Product Information Sandrena 0.1% gel - Aspen Pharmacare Australia
Product Information Sandrena 0.1% gel - Aspen Pharmacare Australia
Product Information Sandrena 0.1% gel - Aspen Pharmacare Australia
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
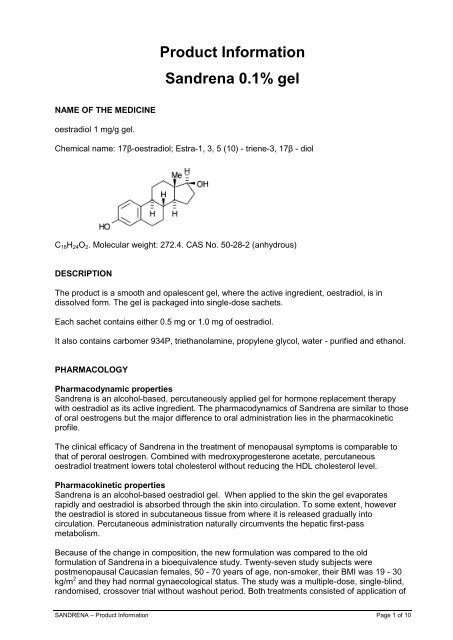
<strong>Product</strong> <strong>Information</strong><strong>Sandrena</strong> <strong>0.1%</strong> <strong>gel</strong>NAME OF THE MEDICINEoestradiol 1 mg/g <strong>gel</strong>.Chemical name: 17β-oestradiol; Estra-1, 3, 5 (10) - triene-3, 17β - diolC 18 H 24 O 2 . Molecular weight: 272.4. CAS No. 50-28-2 (anhydrous)DESCRIPTIONThe product is a smooth and opalescent <strong>gel</strong>, where the active ingredient, oestradiol, is indissolved form. The <strong>gel</strong> is packaged into single-dose sachets.Each sachet contains either 0.5 mg or 1.0 mg of oestradiol.It also contains carbomer 934P, triethanolamine, propylene glycol, water - purified and ethanol.PHARMACOLOGYPharmacodynamic properties<strong>Sandrena</strong> is an alcohol-based, percutaneously applied <strong>gel</strong> for hormone replacement therapywith oestradiol as its active ingredient. The pharmacodynamics of <strong>Sandrena</strong> are similar to thoseof oral oestrogens but the major difference to oral administration lies in the pharmacokineticprofile.The clinical efficacy of <strong>Sandrena</strong> in the treatment of menopausal symptoms is comparable tothat of peroral oestrogen. Combined with medroxyprogesterone acetate, percutaneousoestradiol treatment lowers total cholesterol without reducing the HDL cholesterol level.Pharmacokinetic properties<strong>Sandrena</strong> is an alcohol-based oestradiol <strong>gel</strong>. When applied to the skin the <strong>gel</strong> evaporatesrapidly and oestradiol is absorbed through the skin into circulation. To some extent, howeverthe oestradiol is stored in subcutaneous tissue from where it is released gradually intocirculation. Percutaneous administration naturally circumvents the hepatic first-passmetabolism.Because of the change in composition, the new formulation was compared to the oldformulation of <strong>Sandrena</strong> in a bioequivalence study. Twenty-seven study subjects werepostmenopausal Caucasian females, 50 - 70 years of age, non-smoker, their BMI was 19 - 30kg/m 2 and they had normal gynaecological status. The study was a multiple-dose, single-blind,randomised, crossover trial without washout period. Both treatments consisted of application ofSANDRENA – <strong>Product</strong> <strong>Information</strong> Page 1 of 10
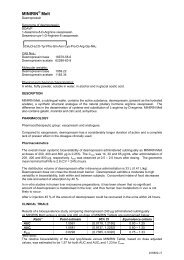
1 gram of the <strong>gel</strong> on a skin area of 400 cm 2 (thigh) once daily for 14 consecutive days. The newformulation was bioequivalent with the old formulation. The estimate for the ratio (the new/theold formulation) of extent of drug absorption, AUC (0-24h) , was 1.05. The associated 90 %confidence interval (89.7 - 123 %) was included within the bioequivalence range of 80 - 125 %.The estimate for the ratio (the new / the old formulation) of the rate of absorption, C max , was1.06. The associated 90 % confidence interval (87.9 - 128 %) was included. The widerconfidence interval for C max was justified because transdermal estradiol can be considered as ahighly variable drug.90% Confidence-intervals of ratio C/A (<strong>Sandrena</strong> new / old formulation)Parameter(meanSD)Formulation C (=new)batch BE036L2A<strong>Sandrena</strong> A (=old)batch BEC16B90% C.I., ratio estimate(log transformed data)AUC (0-24) 2696 2337 2108 890 89.7 – 123 %, 1.05(pmol*h/l)C max (pmol) 157 129 148 118 87.9 – 128 %, 1.06During <strong>Sandrena</strong> treatment the oestradiol/oestrone ratio remains at 0.7, while during peroraloestrogen treatment it usually drops to less than 0.2. The steady state bioavailability of<strong>Sandrena</strong> is 82 per cent compared to the equivalent oral dose of oestradiol valerate.Otherwise the metabolism and excretion of transdermal oestradiol follow the fate of naturaloestrogens.Preclinical Safety DataOestradiol is a natural female hormone with an established clinical use, therefore notoxicological studies have been performed with <strong>Sandrena</strong>. The necessary studies on the irritanteffects of the <strong>gel</strong> have been studied in rabbits and skin sensitisation in guinea pigs. Based onthe results from these studies it can be concluded that <strong>Sandrena</strong> very infrequently could causemild skin irritation. The frequency of the occurrence of dermal irritation can be reduced by dailychange of the application site.CLINICAL TRIALSDifferent adverse reaction rates have been reported with the use of different transdermaloestrogen replacement therapy regimens. Depending on the formulation of the transdermalregimens, <strong>gel</strong> or patch, the rate of skin irritation varies and is considerably lower with the <strong>gel</strong>formulation.In clinical trials with 0.5 - 1.5 g <strong>Sandrena</strong> (0.5 - 1.5 mg oestradiol) 659 women have beentreated for 1 – 2 years. <strong>Sandrena</strong> has been equally effective alleviating climacteric symptoms asoral oestradiol valerate tablets or a transdermal patch. <strong>Sandrena</strong> treatment has also renderedan acceptable bleeding pattern compared with oral or other transdermal regimens.In a clinical trial with 395 women only 3% discontinued the study due to adverse events. Theadverse reaction profile and rate with <strong>Sandrena</strong> has been similar to that of oral and othertransdermal regimens. In clinical trials with <strong>Sandrena</strong> less than 5% of the patients havereported skin irritation while the percentage with the comparative transdermal patch reachedover 30%. The aforementioned studies were, conducted prior to the WHI and Million Womenstudies. [See „INDICATIONS‟ and „DOSAGE AND ADMINISTRATION‟ for recommendedclinical use.]In a large randomised trial involving women who received hormone replacement therapy for anaverage of 5.2 years using conjugated equine oestrogens (0.625 mg/day) continuouslycombined with medroxyprogesterone acetate (2.5 mg/day), adverse effects on cardiovasculardisease and the incidence of breast cancer were observed. The Women‟s Health Initiative studywas designed to investigate the efficacy and safety of long-term hormone replacement therapySANDRENA – <strong>Product</strong> <strong>Information</strong> Page 2 of 10
(HT) in preventing coronary heart disease in healthy postmenopausal women with an intactuterus. The relative risk of coronary heart disease was 1.29 (95% confidence interval 1.02-1.63), corresponding to an increase in the absolute rate from 30 to 37 per 10 000 person-years.The increased risk of breast cancer became apparent after 4 years on study medication. Therelative risk of stroke was 1.41 (1.07-1.85), an increase in the absolute rate from 21 to 29 per 10000 person-years. The relative risk of VTE was 2.11 (1.58-2.82), an increase from 16 to 34 per10,000 person-years. The relative risk of breast cancer was 1.26 (1.00-1.59), an increase from30 to 38 per 10 000 person-years. The study was stopped prematurely because the presetcriterion for invasive breast cancer was fulfilled and a global risk-benefit index supported risksexceeding benefits. In the estrogen only arm global risk-benefit index has not been exceeded,and that arm is continuing. The risks and benefits in women receiving treatment for the shorttermmanagement of climacteric symptoms of oestrogen deficiency or for the management ofpremature menopause were not examined. In a randomised controlled sub group of the WHItrial (referred to as the WHI Memory Study, WHIMS), women of 65 years of age or older(n=4,532, 50% older than 70) treated with conjugated equine oestrogens (0.625 mg/day)continuously combined with medroxyprogesterone acetate (2.5 mg/day) were reported to havea two fold increase in the risk of developing probable dementia. After an average follow up of 4years the absolute risk of probable dementia was 45 per 10,000 in the oestrogen plusprogestagen group compared to 22 per 10,000 in the placebo group.It is unknown if these findings apply to younger postmenopausal women.An observational study of 1,084,110 women, (the Million Women Study) of whom 828,923 werepostmenopausal has shown that, compared to never-users, use of oestrogen-progestagencombined HT is associated with a higher risk of breast cancer (RR=2.00, 95%CI:1.88-2.12)than use of oestrogens alone (RR=1.30, 95%CI:1.21-1.40). In this study the magnitude of theincrease in breast cancer risk was similar for all oestrogen-only preparations, irrespective of thetype, dose or route of administration of the oestrogen (oral RR=1.32, 95%CI:1.21-1.45;transdermal RR=1.24, 95%CI:1.11-1.39 and implanted RR=1.65, 95%CI:1.26-2.16). Likewisethe magnitude of the increased risk was similar for all oestrogen plus progestagen preparations,irrespective of the type of progestagen or the number of days of addition per cycle(sequential
1.6), respectively. Estimated risk for VTE in current users of oral oestrogen replacement therapycompared with transdermal oestrogen replacement therapy users was 4.0 (95% CI 1.9-8.3).These results may be interpreted as meaning that (i) the higher risk of VTE as shown in theWHI study has been further supported for oral therapy; and (ii) current use of oral oestrogen butnot transdermal oestrogen or past use was a risk factor for VTE. Use in the first year was alsomore risky than later use, a finding that is also consistent with the WHI study.If prescribing HT, the potential for increased cardiovascular, thrombotic and neoplastic adverseevents, and an increased incidence of probable dementia in older women, must also beconsidered as part of the risk-benefit assessment. Breast cancer can be fatal. Hormonetreatments should not be used for the long-term maintenance of general health, including theprimary prevention of cardiovascular disease.INDICATIONSShort-term treatment of climacteric symptoms after natural or surgical menopause. Whereverpossible the lowest effective dose should be used.Review the need for continuation of treatment after 6 months, taking into account the risk-benefitratio for the individual user at that moment (including cardiovascular disease and breast cancer,refer Clinical Trials and Precautions). <strong>Sandrena</strong> should only be continued for as long as thebenefit outweighs the risks.CONTRAINDICATIONS Undiagnosed vaginal bleeding. Cerebrovascular disorders, active or recent thromboembolic diseases or thrombophlebitis,severe hepatic disease (including Dubin Johnson and Rotors' syndrome), malignancy of thegenitals or breasts, pregnancy, non hysterectomised women without concomitantprogestagen. Hypersensitivity to the constituents of the preparation.PRECAUTIONSThe benefits and risks of hormone treatment, including <strong>Sandrena</strong> must always be carefullyweighed, including consideration of the emergence of risks as therapy continues. <strong>Sandrena</strong>should be used for the shortest duration consistent with treatment goals. The need forcontinued treatment should be reviewed after 6 months. <strong>Sandrena</strong> should only be continued foras long as the benefit outweighs the risks.Do not use in combination with a progestagen in hysterectomised women.Coronary Artery DiseaseHormone treatment should not be initiated or continued to prevent or treat cardiovasculardisease. There is no evidence from randomised controlled trials of cardiovascular benefit withcontinuous combined conjugated oestrogens and MPA. Large clinical trials showed a possibleincreased risk of cardiovascular morbidity in the first year of use and no benefit thereafter. Forother HT products there are only limited data from randomised controlled trials examiningbenefit in cardiovascular morbidity or mortality. Therefore it is uncertain whether these findingsalso extend to other HT products.SANDRENA – <strong>Product</strong> <strong>Information</strong> Page 4 of 10
Some conditions may be aggravated during oestrogen therapy. Women on oestradiol treatmentwith one of the following conditions (or with a history thereof during previous pregnancy orhormone use) should therefore be closely monitored. These conditions include: mildhypertension, migraine or severe headache, benign breast disease, liver function disturbances,cholestasis, cholelithiasis, diabetes mellitus, asthma, otosclerosis, multiple sclerosis,galactorrhea, elevated prolactin levels, history of herpes gestationis and epilepsy.Check the following before useBefore therapy is initiated, a complete gynaecological examination should be performed andrepeated at least once a year in long-term replacement therapy. A careful appraisal of the risksand benefits should be undertaken before use and after 6 months, and <strong>Sandrena</strong> should onlybe continued as long as the benefit outweighs the risk.Carcinogenicity/mutagenicitySupraphysiological doses of oestradiol have been associated with the induction of tumours inoestrogen-dependent target organs in all rodent species tested. The relevance of these findingswith respect to humans has not been established. Unopposed oestrogen therapy is associatedwith an increased incidence of endometrial carcinoma, particularly with prolonged use.Concurrent progestagen therapy for a minimum of 12 to 14 days reduces the risk of endometrialhyperplasia, (see „DOSAGE AND ADMINISTRATION’). Usually, a withdrawal bleed resemblingnormal menstruation will occur after the progestin period. Unexpected or prolonged uterinebleeding during therapy should be reported to the physician and its cause clarified.There is limited evidence available in the literature suggesting that oestradiol may be weaklygenotoxic. No evidence could be found for an increase in the rate of gene mutation in bacterialor mammalian cells, but there was some evidence for the induction of chromosomal aberrationsand aneuploidy and an increased incidence of sister chromatid exchanges (indicative of DNAdamage) in mammalian cells. None of these effects were induced by oestradiol in humanlymphocyte cultures. Importantly, there was no evidence of micronuclei formation in rodentbone marrow micronucleus assays.Breast CancerEpidemiological studies indicated a small or moderate increase in the probability of havingbreast cancer in women currently or recently using hormone treatment (HT). A largeobservational study, the Million Women Study, has shown that compared to never-users, use ofoestrogen-progestagen combined HT is associated with a higher risk of breast cancer (RR =2.00, 95%CI: 1.88-2.12) than use of oestrogens alone (RR = 1.30, 95%CI 1.21-1.40). A largerandomised clinical trial demonstrated that continuous combined HT is associated with anincrease in breast cancer risk (RR 1.26, 95% CI: 1.00-1.59) (see Women's Health Initiative inClinical Trials). In a separate arm of this trial no increased risk has so far been observed foroestrogen-only therapy. The use of oestrogens alone as well as combined/sequential oestrogenand progestagen use is associated with an increased risk of breast cancer. This emergestowards the end of the first year of treatment (see Million Women Study in Clinical Trials).Breast cancer can be fatal. Therefore, for all HT, the benefits and risks of treatment should becarefully considered (refer to Indications). It is recommended that women are encouraged toreport any changes in their breast to their doctor. Regular breast examinations and, whereappropriate, mammography should be carried out, particularly in women with risk factors forbreast cancer.If prescribing HT, the potential for increased cardiovascular, thrombotic and neoplastic adverseevents, and an increased incidence of probable dementia in older women, must be consideredas part of the risk-benefit assessment (refer to Clinical Trials). The need for continuation oftreatment should be reviewed after 6 months.Observational studies have shown that in women with an intact uterus, the risk of endometrialhyperplasia and endometrial cancer is increased with the use of unopposed oestrogens. TheSANDRENA – <strong>Product</strong> <strong>Information</strong> Page 6 of 10
addition of a progestagen substantially reduces or may even lower the risk for hyperplasia andendometrial cancer.Ovarian CancerAn increased risk of ovarian cancer in menopausal women taking oestrogen-only replacementtherapy (mostly conjugated equine oestrogens) was observed in a large US epidemiologicalstudy that followed over 40 000 HT users for a mean duration of 13.4 years (range: 1 month to19.8 years). The relative risk of ovarian cancer was 1.8 (95% confidence interval 1.1-3.0) forwomen who took oestrogen replacement therapy for 10-19 years and 3.2 (1.7-5.7) for 20 yearsor more of use. This equates to approximately 3 and 8 additional cases per 10 000 womenyearsat these time points (the incidence in non-users was 4.4 per 10 000 women-years). Thisobservation was most obvious in women who had a prior history of hysterectomy (defined assimple hysterectomy or hysterectomy with unilateral oophorectomy). In this subpopulation, therelative risk was 2.0 (0.96-4.3) for women who took oestrogen-only replacement therapy for 10-19 years and 3.4 (95% CI, 1.6-7.5) for 20 years or more of use. The study authors noted thatmuch of the long term use of oestrogen-only HT likely included higher average daily doses ofoestrogen than are currently recommended. It is uncertain whether long-term use of combinedHT confers a different risk than oestrogen-only products. The study did not include <strong>Sandrena</strong>users and, in the absence of data, it is unknown whether <strong>Sandrena</strong> is distinct in this regard.Pregnancy (Category B1)Oestrogens must not be used during pregnancy.LactationOestrogen administration to nursing mothers has been shown to decrease the quantity andquality of milk. Detectable amounts of oestrogens and progestagens have been found in themilk of lactating mothers receiving these compounds, but the effects on the breastfed infanthave not been determined. Oestrogens must not be used during lactation, (see„CONTRAINDICATIONS‟).Effect on ability to drive and use machinesOestrogens such as <strong>Sandrena</strong> do not affect the ability to drive or use machines.INTERACTIONS WITH OTHER MEDICINESNo drug interactions have been identified. There are some indications that oestrogens mayreduce the effects of antihypertensive, anticoagulant and antidiabetic drugs. Potent inducers ofhepatic enzymes, including barbiturates, carbamazepine, meprobamate, phenylbutazone,griseofulvin and rifampin may reduce the effects of oestrogens. The significance of theseinteractions in transdermal application has not been elucidated.ADVERSE EFFECTSAdverse events reported at an incidence of >1% among patients treated with <strong>Sandrena</strong>during controlled trials are shown in the table below:System organ classSkin and appendages (Total %)Skin irritationMusculo-skeletal (Total %)Skeletal/back painCentral- and peripheral nervous system (Total %)HeadacheDizzinessPRODUCT(N=623)%(4.01)3.90(2.56)1.93(6.58)4.491.28CONTROLS(N=256)%(21.48)21.09(3.91)1.95(8.98)6.250.78SANDRENA – <strong>Product</strong> <strong>Information</strong> Page 7 of 10
In patients with intact uteri it is recommended to combine <strong>Sandrena</strong> treatment with cyclicprogestin, for example 10 mg medroxyprogesterone acetate, 2.5 mg norethisterone, 1-2 mgnorethisterone acetate or 10 mg dydrogesterone for 10 -14 days monthly.One to two dose units (0.5 g or 1.0 g) of <strong>Sandrena</strong> (0.5 to 1.5 mg oestradiol) are applied oncedaily on the skin of the lower trunk or the thigh. The application surface area should be one totwo times the size of the hand. <strong>Sandrena</strong> should not be applied on the breasts, on the face oron irritated or broken skin. Accidental contact of the <strong>gel</strong> with the eyes should be avoided. Handsshould be washed thoroughly after application.In clinical trials the use of <strong>Sandrena</strong> has induced dermal irritation only very infrequently. Theprobability of topical irritation can be further decreased by changing the area of application daily(e.g. left and right side on alternate days).If the patient forgets to apply a dose, it should be applied as soon as possible, unless the doseis more than 12 hours late. If the dose is more than 12 hours late, it should be skipped. Misseddoses may induce breakthrough bleeding.Improvement of symptoms generally occurs within a few weeks, but optimal results areobtained when therapy is continued for at least 3 months. <strong>Sandrena</strong> should be prescribed forthe shortest duration consistent with treatment goals. Review the need for continuation oftreatment after 6 months, taking into account the risk-benefit ratio for the individual user at thatmoment.Monitoring AdviceAs for all steroids with hormonal activity, yearly medical examination particularly of the breastsand pelvic areas is advisable. Review the need for continuation of treatment after 6 months(refer to Precautions and Indications).OVERDOSAGEGenerally, oestrogens are well tolerated even in massive doses. Possible symptoms includethose listed under adverse drug reaction. Management is symptomatic.PRESENTATION AND STORAGE CONDITIONS<strong>Sandrena</strong> is a smooth and opalescent <strong>gel</strong>, individually packed in single-dose laminated foilsachets.Pack sizes: 28* x 0.5 g, 91* x 0.5 g, 28 x 1.0 g and 91* x 1.0 g.* not marketed in <strong>Australia</strong>.Incompatibilities:No incompatibilities have been found.Storage conditions: Store below 25 0 C.NAME AND ADDRESS OF THE SPONSOR<strong>Aspen</strong> <strong>Pharmacare</strong> <strong>Australia</strong> Pty Limited34 - 36 Chandos StreetSt. Leonards NSW 2065<strong>Australia</strong>SANDRENA – <strong>Product</strong> <strong>Information</strong> Page 9 of 10
POISON SCHEDULE OF THE MEDICINES4 – Prescription Only MedicineDate of First Inclusion in the <strong>Australia</strong>n Register of Therapeutic Goods (the ARTG)8 April 2003.Date of Most Recent Amendment26 Jan 2012.SANDRENA – <strong>Product</strong> <strong>Information</strong> Page 10 of 10