Uitgangsvraag 1: evidence tables Systematic reviews - Oncoline
Uitgangsvraag 1: evidence tables Systematic reviews - Oncoline
Uitgangsvraag 1: evidence tables Systematic reviews - Oncoline
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
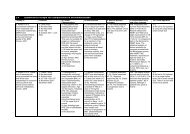
<strong>Uitgangsvraag</strong> 1: <strong>evidence</strong> <strong>tables</strong><strong>Systematic</strong> <strong>reviews</strong>StudyIDMethodPatientcharacteristicsIntervention(s) Results primary outcome Results secondary and otheroutcomesCritical appraisal ofreview qualityFiorica • SR and MA2004 1 • Supported byUniversities and acancer centre• Search date – untilDecember 2002• Search includedMEDLINE &CANCERLIT, (alsonon- English), manualsearches of referencelists, review articles,primary studies,meeting abstracts,bibliographies frombooks, contact withinvestigators• Included studydesigns: RCTs• Number of includedstudies = 6 (N=764)Graham • SR2007 2 • No funding sourcedeclared• Search date – untilOctober 2004• MEDLINE, Pubmed,EMBASE, CINHAL,Cochrane CT &SRCross referencingbibliographies andconsultation withexperts• Included studydesigns: RCTs• Number of studiesincluded = 14 (Sxalone N=1359; CT +Sx N=737; CRT + SxN=372; Sx + CRTN=281)Patients withresectablehistologically provenSCC or ACA of theesophaguswithout metastaticdiseasePatients with locallyadvancedesophageal cancerPreoperative CRT +Sx vs. Sx alone• Sx alone• CRT+ Sx• CT + Sx• Sx + CRT3-year mortality, CRT + Sx vs.Sx alone:OR 0.53, 95%CI 0.31–0.93; p = 0.03(NNT = 10)Subgroup analysis:- ACA: OR 0.24, 95%CI 0.07–0.78;p=0.018- SCC: OR 0.81, 95%CI 0.55–1.19;p=0.29CRT followed by Sx appears to beassociated with the best survival and thelargest expected gain in QALYs.For the first year, the RR (95%CI) of deathfor treatments compared with Sx were:• CRT + Sx: 0.87 (0.75 to 1.02)• CT + Sx: 0.94 (0.82 to 1.08)• Sx + CRT: 1.33 (0.93 to 1.93)The QALYs gained:• Sx alone: 2.07• CRT + Sx: 2.18• CT + Sx: 2.14• Sx + CRT: 1.99• Downstaging, CRT + Sx vs. Sx alone:OR 0.43, 95%CI 0.26–0.72; p = 0.001• Postoperative mortality, CRT + Sx vs.Sx alone: OR 2.10, 95%CI 1.18–3.73;p = 0.01 (NNH = 25)• Overall rate of postoperative adverseevents: 39.4% (137/348) in the CRTgroup vs. 34.3% (123/358) in thesurgery alone group; p=0.16If reduction in utility for multimodalitytreatment increased to 21%, QALYsgained became:• Sx alone: 2.07• CRT + Sx: 2.03• CT + Sx: 1.99• Sx + CRT: 1.85Level of <strong>evidence</strong>: B• Good methodological quality• Includes some small trials, butthis has been adjusted forLevel of <strong>evidence</strong>: A2• Good search method• Documented trial qualityassessment, which was notused• The survival times are drawnfrom studies examining differinghistologies, chemotherapeuticregimens, and radiation doses• The estimates of utility neededto be obtained from anobservational study with alimited number of patients (64)divided between the therapies.It therefore might be unreliable• Resectability was not a specificinclusion criteria in this reviewwhich specifies “locallyadvanced esophageal cancer”
StudyIDMethodPatientcharacteristicsIntervention(s) Results primary outcome Results secondary and otheroutcomesCritical appraisal ofreview qualityLv 2009 4• SR and MA• Source of funding notdeclared, no COIdeclared• Search date - June2009• Searched databases:PubMed and manualsearches,independently and induplicate• Included studydesigns: RCT• Number of includedstudies = 14(N=1737), but seecommentMalthaner2006 5 • SR and MA• Source of funding: noExternal supportsupplied, CochraneReview• Search date: 2006• Searched databasesCENTRAL, MEDLINE,EMBASE,CANCERLIT; nolanguage restrictions• Included studydesigns: RCT• Number of includedstudies = 11(N=2019);8 trials were used forprimary outcomesurvival (N=1729)Patients withresectableesophagealcarcinomaPatients withlocalized potentiallyresectable thoracicesophagealcarcinomaTrials involvingpatients withcarcinomas of thecervical esophaguswere excludedNeoadjuvant CRT +Sx vs. Sx alonePreoperative CT +Sx vs. Sx aloneOverall survival, CRT + Sx vs. Sx: OR(95%CI)• 1.19 (0.94-1.48) for 1-year survival,• 1.33 (1.07-1.65) for 2-year survival,• 1.76 (1.42-2.19) for 3-year survival,• 1.41 (1.06-1.87) for 4-year survival,• 1.64 (1.28-2.12) for 5-year survivalSurvival: 12% risk reduction of mortality forpatients given CT + Sx compared to SxaloneEvidence for treatment effect inconclusive(HR 0.88, 95%CI 0.75-1.04; p=0.15)CRT + Sx vs. Sx: OR (95%CI)• rate of resection 0.82 (0.39-1.73),• rate of complete resection 1.53 (1.33-2.84),• operative mortality 1.78 (1.14-2.78),• all treatment mortality 1.12 (0.89-2.48),• rate of adverse treatment 1.33 (0.94-1.88),• locoregional cancer recurrence 1.38(1.23-1.63),• distant cancer recurrence 1.28 (0.85-1.58),• all cancer recurrence 1.27 (0.86-1.65)• The 5-year survival benefit was mostpronounced when CT and RT weregiven concurrently (OR 1.45, 95%CI1.26-1.79) instead of sequentially (OR0.85, 95%CI 0.64-1.35)• Overall rate of resections: RR 0.96,95%CI 0.92-1.01• Rate of complete resections (R0): RR1.05, 95%CI 0.97-1.15• Tumour recurrence: RR 0.81, 95%CI0.54-1.22• Non-fatal complication rates: RR 0.90,95%CI 0.76-1.06• Risk of toxicity with chemotherapyranged from 11%- 90%Level of <strong>evidence</strong>: B• Moderate quality• Limited search - PubMed onlyalthough manual search done• Good quality appraisal ofstudies and testing forheterogeneity, but no detail ofprimary research• Wrong reporting of p-values!• Study of Walsh is used twice inthe analysis.Level of <strong>evidence</strong>: A2• Good quality SR with metaanalysis• Quality of studies andheterogeneity clearly presentedand taken into account• Hazard ratio used for primaryoutcome in this study tosummarise complete survivalexperience in one analysis
Randomised controlled trialsStudy ID Method PatientcharacteristicsAllum 2009 6Cao 2009 7• RCT• Supported byMedical ResearchCouncil, COIdeclared• Setting:UK and Europeancancer centres• Samplesize: N=802 (CT +Sx: N=400; SxN=402)• Duration –5 yr survival data(median follow up6.1 yrs for Sx and5.9 yrs for CT)• RCT• Funding sourcenot disclosed• Setting:Oncology centre,University, China• Sample size:N=473 (RTn=118, CTn=119, CRTn=118, Sxn=118)• 3 year study• Histologicallyconfirmed, previouslyuntreated, esophagealcancer• Suitable for radicalsurgery with curativeintent• SCC, ACA andundifferentiatedcarcinoma wereincluded• Tumor location:upper, middle,& lowerthirds of theesophagus, gastriccardia• Excluded: postcricoidcancer; comorbidcontraindications toSx or CT• Groups werecomparable• Patients withesophageal SCCstage II or later• Recruited from anongoing clinical trialthat was evaluatingneoadjuvant CRT foresophageal cancer• Comparable groupsIntervention(s) Results primary outcome Results secondary and otheroutcomesCT + Sx vs. Sx aloneCT + Sx:2 cycles of cisplatin80mg/m² IV on day 1,fluorouracil 1000 mg/m²daily as a continuousinfusion over 96 hoursrepeated every 3 weeks;Sx within 3 to 5 weeks ofcompletingchemotherapySx alone:Sx as soon as possible.Sx procedure wasselected by the surgeonaccording to tumour siteand local practicePreoperative RT waspermitted (25 Gy in 5fractions over 1 week,325 Gy in 10 fractionsover 2 weeks, or abiologically equivalentdose)Neoadjuvant RT vs. CTvs. CRT vs. Sx aloneRT group:Daily fractions of 2 Gy(days 1–5, 8–12, 15–19,and 22–26) to a totaldose of 40 GyCT group:PFM regimen:Mitomycin 10 mg/m²/dayon day 1, cisplatin 20mg/m²/ day and 5-fluorouracil 500mg/m²/day ascontinuous infusion over24 h on days 1–5CRT group:CT was carried out atthe first 2 weeks, in the• Overall survival, CT+ Sx vs. Sx:HR 0.84, 95%CI 0.72-0.98;p=0.03• 5-year survival: 23.0% for CT + Sxvs. 17.1% for Sx alone• The treatment effect is consistentin both ACA and SCC, with no<strong>evidence</strong> of heterogeneity oftreatment effect (p=0.81): 5-yearsurvival for ACA 22.6% (CT + Sx)vs. 17.6% (Sx alone), SCC 25.5%(CT + Sx) vs. 17.0% (Sx alone)• 1-year survival: no statisticaldifferences among groups• 3-year survival: RT (69.5%) andCRT (73.3%) statistically differentfrom Sx group (53.4%) (p=0.005and p
Study ID Method PatientcharacteristicsIntervention(s) Results primary outcome Results secondary and otheroutcomessame way as in CTgroup. Combination withconcomitant RT in 4weeks (the same way asin RT group)Critical appraisal of studyqualitySx group:Esophagectomy throughleft thoracotomy withtwo-fieldlymphadenectomyCunningham2006 8 • RCT• Supported byPharmacia forreimbursement ofcost of epirubicinand a grant fromthe MRC; no COI• Setting: hospitalsin UK, theNetherlands,New Zealand,Germany,Singapore andBrazil• Sample size:N=503(perioperative CTN=250, Sx aloneN=253)• Median follow up4 yearsKelsen 20079• RCT• Supported bygrants fromNational CancerinstituteBethesda• Setting: cancercentres in US,UK and Canada• Sample size:N=467 (443 withadequate followup: CT + SxN=216, Sx aloneN=227)• Study duration:median 5 years• Histologically provenACA of the stomachor lower third of theesophagus, stage II orhigher; no <strong>evidence</strong> ofdistant metastases orlocally advancedinoperable disease• Patients of any agewho had a WorldHealth Organization(WHO) performancestatus of 0 or 1• Exclusion criteria:previous cytotoxic CTor RT, uncontrolledcardiac disease, orcreatinine clearanceof 60 ml per minute orless• Group comparability:no significantdifferences betweengroups• Histologicallyconfirmed epidermoidor ACA of theesophagus, includingthe EGJ (stage I, II, orIII, any nodal stage,and no metastasis)• At least 18 years old• Adequate hepatic,renal, and bonemarrow function• Could tolerate theplanned surgicalprocedure• Not received priortherapy for theiresophageal cancerPerioperative CT vs.Sx alonePerioperative CT:3 cycles preoperatively +3 cycles postoperatively;epirubicin (50 mg/m² IVbolus on day 1) +cisplatin (60 mg/m² IVon day 1) + fluorouracil(200 mg/m² daily for 21days by continuous IVinfusion);Sx 3-6 weeks aftercompletion of the3rd cycle of CT;postoperative CTto be initiated 6 to 12weeks after SxSx alone:within 6 weeks afterrandomization in the SxgroupCT + Sx vs. Sx aloneCT + Sx group:3 cycles of CT usingcisplatin and fluorouracil;Patients randomlyassigned to CT who hadstable or respondingdisease, and in whoman R0 resection wasperformed, were toreceive two cycles of CTafter resectionSx alone group:Immediate Sx withagreed surgical• Overall survival, perioperative CTvs. Sx alone: HR for death 0.75;95%CI 0.60-0.93; p=0.009• 5-year survival rate: 36% vs. 23%• Progression-free survival: HR forprogression 0.66; 95%CI 0.53-0.81; p
Study ID Method PatientcharacteristicsStahl 2009 10• RCT• Supported bygrants fromOrtho-Biotechand BaxterDeutschland• Setting:Oncology andSurgeryUniversitydepartmentsGermany• Sample size:N=126 randomlyassigned, N=119evaluated (CT +Sx N=59, CRT +Sx N=60)• 3 yr follow up• Exclusion criteria:patients with tumoursin the cervicalesophagus,supraclavicular/distant metastasis, orT4 tumours• Histologically provenACA of the EGJ (typeI to III )• Untreated patients• Up to 70 yrs• Locally advanceddisease (T3-T4 NXM0)• WHO performancestatus grade 0 to 1,allowing majorsurgery• Normal liver, renaland bone marrowfunctionIntervention(s) Results primary outcome Results secondary and otheroutcomestechniquesFor patients undergoingan R1or R2 resection,RT could be considered(in most cases, CT wasgiven concurrently)CT + Sx vs. CRT + SxCT + Sx group:Induction CT with 2.5courses of PLF:1 course comprised a 6-wk schedule of weeklyfluorouracil (2 g/m², 24-hour infusion) +leucovorin (500 mg/m²,2-hour infusion) +biweekly cisplatin(50mg/m², 1-hourinfusion)CRT + Sx:2 courses of the sameinduction CT (PLF) + 3weeks of combinedCRT: cisplatin (50mg/m², 1-hour infusionIV) on day 1 + 8,etoposide (80 mg/m², 1-hour infusion IV) days 3– 5; RT 30 Gy infractions of 2 Gy, 5fractions per weeksignificantly different)• 59% of Sx only and 63% of CT +Sx underwent R0 resections(p=0.51)• 3-year survival: CT 27.7% (95%CI14.7-42.3%) vs. CRT 47.4%(95%CI 32.8-60.7%), p=0.07; HR0.67, 95%CI 0.41-1.07• Postoperative mortality was nonsignificantlyincreased in the CRTgroup (10.2% vs. 3.8%; p=0 .26)• The number of patients undergoingR0 resection was not differentbetween treatment groups (CT 69.5%vs. CRT 71.5%).• Patients treated with CRT had asignificant higher probability ofshowing pathologic completeresponse (15.6% vs. 2.0%) or tumorfreelymph nodes (64.4% vs. 37.7%)at resectionCritical appraisal of studyqualityLevel of <strong>evidence</strong>: B• Probable central randomization• No blinding• The trial was originally designedas a two-stage adaptive designto recruit > 100 patients per armto prove a hypothesis of asuperiority of 10% in 3 yrsurvival in the CRT arm. Therewas low recruitment,amendment was made to theprotocol and the trial wasclosedSx was performed 3 to 4weeks after the end ofCT or CRTAbbreviations: 95%CI: 95 percent confidence intervals; ACA: adenocarcinoma; COI: conflict of interest; CRT: chemoradiotherapy; CT: chemotherapy; EGJ: esophagogastricjunction; Gy: gray; HR: hazard ratio; MA: meta-analysis; NNH: number needed to harm; NNT: number needed to treat; OR: odds ratio; QA: quality appraisal; QALY: qualityadjustedlife years; RCT: randomized controlled trial; RR: risk ration; RT: radiotherapy; SCC: squamous cell carcinoma; SR: systematic review; Sx: surgery; UK: UnitedKingdom; US: United States.Reference List
1. Fiorica F, Di Bona D, Schepis F, Licata A, Shahied L, Venturi A, et al. Preoperative chemoradiotherapy for oesophageal cancer: A systematic review and metaanalysis.Gut. 2004;53(7):925-30.2. Graham AJ, Shrive FM, Ghali WA, Manns BJ, Grondin SC, Finley RJ, et al. Defining the Optimal Treatment of Locally Advanced Esophageal Cancer: A <strong>Systematic</strong>Review and Decision Analysis. Ann. Thorac. Surg. 2007;83(4):1257-64.3. Jin H-L, Zhu H, Ling T-S, Zhang H-J, Shi R-H. Neoadjuvant chemoradiotherapy for resectable esophageal carcinoma: a meta-analysis. World J Gastroenterol.2009;15(47):5983-91.4. Lv J, Cao X-F, Zhu B, Ji L, Tao L, Wang D-D. Effect of neoadjuvant chemoradiotherapy on prognosis and surgery for esophageal carcinoma. World J Gastroenterol.2009;15(39):4962-8.5. Malthaner RA, Collin S, Fenlon D. Preoperative chemotherapy for resectable thoracic esophageal cancer. Cochrane Database of <strong>Systematic</strong> Reviews. 2006;3.6. Allum WH, Stenning SP, Bancewicz J, Clark PI, Langley RE. Long-term results of a randomized trial of surgery with or without preoperative chemotherapy inesophageal cancer. J Clin Oncol. 2009;27(30):5062-7.7. Cao XF, He XT, Ji L, Xiao J, Lv J. Effects of neoadjuvant radiochemotherapy on pathological staging and prognosis for locally advanced esophageal squamous cellcarcinoma. Dis. Esophagus. 2009;22(6):477-81.8. Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJH, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectablegastroesophageal cancer. N Engl J Med. 2006;355(1):11-20.9. Kelsen DP, Winter KA, Gunderson LL, Mortimer J, Estes NC, Haller DG, et al. Long-term results of RTOG trial 8911 (USA Intergroup 113): a random assignment trialcomparison of chemotherapy followed by surgery compared with surgery alone for esophageal cancer. J Clin Oncol. 2007;25(24):3719-25.10. Stahl M, Walz MK, Stuschke M, Lehmann N, Meyer H-J, Riera-Knorrenschild J, et al. Phase III comparison of preoperative chemotherapy compared withchemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol. 2009;27(6):851-6.