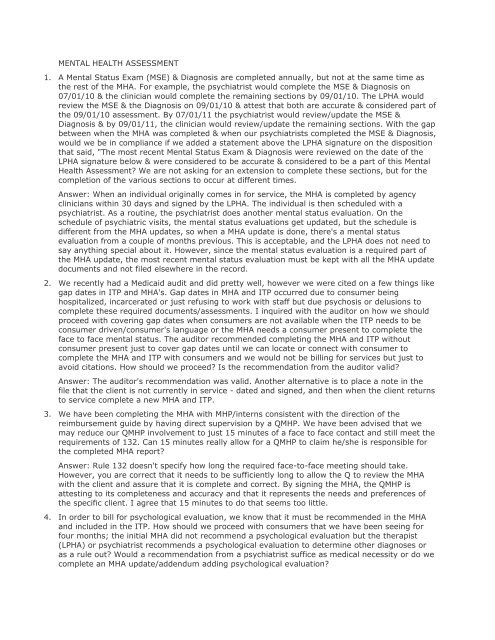
MENTAL HEALTH ASSESSMENT 1. A Mental Status Exam (MSE ...
MENTAL HEALTH ASSESSMENT 1. A Mental Status Exam (MSE ...
MENTAL HEALTH ASSESSMENT 1. A Mental Status Exam (MSE ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>MENTAL</strong> <strong>HEALTH</strong> <strong>ASSESSMENT</strong><strong>1.</strong> A <strong>Mental</strong> <strong>Status</strong> <strong>Exam</strong> (<strong>MSE</strong>) & Diagnosis are completed annually, but not at the same time asthe rest of the MHA. For example, the psychiatrist would complete the <strong>MSE</strong> & Diagnosis on07/01/10 & the clinician would complete the remaining sections by 09/01/10. The LPHA wouldreview the <strong>MSE</strong> & the Diagnosis on 09/01/10 & attest that both are accurate & considered part ofthe 09/01/10 assessment. By 07/01/11 the psychiatrist would review/update the <strong>MSE</strong> &Diagnosis & by 09/01/11, the clinician would review/update the remaining sections. With the gapbetween when the MHA was completed & when our psychiatrists completed the <strong>MSE</strong> & Diagnosis,would we be in compliance if we added a statement above the LPHA signature on the dispositionthat said, "The most recent <strong>Mental</strong> <strong>Status</strong> <strong>Exam</strong> & Diagnosis were reviewed on the date of theLPHA signature below & were considered to be accurate & considered to be a part of this <strong>Mental</strong>Health Assessment? We are not asking for an extension to complete these sections, but for thecompletion of the various sections to occur at different times.Answer: When an individual originally comes in for service, the MHA is completed by agencyclinicians within 30 days and signed by the LPHA. The individual is then scheduled with apsychiatrist. As a routine, the psychiatrist does another mental status evaluation. On theschedule of psychiatric visits, the mental status evaluations get updated, but the schedule isdifferent from the MHA updates, so when a MHA update is done, there's a mental statusevaluation from a couple of months previous. This is acceptable, and the LPHA does not need tosay anything special about it. However, since the mental status evaluation is a required part ofthe MHA update, the most recent mental status evaluation must be kept with all the MHA updatedocuments and not filed elsewhere in the record.2. We recently had a Medicaid audit and did pretty well, however we were cited on a few things likegap dates in ITP and MHA's. Gap dates in MHA and ITP occurred due to consumer beinghospitalized, incarcerated or just refusing to work with staff but due psychosis or delusions tocomplete these required documents/assessments. I inquired with the auditor on how we shouldproceed with covering gap dates when consumers are not available when the ITP needs to beconsumer driven/consumer's language or the MHA needs a consumer present to complete theface to face mental status. The auditor recommended completing the MHA and ITP withoutconsumer present just to cover gap dates until we can locate or connect with consumer tocomplete the MHA and ITP with consumers and we would not be billing for services but just toavoid citations. How should we proceed? Is the recommendation from the auditor valid?Answer: The auditor's recommendation was valid. Another alternative is to place a note in thefile that the client is not currently in service - dated and signed, and then when the client returnsto service complete a new MHA and ITP.3. We have been completing the MHA with MHP/interns consistent with the direction of thereimbursement guide by having direct supervision by a QMHP. We have been advised that wemay reduce our QMHP involvement to just 15 minutes of a face to face contact and still meet therequirements of 132. Can 15 minutes really allow for a QMHP to claim he/she is responsible forthe completed MHA report?Answer: Rule 132 doesn't specify how long the required face-to-face meeting should take.However, you are correct that it needs to be sufficiently long to allow the Q to review the MHAwith the client and assure that it is complete and correct. By signing the MHA, the QMHP isattesting to its completeness and accuracy and that it represents the needs and preferences ofthe specific client. I agree that 15 minutes to do that seems too little.4. In order to bill for psychological evaluation, we know that it must be recommended in the MHAand included in the ITP. How should we proceed with consumers that we have been seeing forfour months; the initial MHA did not recommend a psychological evaluation but the therapist(LPHA) or psychiatrist recommends a psychological evaluation to determine other diagnoses oras a rule out? Would a recommendation from a psychiatrist suffice as medical necessity or do wecomplete an MHA update/addendum adding psychological evaluation?
Answer: You would handle this as you would any other MHA and ITP modification for any otherservice.5. Will a treatment plan review with a specific recommendation for Psychological Evaluation signedby the LPHA suffice as medically necessary? This also would be followed by a treatment planmodification adding the service. Could this be done instead of listing it as a recommendedservice on the MHA for existing (not new) consumers?Answer: This will suffice as long as there is evidence in the record of the reason(s) forrecommending the psychological evaluation.6. The rule states that the mental health assessment must be completed in 30 days after the firstface to face contact. There are times that we conduct more in depth assessments beyond themental health assessment, such as sex offender specific assessments, which are quite lengthy.Can we submit bills for assessment beyond the mental health assessment as long as we havethat assessment complete within the 30 days?Answer: <strong>Mental</strong> health assessment is not a one-time thing. Whenever you're doing anassessment related to the consumer's mental illness and the services being or to be provided,you may bill MHA.7. When a consumer's diagnosis changes during the course of treatment the ITP has to reflect thechanged diagnosis. The goals, objectives, specific services and frequency of services may notneed to change if so determined by the QMHP and LPHA. Would another mental healthassessment be required, in addition to other clinical documentation explaining the diagnosischange?Answer: An addendum to the MHA would be acceptable. The provider's clinical professionalsshould determine what portions of the assessment need to be updated, evaluate the consumer'schanging needs and then reflect changes in the ITP.8. We have a case that has been open for more than 3 months, as such a MHA and treatment planhas been completed, but upon further review the provider now believes a psychiatric evaluationwould be beneficial, but this was not indicated in the recommendations in the MHA. If it is beforethe annual review of the MHA, can you prescribe a service that was not indicated on the MHA bysimply completing a treatment plan review and adding a goal/objective that reflects this servicein a new treatment plan? Or does a MHA addendum also need to be completed to reflect anadditional treatment recommendation?Answer: Psychiatric evaluation, if done as a physician service and billed directly to HFS, does notneed to be on the MHA or ITP. If considered as part of the ongoing mental health assessment, itdoes not need to be on the ITP.9. An auditor said that when a treatment plan is due the MHA is also due. The MHA is current forone year. If a treatment plan is due or expired and the MHA is still current, is there a need to doanother MHA?Answer: If a MHA is updated to reflect needs and preferences significantly different than thecurrent ITP, the ITP should be amended. However, the two of them are not specifically tiedtogether.10. An MHP meets with a client to complete an assessment. The assessment takes two sessions. TheMHP bills assessment for both sessions. However, the QMHP does not see the client until the endof the second session. Is it correct to bill assessment for both services? Can an MHP billassessment for meeting a client the first time, gathering background info, and determiningservices needs? What if a Q does not see this client?Answer: See 132.148a). A mental health assessment is seldom something that happens in onesitting. The Q must have at least one face-to-face with the client before signing off on the mentalhealth assessment report.
1<strong>1.</strong> If we discover that an MHA is not current but the treatment plan is current, can we still bill? Weare thinking we cannot because the LPHA signature on the updated MHA determines medicalnecessity for the treatment plan. Can you clarify?Answer: Services must be based on the consumer's assessed needs. If there is no currentmental health assessment, the treatment plan is not reflective of those needs and services arenot billable.12. When comprehensive testing is done by a licensed clinical psychologist, some of the tests aredone by the client who is alone with paper and pen. Is that reportable and billable time? (Thepsychologist would be in the building but not face to face with the client.) Is the review andwrite-up by the psychologist reportable and billable?Answer: Only interventions provided directly by staff to a consumer are billable. When a staffperson is not providing a direct intervention, that staff person may not bill. In this case, thepsychologist may not bill for something the consumer is doing. Additionally, the completion ofpaperwork is not billable.13. It is my understanding that Rule 132 requires a person to have a face to face contact with aQMHP prior to the billing for a completed <strong>Mental</strong> Health Assessment or <strong>Mental</strong> Health AssessmentUpdate. Is my interpretation of the rule correct? If it is correct, would I be correct in assumingthat in the process of completing and billing for the <strong>Mental</strong> Health Assessment Update by a casemanager who is an MHP (with review and sign-off by an LPHA) that a recent (within the lastcouple of months) meeting with the agency psychiatrist (QMHP/LPHA) would be able to "count"as the face to face meeting with a QMHP prior to the completion of the Assessment Update?Answer: Yes, if the psychiatrist functions as the QMHP, then the face-to-face by the psychiatristis acceptable. Billing for mental health assessment is not required to wait until the face-to-facewith the Q.14. If a <strong>Mental</strong> Health Assessment/Treatment Plan is completed by a licensed clinician, can thatclinician sign off as the LPHA or does the designated agency LPHA have to sign off on thedocuments?Answer: An LPHA is required to review and approve the treatment plan so the signature of anyLPHA meets the "letter of the law". However, it is better clinical practice to have the review andsignature of the LPHA who is responsible for the implementation of the services.15. How do we bill application of quarterly OHIO Scales?Answer: The OHIO Scales is a functional assessment instrument used in the web-basedoutcomes system for C&A, and should be billed as mental health assessment.16. If a <strong>Mental</strong> Health Assessment is started and it is determined that mental health services areinappropriate for the client who is then referred out, does an LPHA still have to sign and does a Qstill have to have a face-to-face?Answer: If the only service is mental health assessment and the client is subsequentlydetermined as inappropriate for mental health services, the assessment report does not need tobe completed, i.e., LPHA signature or face to face with the QMHP. Document the clientstatus/disposition in the record and you may bill for mental health assessment.17. If the treatment plan expires and the client and I do the annual <strong>Mental</strong> Health Assessment in theappointment following the expiration of the plan, it would seem that would be okay because atreatment plan is not required prior to a mental health assessment. Right? Wrong?Answer: <strong>Mental</strong> health assessment updates are not necessarily tied directly to ITP udpates.However, it makes good clinical sense that when assessments are updated and new needs areidentified, that the ITP gets updated as well. You are correct that there is no need to have an ITPto do a mental health assessment or update.
18. Is the requirement for an annual update of the <strong>Mental</strong> Health Assessment a rule violation or apayback issue?Answer: Failure to meet the requirement for an annual update of the <strong>Mental</strong> Health Assessmentis considered a Rule violation and a post-payment issue.19. I wanted to run this by the Medicaid group to make sure that DMH/Medicaid Group is aware ofand supports this way of handling the specific services "Sue acknowledged our need to complywith the documentation requirements not only of Rule 132, but also of JCAHO, Medicare,Medicaid and Northwestern Memorial Hospital, and supported the first option," which is, theattending psychiatrist who sees the client at the time of the intake writes the admitting orders,and lists the recommended services. Please advise if DMH supports this.Answer: No. At the conclusion of the mental health assessment there must be a summaryanalysis, conclusions and recommendations for specific Part 132 services (132.148a)3)T). Therecommendations for services cannot be made prior to completion of the mental healthassessment.20. We want to know specifically if the list of recommended services, (as written by the doctor afterthe MHA is completed) have to actually be in the MHA after the summary analysis, or, can theyrefer the reader to the section in the chart with the doctor's orders for the recommendedservices?Answer: All components of the mental health assessment must be completed. Then a summaryanalysis, conclusion and recommendations for specific Part 132 services must be developed. Rule132 is not specific about where the components must be located, but it must be clear that eachelement is addressed and present as a result of the MHA.2<strong>1.</strong> I am a Clinical Director and would like some clarification regarding the following situation: A childtransitioned from SASS to C/A MH services in early December. The MHA was completed at thebeginning of SASS and indicated a need for intensive services. A new MHA was completed at thebeginning of C/A MH services for new goals and less intensive services. The C/A counselor whohad completed the C/A MHA left the agency in late December and a new C/A provider joined theagency in early January. Can the new C/A service provider simply review the existing MHA withthe family and document that the symptoms, goals and information in the most recent MHA arestill accurate and then develop a new ITP with the same goals but new objectives, or, is itnecessary to do a completely new MHA and ITP? My basic question is: If there is a transfer of aclient from one service provider to another and the MHA remains accurate except for who willprovide services, can a note in the file, stating the MHA remains accurate with a new treatmentplan, be sufficient?Answer: SASS is only a funding stream, so if your agency has done an MHA and an ITP as thechild/youth entered SASS, that MHA and ITP will remain effective as the child/youth moves intonon-SASS funded services. If the responsible staff person changes during this switch, then anaddendum to the ITP is necessary to note the change. Unless the services change, too, there isno change needed to the MHA.22. Does a MHA update need to be done if there is only a change in intervention for a goal alreadyestablished on the tx plan? When does the update need to be done? A new goal is established? Anew service?Answer: If the specific intervention is already recommended on the MHA report, then no MHAupdate need be done. If the service is not recommended, then yes, the MHA must be updated. Ifneeded, it must be done at the same time that the ITP is amended. A new goal must beestablished only if a new service is used or the goal is not in response to recommendationsalready on the MHA report. A new service should be established again, only if not alreadyrecommended on the MHA report.23. In the Post-Payment Review Interpretive Guidelines document of the Collaborative the followingstatement appears: "Clinical assessment is ongoing...assessments can be documented in a
number of ways depending on the agency's practice, such as, MHA addendums, as anassessment portion within a review of the treatment plan, or a clinical progress note..." It is ourunderstanding that a progress note is a progress note, NOT an assessment document. Am Icorrect?Answer: Assessment is not always a formal assessment document/instrument. It is sometimesinformation gathered as the result of interaction with a client. That interaction and the resultscan be documented in a progress note. However, this is not a required means of documentationif you use another.24. Please clarify SASS intensive outpatient services. A SASS consumer is placed in a residentialfacility for two or more months after a psychiatric hospitalization or from home, and the onlyservice provided by our agency is crisis intervention or follow-up case management by our SASSstaff. We don't have a MHA or ITP completed because they are in the residential setting. Creatinga MHA and ITP with that consumer would be duplicate billing - is this true? If so, what aboutcontinuity of care and stabilization? In the SASS handbook, CMH-202.4 states "For children inresidential or group home placement, the SASS provider's involvement in the intensiveoutpatient psychiatric component will be determined on a case-by-case basis and SASS activitiesmust be coordinated with the residential/group home staff and/or the child's case manager." Canwe provide other services such as individual therapy/coping skills or are we limited to crisis and afollow-up case management? What is the status of the MHA and ITP while a consumer resides ina residential facility?Answer: 1) SASS is a funding stream for 90 days following a psychiatric crisis. 2) SASS fundingwill pay for any 132 service. 3) In order to provide anything with SASS besides the crisisservices, there must be a MHA and ITP. 4) Your development of an MHA and ITP for your agencyis not duplicate billing, unless you're trying to claim for something another provider did and alsoclaimed for.25. I came across a situation where a clinician took more than 30 days to complete a MHA. In thisparticular case it took three months to complete it and the "L" signed it the day it was completedand that is not because they went into the hospital. In Rule 132 it states that we should have theMHA completed in 30 days. Would this be a valid MHA? How should we proceed with this andwhat happens to all services provided to the consumer up to this point?Answer: The MHA would be valid. However, please note that the only services that may beprovided prior to completion of the MHA are crisis services and case management services. And,you may only provide 30 days of case management prior to completion of the MHA, so if youragency had been providing case management for the full 3 months, two of those months ofservice could not be claimed.26. If an MHP completes the MHA and a doctor signs as an LPHA and has seen the client prior to thecompletion of the original MHA or MHA update, does that suffice as a counter signature/face toface (vs. a QMHP signature and face to face)?Answer: Rule 132.148a)5) states "A QMHP who has had, at a minimum, one face-to-face orvideo conference contact with the client shall be responsible for the completed mental healthassessment report as documented by his/her dated signature on the mental health assessment.MHPs may participate in the mental health assessment." This means that the Q is responsible forthe MHA report and must sign it. MHPs are not authorized to do the MHA or to be responsible forit. They may only participate. Additionally, 132.148a)7) states, "The mental health assessmentreport shall be reviewed and approved by the LPHA as documented by the LPHA's datedsignature on the mental health assessment." This is a review of the assessments andrecommendations made by the Q, not by an MHP. If the LPHA is acting as a QMHP, e.g., doingthe annual MHA update, assuming responsibility for review of the ITP every 6 months andmodifying the ITP in response to that review, then the L may sign as both the L and the Q.However, an MHP may not act as a Q. In summary, while a doctor would meet the qualificationsfor both the LPHA and the QMHP, the Rule requires that certain functions (besides signature) arerequired of each of those (the L and the Q.) If the doctor performs the FUNCTION of either the L
or the Q, or of BOTH the L and the Q, then the doctor could sign the assessment for thatfunction/both functions as appropriate.27. If a patient is a doctor-only patient, and is not seeing a therapist, is there a requirement underRule 132 that an MHA/ITP must be completed and kept updated? Doctor charges are billeddirectly to public aid and are not billed to MCO/MRO.Answer: Physician services are not covered by Rule 132. When a physician claims for physicianservices directly to HFS, they are governed only by any regulations that HFS has for suchclaiming. If the client, at any time, needs Rule 132 services, all 132 requirements will apply.28. An agency has multiple locations, and sometimes the LPHA who reviews and signs off on theMHA is not in the same office on all days. They can electronically review the MHA. The agencydoes not have electronic signature systems, and is not able to invest the money in one at thistime. Sometimes waiting until the LPHA is back in the office where the person is receiving theservices, could delay getting a signature and therefore treatment. One possible solution would bethat the LPHA could print out and sign the review, but then the LPHA signature and the Qsignature would be on separate pages. Is there anything that says that the signatures all have tobe on the same page? Is there a way for them to do this and have it meet all of our guidelineswithout getting into an electronic signature system?Answer: There is nothing in Rule 132 that requires the L and Q signatures to be on the samepage. However, it must be clear that both are signing the same document. Additionally, the MHAdoes not take effect until the date of the LPHA signature.29. In most cases when we receive a referral for an ICG Client, the youth is either involved in SASSor with an Outpatient Therapist at a Medicaid Certified agency. An LPHA at the referring agencyhas already completed and signed an MHA and noted in the treatment plan that the client needsreferral and linkage to Case Coordination services of an ICG Coordinator. Upon receiving thereferral for Case Coordination, our LPHA requests the current MHA and ITP from the referringagency. At that point our ICG Coordinator meets with the family. The ICG Coordinator (MHP) andLPHA Supervisor review the MHA. The question is: Can our LPHA sign the MHA (below where theother agency's LPHA signed) and state that she concurs if there have been no changes?Answer: It is important to note that each provider must have an MHA and ITP that is their own.The MHA must be developed to reflect the current status of the client as determined by a QMHPand LPHA. An MHP may assist with the MHA development, but the Q must review the MHA andhave at least one face-to-face with the client (not just the family) before signing off on the MHA.Additionally, each provider must then develop their own ITP based on their MHA. It is acceptableto use the referring provider's information as a starting point, but all of it must be reviewed andchanged as appropriate.30. I could not find a standard in Rule 132.148 a) 8) as it pertains to clients who are currentlyinactive, but not yet terminated. If their annual re-assessment is due/overdue, and possibly anITP review, but the client has been inactive for better than a month or two, and we are preparingfor termination due to non-compliance, non-attendance, etc. Should the re-assessment be doneanyway - even without client input, since we are unable to engage them?Answer: Each MHA must be updated annually. If the client is no longer active, but not yet closed,there will be little to update. However, if the update is not done and the record is part of theBALC survey, there will be a citation.3<strong>1.</strong> According to the auditors an LPHA's signature must be on an MHA that is not completed becausethe client did not return. We do not find this in Rule 132. What the rule does state is that theQMHP is responsible for completing the assessment and the LPHA will review and sign the MHA.Is the LPHA signature required on an incomplete MHA? We have documentation that describesthe circumstances that resulted in the MHA not being completed, is this sufficient to substantiatea billing?
Answer: If the only thing that was ever claimed was mental health assessment or crisis, thenthere is no need for an L signature if you were unable to complete the assessment.32. Would failure to update the MHA every time there is a med. change result in the "disallowance ofa claim?" Is an MHA update necessary when the change in medications is otherwise documentedin the record by the psychiatrist?Answer: No. Assessment is an ongoing process in mental health treatment. Any changes inassessment should be documented within the clinical record within the context in which itoccurred, e.g., a progress note related to community support in which the clinician identified anew need. Agencies may document this type of assessment in a variety of ways, throughaddendums to a MHA, as a portion of a treatment plan review, or in a progress note, are threeexamples. Regardless of method, such assessment must be documented in some format andavailable to the reviewer to evidence an identified need leading to inclusion of the service on thetreatment plan.33. In our MHA, employment interests/skills/specialized training is addressed as one element andeducation is addressed as an element. Does this method meet the intent of the Rule?Answer: Yes.34. We had multiple problems with the Post-Payment Review Summary, item #2, which states, "The<strong>Mental</strong> Health Assessment does not contain all required elements." The specific issues weregender, DOB, and Physician related information. These elements are contained in our record andare completed as part of the Assessment. Can multiple documents contain elements of the MHA?For example, can information in an intake/screening form and physical health questionnaire beaccepted as part of the MHA? If yes, is it necessary that the documents be stapled together?Answer: The required elements must be on the MHA report. The fact that you've done them andthey're scattered throughout the record, does not meet the requirement of rule. All theinformation you mentioned is good, but it must be summarized in the MHA report.35. On our MHA, we ask questions about the individual's communication concerns & needs. We donot ask "method of communication". Is determining the individual's communication concerns &needs evidence that we have sufficiently inquired about the person's communication?Answer: No. The requirement is for a method of communication. An individual is not required tohave communication concerns or needs in order to have a method of communication. Manycommunicate through spoken English, but others for example, communicate through AmericanSign Language or spoken Spanish.36. Can we bill an assessment as MHA after the formal MHA has been signed by an LPHA? If anassessment service is performed & billed after completion of the MHA, it is necessary for theMHA to be updated & signed by an "L?" For example, a clinician completes a MHA and obtains anLPHA signature. Several weeks later, the clinician completes a Beck Depression Inventory & billsthat service as MHA. Can this bill stand alone, or are additional signatures required by the "L?"Answer: <strong>Mental</strong> health assessment is an on-going process. Each time an assessment service isprovided, it may be billed as MHA. The MHA report does not have to be updated each time,however, if changes are made to the ITP as a result, the ITP update, changes, addendum, etc.,must be signed by the Q, the L, the client and if applicable, the guardian.37. When a new need surfaces after completion of a MHA, is an update of the MHA required? Forexample, if a consumer with a completed MHA and ITP lost housing and needs assistance inlinking to permanent housing, must the assessment be updated in order to bring this intotreatment?Answer: Yes. This can be done through an addendum to the MHA report, a note in the recorddescribing the changed circumstances and what needs to be done, or an update to the MHAreport.38. Does a MHA update require a face-to-face contact with a QMHP?
Answer: Yes.39. Would documentation of a new assessed need and an updated ITP, both signed by the L and Q,be sufficient documentation for the MHA?Answer: Yes.40. How do we bill an Admission Note - as an assessment or a treatment plan since it is a temporaryversion of both?Answer: First, the only Rule 132 service an admission note may be used for is ACT. Then, it isclaimed as ACT.4<strong>1.</strong> On our MHA we have vocational related questions. If we determine that a more in-depthvocational assessment be completed, based on the results of the MHA, can we complete thevocational assessment and bill as an MHA since it will be part of the MHA, i.e., physicallyattached. We would use this assessment to refer to DORS.Answer: Billing Medicaid for vocational assessments is not allowed. It is not Medicaidreimbursable.42. I understand that if we do an addendum to the ITP to add a service after the initial MHA, theeffective MHA must also have that service recommended on it. How can we document theadditional service on the MHA?Answer: A progress note or a statement added to the MHA to show that the change is neededbased on a change in the client's needs or preferences signed and dated by the LPHA wouldsuffice.43. An agency's specialty assessment (among others) was covered for many years via a capacitygrant issued by C&A to specific providers. It appears that the Multi-Disciplinary Grant will notsurvive the budget cuts. As a way to try to preserve these services, they are looking at alternateways to fund the assessments. Referrals for them come to the C&A Network from other providerswho are currently treating C&A who are in need of these assessments. Could you use thatagency's treatment plan like TLA? Does this assessment qualify for Medicaid billing as a mentalhealth assessment?Answer: One of the problems with the idea is that the brochure says that the evaluation is free.No one may bill Medicaid for a service that is free to non-Medicaid recipients. Additionally, thisappears to be primarily a psychological evaluation and not a mental health assessment.44. I have had a staff ask if they can copy the doctor notes for the annual assessment update andattach to the update instead of listing out the previous medications that have been prescribed.They would be listed on the doctor notes.Answer: We believe it would be best for this information to be photocopied to assure there areno changes made to what the physician has written. Then it is ok.45. I need clarification on the requirement for "previous psychotropic medications" on the <strong>Mental</strong>Health Assessment Update. I am assuming that you are required to list the medications thathave been prescribed during the last year and stopped and not have to list all the previousmedications that the client has ever taken?Answer: Rule 132 doesn't specify what previous medications. It is important to explore with theconsumer what other meds they have taken so that you know their history. Get as much asthey're willing or able to give you.46. Regarding billing a mental health assessment that is required for Medicaid recipients seekingbariatric surgery. I understand that this is a Medicaid-billable service and I want to verify that itis billable under Rule 132.Answer: Per rule 132, a mental health assessment is a formal process of gathering informationregarding a client's mental and physical status and presenting problems...resulting in the
identification of the client's mental health service needs and recommendations for servicesdelivery. A diagnosis of mental illness is not required prior to beginning a mental healthassessment.47. In billing for the MHA, we complete a MHA report that contains all of the required elements. Inorder to bill this, we have been writing "see mental health assessment in file" for the billingprogram. Is this acceptable, or does the note need to describe the intervention?Answer: Notes must always contain a description of the intervention provided.48. If we add a service to an ITP which is not identified on the MHA, do we need to do an MHAupdate with noted changes?Answer: You would certainly need to be able to show documentation that the new service wasneeded. That doesn't necessarily need to be through an official MHA update, but could be anaddendum to the MHA. When the MHA update is required, it could be incorporated. The servicemust be added to the ITP prior to being provided.49. We did an audit and found some charts that had overdue MHA, but did have current TreatmentPlans. We want to know if we have to unbill the services that were provided with the overdueMHA. I know we have to do that for overdue Treatment Plans, but wasn't sure if the MHA was acause for unbilling.Answer: Both the MHA and the ITP must be in effect at the time the services is provided. If theMHA has not been properly updated, then it is not in effect. The bills should be voided.50. Can the QMHP meet with the client for their face-to-face contact if the MHA is not fully completedyet? For example, if the MHA is meeting with the client for the first time and has the QMHP meetwith the client as well, but is not able to fully complete the MHA report on that day, so needs theclient to return a second time to finish it, does the QMHP have to meet with the client again at orafter the second meeting as it is at that time that the entire mental health assessment iscompleted or does the first face-to-face count?Answer: Rule 132 does not specify when the face-to-face must happen.5<strong>1.</strong> In the past I have requested a response as to whether or not a crisis assessment, or morespecifically, the "USARF" would suffice as an assessment for placement in our Crisis StabilizationUnit along with specific orders from the on-call psychiatrist authorizing specific Rule 132 servicesuntil we could complete the full bio-psychosocial assessment with all of the elements required forassessment under the Rule. The response was "no" unless all required assessment elementswere collected and the assessment was signed off by the LPHA. Our on-call staff are not QMHPs(they are MHPs who consult with the on-call psychiatrist from whom the nurses on duty at theCrisis Unit obtain admission orders from). Would their crisis assessment be valid in this scenario,or must it be signed by an LPHA? For weekend admissions, when a comprehensive bioPsychosocial assessment is completed the next business day, would the Crisis Assessmentsuffice, even if the client is capable of assisting in completion of the assessment?Answer: Only crisis & case management MH services may be provided prior to completion of acomplete mental health assessment. Crisis services may be provided anytime. Perhaps thereferral should be made to Crisis Residential instead of Community Support Residential. Thecompletion date of a mental health assessment is determined by the dated signature of theLPHA. During the period of time between completion of the mental health assessment andcompletion of the treatment plan, other 132 services may be provided as long as they end up onthe completed ITP within the required period of time.52. Our clinic's psychiatric nurse sees clients for medical follow-up (weight mgt, blood pressure, etc.)before their appointment with the psychiatrist. Is this sufficient to cover the Rule 132requirement of at least one face-to-face contact by a QMHP prior to the MHA annual review?Answer: Only if s/he functions as the QMHP for the client and is the responsible QMHP for thedelivery of services, i.e., signs the MHA report and ITP as the QMHP.
53. Once a full MHA has been completed, is a QMHP face-to-face required when billing MHA forsupplemental assessments i.e. Ohio Scales, Multnomah etc., (assuming that they are completedwith the client and meet all other billing requirements), or is the QMHP face-to-face required onlywhen doing the initial and then annual MHA?Answer: The face-to-face must be done at the initial and at each annual MHA update.54. Must the QMHP who completes the face-to-face be the same one who signs off on the MHA?Answer: Yes.55. Can we bill for MHA services provided to clients who do not remain with the agency long enoughfor the MHA to be done? Would there be any post-payment review issues for not having acomplete MHA on file for a withdrawn client?Answer: The mental health assessment is an ongoing process by which the provider gathersinformation to assess a client's mental health needs. The MHA report is the product of thatprocess, and may assist in guiding the development of the individual treatment plan. It must bereviewed and signed by the LPHA. When the assessment process is terminated before the reportis completed and signed, the provider can bill for that portion of the process which was actuallycompleted.56. The 30-day time frame for completion of the MHA is difficult to meet with older consumers. It ishard to get them into the office, and they are often put on hold due to medical hospitalization. Ifthe MHA or ITP come due while a client is on hold, and we have to be with the client to bill, howdo we ensure compliance?Answer: There is no leeway in the 30 day requirement. The provider may, and is encouraged to,go to the consumer instead of requiring and/or waiting for the consumer to come into the office.57. We have an initial MHA that includes all required information except the LPHA signature. If theconsumer is later referred for MH services, can we do an MHA update including a face-to-faceand QMHP/LPHA signatures instead of another full MHA, will this meet the requirements of Rule132?Answer: A <strong>Mental</strong> Health Assessment needs to have current information. If the originalinformation remains current, then it can continue to be used for the MHA. The original is notconsidered an MHA because it was never signed, and therefore couldn't be updated.58. Can we use the Admission Note for a consumer, recently discharged from a State-OperatedFacility (SOF), who needs to get in immediately to see our MD? Normally we go through anintake process, then begin the assessment, which can take several sessions. However, when aconsumer is discharged from an SOF, we are pressed to get this completed before they see ourMD. Would using the Admission Note be an option, or is that only allowed for programs otherthan outpatient mental health?Answer: No; an admission note is only allowable with ACT and crisis residential.59. The MHA needs to be completed within 30 days of initial contact. If a client comes in forcounseling and meets with the therapist for one session, fails to show for the next two sessionsand then comes back again, the MHA is due, but the therapist would not have had enoughinformation or time with client to complete it. In the past, we were told that if we documentedthrough case notes that a client does not attend a session, the 30 days was dependent on whenthe client came to session. Is this still true or does the MHA have to be completed within 30 daysno matter what?Answer: It is important to note that counseling may not be provided until the MHA reportrecommending it is completed. There has been no change in the requirement that the MHAreport is to be completed within 30 days of the initial face-to-face contact.60. Can we bill the time spent by the LPHA reviewing (and signing) assessments completed by staffwho are not LPHAs as "assessment?" Since the assessment is not considered "complete" until it
is reviewed and signed by the LPHA it would seem logical that this is part of the assessmentprocess would also be billable as "assessment." Our LPHAs typically spend a minimum of 15minutes reviewing the completed MHA before signing them as the liability implications of theirsigning off on these documents is significant and they take this responsibility seriously.Answer: The rate methodology for mental health assessment, and all other Rule 132 services,includes a significant component for indirect costs. The LPHA review of the assessment andsubsequent signature is part of that indirect cost of providing the service.6<strong>1.</strong> Our agency is having significant difficulty getting consumers receiving a minimal level of service(primarily psychiatric appointments every three months) to spend the time necessary tocomplete an updated MHA. The doctor appointment takes about 20 minutes, and we ask theconsumer for at least an additional 30 minutes. Is there any possibility of having the annual MHAupdate requirement waived for this category of consumers?Answer: There is no provision to waive the requirement for an annual update of the mentalhealth assessment. However, if the consumer is not receiving any Rule 132 services and is onlyseeing the psychiatrist who bills directly to HFS, there is no requirement that 132 standards mustbe used.62. Can the face-to-face contact between the QMHP and client for completion of a mental healthassessment be conducted via video conference? For example, a child is SASS screened locally byan MHP, then hospitalized across the state for a longer than typical period of time. There mightbe the possibility of video contact between a QMHP and that individual while they are still in thehospital. If so, could this be counted as the face-to-face contact?Answer: The one required face-to-face between the QMHP and client prior to completion of theMHA must be face-to-face.63. During a recent BALC review we were cited for not having a 6-digit date as a response to thequestions about last physical exam and last psychiatric exam on mental health assessments(MHA) and MHA updates. Until then we thought that a response of unknown or with month andyear were acceptable responses. We understand this will also be a citation by the Collaborativeduring post payment reviews. Since a number of our MHA updates are not due again for a while,would you please suggest a way to correct this that would be acceptable?Answer: There is no need for a month, date and year indication of the most recent exams. Wecertainly don't want anyone to make up a date when all that can be remembered was that it wasJune 2007. In fact, if the client can remember that it was summer 2007 that would also beacceptable. While unknown is acceptable, it must be clear that it is the client that does not knowand not the staff that do not know because they have not asked the client.64. We understand that Rule 132 states that a treatment plan or review must be done every 6months. However, there are times when the client is unavailable for any number of reasons(hospitalization, no shows, physical illness, etc) at that specific time. If we are not going to billfor services until the new plan is in place, could we write a review note stating that we know thereview or new tx plan is due but the client is not available, state the reason why, and thendocument our plans to reengage the client and have their participation in the planning, or plansfor closure if they don't engage. That note would have clinical relevance. Please consider thiscompromise and advise.Answer: As long as the client is included as someone receiving services from your agency, the 6month reviews must be done according to the 132 timelines.65. Our staff complete the <strong>Mental</strong> Health Assessment and ITP. Psychiatric and medication services,however, are provided by either a Psychiatrist in the community or another Community <strong>Mental</strong>Health Agency. We usually send a copy of the MHA to the Psychiatrist and invite them to the ITP.Must the Psychiatrist sign the MHA and/or ITP?
Answer: The MHA and ITP must be signed by the QMHP, the LPHA and the client/guardian. Allproviders who bill for the provision of Rule 132 services must be certified providers, have a MHAand ITP and bill for the services they provide.66. Can/should we use an Admission Note to authorize additional interventions needed foropen/registered clients with a completed MHA who are admitted to our Crisis Stabilization Unit?The guidelines are clear if the admitted client is "new," without a completed assessment, but notwhen the client is already open and receiving services. If we can use the Admission Note for thispurpose, would we then have to complete an assessment update as well?Answer: If the client is known to you and is an open client, we do not recommend using anadmission note. An admission note requires that you complete a mental health assessment andtreatment plan within 30 days of the admission; it would be more paperwork than is necessary.67. Are children placed in an out-of-state residential facility required to have a face-to-face interviewfor the mental health assessment? Can the residential facility and ICG/SASS provider share themental health assessment and individualized treatment plan if they are jointly developed?Answer: At least one face-to-face is required to be done by the provider's QMHP who works withthe client. The residential facility and ICG/SASS provider may share the mental healthassessment and individualized treatment plan if they are jointly developed and each maintains acopy in their records.68. When providing recommended Rule 132 services in the MHA, is it a requirement to explain eachservice or is listing each service enough?Answer: Rule 132 requires that the written mental health assessment report contain "Summaryanalysis, conclusions and recommendations for specific Part 132 services." Additionally, itrequires that the written ITP be based on the mental health assessment report.69. Since there is an emphasis on ensuring that the MHA and Tx Plan match in terms of serviceneeds and prescribed services, what happens if mid-year some new service needs arise? 1)Should the MHA, not due for another 6 months, be updated earlier to add the service needs? Or,2) Should the MHA have an addendum added stating that new service needs have arisen - and ifso, do the Q and L need to sign again? Or, 3) Will the Tx Plan Review suffice as documentationthat new service needs have arisen and the MHA will not be changed until the annual update isdue?Answer: Any one of these approaches is acceptable if there is clear documentation of thechanging needs and the need for treatment adjustments that are reflected in the serviceschanging. However you do that is up to you.70. If an MHA is not updated within 12 months, but the client remains in services and is scheduled toreturn, should we complete a new MHA or an update?Answer: An MHA update is acceptable if there is still an original MHA in the file that includes allRule 132 required elements. However, if the MHA has expired, a new MHA must be done.7<strong>1.</strong> Please clarify, a client had an MHA in December 2006, an update in July 2007, and an MHA inFebruary 2009. When does the need for an MHA start - from the date of the first MHA, or fromthe date of the most recent update?Answer: Annual updates become due by the date of the most recent MHA or update. In theexample you give, the next update would be required February 2010.72. Can we use a rule-out diagnosis on a <strong>Mental</strong> Health Assessment or Physician/APN evaluation?<strong>Exam</strong>ple: Axis 1, primary billable = 314.01; secondary (not billable) - rule out OppositionalDefiant Disorder.Answer: The ITP shall include a definitive diagnosis that has been determined for all five axes inthe DSM-IV or the ICD-9-CM. If the diagnosis cannot be determined by the time the ITP iscompleted or a rule-out diagnosis is given, the client's clinical record must contain
documentation as to what evaluations will occur in order to provide a definitive diagnosis in theITP. A diagnosis shall be determined within 90 days and the ITP shall be modified to reflect thediagnosis, as necessary. Therefore, each axis must have a definitive diagnosis ultimately withouta rule-out diagnosis. There is no statement in the rule about a secondary diagnosis on any axis.Of course, services provided must be to address the definitive diagnosis.73. The MHA and the psychiatric assessment have large areas of overlap. Our psychiatrist is willingto do a document that would include all points in the MHA and the psychiatric assessment in onecombined document. Is it acceptable to do so and title it "mental health and psychiatricassessment?"Answer: There is nothing in Rule 132 that prohibits an expanded mental health assessment thatincludes more than the Rule 132 required elements, at least one face-to-face by the Q, and Land Q dated signatures. The title of the document could be mental health and psychiatricassessment.74. Providers have 30 days to complete a mental health assessment. Does the 30 day clock start totick with the face-to-face interview, the opening of the case?Answer: The provider shall complete a mental health assessment report within 30 days after thefirst face-to-face contact.75. If a clinician amends or adds an addendum to the MHA before the annual review date, is thesignature of the Q/L required? The additional information may include recommendations forservices to be added to the ITP.Answer: According to the Rule, the ITP is based on the mental health assessment report and anyadditional evaluations. Given this, we do not believe they would need to get a Q/L signature onaddendums, so long as the Q continued to do timely annual updates and incorporated theinformation from addendums into those updates. Certainly, revisions to the ITP should beacknowledged via signature of the Q/L, as well as the consumer.76. In the past, we did linkages from the SOF and were allowed to use the hospital discharge as theassessment until the patient was released and a full assessment could be done.Answer: The current rule requires that, in order to provide case management - transition linkageand aftercare, it must appear on a treatment plan. That treatment plan may be the treatmentplan from the hospital.77. Does the mental health assessment annual update have to be done based on an interviewsession where the client is present? If client has to be present while mental health assessment isconducted, does the same requirement for a QMHP contact apply? If it can be done based onreview of the previous assessment and knowledge of the client (client not present) is this abillable service?Answer: The same principles apply to the mental health assessment and the annual update.Some of the update is completed based on personal knowledge of and contacts with the client.Other pieces of the update can be done by reviewing the client's record, related documents orcollateral contacts. The time spent completing the update can be billed; the client's presence isnot required for billing. This is true for the initial mental health assessment as well. Justremember that time spent writing the report, without the client present, is not billable. Activitiesrelated to paperwork are part of the administrative component of the rate.78. We have staff in the classroom completing a questionnaire while observing a student duringclass. It relates to the student being either on or off the presented task and is used to helpdetermine a diagnosis of ADHD. They are not technically providing a face-to-face service - nointeraction with the client occurs. What would be an acceptable DHS activity code for a servicesuch as this when not in the assessment period, i.e., the assessment has already beencompleted, CS-Individual or CM-<strong>Mental</strong> Health? The service assists the client. If we use a nonface-to-face code, we have always indicated to staff that the location of the service is office; thisobservation is not in the office but the school.
Answer: Assessments may be ongoing, not just prior to completion of a mental healthassessment. The activity that you describe seems to be mental health assessment.79. I have two clients who need to see our PSR Coordinator for assessments (MHA & CASIG). Shehas never met one of these individuals and only had one meeting with the other, so is notfamiliar with either of them. One individual has a significant speech impediment. Some directcare staff have worked with him for a number of years and understand him quite well. The otherindividual is deaf, and though he reads lips well with people he knows, this is not the case withsomeone he has just met. He signs, but will not employ sign language. In addition, hisconversations and responses are skewed by auditory and visual hallucinations. He sees auras,which speak, and to which he responds, therefore, you must separate responses to you fromresponses to the aura. That is a skill gained through experience with him. To ensure theseappointments are effectual, I am having one of my MHPs sit in with these individuals to provideassistance with communication and help them answer questions, etc. Naturally, the PSRCoordinator will bill for the MHA and CASIG, but in such a situation, is it appropriate for bothstaff to bill different services for the same block of time or do you have an alternate suggestion?Answer: Only one staff can bill for a direct intervention with a client at the same service event.The only exception is when the client is hearing impaired or English is not their primarylanguage, and oral interpretation/sign language services are necessary for the provision ofmental health services. The MHP's time with the deaf client may be covered if the MHP is versedin sign language or oral interpreter services, and the service meets the criteria for OralInterpretation and Sign Language in the Service Definition and Reimbursement.80. When a QMHP meets face to face with a client to gather info regarding application for service andto discuss their fee, is this considered part of the assessment?Answer: This does not appear to relate to the mental health needs of the individual and as suchwould not be considered part of a mental health assessment.8<strong>1.</strong> What service do you bill for when completing the annual re-assessment of services?Answer: Billing is always for the intervention provided. In this case, it seems most likely that itwould be mental health assessment.82. Does there need to be a note for the Q's face-to-face for the MHA and MHA Update or does theirdated signature verify that they had a face-to-face with the client?Answer: Often on MHA reports, there is a statement or box to be checked indicating that a faceto-facehas been done. This, along with the Q's dated signature is sufficient evidence of the faceto-face.However, if the agency intends to bill for the time (at least 71/2 min) spent by the Q inthe face-to-face, there must be a signed, dated note describing the intervention provided.83. When doing an annual mental health assessment (MHA) update, does there have to be a face-tofacecontact with the QMHP like an initial MHA? It doesn't really specify in the Rule in regards toannual updates.Answer: Yes.84. How often and in what programs is a provider of MH services required to administer theMultnomah?Answer: None. The Multnomah is optional, not required.85. What service is billed prior to a mental health assessment, following a SASS assessment? If CaseManagement is provided and no mental health assessment is completed due to the child leavingthe area, are there billing consequences? We currently bill ongoing Social History.Answer: You may provide case management prior to completion of the mental healthassessment.86. Can a psychological evaluation be provided and billed without completing the mental healthassessment and ITP beforehand?
Answer: No. Psychological evaluation needs to be a recommended activity identified on the ITP.87. May completion of the LOCUS be billed as part of the mental health assessment?Answer: LOCUS is an event mode billed as Case Management - LOCUS service.88. Does a patient who will need ongoing, lifetime, medication management, seeing a doctor only,require an mental health assessment or is a Psychiatric Evaluation enough basis; what is thetransition or end date?Answer: All patients receiving on-going mental health services billed under Rule 132 must have amental health assessment. The mental health assessment must be updated at least annually.89. Can an updated mental health assessment be documented in chart (progress note) or will therebe a need for an addendum to the mental health assessment yearly?Answer: A progress note is not adequate. The mental health assessment is to be updatedannually by a QMHP and needs to be approved by the LPHA as documented by the LPHA'ssignature on the assessment update.90. What if the consumer prefers to stay in a program, such as PSR, for maintenance/support, untilready to go to work, etc?Answer: PSR activities can only be billed if medical necessity can be documented. The consumermay need assistance in identifying ways to meet their personal goals.9<strong>1.</strong> For a C&A consumer, which contact starts the 30 day countdown for completion of the mentalhealth assessment, the first contact with parent/guardian, who must consent for children under12, or, the first face-to-face with the child/client? These may be two separate contacts, ondifferent dates.Answer: The first face-to-face with the identified client begins the 30 day countdown forcompleting the mental health assessment.92. Please define "client preferences". Is it preference for MH Rx, mental health assessment, shorttermor long-term Rx goals? A mission statement for MH Rx, assessment?Answer: It could be all of the above, but in terms of Rule 132 it would primarily focus on shortand long-term treatment goals.93. We conduct intake face-to-face for completion of mental health assessment, and bill undermental health assessment, but service/mental health assessment is not started until the client isassigned to a therapist. If there is a wait list, can we set the start of service/mental healthassessment as first meeting with the therapist, rather than the intake date?Answer: The Rule requires the mental health assessment report to be completed within 30 daysfrom the first face-to-face contact. You need to identify the first face-to-face contact and followupaccordingly.94. Does DHS have a tool to document consumer preferences?Answer: No.95. Can the CASIG be utilized as a tool to assess consumer preferences?Answer: It may be utilized, but it is not mandated.96. If mental health assessment & CCP done by/with participation of MHP, do both the QMHP whohad the face-to-face, the MHP & the supervising QMHP have to sign, or is the face-to-face Qsignature sufficient to meet the requirement?Answer: The QMHP who had the face-to-face with the consumer is the only signature required byRule 132.
97. For clients involved in a Crisis Assessment, do the 30 days begin at the time of Crisis or the firsttime they are involved in follow-up services to begin a comprehensive mental healthassessment?Answer: 30 days begins at the time of the first contact which can be defined by the agency.98. How is the first face-to-face date of contact determined; may an agency "pick" any date theywish, or must all client contact be documented (who-what-when-where-why) in writing, so thereis no doubt about the first face-to-face?Answer: The second scenario is more accurate.99. What are the consequences of falsifying documentation in regard to first face-to-face, or otherclient contact?Answer: The agency will have to pay back what they have been paid for the service; the staffperson(s) and agency may face legal consequences for defrauding the state.100. I see people for mental health assessment who don't understand how to take theirmedication, what it is, etc. Several people I have seen are also going to several differentproviders, and I may have been the first person to realize this. You can't always wait until thetreatment plan is completed. In our area, it can take weeks to get an appointment with a doctor.Therefore, the mental health assessment needs to include medication monitoring & training -what do you think?Answer: The mental health assessment can be amended or an addendum can be added whenthis need is identified. The targeted goal can then be incorporated into the treatment plan.10<strong>1.</strong> When an admission note is completed within 24 hrs, can services be billed in the twoweek period before the mental health assessment is completed? If so, what services are allowed,any that will be recommended on the mental health assessment, or only those applicable todevelopment of the mental health assessment?Answer: The provider has 30 days to complete the mental health assessment and ITP, and canprovide all services that were recommended on the Admission Note during those 30 days. If themental health assessment is not completed within 30 days, then no services can be billed afterthe 30 day mark, until the mental health assessment and ITP are completed.102. When a client is discharged from an inpatient psychiatric or other IMD setting, the mentalhealth assessment & ITP of the inpatient setting may be used to authorize provision of CM-Transition, Linkage & Aftercare. (per Service Definition & Reimbursement Guide) At this point,they are not likely to meet Rule requirements. What shall we do - is it okay to just keep thelatest copy in the record, or must we immediately ensure that they are compliant with the Rule?Answer: <strong>Mental</strong> health case management services can be provided 30 days prior to completion ofthe mental health assessment. The inpatient ITP should be in the client record if it is used toprovide transition linkage and aftercare services while you are developing an ITP and they do nothave to specifically comply with Rule 132 requirements.103. Once the mental health assessment face-to-face is determined, the majority of privateinsurance companies approve one, or, with an approved exception 2 sessions; how manysessions within the 30 days will the State approve for billing?Answer: There is no maximum number of sessions for completing the mental health assessmentat this time.104. What happens if the agency provides Case Management prior to completion of the mentalhealth assessment, the client fails to continue treatment, and a mental health assessmentcannot be completed; must we reimburse the state?Answer: Nothing happens, because Case management can be billed prior to the completion ofthe mental health assessment.
105. Will the LOCUS count as the annual mental health assessment update?Answer: No. The LOCUS can be used to determine level of care changes for the consumer, butthere are other elements of the assessment that still need to be reviewed annually.106. When a client is placed into Crisis Respite as the result of a Crisis Assessment, the mentalhealth assessment cannot always be completed immediately due to the client's mental status. Aslong as the crisis assessment recommends CS-Residential, med adm & med monitoring, will thatsuffice for billing until the mental health assessment can be completed, usually within 72 hrs?Answer: Only crisis services and case management can be billed prior to the completion of a<strong>Mental</strong> Health Assessment.107. Iroquois county has one of the highest suicide rates in the state, and coupled withKankakee and Ford counties, one of the highest rates nationwide. Procedures for face-to-faceevaluation of prospective consumers are already established, with MH screening & assessmentfor suicidal &/or homicidal risk, including requirements that the person is seen within 24hrs afterinitial contact. Does the therapist have 30 days after the initial screening to complete a mentalhealth assessment?Answer: The mental health assessment must be completed after the first face-to-face contactwith the client. The state is defining first face-to-face contact as the point in time that the clientshows up ready to commit to participation in mental health services. Presentation at the time ofa crisis may not be the first face-to-face contact if the client doesn't return for services when thecrisis is over.108. What has to be included in the annual mental health assessment update?Answer: Rule 132 defines the necessary requirements in 132.148 a) 9). All information should beupdated with only a couple of exceptions.109. Can we bill for the first face-to-face contact prior to the mental health assessmentcompletion?Answer: Yes.110. Is there a unique billing code for the annual mental health assessment update?Answer: No.11<strong>1.</strong> How do we truly identify services consumer need -v- fitting services to the consumer?Answer: A comprehensive assessment should be the basis of developing an appropriatetreatment plan for a consumer.112. How should we bill for psychological evaluation provided by a Master's level professionalwho is not a licensed clinical psychologist? Would the Psychological evaluation then have to meetthe mental health assessment Rule 132 criteria in order to bill?Answer: A psychological evaluation must be conducted and signed by a licensed clinicalpsychologist. A master's level professional may administer standardized testing as part of theevaluation. If the master's level professional administers standardized testing, and the licensedprofessional does the review, analysis and signs, then the work of the master's level should bebilled as psychological evaluation. If a licensed professional does not conduct and sign, thenthere is no psychological evaluation and the master's level person may not bill it as such. In sucha case, if the Rule 132 requirements for mental health assessment are met, the master's levelprofessional may then be considered to be doing part of the mental health assessment process,and may bill as such.113. We are making an effort to reach out to primary care providers in the community tomake mental health services more accessible to the community and more integrated withprimary care. We want to initiate mental health assessments in the primary care setting. We
hope that we can establish this kind of relationship with a number of medical providers in thecommunity. Can we bill under 132 for these assessments as an off-site service?Answer: First, we would stress that it's important to be doing assessments on consumersbelieved to have a MI diagnosis. Second, yes, MHA can be billed as a 132 service. Whether it'sonsite or offsite depends on the circumstances. If the primary care provider provides office spacefor your staff to use to regularly do assessments, e.g. every Monday morning, then that siteshould become one of your certified sites and the service would be billed as onsite. If, however,you are called periodically to do an assessment that needs to be done at the primary careprovider's location and your staff travel there, it would be offsite. If the primary care providerrefers the consumer to you for an assessment and the assessment can be scheduled and done inyour office, then it would be billed as onsite. (2/22/11)114. An agency does some of the initial mental health assessment when a family first calls.Some of the required information for a mh assessment is gathered and recorded. Can this timebe billed as assessment time even though the family/child doesn't come in for maybe a week atwhich time the assessment is completed and other needed information to do the case opening iscompleted? So the agency does some of the mh assessment on one day, but doesn't do all thecase opening things, as well as finishing the assessment until another date. Can the work on thefirst date be billed?Answer: Yes. MHA is not a one-time event. It is the gathering of the Rule 132 requiredinformation and may take several encounters. The MHA report must be completed within 30 ofthe first face-to-face encounter with the client. (2/22/11)115. Can staff bill for time spent reviewing the client's record and gathering information forthe mental health assessment update, e.g., reviewing progress notes, psychiatric consults,hospitalization records, other assessment, etc., without the client present?Answer: Time spent reviewing the client's record, related documents or discussion withcollaterals for the purpose of completing a mental health assessment or mental healthassessment update is billable. Time spent actually writing the results of those reviews is notbillable. (9/1/11)116. An LPHA reviews the MHA but isn’t able to sign it that day because they are requestingsome additions or changes to the assessment. Can they date it the day the reviewed it or dothey have to date it the day the additions/changes occurred?Answer: The LPHA must date the MHA it the day it is sufficiently complete for a review anddetermination by the L that it is complete and ready to sign. The date must be the date of thesignature. (12/1/11)117. A licensed clinical psychologist meets with a family in order to explain the results of theirpsychological evaluation and recommendations for services/approaches for their child. Howwould this service be billed?Answer: A psychological evaluation is done as a result of a recommendation in a mental healthassessment report. In order for psychological evaluation to be billed it must also appear on theITP. When completed, the psych eval report typically comes back to the Q or L who have signedoff on the MHA and ITP for their review. If the eval results in a modification to the ITP, the Qmust discuss with the client (and parents if a child) what modifications need to be made. Thepsychologist may be part of that process. As described, such a meeting would be for thepurpose of ITP modification and would be billed as such. If a psychologist does the eval andthen explains that eval to the client (parents), that alone is not a stand-alone billable service.(12/1/11)118. Rule 132.148(a)(2) states that the clock starts on the 30 days for the assessment to becompleted at the first face-to-face meeting with the client. It is obviously clinically better for usto begin our initial assessment face-to-face to better determine the client’s service needs but
then we often place the client on our waiting list (unless we determine the needs are urgent)which can result in the assessment being completed late.It seems to us that it is probably not the intention of the rule to encourage phone intakes overface-to-face initial assessments so we are wondering if we could be approved to continue withour current system and not be penalized for seeing the client face-to-face. The only way we cansee to comply with the rule is to not see the client in person and do a phone contact insteadwhich seems to be an unfortunate consequence of the rule.Answer: The point of an assessment, as you know, is to determine the need for services. If inthe initial assessment period, you determine that the person doesn’t currently need services,then bill for mental health assessment and close the case. When the person again comes in forservices, do another assessment. The delivery of services must be based on a currentassessment, so even if you don’t close the case, when the person needs or is ready for services,you’re going to need to redo the assessment to be able to appropriately address her/his needs inthe ITP. (12/1/11)