2011 - UCSF School of Medicine - University of California, San ...
2011 - UCSF School of Medicine - University of California, San ...
2011 - UCSF School of Medicine - University of California, San ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Education Day<strong>2011</strong>Monday, April 25, <strong>2011</strong>Millberry Union Conference Center
<strong>UCSF</strong> Education Day <strong>2011</strong>The Haile T. Debas Academy <strong>of</strong> Medical Educatorsand the Office <strong>of</strong> Medical Education present:THE 10 th ANNUAL EDUCATION DAYMillberry Union Conference CenterMonday, April 25, <strong>2011</strong><strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco<strong>School</strong> <strong>of</strong> <strong>Medicine</strong>Welcome 1Schedule <strong>of</strong> Events 2Cooke Award Winners 4Keynote Address Information 5Abstracts for Oral Presentations 7Abstracts for Poster Presentations 13Workshop Descriptions 41Index by Author 42<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>i
<strong>UCSF</strong> Education Day <strong>2011</strong>ScholarshipWorking GroupJody Steinauer, MD, ChairLouise Aronson, MD, MFAAmin Azzam, MD, MADavid Daikh, MD, PhDMichelle Lin, MDTerrence Liu, MDPatricia O'Sullivan, EdDMaxine Papadakis, MDJason Satterfield, PhDJeffrey Tabas, MDArianne Teherani, PhDLeadership and StaffMolly Cooke, MDDirectorHarry Hollander, MDAssociate DirectorCynthia AsheManagerJames BeaudreauSr. Programs AnalystKathleen LandPrograms AnalystAcademy <strong>of</strong> Medical Educators4 Koret Way, LR-102, Box 0563<strong>San</strong> Francisco, CA 94143-0563(415) 514.2282 | (415) 514.9264 (Fax)www.medschool.ucsf.edu/academyMembersShelley Adler, PhDLouise Aronson, MD, MFAColette Auerswald, MD, MSMeg Autry, MDAmin Azzam, MD, MARobert Baron, MD, MSTimothy Berger, MDMartin Bogetz, MDRichard Breiman, MDMarek Brzezinski, MD, PhDAndre Campbell, MDAnna Chang, MDHuiju Carrie Chen, MD, MSEdLee-may Chen, MDRachel Chin, MDPeter Chin-Hong, MD, MASCalvin Chou, MD, PhDDaniel Ciccarone, MD, MPHMolly Cooke, MDDavid Daikh, MD, PhDRobert Dar<strong>of</strong>f, MDGurpreet Dhaliwal, MDMohammad Diab, MDDavid Elkin, MDAlicia Fernandez, MDTracy Fulton, PhDAlan Gelb, MDAndrew Goldberg, MD, MSCEElizabeth Harleman, MDMichael Harper, MDKaren Hauer, MDHarry Hollander, MDKatherine Hyland, PhDDavid Irby, PhDRebecca Jackson, MDSharad Jain, MDC. Bree Johnston, MDS. Andrew Josephson, MDKatherine Julian, MDTimothy Kelly, MDShieva Khayam-Bashi, MDMarieke Kruidering-Hall, PhDAnda Kuo, MDCindy Lai, MDHarry Lampiris, MDMichelle Lin, MDTerrence Liu, MDHelen Loeser, MD, MScDaniel Lowenstein, MDJohn Maa, MDKevin Mack, MD, MSAlma Martinez, MD, MPHSusan Masters, PhDMarcia McCowin, MDCarol Miller, MDIgor Mitrovic, MDJessica Muller, PhDAndrew Murr, MDMaxine Papadakis, MDManuel Pardo Jr., MDJ. Colin Partridge, MD, MPHMichael Peterson, MDAnn Poncelet, MDSusan Promes, MDMichael Rabow, MDPatricia Robertson, MDDana Rohde, PhDMark Rollins, MD, PhDGeorge Rutherford III, MDHenry <strong>San</strong>chez, MDJason Satterfield, PhDGeorge Sawaya, MDNiraj Sehgal, MD, MPHBradley Sharpe, MDWilliam Shore, MDWade Smith, MD, PhDJody Steinauer, MDJeffrey Tabas, MDLowell Tong, MDKimberly Topp, PT, PhD<strong>San</strong>drijn van Schaik, MD, PhDMargo Vener, MD, MPHMaria Wamsley, MDElisabeth Wilson, MD, MPHLisa Winston, MDJohn Young, MD, MPPLeslie Zimmerman, MD© <strong>2011</strong>, <strong>University</strong> <strong>of</strong> <strong>California</strong> RegentsiiThe Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Welcome to Education DayDear Friends,On behalf <strong>of</strong> The Haile T. Debas Academy <strong>of</strong> Medical Educators and the Office <strong>of</strong>Medical Education, we are proud to present the tenth annual Education Day, an eventthat showcases the scholarly work <strong>of</strong> the <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>’s faculty, residents,and students.The program covers a variety <strong>of</strong> important research questions and innovations in medicaleducation. Following a blinded peer review <strong>of</strong> all abstract submissions, the Academy’sScholarship Working Group, which plans Education Day, has selected 51 submissions tobe featured at Education Day. Six <strong>of</strong> these submissions have been selected as oralpresentations based upon their quality and collective relevance to the largest audience <strong>of</strong>medical educators.We are also pleased to <strong>of</strong>fer a number <strong>of</strong> special programs. We welcome Northwestern<strong>University</strong>’s Diane B. Wayne, MD, as this year’s visiting pr<strong>of</strong>essor, who will delivertoday’s keynote address, Use <strong>of</strong> Medical Education Research to Improve Patient CareQuality. And in recognition <strong>of</strong> the recent opening <strong>of</strong> <strong>UCSF</strong>’s new Teaching and LearningCenter, we have also developed several workshops that demonstrate the cutting-edgeeducational technologies that are available to the <strong>UCSF</strong> community.This will be our fifth year presenting the Academy’s Cooke Awards for the Scholarship <strong>of</strong>Teaching and Learning. Please join us for the awards announcement at the conclusion <strong>of</strong>today’s plenary session.We extend a very special thank you to our community <strong>of</strong> medical educators forcontributing so generously to this year’s Education Day. This program provides just asmall glimpse <strong>of</strong> the creativity and excitement <strong>of</strong> their scholarly work here at <strong>UCSF</strong>. Wehope you enjoy the program.Jody Steinauer, MD, MASChair, Scholarship Working GroupMolly Cooke, MDDirector, Academy <strong>of</strong> Medical Educators<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 1
<strong>UCSF</strong> Education Day <strong>2011</strong>Schedule <strong>of</strong> EventsMorning Sessions8:00-9:30 am Meet the Visiting Pr<strong>of</strong>essor:Interactive session featuring a moderated discussion aroundpre-selected themes between <strong>UCSF</strong> faculty and Diane B.Wayne, MD, this year's Education Day keynote speaker.Golden Gate RoomMillberry Union10:00 am-noon Oral Presentations:A Randomized Trial <strong>of</strong> Reflective Learning Guidelines andFeedback among Third Year Medical StudentsLouise Aronson, MD, MFAGolden Gate RoomMillberry UnionBlended Learning: The New Wave <strong>of</strong> Faculty DevelopmentKatherine Hyland, PhDCompetency-Based Curricula for the Health Pr<strong>of</strong>essions in TanzaniaHelen Loeser, MD, MScLongitudinal Interpr<strong>of</strong>essional Curriculum Well Received byFirst-Year Health Pr<strong>of</strong>essions StudentsJennifer Staves, MS3What's Really So Different about Longitudinal IntegratedClerkships (LICs) and Block Clerkships? Findings from aMulti-Center Observational, Work Sampling StudyBridget O'Brien, PhDWriting for Change: Training Residents in Health PolicyAdvocacy through NarrativeLouise Aronson, MD, MFA2 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Afternoon Sessions12:15-12:45 pm Keynote Address:Use <strong>of</strong> Medical Education Research to Improve Patient Care QualityDiane B. Wayne, MD12:50-1:00 pm Cooke Award for the Scholarship <strong>of</strong> Teaching & Learning:Louise Aronson, MD, MFAHelen Loeser, MD, MScBridget O'Brien, PhDGolden Gate RoomMillberry UnionGolden Gate RoomMillberry Union1:00-2:30 pm Moderated Walkaround Poster Session City Lights RoomMillberry Union2:30-3:30 pm Unmoderated Poster Viewing City Lights RoomMillberry Union3:45-5:00 pm Concurrent Breakout Workshops (takes place on the second floor <strong>of</strong><strong>UCSF</strong> library in the Teaching and Learning Center):Leveraging Technology for EducationAmin Azzam, MD, MA; Ryan Brazell; Sean McClelland; ChristianBurke; Renee Courey, PhD; Louise Aronson, MD, MFAPoster Presentations and PrizesLouise Aronson, MD, MFA; Patricia O'Sullivan, EdDScholarship <strong>of</strong> SimulationDiane B. Wayne, MD; <strong>San</strong>drijn van Schaik, MD; Jody Steinauer, MDTeaching andLearning CenterCL-211/212CL-220CL-213/214<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 3
<strong>UCSF</strong> Education Day <strong>2011</strong>Cooke Award for the Scholarship<strong>of</strong> Teaching and LearningThe Academy is pleased to continue the Cooke Award for the Scholarship <strong>of</strong> Teaching and Learning, established in 2007to recognize outstanding scholarly works presented at Education Day. All submissions to Education Day were eligible forthese awards, which are accompanied by a certificate and honorarium. Top-scoring projects were nominated for theaward following a blinded peer review <strong>of</strong> all abstract submissions. Award winners were determined by a ballot in whichScholarship Working Group members ranked the blinded abstracts, excluding those in which they were involved.Please join us in congratulating the <strong>2011</strong> recipients:Louise Aronson, MD, MFAFor her submission as first author in Writing for Change:Training Residents in Health Policy Advocacy throughNarrativeHelen Loeser, MD, MScFor her submission as first author in Competency-BasedCurricula for the Health Pr<strong>of</strong>essions in TanzaniaBridget O'Brien, PhDFor her submission as first author in What's Really SoDifferent about Longitudinal Integrated Clerkships (LICs)and Block Clerkships? Findings from a Multi-CenterObservational, Work Sampling Study4 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Keynote AddressUse <strong>of</strong> Medical Education Researchto Improve Patient Care QualityDiane B. Wayne, MDDr. Wayne is passionate about linking education toimproved quality <strong>of</strong> care. In this lecture she will discussspecific examples <strong>of</strong> medical education research astranslational science and features <strong>of</strong> highly successfuleducational research programs.Dr. Wayne is a clinician-educator at Northwestern <strong>University</strong>. She is the Vice Chair <strong>of</strong>Education in the Department <strong>of</strong> <strong>Medicine</strong> and an Associate Pr<strong>of</strong>essor <strong>of</strong> <strong>Medicine</strong>. Shehas been the Internal <strong>Medicine</strong> Residency Program Director since 2001. During hertenure she has focused on enhancing the national reputation <strong>of</strong> Northwestern's internalmedicine training programs and developing medical education research programs in thedepartment. Her other commitment has been to promoting diversity. For the past twoyears, more than 20 percent <strong>of</strong> incoming interns in the Department <strong>of</strong> <strong>Medicine</strong> havebeen from groups traditionally underrepresented in medicine. Dr. Wayne's researchinterests include simulation-based education, standard setting and competencyassessment <strong>of</strong> students, residents and fellows.Dr. Wayne has received numerous awards, including the 2007 National Award forMedical Education Scholarship from the Society <strong>of</strong> General Internal <strong>Medicine</strong> and the2007 Thomas Hale Ham Award for New Investigators from the Research in MedicalEducation Committee (RIME) <strong>of</strong> the AAMC. She was a 2010 recipient <strong>of</strong> the ParkerPalmer "Courage to Teach" National Program Director Award from the AccreditationCouncil <strong>of</strong> Graduate Medical Education. She has been a Deputy Editor <strong>of</strong> the Journal <strong>of</strong>General Internal <strong>Medicine</strong> since 2006.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 5
<strong>UCSF</strong> Education Day <strong>2011</strong>6 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>A Randomized Trial <strong>of</strong> ReflectiveLearning Guidelines and FeedbackAmong Third Year Medical StudentsLouise Aronson, MD, MFA,aronsonl@medicine.ucsf.edu; Brian Niehaus MD,Brian.Niehaus@ucsf.edu; Laura Hill-Sakurai, MD,HillSakL@fcm.ucsf.edu; Cindy Lai, MD,CLai@medicine.ucsf.edu; Patricia O'Sullivan, EdD,patricia.osullivan@ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Competencies, Evaluation <strong>of</strong>Programs and Curricula, Feedback, ReflectionPurpose: To assess the impact <strong>of</strong> reflective learningguidelines and feedback, individually and together, onthe reflective ability demonstrated by medical students inwritten reflection exercises.Background: In response to national mandates,educators are increasingly incorporating reflection intotheir teaching. However, review <strong>of</strong> medical studentreflections from <strong>UCSF</strong> and elsewhere revealed that mostconsisted <strong>of</strong> anecdotes with few <strong>of</strong> the educationalcomponents described in the literature. We hypothesizethat learners do not reflect in an educationally useful waybecause we have not trained them to do so.Methods: We conducted a randomized, controlled trial<strong>of</strong> the impact <strong>of</strong> reflective learning guidelines and facultyfeedback on reflective skills. All third year medicalstudents wrote reflections on pr<strong>of</strong>essionalism after their1st, 3rd and final clerkships. In a 2x2 design, half thestudents received reflective learning guidelines and halfdid not, and half in each <strong>of</strong> these groups receivedfeedback on both reflective skill and reflection contentand half received feedback on content alone. Reflectionswere scored by trained raters (r= 0.89) using apreviously validated 0 - 6 point rubric. We conducted ananalysis <strong>of</strong> covariance using 1st scores as the covariateand final scores as the dependent variable.Results: Mean reflection scores were 3.81 (sd=1.9)using guidelines and 2.22 (sd=.89) without guidelines(p
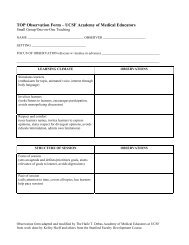
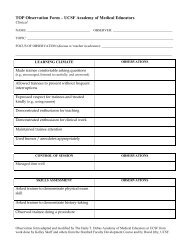
<strong>UCSF</strong> Education Day <strong>2011</strong>TOP mentees will continue to evaluate their mentors'performance.Dissemination: We plan to publish this tool on Med EdPortal and present at national medical educationmeetings.Reflective critique: A team <strong>of</strong> eight AME membersprovided input. This project was presented at the TLCSopening, and valuable input was received. After welaunch the training module, adjustments will be madebased on feedback from users.Competency-Based Curricula for theHealth Pr<strong>of</strong>essions in TanzaniaHelen Loeser, MD, MSc, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,Helen.Loeser@ucsf.edu; Judy Martin-Holland, PhD,MPA, RN, CS, FNP <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Nursing,judy.martin-holland@nursing.ucsf.edu; SharonYoumans, PharmD, MPH, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Pharmacy,youmanss@pharmacy.ucsf.edu; Peter Loomer, DDS,PhD, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Dentistry, peter.loomer@ucsf.edu;Eligius Lyamuya, MD, Muhimbili <strong>University</strong> <strong>of</strong> Health andAllied Sciences, eligius_lyamuya@yahoo.com; PatriciaO’Sullivan, EdD, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,OSullivanP@medsch.ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Competencies, CurricularInnovation, Global Health, Interpr<strong>of</strong>essional EducationPurpose: A strategic Tanzania-U.S. universitypartnership, formed to optimize the impact <strong>of</strong> healthpr<strong>of</strong>essions graduates on health outcomes in Tanzania,led to an interpr<strong>of</strong>essional collaboration to developcompetency-based curricula.Background: Competency-based education was newlymandated inTanzania and Muhimbili <strong>University</strong> <strong>of</strong> Healthand Allied Sciences (MUHAS) embarked upon a reviewand revision <strong>of</strong> their <strong>Medicine</strong>, Dentistry, Nursing,Pharmacy, and Public Health curricula. MUHAS soughtexpertise in undertaking the revision and incorporatingcompetencies into their teaching and assessment. Aninterpr<strong>of</strong>essional team from <strong>UCSF</strong> schools <strong>of</strong> dentistry,medicine, nursing and pharmacy provided consultation.Methods: Curriculum revision began in 2008 andincluded these key steps[1]: (1) extensive stakeholderconsultation; (2) determination <strong>of</strong> Tanzania's healthpriorities; (3) identification <strong>of</strong> competencies necessaryfor Tanzanian health pr<strong>of</strong>essionals; (4) faculty training incompetency-based education; (5) individual courserevision by faculty and (6) demonstrations by <strong>UCSF</strong>collaborators. Data and process that supported thesesteps included national surveys, focus groups,workshops and retreats.Evaluation Plan: By <strong>2011</strong>, curricula in all MUHASschools will be revised to include competency-basedobjectives, new strategies for instruction and studentassessment. Opportunities will be introduced for activelearning, clinical experience and structured fieldwork.Stakeholder consultation and periodic assessment <strong>of</strong>program outcomes by surveys <strong>of</strong> graduates andemployers are planned.Dissemination: MUHAS and <strong>UCSF</strong> faculty arepresenting this curriculum work and outcomes locally,regionally, and internationally. A website is inpreparation for sharing results, and supporting additionalregional and international collaborations.Reflective critique: There is ongoing exchange from allpartnership members evaluating progress to guidedecisions for next steps. MUHAS will pilot some aspects<strong>of</strong> the curriculum to ease the transition to the newapproach. Interpr<strong>of</strong>essional education collaborationshave been productive at MUHAS and <strong>UCSF</strong>.References:1. H. Loeser, P. O'Sullivan, D. Irby. Leadership Lessons fromCurricular Change at <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>. Acad. Med. 82(4):324-330. April 2007Longitudinal Interpr<strong>of</strong>essionalCurriculum Well Received by First-Year Health Pr<strong>of</strong>essions StudentsJennifer Staves, MS3, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>;Alexandria Cerri, Sacred Heart Cathedral PreparatoryHigh <strong>School</strong>; Susan Hyde, DDS, MPH, PhD, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> Dentistry; Brian Alldredge, PharmD, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> Pharmacy; Sharon , PharmD, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong>Pharmacy; Jeff Kilmer, MA, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Nursing;Dorothy Perry, PhD, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Dentistry; HelenLoeser, MD, MSc, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>; KimberlyTopp, PhD, PT, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, Department<strong>of</strong> Physical Therapy; H. Carrie Chen, MD, MSEd, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> <strong>Medicine</strong>Areas abstract covers: UMEDomain(s) addressed: Communication, CurricularInnovation, Evaluation <strong>of</strong> Programs and Curricula,Interpr<strong>of</strong>essional EducationPurpose: We describe the implementation andevaluation <strong>of</strong> a novel interpr<strong>of</strong>essional curriculum forfirst-year dentistry, medicine, nursing, pharmacy, andphysical therapy students.Background: Promoting interpr<strong>of</strong>essional education(IPE) early in the training <strong>of</strong> health pr<strong>of</strong>essions studentscan help lay strong foundations for effective teamwork in<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 9
<strong>UCSF</strong> Education Day <strong>2011</strong>their future careers. We implemented a required yearlongcurriculum for all first-year health pr<strong>of</strong>essionsstudents. The curriculum included 2 half-day events(“IPE Days 1 & 2”) during which students collaborated ininterpr<strong>of</strong>essional teams <strong>of</strong> 9-10 students to addresshealthcare disparities and team communicationchallenges. Student teams also responded to four triggerquestions throughout the year using an online discussionforum.Methods: Students completed satisfaction surveys atthe end <strong>of</strong> each IPE Day and year using a 5-point Likertscale (1=strongly disagree, 5=strongly agree). Wedetermined utilization <strong>of</strong> the online forum by calculatingand categorizing student postings and identifying majorthemes.Results: 477 students participated in the curriculum.Students rated both IPE Days 1 and 2 as effective (Day1=4.06, Day 2=3.92) and relevant to their education(4.30, 4.06). 423 (88.9%) students participated in theonline forum generating 1205 postings. Studentresponse rate to the online questions decreased from83% to 26% over the year. Pharmacy students had thehighest online participation rate (92% responded at leastonce) and nursing the lowest (81%, p=0.02). Majordiscussion themes are presented.Discussion: We successfully implemented a novelinterpr<strong>of</strong>essional curriculum which was well received byfirst-year health pr<strong>of</strong>essions students. However, use <strong>of</strong>the online forums declined over time, suggesting theneed for further curricular refinements to sustainparticipation.Reflection: Input from faculty from all participatingschools was critical to the success <strong>of</strong> thisinterpr<strong>of</strong>essional initiative. Student feedback wasgathered via online and paper surveys, and was used toinform the expansion and refinement <strong>of</strong> the curriculum.What's Really So Different aboutLongitudinal Integrated Clerkships(LICs) and Block Clerkships?Findings from a Multi-CenterObservational, Work Sampling StudyBridget O'Brien, PhD, <strong>UCSF</strong>, bridget.obrien@ucsf.edu;Ann Poncelet, MD, <strong>UCSF</strong>, ann.poncelet@ucsf.edu; LoriHansen, MD, <strong>University</strong> <strong>of</strong> South Dakota, <strong>San</strong>ford<strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, lori.hansen@usd.edu; David Hirsh,MD, Harvard Medical <strong>School</strong>, dhirsh@challiance.org;Barbara Ogur, MD, Cambridge Hospital, HarvardMedical <strong>School</strong>; Edward Krupat, PhD, Harvard Medical<strong>School</strong>; Erik Alexander, MD, Harvard Medical <strong>School</strong>,ealexander@partners.org; Iris Ma, <strong>UCSF</strong>; Karen Hauer,MD, <strong>UCSF</strong>, khauer@medicine.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, Longitudinal Educational ActivitiesPurpose: To compare direct and independent patientcare activities <strong>of</strong> longitudinal integrated clerkship (LIC)and block students at three medical schools.Background: Studies suggest that students in LICsmaintain more patient-centeredness throughout the yearcompared to students in block clerkships. Theexplanation may rest in students’ involvement in directpatient care activities.Methods: We conducted a yearlong, observational,work sampling study at 3 US medical schools with LICand block clerkships. Trained observers documentedstudents’ activities and level <strong>of</strong> participation every 10minutes for 4-hour periods in internal medicine andobstetrics-gynecology. In this analysis, we comparestudents’ participation in direct patient care activities inthe last three months <strong>of</strong> the clerkship year. Each studentwas observed 1-4 times. The observation session is theunit <strong>of</strong> analysis. Data analysis included calculatingmedian percentages <strong>of</strong> session time and Mann-WhitneyU-tests comparing percentage <strong>of</strong> session time that LICand block students’ engage in direct and independentpatient care activities.Results: We observed 44 students (28 LIC,16 block),resulting in 91 late year observations. Despite somedifferences among schools, LIC students overall spentsignificantly more time engaged in direct patient carecompared to block students (45%vs.35%,p=0.040) andmore time performing these direct patient care activitiesindependently than block students (25%vs.9%,p
<strong>UCSF</strong> Education Day <strong>2011</strong>clerkships. This independence may be moredevelopmentally appropriate for late-year clerkshipstudents and warrants further investigation <strong>of</strong> therelationship to students’ patient-centeredness.Reflective Critique: We are conducting ongoingconsultations with research team members andconsultants and incorporating their feedback to improveour analysis.Writing for Change: TrainingResidents in Health Policy Advocacythrough NarrativeLouise Aronson, MD MFA, <strong>UCSF</strong>,aronsonl@medicine.ucsf.edu; Anda Kuo, MD,AKuo@sfghpeds.ucsf.edu; Sharad Jain, MD,Sharad.Jain@ucsf.edu; Vanessa Grubbs, MD,grubbsv@medsfgh.ucsf.edu; Jennifer Siegel, MD,jennifer.siegel@ucsf.edu; Alice HM Chen, MD,achen@medsfgh.ucsf.edufor quality, relevance and usefulness were 4.95, 4.925and 4.975, respectively. Qualitative comments wereequally positive and emphasized usefulness <strong>of</strong> prereading,in-class writing, hearing each other's storiesand reading aloud with peer/faculty feedback. Somewanted more time and a few needed support afterraising upsetting patient experiences. Residentspublished in New York Times (2), Health AffairsNarrative Matters, Huffington Post and Annals <strong>of</strong> Internal<strong>Medicine</strong>.Discussion: Narrative writing is a relevant and usefuladvocacy tool for pediatric and internal medicineresidents in advocacy tracks and was enthusiasticallyreceived by the learners. Trainees were able to developthe basics <strong>of</strong> publishable pieces within the framework <strong>of</strong>a few structured seminars.Reflection: Presentations at WGEA, AGSAreas abstract covers: GMEDomain(s) addressed: Communication, Evaluation <strong>of</strong>Programs and Curricula, Health Policy, MedicalHumanitiesPurpose: To develop, implement and assess acurriculum to train residents in advocacy-based PublicMedical Writing.Background: Medical narratives are used to educate,change opinions and influence policy. From letters to theeditor or opinion columns in newspapers to essays inmedical or policy journals, physician's stories inspirechange and give voice to society's most vulnerable.Although law and business schools train learners inpersuasive communication, medicine has used narrativeprimarily to promote self-reflection and humanism.Methods: Faculty with expertise in narrative, policy andunderserved medicine collaborated to develop a 3-partworkshop for medicine and pediatrics residentsparticipating in advocacy educational tracks. Workshopswere 2 hours long and included: discussion <strong>of</strong> articlesfrom newspapers, medical and health policy journals;discussion <strong>of</strong> audience, venues, advocacy levels andnarrative craft; in-class (session 1) and at-home(sessions 2-3) writing; development <strong>of</strong> ledes (session 1)and in-progress articles (sessions 2-3). Faculty reviewedadditional drafts as needed. Participants scored sessionquality, relevance and usefulness on a 0-to-5 (worst-tobest)scale and provided qualitative feedback. Facultytracked resident publications.Results: All 19 residents completed evaluations. Mosthad little writing experience. Combined session ratings<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 11
<strong>UCSF</strong> Education Day <strong>2011</strong>12 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Poster PresentationsCurriculum Development PostersAdventures in Competency-Based Formative Assessment: Faculty Development toProvide Feedback on Critical Reflections ........................................................................................................................ 16Louise Aronson, MD, MFA; Susan Masters, PhD; Lowell Tong, MD; Kevin Mack; Carol A. Miller,MD; Heidi E. Kirsch, MD; Marieke Kruidering, PhDContinuous Improvement During Third-Year Clerkships .............................................................................................. 16Vanja Douglas, MD; Joseph Liu, BA; Heidi Kirsch, MD; Ann Poncelet, MD; Andy Josephson, MDCurriculum in Developmental Disabilities ........................................................................................................................ 17Clarissa Kripke, MD; Gerri Collins-Bride, RN, ANPDevelopment <strong>of</strong> a Longitudinal Reflective and Narrative Medical Writing Course for ThirdYear Medical Students........................................................................................................................................................ 17Emily Whichard, MS4; Margo Vener, MD, MPH; Louise Aronson, MDFour Primary Care Residency Training Programs Develop Leadership, Cultural Competence,and Community Advocacy and Partnership Curricula through Collaboration ............................................................ 18Sharad Jain, MD; Craig Keenan; Steve Roey; Kathleen HicksFrom Silos to Certainty: Combining Resources to Create an Interdisciplinary Website toImprove Trauma Education and Patient Care .................................................................................................................. 18Eric Lin, MD; Ben Houseman, MD, PhD; Esther Chen, MD; Rochelle Dicker, MD; David Duong,MD; Robert Mackersie, MD; Andre Campbell, MDLeveraging a Near-Peer Medical Student to Improve Orientation and Training on Portfoliosand Competency-Based Development ............................................................................................................................. 19Amanda Angelotti, MS2; Chandler MayfieldLOFT: Development <strong>of</strong> a Leadership Observation and Feedback Tool ........................................................................ 19Read Pierce, MD; <strong>San</strong>drijn van Schaik, MD, PhD; Sonny Tat, MD; Anda Kuo, MDPeer-Facilitated Small Groups to Encourage Cross-Competency Learning ................................................................ 20Laura Byrne; Matthew Schechter; Igor Mitrovic, MD; Tracy Fulton, PhDPreparing for Teaching Health Center Residency Programs: Migrant and Farm Worker 4 thYear Transition Elective ..................................................................................................................................................... 21Adriana Padilla, MDScreening, Brief Intervention, and Referral to Treatment (SBIRT) for Substance Use Disordersamong Resident Physicians: Curriculum Development and Preliminary Evaluation.................................................. 22Neda Ratanawongsa, MD, MPH; Jennifer Manuel, PhD; Daniel Ciccarone, MD, MPH; JenniferHettema, PhD; Brad Shapiro, MD; Sharad Jain, MDStudent Created Modules to Guide Portfolio Implementation ....................................................................................... 22Nicklaus Brandeh<strong>of</strong>f, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco, nicklaus.brandeh<strong>of</strong>f@ucsf.eduTeaching Ultrasound Imaging Perception: “Weathermaps to Recognition”................................................................ 23Marcia McCowin, MD; Virginia Griswold, MD; Stefanie Weinstein, MD; Irene Turman, RVT<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 13
<strong>UCSF</strong> Education Day <strong>2011</strong>Team-Based Journal Club: A Longitudinal Approach to Evidence-Based <strong>Medicine</strong> (EBM)Training During Residency ................................................................................................................................................ 23Renee Kinman, MD, PhD; Serena Yang, MD, MPHCurriculum Evaluation/Educational Research Posters2007 - 2010 Match Data from Model SFGH on Underserved and Primary Care Residency Choice ........................... 25Margo Vener, MD, MPH; Elisabeth Wilson, MD, MPH; Anna Loeb, MS3; Nili Sommavilla, MS3;Julia Bruckner, MS3; Margaret Wheeler, MDA Randomized Trial <strong>of</strong> Hypothesis-Driven versus Screening Neurological Examination .......................................... 25Hooman Kamel, MD, <strong>UCSF</strong>; Gurpreet Dhaliwal, MD; Maulik Shah, MD; Amar Dhand, MD, DPhil;Babak Navi, MD; S. Andrew Josephson, MDA Review <strong>of</strong> Longitudinal Medical Educational Programs Relating to a PsychiatryResidency Clinical Curriculum Redesign......................................................................................................................... 26Colin E. Stewart, MD; Danielle Carlin, MD; John Q. Young, MD, MPP; Amin Azzam, MD, MAAnesthesia Journal Clubs: General Practices and Successful Features ..................................................................... 26Kathryn Price, MS; Marek Brzezinski, MD PhD; H Nicole Tran, MD; Kathy Schlecht, DO; AnnetteMizuguchi, MD, PhD; Stephen Kimatian, MD; Guneet Natt, MD; John Mitchell, MDCreating an Inter-Pr<strong>of</strong>essional Teamwork Education Program for Health Pr<strong>of</strong>essionsStudents in a District Setting in Tanzania ........................................................................................................................ 27Gary Koehler; Siriel Massawe; Helga Naburi; Sebalda LeshabariDiabetes, Hypertension and Asthma…Oh My! Can a Chronic Illness Cohort Help ImproveStudent and Patient Outcomes?........................................................................................................................................ 28Margo Vener, MD, MPH; Ben Howell, MS3; Nicole Gomez, MS3; Kate Chomsky-Higgins, MS3;Nili Sommavilla, MS3; Margaret Wheeler, MDDissemination and Implementation <strong>of</strong> an Evidence-Based, Tobacco-Treatment Curriculum.................................... 28Alan K Louie, MD; Sebastien C. Fromont, MD; Karen Suchanek Hudmon, DrPH, RPH; Sharon M.Hall, PhD; Judith J. Prochaska, PhD, MPHEvaluating a Novel Quality Improvement Curriculum for Third Year Medical Students ............................................. 29David Stern Levitt, BS; Somnath Mookherjee, MDFaculty and Resident Knowledge <strong>of</strong> Health Care Costs ................................................................................................. 29Amy Clouse; Adam Carlson, MD; Bradley Sharpe, MDFaculty Development to Support Competency Based Medical Education in Tanzania:A Situation Analysis ........................................................................................................................................................... 30Molly Fyfe, MA, MPH; Charles MKony; Kelli Barbour; Dorothy Perry; Patricia O’Sullivan, EdD;Sarah MacFarlaneFaculty-Narrated Web-Based Learning Modules Improve Students’ Communication Skillson a High-Stakes Clinical Skills Examination .................................................................................................................. 30Christina A. Lee, MD; Anna Chang, MD; Calvin L. Chou, MD, PhD; Christy Boscardin, PhD;Karen Hauer, MDFeasibility <strong>of</strong> a Supplemental Home-Based Curriculum for Basic Surgical Skills Acquisition .................................. 31Leslie C. Sheu, BA, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, leslie.sheu@ucsf.edu; Hueylan Chern, MD;Patricia S. O'Sullivan, EdD; Ed Kim, MD14 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Geriward: An Interpr<strong>of</strong>essional Team-Based Curriculum on Care <strong>of</strong> the Hospitalized Older Adult.......................... 32Stephanie Rennke, MD; Lynda Mackin, RN, PhD, ANP-BC, CNS; Bree Johnston, MD, MPH;Adam Moylan, PhD; Vicki Jue, PharmD; Cindy Lai, MDIdentifying Curricular Needs for Clinical Medical Education in Tanzania..................................................................... 32Reena Gupta, MD; Molly Fyfe, MPH MA; Charles Mkony, MD; Sarah Macfarlane, PhD MSc;Eligius Lyamuya, MD; Ephata Kaaya, MDImpact <strong>of</strong> Student-Run Clinics on Preclinical Students’ Sociocultural and Interpr<strong>of</strong>essionalAttitudes: A Prospective Cohort Analysis........................................................................................................................ 33Leslie C. Sheu, BA; Cindy J. Lai, MD; Anabelle D. Coelho, MS; Lisa D. Lin, MS; Patricia Zheng,BS; Patricia Hom, BA; Vanessa Diaz, BS; Patricia S. O’Sullivan, EdDIntegrating Multiple Levels <strong>of</strong> Learners into an Interdisciplinary Team-Based Model <strong>of</strong>Ambulatory Care ................................................................................................................................................................. 33Katherine Julian, MD; Bridget O'Brien, PhD; Maria Wamsley, MDLearners' Perspectives on Effective Mentorship............................................................................................................. 34Christy Boscardin, PhD; Renee Courey, PhD; Louise Aronson, MD, MFA; Allison Chen; MarkLovettLights, Camera, Action: Small Group Video Review Promotes Efficient, Effective Clinical Learning....................... 35Margo Vener, MD. MPH; Erika Schillinger, MDMeaningful Innovation or Rearranging Deck Chairs? Comparing Three Formats for aFamily <strong>Medicine</strong> Clerkship ................................................................................................................................................. 35Margo Vener, MD; Nili Sommavilla, Med 3; Julia Bruckner, MS3; Arianne Teherani, PhDMedical Student Perceptions <strong>of</strong> Anesthesiology............................................................................................................. 36Kathryn Price, MS; Guneet Natt, MD; Bridget O'Brien, PhD; Marek Brzezinski, MD, PhD; MartinBogetz, MDMedical Students’ Attention to Multiple Risk Behaviors: A Standardized Patient Examination ................................ 36Judith J. Prochaska, PhD, MPH; Kathleen Gali; Bernie Miller; Karen Hauer, MDPhysical Examination Teaching: A Systematic Review <strong>of</strong> the Literature ..................................................................... 37Somnath Mookherjee, MD; Lara Pheatt, MA; Calvin L. Chou, MD, PhDPilot <strong>of</strong> a Lifelong Pr<strong>of</strong>essional Development Metric in a Scholarly Concentration Program.................................... 38Renee Courey, PhD; Carrie Chen, MD, MSEd; Louise Aronson, MD, MFA; Kristen Fitzhenry, MS;Josh Adler, MD; Additional Pathway to Discovery DirectorsPr<strong>of</strong>essional Deformation: The Repression <strong>of</strong> Personal Values and Attributes in Medical Education..................... 38Michael W. Rabow, MD; Carrie N. Evans, MA; Rachel N. Remen, MDTeaching and Assessing Medical Students’ Skills in Counseling for Behavior Change:A Systematic Review .......................................................................................................................................................... 39Karen E. Hauer, MD; Patricia Carney, PhD; Anna Chang, MD; Jason Satterfield, PhDThe Educational Value <strong>of</strong> Overnight Call Amid Resident Duty Hours Restrictions..................................................... 39Oren K. Fix, MDThe <strong>UCSF</strong> Geriatric Community Resources Clinical Algorithm and Guide .................................................................. 40Christopher A. Bautista; Louise Aronson, MD<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 15
<strong>UCSF</strong> Education Day <strong>2011</strong>Curriculum Development PostersAdventures in Competency-BasedFormative Assessment: FacultyDevelopment to Provide Feedback onCritical ReflectionsLouise Aronson, MD, MFA, <strong>UCSF</strong> Department <strong>of</strong><strong>Medicine</strong>, Division <strong>of</strong> Geriatrics,aronsonl@medicine.ucsf.edu; Susan Masters, PhD,<strong>UCSF</strong>, Department <strong>of</strong> Cellular and MolecularPharmacology, masters@cmp.ucsf.edu; Lowell Tong,MD, USCF, Department <strong>of</strong> Psychiatry; Kevin Mack,<strong>UCSF</strong>, Department <strong>of</strong> Psychiatry; Carol A. Miller, <strong>UCSF</strong>,Department <strong>of</strong> Pediatrics; Heidi Kirsch, MD, <strong>UCSF</strong>,Department <strong>of</strong> Neurology; Marieke Kruidering, PhD,<strong>UCSF</strong>, Department <strong>of</strong> Cellular and MolecularPharmacology, Marieke.Kruidering@ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Faculty Development,Feedback, Portfolios, ReflectionPurpose: To develop and assess a volunteer effort toprovide feedback on reflective skills in medical studentcritical reflections.Background: Literature suggests that reflectionimproves pr<strong>of</strong>essional behavior, teamwork, selfmonitoring,and clinical performance. Reflective skilldevelopment requires repeated practice with timelyfeedback. As medical schools increasingly incorporatereflection into their curricula, they must devise means <strong>of</strong>providing feedback to large numbers <strong>of</strong> learners onexercises that can be assessed for both reflective skilland reflective learning about a specified topic.Methods: A series <strong>of</strong> competency-based, formativeexercises were added across the first-year corecurriculum and linked to the MD Portfolio. We recruitedfaculty and staff to a feedback team via targeted emailsand announcements at curricular committee andAcademy meetings. A 1.5-hour-long training introducedvolunteer reviewers to critical reflection using theLEAP/SOAP model and related feedback guidelines andhad participants practice writing feedback on reflectiveskill development for several de-identified reflectionsamples. RESULTSThe initial call yielded 8 volunteers.A repeat call yielded 4 more. The feedback team <strong>of</strong> 9faculty from 8 departments and 3 educational staffprovided feedback on 456 reflections from September toDecember, 2010. To protect student privacy, reviewerscould not see previous reflections or feedback. Onaverage, faculty provided feedback on 3-5 reflections perweek, which delayed the feedback to students for up to4-6 weeks.Evaluation Plan: Reviewers will complete a surveyabout the experience and their feedback approach. Arater will score the quality <strong>of</strong> feedback in a random subsampleusing qualitative analysis and a feedback rubric.We will compare results from the first and thirdreflections and analyze relevant data from longitudinalstudent focus groups and course evaluations.Dissemination: ECC meetings; Education Day, WGEA,national meetings.Reflective critique: We will use the evaluationinformation to revise next year’s critical reflectioncurriculum.References:1. <strong>San</strong>dars, John. The use <strong>of</strong> reflection in medical education: AMEEGuide No. 44, Medical Teacher, 31: 8, 685 -695, 2009.Continuous Improvement DuringThird-Year ClerkshipsVanja Douglas, MD, <strong>UCSF</strong>, vanja.douglas@ucsf.edu;Joseph Liu, BA, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,joseph.liu@ucsf.edu; Heidi Kirsch, MD, <strong>UCSF</strong>,heidi.kirsch@ucsf.edu; Ann Poncelet, MD, <strong>UCSF</strong>,ann.poncelet@ucsf.edu; S. Andrew Josephson, MD,<strong>UCSF</strong>, ajosephson@memory.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Curricular Innovation, FeedbackPurpose: To develop a web-based interface that allowsstudents and educators to evaluate each other dailyduring clinical rotations.Background: Feedback is an important yet <strong>of</strong>tenneglected part <strong>of</strong> the learning process. Quality toolsbased on the principles <strong>of</strong> Continuous Improvement (CI)provide a medium for effective and immediate feedback.Methods: We developed an online CI module in theCollaborative Learning Environment through whicheducators and students can provide each other dailyfeedback. Over one year, two instructors on an inpatientneurology clerkship were assigned to use the modulewith their third-year students (10 students) and the restattended as usual (7 students). Students completed asurvey about feedback after their rotation. Instructorsusing the module were interviewed. The Wilcoxon ranksumtest was used to compare Likert scales.16 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Evaluation Plan: The module was used an average <strong>of</strong>two times per week. Students using the module weremore satisfied with the amount (p=0.07) and quality(p=0.02) <strong>of</strong> their feedback. Those using the moduleagreed they received more (p=0.02) and higher quality(p=0.06) feedback compared to other rotations duringthird year. All stated the CI module should be adoptedon more clinical rotations. Educators found it timeintensivebut discovered it helped hone their skill atgiving quality feedback.Dissemination: The module will be expanded to otherinstructors in the neurology department in the comingyear.Reflective critique: The number <strong>of</strong> students andeducators using the module was small, but the receptionfrom students was very positive. Educators may still findtime a major hurdle in implementation.Curriculum in DevelopmentalDisabilitiesClarissa Kripke, MD, <strong>UCSF</strong> Department <strong>of</strong> Family andCommunity <strong>Medicine</strong>, kripkec@fcm.ucsf.edu; GerriCollins-Bride, RN, ANP, Community Health Systems,<strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Nursing, gerri.collinsbride@nursing.ucsf.eduAreas abstract covers: UME, GME, CMEDomain(s) addressed: Curricular Innovation, Diversity,Interpr<strong>of</strong>essional Education, Primary CarePurpose: The goal <strong>of</strong> this project is to increase thecompetence <strong>of</strong> health care pr<strong>of</strong>essionals to meet thehealth care needs <strong>of</strong> adults with developmentaldisabilities.Background: In 2006 an interagency collaborative wasestablished to identify barriers to health care for adultswith developmental disabilities and to develop a pilot toaddress them.Methods: The Office <strong>of</strong> Developmental Primary Care(ODPC) was established in the <strong>UCSF</strong> Department <strong>of</strong>Family and Community <strong>Medicine</strong> to bring together aninterpr<strong>of</strong>essional team <strong>of</strong> clinicians to develop training atthe predoctoral, residency and faculty developmentlevels. ODPC developed a curricular map, competenciesand an interpr<strong>of</strong>essional student interest group. Theteam worked with community partners to develop acomprehensive website and set <strong>of</strong> curricular materialsincluding practice pearls, health maintenancerecommendations, information on accessing services,sample power point presentations, empathy exercises,chart forms, links, policy papers and sample referralletters. The team has presented the content in didacticpresentations to over 1300 trainees in different healthdisciplines.Evaluation Plan: The Office <strong>of</strong> Developmental PrimaryCare is tracking hits and downloads to its website (over3000 per month). We are collecting evaluations at everydidactic session.Dissemination: ODPC has integrated a problem basedlearning case into the predoctoral medical schoolcurriculum, developed an elective, integrated a healthadvocate from the Arc <strong>of</strong> <strong>San</strong> Francisco into the familymedicine residency training site and developed diadacticpresentations for over 1300 trainees in variousdisciplines, locally and nationally. Content has beensummarized in a guide to clinical care for all medicalstudents and in a book chapter for nursing students.Reflective critique: Revising and expanding the trainingand web materials is an ongoing, iterative process andwe continue to partner with people with disabilities andtheir advocates in all <strong>of</strong> our curriculum development.Development <strong>of</strong> a LongitudinalReflective and Narrative MedicalWriting Course for Third Year MedicalStudentsEmily Whichard, MS4, <strong>University</strong> <strong>of</strong> <strong>California</strong> at <strong>San</strong>Francisco, emily.whichard@ucsf.edu; Margo Vener, MD,MPH, <strong>University</strong> <strong>of</strong> <strong>California</strong> at <strong>San</strong> Francisco,mvener@fcm.ucsf.edu; Louise Aronson, MD, <strong>University</strong><strong>of</strong> <strong>California</strong> at <strong>San</strong> Francisco,aronsonl@medicine.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Curricular Innovation,Longitudinal Educational Activities, Medical Humanities,ReflectionPurpose: To design a longitudinal writing course forthird year medical students to reflect on their transition toclinical medicine and advance <strong>of</strong> their public writingskills.Background: The literature describes reflection as atool for self-regulated life-long learning and development<strong>of</strong> pr<strong>of</strong>essional practice. The growing diversity <strong>of</strong> typesand venues for narrative medical writing presents anopportunity to help students translate reflective learninginto writings which effectively communicate their uniqueclinician experiences to colleagues and the public.Methods: Curriculum development consisted <strong>of</strong>: (1) aliterature review <strong>of</strong> public medical writing; (2) informalsurveys <strong>of</strong> course directors and medical students aboutreflection and writing interests and needs; (3) selection<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 17
<strong>UCSF</strong> Education Day <strong>2011</strong><strong>of</strong> exemplar readings <strong>of</strong> advocacy and narrative medicalwriting; (4) development <strong>of</strong> a series <strong>of</strong> structuredprompts; and (5) creation <strong>of</strong> a student syllabus andcompanion faculty teaching guide. We then piloted aseven-session course with Model SFGH volunteers in2010-<strong>2011</strong> and solicited their feedback on coursemethods and goals. We obtained Academic Senateapproval and recruited faculty for a 4-session,longitudinal, third year medical student course entitled“Public Medical Writing” to start in the <strong>2011</strong>-12 academicyear.Evaluation Plan: Evaluation will include tracking <strong>of</strong>student enrollment and retention in year one andenrollment in subsequent years, student preparation forsessions, and student completion <strong>of</strong> one short, revised,publication quality narrative medical writing piece. At theend <strong>of</strong> the course, students will complete courseevaluations and a knowledge test <strong>of</strong> public medicalwriting types and venues. Finally we will analyze studentwritings for writing, storytelling and reflective traits usingpreviously validated rubrics.Dissemination: Health & Society Works-in-Progress;Pathways to Discovery symposium; WGEA.Reflective critique: The final course reflects feedbackfrom third year course directors, Model SFGH directors,course pilot participants and other pathways learners.Four Primary Care ResidencyTraining Programs DevelopLeadership, Cultural Competence,and Community Advocacy andPartnership Curricula throughCollaborationSharad Jain, MD, <strong>UCSF</strong>, Sharad.Jain@ucsf.edu; CraigKeenan, UC Davis, craig.keenan@ucdmc.ucdavis.edu;Steve Roey, <strong>San</strong>ta Clara Valley Medical Center,Steve.Roey@hhs.sccgov.org; Kathleen Hicks, AlamedaCounty Medical Center, khicks@acmedctr.orgValley Medical Center) that provide care to underservedpopulations and the development <strong>of</strong> a curriculum thataddresses topics on leadership, advocacy, communitypartnerships, and cultural competency.Methods: Program leadership worked together todevelop training models that can be implemented,evaluated, and ultimately disseminated to a broaderaudience <strong>of</strong> residency training programs. The process <strong>of</strong>developing a comprehensive curriculum for medicineresidents to learn these core topics requiredcollaboration to (1) perform an assessment <strong>of</strong> currentcurricula being delivered and compare these curriculawith the literature and national guidelines, (2) implementcurricular design to facilitate delivery at programs withwide variations in schedules and logistics, and (3)document the impact <strong>of</strong> these innovations on residentphysicians’ knowledge, skills, and attitudes.Evaluation Plan: The impact <strong>of</strong> the curriculum onresidents is currently being assessed using pre- andpost- surveys. Informal survey <strong>of</strong> faculty and residentsinvolved in the curricula demonstrated great satisfactionwith the process and ease <strong>of</strong> delivery with thecurriculum.Dissemination: Collaboration with specific curricularobjectives provides a valuable method for rapiddevelopment and delivery <strong>of</strong> curricula to addressdisparities among training physicians and proved aninvaluable technique that is both transferable and flexibleto fit individual programs’ needs. We also believe thatthis process had significant beneficial impact on facultydevelopment. We plan to disseminate our work throughpresentations at various meetings and to make ourcurriculum available to other programs.Reflective critique: We await learner feedback throughour surveys, as well as from our dissemination efforts.This feedback will help improve the curriculum.Areas abstract covers: GMEDomain(s) addressed: Community <strong>Medicine</strong>, CurricularInnovation, LeadershipPurpose: Physicians, especially those working in safetynet systems, must be trained to address disparitiesserving as "agents <strong>of</strong> change" to improve outcomes fortheir patients.Background: We describe a collaborative processamong four primary care medicine residency trainingprograms (<strong>UCSF</strong>/SFGH, Alameda County MedicalCenter, <strong>University</strong> <strong>of</strong> <strong>California</strong>, Davis, and <strong>San</strong>ta Clara18 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>From Silos to Certainty: CombiningResources to Create anInterdisciplinary Website to ImproveTrauma Education and Patient CareEric Lin, MD, Department <strong>of</strong> Anesthesia, <strong>University</strong> <strong>of</strong><strong>California</strong>, <strong>San</strong> Francisco, lineric@anesthesia.ucsf.edu;Ben Houseman, MD, PhD, Department <strong>of</strong> Anesthesia,<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco,Houseman@anesthesia.ucsf.edu; Esther Chen, MD,Department <strong>of</strong> Emergency <strong>Medicine</strong>, <strong>University</strong> <strong>of</strong><strong>California</strong>, <strong>San</strong> Francisco,esther.chen@emergency.ucsf.edu; Rochelle Dicker, MD,Department <strong>of</strong> Surgery, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong>Francisco, DickerR@sfghsurg.ucsf.edu; David Duong,MD, Department <strong>of</strong> Emergency <strong>Medicine</strong>, <strong>University</strong> <strong>of</strong><strong>California</strong>, <strong>San</strong> Francisco,David.Duong@emergency.ucsf.edu; Robert Mackersie,MD, Department <strong>of</strong> Surgery, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong>Francisco, rmackersie@sfghsurg.ucsf.edu; AndreCampbell, MD, Department <strong>of</strong> Surgery, <strong>University</strong> <strong>of</strong><strong>California</strong>, <strong>San</strong> Francisco, acampbell@sfghsurg.ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Computers and Technology,Curricular Innovation, Longitudinal Educational Activities,Patient CarePurpose: To create an internet resource that enhancestrauma education at <strong>San</strong> Francisco General Hospital(SFGH) by: (1) consolidating educational material fromthe anesthesia, emergency medicine, and surgerydepartments; and (2) providing always-accessiblecontent for learners from any department, training level,or trauma-related rotation.Background: The literature on workplace learning hasshown that there are common organizational factors thataffect learning in any field. Sharing <strong>of</strong> resources is onesuch factor that facilitates learning, while negativefactors include role uncertainty and emphasis on isolatedwork. Medical education studies have furtherdemonstrated that both undergraduate and graduatelearners struggle with such learning barriers, particularlywhen entering a new role or hospital. Staggered shiftsand rotation-centered traditions also hamper the sharing<strong>of</strong> practices and resources. One solution isasynchronous education through an interdisciplinaryonline resource.Methods: We developed a website to function as astand-alone web portal (sfghtrauma.org), with public andpassword-protected areas accessible at all times. SFGHfaculty with prominent roles in trauma education for eachdepartment contributed the curricular materials used foreach trainee rotation. The authors consolidated, created,and agreed upon the final content. All learners receivedwritten and verbal instructions to utilize the website astheir primary information source.Evaluation Plan: Evaluation <strong>of</strong> this work will investigatechanges in faculty teaching perceived learning outcomesfrom students and faculty, and end-<strong>of</strong>-rotationevaluations <strong>of</strong> the website.Dissemination: This resource will be discoverable viainternet search engines and continually accessible toboth the public and <strong>UCSF</strong> community. We plan topublish our outcomes in a relevant educational journal.We will publish our creation process for shared, topicbasedresources on AAMC MedEdPortal.Reflective critique: We are soliciting both learner andfaculty feedback through written questionnaires andfocus groups. Learner and faculty feedback will be usedto continually improve this resource for future learners.Leveraging a Near-Peer MedicalStudent to Improve Orientation andTraining on Portfolios andCompetency-Based DevelopmentAmanda Angelotti, MS2, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,amanda.angelotti@ucsf.edu; Chandler Mayfield, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, chandler.mayfield@ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Communication, Competencies,Computers and Technology, PortfoliosPurpose: To develop near-peer orientation and trainingmaterials to address communications challenges whenpresenting portfolios and competency-baseddevelopment to medical students.Background: <strong>UCSF</strong> launched an electronic portfolio in2009 to support competency-based development. Afterits first year, students reported that they did notunderstand portfolio requirements, value, or purpose andthat technical resources were inadequate and confusing.Methods: A second year medical student developedand delivered a new student orientation session onportfolios and their relationship to competency-baseddevelopment to incoming first year medical students inthe fall <strong>of</strong> 2010. This session clarified how the portfoliosupports pr<strong>of</strong>essional development from the perspective<strong>of</strong> a near peer, provided examples <strong>of</strong> portfolios createdby fellow students and residents, and discussedcompetencies in student-friendly and approachableterms. The student also redeveloped existing onlineresources to clarify the purpose and requirements <strong>of</strong> theportfolio and improve and highlight the technical helpsection.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 19
<strong>UCSF</strong> Education Day <strong>2011</strong>Evaluation Plan: Surveys will be disseminated tostudents to assess the updated training materials. Thesedata will be compared to data from the first year <strong>of</strong>portfolio implementation.Dissemination: The orientation presentation wasdelivered to first year students in the fall <strong>of</strong> 2010 andmaterials have been shared with staff and facultyresponsible for future portfolio training. The updated MDPortfolio Handbook is accessible on iROCKET, theelectronic curriculum platform <strong>of</strong> the <strong>UCSF</strong> <strong>School</strong> <strong>of</strong><strong>Medicine</strong>. A poster abstract has been submitted for the<strong>2011</strong> AAMC Western Regional Conference at Stanford<strong>University</strong>.Reflective critique: Survey data from the first year <strong>of</strong>portfolio implementation and support from CurricularAffairs and the Office <strong>of</strong> Education Technology wereused to develop the revised portfolio training curriculum.A Frequently Asked Questions section will be added tothe handbook based on recent student feedback, and aliterature search will be conducted to seek furthermethods for teaching new medical students about theuse <strong>of</strong> portfolios.LOFT: Development <strong>of</strong> a LeadershipObservation and Feedback ToolRead Pierce, MD, <strong>UCSF</strong>, Read.Pierce@ucsf.edu;<strong>San</strong>drijn van Schaik, MD PhD, <strong>UCSF</strong>,vanschaiks@peds.ucsf.edu; Sonny Tat, MD, <strong>UCSF</strong>,TatS@peds.ucsf.edu; Anda Kuo, MD, <strong>UCSF</strong>,AKuo@sfghpeds.ucsf.eduAreas abstract covers: GME, CMEDomain(s) addressed: Assessment and Testing,Communication, Feedback, LeadershipPurpose: To develop a pilot tool for assessment andfeedback <strong>of</strong> physician leadership skills.Background: Clinical environments provide numerousopportunities to work in multidisciplinary teams.Physicians are <strong>of</strong>ten expected to lead such teams, yetthere is a paucity <strong>of</strong> validated assessment tools forevaluating leadership behaviors in the healthpr<strong>of</strong>essions. Existing tools largely focus on crisissituations such as resuscitations or surgicalemergencies. The Leadership Practice Inventory (LPI) isa validated and reliable leadership assessment toolwidely used in the business world to provide multisourcefeedback in varied settings. This tool, however,does not adequately address experiences on a clinicalteam.Methods: We performed an in-depth literature review onteamwork and team leadership in clinical workenvironments using PubMed and Business SourceComplete. We identified 5 assessment instruments forleadership in clinical crisis situations and modified theLPI tool to incorporate relevant concepts from theseinstruments. The resulting pilot Leadership Observationand Feedback Tool (LOFT) is a 5-domain instrumentwith 15 questions constructed to capture observedleadership behaviors and give suggestions forimprovement using open-ended text.Evaluation Plan: We have started a study amongpediatric and internal medicine residents and anticipatecollecting approximately 80 pilot LOFTs. We will conducta qualitative analysis <strong>of</strong> the LOFT responses untilsaturation has been reached to identify themes anddelineate a spectrum <strong>of</strong> physician behaviors in each <strong>of</strong>the 5 leadership practice domains. This will inform thecreation <strong>of</strong> behavioral anchors on a scale from novice toexpert that we can use to create a quantitative LOFT.Dissemination: We will summarize the qualitativefindings in a manuscript for peer reviewed publication.Reflective critique: Our project was reviewed byESCape prompting us to recognize the need to start witha qualitative LOFT in order to establish behavioralanchors for a quantitative tool.References:1. Posner, B. Leadership Practices Inventory Data Analysis. Retrievedon February 7, <strong>2011</strong> from:http://media.wiley.com/assets/2034/63/LPIAnalysisAug2009.pdf.Peer-Facilitated Small Groups toEncourage Cross-CompetencyLearningLaura Byrne, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,laura.byrne@ucsf.edu; Matthew Schechter, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, matthew.schechter@ucsf.edu; IgorMitrovic, MD, Department <strong>of</strong> Physiology, <strong>UCSF</strong> <strong>School</strong><strong>of</strong> <strong>Medicine</strong>, imitrov@phy.ucsf.edu; Tracy Fulton, PhD,Department <strong>of</strong> Biochemistry, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>,tracy.fulton@ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Basic Science Education,Competencies, Curricular InnovationPurpose: To design a series <strong>of</strong> basic science smallgroups with increased student responsibility forfacilitation and team dynamics.Background: Expert-facilitated small groups provide avenue for application <strong>of</strong> knowledge in <strong>UCSF</strong>’s20 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>preclerkship curriculum. However, administrativeresource-intensivity and uneven facilitator quality impactthe overall effectiveness <strong>of</strong> the modality. Given theincorporation <strong>of</strong> ACGME competencies into UME, thereis a need for early, structured practice in the domains <strong>of</strong>Interpersonal & Communication Skills, Practice-BasedLearning and Pr<strong>of</strong>essionalism.Methods: We developed 3 peer-facilitated (PF) basicscience small group sessions. Content learning isfaculty-supported by electronic and in-person “roving” Q-and-A, and multiple choice questions with instantfeedback. An accompanying self-facilitation curriculumconsists <strong>of</strong> an introductory large group presentation,incorporating audience participation, and a selffacilitateddebriefing after the first group. These sessionswere designed to explicitly address non-medicalknowledge learning by encouraging analysis <strong>of</strong> groupprocess and personal goal-setting.Evaluation Plan: To address the efficacy <strong>of</strong> the PFgroups for medical knowledge acquisition and forpractice <strong>of</strong> specific skills in other competency domains,we have collected student responses to quantitative andopen-ended questions. We have also collected objectiveperformance data from course examination questions.This data will be discussed and compared to thatcollected from more traditional small groups.Dissemination: Curriculum details and preliminaryevaluation data have been shared with curriculumoversight committees, and implementation in othercourses has been discussed. We will considersubmission to MedEdPORTAL and outside conferencesor journals once program evaluation is complete.Reflective critique: Based on pilot-year feedback, thegroups have been modified with increased contentcomplexity, additional multiple-choice questions, and theimproved use <strong>of</strong> technology and the new Teaching andLearning Center for faculty “check-ins” with groups.Future evaluation and implementation will also beinformed by outcomes from implementation <strong>of</strong> Team-Based Learning in the Essential Core.Preparing for Teaching Health CenterResidency Programs: Migrant and FarmWorker 4th Year Transition ElectiveAdriana Padilla, MD, <strong>UCSF</strong> Fresno Family and Community<strong>Medicine</strong>, apadilla@fresno.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Curricular Innovation, PrimaryCare, ReflectionPurpose: The Migrant and Farm worker elective engagesparticipants in a pathway highlighting primary health care incommunity health centers while learning about systemsbased practice. Such pathways will be critical to transition4th year students into teaching health centers.Background: Academic <strong>Medicine</strong>’s November 2010 journalhighlights the challenge <strong>of</strong> “Taking back Year 4.”1 Wallingand Merando further suggest that goals for the fourth yearshould be clarified.2 The Affordable Care Act will promoteteaching health centers (THC) which are expected todevelop in the Central Valley. This elective was designed t<strong>of</strong>acilitate a student’s transition to a rural THC and its uniquesystems based practice to encourage advance practiceskills.Methods: The elective includes clinical care responsibilities3 days a week and 2 days <strong>of</strong> field work activitieshighlighting systems based practice themes to allowdemonstration <strong>of</strong> an awareness <strong>of</strong> and responsiveness tothe larger context and system <strong>of</strong> health care. Fieldworkactivities include orientation to reflective learning and allowfor reflective analysis <strong>of</strong> student learning goals.Evaluation Plan: Participants are evaluated utilizing<strong>UCSF</strong>’s standard clinical evaluation form. Four reflectivesummaries are required from fieldwork learning goals.Qualitative methods will be used to explore the range <strong>of</strong>participant learning themes. Themes will be analyzed toenhance future participant learning and facultydevelopment.Dissemination: Presentations at departmental researchmeetings are planned. Critical will be presentations toTHC’s as they develop. Submission to family medicinejournals and meetings will occur.Reflective critique: Review by a THC was helpful indesigning the elective. Student participant evaluations havepromoted modification. Qualitative analysis will occur withFresno’s family medicine research team.References:1. Stevens C. Commentary: Taking back Year 4: A call to action.AcadMed. 2010;85:1663-1664.2 Walling A, Merando A. The fourthyear <strong>of</strong> medical education: A literature review. AcadMed.2010;85:1698-1704.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 21
<strong>UCSF</strong> Education Day <strong>2011</strong>Screening, Brief Intervention, andReferral to Treatment (SBIRT) forSubstance Use Disorders amongResident Physicians: CurriculumDevelopment and PreliminaryEvaluationNeda Ratanawongsa, MD, MPH, <strong>UCSF</strong>, <strong>San</strong> Francisco,<strong>California</strong>, RatanawongsaN@medsfgh.ucsf.edu; JenniferManuel, PhD, <strong>UCSF</strong>, <strong>San</strong> Francisco, <strong>California</strong>,jennifer.manuel@ucsf.edu; Daniel Ciccarone, MD, MPH,<strong>UCSF</strong>, <strong>San</strong> Francisco, <strong>California</strong>,ciccaron@fcm.ucsf.edu; Jennifer Hettema, PhD,<strong>University</strong> <strong>of</strong> Virginia, Charlottesville, Virginia,JEH7DV@hscmail.mcc.virginia.edu; Brad Shapiro, MD,<strong>UCSF</strong>, <strong>San</strong> Francisco, <strong>California</strong>,Brad.Shapiro@ucsf.edu; Sharad Jain, MD, <strong>UCSF</strong>, <strong>San</strong>Francisco, <strong>California</strong>, sharad.jain@ucsf.eduAreas abstract covers: UME, GME, CMEDomain(s) addressed: Clinical Instruction andPerformance, Evaluation <strong>of</strong> Programs and CurriculaPurpose: A residency curriculum was developed toenhance residents’ confidence and skills with usingSBIRT (Screening, Brief Intervention and Referral toTreatment)Background: SBIRT conducted in medical settings iseffective in reducing risky alcohol and drug use. Selfreporteddiscomfort and lack <strong>of</strong> experience dealing withalcohol and drug problems are associated with lowerconfidence in SBIRT skills among <strong>UCSF</strong> internalmedicine resident physicians. Moreover, half <strong>of</strong> clinicpatients surveyed anonymously at the teaching countyhospital reported lack <strong>of</strong> counseling about safe drinkinglimits by their providers.Methods: We implemented a 7-week, 32-hourlongitudinal SBIRT curriculum for internal medicineresidents (n=32) at the teaching county hospital. Thecurriculum included SBIRT didactics, small groupdiscussions, skills practice role-plays, and site visits tolocal substance use treatment and referral programs.Written narrative reflections, clinical case discussions,and clinical observation checklists were used to evaluateresidents.Evaluation Plan: Qualitative analysis <strong>of</strong> residents’narrative reflections showed an increase in confidenceusing SBIRT skills with their patients. Residents citedlack <strong>of</strong> time, competing work responsibilities, lack <strong>of</strong>preceptor support, and patient resistance as barriers tocontinued use <strong>of</strong> SBIRT. Analysis <strong>of</strong> qualitative checklistdata revealed that residents screened skillfully forsubstance use disorders and employed patient-centeredlistening skills, while struggling with “rolling withresistance” and formulation <strong>of</strong> specific action plans.Dissemination: Dissemination plans include presentingSBIRT curriculum development through posterpresentations and publications in scientific journals. Weare currently working on website development andpossibly a video <strong>of</strong> the SBIRT approach.Reflective critique: Feedback from the residents andtraining staff has been solicited ongoing in order tomodify the training and feedback portions <strong>of</strong> thecurriculum.Student Created Modules to GuidePortfolio ImplementationNicklaus Brandeh<strong>of</strong>f, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong>Francisco, nicklaus.brandeh<strong>of</strong>f@ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Competencies, CurricularInnovation, Longitudinal Educational Activities, PortfoliosPurpose: To describe a student-created step-by-stepguide to help student set up and become familiar withthe MD Portfolio at <strong>UCSF</strong>.Background: In 2009 <strong>UCSF</strong> SOM launched MDPortfolio for students to provide evidence <strong>of</strong> achievement<strong>of</strong> competencies expected by graduates. The systemincluded opportunities for uploading evidence, criticalreflection and obtaining feedback. However, introduction<strong>of</strong> the portfolio required orientation to its purpose andguidance on how to use the electronic platform. Themodules created provided this introduction andguidance.Methods: Faculty advisors in education and technologywere consulted to determine their vision <strong>of</strong> the MDPortfolio and to identify key items to help studentsbecome familiar with the portfolio concept. Six pilotonline competency examples using the Mahara platformand one online introduction module using ArticulateEngage s<strong>of</strong>tware were created and posted to the E-Portfolio September 2009.Evaluation Plan: During development a group <strong>of</strong> 5students and 2 faculty tested the modules for clarity,design and ease <strong>of</strong> use. Before final release, a group <strong>of</strong>18 students evaluated modules for accessibility, design,ease <strong>of</strong> use, and overall incorporation into the E-Portfoliosystem.Dissemination: Presentations were done at theCurriculum Ambassador Showcase 2009, Class <strong>of</strong> 201322 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Orientation, and <strong>UCSF</strong> SOM 3rd Annual FacultyDevelopment Day 2010.Reflective critique: This work provided a foundation forstudents to create a standard portfolio pr<strong>of</strong>ile and learnthe mechanisms <strong>of</strong> the online platform. Due to theevolution <strong>of</strong> the MD portfolio on both a platform andeducational level, many <strong>of</strong> the examples are nowobsolete, but these examples provided the groundworkfor newer, more robust examples for students to use.Teaching Ultrasound ImagingPerception: “Weathermaps toRecognition”Marcia McCowin, MD, <strong>UCSF</strong>, SFVA,marcia.mccowin@ucsf.edu; Virginia Griswold, MD,<strong>UCSF</strong>, SFVA, virginia.griswold@va.gov; StefanieWeinstein, MD, <strong>UCSF</strong>, SFVA,stefanie.weinstein@va.gov; Irene Turman, RVT, SFVA,irene.turman@va.govAreas abstract covers: UME, GMEDomain(s) addressed: Clinical Instruction andPerformance, Curricular Innovation, SimulationPurpose: To give students <strong>of</strong> ultrasound imaging theskills to recognize normal anatomic structures.Background: One <strong>of</strong> the most challenging aspects <strong>of</strong>teaching medical ultrasound to novice learners isenabling the learner to perceive normal anatomicalstructures; “It all looks like weather-maps to me” is acommon comment. The inability to reliably recognizenormal structures significantly delays the goal <strong>of</strong> startingto learn the spectrum <strong>of</strong> normal variation and pathology.When learners attempt the methods (studying atlasesand asking the expert to point out structures) which workwell for CT and MR which have visually obviousreference anatomy, they discover that ultrasound imageshave few visually obvious reference anatomic structuresand using these learning techniques <strong>of</strong>ten results infrustration and failure.Methods: A self-learning powerpoint series wasdeveloped to teach the detailed anatomy required to findvisual reference for abdominal (the abdomen waschosen for ample reference anatomy) ultrasound.Normal contiguous CT images were reconstructed in thecommon planes used for ultrasound and displayed bothunlabeled and then labeled with the required anatomy ina fashion designed to reinforce the relationships <strong>of</strong> thereference anatomy. An explanation <strong>of</strong> the differentappearance <strong>of</strong> the reference anatomy on ultrasoundcompared to CT is followed by ultrasound images,unlabeled and labeled so that the learner can self-test.The series is designed so that the learner can work attheir own pace and retrace steps.Evaluation Plan: Various learners including residentphysicians, medical students, and ultrasound technologystudents will be surveyed as to usefulness <strong>of</strong> the series.Dissemination: We plan to share our experience withour colleagues at the Association <strong>of</strong> <strong>University</strong>Radiologists Annual Meeting.Reflective critique: Ultrasound experts includingphysicians and technologists will be surveyed regardingthe change in perceptive abilities <strong>of</strong> the learners.Team-Based Journal Club: ALongitudinal Approach to Evidence-Based <strong>Medicine</strong> (EBM) TrainingDuring ResidencyRenee Kinman, MD, PhD, Children’s Hospital Central<strong>California</strong>, <strong>UCSF</strong> Fresno Medical Education Program,rkinman@childrenscentralcal.org; Serena Yang, MD,MPH, <strong>UCSF</strong> Fresno Medical Education Program,syang@fresno.ucsf.eduAreas abstract covers: GMEDomain(s) addressed: Curricular Innovation,Longitudinal Educational Activities, ResidencyPurpose: To demonstrate the feasibility <strong>of</strong> a teambased,longitudinal journal club at <strong>UCSF</strong> FresnoPediatric Residency ProgramBackground: Physicians must keep abreast <strong>of</strong> evolvingevidence while monitoring and improving upon theirpractices. Supported by ACGME as an activity that“promotes a spirit <strong>of</strong> inquiry and scholarship,” journalclubs (JC) are utilized by many programs in a variety <strong>of</strong>formats.Methods: In 2009, we began piloting an innovativeteam-based JC format grounded in team-based learningand social & cognitive congruence theories. Residents(PL-1,2,3) are distributed in teams that stay togetherthroughout training. JCs are moderated by a residentwith close faculty support. Prior to each JC, teams areassigned article sections to appraise using standardizedworksheets designed to elicit critical thinking. At the start<strong>of</strong> each JC, teams briefly meet to discuss assignedsections. The moderator then facilitates a large groupdiscussion with each team presenting their section, andfinishes with a discussion <strong>of</strong> “how the article affects mypractice”.Evaluation Plan: Residents are surveyed before JCexposure and annually thereafter to assess confidence<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 23
<strong>UCSF</strong> Education Day <strong>2011</strong>ratings in critical appraisal <strong>of</strong> medical literature. Pre-postintervention data will be analyzed using paired Wilcoxonsigned-rank test. Resident/faculty evaluation <strong>of</strong> JCcurriculum occurs annually. Future plans will assess:residents’ critical appraisal skills using validated tools,resident practice <strong>of</strong> EBM during clinical rotations,resident moderator performance, and faculty perception<strong>of</strong> JC impact on resident education.Dissemination: We will share our curriculum with otherresidency programs at <strong>UCSF</strong>; present at regional andnational conferences; and submit our findings to MedEdPortal.Reflective critique: We plan to refine our curriculumbased on feedback from our faculty and learners, andmedical education forums such as ESCape.24 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Curriculum Evaluation & Educational Research Posters2007 - 2010 Match Data from ModelSFGH on Underserved and PrimaryCare Residency ChoiceMargo Vener, MD, MPH, <strong>UCSF</strong>, mvener@fcm.ucsf.edu;Elisabeth Wilson, MD, MPH, <strong>UCSF</strong>,ewilson@fcm.ucsf.edu; Anna Loeb, MS3, <strong>UCSF</strong>,anna.loeb@ucsf.edu; Nili Sommavilla, MS3, <strong>UCSF</strong>,nili.sommavilla@ucsf.edu; Julia Bruckner, MS 3, <strong>UCSF</strong>,julia.bruckner@ucsf.edu; Margaret Wheeler, MD, <strong>UCSF</strong>,mwheeler@medsfgh.ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Career Choice, CurricularInnovation, Primary CarePurpose: To evaluate whether Model SFGH increasesthe number students matching into primary care and/orunderserved residenciesBackground: The US faces a primary care physicianshortage, especially in underserved communities (1).Students trained in underserved programs have morepositive attitudes toward underserved patients (2) andhigher intentions <strong>of</strong> practicing in underservedcommunities (3). Model SFGH is an innovative 6-monthtrack for third-year students interested in urban health.Students complete three semi-integrated clerkships inunderserved settings, follow continuity patients, andwork in community health.Methods: Using match data from 2007-10, wecompared specialty and program choice <strong>of</strong> graduatingstudents who completed Model SFGH (59) to graduatingstudents who had not participated (600). We alsoevaluated match results from 2004-6, before ModelSFGH.Results: Compared to non-participants, Model SFGHstudents have higher rates <strong>of</strong> matching into primary careresidencies (66% vs. 38%), and/or programs inunderserved communities (37% vs. 18%). Compared tothe three years before implementation <strong>of</strong> Model SFGH,this represents an increase in the rate <strong>of</strong> matching intoprimary care for the total graduating class (40% vs 30%)but not an increase in underserved programs (19% vs20%).Discussion: Model SFGH students match morefrequently into primary care and/or underservedresidencies than non-participants. This increase issignificant in training new primary care physicians; sinceModel SFGH began, the total rate <strong>of</strong> <strong>UCSF</strong> graduatesmatching into primary care has increased. Furtherresearch should clarify what curricular factors(peer/faculty support, patient continuity) most pr<strong>of</strong>oundlyimpact students’ decisions.Reflective critique: We presented this work at STFMfor feedback. Further research will track students whowanted to do Model SFGH but were not selected in thelottery.References:1. Center for Workforce Studies, AAMC, 2007.2. Godkin et al, Teach Learn Med. 2006.3. Ko, et al Academic <strong>Medicine</strong>, 2005.A Randomized Trial <strong>of</strong> Hypothesis-Driven versus ScreeningNeurological ExaminationHooman Kamel, MD, <strong>UCSF</strong>, hooman.kamel@ucsf.edu;Gurpreet Dhaliwal, MD, <strong>UCSF</strong>; Maulik Shah, MD, <strong>UCSF</strong>;Amar Dhand, MD, DPhil, <strong>UCSF</strong>; Babak Navi, MD,<strong>UCSF</strong>; S. Andrew Josephson, MD, <strong>UCSF</strong>Areas abstract covers: GMEDomain(s) addressed: Clinical Instruction andPerformancePurpose: We hypothesized that trainees would performbetter using a hypothesis-driven approach to theneurological examination, rather than the traditionalscreening examination.Background: The neurological examination is importantbut complex and difficult to master.Methods: We randomly assigned 16 medical students toperform screening examinations <strong>of</strong> all major aspects <strong>of</strong>neurological function or hypothesis-driven examinationsfocused on aspects suggested by the history. Eachstudent examined 4 patients, two <strong>of</strong> whom had focaldeficits. Outcomes <strong>of</strong> interest were the correctidentification <strong>of</strong> patients with focal deficits, number <strong>of</strong>specific deficits detected, and examination duration.Outcomes were assessed by an investigator blinded togroup assignments. McNemar’s test was used tocompare the sensitivity and specificity <strong>of</strong> the twoexamination methods.Results: Sensitivity was higher with hypothesis-drivenexaminations than screening examinations (78% versus56%; p = 0.046), although specificity was lower (71%versus 100%; p = 0.046). The hypothesis-driven groupidentified 61% <strong>of</strong> specific examination abnormalities,while the screening group identified 53% (p = 0.008).<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 25
<strong>UCSF</strong> Education Day <strong>2011</strong>Median examination duration was 1 minute shorter in thehypothesis-driven group (7.0 minutes versus 8.0minutes; p = 0.13).Discussion: In this randomized trial comparing twomethods <strong>of</strong> neurological examination, a hypothesisdrivenapproach resulted in greater sensitivity and atrend towards faster examinations, at the cost <strong>of</strong> lowerspecificity, compared to the traditional screeningapproach. Our findings suggest that while a screeningexamination may be preferable when a focal deficit isunlikely, a hypothesis-driven approach may be superiorwhen the history is concerning for an acute focalneurological process.Reflective critique: We are working with our colleaguesin Emergency <strong>Medicine</strong> to further test this curriculum.A Review <strong>of</strong> Longitudinal MedicalEducational Programs Relating to aPsychiatry Residency ClinicalCurriculum RedesignColin E. Stewart, MD, <strong>UCSF</strong>, Department <strong>of</strong> Psychiatry,Colin.Stewart@ucsf.edu; Danielle Carlin, MD, <strong>UCSF</strong>,Department <strong>of</strong> Psychiatry, Danielle.Carlin@ucsf.edu;John Q. Young, MD, MPP, <strong>UCSF</strong>, Department <strong>of</strong>Psychiatry, JQYoung@lppi.ucsf.edu; Amin Azzam, MD,MA, <strong>UCSF</strong>, Department <strong>of</strong> Psychiatry,Amin.Azzam@ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Clinical Instruction andPerformance, Curricular Innovation, LongitudinalEducational Activities, ResidencyPurpose: We sought to review the literature onlongitudinal educational programs, search for bestpractices and innovations, and relate findings to ourclinical curriculum redesign.Background: <strong>UCSF</strong>’s general adult psychiatryresidency is redesigning its clinical curriculum. Based onour knowledge <strong>of</strong> adult and workplace learning, weintend to include longitudinal educational programs inthe curriculum.Methods: Two authors did independent PubMedliterature searches on longitudinal curricula using MeSHterms from seminal articles in the field. Almost 1,000articles were retrieved. After scanning all titles andreading pertinent abstracts, relevant articles werereviewed. Findings were recorded in a template andcommon themes identified.Results: Factors that significantly impact residentsatisfaction and learning include: 1) Clear goals andobjectives, 2) preceptor and patient care continuity, 3)protection from inpatient responsibilities, and 4)adequate ancillary support. Clinic objectives are <strong>of</strong>tenbased on needs assessments completed via residentsurvey. Other longitudinal experiences such ascommunity projects and problem-based learning (PBL)cases can easily be integrated into clinics to complementlearning in clinical settings. As residents advance, theyneed less direct observation, more guidance in practicemanagement, and more opportunities for self-directedquality improvement projects.Discussion: An ideal longitudinal educational programin a psychiatry residency might involve a weeklyexperience in a general psychiatry continuity clinicspanning all four years that involves lasting relationshipswith preceptors and gradually decreasing direct clinicalsupervision complemented by increasing involvement inpractice management decisions and projects. Anadaptation <strong>of</strong> this abstract was submitted to the WGEA.Reflective critique: A psychiatry residency clinicalcurriculum committee (CCC) comprised <strong>of</strong> educatorsfrom multiple <strong>UCSF</strong> training sites meets regularly toreview findings and discuss their implications for ourcurriculum redesign. Resident feedback is also beinggathered from a pilot continuity clinic at our VA trainingsite and will be reviewed by the CCC prior toimplementing further pilot programs.Anesthesia Journal Clubs: GeneralPractices and Successful FeaturesKathryn Price, MS, <strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong>Francisco, <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, kathryn.price@ucsf.edu;Marek Brzezinski, MD PhD, <strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong>Francisco, Department <strong>of</strong> Anesthesia and PerioperativeCare, BrzezinM@anesthesia.ucsf.edu; H. Nicole Tran,MD, Kaiser Permanente: Oakland Medical Center,,hiennicole@gmail.com; Kathy Schlecht, DO, SouthOakland Anesthesia Associates P.C.,2kschlecht@comcast.net; Annette Mizuguchi, MD PhD,Brigham and Women’s Hospital,AMIZUGUCHI@partners.org; Stephen Kimatian, MD,Cleveland Clinic, kimatis@ccf.org; Guneet Natt, MD,<strong>San</strong> Francisco VA Medical Center,guneet_nat@yahoo.com; John Mitchell, MD, HarvardMedical <strong>School</strong>, Beth Israel Deaconess Medical Center,jdmitche@bidmc.harvard.eduAreas abstract covers: GMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, Quality Improvement, ResidencyPurpose: To identify general characteristics <strong>of</strong> journalclub and features associated with higher residentattendance and longevity.26 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Background: Journal clubs(JC) are frequent additionsto anesthesia residency curriculum <strong>of</strong>fering multiplebenefits to medical education. Despite this, faculty <strong>of</strong>tenfield complaints and struggle to maintain attendance andparticipation at JC. Features associated with greaterthan 50% attendance and existence greater than 2 yearswere previously investigated in internal medicine-basedJCs. Successful internal medicine JCs were associatedwith mandatory attendance, larger residencies, andincreased resident leadership. However, little is knownabout general features <strong>of</strong> anesthesia-based JCs.Furthermore, features associated with success have yetto be identified.Methods: Nationwide, 117 anesthesiology programdirectors received an e-mailed survey assessing JCfeatures. Successful JCs were defined as existing morethan four years with an average attendance rate over50%. Data were assessed using chi-square and t-testanalysis.Results: Eighty programs responded (response rate,68%). Seventy-seven (96%) conduct JC. Typically, JCsmeet monthly for 1 hour. Faculty(without residentinvolvement) are highly involved in organizing,moderating, and selecting articles. Attendance is <strong>of</strong>tenmandatory (69%) and recorded (89%). Though practicebasedlearning was the ACGME competency mostemphasized, it also required the most improvement inteaching. Formal JC evaluation was rare (60%).Successful JCs had increased faculty attendance(p
<strong>UCSF</strong> Education Day <strong>2011</strong>Reflective critique: This program may serve as a modelthat informs broader integration <strong>of</strong> multidisciplinaryclinical experience at <strong>UCSF</strong>.Diabetes, Hypertension andAsthma…Oh My! Can a ChronicIllness Cohort Help Improve Studentand Patient Outcomes?Margo Vener, MD, MPH, <strong>UCSF</strong>, mvener@fcm.ucsf.edu;Ben Howell, MS 3, <strong>UCSF</strong>, ben.howell@ucsf.edu; NicoleGomez, MS 3, <strong>UCSF</strong>, nicole.gomez@ucsf.edu; KateChomsky-Higgins, MS 3, <strong>UCSF</strong>,Kate.chomskyhiggins@ucsf.edu; Nili Sommavilla, MS 3,<strong>UCSF</strong>, nili.sommavilla@ucsf.edu; Margaret Wheeler,MD, <strong>UCSF</strong>, mwheeler@medsfgh.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Communication, LongitudinalEducational Activities, Patient Care, Primary CarePurpose: To evaluate whether our 3rd-year chronicillness curriculum improved: 1) students’ understanding<strong>of</strong> chronic illness and management and/or 2) clinicaloutcomes for chronically ill patientsBackground: To care for an aging population, futurephysicians need skills to optimize chronic illnessmanagement (1,2). We designed an innovativecurriculum to improve 3rd-year students’ ability toprovide chronic illness care. Students developed theirown panel <strong>of</strong> chronically ill patients. They performedstructured visits emphasizing understanding the patient’sgoals, self-management, education, and prevention.Methods: Twenty-five students each followed at leastpatients for six months. Using student reports, wetracked patient metrics (blood pressure, glucose, etc)and behavior changes (starting exercise, etc). We als<strong>of</strong>ollowed patient educational outcomes. We assessed theeducational impact to medical students through Likkertsurveys and focus groups.Results: While the average patient did not showsignificant change in blood pressure, etc, selectedpatients demonstrated very impressive changes (eg: 20lb intentional weight loss). Both students and patientsfound these changes highly inspirational. Students alsoreported greater appreciation <strong>of</strong>: 1) the ups and downs<strong>of</strong> chronic illness management; 2) the importance <strong>of</strong>continuity: 3) the value and challenge <strong>of</strong> patienteducation and prevention 4) the need not to stereotypepatients 5) the importance <strong>of</strong> follow up outside <strong>of</strong>ficevisits 6) the importance <strong>of</strong> hope.Discussion: Although chronic care was not optimizedfor all participating patients, helping even one patient intheir panel make substantial health gains had markedimpact on students’ understanding <strong>of</strong> chronic illness andtheir belief that they could improve health outcomes theirpatients.Reflective critique: We plan to present this at WGEAfor feedback. Future efforts will focus on how to extendthis curriculum to third-year students in other longitudinaland block rotations.References:1. Pols, Chronic Illness, 2009.2. Holman, JAMA, 2004.Dissemination and Implementation <strong>of</strong>an Evidence-Based, Tobacco-Treatment CurriculumAlan K. Louie, MD, <strong>UCSF</strong>, alanlouie@lppi.ucsf.edu;Sebastien C. Fromont, MD, <strong>UCSF</strong>,SCFromont@hotmail.com; Karen Suchanek Hudmon,DrPH, RPH, <strong>UCSF</strong>, hudmonk@pharmacy.ucsf.edu;Sharon M. Hall, PhD, <strong>UCSF</strong>, Sharon.Hall@ucsf.edu;Judith Prochaska, PhD, MPH, <strong>UCSF</strong>,JProchaska@ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, Faculty Development, Interpr<strong>of</strong>essionalEducation, ResidencyPurpose: The goal <strong>of</strong> the current study was to improvecompetency in tobacco-treatment by psychiatrictrainees. The objective was to evaluate thedissemination and implementation phase <strong>of</strong> PsychiatryRx for Change, a 4-hour, tobacco-treatment curriculumfor psychiatric residencies and graduate psychiatricnursing programs.Background: Nearly half <strong>of</strong> cigarettes sold in the U.S.are smoked by people with mental illness and substanceuse disorders. Yet, surveys suggest psychiatrists rarelytreat tobacco use and only half <strong>of</strong> psychiatric residencyprograms provide didactics on such treatment, with amedian length <strong>of</strong> 1 hour (Prochaska et al., 2006). Wedeveloped the Psychiatry Rx for Change curriculum toaddress this gap and demonstrated positive educationaloutcomes sustained at 3-months follow-up with 55psychiatric residents (Prochaska et al, 2008). Diffusion<strong>of</strong> Innovations theory (Roger 1995) and the RE-AIMframework (Glasgow & Emmons, 2007) guideddissemination and implementation.Methods: Faculty from psychiatric residencies (n=28)and graduate psychiatric nursing programs (n=15) fromthe Western U.S. attended a one-day Psychiatry Rx for28 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Change training. Pre/post-training and follow-up surveyswere administered.Results: Participants’ rating <strong>of</strong> their overall ability toteach tobacco treatment increased from pre- to posttraining(p
<strong>UCSF</strong> Education Day <strong>2011</strong>17 commonly ordered diagnostic tests. A percent (%)error was calculated for each diagnostic test as [(meanestimated – actual)/actual] x 100. Participants alsoresponded to eight attitudinal questions using a 5-pointLikert scale.Results: Thirty-six attendings and 92 residentscompleted the survey, representing a response rate <strong>of</strong>75% and 82% respectively. All participants regardless <strong>of</strong>their level <strong>of</strong> training grossly under-estimated hospitalcharges (mean error -41.4%), and over-estimatedMedicare reimbursement (mean error +152%).Participants rated their own knowledge <strong>of</strong> costs as poor(2 out <strong>of</strong> 5) and their interest in receiving educationabout costs as high (4.2 out <strong>of</strong> 5).Discussion: At a single academic medical center,internal medicine residents and faculty demonstratedpoor knowledge <strong>of</strong> hospital charges for diagnostic tests.Given this finding and participants’ interest in receivingeducation about medical costs, curricular interventionsaimed at improving physician knowledge <strong>of</strong> healthcarefinances would be appropriate.Reflective critique: Based on these results, acurriculum on costs <strong>of</strong> care is being developed for theresidency program. Additionally, a table outlininghospital charges and Medicare reimbursement forcommonly ordered diagnostic tests will be published inthe next edition <strong>of</strong> the Hospitalist Handbook.Faculty Development to SupportCompetency Based MedicalEducation in Tanzania- A SituationAnalysisMolly Fyfe, MA, MPH, <strong>UCSF</strong> Global Health Sciences,mollyfyfe@yahoo.com; Charles MKony, Muhimbili<strong>University</strong> <strong>of</strong> Health and Allied Sciences,charles_mkony@yahoo.com; Kelli Barbour, <strong>UCSF</strong>Global Health Sciences, kelli.barbour@ucsf.edu;Dorothy Perry, <strong>UCSF</strong> <strong>School</strong> <strong>of</strong> Dentistry,PerryD@dentistry.ucsf.edu; Patricia O’Sullivan, <strong>UCSF</strong><strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, OSullivanP@medsch.ucsf.edu;Sarah MacFarlane, <strong>UCSF</strong> Global Health Sciences,macfarlane@globalhealth.ucsf.eduAreas abstract covers: Faculty DevelopmentDomain(s) addressed: Faculty Development, GlobalHealthPurpose: To use data from graduates, students andfaculty to identify needs in faculty development.Background: Tanzania faces a severe shortage <strong>of</strong>health pr<strong>of</strong>essionals. Muhimbili <strong>University</strong> <strong>of</strong> Health andAllied Sciences (MUHAS) is the largest public healthpr<strong>of</strong>essions university in Tanzania. With the goal <strong>of</strong>enhancing the quality <strong>of</strong> health care graduates, a jointMUHAS and <strong>UCSF</strong> team assessed the facultydevelopment needs at MUHAS.Methods: In 2009, 147 recent MUHAS graduates andtheir supervisors (n=48) were surveyed on theirperceptions <strong>of</strong> how well MUHAS prepared them forpr<strong>of</strong>essional practice. Students (n=41) in 6 focus groupsprovided their perceptions <strong>of</strong> the learning environment.Three faculty focus groups (n=32) revealed needs forfurther pr<strong>of</strong>essional development.Results: MUHAS students, alumni and supervisorsrecognized a need for teaching beyond pr<strong>of</strong>essionalknowledge. Students acknowledge that the lectures areeffective, but they have limited exposure to otherpedagogical methods, identifying needs for activelearning, early and strong clinical experience and facultymentoring. The faculty identified the need to employtechnology, and improve their own teaching mentoringskills.Discussion: MUHAS needs to improve the teaching andlearning process in competencies other thanpr<strong>of</strong>essional knowledge. Both teachers and studentswould benefit from improved mentoring as a key startingpoint. Based on this situation analysis, facultydevelopment will target educational strategies for activelearning in large and small group settings, clinicalteaching skills, and mentoring.Reflective critique: This information has beenpresented by colleagues from MUHAS and based onfeedback we believe would be <strong>of</strong> interest at <strong>UCSF</strong>.Faculty-Narrated Web-BasedLearning Modules Improve Students’Communication Skills on a High-Stakes Clinical Skills ExaminationChristina A. Lee, MD, <strong>UCSF</strong>,christinaaudreylee@gmail.com; Anna Chang, MD, <strong>San</strong>Francisco Veteran Affairs Medical Center,anna.chang2@va.gov; Calvin L. Chou, MD, PhD, <strong>San</strong>Francisco Veteran Affairs Medical Center,calvin.chou@ucsf.edu; Christy Boscardin, PhD, <strong>UCSF</strong>,BoscardinCK@medsch.ucsf.edu; Karen Hauer, MD,<strong>UCSF</strong>, khauer@medicine.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Clinical Instruction andPerformance, Communication, Curricular Innovation,Standardized PatientsPurpose: To determine whether a web-based SPmodule with detailed SP and faculty commentary used30 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>immediately prior to a clinical skills examination leads toimproved communication skills.Background: Web-based standardized patient (SP)modules have been associated with improvement inmedical students’ history taking and physicalexamination skills on clinical performance examinations(CPX). However, the use <strong>of</strong> such modules has not yetcorrelated with improvement in students’ communicationskills.Methods: This was a prospective observational studyinvolving fourth year medical students in academic year2008-2009. A 90 minute web-based module consisting<strong>of</strong> three simulated clinical encounters between a medicalstudent and SP was narrated by an expert clinician andSP to explain expected clinical skills behaviors. All 147students were notified one month prior to the CPX andencouraged to review the learning module prior to theexamination. The outcome measure was CPX scores.Results: 106 students (72%) viewed the web-basedmodule prior to the CPX and logged into the module fora mean <strong>of</strong> 86.4 minutes. There was no difference inUSMLE Step 1 or clerkship summary scores betweenstudents who chose to use the module and those whodid not. Students who watched the module performedsignificantly higher on the CPX communication score(+2.61%, p
<strong>UCSF</strong> Education Day <strong>2011</strong>Reflective critique: This curriculum was designed andevaluated with feedback from surgical faculty andmedical educators, and presented at ESCape. Feedbackfrom residents has prompted the design <strong>of</strong> a manual andtake-home videos, to be integrated into the curriculumnext year.Geriward: An Interpr<strong>of</strong>essional Team-Based Curriculum on Care <strong>of</strong> theHospitalized Older AdultStephanie Rennke, MD, <strong>UCSF</strong>,srennke@medicine.ucsf.edu; Lynda Mackin, RN, PhD,ANP-BC, CNS, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco,lynda.mackin@ucsf.edu; Bree Johnston, MD, MPH,<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco, VA MedicalCenter; Adam Moylan, PhD, <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong>Francisco, amoylan@ucsf.edu; Vicki Jue, PharmD,<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco,vicki.jue@ucsfmedctr.org; Cindy Lai, MD, <strong>University</strong> <strong>of</strong><strong>California</strong>, <strong>San</strong> Francisco, clai@medicine.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Competencies, Interpr<strong>of</strong>essionalEducation, Patient CarePurpose: To develop and implement aninterpr<strong>of</strong>essional team-based curriculum on care <strong>of</strong> thehospitalized older adult. Student objectives were to 1)identify geriatric competencies pertaining to the hospitalsetting; 2) engage in team-based learning to complete abedside exercise and 3) present a patient caseemphasizing systems-based practice.Background: Interpr<strong>of</strong>essional team care is required foreffective management <strong>of</strong> complex patients such as olderhospitalized adults. Health pr<strong>of</strong>essions students benefitfrom learning experiences that mirror current health caremodels. Team-based learning(TBL) is an effectivestrategy to teach students knowledge and skills inpatient care.Methods: GeriWard, <strong>of</strong>fered four times, included 26third year medical students, 12 fourth year pharmacystudents and 13 nursing students during 6 months <strong>of</strong> a12-month pilot. GeriWard included: (1) a two-hourworkshop, teams interviewed and examined an olderpatient focusing on one <strong>of</strong> three geriatric AAMCcompetencies: bladder catheters, restraints and skinassessment/pressure ulcer staging; and (2) medicalstudents presented their findings to the inpatient team.Students completed pre- and post-workshop surveys onattitudes towards interpr<strong>of</strong>essional education (IPE) andself-efficacy around the competencies. Hospital-basedfaculty rated the student presentations on content andapplication to systems-based practice.Results: Students showed improvement in attitudestoward IPE pre and post-curriculum (p= 0.001). Studentsrated self-efficacy on the competencies higher afterparticipating in the curriculum. Hospitalist faculty ratedthe student presentations highly, citing the students’ability to identify opportunities for quality improvementinterventions.Discussion: A curriculum combining team-basedlearning and bedside care increased students’ attitudestowards IPE and self-assessed ability to identify geriatriccompetencies and systems-based practice. Findings willbe presented at the Society <strong>of</strong> Hospital <strong>Medicine</strong>meeting and a manuscript will be developed forpublication.Reflective critique: Backed on feedback from studentsGeriWard will include physical therapy students andexpand to the SFVAMC and SFGH.Identifying Curricular Needs forClinical Medical Education inTanzaniaReena Gupta, MD, <strong>UCSF</strong>, reena.gupta@ucsf.edu; MollyFyfe, MPH MA, <strong>UCSF</strong>, mollyfyfe@yahoo.com; CharlesMkony, MD, Muhimbili <strong>University</strong> <strong>of</strong> Health and AlliedSciences, Tanzania, charles_mkony@yahoo.com; SarahMacFarlane, PhD MSc, <strong>UCSF</strong>,Macfarlane@globalhealth.ucsf.edu; Eligius Lyamuya,MD, Muhimbili <strong>University</strong> <strong>of</strong> Health and Allied Sciences,Tanzania, eligius_lyamuya@yahoo.com; Ephata Kaaya,MD, Muhimbili <strong>University</strong> <strong>of</strong> Health and Allied Sciences,Tanzania, ephata.kaaya@yahoo.comAreas abstract covers: UMEDomain(s) addressed: Clinical Instruction andPerformance, Competencies, Evaluation <strong>of</strong> Programsand Curricula, Global HealthPurpose: To identify curricular needs for clinicalteaching at the Muhimbili <strong>University</strong> <strong>of</strong> Health and AlliedSciences (MUHAS) <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> in Tanzania.Background: Tanzania faces a severe shortage <strong>of</strong>physicians. High student-faculty ratios and limited clinicalteaching facilities challenge medical education atMUHAS. We examined clinical training at MUHAS toinform curricular revision and improve clinical teaching toensure the preparation <strong>of</strong> competent physiciangraduates.Methods: This situation analysis <strong>of</strong> clinical teaching atMUHAS draws on data from three sources. The 2009Tracer Study surveyed recent MUHAS medicalgraduates (n=147) and their supervisors (n=48) on theirperceptions <strong>of</strong> how well MUHAS prepared them for32 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>pr<strong>of</strong>essional practice. Student focus groups (n=41)investigated student perceptions <strong>of</strong> medical educationand the learning environment at MUHAS.Results: MUHAS medical students and recentgraduates identified strengths <strong>of</strong> the curriculum inconferring medical knowledge. However, they identifiedsignificant gaps in their medical education with respectto practical clinical training. Surgical skills andambulatory outpatient care were highlighted as specificdeficiencies in clinical training. Both students and facultyfeel that clinical teaching is impeded by the large number<strong>of</strong> students in clinical sessions, limited facilities toconduct clinical teaching, and limited faculty to supervisestudents.Discussion: Increased practical clinical skill training isneeded to improve graduates’ clinical competency,especially in the areas <strong>of</strong> surgical skills and outpatientambulatory care. Informed by student, graduate, andstakeholder perspectives, MUHAS is currentlyundergoing major curriculum revisions focused oncompetency-based medical education and improvingclinical training.Reflective critique: In partnership with <strong>UCSF</strong>, MUHASis implementing efforts to increase clinical exposure,surgical skills simulation training, ambulatory careprecepting, and faculty development about clinicalteaching methodologies to improve medical educationand the preparation <strong>of</strong> graduates who are betterequipped to address health needs in Tanzania.Impact <strong>of</strong> Student-Run Clinics onPreclinical Students’ Socioculturaland Interpr<strong>of</strong>essional Attitudes: AProspective Cohort AnalysisLeslie C. Sheu, BA, <strong>UCSF</strong>, leslie.sheu@ucsf.edu; CindyLai, MD, <strong>UCSF</strong>, clai@medicine.ucsf.edu; Anabelle D.Coelho, MS, <strong>UCSF</strong>, anabelle.coelho@ucsf.edu; Lisa D.Lin, MS, <strong>UCSF</strong>, lisa.lin@ucsf.edu; Patricia Zheng, BS,<strong>UCSF</strong>, patricia.zheng@ucsf.edu; Patricia Hom, BA,<strong>UCSF</strong>, patricia.hom@ucsf.edu; Vanessa Diaz, BS,<strong>UCSF</strong>, Vanessa.diaz@ucsf.edu; Patricia S. O’Sullivan,<strong>UCSF</strong>, osullivanp@medsch.ucsf.eduBackground: Descriptive studies suggest that studentrunclinics (SRCs) positively impact participatingstudents. However, studies rarely include students frommultiple pr<strong>of</strong>essions, validated instruments, and a controlgroup. At our health pr<strong>of</strong>essions campus, first-yearstudents can participate in SRCs focusing on specificunderserved populations: Latino(a), Asian/PacificIslander, and urban homeless communities. In thisstudy, we used validated measures to explore the impact<strong>of</strong> these SRCs on preclinical students’ sociocultural andinterpr<strong>of</strong>essional attitudes.Methods: Using a pre-post control group design, weconducted a prospective cohort study <strong>of</strong> first-yearmedical, nursing, and pharmacy students whoparticipated in SRCs and those who did not. At thebeginning and end <strong>of</strong> the year, they completed surveysconsisting <strong>of</strong> demographics, validated measures onsociocultural awareness (SAMI) and readiness forinterpr<strong>of</strong>essional learning (RIPLS), and open-endedquestions.Results: Of all participating students, 77% (274 <strong>of</strong> 358)completed the post-survey, with 68% (n=182) havingmatching pre-post surveys. Students held positiveattitudes in sociocultural and interpr<strong>of</strong>essional domains.After adjusting for baseline scores, attitudes did not differsignificantly between those who participated in SRCsand those who did not. In the qualitative analysis, 99%reported reinforced or increased commitment to workingwith the underserved. Forty percent reported that theirexperiences made a positive impact on theirinterpr<strong>of</strong>essional attitudes.Discussion: In this study, we found no quantifiableeffect <strong>of</strong> SRC participation on sociocultural orinterpr<strong>of</strong>essional attitudes. However, students perceivedbenefits in both domains, suggesting that the SAMI andRIPLS may not be sensitive enough for measuring theeffects <strong>of</strong> SRCs. Further studies are needed to assessthe long-term impact <strong>of</strong> preclinical SRCs.Reflective critique: We have incorporated extensivefeedback from advisors and ESCape, and havesubmitted the abstract to an education meeting.Areas abstract covers: UMEDomain(s) addressed: Cultural Competence, Diversity,Evaluation <strong>of</strong> Programs and Curricula, Interpr<strong>of</strong>essionalEducationPurpose: To evaluate the impact <strong>of</strong> student-run clinics(SRCs) on sociocultural and interpr<strong>of</strong>essional attitudesacross health pr<strong>of</strong>essions.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 33
<strong>UCSF</strong> Education Day <strong>2011</strong>Integrating Multiple Levels <strong>of</strong>Learners into an InterdisciplinaryTeam-Based Model <strong>of</strong>Ambulatory CareKatherine Julian, MD, <strong>UCSF</strong>, kathy.julian@ucsf.edu;Bridget O'Brien, Ph.D., <strong>UCSF</strong>,ObrienB@medsch.ucsf.edu; Maria Wamsley, MD,<strong>UCSF</strong>, maria.wamsley@ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, Health Systems, Interpr<strong>of</strong>essional Education,Primary CarePurpose: Near-peer teaching may be more effectivethan expert teaching. This project describes theintegration <strong>of</strong> interns/PISCES students into internalmedicine (IM) resident continuity clinic teams to promotenear-peer teaching among multi-level learners.Background: One limitation <strong>of</strong> the PISCES clerkship isthe relative lack <strong>of</strong> interaction with residents. IMresidents and interns have little interaction in clinic dueto separate continuity clinic days. Increasing teachinginteractions among residents, interns, and medicalstudents is desirable to promote near-peer teaching.Methods: In 2008, IM PGY2/PGY3 continuity clinics atParnassus/Zion were reorganized to create a teambasedmodel <strong>of</strong> care. In 2009, we integrated 14 PISCESstudents and 26 interns into the teams. Each teamconsisted <strong>of</strong> one attending, 2-6 PGY2/3 residents, 2-3interns, one LVN and one administrative assistant. 9 <strong>of</strong>10 teams included PISCES students.Results: Interns/PGY2/PGY3 residents were surveyedregarding their satisfaction with the team model. PISCESstudents participated in focus groups. 36 <strong>of</strong> 70 residentsresponded. 51% reported improved informal peermentoring; 38% reported improved educationalenvironment; 70% reported seeking advice from residentpeers in clinic and 59% reported receiving qualityteaching from resident peers. 87% <strong>of</strong> residentrespondents supported student presence on the teamsbut only 29% felt that students were effectivelyintegrated into the team structure. Although PISCESstudents reported positive learning experiences in IMclinic and appreciated resident interactions, they didn’tstrongly identify as members <strong>of</strong> their clinic team.Discussion: Integrating interns/residents in continuityclinic improved informal peer mentoring, near-peerteaching, collegiality and the clinic educationalenvironment. Residents overwhelmingly supported thepresence <strong>of</strong> students on their clinic teams. However,most residents and students did not feel that studentswere effectively integrated into the team structure.Reflective critique: More work must be done to betterintegrate students into clinic teams and increase theinteraction with interns and residents.Learners' Perspectives onEffective MentorshipChristy Boscardin, PhD, <strong>UCSF</strong>,christy.boscardin@ucsf.edu; Renee Courey, PhD,<strong>UCSF</strong>, CoureyR@medsch.ucsf.edu; Louise Aronson,MD MFA, <strong>UCSF</strong>, aronsonl@medicine.ucsf.edu; AllisonChen, <strong>UCSF</strong>, ChenAM@medsch.ucsf.edu; Mark Lovett,<strong>UCSF</strong>, LovettM@medsch.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, MentoringPurpose: The purpose <strong>of</strong> the study was to identifycharacteristics <strong>of</strong> mentors that students considerimportant for effective mentorship in the Pathwaysprogram.Background: Mentorship can significantly influencepersonal development, career choice, and researchproductivity. The <strong>UCSF</strong> Pathways to Discovery programprovides in depth training for careers beyond the routinepractice <strong>of</strong> medicine. Program success depends oneffective mentoring currently delivered by a team <strong>of</strong>project mentors and program directors. Learnerscurrently identify project mentors based on contentexpertise and project interest.Methods: 10 randomly selected medical studentsparticipated in a focus group. The learners were asked aseries <strong>of</strong> structured, open-ended questions to describetheir experience working with project mentors. 35students also completed a survey item (4 point-scale)rating their overall experience with mentorship.Results: 30 (86%) students rated mentorship quality asvery good or excellent (3 to 4). Learners described aneffective mentor as someone who provided contentexpertise but was also a “good advocate” and <strong>of</strong>feredinsight into the student’s career interests.Discussion: Although learners select mentors based oncontent expertise, learners expect each mentor toprovide scholarly, career development, and psychosocialsupport. While many faculty met their role as projectmentors, learner expectations match program-widegoals rather than narrower project mentor roles. Tobetter align learner expectations and availablementoring, we are 1) creating materials that explain the34 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>function <strong>of</strong> mentorship teams; 2) producing a mentordevelopment module to expand mentor roles to meet thebroader needs <strong>of</strong> students.Reflective critique: The results from the survey and thefocus group were shared with the Pathways programdirectors for feedback and input.Lights, Camera, Action: Small GroupVideo Review Promotes Efficient,Effective Clinical LearningMargo Vener, MD. MPH, <strong>UCSF</strong>, mvener@fcm.ucsf.edu;Erika Schillinger, MD, Stanford <strong>University</strong>,erikas@stanford.eduAreas abstract covers: UMEDomain(s) addressed: Communication, Patient Care,Reflection, Standardized PatientsPurpose: To evaluate two models for faculty-facilitatedsmall group review <strong>of</strong> video-recorded student clinicalencountersBackground: Feedback on video-recorded clinicalencounters helps enhance pr<strong>of</strong>essionalism,interpersonal and communication skills among medicalstudents (1, 2, 3). Unfortunately, video review withindividual students is time-consuming for faculty; thismay limit video usage (4).Methods: During 2010, we reviewed data for 40 thirdyearstudents in group video reviews at a public andprivate medical school. In one model, students wererecorded with standardized patients, faculty selectedpositive moments, and video clips were reviewed insmall groups. In the other model, students wererecorded with actual patients, students selectedchallenging moments, and video clips were reviewed insmall groups. Both small groups included five studentsand one preceptor. Sessions focused onpr<strong>of</strong>essionalism, communication, and relationship skills.Focus groups and open-ended surveys were used forqualitative theme analysis.Results: Students in both groups found video reviewvaluable. Students cited improved communicationstrategies and agenda-setting as particular strengths.Students reported benefit from watching their peers.Preceptors found group debriefing effective and efficient,noting that respect and confidentiality were essential.Preceptors valued gaining insight into students’pr<strong>of</strong>essionalism and self-reflection. All foundtechnological hurdles frustrating.Discussion: Many schools struggle with how to bestteach pr<strong>of</strong>essionalism in a meaningful, time-efficientmanner. Our study suggests group video reviewprovides an effective format for modeling pr<strong>of</strong>essionalskills, providing feedback, and discussingcommunication issues.Reflective critique: We presented this work at STFMfor feedback. Future studies should evaluate whetherlongitudinal video review sessions could add benefit forlearning.References:1. Mann, Adv Health Sci Educ Theory Pract 2007.2. Hodges, Med Educ. 2009.3. Plack, Allied Health. 2005.4. Mathers,Med Educ. 1999.Meaningful Innovation orRearranging Deck Chairs?Comparing Three Formats for aFamily <strong>Medicine</strong> ClerkshipMargo Vener, MD, MPH, <strong>UCSF</strong>, mvener@fcm.ucsf.edu;Nili Sommavilla, Med 3, <strong>UCSF</strong>,nili.sommavilla@ucsf.edu; Julia Bruckner, MS 3, <strong>UCSF</strong>,julia.bruckner@ucsf.edu; Arianne Teherani, PhD, <strong>UCSF</strong>,teherani@medsch.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Curricular Innovation,Evaluation <strong>of</strong> Programs and Curricula, LongitudinalEducational Activities, Primary CarePurpose: To determine which rotation model providedthe most optimal Family <strong>Medicine</strong> learning experienceBackground: Continuity has value as an organizingprinciple in medical education (1); however, blockrotations inherently limit continuity. In longitudinaloutpatient rotations, students value continuity withpatients and preceptors (2,3). To explore innovative 3rdyearmodels, <strong>UCSF</strong> <strong>of</strong>fers the required Family <strong>Medicine</strong>clerkship in three formats — a 6-week block rotation, 6-month longitudinal rotation (Model SFGH), or 12-monthlongitudinal-integrated experience (PISCES).Methods: We assessed course evaluations, writtenexams, clinical practice exam (CPX) scores, andresidency match results for 2008-2010. We alsoevaluated student responses to open-ended surveys.Results: On course evaluations (1=poor; 5=excellent),PISCES students reported the highest teaching quality(block=4.25; 6-month=4.21; 12-month=4.46). Longerclerkship length correlated with students reporting betterfeedback on clinical skills (block=3.77; MSFGH=3.90;PISCES=4.29). Overall clerkship ratings increased inlonger models (block=4.11; MSFGH=4.24;<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 35
<strong>UCSF</strong> Education Day <strong>2011</strong>PISCES=4.32). Students in either longitudinal modelwere more likely to describe continuity relationships withpatients and preceptors/role models as strong positiveinfluences on their medical education. For 2008-2010,Model SFGH matched into Family <strong>Medicine</strong> at a higherrate than other students (18%vs6%).Discussion: Both the 6 month longitudinal and the 12-month longitudinal integrated model seem to <strong>of</strong>fer betterfeedback, positive continuity experiences, and morehighly-rated clerkship experiences than the traditionalmodel. However, longitudinal models are also moreresource-intensive. Any discussion <strong>of</strong> which model isoptimal should include consideration <strong>of</strong> outcomes as wellas resource use.Reflective critique: This work was discussed at STFM.Future research will focus on how to extend optimalaspects <strong>of</strong> the longitudinal models to students in all FMclerkship models.References:1. Hirsh, NEJM 2007.2. Irby, Academic <strong>Medicine</strong> 1995.3. Prislin, Academic <strong>Medicine</strong> 1998.Medical Student Perceptions <strong>of</strong>AnesthesiologyKathryn Price, MS, <strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong>Francisco, <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, kathryn.price@ucsf.edu;Guneet Natt, MD, <strong>San</strong> Francisco VA Medical Center,guneet_nat@yahoo.com; Bridget O'Brien, PhD,<strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong> Francisco, Office <strong>of</strong> MedicalEducation, ObrienB@medsch.ucsf.edu; MarekBrzezinski, MD PhD, <strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong>Francisco, Department <strong>of</strong> Anesthesia and PerioperativeCare, BrzezinM@anesthesia.ucsf.edu; Martin Bogetz,MD, <strong>University</strong> <strong>of</strong> <strong>California</strong> <strong>San</strong> Francisco, Department<strong>of</strong> Anesthesia and Perioperative Care,BogetzM@anesthesia.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Pr<strong>of</strong>essionalism, ReflectionPurpose: To describe students’ perceptions <strong>of</strong>anesthesiology prior to their clinical clerkship.Background: Perceptions <strong>of</strong> another's field <strong>of</strong> practicecan impact interpr<strong>of</strong>essional collaborations. The hiddencurriculum may influence students' perceptions <strong>of</strong> a fieldand these perceptions may persist because studentslack opportunities to challenge them early in training.Inaccurate or negative perceptions may interfere withstudents’ openness to learning and interaction withpatients and team members.Methods: Medical students were asked to "describe onepreconceived notion about the specialty <strong>of</strong> anesthesia"at the start <strong>of</strong> their required <strong>UCSF</strong> anesthesiologyclerkship. Responses were collected from 1,009students from 2003 - 2009. A general inductive approachwas used to analyze students' written preconceptions.Preconceptions were coded with consensus by twoauthors for both theme and tone.Results: Five themes emerged: task responsibilities,patient interaction, lifestyle, reputation, and future <strong>of</strong> thefield. Task responsibilities were discussed mostfrequently(53%), <strong>of</strong>ten with negative tone(56%).Students felt "unclear" about the non-procedural taskresponsibilities <strong>of</strong> anesthesiologists. Patientinteraction(19%) was also perceived negatively(88%),with emphasis on lack <strong>of</strong> longitudinal relationships andlimited time spent with patients. Lifestyle-focusedpreconceptions(10%) were more positive(87%),centering on enviable hours and compensation. Higherlevels <strong>of</strong> substance abuse and difficulty interacting withsurgeons contributed to negative impressions(46%) <strong>of</strong>pr<strong>of</strong>essional reputation(16%). The future <strong>of</strong>anesthesiology(2%) was <strong>of</strong>ten viewed positively(60%),noted for job security and residency competitiveness.Discussion: Negative perceptions can adversely impactinterpr<strong>of</strong>essional respect, communication andcollaboration. Patient care and safety may suffer.Curricular interventions can facilitate more accurate,typically less critical perceptions <strong>of</strong> specialties. Earlierexposure through shadowing, preceptorships andinterest groups, especially during preclinical years, maydispel stereotypes, improving attitudes andunderstanding <strong>of</strong> anesthesiologyReflective critique: Presented and modified accordingto ESCape feedback.Medical Students’ Attention toMultiple Risk Behaviors: AStandardized Patient ExaminationJudith J. Prochaska, PhD, MPH, <strong>UCSF</strong> Department <strong>of</strong>Psychiatry, jprochaska@ucsf.edu; Kathleen Gali, <strong>UCSF</strong>Department <strong>of</strong> Psychiatry, Kathleen.Gali@ucsf.edu;Bernie Miller, <strong>UCSF</strong> Teaching and Learning Center,MillerB@medsch.ucsf.edu; Karen Hauer, MD, <strong>UCSF</strong>Department <strong>of</strong> <strong>Medicine</strong>, khauer@medicine.ucsf.eduAreas abstract covers: UMEDomain(s) addressed: Evaluation <strong>of</strong> Programs andCurricula, Research, Standardized Patients, Healthbehavior changePurpose: This study examined medical students’assessment and treatment <strong>of</strong> multiple risk behaviors in a36 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>standardized patient examination.Background: Risk behaviors tend to cluster andsmokers in particular are likely to engage in multiplerisks. Treating multiple risk behaviors improves patienthealth outcomes and reduces health care costs.Methods: Using a randomized experimental design,medical students’ counseling interactions wereevaluated with a standardized patient presenting withsexual health concerns and current tobacco use withvaried problematic drinking status (alcohol-positive oralcohol-negative). Participants were 156 third yearmedical students at the <strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong>Francisco. Checklists completed by standardizedpatients evaluated students’ clinical performance. Afterthe encounter, students completed surveys <strong>of</strong> theirknowledge and attitudes for treating smokers withalcohol problems.Results: Overall, most students assessed tobacco use(85%); fewer assessed alcohol use (54%). Relative tothe alcohol-negative case, students seeing the alcoholpositivecase were less likely to assess STD history(80% vs. 91%, χ2(1)=4.15, p=.042) or patients’readiness to quit smoking (41% vs. 60%, χ2(1)=5.01,p=.025) and endorsed greater attitudinal barriers totobacco treatment, F(1,155)=4.79, p=.030. Patientsatisfaction, expressed as willingness to continuemedical treatment with the student doctor, wassignificantly lower for the alcohol-positive than thealcohol-negative case, χ2(1)=5.18, p=.023. Clinicalperformance ratings moderated the relationship betweenpatient case version and patient satisfaction.Discussion: When presented with a case <strong>of</strong> multiplerisk behaviors (sexual health, tobacco and alcohol),medical students performed less effectively and receivedlower patient satisfaction ratings than with a caseinvolving fewer behavioral risks. Findings weremoderated by ratings <strong>of</strong> students’ overall clinicalperformance.Reflective critique: The findings support the need forparadigm shifts in medical education that emphasizeassessment <strong>of</strong> multiple risks, new models <strong>of</strong>conceptualizing behavior change as a generalizedprocess, and treatment <strong>of</strong> the whole patient foroptimizing health outcomes.Physical Examination Teaching: ASystematic Review <strong>of</strong> the LiteratureSomnath Mookherjee, MD, <strong>UCSF</strong>, Department <strong>of</strong><strong>Medicine</strong>, Division <strong>of</strong> Hospital <strong>Medicine</strong>,SMookherjee@medicine.ucsf.edu; Lara Pheatt, MA,<strong>UCSF</strong> <strong>School</strong> <strong>of</strong> <strong>Medicine</strong>, Office <strong>of</strong> Medical Education,PheattL@medsch.ucsf.edu; Calvin L. Chou, MD, PhD,<strong>UCSF</strong> and VA Department <strong>of</strong> <strong>Medicine</strong>, Division <strong>of</strong>General Internal <strong>Medicine</strong>, calvin.chou@ucsf.eduAreas abstract covers: UME, GME, CMEDomain(s) addressed: Clinical Instruction andPerformance, Evaluation <strong>of</strong> Programs and Curricula,Patient CarePurpose: To review physical examination (PE) teachingmethods studied in the literature, summarize findings,and recommend best practices.Background: Physicians must be competent in the“synthesis” <strong>of</strong> PE data to make optimal patient caredecisions. Recent reports have bemoaned theinadequacy <strong>of</strong> physicians' PE skills; however, mostschools teach a comprehensive PE without links topatient care. Therefore, PE education needsimprovement, but the most effective teaching methodsare unknown.Methods: We included all publications <strong>of</strong> PE teachingpublished from 1951-<strong>2011</strong> that studied the effects <strong>of</strong> acurricular intervention and reported on teaching efficacy.Data extracted included organ system targeted, studydesign, types <strong>of</strong> curricula, measurements <strong>of</strong> efficacy,and domains <strong>of</strong> PE learning (psychomotor skills,knowledge, communication, and “synthesis” <strong>of</strong> data intoclinical application).Results: Of 3665 papers retrieved, 121 met inclusioncriteria. The most represented organ systems werecardiovascular, musculoskeletal, gynecological, andgeneral (multiple organ systems or comprehensive PE).Sixty-six (55%) studies included control groups. Majorcategories <strong>of</strong> educational interventions includedsimulation with standardized patients (SPs), simulation<strong>of</strong> aspects <strong>of</strong> PE (such as recordings <strong>of</strong> heart sounds),bedside teaching, and peer examination or tutoring.Common assessment methods included checklists withobserved structured clinical examinations, written tests,and surveys <strong>of</strong> learner satisfaction and self-assessedcompetence. Psychomotor skills and knowledgeacquisition were the most common competenciestargeted; seventeen papers (14%) were judged to teachPE in the “synthesis” realm.Discussion: Despite heightened awareness <strong>of</strong> theimportance <strong>of</strong> PE skills in guiding patient care, we foundfew curricula that taught PE “synthesis.” Heterogeneity in<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 37
<strong>UCSF</strong> Education Day <strong>2011</strong>interventions and outcome measurements impedesidentification <strong>of</strong> the most effective teaching methods.Higher quality studies <strong>of</strong> PE teaching, particularly in therealm <strong>of</strong> synthesis, will allow for better identification <strong>of</strong>best practices in this area.Reflective critique: Based on recommendations fromESCape, we will add statistical expertise to the project toassess effect sizes.Pilot <strong>of</strong> a Lifelong Pr<strong>of</strong>essionalDevelopment Metric in a ScholarlyConcentration ProgramRenee Courey, PhD, <strong>UCSF</strong>, renee.courey@ucsf.edu;Carrie Chen, MD, MSEd, <strong>UCSF</strong>,chenhc@peds.ucsf.edu; Louise Aronson, MD, MA,<strong>UCSF</strong>, aronsonl@medicine.ucsf.edu; Kristen Fitzhenry,MS, <strong>UCSF</strong>, FitzhenryK@medsch.ucsf.edu; Josh Adler,MD, <strong>UCSF</strong>, aadlerj@ucsfmedcenter.org; AdditionalPathway to Discovery Directors, <strong>UCSF</strong>Areas abstract covers: UME, GME, IPHEDomain(s) addressed: Competencies, Evaluation <strong>of</strong>Programs and Curricula, Longitudinal EducationalActivities, MentoringPurpose: To design and pilot an assessment tool thatdescribes progress in skills acquisition for scholarshipand leadership careers.Background: The <strong>UCSF</strong> Pathways to Discoveryprogram prepares interpr<strong>of</strong>essional UME and GMEtrainees in discovery and leadership. Learners completeformal curricula and faculty-mentored projects in areasranging from the molecular to the global. Traditionally,assessment measured only course participation, projectquality, presentations, publications, and learnersatisfaction. Because the program aims to launchcareers in innovation, academia and leadership, ameans <strong>of</strong> charting steps along the continuum <strong>of</strong>pr<strong>of</strong>essional development was also required.Methods: We adapted the Dreyfus scale <strong>of</strong> skillacquisition from novice to expert to measure progress inthree competency areas, “Research and Scholarship,”Leadership and Advocacy,” and “Pr<strong>of</strong>essional IdentityDevelopment.” The scale was sent to 52 faculty mentorsand did not allow selection <strong>of</strong> expert.Results: 33/52 faculty mentors responded. For the threecompetency areas, 52%, 64%, and 67%, respectively,placed their mentees at pr<strong>of</strong>icient, the highest availablelevel, describing competency usually achieved at theassistant pr<strong>of</strong>essor stage.Discussion: The number <strong>of</strong> mentors selecting thehighest level <strong>of</strong> achievement greatly exceededexpectations. Program leaders anticipated that mostUME learners would move from novice or beginner tobeginner or competent. The failure to capture accuratedata on the stage <strong>of</strong> learners’ pr<strong>of</strong>essional developmentmay be due to the culture <strong>of</strong> grading. Mentor educationand explicit distinction <strong>of</strong> formative career progressionassessment from summative performance assessmentmay improve appropriate scale use by mentors.Reflective critique: The results <strong>of</strong> the pilot evaluationhave been presented to the Committee on Curriculumand Educational Policy (CCEP). The Pathways toDiscovery Directors have also reviewed this data.Pr<strong>of</strong>essional Deformation: TheRepression <strong>of</strong> Personal Values andAttributes in Medical EducationMichael W. Rabow, MD, <strong>UCSF</strong>,mrabow@medicine.ucsf.edu; Carrie N. Evans, MA,<strong>UCSF</strong>, Carrie.Evans@ucsf.edu; Rachel N. Remen, MD,<strong>UCSF</strong>, drrachel@commonweal.orgAreas abstract covers: UMEDomain(s) addressed: Medical Humanities,Pr<strong>of</strong>essionalism, Reflection, ResearchPurpose: To understand what personal qualities orvalues students believe they might lose or be forced tosurrender during the course <strong>of</strong> their medical education.Background: The process <strong>of</strong> developing character andcommitment to the highest values <strong>of</strong> medicine has beencalled “pr<strong>of</strong>essional formation" (1). However, medicalstudents are at risk for “deformation” as well. Asstudents progress through medical school, they gainpr<strong>of</strong>essional competence but may also be at risk forharm. Prior research has documented the development<strong>of</strong> depression and the loss <strong>of</strong> empathy during medicaltraining. Little research has examined students’ ownexperience <strong>of</strong> such changes.Methods: In 2007-08, Healer’s Art elective studentsinternationally submitted words that described a part <strong>of</strong>themselves that they were wary about showing oractually did not let show in school. These words wereanalyzed using qualitative and quantitative techniques.Results: Words from 673 medical students from 31medical schools were analyzed. Eleven themes wereidentified. The most common themes were Spirituality,Emotional Engagement, Identity/Self-expression,Freedom/Spontaneity, and Relationships. The mostcommon individual words used were “Creativity,”“Family,” “Balance,” “Freedom,” “Love,” and “Peace.”38 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>There were only rare differences in distributions <strong>of</strong>themes across gender, year in school, size <strong>of</strong> school, orschool nationality.Discussion: Healer’s Art medical students identify coreissues and values that they may repress or feel unableto sustain in medical training. According to the dataanalyzed here, medical training involves not onlypr<strong>of</strong>essional formation, but personal deformation as well.Medical educators must attend to both gains inpr<strong>of</strong>essional competence and the personal qualities andvalues that are at risk as students progress throughmedical training.Reflective critique: Judith Wrubel, PhD, anaccomplished qualitative researcher, helped design thestudy and analytic methods.References:1. Rabow MW, Remen RN, Parmelee DX, Inui TS. Pr<strong>of</strong>essionalformation: extending medicine's lineage <strong>of</strong> service into the nextcentury. Acad Med. 2010;85:310-17.Teaching and Assessing MedicalStudents’ Skills in Counseling forBehavior Change: A SystematicReviewKaren E. Hauer, MD, <strong>UCSF</strong>, karen.hauer@ucsf.edu;Patricia Carney, PhD, Oregon Health Sciences<strong>University</strong>, carneyp@ohsu.edu; Anna Chang, MD,<strong>UCSF</strong>, anna.chang2@med.va.gov; Jason Satterfield,PhD, <strong>UCSF</strong>, jsatter@medicine.ucsf.eduAreas abstract covers: UME, GMEDomain(s) addressed: Clinical Instruction andPerformance, Evaluation <strong>of</strong> Programs and Curricula,Patient CarePurpose: To characterize published curricularinterventions to teach medical trainees to counselpatients for behavior change and identify curricularformats that enhance patient outcomes.Background: Unhealthy lifestyle behaviors contribute toapproximately half <strong>of</strong> United States (US) deaths.However, physicians infrequently address importantbehavioral science topics during clinical visits and lacksufficient skill in counseling patients to implementbehavior change.Methods: We conducted a systematic literature search<strong>of</strong> studies published 1965-2010 evaluating curricula oncounseling for behavior change for medial trainees.Included studies described: (1) behavior changecounseling, (2) a teaching intervention for medicaltrainees, and (3) assessment <strong>of</strong> the intervention. Weextracted eligible articles and rated impact on learnersand patients using Kirkpatrick’s hierarchy.Results: Of 2,758 initial citations, 106 met inclusioncriteria. 75 studies described interventions for medicalstudents, and 88 for residents/fellows. Most studiesoccurred in the US (94) at single institutions (91). Themajority (77) occurred in primary care disciplines:internal medicine (36), family medicine (30) andpediatrics (13). The most prevalent study design waspre-post comparison; only 22 studies used a randomizedcontrolled design.The most commonly addressedcurricular topic for counseling for behavior change wassmoking (65 studies) followed by nutrition (27),alcohol/drug use (26), and exercise (20). Theoreticalframeworks uncommonly justified curricularinterventions, although 28 studies used thetranstheoretical model <strong>of</strong> change. 58 studies involved 8or fewer hours <strong>of</strong> curricular time, and 48 spanned 4 orfewer weeks. Outcome measures related to learnerattitudes, knowledge or skills were common; only 8studies showed benefit to patients or organizationalpractice.Discussion: Multi-institutional research on methods <strong>of</strong>teaching trainees counseling for behavior change thatinfluence patients’ health outcomes are urgently neededto ensure trainees’ clinical competence and improvedpatient care.Reflective critique: We will present our manuscript draftat ESCape 3/1/11 for feedback.The Educational Value <strong>of</strong> OvernightCall Amid Resident Duty HoursRestrictionsOren K. Fix, MD, MSc, <strong>UCSF</strong> Medical Center,oren.fix@ucsf.eduAreas abstract covers: GMEDomain(s) addressed: Competencies, Health Systems,Patient Care, Quality ImprovementPurpose: To compare faculty perception <strong>of</strong> theeducational value <strong>of</strong> a rotation with overnight call to onewithout overnight call.Background: The implementation <strong>of</strong> new ACGME dutyhours regulations in July <strong>2011</strong> will place new restrictionson post-graduate year (PGY)-1 trainees, primarily byrestricting consecutive duty hours to 16. Theseregulations limit PGY-1 residents from staying overnightfollowing a normal workday. Residency programs mustconsider the relative educational value <strong>of</strong> overnight callversus alternative duties that provide a similar learningexperience.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 39
<strong>UCSF</strong> Education Day <strong>2011</strong>Methods: An anonymous, 5-item Web-based surveywas e-mailed to clinical faculty <strong>of</strong> a liver transplantrotation. Items solicited opinions about the educationalvalue <strong>of</strong> overnight call, adequacy <strong>of</strong> supervision and thevalue <strong>of</strong> a rotation without overnight call. Answer choiceswere yes/no or multiple choice and includedopportunities for comment. Analyses were descriptiveand qualitative.Results: 10/15 (67%) faculty completed the survey. Allrespondents answered that overnight call waseducationally important for the PGY-1 resident and allfelt that adequate supervision was available. In a rotationwithout overnight call, 90% <strong>of</strong> respondents answeredthat weekend coverage remained educationallyimportant but most felt this did not replace theeducational value <strong>of</strong> overnight call. Respondentsidentified the following competencies learned fromovernight call: development <strong>of</strong> independence,confidence, responsibility, decision-making, prioritizationand communication; cross-covering; and the opportunityto work-up new admissions.Discussion: Despite the scheduling difficulties imposedby new duty hours regulations, overnight call maintains aunique learning experience that should be preservedwhere possible in the training <strong>of</strong> PGY-1 residents.Reflective critique: Survey results were reported to theInternal <strong>Medicine</strong> Residency Program with a proposal tomaintain overnight call if possible, with weekend day asan educationally important, although qualitatively inferior,alternative.References:1. Nasca TJ, Day SH, Amis ES. The new recommendations on dutyhours from the ACGME task force. N Engl J Med 2010;363(2):e3.The <strong>UCSF</strong> Geriatric CommunityResources Clinical Algorithm andGuideChristopher A. Bautista, Christopher.Bautista@ucsf.edu;Louise Aronson, MD, aronsonl@medicine.ucsf.eduBackground: Roughly half <strong>of</strong> current physician visits inmany specialties are from patients >65 years old, andthe population aged >60 is expected to double by 2050.As states increasingly cut services keeping elderlypatients healthy and independent, healthcare providersmust be aware <strong>of</strong>, refer to, and lobby for these vitalgeriatric community resources.Methods: Following a literature review, internetsearches and interpr<strong>of</strong>essional expert focus groups, wedeveloped an algorithm and related guide detailingservices, eligibility, coverage and cost, provider role andlocal contacts. Validity was established through surveys<strong>of</strong> students, residents, faculty and local communityproviders as well as feedback from over 30interpr<strong>of</strong>essional national leaders in Geriatrics. Casebasedpre/post-tests with medical students and residentswere used to evaluate the educational utility <strong>of</strong> the toolsafter a brief introduction.Results: 58% (37/64) <strong>of</strong> survey respondents said thatthey were “somewhat likely” or “very likely” to use thesetools in their clinical practice and teaching. 63% (26/41)<strong>of</strong> learners “agreed” or “strongly agreed” that the toolsmade them more comfortable referring elderly patients tocommunity resources. 64% (9/14) <strong>of</strong> medical studentsand 90% (4/5) <strong>of</strong> residents who completed the pre/posttestscored higher after brief training with the tools.Discussion: The Geriatric Community ResourcesClinical Algorithm and Guide providers a validated andeducationally effective framework to help cliniciansappropriately refer elderly patients to vital communityservices. The tool alone does not help all trainees, some<strong>of</strong> whom may require a dedicated educational sessionon the purpose and uses <strong>of</strong> certain resources.Reflective critique: Presentations at ESCAPE,Geriatrics WIP and dissemination to local and nationalgeriatrics leaders for review led to additional resourcesand refined structure.Areas abstract covers: UME, GME, CME, IPHEDomain(s) addressed: Community <strong>Medicine</strong>,Evaluation <strong>of</strong> Programs and Curricula, Patient Care,Primary CarePurpose: To develop a tool that gives providers apractical conceptual framework for approaching themyriad resources necessary to keep elderly patientshealthy and independent in the community.40 The Haile T. Debas Academy <strong>of</strong> Medical Educators
<strong>UCSF</strong> Education Day <strong>2011</strong>Workshop DescriptionsLeveraging Technology for EducationAmin Azzam, MD, MA; Ryan Brazell; Sean McClelland;Christian Burke; Renee Courey, PhD; Louise Aronson,MD, MFAIn this workshop, participants will learn how to produceonline, interactive, digitally-enhanced learning tools. Thisworkshop will showcase equipment and s<strong>of</strong>twareavailable to educators, and include presentations fromlibrary staff about best practices for creating enhancedlearning tools. Panelists will <strong>of</strong>fer tips for sharing onlinelearning tools with learners and for integrating thesetools into existing courses. Facilitators will demonstratethe process by modifying an existing static educationaltool (e.g., powerpoint lecture slides) into three differentlevels <strong>of</strong> enhancement: 1) web-based slides; 2) audionarration, and 3) an interactive learning module.Learning Objectives:1. Understand techniques for developing online,interactive, digitally-enhanced learning tools.2. Review resources available, including s<strong>of</strong>tware andequipment, available to educators at <strong>UCSF</strong> forproducing learning tools.3. Learn about best practices for sharing online learningtools with learners and opportunities for integratingonline learning into existing courses.Poster Presentations and PrizesLouise Aronson, MD, MFA; Patricia O'Sullivan, EdDIn this workshop, panelists will learn aboutcharacteristics <strong>of</strong> good and bad posters, and learn aboutprinciples <strong>of</strong> poster design to both evaluate and producehigh-quality posters. In an interactive exercise,participants will actively review a range <strong>of</strong> digital posters<strong>of</strong> varying quality using a rubric, with a discussion t<strong>of</strong>ollow about how ratings were established. A follow-updiscussion will focus on best practices in poster visualdesign and graphical presentation <strong>of</strong> information that willhelp participants create and recognize high-qualityposters that are worthy <strong>of</strong> awards when presented atmedical conferences.2. Learn how to better evaluate and review posters, andhow to provide constructive feedback to posterauthors.3. Describe how reviewers typically establish ratingswhen evaluating posters, and how rubrics and otherrating tools can assist the process <strong>of</strong> evaluatingposters.Scholarship <strong>of</strong> SimulationDiane B. Wayne, MD; <strong>San</strong>drijn van Schaik, MD; JodySteinauer, MDIn this workshop, experts will discuss the scholarship <strong>of</strong>simulation as an educational strategy. Panelists willdescribe their own experiences designing simulationresearch projects, and how these activities have affectedtheir own career development. Interactive exercises willhelp participants better understand best practicesassociated with simulation research. Panelists willinspire educators to use simulation for teaching and toimprove the quality and evaluation <strong>of</strong> simulation training.There will be ample opportunity to discuss educators’questions and practical aspects <strong>of</strong> designing simulationresearch.Learning Objectives:1. Describe best practices for incorporating simulationbasededucation into health pr<strong>of</strong>essions education.2. Define strategies for effective simulation-basededucational research.3. Review research gaps and unanswered questions insimulation-based education.Learning Objectives:1. List best practices in poster design in poster visualdesign and graphical presentation <strong>of</strong> information.<strong>University</strong> <strong>of</strong> <strong>California</strong>, <strong>San</strong> Francisco • <strong>School</strong> <strong>of</strong> <strong>Medicine</strong> 41
<strong>UCSF</strong> Education Day <strong>2011</strong>Index by AuthorAdam, Carlson..................................29Adler, Josh .......................................38Adriana, Padilla ................................21Alexander, Erik .................................10Alldredge, Brian..................................9Angelotti, Amanda ............................19Aronson, Louise ....4, 8, 11, 16, 17, 34,38, 40, 41Azzam, Amin ..............................26, 41Barbour, Kelli....................................30Bautista, Christopher........................40Bogetz, Martin ..................................36Boscardin, Christy ......................30, 34Brandeh<strong>of</strong>f, Nicklaus ........................22Brazell, Ryan ....................................41Bruckner, Julia............................25, 35Brzezinski, Marek .......................26, 36Burke, Christian............................8, 41Byrne, Laura.....................................20Campbell, Andre...............................19Carlin, Danielle .................................26Carney, Patricia................................39Chang, Anna ..............................30, 39Chen, Alice HM ................................11Chen, Allison ....................................34Chen, Carrie .....................................38Chen, Esther ....................................19Chen, H. Carrie ..................................9Chern, Hueylan ................................31Chomsky-Higgins, Kate....................28Chou, Calvin...............................30, 37Ciccarone, Daniel .............................22Clouse, Amy.....................................29Coelho, Anabelle D. .........................33Collins-Bride, Gerri ...........................17Courey, Renee ...........................34, 38Courey, Renee .................................41Dhaliwal, Gurpreet............................25Dhand, Amar ....................................25Diaz, Vanessa ..................................33Dicker, Rochelle ...............................19Douglas, Vanja .................................16Duong, David....................................19Evans, Carrie....................................38Fitzhenry, Kristen .............................38Fix, Oren...........................................39Fromont, Sebastien C. .....................28Fulton, Tracy ....................................20Fyfe, Molly..................................30, 32Gali, Kathleen...................................36Gomez, Nicole..................................28Griswold, Virginia .............................23Grubbs, Vanessa..............................11Gupta, Reena ...................................32Hall, Sharon M..................................28Hansen, Lori.....................................10Hauer, Karen..................10, 30, 36, 39Hettema, Jennifer.............................22Hicks, Kathleen ................................18Hill-Sakurai, Laura..............................8Hirsh, David......................................10Houseman, Ben ...............................19Howell, Ben ......................................28Hudmon, Karen Suchanek ...............28Hyde, Susan.......................................9Hyland, Katherine...............................8Jain, Sharad .........................11, 18, 22Johnston, Bree .................................32Josephson, S. Andrew ...............16, 25Jue, Vicki..........................................32Julian, Katherine ..............................34Kaaya, Ephata..................................32Kamel, Hooman ...............................25Kathy, Schlecht ................................26Keenan, Craig ..................................18Kilmer, Jeff .........................................9Kim, Ed.............................................31Kimatian, Stephen............................26Kinman, Renee ................................23Kirsch, Heidi .....................................16Koehler, Gary ...................................27Kripke, Clarissa ................................17Kruidering, Marieke ..........................16Kuo, Anda ..................................11, 20Lai, Cindy ...............................8, 32, 33Land, Kathleen ...................................8Lee, Christina A................................30Leshabari, Sebalda ..........................27Levitt, David Stern............................29Lin, Eric ............................................19Lin, Lisa............................................33Liu, Joseph.......................................16Loeb, Anna.......................................25Loeser, Helen.................................4, 9Loomer, Peter ....................................9Louie, Alan K....................................28Lovett, Mark .....................................34Lyamuya, Eligius ..........................9, 32MacFarlane, Sarah.....................30, 32Mack, Kevin......................................16Mackersie, Robert ............................19Mackin, Lynda ..................................32Manuel, Jennifer...............................22Martin-Holland, Judy ..........................9Massawe, Siriel ................................27Masters, Susan ................................16Mayfield, Chandler ...........................19McClelland, Sean .............................41McCowin, Marcia..............................23Miller, Bernie ....................................36Miller, Carol A. .................................16Mitchell, John ...................................26Mitrovic, Igor ....................................20Mizuguchi, Annette ..........................26Mkony, Charles .......................... 30, 32Mookherjee, Somnath................ 29, 37Moylan, Adam ..................................32Naburi, Helga ...................................27Natt, Guneet............................... 26, 36Navi, Babak......................................25Niehaus, Brian ...................................8O'Brien, Bridget................ 4, 10, 34, 36O'Sullivan, Patricia . 8, 9, 30, 31, 33, 41Patricia, Hom ...................................33Perry, Dorothy.............................. 9, 30Pheatt, Lara .....................................37Pierce, Read ....................................20Poncelet, Ann............................. 10, 16Price, Kathryn ............................ 26, 36Prochaska, Judith ...................... 28, 36Rabow, Michael ...............................38Ratanawongsa, Neda ......................22Remen, Rachel ................................38Rennke, Stephanie ..........................32Roey, Steve .....................................18Satterfield, Jason .............................39Schechter, Matthew .........................20Schillinger, Erika ..............................35Shah, Maulik ....................................25Shapiro, Brad ...................................22Sharpe, Bradley ...............................29Sheu, Leslie C............................ 31, 33Siegel, Jennifer ................................11Sommavilla, Nili ................... 25, 28, 35Staves, Jennifer .................................9Steinauer, Jody ................................41Stewart, Colin E. ..............................26Tat, Sonny........................................20Teherani, Arianne ............................35Tong, Lowell.....................................16Topp, Kimberly...................................9Tran, H. Nicole .................................26Turman, Irene ..................................23van Schaik, <strong>San</strong>drijn .................. 20, 41Vener, Margo ................. 17, 25, 28, 35Wamsley, Maria ...............................34Wayne, Diane B. .......................... 5, 41Weinstein, Stefanie ..........................23Wheeler, Margaret ..................... 25, 28Whichard, Emily ...............................17Wilson, Elisabeth .............................25Yang, Serena ...................................23Youmans, Sharon ..............................9Young, John Q. ................................26Zheng, Patricia.................................3342 The Haile T. Debas Academy <strong>of</strong> Medical Educators