Guidelines for the Treatment of Patients with Neutropenia and Fever
Guidelines for the Treatment of Patients with Neutropenia and Fever
Guidelines for the Treatment of Patients with Neutropenia and Fever
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
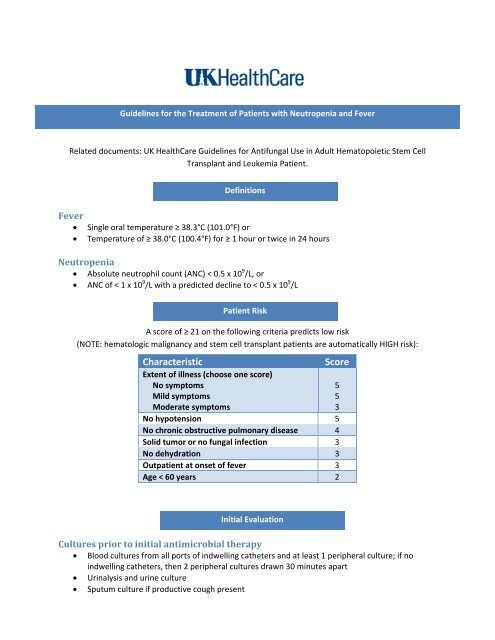
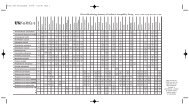
<strong>Guidelines</strong> <strong>for</strong> <strong>the</strong> <strong>Treatment</strong> <strong>of</strong> <strong>Patients</strong> <strong>with</strong> <strong>Neutropenia</strong> <strong>and</strong> <strong>Fever</strong>Related documents: UK HealthCare <strong>Guidelines</strong> <strong>for</strong> Antifungal Use in Adult Hematopoietic Stem CellTransplant <strong>and</strong> Leukemia Patient.Definitions<strong>Fever</strong>• Single oral temperature ≥ 38.3°C (101.0°F) or• Temperature <strong>of</strong> ≥ 38.0°C (100.4°F) <strong>for</strong> ≥ 1 hour or twice in 24 hours<strong>Neutropenia</strong>• Absolute neutrophil count (ANC) < 0.5 x 10 9 /L, or• ANC <strong>of</strong> < 1 x 10 9 /L <strong>with</strong> a predicted decline to < 0.5 x 10 9 /LA score <strong>of</strong> ≥ 21 on <strong>the</strong> following criteria predicts low risk(NOTE: hematologic malignancy <strong>and</strong> stem cell transplant patients are automatically HIGH risk):CharacteristicPatient RiskExtent <strong>of</strong> illness (choose one score)No symptomsMild symptomsModerate symptomsScoreNo hypotension 5No chronic obstructive pulmonary disease 4Solid tumor or no fungal infection 3No dehydration 3Outpatient at onset <strong>of</strong> fever 3Age < 60 years 2553Initial EvaluationCultures prior to initial antimicrobial <strong>the</strong>rapy• Blood cultures from all ports <strong>of</strong> indwelling ca<strong>the</strong>ters <strong>and</strong> at least 1 peripheral culture; if noindwelling ca<strong>the</strong>ters, <strong>the</strong>n 2 peripheral cultures drawn 30 minutes apart• Urinalysis <strong>and</strong> urine culture• Sputum culture if productive cough present
• If watery diarrhea present, stool culture <strong>for</strong> routine pathogens (x1), ova <strong>and</strong> parasites (x1) <strong>and</strong> C.difficileLaboratory/Radiology evaluation• Electrolytes• Serum creatinine <strong>and</strong> blood urea nitrogen• Liver enzymes• CBC <strong>with</strong> differential• Chest X‐Ray if symptoms dictateSubsequent EvaluationCultures prior to changes in antimicrobial <strong>the</strong>rapy• No more than 2 sets <strong>of</strong> blood cultures per 24 hour period• If initial urine/sputum/stool cultures negative <strong>and</strong> no new symptoms present, do not repeatculturesLaboratory reassessment• Reassess labs at least every 3 days, more frequent if risk <strong>for</strong> nephrotoxicity (ex: amphotericin,aminoglycosides)Initial Antimicrobial TherapyIf indwelling ca<strong>the</strong>ter is present <strong>and</strong> appears infected, remove ca<strong>the</strong>ter <strong>and</strong> beginadministration <strong>of</strong> antibiotics.For inpatients, all new antimicrobial agents should be ordered, prepared, <strong>and</strong> administeredSTAT.Oral Therapy (a consideration <strong>for</strong> lowrisk patients)• Lev<strong>of</strong>loxacin 750mg daily +amoxicillin/clavulanate 875mg twice a dayIntravenous Therapy• Cefepime 2g every 8 hours OR Piperacillin/tazobactam 4.5g every 6 hours• Consider adding tobramycin to <strong>the</strong> above regimen (contact pharmacist <strong>for</strong> dosing)• Consider adding vancomycin when at least one <strong>of</strong> <strong>the</strong> following conditions is present (contactpharmacist <strong>for</strong> dosing)o Clinically suspected serious ca<strong>the</strong>ter‐related infections (e.g., bacteremia, cellulitis)o Colonization <strong>with</strong> penicillin‐ <strong>and</strong> cephalosporin‐resistant S. pneumoniae or methicillinresistantStaphylococcus species (ex: MRSA, MRSE)o Positive results <strong>of</strong> blood culture <strong>for</strong> gram‐positive bacteria be<strong>for</strong>e final identification <strong>and</strong>susceptibility testing
oooHypotension or o<strong>the</strong>r evidence <strong>of</strong> cardiovascular instabilitySubstantial mucositisProphylaxis <strong>with</strong> quinolones <strong>for</strong> afebrile neutropenic patients be<strong>for</strong>e onset <strong>of</strong> fever• For patients <strong>with</strong> serious beta‐lactam allergieso Aztreonam 2g every 8 hours + vancomycin (contact pharmacist <strong>for</strong> dosing)• For patients known to be colonized <strong>with</strong> multidrug‐resistant bacteria,o Tailor <strong>the</strong>rapy accordinglySubsequent Antimicrobial TherapyReassess after 35 days <strong>of</strong> treatmentIf Afebrile• Clinically stable, cultures positive:o Caution should be used in prescribing antibiotics <strong>for</strong> a single blood culture positive <strong>for</strong> S.epidermidis <strong>with</strong>out clinical signs <strong>of</strong> infection (consider contamination)o If cultures reveal a source <strong>of</strong> infection, alter antibiotics based on cultures <strong>and</strong> treat <strong>for</strong> ast<strong>and</strong>ard length <strong>of</strong> time• Clinically stable, cultures negative:ooContinue antibiotics until ANC > 500 or 5‐7 days after last fever (maximum 3 weeks)Consider switching to oral <strong>the</strong>rapy• Lev<strong>of</strong>loxacin 750 mg daily plus amoxicillin‐clavulanate 875 mg twice a dayIf Febrile• Consider o<strong>the</strong>r factors or sources <strong>of</strong> infectiono Nonbacterial infectiono Resistant or slow‐responding bacterial infectiono Secondary infectiono Inadequate serum <strong>and</strong> tissue levels <strong>of</strong> <strong>the</strong> antibiotic(s)o Adverse medication effecto Infection at avascular site (abscesses, or ca<strong>the</strong>ters)• Clinically stable, cultures negativeo Continue antibiotics until ANC > 500 (maximum 3 weeks)o Consider switching to oral <strong>the</strong>rapy• Lev<strong>of</strong>loxacin 750 mg daily plus amoxicillin‐clavulanate 875 mg twice a dayo If included in primary treatment, consider discontinuation <strong>of</strong> vancomycin• Clinically unstable, cultures negative• Consult Infectious Diseases• Consider change or addition <strong>of</strong> antibiotic• Consider addition <strong>of</strong> an antifungalooVoriconazole 6mg/kg every 12 hours x2 doses, <strong>the</strong>n 4mg/kg every 12 hours ORLiposomal Amphotericin B 3mg/kg daily. This is <strong>the</strong> primary option <strong>for</strong> patientswho have received posaconazole prophylaxis prior to becoming febrile.
Major Reference:Hughes, et al. 2002 <strong>Guidelines</strong> <strong>for</strong> <strong>the</strong> Use <strong>of</strong> Antimicrobial Agents in Neutropenic <strong>Patients</strong> <strong>with</strong> Cancer.Clin Inf Dis 2002;34:730‐51.