Process - Physician - Fraser Health Authority
Process - Physician - Fraser Health Authority
Process - Physician - Fraser Health Authority
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
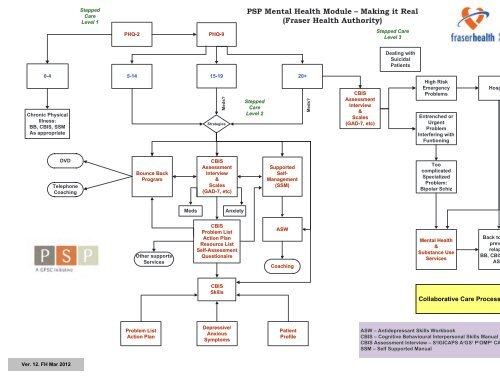
SteppedCareLevel 1PSP Mental <strong>Health</strong> Module – Making it Real(<strong>Fraser</strong> <strong>Health</strong> <strong>Authority</strong>)PHQ-2PHQ-9Stepped CareLevel 3Dealing withSuicidalPatients0-4Chronic PhysicalIllness:BB, CBIS, SSMAs appropriateDVDTelephoneCoaching5-14 15-19 20+Bounce BackProgramMeds?StrategiesCBISAssessmentInterview&Scales(GAD-7, etc)SteppedCareLevel 2SupportedSelf-Management(SSM)Meds?CBISAssessmentInterview&Scales(GAD-7, etc)High RiskEmergencyProblemsEntrenched orUrgentProblemInterfering withFuntioningToocomplicatedSpecializedProblem:Bipolar SchizHospitalDischargedMedsAnxietyOther supportsServicesCBISProblem ListAction PlanResource ListSelf-AssessmentQuestionaireASWCoachingMental <strong>Health</strong>&Substance UseServicesBack to FP topreventrelapse:BB, CBIS, SSM,ASWCBISSkillsProblem ListAction PlanDepressive/AnxiousSymptomsPatientProfileASW – Antidepressant Skills WorkbookCBIS – Cognitive Behavioural Interpersonal Skills ManualCBIS Assessment Interview – S 2 IGICAPS A 2 GS 2 P 3 OMP 2 CAGESSSM – Self Supported Manual
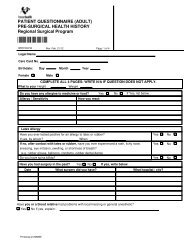
PATIENT HEALTH QUESTIONNAIRE (PHQ-9)NAME: ______________________________________________________________DATE:_________________________Over the last 2 weeks, how often have you beenbothered by any of the following problems?(use “✓” to indicate your answer)Not at allSeveral daysMore than halfthe daysNearly every day1. Little interest or pleasure in doing things2. Feeling down, depressed, or hopeless3. Trouble falling or staying asleep,or sleeping too much4. Feeling tired or having little energy5. Poor appetite or overeating6. Feeling bad about yourself—or thatyou are a failure or have let yourselfor your family down7. Trouble concentrating on things, such as reading thenewspaper or watching television8. Moving or speaking so slowly that other people couldhave noticed. Or the opposite—being so fidgetyor restless that you have been moving around a lotmore than usual9. Thoughts that you would be better off dead,or of hurting yourself in some way0 1 2 30 1 2 30 1 2 30 1 2 30 1 2 30 1 2 30 1 2 30 1 2 30 1 2 3add columns: + +(<strong>Health</strong>care professional: For interpretation of TOTAL,please refer to accompanying scoring card.)TOTAL:10. If you checked off any problems, howdifficult have these problems made it foryou to do your work, take care of things athome, or get along with other people?Not difficult at allSomewhat difficultVery difficultExtremely difficult____________________________PHQ-9 is adapted from PRIME MD TODAY, developed by Drs Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues, with aneducational grant from Pfizer Inc. For research information, contact Dr Spitzer at rls8@columbia.edu. Use of the PHQ-9 may only be made inaccordance with the Terms of Use available at http://www.pfizer.com. Copyright ©1999 Pfizer Inc. All rights reserved. PRIME MD TODAY is atrademark of Pfizer Inc.ZT2420432
Fold back this page before administering this questionnaireINSTRUCTIONS FOR USEPHQ-9 QUICK DEPRESSION ASSESSMENTFor initial diagnosis:for doctor or healthcare professional use only1. Patient completes PHQ-9 Quick Depression Assessment on accompanying tear-off pad.2. If there are at least 4 ✓s in the blue highlighted section (including Questions #1 and #2), consider adepressive disorder. Add score to determine severity.3. Consider Major Depressive Disorder—if there are at least 5 ✓s in the blue highlighted section (one of which corresponds to Question #1 or #2)Consider Other Depressive Disorder—if there are 2 to 4 ✓s in the blue highlighted section (one of which corresponds to Question #1 or #2)Note: Since the questionnaire relies on patient self-report, all responses should be verified by the clinician and a definitive diagnosismade on clinical grounds, taking into account how well the patient understood the questionnaire, as well as other relevantinformation from the patient. Diagnoses of Major Depressive Disorder or Other Depressive Disorder also require impairment of social,occupational, or other important areas of functioning (Question #10) and ruling out normal bereavement, a history of a ManicEpisode (Bipolar Disorder), and a physical disorder, medication, or other drug as the biological cause of the depressive symptoms.To monitor severity over time for newly diagnosed patientsor patients in current treatment for depression:1. Patients may complete questionnaires at baseline and at regular intervals (eg, every 2 weeks) at homeand bring them in at their next appointment for scoring or they may complete the questionnaire duringeach scheduled appointment.2. Add up ✓s by column. For every ✓: Several days = 1 More than half the days = 2 Nearly every day = 33. Add together column scores to get a TOTAL score.4. Refer to the accompanying PHQ-9 Scoring Card to interpret the TOTAL score.5. Results may be included in patients’ files to assist you in setting up a treatment goal, determining degreeof response, as well as guiding treatment intervention.PHQ-9 SCORING CARD FOR SEVERITY DETERMINATIONfor healthcare professional use onlyScoring—add up all checked boxes on PHQ-9For every ✓: Not at all = 0; Several days = 1;More than half the days = 2; Nearly every day = 3Interpretation of Total ScoreTotal Score Depression Severity1-4 Minimal depression5-9 Mild depression10-14 Moderate depression15-19 Moderately severe depression20-27 Severe depression3
<strong>Physician</strong> Referral FormFor adults experiencing mild to moderate depression (PHQ-9 range = 5 to 19),with or without anxiety, community coaches provide telephone delivery of abrief, structured, self-help program to improve mental health.Patient Name: ___________________________________________________________Telephone: ______________________________________________________________Date of Birth: _ ___________________________________________________________Please confirm that the patient:Is not cognitively impairedIs not misusing alcohol or drugsDoes not have a personality disorderIs not severely depressed or at risk to self or othersDoes not have a history of bipolar disorder or psychosisIf available, please include the patient’s PHQ-9 score:PHQ-9 ScoreIs the patient receiving medication for:Depression?Yes NoAnxiety?Yes NoWould the patient prefer to access the program in Cantonese?Yes NoReferring <strong>Physician</strong> and Contact Information:Please transmit referral information to yourBounce Back Community Coach:South <strong>Fraser</strong> (Surrey, Delta, White Rock,Langley, Abbotsford, Chilliwack, Hope)Phone: 604-543-1373 / Fax: 604-543-1369North <strong>Fraser</strong> (New West, Tri-Cities, Maple Ridge,Pitt Meadows, Mission, Harrison, Boston Bar)Phone: 604-515-9889 / Fax: 604-524-2870
CBISCOGNITIVE BEHAVIOURAL INTERPERSONAL SKILLS MANUAL5
AcknowledgementsThe development of the Cognitive Behavioural Skills Manual was initially sponsoredby the Vancouver Island <strong>Health</strong> <strong>Authority</strong>. The General Practice Services Committeeprovided funding to tailor the manual for the Practice Support Program, a joint initiativeof the BC Ministry of <strong>Health</strong> and the BC Medical Association.The preparation of this manual has been a truly collaborative process. Many peoplehave given freely of their time to contribute their experience with cognitive behavioralskills. We wish to acknowledge all of them and in particular:Rivian Weinerman, MD, FRCPC – Site Chief of Psychiatry, VIHAHelen Campbell, MD, FRCPC – Clinical Director, USTAT, VIHAMagee Miller, MSW – Clinical Therapist, VIHAJanet Stretch, RPN – Nurse Therapist, VIHAAnne Corbishley, PHD – Registered Psychologist, VIHAAny part of this manual may be reproduced in any form and by any means withoutwritten permission or acknowledgement. However, permission to alter or modify anypart must rst be obtained from the Shared Care Team, USTAT Clinic, 1119 PembrokeStreet, Victoria BC, V8T 1J5, Phone 250-213-4400, Fax 250-213-4401.General ServicesPractice CommitteeCBIS MANUAL | MAY 20096
Table of ContentsINTRODUCTION. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1• Patient Empowerment In Depression . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2• Tips . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3FLOW CHARTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5ASSESSMENT MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11• Diagnostic Screening Interview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12• Diagnostic Screening Worksheet . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18• Problem List. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20• Problem List Action Plan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21• Resource List. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22• Self-Assessment Questionnaire . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23• Self-Assessment Pro le . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25EDUCATION MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28• Understanding Depression – Frequently Asked Questions . . . . . . . . . . . . . . . . . . 29• Depression – “System-Wide Crash” . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31• Will Medication Help Me? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32ACTIVATION MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33• Anti-Depression Activities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34• Depression’s Energy Budget . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35• Small Goals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37• Problem Solving . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39• Opposite Action Strategy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40• Chunk The Day . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41• Improve the Moment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42• Appreciation Exercise . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43CONTINUED ON NEXT PAGECBIS MANUAL | MAY 20097
Table of Contents. . . CONTINUEDCOGNITION MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44• The Circle of Depression . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45• Common Thinking Errors. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47• Thought Change <strong>Process</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48• Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50• Thought Stopping . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 51• Worry Time . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52• Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53• Assertiveness Skills. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 54• Setting Limits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55• Is Anger a Problem for You? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57RELAXATION MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58• Introduction to Relaxation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 59• Abdominal Breathing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60• Grounding . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62• Body Scan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 63• Passive Relaxation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 64• Stress Busters . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 65• One Minute Stress Break . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 66• Mindfulness . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67• Mindfulness Meditation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 68LIFESTYLE MODULE . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70• <strong>Health</strong>y Habits For Sleeping . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 71• It’s True: You are What You Eat! . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 72• Physical Activity . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 74• The Wellness Wheel . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 75CBIS MANUAL | MAY 20098
IntroductionThe following modules have been designed to be userfriendly for you and your patients.The intent is that patients be empowered througheducation and coping strategies to effectively dealwith the impact of depression on their lives.The introduction section contains an explanationof self-management and patient empowerment andstrategies for you to help your patients implementself-management.CBIS MANUAL | MAY 2009INTRODUCTION | 19
Patient Empowermentin Depression• Self-Management has been considered paramount in the management of chronicdiseases such as diabetes, arthritis and congestive heart failure.• It is now being incorporated into the care of Major Depression, which is beingrecognized as a chronic disease.• Self-Management focuses on the impact patients can have when they take an activerole in their health.• Self-Management is a collaboration of patients with their doctors and other healthcare providers around their health problems.• The goal of self-management is to help patients become educated regarding theirdisease, particular problems of their disease, what to expect from their treatment,and what questions to ask about their care.• Patients are involved in setting the priorities of their treatment, and establishing thegoals of their care.• In this manual we have expanded the scope and de nition of self-management toinclude teaching skills to help patients take a more active stance in their treatment.• Our intention is to assist patients in realizing that they can manage their symptomsand actually are able to change the way they behave, think and feel.• The intent of this manual is to help health care providers empower people withdepression by involving them in learning the skills to manage and/or change theirdepressive symptoms.• We have included assessment tools, educational handouts about depression,and many easy to use activation, cognitive-behavioural, relaxation andlifestyle interventions.CBIS MANUAL | MAY 2009INTRODUCTION | 210
TipsTeachingSelling Strategies• Explain how the self-management strategies impact their depression and supplementany medication they may be taking.ImplementingBite Size• Don’t hand out the whole package of skills at once. Try one at a time. Select theskill/activity that you think fits the person and that she/he is most likely tosuccessfully accomplish.Achieving Goals• Set realistic goals and low expectations. In order to guarantee success aim at theminimum the patient is certain of achieving over a specific period of time. Aim for acommitment of 75% or higher.Building Skills• If they practice skill #1 the first week, then in the second week they can add #2, butstill continue doing #1. The end goal is to have a repertoire of well-practiced skills,which then become automatic.PlanningOrganize• Schedule regular follow-up and remember to use bite-size pieces (one handout ata time) to fit with “real” GP time. Set up binders with sleeves that contain copies ofhandouts for easy use. Keep notes on what handouts have been given.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009INTRODUCTION | 311
TIPS (CONTINUED)SupportingValidate and Encourage• Acknowledge your patient’s feelings, then firmly and gently encourage them to try aself-management strategy.Monitoring and Praise• Ask about skill practice at every visit. Congratulate them on their effort, as well astheir achievements.Practice, Practice, Practice• You may need to help your patients set specific times, frequency, where they willpractice and how they’ll remind themselves to practice.CBIS MANUAL | MAY 2009INTRODUCTION | 412
Flow ChartsThis module contains flow charts that direct you tothe appropriate treatment strategies in this manual.When in doubt — go with the flow.CBIS MANUAL | MAY 2009FLOW CHARTS | 513
Patient NeedsTryASSESSMENT MODULEDiagnostic Questionnaire . . . . . . . . . . . . . . 12Diagnostic Worksheet . . . . . . . . . . . . . . . . . 18AssessmentProblem List. . . . . . . . . . . . . . . . . . . . . . . . . 20Problem List Action Plan . . . . . . . . . . . . . . . 21Resource List. . . . . . . . . . . . . . . . . . . . . . . . 22Self Assessment Questionnaire. . . . . . . . . 23Self Assessment Profile. . . . . . . . . . . . . . . . 25EDUCATION MODULEUnderstanding Depression . . . . . . . . . . . . . 29Depression: “System Wide Crash” . . . . . . . 31EducationWill Medication Help Me? . . . . . . . . . . . . . . 32LIFESTYLE MODULE<strong>Health</strong>y Habits for Sleeping. . . . . . . . . . . . . 71It’s True: You are What You Eat, . . . . . . . . . 72Physical Activity. . . . . . . . . . . . . . . . . . . . . . 74The Wellness Wheel . . . . . . . . . . . . . . . . . . 75Anti-Depression Activities . . . . . . . . . . . . . . 34Depression’s Energy Budget. . . . . . . . . . . . 35Small Goals . . . . . . . . . . . . . . . . . . . . . . . . . 37ActivationProblem Solving . . . . . . . . . . . . . . . . . . . . . 39Opposite Action Strategy . . . . . . . . . . . . . . . 40Chunk the Day . . . . . . . . . . . . . . . . . . . . . . . 41Improve the Moment . . . . . . . . . . . . . . . . . . 42Appreciation Exercise . . . . . . . . . . . . . . . . . 43CBIS MANUAL | MAY 2009FLOW CHARTS | 614
Patient NeedsTryThe Circle of Depression . . . . . . . . . . . . . . . 45Common Thinking Errors . . . . . . . . . . . . . . . 47Thought Change <strong>Process</strong> . . . . . . . . . . . . . . 48Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50CognitionThought Stopping . . . . . . . . . . . . . . . . . . . . 51Worry Time . . . . . . . . . . . . . . . . . . . . . . . . . 52Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . 53Assertiveness Skills . . . . . . . . . . . . . . . . . . . 54Setting Limits. . . . . . . . . . . . . . . . . . . . . . . . 55Is Anger a Problem for You . . . . . . . . . . . . . 57Introduction to Relaxation . . . . . . . . . . . . . . 59Abdominal Breathing . . . . . . . . . . . . . . . . . . 60Grounding,. . . . . . . . . . . . . . . . . . . . . . . . . . 62RelaxationBody Scan . . . . . . . . . . . . . . . . . . . . . . . . . . 63Passive Relaxation . . . . . . . . . . . . . . . . . . . 64Stress Busters . . . . . . . . . . . . . . . . . . . . . . . 65One Minute Stress Break . . . . . . . . . . . . . . 66Mindfulness . . . . . . . . . . . . . . . . . . . . . . . . . 67Mindfulness Meditation . . . . . . . . . . . . . . . . 68<strong>Health</strong>y Habits for Sleeping, . . . . . . . . . . . . 71LifestyleIt’s True: You are What You Eat. . . . . . . . . . 72Physical Activity. . . . . . . . . . . . . . . . . . . . . . 74The Wellness Wheel . . . . . . . . . . . . . . . . . . 75CBIS MANUAL | MAY 2009 FLOW CHARTS | 715
DepressiveSymptomsTryVegetative SignsNot Attendingto ADLLow ActivityLow MotivationACTIVATION MODULEAnti-Depression Activities . . . . . . . . . . . . . . 34Depression’s Energy Budget. . . . . . . . . . . . 35Small Goals . . . . . . . . . . . . . . . . . . . . . . . . . 37Problem Solving . . . . . . . . . . . . . . . . . . . . . 39Opposite Action Strategy . . . . . . . . . . . . . . . 40Chunk the Day, . . . . . . . . . . . . . . . . . . . . . . 41Improve the Moment . . . . . . . . . . . . . . . . . . 42Appreciation Exercise . . . . . . . . . . . . . . . . . 43TearfulSadHopelessHelplessACTIVATION MODULEChunk the Day . . . . . . . . . . . . . . . . . . . . . . . 41Improve The Moment . . . . . . . . . . . . . . . . . 42Appreciation Exercise . . . . . . . . . . . . . . . . . 43NegativeThinkingCognitiveDistortionsCOGNITION MODULEThe Circle of Depression . . . . . . . . . . . . . . . 45Common Thinking Errors . . . . . . . . . . . . . . . 47Thought Change <strong>Process</strong> . . . . . . . . . . . . . . 48Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50Thought Stopping . . . . . . . . . . . . . . . . . . . . 51Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . 53Is Anger a Problem for You . . . . . . . . . . . . . 57Low Self EsteemPassiveACTIVATION MODULEAppreciation Exercise . . . . . . . . . . . . . . . . . 43COGNITION MODULESelf Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . 53Assertiveness Skills . . . . . . . . . . . . . . . . . . . 54CBIS MANUAL | MAY 2009 FLOW CHARTS | 816
AnxiousSymptomsTryOverwhelmedChaoticPanickyACTIVATION MODULEAnti-Depression Activities . . . . . . . . . . . . . . 34Small Goals . . . . . . . . . . . . . . . . . . . . . . . . . 37Problem Solving . . . . . . . . . . . . . . . . . . . . . 39Chunk the Day . . . . . . . . . . . . . . . . . . . . . . . 41RELAXATION MODULEAbdominal Breathing . . . . . . . . . . . . . . . . . . 60Grounding . . . . . . . . . . . . . . . . . . . . . . . . . . 62Passive Relaxation . . . . . . . . . . . . . . . . . . . 64Mindfulness . . . . . . . . . . . . . . . . . . . . . . . . . 67RuminatingObsessingWorryingCOGNITION MODULECircle of Depression . . . . . . . . . . . . . . . . . . 45Thought Change <strong>Process</strong> . . . . . . . . . . . . . . 48Thought Stopping . . . . . . . . . . . . . . . . . . . . 51Worry Time . . . . . . . . . . . . . . . . . . . . . . . . . 52RELAXATION MODULEAbdominal Breathing . . . . . . . . . . . . . . . . . . 60Grounding . . . . . . . . . . . . . . . . . . . . . . . . . . 62Passive Relaxation . . . . . . . . . . . . . . . . . . . 64Stress Busters . . . . . . . . . . . . . . . . . . . . . . . 65AgitatedAnxiousIrritableTenseStressedRELAXATION MODULEIntroduction to Relaxation . . . . . . . . . . . . . . 59Abdominal Breathing . . . . . . . . . . . . . . . . . . 60Grounding . . . . . . . . . . . . . . . . . . . . . . . . . . 62Body Scan . . . . . . . . . . . . . . . . . . . . . . . . . . 63Passive Relaxation . . . . . . . . . . . . . . . . . . . 64Stress Busters, . . . . . . . . . . . . . . . . . . . . . . 65One Minute Stress Break . . . . . . . . . . . . . . 67Mindfulness . . . . . . . . . . . . . . . . . . . . . . . . . 67Mindfulness Meditation . . . . . . . . . . . . . . . . 68CBIS MANUAL | MAY 2009 FLOW CHARTS | 917
Patient ProfileTryPleaserProfileASSESSMENT MODULEPleaser Profile . . . . . . . . . . . . . . . . . . . . . . . 25COGNITION MODULECommon Thinking Errors . . . . . . . . . . . . . . . 47Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . 53Assertiveness Skills . . . . . . . . . . . . . . . . . . . 54Setting Limits. . . . . . . . . . . . . . . . . . . . . . . . 55Is Anger a Problem for You . . . . . . . . . . . . . 57PerfectionistProfileASSESSMENT MODULEPerfectionist Profile . . . . . . . . . . . . . . . . . . . 26COGNITION MODULECommon Thinking Errors . . . . . . . . . . . . . . . 47Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50RELAXATION MODULEAbdominal Breathing . . . . . . . . . . . . . . . . . . 60Stress Busters . . . . . . . . . . . . . . . . . . . . . . . 65One Minute Stress Break . . . . . . . . . . . . . . 66Over-thinkerProfileASSESSMENT MODULEOver-thinker Profile . . . . . . . . . . . . . . . . . . . 27ACTIVATION MODULEImprove the Moment . . . . . . . . . . . . . . . . . . 42Appreciation Exercise . . . . . . . . . . . . . . . . . 43COGNITION MODULECircle of Depression . . . . . . . . . . . . . . . . . . 45Common Thinking Errors . . . . . . . . . . . . . . . 47Thought Change <strong>Process</strong> . . . . . . . . . . . . . . 48Self Talk (Mean Talk) . . . . . . . . . . . . . . . . . . 50Thought Stopping, . . . . . . . . . . . . . . . . . . . . 51Worry Time . . . . . . . . . . . . . . . . . . . . . . . . . 52Good Guilt / Bad Guilt . . . . . . . . . . . . . . . . . 53Is Anger a Problem for You . . . . . . . . . . . . . 57CBIS MANUAL | MAY 2009 FLOW CHARTS | 1018
Assessment ModuleThe Assessment Module contains a diagnosticquestionnaire and worksheet(S²IGECAPS A²GS P³OMP² CAGES)There are two patient handouts, the problem listand resource list that elicit patients’ participation intheir assessment.The problem list worksheet helps formulate anaction plan.The self-assessment questionnaire matches thesection with the highest scores to the correspondingself-assessment profile.High scores on questions:1 – 7 = Pleaser Profile8 – 14 = Perfectionist Profile15 – 21 = Over-thinker ProfileCBIS MANUAL | MAY 2009ASSESSMENT | 1119
Diagnostic Screening InterviewS²IGECAPS A²GS P³OMP² CAGESAlthough this is quite mechanical, your answers to these questions will give us abaseline, which helps us make a more accurate diagnosis and makes sure we are notmissing any other diagnosis.On a scale where 1 = the worst and 10 = the best, please answer on average these days.1 Sadnessa. How sad are you if 1 = the worst and 10 = the best on average these days? . . . .b. Most sad about what? First thing that comes to your mind . . . . . . . . . . . . . . . . . .2 Sleepa. If 1 = the worst and 10 = the best, how would you rate your sleep on averagethese days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. Does it take you minutes or hours to fall asleep? . . . . . . . . . . . . . . . . . . . . . . . . .c. How many hours do you sleep if you add them all up, even if they are interrupted?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .d. Do you feel rested or not rested when you wake up? . . . . . . . . . . . . . . . . . . . . .e. Do you nap during the day? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .f. Do you snore? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 Interest/pleasure in lifea. How would you rate your interest/pleasure in life if 1 = the worst and 10 = the best4 Guilton average these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .a. How would you rate your guilt on average these days if 1 = the worstand 10 = the best on average these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. Most guilty about what? First thing that comes to your mind . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 1220
5 Energy levela. How would you rate your energy level if 1 = the worst and 10 = the best onaverage these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6 Concentrationa. How would you rate your concentration if 1 = the worst and 10 = the best onaverage these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7 Appetitea. How would you rate your appetite if 1 = the most unhealthy and 10 = the mosthealthy, on average these days?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. Have you gained or lost weight in the past months and how much?. . . . . . . . . . .c. Have you ever been anorexic (restricted your food) or bulimic (binge eat or causedyourself to vomit)? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8 Psychomotor Retardationa. That dragged out feeling when you wake up and drag yourself through the day,how would you rate it if 1 = the most dragged out and 10 = not dragged out at all,on average these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. That edgy irritable feeling, 1 = the most irritable and 10 = the least, how would yourate it on average these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9 Suicidea. Now looking at suicide, rst let’s look at suicidal thoughts, then we’ll look atsuicidal intent.b. Looking at suicidal thoughts if 1 = thinking about suicide all the time and 10 = notthinking about suicide at all, how would you rate your thoughts, on averagethese days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .c. Do you have a plan? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .d. Have you gathered materials to carry out suicide? . . . . . . . . . . . . . . . . . . . . . . . .e. What keeps you going and/or gives you hope?. . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 1321
f. Looking at intent, how would you rate your intent, 1= I am de nitely going to do it,you cannot stop me, and 10 = I have thoughts but I don’t intend to do it? . . . . . . .g. Have you ever attempted suicide in the past?. . . . . . . . . . . . . . . . . . . . . . . . . . . .When? . . . . . . . . . . . . . . . . . . . . . How?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .h. Have you ever cut or burned yourself? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10 Anger/Frustrationa. How much frustration/anger do you carry inside you if 1= a lot and 10 = notmuch, on average these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. Most angry about what? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .c. Do you have any homicidal thoughts, and if so against whom? . . . . . . . . . . . . . .11 Anxietya. How much anxiety do you struggle with if 1= the worst and 10 = the best onaverage these days? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12 Generalized Anxietya. There are several types of anxiety; one is a generalized anxiety where a person isa worrywart. Have you ever been called a worrywart? . . . . . . . . . . . . . . . . . . . . .Do you worry more than most people about everyday things and have troublecontrolling it? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Does it keep you awake at night or make you feel sick?. . . . . . . . . . . . . . . . . . . .13 Social Anxietya. Then there is social anxiety where a person is painfully shy, avoids meeting newpeople and worries about being embarrassed or humiliated.14 PanicCan you relate to this? . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .a. Then there are panic attacks where suddenly, out of the blue, your heart is racing,you are breathing quickly, your mouth and ngers may be tingly, and you think youare going to die or loose control. It comes and goes very quickly.Can you relate to this?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .If yes, how many panic attacks a day/week/month? . . . . . . . . . . . . . . . . . . . . . . .CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 1422
15 Phobiasa. Any unrealistic or excessive fears of objects or situations like open spaces, closedspaces, elevators, snakes, or spiders?What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .16 Post Traumatic Stress Disordera. Sometimes people have experienced sexual or physical abuse or suffered majortrauma like MVA or war traumas, or multiple surgeries. Have you had any of these?What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. People can experience symptoms like nightmares or ashbacks, or they startleeasily, become hyper-vigilent, space out and avoid anything that triggers them.Have you had any of these symptoms?What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .17 Obsessive Compulsive Disordera. Do you have any obsessions/compulsions, for instance, do you wash your hands,check things repeatedly, count things, or need everything in perfect order? . . . . .What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Do any of these activities take over an hour a day? . . . . . . . . . . . . . . . . . . . . . . .18 Mood Patternsa. Some people have a low-grade unhappiness for more days then not that goesback at least 2 years. This is called dysthymia.Can you relate to this?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. Sometimes this can dip into a deeper depression causing some of the symptomswe mentioned at the beginning. If it lasts for 2 weeks solid or more we call it amajor depression. Then treated or untreated it may get better and if it occursagain, we call it recurrent major depression.Can you relate to this? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .c. How many episodes have you had that have lasted 2 weeks or more? . . . . . . . .d. What treatment helped you get over past depressions?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 1523
e. Looking at the opposite of depression, this is called bipolar or manic depressivedisorder. Here we are talking about staying up for nights on end without the needfor sleep, talking fast, thinking fast, spending money like it is going out of style,getting into debt, feeling super sexual, being promiscuous. If this lasts for 4 dayssolid or more we can call this a hypomanic or manic episode.Have you had this experience? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19 Psychosisa. Have you ever lost touch with reality, hearing voices or seeing things that othersdon’t, feeling that someone could magically put thoughts into your mind or takethoughts out of your mind, or that you were getting messages from the TV or radio,or being conspired against?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .20 Personalitya. If we were to ask the person who knows you best about your personality, goodthings and bad, what might they say about you and the way you relate to others?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .b. There are several personality styles. Which style would best describe you most ofthe time?■ Generally, I get on well with most people■ Suspicious■ Loner■ Odd or unusual■ Bad or mean■ Emotions feel too intense to tolerate■ Flamboyant or dramatic■ Special or important■ Avoidant■ Need others to take care of me■ Rigid and perfectionistCBIS MANUAL | MAY 2009CONTINUED ON NEXT PAGEASSESSMENT | 1624
21 CAGEHow many drinks might you have in a typical week? . . . . . . . . . . . . . . . . . . . . . . . .Are you concerned about your alcohol use? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Cut down – Have you ever tried to cut down?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Annoyed – Do you get annoyed when others comment on your drinking? . . . . . . . .Guilty – Do you ever feel guilty about your drinking? . . . . . . . . . . . . . . . . . . . . . . . .Eye opener – Have you ever had a drink rst thing in the day to feel better? . . . . . .22 SubstancesDo you use other substances? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .What? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .How often? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Are you concerned about your drug use? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .23 Is there a family history of depression, anxiety, schizophrenia, bipolar or substanceabuse?. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .24 What medications have you been on? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .What medications are you on now? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .For how long? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .What percentage improvement have you felt on your present medications? . . . . . .CBIS MANUAL | MAY 2009ASSESSMENT | 1725
Diagnostic Screening Worksheet(SCALE: 1=WORST, 10=BEST)S²IGECAPS 1 TO 10 COMMENTSSadnessSleepInterest/PleasureGuiltEnergyConcentrationAppetitePsychomotor• Slowing• AgitationSuicide• Thoughts• Plan• Hope• IntentA²GS 1 TO 10 COMMENTSAngerAnxietyGeneralizedSocialCONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 1826
DIAGNOSTIC SCREENING WORKSHEET (CONTINUED)(SCALE: 1=WORST, 10=BEST)P³OMP² 1 TO 10 COMMENTSPanic AttacksPhobiasPTSDOCDMood Patterns• Dysthymia• Depression• ManiaPsychosisPersonalityCAGES 1 TO 10 COMMENTSAlcohol• Cut down• Annoyed• Guilty• Eye openerSubstancesFamily Psych HistoryMedication HistoryCBIS MANUAL | MAY 2009ASSESSMENT | 1927
Problem ListPlease list below every problem that is troubling you. Don’t leave any out.When you come back we will go over this list and decide together what tools mightbe helpful.1 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .11 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CBIS MANUAL | MAY 2009ASSESSMENT | 2028
Problem List Action PlanACTIVATIONRELAXATIONCOGNITIONLIFESTYLEMEDICATIONREFERRALCBIS MANUAL | MAY 2009ASSESSMENT | 2129
Resource ListPlease list below all of your internal resources (these are qualities you possess likeintelligence, sense of humour, creativity, loyalty, perseverance, spirituality, etc) andexternal resources (these can be supports such as family, friends, pets, hobbies,activities, favourite places, nature, positive memories).Internal and external resources help us cope with life.1 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .11 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CBIS MANUAL | MAY 2009ASSESSMENT | 2230
Self-Assessment QuestionnaireName: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Date: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Please rate how well each of the statements below describes your usual way ofinteracting with your world.0 = Never or rarely true to me; 1 = Somewhat true; 2 = Quite a bit true; 3 = Very true of me.1 . . . . . It’s hard for me to say no to people even if I don’t want to agree or don’t havethe time or energy.2 . . . . . I will do almost anything to avoid hurting people’s feelings, whatever the costto myself.3 . . . . . I do lots of things for others, even at the expense of meeting my own needs.4 . . . . . Sometimes I am overwhelmed by things I do for others and have no life ortime of my own.5 . . . . . I am not con dent about expressing my ideas or opinions to others.6 . . . . . Sometimes I think people take advantage of my willingness to help.7 . . . . . I am afraid that people would not like me if I said “no” to them.8 . . . . . I get very upset if I can’t keep things organized and in control.9 . . . . . I always take on extra tasks, and am known for being ef cient.10 . . . . . I push myself to always do my best at everything — I hate making mistakes.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ASSESSMENT | 2331
11 . . . . . I would be very upset if people knew my faults.SELF-ASSESSMENT QUESTIONNAIRE (CONTINUED)12 . . . . . I often struggle to get things done as well as possible.13 . . . . . Sometimes I take much longer than others to do things, because I want to dothem right.14 . . . . . I am afraid that I would be rejected if I did not do excellent work.15 . . . . . When things go wrong, I tend to withdraw and isolate myself.16 . . . . . I spent a lot of time thinking about all the mistakes I have made, and all ofmy failures.17 . . . . . I often think I have done something wrong or there is something wrong with me.18 . . . . . It is very easy for me to see all my faults, but I downplay any good pointsabout myself.19 . . . . . I get dragged down, sometimes for hours, by all the negatives in the world.20 . . . . . I often feel that I am inferior or unworthy compared to others.21 . . . . . I often think of the worst that may happen and imagine how things will go wrong.Please circle any of the following that you feel describe you or that others have used todescribe you.PERFECTIONIST NEGATIVE UNASSERTIVE CONTROLLINGPLEASER PUSHOVER OVER CONSCIENTIOUS CYNICALCBIS MANUAL | MAY 2009ASSESSMENT | 2432
Self-Assessment ProfilePleaser: High scores on questions 1 – 7DESCRIPTION OF TYPEDOMINANT FEELINGSATTITUDETOWARD SELF• Passive, unassertive• Can’t say no or standup for self• Does everythingfor others• Reluctant to drawattention to self• Scared of rejection orbeing disliked• May have dif cultybeing alone• Worried• Helpless• Scared• Overwhelmed• Exhausted• Torn different waysSIMPLE STRATEGIES• I am inferior• I don’t count• I must be good• Everyone wants apiece of me• Take small risks in saying no• Express own ideas, preferences,opinions• Test out to see if expected rejectionoccurs• Build in time for own needs• Plan and rehearse how to set limitswith others• Do things aloneCBIS MANUAL | MAY 2009ASSESSMENT | 2533
Self-Assessment ProfilePerfectionist: High scores on questions 8 – 14DESCRIPTION OF TYPEDOMINANT FEELINGSATTITUDETOWARD SELF• Afraid to makemistakes• Over-controlling• Over-organized• Agonizes overmistakes• Pushes self too hard• Dif culty prioritizing• Take on more thancan manage• May present well andbe very successfulbut cost is high• Afraid of rejection ifothers find out she/he is not perfect or asgood as appears to be• Pressured• Anxious• Vigilant• TensesSIMPLE STRATEGIES• I am flawed andinadequate andmustn’t let otherssee it• I have very highstandards and amworthless if I don’treach them allthe time• Prioritize instead of doing everythingto same high standard• Reduce expectations of self• Set more realistic standards• Have days off from perfection• Stop using “should” for a week• Leave unplanned spaces in the day• Loosen your schedule• Drop some engagements orinvolvementsCBIS MANUAL | MAY 2009ASSESSMENT | 2634
Self-Assessment ProfileOver-Thinker: High scores on questions 15 – 20DESCRIPTION OF TYPEDOMINANT FEELINGSATTITUDETOWARD SELF• Ruminates• Predicts negativeoutcomes• Self-blame• Withdraws andsocially isolates• May be cynical• Constant analysisof self and ownperformance for aws• May blame others orthe system• Hopeless• Gloomy• Alienated• Depressed• May be angry• I am a failure• I am worthless• I never get a break• Nothing goes rightfor meSIMPLE STRATEGIES• Get out and have at least one socialcontact a day• Practice smiling at people• Counter negative thoughts with morerealistic and helpful thoughts• Volunteer• Play with a pet• Stop watching the news• Watch funny movies• Sing• Do an active sportCBIS MANUAL | MAY 2009 ASSESSMENT | 2735
Education ModuleThe Education Module contains 3 handouts providingbasic information on depression and medication forpatients and their families.It includes information regarding the etiology andsymptomatology of depression.CBIS MANUAL | MAY 2009EDUCATION | 2836
Understanding Depression– Frequently Asked QuestionsWho gets depressed?Anyone. Depression can be triggered by many things: for example, a loss, a change forthe worse, an increase in overwhelming responsibilities, or intolerable living conditions.Here are some examples:1 Since George lost his wife, he has become withdrawn, spends much of his daythinking about happier times, as well as his faults as a husband. He can see noreason to keep on living.2 Isabelle has chronic back pain and cannot take care of her family. She feels guiltyabout this and also about her irritability. She has lost interest in her appearance andcan see no hope for the future.3 Tony is a single parent with 3 small children and a low-paying job. He feelsoverwhelmed trying to make ends meet and feels helpless to cope with all hisproblems. Most days, he’d like to just give up.Why are some of us more vulnerable todepression than others?Depression is more easily triggered in some of us. Those of us who have had traumain our lives or who have a family history of depression may be more at risk than others.Some common beliefs can trigger depression; for example, “In order to feel good aboutmyself I should always do well in everything…” “I must always please everyone…”“I must never make any mistakes…”Isn’t it just brain chemicals out of balance?While brain chemicals are likely out of balance, this is only one aspect of depression; forexample, our circumstances, our social supports, and the resources we have in uencewhether we get depressed.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009EDUCATION | 2937
UNDERSTANDING DEPRESSION– FREQUENTLY ASKED QUESTIONS (CONTINUED)Why doesn’t depression just go away?Depression goes far beyond normal feelings of grief or sadness. Depression createsintense thoughts and feelings of worthlessness, helplessness, and guilt. The fatigueand slowness of depression can make us withdraw, procrastinate, or have troubleconcentrating. Sleep, appetite and interest in sex can be affected. When we aredepressed we have trouble enjoying life. Our thoughts turn to the most depressing andnegative aspects of a situation. We become self-blamers. All of these symptoms make italmost impossible to cope, even with small everyday tasks. The less we see ourselvescoping, the more depressed we become.All of these feelings, thoughts, and behaviours help keep depression alive.What can be done about depression?The good news is the many things can help with depression. Research shows that usingseveral approaches provides the best outcome in treating depression. These include(in various combinations) medication, therapy, and self-management activities.A healthy outcome is most likely to occur if depression is tackled early usingself-management.CBIS MANUAL | MAY 2009EDUCATION | 3038
Depression: System-Wide CrashDepression is not who you are. Depression is like a blanket or mask that hides your realpersonality.Depression is not your fault; it is not because you are weak, or a “loser.” Depression isan illness, with symptoms like any other illness.These are some of the common symptoms of depression:BODY BEHAVIOUR MIND FEELINGS• No energy• Sleepchanges• Appetitechanges• Weightchanges• Stomachproblems• No sexualinterest• Lump in throat• Tensemuscles• Diarrhea• Constipation• Feel weigheddown• Pain• Agitated,restless• Cry at leastthing• Can’t startthings• Socialwithdrawal• Can’t nishthings• Clumsy• Slowed down• Snap atpeople• Franticallybusy• Do nothing• Stop hobbies,etc.• Easilydistracted• Poor memory• Can’t thinkclearly• Body imageworry• Can’t makedecisions• Slowedthinking• Racingthoughts• Spaced out• Obsessivethinking• Self-critical• Negativefocus• Worrying• Depressed,down• Anxious,scared• Hopeless• Numb• Discouraged• Worthless,inadequate• Ashamed,guilty• Can’t feelpleasure• Helpless• Lost• Frustrated• Alone• SuicidalthoughtsCBIS MANUAL | MAY 2009 EDUCATION | 3139
Will Medication Help Me?For some people, taking medication can make a significant difference in their moods. Itis especially helpful with sleep, energy levels, and severe mood swings.Sometimes people need to have their sleep problems sorted out and their energy levelsback in order to participate in counseling, start an exercise program or make otherimportant changes in their lives.Talk to your doctor or mental health professional about the medications that are availableand which ones might help you. Make informed decisions.Questions to Discuss• How might this medication help me?• How soon might I notice a difference?• What side effects might I get?• How long do I need to stay on it?• What if I miss a dose?• Will my medication interact with other medications I take?Be PatientMost medications take time to work (up to 6 – 8 weeks for an antidepressant forexample). Remember that a lot of people experience side effects before they getthe bene ts.What can you so?Take your medication at the same time each day.Don’t stop your medications without discussing it with your doctor.CBIS MANUAL | MAY 2009EDUCATION | 3240
Activation ModuleThe Activation Module has been organized so thatmaterial may be handed out to patients sequentiallyor chosen specifically to match patient’s stageof illness.We recommend giving small amounts rather thanoverwhelming patients with too much information.Activating Exercises are ideal for those patients withvegetative symptoms who need to be more active intheir recovery. It includes anti-depression activities,goal setting, problem solving, appreciation exercisesand strategies for managing energy and mood.CBIS MANUAL | MAY 2009ACTIVATION | 3341
Anti-Depression ActivitiesThe activities below are helpful in recovering from depression. To start working on yourrecovery, put a check mark whenever you do one of the activities below. Push a little,often, but not to exhaustion. As you persist, day after day, you may gradually nd yourmood brightening and your energy returning.ACTIVITY MON TUE WED THU FRI SAT SUN1 Self-care (shower, shave, teethetc.)2 Eat three meals, howeversmall (check for each)3 Sleep (# of hours)4 Exercise, however little (# ofminutes)5 Relaxation (# of minutes)6 Accomplish one small task orgoal each day7 Social contact (enough butnot too much)8 Pleasure activities/hobbies(check for each)9 Do something nice foryourself10 Do something nice forsomeone else11 Replace negative thoughtswith helpful thoughts (check# times)12 Miscellaneous (your choice)CBIS MANUAL | MAY 2009ACTIVATION | 3442
Depression’s Energy BudgetEvery day, we wake up with “resources” available for our use that day. These resourcesmight be energy, time, sense of well-being, motivation, etc. The amount of availableresources changes every day, even throughout the day.If we consistently spend beyond our resources, we will go “bankrupt.” The moredepressed or anxious we are, the fewer our resources.This means we need to gure out the actual resources we have at any particular time —not the resources we think we should have, or used to have. This helps us decide whatwe really can do each day.Living Within Your Resource “Box”TOM MARY RANDY• Extraresources• Resourcesneed for basictasks• Agitated,Resourcesneeded forbasic tasks• DepletedresourcesAs you can see Tom has so many resources that he can easily accomplish the requiredbasic tasks for the day. He has extra energy, time, and enthusiasm for other things.The next box shows that Mary only has enough resources to get through basic taskssuch as dressing, making meals, perhaps a few routine chores. If she tries to pushherself to do much more than this, she will pay a price. The next day she will feel moreexhausted and overwhelmed, and her box may be even smaller.In the last box, you can see that Randy is having a bad day and can only reasonablyexpect to do the bare minimum to get through the day.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ACTIVATION | 3543
DEPRESSION’S ENERGY BUDGET (CONTINUED)Increasing the Size of Your Resource BoxIt’s important to go slowly.1 Don’t push yourself outside your box.2 However small your box, use a bit of your daily resources to do anti-depressionactivities such as self care, exercise, relaxation, hobbies etc.3 <strong>Health</strong>y energy and motivation are released and increased when you reducenegative thoughts and replace them with more realistic, helpful thoughts.4 Repeat and persist — it is far more effective to do a very small thing 100 times thanto do a big thing once. You are trying to develop new habits, and these only comewith frequent practice.5 Congratulate yourself for every effort you make no matter how small. The brainresponds very well to this kind of appreciation and you will be rewarded with moreresources, such as hope, well-being, energy and self-con dence.CBIS MANUAL | MAY 2009ACTIVATION | 3644
Small GoalsThe concentration, fatigue and memory problems that go along with depression make itimpossible for people to keep up their same pace.Depression feeds on withdrawal and inactivity.A strategy to help people feel more in charge of their lives and improve their self-esteem isthrough the attainment of daily small goals.The emphasis on small goals is important. It slows down the person who pushes toohard so they don’t get overwhelmed and gently encourages the withdrawn person tobegin taking charge of their life.Select a Small Goal• Choose something that you would like to accomplish and are certain you canachieve in the time you set for yourself.• The task should be easy enough to achieve even if you feel very depressed.• Have a clear idea of when and how you are going to carry out your goal.i.e., “go swimming at the community center pool this Thursday evening for 15minutes,” rather than “go swimming.”If you don’t complete the goal don’t give up — choose another time or break your goalinto smaller parts.Goals that involve action and thoughts are easier to know you’ve achieved than thoseinvolving emotions.When you meet your goal, or part of it, congratulate yourself.Start small — you can always do more when you’ve achieved your goal.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009ACTIVATION | 3745
SMALL GOALS (CONTINUED)Small Goals WorksheetGOAL WHEN WHERE HOW ATTAINEDCBIS MANUAL | MAY 2009ACTIVATION | 3846
Problem SolvingDepression can make even everyday problems seem insurmountable. When worry andself doubt set in, people feel stuck. The following problem solving technique will help youchange your worry into action.LIST the specific problem that you are worrying about.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .BRAINSTORM all possible solutions and options – don’t leave any out.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CHOOSE one of the options or solutions you’ve listed.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .DO IT!. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .EVALUATE results.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .REPEAT steps 3, 4 and 5 as necessary.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .CBIS MANUAL | MAY 2009ACTIVATION | 3947
Opposite Action StrategyHere is an effective way to start fighting back against depression. Catch yourself actingor thinking the way depression wants you to — then do or think the opposite. By doingso, you DEFY depression and take back some control, even if only for a short while.ACTIONS OR THOUGHTS THATSTRENGTHEN DEPRESSIONStay in bed when you feel too miserable toget up. Don’t attend to hygiene. Don’t getdressed.Punish yourself by calling yourself namesevery time you make a mistake (“stupid,”“loser,” “useless”)Worry about all your past mistakes, howbad things are now and how things couldgo wrong in the future.Talk excessively about depressingtopics or how bad you feel to anyonewho will listen.Withdraw, i.e. don’t go out, refuseinvitations, ignore the phone.Tell yourself that everything you do mustbe done really well, if not perfectly, or it’snot worth doing at all.Take on all your usual tasks and expect todo them as well as usual.Pretend that nothing is wrong and getexhausted by the effort to keep up a goodfront.ACTIONS OR THOUGHTS THATWEAKEN DEPRESSIONMake yourself get up even for a shortwhile. Attend to hygiene and get dressedeach day.Encourage yourself to learn from themistake and try again. You will do betterin life if you focus on what you do rightinstead of what you do wrong.Set aside a small amount of time per dayto worry and distract yourself from worrythoughts at other times. Use problemsolving skills on real problems.Deliberately choose lighter topics. Focuson others. Take timeout from depression— talk or limit it to a few minutes at atime.See or talk to someone for a shorttime each day, even when you don’t feellike it.Tell yourself that you just need tomuddle through, not everything needs tobe done perfectly. Dare to be average!Remind yourself that depressionseriously limits your energy. Set realisticexpectations that take into considerationyour depressed state.Tell others that your energy is low (orwhatever you feel OK sharing) and thatthis limits what you can do. Say “No!”CBIS MANUAL | MAY 2009ACTIVATION | 4048
Chunk the DayStrategies that give people a chance to accomplish something are particularly helpfulfor depression.Sometimes you feel too depressed, unmotivated or exhausted to face the day. Here isa strategy that breaks the day into manageable chunks of time:1 Decide on the smallest amount of time you think you might be able to spend on atask. This might be a morning, an hour, even just 10 minutes. This is your “chunk” ofmanageable time.2 Decide what you will do for the chunk of time. Tell yourself: “I only have to keep goingfor this chunk. Then I can stop if I want.”3 When the chunk is over, you can decide to rest, carry on with what you were doing,or change to something else for the next chunk. You can do a whole day in chunks.Most people who try this report that they actually get more done, and as a bonus,their mood improves.FOR EXAMPLE:Let’s say Mary decides she can handle 30 minutes. In those 30 minutes she decides shecan clear off the kitchen table and do the breakfast dishes. Once she’s completed thistask she can then decide to carry on with another chunk, rest for a while, or decide to doanother chunk later in the day. The key is to choose manageable chunks and activities.Keep it small!CBIS MANUAL | MAY 2009ACTIVATION | 4149
Improve the MomentThis strategy provides you with a way to distract yourself from your negative thoughtsand depressed moods.Take time out from feeling bad by doing something to make this moment or the next fewminutes a little better.1 Keep a list of things that you are fairly sure can lift your mood for a while — pet thecat, stretch at your desk, have a shower, think about a vacation, go for a drive, playcomputer games, talk to a colleague who tells funny jokes, etc.2 Deliberately decide, and tell yourself: “I’m going to take a break from feeling so badfor a few minutes” (however long you decide). Then pick one of the items from yourlist and do it.3 When the mood or depressed thoughts try to creep back in, tell them to go away:“I’m improving this moment so go away and don’t bother me.”CBIS MANUAL | MAY 2009ACTIVATION | 4250
Appreciation Exercise“Good for Me’s”Most depressed people focus on their mistakes, what they should have done or couldbe doing, and compare themselves unjustly to others who are not depressed.This is like a marathon runner with a broken leg comparing herself to otheruninjured runners.Depression, like a broken leg, severely limits what you can do. You need to focuson small goals and genuinely congratulate yourself for making an effort, no matterhow small.• Every night, before you go to sleep, find 5 things you did that day which requireda bit of effort on your part. It can be something you committed to (make supper)or something you spontaneously chose to do (set table). Choose small every daythings, not ones that took great effort, because everyday things contribute most to afunctioning life.• Monitor your self-talk. Be supportive and encouraging, even for small achievements,as you would for a friend.• Practice, practice, practice — like all strategies this works best if you do it daily.Writing it down will show you, over time, how far you’ve come.CBIS MANUAL | MAY 2009ACTIVATION | 4351
Cognition ModuleThe Cognition Module contains a handout that explainsthe basic cognitive-behavioural concepts and severalexercises that begin to shift negative cognitions.It also contains strategies to address worry thoughts,guilt, passivity and anger.This Module has been organized so that material can behanded out to patients sequentially or chosen to matchpatients’ specific needs.As mentioned previously, we recommend givingpatients small amounts rather than overwhelmingthem with too much information.CBIS MANUAL | MAY 2009COGNITION | 4452
The Circle of DepressionCognitive-behavioural treatment strategies for depression are based on the interrelationshipbetween behaviours, thoughts, feelings and body. It is easiest to think of it interms of a circle where each is affected by and in turn affects another. This means thatbehaviours, thoughts, feelings and body all affect each other.How we behave affects what we think and feel. For example, if we make ourselves get up,shower, have breakfast and go for a walk, we’ll probably think we accomplished somethingand feel better physically and emotionally.What we think afects how we feel and behave. For example, if we think things are hopeless,we are likely to feel depressed, withdraw and have very little energy.Our feelings affect how we think and behave. If we feel depressed and have dif cultyconcentrating, we may think people will ndus boring and then we may avoidaccepting invitations.Our body responses affect howwe behave, think and feel.When we experience pain,we may stay in bed, thinkthat there is no futureand feel depressed andworthless.Changing feelingsdirectly is almostimpossible. The bestway to feel better is bychanging depressivebehaviours and thoughts.FEELINGSBODYThe Circleof DepressionBEHAVIOURSince behaviours are easyto identify it’s a good place tobegin when you want to makechanges to your thoughts andfeelings.THOUGHTSCBIS MANUAL | MAY 2009CONTINUED ON NEXT PAGECOGNITION | 4553
THE CIRCLE OF DEPRESSION (CONTINUED)For example, Jack has become depressed since losing his job. He spends most of theday in bed. In order to feel better Jack would have to change his negative behavioursor thoughts.Example 1: Changing behaviour firstBEHAVIOUR THOUGHTS FEELINGS BODYDEPRESSINGStays in bedall day.“I’m useless.”“What a loser.DepressedLow energy.HELPFULForces self toget up, have ashower, go fora walk.“At least I didsomething.”“Maybe I couldstart that smallproject.”More in control.More hopeful.More energy.We can see that when Jack changed his behaviour his thoughts and feelings also changed.Example 2: Changing thoughts firstTHOUGHTS BEHAVIOUR FEELINGS BODYDEPRESSINGWhy bother,there’s nouse, it’shopeless.”Doesn’t get up.Sleeps all day.Depressed,feels useless.FatiguedHELPFUL“I’m not sureit’s goingto make adifference,but I’m willingto at least getup and havea shower.”Gets up, hasa shower,decides to walkto the cornershop.Feels goodthat heaccomplishedhis goal. Isable to enjoythe outing.Moreenergy,alertJack was able to challenge his self-defeating thoughts with positive results. Whenhe successfully completed the goal he set for himself, he felt good about hisaccomplishment. This increased his self-esteem, which enabled him to walk to thecorner shop.• Whether the circle spirals down into depression or leads upwards towards wellness,depends on the nature of the behaviours, thoughts, and feelings you choose.CBIS MANUAL | MAY 2009COGNITION | 4654
Common Thinking ErrorsThe situations we find ourselves in don’t cause our depressed feelings — our ways ofperceiving the situations do. Here are some distorted ways of thinking that often increasedepression. Check the ones that most relate to you.FILTERINGEveryone’s life has negative aspects. If you focus only on the negative and filter out allpositive or neutral aspects, your life will indeed seem depressing.EMOTIONAL REASONING“I feel it so it must be true.” Remember feelings are not facts. Emotions are based onsubjective interpretations, not hard evidence.OVER-INCLUSIVEYou think of one problem or demand, then another and another, until you feelcompletely overwhelmed.BLACK OR WHITE THINKINGYou think only in extremes or absolutes, forgetting that most things fall into shades of grey.JUMPING TO CONCLUSIONSYou predict a negative outcome without adequate supporting evidence.MIND READINGYou believe that others are thinking and feeling negatively about you and you react as ifthis is true.PREDICTING THE FUTUREYou anticipate that things will turn out badly and you feel convinced that your predictionsare true.CATASTROPHIZINGYou blow things out of proportion and imagine the worse case scenario. This intensifiesyour fear and makes it difficult for you to cope with the actual situation.SHOULDYou make rigid rules for yourself and others about how things “should” be. When theserules are not followed you become depressed and angry.CBIS MANUAL | MAY 2009COGNITION | 4755
Thought Change <strong>Process</strong>Thoughts go unnoticed as we automatically go through our day. This often leads to thebelief that an event triggers a feeling or behaviour. In fact it is our interpretation of theevent that creates our feelings and behaviours.AWARENESSIn order to change negative thoughts they first must be noticed.• Slow down your thinking• Consciously pay attention to your negative thoughts.• Be a non-judgmental observer of your thoughts.CHANGEOnce you are aware of your negative thoughts the next step is to begin changing them.• Write down your negative thoughts• Ask yourself “Are these thoughts helpful?”• Replace them with more realistic, helpful thoughtsExample 1Adele gets criticized by her boss. She immediately thinks:“This is terrible. She thinks I’m a real loser. She’ll put this on my record and she’ll bewatching me closely. I just can’t mess up again.” She feels panicky and broods over theincident all evening.If instead, Adele slowed down her thinking and paid attention to her negative thoughtsshe would see that these thoughts are not helpful. She may then decide it would bemore helpful to apologize to her boss, carry on working, and make more effort toconcentrate. She could then set aside the incident once it was over.Example 2Sam’s son comes home late one evening. Sam feels angry and thinks — “He’s soinconsiderate! He knows I have an interview tomorrow and I need my sleep.” Sam yellsat his son and is too upset to go back to sleep.If Sam stopped to notice his thoughts he would have time to consider a more balancedperspective. “Usually he is considerate. I know he’s busy saying goodbye to friendsbefore he heads off to university. I’ll talk with him tomorrow. Right now I need my sleep.”Sam goes back to sleep.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009COGNITION | 4856
THOUGHT CHANGE PROCESS (CONTINUED)Thought Change WorksheetSITUATIONNEGATIVE THOUGHTSREALISTIC HELPFULTHOUGHTCBIS MANUAL | MAY 2009COGNITION | 4957
Self Talk (Mean Talk)Depression brings on a flood of mean talk. Depressed people blame themselves; theypick out every little flaw; they brood over mistakes, from miniscule to sizeable; they callthemselves names (Stupid! Useless!); they psych themselves into failure or giving up(“You know you can’t do this; you know you’ll blow it; you always screw up”).This kind of mean talk to yourself is guaranteed to keep you depressed and will definitelynot help you to be more productive or successful.To help in your recovery from depression, make a resolution to treat yourself the way youwould treat someone else you valued, such as a friend dealing with some problems, achild you wanted to help do better in school, or a partner who is coping with a job failure.The Talk Back Technique1 Be Aware: Listen to your own self-talk.2 Evaluate: Decide if your self-talk is helpful or harmful.3 Catch yourself: Notice your “mean talk.” (You will be surprised how often you do this).4 Stop: Immediately tell yourself (in a firm gentle voice)“STOP — THAT’S NOT HELPFUL.”5 Ask yourself: What would you say in this situation to a friend who was feeling downand needed encouragement and support?6 Support yourself: Say to yourself what you would say to a friend.7 Practice, practice, practice: The more you challenge your “mean talk” and replace itwith caring respectful talk, the more likely it is that you will improve your mood.CBIS MANUAL | MAY 2009COGNITION | 5058
Thought StoppingDepression often makes people brood and worry about current problems, things thathave gone wrong in the past and things that might go wrong in the future.When unwanted thoughts won’t get out of your head, try the suggestions in Step 1 andStep 2. See which ones work best for you. Remember: success depends on repetition.Step 1: Stop the thoughts• Picture a large STOP sign• Hear yourself shouting “STOP!”• Count backwards from 100• Recite a poem• Sing a song in your head• Gently snap an elastic band on your wrist and say “STOP”Setp 2: Keep the thoughts awayAs soon as the thoughts fade a little, do something to keep your mind and body busy.This will prevent the thoughts from coming back.• Take a brisk walk and concentrate on what you see around you• Talk to a friend, as long as you talk about something neutral or pleasant• Read a book, as long as it keeps your attention• Play a game, do a jigsaw or crossword puzzle• Do a household chore that requires concentration• Listen to a relaxation tape• Do crafts or hobby workCBIS MANUAL | MAY 2009COGNITION | 5159
Worry TimeIf worries keep nagging at you, try this:1 Pick a time near the end of the day when you will sit down (and won’t be disturbed)for about 30 minutes. You can decide on the amount of time. This is your worry time.2 When a worry comes up during the day, tell it “Go away; I’ll deal with you inworry time.”3 When the time comes up, go to your worry place, think of all your worries and donothing but worry hard for the full time you have set aside.4 At the end of this time (use an alarm clock to remind you), go to a different room ifpossible and get involved in some activity that distracts you.CBIS MANUAL | MAY 2009COGNITION | 5260
Good Guilt / Bad GuiltA world without guilt would be a frightening place. Guilt is the internal pause button thatencourages us to question our behaviors, feelings, intentions, beliefs, judgments, valuesand helps us decide whether something is “right or wrong.”Guilt can be extremely helpful in keeping us on track as we navigate throughrelationships and life.Conversely guilt can be crippling, leading to shame, self-doubt and depression. It canbe a harmful weapon when we use it against ourselves or to control and manipulateanother person.Use the following questions to help you assesswhether your feeling of guilt is helpfulor harmful.1 What happened that led to my feeling of guilt?2 What am I responsible for in this situation?3 What circumstances and/or other people may have contributed to this outcome?4 What percentage of the guilt belongs to circumstances and/or other people?5 What part of the guilt belongs to me?6 What do I do with this guilt?• Learn from my mistakes.• Commit to better actions in the future.• Make restitutions to others.• Avoid shaming myself.• Forgive myself and others.CBIS MANUAL | MAY 2009COGNITION | 5361
Assertiveness Skills– Speaking UpSay yes when you mean yes, no when you mean no, and maybe when you mean maybe— assertiveness means being clear, not necessarily sure.– David RichoAssertiveness is a powerful antidote for the disabling effects that depression can haveon our ability to communicate. It involves the direct and honest expression of yourfeelings and desires in a way that respects yourself and others.If you are experiencing depression, you may have noticed within yourself a tendency tosocially withdraw and to avoid contact with others. You also may have experienced anincrease in misunderstandings between yourself and others.Assertiveness is the ability to:• Be clear about your feelings, choices and agenda (with yourself and others)• Ask for what you want• Take responsibility for your feelings and behaviour.People are born with the capacity to communicate but not always provided with thenecessary training to communicate assertively. Life is full of challenges and no oneis consistently assertive. People also choose passive and aggressive behaviour,sometimes with disastrous results. While you may not be assertive all the time, you canlearn to be more assertive, more of the time. In this way you will reduce the conflicts,disappointments and stresses, which can contribute to triggering depression.At first you may think it’s selfish or demanding to act assertively. Remember thatbehaviour can change attitudes. So act as if your wants and needs are as worthy asthose of others. Gradually, negative inner criticisms will be silenced and your self-esteemwill improve.There are many options available to learn more about assertiveness. There is a vastarray of information available from libraries, the Internet and local bookstores. Often localcommunity centres offer assertiveness courses. As with any new skill, the key to successis practice, practice, practice.CBIS MANUAL | MAY 2009COGNITION | 5462
Setting LimitsMost of us like to be seen as helpful and generous, but for people with depression,saying “NO” can be especially difficult. Depressed people are often afraid that if they setlimits, other people will not like them or want to spend time with them. The only way toprove to yourself that this is not true is to experiment with saying “No.”WON’T PEOPLE DISLIKE ME IF I SAY “NO” TO THEM?They may be annoyed at first because they are used to you agreeing to everything theyask. Most people who learn how to say “No” find that in time they actually get a lot morerespect from others. Saying “No” is for everyone’s benefit.IF I SAY “NO” WON’T I BECOME A SELFISH PERSON?Setting limits doesn’t mean saying “no” to every request, just balancing things so thatothers don’t depend on you all the time for everything. This gives others a chance tolearn how to manage their own lives.WHAT IS THE PRICE FOR ALWAYS SAYING “YES?”You get completely overwhelmed and over time your health is likely to suffer.You have less time and energy to spend with your family and friends.You become irritable, exhausted and perhaps depressed.You feel unappreciated for what you do.You begin to resent the people for whom you do so much.You put your personal needs, plans, and dreams on hold, perhaps forever.Others expect more and more, even take you for granted.Others don’t learn to solve their own problems.Others don’t learn to become independent.Others learn to take advantage of helpful people.Others fail to become helpful themselves.HOW DO I START SETTING LIMITS WITH OTHERS?Choose a small request someone has made that you know they can managefor themselves.Decide what, when and where you will tell them.Rehearse what you will say, and practice using a strong assertive voice.Stay firm; don’t argue or become defensive.Use internal coping statements.Repeat this exercise with other small requests before moving on to moredifficult situations.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009COGNITION | 5563
SETTING LIMITS (CONTINUED)EXAMPLE1 Choose a small request. Your son Joe has asked you to baby-sit nextTuesday evening.2 Decide what, when and where. I’ll call Joe right after dinner and tell him thatI can’t baby-sit for him next Tuesday evening,and that he’ll have to find someone else.3 Rehearse. “Joe, I can’t baby-sit for you on Tuesday and Iwant to give you suf cient time to nd someoneelse.”4 Stay Firm. “As I’ve already said Joe, I can’t baby-sit foryou on Tuesday. You’ll have to make otherarrangements.”5 Use coping statements. My life is as important as anyone else’ s. It’s OK tosay “No.”WOKSHEET1 Choose a small request.2 Decide what, when and where.3 Rehearse.4 Stay Firm.5 Use coping statements.CBIS MANUAL | MAY 2009COGNITION | 5664
Is Anger a Problem for You?Tom arrives home late from the office, empty-handed. Mary expected him an hour agofor a special birthday dinner with her. Mary thinks “He’s forgotten … doesn’t care …I’m so angry,” etc.From this example, we can see that Mary believes her needs have not beenmet, she blames Tom and is about to speak or act in a way that could result in anangry exchange.Mary, like many people, believes that Tom caused her anger by coming home emptyhanded. Actually it’s Mary’s interpretation and the meaning she assigned to the situation,i.e.: bad, unfair, hurtful, etc. that created her anger.Anger is a stress response that includes thinking, bodily sensations and behaviours.Similar to an alarm system its purpose is to let us know that “something is not OK.”Many people, like Mary, respond to the alarm by feeding the anger with more negativethoughts. Usually this has unpleasant and unproductive results. Anger has enormouscosts to the individual and their relationships. Let’s look at what Mary could do that wouldfocus more on satisfying her needs and successfully resolve this con ict.• Information: Make sure she has all the information and there are nomisunderstandings.• Slow down: Take time and think about her responses rather than instinctively reacting.• Problem solve: Assess the situation with as much objectivity as possible anddetermine if there are solution options.• Breathe: Relaxation techniques such as abdominal breathing can reduce physicalreactions and allow her to think more clearly.• Communication: Using I statements, Mary could specify what she was reacting to,what her feelings are, and what she wants.• Thought stopping: If she is becoming overwhelmed by her angry thoughts, she couldsilently but loudly say STOP to herself. She might need to repeat this several times.• Humour: Try to see the humour in a situation, laughter is a great deflector of anger.• Time out: Remove herself from the situation until she’s had time to cool off.If you are concerned about your anger and want better ways to express your needsand solve problems there are many self help books available from your local library orbookstore. You can also seek out an Anger Management course.CBIS MANUAL | MAY 2009COGNITION | 5765
Relaxation ModuleThe Relaxation Module has been organized so thatmaterials can be handed out sequentially. Moreadvanced skills are built on the preceding foundation.This module includes informational handoutsand instructional exercise handouts on abdominalbreathing, grounding, relaxation, mindfulness,meditation and tension release.These exercises will assist with stress managementand provide a positive benefit to overall physical andmental health.These skills are easy to learn and more effective ifdemonstrated in your office.CBIS MANUAL | MAY 2009RELAXATION | 5866
Stress ResponseIntroduction to Relaxation• Our body has a natural, healthy mechanism for responding to perceived threats(stress), called the Fight, Flight or Freeze response.• Our body responds by releasing chemicals (e.g., adrenaline) that cause variousbody systems to change, including our central nervous system. This produces manysymptoms including increased heart rate, rapid breathing and increased agitation.• Our central nervous system has two parts:1 The Sympathetic nervous system that stimulates the Fight, Flight orFreeze response.2 The Parasympathetic nervous system that triggers the relaxation/calmingresponse.Why Relax?• You can’t be physically relaxed (parasympathetic response) and physically stressed(sympathetic response) at the same time.• Abdominal breathing and relaxation techniques trigger the parasympatheticresponse, calming your body and mind.Orientation to Relaxation Training• Relaxation is a skill that can be learned through repeated practice.• We are aiming to train the relaxation response so that it becomes almost automatic.• Initially, you may not notice any major difference in how you feel.• During a practice session, you may experience some unusual feelings in your body,such as warmth, heaviness or a tingly sensation. These sensations are signs thatyour muscles are loosening and relaxing.• Feel free to move around as much as necessary in order to maintain comfort.• It is best to have your eyes closed during a session in order to block outvisual distractions.• Home practice should be carried out once a day. Try to establish regular times forthe practice sessions. Many people find it useful to do their practice sessions atbedtime as it helps them to get to sleep easily.CBIS MANUAL | MAY 2009RELAXATION | 5967
Abdominal BreathingPurpose• Your breathing is directly related to the level of tension you carry in your body.• If you breathe shallowly, in your chest, you will become more tense and moreanxious. This kind of breathing stimulates the sympathetic branch of your nervoussystem, which is connected to the “fight, flight or freeze” response.• If you breathe deeply, in your abdomen, you will become more relaxed. This type ofbreathing stimulates the parasympathetic nervous system, which triggers a relaxingand calming response.<strong>Process</strong>TO DISCOVER HOW YOU ARE BREATHING NOW:• Put one hand on your chest and one hand on your abdomen (belly). Pay attention tohow you are breathing for a few moments. Observed which hand (if any) is moving.• If it is your top hand, you are breathing mostly in your chest — shallowly. This kind ofbreathing will increase body tension and stress/anxiety.• If it is your bottom hand, then you are breathing in your abdomen. This will help youto relax and calm down.• The idea is to learn to breathe in your abdomen more.PRACTICING BREATHING:• When practicing abdominal breathing, put both hands on your abdomen and close orlower your eyes.• First, breathe out fully. Then, as you breathe in, let your abdomen expand. You canimagine that you are gently filling up a balloon in your belly.• Then just let go and feel the balloon emptying slowly and your abdomen flattening asyou exhale.• The more fully you breathe out, the easier it is to breathe in deeply.• Practice breathing this way for 5 minutes twice a day.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009RELAXATION | 6068
Variation – Box BreathingABDOMINAL BREATHING (CONTINUED)Box Breathing incorporates brief holding of breath following inhalation and exhalation.This is very useful during severe anxiety or panic to prevent hyperventilation.INHALECount1-2-3-4HOLDCount1-2(3-4)BoxBreathingHOLDCount1-2(3-4)EXHALECount1-2-3-4CBIS MANUAL | MAY 2009RELAXATION | 6169
GroundingPurpose• Grounding is a calming and centering method that helps you to become morefocused in your body and on the present moment. It reminds you of your strengthand ability to cope in the present.<strong>Process</strong>• Sit in a chair with your feet flat on the floor and your hands placed palms downon the large muscles of your thighs. Gently press your feet into the floor for a fewmoments and release. Feel your strength.• Alternatively, you can ground while walking or standing. Just become aware of yourfeet firmly planted beneath you.• To calm the mind and help to focus in the present, take some deep breaths whilerepeating a calming statement. Choose one thought that you repeat each time youdo the grounding, so that saying it becomes a habit. For example,“I AM LEARNING TO STAY IN THE PRESENT.”“THIS IS ME. I AM HERE. I AM ALIVE. I WILL COPE.”“I AM LEARNING TO COPE.”• You could also ground by focusing on a detailed description of an object in yourenvironment (i.e., colour and shape) and breathing.CBIS MANUAL | MAY 2009RELAXATION | 6270
Body ScanPurpose• Body scan is a relaxation technique that can be used to quickly check the level oftension in your body and to release it.<strong>Process</strong>• Body scan involves scanning your body from feet to head and doing two steps foreach part:1 Focus on body area and note tension.2 Breathing deeply, imagine that your breath goes into that part of the body. As youbreathe out, the tension is released with your breath.• You can take 5 minutes or 30 seconds to do a body scan, making use of it in avariety of settings and situations.CBIS MANUAL | MAY 2009RELAXATION | 6371
PurposePassive Relaxation• Passive relaxation is a relaxation technique that involves taking time to focus yourattention on relaxing your body and mind.• It incorporates deep breathing and body scan.• It takes approximately 20 minutes.• This technique is very important in learning to truly relax your muscles and engagethe parasympathetic relaxation response.• This technique needs to be practiced regularly (ideally every day; minimum 3 timesper week).• By regularly practicing a longer technique you will, with time, increase theeffectiveness of the shorter techniques.<strong>Process</strong>• Get into a comfortable position. Close your eyes and concentrate on deep breathingfor a few minutes.• Focus your attention on each body part (feet, legs, buttocks, abdomen, back, hands,arms, shoulders, neck, jaw, eyes, scalp) and mind.• With each part, direct your breathing there. Breathe out any tension and breathe inrelaxation. Instruct each part to relax (i.e. relax feet, relax, relax).• You may wish to use relaxing music.Variations• You may incorporate visualization. While you are relaxed, imagine being in a specialplace in nature. Imagine what you see, hear, smell, taste and feel. Experience all thesensory details of your special place.• You may also make self-statements (autogenic). Repeat to yourself:“My. . . . . . . . . (name body part) is warm.”“My. . . . . . . . . .(name body part) is heavy.“My. . . . . . . . (name body part) is relaxed.For mind, substitute words peaceful, calm and relaxed.CBIS MANUAL | MAY 2009RELAXATION | 6472
Stress BustersPurpose• Shorter techniques are more flexible than the longer ones. They allow you to relaxand/or release tension quickly in a variety of different settings (e.g., at lunch break, ata meeting, while waiting in line at a store, at a red light etc.)• This flexibility means that you can use these techniques to calm yourself before,during or after stressful situations, or to short-circuit a stress response.• Different short versions will suit different situations so having a number of shortversions offers you the flexibility to choose one that fits the moment best.<strong>Process</strong>• Take a few deep breaths.• Sigh.• Laugh.• Yawn, unclench or move jaw.• Shrug your shoulders several times.• Periodically remind yourself to keep shoulders down and jaw unclenched.• Massage your temples and the upper back of your neck.• Raise your eyebrows and hold them up until the count of 3; release and repeatseveral times.• To relieve eyestrain, rub your palms briskly together, cup hands and place them overopen or closed eyes.• With open or closed lids — rotate your eyes in circles slowly, top, right side, bottom,left side; relax and reverse. Repeat 3 times.• Neck roll: Always move your neck very gently and slowly. Let your chin drop downto the center of your chest. Keeping your chin close to your body, slowly move yourhead to look over your left shoulder. Slowly return to center and repeat on theright side.• Stretch.CBIS MANUAL | MAY 2009RELAXATION | 6573
One Minute Stress BreakBODY CHECKRE-FOCUSBREATH OUTChange positionChange activitychange thoughtchange plansSlowlyLet goRelaxTired?Stiff?Tense?Sore?1 MinuteStressBreakRelax...Stressed?Anxious?Overwhelmed?Depresed?SlowlyDeeplyMOOD CHECKBREATH INHOLDCBIS MANUAL | MAY 2009RELAXATION | 6674
MindfulnessPurpose• Mindfulness is experiencing the present moment in a non-judgmental way. It ispaying attention with a welcoming and allowing attitude … noticing whatever we areexperiencing in our thoughts, behaviour, and feelings.• Making changes in our life begins with awareness. Awareness means payingattention to what we are doing, thinking and feeling. We then have the option toeither accept things or change things.• Practicing mindfulness teaches us to relax and remain alert in the midst of theproblems and joys of life. It encourages us to pause in the moment and respond tolife with curiosity and a welcoming attitude.<strong>Process</strong>• The practice of mindfulness focuses on three areas, mindfulness of bodilysensations, of feelings, and of thoughts.• A good place to begin the practice is to become aware of your breath, simply noticingits sensations in the nose, throat, lungs, or belly. Follow the breath just as it is — longor short, deep or shallow. The goal is not to change it but only to observe and to bemindful of each breath.• Mindfulness can then extend to noticing:sensations in the body, noticing pain, pleasure, heat, cold, tension, relaxation.emotions you may be experiencing such as fear, anger, sadness, happiness, etc.thoughts that arise in the mind in the form of sentences, words, fragments,or images.• The point is to fully experience and be aware of whatever may arise within you.• This type of practice can then continue as you move through your day, being moreand more aware of your reactions and responses in all of your activities.CBIS MANUAL | MAY 2009RELAXATION | 6775
Mindfulness MeditationPurpose• Mindfulness Meditation is learning to pay attention to whatever is happening in thepresent moment in your mind and body. Mindfulness = Paying attention on purpose,in the present, non-judgmentally.• To be “present” in the moment — “Here and Now” — is to be fully alive.• Since mindfulness meditation also involves breath awareness, the parasympatheticsystem is stimulated, resulting in the relaxation response.• It is a relaxation method for learning to work with the mind. It gives us a tool for gainingmore perspective on our thoughts, and more acceptance of present moment reality.• Meditation can contribute to a feeling of inner balance and peace of mind.<strong>Process</strong>THE SITTING PRACTICE OF “MINDFULNESS MEDITATION”The Position/PostureSeat – find a solid, grounded, stable position on a chair or cushion– sit out from the edge of the chair so back can be straight– feel body resting on the chair or cushion– notice the firm pressure of buttocks– let body relax in the position, not too tight and not too looseFeet – flat on floor (grounded)Hands – hands on thighs, palms down (grounded)Back – as straight as possibleChest – soft/openEars – above shouldersChin – ever so slightly in towards the chestJaw – relaxedMouth – slightly open, like “ah”Tongue – touching roof of mouth, behind teeth (less saliva)Eyes – eyes are open and gaze downward about 4’ in front, on the oor, usinga soft focus. If you close your eyes there is a tendency to space out.CBIS MANUAL | MAY 2009RELAXATION | 6876
BreathMINDFULNESS MEDITATION (CONTINUED)• Now as you sit there, start noticing your breath going in and out. Not forcing it orchanging it — just noticing it, paying attention to it. In and Out, In and Out.• Then start putting more emphasis on the out breath. Each time you breathe out,allow yourself to let go and relax.• Occasionally check your body posture, and then go back to paying attention to yourbreath.Thoughts• As you follow your breath, you will notice that thoughts will arise, and your mind willwander. That’s okay and natural.• It may be a thought, an image, or an emotion — just label it all “thinking.”• Just notice that your mind has wandered, label it “thinking” and bring your attentionback to the “In and Out” of the breath.• It is important to be very kind to yourself when you notice that your mind haswandered away. Training your mind is a little like training a puppy. It does not help tobe harsh with the puppy. What helps is to kindly tell the puppy to “stay” over and overagain. Likewise with the mind, just notice it’s wandered away, gently and kindly sayto yourself “thinking” and bring your attention back to the breath.PracticeIt is helpful to set a special time aside each day to practice sitting meditation. You canstart with 5 – 10 minutes a day, increasing to 20 minutes over time. It can also be helpfulto practice at the same time and place each day.VariationWALKING MEDITATION• Walk slowly, hands in front or by sides as you would usually walk.• Pay attention to your body; feel a sense of ease.• With each step, feel the sensations of lifting your food, moving it forward then placingit on the ground.• Notice when the mind has wandered away, label it “thinking” and just bring yourattention back to your body and to moving each foot.• You can say “lifting, swinging, placing” to yourself, to help to stay focused onyour body.CBIS MANUAL | MAY 2009RELAXATION | 6977
Lifestyle ModuleThis module contains informational handouts onvarious lifestyle factors that promote mental andphysical health including sleep, nutrition, substances,physical activity and a wellness wheel.Choose the handouts that correspond to patient needs.CBIS MANUAL | MAY 2009LIFESTYLE | 7078
<strong>Health</strong>y Habits for SleepingDepression often causes a disruption in sleep patterns. Poor sleep contributes todaytime fatigue, low energy, irritability, decreased concentration and increaseddepression. If sleep is a problem for you, practice the following tips.• Go to bed and get up at the same time everyday regardless of how poorly you slept.• If you have not fallen asleep after 20 minutes, get up and do something relaxingor boring until you feel sleepy, then try again. (Repeat if necessary throughoutthe night).• Use relaxation exercises or repetitive mental activity (i.e. counting backwards) topromote sleep.• Avoid naps.• Create a good sleep environment, preferably a cool, dark, quiet room. Earplugs,eyeshades and white noise may be helpful.• Develop a bedtime route. Try a warm bath 90 minutes before bed.• Save your bedroom for sleep, sickness and sex.• Get fresh air and exercise regularly, preferably daily, but not within a few hoursbefore bedtime.• Avoid caffeine, alcohol, and tobacco in the evening, and maybe even the afternoon.• Have a light snack (milk, bananas or peanut butter are good choices) but avoideating a large meal close to bedtime.• Avoid sleeping medication, including over the counter aids, unless prescribed byyour doctor.CBIS MANUAL | MAY 2009LIFESTYLE | 7179
DietIt’s True: You are What You Eat!• Depression frequently affects appetite, either increasing or decreasing it.• Diet (not how much, but what we eat) can affect depression.• It’s important to eat a healthy, balanced diet that is low in sugar, caffeine andjunk food.• Snacks should be nutritious.• Regular and consistent dietary habits are important.• Even if you don’t feel hungry, it’s important to eat healthy meals or snacks severaltimes a day.• If needed, decrease portion size, but make sure you eat something.Substance Use• Although using drugs and alcohol may provide temporary relief of depressivesymptoms, they tend to worsen mood.• Substance misuse contributes to avoiding rather than facing problems. Avoidingemotional problems tends to aggravate them.• Reducing substance use to moderate levels, or even stopping, is essential to healthand recovery.Caffeine• Caffeine comes in several popular forms – coffee, tea, soft drinks and chocolate.• It is a stimulant, acting on our nervous system much like anxiety does.• Caffeine is also an addictive substance.• Some of its side effects are similar to symptoms of depression: sleeplessness,digestive problems, headaches and anxiety.• Withdrawal from caffeine also mimics depression, with irritability, fatigue, appetiteproblems, and poor concentration.• It’s best to be aware of the effect of caffeine and to consider limiting its use.• Please refer to the Caffeine Chart on back to determine your caffeine intake.CONTINUED ON NEXT PAGECBIS MANUAL | MAY 2009LIFESTYLE | 7280
IT’S TRUE: YOU ARE WHAT YOU EAT! (CONTINUED)Caffeine ChartCAFFEINE CONTENT OF COFFEE, TEA, AND COCOA(MILLIGRAMS PER 6 OZ. CUP)Coffee, instant . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .60 – 70 mgCoffee, percolated . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90 – 110 mgCoffee, drip . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .120 – 150 mgCoffee, decaffeinated . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 – 10 mgTea bag, 5 minute brew . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .50 – 60 mgTea bag, 1 minute brew . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .30 – 40 mgCocoa . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10 – 20 mgChocolate (dry, 1 oz.) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5 – 10 mgCAFFEINE CONTENT OF COLA BEVERAGES (PER 12 OZ. CAN)Coca-Cola . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .65 mgPepsi-Cola. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .43 mgDr. Pepper . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .61 mgMountain Dew . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .50 mgCBIS MANUAL | MAY 2009 LIFESTYLE | 7381
Physical ActivityExercise• Regular physical activity helps the treatment of depression by brightening mood,increasing energy, and improving sleep.• Exercise helps increase stamina and reduces the risk of diseases like diabetes, heartdiseases, and osteoporosis.• Exercise can raise the levels of certain chemicals in the brain, including serotonin,which produces happier states of mind, thus helping in the recovery of depression.• When you are depressed, it is good to know that you are taking positive action foryour health.• A realistic, flexible and fun program has the best chance for success.• No one form of exercise has been shown to be superior for depression. What isimportant is to choose a physical activity that you enjoy — and to do it regularly.• You do not need to push yourself to extremes. In fact, moderate and consistentexercise may improve mood more than excessively long, hard workouts.• Your goal should be to feel pleasantly tired, a normal feeling after anyphysical activity.• The key is to start slowly and be patient with yourself. Just a few minutes of walking(or other exercise) is a good place to start.CBIS MANUAL | MAY 2009LIFESTYLE | 7482
The Wellness WheelPHYSICALGROWTHSELF WORTHCreativityGoalsSelfDevelopmentConfidenceIndependenceSuccessCongratulateyourselfNutritionExerciseSleepRelaxationOutdoorsA<strong>Health</strong>yLifeNew activity,situations andrelationshipsShelterIncomeReduced threatof externaldangerNeed to loveNeed to be lovedNeed to belongCommunitySAFETYSpiritualityConnect with natureBELONGINGCHALLENGECBIS MANUAL | MAY 2009LIFESTYLE | 7583
GAD 70 - 45 – 9Mild10 – 14Moderate15 – 21SevereConsiderCauseMedicalPsychologicalOtherPsychologicalAnxietyDisorderPTSDPhobiaPanicDisorderSocialAnxietyOCDGeneralAnxietyGAD Self-AssessmentQuiz
CBISCognitive Behavioural Interpersonal Skills.............................Anxiety Addendum
Table of ContentsFLOW CHARTS..................................................................................................76EDUCATION MODULE ......................................................................................79The Many Faces of Anxiety.............................................................................80Notes to Practitioner........................................................................................81Medical Considerations ...................................................................................82Understanding Generalized Anxiety Frequently Asked Questions ..................83Anxiety “System-Wide Explosion” ...................................................................84Considering Medication for Anxiety Disorders?...............................................85Resources for Self-Help ..................................................................................86COGNITIVE BEHAVIORAL MODULE................................................................87GAD: Self-Assessment Questionnaire ............................................................88GAD: Self-Assessment Profile.........................................................................89Costs and Benefits of Anxiety..........................................................................91How Anxiety Works .........................................................................................92Panic Circle .....................................................................................................94Taking Control of Panic ...................................................................................95Your Emotional Thermometer .........................................................................96Keeping Anxiety in Check ...............................................................................97Anxiety Equation .............................................................................................98Predicting Disaster ..........................................................................................99Anxiety Lies...................................................................................................101Coping Cards ................................................................................................102Coping Plans.................................................................................................103Problem Solving ............................................................................................104Taking Risks..................................................................................................105Assertive Behaviour 101 ...............................................................................107D.E.S.C. Script ..............................................................................................108Patient Empowerment Anxiety Manual VIHA March.2010 i
FLOW CHARTS………………………………………..This module contains flow charts that direct youto the appropriate CBT strategies in this manual.When in doubt – go with the flow.Patient Empowerment Anxiety Manual VIHA March.2010 76
Self-Management &CBT StrategiesGENERALIZEDANXIETY DISORDER• Self-Assessment Questionnaire, pg 88• Self-Assessment Profiles, pg 89• Understanding Generalized Anxiety, pg 83• Anxiety “System-Wide Explosion”, pg 84• Abdominal Breathing, pg 60• Passive Relaxation, pg 64• Mindfulness, pg 67• Costs and Benefits of Anxiety, pg 91• How Anxiety Works, pg 92• Common Thinking Errors, pg 47• Your Emotional Thermometer, pg 96• Thought Stopping, pg 51• Worry Time, pg 52• Anxiety Equation, pg 98• Predicting Disaster, pg 99• Anxiety Lies, pg 101• Coping Cards , pg 102• Coping Plans, pg 103• Problem Solving, pg 105• Taking Risks, pg 106• Self Talk/Mean Talk, pg 50• Good Guilt/Bad Guilt, pg 53• Setting Limits, pg 55• Is Anger A Problem For You?, pg 57SOCIALANXIETY DISORDER• Anxiety “System-Wide Explosion”, pg 84• Abdominal Breathing, pg 60• Grounding, pg 62• Body Scan, pg 63• Costs and Benefits of Anxiety, pg 91• How Anxiety Works, pg 92• Anxiety Equation, pg 98• Taking Risks, pg 105• Self Talk/Mean Talk, pg 50• Assertive Skills, pg 54• Assertive Behavior, pg 107• Setting Limits, pg 55Patient Empowerment Anxiety Manual VIHA.March.2010 77
PANIC DISORDER• Anxiety “System-Wide Explosion”, pg 84• Abdominal Breathing, pg 60• Grounding, pg 62• How Anxiety Works, pg 92• Panic Circle, pg 94• Taking Control of Panic, pg 95• Anxiety Equation, pg 98• Predicting Disaster, pg 99• Coping Cards, pg 103• Taking Risks, pg 105PHOBIA• Anxiety “System-Wide Explosion”, pg 84• Abdominal Breathing, pg 60• Grounding, pg 62• Body Scan, pg 63• Taking Control of Panic, pg 95• Anxiety Equation, pg 98• Coping Cards, pg 102• Taking Risks, pg 105PTSD• Anxiety “System-Wide Explosion”, pg 84• Abdominal Breathing, pg 60• Grounding, pg 62• How Anxiety Works, pg 92• Panic Circle, pg 94• Taking Control of Panic, pg 95• Coping Cards, pg 102• Taking Risks, pg 105OCD• Anxiety “System-Wide Explosion”, pg 84• Stress Busters, pg 65• Meditation, pg 68• One Minute Stress Break, pg 66• Costs and Benefits of Anxiety, pg 91• How Anxiety Works, pg 92• Common Thinking Errors, pg 47• Keeping Anxiety in Check, pg 97• Thought Stopping, pg 48• Anxiety Equation, pg 98• Coping Cards, pg 102• Problem Solving, pg 104• Taking Risks, pg 105Patient Empowerment Anxiety Manual VIHA.March.2010 78
EDUCATION MODULE………………………………………..The education module contains handoutsproviding basic information on anxiety forpractitioners, patients and their familiesIt includes a handout for patients who may beconsidering medication as well as a list ofwebsites and self-help materialsChoose the handouts that correspond to patientneedsPatient Empowerment Anxiety Manual VIHA March.2010 79
The Many Faces of AnxietyPanic Disorder with or without agoraphobia• Recurrent unexpected panic attacks without an obvious trigger• Avoidance of situations where panic attacks have occurred(agoraphobia)Example: A person may have bouts of intense fear and avoid leavingthe house aloneSocial Anxiety Disorder• Excessive or unrealistic fear of social situations or performance• Intolerance of embarrassment or scrutiny by othersExample: A person is so shy that they cannot speak in a groupObsessive Compulsive Disorder• Presence of obsessions (intrusive thoughts, images, or urges thatcause anxiety)• Presence of compulsions (repetitive behaviours or mental acts that areperformed to reduce anxiety)Example: A person washes their hands repetitively until they are rawbecause they are afraid of germsSpecific Phobia• Unreasonable fear of a specific object or situation usually associatedwith avoidanceExample: A person is so afraid of flying that they cannot travel by planeGeneralized Anxiety Disorder• Uncontrollable and excessive worry occurring most days about ordinaryactivities• Intolerance of uncertaintyExample: A person worries a lot about harm coming to their familymembers on a routine trip to townPost Traumatic Stress Disorder• Occurs after a traumatic event to which the patient responds withintense fear, helplessness, or horror• Patients relive the event in memories or dreams; avoid reminders of theevent and experience symptoms of increased vigilanceExample: A person returns from war and relives the battlefield traumasin his nightmares and startles at the sound of loud noisesPatient Empowerment Anxiety Manual VIHA.March.2010 80
Notes to PractitionerDon’t rush to treat anxiety after upsetting events.• Although difficult to tolerate, in most cases anxiety will resolve with time.Early treatment may interfere with the natural ability to process theanxiety.Keep the patient at work or in their usual role as much as possible.• “Taking a break” is usually not a good idea as it can reinforce avoidance.All anxiety cannot be eliminated.• Patients will need to be convinced anxiety is an essential part of theirsurvival system. A little anxiety is not harmful and can indeed be helpful.Avoidance provides immediate relief from anxiety.• Avoidance however reinforces the anxiety. It can be difficult to convincepatients to give up avoidance in favor of new strategies that may initiallyincrease anxiety.Attempting new behaviors will increase anxiety at first.• The most difficult aspect of self-management for anxiety is that relief willnot come until the patient has done the cognitive work and also practicednew skills.Anxiety is rewarded in our society.• Anxious people gain self-esteem through praise for being conscientious,careful, compliant and protective of others as well as for not causingtrouble.Patients with anxiety are generally less motivated for change.• Unlike depressed patients, anxious patients will be reluctant to engage instrategies that may initially increase anxiety until their anxiety becomessevere and interferes with functioning.Patient Empowerment Anxiety Manual VIHA.March.2010 81
Medical ConsiderationsMost Common Medical Conditions That Mimic Anxiety• Endocrine: Thyroid, menopause, adrenal disorders• Cardiovascular: Congestive heart failure, mitral valve prolapse, angina,pulmonary embolus• Respiratory: Asthma, COPD• Metabolic: Diabetes, hypoglycemia• CNS: Migraines, temporal lobe epilepsy, vestibular dysfunction• Hematologic: Vitamin B12 deficiency, anemia• Drugs: Caffeine, nicotine, alcohol, discontinuation syndromes, stimulants,some prescription meds like asthma medicationBaseline Lab Investigations• CBC• Fasting glucose• Electrolytes, calcium, magnesium• Liver enzymes• Urinalysis, urine toxicology for substance abuse• TSH• ECG if indicated• Pregnancy test if indicatedPatient Empowerment Anxiety Manual VIHA.March.2010 82
Understanding Generalized AnxietyFrequently Asked QuestionsWho gets anxious?Everyone! Anxiety is part of the natural way that the mind and body are motivated to prepare and plan fora possible threatening situation or event.What’s the difference between anxiety and fear?Fear is a strong emotion that we feel when faced with immediate danger or threat, such as a fire. Fearmakes us “fight, freeze or flee” depending on which is the best way to cope with the threat. Fear is a selfdefensereaction that can save our lives. Anxiety is a more general nagging kind of fear about somethinggoing wrong in a situation that hasn’t happened yet, and may not even happen. Anxiety wonders “Whatif?” Anxiety is not about what will definitely, immediately happen, only about what might or could happen.When is anxiety a problem?A little bit of anxiety, occasionally, is not a problem at all. In fact, being a bit anxious before an exam or arace or a job interview has been shown to actually improve performance. Anxiety is only a problem whenit becomes excessive. Anxiety can be so debilitating that people are unable to write anything at all inexams; they become sick with worry; they even avoid places or activities that are unlikely to be harmful;they make more mistakes at work because they are too tense. Too much anxiety over things that couldhappen, but have not happened and may never happen, can interfere with a person’s ability to function athome or at work.Why do some people get overanxious?Some people are born with a more sensitive emotional system so they tend to become anxious insituations that might not bother other people. If a child with this inborn tendency is constantly told howdangerous the world is, that child will most likely feel more anxious. Traumatic experiences also maycontribute to increasing anxiety. Some people get overanxious because of the way they cope with theiranxiety. They try to avoid anxiety or they try to get rid of it, and it just gets stronger.What is the treatment?This kind of anxiety, when a person worries about a lot of different things to the point that their life isdisrupted or their health affected, is called Generalized Anxiety Disorder. Cognitive BehaviouralTherapy, which focuses on the inter-relationship between thoughts, feelings and behavior, has beenshown to be very successful in treating anxiety. This type of therapy will not help you get rid of all youranxiety because you need some for everyday life, but it will help you learn to manage and reduce youranxiety. You and your doctor may decide that medications may also be helpful.What can I do?At home, in your daily life, practice all the exercises that you have been given. Research shows that thepeople who have the most success with anxiety treatment are those who practice the most. Practicemeans doing things against the anxiety: taking very small risks; not avoiding places or activities; tryingnew things. When you initially go against your anxiety, you will feel a little more anxious. As you continueyou’ll discover that most of the time what you were anxious about did not come true. Your anxiety willstart to weaken until you feel little or no anxiety in situations that previously scared or worried you.Preparation by practicing coping skills is a potent antidote to disabling anxiety that is often highest whenanticipating fearful situations.Patient Empowerment Anxiety Manual VIHA.March.2010 83
Anxiety“System-Wide Explosion”Anxiety has a significant impact on people, physically, cognitively, emotionally andfunctionally.The following is a list of symptoms that people with anxiety may experience.To understand the extent of anxiety’s impact, circle the symptoms that apply to you.Body Feelings Mind BehaviourTense musclesAnxiousEasily distractedAvoidingNumbness, tinglingNervousPoor memoryAgitated, restlessFeeling hot or chilledFearfulCan’t think clearlyMulti-taskingFlushed faceWorriedCan’t make decisionsCan’t start thingsLump in throatFrightenedConfusionCan’t finish thingsTrembling, shakingTerrifiedRacing thoughtsSnap at peopleWeakness, unsteadyPressured“Spaced out”Frantically busyDizzy, lightheadedOverwhelmedObsessive thinkingSocial withdrawalSweatingFranticWorryingCry at least thingHeart poundingPanickedSelf-criticalHypervigilenceChest painGuiltyNegative thinkingOversleepingInsomniaShySuicidal thoughtsUnable to be aloneWeight lossUncertainFrightening imagesSeeking reassuranceNauseaSelf consciousNightmaresCompulsive behaviorsDiarrheaEmbarrassedSelf medicatingShortness of breathIrritableAddictionsDry mouthAngryPatient Empowerment Anxiety Manual VIHA.March.2010 84
Considering Medication forAnxiety Disorders?For some people, medication is an important part of their anxiety disorder treatment. Sometimes,medications that were originally developed for other conditions can be very effective in treatinganxiety. Anti-depressants, anti-seizure medications, and even anti-psychotic medications can bevery useful treatments for anxiety.How you take your anti-anxiety medication is very important.• Sometimes when you first start a medication it can actually make you feel worse temporarily.Some anti-depressants can cause an initial rise in anxiety, which will go down overtime. Thisis especially true if you start at a dose that is too high or try to increase the dose too quickly.• “Start at low doses and go slow” is the best motto when treating anxiety.• The full benefits of a medication can take up to 8-12 weeks to be fully effective.• Generally, side effects go down and benefits increase over time. It is usually better to bepatient when trying a medication rather than quickly switching to a new one if there is noimmediate improvement.• Ask questions about your medication if you are not sure what to expect.Don’t stop your medication without discussing it with your doctor.• While most anti-anxiety medications are not addictive, it is not safe to stop them “cold turkey.”• If you quickly stop the anti-anxiety medications that are in the benzodiazepine group (Ativan,Clonazepam etc) you can have increased anxiety, insomnia and infrequently, seizures.• If you quickly stop anti-depressant medications you can get uncomfortable symptoms likeelectric shock sensations, dizziness and increased anxiety.• If you decide to stop your medication, it is usually best to taper off it slowly over at least fourweeks and use other coping strategies such as relaxation and try to avoid stimulants likecaffeine.What if my doctor recommends a benzodiazepine?• There are a group of medications called benzodiazepines that can usually be identified byhaving “pam” at the last part of their generic name.• Some common ones are Lorazepam (Ativan) and Clonazepam (Rivotril).• These are effective medications for treating anxiety disorders especially for short-termdistress. Their use does require careful planning as they can cause sedation, cognitiveimpairment and it is possible to become dependent on them.• Usually the use of these medications is limited to short-term use and regular rather than “asneeded”dosing.• If you start finding that these medications are no longer effective or you need higher doses toget the same effect, it is time to talk about other options with your doctor.Patient Empowerment Anxiety Manual VIHA.March.2010 85
Resources for Self-HelpOnline Resources:Anxiety Disorders Association of Canada (ADAC) www.anxietycanada.caAnxiety Disorders of America (ADAA) www.adaa.orgAnxiety Disorders Association of BC (ADABC) www.anxietybc.comBC Partners “Anxiety Disorders Toolkit” www.heretohelp.bc.caFreedom from Fear (FFF) www.freadomfromfear.comCanadian Mental <strong>Health</strong> Association (CMHA) www.cmha.caCMHA BC Division www.cmha.bc.caNational Institute of Mental <strong>Health</strong> www.nimh.nih.gov/publicat/anxiety.cfmClinical Research Unit for Anxiety and Depression (CRUFAD) www.crufad.comThe Anxiety Panic Internet resource (tAPir) www.algy.com/anxietyChangeways Programs www.changeways.comBooks:The Anxiety and Phobia Workbook by Edmund Bourne (1995)The Assertiveness Workbook: How to express your ideas and stand up for yourself at workand in relationships by Randy Paterson (2000)Don’t Panic: Taking Control of Anxiety Attacks by Reid Wilson (1996)Mind Over Mood: Change How You Feel by Changing the Way You Think by DennisGreenberger & Christine Padesky (1995)When Perfect Isn’t Good Enough: Strategies for Coping with Perfectionism by Martin Anthony& Richard Swinson (1998)Patient Empowerment Anxiety Manual VIHA.March.2010 86
COGNITIVE BEHAVIORAL MODULE……………………………………………………………..The cognitive-behavioral module contains a selfassessmentquestionnaire for GAD that matchesthe section with the highest scores to thecorresponding profiles of worrier, avoider or harddriverIt also contains handouts that explain basic CBTconcepts and exercises to shift anxiety drivenbehaviors and cognitionsThis module has been organized so that materialscan be handed out sequentially or chosen to matchpatients’ specific needsPatient Empowerment Anxiety Manual VIHA.March.2010 87
GAD: Self-Assessment QuestionnaireName: __________________________________________ Date: ________________________Please rate how well each of the statements below describes your usual way of interacting withthe world.0 = never or rarely true for me; 1 = somewhat true; 2 = quite a bit true; 3 = very true of me.1. ____I spend a lot of time thinking about what might go wrong for the people I care about.2. ____I am always reminding my family and friends to be careful in what they do.3. ____There seem to be so many dreadful things happening in society these days.4. ____People say I worry too much, but they don’t understand what could go wrong.5. ____I always plan very carefully for events and try to think of everything that could go wrong.6. ____Even after an event has turned out OK, I still think about what could have gone wrong.7. ____I feel better going out if I have someone with me who could help me if I get anxious.8. ____I can’t understand people who say: “Don’t worry; it will all work out.”9. ____I will do everything to protect my family from even the slightest harm.10. ___It’s hard to feel safe anywhere.11. ___I prefer to go to places that are familiar to me and feel safe.12. ___I don’t seem to go out to as many places and events as I used to.13. ___I have high standards for myself and expect to do my best at everything.14. ___I am often overwhelmed by all the things I have to do.15. ___I can’t focus on one thing at a time and therefore nothing much gets done.16. ___I always push myself very hard to do my best at everything.17. ___Sometimes I am so worried about doing things right that I can’t even get started.18. ___People think I am reliable, conscientious and always willing to take on extra tasks.19. ___I get really mad at myself if I make mistakes.20. ___I am afraid that I would be rejected if I did not do excellent work.Patient Empowerment Anxiety Manual VIHA.March.2010 88
Worrier: High scores on questions 1-9GAD: Self-Assessment ProfileMain Fears Main Thoughts Coping Behaviours• Something bad willhappen to self or lovedones• General fear of loomingcatastrophes e.g. floods,disease, etc.• Belief that whateverhappens will beunbearable and toooverwhelming to cope withSuggested Strategies• The world is full ofdanger• Something terrible isgoing to happen• I won’t be able tocope• I won’t be able tostand it• Worry endlessly• Talk to others about worry topics• Seek sympathy for worry• Fail to engage in effective planning• Over plan for every contingency• Nag and remind people aboutbeing careful• Rehash event afterwards, withfocus on what might havehappened• Take a relaxing bubble bath• Listen to soothing music• Do a craft or puzzle• Spend a few minutes appreciating nature• Watch a funny movie• Read a captivating book• Spend time in the garden• Light a fragrant candle• Bake cookies• Pet your dog or cat• Enjoy a massageStay Safe Avoider: High scores on questions 10-12Main Fears Main Thoughts Coping BehavioursAll of above plus• Being left alone tocope with disasterAll of above plus• I need to be protected• I am not strongenough on my ownAll of above plus• Restrict activities to “safe” zone• Avoid going out or being left alone• Keep mental list of dangerous placesand times to avoid e.g. night, crowdsSuggested StrategiesAll of above plus• Take small risks• Call or visit a friend• Get out of the house• Take action, start smallPatient Empowerment Anxiety Manual VIHA.March.2010 89
GAD: Self-Assessment ProfileHard Driver: High scores on questions 13-20Main Fear Main Thoughts Coping Behaviours• Making mistakes• Failing• Not meeting ownand others’standards orexpectations• Rejection• Disappointing selfor others• I have to be perfect butthat’s impossible• I have to keep going• No one knows the real meand how weak I am• If I fail or make a mistakesomething terrible willhappen• I won’t be able to cope• I won’t be able to stand it• Cram schedule too full• Overextending and not setting limits• Set standards and goals too high• Procrastinate• Use self-talk to push self and at thesame time predict failure• Multitask to the point of inefficiency• Assume 100% responsibility forfailureSuggested Strategies• Leave a project undone• Make a mistake on purpose• Schedule down time• Take a mini vacation• Stay in your PJs for a day• Drop your towels on the floor after you usethem• Let your answering machine get yourcalls• Take spontaneous stress breaks• Set limits with family and friends• Do one thing at a time• Focus on the moment• Dare to be averagePatient Empowerment Anxiety Manual VIHA.March.2010 90
Costs and Benefits of AnxietyCheck below to see what benefits anxiety has brought you and what it has cost you.BENEFITSYou are anxious about doing a good enoughjob so you work harder than others.Your employer lets you know how much youare valued, which makes you feel good.You are anxious that people won’t like you soyou do everything you can to please them.People talk about how kind, helpful andgenerous you are.You are afraid that things will go wrong so youalways plan very carefully.You are very vigilant and often catch thingswhen they start to go wrong so that you canhead off bigger problems.You are afraid to make mistakes so you do athorough job of any tasks you take on.People know they can rely on you to doeverything well.You are afraid that if your life gets out of controlthere will be total chaos so you are veryorganized and orderly.People perceive your orderliness as a valuabletrait at work or at home.COSTSWhen you are not at work you still think about work,worrying if you did things correctly.You may take work home.Your stress affects your family because you are toobusy and irritable to spend time with them.People get used to you being helpful and start to takeadvantage of you.People stop appreciating your efforts so you have totry harder to please them.No one seems to think your needs are importantand you feel resentful.You over plan everything and get stressed if the leastlittle thing goes wrong.Your over planning takes fun and spontaneity out ofevents.You are constantly on guard and can’t relax.You are so afraid of a mistake that you do things overand over, which takes an excessive amount of timeand makes you less productive.You procrastinate because you don’t think you can dothe task perfectly.You spend so much time organizing and trying tokeep things under control that you feel constantlystressed and overwhelmed.You are tough to live with because you requireeveryone else to be as organized as you.• The goal is to balance the benefits and costs so that you keep some of the benefits and don’tpay such a heavy price. This is hard to do because anxiety tries to push you to do more: morechecking, more planning, more working, more organizing, more worrying, and more avoiding.• What are the benefits of limiting anxiety? Feeling more relaxed and comfortable; being able toplay and have fun; other people being more comfortable around you; getting some of your ownneeds met; being appreciated even if you are not perfect; feeling better about yourself; sleepingbetter…and so on.• Your first task in limiting anxiety is to recognize what it costs you and others in your life. As youbegin to apply anxiety management strategies, you will often be tempted to go back to your oldanxious habits because your anxiety may increase temporarily. It will be helpful to come backto this page to re-affirm for yourself that you are already paying too much because of youranxiety. It is worth your effort to limit anxiety and not let it run (and ruin) your life.Patient Empowerment Anxiety Manual VIHA.March.2010 91
How Anxiety WorksTHOUGHTSBODYFEELINGSBEHAVIOURSManaging anxiety is easier if you understand how thoughts, feelings, behaviours and bodysensations are linked together and affect each other.In the following example, the same situation seems to produce very different reactions.The way you think about or interpret the situation will influence how you feel and behave.ANXIETY REACTIONSituation: Husband is late coming home.Thoughts: Maybe he’s had an accident.I know something terrible has happened.I can’t stand it if he’s hurt; how will wemanage without his salary?Feelings: Worried, anxiousBody: Heart racing, sweating, light headedBehaviours: Phones hospitals, frets andpaces, yells at kids, forgets to make dinner.HELPFUL REACTIONSituation: Husband is late coming home.Thoughts: Maybe he’s working a bit late.I’ll give him an hour and then call the office;I’m not going to panic until I know for suresomething bad has happened.Feelings: Mild concernBody: Butterflies in stomachBehaviour: Distracts herself by getting onwith usual tasks.Neither woman knows the truth of what has happened. If nothing has happened, the firstwoman is likely to be cranky and angry when her husband finally gets home. The secondwoman will want an explanation but will probably be quite calm.If something bad has happened, the first women will be overwhelmed as she is alreadypanicky, the second woman will handle it better because she is not as panicked from thestart.In this example different thoughts produced different feelings and behaviors.Patient Empowerment Anxiety Manual VIHA.March.2010 92
In this next example the same situation and similar feelings are dealt with in different ways,producing different outcomes.ANXIETY REACTIONSituation: Man wants to ask boss for araiseThoughts: What if he yells at me, tellsme I’m not good enough for a raise?What if he fires me?Feelings: Anxious, nervous, and scaredBody: Trembling, flushed, diarrheaBehaviours: Hesitates outside door andthen goes back to own office.HELPFUL REACTIONSituation: Man wants to ask boss for araiseThoughts: I don’t care what he says.I know he’s a yeller, but I have a right toask. He won’t fire me, not when otherson the job are much worse.Feelings: Anxious and nervous butdeterminedBody: Little shakyBehaviours: Goes in and presents thebest argument he can.The first man lets his anxiety control his behaviour and avoids an anxious situation. He feelsrelieved but engages in negative self-talk and calls himself a coward. The next time he wantsto ask for a raise, he will remember this incident and his anxiety will be even stronger.Avoidance feels good at the time, but makes anxiety worse and reflects badly on self-esteem.If he keeps giving in, over time, his anxiety will continue to grow.The second man fights his anxious feelings and follows through despite his anxiety. Hecongratulates himself on his effort and the next time he faces a difficult situation it’ll be easierfor him to act in spite of the anxiety. By taking risks and not avoiding anxious situations hisanxiety lessens over time.In this example, different behaviour (going against anxiety) produced differentthoughts and feelings.Patient Empowerment Anxiety Manual VIHA.March.2010 93
Panic CircleEvent (public speaking) Physical reactionsbecome PANICCatastrophizingthoughtsI’m having aheart attack.I’m going to die.Emotional reactionsintensifyfear, terror, shockThoughts (interpretation) of danger.I’ll be a disaster. Everyone willthink I’m stupid.Physical reactionsshortness of breath,increased heart rate,butterflies in stomachEmotional responsenervousness, dreadNegative thoughtsI can’t do this.Physical reactions intensifysweating, dizziness, chest painsAnxious people are often hypervigilent about normal body sensations. This excessive focus onbodily sensations creates a negative internal feedback loop that leads to further anxiety andincreases the likelihood of panic.Panic attacks certainly “feel” dangerous, however, our bodies are designed to deal with theincreased adrenaline and eventually the symptoms will dissipate as the liver absorbs theadrenaline.Patient Empowerment Anxiety Manual VIHA.March.2010 94
Taking Control of PanicAnxiety symptoms peak quickly and begin to dissipate in approximately 10 minutes, unlessfurther fueled by negative catastrophic thinking. Therefore your initial response to theonset of panic is extremely important.It is essential that you initiate coping skills at the first hint of increasing anxiety.Coping skills become less effective as the level of anxiety increases and usually are nothelpful at the height of panic.Intensity1098765432100 Mins 10 MinsTimeSteps for taking control of panic• Distract yourself during the initial stages• Initiate deep, slow breathing• Use coping statements• Observe the anxiety – don’t fuel it• Remember anxiety will pass• Repeat all these steps as neededPatient Empowerment Anxiety Manual VIHA.March.2010 95
Your Emotional Thermometer• Imagine a thermometer marked from 0-10. The highest number 10, represents the mostanxious you have ever felt, 0 is the calmest, and 5 represents midway. This is your anxietythermometer.• The numbers 8,9,10 represent an anxiety level that is only appropriate for the most severeproblems and situations. These would be situations that realistically involve a disaster thatis about to happen or has already happened, such as serious accidents, fires, and illness.Events that warrant 8-10 are quite rare in most people’s lives.• The numbers 5, 6, 7, are appropriate for moderately serious events that may havesignificant consequences, such as missing a job interview or your car breaking down on thehighway at night. Even events that warrant 5-7 on the anxiety thermometer are still fairlyunusual.• Most of the things we get anxious about on a daily basis are not serious enough to beworth high levels of anxiety. Realistically, everyday events would be somewhere between1 and 4 on the thermometer. They may feel more intense to anxious people because theytend to react on a much higher level, even to minor events.• Level 8-10 situations can be thought of as crisis and level 1-7 as different sized hassles.• The next time you feel your anxiety rising, stop and ask yourself these two questions tohelp you calm down by putting the event in a realistic context:1. How serious is this, really, in terms of life and death?2. How much anxiety is it really worth?”109 Crisis876 Serious543 Minor21Patient Empowerment Anxiety Manual VIHA.March.2010 96
Keeping Anxiety in CheckYou may temporarily feel increased anxiety when you first try a new strategy. If you stayin the anxious situation until your anxiety begins to drop a little, your anxious brain learnsthat the danger it was warning you about wasn’t really that harmful.SignalsThe following strategies will help keep your anxiety in check.Choose signals to help you stop one activity, such as work, and start another one, such asfamily time. For example, on the way home from work, make a rule for yourself that onceyou pass a certain spot you are not allowed to think about work or do anything connectedwith work. Refocus your thoughts on home and family and if possible plan somethingpleasant for part of the evening. This strategy stops one part of the day “leaking” intoanother and spoiling it.Do it onceIf you have the habit of re-doing tasks in case they are not quite right or good enough,make a rule that you are allowed to check or re-do only once. You need to be strict withyourself about moving on to a different activity and not letting yourself go back and fix orre-do the task repeatedly.GradingAnxious people often have difficulty accepting that not everything needs to be doneperfectly. In house keeping for example, it is important to clean the kitchen and bathroomthoroughly because of germs. The same does not apply to making the beds. A helpfulstrategy is to give your daily tasks a realistic grade in terms of actual importance. Tasksgraded “A” need to be done carefully and thoroughly. “B” tasks need to be done well, butdon’t need quite as much care and attention. “C” tasks can be skimmed over. If you havedifficulty not labeling all tasks “A”, get assistance grading from a family member or friend.Dare to be averageAnxious people often believe that they have to be better than average or they will bejudged as inadequate and not liked. If it were true that only above average people wereacceptable this would mean more than half the human race is unacceptable. If you dareto let yourself be average (even below average!) in one or two areas of your life, you maybe pleasantly surprised how relaxing this is and how forgiving and helpful others can be.Your average-ness is a gift, allowing others the chance to shine and/or the chance toaccept their averageness.Patient Empowerment Anxiety Manual VIHA.March.2010 97
Anxiety EquationAnxiety arises out of exaggerating danger and underestimating coping ability.Magnifying fears + + +________________________Leads to increased anxietyMinimizing Coping – – –How can you reverse this equation to minimize fear and maximize coping? What part ofthis equation do you need to work on first?1) Top: Minimize fear by making estimation of danger more realistic.a) Ask yourself: What’s fact? What’s exaggerated? Can you challenge it? Can youmake it more realistic?b) What are you saying to yourself that magnifies the fear (could be an image)?c) What could you say to yourself to decrease the fear?2) Bottom: Maximize coping by increasing coping resources.a) Identify your internal and external coping resources, past and present.b) Remind yourself that you have coped with other difficult situations.c) Use coping statements, problem solving, distracting, thought stopping,relaxation, assertiveness etc.Remember coping means muddling through somehowPatient Empowerment Anxiety Manual VIHA.March.2010 98
Predicting DisasterThere are two main thoughts that fuel anxiety:1. Something terrible is going to happenAs long as you believe this, you are likely to feel anxious, panicky, scared, worried andeven helpless.In order to manage anxiety it is important to take a look at this “disaster thought” anddecide for yourself how true it is. You can do this by asking yourself the following:“If 100% is definite and certain, how absolutely sure am I, inthis situation, that what I fear is definitely going to happen?”In order to give an answer anywhere close to 100%, you need hard evidence, solidcourtroom evidence, which proves for a fact that your fear will come true.Think of all the other times in the past that you have worried and predicted disaster. Wereyou always right? Most people are not very good at predicting the future!How often does this kind of disaster happen? Research will show you how infrequentlyreally bad things happen to even the unluckiest of people.Now, mark on this line, realistically, how probable, or certain is it that what you fear willhappen?Very unlikely ________________________________________ Very likelyIf you decide that your fear is not very likely to come true, ask yourself the following:“How much time and energy do I want to spend on worryingabout something that is not certain and may not happen atall?”If you have good evidence to believe that what you fear is very likely to happen, there aresome ways you can prepare for it, but worrying impedes clear thinking and sensibledecision-making.Patient Empowerment Anxiety Manual VIHA.March.2010 99
2. When something bad happens, I won’t be able to copeIf you worry about not coping, even before something bad occurs, the disaster will grow inyour mind and you will feel overwhelmed and helpless. You will convince yourself thatyour feared situation will never get better and will completely destroy you.If what you fear does come true and you already feel helpless and overwhelmed, it will bemuch harder for you to cope. Strong emotions interfere with clear thinking and realisticdecision-making.The following ideas suggest new approaches to coping:Coping means muddling through a situation, somehow.Anxious people believe that “coping” means quickly managing every part of a situationperfectly; this is an unrealistic expectation to put on yourself. Problem situations areusually messy and confusing and there may be no way that anyone could manage quicklyor perfectly.Natural feelings of distress make it harder to cope in an ideal way. A more helpfuldefinition of coping is “muddling through a situation somehow.”Tell yourself: “I don’t have to fix all of this really well, by myself, immediately. I just have tofigure a way to muddle through, somehow.” Thinking like this allows you to relax a littlemore, and will actually help you cope better.If you doubt your ability to cope, ask yourself the following:“How many other difficult situations have I coped with in my lifetime?”The fact that you are still alive and functioning is the only proof you need that you areexperienced at coping.Remind yourself: “I have dealt with many tough situations over the years and I will be ableto muddle my way through this one.”This way of dealing with difficult situations promotes clear thinking and realistic decisionmaking.Patient Empowerment Anxiety Manual VIHA.March.2010 100
Anxiety LiesAnxiety tells you that what you are worrying about is going to happen and when it does, itwill be catastrophic!The following two questions will help you dispel the illusions anxiety tries to create.1. Is what I’m worrying about really going to happen?a) Specify what you are worrying about.b) Collect relevant information that either supports or contradicts your fear.c) Determine the probability that what you fear will actually happen.2. Even if it does happen, would it really be as catastrophic as I’m imagining?a) What have you done to cope with similar problems in the past?b) What could you do to cope now?Patient Empowerment Anxiety Manual VIHA.March.2010 101
Coping CardsAnxious people often make the anxiety worse by telling themselves things such as “What ifthe car breaks down; this is all going wrong; we never should have left; this is going to be adisaster.” These thoughts actually reduce our ability to cope.Research has shown that the best way to cope with a difficult situation is to tell yourselfthings that help you calm down and stay grounded, focused on the moment, rather thanpredicting trouble in the future.Below is a list of coping statements to prepare you for difficult situations. You can addothers that work for you. Type out the statements you find helpful on a small card (you caneven have it laminated) and carry it with you.1. I have coped with situations like this before and survived.2. I just have to muddle though – I don’t have to fix everything perfectly rightaway.3. I can try to find someone else to handle part of this.4. This is only going to last a little while longer – I can handle a few moreminutes.5. Anxiety is uncomfortable but it won’t kill me.6. Worrying doesn’t change anything. It only stresses me and wastes my time.7. There isn’t time to do everything perfectly. I need to prioritize and accept thatmany tasks can be done “good enough.”8. If I avoid things, my anxiety will get worse. If I fight anxiety, my life will getbetter.9. Saying no is hard, but I’m not going to be a doormat for others to walk on.10. A little anxiety is OK, it’s harmless; I can ignore it.11. I will start feeling less anxious if I hang on and think about other things.12. Breathe.________________________________________________________________________________________________________________________________________________________________________________________________________________________Patient Empowerment Anxiety Manual VIHA.March.2010 102
Coping PlansFrom time to time things will go wrong, whether you worry or not, however hard you try,because that’s just the way life is.You have a choice: you can either worry about things that might go wrong or you canmake plans for how you will deal with them. If you have some idea of how you mightcope, you will feel less anxious and you will cope much better than if you simply let youranxiety take over.A coping plan is simply a list of steps you think out ahead of time that helps you manage adifficult situation.1. List what has to be done.2. Prioritize what must be done first.3. Recruit others who could help.4. Delegate tasks to each helper.5. Focus only on the task you are doing right at this moment.6. Delay emotional reactions until you have done what needs to be done.7. Pause no matter how much there is to do; you will cope better after a short break.8. Do take care of yourself. Eat, drink plenty of fluids, and get adequate sleep.9. Avoid alcohol and other drugs. They will make you less efficient at coping.10. Accept that this will be a difficult time.11. Tell yourself “I will muddle trough this, one step at a time.”If you find yourself worrying about something that might go wrong, write out a coping planusing these steps and put it away in a safe place. Whenever you start to worry about theproblem, remind yourself “I have planned as best I can for this. I refuse to think about itanymore.”Coping is a step-by-step process. Looking at the big picture and seeing every detailoverwhelms anxious people. It is more calming and effective to think of coping with asituation a small chunk at a time. Concentrating on small pieces of the situation gives youa greater sense of control, which gives you space and time to use your best coping skills.Patient Empowerment Anxiety Manual VIHA.March.2010 103
Problem SolvingAnxiety is strengthened by avoidance. The following problem solving technique is helpfulwhen you feel stuck. It will help change worry into action.1. List the specific problem that you are worrying about.2. Brainstorm all possible solutions and options – don’t leave any out.3. Choose one of the options or solutions you’ve listed.4. Take action!5. Evaluate results.6. Repeat steps 3, 4 and 5 as necessary.Patient Empowerment Anxiety Manual VIHA.March.2010 104
Taking RisksYour anxiety is making you miss out on a lot of things in life. Taking a risk means doingeveryday things that you’ve been avoiding.The only way to get some of those things back in your life is to start doing them. This maysound scary to you. In fact, you may be feeling anxious just at the thought of doing riskythings.There is a way to make it easier to get back to a fuller and more enriched life.• List some of the things you have been avoiding. Choose small everyday things suchas going to a store or a movie.• Number your list with #1 being the least anxiety provoking.• Start with #1 on your list.• Break it down into small manageable progressive steps.• Begin with the first step.• Hang in there until your anxiety starts to drop.• Tell yourself “Good for me. I’m teaching myself that I don’t have to get so panickedabout everything.”• Repeat the experiment daily until you can easily do the activity with little anxiety.• When you have mastered one risk, pick the next from your list, and take the samesteps.Remember, if you stop when your anxiety is rising you have just strengthened your anxietyand made it harder to repeat the activity. By waiting until your anxiety begins to drop, youlearn that what you feared and avoided is not so dangerous.Continue until you put anxiety in its place and take back your life.Patient Empowerment Anxiety Manual VIHA.March.2010 105
Example: Kelly begins by making a list of everyday things she’s been avoiding. She thennumbers the list from the least to the most anxiety provoking. She begins with # 1,banking, and breaks it down into small progressive steps, which she works her waythrough. When her anxiety has sufficiently decreased, she proceeds to # 2 on her list.ListNumber• grocery shopping 4• going to a movie 3• coffee with a friend 5• going to the bank 1• taking a bus 6• going to a mall 2Breakdown # 1 (going to the bank)• organize paperwork• prepare to go out• walk to bank• spend time outside bank• spend time inside bank• line up for teller• transaction with tellerSteps• Begin with first step (organize paperwork)• Hang in until anxiety begins to decrease• Congratulate your effort• Repeat (organizing paperwork) as necessary until anxiety is minimal• Move on to next step (prepare to go out)• Repeat each step until activity (going to the bank) causes little anxiety• Repeat this procedure with # 2 (going to a mall)Patient Empowerment Anxiety Manual VIHA.March.2010 106
Assertive Behaviour 101The following are a number of behaviors that are part of being assertive:• Eye ContactAn effective way of engaging the person you are talking to and conveying sincerity is bymaking culturally appropriate eye contact.• Body Posture97% of what we communicate is through body language. Your message will be moreeffective if you face the person, stand or sit appropriately close to him, lean towardshim, and hold your head erect while maintaining a relaxed body posture.• GesturesA message accented with appropriate gestures takes on added emphasis, while overlydramatic gesturing can be a distraction.• VoiceA whispered monotone seldom convinces another person that you mean business,while shouting arouses defenses that get in the way of communicating. A level, wellmodulatedconversational tone is convincing without being intimidating.• Facial expressionsEffective assertions require an expression that matches the message. Smiling orlaughing while expressing anger is confusing to the recipient and doesn’t get yourmessage across.• TimingSpontaneous assertive expression will generally be your goal, however sometimes youmay need to take “time out” until you have your emotions in check.• ContentIt is more useful to express yourself honestly and spontaneously then it is to endlesslyworry about whether or not you are going to say the perfect words, in the perfect order.It’s important to express yourself assertively, not aggressively, using “I statements” andfocusing on specific behaviors rather then labeling the person.Patient Empowerment Anxiety Manual VIHA.March.2010 107
D.E.S.C. ScriptAssertiveness doesn’t guarantee that we will get all we want, all of the time. The followingtechnique gives us a way of making sure we say what we mean and improves the chance ofbeing understood and avoiding a defensive reaction.Describe• State what happened, just the facts• Be objectiveExpress• State calmly how you feel• Use “I” statementsSpecify• State the specific behaviour you want changed• Choose only one thing at a timeConsequences• State appreciation for changed behaviour• Set limits if outcome is unsatisfactory.Patient Empowerment Anxiety Manual VIHA.March.2010 108
Algorithm for Initiating Antidepressant Therapy in DepressionRefer forpsychotherapy ifpatient preference oradd cognitivebehavioural officeskills to antidepressantmedicationModerate to Severe depression(PHQ 15 or more)Offer AntidepressantMedicationDepressedMoodAntidepressantTreatment AppropriateFor mild depression specific psychologicaltreatments are preferable to antidepressants,PHQ
Application forPsychiatric Medication CoverageA. to be signed as true by the ApplicantName: Gender: ❒ M ❒ FAddress:Postal Code:Telephone:Date of Birth:yyyy mm ddPersonal <strong>Health</strong> Number (PHN)Mandatory1. The cost of the prescribed psychiatric medication is a significant barrier to me taking my medication. I have no otherfinancial coverage, and I believe I qualify for Premium Assistance ($28,000 family adjusted net income plus $3,000per dependent).2. I consent to the release of financial and clinical information about me to the mental health centre and the Ministry of<strong>Health</strong> for the sole purpose of verifying my eligibility for this program.3. I understand that the personal information collected on this form relates directly to and is necessary for programoperations. The information will be handled in accordance with the Freedom of Information and Protection of Privacy Act.If I have any questions about the collection and use of this information, I will contact my <strong>Health</strong> <strong>Authority</strong>.Signature of ApplicantCheck a, b or cI certify that the patient:Dateb. to be signed by the prescribing physician - Send to local Mental <strong>Health</strong> Centre/<strong>Authority</strong>. (Do not sendto MSP/PharmaCare or Mental <strong>Health</strong> & Addictions Headquarters.)a. ❒ has been hospitalized for a psychiatric condition,OR without the medicationb. ❒ is likely to require hospitalization,ORc. ❒ other serious consequences are very likely (e.g. unemployment, child neglect, etc.)Name of prescribing physician (print) Signature Datec. APPROVAL BY MENTAL HEALTH CENTRE / AUTHORITYSignature of Director or DesignateDateNote: This authorization will expire in ❒ 1 yearDate:❒ or earlier Date:hlth 3497 Rev. 2005/11/07171
MAJOR DEPRESSIVE DISORDERNot all medications listed are eligible for coverage under the No-Charge Psychiatric Medication Program (Plan G).Coverage information is provided on the BC PharmaCare website at www.health.gov.bc.ca/pharme/outgoing/plangtable.html.FAMILY PHYSICIAN GUIDE | PHARMACOLOGICAL INTERVENTION87 3.31
APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUESDetailed information on the specific application of these treatment modalities in theperinatal period is in the (1) Best Practices Guidelines relating to ReproductiveMental <strong>Health</strong>, and (2) Self-Care Program for Women with postpartum depression &anxiety (see Resources). See also the section on non-pharmacological therapies inthe Guide.Pharmacotherapy in the Perinatal PeriodPractice Issues: Antidepressants in Pregnancy and Postpartum■ Sustaining maternal mental health throughout pregnancy is the key to ensuringan optimum outcome for the baby.■ As yet, there is little evidence for the efficacy of psychotherapy in the treatmentof moderate to severe depression in pregnant, depressed women.■ Resolution of symptoms for women in this category is best achieved, at present,with antidepressant medications.■ Women with severe depression and with a prior history of depression can betreated with a combination of antidepressant medication and psychotherapy.■ To date, existing evidence suggests that the most commonly used antidepressantmedications, such as SSRIs (e.g., Prozac, Paxil, Zoloft, Luvox and Celexa) andSNRIs (e.g., Effexor), have not been associated with major birth defects.■ There is increasing concern regarding transient neonatal adaptation symptomsfollowing prenatal exposure.■ This has led the <strong>Health</strong> Canada (see <strong>Health</strong> Canada Advisory below) and the USFood and Drug Administration (FDA) to issue warnings regarding third-trimesterSSRI and SNRI use for treating depression during pregnancy.■ The recent concern over the warnings by <strong>Health</strong> Canada and the US FDAregarding infants exposed to antidepressants in the third trimester, has lead to aclinical dilemma for treating physicians. The evidence for these warnings is:– based on case reports and retrospective data.– the number of cases studied tends to be small, particularly with neweranti-depressants■ In addition, the presence/absence of symptoms observed in neonates aregoverned by a complex set of factors including:– prematurity– maternal mental and physical health– use of concomitant substances (e.g., alcohol, cigarettes)– polypharmacy■ Characteristics of this Neonatal Poor Adaptation Syndrome include:– transient course in the infant– resolution within the first few days of life– no evidence of long-term consequences in the children.– the use of multiple psychotropic medications during pregnancy with anSSRI appears to increase the risk of these symptomsNeonatal Management Issues■ An infant can be identified as being at risk for transient Neonatal PoorAdaptation Syndrome if the mother is:– taking a high dose of any antidepressant medication– on more than one medication– if the woman is mentally ill and/or under-treatedFAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES88 7.13
APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES■ The infant’s behaviour should be monitored closely :– by nursing and medical staff– if there are signs of abnormal Central Nervous System (CNS) behaviour, avoidearly discharge and consider a differential diagnosis– obtain infant drug levels if possible where a diagnosis remains unclear■ Supportive neonatal care of symptomatic infants can be provided by usingthe following approach:– provide low level stimulation– support breastfeeding– provide supportive measures where appropriate– follow symptoms closely■ Ensure long-term follow-up for mother and infant.7.14FAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES89
Pharmacotherapy in the Perinatal Period: Specific Medications7.16 FAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES90
Pharmacotherapy in the Perinatal Period: Specific MedicationsFAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES 7.17 91
Pharmacotherapy in the Perinatal Period: Specific Medications7.18 FAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES92
Pharmacotherapy in the Perinatal Period: Specific MedicationsFAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES 7.19 93
Pharmacotherapy in the Perinatal Period: Specific Medications7.20 FAMILY PHYSICIAN GUIDE | APPENDIX 2: WOMEN’S MENTAL HEALTH ISSUES94
MAJOR DEPRESSIVE DISORDER3.32FAMILY PHYSICIAN GUIDE | PHARMACOLOGICAL INTERVENTION95
FAMILY PHYSICIAN GUIDE | ADDRESSING SUICIDAL RISKpage 2 of 696 3.73
Atypical AntipsychoticsClozapine- increased risk of agranulocytosis- Very sedating and cause wt gainInitiation of Treatment:1) Ensure that the results of the WBC and 5 part differential are within an acceptable rangeand were obtained within the last 7 days. Warning: clozapine should not be administered topatients with a baseline WBC < 2.5 and or granulocyte < 1.5 unless otherwise indicated bythe physician's assessment.2) Obtain and record a baseline weight, blood pressure and pulse.3) Administer 12.5 mg po clozapine4) Monitor BP every 30 minutes for one hour. If BP fluctuates then continue to monitor every30 minutes until stable. If BP drops below 90/60 or if the patient experiences any adversereactions the attending physician must be notified to assess patient. Document BP readingson the patient's health record.5) Patient's who have not experienced a drop in BP or other adverse reactions will be given aprescription for clozaril 25 mg po qhs for one week.Ongoing Monitoring:1) Weekly for 26 weeks CBC, WBC and 5 part differential will be obtained and documented.After 26 weeks biweekly CBC and 5 part differential will be obtained for the duration ofclozapine administration. Please note that in the case of a warning fall in the granulocytecount, a CBC and 5 part differential count will be obtained twice per week until otherwiseindicated by the physician.2) The physician will review the lab results to ensure that they are within the acceptablerange prior to authorizing the appropriate pharmacy to provide the patient with another one ortwo week supply of clozapine.3) Appointments with the attending physician are indicated if the patient experiences any ofthe following:• deterioration of mental status• values below normal range for WBC < 2.5 or granulocyte < 1.5.4) Patient's receiving clozapine must have the following assessment completed ANNUALLY:• physical examination• diagnostic investigation including: CBC, WBC and 5 part differential, FBS, creatinine,urea, electrolytes, bilirubin, alkaline phosphatase, AST• ECG will be done if there is a known history of cardiac problems• EEG will be completed if there is a known history of seizures
Olanzapine (Zyprexa)Tablets, wafers: 2.5, 5, 7.5, 10, 15, 20 mg. Intramuscular Injection: 10 mg vial- wafers good for post surgical GI problems- good for bipolar mania, depression and maintenance- problems with weight gain.- Agitation/insomnia 2.5 – 5 mg- Depression 5 – 10mg good alone or with SSRI (Prozac most commonly)- Borderline Personality disordero Good for anxiety, paranoia, impulsivity but not depressiono 5mg / dayRisperidone (Risperdoal)Tablets: 0.25, 0.5, 1, 2, 3, and 4 mg. Oral solution: 1 mg/mL. Orally disintegrating tablets: 0.5,1, 2, 3, and 4 mg. Powder for injection: 12.5, 25, 37.5, and 50 mg.- not as sedating as Olanzapine or Clozapine- good with OCD, Tourettes, schizophrenia, bipolar mania- Depression – used with SSRI may give up to 2.5 x response- side effects:o increased prolactin causing sore breasts, lactationo akithesia (restlessness)Quetiapine (Seroquel)Tablets: 25, 50, 100, 200, 300, and 400 mg- new long acting tab, not much difference but regular may be better for sleep, agitation- not as strong an antipsychotic as above- good for anxiety or insomnia ( 12.5 – 100 mg/hs) – very effective without rebound oraddictive potential- long acting version good as anti-depressant alone- may help with cocaine withdrawlZiprasidone (Zeldox)capsules of 20 mg, 40 mg, 60 mg and 80 mg. The injectable form is available in vialscontaining 20 mg of lyophilized ziprasidone that must be reconstituted with 1.2 ml of sterilewater before injection.- not as sedating, less weight gain- QT prolongation therefore do baseline ECG and watch when patient on cardiac drugs.Safe if normal ECG.Paliperidone (Invega)Tablets: 1.5 mg, 3 mg, 6 mg, and 9 mg- active metabolite of risperidone
Approved Use1. schizoaffective disorder2. Drug psychosis3. schizophrenia4. Bipolar (Risperidone, olanzapine, quetiapine)5. Aggression and psychosis in dementia (Risperdal only)Off label Use1. Agitation/insomniaa. Olanzapine 2.5 – 5mgb. Quetiapine 12.5 – 100mgc. Very effective without rebound or addiction potential2. Anxiety – SSRI’s still mainstay of treatment3. PTSD – improves sleep and anxiety4. Depression – Olanzipine and Quetiapine XR alone or with SSRI5. Borderline Personality disorder – good for anxiety, paranoia, impulsivity but notdepression associated with BPD6. Autism7. Tourettes, stutteringRecommended Monitoring- Increased risk of DM which can be independent of weight gain (up to 10x risk of DM)especially clozapine and Olanzapine- Increased risk of metabolic syndrome- Weight gain especially in first few monthso Worst with clozapine, Olanzapineo Then risperidone, quetiapineo Least likely with Zeldoxo Recommend small, frequent meals with protein and exercise1. Check weight at 0, 1, 2, 3 and 6 mos then q 6 mos2. BP 0 then q 6 mos3. FBS 0, 3 then q 6 mos4. lipids 0, 3 then q 6 mos5. waist circumference with wt.Switching from one to another, go slowly with fragile patients. 20% taper off old and 20%increase on new q weekly over 4 – 5 weeks.
Consortium forOrganizationalMental<strong>Health</strong>careAntidepressantskills at workDealing withDepression forTeensPositiveCoping with<strong>Health</strong>ConditionsCoping withSuicideThoughtsGuide forSurvivors ofSuicideRelaxationAudioWorking withthe Client whois SuicidalWorking withthe SuicidalPatient148
Working with the Suicidal PatientA Guide for <strong>Health</strong> Care Professionals• Assess/Ensure Safety• Build Rapport − introduce yourself, your role, your goals• Assess Current Suicidal Ideation• Obtain Details on Current Attempt (if applicable)• Obtain History• Communicate with Family/FriendsSummary Refer to Mental <strong>Health</strong>/Psychiatry if high risk • Connect with Primary <strong>Health</strong>care Provider(s)• Advise Patient − instill hope, obtain information onexisting supports, provide a safety plan• Provide Referrals at Time of Discharge• Follow-up Post-DischargeTask One: ASSESS1. Assess current suicidal ideationIs suicidal ideation present now?Have you gotten to the point where you did not want togo on? Have you had thoughts of not wanting to be alive?What about right now?Passive Ideation: The patient would rather not be alive, butdoes not indicate a plan that involves an act of initiation= LOWER RISK (e.g., I’d rather not wake up in the morning;I wouldn’t mind if a car hit me when I was crossing the road)Active Ideation: The patient has acute thoughts ofcompleting suicide = HIGHER RISK (e.g., I do think aboutkilling myself; I feel like throwing myself into traffic)Intense, continuous ideation = HIGHER RISKIs there a plan?Do you have a plan as to how you would end your life?Detailed, carefully thought-out plan = HIGHER RISKIs there intent?You talk about wanting to die, and have even considered[taking pills] but are you intending to do this?Low Intent: Suicidal thoughts and fantasies about plans,with absolutely no intent to put these plans into action.Fantasizing about suicide can provide some comfort tothose in distress to know there is always a way out= LOWER RISK (e.g., Oh no, I could never do that, I havechildren)High Intent: Expression of specific intent to end life= HIGHER RISK (e.g., I intend to do this as soon as mydaughter’s graduation is over)Ambivalent or Unclear Intent: Ask about what has helpedin past.What has stopped you from ending your life to this point?What has helped in the past when/if you’ve had thesethoughts?2. Obtain details if there is a suicide planHow lethal is the plan?How lethal does the patient believe the method(s) to be?Is there access to means?Obtain specific details.What pills do you have or would you take to overdose?Exactly where would you get a gun from?Has patient chosen a time and/or place?How isolated is the patient? What preparations have beenmade (e.g., buying rope)?Has patient made final arrangements?Has patient prepared a suicide note, settled their affairs orcommunicated to others?Higher lethality, access to means, preparationsand arrangements = HIGHER RISKNote: This document is intended to be a guide to working with the suicidal adult, and should not replace a psychiatric consultation.When suicide risk exists, an expert opinion should be sought to determine the need for hospitalization and clarification of diagnosis.149
3. Gather details on current andprevious attemptsPrevious attempts, especially inpast year = HIGHER RISKTriggers of Present AttemptWalk me through the last 24 hours. At what point did youconsider suicide?Triggers of Past AttemptsTell me about other times you have seriously consideredsuicide or made an attempt. What chain of events led upto attempts you’ve made in the past?LethalityAssess the lethality of the method(s). What was thelikelihood that the patient would be found after they madethe attempt?ImpulsivityWas attempt carried out in the heat of anger (impulsive) orwas it carefully thought-out (planned), with day and timepicked in advance? What was the direction of hostility (goalto hurt self or others)?IntoxicationWas patient intoxicated at time of attempt (substance usecan lead to disinhibition and can contribute to individualsacting in atypical ways)?Expectations of DyingWhat did you think would happen to you when you [cut yourwrists/took an overdose]? How did you think others wouldrespond? Did you truly think you would die?OutcomeWas medical intervention required? How was this accessed(e.g., patient called for help vs. being found unresponsive byothers)?4. Obtain information on psychiatricand other historyObtain information on psychiatric history (e.g., depression,psychosis), including symptoms that may suggestundiagnosed mental illness; substance use/abuse (alcohol,drugs); and past/current mental health treatment, includingall current and past psychiatric medications.Obtain information on other chronic and acute stressors(e.g., loss of relationship, loved one, job; gambling/financialstressors; trauma/abuse; struggle with sexual identity issues;changes/discontinuation of medications).Assess for protective factors, such as family, friends, pets,religion, and therapist.Ask about any other relevant and contributory factors.Is there anything else I should know about?5. Conduct mental status examinationEmotional StateWhat is the patient’s self-reported mood vs. their observedaffect?Extremes in emotional state/mood (no vitality,emotionally numb or unbearable emotionalpain/turmoil) = HIGHER RISKBehaviour & AppearanceHow is the patient behaving (agitated, alert, cooperative)?How do they appear (hygiene, speech)?Thought <strong>Process</strong>Is the patient oriented? Are attention, concentration andmemory intact? Assess thought process (logical, organized),thought content (paranoid, delusional), and judgment andreasoning.Feelings about SurvivalGuilt, remorse, embarrassment = LOWER RISKDisappointment, self-blame = HIGHER RISK(e.g., I couldn’t even get this right and kill myselfproperly)150
Problem-Solving CapacityCan the patient generate strategies and options forproblem-solving through their difficulties?Reasons for Living & Level of HopeWhat reasons do you have for living? How hopeful do you feelthat your current situation could change? What is needed tochange to help you feel not so hopeless?Feelings of hopelessness, helplessness, and view offuture as empty or meaningless = HIGHER RISK6. Communicate with families/significant other(s)Obtain contact information for, and consent to speakwith, family/significant other(s). Connecting with familyand friends demystifies what’s happening, and allows thepatient’s support system to develop confidence in theassessment and treatment process.Inform next of kin/emergency contact if patient has madesuicide attempt.Note: In an emergency, consent is not required to releaseinformation to family/significant other(s), although it is acourtesy to inform the patient of disclosure of information.Consent is also not required to obtain information fromfamily/significant other(s).Solicit input from family or significant others, as this ishelpful for risk assessment and safety planning. Inquireabout changes in behaviour, signs of depression,hopelessness, past attempts, any communication of intent,difficulties adhering to treatment, and examples of riskybehaviour (important when decisions are made aboutcertification).7. When to make a specialist referralRefer patients with a psychiatric history to mental health/psychiatry.The high-risk patient should be admitted to hospital orprovided a high-priority referral for a mental health orpsychiatric assessment to provide recommendations aboutmanagement.SAD PERSONS provides a useful screening acronym toidentify the high risk patient:Sex (male)Age (adolescent or elderly)DepressionPrevious attemptEthanol abuseRational thinking loss (psychosis)Social supports lackingOrganized planNo spouse/partnerSickness – especially chronic/uncontrolled painOther factors suggesting high risk are: multiple risk factors;profound hopelessness; lack of protective factors; highlethality; premeditation of present attempt; and/or familyhistory of suicide, depression or substance abuse.8. Communicate with primary careprovider(s)Obtain information from patient and/or their familyabout the patient’s current health and mental health careprovider(s). Communicate with patient’s primary careprovider(s) to ensure continuity of care.Include family/significant other(s) in discussions regardingsafety and treatment planning (discuss ways family/friendscan implement support in the patient’s home environment).Acknowledge feelings of family/friends (e.g., fear, anger).Guide them to seek psycho-educational and emotionalsupports for themselves. Provide referrals for supportagencies.151
Task Two: ADVISE1. Provide meaning and supportExplain a Model of SuicideProvide a model to help the patient understand theirsuicidality, and to normalize their feelings. People thinkseriously about suicide when they experience the 3 I’s intheir life situation: Intolerable (meaning their life situationis so painful that it seems unbearable), Interminable (itseems like it’s going to go on like this forever), andInescapable (it seems like nothing they’ve tried haschanged or will change their experience).Provide Coping StrategiesProvide strategies for coping that target the 3 I’s: Intolerable(distress reduction/tolerance strategies); Interminable(cognitive challenging techniques); and Inescapable(effective problem-solving). Provide Coping with SuicidalThoughts, a document to help individuals decreasethoughts of suicide, develop a safety plan and connect withhelpful resources.Reinforce the Value of TreatmentTreatment (both therapy and medication) can help to reduceyour suffering. Therapy can help you to identify and addressunderlying issues that are contributing to you feeling thisway, and provide you new ways of dealing with your lifeproblems. Medication can help you with difficulties you arehaving with [depressed mood, anxiety, sleep, appetite].Address Ambivalence in Order to Instill HopeMany people have mixed feelings about suicide, and are justlooking for some way to get out of the pain they are feeling.There are ways you can find support to help with that painthat don’t include ending your life.Reinforce Positive Coping Used in the PastWhat has helped in the past when you’ve had these thoughts?2. Develop a safety planDevelop an interim, written safety plan with the patient tohelp them stay safe until they secure longer-termprofessional supports. Provide written safety plan to patient,primary care provider and family/significant other(s).Discuss with the patient how to make their environmentsafe (remove risky means of self-harm; have friend or familyon-site for the short-term).Generate with the patient adaptive means of self-soothingand coping with distress (calling a friend, going for a walk).Generate with the patient reasons they have for living, andmethods they have used to cope in the past. Work withthe patient on completing the Safety Plan provided in thepatient handout, Coping with Suicidal Thoughts.Indicate to patient that if they try these steps and still do notfeel safe, they should go to a hospital emergency room orcall 911.3. Provide informationProvide a written copy of a treatment plan, including detailsof medications (if applicable) and dates of follow-upappointments to patient, primary care provider and family/significant other(s).If the patient is prescribed antidepressants, explain thatthere may be temporary increased risk as symptoms ofdepression resolve at different rates, and improvement ofmood may be delayed in comparison to improvement inphysical symptoms such as energy or sleep.Provide contact numbers of primary care providers (familyphysician, psychiatrist, psychologist), local crisis lines(1-800-SUICIDE) and mental health centres.Instill hope. Most importantly, let the patient and theirfamily/friends know that there is help available. Indicate thatalthough you cannot guarantee that there will be no furtherattempts or difficult feelings, prognosis will be much betterif the patient adheres to the treatment plan. Indicate that itmay take time to find the right diagnosis and treatment, andtime for patient to make accompanying changes.4. Follow-upFollow-up with the patient and/or family or significantother(s) within 48 hours to answer any questions they have,and to offer further information, including providingreferrals.Copies of this document, as well as the document Coping with Suicidal Thoughts, can be downloaded at no cost from the B.C. Ministryof <strong>Health</strong> (www.health.gov.bc.ca/mhd) or from the Centre for Applied Research in Mental <strong>Health</strong> and Addiction (www.carmha.ca).152
SUPPORTED SELF‐MANAGEMENT FOR DEPRESSIONSTEP ONE: PRESCRIBE THE ANTIDEPRESSANT SKILLS WORKBOOKProblem SolvingBehavioural ActivationActions• Withdrawal• Reducedactivity• Poor self-careSituations• Loss• Conflict• IsolationRealistic ThinkingThoughts• Harsh self-criticism• Over-pessimistic aboutcurrent situation• Catastrophic about futurePhysiology• Altered sleep• Low energy• Changes in brainchemistryEmotions• Sadness• Despair• NumbnessSEE PAGE 6 Antidepressant Skills WorkbookKey messages:• We can work together to change how you feel• Others have found these ideas very helpful• You’ll need to do some reading and practice• I’m happy to work with you on this ‐‐ we’ll set some regular visits to checkhow you’re doing and work out problemsDoes this seem like something you’d like to try?153
SUPPORTED SELF‐MANAGEMENT FOR DEPRESSIONSTEP TWO: HELP THE PATIENT FIND A STARTING POINTPt isinactive/isolatedBEHAVIOURAL ACTIVATION- Identifying target areas (eg Social Contact, Self Care)- Setting goals (Specific, Realistic, Scheduled)Page 18Patient is feelingoverwhelmed,“can’t cope”Patient has overlynegative thoughtsPatient hasanxiety/tensionREALISTIC THINKING-Identifying depressive thoughts‐Coming up with realistic thoughts-Challenging depressive thinking‐Practicing realistic thinkingPROBLEM SOLVING-Identifying a mildly difficult problem-Coming up with actions-Evaluating pros and cons, Choosing-Making a planRELAXATION TRAINING‐Getting CD or downloading audiofile‐Practicing weeklyPage 30Page 39Free download:www.comh.ca/selfcare/The Antidepressant Skills Workbook is available for free download at www.comh.ca/selfcare/.Also available at that website are: translations into French, Chinese and Punjabi; an audiobookversion; versions for adolescents and the workplace; and other useful clinical tools.REFERENCES:• Bilsker D, Goldner EM. Training GPs to prescribe depression self‐management. In TheOxford Guide to Low‐intensity CBT Interventions, Oxford University Press (expected 2010).• Bilsker D, Anderson E. Supported Self Management for depression in primary care. InPsychiatry in Primary Care: A Concise Canadian Handbook, Centre for Addiction & Mental<strong>Health</strong> (expected 2010).• Bilsker D, Anderson J, Samra J, Goldner EM, Streiner D (2009). Behavioural interventions inprimary care. Canadian Journal of Community Mental <strong>Health</strong> 27: 179‐189.154
SELF-CARE DEPRESSION PROGRAM2ND EDITIONANTIDEPRESSANTSKILLS WORKBOOK
TABLE OF CONTENTSIntroduction 1What is depression? 3What causes depression? 6What can you do about depression? 14More about medication 16Antidepressant Skills 181. Reactivating your Life 192. Thinking Realistically 303. Solving Problems 39The road ahead: Reducing the risk of relapse 49The story of Margaret 53Suggested reading 54Useful information 55Diet 56Physical activity 57Sleep 58Caffeine 60Drugs and Alcohol 61Worksheets 63
INTRODUCTIONDepression is among the most painful and difficult of all humanexperiences. It robs those who have it of energy, interest, and thewill to make things better. It brings with it a profoundly negativeview of the self, the world, and the future. During depression, it seemsas though nothing can change, as though you will never get better.But depressed people do get better and depressiondoes end. There are effective treatments and self-helpskills to deal with depression. <strong>Health</strong> care professionalsgive depression treatments, but you can learn self-helpskills and apply them to your own life. This guideteaches a set of antidepressant skills you can use tomanage depression. Sometimes the skills can be usedon their own, when the depression isn’t too severe.Sometimes they have to be used along with treatmentsby professionals.The emphasis in this book is on three steps:reactivating your life; changing negative thinkinghabits; and solving problems as they arise. In addition,some of the lifestyle choices associated with reducingdepression are discussed in the Useful Informationsection at the back of the book. Although medicationbasedapproaches are discussed briefly, most of ouremphasis is on these other approaches: antidepressantskills rather than antidepressant pills.We hope that the workbook will be helpful for you. Butreading it will not be enough. For the approaches towork, you will have to put them into practice. We havetried to present all of the strategies in a clear, step-bystepformat that will help you to work steadily towardyour goals.SELF-CARE DEPRESSION PROGRAM1 ANTIDEPRESSANT SKILLS WORKBOOK
INTRODUCTIONTake a moment now to ask yourself three questions. Mark your answers on the scales below. On a scale of 0 to 100:How much of a negative effect has low mood had on my life?0 50 100NO EFFECTEXTREMELY NEGATIVE EFFECTHow important is it to me to feel better?0 50 100NOT IMPORTANT AT ALLEXTREMELY IMPORTANTAm I willing to make getting better a priority in my life?0 50 100NOT A PRIORITY AT ALLEXTREMELY HIGH PRIORITYIf you scored less than 50 on two or three scales, you may be considering change, but still feel uncertain.If that’s the case, read the workbook and think it over.If you scored 50 or more on two or three scales, you’re ready to change. You’ve had enough and you’reprepared to dedicate some time each day to getting better.Go to the next page and let’s get started . . .SELF-CARE DEPRESSION PROGRAM2 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT IS DEPRESSION?Most times when you feel down, you’re not depressed. Feeling sad or lowis a big part of life and can’t be avoided. When something goes wrong inyour life, whether it’s an argument with your partner, conflict with yourboss, or a physical illness, your mood might drop.Depression is not…Most times when you feel down, you’re not depressed.Feeling sad or low is a big part of life and can’t beavoided. When something goes wrong in your life,whether it’s an argument with your partner, conflictwith your boss, or a physical illness, your moodmight drop.If you feel especially sad or irritable because of thissituation, maybe with poor sleep, not wanting to seefriends or family, eating too much or not enough – thenyou’re probably experiencing low mood. Low mood willtypically go away in a week or two, especially if there’san improvement in the situation that started it.Depression is…But suppose it doesn’t go away and just gets worse.You might be depressed:1. if your mood is very low or you have almost nointerest in your life almost everyday, and thisfeeling goes on for weeks; AND2. if you have other problems like:■ big changes in weight or appetite;■ not being able to sleep enough or sleepingtoo much;■ feeling that you are always restless orslowed-down;■ thinking that you are worthless or guilty;■ feeling really tired much of the time;■ feeling numb or empty;■ having a lot of trouble concentratingor making decisions;■ thinking about death or suicide.SELF-CARE DEPRESSION PROGRAM3 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT IS DEPRESSION?The two most common types of depression are called mild depressionand major depression.Each of these includes the same kinds of problems (theones we’ve listed above) but major depression is moresevere. Usually, when a person gets depressed, it’s themild kind. Your family physician, a psychiatristor a psychologist can tell you whether you havea depression.FEELING OKAYMILD DEPRESSIONTheLOW MOODMAJOR DEPRESSIONFeelingsadness goessad becauseMisery, despair,somethingon too long. Veryit goes on andhappened.gethard toon.outFeelingof the low mood.numb orempty.SELF-CARE DEPRESSION PROGRAM4 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT IS DEPRESSION?A few observations about depression . . .■ Depression is hard to diagnose on your own.Our moods affect our judgment of ourselves. So it’soften hard to judge whether we are really depressed.Usually it takes a trained professional to makethe diagnosis.■ If you have depression, you are not alone.More than 4% of adults are depressed at any giventime, and more than 15% of adults will be depressedat some time in their lives.■ Depression is not a sign of weakness.Many capable, intelligent, and extremelyaccomplished people have been depressed.Being depressed does not mean that you havea “weak personality” or a character flaw.If you think you have depression . . .If you think that you have depression, it is importantthat you find help. The skills in this workbook aremeant to help you with your depression, but youshouldn’t have to do it alone. Getting another opinionfrom someone you trust can help you understand yourproblems or put them in perspective. If you continueto feel depressed, seek the help of a health careprofessional. This can be your family physician, apsychologist, psychiatrist or other mental healthprofessional. They can help you with a number ofdifferent treatments for depression. A good thingabout these treatments is that they work wellalongside skills you learn from this workbook.If you feel like hurting yourself . . .For many people, depression makes life seem hopelessand unmanageable. Most depressed people feel this wayfrom time to time. For a small number of individualsthis feeling of hopelessness gets so strong that theybegin to think that life itself is not worth living. Ifthis happens to you or someone you know, it’s time toget help. Find a health care professional to help youget past these feelings. If you can’t wait for anappointment, there are a number of crisis lines, staffed24/7, that you should call. Go to your yellow pages andlook under Crisis Centres to find the numbers in yourarea. You might also visit the Emergency Room at yourlocal hospital.Remember, things can get better.SELF-CARE DEPRESSION PROGRAM5 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?People become depressed for a wide variety of reasons.Research has identified a number of factors associatedwith causing and continuing the depressed state. Thediagram below shows the five major factors: situation;thoughts; emotion; physiology; and action. Each ofthese areas of your life can play a role in the developmentof depression, and depression itself can havean impact on all of them. On the following pages weconsider each of these factors in more detail.ACTION• social withdrawal• reduced activitylevel• poor self-carePHYSIOLOGY• altered sleep• low energy• changes in brainchemistrySITUATION• loss• isolation• conflict• stressEMOTION• discouragement• sadness• despair• numbness• anxietyTHOUGHTS• negative thinkinghabits• harsh self-criticism• unfair & unrealisticSELF-CARE DEPRESSION PROGRAM6 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?SituationDepression is often triggered by very stressful life situations.If your attempts to cope with these situations byimproving or accepting them have not been successful,you may begin to feel overwhelmed and hopeless. Thenthe risk of a depressive episode increases. Some situationsthat can be associated with depression include:■ Major life events, particularly involving loss. Eventssuch as the death of a loved one, moving, divorce,financial setbacks, or job loss are major disruptionsin one’s life.■ Lack of contact with other people. Social isolationis a significant risk factor for depression.■ Relationship conflict. Times of conflict inpersonal relationships, whether marital or family,are extremely stressful and can contribute to theonset of depression.■ Stress related to your physical health. This isespecially true for health problems that are chronic,cause a lot of pain or disability, and only get partlybetter with treatment. Some physical illnesses ortheir treatments can trigger depression by theireffects on the body. For example, hypothyroidism(a condition in which the thyroid gland secretestoo little thyroid hormone) is often associatedwith fatigue and depression.That doesn’t mean people only get depressed whenthings are going badly. Some people get depressedwhen their life has been going smoothly: depressionjust seems to come out of nowhere! Antidepressantskills like the ones taught in this book are just asuseful for these people.■ Stress related to your job. This can takethe form of employment uncertainty (notknowing whether your job will continue),friction with supervisors and co-workers,or overwork (human beings were neverdesigned to work 16 hours a day,either in an occupation oraround home).SELF-CARE DEPRESSION PROGRAM7 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?ThoughtsEach of us is affected differently by outside events,depending on how we think about those events.Imagine two people walking into a party. One personis naturally outgoing, anticipates enjoying herself agreat deal, and sees the group of partygoers as friendlyand receptive. The other dreads social gatherings,anticipates feeling miserable, and sees the other peopleas judgmental and rejecting. Each person’s thoughtsdetermine how the event is experienced. Researchevidence has shown that depressed individuals oftenhave distorted ways of thinking about the world thatcan trigger or worsen the experience of depression.SELF-CARE DEPRESSION PROGRAM8 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?Distorted ways of thinkingUnrealistic, negative thoughtsabout the situation.You see the situation in an unrealistically pessimisticway, emphasizing its negative or threatening aspectsand ignoring more positive or promising aspects.Unfair, negative thoughts about yourself.You think about yourself in a very critical fashion,judging yourself in a harsh and unfair manner.Unrealistic, negative thoughtsabout the future.You anticipate a future that is bleak and disappointing,exaggerating the likelihood of very negative outcomes.Taken together, we call this the Negative Triad: thinkingin an unfair and unrealistic, negative way about yourcurrent situation, yourself, and your future.These ways of thinking often start in childhood. Somepeople grew up in families where only negative andcritical comments were made. In other families,children were discouraged from saying positive thingsabout themselves and rewarded for being self-critical.Whether these negative thinking styles are caused bythe depression or started in childhood, they haveenormous influence on your experience of the world.Not surprisingly, these ways of thinking about theworld increase the negative impact of difficult lifesituations and predispose people to emotional pain.A person with depressive thinking can becomediscouraged or hopeless even when things aregoing well.SELF-CARE DEPRESSION PROGRAM9 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?EmotionDepression often begins with feelings of discouragementand sadness after unsuccessful attempts to deal witha difficult life situation. However, as the depressioncontinues, these feelings of unhappiness give way tomore severe and painful kinds of emotional experience.The depressed individual is overcome by a sense ofdespair, a pervasive mood of hopeless misery. A feelingof intense anxiety (physical tension, worry, and asense of impending doom) often accompanies thesedepressed feelings.Some depressed people experience a general sense ofemotional numbness, an inability to feel anything. Itis as though the psychological pain has become sointense that your mind simply switches off youremotions, like a circuit breaker.Remember that depressed people interpret the world inan unrealistically pessimistic way and judge themselvesin a harsh and unfair manner. The emotions they feelare based in large part on this negative way of interpretingtheir lives. If their thoughts about the worldare unrealistic and negative, then their emotions willalso be unrealistic and negative.It may be hard to think about emotions as unrealistic.But imagine a person who firmly believes that airplanetravel is extremely dangerous and that planes are fallingout of the sky frequently. That person will feel veryfrightened when flying. This fear, however, is basedon a false belief about airplane safety and is, therefore,unrealistic and inappropriate to the situation. Similarly,depressed individuals often have beliefs about theworld and themselves that are unrealistic and leadto unrealistic, negative emotions.SELF-CARE DEPRESSION PROGRAM10 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?PhysiologyDepression is accompanied by a variety of physicalsymptoms. One of the most powerful physical changesaccompanying depression is impaired sleep. Usually,this involves an inability to get enough sleep, whetherbecause the person has difficulty falling asleep, repeatedlywakes during the night, or awakens much too early.Sometimes the person may sleep too much, caused bya desire simply to hide away in sleep or a fatigue sopervasive that there never seems to be enough sleep.When sleep is “non-restorative” – that is, the persondoes not awake feeling refreshed and rested – itbecomes harder to face the day and deal with problems.Depressed people often feel that they lack energy andare exhausted by everyday activities.One theory of depression is that it is caused by changesin brain function, a “chemical imbalance”. There isresearch showing that, for some depressed people,certain neurochemicals in the brain are less active.It is unclear, however, whether these changes in brainchemistry commonly cause depression. All we know isthat depression is often associated with changes inbrain chemistry.The physiological changes of depression make it harderto cope with life problems or even to follow the stepsof a depression management program like this one.Antidepressant medication can often be quite helpfulin restoring sleep and regaining your sense of physicalenergy. It can allow you to actively learn and try outthe new skills needed to overcome depression.SELF-CARE DEPRESSION PROGRAM11 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?ActionDepression usually has a significant impact on a person’s behaviour. Here are some of the main areas affected:Not doing rewarding activities.Hobbies, crafts, sports, reading, and travel may all suffer. Depressed people often feel too tired or unmotivated topursue these activities, and the less they participate in them, the less they feel able to do so. Most depressedpeople suffer from anhedonia, reduced ability to have fun or get enjoyment from things. Why would you goto the movies, engage in hobbies, or do the things you used to enjoy if you didn’t think you would enjoythem? Inactivity becomes a habit. As a result, the depressed person no longer receives the personalsatisfaction provided by these activities, further contributing to the sense of discouragement.Not taking care of yourself.Activities designed to maintain one’s body and appearance are frequently neglected. Depressed individualsmay take less care in personal grooming or dress than usual. In addition, exercise is often reduced, whetherthis involves formal fitness activities such as jogging or simply walking around the neighbourhood. Eliminatingexercise contributes to depression by removing a powerful source of physical well-being and increased selfesteem.As well, the depressed person often has disrupted eating habits, whether this means inadequate intake(“forgetting to eat”) related to a lack of appetite, or overeating as a form of self comfort.SELF-CARE DEPRESSION PROGRAM12 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAUSES DEPRESSION?Not doing small duties.A depressed person often neglects or procrastinates doing small, necessary duties, like running errands, takingout the garbage, cleaning house, or caring for the garden. Failing to complete these chores adds to the depressedperson’s sense of inadequacy and lack of control over life. It also creates friction with others and places furtherstress on relationships.Withdrawing from family and friends.Social invitations are refused, phone calls are ignored, and habitual get-togethers with family or friends somehowjust don’t happen. Social isolation is a strong contributor to depressed mood, taking you away from the warmthand sense of connection to others, basic to all of us. Depressed people often believe that others have no interestin their company, given how miserable or emotionally flat they are feeling.SELF-CARE DEPRESSION PROGRAM13 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAN YOU DO ABOUT DEPRESSION?MILD DEPRESSION■ Talking to family and trusted friends about howyou’ve been feeling is usually a good thing to do.They can help you figure out solutions to some of theproblems you’ve been dealing with; besides, justknowing that people care about you is helpful.■ Write about problems you’re facing, your feelings andthoughts, and possible solutions. This can help youunderstand what you’re going through and whatchoices you have.■ Speak to a family physician, psychiatrist or psychologist.A professional can help you figure out what’sbeen going on and can make useful suggestions.■ In some cases, antidepressant medications can behelpful in overcoming Mild Depression. But for mostindividuals with Mild Depression, the answer does notlie in medication.Learning and practicing the antidepressant skills in this guide is likelyto be very helpful in overcoming Mild Depression.SELF-CARE DEPRESSION PROGRAM14 ANTIDEPRESSANT SKILLS WORKBOOK
WHAT CAN YOU DO ABOUT DEPRESSION?MAJOR DEPRESSIONIn addition to the actions described previously…■ Definitely see your family physician if you thinkyou might be this depressed. Major Depression is aserious problem and should be diagnosed by a familyphysician, psychiatrist or psychologist.■ Antidepressant medications are the most commonlyprescribed treatments for Major Depression and areusually effective.■ An equally effective treatment for most cases ofMajor Depression is Cognitive Behavioural Therapy(CBT). CBT is a talking therapy that teaches new skillsfor thinking and acting more effectively. This guide isbased on CBT methods.■ Yet another effective treatment is interpersonaltherapy (IPT), a talking therapy that teaches newskills for dealing with partners, friends and family.■ For long-lasting or recurrent depression, the mostpowerful approach is to combine antidepressantmedication with one of these kinds of talkingtherapy.Learning and practicing the antidepressant skills in this guide is likely to help in overcomingMajor Depression. BUT remember that the skills taught in this guide will not be enough bythemselves to fix something this serious. If you have a Major Depression, you should seekprofessional help.SELF-CARE DEPRESSION PROGRAM15 ANTIDEPRESSANT SKILLS WORKBOOK
MORE ABOUT MEDICATIONMedication is quite helpful in a number of cases. Many of thosewho take antidepressant medication experience a lift in moodand a reduction in other symptoms (such as loss of appetite ordifficulty concentrating).But medication is seldom a complete treatment formood problems: it is also important to make changesin how you think about and handle your life. Don’t usemedication as a way of allowing you to keep living anunhealthy or unfulfilling lifestyle. Instead, medicationcan give you the energy and mood lift you need tomake changes (such as starting a regular exerciseprogram, learning assertiveness skills, or definingand working toward your life goals).SELF-CARE DEPRESSION PROGRAM16 ANTIDEPRESSANT SKILLS WORKBOOK
MORE ABOUT MEDICATIONHere are some additional points about medication:Different medications workfor different people.It can take time to find a medication (or a combinationof medications) that works well for a person withouttoo many side effects. Side effects may include sleepdifficulty, change in appetite and loss of sexual desire.Never stop taking medication suddenly.Some people have unpleasant reactions to discontinuingantidepressant medications. If you wish to stop amedication, consult with your prescribing physician.Usually you will stop in stages by gradually takingless over time.Certain people benefit from takingmedication for a long time.For some people, antidepressant medication continuesto have beneficial effects over the long term. Mostpeople take medication for a while in order to getthe strength to make positive changes, then graduallystop using it.It can be tempting to stop taking amedication as soon as you get thelevel of improvement you want.The result is often a rapid return of the problem. Itis generally best to stay on the medication until yourmood has been steady for a while. Reductions inmedication may then be done gradually while yourmood is monitored.SELF-CARE DEPRESSION PROGRAM17 ANTIDEPRESSANT SKILLS WORKBOOK
ANTIDEPRESSANT SKILLSIn this section, you will learn three skills that can stop your mood fromsliding down, lessen your depression and help prevent it from happeningagain. The skills are:Reactivating Your Life ■ Thinking Realistically ■ Solving ProblemsWe will explain how each of these skills helps fightdepression and show you in a step-by-step way howto use the skill. It’s best to think about these skillsthe way you would if you were learning a new job or anew sport: practice is very important. Some people findit helpful to share this guide with a spouse, trustedfriend, counsellor or family member – this person canhelp you keep practicing even when you feel low energyor unmotivated. If there’s no one like that, then keeppracticing the antidepressant skills. As you work throughthe skills, it will gradually get easier and the result isworth it.Depression involves all areas of your life: youremotions, thoughts, actions, physical functioning, andlife situation (including social support, family relationships,employment, finances, and so on). Each ofthese areas is connected to all the others. As a result,changes in one area produce changes in the others.When depression first develops, negative changes inone cause the others to get worse as well. But whenyou are working on getting better, changing one arealeads to improvements in the others. The goal of treatmentis to get all areas of your life spiraling upward,each producing positive change that improves the others.SELF-CARE DEPRESSION PROGRAM18 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEDuring depression, most people don’tdo the things that normally keeptheir mood positive.But if you stop taking care of yourself or doing thethings you normally like, your life becomes more dulland depressing. Although it can feel as though youare comforting yourself by being less active, in factyou are probably helping the depression get worse.In other words:DEPRESSIONINACTIVITYDepression leads to inactivity, but inactivity makesdepression worse. What seems like a good coping strategyactually tends to maintain or intensify depression. Thesolution: don’t wait until you feel like doing more.Waiting actually makes it less likely that you will getbetter. And don’t wait until you feel motivated – asyou get better, you will regain a sense of motivation.Action starts first, motivation kicks in later. Settinggoals to increase your activity level is a powerfulmethod for managing depression.The aim is to gradually get yourself moving eventhough you might not feel like it. These are thesteps to gradually reactivating your life.SELF-CARE DEPRESSION PROGRAM19 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 1: Identify activities to increaseThere are four main areas in which depressed peopleoften reduce their activity. These are: Involvementwith Family & Friends; Personally Rewarding Activities;Self-Care; and Small Duties.In order to identify some goals to work on, take amoment to consider each of these areas. List someactivities in each area that have been affected bydepression (or that had been neglected even beforethe depression began) and that could be increased.Personally Rewarding ActivitiesExamples:Reading magazines. Walking in a natural setting. Doing crafts or hobbies. Planning travel.Seeing movies, plays, or games.Increasing your activity in this area will make a difference because:1. it reminds you of your own interests, the things that are important to you2. it provides you with badly-needed rewards as your depression starts to liftYour ideas:SELF-CARE DEPRESSION PROGRAM20 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFESelf-CareExamples:Getting dressed each day. Taking time to shower and get cleaned up. Exercising. Eating breakfast. Eating morenutritious food. (Lifestyle factors associated with reducing depression are discussed in the information sheetsat the back of the book.)Increasing your activity in this area will make a difference because:1. it will directly enhance your sense of physical well-being2. it helps remind you that you are a competent personYour ideas:SELF-CARE DEPRESSION PROGRAM21 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFESmall DutiesExamples:Opening the mail. Paying bills. Housecleaning. Grocery shopping. Running errands.Increasing your activity in this area will make a difference because:1. it increases your sense of control2. it reduces tension with others as you begin to take on a share of the workYour ideas:SELF-CARE DEPRESSION PROGRAM22 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEInvolvement with family and friendsExamples:Inviting people to do things. Keeping in contact with people where you used to live.Returning phone calls. Getting out to a social group or class.Increasing your activity in this area will make a difference because:1. it will help you regain a sense of being connected to others2. it gives other people the chance to provide reassurance and support3. it takes you away from being alone and thinking depressing thoughtsYour ideas:SELF-CARE DEPRESSION PROGRAM23 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 2: Choose two of these activitiesPick two activities that are most practical for you to begin changing now. Your first two choices should befrom different areas.Activity 1:Activity 2:SELF-CARE DEPRESSION PROGRAM24 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 3: Set realistic goalsFor each of the activities you have chosen, set amanageable goal for the coming week. Keep in mindthat depression makes it difficult to get moving. As aresult, you need to set your goals much lower thanyou ordinarily would.see whether it needs any repairs. If you would like toget the house cleaned up, your first goal might be tovacuum one room, or dust one shelf. If you want tosocialize with people again, your first goal might be totalk to one friend on the telephone for five minutes.For example, if you would like to start riding a bicycleagain, your first goal might be to find your bicycle andTo succeed, your goals must be:SpecificDepression can make almost anything seem like a failure. You need to have a very clear idea of your goal so thatyou will know you have succeeded.RealisticYou may find it tempting to set your goals based on how much you think you should be able to accomplish. Don’t.Keep in mind that depression slows you down and makes things more difficult. Your goals should be easy enoughto be achievable even if you feel very depressed in the coming week. Sometimes it seems overwhelming to thinkof starting a new activity. In that case, try setting the goal of gathering information related to the activity: forexample, finding out what sorts of exercise activities are available in your local community centre.ScheduledYou should have a clear idea when and how you are going to carry out your activation goal. “Take a walkThursday evening for 15 minutes” is much better than “Walk more.”SELF-CARE DEPRESSION PROGRAM25 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 3: Set realistic goals, continuedHere is an example:Frank started with two goals: slightly increasing his level of physical activity (from none to one short walk eachweek) and increasing his level of social activity (from none to going out with his wife and daughter every twoweeks). His goals looked like this:ACTIVITY HOW OFTEN? WHEN EXACTLY?Walk, 15 minutes Once a week to start Thursday eveningGoing out with my wife and daughter Once every 2 weeks Saturday or Sunday eveningsHe used his appointment book to write in each of these activities. After he did each activity,he checked it off in his book.SELF-CARE DEPRESSION PROGRAM26 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 3: Set realistic goals, continuedTry setting some goals that would be realistic to do this week. Decide how often or for how longyou will do the activity, and when you will do it.Now write your goals:ACTIVITY HOW OFTEN? WHEN EXACTLY?1.2.Think of your activity goals as appointments with yourself.Treat these goals as respectfully as you would anappointment with your physician. If you must cancelone of these appointments with yourself, rescheduleimmediately and don’t miss it.Note: Don’t give yourself extra credit for doing morethan the goal you set for yourself. If you do more,that’s fine, but that doesn’t allow you to miss the nextappointment. If you let that kind of trade-off happen,your goals will soon be neglected.It’s a good idea to buy an appointment book to keep track of your goals.When you've done the goal, check it off in the book to show yourself what you'veaccomplished – in the early stages of getting better, that's the reward.SELF-CARE DEPRESSION PROGRAM27 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 4: Carry out your goalsIt’s important to realize that you probably won’t“feel like” doing your activity goals. In depression, yourmotivation to do things is much less than usual. But ifyou wait until you feel like it, most likely nothing willhappen. Do the activity because you set a goal for yourselfand because it will help you get better. After you’vedone and checked off each goal, you will see whatyou’ve accomplished.In the early stages of recovering from depression, it’slikely that you won’t get much enjoyment from youractivities, but as you continue to increase your activitylevel and focus on recovery, you will gradually regainthe ability to enjoy activities. You’ll even regain theability to motivate yourself!If you completed a goal, did you congratulate yourself?If not, do so now. Depression is likely to make youfocus on the things you haven’t done, and ignore ordownplay your accomplishments. This keeps the depressiongoing, because you will constantly feel like a failure.Deliberately remind yourself of achievements, no matterhow small they may seem. “All right, I planned to walkaround the block and I did it. Good.” Don’t ignore smallvictories or think they don’t count. They do, especiallyduring depression. If you find yourself minimizing yourown achievement (“but that was such a small thing todo”), remember that completing small goals whiledepressed is like walking a short distance with a veryheavy pack. Meeting goals while depressed is challengingand deserves to be recognized.If you didn’t succeed, what got in the way? What canyou do to make the goal easier? Recognize that yourgoal may have been too ambitious. Try making it smallerfor next week, or substitute a different goal. Depressedpeople often set their goals too high, fail to reachthem, and become discouraged. The problem is not thatthey are lazy, but that they are too eager to get well!Scale back to something you are sure you can do, evenif you feel no better this week than you did last week.Washing one dish, making one phone call, opening onebill, walking around one block, or spending five minutesat a hobby: these are all perfectly reasonable goals. Asyour energy comes back you will be able to do more.But for now, allow yourself to get started slowly.SELF-CARE DEPRESSION PROGRAM28 ANTIDEPRESSANT SKILLS WORKBOOK
REACTIVATING YOUR LIFEStep 5: Review your goalsAfter two weeks of doing these goals, review the situation.■ Do you want to increase the goals slightly or keep doing them at the same level until it feels pretty comfortable?It’s your choice.■ This is a good time to add another goal. Pick one from another area. For example, if you had Self-Care andPersonally Rewarding Activities goals before, choose one from Involvement with Family & Friends or from SmallDuties.New Activity:ACTIVITY HOW OFTEN? WHEN EXACTLY?Write the new goal into your schedule along with the 2 continuing goals. Remember, check off the activity goal asyou do it and praise yourself for completing it.After two weeks of doing these goals, review thesituation again. Are there any goals that were notgetting done? What got in the way? Do you need toreduce or change the goal?Keep going! Continue to set your ongoing goals, andconsider adding additional goals as your energy permits.If you complete a task (for example, if you have nowfinished gathering information about recreational activitiesin your community), then move on to a new goal.Keep using the procedure:■ Set your 3 goals.■ Write them in your schedule.■ Check off each goal as you do it.■ Praise yourself each time.■ Review the goals every two weeks to decide if theyneed modification and whether you are ready toadd a new goal.Eventually, you’ll be working on 3-4 goals at a time ormaybe more. Don’t get carried away, though: having toomany goals can get overwhelming.SELF-CARE DEPRESSION PROGRAM29 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYNegatively distorted thinkingfeeds into depression. We callit depressive thinking.Depressive thinking is unrealistic and unfair:■ unrealistic, negative thoughts about your situation;■ unrealistic and unfair, negative thoughtsabout yourself;■ unrealistic, negative thoughts about your future.The aim is to challenge depressive thinking and replaceit with realistic thinking.Realistic thinking is:■ accurate about your situation, seeing thingsclearly as they are;■ fair about yourself, looking in a balanced way atthe positive and negatives in your life;■ accurate about your future, not exaggeratingbad outcomes.So what’s the goal in dealing with depressive thinking?Is it to think positive thoughts all day long? Do we wantto kid ourselves that nothing bad will ever happen?No. Overcoming depressive thinking doesn’t meanreplacing it with positively distorted thinking (everyoneloves me, nothing bad will ever happen, I will alwaysget what I want). The point is that thinking in anunrealistic way, whether positive or negative, causesus to feel and react inappropriately. The aim is toevaluate our lives and ourselves in a realistic manner.The goal is fair and realistic thinking.That means being fair and realistic about yourself (payingattention to good qualities and strengths as well asproblems), about your current situation (weighing thepositive and negative aspects of your life accurately)and about your future (not exaggerating the likelihoodof very negative outcomes). So, how do you changedepressive thinking?Following are the steps . . .SELF-CARE DEPRESSION PROGRAM30 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 1: Learn to identify depressive thoughtsDepressive thoughts are unfair and unrealistic. They are distorted because they are inaccurate reflections ofhow the world is or how you are. The table below (and continued on the next page) describes some commonforms of distorted thinking in depression 1 :Filtering.In this kind of depressive thinking, you only look at the bad, never the good. Because all you see is the negativeside, your whole life appears to be negative. But realistic thinking equally considers positive and negativeaspects of your life.Overgeneralization.In this kind of depressive thinking, one negative event seems like the start of a never-ending pattern. If onefriend leaves, they all will. If you fail the first time, you’ll fail every time. But realistic thinking recognizesthat one disappointing situation does not determine how other situations will turn out.All or Nothing Thinking.You see the world in terms of extremes. You are either fat or thin, smart or stupid, tidy or a slob, depressed orjoyful, and so on. There is no in-between. Gradual progress is never enough because only a complete change willdo. “Who cares that I did half of it? It’s still not finished!” But realistic thinking sees people and events asfalling somewhere between the extremes, towards the middle, where most things are found.Catastrophizing.A small disappointment is seen as though it were a disaster. For example, you were slightly late in completinga small project, so your entire month is ruined: you react to the imagined catastrophe (a terrible month) ratherthan to the little event (a late project). But realistic thinking sees events in their true importance, notoveremphasizing negative events.Labeling.You talk to yourself in a harsh way, calling yourself names like “idiot”, “loser”, or whatever the worst insults arefor you. You talk to yourself in a way you would never talk to anyone else. But realistic thinking doesn’t usethese kind of insults because they are not fair, you wouldn’t talk to anyone else that way, and they areunnecessarily discouraging.1These types of distorted thinking are described in an excellent book, Feeling Good by David Burns (Avon, 1992).SELF-CARE DEPRESSION PROGRAM31 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 1: Learn to identify depressive thoughts, continuedMind-reading.You feel as though you know what others are thinking about you, and it’s always negative. So you react towhat you imagine they think, without bothering to ask. But realistic thinking recognizes that guessingwhat others think about you is likely to be inaccurate, especially when you are depressed.Fortune-telling.You feel as though you know what the future will bring, and it’s negative. Nothing will work out, so why bothertrying? But realistic thinking recognizes that you don’t know how things will turn out: by staying opento the possibility of positive results, you’ll be more hopeful and more likely to make things better.Perfectionism.It’s only good enough if it’s perfect. And because you can’t make most things perfect, you’re rarely satisfiedand can rarely take pride in anything. But realistic thinking gives credit for accomplishments, even if theresult is less than perfect. Few of us reach perfection in what we do, but our achievements are meaningful.Shoulds.You think that you know how the world should be, and it isn’t like that. You know what you should be like, andyou aren’t. Result: You are constantly disappointed and angry with yourself and with everyone around you.But realistic thinking understands the limitations of the world and of yourself — trying for improvement butalso accepting how things are.There are other types of depressive thinking, but these are some of the most common ones. When you catchyourself thinking depressively, it can be useful to look at this list to see if you are using one of them.SELF-CARE DEPRESSION PROGRAM32 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 2: Recognize your own depressive thoughts and howthey trigger low mood.Most thinking is so quick and so automatic that wedon’t even realize we are doing it. We must learn tobecome aware of depressive thinking as it occurs. Anexcellent strategy is to carry around pencil and paperfor a week.Although depression can seem like a constant darkcloud, it actually varies over the course of the day.Every time your mood sinks, ask yourself thisimportant question:“What was going through my mind just then?”What were you thinking about? What were you reactingto? Write this down. For example, perhaps getting onthe bus one morning you suddenly felt a deepeningof the gloom you’ve been feeling. What was goingthrough your mind just then? Perhaps you noticedthat everyone on the bus was facing you, and you hadthe thought that they were judging you negatively.Excellent! Write it down.Keep recording your thoughts until you notice that thesame kinds of depressive thinking come up again andagain. You might find yourself placing a checkmarkbeside some of the thoughts you wrote down earlier.“Oh, that one again.” When this happens, you haveprobably identified the most common kinds ofdepressive thinking you do.Write some of these depressive thoughts here:Then what? Some of your depressive thoughts may seemobviously distorted. “Wait, the reason they were facingme on the bus is that I was at the front, not becausethey wanted to look at what a loser I am!” It can sometimesbe enough just to know that your mind generatesdepressive thinking in certain kinds of situations. Try tobecome aware of the depressive thinking as it happensand remind yourself where it comes from. “I think thisway because my mood is low and because I was a selfconsciouskid – not because they were all judging me.”You may find that you take the depressive thoughtsless seriously once you know where they come from.When you become aware of depressive thoughts youmay feel tempted to attack yourself. “How could I thinksuch stupid thoughts?” Depression causes you to beself-critical, and recognizing depressive thinking cangive you one more way to beat up on yourself. Don’t.Instead, remind yourself that depressive thoughts arethe product of low mood and of your personal history.You are not stupid for having them. They are normalduring depression.SELF-CARE DEPRESSION PROGRAM33 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 3: Learn to challenge these depressive thoughts and replace themwith fair and realistic ones.Challenging depressive thoughts involves deliberatelyrethinking the situation that got you upset. To do thisyou can use a strategy called Challenging DepressiveThoughts. Take a piece of paper and divide it intocolumns, like the example below. There’s a sampleof this form at the back of the manual. Feel free tophotocopy it if you wish.Challenging Depressive ThoughtsSituation: Friend cancels lunch date.DEPRESSIVE THOUGHTShe doesn’t like me.(Mind-reading)No one likes me. I’m unlikable.(Overgeneralization)The world is a cold and rejecting place.(Catastrophizing)I’ll always be alone.(Fortune-Telling)REALISTIC THOUGHTI don’t know why she cancelled; maybesomething urgent came up. It’s only lunch.Some people do seem to like me, so I mustbe likable.This lunch doesn’t mean much about the worldas a whole. I’ve been accepted before.I can’t tell the future. One lunch doesn’t mean noone will ever like me.First, make a brief note of the situation. Some examples: “Talking to daughter,” “Walking to work,” “Planning tomake dinner.” Next, write down the negative thoughts that seem related to how you feel. If you like, you can tryto classify the type of distortion involved (as shown above).Finally, think about the situation and try to come up with a more fair and realistic assessment of the situation.Hint: Depressive thinking often goes way beyond the facts. Often the fair and realistic thought is simply to remindyourself that you don’t have enough information to know for certain what’s happening. “I don’t know why shecancelled lunch; there might be hundreds of possible reasons.”SELF-CARE DEPRESSION PROGRAM34 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 3: Learn to challenge these depressive thoughts and replace themwith fair and realistic ones, continuedCalling yourself insulting names like “idiot” will causeyou to feel more discouraged; as a result, you may giveup on a task. But giving yourself encouragement andfair evaluation is likely to result in trying harder, whichincreases the odds of a successful outcome.When you’re down or depressed, it’s not easy to comeup with fair and realistic thoughts. Here are somequestions that will help you do this.Depressive Thought:Can I get more evidence, like asking someone about the situation?Would most people agree with this thought? If not, what would be a more realistic thought?We are often much more realistic about other people than about ourselves.What would I say to a friend in a similar situation?What will happen if I continue to think this way?What is another way of thinking that is more encouraging or useful?SELF-CARE DEPRESSION PROGRAM35 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 3: Learn to challenge these depressive thoughts and replace themwith fair and realistic ones, continuedNow use these questions to come up with more realistic ways of thinking about a situation that upset you. Noticethat it usually feels better to think realistic thoughts than depressive thoughts.Situation:DEPRESSIVE THOUGHTSREALISTIC THOUGHTSSELF-CARE DEPRESSION PROGRAM36 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 4: Practice realistic thinking.It’s not enough to come up with a fair and realisticthought just once. Depressive thinking gets repeatedover and over, sometimes for years, until it becomesautomatic. More balanced thinking will help you tofeel better, but it won’t be automatic – at least not fora while. The good news is that changing depressivethinking doesn’t take years: in fact, depressed peopleoften begin to notice emotional differences after onlya few weeks of practicing this antidepressant skill.Certain kinds of situations can really trigger depressivethinking. Situations likely to trigger depressive thinkingmight include meeting with your boss, attending asocial gathering with people you don’t know well, orhaving a disagreement with a family member. In orderto get the greatest benefit from this approach, youmust catch yourself in situations that normally triggerdepressive thoughts for you.1.2.3.Try to think of a few situations where you often have depressive thoughts.Write them here:SELF-CARE DEPRESSION PROGRAM37 ANTIDEPRESSANT SKILLS WORKBOOK
THINKING REALISTICALLYStep 4: Practice realistic thinking, continuedWhen you find yourself in these situations, deliberatelyrehearse your fair and realistic thinking. Don’t assumethat it will happen on its own. You will have to tellyourself how to look at the situation, just as you mightgive advice or encouragement to a friend. Talk back tothe depressive thinking. Don’t allow depressive thinkingto happen without replying to it. Every time youtalk back, you make the depressive thinking weaker andthe realistic thinking stronger. But it takes time beforerealistic thoughts have more influence over you thandepressive ones.You will probably find that, for the first while, therealistic thinking sounds false to you. For example:you’ve been thinking in a perfectionistic way aboutyour work, telling yourself that “my work has to be100% or else it’s worthless,” but you are given verylittle time to complete each task, so you often feellike a failure. You realize that this is unrealistic thinkingand come up with the fair and realistic thought that“achieving 80% is acceptable in this job, given thetime I have; that’s all anyone else accomplishes.” Atfirst, this realistic thought will seem false, as thoughyou are just fooling yourself. Only with time andrepetition does realistic thinking – the truth – beginto feel true to you. Eventually you will come toaccept realistic thoughts.SELF-CARE DEPRESSION PROGRAM38 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYDepression is often the result of life problems that have becomeoverwhelming. The strategies for solving them have beenineffective, or may even have made them worse.Why is it that as people get depressed, their ability tosolve problems declines? There are several reasons:■ Solving problems takes energy. As depressionworsens, the energy level declines.■ Everyday problems take a backseat to a biggerproblem – the depression itself. Because the personbecomes so concerned about the mood problem,other problems slide and get worse.■ Depression causes difficulties in concentration,memory, decision-making ability, and creativity.Most problem-solving requires all of these skills.Given all of these factors, it is no great surprise thatproblems don’t get solved and instead pile up. Whatcan be done? First, recognize that your problem-solvingability may not be as good as it usually is. Don’tbeat yourself up over this. It is a normal symptomof depression, and it does get better. Then sit downand follow these next steps...SELF-CARE DEPRESSION PROGRAM39 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 1: Choose a problemThe first step in problem solving is to choose a problem.Sometimes, depressed individuals have difficulty identifyingspecific problems in their lives – they see everythingas one huge problem. For them, identifyingparticular problems worth tackling is quite helpful.It brings them closer to finding realistic answers.One way to identify problems is to pay close attentionto how your mood changes through the week. Noticewhat’s happening when your mood goes down: whatwere you thinking about; where were you; and whathappened just before your mood changed? Changes inyour mood can be a helpful guide to show you wherethe problems are.Some of your problems might be large ones (for example,“I have an eviction notice that comes up next week”)while some are small (“I’m going to need carrots if Iwant to make that salad tonight”). Other problems aresomewhere in between (“There’s a pile of mail on mydesk that I haven’t had the courage to look at in overa week”).Choose one of the smaller problems that is happeningnow. Later, you can move up to larger problems. Tryto be specific. For example, “My relationships are amess” isn’t specific: it’s not clear what the problem is.“My best friend hasn’t called me in a month” is morespecific and makes it clear what is going wrong andwhat you want to change.The problem you choose is:SELF-CARE DEPRESSION PROGRAM40 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 2: Think of actions to help solve the problemWrite down three things you could do to help solve theproblem. Consider things you can do that don’t dependon somebody else. Don’t try to decide which one is best:just come up with different actions you might carry out.Don’t worry if you tried something before and it didn’twork – situations change. And don’t worry whether theactions will solve the problem completely – your aimnow is to be doing something useful, not to fix thewhole problem.Here is an example:It was done by Amy, employed as executive secretary to a senior manager.The Problem:My workload is overwhelming – files are piling up in my tray and, even though I work long hours, I keepgetting further behind. I’ve told my boss that the workload has been growing quickly, but she doesn’t doanything about it. The whole situation seems out of control and I’m starting to feel pretty depressed.Possible Actions:1. Just keep going, maybe my boss will notice how overloaded I am and she will get another employeeto take over some of the work.2. March in to my boss’s office and let her know that I’ve had enough, ask her to stop makingunreasonable requests.3. Write down all the jobs that are on my desk, then note which ones are urgent to do today, and whichones need to be done this week, this month or this century. That way, I’ll be focusing my energy on thehighest priority tasks and I can plan ahead a little more effectively.SELF-CARE DEPRESSION PROGRAM41 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 2: Think of actions to help solve the problem, continuedWrite three possible things you might do about the problem you’ve identified.The Problem:My workload is overwhelming – files are piling up in my tray and even though I work long hours I keepgetting further behind. I’ve told my boss that the workload has been growing quickly, but she doesn’t doanything about it. The whole situation seems out of control and I’m starting to feel pretty depressed.Possible Actions:1.2.3.SELF-CARE DEPRESSION PROGRAM42 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 3: Compare these actionsConsider which of these actions are most likely to help the problem. Look at the advantages and disadvantages ofeach one.This is what Amy wrote:ACTION ADVANTAGES DISADVANTAGES1. Just keep going ■ It’s what I’m used to doing ■ It will probably keep getting worse■ I won’t get into conflict■ If I fall behind much more, I couldget into big trouble■ I’ll become even more depressed2. Let my boss know that ■ I’ll be speaking my mind ■ I don’t enjoy confronting peopleI’ve had enough ■ My boss might fix the situation ■ My boss might get angry with mefor being so direct, and this mightbecome a new problem3. Prioritize my jobs ■ I can catch up with the urgent jobs ■ I’ll still need to deal with the■ That would take some pressure off workload problem at some pointso I can look for other solutions■ I would feel more in control of thesituation, that would help my moodSELF-CARE DEPRESSION PROGRAM43 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 3: Compare these actions, continuedNow it’s your turn:ACTION ADVANTAGES DISADVANTAGES1.2.3.SELF-CARE DEPRESSION PROGRAM44 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 4: Pick the best oneLook over the advantages and disadvantages for eachaction and decide which one is best (or perhaps leastbad). There are no fixed rules for how to make thischoice: the only rule is that one of the actions must bechosen so that you can begin. Look over the possibilities,think about the good and bad points of each, then justpick one. It should be an action that takes you at leastpartway towards a solution. Give yourself a limited timeto make this decision so it doesn’t drag on. Remember,if you start to move in one direction and discover thatit really doesn’t work, you can try another action.Amy, the overworked secretary, chose her third action,prioritizing her jobs so she could focus on the mosturgent ones.Which action do you choose?SELF-CARE DEPRESSION PROGRAM45 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 5: Make an action planThere aren’t very many problems that you will solvecompletely with just one action. But there might bemany actions that will take you partway toward asolution. If you have a financial problem, for example,then perhaps your first action should be to gather thepaperwork together so that you can look at it. Justgathering the paper won’t solve the problem, but it willtake you closer to a solution than you were before. Theimportant thing is to get started on a solution.Your plan of action should follow four rules that can be abbreviated as M.A.S.T.In other words:Manageable. Even if you don’t feel any better in the coming week than you did last week (even if you feel a littleworse), you could do it anyway. It’s better to accomplish a goal that is too small than to fail at an ambitious one.Here’s a bad example: For my first time out, run a marathon. Better example: Walk one block.Action-oriented. Make a plan for what you will do, not how you will think or feel while you are doing it. Youhave a certain amount of control over what you do, but you have less control over your emotions and thoughts.Bad example: Spend a pleasant hour with my children. Better example: Spend one hour with my children.Specific. It should be very clear what you need to do. Bad example: Get in shape. Better example: Phone thecommunity centre to find out whether they teach yoga.Time-limited. Your plan should take only a short time to carry out. Don’t plan to change your style forever.Bad example: Keep up regular exercise for the rest of my life. Better example: Walk 20 minutes three times a week,review after two months.What’s the plan, exactly?SELF-CARE DEPRESSION PROGRAM46 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 6: EvaluateCome back to this section when a week has passed or when you have achieved your goal.What was the outcome? What went right? What went wrong?Depressed mood will tempt you to dwell on failures andon the things you haven’t done, rather than to congratulateyourself on any progress you have made. If yousucceeded at your goal, deliberately make yourself thinkabout that success (even though the problem still hasn’tbeen solved).SELF-CARE DEPRESSION PROGRAM47 ANTIDEPRESSANT SKILLS WORKBOOK
SOLVING PROBLEMS EFFECTIVELYStep 7: Move OnUse this experience to plan your next step.You have three main options:Keep going. Example: Spend another 20 minutes finding the papers.Revise your goal and try again. Example: Cleaning the garage for one hour was too difficult, so plan to workon it for just 10 minutes instead.Take a new approach. Perhaps you learned something useful from your first effort that suggests another wayof handling the issue. Example: Talking face to face with Aunt Sarah didn’t work, so write her a letter instead.Based on your experience, what is the next step?Keep working on this issue in a step-by-step manner. Record your efforts on paper. Keep reminding yourself about theprogress you make.SELF-CARE DEPRESSION PROGRAM48 ANTIDEPRESSANT SKILLS WORKBOOK
THE ROAD AHEAD:REDUCING THE RISK OF RELAPSEMajor depressive episodes end. It often doesn’t feel as thoughthey will, but they do. Unfortunately, many people go on tohave another episode months, years, or decades later.Is there anything you can do to reduce the risk ofrelapse? Yes. You may or may not be able to eliminatethe possibility of having another episode. But you canmake episodes less likely, less severe, and less frequent.Keep up your effortsWhen you feel terrible, it’s obvious that you need tomake your mental health a real priority. When you feelbetter, it can be tempting to forget all about takingcare of yourself. If you feel “good enough”, you maywant to stop working away at activity increase, realisticthinking, and problem-solving.Think about the strategies you have been using to cope.Are there some that you will need to keep up over thelong term, even after you feel better?What strategies do I need to keep up?SELF-CARE DEPRESSION PROGRAM49 ANTIDEPRESSANT SKILLS WORKBOOK
REDUCING THE RISK OF RELAPSEPlan ahead for stressWe all have difficult times in our lives – some of usmore than others. For the person who has recentlyrecovered from depression, stressful times may be a riskfactor for relapse. The solution is not to avoid all possibilityof stress (which none of us can do), but to planahead to manage the stress effectively.Some stressful events can be predicted. Perhaps youknow that on a certain date you will go back to work.Perhaps Christmas is always stressful for you, andDecember is coming. Perhaps a stressful family gatheringis scheduled. Perhaps you are expecting a baby,whose birth will bring many demands. You can planahead for these events to make them less difficult.Here are some strategies:When possible, introduce the stress gradually. If, for example, you are returning to work soon, you mightcheck to see if you could go back part-time at first.Lighten up on ongoing responsibilities. If you are taking a night school course, for example, give yourselfpermission to eat out more often or have a slightly less tidy home.Keep up your self-care. How do you keep yourself balanced? Don’t give these things up when you need them themost. If a weekly lunch with a close friend is important to you, keep doing it. If exercise helps a lot, do everything youcan to keep exercising during stressful times.SELF-CARE DEPRESSION PROGRAM50 ANTIDEPRESSANT SKILLS WORKBOOK
REDUCING THE RISK OF RELAPSECreate a Mood Emergency Action PlanIf you plan ahead for a relapse, you may be able to gethelp faster than last time. As a result, the depressionmay not become as severe, last as long, or be as difficultto recover from. By planning a course of effectiveaction ahead of time, you may not be as anxious, andyou may actually reduce the possibility of a return ofthe depression.If you were to become depressed again, what are someof the things that you could do to help yourself and getbetter as quickly as possible?Here are some areas to think about:Increase rewarding activities. Use the steps in the section called “Reactivating Your Life”.Reduce your obligations. How could you plan ahead to scale back the demands on your energy in the event ofdepression? For example, perhaps you could get an agreement in advance to reduce your work hours or to get help withchildcare from a family member.Get professional help. Consider giving permission to a few friends or family members to tell you (or perhaps yourdoctor) when they notice your mood seems to be sliding.Get support. Who could help you and what kinds of help would you need? Perhaps you need someone to talk to, ormaybe you would prefer practical help – like assistance with grocery shopping.Manage your lifestyle. A mood decline is no time to stop exercising, or getting out of the house, or eatingproperly, or keeping a good sleep schedule. What are the lifestyle factors that help your mood the most?Take some time to think about how you could get to work early in a depressive episode to prevent it fromgetting worse. What would have helped this time? Use the list above as a starting point and make up a clearplan of action.SELF-CARE DEPRESSION PROGRAM51 ANTIDEPRESSANT SKILLS WORKBOOK
Congratulations! You have now made it to the end of thisguide to managing depression. Of course, just reading the guide isn’tenough. To get the benefits of these well-researched and effectivetechniques, you have to actually put them into action in your life.It’s worth the effort. You’re worth the effort.
THE STORY OF MARGARETHere is the experience of one person whoused these methods effectively.Margaret is a married teacher in her mid-30s who came to her family physician withsymptoms of depression. She had recentlytransferred to an inner city school, attractedto the challenge of the work. But she foundshe could not accomplish what had beennormal for her, although she worked longhours. She began to sleep poorly and toworry almost all the time. She criticizedherself in a harsh manner for not doing aswell as she expected. Her mood began todrop until she felt miserable. This madeit more difficult to perform her job andshe became even more self-criticaland depressed.Antidepressant medication was prescribedby her family physician. This helped hersleep, raised her energy level and greatlyreduced her emotional suffering.When she read through the section onReactivating Your Life, she realized thatshe had been avoiding her friends sinceshe took the job and especially since shebecame depressed. She set the goal of meetinga friend once a week for tea. Later onshe increased this to includeother social activities. After the first month,she added moderate exercise as a goal.When she read through the section onThinking Realistically, she recognized severalcognitive distortions: she had a very selfcriticalway of thinking; she expectedherself to perform perfectly; and sheignored praise from others. She usedquestions from the self-care guide to comeup with more fair and realistic ways ofthinking: What evidence do you have? Shehad received positive evaluations and acolleague told her she was doing as wellas possible in the situation. What wouldyou say to a friend in the same situation?She wrote out the fair and supportive wordsshe would say to a friend, then practicedsaying them to herself. What is a lessextreme way of looking at the situation?She wrote down some more realisticthoughts about the job situation, thenreminded herself of these whenever shenoticed the unrealistic, negative thoughts.The combination of antidepressant medicationand self-care methods led to a gradualimprovement in her depression, a more fairand accepting attitude towards herself,more realistic self-expectations, and moreenjoyment of her life.SELF-CARE DEPRESSION PROGRAM53 ANTIDEPRESSANT SKILLS WORKBOOK
SUGGESTED READINGON DEPRESSION AND RELATED TOPICSBurns, David D. Feeling Good (1992, Avon Books) or The Feeling Good Handbook (1999,Plume Books). Extremely successful self-help books on depression and anxiety. Theemphasis is on specific exercises to carry out.Catalano, Ellen Mohr (1990). Getting to Sleep. Oakland: New Harbinger Publications. Auseful book that describes a variety of sleep problems and offers concrete suggestionsfor dealing with them.Paterson, Randy (2002). Your Depression Map: Find the Source of Your Depression andChart Your Own Recovery, New Harbinger Publications, Inc. A guide to developingindividualized strategies for recovering from depression.Greenberger, Dennis and Padesky, Christine (1995). Mind Over Mood. Guilford Publications,Inc. A hands-on workbook for therapy clients suffering from depression, panic attacks,anxiety, eating disorders, substance abuse, and relationship problems.Cronkite, Kathy (1994). On the Edge of Darkness. New York: Delta. First-person accountsfrom well-known people who have been through serious depression.Seligman, Martin E. P. (1992). Learned optimism. New York: Simon and Schuster.How to overcome a sense of helplessness in your life.SELF-CARE DEPRESSION PROGRAM54 ANTIDEPRESSANT SKILLS WORKBOOK
SELF-CARE DEPRESSION PROGRAMUSEFUL INFORMATIONAND WORKSHEETS
DIETThe Canada Food GuideGuidelines are per day foradults. The actual amount offood needed depends on yourage, body size, and activitylevel. The guide recommendschoosing low-fat alternativeswhere practical.Grain products:5-12 servings. Examples of aserving: one slice of bread;30g of cold cereal; 3/4 cupof hot cereal; half a bagel;half a cup of pasta or rice.Vegetables and fruit:5-10 servings. One mediumsize vegetable or piece offruit, one cup of salad, halfa cup of juice.Milk products:2-4 servings (more if pregnantor breast-feeding). One cupof milk, 3/4 cup yogurt,50g cheese.Meat and alternatives:2-3 servings. 50-100g meat,poultry, or fish, 1-2 eggs,2/3 cup beans, 1/3 cup tofu,2 tbsp peanut butter.Food is the most obvious source of our energy. When we aredepressed, however, our diet often suffers. Some people overeat.A more common problem is lack of appetite. If this occurs, it isimportant to remember that although you may not feel particularlyhungry, your body’s need for fuel continues. Here are sometips on keeping up adequate nutrition during difficult times.Eat regular meals. It is usually easiest to eat (and to controlwhat you eat) if you keep to a routine. Try to have three setmealtimes per day. Ensure that you have enough food at homefor all three.Eat by the clock, not by your stomach. If you have lostyour appetite, push yourself to eat at mealtimes anyway. If youhave been overeating, try to eat only at mealtimes while sittingat the table.Make it easy. The important thing is to eat, not to cook.Buy foods that are easier to prepare (but keep an eye on theirnutritional value).Make extra. You can cut your preparation time by makinglarger amounts and refrigerating or freezing certain dishesfor reheating later.Make it healthy. Stock up on nutritious food and snacksusing the Canada Food Guide (see the box).Watch your sugar intake. Avoid eating too much refinedsugar. Complex carbohydrates are generally preferable (particularlywhole grain products, brown rice, and potatoes).Avoid dieting. Avoid strict diets, even if you wish to loseweight. It is much better to adopt healthy (rather than restrictive)eating habits and increase your activity level. Ask yourphysician for advice before attempting to lose weight.SELF-CARE DEPRESSION PROGRAM56 ANTIDEPRESSANT SKILLS WORKBOOK
PHYSICAL ACTIVITYRegular physical activity is related to improved mental and physical well-being. Recentresearch indicates that physically fit people are less vulnerable to depression, and thatregular exercise can markedly reduce symptoms of depression for many people.Exercise affects mood in four ways. First, it can produce a brief “runner’s high” just afterexercising in some people (during depression this effect may not occur). Second, after afew weeks of regular exercise (three to four times a week, at least 20 minutes at a time),a general improvement in mood tends to begin. Third, improvements in physical fitnessare associated with improved energy, which can enable you to do more. Finally, exercisecan be a good way of “burning off” stress when you are feeling tense.Here are some tips for developing an exercise program:Get a physical. Before starting, ask your physician about any limitations on your activity.Pick the right activities. The biggest challenge is keeping at it. Pick activitiesthat you really enjoy. Both aerobic (cardiovascular) exercise (in which your heart rateaccelerates into a target range for 20 minutes or more) and anaerobic exercise (such asweight training or yoga) have shown positive effects on mood. Select the type that suitsyou best. Variety also helps: pick more than one activity and alternate them.Stretch and warm up first. Learn how to do stretching exercises properly, thenmake sure to do them before each exercise session. This can help reduce the likelihoodof exercise-related pain or injury.Frequency is more important than duration. Regular short periods of exercise(three to four times a week) are better than irregular long periods.Focus on enjoyment. People who exercise for enjoyment and challenge seem to showbigger mood improvements than people who exercise mainly to look better. Try to put anemphasis on how you will feel rather than how you want to look.Monitor if bipolar. The effect of exercise on bipolar (manic-depressive) mood problemsis less clear than for other forms of depression. Strenuous exercise during a manic episodeor upswing in mood may aggravate the problem in some cases. Gentler exercise at thesetimes may be preferable.Nothing changes overnight. Use goal-setting when developing a fitness program, andbe sure to pick something achievable. For example, aim to swim once for five minutesrather than starting off by committing yourself to a daily 70 laps.SELF-CARE DEPRESSION PROGRAM57 ANTIDEPRESSANT SKILLS WORKBOOK
SLEEPStress, anxiety, and depression often disrupt sleep, but this sleep disruption can lead toeven more anxiety and depression. In other words, sleep difficulties are a cause and aneffect of mood problems. Regardless of which came first, it can be worth the effort towork on getting a good night’s sleep.Here are some tips:Avoid over-the-counter sleeping medication. Although it may help you to fallasleep, the type of sleep you get will usually not be as helpful as normal sleep. Instead,take sleeping medication only as directed by your physician. If you do take sleep medication,remember that the mark of its success is how you feel during the day, not whether it actuallyputs you to sleep. Report the results to your physician.Set a standard bed-time and rising time. Your body operates on a 24-hour cyclethat can be disrupted by going to bed and getting up at different times. This is what causesjet lag: not the air travel, but the change in sleeping hours. Having regular hours for goingto bed and getting up can help to set your internal clock.Don’t go to bed too early. If you never get to sleep before 1 a.m., don’t go to bedbefore 12. Want to get to sleep earlier? Start by setting your bed-time between 30 minutesand an hour before the time you have normally been getting to sleep. Then gradually begingoing to bed earlier (by, say, a half-hour a week).Save your bedroom for sleep. Avoid associating this area with activities that areinconsistent with sleep – like working, eating, arguing, exercising, using the telephone,watching television, and so on. Sex, though, is fine.SELF-CARE DEPRESSION PROGRAM58 ANTIDEPRESSANT SKILLS WORKBOOK
SLEEPCreate a good sleep environment. The best bedroom temperature for mostpeople is 18˚ to 21˚ (65˚F to 70˚F). If noise is a problem, some options include earplugs,soundproofing the room (cloth hangings can help a bit), and devices that emit white noise(e.g., fans or special noise machines). Eliminate hourly watch beepers or clocks that gong.If a restless bed partner is a problem, consider a larger bed, special mattress, or even twinbeds for a time.Avoid napping during the day. Unless, that is, you are a great 20-minute napper.Longer daytime naps can disrupt your ability to get to sleep at night.Prepare for sleep. Avoid strenuous activity, exercise, heavy meals, and bright light forat least one hour before going to bed.Practice breathing or distraction strategies when attempting to get tosleep. Focusing on your worries or on how much you need to get to sleep will only keepyou awake. Practice any mental exercise that takes your mind away from these topics.SELF-CARE DEPRESSION PROGRAM59 ANTIDEPRESSANT SKILLS WORKBOOK
CAFFEINECaffeine stimulates the sympathetic nervous system, which governs the stress response.If your depression comes with a lot of anxiety, the last thing you need is a chemicalthat makes the stress response system more active. Caffeine can also aggravate tensionheadache, irritable bowel syndrome, chronic pain, and other physical problems.Caffeine is an addictive drug. Heavy users can become psychologically dependenton it, develop tolerance (meaning that more caffeine is needed to get the same effects),and undergo withdrawal if they don’t get it. Withdrawal symptoms include headache,drowsiness, irritability, and difficulty concentrating. Many people discover that theyare dependent on caffeine when they go for a day or two without coffee and developsplitting headaches.How much caffeine does it take to become dependent on it? Estimates vary, but450 milligrams per day is about average. Some people are more sensitive, others less.Use the table below to calculate your average daily consumption. Notice the smallserving sizes. Your coffee cup may hold three or four of these!If you decide to try reducing your caffeine intake, do so slowly to avoid the withdrawalsymptoms. Drop your intake by about half for 4-6 days, then half of the remainder, thenhalf again until you are drinking no more than 2 cups per day.Substance Amount in mg # per day TotalCoffeeDrip (5 oz.) 130 x _______ = _______Instant freeze-dried (5 oz.) 70 x _______ = _______Decaffeinated (5 oz.) 3 x _______ = _______Espresso drinks (1 shot) 90 x _______ = _______Tea5-minute steep (5 oz.) 60 x _______ = _______3-minute steep (5 oz.) 35 x _______ = _______OtherHot cocoa (5 oz.) 10 x _______ = _______Regular or diet cola (12 oz.) 45 x _______ = _______Most other soft drinks (12 oz.) 0 x _______ = _______Small chocolate bar 25 x _______ = _______Total = _______SELF-CARE DEPRESSION PROGRAM60 ANTIDEPRESSANT SKILLS WORKBOOK
DRUGS AND ALCOHOLOne of the reasons that depressed people use recreational drugs and drink alcohol is thatthese substances can make them feel better in the short run. But, in the long run, theycan make depression worse:■ Problems are avoided rather than dealt with.■ Performance at work, at home, and in social situations is impaired.■ Psychological and/or physical dependence can develop.■ Physical health can be impaired.During periods of depression, alcohol and drug use may seem particularly tempting. But, atthese times, using such substances is a bad idea. Your tolerance for their effects and yourability to control your use may both be lower than usual. The situation usually requiresconcrete, constructive action rather than a retreat into substance use. As well, drugs andalcohol interact with many prescription medications, including most of the medicationsprescribed for anxiety and depression. In general, then, it is best to follow theseguidelines for a sustaining and sustainable lifestyle:■ Avoid using alcohol or recreational drugs during periods of depression or severe stress.■ Avoid using alcohol or recreational drugs if you have a personal or family historyof substance abuse.■ Even if you are feeling fine and have no history of abuse, adopt a personal policy touse these substances only in moderation.The prospect of eliminating alcohol and drug use from your life can be a daunting one.Remember that while using none is best for some people, reducing your intake is betterthan becoming overwhelmed and giving up. Use the principles of goal-setting to helpyou examine the problem and overcome it a bit at a time.If your use of drugs or alcohol is altogether out of your control, you are in good company:many people have had this problem. A number of organizations exist that can help you toregain control. Ask your physician for more information.SELF-CARE DEPRESSION PROGRAM61 ANTIDEPRESSANT SKILLS WORKBOOK
CHALLENGING DEPRESSIVE THOUGHTSSituation:DEPRESSIVE THOUGHTSREALISTIC THOUGHTS
COMING UP WITH REALISTIC THOUGHTSDepressive Thought:Can I get more evidence, like asking someone about the situation?Would most people agree with this thought? If not, what would be a more realistic thought?We are often much more realistic about other people than about ourselves.What would I say to a friend in a similar situation?What is a less extreme way of looking at the situation?What will happen if I continue to think this way?What is another way of thinking that is more encouraging or useful?
PROBLEM SOLVINGACTION ADVANTAGES DISADVANTAGES1.2.3.
GOAL SETTINGACTIVITY HOW OFTEN? WHEN EXACTLY?
AnxietyDementiaDementiaBipolar155
Practice Support ProgramGeneralized Anxiety Disorder GAD-7GAD-7 Screening QuestionsDuring the last 2 weeks, howoften have you been botheredby the following problems?1 Feeling nervous, anxious, or onedge2 Not being able to stop or controlworrying3 Worrying too much aboutdifferent thingsnot at allseveraldaysmore thanhalf thedaysnearlyevery day0 1 2 30 1 2 30 1 2 34. Trouble relaxing 0 1 2 35. Being so restless that it is hardto sit still6. Becoming easily annoyed orirritable7. Feeling afraid as if somethingawful might happen0 1 2 30 1 2 30 1 2 3Total Score: _______ = Add columns: _____ + _____ + _______If you checked off any problems, how difficult have these problems made it for youto do your work, take care of things at home, or get along with other people?Not difficult Somewhat Very Extremelyat all difficult difficult difficultMar 23, 2009 1 of 2 Mental <strong>Health</strong> Module156
Practice Support ProgramGeneralized Anxiety Disorder GAD-7Scoring and Interpretation of Scores:GAD-7 Anxiety Severity: This is calculated by assigning scores of 0, 1, 2, and 3, to theresponse categories of “not at all,” “several days,” “more than half the days,” and “nearlyevery day,” respectively. GAD-7 total score for the seven items ranges from 0 to 21.Scores of 5, 10, and 15 represent cut points for mild, moderate, and severe anxiety,respectively. Though designed primarily as a screening and severity measure forgeneralized anxiety disorder, the GAD-7 also has moderately good operatingcharacteristics for three other common anxiety disorders – panic disorder, social anxietydisorder, and post-traumatic stress disorder. When screening for individual or any anxietydisorder, a recommended cut point for further evaluation is a score of 10 or greater.Using the threshold score of 10, the GAD-7 has a sensitivity of 89% and a specificity of82% for generalized anxiety disorder. It is moderately good at screening three othercommon anxiety disorders – panic disorder (sensitivity 74%, specificity 81%), socialanxiety disorder (sensitivity 72%, specificity 80%), and post-traumatic stress disorder(sensitivity 66%, specificity 81%).Interpreting Scores5-9 mild anxiety10-14 moderate anxiety (1)15-21 severe anxiety(1)When screening for individual or any anxiety disorder, a recommendedcut point for further evaluation is a score of 10 or greater.Source: Robert L. Spitzer, MD; Kurt Kroenke, MD; Janet B. W. Williams, DSW; Bernd Löwe, MD, PhD A briefmeasure for assessing generalized anxiety disorder. The GAD-7, Arch Intern Med. 2006;166:1092-1097.Mar 23, 2009 2 of 2 Mental <strong>Health</strong> Module157
MONTREAL COGNITIVE ASSESSMENT (MOCA)NAME :Education :Sex :Date of birth :DATE :VISUOSPATIAL / EXECUTIVE5DN A M I N GE AEndB1BeginC423CopycubeDraw CLOCK (Ten past eleven)( 3 points )[ ] [ ] [ ] [ ]Contour Numbers[ ]HandsPOINTS__/5[ ] [ ] [ ]__/3M E M O R YRead list of words, subjectmust repeat them. Do 2 trials.Do a recall after 5 minutes.1st trial2nd trialFACE VELVET CHURCH DAISY REDNopointsATTENTIONRead list of digits (1 digit/ sec.).Subject has to repeat them in the forward order [ ] 2 1 8 5 4Subject has to repeat them in the backward order [ ] 7 4 2__/2Read list of letters. The subject must tap with his hand at each letter A. No points if ≥ 2 errors[ ] F B A C M N A A J K L B A F A K D E A A A J A M O F A A BSerial 7 subtraction starting at 100 [ ] 93 [ ] 86 [ ] 79 [ ] 72 [ ] 65LANGUAGEDELAYED RECALLORIENTATIONRepeat : I only know that John is the one to help today. [ ]The cat always hid under the couch when dogs were in the room. [ ]Fluency / Name maximum number of words in one minute that begin with the letter F [ ] _____ (N ≥ 11 words) __/1ABSTRACTION Similarity between e.g. banana - orange = fruit [ ] train – bicycle [ ] watch - ruler__/2OptionalHas to recall wordsWITH NO CUECategory cueMultiple choice cue[ ] Date [ ] Month [ ] Year [ ] Day [ ] Place [ ] City© Z.Nasreddine MD Version 7.0 www.mocatest.org Normal ≥ 26 / 30Administered by: ___________________________________________________4 or 5 correct subtractions: 3 pts, 2 or 3 correct: 2 pts, 1 correct: 1 pt, 0 correct: 0 ptFACE VELVET CHURCH DAISY RED[ ] [ ] [ ] [ ] [ ]TOTALPoints forUNCUEDrecall onlyAdd 1 point if ≤ 12 yr edu__/1__/3__/2__/5__/6__/30158
Montreal Cognitive Assessment(MoCA)Administration and Scoring InstructionsThe Montreal Cognitive Assessment (MoCA) was designed as a rapid screening instrument for mild cognitivedysfunction. It assesses different cognitive domains: attention and concentration, executive functions,memory, language, visuoconstructional skills, conceptual thinking, calculations, and orientation. Time toadminister the MoCA is approximately 10 minutes. The total possible score is 30 points; a score of 26 orabove is considered normal.1. Alternating Trail Making:Administration: The examiner instructs the subject: "Please draw a line, going from anumber to a letter in ascending order. Begin here [point to (1)] and draw a line from 1 then to Athen to 2 and so on. End here [point to (E)]."Scoring: Allocate one point if the subject successfully draws the following pattern:1 −A- 2- B- 3- C- 4- D- 5- E, without drawing any lines that cross. Any error that is not immediatelyself-corrected earns a score of 0.2. Visuoconstructional Skills (Cube):Administration: The examiner gives the following instructions, pointing to the cube: “Copythis drawing as accurately as you can, in the space below”.Scoring: One point is allocated for a correctly executed drawing.• Drawing must be three-dimensional• All lines are drawn• No line is added• Lines are relatively parallel and their length is similar (rectangular prisms areaccepted)A point is not assigned if any of the above-criteria are not met.3. Visuoconstructional Skills (Clock):Administration: Indicate the right third of the space and give the following instructions:“Draw a clock. Put in all the numbers and set the time to 10 after 11”.Scoring: One point is allocated for each of the following three criteria:• Contour (1 pt.): the clock face must be a circle with only minor distortionacceptable (e.g., slight imperfection on closing the circle);• Numbers (1 pt.): all clock numbers must be present with no additional numbers;numbers must be in the correct order and placed in the approximate quadrants on theclock face; Roman numerals are acceptable; numbers can be placed outside thecircle contour;• Hands (1 pt.): there must be two hands jointly indicating the correct time; the hourhand must be clearly shorter than the minute hand; hands must be centred within theclock face with their junction close to the clock centre.A point is not assigned for a given element if any of the above-criteria are not met.MoCA Version November 12, 2004© Z. Nasreddine MDwww.mocatest.org1159
4. Naming:Administration: Beginning on the left, point to each figure and say: “Tell me the name ofthis animal”.Scoring: One point each is given for the following responses: (1) camel or dromedary, (2)lion, (3) rhinoceros or rhino.5. Memory:Administration: The examiner reads a list of 5 words at a rate of one per second, giving thefollowing instructions: “This is a memory test. I am going to read a list of words that you willhave to remember now and later on. Listen carefully. When I am through, tell me as manywords as you can remember. It doesn’t matter in what order you say them”. Mark a checkin the allocated space for each word the subject produces on this first trial. When the subject indicatesthat (s)he has finished (has recalled all words), or can recall no more words, read the list a secondtime with the following instructions: “I am going to read the same list for a second time. Try toremember and tell me as many words as you can, including words you said the first time.” Put acheck in the allocated space for each word the subject recalls after the second trial.At the end of the second trial, inform the subject that (s)he will be asked to recall these wordsagain by saying, “I will ask you to recall those words again at the end of the test.”Scoring: No points are given for Trials One and Two.6. Attention:Forward Digit Span: Administration: Give the following instruction: “I am going to saysome numbers and when I am through, repeat them to me exactly as I said them”. Read the fivenumber sequence at a rate of one digit per second.Backward Digit Span: Administration: Give the following instruction: “Now I am going tosay some more numbers, but when I am through you must repeat them to me in the backwardsorder.” Read the three number sequence at a rate of one digit per second.Scoring: Allocate one point for each sequence correctly repeated, (N.B.: the correct responsefor the backwards trial is 2-4-7).Vigilance: Administration: The examiner reads the list of letters at a rate of one per second,after giving the following instruction: “I am going to read a sequence of letters. Every time I say theletter A, tap your hand once. If I say a different letter, do not tap your hand”.Scoring: Give one point if there is zero to one errors (an error is a tap on a wrong letter or afailure to tap on letter A).MoCA Version November 12, 2004© Z. Nasreddine MDwww.mocatest.org2160
Serial 7s: Administration: The examiner gives the following instruction: “Now, I will askyou to count by subtracting seven from 100, and then, keep subtracting seven from your answer untilI tell you to stop.” Give this instruction twice if necessary.Scoring: This item is scored out of 3 points. Give no (0) points for no correctsubtractions, 1 point for one correction subtraction, 2 points for two-to-three correct subtractions,and 3 points if the participant successfully makes four or five correct subtractions. Count eachcorrect subtraction of 7 beginning at 100. Each subtraction is evaluated independently; that is, ifthe participant responds with an incorrect number but continues to correctly subtract 7 from it,give a point for each correct subtraction. For example, a participant may respond “92 – 85 – 78 –71 – 64” where the “92” is incorrect, but all subsequent numbers are subtracted correctly. This isone error and the item would be given a score of 3.7. Sentence repetition:Administration: The examiner gives the following instructions: “I am going to read you asentence. Repeat it after me, exactly as I say it [pause]: I only know that John is the one to helptoday.” Following the response, say: “Now I am going to read you another sentence. Repeat it afterme, exactly as I say it [pause]: The cat always hid under the couch when dogs were in the room.”Scoring: Allocate 1 point for each sentence correctly repeated. Repetition must be exact. Bealert for errors that are omissions (e.g., omitting "only", "always") and substitutions/additions (e.g.,"John is the one who helped today;" substituting "hides" for "hid", altering plurals, etc.).8. Verbal fluency:Administration: The examiner gives the following instruction: “Tell me as many words asyou can think of that begin with a certain letter of the alphabet that I will tell you in a moment. Youcan say any kind of word you want, except for proper nouns (like Bob or Boston), numbers, or wordsthat begin with the same sound but have a different suffix, for example, love, lover, loving. I will tellyou to stop after one minute. Are you ready? [Pause] Now, tell me as many words as you can think ofthat begin with the letter F. [time for 60 sec]. Stop.”Scoring: Allocate one point if the subject generates 11 words or more in 60 sec. Record thesubject’s response in the bottom or side margins.9. Abstraction:Administration: The examiner asks the subject to explain what each pair of words has incommon, starting with the example: “Tell me how an orange and a banana are alike”. If the subjectanswers in a concrete manner, then say only one additional time: “Tell me another way in whichthose items are alike”. If the subject does not give the appropriate response (fruit), say, “Yes, andthey are also both fruit.” Do not give any additional instructions or clarification.After the practice trial, say: “Now, tell me how a train and a bicycle are alike”. Followingthe response, administer the second trial, saying: “Now tell me how a ruler and a watch are alike”.Do not give any additional instructions or prompts.MoCA Version November 12, 2004© Z. Nasreddine MDwww.mocatest.org3161
Scoring: Only the last two item pairs are scored. Give 1 point to each item pair correctly answered.The following responses are acceptable:Train-bicycle = means of transportation, means of travelling, you take trips in both;Ruler-watch = measuring instruments, used to measure.The following responses are not acceptable: Train-bicycle = they have wheels; Ruler-watch = theyhave numbers.10. Delayed recall:Administration: The examiner gives the following instruction: “I read some words to youearlier, which I asked you to remember. Tell me as many of those words as you can remember. Makea check mark () for each of the words correctly recalled spontaneously without any cues, in theallocated space.Scoring: Allocate 1 point for each word recalled freely without any cues.Optional:Following the delayed free recall trial, prompt the subject with the semantic category cue providedbelow for any word not recalled. Make a check mark () in the allocated space if the subjectremembered the word with the help of a category or multiple-choice cue. Prompt all non-recalledwords in this manner. If the subject does not recall the word after the category cue, give him/her amultiple choice trial, using the following example instruction, “Which of the following words do youthink it was, NOSE, FACE, or HAND?”Use the following category and/or multiple-choice cues for each word, when appropriate:FACE: category cue: part of the body multiple choice: nose, face, handVELVET: category cue: type of fabric multiple choice: denim, cotton, velvetCHURCH: category cue: type of building multiple choice: church, school, hospitalDAISY: category cue: type of flower multiple choice: rose, daisy, tulipRED: category cue: a colour multiple choice: red, blue, greenScoring: No points are allocated for words recalled with a cue. A cue is used for clinicalinformation purposes only and can give the test interpreter additional information about the type ofmemory disorder. For memory deficits due to retrieval failures, performance can be improved with acue. For memory deficits due to encoding failures, performance does not improve with a cue.11. Orientation:Administration: The examiner gives the following instructions: “Tell me the date today”. Ifthe subject does not give a complete answer, then prompt accordingly by saying: “Tell me the [year,month, exact date, and day of the week].” Then say: “Now, tell me the name of this place, andwhich city it is in.”Scoring: Give one point for each item correctly answered. The subject must tell the exactdate and the exact place (name of hospital, clinic, office). No points are allocated if subject makes anerror of one day for the day and date.TOTAL SCORE: Sum all subscores listed on the right-hand side. Add one point for an individualwho has 12 years or fewer of formal education, for a possible maximum of 30 points. A final totalscore of 26 and above is considered normal.MoCA Version November 12, 2004© Z. Nasreddine MDwww.mocatest.org4162
Appendix CNAME OF PATIENTStandardized Mini-Mental State Examination (SMMSE)DATEDirections for administration of the SSMSE:1. Before the questionnaire is administered, try to get theperson to sit down facing you. Assess the person’s abilityto hear and understand very simple conversation, e.g.What is your name? If the person uses hearing or visualaids, provide these before starting.2. Introduce yourself and try to get the person’s confidence.Before you begin, get the person’s permission to askquestions, e.g. Would it be alright to ask you the samequestions about your memory? This helps to avoidcatastrophic reactions.3. Ask each question a maximum of three times. If thesubject does not respond, score 0.4. If the person answers incorrectly, score 0. Accept thatanswer and do not ask the question again, hint, orprovide any physical clues such as head shaking, etc.5. The following equipment is required to administer theinstrument: A watch, a pencil, Page 3 of this SMMSE withCLOSE YOUR EYES written in large letters and two fivesidedfigures intersecting to make a four-sided figure,and Page 4, a blank piece of paper.6. If the person answers: What did you say?, do not explainor engage in conversation. Merely repeat the samedirections a maximum of three times.7. If the person interrupts (e.g. What is this for?), reply: I willexplain in a few minutes, when we are finished. Now ifwe could proceed please… we are almost finished.I am going to ask you some questions and give you some problems to solve. Please try to answer as best as you can.1. Time: 10 seconds for each reply:a) What year is this? (accept exact answer only).b) What season is this? (accept either: last week of the old season or first week of a new season).c) What month is this? (accept either: the first day of a new month or the last day of the previous month).d) What is today’s date? (accept previous or next date).e) What day of the week is this? (accept exact answer only)./1/1/1/1/12. Time: 10 seconds for each reply:a) What country are we in? (accept exact answer only).b) What province are we in? (accept exact answer only).c) What city/town are we in? (accept exact answer only).d) (In home) What is the street address of this house? (accept street name and house number or equivalentin rural areas).(In facility) What is the name of this building? (accept exact name of institution only).e) (In home) What room are we in? (accept exact answer only).(In facility) What floor of the building are we on? (accept exact answer only)./1/1/1/1/13. Time: 20 secondsSay: I am going to name three objects. When I am finished, I want you to repeat them. Remember what theyare because I am going to ask you to name them again in a few minutes. (Say the following words slowly atapproximately one-second intervals): Ball / Car / Man.For repeated use: Bell, jar, fan; Bill, tar, can; Bull, bar, pan.Please repeat the three items for me. (score one point for each correct reply on the first attempt.)If the person did not repeat all three, repeat until they are learned or up to a maximum of five times(but only score first attempt)./3Cognitive Impairment in the Elderly – Recognition, Diagnosis and ManagementRevised January 30, 2008163
4. Time: 30 secondsSpell the word WORLD. (you may help the person to spell the word correctly) Say: Now spell it backwardsplease. If the subject cannot spell world even with assistance, score 0. Refer to Page 3 for scoring instructions.5. Time: 10 secondsSay: Now what were the three objects I asked you to remember?(score one point for each correct answer regardless of order)6. Time: 10 secondsShow wristwatch. Ask: What is this called?(score one point for correct response: accept “wristwatch” or “watch”; do not accept “clock” or “time”, etc.).7. Time: 10 secondsShow pencil. Ask: What is this called?(score one point for correct response; accept ”pencil” only; score 0 for pen)8. Time: 10 secondsSay: I would like you to repeat a phrase after me: No ifs, ands or buts.Score one point for a correct repetition. Must be exact, e.g. no ifs or buts, score 0).9. Time: 10 secondsSay: Read the words on this page and then do what it says. Then, hand the person the sheet with CLOSE YOUREYES on it. If the subject just reads and does not close eyes, you may repeat: Read the words on this page andthen do what it says (a maximum of three times). Score one point only if the subject closes eyes. The subjectdoes not have to read aloud.10. Time: 30 secondsHand the person a pencil and paper (Page 3). Say: Write any complete sentence on that piece of paper.Score one point. The sentence must make sense. Ignore spelling errors.11. Time: 1 minute maximumPlace design, eraser and pencil in front of the person. Say: Copy this design please. Allow multiple tries. Waituntil the person is finished and hands it back. Score one point for a correctly copied diagram. The person musthave drawn a four-sided figure between two five-sided figures./5/3/1/1/1/1/1/112. Time: 30 secondsAsk the person if he is right or left handed. Take a piece of paper, hold it up in front of the person andsay: Take this paper in your right/left hand (whichever is non-dominant), fold the paper in half once with bothhands and put the paper down on the floor. Score one point for each instruction executed correctly.Takes paper in correct handFolds it in halfPuts it on the floorTotal Test Score:Adjusted Score/1/1/1/30/22Please note: This tool is provided for use in British Columbia with permission by Dr. D. Willam Molloy. This questionnaire should not be further modified orreproduced without the written consent of Dr. D. William Molloy. Molloy DW, Alemayehu E, Roberts R. Reliability of a standardized Mini-Mental State Examinationcompared with the traditional Mini-Mental State Examination. American Journal of Psychiatry,1991;148(1): 102-105.Cognitive Impairment in the Elderly – Recognition, Diagnosis and ManagementRevised January 30, 2008164
Item 11Scoring WORLD backwards (instructions for item #4)Write the person’s response below the correct response.Draw lines matching the same letters in the correct response and the response given.These lines MUST NOT cross each other. Draw only one line per letter.The person’s score is the maximum number of lines that can be drawn without crossing any.Examples:FoldlineD L R O WD L R O W= Score 5D L R O WD R W O D= Score 3D L R O WL O W R O= Score 3D L R O WL= Score 1D L R O WL R R W O= Score 3D L R O W= Score 0Fold along this line and show instructions to personItem 9Close your eyesCognitive Impairment in the Elderly – Recognition, Diagnosis and ManagementRevised January 30, 2008165
Item 10Sentence WritingCognitive Impairment in the Elderly – Recognition, Diagnosis and ManagementRevised January 30, 2008166
Appendix CStandardized Mini Mental State Examination (SMMSE) Cont’dTable 1. Stages of Cognitive Impairment as Defined by SMMSE ScoresSCORE DESCRIPTION STAGE DURATION (Years)30-26 Could be normal Could be normal Varies25-20 Mild Early 0 to 2319-10 Moderate Middle 4-79-0 Severe Late 7-14Table 2. Areas of Functional ImpairmentSMMSE SCORE ACTIVITIES OF DAILY LIVING COMMUNICATION MEMORY30-26 Could be normal Could be normal Could be normal25-20 Driving, finances, shopping Finding words, repeating, Three-item recall,going off topicorientation to time then place19-10 Dressing, grooming, toileting Sentence fragments, vague Spelling WORLD backward,terms (i.e: this, that) language, and three-stepcommand9-0 Eating, walking Speech disturbances such Obvious deficits in all areasas stuttering and slurringAdapted from: Vertesi A, Lever JA, Molloy DW, et al. Standardized mini-mental state examination: Use and interpretation.Canadian Family <strong>Physician</strong> 2001;47:2018-2023.Cognitive Impairment in the Elderly – Recognition, Diagnosis and ManagementRevised January 30, 2008167
THE MOOD DISORDER QUESTIONNAIREInstructions: Please answer each question to the best of your ability.1. Has there ever been a period of time when you were not your usual self and...YES...you felt so good or so hyper that other people thought you were not your " "normal self or you were so hyper that you got into trouble?...you were so irritable that you shouted at people or started fights or arguments? " "...you felt much more self-confident than usual? " "...you got much less sleep than usual and found you didn’t really miss it? " "...you were much more talkative or spoke much faster than usual? " "...thoughts raced through your head or you couldn’t slow your mind down? " "...you were so easily distracted by things around you that you had trouble " "concentrating or staying on track?...you had much more energy than usual? " "...you were much more active or did many more things than usual? " "...you were much more social or outgoing than usual, for example, you " "telephoned friends in the middle of the night?...you were much more interested in sex than usual? " "...you did things that were unusual for you or that other people might have " "thought were excessive, foolish, or risky?...spending money got you or your family into trouble? " "2. If you checked YES to more than one of the above, have several of these " "ever happened during the same period of time?3. How much of a problem did any of these cause you – like being unable towork; having family, money or legal troubles; getting into arguments or fights?Please circle one response only.No Problem Minor Problem Moderate Problem Serious Problem4. Have any of your blood relatives (i.e. children, siblings, parents, grandparents, " "aunts, uncles) had manic-depressive illness or bipolar disorder?5. Has a health professional ever told you that you have manic-depressive illness " "or bipolar disorder?NO© 2000 by The University of Texas Medical Branch. Reprinted with permission. This instrument is designed for screening purposes only and is not to be used as a diagnostic tool.168
SCORING THE MOOD DISORDERQUESTIONNAIRE (MDQ)The MDQ was developed by a team of psychiatrists, researchers and consumer advocates to addressa critical need for timely and accurate diagnosis of bipolar disorder, which can be fatal if left untreated.The questionnaire takes about five minutes to complete, and can provide important insights intodiagnosis and treatment. Clinical trials have indicated that the MDQ has a high rate of accuracy; it isable to identify seven out of ten people who have bipolar disorder and screen out nine out of tenpeople who do not. 1A recent National DMDA survey revealed that nearly 70% of people with bipolar disorder had receivedat least one misdiagnosis and many had waited more than 10 years from the onset of their symptomsbefore receiving a correct diagnosis. National DMDA hopes that the MDQ will shorten this delay andhelp more people to get the treatment they need, when they need it.The MDQ screens for Bipolar Spectrum Disorder, (which includes Bipolar I, Bipolar II andBipolar NOS).If the patient answers:1. “Yes” to seven or more of the 13 items in question number 1;AND2. “Yes” to question number 2;AND3. “Moderate” or “Serious” to question number 3;you have a positive screen. All three of the criteria above should be met. A positive screen shouldbe followed by a comprehensive medical evaluation for Bipolar Spectrum Disorder.ACKNOWLEDGEMENT: This instrument was developed by a committee composed of the following individuals: Chairman,Robert M.A. Hirschfeld, MD – University of Texas Medical Branch; Joseph R. Calabrese, MD – Case Western Reserve Schoolof Medicine; Laurie Flynn – National Alliance for the Mentally Ill; Paul E. Keck, Jr., MD – University of Cincinnati College ofMedicine; Lydia Lewis – National Depressive and Manic-Depressive Association; Robert M. Post, MD – National Institute ofMental <strong>Health</strong>; Gary S. Sachs, MD – Harvard University School of Medicine; Robert L. Spitzer, MD – Columbia University;Janet Williams, DSW – Columbia University and John M. Zajecka, MD – Rush Presbyterian-St. Luke’s Medical Center.1 Hirschfeld, Robert M.A., M.D., Janet B.W. Williams, D.S.W., Robert L. Spitzer, M.D., Joseph R. Calabrese, M.D., Laurie Flynn, Paul E. Keck, Jr., M.D.,Lydia Lewis, Susan L. McElroy, M.D., Robert M. Post, M.D., Daniel J. Rapport, M.D., James M. Russell, M.D., Gary S. Sachs, M.D., John Zajecka, M.D.,“Development and Validation of a Screening Instrument for Bipolar Spectrum Disorder: The Mood Disorder Questionnaire.” American Journal ofPsychiatry 157:11 (November 2000) 1873-1875.169
Practice Support ProgramGlobal Assessment of Functioning (GAF)The Global Assessment of Functioning (GAF) is a numeric scale (0 through 100) used by mentalhealth clinicians and physicians to subjectively rate the social, occupational and psychologicalfunctioning of adults, e.g., how well or adaptively one is meeting various problems-in-living. Itexcludes physical and environmental impairment. The scale is presented and described in theDSM-IV-TR on page 32. Children and adolescents under the age of 18 are evaluated on theChildren's Global Assessment Scale, or C-GAS.CodeDescription of Functioning91 - 100 Superior functioning in a wide range of activities, life’s problems never seem to get out ofhand, is sought out by others because of his/her many positive qualities. No symptoms.81 - 90 Absent of minimal symptoms, good functioning in all areas, interested and involved in a widerange of activities. Socially effective, generally satisfied with life, no more than everydayproblems or concerns (e.g., an occasional argument with family members).71 - 80 If symptoms are present, they are transient and expectable reactions to psycho-socialstressors (e.g., difficulty concentrating after family argument); no more than slight impairmentin social, occupational, or school functioning (e.g., temporarily falling behind in schoolwork).61 - 70 Some mild symptoms (e.g., depressed mood and mild insomnia) or some difficulty in social,occupational, or school functioning (e.g., occasional truancy, or theft within the household),but generally functioning pretty well, has some meaningful relationships.51 - 60 Moderate symptoms (e.g., flat affected speech, some panic attacks) or moderate difficulty insocial, occupational, or school functioning (e.g., few friends, conflicts with or co-workers).41 - 50 Serious symptoms (e.g., suicidal ideation, obsessional rituals, frequent shoplifting) or anyserious impairment in social, occupational, or school functioning (e.g., unable to keep a job).31 - 40 Some impairment in reality testing (e.g., speech is at times illogical, obscure, or irrelevant) ormajor impairment in several areas, such as work or school, family relations, judgment,thinking, or mood (e.g., depressed man avoids friends, neglects family, and is unable to work;child frequently beats up younger children, is defiant at home, and is failing at school).21 - 30 Behavior is considerably influenced by delusions or hallucinations or serious impairment incommunication or judgment (e.g., sometimes incoherent, acts grossly inappropriately, suicidalpreoccupation) or inability to function in almost all areas (e.g., stays in bed all day; no job,home or friends).11 - 20 Some danger of harm to self or others (e.g., suicidal attempts without clear expectation ofdeath; frequently violent; manic excitement) or occasionally fails to maintain minimum personalhygiene (e.g., smears feces) or gross impairment in communication (e.g., largely incoherent ormute).1 - 10 Persistent danger of severely hurting self or others (e.g., recurrent violence) or persistentinability to maintain personal hygiene or serious suicidal act with clear expectation of death.Note: This version of the GAF scale is intended for academic use only. Although it is based on the clinicalscale presented in the DSM – IV TR, this summary lacks the detail and specificity of the original document.The complete GAF scale on page 32 of the DSM - IV TR, should be consulted for clinical use.Mar 23, 2009Mental <strong>Health</strong> Module170
FORM 4MENTAL HEALTH ACT[ Sections 22, 28, 29 and 42,R.S.B.C. 1996, c. 288 ]MEDICAL CERTIFICATE(INVOLUNTARY ADMISSION)I, , M.D., certify that I examinedphysician’s name (please print)first and last name of person examined (please print)on .dd / mm / yyyyIn summary form, the reasons for my opinion are: (information maybe obtained through interviews, observations and collateral sources)1. In my opinion, this person:has a disorder of the mind that requirestreatment and which seriously impairsthe person’s ability to react appropriatelyto his/her environment or to associatewith others (section 1 of the Mental<strong>Health</strong> Act);2. In my opinion, this person:(a) requires treatment in or through adesignated facility; and(b) requires care, supervision andcontrol in or through a designatedfacility to prevent his/her substantialmental or physical deterioration orfor the protection of the person orfor the protection of others; and(c) cannot suitably be admitted as avoluntary patient.This person was was notbrought to me by a police officer orconstable under section 28 of the Act.Note: if above space is insufficient, continue on back of formSignedphysician’s signaturedate of signature (dd / mm / yyyy)physician’s address (please print)telephoneNote: This medical certificate, when duly signed, is authority for anyone to apprehend the person who is the subject of this certificate and totransport the person to a designated facility for admission and detention for a 48 hour period. If a second medical certificate is completedwithin that period, it provides authority to detain the person for one month from the date of admission under the first certificate.If this is a first medical certificate, it becomes invalid on the 15th day after the date upon which the physician examined the person who isthe subject of the certificate unless the person has been admitted on the basis of it.HLTH 3504 Rev. 2005/06/01 (PINK)110
Referral Formsfor GPsMental <strong>Health</strong> &Substance UseServices GuideMetabolicMonitoringMental <strong>Health</strong>Fees SummaryInformationAdditionalResources
CommunityMHSU ReferralFormBounceBackProgram ReferralCRESST/Afterhours/Car 67Referral FormEating DisordersProgramReferralsSubstance UseServicesNeuropsychAssessmentServicesEarly PsychosisInterventionReferralsBC PharmacarePlan G FormBC PharmacareSpecial <strong>Authority</strong>Form
REFERRAL FORM: Community Mental<strong>Health</strong> and Substance Use Services*MHXX*MHXX104521BA. REFERRAL SOURCERev: Mar 28/11Page: 1 of 2REFERRAL DATE(DD/MM/YY)DATE RECEIVEDAT MHC (DD/MM/YY)REFERRAL TIME(24 hr clock)TIME REFERRALRECEIVED (24 hr)REFERRAL SOURCE(i.e. self, program/site)REFERRAL MADE NAME ROLEPHONE #BY(incl. ext.)REFERRALRECEIVED BYB. CLIENT INFORMATIONNAMEADDRESSGENDERABORIGINAL IDENTITYALIAS(if any)NO FIXED PHNADDRESS DOBHOMELESS (DD/MM/YY)CITY PROVINCE POSTAL CODEPHONE NUMBER HOMENO PHONENUMBERNEXT OF KINMALE FEMALE UNKNOWN / UNDIFFERENTIATEDABORIGINALNON-ABORIGINALUNKNOWN / NOT ASKEDCAN WE LEAVE A MESSAGE AT THIS NUMBER?OTHER CAN WE LEAVE A MESSAGE AT THIS NUMBER? YES NONAMERELATIONSHIPPHONE CAN WE LEAVE A MESSAGE AT THIS NUMBER? YES NOALTERNATECONTACTNAME RELATIONSHIPSAME AS NEXT OFKINPHONE CAN WE LEAVE A MESSAGE AT THIS NUMBER? YES NOGENERALPRACTITIONERPHONEFAXYESNONO GENERAL PRACTITIONERDURING HOSPITALIZATION ONLYPrint Shop # 261974PSYCHIATRISTPHONEC. REASON FOR REFERRALREASON FOR REFERRAL:FAXNO PSYCHIATRISTDURING HOSPITALIZATION ONLYSERVICES REQUESTED / DESIRED OUTCOME:CURRENT DIAGNOSES (IF KNOWN, PSYCHIATRIC AND MEDICAL):
REFERRAL FORMMental <strong>Health</strong> and Substance Use ServicesCont'dPage: 2 of 2D. PREVIOUS CONTACTSPREVIOUS CONTACTS WITH HOSPITAL, COMMUNITY MENTALHEALTH AND ADDICTIONS OR FORENSIC SERVICES?HOSPITALMOSTCOMMUNITY MHARECENTCONTACTSSERVICES. FORENSICSERVICESNO YES UNKNOWNIF REFERRAL FROM HOSPITAL, ACTUAL OR EXPECTED DISCHARGE DATE (DD/MM/YY)DATE (DD/MM/YY)DATE (DD/MM/YY)DATE (DD/MM/YY)EXTENDED LEAVENOYES - CERTIFICATE EXPIRY DATE (DD/MM/YY)TO BE COMPLETED WHEN REFERRAL IS MADE FROM HOSPITALS OR OTHER HEALTHCARE PROVIDERSE. MEDICATION AND ALLERGY INFORMATIONCURRENT MEDICATIONS or MAR and/or CURRENT PRESCRIPTIONS and/or PHARMANET PROFILE ATTACHED(including known OTCs, herbals and vitamins)LONG-ACTING NAME DOSAGE FREQUENCYINJECTIBLEMEDICATION WHEN LAST GIVEN (DD/MM/YY) WHEN NEXT DUE (DD/MM/YY)MEDICATION COVERAGE SELF PLAN G OTHER:ALLERGIESALLERGY PROFILE ATTACHEDFOR OFFICE USE ONLY. THIS SECTION TO BE COMPLETED BY MHSU CLINICIANF. MENTAL HEALTH CENTRE FOLLOW UP1st ATTEMPT DATE CONTACT CONTACT NO IF NO REASON:TO CONTACT (D/M/Y) MADE BY SUCCESSFUL YES2nd ATTEMPT CONTACT CONTACT NO IF NO REASON:DATETO CONTACT MADE BY SUCCESSFUL YES3rd ATTEMPT CONTACT CONTACT NO IF NO REASON:DATETO CONTACT MADE BY SUCCESSFUL YESFOLLOW UP DATE LETTER CONTACT NO IF NO REASON:LETTER SENT SENT SENT BY SUCCESSFUL YESINITIAL SCREENINGINTAKEINTAKEDATE (DD/MM/YY) CLINICIAN SIGNATUREFILE OPENEDFILE NOT OPENED / CANCELLEDOPEN DATE(DD/MM/YY)1st APPOINTMENT(IF APPLICABLE)REVIEW DATE(DD/MM/YY)DATE(DD/MM/YY)REASON(S)NOT OPENED
CRESST/AFTERHOURS/CAR 67 Referral:Click here for CRESST Referral FormMHAH can be called directly at 1-877-384-8062 by anyonein need of a crisis.Car 67 services are generated through the RCMP bycalling the RCMP first. The Car 67 phone number is notlisted and only given to MH professionals. A GP cannotcall the Car 67 directly. If there is an open case file thetherapist can call the Car or send a referral.CRESST services are emergency psychiatric facilitiesproviding support for clients experiencing a mental healthcrisis. CRESST endeavours to prevent unnecessaryhospitalizations and maintain client autonomy in a safe,supportive, and supervised setting. Clients stay at thefacility voluntarily. Access to these facilities located inAbbotsford, Surrey, and New Westminster is throughMental <strong>Health</strong> Centre case managers, psychiatrists,Emergency Mental <strong>Health</strong> Services and physicians.
MENTAL HEALTH AFTER HOURSPLEASE LEAVE VOICE MAIL TO INDICATETHAT THE REFERRAL HAS BEEN FAXEDPhone: 1-877-384-8062Fax: 604-587-4227CAR 67 (Surrey Only)Phone: 604.599.0502(RCMP Non Emerg)Emergencies 911 Request for Service Alert/Information Only Follow-UpREFERRAL FORMMental <strong>Health</strong> ServicesCRESST (Surrey)13525 – 98 th Ave., Surrey, BC V3T 1B9Phone: 604.587.4220 Fax: 604.587.4227CRESST (New West)220 Sherbrooke St., N. West, BC V3L 3M2Phone: 604.521.1205 Fax: 604.521.2619CRESST (Abbotsford)33720 McDougall Ave., Abbots., V2S 1W4Phone: 604.870.7583 Fax: 604.852.7102Date Referred: Time: Person & Place Referring: Referring Agency Phone Number:Date of Last Face-to-Face Contact:Client Name: Alias(es): DOB (yy/mm/dd) Sex M FAddress: City: Postal Code: Phone(s) #:Call Blocking: Y NPHN: Next of Kin/Relationship: Phone #:Family <strong>Physician</strong>:Phone:Psychiatrist:Phone:Mental <strong>Health</strong> Centre: Mental <strong>Health</strong> Therapist: Phone:Diaoses:Axis I:Axis II:Axis III:Axis IV: Axis V:For MHAH & Car 67 Only: Last MHC Visit:Next Scheduled Visit:Last Hospitalization:BEHAVIOURSSubstance Misuse: Current Y N History Y NSubstance Used Date Last Used Amount Used FrequencyCurrently Suicidal Y N Plan/Means:Last Suicide Attempt (yy/mm/dd)Details of History of Suicide Attempts:Aggression: Current Aggression? Y N Hx of Violence /Aggression Y NDetails of History of Aggression:(include weapons and method)Date of Last Incident: Does the Client Have a weapon? Unknown Y NFire Setting: Y N Date of Last Incident: Type:Sexual Issues: Y N Date of Last Incident: Type:Legal Issues: Y N Date of Last Incident: Type:07/09 C:\Users\Bruce\Documents\MD-DOC\PSP\Mental <strong>Health</strong>\<strong>Fraser</strong> Valley\Cresst referral.doc1
MEDICAL/PHYSICAL/PSYCHIATRIC:Current Mental State (include auditory hallucinations, delusions, paranoid, etc.)Details of Current Problems:Medical/Physical Problems::Diet: (for CRESST)Medication Coverage:ID Number: Plan G Regular Income Assistance PWD* PWMB** Veteran Affairs Aboriginal Status Extended Medical SelfInjection: Yes No Date Last Given:Name, Dose, Frequency:Medications:Allergies/Adverse Effects (medication, environment, food)Has there been Recent Change to Meds?: Yes No Is the Individual Med Compliant? Yes NoNot Applicable to CRESSTCertified: Y NOn Extended LeaveCertified: Y NOriginal Certificate(s) sent to:Copies of Extended Leave sent to:SPECIFIC INSTRUCTIONS/REQUESTS (use extra sheet if necessary, but be sure to fax ALL information)Placement Plan: (Where will the client go from CRESST?)FOR CRESST: A two (2) week prescription for all medical, psychiatric and over the counter medication, including smokingcessation aids if applicable, is required (i.e. new Rx, written or phoned into CRESST).* PWD = Person with Disability** PWMB = Person with Multiple Barriers07/09 C:\Users\Bruce\Documents\MD-DOC\PSP\Mental <strong>Health</strong>\<strong>Fraser</strong> Valley\Cresst referral.doc2
DOCUMENTATION REQUIRED UPON REFERRAL TO CRESSTMental <strong>Health</strong> Centre Teams, <strong>Physician</strong>s and Psychiatrists Completed CRESST Referral Form & Written prescription (medical/psychiatric/verbal order/ transfer prescription from client’s own pharmacy to facilitypharmacy). Most recent note from primary therapist. Most recent note from psychiatrist. Any consult reports/notes. Extended leave documentation.Hospital Emergency Departments Completed CRESST referral form & Written prescription (medical/psychiatric/verbal order/ transfer prescription from client’s own pharmacy to facilitypharmacy. Psychiatric emergency nurse’s completed assessment. Any consultant reports/notes. Laboratory results of blood work or other relevant test results by the referring hospital.Inpatient Units of General Hospital Completed CRESST referral form & Initial psychiatric nursing assessment. Nursing notes of the client’s last two days in hospital. Psychiatrist’s consultation notes/report. Laboratory results of blood work or other relevant test results performed by the referring hospital. Written medical and psychiatric prescription (minimum 2 week medication for clients with no PHN or prescriptioncoverage). Special Authorization to be completed and processed. Medication authorization forms completed and processed for those not covered by MSP. Social Work notes including relevant reports and documentation of processed forms for clients referred to CRPprograms, or any referrals already made for clients being considered for CRP. Extended leave documentation. Other relevant assessments (i.e. O.T. assessments, etc.)07/09 C:\Users\Bruce\Documents\MD-DOC\PSP\Mental <strong>Health</strong>\<strong>Fraser</strong> Valley\Cresst referral.doc3
Eating Disorders Programs in FH:<strong>Fraser</strong> North:Community Referral FormEating Disorders Brochure<strong>Fraser</strong> South:Adult Adult Referral Referral Form FormChild and & Youth Referral Form<strong>Fraser</strong> East:Telephone: 604 870 7800Fax: 604 870 7801Kelley Fitzpatrick, MSWEating Disorder TherapistAbbotsford Mental <strong>Health</strong>This program is part of the <strong>Fraser</strong> East but we are not a co-located program. I provide bothindividual and group therapy as well as case management for these clients. Typically there isonly one group running at a time as there is only one of me. Clients are also able to access anout-patient dietician who is based at Abbotsford Regional Hospital.Clients who see me are required to have regular follow-up with their family physicians formedical monitoring. Because of this, it is preferrable that they are referred by their G.P. I doalso accept self-referrrals. There is no referral form. G.P.'s simply fax our office the relevantinfo.This includes:1. Client demographics- name, address, phone numbers, PHN etc.2. Eating Disorder Diagnosis and any other relevant diagnoses3. Information pertaining to current symptoms and onset, medications, weight if available4. Follow-up plan with G.P. - i.e. medical monitoring 5. Any bloodwork or other relevant tests ifavailableThey can also phone and have our clerical staff will take down all of the information. Once thereferral is complete, I will then contact the client to complete a telephone screening and tellthem more about our services.
Adult Eating Disorders ProgramReferrals to: Tri-Cities Mental <strong>Health</strong>Centre#1—2232 Elgin AvenuePort Coquitlam, B.C., V3C 2B2Tel (604) 777-8400 Fax (604) 777-8411www.fraserhealth.caDate:NEW CLIENT REFERRAL<strong>Fraser</strong> North Eating Disorders ProgramReferral Criteria:The Eating Disorder Program services clients with eating disorders as outlined in the DSM IV. The client will have:a) An intense preoccupation and concerns with body shape and sizeANDb) Significant low weight or weight loss due to voluntary restricting of food intake (i.e. 15% of baseline normal weight).ORc) Binge eating more than two times per week for three months accompanied by feeling out of control (i.e. can’t stop binge orcontrol how much is eaten) and purging behaviour (i.e. vomiting, laxatives, post-binge fasting, excessive exercise…).Exclusion criteria:The EDP does not provide services in the following instances:1. The patient is under 19 years of age.2. Alcohol or substance abuse is the primary presenting problem.3. The client does not have a General Practitioner/Primary Family <strong>Physician</strong>. Given our limited resources, the EDP can not be asubstitute for a client’s General Practitioner. As such referrals of individuals who do not have a family physician can not beaccepted.4. The client is acutely suicidal or in crisis.5. Acute psychiatric disorders account for decreased food intake such as: Thought Disorders (e.g. someone with schizophrenia who has delusions around food). Major Depression or Post Partum Depression where decreased food intake is due to mood.6. Binge eating disorder (i.e. binge eating without any compensatory behaviour).7. The client is not a resident of the <strong>Fraser</strong> North <strong>Health</strong> Area.Referral Source: (Family <strong>Physician</strong>)Name:Office Phone:Address:Office Fax:Client Information – Please complete:Client’s Surname:Client’s First Name:Current Address (include postal code):Gender:MDOB: (mm/dd/yy)FHome Phone # Work Phone #PHN:1
Current Height:Lowest Wt:Highest Wt:Client’s desired weight:Current Wt:Age:Age:/ /Date obtained: (mm/dd/yyyy)Vital SignsTemp ______________ Resp _____________________Pulse Sitting _______________________BP Lying __________________________Pulse Standing ______________________BP Standing ________________________Eating Disorder Related Behaviours:Restricting: Yes No History of RestrictingDaily intake: less than 1 meal/day 1 meal/day 2 meals per day or morePurging: (over the past 3 months)Vomiting Yes No Frequency: daily 2-3x / week less than once / weekHistory of purging, if not purging currently Yes NoExercise – hours per week 0-3 4-10 10-15 15-20 20-30 30 +Laxatives: Yes No History of Laxative AbuseType(s) used:Frequency / number per day: 1 to 10 10 to 20 more than 20Other Purging Methods:Diuretics Thyroid Medications IpecacAppetite Suppressants Insulin manipulation Other _______________________Binge Eating (Objectively large amount of food within any 2 hour period; experience loss of control)Yes No Frequency: daily weekly monthly2
Medical History:Medical causes of low weight or vomiting ruled out? Yes NoAmenorrhea Yes No LMPHistory of Amenorrhea Yes NoBCP Yes NoPregnant Yes No Week of Pregnancy at Referral:Diabetes: (insulin dependent) Yes NoGI Disorders (i.e. Crohn’s, Celiac Disease): Yes NoAllergies:Other medical conditions:Current Medications (Please list with dosage):Psychiatric History:Please describe any psychiatric symptoms of concern, or current diagnoses:Suicidal Ideation Yes NoDescribe:Self Harm Yes NoDescribe:Substance/Alcohol Abuse Yes NoWhich substances?tobaccomethamphetaminealcoholprescription medscannabisother, please describecocaineTreatment received?:3
Current Treatment for ED /Psychiatric concerns? Yes NoPast Treatment for ED /Psychiatric concerns? Yes NoIf “yes”, please indicate who else is/was providing services for this clientPsychiatristMental <strong>Health</strong> ClinicianPsychologistSt. Paul’s Hospital ED programBC Children’s Hospital ED Program Other: ________________________Lab Work – A current (within 2 months) copy of the following is required:1) ECG2) Full blood biochemistry including all of the below:- CBC and Diff - Serum Phosphate, Magnesium, Zinc- Ferritin, B12 - BUN, Creatinine- Random Blood Sugar - Na, Cl, K, Bicarb- TSH - Serum Protein- ALT, AST, Alk Phos, Bilirubin3) Microscopic Urinalysis to include Specific Gravity.PLEASE REMEMBER TO INCLUDE: (1) all relevant tests (i.e. blood work and ECG),(2) symptoms and frequency,(3) current height and weight,(4) highest and lowest weights, and(5) GP contact info as you will be providing on-goingmedical care for this patient.Please advise your patient that we have a waiting list of at least several months and that she/he will not be put on ourwaiting list until the referral process has been completed. This process includes your completed referral form, blood work,and an ECG. Once on the list, we will invite the patient for an Orientation Session.__________________________________Doctor’s Name & Signature______________________________DateIf you have any questions re completing the referral, please call us at 604-777-8400 and ask for Intake.05/05/094
Who Are We?This is a specialized program operating withinMental <strong>Health</strong> Services and supported by<strong>Fraser</strong> <strong>Health</strong> <strong>Authority</strong> and the Ministry ofChildren and Family Development.Our services are provided to adults and youthon an out-patient basis. We are committedto serving our clients in a timely manner. Inthe adult program we have introduced anumber of groups to facilitate services to allthose who are referred. In addition to thesegroups, adult clients who are committed tomaking behavioural changes will be offeredservices which may include individual therapy,medical, nutritional, family support andgroups. Child and youth clients are offeredindividual therapy, medical, nutritional andfamily support.Our team strives to create a supportive andsafe environment. We believe that ourpractice must be guided by the needs of ourclients – who are active participants in theirtreatment.We are a community based out-patientprogram. Severely ill individuals may bereferred to their local Community Hospitaland/or Provincial treatment facilities at St.Paul’s Hospital or BC Children’s Hospital.We serve the communities of Burnaby, NewWestminster, Pitt Meadows, Maple Ridge andthe Tri Cities area.<strong>Fraser</strong> North EatingDisorders ProgramFor Inquiries and Referral InformationPlease contact the Program<strong>Fraser</strong> North Eating DisorderProgram#303-3003 St Johns StreetPort Moody BC V3H 2C4Child & Youth Eating DisorderProgram 604 469-7600Adult Eating Disorder Program604 777-8400<strong>Fraser</strong> NorthEatingDisordersProgramProviding a continuumof services to both youthand adult clients andtheir families who aredealing with anorexianervosa and bulimianervosa.“We believe that treatment is bestdelivered by a group of diversehealthcare professionals with specifictraining, competence and experience inthe area of eating disorders.”
Referral <strong>Process</strong>All clients referred into the program arerequired to have their family physiciancomplete a detailed referral including currentlab data and attend an orientation night.Appropriate referrals will be assessed by ourteam. On the basis of that assessment, andin conjunction with the client, an initialtreatment plan will be recommended; followup care will be re-evaluated on an ongoingbasis. Clients will be required to attendgroups.Services OfferedThe <strong>Fraser</strong> North Eating Disorder Programprovides a continuum of services thatmay include:Individual TherapyGroup TherapyFamily TherapyMedical and Nutritional supportTreatment is led by qualified healthprofessionals specializing in eating disordertreatment.Adult Groups OfferedOrientation NightIndividuals referred to the EDP will be notifiedof the upcoming orientation date. Orientationprovides an overview of the program andintroduction to the ED team. Initialassessments are also booked at this time. Ifenrolled in the program, clients may participatein the following groups:1) Educational Support Group: This groupoffers participants an opportunity to explorethe function of the eating disorder in theirlives, their thoughts and feelings aboutrecovery, and the change process. Participantsare also offered nutritional and medicalinformation.2) Coping Skills Group: This group offersparticipants an opportunity to learn healthycoping skills such as mindfulness meditation,distress tolerance, emotion regulation, andinterpersonal effectiveness, and explore waysthese skills may aid in their recovery.3) Cognitive Behavioral Therapy (CBT)Group: This group is offered to clients who areready and motivated for change, and activelyengaged in their recovery. Participants arerequired to set behavioural goals, practice selfmonitoring,keep thought records, identifythinking traps, and challenge negativethoughts.4) Bridging Group: This weekly supportgroup is offered to clients when they are notengaged in any other EDP group.Child & Youth EatingDisorder Program*all groups are 8 weeks in duration
<strong>Fraser</strong> South Eating Disorders Program#129 – 6345 120 th StreetDelta, BC V4E 2A6Phone:Date:604.592.3700 Fax: 604.591.2302NEW CLIENT REFERRALAdult Program - <strong>Fraser</strong> South Eating Disorders ProgramReferral Criteria:The Eating Disorder Program services clients with eating disorders as outlined in the DSM IV. The client will have:a) An intense preoccupation and concerns with body shape and sizeANDb) Significant low weight or weight loss due to voluntary restricting of food intake (i.e. 15% of baselinenormal weight).ORc) Binge eating more than two times per week for three months accompanied by feeling out of control (i.e.can’t stop binge or control how much is eaten) and purging behaviour (i.e. vomiting, laxatives, post-bingefasting, excessive exercise…).Exclusion criteria: The EDP does not provide services in the following instances:1. Alcohol or substance abuse is the primary presenting problem.2. The client does not have a General Practitioner. Given our limited resources, the EDP can not be asubstitute for a client’s General Practitioner. As such referrals of individuals who do not have a familyphysician can not be accepted.3. The client is acutely suicidal or in crisis.4. Acute psychiatric disorders that account for decreased food intake such as: Thought Disorders (e.g. someone with schizophrenia who has delusions around food). Major Depression or Post Partum Depression where decreased food intake is due to mood.5. Binge eating disorder (i.e. binge eating without any compensatory behaviour).6. The client is not a resident of <strong>Fraser</strong> South <strong>Health</strong> Area.Referral Source: (Must Be A Family <strong>Physician</strong>)Name:Office Phone:Office Fax:Address:Client Information – Please complete:Client’s Surname:Client’s First Name:Gender:MFDOB: (yyyy/mm/dd)Current Address (include postal code):Home Phone # Work Phone #Contact Name (Next of Kin) Home Phone #Work Phone #Relationship to patient:PHN:Program:Adult1
Current Height:Lowest Wt:Highest Wt:Client’s desired weight:Current Wt:Age:Age:/ /Date obtained: (yyyy/mm/dd)Vital SignsTemp ______________ Resp _____________________Pulse Sitting _______________________BP Lying __________________________Pulse Standing ______________________BP Standing ________________________Eating Disorder Related Behaviours:Restricting: Yes No History of RestrictingDaily intake: less than 1 meal/day 1 meal/day 2 meals per day or morePurging: (over the past 3 months)Vomiting Yes No Frequency: daily 2-3x / week less than once / weekHistory of purging, if not purging currently Yes NoExercise – hours per week 0-3 4-10 10-15 15-20 20-30 30 +Laxatives: Yes No History of Laxative AbuseType(s) used:Frequency / number per day: 1 to 10 10 to 20 more than 20Other Purging Methods:Diuretics Thyroid Medications IpecacAppetite Suppressants Insulin manipulation Other _______________________Binge Eating (Objectively large amount of food within any 2 hour period)Yes No Frequency: daily weekly monthly2
Medical History:Medical causes of low weight or vomiting ruled out? Yes NoAmenorrhea Yes No LMPHistory of Amenorrhea Yes NoBCP Yes NoPregnant Yes No Week of Pregnancy at Referral:Diabetes: (insulin dependent) Yes NoGI Disorders (i.e. Crohn’s, Celiac Disease): Yes NoAllergies:Other medical conditions:Current Medications (Please list with dosage):Psychiatric History:Please describe any psychiatric symptoms of concern, or current diagnoses:Suicidal Ideation Yes NoDescribe:Self Harm Yes NoDescribe:Substance/Alcohol Abuse Yes NoWhich substances?Treatment:3
Current Treatment for ED /Psychiatric concerns? Yes NoPast Treatment for ED /Psychiatric concerns? Yes NoIf “yes”, please indicate who else is/was providing services for this clientPsychiatristMental <strong>Health</strong> ClinicianPsychologistSt. Paul’s Hospital ED programBC Children’s Hospital ED Program Other: ________________________Working ED Diagnosis:Anorexia Nervosa, Restricting typeAnorexia Nervosa,Binge-eating/Purging typeBulimia Nervosa, Purging typeBulimia Nervosa, Non-purging typeEating Disorder Not Otherwise SpecifiedLab Work – A current (within 2 months) copy of the following is required:1) ECG2) Full blood biochemistry including all of the below:- CBC and Diff - Serum Phosphate, Magnesium, Zinc- Ferritin - BUN, Creatinine- Random Blood Sugar - Na, Cl, K, Bicarb- TSH - Serum Protein- ALT, AST, Alk Phos, Bilirubin3) Microscopic Urinalysis to include Specific Gravity.PLEASE REMEMBER TO INCLUDE: (1) all relevant tests (ie, blood work and ECG),(2) symptoms and frequency,(3) current height and weight,(4) highest and lowest weights, and(5) GP contact info as you will be providing on-goingmedical care for this patient.Please advise your patient that she/he will not be put on our waiting list until the referral process has beencompleted. This process includes your completed referral form, blood work, an ECG and the patient’sattendance of an Information Session. Once on the list the patient will be invited for an assessmentappointment.__________________________________Doctor’s Signature______________________________DateIf you have any questions re completing the referral, please call us at 604 592-3700 14/12/094
<strong>Fraser</strong> South Eating Disorders Programc/o Child and Youth Mental <strong>Health</strong> (CYMH)Surrey North Intake Officeph 604.951.5844 fax: 604.951.5917Date:NEW CHILD & YOUTH CLIENT REFERRAL<strong>Fraser</strong> South Eating Disorders ProgramReferral Criteria:The Eating Disorder Program services clients with eating disorders as outlined in the DSM IV. The client will have:a) An intense preoccupation and concerns with body shape and sizeANDb) Significant low weight or weight loss due to voluntary restricting of food intake (i.e. 15% of baselinenormal weight).ORc) Binge eating more than two times per week for three months accompanied by feeling out of control (i.e.can’t stop binge or control how much is eaten) and purging behaviour (i.e. vomiting, laxatives, post-bingefasting, excessive exercise…).NB: Referral for clients that are pre-pubescent must come from a paediatrician.Exclusion criteria:The EDP does not provide services in the following instances:1. Alcohol or substance abuse is the primary presenting problem.2. The client does not have a General Practitioner. Given our limited resources, the EDP can not be asubstitute for a client’s General Practitioner. As such referrals of individuals who do not have a familyphysician can not be accepted.3. The client is age 12 or under and is not referred by a paediatrician.4. The client is acutely suicidal or in crisis.5. Acute psychiatric disorders account for decreased food intake such as: Thought Disorders (e.g. someone with schizophrenia who has delusions around food). Major Depression or Post Partum Depression where decreased food intake is due to mood.6. Binge eating disorder (i.e. binge eating without any compensatory behaviour).7. The client is not a resident of <strong>Fraser</strong> South <strong>Health</strong> Area.Referral Source: (Family <strong>Physician</strong> or Paediatrician if age 12 or under)Name:Office Phone:Address:Client Information – Please complete:Client’s Surname:Client’s First Name:Office Fax:Gender:MFDOB: (yyyy/mm/dd)Current Address (include postal code):Home Phone # Work Phone #Parent/Guardian Name: Home Phone #Work Phone #Parent/Guardian Name: Home Phone #Work Phone #May we contact the Client’s Parents/Guardian? Yes NoPHN:Program:Child & Youth1
Current Height:Lowest Wt:Highest Wt:Client’s desired weight:Current Wt:Age:Age:/ /Date obtained: (yyyy/mm/dd)Vital SignsTemp ______________ Resp _____________________Pulse Sitting _______________________BP Lying __________________________Pulse Standing ______________________BP Standing ________________________Eating Disorder Related Behaviours:Restricting: Yes No History of RestrictingDaily intake: less than 1 meal/day 1 meal/day 2 meals per day or morePurging: (over the past 3 months)Vomiting Yes No Frequency: daily 2-3x / week less than once / weekHistory of purging, if not purging currently Yes NoExercise – hours per week 0-3 4-10 10-15 15-20 20-30 30 +Laxatives: Yes No History of Laxative AbuseType(s) used:Frequency / number per day: 1 to 10 10 to 20 more than 20Other Purging Methods:Diuretics Thyroid Medications IpecacAppetite Suppressants Insulin manipulation Other _______________________Binge Eating (Objectively large amount of food within any 2 hour period)Yes No Frequency: daily weekly monthly2
Medical History:Medical causes of low weight or vomiting ruled out? Yes NoAmenorrhea Yes No LMPHistory of Amenorrhea Yes NoBCP Yes NoPregnant Yes No Week of Pregnancy at Referral:Diabetes: (insulin dependent) Yes NoGI Disorders (i.e. Crohn’s, Celiac Disease): Yes NoAllergies:Other medical conditions:Current Medications (Please list with dosage):Psychiatric History:Please describe any psychiatric symptoms of concern, or current diagnoses:Suicidal Ideation Yes NoDescribe:Self Harm Yes NoDescribe:Substance/Alcohol Abuse Yes NoWhich substances?Treatment:3
Current Treatment for ED /Psychiatric concerns? Yes NoPast Treatment for ED /Psychiatric concerns? Yes NoIf “yes”, please indicate who else is/was providing services for this clientPsychiatristMental <strong>Health</strong> ClinicianPsychologistBC Children’s Hospital ED ProgramOther: ________________________Working ED Diagnosis:Anorexia Nervosa, Restricting typeAnorexia Nervosa,Binge-eating/Purging typeBulimia Nervosa, Purging typeBulimia Nervosa, Non-purging typeEating Disorder Not Otherwise SpecifiedLab Work – A current (within 2 months) copy of the following is required:1) ECG2) Full blood biochemistry including all of the below:- CBC and Diff - Serum Phosphate, Magnesium, Zinc- Ferritin - BUN, Creatinine- Random Blood Sugar - Na, Cl, K, Bicarb- TSH - Serum Protein- ALT, AST, Alk Phos, Bilirubin3) Microscopic Urinalysis to include Specific Gravity.PLEASE REMEMBER TO INCLUDE: (1) all relevant tests (ie, blood work and ECG),(2) symptoms and frequency,(3) current height and weight,(4) highest and lowest weights, and(5) GP contact info as you will be providing on-goingmedical care for this patient.Please advise your patient that she/he will not be put on our wait list until the referral process has beencompleted. This process includes your completed referral form, blood work, and ECG. Patients areencouraged to attend our Information Session, held the third Thursday of every month @ 4:30 pm at theNorth Delta Mental <strong>Health</strong> Centre. Once on the list, we will invite the patient in for a Screening and BriefOrientation Session and if appropriate an Assessment Appointment will then be scheduled.__________________________________Doctor’s Signature______________________________DateIf you have any questions re completing the referral, please call us at 604 951.5844 08/31/104
<strong>Fraser</strong> East:This program is part of the <strong>Fraser</strong> East but we are not a co-located program. I provide bothindividual and group therapy as well as case management for these clients. Typically there isonly one group running at a time as there is only one of me. Clients are also able to access anout-patient dietician who is based at Abbotsford Regional Hospital.Clients who see me are required to have regular follow-up with their family physicians formedical monitoring. Because of this, it is preferrable that they are referred by their G.P. I do alsoaccept self-referrrals. There is no referral form. G.P.'s simply fax our office the relevant info.This includes:1. Client demographics- name, address, phone numbers, PHN etc.2. Eating Disorder Diagnosis and any other relevant diagnoses3. Information pertaining to current symptoms and onset, medications, weight if available 4.Follow-up plan with G.P. - i.e. medical monitoring 5. Any bloodwork or other relevant tests ifavailableThat's about all that I would be needing for the referral.They can also phone and have our clerical staff will take down all of the information. Once thereferral is complete, I will then contact the client to complete a telephone screening and tellthem more about our services.Abbotsford Mental <strong>Health</strong> Contact Information:Telephone: 604 870-7800Fax: 604 870-7801I hope that this answers your questions. Please feel free to contact me with any other questions.Kelley Fitzpatrick, MSWEating Disorder TherapistAbbotsford Mental <strong>Health</strong>(604) 870-7800
:http://www.bcguidelines.ca/pdf/problem_drinking.pdfhttp://www.who.int/substance_abuse/activities/assist/en/index.htmlThe SU services that MDs can refer directly to include detox(Creekside and Riverstone in Chilliwack), the public outpatientcounseling services in each community (Share in Coquitlam,<strong>Fraser</strong>side in New West etc.) and residential services (MRTC andKinghaven and the support recovery homes that FHA hascontracted beds at ie: The Last Door, Phoenix House, InnerVisions, Charlford House, Westminster House and HannaHouse). Referral information for inpatient is generally availablefrom their websites.
Fact SheetPanic Disorder GroupDoes this describe you?♦♦Do you feel at the mercy of your emotions?Do you have unexpected abrupt surges of intense fear or dread that make you think youare sick, dying, or losing your mind?♦ When these scary feelings occur, does your heart feel as though it's going to burst out of your chest? Does it feel asif you are "on guard," waiting for these feelings to happen again?♦ Has your anticipation of the scary feelings interfered with your normal daily routine or prevented you from doingthings you would normally do? Maybe the anticipation is so overwhelming that you try to avoid driving, crowdedstores, or other situations where you feel trapped or where it seems difficult to get help?If so, you may be experiencing panic attacks and associated anxiety. Group Therapy Services offers a therapy group forthose challenged by anxiety and panic. The group will help teach you to control your “out-of-control” fearful emotions.The group is 11 weeks long and each session is 2 hours in length. Each session teaches specific skills that continue tobuild on each other, allowing you to regain a sense of mastery over your life. Homework is an essential part of the groupand participants should be able to commit to some out of session work.Session topics will include:• Learning About Emotions and Your Responses• Developing Control of Physical Responses Using:i) breathing control techniquesii) muscle relaxation training• Making the Unexpected Predictable• Learning To Be An Observer of Your Own Thoughts, Feelings, and Behaviour• Learning To Go Into Feared Situations with ConfidenceThe experience of anxiety, panic and avoidance can occur across all levels of socioeconomic status, professions, andtypes of persons. across all kinds of people, across all levels of socioeconomic status, and professions. But, panic and/oranxiety doesn’t have to run your life! Come and join our group and find out how!For information please call: (604) 520-4397For a referral, please contact your localmental health centre:Royal Columbian HospitalGroup Therapy Services3 rd Floor, 260 Sherbrooke StreetNew Westminster, BC V3L 3M2www.fraserhealth.caNew Westminster Mental <strong>Health</strong> Centre(604) 777-6800Tri-Cities Mental <strong>Health</strong> Centre(604) 777-8400
Fact SheetObsessive Compulsive GroupDoes this describe you?♦ Do you have repeated unwanted thoughts or images that cause significant distress and are time consuming? Forexample, doubting that the door is locked, or being contaminated with germs, thoughts of doubt about whether youmight have harmed someone or turned off the stove.♦ Do you perform deliberate behaviours (e.g. washing, checking, ordering) or mental rituals (e.g. praying, counting,repeating phrases) that are carried out to reduce the anxiety caused by the obsessions?♦ Some common Obsessions include fear of contamination, thoughts of doubt, fear of harming yourself or others,thoughts about doing something horrible to someone you love.♦ Compulsions are often related to Obsessions. If you worry about being contaminated by germs, you might have theurge to clean all the time. Compulsions can include washing and checking a lot , hoarding things, needing to orderand arrange things in a certain way, mental rituals like replacing a bad thought with a good thought, or repeat aprayer when you have thoughts about something bad happening, or asking for reassurance.Group Therapy Services offers a Cognitive Behaviour Therapy Group for those challenged by Obsessive CompulsiveDisorder (OCD). The group will teach you how to manage your obsessions and compulsions. The group meets weeklyfor 12 weeks and each session is 2-hours in length. Each session teaches specific skills that continue to build on eachother, allowing you to regain a sense of mastery over your life. Homework is an essential part of the group andparticipants should be able to commit to some out of session work.The experience of obsessions and compulsions can occur across all levels of socioeconomic status, professions, and typesof persons. But, OCD doesn’t have to run your life! Come and join our group and find out how!For information please call: (604) 520-4397For a referral, please contact your localmental health centre:New Westminster Mental <strong>Health</strong> Centre(604) 777-6800Tri-Cities Mental <strong>Health</strong> Centre(604) 777-8400Royal Columbian HospitalGroup Therapy Services3 rd Floor, 260 Sherbrooke StreetNew Westminster, BC V3L 3M2www.fraserhealth.ca
Fact SheetGeneralized Anxiety GroupDoes this describe you?♦♦Do you have repeated and exaggerated worries about routine life events and activities?Do you anticipate the worst even though others would say there is no reason to expect it?♦ Do you have physical symptoms that include nausea, trembling, fatigue, muscle tension or headaches?If so, you may be experiencing Generalized Anxiety Disorder (GAD). Group Therapy Services offers a therapy group forthose challenged by GAD. The group will teach you to control your “out-of-control” worries and the resulting anxiety.The group meets weekly for 14 weeks and each session is 90-minutes in length. Each session teaches specific skills thatcontinue to build on each other, allowing you to regain a sense of mastery over your life. Homework is an essential partof the group and participants should be able to commit to some out of session work.Session topics will include:• Learning to Understand and Influence Your Worries and Your Intolerance to Uncertainty• Improving Your Relationship with Problems• Identifying Two Types of Worries• Learning To Reduce Your Avoidance of Certain Thoughts• Learning To Develop Skills to Deal with RelapseThe experience of worry, anxiety and avoidance can occur across all levels of socioeconomic status, professions, andtypes of persons. But, GAD doesn’t have to run your life! Come and join our group and find out how!For information please call: (604) 520-4397For a referral, please contact your localmental health centre:New Westminster Mental <strong>Health</strong> Centre(604) 777-6800Tri-Cities Mental <strong>Health</strong> Centre(604) 777-8400Royal Columbian HospitalGroup Therapy Services3 rd Floor, 260 Sherbrooke StreetNew Westminster, BC V3L 3M2www.fraserhealth.ca
Fact SheetDepression Group• The Depression Group teaches persons with depression a variety of cognitive behavioral skills that include goalsetting, challenging negative automatic thoughts and stress management. Strategies for discovering and alteringdistorted or negative ways of thinking are explored in the group sessions.• Assigned homework is an important part of the depression therapy group. Participants commit some time to thiswork outside of the group sessions.• This group meets weekly for 10 weeks and each session is 2 hours in length.How does the group work?Using a Cognitive Behavioural Therapy format, we teach individuals the basics of goal setting, then introduce otherresearch supported strategies for working with depression that include challenging negative thoughts, core beliefs,assumptions, goal setting and behavioural activation. Within the group, participants are able to support and encourageeach other’s commitment to change and benefit from ‘lessons learned’ by others in the group. We are also able to worktogether to challenge inaccurate core beliefs, unconditional assumptions, and examine the ‘good reasons’ we have fordoing the things we do. We are able to examine experiences non-judgmentally and investigate alternate strategies forliving. The group can provide feedback about how we are reconstructing our beliefs and to engage in more accurateappraisals of our environment, our feelings and our thoughts. The group's facilitator presents information almost in theform of a lecture. There are also group discussions about the material, and homework exercises to practice skills learnedin the group.The experience of depression can occur across the life span, levels of socioeconomic status, professions, and types ofpersons. But Depression doesn’t have to run your life! Come and join our group and find out how!For information please call: (604) 520-4397For a referral, please contact your localmental health centre:New Westminster Mental <strong>Health</strong> Centre(604) 777-6800Tri-Cities Mental <strong>Health</strong> Centre(604) 777-8400Royal Columbian HospitalGroup Therapy Services3 rd Floor, 260 Sherbrooke StreetNew Westminster, BC V3L 3M2www.fraserhealth.ca
4 th Floor Sherbrooke Centre Tel (604) 520-4662New Westminster, BC Fax (604) 520-4871V3L 3M2 Canadawww.fraserhealth.caREFERRAL FORM – NEUROPSYCHOLOGICAL ASSESSMENT SERVICESDate of Referral (dd/mm/yr):PHN:Last Name: First Name: DOB (dd/mm/yr):Address: City: Home Phone:Occupation Status: First Language: Interpreter Needed: Y NPlease circle: Inpatient OutpatientFloor _____If they cannot be seen as an inpatient, do you want them seen as an outpatient? Y NPLEASE PRINT LEGIBLYReferral Source (Name of Person and Site):Phone:Address:FaxCURRENT DIAGNOSIS: __________________________________________________________________________________________________CURRENT MEDICATIONS: _____________________________________________________________________________________________________________________________________________________________________________________________________________________REFERRAL QUESTION (Please be as specific): ________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________PLEASE CHECK ALL APPLICABLE: Attention/Concentration Problems Memory Problems Problems with Orientation Seizures/Seizure-Like Symptoms History of Traumatic Brain Injury (TBI) Intellectual Functioning History of Loss of Consciousness (LOC) Significant Medical Problems – Specify______________________________________________________________________ Neurological Disorder – Specify ____________________________________________________________________________ Other Observed Cognitive Problems – Specify _______________________________________________________________PLEASE ATTACH COPIES OF THE FOLLOWING IF AVAILABLE: MRI, CT Scan Report EEG Report Previous Intellectual/Learning/Neuropsychological Assessment Psychiatric Consultation ReportDATE REFERRAL RECEIVED (dd/mm/yr): _______________REFERRAL NAME (PLEASE PRINT) _______________________________Criteria for patients to be seen by the Neuropsychology Service at Royal Columbian Hospital: (1) patients who live within the <strong>Fraser</strong><strong>Health</strong> <strong>Authority</strong> catchment area; (2) patients who are 18 years and older, and; (3) patients associated with a mental health team.Exclusion criteria include: (1) patients involved in litigation; (2) patients injured at the workplace, and; (3) patients who only needintelligence testing done.
EPI: Early Psychosis Intervention:The EPI provides services to people who are experiencing psychosis for the first time. Thisservice includes medication management, education - individual and group, support, copingand stress management, relapse prevention, and assistance with other needs such aseducation, work, housing, drug abuse, etc. Referrals can be made by anyone, includingfriends, family, schools, or family doctors by telephone or fax (GP).<strong>Fraser</strong> South LocationEarly Psychosis Intervention15521 Russell Ave.White Rock, BC V4B 2R4Contact us at: 604-538-4278SouthReferralFormEPI specialists work at every youth and adult mental health centre in Surrey, Delta, WhiteRock and Langley.<strong>Fraser</strong> North LocationEarly Psychosis Intervention ProgramRoyal Columbian Hospital4th Floor, Sherbrooke Centre260 Sherbrooke StreetNew Westminster, B.C. V3L 3M2Contact us at: 604-777-8386NorthReferralFormWe serve the communities of Maple Ridge, Tricities (Port Moody, Port Coquitlam, Coquitlam),New Westminster, and Burnaby.<strong>Fraser</strong> East LocationsAbbotsford Site11 - 32700 George Ferguson WayAbbotsford, BC V2T 4V6Chilliwack Site45470 Menholm RoadChilliwack, BC V2P 1M2Contact us at:Cell: 1-866-870-7847 (toll free)Landline: 604 851 4700 ext. 646404No referral form, refer by phone call to above numberWe provide service to the communities of Mission, Abbotsford, Chilliwack, Hope, & Agassiz.
Early Psychosis Intervention Programc/o Peace Arch Hospital15521 Russell AvenueWhite Rock, BC V4B 2R4Telephone: (604) 538-4278Fax: (604) 538-4277GP Referral FormFamily Doctor: _______________________Billing No.___________Tel. No.___________________Fax. No.________________ Address:________________________________________________Date:____________________ (dd/mm/yy)Client Name:_________________________________ Date of Birth:______________(dd/mm/yy)PHN:_________________________ Client Telephone No.______________________________Client Address: ________________________________________________________________Current Medication___________________________________________________________________________________________________________________________________________Referral information: Relevant history/ presenting problems/ known risks.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________ No prior treatment for psychosis. Client aware ofreferral Fax to EPI Intake: 604-538-4277
REFERRAL FORMEARLY PSYCHOSIS INTERVENTION (EPI) PROGRAMBurnaby, New Westminster, Tri-cities, Maple Ridge or Pitt MeadowsREFERRAL CRITERIA: Age 13 – 30 with suspected or first episode psychosis(Please note that substance use does not disqualify from referral).Check all that apply:Suspected PsychosisDelusionsHallucinationsDisorganized speechFamily history of psychotic disorder & serious psychosocial deteriorationGrossly disorganized behaviourNegative symptoms - e.g. flat affect or avolitionOTHER CONCERNS:_____________________________________________________________________________________________________________________________________________________________________________________________Referred By: _______________ Phone: _______________ DATE: ______________CLIENT’S LEGAL NAME: _______________________________________________D.O.B: __________________ M F PHN: ______________________ADDRESS:____________________________________________________________PHONE: ______________________________________________________________NEXT OF KIN:_________________________________________________________FAMILY PHYSICIAN: _____________________________ Phone: ______________PLEASE FAX REFERRAL TO: 604 – 520 – 4871EPI Intake Clinician will contact client to arrange initial assessment andconsultation with one of the EPI Psychiatrists.TO CONTACT EPI INTAKE CLINICIAN CALL: 604 – 777 - 8386Early Psychosis Intervention (EPI) ProgramRoyal Columbian Hospital, 4th Floor - 260 Sherbrooke Street, New Westminster, B.C. V3L 3M2
*Additional Resources*For Information or Referral or ServiceNote: These are not family care providers or a substitution<strong>Health</strong> and Seniors Information Line1-800-465-4911Alcohol & Drug Information & Referral Service1-800-663-1441Lower Mainland:(604) 660-9382<strong>Health</strong>Link BC 8-1-1<strong>Health</strong>Link BC helps you learn about health topics, check your symptoms andfind the health services and resources that you need for healthy living. Call 8-1-1to consult with a nurse, pharmacist or dietician.http://www.healthlinkbc.caKids Help Phone1.800.668.6868Problem Gambling Help Line:1.888.795.6111<strong>Fraser</strong> <strong>Health</strong> – After Hours Mental <strong>Health</strong>1-877-384-8062<strong>Fraser</strong> <strong>Health</strong> – Crisis Line604-951-8855 or 1-877-820-7444Crisis Intervention and Suicide Prevention Centre:1-800-SUICIDE1800-(784-2433)Victim Link1.800.563.0808
<strong>Fraser</strong>healthHome <strong>Health</strong>For access to subsidized Personal Care Home Support; Case Management;Nursing Care; Physiotherapy, Occupational Therapy, Residential Care andAssisted Living …and more…Abbotsford Home <strong>Health</strong>604-556-5000Burnaby Home <strong>Health</strong>604-918-7447Langley Home <strong>Health</strong>604-532-6500Maple Ridge Home <strong>Health</strong>604-476-7100New Westminster Home <strong>Health</strong>604-777-6700Tri-Cities Home <strong>Health</strong>604-777-7300White Rock Home <strong>Health</strong>604-541-6800South <strong>Fraser</strong> Central Intake604-953-4965Royal Columbian Group Therapy ServicesReferrals to RCH Group Therapy Services are made through the mental healthcentres in our catchment area. Prior to entering one of our groups, an intakeassessment is completed at one of these centres. The mental health centres inour catchment area are New Westminster Mental <strong>Health</strong> Centre (604) 777-6800 and Tri-Cities Mental <strong>Health</strong> Centre (604) 777-8400, which serve NewWestminster, Coquitlam, Port Coquitlam and Port Moody.DepressionGADOCDPanicBrochureBrochureBrochurePanicBrochure
Mental <strong>Health</strong>and Addiction… supporting individualson their recoveryjourneys.ServicesJune 2008respect · caring · trust
Contents<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services. 4Introduction.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5Addiction Services . 61. <strong>Health</strong> Promotion and Prevention.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62. Outpatient/Outreach .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 73. Withdrawal Management and Detox .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 84. Intensive Day Treatment .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 95. Short-term Residential (less than 90 days)............................................. 96. Long-term Residential........................................................... 107. Housing ..................................................................... 10Self-help Groups................................................................. 11For more information on services .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11Links to Addictions Resources.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11Mental <strong>Health</strong> Services. 12Community Mental <strong>Health</strong> Centres................................................... 121. <strong>Health</strong> Promotion and Prevention.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 132. Primary and Shared Care. ....................................................... 133. Urgent/Emergent/Crisis.......................................................... 134. Community and Outpatient .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 165. In-patient and Day Treatment.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 186. Tertiary Care .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 197. Residential Care and Housing.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20Community Mental <strong>Health</strong> Advisories................................................. 20Links to Mental <strong>Health</strong> Resources.. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20Contracted Agencies .. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 3
<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong>and Addiction ServicesVisionBest in Mental <strong>Health</strong> and Addiction Services within a recovery-oriented system.PurposeTo improve the overall health status of individuals and families in <strong>Fraser</strong> <strong>Health</strong> through health promotion and theprovision of high quality, comprehensive and integrated Mental <strong>Health</strong> and Addiction Services.ValuesTo provide care based upon respect, compassion, integrity, and accountability.4<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
<strong>Fraser</strong> <strong>Health</strong>’scommitment<strong>Fraser</strong> <strong>Health</strong> is dedicated to providing aresponsive, inclusive and recovery-orientedsystem of mental health and addictions care – asystem that recognizes that recovery is a deeplypersonal and unique process.Mental illness and substance misuse touch many lives.They can settle over a household like a cloud, puttinga young life on hold while parents desperately seekanswers. They can turn a pragmatic, cheerful andproductive person into someone who is fearful, angryand desperately unhappy. They can touch our familiesand our friends, perhaps our mother, or son or ourgrandfather. According to statistics, each of us has a onein five chance of struggling with mental illness and/orsubstance abuse, at some time in our life.The hopeful news is that prevention, early diagnosisand timely intervention, can make a real difference.With this in mind, <strong>Fraser</strong> <strong>Health</strong> provides a widerange of acute and community services and iscommitted to making significant investments toenhance its mental health and addiction resources overthe next few years. As well, it contracts with communityagencies to provide services that complete and complementits services.Mental <strong>Health</strong> and Addiction principal services are divided into the following categories:ÎÎ Youth and Young AdultÎÎ AdultÎÎ Older AdultÎÎ Specialized Services Eating Disorders Concurrent Developmental Disabilities Reproductive Mental <strong>Health</strong> Mentally Disordered OffendersÎÎ Specific Population Services Aboriginal Communities Diverse Communities (Multicultural Population, Lesbian, Gay, Bisexual, Transgendered Population) Homeless PopulationÎÎ AddictionsÎÎ Tertiary ServicesÎÎ HousingThe following is a snapshot of services within <strong>Fraser</strong> <strong>Health</strong>. There is a degree of variability in the services availablein each community – therefore all services listed are not necessarily available in every community. For detailedinformation on services available in a specific community please contact the local mental health or addictions centreor go to www.fraserhealth.ca/services/mentalhealthandaddictions<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 5
ADDICTION SERVICESAddiction ServicesIn April 2002, the responsibility for thedelivery of addiction services was placed withthe regional health care delivery systems forthe first time in B.C.’s history. Since then,<strong>Fraser</strong> <strong>Health</strong> has been dedicated to buildinga comprehensive continuum of supportand service for individuals with problemsubstance use.Harm Reduction<strong>Fraser</strong> <strong>Health</strong> has adopted a Harm Reduction Policy that focuses onkeeping people safe and minimizing injury, disease and death thatcan result from substance use. This approach recognizes our clients’strengths and needs, and meets our clients wherever they are in theircourse of recovery. The approach empowers clients to set their owngoals, while our services support our clients to achieve them.1 2 3 4 5 6<strong>Health</strong>Promotion &PreventionSecond Stage HousingHarmReductionOutpatientOutreachWithdrawalManagementServices7. Addictions HousingDayTreatmentShort-termResidential
ADDICTION SERVICES2. Outpatient/OutreachOutpatient ServicesTrained professionals at outpatientservices offer free, confidentialinformation, assessment, counsellingand referral for people with problemsubstance use. Service is also availablefor people who are affected bysomeone else’s problem. Treatmentincludes individual, family, couplesand group work, as well as aftercaresupport.Drug and AlcoholResource Team (DART)– Surrey MemorialHospitalDART provides early interventionand counselling to in-patients inacute care who may also be copingwith a substance abuse problem.The hospital-based team works withpatients and hospital staff to provideearly identification, assessment,intervention, and referrals tocommunity resources. Services alsoinclude education to patients andtheir families, facilitating transitionsfrom the hospital, and collaborativework with other health careproviders.Concurrent DisordersServicesDirect ServicesBurnaby Addictions Services604-453-1910Surrey Addictions Services604-953-4900Contracted AgenciesAbbotsford CommunityServices 604-850-5106Agassiz-HarrisonCommunity Services 604-792-2585Family Services GreaterVancouver Burnaby Services604-453-1910Tri-Cities: SHARE Familyand Community Services604-936-3900Chilliwack Addictionsand Prevention Services604-824-6883Deltassist Family andCommunity Services604-594-3455Hope Transition Society,Addictions and Prevention604-869-2466Langley CommunityMaple Ridge: AlouetteAddiction Services604-467-5179Services 604-534-7921Specialized support and servicesare available in each <strong>Fraser</strong> <strong>Health</strong>community for adults and youthexperiencing both substance abuse and mental health issues. The overarching goal of the Concurrent DisordersTherapists is to increase awareness and understanding of concurrent disorders, to provide education, consultation andsupport to care providers in both the addictions and mental health fields and to provide direct individual and grouptreatment of concurrent disorders.Mission: <strong>Fraser</strong> HouseOutpatient Clinic604-826-6810Mission Indian FriendshipSociety 604-826-1281New Westminster:<strong>Fraser</strong>side CommunityServices 604-522-3722Surrey: DiverseCityCommunity ResourceSociety 604-597-0205White Rock: Peace ArchCommunity Services604-538-2522ContractedSpecialized OutreachServices for YouthOdyssey 604-299-6377Pacific CommunityResources Society604-412-7950IMPACT Society604-853-1766<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 7
ADDICTION SERVICESYouth Addictions Outreach ProgramYouth Outreach Workers work across <strong>Fraser</strong> <strong>Health</strong> with a focus onengaging youth whose drug use includes crystal methamphetamine,recognizing approximately 80 per cent of youth are poly-drugusers. These workers encourage and assist youth in accessing othercomponents of the addiction system of care and also provide some earlyintervention services.Matrix ProgramThe customized Matrix Program for Maple Ridge and Pitt Meadowsoffers withdrawal management, clinical interventions, and aftercareservices for youth 16 to 24 years old, along with support to their familyand others affected by their substance use. Utilizing a ‘wrap-around’approach to youth-centred addition treatment, this community basedprogramis led by the Maple Ridge Treatment Centre.3. Withdrawal Management and DetoxIn-patient Detox FacilitiesWithdrawal management services provide safe, supportive medically supervised environments for individualswithdrawing from the acute effects of alcohol and/or other drugs.Creekside Withdrawal Management Centre (24 adult and six dedicated youth beds) 604-587-3755(Virtual tour of Creekside is available at www.fraserhealth.ca/Services/Mental<strong>Health</strong>andAddictions/AddictionServices/pages )Chilliwack Withdrawal Management Unit, Chilliwack General Hospital (eight adult and one youthbed) 1-866-795-0600 (toll free)DaytoxDaytox is a medically monitored day program for withdrawal management forindividuals who do not require intensive residential withdrawal managementservices. It provides an alternative support option other than detox orhospitalization for adults (19 and older) assessed as being suitable—to ensuredaytox will meet their withdrawal management needs, and who have asupportive home environment.Home DetoxAmong the outreach services provided by the Matrix Program in Maple Ridgeand Pitt Meadows is home detox for youth 16 to 24 years old.8<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
ADDICTION SERVICES4. Intensive Day TreatmentTEAM, MELL, WELLJackson Murray - 604-589-7080These four-to five-week contracted programs offer free intensive therapeutic group counselling in a non-residentialsetting.DEWY (Day, Evening, Weekend Youth program)This 12-week program offers free intensive therapeutic group counselling in a non-residential setting for high-riskyouth, 12-18 years old, experiencing alcohol, drug and/or related problems, and whose assessment indicates that theywill be effectively supported only through receipt of intensive treatment services.5. Short-term Residential (less than 90 days)Intensive Residential TreatmentThese facilities offer intensive treatment programs that include groups, with some individual and family counselling.Direct ServiceMaple Ridge Treatment Centre - 604-467-3471 (Men Only) www.mrtc.bc.caContracted AgenciesKinghaven (men) 604-864-0039Peardonville (women and their pre-school age children)604-856-3966<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 9
ADDICTION SERVICES6. Long-term ResidentialStabilization and Transitional Living Residences (Support Recovery)These contracted residences offer a safe living environment, free of alcohol and other drugs for individuals who arepursuing their recovery. They provide pre-treatment stabilization and post-treatment reintegration into the community.Women’s facilities:Charlford 604-420-4626Hannah House 604-468-2032Liz’s House 604-583-2502Mollie’s Place 604-856-3966, local 120Westminster House 604-524-5633Men’s facilities:Inner Visions 604-468-2032Last Door 604-525-9771Path to Freedom 604-576-6466Phoenix House 604-583-7166Valley Recovery 604-864-0039Youth ServicesLast Door For Youth (male facility) 604-520-35877. HousingSecond Stage Housing<strong>Fraser</strong> <strong>Health</strong> partners with B.C. Housing to provide second stage supportive housing for clients who have completedsupport recovery programs. While the subsidized apartments and support are located in Burnaby, New Westminsterand Surrey, the program is available to all clients living in <strong>Fraser</strong> <strong>Health</strong>.10<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
ADDICTION SERVICESSelf-help GroupsSelf-help groups are a worldwide community. These 12-Step support groups (independent of <strong>Fraser</strong> <strong>Health</strong> addictionservices) are available days, evenings and weekends.AA Alcoholics Anonymous 604-434-3933NA Narcotics Anonymous 604-873-1018CA Cocaine Anonymous 604-662-8500Al-Anon (For family, friends of alcoholics) 604-688-1716Alateen(For teenagers of alcoholics) 604-688-1716Nar-Anon (For family, friends of drug users) 604-878-8844CoDA Co-Dependents Anon 604-515-5585GA Gamblers Anonymous 604-878-6535Crystal Meth Anonymous 604-633-4242Links to Addictions Resourceswww.heretohelp.bc.cawww.youarethelink.cawww.preventionsource.bc.caFor moreinformation onservicesAlcohol and DrugInformation ReferralA 24-hour free telephone serviceprovides information about provincewideaddiction services.Local: 604-660-9382 Toll-free line:1-800-663-1441<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 11
MENTAL HEALTH SERVICESMental <strong>Health</strong> Services1 2 3 4 5 6<strong>Health</strong> Promotion& PreventionPrimary &Shared CareUrgent/Emergent/CrisisCommunity &OutpatientIn-patient & DayTreatmentTertiary Care7. Mental <strong>Health</strong> HousingSupported Housing Supported Living Program (SIL) Minimum Barrier HousingMH ResidentialFamily Care HomeCommunity Mental <strong>Health</strong> CentresServices available through the centres include: Adult Community Support Services, Adult Short-Term Assessmentand Treatment, Community Residential Program, Geriatric Program, Crisis Intervention, Day/Outpatient Program,Addictions Counselling, Concurrent Disorders Services, Group Therapy, Peer Support, and Mental <strong>Health</strong> After-HoursServices.Abbotsford Mental <strong>Health</strong>604-870-7800Hope Mental <strong>Health</strong> Centre604-860-7733Agassiz Mental <strong>Health</strong> Services604-793-7160Langley Mental <strong>Health</strong>604-514-7940Burnaby North Mental <strong>Health</strong> Team604-949-7730Maple Ridge Mental <strong>Health</strong> Centre604-476-7165Burnaby Services (South Team)604-777-6870Mission Mental <strong>Health</strong> Centre604-814-5600Burnaby Services (Central Team)604-453-1930New Westminster Mental <strong>Health</strong> Centre604-777-6800Chilliwack Mental <strong>Health</strong>604-702-4860Royal Columbian Hospital Psychiatric Services604-520-4664Delta Mental <strong>Health</strong> Centre – north604-592-3700Surrey Mental <strong>Health</strong> Centre604-953-4900Delta Mental <strong>Health</strong> Centre – south604-948-7010Surrey (Primary Care Clinic)604-953-4940Developmental Disabilities Mental <strong>Health</strong>Services – <strong>Fraser</strong> 604-777-8475Tri-Cities Mental <strong>Health</strong> Centre (Port Coquitlam)604-941-3471Developmental Disabilities Mental <strong>Health</strong>Services –Burnaby/Vancouver Coastal604-918-7540White Rock/South Surrey Mental <strong>Health</strong> Centre604-541-684412<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
MENTAL HEALTH SERVICES1. <strong>Health</strong> Promotion and Prevention(See description in Addictions section)A variety of <strong>Health</strong> Promotion and Prevention activities are provided by Mental <strong>Health</strong> Centres, i.e. education andawareness building during National Mental <strong>Health</strong> Week in May, Mental Illness Awareness Week in October, NationalAddictions Awareness Week in November; health fairs; information brochures, education sessions, <strong>Health</strong>y Body<strong>Health</strong>y Mind one-time grants for initiatives that promote and encourage healthy lifestyle changes, smoking cessationprograms, etc.<strong>Fraser</strong> <strong>Health</strong>’s website also provides a variety of mental health and addictions information.Early Psychosis Intervention (EPI) ProgramThe goal of the EPI program, a partnership between <strong>Fraser</strong> <strong>Health</strong> and Ministry of Children and Family Development,Child and Youth Mental <strong>Health</strong> is to recognize the signs and symptoms of psychosis early so that effective treatmentcan be started as soon as possible. The program provides clinical services and education for youth and young adultsages 13-35 years old – with the intent of promoting wellness, reducing socially-isolating behaviour, and restoringprevious levels of functioning.2. Primary and Shared CareShared Care ProgramsThis program aims to assist family doctors in caring for their patients who have mental health concerns. The programis directed at adults and youth who need short-term mental health support. Each client is assessed by a mental healthnurse in the physician’s office, who can help them connect with community services, counselling and other localresources. Formal psychiatric assessment and consultation with a psychiatrist is available through the shared carenurse.Primary CareThe primary care clinics administered by Surrey and Burnaby Mental <strong>Health</strong> and Addiction Services provide medicalcare, health education, and advocacy, to individuals including youth experiencing mental health problems as well as totheir families. The clinics embrace an integrated approach to service delivery through coordination of care with mentalhealth services, hospital and other community agencies.3. Urgent/Emergent/CrisisCar 67 (available in Surrey)Through the Mobile Outreach a mental health nurse and a RCMP officer in an unmarked police car, respond to urgentcases where it is believed that an individual experiencing mental health difficulties is at risk of harming himself/herself.The team provides intervention, assessments and referrals to individuals experiencing a mental health crisis.<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 13
MENTAL HEALTH SERVICESDelta Mental <strong>Health</strong>/Delta Police Community OutreachMental <strong>Health</strong> and Addictions designated staff work with a Delta Police Officer to:ÎÎÎÎÎÎÎÎAssist with outreach regarding mental health related calls received by Delta Police.Participate in response planning regarding mental health situations the police encounter.Formalize liaison with other related services (i.e. substance abuse counselling) so identified clients can be referredfor further supportive services and follow-up.Provide enhanced training on mental health conditions for the police.Emergency Mental <strong>Health</strong> ServicesThe After Hours Service provides emotional support for individuals who are experiencing a mental health crisis. Aswell, it provides referrals and linkage with community resources.For communities in the north area of <strong>Fraser</strong> <strong>Health</strong>:Phone: 604-527-0009Hours: Monday to Friday: 3:30 p.m. to 11 p.m.Weekends and holidays: 1:30 p.m. to 11:30 p.m.For communities in the south area of <strong>Fraser</strong> <strong>Health</strong>:Phone: 604-587-4222Hours: Monday to Friday: 4:30 p.m. to 11 p.m.Weekends and holidays: 1 p.m. to 11 p.m.For communities in the east area of <strong>Fraser</strong> <strong>Health</strong>:Emergency Mental <strong>Health</strong> Services have two service arms - Abbotsford/Mission and Chilliwack/Hope. The programaugments the urgent response mental health services and complements the role of hospital emergency room, otherfirst responders (police, crisis line and ambulance) and associated service providers (family doctors, addiction services).Phone: 604-820-1166Hours: Monday through Sunday: 1 p.m. to midnight.Crisis LineTrained volunteers provide 24-hour telephone support and crisis intervention counselling, seven days a week.South <strong>Fraser</strong> Regional 24-hour Crisis Line 604-951-8855A service provided by Surrey Community Services Society. Serves Delta, Langley, Surrey, and White Rock.14<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
MENTAL HEALTH SERVICES<strong>Fraser</strong> Valley Regional Crisis Line 604-820-1166 or 1-877-820-7444A service provided by Mission Community Services Society, serving Abbotsford, Agassiz, Boston Bar, Chilliwack,Harrison Hot Springs, Hope, Kent, Mission, and Yale.Greater Coquitlam Crisis and Information Line 604-540-2221A service provided by SHARE Family and Community Services Society. Serves Anmore, Belcarra, Burnaby,Coquitlam, Maple Ridge, New Westminster, Pitt Meadows, Port Coquitlam, and Port Moody.Adolescent and Youth Crisis ResponseThis program supports adolescents 12-18 years of age who are in an acute mental health crisis. Assessment, shorttermcrisis intervention and short-term resource coordination and referral are provided.Psychiatric LiaisonPsychiatric Liaison Nurses work in emergency departments across <strong>Fraser</strong> <strong>Health</strong> with a focus on responding to theneeds of individuals in crisis coming into the ERs. They provide assessments, early interventions, understanding andsupport, and help link individuals with community resources.Adolescent Psychiatric Unit (APU)The 10-bed psychiatric unit at Surrey Memorial Hospital and six-bed unit at Abbotsford Regional Hospital (openAugust 2008) provide assessment, stabilization and initial treatment for youth between 12 and 18 years old who livein <strong>Fraser</strong> <strong>Health</strong>.Psychiatric Assessment Unit (PAU)The goal of the 10-bed short-stay PAU is to provide assessment and treatment to induce rapid stabilization forpatients whose behaviour and symptoms cannot be managed on a general in-patient psychiatric unit.Adult Short-term Assessment and Treatment (ASTAT)This program ensures adults with serious acute mental disorders have access to responsive, sensitive, and relevantassessment and treatment, and are linked with service providers. The goal is to provide treatments that restore thecapability of adults with serious acute mental disorders to resume activities in caring for their families, coping withtheir jobs and participating in their communities.Community Residential Short-Stay and Treatment (CRESST)(located in Abbotsford, New Westminster, Surrey)These emergency psychiatric facilities provide support for clients experiencing a mental health crisis. CRESSTendeavours to prevent unnecessary hospitalizations and maintain client autonomy in a safe, supportive, andsupervised setting.<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 15
MENTAL HEALTH SERVICES4. Community and OutpatientAdult Short-term Assessment and Treatment(See description in urgent/emergent/crisis section)Adult Community Support ServicesThis team serves primarily individuals who are experiencing a major mentalillness requiring longer-term case management in the community to achieve andmaintain essential life necessities such as adequate housing, nutrition, financialresources, medical and psychosocial care.Assertive Community Management (ACM)This team offers intensive case management for individuals experiencing aserious and persistent mental illness that causes significant and enduring functional disabilities.Services are taken to the client, thus providing assertive outreach for clients when needed. The team aims to prevent(re) hospitalization through aggressive enhancement of community supports and services, advocacy for clients, longtermsupport and focusing on the full range of human needs (vocational, education, social, recreational, housing andother personal needs).Developmental Disabilities Mental <strong>Health</strong> ServicesSpecialized multidisciplinary mental health teams provide respectful and individualized assessment, treatment andeducation for adolescents and adults with both developmental disabilities (IQ of 70 or less) and complex mentalhealth needs. Their goal is to optimize well-being and quality of life. The teams also provide educational, training, andconsultative services, and work in collaboration with existing community resources and support networks.Specialized Youth ServicesA Youth Team provides specialized counselling and educational support to children and youth between the ages of12-18 years old.Concurrent Disorders(See description in Addiction Services)Geriatric ServicesThis specialized outreach service supports people 65 years and over who are affected by dementia, major affectivedisorder, or other severe mental illnesses. Multidisciplinary in nature, the team consists of psychiatry, social workand nursing and operates out of the local mental health centre. Clients may live in their own home or in supportivehousing.16<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
MENTAL HEALTH SERVICESEarly Psychosis Intervention(See description in <strong>Health</strong> Promotion section)Eating DisordersFor nutritional and medical management of anorexia nervosa, bulimia nervosa and other eating disorders. Servicescurrently provided include outpatient services (individual therapy, family therapy, nutrition support, medicalmonitoring), limited group programs, limited community support and professional consultation.Se-Cure (Self-Cure) (available in Burnaby)Se-Cure’s approach is integrative, focusing on treatments in harmony with natural healing processes, taking intoaccount individual differences and preferences. Treatment makes use of current scientific knowledge about brainfunction and what may cause and contribute to anxiety symptoms and what has been found helpful in establishingstability. The program offers individual assessments, short-term cognitive behavioral therapy and educational, skillbuildingsupport groups.Psychosocial RehabilitationWithin <strong>Fraser</strong> <strong>Health</strong>, in addition to the important role of hospital and community mentalhealth teams in the provision of recovery-oriented services, there are also psychosocialrehabilitation services (life skills training, occupational therapy, vocational counselling,recreation therapy, etc.) and mental health advisory groups, clubhouses, peer supportworkers, peer-directed skill training, self-help groups, family support groups, advocacyservices, housing support services, etc.Group TherapyGroup therapy provides a unique opportunity to share issues, struggles and successes with others, while learningimportant new skills and options for life’s challenges. Some examples of groups: Anger Management, Coping WithChange, Depression, Difficult Emotions, Dual-Diagnosis Recovery, <strong>Health</strong>y Lifestyle, Life Skills, Panic and Anxiety,Relationship, Relaxation, Self-Esteem, Stress Management, Survivors of Sexual Abuse.Reproductive Psychiatric Clinic(Royal Columbian Hospital)This clinic provides psychiatric services during pregnancy planning, duringpregnancy, and for one year post-partum for patients needing psychiatricassessment and/or follow-up (medication management, counselling).<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 17
MENTAL HEALTH SERVICESMinistry of Employment and Income Assistance (MEIA) ProgramMentally disordered offenders can successfully reduce their risk of relapsing into crime, thanks to a partnership effortby Mental <strong>Health</strong> and Addictions, the Ministry of Employment and Income Assistance, Ministry of Public Safetyand Solicitor General, Corrections Branch, and Community Corrections. Through one visit, a client can report to aProbation Officer, see the Mental <strong>Health</strong> and Addictions Counsellor and touch base with the Employment AssistanceWorker.Clubhouse Without Walls (Surrey, White Rockand Delta)This program reaches out to support young people where they’re at bothphysically and in their recovery, rather than having them come to a specificplace. <strong>Fraser</strong> <strong>Health</strong>, Ministry of Children and Family Development - Child/Youth Mental <strong>Health</strong> and Options-Services to Communities have partneredto offer this innovative initiative in an attempt to address a gap in service foryoung adults (16-24) living with a mental illness in Surrey, White Rock andDelta. The program has three main components – leisure/social recreation,residential and vocational – all with an overarching goal to encourage andsupport individuals as they reintegrate into available programs in theircommunities.5. In-patient and Day TreatmentIn-Patient Psychiatric UnitsThese units provide psychiatric treatment for individuals who present with acute psychiatric disorders and severeemotional problems, for which psychiatric in-patient treatment intervention is necessary. The goal of this program isto assist individuals to stabilize and improve their mental, physical, functional and social abilities. The program offerscoordinated and integrated services that include: assessment, diagnosis, treatment and discharge planning, withreferrals for continuing community mental health after care.Adolescent Psychiatric Unit(See description in Urgent/Emergent/Crisis section)Psychiatric Assessment Unit(See description in Urgent/Emergent/Crisis section)Acute Home Treatment (Langley and White Rock/South Surrey)This program provides home-based psychiatric treatment, as an alternative to in-patient hospital treatment forindividuals with acute mental disorders, who would otherwise need admission; offering short-term, intensive homebasedtreatment, with staff available seven days a week. Psychiatric nurses work with referring psychiatrists to supportpatients suffering acute psychiatric illness, aged 17 years and older and who can be safely managed and are agreeableto receiving care in their home environment.18<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
MENTAL HEALTH SERVICESAdolescent Day TreatmentThis regional community-based program provides a wide range of individualized mental health services andeducational programming for adolescents with acute psychiatric illness. Youth ages 13-18 attend the program fourdays a week for six months.Outpatient Partial Hospitalization Program(Chilliwack General Hospital)This program provides treatment for adults experiencing varying degrees of situational, mental, behavioural oremotional problems, which interfere with their daily living but do not require full hospitalization. The treatment focusis primarily on psycho-educational, cognitive-behavioural and process-oriented group therapy.6. Tertiary Care<strong>Fraser</strong> <strong>Health</strong> is developing a continuum of tertiary mental health services to provide more intensive, longer-term carefor individuals with serious and persistent mental illness, whose complex needs can’t be met in existing communityprograms.Specialized Residential Programs for individuals requiring more intensive ongoing supports in a residential settingto work towards recovery.Cottonwood Lodge 604-777-8724(Virtual tour of Cottonwood Lodge on Riverview Hospital grounds is available at: www.fraserhealth.ca/Services/Mental<strong>Health</strong>andAddictions/Pages/Cottonwood)Connolly Lodge 604-777-8724Delta View Habilitation Centre 604-519-8503Adult Tertiary Rehabilitation Care for individuals with a serious mental illness requiring intensive psychosocialrehabilitation to assist them in managing their illness and reaching their goals.Geriatric Tertiary Acute Service for elderly individuals requiring longer-term assessment, treatment and acutestabilization of mental health issues.Adult Tertiary Acute Care will provide assessment and treatment under both general and intensive care models.Geriatric Behavioural Stabilization Care for elderly complex individuals (55 years and older) with serious andpersistent mental health issues who require more intensive stabilization and rehabilitation, allowing them to functionat their optimum in light of their illness.Delta View Habilitation Centre 604-519-8503Complex Neuro-psychiatry Care provides treatment, care and supportive rehabilitation for those who have acombination of complex neurological disorders, high medical needs, and behavioural challenges.Delta View Habilitation Centre 604-519-8503Community Tertiary Rehabilitation Services for individuals requiring more intensive psychosocial rehabilitation toassist them in managing their illness and in reaching their goals than what is available in existing community mentalhealth residential rehabilitation services<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 19
MENTAL HEALTH SERVICES7. Residential Care and HousingMental <strong>Health</strong> and Addictions offers a variety of residential and supportive housing services for people experiencing aserious and persistent mental illness. These programs range in scope from 24-hour licensed care to rent subsidies andsupport. All programs provide case management services for individuals who are at various levels of recovery fromtheir mental illness.Examples of residential care and housing include:Î Î Licensed Residential Care facilities (staffed 24 hours per day)Î Î Supported Housing – a variety of housing and support models including congregate,transitional housing, bridging and Supported Independent Living (SIL) – subsidized rent withsupportÎ Î Family Care Home – privately owned homes provide 24 hour care and supportÎ Î Minimum Barrier Housing – housing provided for persons experiencing difficulty infinding and keeping housing.More information on residential and housing opportunities can be obtained by contacting thelocal community mental health centre.Community Mental <strong>Health</strong> AdvisoriesMental <strong>Health</strong> and Addictions Advisory Groups provide an opportunity for stakeholders (mental health consumers,family members, and community agency representatives) to discuss issues with <strong>Fraser</strong> <strong>Health</strong> staff related to thedevelopment, implementation and evaluation of MH&A services on a local or regional basis. Most advisoriesare chaired by a consumer or family member and meet on a monthly basis. The advisories provide a forum todiscuss systemic issues and identify areas of improvement in service delivery. In addition they are able to liaise withgovernment and community agencies to improve the responsiveness of those services to the needs of consumers andtheir families. Advisories are also able to promote public education about mental health and addictions issues.ÎÎFor contact information go to www.fraserhealth.ca/Services/Mental<strong>Health</strong>andAddictionsLinks to Mental <strong>Health</strong> ResourcesÎÎ www.heretohelp.bc.caÎÎ www.cmha.caÎÎ www.camh.netÎÎÎÎwww.bckidsmentalhealth.orgwww.psychosissucks.ca20<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services
MENTAL HEALTH SERVICESContracted AgenciesAbbotsford Community Services SocietyAbbotsford Seniors Peer Support ServicesAnxiety Disorders Association of BCBC Schizophrenia SocietyBurnaby Family Life InstituteBurnaby Mental Wealth SocietyCanadian Mental <strong>Health</strong> AssociationCommunitas Supportive Care SocietyCreative Centre SocietyCythera Transition House SocietyDelta Advocates for Community Mental<strong>Health</strong>District of Mission, Parks and RecDIVERSECity Community ResourcesSocietyDouglas CollegeDr. Fritz & AssociatesFamily Education & Support CentreFamily Services of Greater Vancouver<strong>Fraser</strong> North Community VolunteerConnections<strong>Fraser</strong>side Community Services SocietyGoverning Council ofthe Salvation Army in CanadaL & T Rehab ServicesLookout Emergency Aid SocietyMaple Ridge/Pitt Meadows CommunityServicesMinistry of Children &Family DevelopmentMission Clubhouse SocietyMission Community ServicesMood Disorders Association of BCMotivation Powerand Achievement SocietyMR/PM Parks & LeisureNew View SocietyNewton Advocacy Group SocietyOptions: Services to Communities SocietyPacific Post Partum Support SocietyPioneer Community Living AssociationPLEA Community Services Society of BC(FolkStone)Progressive Housing SocietyShare Family & Community ServicesSocietyStepping Stone Community ServicesSurrey Community Services SocietyTownship of LangleyTriCity Women’s Resource SocietyAntonio C.L. Inc.Argyll Lodge Ltd.Azimuth <strong>Health</strong> Program ManagementLtd.Barclay Lodge LtdBeatrix CalixterioBisha Enterprises Inc.Bonnie Lee Barker & Gordon TrelinskiBresco Enterprises Ltd.Brookswood Court SpecializedAdult Care Facility Ltd.Buena Vista Lodge Ltd.Chelsey House 2003 Ltd.Correa Holdings Ltd.Crestlene Lodge Ltd.Delta Lodge Ltd.Delta View Habilitation CentreEverett Rest Home LtdGood Shepherd Lodge Inc.H & H Total Care Services Inc.Hazelmere Lodge Ltd.Hillside Lodge Ltd.Horniblow Family CareI.D.S. Management Ltd.Ilapogu Investments Inc.Invicta Enterprises IncorporatedJosephine Care Home Inc.Lorna M. KingMeadowview ManorMei Enterprise Ltd.Merv Holmes & Gail BedfordMurrayville Manor Specialized Adult CareFacility Ltd.New Dimensions Care Inc.Norma Thompson HomePinetree Lodge Ltd.Piza Holdings Inc.Pungun Holding Ltd.Scottsdale House Enterprises Ltd.Skipton Holding Ltd.Trejan Lodge LtdVCPC Holdings Ltd.Victoria Rest Home LtdWaddell’s Haven Guest Home Ltd.<strong>Fraser</strong> <strong>Health</strong> Mental <strong>Health</strong> and Addiction Services 21
Mental <strong>Health</strong> & AddictionsHEALTHY LIFESTYLE ACTION PLAN*MHXX*MHXX104077ARev: Jul 13/10Page: 1 of 2My Action Plan for a <strong>Health</strong>y LifestyleToday's date:My Primary <strong>Health</strong> Care Provider:My focus is on (check any or all):<strong>Health</strong>yeatingPhysicalactivity<strong>Health</strong>ychoices• Eating 7-10 servings of • Getting a minium of 30• Having a positive outlookfruits and veggies per dayminutes of exercise per day • Managing my stress levels• Eating from all food groups, • Doing endurance activities • Having social supportslimited fats and sugars(walking, running, sports)(family, friends)• Eating smaller portion sizes • Doing strength activities• Having fun and making time• Eating the right number of(lifting weights)for leisureservings• Flexibility activities• Getting adequate rest• Reading food labels• Drinking water(stretching, yoga)• Being smoke-freeTo improve my health I would like to:Goal #1Target:Support I need:Goal #2Target:Support I need:Goal #3Target:Support I need:Target date:Target date:Target date:
HEALTHY LIFESTYLE ACTION PLAN Cont'dPage: 2 of 2Any obstacles that may keep me from reaching my goal:Progress:Date:Goal #1:Goal #2:Goal #3:Date:Goal #1:Goal #2:Goal #3:Date:Goal #1:Goal #2:Goal #3:
Client name: _______________________________METABOLIC MONITORING FORMMENTAL HEALTH AND SUBSTANCE USE (MHSU)PHN: _____________________________________DOB (dd/mm/yy): ________________ Age: _______Gender: Male Female Unknown/undifferen.Psychiatrist: _______________________________MHXX104076B Rev: Apr. 11/11Page: 1 of 3VULNERABILITIES – To be completed at baseline / first screeningHigh riskLow riskPersonal medical history Diabetes No or unknown historyHigh cholesterolHypertensionHeart diseaseOther: _________________________No or unknown historyNo or unknown historyNo or unknown historyNo or unknown historyFamily medical history Diabetes No or unknown history(First-degree relative – i.e.,High cholesterolNo or unknown historymother/father/sibling)HypertensionNo or unknown historyHeart diseaseOther: _________________________Ethnicity Aboriginal Arab(Origin/descent should be basis forAfricanCaucasianclassification, not country of residence)AsianHispanicSouth AsianTobacco use Current user Non-userPhysical activityNutrition(STC = Starting the Conversation tool)Quit < 7 days agoQuit ≥ 7 days ago< 30 min / day or 150 min / week or noappreciable exercise (sedentary)No or unknown historyNo or unknown history≥ 30 min / dayHigher STC score (8 – 16) Lower STC score (0 - 8)ADDITIONAL VULNERABILTIES FOR CVD AND DIABETESMale genderPrint Shop #261926Cardiovasculardisease riskFamily history of premature coronary heart disease (first degree relative - male 45 years) Special populations (e.g., low socioeconomic status, major mental disorders, treatmentwith protease inhibitor, glucocoricoids, or psychotropic medication treatment) History of impaired glucose tolerance or impaired fasting glucose (associatedwith insulin resistance)Presence of complications associated with diabetesHistory of vascular disease (coronary, cerebrovascular or peripheral)Female: History of gestational diabetes or delivery of macrosomic infantFemale: Polycystic ovary syndrome
This page is intentionally blank and acts as a back page space filler only
Client name: _______________________________METABOLIC MONITORING FORMMENTAL HEALTH AND SUBSTANCE USE (MHSU)PHN: _____________________________________DOB (dd/mm/yy): ________________ Age: _______Gender: Male Female Unknown/undifferen.Psychiatrist: _______________________________MHXX104076B Rev: Apr. 11/11Page: 2 of 3GPNo GP, refer to:METABOLIC MONITORINGRisk factor Defining level BaselineDateDateDateDateDateInitialsInitialsInitialsInitialsInitialsInitialsTest date (dd/mm/yy) Moderate riskWeight(kg / lbs) Waistcircumference Bloodpressure Triglycerides FastingHDLcholesterol≥ 5% increasefrom baselineM > 102cm/40inF > 88cm/35inTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskAt risk At risk At risk At risk At risk At risk> 140/90, or> 130/80 ifdiabetes /disease* Tx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At risk> 1.7 mmol/LMF≤ 1.03mmol/L≤ 1.29mmol/LTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskHigh risk FastingglucoseMetSdiagnosisPsychotropicmedicationsDiabetes-DKA checklist> 5.6 mmol/L≥ of factorsNew start/changein last 3 monthsSigns andsymptomsTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskMetS MetS MetS MetS MetS MetSNewChangeAt riskNo S&SNewChangeAt riskNo S&SNewChangeAt riskNo S&SNewChangeAt riskNo S&SFollow up (as per FH MHSU guidelines – risk levels and associated monitoring frequencies)Current risk(low / moderate / high)Repeat PHYSICAL MEASURESin X months?Repeat LABS in X months?NewChangeAt riskNo S&SNewChangeAt riskNo S&SReviewed with physician /physician confirmation (signature)Referred to GP / primary careprovider (Y/ N)DKA: diabetic ketoacidosis; Initials: sign initials; MetS: metabolic syndrome; S&S: Signs and symptoms; Tx: Treatment (meds for risk factor)* if client has diabetes, renal disease or other target organ damage (i.e., cerebrovascular disease, coronary heart disease (CHD), leftventricular hypertrophy (LVH), chronic kidney disease (CKD), peripheral vascular disease and hypertensive retinopathy.Next page
METABOLIC MONITORING FORMMENTAL HEALTH AND SUBSTANCE USE (MHSU)Client name: _______________________________Page: 3 of 3Additional laboratory investigations as per risk level and BC Mental <strong>Health</strong> and Addictions recommendationsRisk factor Risk level BaselineTest date (dd/mm/yy) DateDateDateDateDateInitialsInitialsInitialsInitialsInitialsInitialsTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskTx At risk Tx At risk Tx At risk Tx At risk Tx At risk Tx At riskDateLifestyle factors (health lifestyle actionplan, nutrition, physical activity/ FITT, smoking)DateEducation provided (monitoring, heart disease, DKA/diabetes, BP, cholesterol, smoking cessation, lifestyle)DateReferrals made (send this form with allreferrals, transfers and discharges)DateNotesHigh risk = Any of the following conditions are present: 1)On psychotropic medications AND presence of any riskfactors or on treatment for any risk factors; OR 2) New starton psychotropic medications with high or moderate risk ofweight gain (see Tables 7 and 8 in guidelines, e.g.,atypicals/second-generation antipsychotics)Moderate risk = Any of the following conditions arepresent: 1) New start on all other psychotropic medications(those with low risk of weight gain – see Tables 7 and 8 inguidelines); OR 2) On psychotropic medications but nochanges in past 3 months; OR 3) Greater than or equal to5% increase in weight seenLow risk = No metabolicrisk factors present; ANDnot on psychotropicmedications
Taking Wellness to Heart! Metabolic MonitoringWHO: All Mental <strong>Health</strong> andSubstance Use clientsWHEN: Face to face, when file is opened or at earliest opportunity (i.e., when it is therapeuticallyappropriate to do so), and prior to initiating psychotropic medication treatment.Screening / intakeFrontline MHSUClinician take baselinehealth and risk levelPrevention, intervention, and ongoing monitoring and maintenanceMHSU Clinician and <strong>Physician</strong> review baselinehealth and risk level and follow up as appropriateMHSU Clinician and <strong>Physician</strong> repeat screening andfollow up regularly1. At baseline, retrievevulnerabilitiesinformation.2. Take and/or recordbaseline measures:waist circumference,weight, blood pressureand recent lab work.3. Retrieve medicationinformation.4. Complete Diabetes-DKA checklist.5. If unable to retrieveinfo, look for alternativeways, flag for follow up,and document.6. Complete follow upsection of form: currentrisk, repeat measuresin X months, etc.MHSU Clinician follow up:1. Determine risk levels andmonitoring frequenciesand confirm with andnotify MHSU Psychiatrist/<strong>Physician</strong> of risk.2. Provide or reviewparticipation in healthylifestyle education.3. Provide smokingcessation education and/or brief intervention (ifrequired).4. Schedule next monitoringappointment.5. Share information withrelevant parties (e.g.,GP).MHSU Psychiatrist/<strong>Physician</strong> follow up:1. Determine/confirmrisk level andmonitoringfrequencies.2. Treat and/or referto GP/specialist,as required.3. Requests labtests.4. Consider riskbenefitofmedicationtherapy.5. Share informationwith relevantparties (e.g., GP).HIGH RISKMODERATERISKLOW RISKPhysicalmeasuresRepeat monthlyfor 3 months anduntil stable, then3-monthly.Repeat 3-monthly.Repeat annually.LabinvestigationsRepeat 3-monthlyfor 6 months anduntil stable, thenannually.Annually; if ≥ 5%weight increase,repeat 6-monthlyuntil stable.Repeat annually.1. Continue to treat and/or refer to GP/specialist, asrequired.2. Continue to provide or review participation in healthylifestyle education.3. Continue smoking cessation education and/ or briefintervention (if required).4. Continue to share information with relevant parties(e.g., GP).HEALTHY LIFESTYLE EDUCATION: At each stage/review point, clients should be referred to healthy lifestyleeducation and/or their participation in education should be reviewed for opportunities to be enhancedRevised April 11, 2011 Page 1 of 2 Mental <strong>Health</strong> and Substance Use
Diagnostic Criteria and Risk Level DefinitionsCriteria for clinical diagnosis of Metabolic SyndromeClinical diagnosis of metabolic syndrome = Any three (3) or more of fiverisk factors are present:Risk factor Defining levelRelated medicalconditionElevated waist Male: ≥ 102 cm (40 inches) Abdominal obesitycircumference a,b Female: ≥ 88 cm (35 inches)Elevated bloodpressureIf no co-morbid conditions: >140/90If self measured: > 135/85If client has diabetes, renaldisease or other target organdamage c : > 130/80Hypertensionor drug treatment forhypertensionElevatedtriglyceridesReduced highdensitylipoproteincholesterol (HDL-C)Elevated fastingglucose e(antihypertensive)> 1.7 mmol/LHigh cholesterol /or drug treatment for elevated Dyslipidemiatriglycerides dMale: < 1.03 mmol/L High cholesterol /Female: < 1.29 mmol/L Dyslipidemiaor drug treatment for reducedHDL-C d≥ 5.6 mmol/L or drug treatmentfor elevated glucoseDiabetesNotes:a If waist circumference is difficult to obtain, abdominal obesity may be ‘eye-balled’or if BMI is ≥ 30 kg/m 2 , it can be initially assumed.b The <strong>Health</strong> Canada defining levels for waist circumference are recommended foruse with all Canadian adults (except for pregnant and lactating women) and areused in these guidelines. Ethnic-specific data is available in the guidelines.c Target organ damage includes: cerebrovascular disease, coronary heart disease(CHD), left ventricular hypertrophy (LVH), chronic kidney disease (CKD),peripheral vascular disease and hypertensive retinopathy.d The most commonly used drugs for elevated triglycerides and reduced HDL-Care fibrates and nicotinic acid. A patient taking one of these drugs can bepresumed to have high triglycerides and low HDL-C.e Most with type 2 diabetes mellitus will have metabolic syndrome by this criteria.Risk levels definitionsRisk levelHigh riskModerateriskLow riskDefinitionAny of the following conditions are present:• On psychotropic mes AND presence of any risk factors or ontreatment for any risk factors; OR• New start on psychotropic medications with high or moderaterisk of weight gain (see Tables 7 and 8)Any of the following conditions are present:• New start on all other psychotropic meds (those with low risk ofweight gain – see Tables 7 and 8); OR• On psychotropic medications but no changes in past 3 months 1 ;OR• Greater than or equal to 5% increase in weight seen 2• No metabolic risk factors present; AND not on psychotropicmedicationsRevised April 11, 2011 Page 2 of 2 Mental <strong>Health</strong> and Substance Use
Mental <strong>Health</strong> and Substance Use Revised April 11, 2011CLINICAL ALGORITHM FOR METABOLIC MONITORINGLEGENDWithin normal range: No actionFurther action requiredTreatment requiredPhysical measuresABDOMINAL OBESITYWeightWaistcircumference*WeightWaistcircumference*BLOOD PRESSURE< 5% increase in weight from baseline< 102 cm/40 in or < 88 cm/35 in> 5% increase in weight from baseline≥ 102 cm/40 in or < 88 cm/35 inscreening & assessment* See Guidelines Table 1 for ethnic-specific guidelines< 140/90 mmHg (if no co-morbid conditions)> 140/90 mmHg (> 135/85 if self-measured, > 130/80 ifdiabetes, renal disease or other target organ disease)Drug treatment for hypertension (antihypertensive)If LOW RISKIf MODERATE RISKIf HIGH RISKIf LOW RISKIf MODERATE RISKIf HIGH RISKprevention & interventionRepeat measurement and treat / referas per BC overweight and obesityguidelinesRepeat measurement and treat / referas per BC hypertension guidelinesRepeat annuallyRepeat 3-monthlyRepeat annuallyRepeat 3-monthlymonitoring• Repeat monthly for 3 months and until stable,• Then 3-monthly• Repeat monthly for 3 months and until stable,• Then 3-monthlyFASTING LIPIDSTriglycerides (TG)≤ 1.7 mmol/LIf LOW RISKRepeat annuallyLaboratory investigationsHDL-cholesterol ≥ 1.03 mmol/L or ≥ 1.29 mmol/LTriglycerides (TG) > 1.7 mmol/LHDL-cholesterol < 1,03 mmol/L or < 1.29 mmol/LDrug treatment for dyslipidemiaFASTING BLOOD GLUCOSEFasting plasma < 5.6 mmol/Lglucose (FPG) 5.6 – 6.9 mmol/L≥ 7.0 mmol/LDrug treatment for elevated glucoseIf MODERATE RISKIf HIGH RISKIf LOW RISKIf MODERATE RISKIf HIGH RISKTreat / refer as perBC cardiovascular disease guidelinesTreat / refer as perBC diabetes care guidelines• Annually• If ≥ 5% weight increase or if lipids abnormal, repeat 6-• monthly until stable, then annually• Repeat 3-monthly for 6 months and until stable,• Then annuallyRepeat annually• Annually• If ≥ 5% weight increase, repeat 6-monthly until stable,• then annually• Repeat 3-monthly for 6 months and until stable,• Then annually<strong>Health</strong>y lifestyle education: At each stage/review point, clients should be referred to healthy lifestyle education and/or their participation in healthy lifestyle education should be reviewed
Mental <strong>Health</strong> and Substance Use Revised April 11, 2011Criteria for clinical diagnosis of Metabolic SyndromeClinical diagnosis of metabolic syndrome = Any three (3) or more of five risk factorsare present:Risk factor Defining levelRelated medicalconditionElevated waist Male: ≥ 102 cm (40 inches) Abdominal obesitycircumference a,b Female: ≥ 88 cm (35 inches)Elevated bloodpressureIf no co-morbid conditions: > 140/90If self measured: > 135/85If client has diabetes, renal disease orother target organ damage c : >130/80Hypertensionor drug treatment hypertensionElevatedtriglyceridesReduced highdensitylipoproteincholesterol (HDL-C)Elevated fastingglucose eHigh cholesterol /High cholesterol /(antihypertensive)> 1.7 mmol/Ltriglycerides dor drug treatment for elevatedDyslipidemiaMale: < 1.03 mmol/Lor drug treatment for reduced HDL-C dFemale: < 1.29 mmol/LDyslipidemia≥ 5.6 mmol/L or drug treatment forelevated glucoseDiabetesNotes:a If waist circumference is difficult to obtain, abdominal obesity may be ‘eye-balled’ or if BMI is ≥30 kg/m 2 , it can be initially assumed.b The <strong>Health</strong> Canada defining levels for waist circumference are recommended for use with allCanadian adults (except for pregnant and lactating women) and are used in these guidelines.Ethnic-specific data is available in the guidelines.c Target organ damage includes: cerebrovascular disease, coronary heart disease (CHD), leftventricular hypertrophy (LVH), chronic kidney disease (CKD), peripheral vascular disease andhypertensive retinopathy.d The most commonly used drugs for elevated triglycerides and reduced HDL-C are fibrates andnicotinic acid. A patient taking one of these drugs can be presumed to have high triglyceridesand low HDL-C.e Most with type 2 diabetes mellitus will have metabolic syndrome by this criteria.Follow up legendWithin normal range:No actionNo follow up required with respect to the specific risk factorFurther action required Refer to <strong>Physician</strong> for follow up, as per BC guidelinesTreatment required<strong>Physician</strong> treatment requiredRisk levels and associated recommended monitoring frequenciesRisk level DefinitionAny of the following conditions are present:High risk • On psychotropic meds AND presence of any risk factors or on treatment for any risk factors; OR• New start on psychotropic medications with high or moderate risk of weight gain (see Tables 7 and 8)Any of the following conditions are present:Moderaterisk• New start on all other psychotropic meds (those with low risk of weight gain – see Tables 7 and 8); OR• On psychotropic medications but no changes in past 3 months 1 ; OR• Greater than or equal to 5% increase in weight seen 2Low risk • No metabolic risk factors present; AND not on psychotropic medicationsRisk factorFrequency of monitoring by risk level 4High risk Moderate risk Low riskWeight, waistcircumferenceBC overweight andobesity guidelines• Baseline 5• Monthly for 3 months and untilstable• Then 3-monthly• Baseline 5• Then 3-monthly• Baseline 5• ThenannuallyBlood pressureBC hypertensionguidelinesLipids(triglycerides,HDL-C)BC cardiovasculardisease guidelinesFasting glucose(and Hb1Ac, ifphysicianrequests)• Baseline 5• Monthly for 3 months and untilstable• Then 3-monthly• Baseline 5• 3-monthly for 6 months and untilstable• Then annually• Baseline 5• 3-monthly for 6 months and untilstable• Then annuallyIf abnormal, screen/treat/refer as perBC diabetes care guidelines andscreening algorithmDiabetes-DKA • Baseline 5checklist 3 • Then monthly or at every visit• Baseline 5• Then 3-monthlyBaseline 5 (if no access to results fromprevious 6 months 6 ) and:• If ≥ 5% weight increase 2 or if lipidsabnormal: 6-monthly until stable, thenannually• Otherwise, annuallyBaseline 5 (if no access to results fromprevious 6 months 6 ) and:• If ≥ 5% weight increase 2 : 6-monthly untilstable, then annually• If fasting glucose abnormal: Screen/treat/refer as per as per BC diabetes careguidelines and screening algorithm• Otherwise, annually• Baseline 5• Then 3-monthly or at every visit• Baseline 5• Thenannually• Baseline 5• Thenannually• Baseline 5• Thenannually• Baseline 5• ThenannuallyNotes:1. Changes in psychotropic medications = Significant increase in dose proportional to baseline or change in medications.2. An unhealthy or risky weight gain = A rapid increase in weight (≥ 5%) over a short period of time.3. DKA = Diabetic ketoacidosis. Please see Table 9 for the Diabetes and DKA checklist.4. These are recommended monitoring guidelines. Ordering of monitoring is based on clinical assessment and exceptions may be justified byclinical circumstances. The frequency of testing depends on the individual client and the physician's assessment.5. Baseline is ideally at pre-treatment baseline, i.e., before or within 7 days of new medication start.6. Previous lab work should be no older than 6 months and if there is any reason for concern about previous lab work (e.g., changes inmetabolic risk factors or in other risk factors), lab work should be repeated to establish baseline, or at any point.
Collaborative Care <strong>Process</strong> Map-Episode of Care for MHSU Clients Referred by PCPs (Primary Care Providers)[DRAFT VERSION 11] Mar 8, 2012ReferralIntakeOngoing TreatmentDischarge/TransitionReferral to RapidAccess Clinic (RAC)for Psych ConsultReferral to Mental<strong>Health</strong> &Substance Use(MHSU) CentreCommunityMHSU ServicesReferral FormReasons for Referral:non-urgent psychiatrist referralpsychiatric assessmentCrisis interventionShort term stabilizationAccess to therapy (i.e. groups)Intake assessmentCase consultationCase managementReferral to community servicesSubstance Use servicesOutreachEarly psychosis InterventionReferral pre-registered /loggedby MHSU admin staffReferral screened /triagedby MHSU clinicianPCP receivesconfirmation of receiptof referral request byphone call or letter fromclinician within 5business days indicatingdisposition of referral.When possible, face toface meeting arrangedwith client &/or GP.Unsuitable Client:Recommendationto appropriateservicesSuitable Client:Assigned toMHSU team orRACReferral to otherresourcesPsychiatrist Assessmentand Treatment Plan /RecommendationsCopy of Assessmentand Treatment PlanLetteracknowledgingreceipt of referraland indicatingdisposition ofreferral and type ofservice offered (ieface to face, phonecall, etc)Ongoing TreatmentConsult ReportPCP/Clinician maycontact psychiatrist byphone for follow upquestions/advice (seeVIHA protocol)Case review Q6 months(documented on RecoveryPlan Review)Copy of Recovery PlanReviewUnplannedDischarge:Outreach visit orletter sent due toloss of contactPlanned Discharge:If end of treatment,client relocates toanother community, etc.then PCP alerted via p/cletter or fax requestingconsultationPreparing for discharge:Pre-Discharge meetingconsultation with PCPDischarge Planning –Plan transition back toPCP careFile keptpending up to 1month’s timeLetter or phonecall to PCP forplan of actionTermination SummaryInclude name and phone number ofperson for PCP to contact for questionsor advice if neededCopy of Termination SummaryAfter Discharge:Follow-up with PCP & patient in 1 month’stime (file left pending at times or closed inconsultation with PCPNote:Community Patient Conferencing Fees: 14016 and 14046 Compensates GP whenconferencing for the creation of a coordinated clinical action plan for patients living in thecommunIty or facility based, with more complex needs, including patients with mentalhealth conditions. The following codes may be utilized at various points in the episode ofcare for MHSU patients:GP Mental<strong>Health</strong>Planning Fee14043CounselingVisits:Fee code 14044,14045, 14046, -14048GP CommunityPatientConferencing Fee14016GP Telephone/Email follow upManagement fee14079
Fax requests in Victoria to 250 405-3605 or, from elsewhere in BC, to 1-800-609-4884 (toll free).OR mail requests to: PharmaCare, Box 9652 Stn Prov Govt, Victoria, BC V8W 9P4section 1 – prescriber informationname & mailing address mail confirmationpharmacarespecial authority requestThis facsimile is Doctor-Patient privileged and contains confidential information intended only for PharmaCare. Any other distribution, copying or disclosure is strictly prohibited.If you have received this fax in error, please write “MIS-DIRECTED” across the front of the form and fax toll-free to 1 800 609-4884, then destroy the pages received in error.Use this form to request: • Exemptions to the Reference Drug Program (RDP)• Exemptions to the Low-Cost Alternative Program (LCA)• Limited Coverage Drugs (Please see step 4 on reverse)application dateForms with information missingwill be returned for completion.Should approval be granted for this Special <strong>Authority</strong> request, PharmaCare’s authorization is solely for the purpose of providing prescription benefit for the cost of the requestedmedication. PharmaCare makes no representation about the suitability of the requested medication for the patient’s, or any other, medical condition or problem.Please see reverse for category definitions and instructions on completing this form.yyyy mm dd area codePrescriber’s telephone #Prescriber’s college ID #Prescriber’s fax #area codesection 2 – patient informationpersonal health number (PHN)patient (family) namedate of birth (YYYY / mm / DD)patient (given) name(s)section 3 – Medication detail informationrequested drug exemption (indicate both medication and dosage requested) new Request renewalindication(s) for special authorityTreatment Failure on Reference Drug /Low-Cost Alternative / First-Line Agent(please list medications tried)Adverse Reaction to Reference Drug /Low-Cost Alternative / First-Line Agent (please listmedications tried and specify adverse reaction)Drug / Drug Interaction with Reference Drugor First-Line Agent (please list both drugs thatmay interact)Diagnosis and other patient-specific indicatorsPersonal information on this form is collected for the operations of the Ministry of <strong>Health</strong>. The Ministry will use the information in the decision to provide PharmaCare benefits for themedication requested, and for implementation, monitoring and evaluation of this and other Ministry programs, and for the management and planning of the health system generally.Personal information will be used and disclosed in accordance with the privacy protection provisions of the Freedom of Information and Protection of Privacy Act. If you have anyquestions about the collection of this information, call <strong>Health</strong> Insurance BC from Vancouver at 1-604-683-7151 or from elsewhere in BC toll free at 1-800-663-7100 and ask to consulta pharmacist concerning the Special <strong>Authority</strong> process.I have discussed with the patient the purpose of the release of the patient’s information to PharmaCare to obtain Special <strong>Authority</strong> forprescription benefit and for the purposes set out above.Presciber’s Signature (Mandatory)PharmaCare may request additional documentation to support this Special <strong>Authority</strong> request.Patient Signature (Optional)pharmacare use onlyeffective dateYYYY / MM / DDDuration of therapy /termination dateYYYY / MM / DDHLTH 5328 Rev. 2010/03/02
Fax the Special <strong>Authority</strong> Request to:victoria 250 405-3605Rest of BC (toll-free) 1 800 609-4884OR Mail to:PharmaCarePO Box 9652 Stn Prov Govt, Victoria BC V8W 9P4Please allow 48 hours (excluding weekends) for RDP Exemptions,and two weeks for LCA Exemptions and Limited Coverage Drugs.Completing the Special <strong>Authority</strong> Request form:1. Use one form for each patient and each drug.2. Attention to the information requirements ensures a complete and timely review. Requests containing insufficientinformation will be returned to the physician. All sections of the form must be completed.3. Extension of Coverage: If you anticipate that a patient will require the product beyond the approval period, applyfor an extension of coverage at least two (2) weeks before expiration. (Note: Coverage is not continuedautomatically.) Approval of this request should be in place before the first prescription is filled. Requests forextensions should include a comment on the patient’s response/progress on therapy.4. Some medications require the completion of a drug-specific Special <strong>Authority</strong> request form (e.g., cyclosporineand leflunomide for rheumatoid arthritis, DMARDs for Multiple Sclerosis, interferon alpha and lamivudine forHepatitis B, low molecular weight heparin, pegylated interferon/ribavirin for Hepatitis C, proton pumpinhibitors, etc.).Please note:• Results are provided automatically by mail or fax unless otherwise requested.• Actual coverage is subject to the usual rules of the patient’s PharmaCare plan. Approval does not necessarilyimply 100% coverage.• All BC residents registered with the Ministry of <strong>Health</strong> are eligible for PharmaCare coverage.
• • o
o o o o o o o • • • o o o o o o o o •