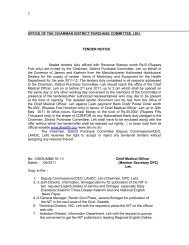
Tender Notice Dt - Department of Health , J&K
Tender Notice Dt - Department of Health , J&K
Tender Notice Dt - Department of Health , J&K
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
g) The Insurer needs to file a report to nodal agency explaining reasonsfor denial <strong>of</strong> every such claim.h) Denial <strong>of</strong> authorization (DAL)/guarantee <strong>of</strong> payment is by no meansdenial <strong>of</strong> treatment by the health facility. The health care providershall deal with such case as per their normal rules and regulations.i) Authorisation letter [AL] will mention the authorization number andthe amount guaranteed as a package rate for such procedure forwhich package has not been fixed earlier. Provider must see thatthese rules are strictly followed.j) The guarantee <strong>of</strong> payment is given only for the necessary treatmentcost <strong>of</strong> the ailment covered and mentioned in the request forAuthorisation letter (RAL) for hospitalization.k) The entry on the smart card for blocking as well at discharge wouldrecord the authorization number as well as package amount agreedupon by the hospital and insurer. Since this would not be available inthe package list on the computer, it would be entered manually by thehospital.l) In case the balance sum available is considerably less than thePackage, provider should follow their norms <strong>of</strong> deposit/running billsetc. However provider shall only charge the balance amount againstthe package from the beneficiary. Insurer upon receipt <strong>of</strong> the bills anddocuments would release the guaranteed amount.m) Insurer will not be liable for payments in case the informationprovided in the “request for authorization letter” and subsequentdocuments during the course <strong>of</strong> authorization, is found incorrect ornot disclosed.Note: In the cases where the beneficiary is admitted in a hospital duringthe current policy period but is discharged after the end <strong>of</strong> the policy period,the claim has to be paid by the insurance company which is operatingduring the period in which beneficiary was admitted.14. Repudiation <strong>of</strong> claim:In case <strong>of</strong> any claim is found untenable, the insurer shall communicatereasons in writing to the Designated Authority <strong>of</strong> the State/ Nodal Agency,<strong>Health</strong> provider for this purpose with a copy to the beneficiary. Such claimsshall be reviewed by the Central/State/ District Committee on monthly/quarterly basis.15. Delivery <strong>of</strong> Services by Intermediaries:The Insurer may enter into service agreement(s) with one or more19