Demographic and Health Surveys Methodology - Measure DHS
Demographic and Health Surveys Methodology - Measure DHS
Demographic and Health Surveys Methodology - Measure DHS
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
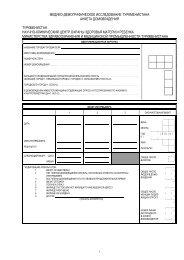
H<strong>and</strong>ling of Missing ValuesSiblings whose maternal status at the time of death are unknown to the respondent or are missing in thedata set are allocated as maternal deaths in the proportion they have to all deaths (e.g., if unknown statusdeaths are 10% of all deaths in an age group of respondent, then the number of maternal deaths in that agegroup is increased by 10%).Siblings whose maternal status at the time of death is unknown to the respondent or is missing in the dataset are allocated to maternal deaths in the proportion they are to deaths of any maternal status. For eachage group of respondents, the number of deaths of known maternal status is divided by the number ofdeaths of any status to get the proportion of maternal deaths. This proportion is then multiplied by thenumber of deaths of unknown status to calculate the number of deaths to add to the known maternaldeaths to get the total number of maternal deaths in each respondent age group.Notes <strong>and</strong> ConsiderationsThe indirect method of calculating maternal mortality lifetime risk <strong>and</strong> the maternal mortality ratio isbased on applying models of fertility <strong>and</strong> maternal mortality rates. The number of sisters of respondentsis converted into “sister units of risk” equivalent to women-years of exposure to the risk of mortality inthe reproductive age (i.e. since age 15 years) by multiplication with adjustment factors calculated on amodel age-fertility distribution. The conversion from the lifetime risk of maternal mortality to thematernal mortality ratio assumes a model pattern of maternal mortality by age <strong>and</strong> by parity.“Because the method relies heavily on a number of assumptions about the relationshipsbetween fertility <strong>and</strong> age-specific maternal mortality, it should not be used in settingswhere levels of fertility are low (Total Fertility Rate below 3), or where there have beenrecent <strong>and</strong> marked declines in fertility, or where major migration has occurred. While themethod is relatively simple <strong>and</strong> inexpensive to use, the overall results relate to a pointaround 10-12 years prior to the survey, a major disadvantage. However, it is possible tocalculate estimates for more recent periods by limiting the upper age of the respondentsto, say, adults aged below 30 years old. In this case, the overall maternal mortalityestimate would relate to a period some seven years prior to the survey. The disadvantageof limiting the upper age of respondents is, however, that a large number of householdsneed to be visited to achieve the desired sample size of adult respondents”. [World <strong>Health</strong>Organisation, 1997. The sisterhood method for estimating maternal mortality:Guidance for potential users. WHO/RHT/97.28].The <strong>DHS</strong> maternal mortality module questionnaire collects information from respondents (female <strong>and</strong>male) about the maternal status of the death of their sisters born to the same mother by asking if the sisterdied while pregnant, during delivery or within two months after the end of a pregnancy or a childbirth.Younger (<strong>and</strong> male) respondents may not know that their older sister was even pregnant if the sister wasseveral years older or died during pregnancy or from an induced abortion, thus biasing maternal mortalityrates downward. Women who intend to have an induced abortion may also not disclose their pregnancystatus to family members. On the other h<strong>and</strong>, deaths due to non-maternal causes, such as accidents <strong>and</strong>illnesses, will be included as maternal deaths if they occurred during pregnancy or within two monthsafter the end of the pregnancy or childbirth. Simulation models show that up to one-third of classified asmaternal may not be due to maternal causes, resulting in an upward bias. The final result of both thesebiases, which operate simultaneously, is unknown.Guide to <strong>DHS</strong> Statistics 159 Updated September 2006






![Obtaining Informed Consent for HIV Testing [QRS4] - Measure DHS](https://img.yumpu.com/49850117/1/190x245/obtaining-informed-consent-for-hiv-testing-qrs4-measure-dhs.jpg?quality=85)