Pain Assessment in Advanced Dementia - Pain Resource Center
Pain Assessment in Advanced Dementia - Pain Resource Center
Pain Assessment in Advanced Dementia - Pain Resource Center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
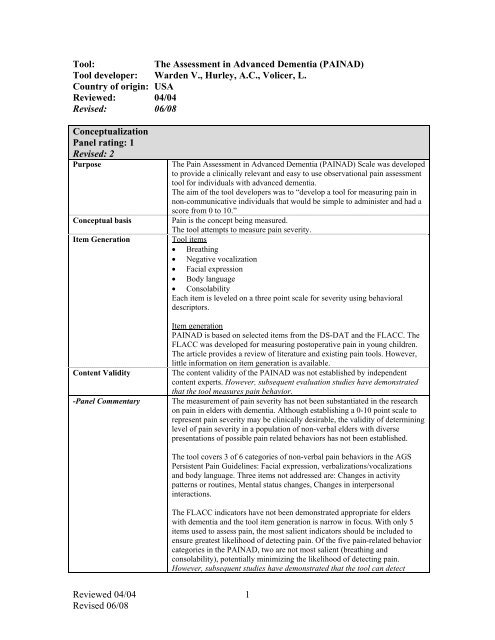
Tool:The <strong>Assessment</strong> <strong>in</strong> <strong>Advanced</strong> <strong>Dementia</strong> (PAINAD)Tool developer: Warden V., Hurley, A.C., Volicer, L.Country of orig<strong>in</strong>: USAReviewed: 04/04Revised: 06/08ConceptualizationPanel rat<strong>in</strong>g: 1Revised: 2PurposeConceptual basisItem GenerationContent Validity-Panel CommentaryThe <strong>Pa<strong>in</strong></strong> <strong>Assessment</strong> <strong>in</strong> <strong>Advanced</strong> <strong>Dementia</strong> (PAINAD) Scale was developedto provide a cl<strong>in</strong>ically relevant and easy to use observational pa<strong>in</strong> assessmenttool for <strong>in</strong>dividuals with advanced dementia.The aim of the tool developers was to “develop a tool for measur<strong>in</strong>g pa<strong>in</strong> <strong>in</strong>non-communicative <strong>in</strong>dividuals that would be simple to adm<strong>in</strong>ister and had ascore from 0 to 10.”<strong>Pa<strong>in</strong></strong> is the concept be<strong>in</strong>g measured.The tool attempts to measure pa<strong>in</strong> severity.Tool items• Breath<strong>in</strong>g• Negative vocalization• Facial expression• Body language• ConsolabilityEach item is leveled on a three po<strong>in</strong>t scale for severity us<strong>in</strong>g behavioraldescriptors.Item generationPAINAD is based on selected items from the DS-DAT and the FLACC. TheFLACC was developed for measur<strong>in</strong>g postoperative pa<strong>in</strong> <strong>in</strong> young children.The article provides a review of literature and exist<strong>in</strong>g pa<strong>in</strong> tools. However,little <strong>in</strong>formation on item generation is available.The content validity of the PAINAD was not established by <strong>in</strong>dependentcontent experts. However, subsequent evaluation studies have demonstratedthat the tool measures pa<strong>in</strong> behavior.The measurement of pa<strong>in</strong> severity has not been substantiated <strong>in</strong> the researchon pa<strong>in</strong> <strong>in</strong> elders with dementia. Although establish<strong>in</strong>g a 0-10 po<strong>in</strong>t scale torepresent pa<strong>in</strong> severity may be cl<strong>in</strong>ically desirable, the validity of determ<strong>in</strong><strong>in</strong>glevel of pa<strong>in</strong> severity <strong>in</strong> a population of non-verbal elders with diversepresentations of possible pa<strong>in</strong> related behaviors has not been established.The tool covers 3 of 6 categories of non-verbal pa<strong>in</strong> behaviors <strong>in</strong> the AGSPersistent <strong>Pa<strong>in</strong></strong> Guidel<strong>in</strong>es: Facial expression, verbalizations/vocalizationsand body language. Three items not addressed are: Changes <strong>in</strong> activitypatterns or rout<strong>in</strong>es, Mental status changes, Changes <strong>in</strong> <strong>in</strong>terpersonal<strong>in</strong>teractions.The FLACC <strong>in</strong>dicators have not been demonstrated appropriate for elderswith dementia and the tool item generation is narrow <strong>in</strong> focus. With only 5items used to assess pa<strong>in</strong>, the most salient <strong>in</strong>dicators should be <strong>in</strong>cluded toensure greatest likelihood of detect<strong>in</strong>g pa<strong>in</strong>. Of the five pa<strong>in</strong>-related behaviorcategories <strong>in</strong> the PAINAD, two are not most salient (breath<strong>in</strong>g andconsolability), potentially m<strong>in</strong>imiz<strong>in</strong>g the likelihood of detect<strong>in</strong>g pa<strong>in</strong>.However, subsequent studies have demonstrated that the tool can detectReviewed 04/04Revised 06/081
presence of pa<strong>in</strong>.Scor<strong>in</strong>g of the breath<strong>in</strong>g <strong>in</strong>dicator seems unrelated to pa<strong>in</strong> severity.Breath<strong>in</strong>g does not seem to be a key <strong>in</strong>dicator of pa<strong>in</strong>. However, the tooldevelopers argue that one of the known areas believed to cause negativefeel<strong>in</strong>gs for persons with dementia is the aversive symptoms associated with<strong>in</strong>tercurrent respiratory <strong>in</strong>fections and that pneumonia is a the proximal causeof death for many demented persons. Thus, they <strong>in</strong>cluded the breath<strong>in</strong>g item.We perceive consolablity as a response to an <strong>in</strong>tervention, not a behavioralmanifestation of pa<strong>in</strong>. However, the relationship between consolability andpa<strong>in</strong> may be an area for future research <strong>in</strong> this population.The validity for the scor<strong>in</strong>g of items accord<strong>in</strong>g to pa<strong>in</strong> severity or separationof behaviors with<strong>in</strong> each major category is not established, (eg. Breath<strong>in</strong>g isscored: Normal=0, Occasional labored breath<strong>in</strong>g/Short period ofhyperventilation =1, Noisy labored breath<strong>in</strong>g/Long period ofhyperventilation/Cheyne-Stokes respirations=2). However the tool appears toidentify higher and lower levels of pa<strong>in</strong> <strong>in</strong> an <strong>in</strong>dividual.Although the PAINAD does not adequately sample the content area ofbehavioral <strong>in</strong>dicators for pa<strong>in</strong> <strong>in</strong> elders with dementia who are unable tocommunicate, studies have demonstrated that the tool measures pa<strong>in</strong>. It maynot detect pa<strong>in</strong> <strong>in</strong> patients that demonstrate pa<strong>in</strong> with behaviors other thanthose <strong>in</strong>cluded <strong>in</strong> the tool.SubjectsPanel rat<strong>in</strong>g: 1Revised: 3Subjects Study 1 (Warden et al., 2003)Long term care VA <strong>Dementia</strong> Special Care Unit (96 patient unit).Subjects: 19 veterans, all CaucasianAverage age: 78.1 years (±5), Range 66-85 yearsGender: Female: 0, Male: 100%The subjects had dementia for 8.7 years on average (±4.7), Range 1-20.Length of time <strong>in</strong> residence: 16.5 months average (±13.5), Range 1-50months.MMSE: 2.8 ±4.5, Range 0-16.Bedford Alzheimer Nurs<strong>in</strong>g Severity Subscale: average 16.4 ±4.4, Range 9-23.Study 2 Lane et al., 2003)QI study – charts of 25 patients were used.No demographic data or disease characteristics are available for thesesubjects.Study 3 (Costardi et al., 2006)Geriatric Evaluation and Rehabilitation Unit, Northern Italy (n=1)Subjects: 20 with chronic pa<strong>in</strong> and dementiaAverage age: 82 (SD=5.9) years; Range: 73-93 yearsGender: Female 80% Male: 20%MMSE: 16.4 + 3.8, range 10-22Study 4 (Hutchison et al., 2006)Acute care hospital, US (n=1)Subjects: 53 control and 27 PAINAD with acute postop pa<strong>in</strong>Reviewed 04/04Revised 06/082
Average Age: 85.2 control and 88 PAINADGender: 85% female <strong>in</strong> control and 78% female <strong>in</strong> PAINADMMSE: control: 0% with less than 25 <strong>in</strong> control and 100% diagnoseddementiaPAINAD group: 23.6% with MMSE less than 25 and 76.4% diagnoseddementiaStudy 5 (Leong et al., 2006)Nurs<strong>in</strong>g Home <strong>in</strong> S<strong>in</strong>gapore (n=1)Subjects: 88 with moderate and severe dementiaAverage Age: 79.6 (SD=8.3)Gender: 61.4% female; 38.6% maleMMSE: Not reportedStudy 6 (van Iersel et al., 2006)Palliative care patients <strong>in</strong> NH sett<strong>in</strong>g (n=17)Patients who could not express pa<strong>in</strong>Subjects: 157 patientsAverage Age: 85 years; range 22-100Gender: 78% female; 22% maleMMSE: Not reportedStudy 7 (Zwakhalen et al., 2006)Nurs<strong>in</strong>g Homes <strong>in</strong> Netherlands (n=3)Subjects: 128 patients with dementia; both acute and chronic pa<strong>in</strong>Average Age: 82.4 (SD=6.8) years; range 60-96Gender: 78.1% female; 21.9% maleMMSE: Not reported; Cognitive Performance Scale: 21.9% mild, 28.1%moderate, 47.7% severeStudy 8 (Schuler et al., 2007)Nurs<strong>in</strong>g Homes <strong>in</strong> Germany (n=8)Subjects: 99 residents with dementiaAverage Age: 84.9 (SD=7.5)Gender: 80% female; 20% maleMMSE: Mean 12.1 (SD=9.7)Study 9 (Cohen-Mansfield & Lipson, 2008)Nurs<strong>in</strong>g homes <strong>in</strong> US (n=4)Subjects: 121 with dementiaAverage Age: 88 (range 59-101)Gender: 81.8% femaleMMSE: Mean 6.3 (range 0-20)Study 10 (DeWaters et al., 2008)Orthopedic unit <strong>in</strong> US hospital (n=1)Subjects: 25 verbal older persons, <strong>in</strong>cludes 13 cognitively <strong>in</strong>tact and 12cognitively impaired personsAverage age: 81.24 (range 65-95)Gender: 84% femaleMMSE: 20.52 (range 9-30) plus diagnosis of dementia or confusion-Panel Commentary The PAINAD has received considerable attention <strong>in</strong>ternationally and 7additional studies have been conducted that provide additional psychometricdata on this tool. The PAINAD was translated and tested <strong>in</strong> S<strong>in</strong>gapore,Belgium, Italy, Netherlands, and Germany, as well as two studies <strong>in</strong> the US.The majority of additional study has been conducted <strong>in</strong> NHs, however test<strong>in</strong>gReviewed 04/04Revised 06/083
has also occurred <strong>in</strong> acute care hospitals and geriatric rehabilitation center.These studies have added data with female subjects, a gap <strong>in</strong> the developmentstudies. There is still limited data on <strong>in</strong>dividuals from different races,although cultural variation has been tested across countries. All studies have<strong>in</strong>cluded <strong>in</strong>dividuals with dementia. Age of subjects across studies isappropriate with mean age of samples rang<strong>in</strong>g from 78 to 88 years.Adm<strong>in</strong>istration, Scor<strong>in</strong>g, FeasibilityPanel rat<strong>in</strong>g: 2Revised: 3Adm<strong>in</strong>istration, Scor<strong>in</strong>g,FeasibilityIn the pilot test, subjects were observed for 5 m<strong>in</strong>utes prior to scor<strong>in</strong>g.Def<strong>in</strong>itions for each item are provided.The scor<strong>in</strong>g system is based on a 3 po<strong>in</strong>t scale: 0, 1, 2.Total scores range from 0 to 10 po<strong>in</strong>ts, a maximum of 2 po<strong>in</strong>ts per category.The tool developers report that because they wanted the 10 po<strong>in</strong>t scale, theydeterm<strong>in</strong>ed that there would be a 3 po<strong>in</strong>t rat<strong>in</strong>g option for each item, and that<strong>in</strong> general, 0=none, 1=small or some or occasionally, and 2=large or a more<strong>in</strong>tense negative behavior mak<strong>in</strong>g that item operational. Specific def<strong>in</strong>itionsfor each behavior are provided.No <strong>in</strong>terpretation of the score is provided.A two hour tra<strong>in</strong><strong>in</strong>g program was developed <strong>in</strong>clud<strong>in</strong>g video tra<strong>in</strong><strong>in</strong>g tapes.Study 3 (Costardi et al., 2006)Comment easily adm<strong>in</strong>istered with appropriate tra<strong>in</strong><strong>in</strong>gStudy 4 (Hutchison et al., 2006)Raters received 15 m<strong>in</strong>ute <strong>in</strong>-service <strong>in</strong>struction. Cl<strong>in</strong>icians reported easy toadm<strong>in</strong>ister, requir<strong>in</strong>g less than 1 m<strong>in</strong>ute of time.Study 5 (Leong et al., 2006)No comments provided.Study 6 (van Iersel et al., 2006)Care providers (n=17): 80% agreed or had no op<strong>in</strong>ion (20% disagreed) thatthe PAINAD was a good measure to judge pa<strong>in</strong> and 76% agreed or had noop<strong>in</strong>ion that PAINAD was easy to use (28% disagreed). Breath<strong>in</strong>g andconsolability <strong>in</strong>dicators were less good <strong>in</strong>dicators (
Scor<strong>in</strong>g procedures are clearly described.No guide to <strong>in</strong>terpretation of tool score is provided. The tool developers arguethat cl<strong>in</strong>icians are familiar with a 0-10 scale and that it is assumed that 0means no observed pa<strong>in</strong> and 10 means a high level of observed pa<strong>in</strong> thatshould be treated.However, this assumes that judg<strong>in</strong>g severity of pa<strong>in</strong> represented by behavioralpresentation <strong>in</strong> non-verbal elders is valid—which has not been substantiated<strong>in</strong> the literature.Subsequent studies have demonstrated strong cl<strong>in</strong>ical utility withadm<strong>in</strong>istration possible with<strong>in</strong> 1-3 m<strong>in</strong>utes, limited tra<strong>in</strong><strong>in</strong>g required(m<strong>in</strong>imum of 15 m<strong>in</strong>utes to 2 hours), and reported ease of use by raters.ReliabilityPanel rat<strong>in</strong>g: 1Revised: 3Internal consistency Study 1 & 2 (Warden et al, 2003; Lane et al., 2003)Internal consistency was evaluated based on data from a sample of 19veterans and QI data from 25 residents. (For sample characteristics seesubjects above).Raters were 4 professional nurses with experience on dementia special careunits and a master’s level social work <strong>in</strong>tern. Three observations of subjectsfor 5 m<strong>in</strong>utes were made under different conditions as <strong>in</strong>dicated below. Toachieve 10 participants per item, the research and QI data were pooled andexam<strong>in</strong>ed for <strong>in</strong>ternal consistency.Observation 1: Dur<strong>in</strong>g rest or no activity: Cronbach’s alpha=.50Observation 2: Pleasant activity: movement could lead to pa<strong>in</strong>:Cronbach’s alpha=.59, .63Observation 3: Potentially unpleasant caregiv<strong>in</strong>g activity (eg. Transfers,bath<strong>in</strong>g, toilet<strong>in</strong>g) Cronbach’s alpha=.50, .67.Additional data on <strong>in</strong>ternal consistency has been reported by 3 studies.Study 3 (Costardi et al., 2006)Internal consistency=0.74Study 7 (Zwakhalen et al., 2006)Cronbach’s alpha 0.69-0.74; Breath<strong>in</strong>g scored consistently low -.51 to .12Study 8 (Schuler et al., 2007)Cronbach’s alpha= 0.85Study 10 (DeWaters et al., 2008)Cronbach’s alpha for comb<strong>in</strong>ed group 0.852Cronbach’s alpha for cognitively <strong>in</strong>tact group =0.846Cronbach’s alpha for cognitively impaired group =0.847Interrater reliability Study 1 (Warden et al., 2003)Interrater reliability is reported for 19 subjects by pairs of simultaneousobservations by two <strong>in</strong>dependent raters.Pearson’s correlation coefficient:• Dur<strong>in</strong>g pleasant activity r=.97• Dur<strong>in</strong>g unpleasant activity r=.82.Additional data on <strong>in</strong>ter-rater reliability has been reported by 4 studiesStudy 3 (Costardi et al., 2006)Two raters same day=0.87 (p=.001)Reviewed 04/04Revised 06/085
Study 7 (Zwakhalen et al., 2006)Inter-rater reliabilities reported: 0.75 (rest), 0.85 (after flu vacc<strong>in</strong>e) and 0.81(patient-specific moment of potential pa<strong>in</strong>). Agreement less strong at rest thandur<strong>in</strong>g potential pa<strong>in</strong>ful activity.Study 8 (Schuler et al., 2007)Two nurses morn<strong>in</strong>g and even<strong>in</strong>g assessments: reliability= 0.80 (p=.001)Study 9 (Cohen-Mansfield & Lipson, 2008)Inter-rater agreement across three RAs: ICC=0.92Test-retest reliabilityStudy 10 (DeWaters et al., 2008)Interrater reliability between 2 master’s prepared nurse RAs for ten videovignette rat<strong>in</strong>gs: ICC= 0.98No test-retest reliability is reported.Data on test-retest and/or <strong>in</strong>tra-rater reliability reported <strong>in</strong> 3 studies.Study 3 (Costardi et al., 2006)One expert rater at basel<strong>in</strong>e and after 15 days=0.88 (p=.045)Study 7 (Zwakhalen et al., 2006)Intra-rater reliability=0.89; compar<strong>in</strong>g rat<strong>in</strong>g <strong>in</strong> person with rat<strong>in</strong>g on video-Panel commentaryStudy 8 (Schuler et al., 2007)One nurses morn<strong>in</strong>g and even<strong>in</strong>g assessments; r=0.90 (p
Concurrent validity was reported based on associations from observations ofpa<strong>in</strong> dur<strong>in</strong>g 1) presumed pleasant conditions for 18 veterans and 2) presumedunpleasant conditions for 19 veterans (p=.001 for all correlations).1) Presumed pleasant conditions (n=18)PAINAD (1) & <strong>Pa<strong>in</strong></strong>-VAS (1) r=.92PAINAD (1) & <strong>Pa<strong>in</strong></strong>-VAS (2) r=.89<strong>Pa<strong>in</strong></strong>-VAS (1) & PAINAD (2) r=.93PAINAD (2) & <strong>Pa<strong>in</strong></strong>-VAS (2) r=.952) Presumed unpleasant conditions (n=19)PAINAD (1) & <strong>Pa<strong>in</strong></strong> VAS (1) r=.82PAINAD (1) & <strong>Pa<strong>in</strong></strong> VAS (2) r=.90<strong>Pa<strong>in</strong></strong>-VAS (1) & PAINAD (2) r=.90PAINAD (2) & <strong>Pa<strong>in</strong></strong>-VAS (2) r=.91Discrim<strong>in</strong>ant validityStudy 1(For sample characteristics see subjects above.)Subjects (n=19) were observed 3 times to establish expected pa<strong>in</strong> withsignificant outcomes (F 1,17 = 10.93, P
Study 6 (van Iersel et al., 2006)Construct: 185 care providers report on perceptions of measure of pa<strong>in</strong>.80% agreed that three <strong>in</strong>dicators were most valuable <strong>in</strong> measur<strong>in</strong>g pa<strong>in</strong>:facial expression, vocalization and body language. Breath<strong>in</strong>g andconsolability less good <strong>in</strong>dicators (
number of patients with behaviors reflect<strong>in</strong>g the high end of the scale scor<strong>in</strong>gis still small.Concurrent validityCorrelations among the pa<strong>in</strong> tools are strong. However, lack of <strong>in</strong>dependentraters for scor<strong>in</strong>g of the pa<strong>in</strong> tools and the associated VAS’s potentiallyimpacts the level of associations.Further study of the PAINAD provides support for good concurrent validitywith across tool correlations rang<strong>in</strong>g from 0.65 to 095 with the exception ofcomparison of the PAINAD to self report of pa<strong>in</strong> (0.30).Discrim<strong>in</strong>ant validityStudy 1 results show differences <strong>in</strong> expected outcome, although scores arecompressed at the lower end of the scale and further study is needed.The results of study 2 (QI study) appear to capture pa<strong>in</strong> and change <strong>in</strong> pa<strong>in</strong>.However, limited <strong>in</strong>formation on subjects, variability of raters/assessors,control over chart audit data limits conclusions that can be reached for <strong>in</strong>itialtool development and suggest the need for more controlled study.Further study of the PAINAD provides some support for construct, predictive,concurrent and discrim<strong>in</strong>ant validity. The most recent study that exam<strong>in</strong>estool sensitivity <strong>in</strong> detect<strong>in</strong>g change from treatment raises questions regard<strong>in</strong>gthe tools ability to do so with persons with severe dementia. Further study isneeded.Although studies have raised concern regard<strong>in</strong>g the items of breath<strong>in</strong>g andconsolability, authors urge ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g the current items structure to allow<strong>in</strong>ternational comparisons. Because removal of items did not demonstrateimproved <strong>in</strong>ternal consistency, this recommendation seems supportable.Summary of panel evaluation of pa<strong>in</strong> assessment toolThe PAINAD was developed as a shorter, easier observation tool for assess<strong>in</strong>g pa<strong>in</strong> <strong>in</strong> nonverbal elders. Thetool items <strong>in</strong>cluded are not comprehensive, but subsequent studies have provided data suggest<strong>in</strong>g the tooldoes detect pa<strong>in</strong> and chang<strong>in</strong>g levels of behavior (not pa<strong>in</strong>) <strong>in</strong>tensity. Because of the small number of itemsthat are used to detect pa<strong>in</strong>, the ability of the PAINAD to detect pa<strong>in</strong> <strong>in</strong> those with less obvious changes <strong>in</strong>behavior (e.g. mental status changes, aggressive behavior, changes <strong>in</strong> activities) may still be compromised.Although cl<strong>in</strong>icians desire to have a tool that provides a 1-10 score similar to the 1-10 NRS commonly usedas the gold standard <strong>in</strong> verbal patients, the soundness of establish<strong>in</strong>g a rat<strong>in</strong>g scale with pa<strong>in</strong> severity scor<strong>in</strong>gof behaviors has not been substantiated <strong>in</strong> the literature. Completed studies suggest the tool could be used toshow higher and lower levels of pa<strong>in</strong>, but there is no data to attach level of pa<strong>in</strong> severity to the numberobta<strong>in</strong>ed with the tool.Tool reliability is good for <strong>in</strong>terrater reliability, but <strong>in</strong>ternal consistency is only moderate and stability hasnot been demonstrated. Tool has good reliability <strong>in</strong> all areas.Some conceptual and methodological issues have been identified with the development and test<strong>in</strong>g of thePAINAD. However, the positive f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> detection of changes <strong>in</strong> pa<strong>in</strong> behavior follow<strong>in</strong>g <strong>in</strong>tervention <strong>in</strong>the QI study reported suggests additional study <strong>in</strong> controlled circumstances is warranted. Follow-up studieshave cont<strong>in</strong>ued to document ability to detect pa<strong>in</strong> and differentiate pa<strong>in</strong> and no pa<strong>in</strong> groups. Follow-upstudies must be differentiated accord<strong>in</strong>g to degree of dementia <strong>in</strong> the sample population, whether they studyacute or chronic pa<strong>in</strong> and the sett<strong>in</strong>g of care. Further study of tool sensitivity to detect change <strong>in</strong> behavior <strong>in</strong>response to treatment is needed.Reviewed 04/04Revised 06/089
Source of evidenceWarden, V., Hurley, A.C., Volicer, L. (2003). Development and psychometric evaluation of the <strong>Pa<strong>in</strong></strong><strong>Assessment</strong> <strong>in</strong> <strong>Advanced</strong> <strong>Dementia</strong> (PAINAD) Scale. Journal of the American Medical Directors,Jan/Feb, 9-15.Lane, P., Kuntupis, M., MacDonald, S., McCarthy, P., Panke, J., Warden, V., Volicer, L. (2003). A pa<strong>in</strong>assessment tool for people with advanced Alzheimer’s and other progressive dementias. HomeHealthcare Nurse, 21(1), 32-37.DeWaters, T., Faut-Callahan, M., McCann, J. J., Paice, J. A., Fogg, L., Holl<strong>in</strong>ger-Smith, L., et al. (2008).Comparison of self-reported pa<strong>in</strong> and the PAINAD scale <strong>in</strong> hospitalized cognitively impaired and<strong>in</strong>tact older adults after hip fracture surgery. Orthopaedic Nurs<strong>in</strong>g / National Association ofOrthopaedic Nurses, 27(1), 21-28.Costardi, D., Rozz<strong>in</strong>i, L., Costanzi, C., Ghianda, D., Franzoni, S., Padovani, A. & Trabucchi, M. (2006).The Italian version of the pa<strong>in</strong> assessment <strong>in</strong> advanced dementia (PAINAD) scale. Archives ofGerontology and Geriatrics, 44(2), 175-180.Hutchison, R., Tucker, W., Kim, S. & Gilder, R. (2006). Evaluation of a behavioral assessment tool for the<strong>in</strong>dividual unable to self-report pa<strong>in</strong>. American Journal of Hospice and Palliative Medic<strong>in</strong>e, 23(4),328-331.Leong, I., Chong, M. & Gibson, S. (2006). The use of a self-reported pa<strong>in</strong> measure, a nurse-reported pa<strong>in</strong>measure and the PAINAD <strong>in</strong> nurs<strong>in</strong>g home residents with moderate and severe dementia: a validationstudy. Age and Age<strong>in</strong>g, 35, 252-256.Schuler, M., Becker, S., Kaspar, R., Nikolaus, T., Kruse, A. & Basler, H. (2007). Psychometric propertiesof the German “<strong>Pa<strong>in</strong></strong> Assesssment <strong>in</strong> <strong>Advanced</strong> <strong>Dementia</strong>” (PAINAD-G) <strong>in</strong> Nurs<strong>in</strong>g Home residents.American Medical Directors Association, July, 388-395.Van Iersel, T., Timmerman, D. & Mullie, A. (2006). Introduction of a pa<strong>in</strong> scale for palliative care patientswith cognitive impairment. International Study of Palliative Nurs<strong>in</strong>g, 12(2), 54-59.Zwakhalen, S., Hamers, I. & Berger, M. (2006). The psychometric quality and cl<strong>in</strong>ical usefulness of threepa<strong>in</strong> assessment tools for elderly people with dementia. <strong>Pa<strong>in</strong></strong>, 126, 210-220.Cohen-Mansfield, J. & Lipson, S. (2008). The utility of pa<strong>in</strong> assessment for analgesic use <strong>in</strong> persons withdementia. <strong>Pa<strong>in</strong></strong>, 134(1-2), 16-23.Key to panel rat<strong>in</strong>g3= Available evidence is strong2= Available evidence supports need for further test<strong>in</strong>g1= Available evidence is <strong>in</strong>sufficient and/or tool revisions are needed0= Evidence is absentContact address for tool developer:Victoria Warden, RNGRECC (182B)E. N. Rogers Memorial Veterans Hospital, 200 Spr<strong>in</strong>gs Road, Bedford, MA 01730.E-mail: Victoria.Warden@med.va.gov.Evaluation completed by:K. Herr, S. Decker, K. Bjoro, University of Iowa.Reviewed 04/04Revised 06/0810
Revision completed 06/08 by:K. Herr, H. Bursch, B. Black, The University of IowaContact <strong>in</strong>formation: keela-herr@uiowa.eduReviewed 04/04Revised 06/0811