Antimicrobial Use Guidelines (AMUG) version 21 - UW Health
Antimicrobial Use Guidelines (AMUG) version 21 - UW Health
Antimicrobial Use Guidelines (AMUG) version 21 - UW Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
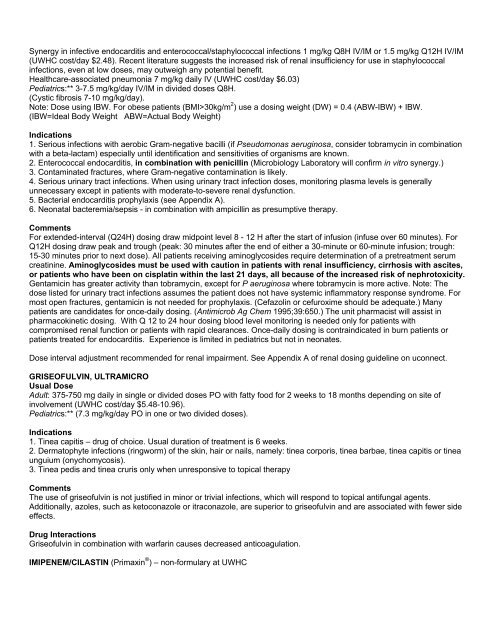
Synergy in infective endocarditis and enterococcal/staphylococcal infections 1 mg/kg Q8H IV/IM or 1.5 mg/kg Q12H IV/IM(<strong>UW</strong>HC cost/day $2.48). Recent literature suggests the increased risk of renal insufficiency for use in staphylococcalinfections, even at low doses, may outweigh any potential benefit.<strong>Health</strong>care-associated pneumonia 7 mg/kg daily IV (<strong>UW</strong>HC cost/day $6.03)Pediatrics:** 3-7.5 mg/kg/day IV/IM in divided doses Q8H.(Cystic fibrosis 7-10 mg/kg/day).Note: Dose using IBW. For obese patients (BMI>30kg/m 2 ) use a dosing weight (DW) = 0.4 (ABW-IBW) + IBW.(IBW=Ideal Body Weight ABW=Actual Body Weight)Indications1. Serious infections with aerobic Gram-negative bacilli (if Pseudomonas aeruginosa, consider tobramycin in combinationwith a beta-lactam) especially until identification and sensitivities of organisms are known.2. Enterococcal endocarditis, in combination with penicillin (Microbiology Laboratory will confirm in vitro synergy.)3. Contaminated fractures, where Gram-negative contamination is likely.4. Serious urinary tract infections. When using urinary tract infection doses, monitoring plasma levels is generallyunnecessary except in patients with moderate-to-severe renal dysfunction.5. Bacterial endocarditis prophylaxis (see Appendix A).6. Neonatal bacteremia/sepsis - in combination with ampicillin as presumptive therapy.CommentsFor extended-interval (Q24H) dosing draw midpoint level 8 - 12 H after the start of infusion (infuse over 60 minutes). ForQ12H dosing draw peak and trough (peak: 30 minutes after the end of either a 30-minute or 60-minute infusion; trough:15-30 minutes prior to next dose). All patients receiving aminoglycosides require determination of a pretreatment serumcreatinine. Aminoglycosides must be used with caution in patients with renal insufficiency, cirrhosis with ascites,or patients who have been on cisplatin within the last <strong>21</strong> days, all because of the increased risk of nephrotoxicity.Gentamicin has greater activity than tobramycin, except for P aeruginosa where tobramycin is more active. Note: Thedose listed for urinary tract infections assumes the patient does not have systemic inflammatory response syndrome. Formost open fractures, gentamicin is not needed for prophylaxis. (Cefazolin or cefuroxime should be adequate.) Manypatients are candidates for once-daily dosing. (Antimicrob Ag Chem 1995;39:650.) The unit pharmacist will assist inpharmacokinetic dosing. With Q 12 to 24 hour dosing blood level monitoring is needed only for patients withcompromised renal function or patients with rapid clearances. Once-daily dosing is contraindicated in burn patients orpatients treated for endocarditis. Experience is limited in pediatrics but not in neonates.Dose interval adjustment recommended for renal impairment. See Appendix A of renal dosing guideline on uconnect.GRISEOFULVIN, ULTRAMICROUsual DoseAdult: 375-750 mg daily in single or divided doses PO with fatty food for 2 weeks to 18 months depending on site ofinvolvement (<strong>UW</strong>HC cost/day $5.48-10.96).Pediatrics:** (7.3 mg/kg/day PO in one or two divided doses).Indications1. Tinea capitis – drug of choice. Usual duration of treatment is 6 weeks.2. Dermatophyte infections (ringworm) of the skin, hair or nails, namely: tinea corporis, tinea barbae, tinea capitis or tineaunguium (onychomycosis).3. Tinea pedis and tinea cruris only when unresponsive to topical therapyCommentsThe use of griseofulvin is not justified in minor or trivial infections, which will respond to topical antifungal agents.Additionally, azoles, such as ketoconazole or itraconazole, are superior to griseofulvin and are associated with fewer sideeffects.Drug InteractionsGriseofulvin in combination with warfarin causes decreased anticoagulation.IMIPENEM/CILASTIN (Primaxin ® ) – non-formulary at <strong>UW</strong>HC