WV I/DD Waiver Training for Providers - DHHR
WV I/DD Waiver Training for Providers - DHHR
WV I/DD Waiver Training for Providers - DHHR
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Initial Eligibility Determination Process• The IP completes the IPE andsubmits it to APS within 60 days ofthe initial application• APS will verify the IPE is complete,signed/dated and will <strong>for</strong>ward tothe Medical Eligibility ContractedAgent (MECA)• The MECA will verify clinically(diagnosis, deficits, etc)7
Initial Eligibility Determination Process• Once received, the MECA has 30days to make a medical eligibilitydetermination• Timeline Summary:– 60 days <strong>for</strong> IP to submit IPE– 30 days <strong>for</strong> the MECA to make adetermination– 90 days total between application anddetermination8
Initial Eligibility Determination Process• The applicant will be notified of thedetermination of the MECA in a Noticeof Decision letter• If determined medically eligible, theapplicant will receive an in<strong>for</strong>mationalpacket describing the program andService Options9
Initial Eligibility Determination Process• Within 90 days of receiving a slot,member will receive Freedom ofChoice (<strong>WV</strong>-BMS-I/<strong>DD</strong>-2) <strong>for</strong>m (may beless than 90 days if a slot becomes availablesometime throughout the year-other than 7/1)– Choice between ICF/MR or I/<strong>DD</strong> <strong>Waiver</strong>– Choice of Service Coordination agency– Choice of Participant-Directed and/orTraditional Services10
Initial Eligibility Determination Process• Once determined medically eligible andnotified that a slot is available, the applicantmust apply <strong>for</strong> financial eligibility at theirlocal <strong>DHHR</strong> prior to enrollment• Provider must verify that both medical andfinancial eligibility are established prior tobeing reimbursed <strong>for</strong> services provided• If determined ineligible, the applicant has90 days to appeal with the Board of Review11
Re-eligibility Determination Process• Medical eligibility must be re-determinedannually• APS will conduct the functional assessmentwhich will be used to determine theindividualized budget and annual medicaleligibility• APS will <strong>for</strong>ward the assessment to theMECA• The MECA will determine medical eligibilityannually based on this functionalassessment12
Re-eligibility Determination Process• Agencies will continue to completerecertification packets through October 1,2011• Any <strong>DD</strong>1 (<strong>for</strong>mer <strong>DD</strong>14) signed be<strong>for</strong>e10/1/2011 will access ―old‖ process; ifsigned 10/1/2011 or after, will access ―new‖process• Beginning October 1, 2011, theassessments completed by the SSFs willbe sent to PC&A <strong>for</strong> review <strong>for</strong> annualmedical eligibility13
Member Rights• The right to choose between ICF/MRor I/<strong>DD</strong> <strong>Waiver</strong>• The right to choose ServiceCoordination agency• The right to choose Participant-Directed and/or Traditional Services• The right to have multiple providers• The right to voice dissatisfaction withservices• The right to a Medicaid Fair Hearing14
Member Rights• <strong>Providers</strong> must:– Ensure that a member is not dischargedunless a viable discharge/transfer plan isin place that effectively transfers allservices the member needs to anotherprovider or providers and is agreed uponby the member and/or their legalrepresentative and the receiving provideror providers15
Member/Family/Legal Rep Responsibilities• Member may be discharged from the I/<strong>DD</strong><strong>Waiver</strong> Program if not compliant withresponsibilities:– Be present during Interdisciplinary TeamMeetings (IDT)– Participate in annual functional assessmentswhich will determine medical eligibility andbudget– Comply with I/<strong>DD</strong> <strong>Waiver</strong> policies includingmonthly SC home visits– Implement portions of the Individual ProgramPlan (IPP) <strong>for</strong> which they have acceptedresponsibility• Maintain a safe environment <strong>for</strong> employees towork16
Member/Family/Legal Rep Responsibilities• Report suspected fraud to Medicaid FraudControl Unit:– MFCU is charged with investigatingsuspected Medicaid fraud and makingapplicable referrals <strong>for</strong> prosecution– Investigate alleged abuse, neglect andfinancial exploitation of persons whoreceive Medicaid17
Member/Family/Legal Rep Responsibilities• Examples of Medicaid Fraud:– Billing <strong>for</strong> services while abusing,neglecting, exploiting the member– Billing <strong>for</strong> services that never occurred– Double-billing– Billing <strong>for</strong> unnecessary services18
Member/Family/Legal Rep Responsibilities• If Medicaid Fraud is suspected, you mustcontact the Medicaid Fraud Control Unitat:1-888-FRAUD<strong>WV</strong> (1-888-372-8398)(304) 558-1970https://www.wvdhhr.org/oig/mfcu/secRepFrd/• Reports of fraud can be completed via:– Phone– Online reporting <strong>for</strong>m– In writing19
Member/Family/Legal Rep Responsibilities• All people providing services aremandated reporters• If abuse/neglect is suspected,contact:– Adult Protective Services1-800-352-6513– Child Protective Services1-800-352-6513– Local County <strong>DHHR</strong> Office20
Member Grievance/Complaints• Members/Legal Representativeshave the right to access theMedicaid Fair Hearing processconsistent with state and federallaw21
Member Appeals• If medical eligibility is denied/terminated,APS Healthcare will <strong>for</strong>ward a Notice ofDecision and a Request <strong>for</strong> Hearing <strong>for</strong>m tothe member or their legal representative22
Member Appeals• To appeal, the member/representativemust submit the Request <strong>for</strong> Hearing<strong>for</strong>m to the Board of Review within 90days of receipt of the Notice ofDecision– The applicant may have a psychologicalevaluation completed by a member of theIPN (selected by the member) at theexpense of the Bureau <strong>for</strong> MedicalServices (BMS)23
Member Appeals• If medical eligibility is terminated and themember/representative wishes to continueexisting services throughout the appealprocess, the Request <strong>for</strong> Hearing <strong>for</strong>m mustbe submitted within 13 days (otherwise,services will cease)• When a member/representative chooses topetition the circuit court following the finalappeal decision of a Medicaid Fair Hearing,services being appealed are not continuedwhile petitioning the circuit court24
Member Discharge from Program• Income or assets exceed limits (notfinancially eligible)• Not medically eligible• Voluntary termination• Member is deceased• Failure of member/guardian to complywith policy (assessments, IDTs, homevisits)• Not accessing direct support services <strong>for</strong>180 consecutive days25
Staff <strong>Training</strong>Requirements26
Staff <strong>Training</strong> Requirements• All agency staff (excluding contractedextended professionals) having directcontact with members must meet thequalifications listed below:– Acceptable CIB (<strong>WV</strong> State Policefingerprint CIB initially and then every 3years thereafter)– Acceptable NCIC (Federal fingerprintinitially if applicant has lived out of <strong>WV</strong> inpast 5 years)– Protective Services Record Check (notreq <strong>for</strong> Personal Options)www.wvdhhr.org/bcf27
Staff <strong>Training</strong> Requirements• Continued:– Cannot be on the list of excludedindividuals maintained by the Office ofthe Inspector Generalhttp://exclusions.oig.hhs.gov/– Must be over the age of 18– Must have the ability to per<strong>for</strong>m thetasks28
Staff <strong>Training</strong> Requirements• Documentation of training initially andannually as mandated by OHFLACincluding:– Treatment policies and procedures– Consumer Rights– Emergency Procedures, such as CrisisIntervention and restraints– Emergency Care to include Crisis Plansor Emergency Disaster Plans– Infectious Disease Control29
Staff <strong>Training</strong> Requirements• Continued:– Heimlich maneuver– Cardiopulmonary Resuscitation (CPR) throughthe American Heart Association (AHA) orAmerican Red Cross (ARC)– First Aid through the American HeartAssociation (AHA) or American Red Cross(ARC)– Member-specific needs (including specialneeds, health and behavioral health needs)– Recognition, documentation, and reporting ofsuspected abuse/neglect and exploitation– Agency staff who function as ApprovedMedication Assistive Personnel (AMAP) musthave high school diplomas or the equivalent andbe certified AMAPs30
Individual Program Plan (IPP)/Interdisciplinary Team (IDT)Meeting31
IPP/IDT• At a minimum, the IDT consists of:– The member– The legal representative and/orParticipant-Directed representative, ifapplicable– The member’s Service Coordinator– Representatives of all I/<strong>DD</strong> <strong>Waiver</strong>agencies/providers that provide services<strong>for</strong> the individual– A Medley Advocate if the member is aMedley Class Member32
IPP/IDT• Other team members may include:• Professionals:– Therapeutic Consultant (TC)– Behavior Support Professional (BSP)– Registered Nurse (RN)– Physical Therapist– Occupational Therapist– Speech Therapist– Registered Dietician33
IPP/IDT• Continued:• Direct Service <strong>Providers</strong>:– Day Habilitation providers– Person-Centered Support workers– Respite providers– Supported Employment providers– LPNs (when the member receives 8hours or more nursing in one day)34
• Continued:IPP/IDT– Service providers from other systems such as:the local education agency/public schools,Division of Rehabilitation Services (DRS), orBirth to Three (provided that no duplication ofservice exists)– Family Based Care Specialist (when memberresides in a Specialized Family Care Home)– Advocate (when applicable)– Involved parties such as: friends, extendedfamily, the representative payee and theindividual’s significant other35
IPP/IDT Meetings• Initial IPP: Developed within 7 days ofintake• 30-day IPP: Plan is finalized within 30 daysof intake• Transfer IPP: Member transfer from oneSC agency to another• Critical Juncture IPP: When there is asignificant change in the member’s life• Annual IPP: Annual plan with IDT reviewsevery 90 days (or 180 with team approval)36
Anchor Date• Formerly known as ―fixed date‖• Start date of the service year• IPP meeting will need to be within 30days prior to Anchor Date• For new members, this will be the firstday of the month after medicaleligibility is established37
Anchor Date• BMS has approved up to a 9-monthextension on eligibility dates• This will allow APS to align currentmembers’ fixed IPP dates witheligibility dates• This will be the ―Anchor Date‖ <strong>for</strong> allexisting members38
IPP/IDT• The 60-day window inwhich to conduct AnnualIPPs has been reducedto the 30 days prior tothe Anchor IPP date• Example: If the AnnualAnchor date is July 1,then the Annual IPPmeeting must beconducted betweenJune 1 st and July 1 st39
IPP/IDT• If unavoidable circumstances preventthe IDT from meeting and developingthe annual IPP prior to date due, theSC may request to continue servicesfrom the existing plan• APS Healthcare must approve any―Requests to Continue Services‖ (<strong>WV</strong>-BMS-I/<strong>DD</strong>-12) and must include aspecific end date40
IPP/IDT• If the member chooses self-directedservices, the monthly spending planmust be attached to the IPP whenthe monthly spending plan isavailable• IPP must have a direct correlationbetween the assessments and theISP– Assessed needs must be addressed41
IPP/IDT• Services purchased/provided must be:–Based on assessed need–Agreed upon by the IDT–Included in the IPP42
Service Delivery Models:1. Traditional2. Participant-Directeda. Agency with Choiceb. Personal Options43
Service Delivery Model• Member may choose to changeservice delivery models at any timethroughout the service year– This must be indicated on the I/<strong>DD</strong>-2Freedom of Choice Form• Member may also change from anyservice delivery model to another• Ex. – Traditional/Personal Options →Traditional/AwC• or Traditional/Personal Options →Traditional44
I/<strong>DD</strong>-2 Freedom of Choice• Traditional: Traditional Services are providedthrough an agency (The Agency employs/managessupport staff)• Traditional and Agency with Choice: Theagency and member (or representative) comanagessupport staff - the agency providesFinancial Management Services (FMS)• Traditional and Personal Options: Member (orrepresentative) is responsible to manage supportstaff - <strong>WV</strong>’s contracted Fiscal/Employment Agentserves as the FMS• I am unable to choose at this time: Memberautomatically defaults to current service deliverymodel45
Traditional Service Delivery Model• The Provider agency has theresponsibility to secure, hire,discipline, manage, set work scheduleand set wages <strong>for</strong> staff• Provider agency is responsible <strong>for</strong>making sure staff have requiredcredentials/ training• Staff are employees or contractors ofthe Provider agency46
Traditional Service Delivery Model• The way services have been provided(with or through an approved I/<strong>DD</strong><strong>Waiver</strong> Provider agency) isconsidered the ―Traditional ServiceDelivery Model‖• All services (except ParticipantdirectedGoods and Services) areavailable under this model47
Participant-Directed• Participant-Direction is a person-centeredservice delivery system where individuals havegreater choice and control over the servicesthey receive and the individuals who providethem• Members will have options to exerciseemployer authority and/or budget authority– Employer Authority: Control over theParticipant-Directed Services and theindividuals and organizations who provide them– Budget Authority: Control over how theparticipant-directed portion of the budget isspent48
Participant-Directed• Participant-Directionincreases choice andcontrol but alsoincreasesresponsibility• Members may directtheir own serviceswith or without theassistance of a legalor non-legalrepresentative49
Participant-Directed• All program members will have theopportunity to direct their services withthe following exceptions:– Participant-Directed Services will not beavailable to individuals living in OHFLAClicensed residential settings– Individuals and/or their representativesthat do not follow policies/procedurespertaining to Participant-DirectedServices may be required to return to thetraditional option <strong>for</strong> service delivery50
Participant-Directed• Only the following services may beParticipant-Directed:–Transportation–Person Centered Support Services–Respite Care–Goods & Services (PDGS)• To access PDGS, the member mustalso access at least one other type ofPDS during the budget year – i.e.PCS, Respite, and/or Transportation51
Participant-Directed• There are two Financial ManagementService (FMS) models available to supportthe use of Participant-Directed Services:– Agency with Choice (AwC)• The I/<strong>DD</strong> <strong>Waiver</strong> provider serves as the fiscal agentand is the employer of record• The member and/or their legal representative alongwith the AwC provider have a co-employer relationship– Personal Options• The personal options vendor serves as the fiscalagent and the member serves as the employer ofrecord52
Agency with Choice• Under this model, the provider and themember/legal representative enterinto a co-employer arrangement• The provider is the primary employerof record, while the member/representative is the secondary ormanaging employer of the member’squalified support workers53
I/<strong>DD</strong> <strong>Waiver</strong> Traditional andParticipant-Directed ServiceDelivery Model Crosswalk54
Public Partnerships, LLC<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong>Personal Options55
About Public Partnerships, LLC• PPL is the largestprovider of financialmanagement services <strong>for</strong>self direction in the US• PPL was founded in 1999to focus exclusively onthe financial andmanagement operationsof participant-directedservices.• PPL manages payrollservices <strong>for</strong> 40,000participant-directedemployees.PPL has contracts in 20states & the District ofColumbia serving about36,000 individuals with avariety of needs56
Public Partnerships in West VirginiaSince February, 2007 PPL has beencontracted by the <strong>WV</strong> Bureau <strong>for</strong> MedicalServices to provide Financial ManagementServices (FMS) and Resource Consultantservices <strong>for</strong> the Aged and Disabled <strong>Waiver</strong>(ADW) program.The ADW Personal Options program hasgrown from 15 participants in July, 2007 to875 participants in July, 2011. (18% ofactive ADW members.)57
Public Partnerships in West Virginia• Resource Consulting– In<strong>for</strong>mation and Assistance– Employer & Employee Enrollment– Assisting in Spending Plan Development– Monitoring and Reporting• Fiscal/Employer Agent Services– Accounting– Verification of Provider/Vendor Qualifications (CPR, CBC)– Payroll– Accounts Payable– Tax Services– Reporting• Customer Service58
<strong>WV</strong> I<strong>DD</strong> <strong>Waiver</strong> Personal Options Services• Person-Centered Supports• Respite• Transportation• Participant-Directed Goods andServices (PDGS)59
Participant-Directed Goods and ServicesParticipant-Directed Goods andServices (PDGS) are services,equipment or supplies not otherwiseprovided through the <strong>Waiver</strong> programor through the Medicaid State Planthat address an identified need in theIPP.60
Participant-Directed Goods and Services• Limited to $1,000 per member’s IPP year incombination with Traditional EnvironmentalAccessibility Adaptations- Vehicle and Home andParticipant-Directed Goods and Services-AwC• To access PDGS the member must also access atleast one other type of participant-directed serviceduring the budget year—i.e. PCS, Respite and/ortransportation• PDGS cannot be accessed as a means ofreimbursement <strong>for</strong> items or services that havealready been obtained and not been pre-approvedby the Personal Options F/EA61
Benefits of Directing Your Own Services• Budget Authority– You decide how to spend your participantdirectedbudget– No unit caps on Transportation, PCS or Respite• Employer Authority– You hire and train your own workers– You determine your workers’ schedules andwork hours– You decide how much to pay your workerswithin a range of minimum wage to the Medicaidrate <strong>for</strong> the service (i.e. PCS and Respite =$7.25 - $9.88 per hour)62
Personal OptionsWhat have youheard aboutdirecting your ownservices?63
ResponsibilitiesRUMORYou won’t be able tohandle theresponsibilities ofdirecting your ownservices.FACTPPL will assign aResource Consultant toassist you with yourresponsibilities.You may also appoint arepresentative to helpyou with yourresponsibilities.64
ResponsibilitiesRUMORIf you make a mistakedirecting your ownservices, you couldlose your <strong>Waiver</strong> slot.FACTIf you experiencedifficulties directingyour own services, youwill not lose your slot.PPL may recommendthat you appoint arepresentative ortransfer back totraditional services.65
Access to Participant-Directed ServicesRUMORYou can only accessparticipant-directedservices if you’reunable to obtainservices through atraditional serviceprovider.FACTParticipant-directedservices are availableto all I/<strong>DD</strong> <strong>Waiver</strong>members except thosethat live in homeslicensed by OHFLAC.66
Access to Participant-Directed ServicesRUMORYou may not direct yourown services if you areunder 18 years of ageor an adult with a legalrepresentative.FACTAny I/<strong>DD</strong> member mayself-direct except <strong>for</strong>those living in alicensed home.Some members mayrequire the assistanceof a representative.67
Changing Service ModelsRUMORIf you change to aparticipant-directedservice model youwon’t be allowed toreturn to the traditionalservice model.FACTYou have the right tochange your servicemodel at any time and<strong>for</strong> any reason.Your ServiceCoordinator and PPLwill assist you with thetransition to preventgaps in service.68
BenefitsRUMORIf you choose to directyour services you willlose your benefits—i.e.SSI.FACTThe service model youchoose does not impactyour benefits.Your workers’ wagesmay impact theirbenefits but the same istrue <strong>for</strong> workersemployed by traditionalservice providers.69
BudgetsRUMORIf you choose to directyour own services, yourindividualized budgetamount will bedecreased.FACTYour individualizedbudget amount is notaffected by the servicemodel you choose.Directing your ownservices does not alteryour ability to negotiatethe amount of yourindividualized budget.70
BudgetsRUMORIf you choose to directyour own services, youwill receive cash <strong>for</strong>your participantdirectedbudget.FACTPersonal Optionsparticipants do notreceive cash. Theyexercise budgetauthority over anannual participantdirectedbudget.71
Hiring WorkersRUMORIf you choose to directyour own services, youwill not be allowed tokeep your existingworkers.FACTYou may hire yourexisting ResidentialHabilitation, AdultCompanion andRespite workers if theychoose to work <strong>for</strong> youand meet allqualifications.72
Hiring WorkersRUMORIf you choose toPersonal Options, yourworkers will beemployees of PPL.FACTWorkers are employedby the programmember. PPL acts asthe ―agent of theemployer‖ <strong>for</strong> payrolland tax purposes.73
Hiring WorkersRUMORIf you choose toPersonal Options, yourlegal guardian will nolonger be allowed to bepaid <strong>for</strong> providingservices to you.FACTLegal guardians are notrestricted from beingpaid workers.Only under certaincircumstances and withsafeguards may aparticipant’s appointedrepresentative also bea paid worker.74
Hiring WorkersRUMORYour workers’ hoursand wages will be cut ifthey choose to work <strong>for</strong>you instead of working<strong>for</strong> a traditional provideragency.FACTPersonal Optionsservices are not subjectto the caps ontraditional services.You decide yourworkers’ wages/hours.May work more than 40hours but not eligible<strong>for</strong> overtime pay.75
TaxesRUMORIf you direct your ownservices, your workerswill have to pay moretaxes.FACTYour workers’ taxes willnot increase unless youchoose to pay a higherwage or increase theirhours.76
Traditional SupportsRUMORIf you choose to directyour own services, youwill lose the support ofyour ServiceCoordinator and/orTherapeuticConsultant.FACTSelf-directing membersmay continue to accessall traditional servicesincluding ServiceCoordination andTherapeuticConsultant.77
Where do you start?To begin directing your ownservices you must first complete aFreedom of Choice <strong>for</strong>m which isavailable through your ServiceCoordinator, APS Healthcare orthe Bureau <strong>for</strong> Medical Services(BMS).78
Where do you start?• Once you choose the Personal OptionsFMS Model, you will be referred to PPL andone of our staff will contact you to providein<strong>for</strong>mation, answer questions and in<strong>for</strong>myou of the enrollment process.• If during the enrollment period you changeyour mind about Personal Options, you onlyhave to complete a new Freedom of Choice<strong>for</strong>m indicating you wish to remain in theTraditional model.79
Where do you start?• Next, you must hold an IDT meeting– Annual Team Meeting– Critical Juncture Meeting• At the meeting you will choose thetypes and amounts of traditional andparticipant-directed services that arenecessary to meet your assessedneeds.80
Where do you start?• Following the team meeting, yourService Coordinator will submit yourrequested services to APS Healthcare<strong>for</strong> review and authorization.• Once your participant-directed budgethas been authorized by APSHealthcare, you will meet with a PPLResource Consultant to completeemployer/employee enrollment and todevelop your spending plan.81
Employer & Employee Enrollment• Your Resource Consultant will provide youwith an Employer Packet and an EmployeePacket which contain all the <strong>for</strong>msnecessary <strong>for</strong> you to begin directing yourservices and hiring your workers.• During your initial meeting, your ResourceConsultant will provide training andassistance regarding the completion ofEmployer/Employee packets.82
Spending Plan• Your spending plan identifies thetypes and amounts of participantdirectedservices that you choose tomeet your needs.• The spending plan also identifies thewage you choose to pay each of yourworkers so that you can see exactlyhow your participant-directed budgetwill be used.83
Paperwork• Each of your workers will be requiredto submit to PPL a timesheet andtransportation invoice <strong>for</strong> the servicesprovided to you during each payperiod.• If you receive Therapeutic Consultantor Behavior Support Professionalservices, your workers may also berequired to document trainingactivities.84
Ongoing Support• Your PPL Resource Consultant will contactyou each month to ensure your spendingplan continues to meet you needs• A “Family Friendly Report” will be madeavailable to you each month so you can seehow your budget is being spent• PPL’s web portal allows you to access yourin<strong>for</strong>mation at all times• Electronic time sheets and transportationinvoices prevent errors and delays inworkers’ paychecks85
Satisfaction• PPL strives to ensure participants are verysatisfied with their financial managementand Resource Consultant services.• Participant satisfaction is measured andmonitored by BMS on a regular basis.• PPL offers a toll-free Customer Servicenumber <strong>for</strong> participants and their workers.• A <strong>for</strong>mal grievance procedure is available<strong>for</strong> participants that want to file a complaintregarding PPL’s services.86
For More In<strong>for</strong>mationIf you have questions or wish torequest additional in<strong>for</strong>mation, pleasecontact PPL:– Public Partnerships, LLC, 601 EastBrockway Avenue, Morgantown, <strong>WV</strong>26501– Email: pplwvidd@pcgus.com– Phone: 1-877-908-175787
I/<strong>DD</strong> <strong>Waiver</strong> General Changesand Available Services88
Psychologist In<strong>for</strong>mation• New services do not include a code<strong>for</strong> Psychologists to participate in IPPs• Psychologists can continue toparticipate in IPPs (by billing thePsychologist IPP code only) throughthe remainder of the member’s serviceyear, if noted on the member’s currentIPP by billing the remaining units ofIPP Development-Psychologist89
General Service Changes• Annual and triennial psychologicalevaluations previously completed by thepsychologist are eliminated– A member may have psychological evaluations,if needed, completed by accessing the StatePlan– The IPN Psychologist will complete IndependentPsychological Evaluation <strong>for</strong> initial eligibilitydetermination by the MECA– APS will complete functional assessmentannually <strong>for</strong> re-eligibility determination by theMECA90
General Service Changes• Person-Centered Support ServicesReplaces:– Agency Residential Habilitation– Community Residential Habilitation– Adult Companion– Community-Based Day Habilitation• Facility Day Habilitation is a separate code• Day services are no longer required <strong>for</strong>adults• Members may receive up to 416 units/104hours annually of Physical Therapy,Occupational Therapy and Dietary Therapycombined91
General Service Changes• Nursing Changes:– RNs and LPNs are allowed to bill <strong>for</strong>travel time to ISS/Group Homes andlicensed day program sites in order toper<strong>for</strong>m medication administrationactivities only– Annual Nursing Assessments are nolonger required92
All Direct Care Services (excluding Respite) underthe Traditional Service Option-Combined• Members in Natural Family/SpecializedFamily Care Home Settings eligible <strong>for</strong>public education may receive a max of11,680 units/2,920 hours annually (averageof 8 hours per day)• Members in NF/SFCH setting not eligible<strong>for</strong> public education may receive a max of17,520 units/4,380 hours annually (averageof 12 hours per day)• Members in an ISS or GH setting mayreceive a max of 35,040 units/8,760 hoursannually (average of 24 hours per day)93
All Direct Care Services (excluding Respite) underthe Traditional Service Option-Combined• Public Education Services aredefined as school services <strong>for</strong>students through the end of the schoolyear when the student turns twentyone(21) years of age or the studenthas met graduation requirements <strong>for</strong> astandard high school diploma asdefined by the Individuals withDisabilities Education Act (IDEA) and<strong>WV</strong> policy 241994
Behavior Support Professional• Oversees all areas of Positive BehaviorSupport services:– Develops Positive Behavior SupportPlans, Protocols and Guidelines– Assesses and evaluates behavioral datato monitor the effectiveness of thePositive Behavior Support Plan– Trains providers to implement PositiveBehavior Support Plans95
Behavior Support Professional• Continued:– Develops methodology <strong>for</strong> interventionwith the member– Presents proposed restrictive measuresto the agency’s HRC if no otherprofessional is presenting the samein<strong>for</strong>mation– Attends and participates in IDT meetingsand annual functional assessments– Member may have only one BehaviorSupport Professional96
Behavior Support Professional• 960 units/240 hours annually incombination with Therapeutic ConsultantServices• Member is limited to one BSP or TC ifreceiving all services from a single provider• If member receives direct care servicesfrom more than one I/<strong>DD</strong> <strong>Waiver</strong> provider,the member/legal representative isresponsible <strong>for</strong> choosing which provider willprovide BSP services (if applicable)97
Behavior Support Professional• BSP Staff Qualifications:– Bachelor of Arts (BA) or Bachelor ofScience (BS) degree in humanservices field –and-– Two years experience in the I/<strong>DD</strong> field–and-– Documented evidence of enrollment inthe Applied Positive Behavior Support(APBS) standards of practicecoursework/training98
Behavior Support Professional• Board Certified Assistant Behavior Analyst(BCaBA) Certificate –and-:– Bachelor's degree –and-– One year experience working with individuals withI/<strong>DD</strong> –and-– Completion of the <strong>WV</strong>-APBS Network’s three houroverview of Positive Behavior Support• Board Certified Behavior Analyst (BCBA)Certificate-Master's degree –and-:– One year experience working with individuals withI/<strong>DD</strong> –and-– Completion of the <strong>WV</strong>-APBS Network’s three houroverview of Positive Behavior Support99
Provider Agency ApplicationProcess <strong>for</strong>Positive Behavior Support (PBS)<strong>Training</strong> Approval100
PBS <strong>Training</strong> Development and Approval• Behavior Support ProfessionalServices provisionally (pertains tothose who currently provide BS orBA):– Enrollment Application: serves asletter of intent indicating how the agencyintends to meet qualifications <strong>for</strong> theirstaff to provide Behavior SupportProfessional• This application should be submitted to APSHealthcare101
PBS <strong>Training</strong> Development and Approval• To meet qualifications, agenciesmust either:– Submit training and receive approval of<strong>WV</strong>APBS Network– Have staff trained by another agencywhose PBS training was approved(enrolled/completed by timeline set inmanual-6 months)– Have staff enrolled in training <strong>for</strong>completion of Board Certified Analyst orBoard Certified Assistant BehaviorAnalyst credential102
PBS <strong>Training</strong> Development and Approval• Complete the Application <strong>for</strong> PositiveBehavior Support <strong>Training</strong> Approval(Questionnaire and Review Tools)• Submit the application and all parts of PBStraining electronically:wvapbs@gmail.com103
PBS <strong>Training</strong> Development and Approval• Upon review by the <strong>WV</strong>APBS Leadershipteam the application and an approval ordenial letter will be returned to you inelectronic <strong>for</strong>mat (This must be maintained<strong>for</strong> agency records)• <strong>Providers</strong> are responsible <strong>for</strong> maintainingtraining records• <strong>WV</strong> APBS Network has acceptedresponsibility of approving developedcurriculums104
Positive Behavior Support in <strong>WV</strong>• The provisional qualification processis the first step toward a unifiedapproach to positive behavior supportpractice in West Virginia• All providers are encouraged topursue the Positive Behavior SupportEndorsement when it becomesavailable105
Positive Behavior Support in <strong>WV</strong>• The <strong>WV</strong> Statewide Positive BehaviorSupport Endorsement process iscurrently being developed by the <strong>WV</strong>APBS Network and its affiliates withimplementation expected by 2015106
Behavior Support Professional• Develops skills and maladaptivebehavior training programs– Trains direct care employees– Develops positive behavior support plans– Develops adaptive behavior plans• Active treatment is not a requirementin services, however, assessed needsmust be addressed in the IPP– The need <strong>for</strong> active treatment is stillrequired <strong>for</strong> ICF/MR and <strong>Waiver</strong> eligibility107
Behavior Support Professional• Member must require this level of support– Member must currently exhibit maladaptive behaviors sosevere that the adaptive functioning and ability to receiveadaptive training is limited or impossible unlessmaladaptive behaviors are reduced or eliminated –or-– Member may have a history of behaviors beyond oneyear that have resulted in severe life threateningsituations such as fire setting or arson or sexual assault oroffending behaviors that result in bodily harm to others orself• Members have the option to receive in<strong>for</strong>malhabilitation programming through natural supports• Limit: 240 hours per IPP year combined withTherapeutic Consultant108
Behavior Support Professional:Individual Program Planning• Replaces the <strong>for</strong>merIPP Developmentcode• Limited to 4 eventsper member’s serviceyear• Must be presentduring the IPPmeeting in order to bill(attending by phone isnot billable)109
Crisis Services• Under emergentcircumstances, whichplace the member’s orothers’ health and safetyat risk, crisis service maybe immediatelyimplemented without priorauthorization up to amaximum of 72 hours• 2:1 staff/member ratio• Limit: 336 hours/IPP year110
Dietary Therapy• Nutritional assessment and therapy<strong>for</strong> diseases that have a nutritioncomponent– Preventative health and diet assessment– Weight management• Limit: 104 hours/IPP year combinedwith Physical Therapy andOccupational Therapy111
Electronic Monitoring• Oversight and monitoring within the residentialsetting through off-site electronic surveillance• Unit = 1 Hour• Service may be provided in the adult member’sfamily residence, a licensed group home and inany ISS• All systems or companies used or contracted bythe I/<strong>DD</strong> <strong>Waiver</strong> provider must meet the standardsset by BMS• Must be pre-approved by BMS be<strong>for</strong>e providingany services112
Electronic Monitoring• Any member wishing to access thisservice must first be assessed andapproved by the I/<strong>DD</strong> <strong>Waiver</strong> provider’sHuman Rights Committee (HRC)• The approval of the HRC must bedocumented and attached to themember’s IPP• SC must conduct a home visit thatincludes a programmatic review of thesystem, as well as, a drill at 7 days ofimplementation, again at 14 days, and atleast quarterly thereafter (in addition to thenormal required monthly home visit)113
Electronic Monitoring• The I/<strong>DD</strong> <strong>Waiver</strong> provider has standbyintervention staff who meet thefollowing standards:– Responds by being at the member’sresidential living site within 20 minutes orless from the time an incident is identifiedby the remote staff and the stand-by staffacknowledges receipt of the notificationby the remote staff– The IDT has the authority to set a shorterresponse time based on individualmember needs114
• Continued:Electronic Monitoring– Assists the member in the home asneeded to ensure the urgent need/issuethat generated a response has beenresolved– Each time an emergency response isgenerated, an incident report must besubmitted to the West Virginia IncidentManagement System (<strong>WV</strong> IMS) by theI/<strong>DD</strong> <strong>Waiver</strong> provider115
Electronic Monitoring• May not be used in Specialized FamilyCare Homes• Must be approved by BMS• May not be used to monitor direct carestaff• May not be billed at the same timeany other direct care service is billed<strong>for</strong> a member116
Environmental Accessibility Adaptation: Homeand/or Vehicle• Environmental AccessibilityAdaptations are physical adaptations tothe home or vehicle• Must be documented on the member’sIPP• To maximize the member’s accessibilityto the home or vehicle117
Facility-Based Day Habilitation• Structured program that uses meaningful andproductive activities designed to promote theacquisition of skills or maintenance of skills<strong>for</strong> the member outside the home• Limit: 6,240 units or 1560 hours/IPP year• Staff to member ratios <strong>for</strong> this service are1:1-2, 1:3-4, and 1:5-6• Staff may not be a family member or anyother individual who lives in the member'shome118
Occupational Therapy• Evaluation and training in areasof fine and gross motor–Self care training–Sensory training–Assistance and training <strong>for</strong>adaptive aids• Limit: 104 hours/IPP year combinedwith Physical Therapy and DietaryTherapy119
Participant-Directed Goods and Services• Participant-Directed Goods and Services(PDGS) are defined as services, equipmentor supplies not otherwise provided throughthe waiver and meets the followingrequirements:– An item or service that would decreasethe need <strong>for</strong> other Medicaid servicesand/or increase a member’s safety andopportunities in the community– The member does not have the funds topurchase the item or service or the itemor service is not available throughanother source120
Participant-Directed Goods and Services• Continued:– PDGS are purchased from the Participant-Directed budget– The need <strong>for</strong> PDGS must be documented in theIPP– PDGS must be pre-approved by PersonalOptions or AwC and purchase must bedocumented by receipts or other documentationof the goods or services from the establishedbusiness or otherwise qualified entity orindividual– Member must access at least one other PDS –i.e. Respite, Person-Centered Supports121
Participant-Directed Goods and Services• Limit: 1000 units ($1,000) per IPPyear in combination with TraditionalEnvironmental AccessibilityAdaptations- Vehicle and Home122
Participant-Directed Goods and Services• Examples of exclusions include:– Goods, services or supports covered bythe State Plan, Medicare, other thirdparties,including education, home-basedschooling and vocational services– Goods, services and supports availablethrough another source– Medications, vitamins and herbalsupplements– Personal hygiene items– Refer to I/<strong>DD</strong> Manual <strong>for</strong> a complete list123
Person-Centered Support• Person-CenteredSupport (PCS) servicesconsist of trainingand/or support activitiesthat enable the memberto live and inclusivelyparticipate in thecommunity• PCS combines AgencyResidential Habilitation,Community DayHabilitation & AdultCompanion Services124
Person-Centered Support: Agency• Agency staff may not be any individual wholives in the member's home• Member ratio codes <strong>for</strong> this service are 1:1,1:2, 1:3 and 1:4• PCS: Agency is not available while themember is hospitalized (except when thebehavioral needs of the member arise due tothe temporary to change in environment)• PCS: Agency is not available in nursinghomes, psychiatric hospitals or rehabilitativefacilities125
Person-Centered Support: Family• Must be a family member (excludingspouse) who lives in the member's home ora Specialized Family Care providerdelivering the service in a SFC home• Person-Centered Support (PCS) servicesconsist of training and/or support activitiesthat enable the member to live andinclusively participate in the community• 1:1 and 1:2 are the only codes available inthe member’s family residence and inSpecialized Family Care Homes126
Person-Centered Support: Limitations• PCS (all types)–Not available in nursing homes,psychiatric hospitals orrehabilitative facilities127
Physical Therapy• Screening, assessment and treatmentdesigned to preserve and improve yourindependence– Gross and fine motor skills– Range of motion– Strength– Muscle tone• Limit: 104 hours/IPP year combinedwith Dietary Therapy and OccupationalTherapy128
Respite• Designed to provide assistance/relief to theprimary caregiver• Not available in medical hospitals, nursinghomes, psychiatric hospitals or rehabilitativefacilities• Ratios <strong>for</strong> this service are 1:1, 1:2, and 1:3• Only 1:1 or 1:2 ratios are allowed to be utilizedin a member’s family residence or in aSpecialized Family Care Home• Limit: 1,728 hours/IPP year129
Respite: Crisis Site• Respite: Crisis Site Services are to providetemporary substitute care <strong>for</strong> an individualwho is in need of an alternative residentialsetting due to behavioral needs or lack ofsupports• 30 day maximum stay• May only be provided in BHHF Crisis sites• Under emergent circumstances which placethe member’s or others’ health and safety atrisk, crisis services may be immediatelyimplemented without prior authorization up toa maximum of 72 hours130
Service Coordination• Designed to ensure accessibility, accountability andcontinuity of support and services• Per<strong>for</strong>m the same function <strong>for</strong> all of their members,regardless of which service delivery model themember chooses• Present member’s proposed restrictive measures tothe Human Rights Committee if no other professionalis presenting the same in<strong>for</strong>mation• Comply with reporting requirements of the <strong>WV</strong> IMS• Participate in annual functional assessments131
Service Coordination• Limit: 872 units/IPP year• Up to 4 units of Service Coordination permonth per member served may be billed toreview provision of services in order toverify the member receives services asindicated on the IPP and within programparameters• There is no longer a monthly cap• There is no IPP Development code(attending the IDT is regular SC code –Units were increased from 840 to cover devcode)132
Service Coordination• Service Coordination cannot be billed<strong>for</strong> the entire calendar month if ahome visit did not occur within thatcalendar month (unless exceptionapproved in advance by APSHealthcare and documented on <strong>WV</strong>-BMS-I/<strong>DD</strong>-12)133
Skilled Nursing• Licensed Practical Nurse: monitoring, directnursing care, etc.– More than two hours/day requires priorauthorization and that the nurse provide direct-caresupport– Max of 11,680 units/2920 hours (Average 8hours/day) can be prior authorized– May bill travel time to/from ISS, GH, licensed DHsite only to administer medication• Registered Nurse: nursing services outsidethe scope of an LPN– Max of 120 hours/year can be prior authorized– IPP Planning: may bill to attend team meetings134
Speech Therapy• Screening, assessment and directintervention to improve speech andhearing disabilities• 96 units/events per year <strong>for</strong> membersbelow age 24• 48 units/events per year <strong>for</strong> membersage 24 and over135
Supported Employment• Services that enable the member toengage in paid, competitiveemployment, in integrated communitysettings• Limit: 8,320 units/2,080 hours/IPPyear• This limit is combined with other directcare services available through theTraditional Option136
Therapeutic Consultant• Develops training plans and providestraining in the person-specific aspects andmethod of a plan of intervention orinstruction to the primary care providers• Skills Specialist = Therapeutic Consultant• Behavior Specialist, Behavior Analyst,Behavior Analyst Psychologist = BehaviorSupport Professional if enrolled in a <strong>WV</strong>APBS Network approved curriculum137
Therapeutic Consultant• Active treatment is not a requirement;however, assessed training needsmust be addressed in the IPP• Members have the option to receivein<strong>for</strong>mal habilitation programmingthrough natural supports• Limit: 960 units/240 hours incombination with BSP per IPP year138
Therapeutic Consultant:Individual Program Planning• Member is allowed 2 TherapeuticConsultants (if from differentagencies)• 4 events per member’s service year• More than one Therapeutic Consultantmay bill <strong>for</strong> this service during an IDTmeeting, however there is still anannual limit of 4 events139
Transportation Miles• Transport to the site of a planned activity orservice which is addressed on the IPP andbased on assessed need• 9,600 miles annually (average of 800 miles/month)• Non Emergency Medical Transportation may beavailable through the local <strong>DHHR</strong> but cannotduplicate <strong>Waiver</strong> transportation www.wvdhhr.org• The IPP must specify the number of miles perservice– Ex: Up to 100 miles per month shall be used <strong>for</strong>transporting the member to and from their job location140
Transportation Trips• 4 one way trips per day or 874 tripsannually in agency vehicle– Must have original capability to seat atleast 8 but fewer than 16 passengers• The member’s IPP must specify thenumber of trips per service– Ex: Up to 20 trips per month shall beused <strong>for</strong> transporting the member to andfrom his job location141
Administrative Changes• <strong>Providers</strong> will be required to completequarterly self reviews– Submit to Erica Workman ateworkman@apshealthcare.com• <strong>Providers</strong> must submit incidentreports through the <strong>WV</strong> IMSwww.wvdhhr.org/bhhf/waiver/waiver_ims/142
Reporting Requirements• I/<strong>DD</strong> providers must utilize the <strong>WV</strong>IMS to track the types of incidentslisted below:– Simple Incidents– Critical Incidents– Abuse, Neglect and ExploitationIncidents• SCs may bill <strong>for</strong> entering incidentsinto <strong>WV</strong> IMS <strong>for</strong> those members ontheir caseload143
Reporting Requirements• Contact Pat Nisbet <strong>for</strong> IncidentManagement System username andpassword assistancePatricia.S.Nisbet@wv.gov144
Transition Plan145
Transition Plan• A Crosswalk has been developed toassociate new rates with old codes• Molina will update their system toallow new rates as of October 1, 2011• This will allow members to continue toaccess services on their current planwithout making changes (but<strong>Providers</strong> can be paid at new rates)146
Transition Plan: ARHCRH• <strong>Providers</strong> who have classifiedcommunity residential habilitation(CRH) providers as agency residentialhabilitation (ARH) providers will needto roll back any unused ARH units toallow appropriate billing throughMolina– Ex: If you have been authorized 100units of ARH and used 60 units, then 40units will need to be rolled back147
Transition Plan: ARHCRH• After rollback of ARH units, SC willneed to purchase CRH units, so thatthe appropriate code/rate will beaccessed through Molina• Applies ONLY to those agencies thathave classified CRH providers asARH providers• Does not require a Critical Juncturemeeting148
Transition Plan: DH• Continue to bill the DH or PV code(s) <strong>for</strong> themember until either the Annual or CriticalJuncture.• Services provided 10/1/2011 and after - Submitthe new rate <strong>for</strong> this code to Molina <strong>for</strong> payment(ex. Code <strong>for</strong> DH 1:1 is T2021U4. Bill T2021U4with a rate of $4.98 per unit• At Annual IPP or Critical Juncture: If the memberis accessing Day Habilitation primarily in thecommunity, this would equate to Person-CenteredSupport• At Annual IPP or Critical Juncture: If the memberis accessing Day habilitation in a facility, thiswould equate to Facility-Based Day Habilitation149
Transition Plan• Members will have the option to staywith the services currently on the IPPuntil their next Annual IPP– With this option, members will bephased-out of the ―old‖ services bySeptember 30, 2012150
Transition Plan• If accessing new services, themember is subject to the newpolicy manual and all applicablerules• At no time should the IPP reflect―old‖ AND ―new‖ services151
Transition Plan• A face-to-face team meeting (CriticalJuncture) must be held <strong>for</strong> thefollowing reasons:– If all team members do not agree onservices that the member receives– If the member receives a brand newservice• Ex: If member has never accessedSupported Employment services be<strong>for</strong>e– If the member requires a greater amountof services than is on the plan (increasein number of units)152
Transition Plan• A face-to-face team meeting (CriticalJuncture) must be held <strong>for</strong> thefollowing reasons:– If the member is going to have a newgoal implemented– If the member chooses to go with aParticipant-Directed option (AwC orPersonal Options)153
Transition Plan• If the member accesses new servicesprior to the expiration of their serviceyear, the Service Coordinator mustroll back current authorizations priorto purchasing new services• Effective October 1, 2011 andgreater, new services will be availableto purchase and old services may nolonger be purchased154
Transition Plan• Only under special circumstances,exceptions to authorizing ―old‖services can be granted after10/01/2011:– Service date must have occurred prior to10/1/2011– IPP start date must have been prior to10/01/2011– Must be deemed an ―exception‖ by APS(cannot be just because provider failedto purchase previously)155
Transition Plan• In summary, members may continueservices on their current plan throughthe remainder of their service yearunless needs change or a CriticalJuncture needs to occur• If they have the need <strong>for</strong> a CriticalJuncture, SC must roll back all auths<strong>for</strong> ―old‖ services and purchase ―new‖services to get through the remainderof the member’s service year156
Purchasing on theCareConnection®157
Purchasing• IDT convenes and identifies allneeded• Services,• <strong>Providers</strong>,• Units and• Supports• SC enters all chosen services inCareConnection®158
Purchasing• Registration Coordinators will reviewservices <strong>for</strong> appropriateness:– Within budget?– Within service limits?– Within program parameters (ex. max #hours/day depending on livingarrangement)?– Has the team met the member’s healthand safety needs?159
Purchasing• Even when the member choosesparticipant-directed services, the totalamounts of services entered in theCareConnection® cannot exceed theliving arrangement maximum directcare units (ex. 8 hrs/day + Respite <strong>for</strong>child)• If PD, the cost <strong>for</strong> these services isbundled and will be considered the―Participant-Directed Budget‖160
Purchasing• The authorizations <strong>for</strong> serviceswill be then be <strong>for</strong>warded to eitherAwC or PPL and either theagency (AwC) or ResourceConsultant (PPL) will contact themember to develop a participantdirectedspending plan• This spending plan will beattached to the member’s IPP161
Purchasing• IDTs must make every ef<strong>for</strong>t topurchase services within themember’s assigned budget• Registration Coordinators cannotexceed service limits whenauthorizing services• Negotiating services in excess of theassigned budget should only be <strong>for</strong>those members identified as ―outliers‖162
Purchasing• Once approved by APS, servicereferrals go to all selected providers• Selected providers eitheraccept/reject service referrals• If accepted, the provider will receivean authorization <strong>for</strong> payment163
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms164
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• Agencies that wish to computerizeany of the <strong>for</strong>ms may do so• The <strong>for</strong>ms cannot be altered and mustbe utilized (if applicable)• It will be required that some <strong>for</strong>ms areuploaded into the CareConnection®165
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-1 Application• <strong>WV</strong>-BMS-I/<strong>DD</strong>-2 Freedom of Choice(Replaces the <strong>DD</strong>-7/7A)– Choice of I/<strong>DD</strong> <strong>Waiver</strong> or ICF/MR– Choice of I/<strong>DD</strong> <strong>Waiver</strong> Service CoordinationProvider– Choice of Service Delivery Model• <strong>WV</strong>-BMS-I/<strong>DD</strong>-3 Monthly/Bi-Monthly SCVisit– One <strong>for</strong>m <strong>for</strong> all Home and/or Day Visits– More narrative than previous version166
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-4 Initial IPP• <strong>WV</strong>-BMS-I/<strong>DD</strong>-5 IPP– Includes Service Delivery Options (Traditional,Participant-Directed)– Meeting minutes– Specific section <strong>for</strong> medications– Service Plan (<strong>Waiver</strong> services and Natural Supports)– Habilitation plan and task analysis are combined– PBS plan– Crisis plan– Participant-directed spending plan (if applicable)– Signature sheet167
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-6 Certificate of <strong>Training</strong>(<strong>for</strong>merly <strong>DD</strong>13)• <strong>WV</strong>-BMS-I/<strong>DD</strong>-7 Direct SupportDocumentation <strong>for</strong> Traditional and AwC– Service Log (documents time spent percode/per staff person)– Direct Support Progress Note (optional andused to identify if something out of theordinary occurs during service provision)– Transportation Log168
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-8 Request <strong>for</strong>Environmental AccessibilityAdaptations (EAA) and Goods &Services (G&S)• <strong>WV</strong>-BMS-I/<strong>DD</strong>-9 Request <strong>for</strong> NursingServices• <strong>WV</strong>-BMS-I/<strong>DD</strong>-10 Transfer/Discharge– Mimics required fields on the CareConnection®when transferring or discharging a programmember169
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-11 Notification ofMember Death• <strong>WV</strong>-BMS-I/<strong>DD</strong>-12 Request toContinue Services -Serves todocument requests <strong>for</strong>:– An eligibility extension– An exception to conducting the monthlySC home visit or day visit– IPP exceptions (outside of timelines,member or legal representativeunavailable)170
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Forms• <strong>WV</strong>-BMS-I/<strong>DD</strong>-13 AnnualFunctional Assessment DataModification Request– Formal request that the ASO modifyin<strong>for</strong>mation collected during themember’s annual functional assessment– All in<strong>for</strong>mation submitted to the ASOmust be in writing, and this <strong>for</strong>m mustbe completed in its entirety prior to theASO considering your request– May only be completed by the memberor the legal representative171
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Contacts172
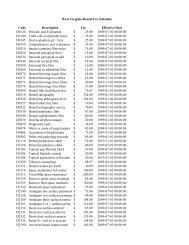
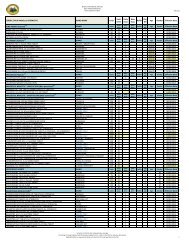
<strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> ContactsSERVICE COMPANY PHONE NUMBER FAX NUMBERI/<strong>DD</strong> ProgramManagerBureau <strong>for</strong> MedicalServices304-356-4904 304-558-4398AdministrativeServicesOrganization(ASO)APS Healthcare, Inc. 866-385-8920 866-521-6882ClaimsProcessingMedical EligibilityContracted Agent(MECA)Fiscal EmployerAgent (F/EA)Personal OptionsMolina MedicaidSolutionsPsychologicalConsultation &Assessment (PC&A)Public Partnerships,LLC (PPL)888-483-0793(<strong>for</strong> <strong>Providers</strong>)304-348-3380(<strong>for</strong> Members)877-902-1206(Help desk)304-348-3380304-776-7230 304-776-7247877-908-1757 304-296-1932173
Wrap Up• Questions/Comments?• Please complete satisfaction surveybe<strong>for</strong>e leaving• Thank you and have a safe trip home!• The Chapter 513 I/<strong>DD</strong> <strong>Waiver</strong>Services Manual can be found athttp://www.dhhr.wv.gov/bms/Pages/default.aspx• <strong>WV</strong> I/<strong>DD</strong> <strong>Waiver</strong> Websitehttp://www.dhhr.wv.gov/bms/hcbs/I<strong>DD</strong>/Pages/default.aspx174