Clinical Assessment Tool - Children over 2 with acute asthma and ...
Clinical Assessment Tool - Children over 2 with acute asthma and ...
Clinical Assessment Tool - Children over 2 with acute asthma and ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
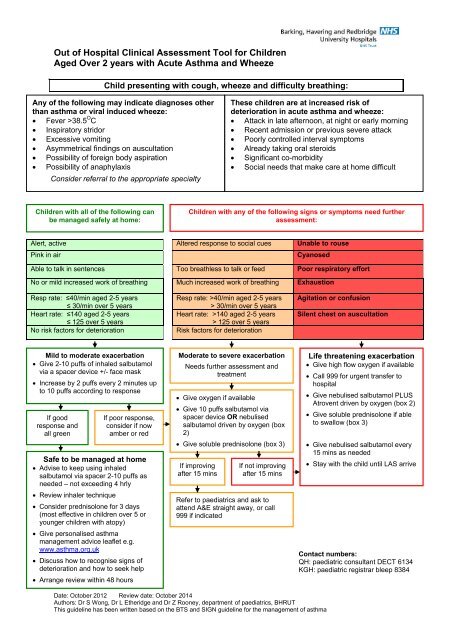
Out of Hospital <strong>Clinical</strong> <strong>Assessment</strong> <strong>Tool</strong> for <strong>Children</strong>Aged Over 2 years <strong>with</strong> Acute Asthma <strong>and</strong> WheezeChild presenting <strong>with</strong> cough, wheeze <strong>and</strong> difficulty breathing:Any of the following may indicate diagnoses otherthan <strong>asthma</strong> or viral induced wheeze:• Fever >38.5 O C• Inspiratory stridor• Excessive vomiting• Asymmetrical findings on auscultation• Possibility of foreign body aspiration• Possibility of anaphylaxisConsider referral to the appropriate specialtyThese children are at increased risk ofdeterioration in <strong>acute</strong> <strong>asthma</strong> <strong>and</strong> wheeze:• Attack in late afternoon, at night or early morning• Recent admission or previous severe attack• Poorly controlled interval symptoms• Already taking oral steroids• Significant co-morbidity• Social needs that make care at home difficult<strong>Children</strong> <strong>with</strong> all of the following canbe managed safely at home:<strong>Children</strong> <strong>with</strong> any of the following signs or symptoms need furtherassessment:Alert, active Altered response to social cues Unable to rousePink in airCyanosedAble to talk in sentences Too breathless to talk or feed Poor respiratory effortNo or mild increased work of breathing Much increased work of breathing ExhaustionResp rate: ≤40/min aged 2-5 years≤ 30/min <strong>over</strong> 5 yearsHeart rate: ≤140 aged 2-5 years≤ 125 <strong>over</strong> 5 yearsNo risk factors for deteriorationResp rate: >40/min aged 2-5 years> 30/min <strong>over</strong> 5 yearsHeart rate: >140 aged 2-5 years> 125 <strong>over</strong> 5 yearsRisk factors for deteriorationAgitation or confusionSilent chest on auscultationMild to moderate exacerbation• Give 2-10 puffs of inhaled salbutamolvia a spacer device +/- face mask• Increase by 2 puffs every 2 minutes upto 10 puffs according to responseIf goodresponse <strong>and</strong>all greenIf poor response,consider if nowamber or redSafe to be managed at home• Advise to keep using inhaledsalbutamol via spacer 2-10 puffs asneeded – not exceeding 4 hrly• Review inhaler technique• Consider prednisolone for 3 days(most effective in children <strong>over</strong> 5 oryounger children <strong>with</strong> atopy)• Give personalised <strong>asthma</strong>management advice leaflet e.g.www.<strong>asthma</strong>.org.uk• Discuss how to recognise signs ofdeterioration <strong>and</strong> how to seek help• Arrange review <strong>with</strong>in 48 hoursModerate to severe exacerbationNeeds further assessment <strong>and</strong>treatment• Give oxygen if available• Give 10 puffs salbutamol viaspacer device OR nebulisedsalbutamol driven by oxygen (box2)• Give soluble prednisolone (box 3)If improvingafter 15 minsIf not improvingafter 15 minsRefer to paediatrics <strong>and</strong> ask toattend A&E straight away, or call999 if indicatedLife threatening exacerbation• Give high flow oxygen if available• Call 999 for urgent transfer tohospital• Give nebulised salbutamol PLUSAtrovent driven by oxygen (box 2)• Give soluble prednisolone if ableto swallow (box 3)• Give nebulised salbutamol every15 mins as needed• Stay <strong>with</strong> the child until LAS arriveContact numbers:QH: paediatric consultant DECT 6134KGH: paediatric registrar bleep 8384Date: October 2012 Review date: October 2014Authors: Dr S Wong, Dr L Etheridge <strong>and</strong> Dr Z Rooney, department of paediatrics, BHRUTThis guideline has been written based on the BTS <strong>and</strong> SIGN guideline for the management of <strong>asthma</strong>
Out of Hospital <strong>Clinical</strong> <strong>Assessment</strong> <strong>Tool</strong> for <strong>Children</strong>Aged Over 2 years <strong>with</strong> Acute Asthma <strong>and</strong> WheezeBox 1: Normal Paediatric Values:Age Resp Rate Heart Rate 12 yr 15 – 20 60 - 100Box 2: Guidelines for use of bronchodilatorsInhaled β 2 agonists are the first line treatment for <strong>acute</strong> <strong>asthma</strong> <strong>and</strong> wheeze, except in life threateningcases• Salbutamol: up to 10 puffs of a metered dose inhaler (MDI) via a spacer device can be safelygiven, up to 4 hourly. MDIs should never be given directly into the mouth in children. <strong>Children</strong>under 3 years will need a face mask connected to the mouthpiece of the spacer. After each puffof the MDI allow the child to take 5 breaths <strong>and</strong> then repeat.Oxygen driven nebulised bronchodilators should be used in children <strong>with</strong> red features (life threateningcases), those who cannot tolerate a spacer device, or who are worsening despite inhaled treatment• Salbutamol: dose 2-5 years give 2.5mg, <strong>over</strong> 5 years give 5mg• Ipratropium: dose under 12 years give 250micrograms, 12-16 years give 500microgramsBox 3: Guidelines for oral corticosteroids• Give soluble prednisolone by mouth once daily for 3 days• Dose is 20mg for children aged 2-5 years <strong>and</strong> 30-40mg for children aged 5-16 years• If the child has already been taking an oral corticosteroid for more than a few days then increasethe dose to 2mg/kg (max 60mg) for the time needed to bring about rec<strong>over</strong>y• Weaning is unnecessary unless the length of steroid treatment exceeds 14 days• <strong>Children</strong> can continue <strong>with</strong> their usual maintenance inhaled steroids while taking oral steroids• There is limited evidence for the benefit of steroids in pre-school children <strong>with</strong> simple viral inducedwheeze <strong>and</strong> there are potential side effectsBox 4: Guidelines for using peak expiratory flow rate (PEF) in the assessment of <strong>acute</strong> <strong>asthma</strong>Measurement of PEFR can help guide assessment of the severity of exacerbations in children <strong>over</strong>the age of 5 years who are able to perform a PEFR. Take the best of 3 measurements.• PEFR >50% predicted = green (mild to moderate)• PEFR 33-5-% predicted = amber (moderate to severe)• PEFR


![[4] Biopsy Leaflet.pub - Barking, Havering and Redbridge University ...](https://img.yumpu.com/51285530/1/190x134/4-biopsy-leafletpub-barking-havering-and-redbridge-university-.jpg?quality=85)