Our Health Care Delusion – Macleans - The Canadian Association ...
Our Health Care Delusion – Macleans - The Canadian Association ...
Our Health Care Delusion – Macleans - The Canadian Association ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
NationalSpecial report<strong>Our</strong> health care delusionThink we have the best health care in the world? Think again. One studyranked us dead last in timeliness and quality of care. Ken MacQueen reports.On Jan. 26, Maclean’s is hosting “<strong>Health</strong> <strong>Care</strong>in Canada: Time to Rebuild Medicare,” a townhall discussion at the Sir James Dunn <strong>The</strong>atre,Dalhousie University, Halifax. <strong>The</strong> event,in conjunction with the <strong>Canadian</strong>Medical <strong>Association</strong>, will be broadcastlive by CPAC. <strong>The</strong> conversationon health reform continues in thecoming months in the magazine andat town halls in Toronto, Edmonton,Vancouver and Ottawa.A distraught 41-year-old man fromWest Kelowna, B.C., arrived at the emergencydepartment of Kelowna General Hospital onthe night of Dec. 28. “He was broken mentally,”his wife later told the local Daily Courier.“He wanted help.” By her account, hewaited 90 minutes without seeing a doctor,SYSTEMCRITIC LPART 1 OF 6minor by today’s emergency room standards.Kelowna RCMP put the wait at just 45 minutes.Regardless, he snapped, warning staffthat he’d drive his truck into the hospitalif he didn’t get treatment. Whenthreats didn’t get results, he stormedout and returned at the wheel ofhis Chevy Blazer. As promised, hesmashed through the ER’s doubledoors, narrowly missing two elderlypeople (one assumes they were elderlybefore their wait in emergency) and came toa halt in a hospital hallway.Police arrived to find him waiting co-operativelyin his truck. <strong>The</strong> bed he was assignedthat night was in the RCMP detachment cell;he faces several charges including dangerousoperation of a motor vehicle. While his strategywas extreme, his cry for attention reson-ates with many who’ve had the misfortuneto trade germs and waste time in one of Canada’soverstressed emergency wards.It’s a <strong>Canadian</strong> conceit that ours is one ofthe best public health care systems in theworld, a defining characteristic of nationhood;something that separates us from theAmericans. In a poll by Angus Reid PublicOpinion in June, 69 per cent of <strong>Canadian</strong>ssaid they’re proud of the health care system,edging out the state of <strong>Canadian</strong> democracy,multiculturalism and bilingualism.Yet the reality, based on any number ofinternational comparisons, shows that pridein a supposedly world-beating standard ofcare is often misplaced, an “illusion,” as LiberalMP and medical doctor Keith Martinputs it. <strong>The</strong> sorry state of the nation’s emergencywards is just one indicator of troublePeter Power/Toronto Star18 JANUARY 31, 2011
Dave Trifunov/CP; Peter Lee/Waterloo Region Record/CPtoday and trouble to come. ERs are just “thecanary in the coal mine,” says Dr. John Ross,Nova Scotia’s adviser on emergency care.Martin, a former family and emergencyroom doctor and an MP from VancouverIsland, has been saying as much since heentered federal politics 17 years ago as aReform party member. He practised medicinepart-time until about three years ago,experiencing the same things that first spurredhim into politics: the indignity of examiningpatients on gurneys in hospital hallways;people enduring such agonizing waits for hipor knee replacements that they suffered heartattacks; tumours that grew to inoperable sizesas people waited months for diagnostic scans.“Those,” he says, “are the casualties of ourhealth care system, and the casualties of theinaction of modernizing the system, thatOverused ERs: A man in Kelowna drove into the ER; five million <strong>Canadian</strong>s don’t have a doctorpeople don’t talk about.”Emergency wards are all too often the firstpoint of contact with the health care system,a problem exacerbated by the fact that fivemillion <strong>Canadian</strong>s don’t have a family physician,and because acute-care beds are oftenstuffed with elderly patients who would bebetter served in long-term care facilities.Often the waits are excruciating. For a manin the throes of a mental breakdown, drivingto, and through, the ER of Kelowna Generalshould have been the last, worst option.“He was at the end of his rope,” his wife said.“You can’t see a psychiatrist. It takes a whileto get an appointment. That’s why peoplego to hospital.”And what they often find in maxed-out ERsis a chaotic environment and waits, of six,eight hours and more. <strong>The</strong> consequences canbe deadly. In Edmonton’s Royal AlexandraHospital this September, Shayne Hay reportedto the hospital’s emergency ward, telling staffhe was suicidal. He was placed in a room onan emergency stretcher and checked periodically,though repeated requests to see a counsellorwent unanswered, his family says. Some12 hours later he was found dead, hangingfrom a strap of his backpack. In Montreal,long waits in the ER at Maisonneuve-Rosemonthospital were blamed by families forcontributing to the deaths of two people lastyear. Mariette Fournier, 86, spent four dayson a stretcher in the hallway waiting for a bedin the geriatric department. She contractedpneumonia, developed a blood clot, and diedon Feb. 23, a day after finally getting a bed.That same month, 75-year-old MieczyslawFigiel died beside the triage nursing station,with his daughter banging on the station’swindow as he gasped for breath. <strong>The</strong> ER wasat 180 per cent capacity.<strong>The</strong> problems in ERs across the countryare symptomatic of a wider malaise. Numerousinternational comparisons suggest ouriconic universal health system is not the worldleader of the national imagination. “<strong>Canadian</strong>sare selling themselves short,” says areport card produced last June by the WaitTime Alliance, comprised of 14 national medicalassociations. “Unfortunately, Canada isone of the few developed countries with universalhealth care systems where patients faceMACLEAN’S MAGAZINE 19
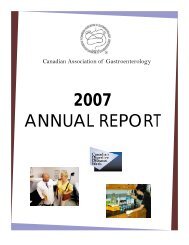
long waits for necessary care,” says the report,aptly titled “No Time for Complacency.”More and more voices are calling for healthcare to be put on the agenda. Former Toryprime minister Brian Mulroney and formerLiberal senator Michael Kirby alluded recentlyto the challenge of a badly needed “nationaladult conversation” on health reform. “Unfortunately,intelligent debate about what shouldbe done has basically ground to a halt byincendiary claims that any attempt to updatethe system amounts to treason—a repudiationof sacred <strong>Canadian</strong> values.” <strong>The</strong> <strong>Canadian</strong>Medical <strong>Association</strong> (CMA), representing74,000 doctors, has undertaken a massivereview and public consultation, including aseries of televised town hall meetings acrossCanada. <strong>The</strong> first, in conjunction with Maclean’sand CPAC, is set for Halifax on Jan. 26.“I think it’s time for all <strong>Canadian</strong>s to get involvedin this discussion,” says CMA president Dr.Jeff Turnbull, who sees many of the fault lines—maxed-out emergency wards, cancelled surgeries,strained budgets, frustrated patientsand stressed staff—at the Ottawa Hospitalwhere he is chief of staff.<strong>The</strong> evidence of a looming crisis comes notfrom comparing <strong>Canadian</strong> to American healthcare—a unique and expensive beast—but bytaking a world view, as assessed by the ParisbasedOrganisation for Economic Co-operationand Development (OECD),the U.S.-based CommonwealthFund, the <strong>Health</strong>Council of Canada and othergroups. “We believe our ownrhetoric around ‘we’re thebest in the world.’ What these[international] surveys andour own work are telling usis: no,” says John Abbott, CEO of the <strong>Health</strong>Council, an independent national agencymandated to monitor and encourage healthreform. “If you look at cost, we’re maybe inthe middle of the pack. If you’re looking atoverall quality indicators, quality of life, longevity,on these factors we can learn fromothers. When you look at how we can accessthe system in a reasonable and timely way, weNationalTurnbull sees firsthandmaxed-out Ers,cancelled surgeries,frustrated patientsand stressed staffrate quite low,” he says.Neither Canada nor theU.S. come close to being thegold standard for healthcare. Canada placed secondlast in a comparison lastJune of seven countries bythe Commonwealth Fund,a U.S. charity that promoteshealth policy reform. <strong>The</strong>U.S. ranked last, scoring dismallyon access, efficiency,equity and quality care, despiteper-capita healthspending of US$7,290. That’svastly more than the spendingin top-ranked countries:the Netherlands, the U.K.and Australia. (Germanyranked fourth, New Zealandfifth.) Canada, sixth in results,was the second mostexpensive at US$3,895 percapita.<strong>Canadian</strong>s scored well onleading “long, healthy productive lives,” butit was mid-pack or worse on every other measure.<strong>The</strong> report, based on national statistics,and patient and doctor surveys, shows Canadascored poorly on chronic care and use ofelectronic records. <strong>Canadian</strong> patients reportedthe second highest rate ofperceived medical errors.Canada was dead last on twokey measures: quality care,defined as “effective, safe,coordinated and patientcentred,”and timeliness ofcare. While cost prohibitsmillions of uninsured Americansfrom accessing needed health care, waittimes, not finances, are the impediment inthe U.K. and Canada, the report says. “<strong>The</strong>reis a frequent misperception that such tradeoffsare inevitable; but patients in the Netherlandsand Germany have quick access tospecialty services and face little out-of-pocketcosts,” the report notes. Poor access to primarycare contributes to Canada’s overuse ofCall for reform: <strong>The</strong> CMA’s Dr. Jeff Turnbull wants public inputemergency wards, it adds: “Of sicker respondents,those in Canada and the U.S. were mostlikely to visit the emergency department fora condition that could have been treated bya regular doctor had one been available.” <strong>Canadian</strong>sand Americans use the ER at ratesthree to four times that of Germany and theNetherlands.Canada scored no better in a Commonwealthstudy in November of 11 wealthy countries,released with the <strong>Canadian</strong> <strong>Health</strong>Council. <strong>The</strong> lack of a publicly funded drugprogram, unlike most countries surveyed,raised affordability issues. One in 10 <strong>Canadian</strong>sreported not filling a prescription orskipping a dose because of cost. <strong>The</strong> studyalso focused on <strong>Canadian</strong>s’ overreliance onemergency departments. <strong>Canadian</strong>s havethe greatest difficulty accessing care on weekendsand holidays. “As a result, <strong>Canadian</strong>sare the biggest users of emergency departments,compared with the other 10 countries,”the report said.<strong>Canadian</strong> wait times—“widely regarded asPHOTOGRAPH BY Blair GablePOLITICAL AUTHORITYReturning Monday, January 31 stPRIMETIME POLITICSWith Peter Van DusenMON – THURS 8 PM ET/5 PM PTInformed, in-depth and compellingpolitical coverage from Parliament Hill.
the Achilles heel of the system”—are just oneof many concerns raised in recent OECDstudies. Making patients wait is really a meansof rationing health care, a blunt, ineffectiveway of dealing with a looming health-drivenfiscal crisis faced by Canada and other countries,say OECD economists. “In the absenceof adaptations,” an analysis said in September,“costs are expected to mount relentlesslyin coming decades because of populationaging, technological progress and relativeprice developments, putting a potentiallyunsustainable burden on public budgets.”Canada has the sixth highest rate of healthexpenditures as a share of the economy among32 OECD countries. Nor is health care as“free” as some <strong>Canadian</strong>s think. When publicspending is combined with the 30 per centspent privately on health (for such things asdrugs, vision care, dental, long-term andhome care), <strong>Canadian</strong>s personally, and astaxpayers, face the fifth highest per-capitacosts among the 32. For all that, Canada hasfewer doctors, fewer hospital beds and fewerhigh-tech diagnostics (CT scanners and MRIunits) than the OECD average. <strong>Canadian</strong> lifeexpectancy, at 80.7 years, is more than a yearhigher than the OECD average, but theJapanese, Swiss, Italians and Australians outliveus. <strong>Our</strong> infant mortality rate, while betterthan the U.S., is slightly worse than theOECD average. All told, as a foundation for<strong>Canadian</strong> values, it needs work.Bumping against the <strong>Canadian</strong> health caresystem can be a bruising experience for patients.Last year, the Regina-based Frontier Centre,a conservative think tank, joined forces withthe Belgium-based <strong>Health</strong> Consumer Powerhousefor its third annual comparison of the“consumer friendliness” of <strong>Canadian</strong> healthcare against that in 33 European countries.<strong>The</strong> survey tracks cost, medical outcomes,wait times, access to new technologies anddrugs, among other measures. Canada ranked25th among the 34 countries, just ahead ofSlovakia, just behind Portugal.“<strong>Canadian</strong>s are paying for a world-classhealth care system but for a variety of reasonsthey are not getting one,” the Frontier reportsaid. Waits for such diagnostic tests as MRIscan last months; “in comparison the typicalwait time in top European countries is lessthan a week.” Drug costs are higher in Canadathan subsidized plans in most Europeancountries, and approval times for new drugslag considerably. It takes an average 314 daysfor approved medicines to be entered intoprovincial subsidy programs, an improvementfrom a more than 500-day wait of sixyears earlier, but still far behind the standardof 150 days or less in Ireland and Germany.<strong>The</strong> Frontier Centre, a champion of freeEffectivenessof <strong>Care</strong>Timelinessof careper capitahealthexpenditures*markets, puts most of the credit for the successof the Netherlands and Germany, whichfinished second, on their competing systemof private health insurers. (In Germany, competinginsurers offer a standard benefit package,and higher-income earners can opt outof the mandatory plan to purchase privatecoverage. <strong>The</strong> Netherlands requires the purchaseof a mandatory comprehensive healthinsurance package provided by a mix of nonprofitand for-profit insurers.) Still, it notes<strong>Canadian</strong> universal medicare produces impressivesurvival rates for heart attacks and variouscancers. “In Canada you may wait a verylong time to see your doctor, but once youdo,” it notes, “[the] quality of care you receivewill generally be quite good.”<strong>The</strong> coming years present both challengeand opportunity for <strong>Canadian</strong> health care.<strong>The</strong> next opportunity for profound changecomes in 2014 with the expiration of a 10-yearhealth accord among the federal government,provinces and territories. That deal, whichthen-prime minister Paul Martin optimisticallysaid would fix health care for a generation,provided $41 billion in additional federalfunding, and contained a commitmentthat provinces cut wait lists and account betterfor spending. But a health care systemthat cost $192 billion last year has only slightlyA tarnished national treasureA recent international study finds Canada delivers the second most expensivehealth care among seven countries, yet it finishes last in effective and timely care.BRITAINNetherlands GermanyNewBRITAINUnitedZealandStatesAustraliaNewZealand$2,454BestAustraliaBRITAIN$2,992NetherlandsAustralia$3,357UnitedStatesGermany$3,588NewZealandNetherlands$3,837GermanyCanada$3,895CanadaCanadaUnitedStates$7,290worst*U.S. dollars, 2007 data. Source: commonwealth fundshifted course, though there are improvementsin wait times in areas like cataract andbypass surgery, and cancer treatment.If politicians, especially the federal Conservativegovernment, seem reluctant toengage, it’s perhaps understandable. U.S.President Barack Obama’s health care reformbill was passed last year at enormous politicalcost, and with a bruising national debatethat refuses to die. British Prime MinisterDavid Cameron is already drawing fire forannouncing this week plans to add greaterprivate sector involvement in the National<strong>Health</strong> Service, already one of the world’sbest performing systems. Prime Minister StephenHarper has cautiously avoided revealingdetails of federal plans for a renewedProudly oPerated by these leading comPaniesPolitics • Parliament • Public AffairsCPAC.ca
accord. In his previous role as vice-presidentof the National Citizens Coalition, he was nofan of the blueprint for Canada’s public healthcare system, declaring in 1997: “It’s past timethe feds scrapped the Canada <strong>Health</strong> Act.”<strong>The</strong> CMA’s consultation, including a dedicatedwebsite already filling with thousandsof comments, is an attempt to engage thepublic—their patients—in writing a prescription;one that will spur governments toupdate and expand the Canada <strong>Health</strong> Act.<strong>The</strong> CMA’s Turnbull wants to move beyonddoctrinaire positions onprivate versus public healthcare delivery. “I think we’regoing to have a mélange, amix, as we currently do, butwe’ve got to have somethingthat delivers service to <strong>Canadian</strong>swhen we need it. I’mafraid unless we do somethingwe won’t be able to do that.”<strong>The</strong> OECD offered its prescription in September,some of which would violate theexisting Canada <strong>Health</strong> Act. It says <strong>Canadian</strong>sshould pay small fees or deductibles for usinghealth services, as most other OECD countriesrequire, to limit overuse of the system.It also wants competition from the privatesector and performance benchmarks for doctorsand hospitals. Conversely, it recommendsexpanding medicare as most OECD countrieshave, to publicly pay an array of healthand drug costs beyond doctor and hospitalvisits, a position also backed by the CMA.While this could add costs, the report notes,“government may need to devise a statutory(or decent minimum) care package determinedby the public’s willingness to pay thenecessary taxes.”Until a consensus on national standardsemerges, if such a thing is possible, provincesare charting their own course, sometimeswith rocky results. In Alberta, MLA and emergencydoctor Raj Sherman was suspended inNovember from the government caucus forcriticizing the Conservative health policy, andthe backlogged state of emergency wards. Asthe controversy flared, Stephen Duckett wasfired as CEO from Alberta <strong>Health</strong> Services,the super-board of 90,000 health care workersthe government instituted two years agoin hopes of getting a grip on spiralling costsand poor outcomes.Duckett delivered a defiant farewell speechlast month, but one tinged with regret. ERwait times have only grown worse, he said.At the start of the last decade 60 per cent ofpatients were admitted within eight hours.Now that happens just 25 per cent of theCANADA RANKED 25thamong 34 countriesin one study, justahead of slovakia,just behind PortugalNationaltime. “Neither level [is] acceptable, of course.”He warned of “a chronic disease tsunami”that requires fresh thinking. <strong>Care</strong> needs tohappen first outside of hospitals, at home,or via telephone consults, and in communitysettings. “This requires a transformationof the Alberta mindset, which still seems tobe to equate health care progress with moreacute beds.”Nova Scotia is also attempting reform,spurred by the state of its emergency departments.Ross, a veteran emergency care physician,issued a series of recommendationsin Octoberto correct a litany of problemsuncovered in a yearlonginvestigation. Patients,waiting up to six weeks forappointments with familydoctors, end up in emergency.So, too, do chroniccare patients, those with mental health issues,and far too many with minor complaints.Emergency wards are clogged with everythingbut emergencies. Almost 90 per cent of ERvisits can be better handled at less cost inclinics, Ross found. Just 1.1 per cent of ERcases are severe, and 0.1 per cent threatenlife or limb, he found. <strong>The</strong> problem feeds onitself, consuming hospital budgets and resources.As a result, cash-strapped hospitals closedERs across the province for the equivalent of795 days last year.By year end, <strong>Health</strong> Minister MaureenMacDonald accepted all 26 of Ross’s recommendations,setting standards for emergencycare, and diverting patients to more appro-priate services. <strong>The</strong>re is a need to flip prioritiesand put the patient first, Ross concluded.“We have allowed the system to see the patientmore as a burden than its very reason forbeing. To some, patients are ‘cost drivers’ andto others they border on being nuisances whoget in the way of a smoothly functioningbureaucracy.”A recommitment to patient-centred care,as obvious as that sounds, is also the goal ofthe CMA. One of Turnbull’s roles as chief ofstaff at Ottawa Hospital is fielding publiccomplaints. <strong>The</strong>y are easy enough to comeby in a hospital that has not run below 100per cent capacity for about a year; where thisday there are 38 admitted patients with nobeds; where the daily morning discussion isnot if surgeries will be cancelled today, buthow many.It’s long past the time for that national adultconversation, not just about the health of asystem but about the needs of the people. Historyshows a national consensus can be achieved,though it was a torturous journey. After yearsof acrimonious debate, and incalculable humancost, the blueprint was finally drafted in 1964when Justice Emmett Hall tabled his royalcommission report recommending medicarefor all of Canada. Fifty years later, 2014 representsa chance once again to make that visiontruly world-class.<strong>The</strong> Halifax town hall will be moderated byMaclean’s Ken MacQueen, with opening remarksby Dr. Jeff Turnbull, CMA president. <strong>The</strong> panelfeatures Dr. Jane Brooks, President, Doctors NovaScotia; Dr. John Ross, Nova Scotia adviser onemergency care; Maureen Summers, CEO of the<strong>Canadian</strong> Cancer Society, Nova Scotia; AndrewCoyne, National Editor, Maclean’s.No drug program: One in 10 <strong>Canadian</strong>s report not filling a prescription because of the costPhotograph by Christopher Pike22 JANUARY 31, 2011