Ultrasound assessment of fetal headâperineum distance before ...
Ultrasound assessment of fetal headâperineum distance before ...
Ultrasound assessment of fetal headâperineum distance before ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204Published online 5 June 2008 in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/uog.5360<strong>Ultrasound</strong> <strong>assessment</strong> <strong>of</strong> <strong>fetal</strong> head–perineum <strong>distance</strong><strong>before</strong> induction <strong>of</strong> laborT. M. EGGEBØ*, C. HEIEN*, I. ØKLAND*, L. K. GJESSING*, P. ROMUNDSTAD†and K. Å. SALVESEN‡*Department <strong>of</strong> Obstetrics and Gynecology, Stavanger University Hospital, Stavanger and †Department <strong>of</strong> Public Health, NorwegianUniversity <strong>of</strong> Science and Technology, ‡National Center for Fetal Medicine, Trondheim University Hospital (St Olav’s Hospital) andDepartment <strong>of</strong> Laboratory Medicine, Children’s and Women’s Health, Norwegian University <strong>of</strong> Science and Technology, Trondheim,NorwayKEYWORDS: Bishop score; cervical angle; cervical length; <strong>fetal</strong> head–perineum <strong>distance</strong>; induction <strong>of</strong> labor; occiputposterior; ultrasoundABSTRACTObjectives To evaluate <strong>fetal</strong> head–perineum <strong>distance</strong>measured by ultrasound imaging as a predictive factorfor induction <strong>of</strong> labor, and to compare this <strong>distance</strong>with maternal factors, the Bishop score and ultrasoundmeasurements <strong>of</strong> cervical length, cervical angle andocciput position.Methods The study included 275 women admitted forinduction <strong>of</strong> labor. The <strong>fetal</strong> head–perineum <strong>distance</strong>was measured by transperineal ultrasound imaging asthe shortest <strong>distance</strong> from the outer bony limit <strong>of</strong> the<strong>fetal</strong> skull to the skin surface <strong>of</strong> the perineum. Cervicallength and angle was measured by transvaginal ultrasoundexamination, and <strong>fetal</strong> head position was assessedby transabdominal ultrasound imaging. The Bishopscore was assessed without knowledge <strong>of</strong> ultrasoundmeasurements. Receiver–operating characteristics (ROC)curves were used for evaluation <strong>of</strong> the probability <strong>of</strong> asuccessful vaginal delivery. The time from induction todelivery was tested using Cox regression analysis withultrasound measurements, parity and body mass index(BMI) as possible predictive factors.Results Areas under the ROC curve for prediction <strong>of</strong>vaginal delivery were 62% (95% CI, 52–71%) for<strong>fetal</strong> head–perineum <strong>distance</strong> (P = 0.03), 61% (95% CI,51–71%) for cervical length (P = 0.03), 63% (95% CI,52–74%) for cervical angle (P = 0.02), 61% (95% CI,52–70%) for Bishop score (P = 0.03) and 60% (95%CI, 51–69%) for BMI (P = 0.05). The Cesarean deliveryrate was 22% among nulliparous and 5% among parouswomen (P < 0.01). Parity, <strong>fetal</strong> head–perineum <strong>distance</strong>,cervical length and cervical angle were contributingfactors predicting vaginal delivery within 24 h in a Coxregression model. Occiput posterior position had nosignificant predictive value.Conclusions Fetal head–perineum <strong>distance</strong> measured bytransperineal ultrasound examination can predict vaginaldelivery after induction <strong>of</strong> labor, with a predictive valuesimilar to that <strong>of</strong> ultrasonographically measured cervicallength and the Bishop score. However, we judge none <strong>of</strong>these methods used alone to be good enough in a clinicalsetting. Copyright © 2008 ISUOG. Published by JohnWiley & Sons, Ltd.INTRODUCTIONInduction <strong>of</strong> labor (IOL) is one <strong>of</strong> the most frequentobstetric procedures and occurs in 13–20% <strong>of</strong> termpregnancies 1,2 . IOL is associated with an increased risk<strong>of</strong> operative delivery 3,4 , with a Cesarean delivery rate <strong>of</strong>around 25% in nulliparous women and around 5% inparous women 5 .The Bishop score remains the ‘gold standard’ forassessing suitability for IOL 6 , but it is a subjectiveevaluation with limitations 7,8 . Parity and body mass index(BMI) are other factors predictive <strong>of</strong> labor induction 9–11 ,and transvaginal ultrasound measurements <strong>of</strong> cervicallength and cervical angle may be added to the list.Transvaginal ultrasound measurements perform betterthan the Bishop score in some studies 8,9,11 –14 , but notin others 15 –17 . A recent meta-analysis concluded thatCorrespondence to: Dr T. M. Eggebø, Department <strong>of</strong> Obstetrics and Gynecology, Stavanger University Hospital, 4068 Stavanger, Norway(e-mail: tme@lyse.net)Accepted: 1 March 2008Copyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd.ORIGINAL PAPER
200 Eggebø et al.transvaginal ultrasound imaging was equal to the Bishopscore, but the authors called for more research 18 .The timing <strong>of</strong> IOL for common indications suchas diabetes, post-term pregnancy and pre-eclampsia iscontroversial. If a successful labor outcome could bepredicted, IOL could be considered in cases with ‘s<strong>of</strong>tindications’ or on maternal request. Thus, any reliablemethods <strong>of</strong> preinduction <strong>assessment</strong> would be valuabletools in counseling women <strong>before</strong> IOL.<strong>Ultrasound</strong> measurement <strong>of</strong> the <strong>fetal</strong> head–perineum<strong>distance</strong> has not been evaluated as a predictive factor inwomen scheduled for IOL, but it was found to predictlabor outcome for women with prelabor rupture <strong>of</strong>membranes at term 19 . The aim <strong>of</strong> the present study wasto evaluate <strong>fetal</strong> head–perineum <strong>distance</strong> measured bytransperineal ultrasound imaging as a predictive factorfor IOL, and to compare this <strong>distance</strong> with maternalfactors, Bishop score and ultrasound measurements <strong>of</strong>cervical length, cervical angle and occiput position.METHODSIn all, 5487 women delivered at Stavanger UniversityHospital from January 2006 to March 2007. Womenwere eligible for the study if they had a live singletonpregnancy with cephalic presentation and a gestationalage <strong>of</strong> more than 37 completed weeks according to amid-trimester scan. Women with a previous Cesareansection were not eligible. Of the 4918 women eligible forinclusion in the study, 710 had IOL and, <strong>of</strong> these, 275(39%) were included in the study. The main reason fornon-inclusion was unwillingness to participate. The localethics committee approved the study and all women gavewritten informed consent. The characteristics <strong>of</strong> the studypopulation and the indications for IOL are presented inTable 1.Table 1 Characteristics <strong>of</strong> the study population (n = 275)Parameter% or median (range)Nulliparous 47Maternal age (years) 30 (18–45)Body mass index (kg/m 2 ) 24 (17–45)Gestational age (weeks) 40 (37–43)Caucasian 96Cesarean delivery 13Operative vaginal delivery 18Epidural analgesia 54Blood loss (mL) 300 (100–3400)Indication for induction <strong>of</strong> laborPost-term pregnancy 26Pre-eclampsia/hypertension 8Diabetes 3Fetal growth restriction 5Macrosomia 10Maternal request 12Prelabor rupture <strong>of</strong> membranes 20Oligohydramnios 3Other 13Two obstetricians and three specially trained midwivesperformed the ultrasound measurements with an EUBHitachi 5500 (Kashiwa, Japan) device with a 3.5–7.5-MHz multifrequency transabdominal transducer and a5.0–9.0-MHz multifrequency transvaginal transducer.The Bishop score was assessed after the scan andimmediately <strong>before</strong> IOL by the obstetrician on call,who was blinded to the ultrasound measurements. Allexaminations were performed with the woman in a supineposition and with an empty bladder.The <strong>fetal</strong> occiput position was evaluated by transabdominalultrasound imaging and classified as describedby Rane et al. 11 . The <strong>fetal</strong> head–perineum <strong>distance</strong> wasmeasured as the shortest <strong>distance</strong> from the outer bonylimit <strong>of</strong> the <strong>fetal</strong> skull to the skin surface <strong>of</strong> the perineumby a transperineal ultrasound examination in a transverseview, as described in a previous study 19 . The transducerwas moved and angled until the shortest <strong>distance</strong> tothe <strong>fetal</strong> head was visualized. The s<strong>of</strong>t tissue was compressedwith firm pressure without creating discomfortfor the woman. The cervix was evaluated by transvaginalultrasound examination without putting pressure on thecervix. The cervical length was measured as describedby Valentin et al. 20 , and the posterior cervical angle wasassessed as described by Rane et al. 11 . The mean <strong>of</strong> threemeasurements was used in the calculations.IOL was performed according to the managementprotocol <strong>of</strong> the hospital <strong>before</strong> the study. Labor wasinduced with amniotomy followed by oxytocin if thecervix was favorable (Bishop score ≥ 6). If the cervix wasunfavorable, labor was induced with 25 µg misoprostolapplied vaginally every 4 h (up to a maximum <strong>of</strong> 100 µgin 24 h and a total maximum dose <strong>of</strong> 200 µg) untilcontractions were regular. Previous studies have useddiverse definitions for successful IOL 8,11,21 . We definedsuccessful IOL as resulting in a vaginal delivery, eitherspontaneous or operative, with no limit on the time forthis to occur.The <strong>fetal</strong> head–perineum <strong>distance</strong> was evaluated atcut-<strong>of</strong>f levels <strong>of</strong> 40 mm, 45 mm and 50 mm, cervicallength at cut-<strong>of</strong>f levels <strong>of</strong> 20 mm, 25 mm and 30 mm,and cervical angle using cut-<strong>of</strong>f levels <strong>of</strong> 90 ◦ and 120 ◦degrees. The cut-<strong>of</strong>f points were chosen according toprevious studies 8,11,19,22,23 and the fact that World HealthOrganization Stage 0 (<strong>fetal</strong> head at the ischial spines) isapproximately 5 cm from the perineum 24 . The <strong>fetal</strong> headposition was evaluated as occiput posterior comparedwith other positions 11 .In a previous study <strong>of</strong> women with prelabor rupture <strong>of</strong>membranes at term 19 , we reported Cesarean delivery rates<strong>of</strong> 4% among women with a short <strong>fetal</strong> head–perineum<strong>distance</strong> and 15% among women with a long <strong>distance</strong>.Using an alpha <strong>of</strong> 0.05 and a power <strong>of</strong> 0.8, and assuminga ratio <strong>of</strong> 2 : 1 for long to short <strong>distance</strong>, we calculatedthat 250 women were needed for an adequately poweredstudy.Data were entered into the statistical s<strong>of</strong>twarepackage SPSS version 14.0 (Chicago, IL, USA). Forstatistical analyses, Mann–Whitney U-tests, Chi-squareCopyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd. <strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204.
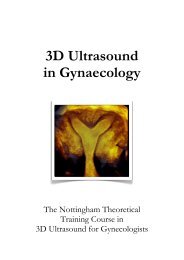
<strong>Ultrasound</strong> <strong>assessment</strong> <strong>before</strong> induction <strong>of</strong> labor 201tests, Fisher’s exact tests and Pearson correlation wereused. The predictive value <strong>of</strong> maternal factors, ultrasoundmeasurements and Bishop scores for a successfulvaginal delivery was evaluated using receiver–operatingcharacteristics (ROC) curves, and the area under thecurve was used as discriminator. The induction–deliveryinterval within 24 h was evaluated using Kaplan–Meiersurvival analyses and Cox regression analyses. Womenexperiencing a Cesarean section or a time to delivery> 24 h were censored. In the Cox regression analyses,<strong>fetal</strong> head–perineum <strong>distance</strong>, cervical length, cervicalangle, occiput position, parity and BMI were tested aspossible predictive factors. In additional analyses, wealso adjusted for maternal age, gestational age, birthweight and head circumference as possible confounders.The Bishop score was not tested in the survival analysesbecause the induction methods were stratified accordingto this score. P < 0.05 was considered significant.RESULTSThe overall Cesarean delivery rate was 13%. Onehundred and thirty (47%) women were nulliparous. TheCesarean delivery rate among nulliparous women was22% compared with 5% among women with one ormore previous vaginal deliveries (P < 0.01).Table 2 shows test characteristics <strong>of</strong> maternal characteristics,the Bishop score and ultrasound measurementsas predictive factors for a successful vaginal delivery.Areas under the ROC curve for prediction <strong>of</strong> vaginaldelivery (Figure 1) were 62% (95% CI, 52–71%) for<strong>fetal</strong> head–perineum <strong>distance</strong> (P = 0.03), 61% (95% CI,51–71%) for cervical length (P = 0.03), 63% (95% CI,52–74%) for cervical angle (P = 0.02), 61% (95% CI,52–70%) for Bishop score (P = 0.03), 60% (95% CI,51–69%) for BMI (P = 0.05), 51% (95% CI, 41–61%)for maternal age (P = 0.85) and 56% (95% CI, 45–66%)for gestational age (P = 0.27). The ROC curves indicatedthat <strong>fetal</strong> head–perineum <strong>distance</strong> ≤ 40 mm, cervicalSensitivity (%)100806040200 0 20 40 60 80 100False-positive rate (%)Figure 1 Receiver–operating characteristics curves for <strong>fetal</strong>head–perineum <strong>distance</strong> ( ), cervical length ( ) and Bishopscore ( ) in predicting a vaginal delivery.length ≤ 25 mm and cervical angle > 90 ◦ were the bestcut-<strong>of</strong>f levels for predicting vaginal delivery.The mean <strong>distance</strong> from the <strong>fetal</strong> head to the perineumwas 47.5 mm and the median was 46 (range, 26–108)mm. The Cesarean delivery rate was 4% among 73 womenwith a short <strong>distance</strong> (≤ 40 mm) and 16% among 202women with a long <strong>distance</strong> (P = 0.01). Characteristics<strong>of</strong> labor outcomes stratified according to a cut-<strong>of</strong>f level at40 mm are presented in Table 3.The mean cervical length was 27.6 mm and the medianwas 28 (range, 6–54) mm. The Cesarean delivery rate was8% among 112 women with a short cervix (≤ 25 mm)and 17% among women with a long cervix (P = 0.05).The cervical length and the <strong>fetal</strong> head–perineum <strong>distance</strong>were correlated (Pearson r = 0.39, P < 0.01).Table 2 Test characteristics <strong>of</strong> ultrasound measurements, maternal characteristics and Bishop score in predicting vaginal deliverySensitivity(% (95% CI))FPR(% (95% CI))PPV(% (95% CI))NPV(% (95% CI)) LRFetal head–perineum <strong>distance</strong> (mm)≤ 40 29.3 (23.6–35.5) 8.3 (1.7–22.5) 95.9 (88.5–99.1) 16.3 (11.5–22.2) 3.5≤ 45 49.4 (42.9–55.9) 41.7 (25.5–59.3) 88.7 (82.1–93.6) 14.8 (9.4–21.7) 1.2≤ 50 67.4 (61.0–73.3) 47.2 (30.4–64.5) 90.4 (85.2–94.3) 19.6 (12.2–28.9) 1.4Cervical length (mm)≤ 20 26.4 (20.9–32.4) 13.9 (4.7–29.5) 92.6 (83.7–97.6) 15.0 (10.4–20.6) 1.9≤ 25 43.1 (36.7–49.6) 25.0 (12.1–42.2) 92.0 (85.3–96.3) 16.6 (11.2–23.2) 1.7≤ 30 62.3 (55.9–68.5) 44.4 (27.1–61.9) 90.3 (84.7–94.4) 18.2 (11.5–26.7) 1.4Cervical angle ( ◦ )> 90 87.9 (83.0–91.7) 61.1 (43.5–76.9) 90.5 (86.0–94.0) 32.6 (19.1–48.5) 1.4≥ 120 37.7 (31.5–44.1) 27.8 (14.2–45.2) 90.0 (82.4–95.1) 14.9 (9.9–21.0) 1.4Para 1+ 57.7 (51.2–64.1) 19.4 (8.2–36.0) 95.2 (90.3–98.0) 22.3 (15.5–30.4) 3.0BMI < 30 kg/m 2 84.9 (79.8–89.2) 77.8 (60.8–89.9) 87.9 (83.0–91.8) 18.2 (8.2–32.7) 1.1Bishop score ≥ 6 43.5 (37.1–50.1) 25.0 (12.1–42.8) 92.0 (85.4–96.3) 16.7 (11.3–23.3) 1.7FPR, false-positive rate; LR, likelihood ratio; NPV, negative predictive value; PPV, positive predictive value.Copyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd. <strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204.
202 Eggebø et al.Table 3 Characteristics <strong>of</strong> labor stratified into groups with short(≤ 40 mm) or long (>40 mm) <strong>fetal</strong> head–perineum <strong>distance</strong>100Fetal head–perineum <strong>distance</strong>≤ 40 mm(n = 73)> 40 mm(n = 202) P*Epidural analgesia (%) 47 56 0.17Cesarean delivery (%) 4 16 0.01Operative vaginal19 17 0.65delivery (%)Birth weight (g) 3577 (603) 3741 (585) 0.08Apgar score 1 min 8.68 (1.04) 8.44 (1.18) 0.04Apgar score 5 min 9.23 (0.64) 9.15 (0.80) 0.66Umbilical artery pH 7.26 (0.08) 7.24 (0.08) 0.07Umbilical artery−3.16 (3.57) −3.66 (3.36) 0.23base excessDuration <strong>of</strong> labor (min)Induction to delivery 540 (371) 809 (541) < 0.01Labor (stages 1 + 2) 259 (120) 321 (195) 0.06Labor stage 2 21 (20) 21 (21) 0.80Values are % or mean (SD). *Mann–Whitney U-test, Chi-squaretest or Fisher’s exact test.The mean cervical angle was 109 ◦ and the medianwas 110 ◦ (range, 60–150 ◦ ). The Cesarean delivery ratewas 33% among 43 women with a cervical angle ≤ 90 ◦compared with 9% if the cervical angle was > 90 ◦(P < 0.01). Cervical angle correlated with cervical length(Pearson r =−0.23, P < 0.01) and <strong>fetal</strong> head–perineum<strong>distance</strong> (Pearson r =−0.19, P < 0.01).In all, 61 (22%) women had the <strong>fetal</strong> head in anocciput posterior position <strong>before</strong> the start <strong>of</strong> induction.The Cesarean delivery rate was 7% compared with15% among women with <strong>fetal</strong> heads in other positions(P = 0.13).The time from induction to delivery is demonstratedfor women with a <strong>fetal</strong> head–perineum <strong>distance</strong> ≤ 40 mmand those with a <strong>distance</strong> > 40 mm in a Kaplan–Meiersurvival plot (Figure 2). The difference between groupswas statistically significant (P < 0.001, log rank test).Twenty-four hours after induction 3% (95% CI, 0–10%)<strong>of</strong> women with a short <strong>distance</strong> and 11% (95% CI,7–17%) <strong>of</strong> women with a long <strong>distance</strong> were still in labor.In a multivariate Cox regression analysis, parity,<strong>fetal</strong> head–perineum <strong>distance</strong> ≤ 40 mm, cervical length≤ 25 mm and cervical angle > 90 ◦ predicted vaginal deliverywithin 24 h (Table 4). BMI and occiput posterior positionwere not contributing factors. Multivariable adjustmentsfor potential confounders did not change the results.There was one catastrophic event in the study group.One woman had a sudden cardiac arrest 10 h after IOL. ACesarean delivery was performed immediately. A healthybaby was delivered, but the mother died. A medicolegalautopsy was performed, and the conclusion was amnioticfluid embolism.DISCUSSIONFetal head–perineum <strong>distance</strong> measured by transperinealultrasound examination was found to be a predictor <strong>of</strong>Percentage <strong>of</strong> women undelivered8060402000 5 10 15 20 25Time to delivery (h)Figure 2 Kaplan–Meier estimates <strong>of</strong> proportions <strong>of</strong> women notdelivered within 24 h, according to sonographically measured <strong>fetal</strong>head–perineum <strong>distance</strong> (≤ 40 mm, ; > 40 mm, ). Womenexperiencing Cesarean section or a time to delivery > 24 hwerecensored. P < 0.001 (log rank test).Table 4 Relative risk (hazard ratio) for a vaginal delivery within24 h after induction according to <strong>fetal</strong> head–perineum <strong>distance</strong>,cervical length, cervical angle, occiput position, parity and bodymass index (BMI) determined by Cox regression analysisHazard ratio(95% CI) PFetal head–perineum <strong>distance</strong> (mm) 0.001> 40 1.00 (reference)≤ 40 1.67 (1.23–2.26)Cervical length (mm) < 0.001> 25 1.00 (reference)≤ 25 2.35 (1.75–3.14)Cervical angle ( ◦ ) 0.005≤ 901.00 (reference)> 90 1.92 (1.22–3.04)Fetal head position 0.13Occiput anterior or transverse 1.00 (reference)Occiput posterior 1.27 (0.93–1.75)Parity < 0.001Nullipara1.00 (reference)Para 1+ 3.25 (2.43–4.35)BMI (kg/m 2 ) 0.50≥ 301.00 (reference)< 30 1.14 (0.78–1.65)Women experiencing Cesarean section or a time to delivery > 24 hwere censored.vaginal delivery after IOL, and the predictive values weresimilar for this method and ultrasound-measured cervicallength and the Bishop score. However, we judge none <strong>of</strong>these methods used alone to be good enough in a clinicalsetting.Parity was the best predictor <strong>of</strong> vaginal delivery.BMI, Bishop score and ultrasound measurements <strong>of</strong><strong>fetal</strong> head–perineum <strong>distance</strong>, cervical length and cervicalangle predicted a vaginal delivery with around 60% underCopyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd. <strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204.
<strong>Ultrasound</strong> <strong>assessment</strong> <strong>before</strong> induction <strong>of</strong> labor 203the ROC curve area. Parity, <strong>fetal</strong> head–perineum <strong>distance</strong>,cervical length and cervical angle were statisticallysignificant contributing factors to vaginal delivery within24hinaCoxregressionmodel.The fact that parity was the single best predictor wasin accordance with previous studies 12,13 . We could notconfirm the importance <strong>of</strong> maternal age, which has beenemphasized in other studies 3,9 . This may be due to a ratherlow Cesarean delivery rate in our department. Some studiesrecommend ultrasound measurements, such as occiputposterior position, cervical length, cervical angle or cervicalwedging, as additional predictive variables 8–14,22 , butother authors disagree 15 –17 . Rozenberg et al. emphasizethat heterogeneous populations, lack <strong>of</strong> standardization<strong>of</strong> the method <strong>of</strong> induction, different ultrasoundmeasurements and different endpoints can give conflictingresults 16 . Some authors have suggested modelswith combinations <strong>of</strong> maternal factors and ultrasoundmeasurements 10,11,21 .Tan et al. found ultrasound measurements <strong>of</strong> cervicallength and the Bishop score to be <strong>of</strong> similar value in predictinga Cesarean delivery 23 .Raneet al. found cervicalangle to be a predictive factor for successful IOL 11 ,andthese results are in accordance with our findings.Fetal head position had no predictive value for vaginaldelivery after IOL. This is in accordance with a study fromPeregrine et al. 25 , but not with other studies 11,26 .Mostfetuses were in the occiput posterior position close to thelimit values (4 o’clock or 8 o’clock 11 ), and in a previousstudy we found that 30% <strong>of</strong> fetuses moved the head duringan ultrasound examination <strong>before</strong> the start <strong>of</strong> labor 27 .In a recent editorial, Sherer has pointed out the needfor new methods for measuring <strong>fetal</strong> head descent 28 .Dietz and Lanzarone evaluated ultrasound-measuredengagement <strong>of</strong> the <strong>fetal</strong> head as a predictive factor foroutcome in spontaneous labors by relating the <strong>fetal</strong>head to the symphysis pubis 29 . However, we believe thatmeasurement <strong>of</strong> <strong>fetal</strong> head–perineum <strong>distance</strong> is easier.Fetal head station is determined after digital <strong>assessment</strong><strong>of</strong> the relationship between the <strong>fetal</strong> head and the maternalischial spine 24 . In our experience, the ischial spine isdifficult to visualize with ultrasound imaging. Instead weused the outlet <strong>of</strong> the birth canal as a reference line.This is an intuitively useful reference line, being the ‘goalline’ <strong>of</strong> parturition. Because the birth canal is curved,there is an association, but not a direct relationship,between <strong>fetal</strong> head–perineum <strong>distance</strong> and <strong>fetal</strong> headstation. A schematic drawing <strong>of</strong> <strong>fetal</strong> head descent in acurved birth canal and the association with the remaining<strong>fetal</strong> head–perineum <strong>distance</strong> is illustrated in Figure 3.Measurements may vary with the degree <strong>of</strong> compression<strong>of</strong> the s<strong>of</strong>t tissue. In our experience, the examiner will meetfirm resistance when the perineal s<strong>of</strong>t tissue is compressed,without causing discomfort to the woman. We have foundthe interobserver and intraobserver variability <strong>of</strong> themethod to be acceptable 19 . Thus, we believe that thismethod can be used to assess <strong>fetal</strong> head descent, eventhough the relationship with the well established concept<strong>of</strong> <strong>fetal</strong> head station is less clear. An unclear relationshipFetal headRemaining<strong>distance</strong>PerineumFigure 3 Schematic drawing <strong>of</strong> <strong>fetal</strong> head descent in a curved birthcanal showing association with remaining <strong>fetal</strong> head–perineum<strong>distance</strong>.should not undermine the potential clinical value <strong>of</strong> theproposed method, which is easy and quick to perform.The method should be validated in new studies for headdescent during labor, in particular during protracted laborand <strong>before</strong> operative vaginal deliveries.The <strong>fetal</strong> head–perineum <strong>distance</strong> predicts laboroutcome after IOL. The clinical value <strong>of</strong> this ultrasoundmeasured<strong>distance</strong> is similar to that <strong>of</strong> ultrasound<strong>assessment</strong> <strong>of</strong> cervical length and the Bishop score. Futurestudies should evaluate if and how these predictive factorscan be combined.ACKNOWLEDGMENTSMargrethe Tangerud and Karin Stangeland did some <strong>of</strong>the ultrasonographic examinations.REFERENCES1. Gjessing LK. Results from Department <strong>of</strong> Obstetrics, StavangerUniversity Hospital, 1997–2007; http://www.kvinneklinikkensus.com/01results/obstetr/publ B1 STANDARD.htm[Accessed 1 September 2007].2. Government Statistical Service. NHS Maternity Statistics,England: 2003–04. Bulletin 2005/10: March 2005;http://www.dh.gov.uk/assetRoot/04/10/70/61/04107061.pdf[Accessed 1 September 2007].3. Maslow AS, Sweeny AL. Elective induction <strong>of</strong> labor as a riskfactor for cesarean delivery among low-risk women at term.Obstet Gynecol 2000; 95: 917–922.4. Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk <strong>of</strong> cesareandelivery with elective induction <strong>of</strong> labor at term in nulliparouswomen. Obstet Gynecol 1999; 94: 600–607.5. Heffner LJ, Elkin E, Fretts RC. Impact <strong>of</strong> labor induction,gestational age, and maternal age on cesarean delivery rates.Obstet Gynecol 2003; 102: 287–293.6. Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol1964; 24: 266–268.7. Hendrix NW, Chauhan SP, Morrison JC, Magann EF,Martin JN Jr, Devoe LD. Bishop score: a poor diagnostic testCopyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd. <strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204.
204 Eggebø et al.to predict failed induction versus vaginal delivery. South Med J1998; 91: 248–252.8. Pandis GK, Papageorghiou AT, Ramanathan VG, ThompsonMO, Nicolaides KH. Preinduction sonographic measurement<strong>of</strong> cervical length in the prediction <strong>of</strong> successful induction<strong>of</strong> labor. <strong>Ultrasound</strong> Obstet Gynecol 2001; 18: 623–628.9. Rane SM, Guirgis RR, Higgins B, Nicolaides KH. Models forthe prediction <strong>of</strong> successful induction <strong>of</strong> labor based on preinductionsonographic measurement <strong>of</strong> cervical length. JMaternFetal Neonatal Med 2005; 17: 315–322.10. Peregrine E, O’Brien P, Omar R, Jauniaux E. Clinical andultrasound parameters to predict the risk <strong>of</strong> cesareandelivery after induction <strong>of</strong> labor. Obstet Gynecol 2006; 107:227–233.11. Rane SM, Guirgis RR, Higgins B, Nicolaides KH. The value <strong>of</strong>ultrasound in the prediction <strong>of</strong> successful induction <strong>of</strong> labor.<strong>Ultrasound</strong> Obstet Gynecol 2004; 24: 538–549.12. Rane SM, Guirgis RR, Higgins B, Nicolaides KH. Pre-inductionsonographic measurement <strong>of</strong> cervical length in prolongedpregnancy: the effect <strong>of</strong> parity in the prediction <strong>of</strong> the needfor Cesarean section. <strong>Ultrasound</strong> Obstet Gynecol 2003; 22:45–48.13. Rane SM, Pandis GK, Guirgis RR, Higgins B, Nicolaides KH.Pre-induction sonographic measurement <strong>of</strong> cervical length inprolonged pregnancy: the effect <strong>of</strong> parity in the prediction<strong>of</strong> induction-to-delivery interval. <strong>Ultrasound</strong> Obstet Gynecol2003; 22: 40–44.14. Laencina AM, Sanchez FG, Gimenez JH, Martinez MS, MartinezJA, Vizcaino VM. Comparison <strong>of</strong> ultrasonographic cervicallength and the Bishop score in predicting successful laborinduction. Acta Obstet Gynecol Scand 2007; 86: 799–804.15. Gonen R, Degani S, Ron A. Prediction <strong>of</strong> successful induction<strong>of</strong> labor: comparison <strong>of</strong> transvaginal ultrasonography and theBishop score. Eur J <strong>Ultrasound</strong> 1998; 7: 183–187.16. Rozenberg P, Chevret S, Chastang C, Ville Y. Comparison <strong>of</strong>digital and ultrasonographic examination <strong>of</strong> the cervix inpredicting time interval from induction to delivery in womenwith a low Bishop score. BJOG 2005; 112: 192–196.17. Rozenberg P, Chevret S, Ville Y. [Comparison <strong>of</strong> pre-inductionultrasonographic cervical length and Bishop score in predictingrisk <strong>of</strong> cesarean section after labor induction withprostaglandins.] Gynecol Obstet Fertil 2005; 33: 17–22.18. Crane JM. Factors predicting labor induction success: a criticalanalysis. Clin Obstet Gynecol 2006; 49: 573–584.19. Eggebø TM, Gjessing LK, Heien C, Smedvig E, Økland I,Romundstad P, Salvesen KA. Prediction <strong>of</strong> labor and delivery bytransperineal ultrasound in pregnancies with prelabor rupture<strong>of</strong> membranes at term. <strong>Ultrasound</strong> Obstet Gynecol 2006; 27:387–391.20. Valentin L, Bergelin I. Intra- and interobserver reproducibility<strong>of</strong> ultrasound measurements <strong>of</strong> cervical length and width in thesecond and third trimesters <strong>of</strong> pregnancy. <strong>Ultrasound</strong> ObstetGynecol 2002; 20: 256–262.21. Dietz HP, Lanzarone V, Simpson JM. Predicting operativedelivery. <strong>Ultrasound</strong> Obstet Gynecol 2006; 27: 409–415.22. Bartha JL, Romero-Carmona R, Martinez-Del-Fresno P,Comino-Delgado R. Bishop score and transvaginal ultrasoundfor preinduction cervical <strong>assessment</strong>: a randomized clinical trial.<strong>Ultrasound</strong> Obstet Gynecol 2005; 25: 155–159.23. Tan PC, Vallikkannu N, Suguna S, Quek KF, Hassan J. Transvaginalsonographic measurement <strong>of</strong> cervical length vs. Bishopscore in labor induction at term: tolerability and prediction<strong>of</strong> Cesarean delivery. <strong>Ultrasound</strong> Obstet Gynecol 2007; 29:568–573.24. World Health Organization. Department <strong>of</strong> ReproductiveHealth and Research. Managing complications in pregnancyand childbirth : a guide for midwives and doctors. WorldHealth Organization: Geneva, 2003.25. Peregrine E, O’Brien P, Jauniaux E. Impact on delivery outcome<strong>of</strong> ultrasonographic <strong>fetal</strong> head position prior to induction <strong>of</strong>labor. Obstet Gynecol 2007; 109: 618–625.26. Akmal S, Kametas N, Tsoi E, Howard R, Nicolaides KH.Ultrasonographic occiput position in early labour in theprediction <strong>of</strong> caesarean section. BJOG 2004; 111: 532–536.27. Eggebø TM, Heien C, Økland I, Gjessing LK, Smedvig E,Romundstad P, Salvesen KA. Prediction <strong>of</strong> labour and deliveryby ascertaining the <strong>fetal</strong> head position with transabdominalultrasound in pregnancies with prelabour rupture <strong>of</strong> membranesafter 37 weeks. Ultraschall Med 2008; 29: 179–183.28. Sherer DM. Intrapartum ultrasound. <strong>Ultrasound</strong> ObstetGynecol 2007; 30: 123–139.29. Dietz HP, Lanzarone V. Measuring engagement <strong>of</strong> the <strong>fetal</strong>head: validity and reproducibility <strong>of</strong> a new ultrasoundtechnique. <strong>Ultrasound</strong> Obstet Gynecol 2005; 25: 165–168.Copyright © 2008 ISUOG. Published by John Wiley & Sons, Ltd. <strong>Ultrasound</strong> Obstet Gynecol 2008; 32: 199–204.