performance compares at both a local andnational level.Data sourcesAttainment and exception reporting data for individual Hammersmith and Fulham practices werecalculated from the most recent QMAS submissions (June 02 2008). Historical attainment figureswere sourced from <strong>QOF</strong> 2004/5 data compiled and made publicly available by Dr Gavin Jamie athttp://www.gpcontract.co.uk. The indicators DM 20 and MH 6 were not introduced until <strong>QOF</strong>2006/7 and historical data from that session are used instead for these.National attainment and exception rates (for all indicators except CS 1) were calculated frompractice-level data (for England) from the 2007/08 <strong>QOF</strong> submission made publicly available by theNHS Information Centre.http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-andperformance/the-quality-and-outcomes-framework/qof-2007/08/data-tablesException reporting data for CS 1 were kindly provided by the Information Centre.116
Using the graphsThe following graphs are cumulative distribution plots of attainment and exception reporting for31 Hammersmith and Fulham practices (thick red continuous line) and all practices in England(dotted thick purple line) in June and April 2008, respectively. Median values for each distributionare plotted on the X-axis (as coloured diamonds). Each attainment graph includes a summary ofthe percentage improvement required for a median practice to reach the revised <strong>QOF</strong>+ upperthreshold (dotted arrow with quoted number). Current <strong>QOF</strong> and <strong>QOF</strong>+ thresholds are marked oneach attainment graph.For a given X-Y combination, where X represents either a specified level of attainment orexception reporting, reading against the Y-axis yields the percentage of practices whose rate isless than or equal to the X-axis value. For convenience, the right hand Y-axis also includes theabsolute number of Hammersmith and Fulham practices that a given percentage represents (outof a maximum of 31 practices). Some practices gave incomplete exception reports and areomitted from the analysis for certain indicators. In these cases, the denominator number ofpractices is shown by the maximum of the right-hand Y-axis scale (typically 29).The plots allow questions of the form “How many practices achieved at most/at least n percent?”to be readily answered by simply reading the value off the corresponding Y-axis (and subtractingfrom 100% where necessary). Centiles can also be determined by picking a Y-axis percentage andfinding the corresponding X-axis value.For attainment, the ideal distribution is one that tracks along the X-axis at or close to zero on theY-axis before a very steep, late jump to 100%. A significant deviation from national performanceis evident for CS 1 (and, to a lesser degree, CHD 10 and DM 17). Worryingly, performance for CS 1does not appear to have improved appreciably in the four years since <strong>QOF</strong> was launched.The situation is less clear for exception reporting. In general, a curve lying to the left of thenational distribution and without a long asymptote to 100% on the Y-axis is probably preferable(i.e. below average rates of exception reporting and without high-rate outliers).117
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentAsthma 6Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108611.4%42030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians118
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentBP 5Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108610.1%42030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians119
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentCHD 6Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108647.5%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians120
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentCHD 8Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound <strong>QOF</strong>+ Upper Bound30282624222018161412108645.2%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians121
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentCHD 10Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound3028262422201816141210818.1%642030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians122
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentCS 1Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong>+ Upper Bound30282624222018161412108649.5%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%3090%National <strong>QOF</strong> 07/0828H&F June 082680%242270%2060%181650%1440%121030%820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians123
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentDM 12Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108644.2%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians124
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentDM 17Attainment<strong>QOF</strong> Lower Bound<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound100%3090%National <strong>QOF</strong> 07/0828H&F June 082680%H&F <strong>QOF</strong> 04/052470%222060%1850%161440%1230%10820%610%47.7%20%030% 40% 50% 60% 70% 80% 90% 100%AttainmentMediansException Reporting100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians125
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentDM 20Attainment<strong>QOF</strong> Lower Bound <strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound100%3090%National <strong>QOF</strong> 07/0828H&F June 082680%H&F <strong>QOF</strong> 06/072470%222060%1850%161440%1230%10820%610%10.3%420%030% 40% 50% 60% 70% 80% 90% 100%AttainmentMediansException Reporting100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians126
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentMH 6Attainment100%90%80%70%60%50%40%30%20%10%0%<strong>QOF</strong> Lower BoundNational <strong>QOF</strong> 07/08H&F June 08H&F <strong>QOF</strong> 06/07Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108648.8%2020% 30% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians127
Percentage of practices at or below given level of attainmentPercentage of practices at or below given rate of exceptingNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentStroke 6Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108646.1%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians128
Percentage of practices at or below given rate of exceptingPercentage of practices at or below given level of attainmentNumber of H&F practices at or below given rate of exceptingNumber of H&F practices at or below given level of attainmentStroke 8Attainment<strong>QOF</strong> Lower Bound100%90%National <strong>QOF</strong> 07/08H&F June 0880%H&F <strong>QOF</strong> 04/0570%60%50%40%30%20%10%0%Exception Reporting<strong>QOF</strong> Upper Bound<strong>QOF</strong>+ Upper Bound30282624222018161412108649.0%2030% 40% 50% 60% 70% 80% 90% 100%AttainmentMedians100%90%80%70%National <strong>QOF</strong> 07/08H&F June 08282624222060%50%40%30%1816141210820%6410%20%00.1% 0.5% 1.0% 5.0% 10.0% 50.0% 100.0%Exception reporting rateMedians129
Appendix 4Methodology for the design and development of thenew indicators for <strong>QOF</strong>+Methodology for the creation of new indicator areas long listTo inform development of new <strong>QOF</strong>+ indicators, a member of the group conducted an initialreview of the existing literature on quality improvement in health care settings, and ondevelopment of quality indicators. The methodology chosen for development of the new clinicalindicators drew on the methodology for reviewing the Quality and Outcomes Framework –the<strong>QOF</strong> Review (Lester, 2006) and for developing indicators for the quality of health promotion,prevention and primary care at the health systems level in OECD countries (Marshall et al., 2004).The <strong>QOF</strong> Review is an independent academic process which advises the NHS Employees and GPnegotiators on a range of evidence based clinical indicators. This Review is a collaborationbetween the Universities of Birmingham and Manchester, the Society of Academic Primary Careand the Royal <strong>College</strong> of General Practitioners.Potential local, national, and international sources for new indicator areas were identified andconsidered. Local data sources included the NHS Hammersmith and Fulham public health report(Zeuner, 2008), PCT Operating Plan 2008/9 (Hammersmith and Fulham PCT, 2008) and localenhanced service schemes (Hammersmith and Fulham PCT, 2008). National data sources includedthe Healthcare Commission Key Performance Indicators (Healthcare Commission, 2008), NHSVital Signs indicators (DoH, 2008) and recent national guidance, including that produced by theNational Institute for Health and Clinical Excellence (NICE), as well as considering topicsaddressed by other Local Enhanced Services schemes nationally. The OECD indicators developedfor use in a primary care setting were also considered (Marshall et al., 2004). Selected localstakeholders including the Local Director of Public Health were consulted to seek their views onpotential approaches for creation of the long list. The members of the <strong>QOF</strong>+ Development Group,which included GPs and Consultants in Public Health, contributed additional ideas for potentialnew indicator areas. Documentation from NHS Hammersmith and Fulham’s Patient and PublicInvolvement Forum was also reviewed to gain a perspective on the views of local patients inorder to help inform the process (Hammersmith and Fulham PCT, 2007). A full formalconsultation with local stakeholders including primary care and patients was not performed atthis stage however, due to the time restraints and subsequent tight deadlines that the group wasworking within.Following discussion within the <strong>QOF</strong>+ development group, it was decided that areas wouldinitially be included on the long list if they were identified as either a local or national priorityarea. The group agreed that an area would be defined as a local priority if it was highlighted inthe NHS Hammersmith and Fulham Annual Public Health Report (Zeuner, 2008). A nationalpriority area would be defined by its inclusion as a Key Performance Indicator by the HealthcareCommission (Healthcare Commission, 2008). It was agreed that a key theme of <strong>QOF</strong>+ should bethe focus on reducing health inequalities locally. The PCT public health report focuses on areasrelevant to health inequalities locally, and these were therefore used to help identify potentialnew indicator areas for <strong>QOF</strong>+ (Zeuner, 2008). Following discussion within the <strong>QOF</strong>+ developmentgroup, with the PCT and with national experts in quality improvement, it was felt that due to the130
tight timescale of this project, it was beyond the scope of <strong>QOF</strong>+ to incorporate all the LESschemes currently offered by the PCT. However, it was felt that it would be feasible to considerinclusion of selected existing LES schemes which were more likely to fit into the <strong>QOF</strong>+ framework.The LES which were considered for inclusion within <strong>QOF</strong>+ for year 1 included CVD PrimaryPrevention, Smoking Cessation, Immunisations and Choose and Book (which was underdevelopment by the PCT).Following further discussion, it was decided to:consider adapting the existing CVD Primary Prevention and immunisations LES for <strong>QOF</strong>+,stop development of new indicators for Choose and Book through <strong>QOF</strong>+ as there wasalready a proposed LES for this and there were practical issues around indicatordevelopment (e.g. most GPs do not read-code referrals so it would be difficult to use anindicator to evaluate what percentage of referrals were made through Choose andBook), and toconsider development of indicators for smoking cessation in parallel to the existing LESon smoking cessation.Following review of the long list, it was agreed that areas that were already incorporated into thenational <strong>QOF</strong> should not be included as new indicators for the clinical domains of <strong>QOF</strong>+, but couldinstead be considered in terms of raising thresholds of the existing indicators. These areas includeheart failure, CVD, hypertension, stroke, diabetes, COPD, CKD, mental health, dementia, palliativecare (BMA, 2006).Remaining indicator areas were classified using the OECD framework of Health Promotion,Preventative Care, and Diagnosis and Treatment (Marshall et al., 2004), as well as the followingdomains of quality: Patient-centredness/Empowerment, Organisational and Safety. A decisionwas initially taken not to include organisational indicators or indicators related to primary careaccess within <strong>QOF</strong>+, in view of the presence of this area within the national <strong>QOF</strong>, and in view ofthe limited timescale for roll-out of the scheme. In addition, the <strong>QOF</strong>+ Development Group wasaware of the possibility that incentive arrangements for organisational quality through thenational <strong>QOF</strong> may change as a result of the roll-out of practice accreditation schemes including ascheme developed by the Royal <strong>College</strong> of General Practitioners (National Primary Care Researchand Development Centre, 2008).However, additional funding for <strong>QOF</strong>+ became available at a later stage of the project, and it wasthen decided to incorporate aspects of the <strong>Imperial</strong> <strong>College</strong> Data Quality project into <strong>QOF</strong>+.Additional domains relating to patient experience, patient safety, patient information and patientregistration (new patient screening for Tuberculosis) were developed further by NHSHammersmith and Fulham using a separate methodology.131
As a result of the prioritisation process for new clinical indicators, a long list of twenty potentialpriority areas was identified. For the purposes of further evaluation of these areas through astructured consultation with local stakeholders, four areas (including chronic disease case finding,reduction of healthcare-associated infections (eg MRSA), data quality on ethnic group and qualityof medical records) were removed from the long list as they were identified as fundamentalcomponents of <strong>QOF</strong>+, and would therefore be automatically incorporated within <strong>QOF</strong>+. Thisresulted in a final long list of 16 areas.AlcoholAdult smokingBreastfeeding initiation and maintenanceChildhood immunisationChildhood obesityCVD primary preventionDrug misuseIncreasing attendance for breast screeningIncreasing attendance for cervical screeningInfluenza immunisationMeasurement of patient experienceOsteoarthritisSelf-management of long-term conditionsSexual health, including STI screening and preventionSmoking in pregnancyTuberculosis screeningConsultation with local stakeholders to select priority areas for thedevelopment of <strong>QOF</strong>+ indicatorsThe final long list of potential indicator areas was developed into a Delphi questionnaire. Thisquestionnaire was piloted among the group, and wording and structure modified as a result. Thequestionnaire was then circulated to a local stakeholder panel for consultation to seek their viewsthrough participation in a consensus building exercise.The local stakeholder panel was drawn from NHS Hammersmith and Fulham and from localprimary care services and included the Director of Public Health, Head of Primary CareDevelopment, Professional Executive Committee (PEC) Chair, a local GP and a local PracticeNurse. The merits of including a patient representative on the panel were debated, but in view ofthe fact that the group had been unable to make contact with the PCT’s Patient and PublicInvolvement Forum, it was decided that a patient representative would not be included in view ofthe tight timescale for indicator development. It was also proposed that the panel included apractice manager. However, attempts to identify a practice manager for this purpose wereunsuccessful, and therefore there was no practice manager representation for the first phase ofthe structured consultation process. The local stakeholder panel’s views were used to help select132
which additional priority areas would be included in <strong>QOF</strong>+ through a structured consultation toprioritise areas on the basis of their importance.The consultation method used incorporates aspects of both the Delphi Technique and the RANDAppropriateness Method. These are robust research methodologies with substantial literature tosupport them. The approach involves identifying experts and obtaining their views anonymously.This provides qualitative and quantitative information on expert views.The Delphi technique is a postal method which involves two or more rounds of questionnaires.Researchers clarify a problem, develop questionnaire statements to rate, select panellists to ratethem, conduct anonymous postal questionnaires, and feed back results (statistical, qualitative, orboth) between rounds (Campbell et al., 2003).The RAND appropriateness method requires a systematic literature review for the condition to beassessed, generation of indicators based on this literature review, and the selection of expertpanels. A postal survey then takes place, in which panellists are asked to read the evidence andrate the preliminary indicators, and a face to face panel meeting (not conducted in thedevelopment of the <strong>QOF</strong>+ indicators), in which panellists discuss and re-rate each indicator. Itincorporates a rating of the feasibility of collecting data (Campbell et al., 2003). It has beendescribed as the only systematic method of combining expert opinion and evidence (Naylor,1998).The rating scale used was based on the RAND appropriateness method. Indicators with an overallmedian rating of 7, 8, or 9 without disagreement for each criterion of importance, scientificsoundness, feasibility and clarity were retained; indicators rated with an overall median of 1-3 were removed; indicators rated with an overall median of 4-6 were rated as equivocal, andthese were further discussed by the group and retained if thought to be particularly important toinclude within <strong>QOF</strong>+. Disagreement was defined as 30% or more scores in both the bottom (1-3)and top (6-9) tertile.After obtaining questionnaire responses from the local stakeholder panel in the first round, asecond round of structured consultation was used to achieve consensus among respondents.Respondents were provided with a summary of the panel’s responses from the first round andasked to consider their own responses in light of this, rating each indicator again using the samemethod as in the first round.The results of this consultation showed consensus for the following indicator areas: CVD PrimaryPrevention, Alcohol, Smoking, Smoking in Pregnancy and Breastfeeding. In addition, the areas ofcervical screening and immunisations were rated as equivocal and were retained by the group inview of their local importance. Following further discussion, it was felt that since cervicalscreening indicators were already incorporated into national <strong>QOF</strong>, they could be incentivised in<strong>QOF</strong>+ by raising thresholds instead of developing new indicators. It was decided that the DirectedEnhanced Service (DES) currently in place for Immunisations was comprehensive and that itwould not be developed further through <strong>QOF</strong>+. The remaining potential indicator areas were notdeveloped further at this stage as they did not achieve consensus on ratings of importance.Indicators relating to measurement of patient experience, self management of long-termconditions and new entrant screening for TB were however developed at a later stage by the PCTthrough the methodology for the non-clinical indicators, and included within the “patientexperience”, “patient information” and “new patient screening” domains.133
Methodology for the development of new indicatorsIn addition to the indicator areas selected through the structured local consultation, the groupdeveloped new indicators for ethnicity recording (incorporating recording of first language) anddata quality (records). In addition, funding was made available by the PCT in the later stages ofthe project for the incentivisation of indicators relating to additional non-clinical domains. Toinform development of new <strong>QOF</strong>+ non-clinical indicators, a member of the group conducted aninitial brief review to assess the importance of each indicator area (on the basis of nationalguidance and the local context), which Healthcare Commission core standards would be met byinclusion of the proposed indicators, and the anticipated training and development needs.For each selected new indicator area, a literature review of the evidence base was undertaken,and this was used to guide development of indicators, ensuring that new indicators would reflectbest available evidence. National policy and relevant national guidelines, as well as evidence oflocal performance and evaluations of relevant Local Enhanced Services (LES) schemes, includingthe Hammersmith and Fulham CVD Primary Prevention LES and the Lewisham Alcohol LES(Mookherjee, 2007), were used to inform the process. A database of national and <strong>London</strong>-basedLES schemes was created by the group which acted as an additional resource for indicatordevelopment. Consultation also took place with recognised national and international experts inselected indicator areas including alcohol and data quality (records), and with relevant localservices including the Hammersmith and Fulham Drug and Alcohol Team. The process of indicatordevelopment was also informed by the <strong>QOF</strong> evidence-based reports produced by the NationalPrimary Care Research and Development Centre (National Primary Care Research andDevelopment Centre, 2008). These reports were generated by the nationwide call for evidence tohealth professionals and patient groups in Spring 2007 and published evidence base. Each reportand its associated set of indicators was “commented on by members of the Royal <strong>College</strong> ofGeneral Practitioners Patient Participation Group and IT experts to ensure that proposedindicators made sense to patients and would work within primary care IT systems” (NationalPrimary Care Research and Development Centre, 2008).Proposed new <strong>QOF</strong>+ indicators were discussed at regular face-to-face <strong>QOF</strong>+ development groupmeetings and through email between group members, in order to further revise and refine them.An evidence-based “<strong>QOF</strong>+ Report” on each indicator was produced. This was modelled on theevidence-based reports produced as part of the national <strong>QOF</strong> process, and incorporated similarheadings (where appropriate) including proposed indicators, background, priority and relevanceto national policy, prevalence of condition, associated morbidity and mortality, review ofevidence, degree of perceived professional consensus, degree of perceived support from patientsand carers, health impact, and workload and implications for primary care. Additional categoriesrelating to local context, impact on health inequalities and training implications for primary carewere also included.During the final few months prior to launch of the <strong>QOF</strong>+ scheme, the Department of Healthannounced a number of new Directed Enhanced Services (DES), which include Alcohol andEthnicity (NHS Employers, 2008). In light of this, the alcohol and ethnicity indicators for <strong>QOF</strong> <strong>Plus</strong>were reviewed and revised to ensure they were in line with the DES, and this process wasfacilitated by discussions with national and international experts in these areas.134
Consultation with local practicesLocal practices were consulted on the proposed <strong>QOF</strong>+ Scheme including the proposed new <strong>QOF</strong>+indicators. This consultation process took place through a face-to face meeting with primary careteams (GPs, practice managers and practice nurses) and through consultation conducted throughemail.Assessment of new indicatorsCampbell et al. (2003) comment that “although it may never be possible to produce an error- freemeasure of quality, measures should be tested during their development and application foracceptability, feasibility, reliability, sensitivity to change, and validity. This will optimise theireffectiveness in quality improvement strategies. Marshall et al. (2002) highlight the role ofconsensus techniques in facilitating quality improvement.Proposed new indicators were assessed using the OECD (Organisation for Economic Co-operationand Development) criteria of importance, scientific soundness and feasibility as defined below(Marshall et al., 2004). Each indicator was also assessed for clarity.Scientific Soundness refers to the extent to which you believe that each indicator makes senselogically and clinically, and captures meaningful aspects of the quality of care.Importance refers to the extent to which you believe that each indicator is important formeasuring the quality of primary care. The following dimensions were taken into account whenevaluating each indicator:Impact on healthDoes the indicator address areas in which there is a clear gap between the actual andpotential levels of health?Policy importance. Are policymakers and the general public concerned about this area?Susceptibility to being influenced by primary care. Can the primary health care systemmeaningfully address the aspect or problem being measured by the indicator?Feasibility refers to the extent to which you believe that each indicator is feasible in primary care,and to what extent you believe that the value of the information contained in each indicatoroutweighs the cost of data collection and reporting.Clarity refers to the extent to which you believe that each indicator is expressed in clear, preciseand unambiguous language.Members of the <strong>QOF</strong>+ Development Group assessed the indicators in terms of importance. Theassessment of feasibility and clarity of indicators was also informed by consultation with local andnational experts in the proposed indicator areas, including the local Professional and ExecutiveCommittee, Clinical lead for Child Protection, the Hammersmith and Fulham TB Action Group, thelocal Drug and Alcohol Team, Professor Richard Baker and Professor Colin Drummond. Changeswere made to the wording of some indicators as a result.135
Assessment of new clinical and records indicatorsStructured consultation with local stakeholders drawn from the PCT and from primary care wasused further inform indicator development. As part of this consultation, local stakeholders wereasked to assess each proposed new indicator in the clinical and records domains using the OECD(Organisation for Economic Co-operation and Development) criteria of importance, scientificsoundness and feasibility as defined above (Marshall et al., 2004), and also to assess eachindicator for clarity. Each indicator was rated using a 9-point Likert scale. Local stakeholders werealso asked to comment on any aspect of the indicator – including wording of the indicator andproposed thresholds.The consultation method used incorporated aspects of both the Delphi Technique and the RANDAppropriateness Method as described above. After obtaining questionnaire responses from thelocal stakeholder panel in the first round, a second round of structured consultation was used toachieve consensus among respondents. Respondents were provided with a summary of thepanel’s responses from the first round and asked to consider their own responses in light of this,rating each indicator again using the same method as in the first round.As a result, all proposed new indicators were rated by the panel as scientifically sound, relevant,feasible and clear, and consensus was achieved for all indicators.Assessment of new indicators in non-clinical domainsThe process of assessment was informed by consultation with practices on the group’s <strong>QOF</strong>+proposals for non-clinical indicators. Feedback received from practices was used by the <strong>QOF</strong>+Development Group to help assess the indicators further in terms of acceptability, importance,soundness (face-validity), feasibility and clarity of the proposed indicators.Response to feedback on proposed new indicatorsA number of proposed indicators were assessed by the group as being either not acceptable topractices, not sound in terms of face validity or not feasible, following internal review and takingaccount of feedback from practices and from local and national experts. These includedindicators in the patient experience and patient safety domains. These indicators weresubsequently removed.There is currently much debate in the literature about the value of paying practices according tothe results of patient surveys, with concern about the potential perverse effects associated withthis approach (Elwyn et al. 2007). Concerns about indicators relating to the results of patientsurveys were also expressed locally by a number of practices as part of the consultation process.This stimulated further debate within the <strong>QOF</strong>+ Development Group relating to the justificationfor inclusion of these indicators. As a result, these indicators were removed. However, during thefinal phases of the <strong>QOF</strong>+ development process, the results of the Picker Institute Patient Surveyfor Hammersmith and Fulham were published, and these showed that Hammersmith and Fulhampractices were performing below the national average for areas relating to patient access,including being seen within 48 hours, and experiences with getting through to practices on thephone. As a result, the PCT considered inclusion of indicators relating to the results of a localpractice Picker Institute patient survey for these two dimensions compared with the national136
average. It was felt that including these indicators in a local <strong>QOF</strong> would not be out of line with thedirection of travel nationally, and that they should be seen as one aspect of a broader approachincorporating indicators relating to patient survey feedback sessions and evidence ofimplementing actions in low scoring areas. The <strong>QOF</strong>+ Development Group sought further adviceon this issue from Professor Richard Baker, who chaired the national <strong>QOF</strong> patient experienceexpert group which formed part of the <strong>QOF</strong> Review (Lester, 2006). Professor Baker supported thePCT’s proposed approach.Final consultation with local practicesDuring the final month of the scheme’s development, the <strong>QOF</strong>+ Development Group consultedwith practices (GPs, practice nurses and practice managers) on the group’s <strong>QOF</strong>+ proposalsthrough regular consultation conducted through email.Methodology for point allocation for the new <strong>QOF</strong>+ indicatorsThe <strong>QOF</strong>+ Development Group provided recommendations for <strong>QOF</strong>+ point allocations. This wasinformed by considering point allocations for comparable existing <strong>QOF</strong> indicators, currentachievement of <strong>QOF</strong> indicators by practices in Hammersmith and Fulham, and perceivedworkload implications for practices.In addition, a structured consultation with local stakeholders was used to inform the process ofpoint allocation for the clinical and records indicators, consistent with the methodology used inthe national Quality and Outcomes Framework (National Primary Care Research andDevelopment Centre, 2008). The local stakeholders were drawn from the PCT (including the LocalDirector of Public Health and Medical Director), public health and primary care, and included alocal GP, practice nurse and practice manager. The <strong>QOF</strong>+ Development Group also made somemodifications to the wording of indicators, incorporating feedback from the structuredconsultation of local stakeholders.The local Director of Public Health and Medical Director approved the final allocation of <strong>QOF</strong>+points, in accordance with the guidance from the NHS Primary Care Contracting Website (PrimaryCare Contracting, 2008) which states“There is no set workload represented by a <strong>QOF</strong> point. However, any local frameworksused by PMS contractors should be comparable to the National <strong>QOF</strong> in terms of the workneeded to earn the same amount of money. A senior clinician, probably the localDirector of Public Health, needs to make this judgement.”137
Communication with the PCT’s health informatics teamFollowing development of new <strong>QOF</strong>+ indicators, the <strong>QOF</strong>+ Development Group worked with thePCT’s Health Informatics Team to help identify existing read codes for indicators and to provideclinician input into the development of appropriate templates on EMIS and VISION to facilitate<strong>QOF</strong>+, and to provide assistance with the development of the Business Rules for the <strong>QOF</strong>+ NewIndicators. The group also liaised with EMIS and VISION technical advisors to help inform theprocess. Templates were developed and piloted in 2 local practices, with input from practicestaff. Minor changes were made to the wording of some of the indicators following discussionswith the Health Informatics Team. It is anticipated that IT support within <strong>QOF</strong>+ will lead toimproved practice profiling, equity assessment using patient level data, timely progress reports topractices, and will inform who to target with a broader quality improvement support package.As the QMAS does not enable collection of data for <strong>QOF</strong>+, practices will be required to sign up tothe Apollo system to participate in the scheme. This will mean that anonymised medical recordsof all registered patients will be stored centrally by the PCT to enable analysis of performance andpermit monthly feedback of performance to practices. Resources will be put in place for the dataanalysis and to feedback performance data to practices by the team that will evaluate thescheme. In addition IT developments will also be put in place – this might include thedevelopment of a web-based reporting tool that practices can use to examine their ownperformance data and compare their practices against the other practices in the PCT.138
A4.10 ReferencesBMA (2006) Revisions to the GMS Contract 2006/7Boynton PM, Greenhalgh T (2004). Hands-on guide to questionnaire research: selecting, designing,and developing your questionnaire. British Medical Journal 328:1312-5Campbell SM, Braspenning J, Hutchinson A, Marshall MN (2003) Applying quality indicators in primarycare British Medical Journal 326:816-819Department of Health (2008) Operational Plans 2008/9-2010/11 The Stationary OfficeElwyn G, Buetow S, Hibbard J, Wensing M. Respecting the subjective: quality measurement from thepatient's perspective. British Medical Journal 335Hammersmith and Fulham PCT (2007) Patient and Public Involvement Strategy 2006/7 <strong>London</strong>Hammersmith and Fulham PCT (2008) Operating Plan 2008/9 [Online, Accessed June 07 2008]Available at: http://www.hf-pct.nhs.uk/library/boardpapers/Mar08/_15_%20completecorrected.pdfHealthcare Commission (2008) Annual Health Check 2008/9 [Online, Accessed June 15 2008] Availableat:http://www.healthcarecommission.org.uk/guidanceforhealthcarestaff/nhsstaff/annualhealthcheck/annualhealthcheck2008/09/qualityofs/nationalprioritiesprimarycaretrusts.cfmLester H (2006) Methodology for reviewing the quality and outcomes framework [Online, AccessedJune 07 2008] Available at: http://www.pcpoh.bham.ac.uk/primarycare/<strong>QOF</strong>/qof_methodology.shtmlMarshall M, Campbell SM, Hacker J, Roland MO, eds (2002). Quality indicators for general practice: apractical guide for health professionals and managers. <strong>London</strong>: Royal Society of MedicineMarshall M, Leatherman S, Mattke S et al. (2004) Selecting Indicators for the Quality of HealthPromotion, Prevention and Primary Care at the Health Systems Level in OECD Countries OECD HealthTechnical Papers. Employment, Labour and Social Affairs CommitteeMookherjee J (2007) Evaluation of Lewisham’s locally enhanced service for alcohol *Online, AccessedAugust 29 2007] Available at: http://www.alcoholpolicy.net/2007/08/evaluation-of-l.htmlNational Primary Care Research and Development Centre (2008) <strong>QOF</strong> Reports 2008 [Online, AccesssedAugust 10 2008] Available at:http://www.pcpoh.bham.ac.uk/primarycare/<strong>QOF</strong>/qof_reports2008.shtmNaylor CD (1998). What is appropriate care? New England Journal of Medicine 338:1918-20NHS Alliance (2003) Engaging GPs in the new NHS. Retford: NHS AllianceNHS Employers (2008) Clinical Directed Enhanced Services (DES) Guidance for GMS Contract 2008/9Oxman AD TMDDHRB (1995) No magic bullets: a systematic review of 102 trials of interventions toimprove professional practice. Canadian Medical Association Journal 153:1423-31Primary Care Contracting (2008) What is the workload associated with 1 <strong>QOF</strong> point? [Online, AccessedSeptember 01 2008] Available at: http://www.pcc.nhs.uk/qanda.php?article_request=133Zeuner D (2008) Annual Report of the Director of Public Health 2007-2008. Hammersmith and FulhamPCT139
Appendix 5Methodology for the development of thetraining and support packageDevelopment of the training and support packageFinancial incentives delivered in isolation are unlikely to lead to optimal quality improvement(Oxman, 1995). For this reason, a range of interventions is being developed to support practicesparticipating in <strong>QOF</strong>+ to improve the quality of care delivered to their patients. Theseinterventions include additional educational and training activities, audit, academic detailing,enhanced IT support and development of a resource pack for practices. These interventions willincorporate both face-to-face and e·learning components through a blended learning approach.As part of the support package, a dedicated email address has been set up by the PCT for generalhelp and support required by practices with any aspect of <strong>QOF</strong>+. An additional service, titled “Askthe Specialist” has also been set up by the PCT to enable practices to access more focussed adviceabout the management of specific problems. Practices can email requests which will then bescreened and forwarded to the relevant specialists. A detailed practice training and supportneeds analysis is currently in progress and will inform further development of the <strong>QOF</strong>+ trainingand support package.Development of the training and support package for existing <strong>QOF</strong> indicators was informed byconsultation with national experts, by analysis of data on achievement for existing <strong>QOF</strong> forindividual practices (obtained through information collated from the QMAS website), and by atraining and support needs assessment conducted among all local practices through aquestionnaire which was developed by and piloted on members of the <strong>QOF</strong>+ development team.The questionnaire was developed using the principles of questionnaire design (Boynton et al.,2004).The <strong>QOF</strong>+ Development Group also identified training needs associated with the proposed newindicator areas and proposed mechanisms by which this could be addressed, which includedattendance at courses, online resources, face-to-face in-practice training and additional ITsupport. Proposed training resources were developed following consultation with relevant localexpertise (including the Hammersmith and Fulham Drug and Alcohol Team), the Royal <strong>College</strong> ofPractitioners (RCGP) and the Department of Health, and these are included in the Resource Packfor <strong>QOF</strong>+ new indicator areas which has been produced for local practices.140
Results of data analysis of practice achievement for selected existing<strong>QOF</strong> indicatorsAnalysis of data on <strong>QOF</strong> achievement by individual practices suggested possible generaltraining/support needs (for most practices) in the areas of Mental Health and Cervical Screening.The data also highlighted a small number of underperforming practices which may need moreglobal (rather than specific) support. This support may need to be more administrative andmanagerial than clinical.Results of practice training and support needs assessmentAnalysis of data from a training and support needs assessment of local primary care practitioners(GPs, practice nurses and practice managers) showed that the majority of practices would valueincreased administrative support, including additional training for administrative staff. A numberof practices felt that additional clinical training and support for practice nurses would bebeneficial.Practices described a range of methods for delivery of training that they would find useful,including online modules, educational meetings and individual practice trainer visits. It isenvisaged that the <strong>QOF</strong>+ training and support package will incorporate all these mechanisms toencompass a wide range of learning styles and preferences.A number of practices highlighted the importance of tailoring training to individual practiceneeds. To this end, those practices signing up to <strong>QOF</strong>+ will receive an additional training bursarywhich will allow them to determine how best their training needs may be met.One practice felt that it would be useful if the PCT hosted regular <strong>QOF</strong>+ meetings for practices tofacilitate sharing of ideas between practices. This idea will be developed further by the PCT.A5.4 ReferencesOxman AD TMDDHRB (1995). No magic bullets: a systematic review of 102 trials of interventions toimprove professional practice. Canadian Medical Association Journal 153:1423-31141
Appendix 6Summary of the <strong>QOF</strong>+ schemeThrough <strong>QOF</strong>+, practices will be rewarded with <strong>QOF</strong>+ points for achievement of higher thresholdsfor a selected number of existing national <strong>QOF</strong> indicators for which Hammersmith and Fulham iscurrently underperforming:Asthma 6, BP 5, CHD 6, CHD 8, CHD 10, CS 1, DM 12, DM 17, DM 20, MH 6, Stroke 6, Stroke 8.Additionally, practices will be rewarded for achievement of new <strong>QOF</strong>+ indicators which havebeen developed in clinical and non-clinical domains covering the following areas: CardiovascularDisease (CVD) Primary Prevention, Alcohol, Smoking Cessation (Adults), Smoking Cessation(Pregnant women), Breastfeeding, Ethnicity, Records, New Patient Screening (New entrantscreening for TB), Patient Information, Patient Experience and Patient Safety. The clinical areasselected were identified as priorities on the basis of being included in both the NHSHammersmith and Fulham Annual Public Health Report (Zeuner, 2008) and in the KeyPerformance Indicators from the Healthcare Commission (Healthcare Commission, 2008).Indicators are likely to change for subsequent years of <strong>QOF</strong>+ in line with latest best evidence andpotential changes to national <strong>QOF</strong> indicators.<strong>QOF</strong>+ has adopted the same approach to payment as the national <strong>QOF</strong> scheme, using the samevalue for a <strong>QOF</strong>+ point (1 point = £124.60), the same approach to exception reporting and thesame mechanism for adjustment according to Contractor Population Index and AdjustedPrevalence Disease Factors (for clinical indicators if appropriate).A <strong>QOF</strong>+ Training and Support package has been developed to support implementation of <strong>QOF</strong>+.This includes the production of a Resource Pack for practices relating to the new <strong>QOF</strong>+ indicators,and the creation of an email support service, ‘Ask the Specialist’. Attainment statistics will becalculated centrally on a monthly basis. These will be used to assist practices in self-monitoring ofprogress and to trigger intervention by the <strong>QOF</strong>+ support and development team if attainment ismore than a month behind the agreed trajectory towards aspiration targets.A programme of multimodal evaluation, currently under development, aims to assist monitoringof the scheme and to support the PCT in its efforts to better understand health inequalities withinHammersmith and Fulham. It is hoped that this evaluation will assist in the identification anddesign of future indicator areas.A6.2 ReferencesZeuner D (2008) Annual Report of the Director of Public Health 2007-2008. Hammersmith and FulhamPCT142
Additional <strong>QOF</strong>+ resources and content are available to download from:requires N3 connection143