Trust Board papers July 2012 - Barking Havering and Redbridge ...
Trust Board papers July 2012 - Barking Havering and Redbridge ...
Trust Board papers July 2012 - Barking Havering and Redbridge ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
TRUST BOARD MEETINGWednesday, 4 <strong>July</strong> <strong>2012</strong> at 1.00 pm<strong>Board</strong> Room, <strong>Trust</strong> HeadquartersQueen’s HospitalA G E N D A1. Apologies for Absence2. Minutes of the meeting held on 2 May <strong>2012</strong> (Attachment A)3. Matters Arising <strong>and</strong> Actions4. GOVERNANCE:4.1 Care Quality Commission (SB) (Attachment B)5. QUALITY AND PATIENT STANDARDS5.1 Quality & Patient St<strong>and</strong>ards Performance Report – (Attachment C)May <strong>2012</strong> (NM/DCW/RMcA)5.2 Emergency Care/RESET Programme Update (CG) (Attachment D)5.3 Maternity Services Update (DCW/CG) (Attachment E)5.4 Learning Disability Progress Report (DCW) (Attachment F)6. FINANCE, WORKFORCE AND ACTIVITY6.1 Milestone Tracker/Composite Plan (NM) (Attachment G)6.2 Finance Report – Month 2 (May) <strong>2012</strong>/13 (DIW) (Attachment H)6.3 Workforce Key Performance Indicators (RMcA) (Attachment I)6.4 Transformation <strong>Board</strong> Update (DH) (Attachment J)7. INFORMATIONMatters for Noting:7.1 Interim Chair <strong>and</strong> Chief Executive’s Report (Attachment K)7.2 Declaration of Members’ Interests <strong>2012</strong>/13 (Attachment L)7.3 Infection Control annual report (DCW) (Attachment M)7.4 Minutes of the Quality & Safety Committee meeting held on (Attachment N)the 17 April <strong>2012</strong>7.5 Minutes of the Charitable Funds Committee meeting held on (Attachment O)the 27 March <strong>2012</strong>8. Any Other BusinessDate of Next Meeting: The next public meeting will be held on Wednesday,5 September <strong>2012</strong> at 1.00 p.m. in the <strong>Board</strong> Room, <strong>Trust</strong> Headquarters, Queen’s Hospital9. Questions from the Public10. Exclusion of the Public <strong>and</strong> Press In accordance with the Public Bodies Admission toMeetings Act), to resolve to exclude members of the public <strong>and</strong> press from the remainderof the meeting.<strong>Trust</strong> <strong>Board</strong> Agenda – 4 <strong>July</strong> <strong>2012</strong> 1
1BARKING, HAVERING AND REDBRIDGE UNIVERSITYHOSPITALS NHS TRUSTMinutes of the Part I <strong>Trust</strong> <strong>Board</strong> Meeting held on the 2 May <strong>2012</strong>in the <strong>Board</strong> Room, <strong>Trust</strong> Headquarters, Queen’s HospitalPresent: Mr George Wood Interim ChairmanMrs Averil Dongworth Chief ExecutiveMr Stephen Burgess Medical DirectorDr Maureen Dalziel Non-Executive Director (Designate)Mrs Cathy Geddes Chief Operating OfficerMr William Langley Non-Executive DirectorMrs Ruth McAllDirector of Human Resources & ODMr Keith Mahoney Non-Executive DirectorMr Neill MoloneyDirector of Planning & PerformanceDr Robert RoyceDirector of StrategyProf Anthony Warrens Non-Executive DirectorMs Deborah Wheeler Director of NursingMr Phil WilsonNon-Executive Director, NELCMr David WraggDirector of FinanceMs Caroline Wright Non-Executive DirectorIn Attendance: Mr Nick Hulme Project Lead for Integrated ServicesMs Imogen Shillito Director of CommunicationsMrs Sue WilliamsExecutive Assistant/<strong>Trust</strong> <strong>Board</strong> SecretaryMr Wood opened the meeting by welcoming Dr Maureen Dalziel as Non-Executive Director (Designate) forthe <strong>Trust</strong>. Mr Wood also welcomed members of the Public, including two prospective c<strong>and</strong>idates forConsultant posts at the <strong>Trust</strong>.<strong>2012</strong>/001 APOLOGIES FOR ABSENCEMr Michael White, Non-Executive Director.<strong>2012</strong>/002 MINUTES OF THE PART I MEETING HELD ON 7 MARCH <strong>2012</strong>The minutes of the Part I meeting held on the 7 March <strong>2012</strong> were noted as a true record <strong>and</strong> signed by theInterim Chairman.<strong>2012</strong>/003 MATTERS ARISINGAll actions from the previous meeting completed, or on the agenda for today’s meeting.<strong>2012</strong>/004 CARE QUALITY COMMISSION ACTION PLAN UPDATEMr Burgess presented the Programme Management Office CQC <strong>Trust</strong>-wide Action Plan Progress Report<strong>and</strong> the updated CQC <strong>Trust</strong>-wide Action Plan for March. At present 39% of the 59 recommendations duefor completion by the end of March had been achieved <strong>and</strong> the majority of the others remained on courseto reach their conclusion within the next week or two. The PMO remained cautiously confident that the<strong>Trust</strong> would have 67 of its 81 recommendations green/blue by the end of April. This current position wouldbe presented to the Care Quality Commission <strong>and</strong> External Stakeholders at the Roundtable Event on the 8May. Mr Burgess confirmed that progress was good <strong>and</strong> he did not have to report any insurmountableblockages to the delivery of the Action Plan.The <strong>Trust</strong> <strong>Board</strong> noted the report.<strong>2012</strong>/005 BOARD ASSURANCE FRAMEWORK 2011/12 – QUARTER 4Mr Burgess pointed out to the <strong>Board</strong> that the <strong>Board</strong> Assurance Framework (BAF) was in a transitionalstage <strong>and</strong> its current format was not the final version. The <strong>Trust</strong> was working to improve it <strong>and</strong> would beholding further meetings in the next month to achieve this. Mr Burgess highlighted the detailed sections<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
2on Emergency Care, Infection Control <strong>and</strong> Complaints Management, which were additional to the previousBAF that was presented to the <strong>Board</strong>. He also highlighted the two sections on Governance <strong>and</strong> FinancialGovernance.Mr Wood raised the issue of the gaps in assurance in the Women & Children Services section <strong>and</strong> thecontinued overspending in Maternity due to overbooking of agency <strong>and</strong> bank staff. A review had beenundertaken in the early part of March regarding this continued reliance on bank <strong>and</strong> agency staff <strong>and</strong> it wasnoted that this was due to staff returning from maternity leave <strong>and</strong> then taking their annual leave. TheDirector of Nursing <strong>and</strong> the Chief Operating Officer were reviewing this <strong>and</strong> looking at what was requiredgoing forward. Mr Mahoney raised the number of Insufficient Workforce (20%) of the trends of risks on theRisk Register. Mr Burgess informed the <strong>Board</strong> that the <strong>Trust</strong> was aware that there was a gap inConsultants <strong>and</strong> Middle Grade Doctors in A&E <strong>and</strong> this was reflected in this number. Mr Langley raisedthe issue that the <strong>Trust</strong> was rated ‘red’ on Partnership Working <strong>and</strong> was still awaiting Department of Healthtools. The <strong>Board</strong> discussed the benefit of putting something else in place for the time being <strong>and</strong> agreedthat this required <strong>Board</strong> input, although everyone was aware that there was tangible evidence thatrelationships with partners had vastly improved. It had been noted at a meeting earlier in the weekbetween Local Authorities, Commissioners, Community Services <strong>and</strong> the <strong>Trust</strong> that the dialogue was now‘we’, rather than in the singular. Although the <strong>Trust</strong> did not have the tools in place, the <strong>Board</strong> felt thatPartnership working could be moved to ‘amber’ in order to demonstrate the improvement in relationships,which would be noted in the <strong>Trust</strong>’s TFA by NHS London <strong>and</strong> the Department of Health.The <strong>Trust</strong> <strong>Board</strong> noted the changes to the BAF. The <strong>Board</strong> agreed that Partnership Working could bechanged to ‘amber’.<strong>2012</strong>/006 HEALTH4NEL UPDATEMr Royce, as the <strong>Trust</strong>’s Executive Lead for Health4NEL, presented an update to the <strong>Board</strong> from a briefingpaper prepared by Heather Mullin, Project Lead for Health4NEL. He confirmed that these briefing <strong>papers</strong>were being presented to all <strong>Board</strong>s of organisations in the Sector. Mr Royce highlighted the KeyDeliverables section <strong>and</strong> the amount of work involved with the commencement of implementation, alongwith the challenging timeline for these changes to be made. He also highlighted that in order to managethe activity, 100 beds would need to be released at Queen’s Hospital. This figure needed to be confirmedwithin the bed modelling work that was currently being undertaken. The original IRP had set out a figure of164 beds.Mr Royce informed the <strong>Board</strong> that there was a whole range of enabling capital works required, particularlyat Queen’s <strong>and</strong> the <strong>Trust</strong> now had confirmation from NHS London that it would be required to produce anOutline Business Case (OBC) <strong>and</strong> not go straight to a Full Business Case (FBC). The <strong>Trust</strong> was thereforeworking on the basis of the OBC being completed by the 31 <strong>July</strong>. It was very important that the OBC <strong>and</strong>the Long Term Financial Model (LTFM) were entirely intertwined <strong>and</strong> one informed the other. Once theOBC had been prepared <strong>and</strong> assuming sign-off by the <strong>Board</strong> <strong>and</strong> the Commissioners, it would then go toNHS London <strong>and</strong> if approved there the <strong>Trust</strong>, with its Commissioner, would move to the preparation of anFBC. The <strong>Board</strong> noted that the preparation of an OBC would impact on the timing of implementation. MrRoyce had a copy of the framework for the production of the Business Case <strong>and</strong> informed all <strong>Board</strong>members that this was available from him if anyone wished to review it.Mr Royce reported that it was planned to have the Urgent Care Centres treating 50% of patients presentingat the Hospitals by June 2013. This target was a considerable way off on both sites (King George <strong>and</strong>Queen’s), but on a more positive note, in relation to the Midwifery Led Unit (MLU), Cornflower A wasclosed as planned at the end of April, enabling the estates work to commence, so the MLU scheme wasnow ‘up <strong>and</strong> running’. The Chief Executive informed the <strong>Board</strong> that as the <strong>Trust</strong> had closed Cornflower A,it had opened a contingency ward at King George Hospital. The Chief Operating Officer raised the pointthat there were no Urgent Care Centres in the Sector that took 50% of patients (could meet 50% if youincluded Paediatrics), but it was extremely difficult to get to 50% <strong>and</strong> this therefore needed to be factored in<strong>and</strong> reviewed. Mr Royce would feedback these concerns to the Health4NEL Project Team <strong>and</strong> wouldpropose that the <strong>Trust</strong> would like to see a realistic analysis being undertaken as things moved forward.<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
3Mr Royce informed the <strong>Board</strong> that there was a specific workstream to look at King George Hospital withinthe context of the whole health economy <strong>and</strong> it was recognised that this was a key deliverable that had tobe met. The LTFM would include King George <strong>and</strong> how other communities fitted into it. Mr Royce wouldupdate the <strong>Board</strong> on progress at the <strong>July</strong> <strong>Board</strong> meeting, but he emphasised that it was important thatgiven the fact that the Commissioner’s <strong>and</strong> NHS London would no longer be around in March next year,that there was a completely solid plan in place by October this year at the latest.The <strong>Trust</strong> <strong>Board</strong> confirmed their support of the action plan <strong>and</strong> noted those areas which would be led bythe <strong>Trust</strong>.Action: Rob Royce 4.7.12<strong>2012</strong>/007 QUALITY & PATIENT STANDARDS PERFORMANCE REPORT – MARCH <strong>2012</strong>Mr Moloney presented the Quality & Patient St<strong>and</strong>ards Performance Report for March <strong>2012</strong>. Mr Langleyraised the issue of the team of Social Workers from <strong>Havering</strong> Social Services <strong>and</strong> a <strong>Trust</strong> DischargePlanning Nurse piloting six day working for six weeks <strong>and</strong> that although two weekends of the six hadshowed improved discharge performance, the others were disappointing. Mrs Geddes did not know thedetail around the pilot, but she commented that although additional resources could be put in, the <strong>Trust</strong> didnot have enough Consultant presence at the moment to facilitate an increase in discharges. This was partof the work she was taking forward with McKinsey. It could be something very simple like an administratorwho worked all week, but did not work at the weekend. It was therefore about finding out how the wholesystem worked <strong>and</strong> ensuring that everyone was clear <strong>and</strong> understood changes being made <strong>and</strong> how theyinter-related with other organisations.The <strong>Board</strong> agreed that it was good news that the <strong>Trust</strong> was delivering consistently on a whole range of keyperformance indicators, including the 18 week target, Cancer <strong>and</strong> Elective Admissions. An area ofconcern was the lack of confidence in the <strong>Trust</strong>, its Doctors <strong>and</strong> nurses <strong>and</strong> midwives. This wasdisappointing, due to the number of people that had been recruited recently. The fact that there was nosense as to what mitigating action the <strong>Trust</strong> was planning to take to address this was also of concern. MsWheeler confirmed that these were responses on the ‘real time’ surveys <strong>and</strong> there had been a report to theQuality & Safety Committee regarding this. She informed the <strong>Board</strong> that the h<strong>and</strong> held devices on thewards had now been installed at King George. The <strong>Trust</strong> had seen more information coming through overthe last couple of months from these sources <strong>and</strong> this would assist in providing more robust data. Thisdata could be drilled down to ward/unit level <strong>and</strong> the Director of Nursing’s Department was talking to thenew Clinical Directors to see how they could use this information with their teams.The <strong>Trust</strong> had recently received the Patient Survey <strong>and</strong> the Inpatient Survey, both of which were not good<strong>and</strong> the Chief Executive confirmed that she had spoken to the Senior Leaders in the <strong>Trust</strong> this week <strong>and</strong>given them the results. Mrs Dongworth confirmed that the <strong>Trust</strong> would be taking all the work on thisthrough the Transformation <strong>Board</strong> <strong>and</strong> tracking it to ensure improvement over time.The Chief Executive drew the <strong>Board</strong>’s attention to the <strong>Trust</strong>’s performance on MRSA. Ms Wheelerinformed the <strong>Board</strong> that the <strong>Trust</strong> had exceeded the trajectory for last year by two. The target for this yearhad been set at seven <strong>and</strong> the <strong>Trust</strong> had already reported one case during April. Ms Wheeler confirmedthat a root cause analysis on this case was being undertaken. The <strong>Trust</strong> had been under scrutiny, as thiswas the first reported case in London. The Chief Executive confirmed that the <strong>Trust</strong> was sighted that, eventhough the target was seven, it wanted to come in under this figure by the year end <strong>and</strong> Mrs Dongworthhad invited an External Assessor, who was a Microbiologist at another <strong>Trust</strong>, to look at the <strong>Trust</strong>’s InfectionControl processes <strong>and</strong> the incidents of Norovirus last year. The <strong>Trust</strong> had had ongoing ward closuresthrough April for Norovirus. The External Assessor would look to see if there was anything that the <strong>Trust</strong>should do to tighten up its policies.The <strong>Trust</strong> <strong>Board</strong> noted the content of the report <strong>and</strong> supported the actions to bring the performance back inline with trajectory/target.<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
4<strong>2012</strong>/008 EMERGENCY CARE REPORT ON MARCH <strong>2012</strong> PERFORMANCEThe Chief Executive advised the <strong>Board</strong> that along with the Chief Operating Officer, she had attended aTFA Escalation meeting at the Department of Health with David Flory on the 17 April <strong>and</strong> he had made itquite clear the Emergency Care Pathway/Access target was the Department’s biggest concern, along withthe <strong>Trust</strong>’s finances. With regard to the Emergency Care Target, it was made very clear that theDepartment was setting the <strong>Trust</strong> a realistic target of continuous improvement, rather than a percentage bya set deadline.The Chief Operating Officer presented an update on the work started through the RESET Programme(Jonathan Dimson <strong>and</strong> Nicola Yates from McKinsey were present for this agenda item). In terms ofperformance, the <strong>Trust</strong> achieved 81.15% for the week ending 22 April <strong>and</strong> improved to 86.47% for theweek ending 29 April (KGH achieved 95%) <strong>and</strong> was the best performance for the last five weeks. The<strong>Board</strong> was shown a video, taken by McKinsey, on the Emergency Care Pathway. This was a powerfulmessage in terms of how the <strong>Trust</strong>’s staff viewed the Pathway at the moment, as well as some commentsfrom patients on the care they had received. Mrs Geddes confirmed that next week the <strong>Trust</strong> would befocusing more on the workstream relating to pre 11.00 a.m. discharges, as these were currently indicatingvery low numbers during the week <strong>and</strong> non at the weekend. She also confirmed that there would be a lotof changes taking place around the pre 11.00 a.m. discharges <strong>and</strong> starting from next week the <strong>Trust</strong> wouldbe looking at ways of getting the weekend discharge process in train very quickly. This would involvereviewing Job Plans, in order to get Consultants to come in at the weekend. The <strong>Board</strong> agreed thatCaroline Moore, one of the Deputy Directors of Nursing, should be commended for all her hard work inrelation to the improvement in the bed management process. Ms Geddes confirmed that an additionalresource had been put into the RATing area to enhance that process.Multi-disciplinary ward rounds at 8.00 a.m. had commenced this week <strong>and</strong> in addition to everything elsegoing on, the <strong>Trust</strong> was reviewing the length of stay of all patients over 30 days. As these reduced, the<strong>Trust</strong> would start looking at reviewing those patients with lengths of stay of over 14 days.The Chief Operating Officer was pulling together a Business Case around the costs of the changes to theEmergency Care Pathway, as there would be a cost if the <strong>Trust</strong> was going to ask Consultants to come in atthe weekend. In addition to Consultants working at the weekend, the Medical Director raised the point thatsupport services needed to be in place at the weekend, in order for the hospital to work on a 7/7 basis.Mr Wood thanked McKinsey’s for their work to-date <strong>and</strong> commented that the <strong>Trust</strong> would want to seecontinual sustained improvement. The <strong>Trust</strong> was working towards sustainability, but was sitting on a highlyvolatile system at the moment, <strong>and</strong> was not under any illusion that everything was fixed, as it was not.Mr Burgess informed the <strong>Board</strong> that an Interview Panel had been set in June for Consultants <strong>and</strong> MiddleGrades for the A&E Department <strong>and</strong> indications were that the <strong>Trust</strong> had attracted a good field ofc<strong>and</strong>idates. The aim of the <strong>Trust</strong> was to fill substantive posts with good quality individuals who would servethe organisation well. The medical staff in A&E felt more confident that the <strong>Trust</strong> would be in a betterposition than before to appoint to some of these posts. Recognition to Derek Hicks, Clinical Director forEmergency Care, <strong>and</strong> his colleagues, was given by the <strong>Board</strong> that with everything going on they had givensome of their personal time to go out to headhunt people, so the <strong>Trust</strong> would be able to recruit. Last year,the <strong>Trust</strong> could not get anyone to even fill in an application for a post in A&E.The <strong>Trust</strong> <strong>Board</strong> noted the performance <strong>and</strong> noted the actions taken to improve performance.<strong>2012</strong>/009 MATERNITY SERVICE UPDATE – MARCH <strong>2012</strong>Ms Wheeler distributed the Maternity Services Weekly Performance Report for the week commencing the16 April <strong>2012</strong>, together with a revised copy of the Balanced Scorecard with performance up to the end ofMarch. Ms Wheeler confirmed that the <strong>Trust</strong> was meeting regularly with the Commissioner’s <strong>and</strong> they hadasked the <strong>Trust</strong> to reflect back on the performance reporting over the last six months <strong>and</strong> to put forward aproposal about a revised assurance process that would change the way discussions were framed with the<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
5Commissioner’s <strong>and</strong> would move on to a more sustainable process, rather than detailed aspects of theservice being continuously discussed at meetings.Ms Wheeler informed the <strong>Board</strong> that elective c-sections had been repatriated to the <strong>Trust</strong> from theHomerton since the beginning of April <strong>and</strong> two elective lists per week were running at King GeorgeHospital. Initial indications from women were that they were reporting very good patient experiences. Inrelation to the ‘capping’ of deliveries, the <strong>Trust</strong> had a meeting with the Commissioner next week to reviewthis.Mr Wood referred to the recruitment of 18 midwives <strong>and</strong> the continued use of 42 bank <strong>and</strong> agency staff.Ms Wheeler confirmed that this was partly around e-rostering <strong>and</strong> the impact of annual leave that hadaccrued for midwives on maternity leave, as referred to earlier under the BAF agenda item. Other staff hadalso held back on taking annual leave whilst the service was in crisis <strong>and</strong> had waited for new people tocome into post. Sickness rates had also impacted on the usage of bank <strong>and</strong> agency staff.The <strong>Trust</strong> <strong>Board</strong> noted the content of the report.<strong>2012</strong>/010 REVIEW OF COMPLANTS MANAGEMENTMs Wheeler presented the report from NHS London received mid March, following the review of complaintsmanagement, structures <strong>and</strong> processes undertaken in January this year. The action plan attached to thereport was a draft discussed at the <strong>Trust</strong> Executive Committee last week <strong>and</strong> Ms Wheeler was veryconscious that the new Clinical Directors had not been involved in the initial process, as the Divisions hadbeen in place at the time. Therefore at the <strong>Trust</strong> Executive Committee meeting Ms Wheeler had asked forcomments back by the end of this week, following which the action plan would be formally signed-off <strong>and</strong>the Clinical Directors would take ownership going forward.Ms Wheeler reported that complaints were continuing to be received at the same level; over 100 inFebruary. The biggest volume coming in was around Emergency Care, particularly the EmergencyDepartment. Additional administration support had been put into the Emergency Care Directorate, but theissue now was freeing up clinician’s time to prepare meaningful responses. One of the Associate MedicalDirectors was providing support to the Clinical Director in this regard. Ms Wheeler also informed the <strong>Board</strong>that the Complaints Department was looking at other ways of helping, in order to ensure complaints wereresponded to properly <strong>and</strong> quickly. It was recognised that the whole complaints process had not beenworking well, but the interviews for the report had taken place at the end of December, beginning ofJanuary before more processes had been put in place. The quality assurance for the complaint lettersremained at Executive Director level, but all complaint responses were signed-off by the Clinical Directorsbefore being forwarded for final sign-off. Ms Wheeler confirmed that the Complaints Department hadreceived positive feedback from staff now that they were copied in to the complaint letters/responses.Mr Wood highlighted that some of the recommendations contained in the report had not been included inthe action plan. Ms Wheeler informed the <strong>Board</strong> that she was trying to establish the complaints team as aresource <strong>and</strong> response unit for the organisation, rather than the driver for what happened. This linked intothe Care Quality Commission work <strong>and</strong> the cultural change required for how people work. The currentsystem was not delivering what was required <strong>and</strong> there did not appear to be any actions included aboutwhat the <strong>Trust</strong> was going to do to address this.It was agreed that Ms Wheeler would report back at the <strong>July</strong> <strong>Trust</strong> <strong>Board</strong> meeting on where the <strong>Trust</strong> waswith all of the above work. The question of a dedicated meeting room for complaints was highlighted by MsWheeler, as most meeting rooms were within clinical areas <strong>and</strong> were not a good place to conductconfidential complaints meetings. This issue would be addressed quickly.The <strong>Trust</strong> <strong>Board</strong> noted the attached draft action plan <strong>and</strong> the verbal update given to reflect the discussions<strong>and</strong> decisions from the <strong>Trust</strong> Executive Committee meeting.Action: Deborah Wheeler 4.7.12<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
6<strong>2012</strong>/011 ISSUES FOR ESCALATION FROM QUALITY & SAFETY COMMITTEEMr Burgess drew to the <strong>Board</strong>’s attention the Quality & Safety Committee’s recommendation that the <strong>Board</strong>give consideration for patient’s being invited to attend the Public <strong>Trust</strong> <strong>Board</strong> meetings to present theirexperiences/stories. The Patient Stories paper had been prepared by Gary Etheridge, Deputy Director ofNursing. The <strong>Board</strong> discussed whether, with all the current workload, this was the right time to take thisforward, as it would create additional work at a time when people were already very busy <strong>and</strong> shouldperhaps be deferred for the time being.The Chief Operating Officer informed the <strong>Board</strong> that this was a practice that had been in place when shewas at Whipps Cross <strong>and</strong> it had been recognised as really powerful <strong>and</strong> should be a top priority for this<strong>Trust</strong>. Mrs Geddes felt it was really important for the <strong>Trust</strong> <strong>Board</strong> to agree to this recommendation fromthe Quality & Safety Committee. It was proposed that Caroline Wright <strong>and</strong> Anthony Warrens, as Co-Chairsof the Quality & Safety Committee, should test it out at their meeting, work the recommendation through<strong>and</strong> bring back a proposition to the <strong>Board</strong>.The <strong>Trust</strong> <strong>Board</strong> noted the paper presented to the Quality & Safety Committee, supported it in principle, butagreed to defer for 3-6 months to provide the opportunity for the Co-Chairs of the Quality & SafetyCommittee to review the recommendation <strong>and</strong> to put a proposition together for the <strong>Board</strong>.Action: Caroline Wright/Anthony Warrens 5.9.12<strong>2012</strong>/012 TRIPARTITE FORMAL AGREEMENT MILESTONE TRACKERMr Moloney presented the Tripartite Formal Agreement (TFA) Milestone Tracker, which was the formaldocument being used by NHS London <strong>and</strong> the Department of Health to assess the <strong>Trust</strong>’s performancetowards becoming a Foundation <strong>Trust</strong>. The TFA set out the timeframe <strong>and</strong> the indicators that the <strong>Trust</strong>needed to meet around actions from the previous financial year – delivery of CIP <strong>and</strong> control total,Financial Planning (<strong>2012</strong>/13 SLA <strong>and</strong> Productivity Programme), Care Quality Commission –implementation of recommendations, Service Performance <strong>and</strong> implementation of Health4NEL. Aspreviously mentioned, detailed discussions had been held with NHS London <strong>and</strong> the Department of Healthwhen the Chief Executive <strong>and</strong> Chief Operating Officer had met with David Flory recently to review the TFA.The Chief Executive informed the <strong>Board</strong> that Neill Moloney <strong>and</strong> Helen Brown, Director of Performance &Delivery at NHS North East London <strong>and</strong> the City (NELC), were looking at how they could take the format ofthe TFA to the next level <strong>and</strong> were also reviewing the milestones that needed to be achieved. This wouldresult in a new format for the TFA being used for the next <strong>Trust</strong> <strong>Board</strong> report.Mr Wood raised the issue of the <strong>Trust</strong> meeting the agreed Emergency Care trajectory <strong>and</strong> Mrs Geddesconfirmed that she had prepared a draft trajectory to get the <strong>Trust</strong> to 95% by the end of <strong>July</strong>, but this wouldbe firmed up once the letter awaited from David Flory, following the meeting on the 17 April, was received.Mrs Geddes would provide copies of the trajectory for all members of the <strong>Board</strong> at the <strong>July</strong> <strong>Trust</strong> <strong>Board</strong>meeting.The <strong>Trust</strong> <strong>Board</strong> noted the report.Action: Cathy Geddes 4.7.12<strong>2012</strong>/013 BUSINESS PLAN <strong>2012</strong>/13Mr Moloney presented the Business Plan for <strong>2012</strong>/13. This plan sat on top of the Directorate <strong>and</strong>Corporate Departments Business Plans <strong>and</strong> pulled together all planning assumptions <strong>and</strong> key priorities for<strong>2012</strong>/13. It also included a detailed analysis of the workforce plans <strong>and</strong> the underlying financialassumptions. Mr Moloney reported that there was still a gap on the QIPP (CIP Programme) <strong>and</strong> thiswould be the focus of the next few weeks. Following a question from Mr Langley regarding interdependencieswith other organisations within the local economy, Mr Moloney informed the <strong>Board</strong> that the<strong>Trust</strong> was not currently fully engaged <strong>and</strong> there was a lot more work to be done. Part of this work would<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
7include Integrated Services within the Health4NEL implementation, which Mr Nick Hulme was leading on.Services currently in place needed to change considerably <strong>and</strong> the <strong>Trust</strong> would expect to see this occurringduring <strong>2012</strong>. Mr Moloney also informed the <strong>Board</strong> that the Commissioning Strategic Plans were beingreviewed, as these were ambitious in terms of their attempts to reduce non-elective admissions <strong>and</strong>outpatients. The <strong>Trust</strong> was due to receive these Plans shortly <strong>and</strong> would then have a better idea of thelevel of investment that would be put into the community. These Plans would also have a section on interdependencies.Mr Wood raised the point that he would like to see tracking of the WTE by Directorates, along with thepayroll budgets; the WTE figures were included in the Plan, but were at Divisional level, not Directoratelevel. To achieve the <strong>Trust</strong>’s QIPP, the organisation must see significant reductions in headcount. Most ofthis would come out by the elimination of bank <strong>and</strong> agency staff. Mr Wragg confirmed that the Plans, asthey stood, had WTE projected by month <strong>and</strong> had been built into the budgets by month, but the key bitmissing was the QIPP target of £23m. Mr Wragg was reporting that the <strong>Trust</strong> was up to £9.5m ‘green’rated schemes for the QIPP, a further £4m ‘amber’, but the substantial proportion of £10m not yet rag ratedwould be driven by workforce reductions, which was not currently built into the budgets. With the supportof the Commissioner’s, a team from Ernst & Young had been appointed to look at the robustness of theQIPP <strong>and</strong> to identify further schemes to close the gap. Ernst & Young had already started this work <strong>and</strong>would be in the <strong>Trust</strong> for another five weeks. Regular updates on progress would be reported through tothe <strong>Trust</strong> Executive Committee, the Transformation <strong>Board</strong>, <strong>and</strong> also through to the Finance & ProgrammeManagement Committee. Mr Wragg informed the <strong>Board</strong> that the process was behind where the <strong>Trust</strong>would want it to be, but the Executive Team was absolutely clear it had to deliver a 5.5% reduction onincome as its QIPP <strong>and</strong> the process was now in place to deliver this. This key piece of work beingundertaken by Ernst & Young regarding the QIPP gap would enable the Business Plan to be completed<strong>and</strong> ready for ratification by the <strong>Trust</strong> <strong>Board</strong>.Mr Wood registered his concerns around the fact that the <strong>Trust</strong> had recruited 250 new staff, but the bank<strong>and</strong> agency costs had not declined.Ms Wright questioned the fact that there did not appear to be anything in the Business Plan to address the<strong>Trust</strong>’s cultural problems. The <strong>Trust</strong> needed to set out the action that it would be taking to address this <strong>and</strong>the Chief Executive confirmed that it had been agreed that the Transformation <strong>Board</strong> would be looking atthe work programmes to fill this gap <strong>and</strong> would come back to the <strong>Trust</strong> <strong>Board</strong> on the timelines <strong>and</strong> whenthe <strong>Trust</strong> expected the Plan to be populated. This would also be incorporated into next year’s BusinessPlan as well.The <strong>Trust</strong> <strong>Board</strong> noted the current version of the Business Plan for <strong>2012</strong>/13.<strong>2012</strong>/014 INCOME AND EXPENDITURE BUDGETS <strong>2012</strong>/13Mr Wragg reported that the position showed an income <strong>and</strong> expenditure budget deficit of £39.7m,excluding the impact of impairments <strong>and</strong> IFRS. The report set out the bridge reconciliation from the2011/12 outturn position, the proposed budget control totals at Directorate level, QIPP targets for <strong>2012</strong>/13<strong>and</strong> the key assumptions <strong>and</strong> risks. Mr Wragg informed the <strong>Board</strong> that a good contract had been agreedwith the Commissioner’s <strong>and</strong> they were comfortable with the assumptions that had been built in to theposition <strong>and</strong> the way it had been spread across the Clinical Directorates. The <strong>Trust</strong> was expected todeliver the required QIPP cost reduction programme, as other <strong>Trust</strong>s were delivering around 5% to 7%within their plans. NHS London <strong>and</strong> the Commissioner’s were concerned at the level of the QIPP schemesthat were not rated ‘green’, although they recognised the plan was moving forward. The <strong>Trust</strong> had beenworking through this with the Commissioner’s, with the assistance of Ernst & Young, to deliver a morerobust QIPP position.Along with the work being carried forward, which had been referred to above, Mr Wragg <strong>and</strong> the ChiefOperating Officer had been interviewing external Consultants in order to appoint an Interim QIPPProgramme Director to support existing resources <strong>and</strong> to lead the QIPP Programme once Ernst & Younghad completed their current contract. This additional support would provide the <strong>Trust</strong> with its own team tocontinue the monitoring <strong>and</strong> management of the process. Ernst & Young expected to be able to validatetheir work in five weeks time <strong>and</strong> would be preparing an interim report for the Finance & Programme<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
8Management Committee later this month <strong>and</strong> the Transformation <strong>Board</strong> in June. Mr Wragg reported thatErnst & Young was also assisting with the other key element, which was the Long Term Financial Model(LTFM) <strong>and</strong> the three to five year QIPP plan.Mr Langley raised the issue of the current position of the Project Management Office (PMO) staff who werecurrently monitoring Emergency Care, Maternity <strong>and</strong> delivery of the CQC Action Plan. Mr Wragg informedthe <strong>Board</strong> that the <strong>Trust</strong> was currently using an Interim Management Advisory Service in the PMO <strong>and</strong> thedecision on the future of this area, following any recommendations from Ernst & Young that the <strong>Trust</strong> wouldwant to build on, would be made by the new Director of Transformation, Dorothy Hosein, as she would bethe Executive Director Lead for the PMO in the future.The <strong>Trust</strong> had already made two new appointments to the Service Transformation team; a Clinical Lead forQIPP Programme <strong>and</strong> a Head of Service Transformation; two excellent appointments.The <strong>Trust</strong> <strong>Board</strong> agreed the proposed budgets for <strong>2012</strong>/13.<strong>2012</strong>/015 FINANCE REPORT – MONTH 12 (MARCH) 2011/12Mr Wragg confirmed that the <strong>Trust</strong> had delivered the year end control total of £49.9m before £1.1mimpairment reversals. Against plan the adverse variance was £10m, the key variances being income£20.4m favourable, pay £21m adverse <strong>and</strong> non-pay £9.7m adverse. Mr Wragg confirmed the substantialnon delivery of the Cost Improvement Programme (QIPP), which was the major cause of the extent towhich the <strong>Trust</strong> had slipped from the original control total of £40m (£13.9m reported as implemented, whichleft a £14.4m shortfall against the £28.3m target).Mr Wragg reported to the <strong>Board</strong> that the <strong>Trust</strong> had met its statutory targets <strong>and</strong> had a £1.3m underspendon capital allocation to carry forward to next year. There had been a significant injection of cash at the endof the financial year <strong>and</strong> the <strong>Trust</strong>’s debtors had dropped drastically.The <strong>Trust</strong> <strong>Board</strong> noted the report.<strong>2012</strong>/016 ACCOUNTABILITY FRAMEWORK FOR FINANCIAL PERFORMANCE AND COSTCONTROL (ESCALATION POLICY)Mr Wragg informed the <strong>Board</strong> that he had taken comments from colleagues <strong>and</strong> had put together aframework for the management of the Clinical Directorates, with a clear escalation process to be usedthrough the performance management structure. He confirmed that the framework had been designed toexert financial control, rather than correct poor individual performance <strong>and</strong> would be rolled out with effectfrom the M1 performance review meetings. All concerned would be informed that there would be a changein policy in that people would now be held to account <strong>and</strong> this would be communicated to the organisation.Mr Wragg confirmed that meetings would be held with anyone who needed to talk through the framework,in order to fully underst<strong>and</strong> it.The <strong>Trust</strong> <strong>Board</strong> noted the contents of the report <strong>and</strong> approved the framework.<strong>2012</strong>/017 WORKFORCE KEY PERFORMANCE INDICATORS – MARCH <strong>2012</strong>Mrs McAll highlighted several areas from the report, including the recruitment of 209 new staff in post,although there still remained some areas, such as A&E, where recruitment remained a challenge. Asreported earlier in the meeting, the <strong>Trust</strong> had been very encouraged that it had some good Consultant <strong>and</strong>Middle Grade Doctor applicants coming through for interview. Reported sickness absence rates haddecreased for the month of March by 1.40% on the February position, falling from 5.81% to 4.41%. Asreported at the last <strong>Trust</strong> <strong>Board</strong> meeting, the HR Department was doing a lot of work around sicknessreviews <strong>and</strong> were targeting Occupational Health referrals. For the month of March the <strong>Trust</strong>’s annualisedturnover decreased to 10.9% from 11.0% in February, which was 1.1% below the average of other largeAcute <strong>Trust</strong>s of a similar size. Mrs McAll reported that over the last four weeks the <strong>Trust</strong> had seen asignificant decrease in the usage of temporary staff.<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
9The HR Department proposed to commence new starter <strong>and</strong> exit questionnaires, focusing on A&E <strong>and</strong>Midwifery where there were currently a higher than average turnover of staff (current turnover in A&Enursing 18.9% <strong>and</strong> in Midwifery 16.6%) <strong>and</strong> this information would be built into future reports.Mr Wood felt the sickness absence rate was disappointing <strong>and</strong> the lack of ‘Not known’ in terms of thereporting for sickness absence was unacceptable. The <strong>Trust</strong> would reinforce across the organisation thatLine Managers needed to be informed of the reason for sickness absence <strong>and</strong> this must be reported on thesystem. Mr Langley felt it would be useful to have a trend analysis on this so the <strong>Board</strong> could see theinroads being made <strong>and</strong> also the effectiveness of actions, rather than just seeing high numbers. The workbeing undertaken by the HR Department on training Line Managers would help. With the e-rosteringsystem the <strong>Trust</strong> recorded very accurately its sickness absence rates, perhaps more than other <strong>Trust</strong>s, <strong>and</strong>although the <strong>Trust</strong> was running at 4 - 5%, it wanted to get below 4%. As well as the initiatives being run bythe HR Department, the <strong>Trust</strong> needed to set stretch targets for each Directorate <strong>and</strong> foster team workingthrough the OD strategy. The <strong>Trust</strong> needed to get Operational Managers to underst<strong>and</strong> that theorganisation was struggling to achieve the £23m savings <strong>and</strong> they were losing an opportunity in this area tomake savings.Mrs McAll reported that this was the last report that would be based on the old Divisional structure <strong>and</strong> nextmonth’s would be set out in the new Directorate structure format.The <strong>Trust</strong> <strong>Board</strong> noted the report.<strong>2012</strong>/018 CARBON MANAGEMENT PLANMr Royce reported that the <strong>Trust</strong> had been working in collaboration with the Carbon <strong>Trust</strong>, an organisationcreated in 2001 by the UK Government to help organisations reduce their emissions. The reduction incarbon emissions had financial consequences for the <strong>Trust</strong>, as well as for the environment. The paperpresented to the <strong>Board</strong> set out the scale of the challenge <strong>and</strong> outlined the actions required. The <strong>Board</strong>agreed that they were fully in agreement to drive this programme down through the organisation <strong>and</strong> wouldbe pro-active in pushing this agenda. Quite a few of the actions had a lengthy pay-back period <strong>and</strong> insome cases required significant capital investment. As the Chair of the Capital Planning Group, Mr Roycewould be looking to undertake some of these actions this year in the <strong>2012</strong>/13 Capital Programme, in orderto move the Plan forward. There were Grants available, but a lot of the funding had to come from the<strong>Trust</strong>’s Capital Programme. Mr Royce reported that the <strong>Trust</strong> was expected to fund the Programmes toreduce its carbon emissions <strong>and</strong> if it did not, it would be taxed.Mr Mahoney stated that there were normally quite a few savings to be made from good housekeeping,which could be used to fund the capital required in the longer term. Mr Royce also pointed out that the<strong>Trust</strong> had two pieces of Estate which were in a different preparedness for the future, therefore theinvestment would be different for the two sites.The <strong>Trust</strong> <strong>Board</strong> noted the content of the paper, approved the Carbon Management Plan <strong>and</strong> endorsed theactions described in the Plan for implementation.<strong>2012</strong>/019 MATTERS FOR NOTING:INTERIM CHAIR AND CHIEF EXECUTIVE’S REPORTThe <strong>Trust</strong> <strong>Board</strong> noted the Interim Chair <strong>and</strong> Chief Executive’s Report.<strong>2012</strong>/020 MINUTES OF THE QUALITY & SAFETY COMMITTEE MEETING HELD ON THE14 FEBRUARY <strong>2012</strong>The <strong>Trust</strong> <strong>Board</strong> noted the minutes of the Quality & Safety Committee meeting held on the 14 February<strong>2012</strong>.<strong>2012</strong>/021 MINUTES OF THE STRATEGIC PARTNERSHIP BOARD MEETING HELD ON THE22 NOVEMBER <strong>2012</strong>The <strong>Trust</strong> <strong>Board</strong> noted the minutes of the Strategic Partnership <strong>Board</strong> meeting held on the 22 November<strong>2012</strong>.<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
10<strong>2012</strong>/022 MINUTES OF THE CHARITABLE FUNDS COMMITTEE MEETINGS HELD ON THE1 AND 28 FEBRUARY <strong>2012</strong>The <strong>Trust</strong> <strong>Board</strong> noted the minutes of the Charitable Funds Committee meetings held on the 1 <strong>and</strong> 28February <strong>2012</strong>.<strong>2012</strong>/023 ANY OTHER BUSINESSNo further business.Meeting closed at 3.35 p.m.The next meeting of the <strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> <strong>Board</strong> will takeplace on Wednesday, 4 <strong>July</strong> <strong>2012</strong> in the <strong>Board</strong> Room, <strong>Trust</strong> Headquarters, Queen’s Hospital.<strong>Trust</strong> <strong>Board</strong> Minutes Part I – 2 May <strong>2012</strong>
TRUST BOARD MEETINGActions from Minutes of Part I meeting held on 2 May <strong>2012</strong>in the <strong>Board</strong> Room, <strong>Trust</strong> Headquarters, Queen’s HospitalAgenda ItemActionDeadlineDateDateCompleted/Update/Agenda Item2011/108(PerformanceReport)<strong>2012</strong>/006(Health4NELUpdate)<strong>2012</strong>/011(Issues forEscalationfrom Quality &SafetyCommittee)<strong>2012</strong>/012(TripartiteFormalAgreementMilestoneTracker)Update on non-elective length ofstay at next <strong>Trust</strong> <strong>Board</strong> meeting.Provide an update on Health4NELat <strong>July</strong> <strong>Trust</strong> <strong>Board</strong> meeting.Review Patient Stories paper atQuality & Safety Committee <strong>and</strong>prepare proposition for <strong>Trust</strong><strong>Board</strong> members to review atSeptember <strong>Trust</strong> <strong>Board</strong> meeting.Provide copies of the EmergencyCare trajectory at the <strong>July</strong> <strong>Trust</strong><strong>Board</strong> meeting.NM 4.7.12 4.7.12(included in Quality &Patient St<strong>and</strong>ardsPerformance Report)RR 4.7.12 Deferred toSeptemberCW/AW 5.9.12CG 4.7.12 4.7.12Interim Chair …………………Date …………………..<strong>Trust</strong> <strong>Board</strong> Meeting (Part I) 2 May <strong>2012</strong>
TRUST BOARD MEETING2 May <strong>2012</strong><strong>Board</strong> Room, <strong>Trust</strong> Headquarters, Queen’s HospitalPoints <strong>and</strong> Questions raised by members of the Publicat the above <strong>Trust</strong> <strong>Board</strong> meetingQuestion:Mr Skillman mentioned that during theLINk site visit to the Sunrise Wards theyhad observed water jugs being filled,rather than half filled. This made itdifficult for older people to lift the jugs.Response/Action:It was confirmed that the <strong>Trust</strong> hadworked with Sodexo on this <strong>and</strong> hadsourced some half size jugs.Mr Skillman also highlighted that thewater jugs were filled about three timesa day <strong>and</strong> pointed out that when therewas Norovirus on the wards, by takingall the jugs away to refill at the sametime, jugs could get mixed up <strong>and</strong> therewas a possibility of cross infection.Ms Wheeler confirmed that all waterjugs were washed before refilling, butshe would follow this point up with allthe Wards.Regarding the Maternity Report, MrSkillman had attended the Cluster<strong>Board</strong> meeting when maternitynumbers were discussed (a reductionof 2k in <strong>2012</strong>/13). What were the<strong>Trust</strong>’s figures?Why had there been a divert from KGHto Queen’s, as the number of midwiveshad increased <strong>and</strong> the <strong>Trust</strong> was ableto h<strong>and</strong>le the number of births safely?There was a lot of work to do this yearto plan appropriately when activitytransferred across the whole healtheconomy, including Newham <strong>and</strong>Whipps Cross <strong>and</strong> there was reducedactivity at KGH, but plans had not beenfinalised, so the <strong>Trust</strong> was unclear onthe effect.This was about flow <strong>and</strong> the ‘cap’ thatwas still in place. There were furtherdiscussions planned for next weekabout the removal of the ‘cap’.When the MLU is in place, whatescalation plans would be put in place?There would be two escalation plans inplace, one for the MLU <strong>and</strong> one for theLabour Ward, which would form part of<strong>Trust</strong> <strong>Board</strong> Meeting (Part I) 2 May <strong>2012</strong>
Question:Response/Action:the overall escalation plan for theMaternity Unit.Are the C-sections taking place at KGHa permanent arrangement?Yes, until such time as they can berepatriated back to Queen’s. This wasall part of the <strong>Trust</strong>’s bigger plan tobring the KGH maternity unit over toQueen’s.<strong>Trust</strong> <strong>Board</strong> Meeting (Part I) 2 May <strong>2012</strong>
EXECUTIVE SUMMARYTITLE:Care Quality CommissionBOARD/GROUP/COMMITTEE:TRUST BOARD – Part I1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:<strong>Trust</strong>wide Action PlanSince the last report to the <strong>Trust</strong> <strong>Board</strong> in May, the CQCaction plan has been revised. It is now produced in twoparts. One part is the ‘Development Plan’ where actionsidentified by the CQC in their report that are still to becompleted <strong>and</strong>/or new actions that have been identified aspart of the review process to achieve improvement, areadded. This Plan also shows the longer-term actions suchas culture change, leadership <strong>and</strong> strategy in a separateworksheet for ease of reference <strong>and</strong> it has been amendedto show Clinical Director responsibilities.The second part is a ‘Maintenance Plan’ where completedactions are placed once the supporting evidence has beencollected. This was developed to facilitate the ongoingmonitoring of actions to ensure improvements aresustainable.From the 9 th <strong>July</strong> the Transformation <strong>Board</strong> will be takingover the current Project Management Officeresponsibilities, although the existing Project <strong>Board</strong> willcontinue in its current format.The monthly update on progress is attached forinformation.<strong>Trust</strong>wide Review – Progress ReportThe CQC progress report was received on the 20 th June<strong>and</strong> checked for factual accuracy. This report reflects theposition at the <strong>Trust</strong> almost one year on from the CQC’soriginal investigation visits. Where inaccuracies wereidentified in the draft report these were highlighted to theCQC who made changes to their report where theyaccepted the <strong>Trust</strong>’s comments. Their summary ofprogress below shows the CQC’s decision of the currentstatus against the 81 action points:Met 27Part met 48Not met 6The CQC found the direction of travel at the <strong>Trust</strong> to beencouraging but felt we still have some way to go beforewe are consistently delivering the st<strong>and</strong>ards of care thatlocal people are entitled to expect. Their report shows thatimprovements have been made, <strong>and</strong> continue to be made,but they still have concerns about the st<strong>and</strong>ard of A&Eservices <strong>and</strong> about the sustainability of some of theimprovements.The release of the progress report heralds the end of theCQC’s investigation into wider governance structures atthe <strong>Trust</strong>, but they will continue to carry out unannouncedinspections as part of their planned reviews or if theyreceive information raising concerns about our services.Warning NoticesIn the last briefing to the <strong>Trust</strong> <strong>Board</strong> information wasprovided about the return visits to the <strong>Trust</strong>’s maternitydepartments at Queen’s <strong>and</strong> KGH, A&E at Queen’s,Radiology <strong>and</strong> Beech Ward. Their compliance reportswere checked for factual accuracy <strong>and</strong> returned to theCQC.□ TEC ……………..….. □ STRATEGY……….….……□ FINANCE ……..……… □ AUDIT ………….………….□ QUALITY & SAFETY …………..………….....……….…□ WORKFORCE ………………………………………….…□ CHARITABLE FUNDS ………………………………...…X TRUST BOARD …………4.7.12…………….……….….□ REMUNERATION ………………………………….….....□ OTHER …………………………..……. (please specify)
The final reports on these visits have now been received<strong>and</strong> circulated to relevant staff requesting action plans tobe developed. It is anticipated that these will beincorporated into the <strong>Trust</strong>’s existing action plan to ensureall issues are monitored centrally.The deadline for the <strong>Trust</strong>’s response to the CQC is the 5 th<strong>July</strong>, with an internal deadline for receipt of the actionplans of the 3 rd <strong>July</strong>. In summary the CQC’s findings areas follows:Maternity @Queen’sMaternity @KGHA&ERadiologyOutcome 4: Care <strong>and</strong>welfare of peopleOutcome 11: Safety,availability <strong>and</strong> suitabilityof equipmentOutcome 13: StaffingOutcome 11: Safety,availability <strong>and</strong> suitabilityof equipmentOutcome 13: StaffingOutcome 4: Care <strong>and</strong>welfare of peopleOutcome 4: Care <strong>and</strong>welfare of peopleOutcome 13: StaffingOutcome 16: Assessing<strong>and</strong> monitoring the qualityof service provisionOutcome 1: Respecting<strong>and</strong> involving peopleOutcome 13: StaffingModerateconcernMinorconcernsModerateconcernsCompliantCompliantMajorconcernCompliantCompliantMinorconcernBeech WardModerateconcernModerateconcernTermination of PregnancyThe report into the Special Review visit for Termination ofPregnancy was received <strong>and</strong> the <strong>Trust</strong> was found to becompliant. No further actions were required.2. DECISION REQUIRED: CATEGORY:The <strong>Trust</strong> <strong>Board</strong> is asked to note the above report <strong>and</strong> theprogress being made against the CQC requirements.3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:None known4. DELIVERABLES□ NATIONAL TARGET □ RMSX CQC REGISTRATION □ HEALTH & SAFETY□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE ……………………………....□ OTHER …………………….. (please specify)AUTHOR/PRESENTER: Mr Stephen Burgess, MedicalDirectorDATE: 25 th June <strong>2012</strong>Compliance with the Care Quality Commission’s ‘Essential St<strong>and</strong>ards of Quality & Safety’5. KEY PERFORMANCE INDICATORSCompliance with the Care Quality Commission’s ‘Essential St<strong>and</strong>ards of Quality & Safety’AGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
Programme Management OfficeCQC <strong>Trust</strong>-wide Action PlanMonthly Progress Reportto BHRUT <strong>Board</strong>June <strong>2012</strong>Version: <strong>2012</strong>0626.1
1.0 Purpose of this ReportThis report has been produced for the benefit of the <strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University HospitalsNHS <strong>Trust</strong> (BHRUT) <strong>Board</strong>, <strong>and</strong> its Quality & Safety Committee. Its purpose is to provide transparency <strong>and</strong>reassurance that BHRUT is progressing necessary action, to meet the requirements of the recommendationsidentified in the CQC Investigation Report, published in October 2011.At the same time the report will highlight, <strong>and</strong> provide a point of escalation for, any identified risks associatedwith a failure to achieve any of the target dates set. Reports are submitted toward the end of each month; theprevious report having being issued on 31 st May <strong>2012</strong>.2.0 Background to the <strong>Trust</strong>-wide Action Plan ProgrammePrior to 2010/11, BHRUT had a high number of ‘conditions’ placed on it requiring improvements in care.Whilst some of these were lifted during 2010/11, a number of warning notices were subsequently issued tothe <strong>Trust</strong> (in March, June <strong>and</strong> <strong>July</strong> 2011), on staffing levels <strong>and</strong> maternity care. These were responded to ina separate regulatory report.At the end of October 2011, the CQC published its full Investigation Report, containing a total of 75recommendations, with which BHRUT were required to comply; a further 6 recommendations were added inlate November 2011. These 81 recommendations are spread across a number of general categories –strategy, capacity, leadership – <strong>and</strong> some more specific outcomes, including those in relation to maternityservices.Upon receipt of the full Investigation Report, BHRUT constructed a <strong>Trust</strong>-wide Action Plan, detailing all 81recommendations, <strong>and</strong> began populating the plan with the necessary actions required to achievecompliance; along with an identification of officers <strong>and</strong> clinicians responsible for delivery, <strong>and</strong> the targetdeadline dates.3.0 Progress to dateInitial construction of the Action Plan was undertaken by the <strong>Trust</strong>’s Clinical Governance Team inconjunction with operational staff, <strong>and</strong> the <strong>Trust</strong>’s Programme Management Office (PMO) appointed asguardians of its progress in mid-November 2011.In December 2011, a Project <strong>Board</strong> was appointed, chaired by the <strong>Trust</strong>’s Medical Director, <strong>and</strong> Terms ofReference approved. This group meets fortnightly, <strong>and</strong> is responsible for ensuring that actions in the plan areimplemented in a timely <strong>and</strong> rigorous manner.The detail of key progress made in the previous reporting period was as follows:• Since the previous report, of the 24 items then reported as red, 4 have completed <strong>and</strong> turnedgreen/blue with no further items added since turning red at month end; leaving 20 items at ‘red’status.• The number of fully completed items (green or blue) has increased from 37 to 47, which means that,currently, 58% of the 81 recommendations are fully complete. Inspection of the whole plan willconfirm that a significant number of individual actions are now completed.• A comprehensive review of the plan was undertaken, in advance of the proposal to freeze theexisting plan <strong>and</strong> create a Development <strong>and</strong> a Maintenance plan.• Work with Parkhill has commenced on an audit, to seek independent assurance that the <strong>Trust</strong>’sgovernance of the plan, its delivery of service improvements <strong>and</strong> the evidence gathered, is capableof withst<strong>and</strong>ing scrutiny.• The major work being done by McKinsey Consulting, who are managing the RESET programme,has now been cross-referenced to the existing plan <strong>and</strong> will also inform the new Development Planreferred to above.The details of key progress made in this reporting period are as follows:• Since the last report, of the 20 items then reported as red, 4 have completed <strong>and</strong> turned green/bluewith no further items added since turning red at month end; leaving 16 items at ‘red’ status (seeparagraph 5).4
• The number of fully completed items (green or blue) has increased from 47 to 51, which means that,currently, 63% of the 81 recommendations are fully complete. Inspection of the whole plan willconfirm that a significant number of individual actions are now completed (also referenced inparagraph 5 below).• The original CQC <strong>Trust</strong>wide Action Plan was ‘frozen’ at 31 st May <strong>2012</strong> <strong>and</strong> the new Development<strong>and</strong> Maintenance Plans created (see below).• Work with Parkhill has continued on the audit, to seek independent assurance that the <strong>Trust</strong>’sgovernance of the plan, its delivery of service improvements <strong>and</strong> the evidence gathered, is capableof withst<strong>and</strong>ing scrutiny. Their draft report is awaited.• Some of the items within the Development Plan have been reviewed, enhanced <strong>and</strong> exp<strong>and</strong>ed, inorder to ensure that they are comprehensive, reflect the true extent of the work to be undertaken<strong>and</strong>, thus, enable more effective monitoring of progress. (An example being strategicrecommendation S2, which has increased from 1 action to 13, to encapsulate the full range of theHealth4Nel programme.)As indicated in the last monthly report, the original CQC <strong>Trust</strong>wide Plan was ‘frozen’ as at 31 st May <strong>2012</strong>.The reasoning behind this was twofold:• Once improvements had been achieved, it was essential that they become embedded <strong>and</strong> are seenas ‘business as usual’. Therefore, sustainability needs to be monitored;• The longer the plan existed in its original form, the more likely it was to become less ‘current’; astime progresses, additional improvements will be identified. Therefore, it was seen as essential thatthis flexibility was captured.Consequently, the decision was taken to create a ‘Maintenance Plan’ - in order to satisfy the first of thosepoints – <strong>and</strong>, a Development Plan – to satisfy the second of those points.Those recommendations fully completed, <strong>and</strong> evidenced, would drop into the Maintenance Plan, where amonitoring programme would be developed. Currently the recommendations in the Maintenance Plannumber 11, shown as ‘blue’ on the dashboard below. In future iterations, this dashboard may well need toevolve to reflect the changing nature of these plans.Those recommendations that remained incomplete would continue to sit in the Development Plan untilcomplete, currently those number 70.The Development Plan would become a dynamic document, constantly being improved <strong>and</strong> enhanced toreflect ideas <strong>and</strong> the evolving nature of some of the projects. To that end, those projects that have a deadlinedate that has not yet been reached – currently numbering 14 – have been dropped into a separateworksheet within the Development Plan – named as a ‘longer-term development plan’.The timing of this major change to the formatting of the plans has also coincided with the issue of the CQC’supdate report. This report is discussed in a little more detail below but, significantly, it states that it “marks theend of the CQC’s investigation” <strong>and</strong>, therefore, the changes we have made would seem entirely appropriate.In addition to the dashboard evolving, it is also reasonable to note here that future reports may also need tochange, in the format of their content.
4.0 Performance against Key IndicatorsThis is a Headline Dashboard showing current status of progress against the 81 original recommendations.Red indicates non-compliance with, or at serious risk of not meeting, target completion date;Amber indicates progress on-course for compliance with target completion date;Green indicates outcome achieved;Blue was added in <strong>and</strong> indicates that evidence of compliance has been stored in the electronic database.Risk Status / Category Red Amber Green Blue1 High RiskStrategy 1 1Capacity 1Leadership 1 1 2 1Maternity 1 1 7 1General Outcomes 7 4 11 52 Medium RiskMaternity 1 4General Outcomes 4 4 10 33 Low RiskMaternity 1General Outcomes 2 2 5Totals (81) 16 14 40 11Note: Whilst compliance against a single recommendation may not have been fully met, some of the singleactions <strong>and</strong> tasks required for attaining that recommendation may have been completed. The BRAG ratingagainst the single recommendation will not show green until all actions pertaining to it have been completed;then blue when evidence has been filed in the <strong>Trust</strong>’s central database. At this point, the recommendationwill drop into the ‘Maintenance Plan’.5.0 Risk <strong>and</strong> Issue EscalationAs indicated in paragraph 3, <strong>and</strong> confirmed in the dashboard at paragraph 4, there are 16 recommendationsthat are at ‘red’ status in the current Development Plan, plus 14 amber-rated recommendations.5.1 The current position on each of those red-rated recommendations is as follows:Leadership• Recommendation L2 – Put a cultural change programme in place. (6 actions – 3 incomplete.) Project<strong>Board</strong> members are currently reviewing this item, as it is thought that we may have delivered it, in termsof the original requirements in the plan. 3 of 6 actions are showing as incomplete but, that may berevised. However, embedding culture change is a much longer term piece of work <strong>and</strong> one that shouldremain in the Development Plan.Maternity• Recommendation M7 – transfer of babies to NICU. (2 actions – 1 incomplete.) Audit prompted by CQCAction Plan proved that this was a non-issue but, had resulted in a sub-action plan to reinforce. This hasall but been delivered.•6
• Recommendation M14 – record keeping/management. (3 actions – 1 incomplete.) It is now consideredthat this recommendation is probably complete. The literal application of the recommendation/actions inthe CQC plan have been delivered. Since 1/1/12, all new birth records are tracked <strong>and</strong>, once we reach1/9/12, this will mean that all are.Outcome 4• Recommendation G5 – empowerment to challenge. (4 actions – 2 incomplete.) This work has now beenrolled into the RESET programme: workstreams 1&2.• Recommendation G6 – staff following hospital policy. (4 actions – 1 incomplete.) In terms of the originalCQC recommendation, only 1 of 4 actions remain outst<strong>and</strong>ing, relating to an anaesthetic leaflet; which isbeing designed by one of the clinical fellows.• Recommendation G10 – discharge <strong>and</strong> bed management (linked to RESET). (6 actions –2 incomplete.)Incomplete actions should hopefully be delivered by end of June.• Recommendation G11 - Produce <strong>and</strong> disseminate clear guidance on the <strong>Trust</strong>’s expectations for all staffon the prescribing <strong>and</strong> dispensing of TTA medication. (5 actions – 2 incomplete.) (linked to RESET work)All processes <strong>and</strong> procedures are in place but, the software does not currently permit effectivemonitoring of compliance. Discussions underway with Project <strong>Board</strong> members <strong>and</strong> a business case isbeing prepared to seek budget for the enhancement.Outcome 10• Recommendation G25 – Clear lines of sight in inpatient areas. (1 actions – 1 incomplete.) Furtherconsideration needs to be given as to how the <strong>Trust</strong> can meet CQC expectations. In the meantime,Divisional Nurse Directors are progressing it by working on delivery of the SNCT, <strong>and</strong> implementinghourly rounds.• Recommendation G26 – Develop appropriate facilities in day surgery. (2 actions – 2 incomplete.) Oneaction is progressing, but will necessitate some internal building work. The other action is dependentupon Health4NEL programme, yet to be finalised. Therefore, delivery is some months away <strong>and</strong> ourdeadline date may need revising once plans are finalised.Outcome 11• Recommendation G29 – develop sense of responsibility. (2 actions – 2 incomplete.) One action is linkedto L2 <strong>and</strong> subject to review <strong>and</strong> inclusion in the Development Plan; <strong>and</strong> one action needs to becompleted but, its progression is dependent upon a Clinical Governance Report to <strong>Trust</strong> <strong>Board</strong> on 4th<strong>July</strong>.Outcome 13• Recommendation G30 - accurate, clear, comprehensive workforce data. (2 actions – 2 incomplete.)Unfortunately, this item has slipped; it has been escalated to Director of HR <strong>and</strong> current anticipateddelivery is mid-<strong>July</strong> <strong>2012</strong>.• Recommendation G31 – workforce strategy. (3 actions – 2 incomplete.) Remaining actions relate toWorkforce Strategy - included in HR Business Plan. It is understood that this was due to be discussed atTEC in June, but was pulled from agenda by CEO.• Recommendation G36 – skills escalation programme. (4 actions – 1 incomplete.) 1 of 4 actions remainincomplete. A&E workforce review completed. All staff grades /types reviewed. Further work needed onthe role of Doctor's assistant. Potential support from other organisations being worked through. Trainingprogramme for consultation being developed.Outcome 14• Recommendation G37 (Refresh whistle-blowing policy) – This item is in relation to the BHRUT Whistleblowingpolicy, (3 actions – 2 incomplete.) Ostensibly complete. Remaining actions requireWhistleblowing Policy to be ratified at Policy Ratification - deferred <strong>and</strong> on agenda for 25/6/12. On theunderst<strong>and</strong>ing the policy will be ratified work has started to prepare a training course to deliver theoutst<strong>and</strong>ing actions.• Recommendation G38 - develop <strong>and</strong> deliver training for staff to support the development of qualityservices. (3 actions – 1 incomplete.) Remaining action is almost complete. The issue is attendance atm<strong>and</strong>atory training: e-modules are coming on line but, performance management <strong>and</strong> escalation needsembedding.
Outcome 21• Recommendation G50 – records management. (7 actions – 2 incomplete.)2 of 7 actions incomplete. However, one of those involves the development of an e-learning module onrecord-keeping at induction. This is underway but, delivery is anticipated end of <strong>July</strong>.5.2 The current position on each of those amber-rated recommendations is as follows:Strategy• Recommendation S2 – Identify <strong>and</strong> implement plans to secure a long term solution to reduce overcapacity. (1 actions – 1 incomplete.) This recommendation has now been exp<strong>and</strong>ed to reflect the fullimpact of the Health4NEL proposals, in order that a more effective measure of progress can be taken.The result is that there are now 13 actions progressing.Capacity• Recommendation C1 – Improve the flow of patients. (4 actions – 3 incomplete.) Action is progressing;however, the deadline date may need reviewing, as 1 of the outst<strong>and</strong>ing actions links strongly to S2above.Leadership• Recommendation L1 – Right leaders <strong>and</strong> managers in place. (3 actions – 1 incomplete.) It wasanticipated that the remaining action would be completed when the appointment to positions in the newstructure were completed in June. However, events of this month have now raised questions about thelikelihood of delivering as anticipated.Maternity• Recommendation M1 – Identify <strong>and</strong> implement immediate solutions to deliver safe maternity services. (3actions – 1 incomplete.) This, too, is linked to the Health4NEL programme <strong>and</strong> it is anticipated that therevised date for delivery of the outst<strong>and</strong>ing action will be 1 November <strong>2012</strong>.Outcome 4• Recommendation G4 – Develop the ED strategy. (4 actions – 2 incomplete.) Being progressed <strong>and</strong>Jonah is due to be re-rolled with the support of ‘ward sponsors’.Outcome 10• Recommendation G20 – Review directional signage. (3 actions – 2 incomplete.) Progressing – phaseone due to be completed June ’12.• Recommendation G21 – Review paediatric emergency facilities. (2 actions – 1 incomplete.) This, too, islinked to the Health4NEL programme. This recommendation is now linked to the exp<strong>and</strong>ed version of S2<strong>and</strong> will provide more comprehensive detail of the programme. Revised delivery dates will becomeavailable once the preferred reconfiguration option is known.• Recommendation G22 – Finalise <strong>and</strong> implement plans to improve X-ray facilities. (3 actions – 2incomplete.) See G21 above.• Recommendation G23 – Appropriate waiting facilities available for patients <strong>and</strong> relatives in the urgentcare centre. (1 actions – 1 incomplete.) See G21 above.Outcome 13• Recommendation G32 – Carry out systematic skill mix <strong>and</strong> staffing needs analysis. (12 actions – 6incomplete.). Skills for Health completed their skill-mix review of A <strong>and</strong> E at the end of May <strong>and</strong> an actionplan for implementation of their recommendations, plus other recommendations concerning staffing, wasdue to be submitted to the Workforce Committee on 25 th June. Once it has been to that Committee it willgo to the Staff Joint Committee in <strong>July</strong> <strong>and</strong> discussions will then take place with staff in the Department.Outcome 16• Recommendation G40 – Ensure that adequate systems of governance are in place. (4 actions – 1incomplete.) Clinical Governance Report has been subject to revisions <strong>and</strong> aligning with new directoratebusiness plans. Due to be considered by TEC at June meeting <strong>and</strong> <strong>Trust</strong> <strong>Board</strong> in <strong>July</strong> '12.• Recommendation G42 – Carry out a comprehensive review of all corporate <strong>and</strong> clinical governancesystems. (3 actions – 2 incomplete.) Clinical Governance Report has been subject to revisions <strong>and</strong>aligning with new directorate business plans. Due to be considered by TEC at June meeting <strong>and</strong> <strong>Trust</strong><strong>Board</strong> in <strong>July</strong> '12.8
Outcome 21• Recommendation G51 – Develop integrated patient administrative <strong>and</strong> information systems. (1 actions –1 incomplete.) This is a long-term piece of work, with delivery not expected until way into 2013. TheDevelopment Plan has been enhanced to include milestones to enable progress to be more effectivelymonitored <strong>and</strong> identified.Outcome 6• Recommendation G52 – Engage with <strong>and</strong> develop effective working relations with external providers <strong>and</strong>partners. (3 actions – 1 incomplete.) Stakeholder survey due to be progressed June <strong>2012</strong>.It is interesting to note that the CQC Update Report, due to be published 27 th June <strong>2012</strong> reflects that only 6of the 81 recommendations are ‘not met’. Whilst subtle differences in the CQC’s measure of ‘not met’,compared to the <strong>Trust</strong>’s ‘red-rated’, will explain some of this, it may also be apparent that the <strong>Trust</strong> is beingvery reasonable in its self-assessment.Whilst most of these recommendations are progressing towards completion, the Project <strong>Board</strong> will need toclosely monitor the impact on L1; G31; G40 & G42, where changes at Executive Level may have an impact.What is true to say is that the Development Plan is being used to drive progress <strong>and</strong> implementation, <strong>and</strong> theMaintenance Plan will be used to measure sustainability.6.0 Activity during the next period – <strong>July</strong> <strong>2012</strong>The Project <strong>Board</strong> for the CQC <strong>Trust</strong>wide Action Plan will, from now, report to the <strong>Trust</strong>’s Transformation<strong>Board</strong>. At the same time, personnel changes within the Programme Management Office will mean that ah<strong>and</strong>over will be effected before 6 th <strong>July</strong> <strong>2012</strong>.This is a crucial activity in the next period, in order to ensure that there is no loss of momentum <strong>and</strong> there isno impact on the quality of patient care.Alongside this, work will continue to move the red-rated items toward completion at the earliest possibleopportunity; enhance the Development Plan to ensure that it is comprehensive; gather evidence on thoseactions that are completed in order that they can be dropped into the Maintenance Plan; <strong>and</strong> to exp<strong>and</strong> thatplan to ensure that there is an adequate <strong>and</strong> appropriate methodology to measure sustainability – using theCQC’s ‘Essential St<strong>and</strong>ards of Quality & Safety’ as a minimum.The PMO will continue to report back to the Project <strong>Board</strong>, should any significant risks be identified. TheProject <strong>Board</strong> will continue to meet fortnightly to check <strong>and</strong> monitor progress, <strong>and</strong> any risks identified by thePMO.7.0 SummaryThis reporting period has marked a watershed in terms of the CQC <strong>Trust</strong>wide Action Plan.Firstly, our decision to freeze the original plan at 31 st May, <strong>and</strong> create a Development Plan <strong>and</strong> aMaintenance Plan, was undertaken to recognise the need to measure the embedding of improvements; <strong>and</strong>also to facilitate the flexibility required to reflect the evolving <strong>and</strong> emerging nature of projects as theyprogress.Secondly, the CQC Progress Report indicates that it is acknowledged that the <strong>Trust</strong> is making progressagainst the original 81 recommendations. As such, the CQC have stated that the report ‘marks the endof…(its)…investigation’.Thirdly, the Transformation <strong>Board</strong>, along with new personnel within the Programme Management Office, willnow move forward the <strong>Trust</strong>’s delivery of both the Development <strong>and</strong> the Maintenance Plan.Consequently, it is felt that this report effectively marks the end of ‘phase one’, ahead of the migration into a‘phase two’.
As such, we can report the following summary of the current position:• 16 red recommendations;• 14 amber recommendations;• 40 green recommendations.The number of evidenced items in the maintenance plan is:• 11 blue recommendations.Progress TableRecs due Complete %March 56 42 75April 66 50 76May 67 51 76Total 81 51 6310
CQC’s InvestigationIntroductionThe report is an update on progress against the 81 recommendations which weremade as a result of the CQC’s investigation.CQC’s view is that BHRUT has made satisfactory progress against most of therecommendations made in it’s investigation.A number of significant recommendations remain part met <strong>and</strong> a small numberunmet, in many cases because the impact of changes in policy have not yetdelivered better outcomes in practice.The report marks the end of the CQC’s investigation. Quality of care at the <strong>Trust</strong> willnow be monitored through regular unannounced inspections.The <strong>Trust</strong> Wide Action PlanA number of actions were developed in order to deliver the 81 recommendations.The total number of actions developed were 256.The range of actions within the recommendations varied between as few as 1 <strong>and</strong> asmany as 12.Each recommendation is ‘RAG’ rated:Blue – All actions achieved <strong>and</strong> evidence logged.Green – All actions achieved. Not all evidenced.Amber – Actions progressingRed – Actions not progressing or exceeded time deadline.At the end of May the action plan was changed to consist of a Maintenance Plan <strong>and</strong>a Development Plan.The Maintenance Plan contains those recommendations which are RAG rated blue(actions complete <strong>and</strong> evidenced). As of the 22 nd June, 11 recommendations havebeen placed in the Maintenance Plan.The Development Plan has been subdivided into a Short Term Plan(recommendations due to be delivered) <strong>and</strong> a Long Term Development Plan.Currently 9 recommendations sit within the longer term plan. These are all rated asamber.Of the remaining 61 recommendations, 16 are currently red rated.CQC Assessment of PlanThe CQC assessed progress against the 81 recommendations as either met, partmet or not met. 27 were rated as met (33%), 48 as part met (59%) <strong>and</strong> 6 as unmet(8%).1
ReconcilliationAgainst the Maintenance Plan, the CQC agreed that 8 of the 11 recommendationswere met. 3 were assessed as part met, 1 because success needed to bedemonstrated over time.Against the longer term plan, all 9 recommendations were rated as part met, thusagreeing with the project board’s assessment.6 are related to Health4NEL proposals including facilities redesign. 6 are related tothe RESET project <strong>and</strong> workstreams within <strong>and</strong> 6 are related to long term impactwhich will need assessment in the future before the recommendations can be fullymet.In comparing the project board’s assessment against CQC assessment, there isagreement in 54 of the 81 recommendations. In 20 recommendations the <strong>Trust</strong> hasassessed progress rather more favourably. This is due in part to the assessmentbeing at different times, recommendations moving to RESET <strong>and</strong> Health4NEL <strong>and</strong>the need for longer term assessment before recommendations can be met.Stephen Burgess,Medical Director, BHRUT.June <strong>2012</strong>2
Update on investigation report<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong><strong>Redbridge</strong> UniversityHospitals NHS <strong>Trust</strong>Queen’s HospitalKing George HospitalJune <strong>2012</strong>
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportContentsPage1.1 The <strong>Trust</strong> 31.2 Regulatory background 31.3 CQC’s investigation 42.1 Executive Summary 52.2 Leadership, strategy <strong>and</strong> capacity 62.3 Maternity 72.4 Emergency Care 82.5 Complaints 83.1 Compliance activity at the <strong>Trust</strong> 93.2 Queen’s Hospital, Romford, <strong>and</strong> King George Hospital, Ilford(maternity services) 103.3 Queen’s Hospital, Romford (accident <strong>and</strong> emergency services) 113.4 The RESET programme at the <strong>Trust</strong> 113.5 Queen’s Hospital, Romford (radiology services) 133.6 King George Hospital, Ilford: Beech Ward(specialist stroke rehabilitation) 134 CQC’s recommendations –monitoring of progress against the CQC action plan 152
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report1.1 The <strong>Trust</strong><strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> (the <strong>Trust</strong>)serves a population of around 700,000 in outer north east London. It operatesacross two main sites; Queen’s Hospital in Romford, which opened in 2006, <strong>and</strong>King George Hospital at Ilford, which opened in 1993.The <strong>Trust</strong> provides services to people across three local authority areas, <strong>Havering</strong>,<strong>Redbridge</strong>, <strong>and</strong> <strong>Barking</strong> <strong>and</strong> Dagenham, <strong>and</strong> general <strong>and</strong> emergency services tothe population of west Essex with some specialist services to all of Essex. Thethree areas have different demographic backgrounds. <strong>Havering</strong> has a populationof around 232,000 <strong>and</strong> low levels of deprivation, <strong>Redbridge</strong> has around264,000 people <strong>and</strong> average levels of deprivation, <strong>and</strong> <strong>Barking</strong> <strong>and</strong> Dagenhamhas around 172,000 people <strong>and</strong> high levels of deprivation.Queen’s Hospital at Romford is in the <strong>Havering</strong> local authority area, <strong>and</strong> is themain hospital for people from that area, while King George Hospital is in Ilford,<strong>and</strong> mainly serves people in <strong>Redbridge</strong> <strong>and</strong> <strong>Barking</strong> <strong>and</strong> Dagenham.1.2 Regulatory backgroundThe <strong>Trust</strong> had a history of poor performance under the previous regulatoryframework, prior to CQC registration in April 2010. It has long-st<strong>and</strong>ing <strong>and</strong>escalating debts. There have been numerous changes at executive level.At the time of registration with CQC, the <strong>Trust</strong> had a high number of ‘conditions’placed on it to m<strong>and</strong>ate improvements in care. A series of inspections in2010/11 resulted in some of these conditions being lifted, but also resulted inCQC issuing warning notices (in March, June <strong>and</strong> <strong>July</strong> 2011) on staffing levels<strong>and</strong> maternity care.CQC saw some signs of improvement, but its judgement was that continuing totackle poor care on a case-by-case basis was not going to address deep-seatedproblems at the <strong>Trust</strong>. As a result, the Commission took the decision to launch afull investigation into the quality of care at Queen’s Hospital <strong>and</strong> King GeorgeHospital.The investigation was designed to assess the systems <strong>and</strong> procedures the <strong>Trust</strong>had in place to ensure people were protected against the risk of inappropriatecare <strong>and</strong> treatment. The CQC team focused on three care pathways – maternity,elective vascular surgery, <strong>and</strong> emergency care, <strong>and</strong> examined the <strong>Trust</strong>’s governance<strong>and</strong> management systems. More details are available in the full investigationreport (available on CQC’s website www.cqc.org.uk), which was published inOctober 2011 <strong>and</strong> updated with further sections in November 2011.3
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report1.3 CQC’s investigationThis report is an update on progress against 81 recommendations which weremade as a result of CQC’s investigation.A CQC investigation allows the regulator to make recommendations outside itsscope – for example, to draw attention to service configuration <strong>and</strong>commissioning issues. These issues can have a direct or indirect impact on theprovider’s ability to deliver care that meets CQC’s essential st<strong>and</strong>ards of quality<strong>and</strong> safety. Responsibility for implementing these recommendations sits with theprovider <strong>and</strong>, where appropriate, with commissioners.The full set of recommendations addressed a range of outcome areas coveredby CQC’s essential st<strong>and</strong>ards: respecting <strong>and</strong> involving people, care <strong>and</strong> welfare,safeguarding, cleanliness <strong>and</strong> infection control, management of medicines,equipment, staffing, supporting workers, assessing <strong>and</strong> monitoring the qualityof service, records, cooperating with other providers, <strong>and</strong> complaints.A <strong>Trust</strong>-wide action plan was introduced in response to the recommendations.A project board was appointed by the <strong>Trust</strong> in December 2011, chaired by the<strong>Trust</strong>’s medical director, to ensure that the action plan was implemented <strong>and</strong> thatprogress against this was reviewed fortnightly.The final section of this report assesses progress against each of the 81recommendations. This assessment is partly based on the <strong>Trust</strong> <strong>and</strong> NHSLondon’s views, but CQC’s inspection findings have also been considered.Some of the <strong>Trust</strong>’s views on progress have been modified where inspectionevidence suggests otherwise.Progress against these recommendations is not equivalent to compliance withCQC’s essential st<strong>and</strong>ards. Where the recommendations have an impact on careoutcomes that fall under CQC’s core regulatory remit, compliance has beenchecked via inspection. As a result, this report includes a summary of recentunannounced inspections at the <strong>Trust</strong>. Full reports for these inspections can befound on CQC’s website.Several themes are highly significant in light of what CQC’s investigation found– particularly issues around leadership <strong>and</strong> governance, maternity, accident <strong>and</strong>emergency care, <strong>and</strong> complaints h<strong>and</strong>ling. As a result, a brief section on each ofthese has been included in this report in summary.4
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report2.1 Executive SummaryCQC’s view is that <strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS<strong>Trust</strong> has made satisfactory progress against most of the recommendations madein its investigation.The investigation has stimulated a clear improvement in the safety <strong>and</strong> quality ofcare in maternity <strong>and</strong> radiology services at the <strong>Trust</strong>. Governance <strong>and</strong> leadershipstructures have been overhauled as a result of CQC’s recommendations. Work isunderway to develop <strong>and</strong> embed a culture of patient-centred care that runs fromthe <strong>Board</strong> right through to the front line.Action has been taken in the majority of areas highlighted in CQC’s investigation,although a number of significant recommendations remain part-met <strong>and</strong> a smallnumber unmet – in many cases, because the impact of changes in policy havenot yet delivered better outcomes in practice.Maternity has been the greatest focus for the <strong>Trust</strong> <strong>and</strong> commissioners, reflectingthe level of concern identified by CQC. Recent evidence suggests this hasresulted in a marked reduction in the risk of poor maternity care at Queen’sHospital. This view is supported by CQC’s unannounced inspections, interviewswith staff <strong>and</strong> service users, <strong>and</strong> information from other stakeholders. CQC madeclear that it was prepared to restrict services – one of its strongest enforcementpowers – if maternity did not improve <strong>and</strong> the <strong>Trust</strong>’s response, supported byNHS London, has started to deliver results.These improvements need to be seen in context. The direction of travel at the<strong>Trust</strong> is right, but the quality of care on offer is still unacceptable in some areas– particularly in accident <strong>and</strong> emergency at Queen’s Hospital, where too manypeople are at risk of receiving poor care. More needs to be done in medicinesmanagement, in staffing across the <strong>Trust</strong>, <strong>and</strong> in making sure that the Queen’sHospital site is more patient-friendly. Complaints have increased (almostcertainly because of the attention created by CQC’s investigation) <strong>and</strong> the <strong>Trust</strong>is struggling to cope with the volume.Whether the improvements seen so far can be sustained is a big question <strong>and</strong>the <strong>Trust</strong>’s leadership is aware of this, as are those involved in making decisionsabout future configurations of services. For example, the positive changes inmaternity have come about in part as a result of extensive support fromcommissioners. This kind of joint effort is tough to sustain, particularly whenaccident <strong>and</strong> emergency <strong>and</strong> maternity – two services facing huge dem<strong>and</strong> atthe <strong>Trust</strong> – need ongoing support <strong>and</strong> attention.This report marks the end of CQC’s investigation. Quality of care at the <strong>Trust</strong> willnow be monitored through regular unannounced inspections. There are broaderdebates underway about the configuration of services in this part of London.If changes are made to services at this <strong>Trust</strong>, CQC’s role will be to assess whetheressential st<strong>and</strong>ards of quality <strong>and</strong> safety are met, however they are delivered.5
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report2.2 Leadership, strategy <strong>and</strong> capacityCQC’s view is that there has been considerable progress at executive level in the<strong>Trust</strong> in terms of taking ownership of the problems found during <strong>and</strong> sinceregistration in April 2010. It is early days, <strong>and</strong> the effort invested will take timeto have a lasting impact on frontline care, but the direction of travel ispromising. Given the <strong>Trust</strong>’s history of poor performance <strong>and</strong> failure to takeresponsibility for its problems over many years, some of the most significantprogress to date has been through the <strong>Trust</strong> acknowledging its challenges <strong>and</strong>opening itself to partnership working to create a climate that will promoteimprovement.NHS London is supporting the development of a number of clinical fellows atthe <strong>Trust</strong> as part of a clinical leadership <strong>and</strong> engagement programme. A newmanagement structure based around clinical directors <strong>and</strong> associate directors hasbeen introduced to bring in clearer lines of accountability <strong>and</strong> responsibility forthe quality of care. A major programme of internal engagement is underway totry to build a stronger sense of shared purpose between management <strong>and</strong> staffto deliver better care.The Chief Executive <strong>and</strong> members of the <strong>Board</strong> <strong>and</strong> Executive Team have beenopen <strong>and</strong> honest about the <strong>Trust</strong>’s problems <strong>and</strong> have demonstrated clearownership when seeking to tackle the challenges that lie ahead. The seniormanagement tier has been reshaped with a strong focus on drivingaccountability, transparency <strong>and</strong> responsibility for quality into the structure.The <strong>Trust</strong> recently announced that five members of the senior management teamwould be leaving or changing role. This has been explained as a move to supportthe clinical leaders <strong>and</strong> the change process, but the impact of this is not yetknown. Once these posts are filled <strong>and</strong> a stable Executive Team is in place, thenext challenge will be to ensure that the drive for improvement is embeddedacross the <strong>Trust</strong>. Given the amount of poor care seen in the CQC investigationthat was attributable to management <strong>and</strong> culture, this is critical to the <strong>Trust</strong>’sfuture success.The <strong>Trust</strong>’s interim Chair <strong>and</strong> <strong>Board</strong> are offering stronger challenge to theExecutive <strong>and</strong> the interim Chair has explicitly said that care quality is theirpriority; the new governance structures should enable the <strong>Board</strong> to carry outtheir scrutiny roles more effectively, <strong>and</strong> as a result take on more accountabilityfor quality within the <strong>Trust</strong>.6
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report2.3 MaternityThe pressures on maternity services are such that the <strong>Trust</strong> has not been able torespond to CQC’s regulatory challenge alone. Dem<strong>and</strong> is huge <strong>and</strong> there was nosign of this reducing without active intervention. A combination of volume <strong>and</strong>the capacity of staff to deal with complex cases are behind many of theproblems CQC <strong>and</strong> other bodies have seen (e.g. the Royal College ofObstetricians <strong>and</strong> Gynaecologists’ report for NHS London at the <strong>Trust</strong> late lastyear).Late in 2011, CQC made clear that it was considering a legal restriction on thenumber of births at Queen’s Hospital. This led to an escalation in theimprovement work underway <strong>and</strong> saw the <strong>Trust</strong> receive extensive support fromcommissioners.NHS London’s response has involved drawing on expertise <strong>and</strong> insight fromacross London, <strong>and</strong> looking at the challenges faced at the <strong>Trust</strong> in the context ofdem<strong>and</strong> <strong>and</strong> service provision the entire north-east London area. This hasreflected the analysis of the ‘Health for North East London’ programme <strong>and</strong> hasresulted in an ambitious plan to reduce dem<strong>and</strong> on maternity at the <strong>Trust</strong>equivalent to some 2,000 births a year by the end of <strong>2012</strong>/13, compared topre-investigation levels.The North East London <strong>and</strong> City cluster has taken on formal responsibility forimplementation of this maternity plan, which will see decisions taken across thecluster to improve access to safe maternity care. This has already seen plansimplemented (spring <strong>2012</strong>) to move around 20 bookings a week from the <strong>Trust</strong>to Barts Healthcare, taking advantage of capacity elsewhere in the cluster(particularly Newham Hospital). These bookings will translate into births fromNovember.NHS North East London’s proposed response to the challenges faced inmaternity is wide-ranging, innovative <strong>and</strong> proportionate. The proof of the planwill be in its delivery. Success will mean primary care playing its part; GPs <strong>and</strong>community midwives have a critical role in ensuring that mothers-to-beunderst<strong>and</strong> the context in which birth options are presented to them.Within the <strong>Trust</strong>, recruitment <strong>and</strong> retention of a suitable body of skilled <strong>and</strong>experienced midwives continues to be a challenge. The <strong>Trust</strong> currently hasamong the best ratios of staff to mothers in London, but this has only comeabout after six months of intense support from external partners. Holding on tomidwife recruits in the London employment market is an ongoing challenge (<strong>and</strong>is not unique to this <strong>Trust</strong>). The NHS North East London plan to reduce dem<strong>and</strong>is likely to be the only sustainable answer.CQC will continue to assess the quality <strong>and</strong> safety of maternity services at this<strong>Trust</strong>, <strong>and</strong> in maternity units in other trusts taking part in this plan, throughout<strong>2012</strong>/13.7
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report2.4 Emergency CareEmergency care remains the area of greatest concern to CQC. Dem<strong>and</strong> onservices is enormous <strong>and</strong> our original investigation <strong>and</strong> inspections since havefound this service is consistently failing to meet essential st<strong>and</strong>ards.A combination of dem<strong>and</strong>, problems with staffing, challenges in streamingpatients properly, <strong>and</strong> blockages elsewhere in the hospital mean the emergencydepartment at Queen’s in particular is struggling to deliver acceptable care.Patients often face significant delays in admission, treatment <strong>and</strong> discharge.The lack of available beds across the hospital causes a backlog that has animpact on people arriving in A&E. The hospital continues to struggle to recruitmiddle grade doctors <strong>and</strong> there is reliance on doctors from locum agencies.This reduces the level of senior medical cover in the department, meaning it canbe difficult to find people qualified to make decisions about treatment, whichleads to delays in people being given access to the right care.This level of concern about emergency care is corroborated by a range ofexternal sources, ranging from information from patients <strong>and</strong> other stakeholders,through to performance data <strong>and</strong> other regulatory sources. A major programmeof work is underway at the <strong>Trust</strong>, supported by external partners, to try toaddress this. More detail on this programme - <strong>and</strong> on our recent inspectionfindings - is in section 3.2.5 ComplaintsThe <strong>Trust</strong> has seen a dramatic increase in complaints in recent months, from atypical level of around 40 a month to around 120 a month in early <strong>2012</strong>. Staffattitude <strong>and</strong> communication are a key theme of many of these.<strong>Trust</strong> response speeds have increased <strong>and</strong> complaints are now all signed off byan executive director. Patient feedback kiosks are going up across the <strong>Trust</strong>,<strong>and</strong> discussions have taken place about introducing an integrated electronicpatient record. The approach to complaints h<strong>and</strong>ling looks to be much better,with far greater involvement of senior management <strong>and</strong> better processes in placeto ensure lessons are learned from mistakes, but the increase in volume meansthe improved process needs to keep pace with a surge in dem<strong>and</strong>.CQC has seen a rise in information received about this <strong>Trust</strong> since theinvestigation was launched. Anecdotal accounts from stakeholders, includinglocal MP’s offices, indicate that they too have seen an increase in the volume ofcorrespondence about the <strong>Trust</strong>. Some of these complaints pre-date CQC’sinvestigation, although many are more recent. It is hard to know whether thisincrease is a result of more poor care, or a result of greater awareness about the<strong>Trust</strong>’s challenges <strong>and</strong> therefore more willingness on the part of patients <strong>and</strong>their families to raise concerns.8
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportThis remains an area where the <strong>Trust</strong>’s performance must improve. The <strong>Trust</strong> is ina challenging position given the volume of complaints it is now dealing with, butpatients <strong>and</strong> other stakeholders have made clear they expect to see betterperformance in this area despite the increased dem<strong>and</strong>.3.1 Compliance activity at the <strong>Trust</strong>CQC has carried out a significant amount of inspection activity in parallel withthe investigation. The <strong>Trust</strong> was registered with CQC in April 2010 with eightconditions on its registration, setting out improvements that had to be madeagainst eight essential st<strong>and</strong>ards. This was among the highest levels of concernidentified during registration.During the course of 2010/11 most of these registration conditions were lifted,but ongoing compliance monitoring raised further concerns – particularly inmaternity <strong>and</strong> in accident <strong>and</strong> emergency at the Queen’s Hospital site in Romford.Warning notices were served on the <strong>Trust</strong> in March 2011 regarding staffing <strong>and</strong>care in maternity, in June 2011 regarding patient care in A&E, <strong>and</strong> in <strong>July</strong> 2011regarding staffing levels. These compliance concerns triggered the investigationreferred to above. In parallel to the investigation, unannounced inspections tookplace in September <strong>and</strong> October 2011 to assess compliance with these warningnotices. Given the level of concern about maternity, weekly visits took place overeight weeks during October <strong>and</strong> November. Evidence from these visits – whichincluded an independent midwife – was incorporated into compliance reportspublished in early <strong>2012</strong>.In these reports, CQC continued to have major concerns about care <strong>and</strong> welfarein A&E <strong>and</strong> in maternity <strong>and</strong> moderate concerns about staffing in maternity.Throughout the period since the investigation, CQC has received regularinformation from people who use services at the <strong>Trust</strong>, from local MPs, fromLINks, <strong>and</strong> from other sources including staff at the <strong>Trust</strong>. Information fromthese has been factored into compliance activity where appropriate.CQC took part in a risk summit about the <strong>Trust</strong> on 6 February with NHS London,the cluster, <strong>and</strong> the Department to discuss the ongoing challenges faced bythe <strong>Trust</strong>.Information received during this period <strong>and</strong> CQC’s assessment of risk led tofurther inspection activity in <strong>2012</strong>, specifically:• An unannounced inspection of maternity services at Queen’s Hospital from19 to 21 March• An unannounced inspection of A&E services at Queen’s Hospital on 28 March• An unannounced inspection of radiology services at Queen’s Hospital on28 March, with a follow up on 4 April9
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report• An unannounced visit to stroke rehabilitation services at King George Hospitalon Saturday 17 March, in response to patient concerns raised with CQCWe received information after the maternity inspection alleging that staff <strong>and</strong>equipment had been moved between sites to try to influence our judgement.As a result, we went to both the Queen’s <strong>and</strong> King George hospital sites for asimultaneous unannounced inspection on the night of 4 April to confirm thatevidence gathered during our initial inspection was robust (see below).These compliance reports have been published alongside this update <strong>and</strong> can befound on CQC’s website.3.2 Queen’s Hospital, Romford, <strong>and</strong> King GeorgeHospital, Ilford (maternity services)We carried out an unannounced inspection of maternity services at Queen’sHospital on 19 March. This covered a three-day period <strong>and</strong> CQC had supportfrom a maternity expert from the Nursing <strong>and</strong> Midwifery Council. We looked atthree of CQC’s essential st<strong>and</strong>ards: ‘care <strong>and</strong> welfare of people who use services’(outcome 4), ‘equipment st<strong>and</strong>ards’ (outcome 11), <strong>and</strong> ‘staffing’ (outcome 13).The changes that have been introduced in maternity are detailed elsewhere inthis report. All new mothers we spoke to gave largely positive feedback abouttheir stay, including the support received from midwives <strong>and</strong> the pain reliefavailable. Staff told us care had improved as a result of several factors –a significant increase in anaesthetist cover, achieving 100% in one to one carein established labour, increased paediatric care on the postnatal ward to improvedischarge, some improvements in triage times, the moving of the antenatal wardto next to the labour ward, <strong>and</strong> a reduction in births that had helped theservice’s ability to deal with dem<strong>and</strong>. The sustainability of these improvementswill be assessed over time.Equipment raised some concerns at Queen’s; while staff were not aware of itbeing moved between sites, <strong>and</strong> there was a general view that there was enoughequipment, it was not always easy to find. The <strong>Trust</strong> has improved policies forchecks on equipment, but we found evidence that these were not alwayscarried out.The <strong>Trust</strong> vacancy rate for midwives has reduced from 17% to around 11%.Recruitment <strong>and</strong> retention is a constant challenge <strong>and</strong> the <strong>Trust</strong> is now targetingUK midwives after a significant number hired from overseas left. The <strong>Trust</strong>currently has more midwives in place than is indicated as a result of a ‘birth rateplus’ assessment. Midwives generally felt that staffing was much better, althoughthey expressed concern about sustainability <strong>and</strong> the skills mix when so manymidwives were newly qualified or new to the <strong>Trust</strong>. Midwifery care assistants(MCAs) had more significant concerns about shortages, which were supportedby daily records. Staff told inspectors that they generally felt supported bymanagement <strong>and</strong> that morale was better.10
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportAfter our first inspection we received concerns from a member of staff suggestingstaff <strong>and</strong> equipment had been moved between hospital sites to mislead inspectors.We returned to the <strong>Trust</strong>, again unannounced, on the evening of 4 April to speakto members of staff on both day <strong>and</strong> night shifts at the Queen’s Hospital <strong>and</strong>King George sites. We found no evidence to substantiate the concerns at eitherhospital other than those already covered above, although we did receiveconfirmation that members of staff were sometimes moved when another sitewas short-staffed. No member of staff thought this had put patients at risk.3.3 Queen’s Hospital, Romford (accident <strong>and</strong>emergency services)CQC carried out an unannounced inspection of accident <strong>and</strong> emergency atQueen’s Hospital on 28 March <strong>2012</strong>. We looked at one of CQC’s essentialst<strong>and</strong>ards: ‘care <strong>and</strong> welfare of people who use services’ (outcome 4).Major concerns were identified in this service during our last inspection.The <strong>Trust</strong> has made several changes as a result of these, but the departmentcontinues to fail in meeting quality indicators <strong>and</strong> patients remain at too higha risk of receiving poor care.These issues were being picked up by the <strong>Trust</strong> – the introduction of a rapidassessment <strong>and</strong> treatment process was welcomed by nursing <strong>and</strong> ambulancestaff, a recruitment strategy is in place to address the high number of vacancies,<strong>and</strong> the deanery is increasing the number of specialist registrars from two to fivefrom August <strong>2012</strong> – but progress has been challenged by the level of dem<strong>and</strong>.Staff told inspectors that they felt there was a ‘whole hospital’ approach toimprove discharges <strong>and</strong> hospital-wide support for A&E. They did, however, alsosay that the key problem is too many people ‘coming through the doors’ <strong>and</strong>questioned whether more could be done externally to reduce dem<strong>and</strong>.CQC’s level of concern about this area of care has remained high since the <strong>Trust</strong>was registered. The RESET programme (see 3.4) represents a watershedopportunity to introduce sustainable improvement to manage dem<strong>and</strong> in A&E byaddressing performance challenges throughout the hospital. CQC will be seekingfurther assurance that it is having an impact in the near future.3.4 The RESET programme at the <strong>Trust</strong>The <strong>Trust</strong>, with external support funded by NHS North East London, has put inplace an intensive improvement programme for emergency care. The ‘RESET’(Rapid End-to-end Sustainable Emergency Transformation) programme’s aim isto deliver rapid <strong>and</strong> sustainable improvements in the emergency care pathway.The full patient pathway is in scope, with a priority on the urgent care centre,emergency department, medical <strong>and</strong> elderly wards. This programme wasunderway when CQC carried out its latest unannounced inspection.11
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportRESET has identified that performance in the emergency care pathway is worsethan 2011, as evidenced by failure to reach the four-hour A&E target. Queen’shospital is the focus of the programme because they have two-thirds ofattendances (113,000 at Queen’s, 78,000 at King George), but almost four outof every five breaches.The RESET programme identified many challenges that CQC has picked upthrough its compliance work – high use of locums <strong>and</strong> agency staff, ineffectivebed management, <strong>and</strong> poor discharge – but has gone into a far more detaileddiagnosis of underlying issues.This analysis includes highlighting inconsistent triage, poor use of the urgentcare centre, a lack of accountability <strong>and</strong> effectiveness in bed management,discharges taking place late in the day (peaking at 4pm) rather than at 11am asneeded; <strong>and</strong> long lengths of stay, largely driven by factors within the <strong>Trust</strong>’scontrol. Length of stay across the <strong>Trust</strong> is variable (around 48% of patientsexceed the expected date, for internal <strong>and</strong> external reasons) <strong>and</strong> long-staypatients are a challenge in elderly care <strong>and</strong> general medicines. All these createsignificant strains across the care pathway.Staff have contributed to the RESET programme <strong>and</strong> it is clear that many feelunder a great deal of pressure, whether from too much work, high patient-tonurseratios, through to only hearing negatives in the media <strong>and</strong> the constantairing of the <strong>Trust</strong>’s problems in public. RESET aims to both improve performance<strong>and</strong> (through this, in part) build a better working environment for staff.A broad programme of work is underway through RESET with emergencydepartment performance <strong>and</strong> flow, continuity of care <strong>and</strong> discharge rates in themedical assessment unit, <strong>and</strong> discharge, best practice care for complex patients,<strong>and</strong> effective care for elderly patients being prioritised. Initial results madeavailable to CQC indicate an improvement in A&E waiting times <strong>and</strong> week-onweekfalls in the number of breaches, although these results must be sustainedto demonstrate that this has taken root.The number of discharges per day has increased since the introduction of aboard round in the medical assessment unit. Planning for the following day’sdischarges is now taking place at 3pm the day before with a senior nurse lead<strong>and</strong> doctor in attendance. Consultant support has been increased to tackle issueswith care of the elderly <strong>and</strong> length of stay; more ward rounds have beenintroduced <strong>and</strong> lengths of stay are being reduced to more effective levels. Moreclinical nurse specialists have been introduced to improve the specialist responseto cases coming from the medical assessment unit <strong>and</strong> emergency department.Plans are in place to try to ensure that these improvements are sustained <strong>and</strong>built upon. Selected initiatives are due to be rolled out to King George. CQC willseek assurance that RESET is having an impact via unannounced inspections atsome point in the months to come.12
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report3.5 Queen’s Hospital, Romford (radiology services)CQC’s original investigation identified serious concerns with radiology services<strong>and</strong> these unannounced inspections, which took place on 28 March <strong>and</strong> on 4April, were designed to assess whether improvements had taken root. The CQCteam included radiology experts, who also helped review our report. We checkedthree of CQC’s essential st<strong>and</strong>ards: ‘care <strong>and</strong> welfare of people who use services’(outcome four), ‘staffing’ (outcome 13) <strong>and</strong> ‘assessing <strong>and</strong> monitoring thequality of service provision’ (outcome 16).Details of the <strong>Trust</strong>’s work to improve clinical management, audit <strong>and</strong> staffingare included later in this report. We were presented with evidence that showed aweekend rota to reduce the backlog from A&E; a new ‘hot reporting’ rota hassped up the process <strong>and</strong> weekly checks on turnaround times for x-rays <strong>and</strong>scans. Turnaround times have significantly improved <strong>and</strong> people referred for CTscans from A&E have exceeded national targets. Compliance with a NationalPatient Safety Agency (NPSA) alert from 2007 has improved.A new role of clinical director for radiology has been created <strong>and</strong> radiologybecame a department in its own right on 1 April. Radiology leads withresponsibility for care pathways have been introduced. <strong>Trust</strong> documentationverified that vacancies in radiology are now minimal <strong>and</strong> new posts have beencreated through extra activity <strong>and</strong> better financial management. Staff have beengiven support to develop their reporting skills <strong>and</strong> a quality <strong>and</strong> safety audit fornewly-qualified radiographers has been introduced. Anaesthetic support hasincreased.A new <strong>Trust</strong> audit form <strong>and</strong> process has been introduced, but planned audits hadnot always been carried out <strong>and</strong> the clinical director <strong>and</strong> general manager forradiology indicated not enough audit had taken place.3.6 King George Hospital, Ilford: Beech Ward(specialist stroke rehabilitation)We carried out an unannounced visit of Beech Ward on 17 March as a result ofconcerning information about privacy <strong>and</strong> dignity, use of call bells, <strong>and</strong> staffbehaviour that we had received from current <strong>and</strong> former patients. We checkedtwo of CQC’s essential st<strong>and</strong>ards; ‘Respecting <strong>and</strong> involving people who useservices’ (outcome one) <strong>and</strong> ‘Staffing’ (outcome 13).The inspection took place on a Saturday afternoon <strong>and</strong> evening. We talked topatients <strong>and</strong> relatives about the care they had received <strong>and</strong> to staff about issueson the ward. Patients <strong>and</strong> relatives had mixed views; while some were positiveabout the care they had received, others told us that staff were sometimesabrupt <strong>and</strong> a bit rough, <strong>and</strong> that patients had to wait a long time to havecontinence pads changed or to be taken to the toilet.13
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportStaff told our inspectors that they were stretched because of shortfalls instaffing <strong>and</strong> that this had affected their ability to deliver good care. We foundevidence that shifts were not staffed in accordance with rotas, <strong>and</strong> that not allstaff had attended stroke training (particularly a problem on night duty).Management <strong>and</strong> staff were aware of <strong>and</strong> seeking to tackle these concerns.CQC has set a deadline for the <strong>Trust</strong> to address these <strong>and</strong> will be following up tocheck whether enforcement action is necessary.14
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4 CQC’s recommendations –monitoring of progress against the CQC action planThe following pages set out the recommendations made in CQC’s investigationreport <strong>and</strong> include an assessment by CQC of whether these appear to be met,part met or not met. This assessment is based on the <strong>Trust</strong>’s reporting ofprogress to NHS London against its ‘CQC Action Plan’, <strong>and</strong> where appropriate isinformed by CQC’s compliance activity. In some cases, the <strong>Trust</strong> may have takenmeasures to improve procedure but CQC has not yet seen a marked improvementin care quality. This will be followed up through our core regulatory work.Please note that this assessment (met, part met, or not met) is not equivalent toa statement of compliance or non-compliance with CQC’s ‘essential st<strong>and</strong>ards’– the regulations <strong>and</strong> illustrative outcomes published in the CQC ‘Guidanceabout compliance’. For the latest view of compliance, please refer to CQC’sinspection reports.Progress againstrecommendations:summaryPage Area Met Part met Not met16 Strategy <strong>and</strong> capacity 0 3 017 Maternity 9 6 121 Leadership 1 4 023 Respecting <strong>and</strong> involving 2 1 024 Care <strong>and</strong> welfare - Emergency 0 2 125 Radiology 1 2 026 Discharge 0 3 027 Surgery 2 0 028 Cooperation 1 2 029 Safeguarding 3 0 030 Cleanliness 1 2 031 Medication 0 2 032 Premises 1 5 134 Equipment 2 0 135 Staffing 2 5 138 Supporting staff 1 1 039 Quality monitoring 1 5 041 Complaints 0 3 143 Records 0 2 0Total 27 48 615
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.1 Strategy <strong>and</strong> capacity1. The <strong>Trust</strong>, in conjunction with NHS London, should seekappropriate external expertise to support a programme oforganisational change <strong>and</strong> service improvement.Part metThe <strong>Trust</strong> has introduced 10 clinical fellows <strong>and</strong> four midwifery clinicalfellows as part of a clinical leadership <strong>and</strong> engagement programme,supported by NHS London. Commissioners are offering support at executivelevel in the development of the <strong>Trust</strong>’s programme management board tocoordinate the transformation programme. Health for NEL, Skills for Health,<strong>and</strong> the RESET programme in A&E are evidence of the <strong>Trust</strong>’s willingness toengage external support.2. The <strong>Trust</strong>, in conjunction with its commissioners <strong>and</strong>other partners, should identify <strong>and</strong> implement plans tosecure a long term solution to reduce over capacity atQueen’s Hospital.Part metThe Health for NEL proposals <strong>and</strong> estates reconfiguration plan for the <strong>Trust</strong>should see dem<strong>and</strong> reduce significantly over the next two years to addresscapacity issues. This includes seeing dem<strong>and</strong> on maternity fall by 15-20%(between 1,500 <strong>and</strong> 2,000 births a year) by April 2013 through effectiveuse of alternative maternity resources in North East London. Successdepends on partnership working <strong>and</strong> ongoing commissioner engagement,including the role of primary care in making sure that people are aware ofthe treatment choices open to them.3. Improve the flow of patients not only in the emergencydepartment, but across the whole hospital to ensure thatprocesses that do not add value are removed <strong>and</strong> patientsare seen <strong>and</strong> treated in a timely fashion.Part metA range of work is underway to address this – bed mapping, revised lengthof stay, reviews of decisions to admit, care pathways in place for emergency<strong>and</strong> gynaecology care. The RESET programme in A&E is designed to ensurestronger visibility <strong>and</strong> accountability of care pathways throughout thehospital, from admission to discharge. Progress in this will be carefullymonitored both within the <strong>Trust</strong> (including at Executive <strong>and</strong> <strong>Board</strong> level) <strong>and</strong>by external partners.16
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.2 Maternity4. In conjunction with its commissioners <strong>and</strong> otherpartners, identify <strong>and</strong> implement immediate solutions todeliver safe maternity services at the trust, especially atQueen’s Hospital, while developing plans to secure along-term solution.Part metWork with NHS London in the short-term <strong>and</strong> in the longer term via Healthfor NEL, has so far <strong>and</strong> should address the highest risks to safety formothers. Improved audit <strong>and</strong> reporting on c-sections is in place. An audit of1:1 care in established labour saw the <strong>Trust</strong> achieve 100%. CQC’s inspectionshave confirmed that improvements have been made <strong>and</strong> are so far beingsustained.5. Ensure that it configures its maternity services wards<strong>and</strong> departments appropriately to improve the quality ofantenatal <strong>and</strong> postnatal care at Queen’s Hospital.MetAntenatal <strong>and</strong> postnatal wards have been moved to ensure a better patientflow. Incidents <strong>and</strong> complaints about the design of the ward are being actedupon.6. Ensure that there are suitable numbers of midwives toprovide one-to-one care for all women during establishedlabour.MetAudit so far has indicated 100% success; the target for the year is to achievean average of 98% across <strong>2012</strong>.7. Ensure that learning from incidents in maternityservices takes place to reduce the risk to women of unsafecare.Met‘Lessons learned’ sessions are now part of m<strong>and</strong>atory training days <strong>and</strong>near-miss meetings. A newsletter is in place to disseminate learning. Moresupervisors of midwives have been recruited <strong>and</strong> this material feeds intotheir meetings.17
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report8. Take appropriate steps to ensure that all women canreceive adequate pain relief when they need it.MetThis is audited weekly by the cluster; cover has been extended from 8am to8pm, with out of hours cover needing to be increased. CQC’s inspectionshave identified a clear improvement in this area.9. Further improve the maternity triage process with theintroduction of regular monitoring <strong>and</strong> learning to ensurethat services improve for all mothers.Part metNew pathway implemented with monitoring in place; performance reportedweekly to NHS London; triage working group in place. Performance levelsneed to improve.10. Take appropriate action to ensure that babies are nottransferred to the neonatal care unit unnecessarily.Not metPolicy <strong>and</strong> guidelines in place but being reviewed; <strong>Trust</strong> audit has recentlytaken place. Performance outputs not meeting required levels.11. Ensure it uses all staff <strong>and</strong> systems effectively toimprove the discharge process.MetIncrease in qualified midwives allows better discharge; improved process <strong>and</strong>audit in place with regular reporting.12. Undertake a skill mix review in its maternity services,for example Birth Rate Plus.MetBirth Rate Plus review undertaken in addition to <strong>Trust</strong>’s own review ofskills mix.18
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report13. Continue with its recruitment plans in maternityservices to ensure that it has suitable numbers of qualifiedstaff across all service delivery departments.Part metRecruitment is on target to deliver a 1:29 ratio, with higher numbers ofsubstantive staff in post. CQC inspections have identified some concernsaround midwifery care assistant staffing levels. <strong>Trust</strong> has faced challenges inrecruitment <strong>and</strong> retention, although these are not particular to this <strong>Trust</strong>alone.14. Review the clarity of its reporting processes withregard to cardiotocography (CTG) training in maternityservices.MetAll new doctors receive CTG training on appointment; attendance figures areaudited on a monthly basis as part of the maternity dashboard.15. Increase the level of training on the interpretation ofCTGs, so that all staff have undertaken this.Part metAll midwives were due to have completed training by end of March <strong>2012</strong>,although the maternity dashboard showed 84% complete. Regular audits ofattendance are in place.16. Increase the number of supervisors of midwives as amatter of priority, to improve the quality of supervision<strong>and</strong> reduce the burden on those currently in post.MetAdditional supervisors of midwives have been recruited <strong>and</strong> are in place;ongoing review <strong>and</strong> recruitment should deliver a 1:16 ratio by September<strong>2012</strong>.17. Improve the quality of record keeping <strong>and</strong> recordsmanagement in maternity services.Part metTraining for staff <strong>and</strong> a maternity records tracker <strong>and</strong> audit process are inplace, but some problems with implementation <strong>and</strong> targets not being met todate. More that 50% of staff have now been trained in appropriategovernance.19
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report18. Assure itself that it has the right managers <strong>and</strong>leaders in maternity services to deliver high quality safeservices for women.MetDirector of midwifery joined the <strong>Trust</strong> in March <strong>2012</strong>, review of previousallegations of abusive / rude behaviour completed, new allegationsproactively investigated. ‘Role play’ training in place to ensure staff listen to<strong>and</strong> act professionally with women in labour, <strong>and</strong> their birth partners at alltimes. Senior maternity managers, midwives, clinical directors <strong>and</strong>consultants aim to act as role models to drive home message on zerotolerance of abuse <strong>and</strong> rudeness from staff at any level in the <strong>Trust</strong>.19. Ensure that maternity audit processes are integratedwith the rest of the <strong>Trust</strong>.Part metWhile a clinical audit plan is in place <strong>and</strong> infection control is being audited,an audit midwife has only recently been recruited. The full set of policy <strong>and</strong>process measures are in place but performance is not meeting expectedlevels as of the time of writing.20
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.3 Leadership20. Ensure its board assures itself that it has the rightleaders <strong>and</strong> managers in place to develop the trust <strong>and</strong>improve the quality of services.Part metThe <strong>Trust</strong> <strong>Board</strong> has completed its review of the Executive Team, leadingto appointments of chief operating officer <strong>and</strong> director of transformation.A new management structure is in place based around clinical directorates,led by clinical directors <strong>and</strong> associate directors. Recent information indicatesthat there are several changes being made to senior management at the<strong>Trust</strong> <strong>and</strong> the impact of this will need to be assessed. Significant staffengagement process is underway to consult on wider implementation ofnew structure.21. Put a cultural change programme in place across theorganisation. The programme of change needs to engageall staff so that the trust can clearly articulate what theexpectations are of individual staff, what a highperforming organisation feels like to work in <strong>and</strong> be clearof the penalties for staff they should not behaveappropriately.Part metBuilding blocks are in place – ‘Big Conversation’ underway with staffengagement group set up <strong>and</strong> several staff engagement meetings held.Executive team now dedicate one day a month to take on a front line role inorder to increase underst<strong>and</strong>ing of care challenges <strong>and</strong> improve managementvisibility <strong>and</strong> accessibility. Conflict resolution training is being delivered formanagers; BHRUT Code being reviewed with significant staff input,including seeking clear examples of acceptable <strong>and</strong> unacceptable practice.Consultants are carrying out an analysis of team working <strong>and</strong> practice inwomen’s services.22. Develop a culture of whole systems working across alldivisions to reduce ‘silo’ working <strong>and</strong> the combative natureof bed management.Part metWeekly operations meeting, with directorate managers, is now in place;multidisciplinary working being pursued as part of RESET project. New bedmanagement structures is in place, with all divisions <strong>and</strong> specialitiesattending; Matrons working together to ensure effective discharge process.21
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report23. Develop a programme of support for managers so thatstaff with the capability can be freed to undertake theirmanagerial roles effectively.MetStaff engagement process is underway; appraisal rates for managers haveimproved <strong>and</strong> monthly performance reviews now being introduced.24. Explore how to improve its communications bothinternally <strong>and</strong> externally so that perceptions of poorcommunication can be reduced.Part metInternally, significant staff engagement is underway; externally, meetingshave taken place with LINks <strong>and</strong> Improving Patient Experience Group(IPEG); stakeholder briefings being disseminated; stakeholder event withcommissioners, CQC, LINks, IPEG <strong>and</strong> local authorities took place in May.Some feedback to CQC suggests there are further improvements that couldbe made, particularly in terms of engagement with MPs.22
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.4 Respecting <strong>and</strong> involving people (outcome 1)25. Ensure that it acts on the outcomes of its own <strong>and</strong>national patient surveys <strong>and</strong> demonstrate thatimprovements to the quality of the patient experienceacross the trust are made.MetAnnual report on findings is to be produced to coincide with national survey;<strong>Board</strong> now receiving quarterly reports to update on learning. Six-monthlyreports for Hospital Life <strong>and</strong> the Link on improvements achieved as a resultof real-time surveys. Feedback from NHS Choices <strong>and</strong> Patient Opinion is tobe acted on bi-monthly from February <strong>2012</strong>.26. Enhance its existing systems for involving patients inthe development of services to ensure that the patient’svoice is an integral part of every division, ward <strong>and</strong>department engagement strategy.MetRevised patient experience strategy in place, with divisions to develop <strong>and</strong>implement six-monthly patient engagement forums. Links with IPEG willprovide two-way information channels. Real time survey is being rolled outacross wards through <strong>2012</strong>; the first report from this went to the Quality<strong>and</strong> Safety Committee in February <strong>2012</strong>.27. Make sure that proactive <strong>and</strong> m<strong>and</strong>atory training <strong>and</strong>education regarding dignity, respect <strong>and</strong> tolerance isdelivered to all staff.Part metDignity <strong>and</strong> respect benchmarking has been done; compliance reports onnon-attendance are being reviewed <strong>and</strong> a m<strong>and</strong>atory training programme isbeing developed. A leaflet for new staff about the <strong>Trust</strong>’s expectations ofbehaviour has been drafted <strong>and</strong> is due to be reviewed with the staffengagement group before roll out. The BHRUT Code is being reviewed <strong>and</strong>will be issued to all new starters with contract. Quality of Care audits ofdignity <strong>and</strong> respect have been carried out in December <strong>and</strong> March so far <strong>and</strong>will continue in order to audit feedback from the real time patient survey.Bank managers to ensure that competence of all temporary clinical staff inthis respect is monitored; if concerns are raised about temporary staff theyshould either not be booked again or only done so with documentedsupervision.23
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.5 Care <strong>and</strong> welfare of people who use services(outcome 4)Emergency department28. Develop its strategy <strong>and</strong> work for improving flow ofemergency/urgent patients. This strategy needs to havethe engagement of all clinicians <strong>and</strong> managers as a keycomponent.Part metThe ‘Discharge JONAH’ tool is being implemented to focus on discharge <strong>and</strong>length of stay. Daily meetings, weekly performance reviews, <strong>and</strong> the RESETproject mean there is frequent <strong>and</strong> in-depth scrutiny; this will be met whenoutputs match the aspirations in a sustainable way.29. Develop a culture where everyone feels empowered tochallenge episodes of variable or poor practice, includingregular monitoring of practice <strong>and</strong> feedback <strong>and</strong> learningopportunities for staff.Not metThe appraisal process for emergency department staff has been reviewed; allstaff in this area have personal development plans. Hourly vital signs checksare underway <strong>and</strong> monthly spot audits are being carried out to ensure stafffeel empowered to challenge poor performance. Patient satisfaction surveysare in place <strong>and</strong> staff are reminded of the importance of challenging poorpractice as a st<strong>and</strong>ing item on A&E team meetings. Audit results do not yetsupport the processes that have been put in place.30. Ensure that all staff, both permanent <strong>and</strong> temporary,follow hospital policy <strong>and</strong> procedures.Part metAs noted, the appraisal process for emergency department staff has beenreviewed; spot audits of elective surgical consent have indicated some issueswith consistency; not all emergency patients receive all the information theyneed about procedures; <strong>and</strong> a new information leaflet on anaesthesia risks isbeing developed. Performance indicators are still negative.24
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportRadiology31. Develop its planning <strong>and</strong> bed management processesto ensure all patients are cared for in appropriate facilities.Part metMatrons <strong>and</strong> ward sisters are monitoring this but the <strong>Trust</strong> has not yetestablished how best to measure success in this area. The X-Ray departmenthas introduced appropriate checklists for ensuring patients are properlyprepared.32. Put in place clear protocols for the management ofinterventional radiology patients with audit <strong>and</strong>improvement cycles to ensure st<strong>and</strong>ards are attained <strong>and</strong>maintained.Part metAudit processes are in place <strong>and</strong> are monitored at interventional radiologymeetings <strong>and</strong> at the Divisional <strong>Board</strong>. SOPs are in place <strong>and</strong> are beingimplemented for each procedure in interventional radiology. CQC’scompliance activity supports the <strong>Trust</strong>’s assessment of significant progress inthis area, although more audit activity needs to be delivered for this to beconsidered fully met.33. Ensure that it fully implements the 2007 NPSA alertregarding radiology imaging results being communicated<strong>and</strong> acted on as a matter of urgency.MetA distinct operational <strong>and</strong> clinical policy is in place, supported by cyclicalaudits; a longer-term measure will be a reduction in incidents by March2013.25
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportDischarge34. Develop its discharge <strong>and</strong> bed management teams<strong>and</strong> processes to ensure that they are interlinked <strong>and</strong> thatpatient flow is managed effectively from the point of entryto the point of discharge.Part metA single discharge policy is now in place with clear roles <strong>and</strong> responsibilitiesestablished <strong>and</strong> six discharge specialists employed to help with complexdischarges. The RESET project is playing a crucial role in ensuring thatdischarge is managed across all relevant pathways <strong>and</strong> wards. The DischargeJONAH project <strong>and</strong> accompanying audits are in place. Daily meetings withmatrons <strong>and</strong> senior nursing staff review the bed position <strong>and</strong> delays. Theunderpinning processes <strong>and</strong> policies are in place here, but CQC’s inspections<strong>and</strong> other performance measures make clear that delivery needs to improveto match the <strong>Trust</strong>’s aspirations.35. Ensure that clear guidance outlining the expectationsof all staff is produced <strong>and</strong> enforced so that theprescribing <strong>and</strong> dispensing of ‘to take away’ medication ismanaged effectively <strong>and</strong> patient discharges are notdelayed. The trust needs to ensure that it monitorsadherence with policy, guidance <strong>and</strong> audit <strong>and</strong> takes anyappropriate action to support staff to deliver a highquality service.Part metThe <strong>Trust</strong> has suitably robust guidance <strong>and</strong> policies, which is reaffirmed atinduction. Pharmacy is meeting dispensing targets, but better monitoring<strong>and</strong> audit needs to be introduced to ensure that treatment is appropriate<strong>and</strong> supported by suitable information. This has also been linked into theRESET project. The <strong>Trust</strong>’s Visible Leadership programme has included afocus on this area of care, with reports to the Nursing <strong>and</strong> Midwifery <strong>Board</strong><strong>and</strong> Quality <strong>and</strong> Safety Committee.36. Review <strong>and</strong> rationalise the discharge <strong>and</strong> bedmanagement information systems to ensure that the mosteffective <strong>and</strong> accurate system is fully utilised.Part metThe Discharge JONAH tool has been rolled out as per above; this is linked inwith the RESET project. As mentioned, the underpinning measures are inplace but performance is yet to meet expectations.26
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation reportSurgery37. Develop its day case surgery service to ensure thatappropriate patient flow is maintained including effectivepre operative assessment.MetAdmission times are being staggered to reflect the theatre list <strong>and</strong> restrictthe pre-surgery wait to four hours where possible; admission letters nowrefer to appropriate time of arrival <strong>and</strong> likely delays. Revised audit processesare in place to monitor progress.38. Improve st<strong>and</strong>ards of care for obstetric patients whoundergo minor surgical procedures.MetImproved patient satisfaction <strong>and</strong> flow is being monitored; some electivepatients do risk missing treatment due to over-extension of theatre lists, butthis process is under close scrutiny <strong>and</strong> review to make sure the risk of this isminimised <strong>and</strong> patients – where affected – are informed. Emergencyprocedures are prioritised to minimise waiting times <strong>and</strong> avoid harmfuldelays.27
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.6 Cooperation with other providers (outcome 6)39. Continue to engage, <strong>and</strong> develop effective workingrelations, with external providers <strong>and</strong> partners.Part metRegular stakeholder briefings have been introduced <strong>and</strong> the <strong>Trust</strong> has set upa regular programme of meetings at patient representative groups, OSCs,<strong>and</strong> briefing to media. CQC recently attended a stakeholder meeting at the<strong>Trust</strong> <strong>and</strong> feedback from local authority partners <strong>and</strong> the Improving PatientExperience Group was that communications with stakeholders hadsignificantly improved.40. Work with partners to ensure adequate provision ofspecialist rehabilitation services.MetDischarge partnership boards are held on a bi-weekly basis to discusscomplex discharges <strong>and</strong> the relationship between all relevant organisations.Access initiative meetings are held with <strong>Barking</strong> <strong>and</strong> Dagenham, <strong>Redbridge</strong><strong>and</strong> <strong>Havering</strong>. All site managers across acute <strong>and</strong> community services use asingle electronic bed system, which is helping discharges. A community bedreview is underway in line with the Health for NEL programme.41. Work with social care partners to develop robustworking practices to ensure appropriate admission <strong>and</strong>discharge practices.Part metA programme director is working at the <strong>Trust</strong> with funding from the Clusterto liaise between the acute <strong>Trust</strong> <strong>and</strong> borough <strong>and</strong> community services. Thispost will currently run until October <strong>2012</strong>. There is now a central point forescalation <strong>and</strong> consideration is being given to allocating a budge to theprogramme director to allow them to make spot purchases to resolvecomplex discharge problems. Work is underway to streamline processesacross all boroughs to access community services. Gaps in acute <strong>Trust</strong>resources are being identified to improve discharge to community services;early data indicates reduced length of stay.28
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.7 Safeguarding people from abuse (outcome 7)42. Complete the recruitment of senior staff intosafeguarding roles.MetStaff have been appointed to fill the relevant posts for safeguarding adults<strong>and</strong> safeguarding children.43. Ensure that all staff are able to access <strong>and</strong> receive theappropriate level of safeguarding adults <strong>and</strong> safeguardingchildren training.MetA safeguarding training strategy is in place with data on staff trainedcollected <strong>and</strong> reviewed centrally.44. Continue to develop its joint working practice withexternal partners.MetThe director <strong>and</strong> deputy director of nursing now attend a range of externalsafeguarding meetings; external stakeholders sit on the <strong>Trust</strong>’s ownsafeguarding meetings, chaired by the Director of Nursing. Named nursesnow sit on external sub-committees as necessary.29
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.8 Cleanliness <strong>and</strong> infection control (outcome 8)45. Ensure that all equipment <strong>and</strong> disposable productsare stored appropriately.Part metWard managers have completed risk assessments of equipment management<strong>and</strong> storage facilities. A new <strong>Trust</strong> environment / equipment disposal policyis in place. Weekly walkabouts with facilities <strong>and</strong> estates have beenimplemented <strong>and</strong> an action log is in place.46. Ensure that all public toilets are kept clean especiallyin areas of high usage.MetA site review of all public toilets has taken place <strong>and</strong> cleaning schedules havebeen reviewed in terms of frequency <strong>and</strong> content to ensure compliance withthe National St<strong>and</strong>ards of Cleanliness 2007 / PEAT st<strong>and</strong>ard. A rapidresponse team is in place for ad-hoc cleaning. Audits are in place, spotchecks by senior executives have been introduced, <strong>and</strong> patient <strong>and</strong> publicfeedback is monitored.47. Ensure that staff are not posing an increased risk topatients from cross infection. The trust should take anynecessary steps to ensure that staff can store personalproperty as necessary.Part metThe staff uniform <strong>and</strong> dress code policy is being reviewed to ensurest<strong>and</strong>ards are understood <strong>and</strong> remedial actions are available. An infectioncontrol annual plan is in place <strong>and</strong> is reported against to Infection ControlCommittee every other month.30
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.9 Management of medicines (outcome 9)48. Reinforce its policy on medication prescribing,dispensing <strong>and</strong> administration, ensuring that all staff areaware of their roles <strong>and</strong> responsibilities.Part metA briefing for clinical staff explaining the importance of this policy <strong>and</strong>setting out accountabilities for prescribing <strong>and</strong> administration has beenprepared; this is due to be rolled out shortly. A Policy Ratification Group hasbeen set up to ensure policies are corporately signed off, published on theintranet, with summaries added to the Link to raise awareness of changes<strong>and</strong> expectations around compliance. Trends <strong>and</strong> issues relating toprescribing <strong>and</strong> medicines are reported in the Link, with a bimonthlyprescribing newsletter in place to ensure a strong focus on medicines safety.An ongoing audit programme has looked at omitted drugs in the MAU,pharmacist errors, <strong>and</strong> is looking at a range of other relevant issues.49. Ensure that the results of learning from medicationerrors are widely publicised across all services in theorganisation.Part metSafe Medicines Practice Group in place <strong>and</strong> produces a summary of incidentthemes <strong>and</strong> serious incidents to be used in directorate meetings. Pharmacists<strong>and</strong> wards receive monthly reports on medicines <strong>and</strong> prescribing. Errortrends are fed back to relevant directorates <strong>and</strong> are published on theintranet.31
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.10 Safety <strong>and</strong> suitability of premises (outcome 10)50. Review the directional signage at Queen’s Hospital.The trust should ensure that it seeks the input of patients,relatives, visitors <strong>and</strong> staff, to ensure that any new signagemeets the needs of its populations.Part metWorking group involving patients, non-execs <strong>and</strong> staff set up in December2011 to set signage st<strong>and</strong>ards; main signage reviewed with specialist input<strong>and</strong> new signs commissioned to arrive in June <strong>2012</strong>. Leaflet <strong>and</strong> map underreview to ensure signage is in context of better overall patient information.51. Review the emergency department paediatricfacilities at Queen’s Hospital in line with the st<strong>and</strong>ardsoutlined in Services for children in EmergencyDepartment’s document <strong>and</strong> then develop an appropriatestrategy involving both the emergency <strong>and</strong> paediatricdepartments.Part metPaediatric waiting areas reviewed <strong>and</strong> funding agreed to improveobservation of sick children; project group set up to implement Health forNEL redesign of paediatric services.52. Finalise <strong>and</strong> implement plans to improve x-rayfacilities <strong>and</strong> ensure that patients waiting for x-rays in theemergency department are appropriately cared for.Part metReview of x-ray services including department layout linked to Health forNEL programme; project group set up with dedicated project managementsupport. Current process of caring for patients in waiting area addressed viaa short-term solution using a mobile x-ray device to limit patient waitingtimes.53. Ensure that appropriate waiting facilities are availablefor patients <strong>and</strong> relatives in the urgent care centre.Part metAs above, these waiting facilities are being reviewed as part of the Health forNEL programme.32
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report54. Explore options <strong>and</strong> take action to improve access tonatural light <strong>and</strong> ventilation in all clinical areas thatcurrently do not have windows at Queen’s Hospital.MetNatural light bulb pilot is underway to address areas where natural light isnot accessible. All patient-access areas where neither natural light norventilation is available are being identified. All reviews of capitalimprovement now include consideration of the environment in which care isdelivered, <strong>and</strong> any opportunity to provide access to natural light <strong>and</strong>ventilation will be taken.55. Review <strong>and</strong> take any necessary action in all inpatientareas to ensure that there are clear lines of sight so thatpatients can be observed at all times.Not metThe ‘hourly staffing of wards’ element of the Safer Nursing Care Tool <strong>and</strong>other tools are being used to try to ensure there is suitable observation ofpatients, although concerns about staffing levels suggest there is room forimprovement.56. Develop appropriate facilities to ensure the day casesurgical patients are cared for in appropriate environmentsat Queen’s Hospital.Part metThe use of overnight recovery has been reviewed <strong>and</strong> works are underway toimprove facilities subject to funding. There is a plan in place to develop a23-hour facility in the day surgery unit <strong>and</strong> allow space in Recovery to beused as a ‘day of surgery’ admissions area, but these are pending theoutcomes of the bed-modelling work stream.33
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.11 Safety, availability <strong>and</strong> suitability of equipment(outcome 11)57. Review the availability of medical devices in clinicalareas to ensure that appropriate levels of equipment areavailable for the acuity of patients that it receives atQueen’s Hospital. Further revalidation of the review needsto take place following any changes to service provision.MetA matron-led audit of equipment took place in November 2011. This showedareas where equipment was above the current register <strong>and</strong> highlighted someshortfalls. The latter have been picked up via business cases (expenditure of£240k was approved for immediate procurement in March <strong>2012</strong>) <strong>and</strong> shortfallsare routinely considered at the Medical Devices Committee. A manual equipmentloan process is in place to keep track of equipment (an electronic system wasconsidered but was too expensive). This is supported by a colour-coding systemwhich was introduced via a successful pilot. The existence of four separate contractsfor therapy equipment (<strong>Trust</strong> <strong>and</strong> three local authorities) means accessibilityissues will remain until contract renegotiations can take place. There are nobarriers to clinical areas obtaining stationery at any time it is needed. The MedicalDevices Policy has been reviewed, signed off <strong>and</strong> published; a new escalationprocess is in place to address faulty equipment, including matrons / managersaddressing governance issues with staff where reporting has not taken place.58. Ensure that systems are in place in all clinical areas sothat sufficient disposable equipment is available.MetA medical devices audit has been completed <strong>and</strong> business planning forequipment for <strong>2012</strong>-13 reflected its findings. A process for monitoring,ordering <strong>and</strong> administering disposable equipment is well-established <strong>and</strong> subjectto audit; this is supported by the colour-coding <strong>and</strong> loan equipment protocol.59. Develop as part of its cultural change programmepeople’s sense of responsibility to take positive action toensure that clinical areas are suitably equipped to providesafe patient care.Not metThis will be audited by monitoring complaints on availability of equipment<strong>and</strong> regular equipment audits; a business case may be considered for adedicated medical devices coordinator / trainer if the need is firmlyidentified. CQC’s inspections suggest this remains a serious issue that needsto be addressed.34
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.12 Staffing (outcome 13)60. Continue to review its human resource informationsystems <strong>and</strong> ensure that accurate data is available for theentire organisation, so that a clear <strong>and</strong> comprehensiveunderst<strong>and</strong>ing of vacancies can be established.Not metThe <strong>Trust</strong> has introduced a phased programme to consolidate establishmentdata against the electronic staff record, including cleansing the record ofposts that are no longer in use, <strong>and</strong> with finance support. There have beenchallenges in aligning the HR ledger data with the electronic record. Furtherwork is needed <strong>and</strong> there is, as yet, no formal process in place or agreed formanaging establishment control. The move to electronic staff change /termination forms has been difficult to implement, <strong>and</strong> there has been adelay in getting fully accurate reporting on vacancies <strong>and</strong> establishment.61. Continue to review its workforce strategy to ensurethat it meets the needs of the organisation <strong>and</strong> reflectsthe reality of service delivery.Part metA review of the Workforce Strategy has been completed <strong>and</strong> is now beingtested via the staff engagement group.62. Undertake systematic skill mix <strong>and</strong> staffing needsanalysis to ensure that they have the right staff with theright skills at the right locations <strong>and</strong> that trust is receivingvalue for money.Part metSkills for Health are supporting the <strong>Trust</strong> in this, funded via NHS LondonFinancial Support. Pilot work in the Emergency <strong>and</strong> Maternity Departmentsis underway. Future phases are heavily dependent on the success of the pilotanalysis <strong>and</strong> capacity to roll its findings out across the <strong>Trust</strong> <strong>and</strong> this will onlybe able to be assessed in the longer term. CQC compliance activity continuesto suggest that the <strong>Trust</strong> faces challenges in terms of building a sustainableworkforce with the right skills mix.35
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report63. Continue to recruit appropriate permanent staff toensure that it reduces its reliance on agency <strong>and</strong> locumstaff improving the quality of care, <strong>and</strong> have in placeeffective retention strategies.Part metAn accelerated recruitment project <strong>and</strong> reduced use of agency staff havebeen put in place, with recruitment needs assessed on a monthly basis. Exitinterviews are now in place as part of KPIs <strong>and</strong> are reviewed by Directors.The <strong>Trust</strong> has introduced suitable procedures here, but CQC complianceactivity has identified ongoing challenges around locum use, particularlyin A&E.64. Develop <strong>and</strong> improve the human resources supportfor the divisions so that managers can take effectiveaction against staff where there are performance concerns.MetMediation training has been delivered to support managers; performancemanagement policies <strong>and</strong> processes are in place for <strong>2012</strong>-13 to supportmanagers in taking early action against poor performance. Revised policieshave been approved by staff <strong>and</strong> HR performance is reviewed at directoratelevel on a monthly basis.65. Explore <strong>and</strong> develop strategies for delivering serviceswith different staff groups so that reliance on difficult torecruit staff groups is reduced.MetJob descriptions are being reviewed to ensure they reflect the need forflexibility; provisions for this within current contracts are being reviewed. Aflexible working policy has been agreed with the staff <strong>and</strong> take up is beingmonitored as part of recruitment KPIs.36
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report66. Support a skills escalation programme in theemergency department that seeks to develop nurses whohave already successfully completed an emergency nursepractitioner or advanced clinical practitioner course <strong>and</strong>reduce reliance on them undertaking traditional nursingduties due to shortages of staff.Part metA review of the A&E workforce has been completed <strong>and</strong> the unit has beenbenchmarked against other comparable trusts. A review of the skills mix,current roles, <strong>and</strong> supporting roles has been undertaken <strong>and</strong> budgetsreviewed in light of this. Current staff are taking part in an ongoing trainingprogramme to ensure staff update <strong>and</strong> refresh their skills. CQC’s complianceactivity has identified ongoing staffing challenges in A&E <strong>and</strong> the longertermimpact of this review work will need to be assessed at some point inthe future.67. Ensure that its whistleblowing systems <strong>and</strong> processesallow staff a route to raise concerns early so that quickaction can be taken <strong>and</strong> staff feel empowered to raiseconcerns.Part metThe <strong>Trust</strong>’s whistleblowing policy has been revised <strong>and</strong> communicated tostaff through Team Brief, the Link <strong>and</strong> the intranet. Staff feedback on theeffectiveness of the policy is now part of the staff engagement strategy <strong>and</strong>new starters will be audited after six months to see if they are aware of it.Delivery of this recommendation is contingent on cultural changeembedding itself across the <strong>Trust</strong> (although it should be noted that CQC hasusually found staff open <strong>and</strong> willing to talk frankly about challenges duringinspections, whether in confidence or openly).37
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.13 Supporting workers (outcome 14)68. Continue to develop <strong>and</strong> deliver training for staff tosupport the development of quality services, seekingalternative solutions where staff have difficulty accessingtraining due to staffing constraints.Part metAn annual training needs analysis is carried out <strong>and</strong> new m<strong>and</strong>atory <strong>and</strong>statutory training programmes are in place. Staff education is supported byspecialist trainers <strong>and</strong> compliance is reported to the <strong>Trust</strong>’s Education <strong>Board</strong>.Recording of training attendance has been improved <strong>and</strong> should be reportedto line managers. Better reporting <strong>and</strong> benchmarking is needed to considerthis met.69. Ensure that appropriate supervision is provided tomedical staff <strong>and</strong> that more junior medical are not leftwithout appropriate support, especially at weekends <strong>and</strong>at night.MetThe <strong>Trust</strong>’s supervision policy has been reviewed by a working party (part ofthe Post-Graduate Medical Education Committee) to include KPIs <strong>and</strong>introduce accountability to this area. Benchmarking <strong>and</strong> audit will ensurethis is sustainable.38
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.14 Assessing <strong>and</strong> monitoring the quality of service(outcome 16)70. Ensure that it has adequate systems of governance topromote high quality care for patients <strong>and</strong> to deal withconcerns about performance in an effective <strong>and</strong> timelymanner.Part metClinical <strong>and</strong> committee structures have been reviewed <strong>and</strong> a new ClinicalGovernance Structure has recently been considered by the <strong>Trust</strong>’s <strong>Board</strong>.Exp<strong>and</strong>ed central data collection for the Quality <strong>and</strong> Safety Committee hasbeen proposed. A central monitoring <strong>and</strong> evidence database has beenintroduced for Serious Incidents, with <strong>Trust</strong>-wide audits being introduced<strong>and</strong> KPIs introduced for reporting <strong>and</strong> completion of investigations. Aweb-based incident reporting system is being introduced across the <strong>Trust</strong>after a pilot in maternity.71. Develop a system of governance that offers itaccurate <strong>and</strong> real time information that translates into aneffective assurance process.Met72. Carry out a comprehensive review of all corporate <strong>and</strong>clinical governance systems across the organisation toensure that effective <strong>and</strong> streamlined systems <strong>and</strong>reporting structures are in place to provide robustassurance to the board.Part metClinical <strong>and</strong> committee structures have been reviewed <strong>and</strong> a new ClinicalGovernance Structure has recently been considered by the <strong>Trust</strong>’s <strong>Board</strong>.A complete review of <strong>Trust</strong> corporate committees has been completed <strong>and</strong>was recently put to the <strong>Trust</strong> <strong>Board</strong>. A complete review of maternity clinicalgovernance was completed by October 2011 to ensure full integration withthe <strong>Trust</strong>’s main governance structures. The review also led to Divisionalmanagers taking on responsibility for alerting clinical governance teams toall external quality <strong>and</strong> safety recommendations (reinforced throughstringent audit <strong>and</strong> reporting), with regular reporting between HR <strong>and</strong>Clinical Governance to ensure joint management of patient safety issues.39
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report73. Ensure that it has systems in place that allow effectivesharing <strong>and</strong> learning across the whole organisation.Part metExisting guidance on learning from serious incidents has been reviewed <strong>and</strong>KPIs for implementation have been introduced. A bi-monthly ‘LessonsLearned’ group meets to generate shared learning. This includes using thecontent of Ombudsman action plans to ensure learning points areappropriately extracted <strong>and</strong> shared. A rolling programme of articles in theLink is supporting learning. Directorate <strong>Board</strong>s now review Serious Incidentreports <strong>and</strong> action plans to ensure timely implementation. Clinical Directorsare sent details of each relevant Serious Incident <strong>and</strong> these are agenda itemsfor directorate clinical governance meetings until they are responded to in asuitable way. This recommendation will only be fully met when success canbe demonstrated over time. CQC <strong>and</strong> other stakeholders not only expect tosee evidence that Serious Incidents are being dealt with internally, but alsoto see commissioners <strong>and</strong> other external organisations being informed whenrelevant.74. Ensure that the incident reporting system for thewhole trust is operating effectively <strong>and</strong> all staff arelearning from incidents rather than simply reportingincidents.Part metAs noted above, a web-based incident reporting system is being introducedacross the <strong>Trust</strong> after a pilot in maternity. If the proposed clinical governancestructure is introduced as planned, directorate boards will take onresponsibility for regular reviews of learning from incidents. Learning fromincidents is now integrated into the ward staff meeting structure, <strong>and</strong> betterstructures have been introduced to ensure learning is shared between staffacross divisions. Again, this will need to be demonstrated over time.75. Ensure that it has appropriate levels of staff in placeto allow its governance systems to function effectively <strong>and</strong>that these staff are embedding appropriate systems inclinical services.Part metFollowing the review of governance, suitable staff have been identified toensure its recommendations are properly implemented. As above, proof ofsuccess will be seen through delivery.40
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.15 Complaints (outcome 17)76. Continue to develop <strong>and</strong> improve its complaintsh<strong>and</strong>ling systems to ensure that complaints are respondedto fully <strong>and</strong> in a timely manner.Part metA review of outst<strong>and</strong>ing Ombudsman complaints has taken place; adedicated manager has been appointed to follow up compliance with actionplans or to report non-compliance to the Director of Nursing. Complaintnumbers <strong>and</strong> trends are reported to the Quality <strong>and</strong> Safety Committee. PALSprocesses have been reviewed to try to address patient concerns at an earlierstage. CQC is aware that the <strong>Trust</strong> has seen a significant increase incomplaint numbers since the investigation was published last year; as aresult, while the underpinning systems have been improved, they arestruggling to cope with an unprecedented surge in numbers.77. Develop <strong>and</strong> support staff to ensure that opentransparent investigations take place, that complainantsare involved as necessary <strong>and</strong> that culturally complaintsare seen as opportunities to learn <strong>and</strong> improve the qualityof care.Part metNHS London has supported the <strong>Trust</strong> to undertake a root cause analysistraining campaign for senior management to ensure the importance of timelyinvestigation of complaints is fully understood. A report of trends <strong>and</strong>themes aggregated across the <strong>Trust</strong> is reported every other month, includingidentification of trends <strong>and</strong> hotspots.78. Ensure that any staff identified in a complaint areinvolved in resolving the complaint <strong>and</strong> the resultinglearning, but where there is a complaint about anindividual there is appropriate separation of theinvestigation from the individual.Not metA revised policy has been drafted <strong>and</strong> is awaiting senior managementapproval; it is currently available to staff but will only be considered on itsway to being met when it is implemented <strong>and</strong> progress audited.41
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report79. Develop its reporting mechanisms to ensure that theboard are fully informed of all complaints, that detailedtrend analysis takes place <strong>and</strong> that the board can assureitself that learning is taking place, <strong>and</strong> repetition ofthemes is reduced.Part metThe <strong>Trust</strong> Executive Committee <strong>and</strong> <strong>Board</strong> now receive a monthly complaintsanalysis; reporting is discussed at the bimonthly Quality <strong>and</strong> SafetyCommittee. The Patient Experience report to the Quality <strong>and</strong> SafetyCommittee includes a full analysis by directorate <strong>and</strong> highlights key issues.Reporting began in April <strong>2012</strong>42
<strong>Barking</strong>, <strong>Havering</strong> <strong>and</strong> <strong>Redbridge</strong> University Hospitals NHS <strong>Trust</strong> - Update on investigation report4.16 Records (outcome 21)80. Improve its systems for records management toensure that notes can be retrieved effectively <strong>and</strong>expediently, <strong>and</strong> reduce the risks associated with multiplesets of temporary notes <strong>and</strong> poor data h<strong>and</strong>ling.Part metThe <strong>Trust</strong>’s Medical Records Committee has been re-established with newTerms of Reference; training levels for healthcare professionals are discussedat this Committee on a regular basis. Weekend transport for transfer of noteshas been reintroduced <strong>and</strong> a nursing documentation booklet has beenpiloted across several wards <strong>and</strong> will be fully implemented by the autumn.81. Develop integrated patient administration <strong>and</strong>information systems to ensure that, where ever a patientis being treated within the trust, their full healthcarehistory can be accessed by all staff.Part metA procurement process is underway to introduce an effective system toenable access to patient histories. Funding challenges have slowedintroducing of a full electronic patient record.43
EXECUTIVE SUMMARYTITLE:BOARD/GROUP/COMMITTEE:Quality <strong>and</strong> Patient St<strong>and</strong>ards PerformanceReport – May <strong>2012</strong><strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:The Quality <strong>and</strong> Patient St<strong>and</strong>ards Performance Reportprovides an analysis of performance against trust-wide<strong>and</strong> national targets for the following domains:• Patient Safety <strong>and</strong> Quality• Performance• Workforce• Productivity• FinanceThe following areas where year to date (YTD)performance is of concern are discussed within the report:□ PEQ……….…...……. □ STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT ………….……..….□ CLINICAL GOVERNANCE …………..………….....……□ CHARITABLE FUNDS ………………………………...… TRUST BOARD – June <strong>2012</strong>□ REMUNERATION ………………………………….…...□ OTHER …………………………..……. (please specify)• % of SI’s reported within 48 hours -• MRSA Bacteraemias• Clostridium Difficile• MRSA Screening – Emergency• % Complaints Responded to Within 30 days.• Pressure Ulcers• Elective <strong>and</strong> Non-elective Re-admissions
2. DECISION REQUIRED: CATEGORY:The <strong>Trust</strong> <strong>Board</strong> is asked to note the content of the report<strong>and</strong> support the actions to bring the performance back inline with trajectory/target. NATIONAL TARGET □ CNST□ CQC REGISTRATION □ HEALTH & SAFETY□ ASSURANCE FRAMEWORK CQUIN/TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE ……………………………....□ OTHER …………………….. (please specify)AUTHOR: Claire Burns, Head of Planning, Commissioning<strong>and</strong> InformationPRESENTER: Neill Moloney, Director of DeliveryDATE: June <strong>2012</strong>3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:Not applicable.4. DELIVERABLESThe delivery of the <strong>Trust</strong> wide objectives.5. KEY PERFORMANCE INDICATORSPlease see attached <strong>Trust</strong> Performance Dashboard.AGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
Performance ReportMay <strong>2012</strong>Performance Indicators - Exception Report1. IntroductionThe performance report has been revised for <strong>2012</strong>/13. The dashboard now covers the followingareas• Patient Safety <strong>and</strong> Quality• Performance• Workforce• Productivity• FinanceThere are a number of new indicators included for <strong>2012</strong>/13. This report provides the <strong>Board</strong> with anoverview of mitigating actions to be taken by Business Units to improve performance to ensureperformance meets the target, ld. Finance <strong>and</strong> Human Resources performance are subject toseparate reports to the <strong>Trust</strong> <strong>Board</strong>. Where either the staff appraisal or basic life support trainingdoes not achieve the performance target a commentary has been included in the exception report.2. Patient Safety <strong>and</strong> Quality% of SI’s reported within 48 hours - This is a new indicator for <strong>2012</strong>/13. The target has been set inline with the CQUIN which has a quarterly trajectory.There was an improvement in the % of SI’sreported within 48 hours during Mayachieving a performance of 29% over twomonths. The SI CQUIN goals have beenissued to Clinical Directors who have beenrequested to ensure all services underst<strong>and</strong>the importance of urgent SI reporting.Clinical Governance is closely monitoringcompliance <strong>and</strong> raises with services <strong>and</strong> theappropriate Clinical Director any nonconformanceMRSA BacteraemiasThere was 1 case of MRSA bacteraemia during May. The cause was thought to be urinary tractinfection associated with urinary catheterisation. A root cause analysis meeting has been held <strong>and</strong>some failings in compliance with catheterisation policy have been identified. There were also somefailings in medicines management – antibiotics not given in a timely manner – <strong>and</strong> issues regardingurological management were raised. An action plan has been prepared <strong>and</strong> a response is due by theend of June. The project to introduce Aseptic Non-Touch Technique (ANTT) across the trust isprogressing well <strong>and</strong> implementation will commence in <strong>July</strong>. This project will address many of theissues associated with previous causes of MRSA bacteraemia such as infection associated withwounds <strong>and</strong> intravascular lines.Clostridium DifficileThere were 7 cases of infection during May, 4 at Queens <strong>and</strong> 3 at King George, one of which was acase of relapsing infection, not a new case, but is reportable according to the criteria. All cases havebeen reviewed <strong>and</strong> there is no obvious connection between them. Individual review of the patientscare by ward staff showed between 95 <strong>and</strong> 100% compliance with policy – a considerablePage 1 of 10
improvement on previous findings. Therefore the reason for the increase remains obscure. Additionalhigh level cleaning of A&E <strong>and</strong> admissions wards has been carried out as the potential for spread ofinfection among newly admitted patients may be higher than on other wardsMRSA Screening – Elective The <strong>2012</strong>/13 target forMRSA screening has been agreed at 85% forelective screening The current performance for thescreening of elective admissions MRSA screeninghas remained static at 78% but with non-electivescreening increasing from 69% in April to 74% inMay. The completion of waiting list clinical coding isaffecting elective performance. If coding is nottimely or complete the number of excluded recordsis lower than could be. This issue has beendiscussed with the Clinical Coding Department whoare working on increasing coding of the waiting list.MRSA Screening – Emergency The <strong>2012</strong>/13 targetsfor MRSA screening has been agreed at 95% for nonelectivescreening. The majority of the emergencypatients enter via the CAU where the screening isdone however, where we have direct access to thewards the matrons are aware of the MRSA PTL <strong>and</strong>this has been flagged to the ward staff. The responseto this will be reviewed at the weekly medical matronsmeeting <strong>and</strong> an action plan will be required to becompleted for those areas that are not achieving.% Complaints Responded to Within 30 days. This measure will be changed to % Complaintsresponded to within the agreed timeframe, in line with the national st<strong>and</strong>ard. As of 18.6.12, 28 opencomplaints were more than 3 months old. Two remain from 2011, <strong>and</strong> are expected to be dealt withby the time of the <strong>Board</strong> meeting, when a further update will be available. Overall, this is a 50%reduction on the number open at the beginning of January, <strong>and</strong> a 75% reduction on the number openfor more than three months. Weekly performance meetings remain in place with the directorates tosustain the performance going forwards <strong>and</strong> clear the remaining backlog of older complaints.Pressure Ulcers There were 2 grade 4 pressure ulcers reported in May, although both of these wereidentified as a result of patient complaints <strong>and</strong> related to care given some time previously; one fromFebruary <strong>2012</strong> <strong>and</strong> the second one from May 2011. There have been no new hospital acquiredgrade 4 pressure ulcers in April or May, <strong>and</strong> it is now over 110 days since the last instance within the<strong>Trust</strong>. This is a significant improvement on the position last year. Grade 3 pressure ulcers havecontinued to be reported at a consistent rate for the last 3 months, although there has been a slightreduction in those numbers over the last year. The <strong>Trust</strong>-wide action plan for reducing pressureulcers continues to be implemented, with patients being risk assessed on admission <strong>and</strong> then at leastweekly. Referrals to the tissue viability have team have significantly increased as a result of the workto highlight the need for early intervention. The team are now facing a challenge to ensure that everyreferral is seen within 24 hours.Page 2 of 10Elective <strong>and</strong> Non-elective Re-admissions
not yet been set. However the performance is currently not improving. With elective readmissionsrising from 2.97% in April to 3.4% in May <strong>and</strong> non-elective admissions rising from 12.75% to 13.9%in the same periodThe RESET work streams do not directly address readmission rates but with the focus on earlier <strong>and</strong>safer discharge some improvement is to be expected over the coming weeks.There is also a programme of work being led by Alison Browne <strong>and</strong> Caroline Moore to try to integratemore closely the Community Discharge <strong>and</strong> Support teams with BHRUT Discharge team to supportmore effective <strong>and</strong> sustainable discharge.The Integrated Case Management work is being continued by ONEL in partnership with the <strong>Trust</strong>.The <strong>Trust</strong> is also working on a project inconjunction with NELFT to implement aCommunity Treatment team to‘gatekeep’ admissions <strong>and</strong>readmissions for the frail elderly. Thiswork is in the early stages of discussionbut there is strong commitment by bothproviders to implement this team.Patient Experience the first measurefor this indicator is to achieve 50% of discharged patients completing a survey. To ensure the futuresuccess of real time patient surveys, this initiative needs to be owned <strong>and</strong> driven forward by theBusiness Units. To this end the following actions have been instigated :• Active encouragement by Matrons to ensure that all ward areas achieve a minimum of50% of discharged patients undertaking a real time survey.• Survey results to be discussed at Business Unit meetings• Real time patient survey results to be incorporated into Business Unit reporting• All areas which have h<strong>and</strong> held devices will be able to access their real time surveysonline via a unique link <strong>and</strong> passcodeThe questionnaires used in the Real Time Surveys are being reconfigured <strong>and</strong> will include thequestion “How likely is it that you would recommend this service to friends <strong>and</strong> family”? Thequestionnaires together with 10 additional kiosks will be implemented across the <strong>Trust</strong> by late June<strong>2012</strong>Same Sex Breaches There were 21 single sex breaches for the month of May <strong>2012</strong>.These occurredwithin the High Dependency Unit (17), <strong>and</strong> Intensive Therapy Unit (3) at Queen’s Hospital. At KingGeorge Hospital, a single sex breach occurred in the High Dependency Unit (1). This is animprovement from the April when there were 30 single sex breaches. Following a discussion withinthe service it has been agreed that a modified root cause analysis will be undertaken for all breachesof this st<strong>and</strong>ard. The outcome will be circulated for discussion <strong>and</strong> learning across the organisation.All of the breaches occurred due to delays in the transfer out of patients who had been ‘steppeddown’ to general care. This was due to constraints on the availability of suitable beds for step downPage 3 of 10
Page 4 of 10due to patient flow delays across theorganisation. The Rapid End to EndSustainable Emergency Transformation(RESET) programme is expected to resolvethe issue of the delay in transferring ‘steppeddown’ patients from CCU, ITU <strong>and</strong> HDU tothe general wards at Queens.
3. PerformanceCancer Targets Although compliance with the CWT targets was achieved for the full yearending 31st March <strong>2012</strong>, the 62-day performance fell in February <strong>and</strong> March <strong>2012</strong>; this noncompliantperformance has continued into the new financial year. The main issue affectingthe 2 week wait target is that of capacity; there has been lost capacity due to sickness indermatology. There have also been an increased number of patients who are unavailablefor their appointment dates. In the main, the breaches have been caused by admin delays,followed by patient choice, then capacity issues. This reflects the fact that escalation hasnot been taking place as it should. The escalation policy has been re-circulated <strong>and</strong> thefocus of the weekly PTL meetings is to now identify any delayed escalation, with plans beingput in place to avoid the breach.The table below shows the breaches in April broken down to into the main reasons:PatientChoice Medical Capacity AdminComplexPathway TRUS/MRITotal 4.5 3 3.5 6 2 1.5 20.5Percentage 22% 15% 17% 29% 10% 7%In order to reduce the numbers of breaches, <strong>and</strong> bring the 2 week wait, BOS <strong>and</strong> 62-dayscreening performance back to target the following actions have been put into place:• Review format of Weekly Friday PTL meeting to focus on all targets (e.g. 2ww) <strong>and</strong>discuss service improvement as well as reviewing individual patients <strong>and</strong> escalatingdelays that haven’t been actioned;• Escalation policy has been updated <strong>and</strong> re-circulated;• Lead Clinician for Cancer to attend the MDT Meetings with the Lead Nurse for Cancer toensure further engagement from the Lead Clinicians;• The H&N MDT has met on a weekly basis for the past few weeks to review theirpathway. These meetings continue.• MDT structure has been reviewed to provide support for the MDT Coordinators duringtimes of leave or sickness.Emergency Department (ED)The <strong>Trust</strong> maximum wait target is measured on all attendances atA&E <strong>and</strong> UCC facilities on both <strong>Trust</strong> sites. The performance against this st<strong>and</strong>ard is shown below<strong>and</strong> has improved in May in line with the agreed trajectory. Local specialty referral Key PerformanceIndicators (KPIs) are now in place as a measure of the <strong>Trust</strong>’s own internal professional st<strong>and</strong>ards.Measuring against these KPIs has now commenced <strong>and</strong> although performance is currently poorthere are a number of initiatives withinED <strong>and</strong> across specialties to addressthis going forward. These include:• extended rapidassessment <strong>and</strong> treatmentwithin ED to all patients• dedicated specialtyresponse to the ED insome areas• receiving rooms• assessment unitsPage 5 of 10
• improved escalation processesThe number of ambulance black breaches has significantly improved in May which is as adirect result of the extended rapid assessment <strong>and</strong> treatment within ED <strong>and</strong> the revised bedmanagement system whereby there is a bed manager responsible for managing both the‘front’ <strong>and</strong> ‘back’ door admissions. These improvements are being managed through theMcKinsey RESET programme, details of which are included under the Emergency CareRESET update.Page 6 of 10
4. WorkforceBasic Life Support Training (BLS) The latest resuscitation training compliance report, coveringthe period 1 st June 2011 – 31 st May <strong>2012</strong> reports <strong>Trust</strong> compliance at 77.86% an increase of1.57% on the previous report. Compliance reporting continues which identifies staff, at all levels,who still require resuscitation training. Attendance at Adult In-Hospital Life Support trainingsessions is improving but there are still a relatively large number of unfilled places, or nonattendanceon a number of courses as demonstrated by the low increase in overall compliance. Inorder to improve compliance rates the resuscitation service has offered targeted training to severalstaff groups where service dem<strong>and</strong>s makes releasing staff to attend advertised training sessionsdifficult. These session have been scheduled over the next few weeks <strong>and</strong> months,Page 7 of 10
5. ProductivityLength of Stay (LoS) There has been deterioration in LoS across the board with theexception of Elective (including 0 days). This was due to Bank Holiday leading to areduction in discharges Some of this may be due to the opening of Japonica ward at KGHfor the complex discharges which has introduced an additional step in these patientspathway which inherently increases their LoSThere is a new stream of work which focuses on weekend discharges – the additional support put infor the recent Bank Holiday weekends has proven to expedite discharge - a dedicated dischargeteam will be established in the short term while a proposal for Consultant 7 day working for medicalspecialties is worked through. A full update of the RESET work streams addressing LoS is givenunder the Emergency Care report.Delayed Transfers of Care has increased by 1% which will be a contributory factor in the observedincrease in length of stay. On reviewing the Jonah data, the number of patients in delay has increaseas well as the LoS for these patients..Work is now focusing on this with theward sisters <strong>and</strong> matrons to ensurethat while we have Japonica openevery effort is made to expedite timelydischarge.Performance for May was 4.99%against April’s performance of 3.9%which is very disappointing given theeffort that has been made to reduce thewait for community beds.The main cause for DTOC related tothe Health Needs Assessment process,Page 8 of 10
with most of the delays occurring on Japonica ward at KGH.The reasons for delays <strong>and</strong> their mitigation are:• Awaiting completion of the Health needs assessment by hospital staff – patientshave been transferred to Japonica with incomplete HNA or inadequate HNA whichhave to be repeated. This is lengthy process <strong>and</strong> the ward staff do not know thepatients. Additional complex discharge team resource has been assigned to clearthe backlog.• The moves to Japonica at KGH were undertaken to create capacity on the Queenssite to improve A&E performance, but this has had an adverse effect on DTOCperformance. RESET project work stream informed.• Delays caused by waiting for Occupational Therapy reports as part of theassessment process due to service capacity issues. Escalated as part of RESETproject• A delay in medical reviews of care after a section 5 has been issued. Escalated aspart of RESET project• Waiting ratification for nursing care funding – there were some delays this month.This has been escalated to the PCTA significant reduction (average was 20 <strong>and</strong> by the end May was 6) in the number of DTOC delaysrelated to waiting for non-acute beds resulted from the following actions which were undertakenduring May:• A single management structure for all community beds across NEL is now in place• A review of the referral <strong>and</strong> admission criteria into rehabilitation beds <strong>and</strong> serviceshas been undertaken• A single referral <strong>and</strong> assessment process for rehabilitation is now in place• A regular review of all in patients is undertaken to identify patients for early dischargeresulting in an increase in capacity, with a reduction in LOS, across all sites forcommunity beds• A reduction in the number of days patients wait for a community bed <strong>and</strong> a reductionin the number of patients waiting.• A reporting template has been agreed with NELFT so that Commissioners maymanage DTOC performance.Stroke rehabilitation processes have been harmonised to ensure that patients have all theirrehabilitation in one site <strong>and</strong> this has resulted in a significant drop in patients waiting for strokerehabilitation.% Patients Discharged Between 6 am <strong>and</strong> 11am -This is a new target this year. General Managers<strong>and</strong> Service Managers are actively supporting ward board rounds each morning to enable them to bemore proactive in managing operational issues which prevent a patient’s timely discharge.Page 9 of 10Outpatient First to Follow-up Ratio TheYTD first to follow up ratio has shown a
small improvement but remains below the performance target rate of 2.13 at 2.27. All outpatientclinic profiles have been reviewed across all specialties <strong>and</strong> changes have been applied to theclinics. As many of the specialties have clinics that are already fully booked <strong>and</strong> in some casesoverbooked, the re-profiling exercise is not expected to result in an improvement to the FFU ratiountil mid year. It was agreed, via the outpatient work stream, that the unregulated practice ofchanging slots within the clinic profile, especially changing new slots to follow ups slots, is to cease.The current list of staff across the <strong>Trust</strong> able to change slots has been reviewed as it was felt misuseof this functionality was taking place <strong>and</strong> affecting the <strong>Trust</strong>’s FFU ratio performance.DNA Rate 1 st Appointment The DNA rate for firstappointments has made progress <strong>and</strong> reached thetarget rate of 9.70%, but it is fairly static on previousmonth’s figures. The texting pilot in four specialitiesgynaecology, rheumatology, urology <strong>and</strong> T&O hasbeen completed. Except for T&O all specialities inthe pilot have shown improvement in DNA rates withmost the favourable impact seen in gynaecology.Funding has been agreed for a <strong>Trust</strong> wide textingreminder service <strong>and</strong> will be phased in over the next6 months.DNA rate for follow up appointments The DNA rate for follow up appointments has reached theperformance target of 10.30% at 9.92%. Inorder to further reduce the level of DNA'sthe <strong>Trust</strong> is looking to move to full partialbooking of follow up attendances. This is asignificant initiative <strong>and</strong> marks a transition toa more pro-active management ofOutpatients <strong>and</strong> promises significant gainsin efficiency <strong>and</strong> patient satisfaction. Apaper detailing the investment required toimplement full partial booking has beenproduced for the Director of Strategy fordiscussion by the <strong>Trust</strong> Executive.Page 10 of 10
April May Target red Trend April May Target red Trend April May Target Red TrendSHMI ‐ quarterly Sept 11 93.9293.92 95.00 = % untreated waiting less than 18 weeks 93.0% 93.7 92% 87% ↑ LOS (Elective) 3.12 3.0 3.1 3.48 ↓% emergency admitted patients review bysenior clinician within 12 hours 95% 96% RTT admitted in 18 weeks 90.7% 90.1 90% 85% ↓ LOS (Non‐Elective) 5.29 5.43 4.454 5.05 ↑% emergency admitted patients review byconsultant within 12 hours 95% 96% RTT non‐admitted in 18 weeks 98.7% 99.5 95% 90% ↑ LOS (Elective‐ excluding 0 LOS) 3.48 3.52 3.5 3.92 ↑Maternal Death Rate per 100000 ( rolling 1245 April 38 46 Aprilm) 32.09 31.09 May39 May ↑ RTT not delivered in all specialties 10 13 0 >20 ↓ LOS (Non‐ Elective‐excluding 0 LOS) 6.58 6.83 5.8 6.53 ↑% Day case rate ‐ All 87.74% 88.57% 80% 75% ↑Serious Untoward IncidentsCancerDTOC 3.90% 4.99% 3.50% 5.00% ↓Number 61 14 18 19 ↑ 2 Wk. % seen all urgent refs & ref for breast** 91.5% 95.70% 93% 88% ↓ admissions on day of surgery 79.1 86.42 85% 80% ↑% reported within 48Hours ‐ quarterly 29%30% ( Q1) 29% ↑ 2 Wk. GP RefTo 1st OP for susp cancer** 91.2% 96% 93% 88% ↓ % patients discharged between 6 am <strong>and</strong> 11 am 9.95% 9.96% 50% ↓MRSA BacteraemiaC Diff InfectionPatient Safety <strong>and</strong> QualityReducing hospital mortalityInfection Control21301 April 00May4 April 5MayPerformanceReferral to Treatment2 Wk GP Ref To 1st OP for breast symptoms** 94.5% 93.80% 93% 88% ↓31 Day 2nd Or Subs Treatment ‐ Surgery** 100.0% 100% 94% 89% =2 April 1May = 31 Day 2nd Or Subs Treatment ‐ Drug 100.0% 95.70% 98% 93%=Enhanced Recovery% patients with an ERP code entered onto the nationaldatabase 95% 95%5 April6 May ↓ 31 Day DTT for all cancers** 100.0% 98% 96% 91% ↑ % planned colorectal having GDFT 80% 80%MRSA Elective Screening 78% 78% 85% 77% = 62 Day RTT From Cancer Screening** 66.7% 90% 85% ↓ % emergency abdominal patients having GDFT 80% 80%MRSA Emergency Screening 69% 74% 85% 77% ↑ 62 Days ‐ treated from referral 80.7% 86% 80% ↓62 Day RTT From Hosp Specialist** 100.0% 85% 80% ↑OutpatientsComplaints62 Days Urgent RTT of all cancers** 80.4% 85% 80% ↑ FFU Ratio 2.61 2.27 2.16 2.2 ↑% complaints responded to in line with60% April 70% 54% Aprilagreement with patients 43% May63% May n/a 31 Day Subs Treatment ‐ Radiotherapy** 98.4% 94% 89% ↓ DNA First 10.45% 9.67% 9.37% 10.41% ↑number of complaints not yet responded toover 3 months old 10 28 25 in May 27 in May ↓ DNA Follow‐Up 10.52% 9.92% 9.33% 10.37% ↑A&E number extra clinics run in month 16 25 ↓79.50% AprilDementiaFour‐Hour Maximum Wait In A&E 83.90% 89.49% 95% 87.49% May% patients aged over 75% having a mental testscore 42%25% (Q1) 24%Percentage of patients referred to speciality team
RapidEnd-to-endSustainableEmergencyTransformation<strong>Trust</strong> <strong>Board</strong> update27 th June <strong>2012</strong>
Headlines on progress▪ Overall <strong>Trust</strong> cluster performance continues to improve– Overall 4 hour breaches have been trending on a positive trajectory. Last week (18 th June – 25 thJune) the <strong>Trust</strong> achieved performance of 93.6%, the highest since October 2011. During the week of4 th June –10 th June the <strong>Trust</strong> achieved 91.9% against a trajectory of 88.3% <strong>and</strong> the previous week(29 th May – 3 rd June) 91.3% against a trajectory of 88.3%– Performance during the week of 11th June – 17th was poor (85.9%) with admissions <strong>and</strong> breachesincreasing significantly▪ Jubilee weekend performance demonstrated that the <strong>Trust</strong> can plan <strong>and</strong> execute. However it hasalso highlighted that planning needs to extend to the days following bank holiday weekends– Breaches spiked in the week after jubilee weekend <strong>and</strong> at the beginning of the following week– Preparation ensured high level of discharges before the jubilee weekend. However subsequentlydischarges were low <strong>and</strong> the number of complex patients in the hospital increased– Insufficient staffing in ED after the Jubilee weekend led to lack of senior decision making <strong>and</strong> tobreaches. RATing <strong>and</strong> senior ED leadership on site from Tues onward helped breach recovery▪ Initiatives are owned by trust teams, with routine monitoring <strong>and</strong> feedback– RATing has been extended to UCC <strong>and</strong> will be extended to KGH in August– Productivity improvements <strong>and</strong> workplace organisation is being implemented in UCC <strong>and</strong> majors– MAU continues to achieve consistent improved performance in 8am-5pm discharges <strong>and</strong> transfers– Pre-11 initiatives now owned by ward sponsors, providing daily feedback on ward performance– Weekend discharges now routinely monitored– Consultant <strong>and</strong> ward performance feedback dialogues now routine, with desire for more information
Performance – <strong>Trust</strong> Cluster Type 1,2,3 1% Patients treated in 4 hours, Target 95%April<strong>2012</strong>May<strong>2012</strong>May June June June28 th –3 rd 4 th –10 th 11 th –17 th 18 th –24 thWeek 5 Week 1 Week 2 Week 3QH 77.49% 85.71% 90.42% 88.74% 79.87% 93.38%KGH 92.92% 94.75% 92.51% 96.32% 94.57% 93.77%<strong>Trust</strong> 83.90% 89.49% 91.30% 91.94% 85.94% 93.55%1 This includes UCC KGH in KGH Cluster from 04/04/11 <strong>and</strong> UCC QH in QH Cluster 04/04/11 to 31/07/11; walk-in centres not includedSource: Performance Data team, B2 report 27/06/<strong>2012</strong>2
A&E 4hr target performanceA&E 4hr target achievement (Whole <strong>Trust</strong>) 11009590858075706560555005.0319.0302.041 Type 1, 2, 3 breaches includedSource: BHRU <strong>Trust</strong> B2 Report; 1st Mar <strong>2012</strong> – 26 th June <strong>2012</strong>Our performanceNational targetOur target16.04 30.04 14.05 28.05 11.06 25.06
A&E Black BreachesA&E Black Breaches (Whole <strong>Trust</strong>) 11816Number of black breaches151816Our performance14131210864287654321 12121133005Mar19Mar02Apr16Apr30Apr14May28May4June11June20June1 Black breaches from both sites are includedSource: Ambulance SUI list Master; 1st Mar <strong>2012</strong> – 5 th June <strong>2012</strong>
Last week Queen’s saw its best overall breach performancesince October 2011….May AverageattendanceW/day: 427W/end: 326483447418399393375357AttendancesConversion rate,percent28 34 31 30 32 31 36May Averages:Discharge w/day: 146Admission w/day: 140Admission w/end: 116Discharge w/end: 104164155156150142136131 133130129121117113DischargesAdmissions713341122882444BreachesMon18/06Tue19/06Wed20/06Thu21/06Fri22/06Sat23/06Sun24/06Source: B2 data, all divisions5
…versus the week following Jubilee weekend whenperformance was poorAverage433attendance385W/day: 427 343 346351W/end: 326465416397329375411467465AttendancesConvention rate,percent35 30 30 34 33 30 35 40 36 32 36 30 29181AverageDischarge w/day: 146Admission w/day: 140Admission w/end: 116Discharge w/end: 1041511261041037912910311592139123146157158159119118 12071149146147111146135DischargesAdmissions115118138124129Breaches454050513441120Fri1/6Sat2/6Sun3/6Mon4/6Tue5/6Wed6/6Thu7/6Fri8/6Sat9/6Sun10/6Mon11/6Tue12/6Wed13/66
ED <strong>and</strong> MAU update• Achievements• Had an average of 17 breaches/day at the Queen’s site, the lowest since mid-April start of initiatives• MAU achieved consistent average throughput of 36 patients between 8 am-5 pm• Conducted an early diagnosis of KGH emergency pathway in ED <strong>and</strong> MAU• Started formulating a new bed management escalation plan• Ten week ED transformation plan agreed• Challenges• One Black breaches last week, ED is approaching this through the change oflayout in Ambulances RATing• We had a challenging KGH performance, with main reasons being quality ofsenior leadership, availability of beds <strong>and</strong> flow processes at different interface• Performance in both sites’ ED remain dependent on the quality of ED leadershipavailable• Priorities• Embed RATing through design <strong>and</strong> production of guidelines <strong>and</strong> training videos• Start improvement initiatives including RATing, 8 a.m <strong>Board</strong> round <strong>and</strong> Acutemedicine evening consultant cover• Coach new UCC lead to implement UCC flow initiatives agreedCoach Majors lead to implement Majors’ flow initiatives agreed
50454035302520151050The total number of discharges has increased since theintroduction of the MAU board roundPre-11, total <strong>and</strong> average weekly discharges from MAU unit, number of patients1715 16 1510 107 75 4 3 4 422 2 20 1 2Mon23/04Mon30/04All discharged (transferred to ward or home) from 8am-5pm11am: discharged by 11am, Cat B494748Weekly average for 5pm 4646454041383435 35 36 363230 3130312927 27 2822222223 23 23 23222220 20181616Tue08/059 9 9 9 986 6 6 7 7 7 65 5 564 4 5 4421Mon14/05Mon21/05Mon28/05Wed06/06Mon11/067565 4 522Mon18/063Mon25/06Source: Daily collection of data, Initiative started 23 rd April <strong>2012</strong> – 9 th May <strong>2012</strong>; * Estimate
Breaches has been reduced by an average of 30/day sincestart of RATing500QH’s daily attendances <strong>and</strong> type 1 breaches in major/UCC,number of patientsAttendancesBreaches in main EDBreaches in UCCAverage400426421425 425425413414420412403405409 405 401389391 398 403401386393 389380 383384370374379 382380375362370360365366355 356358 358 3553633423493493443343293002001000RATing trial startedMon-Fri 9am-5pmWalk-in <strong>and</strong> Ambulance majors107108 109 11689 91 85 90 83 8880 81 8564616252424837Mon16/4Mon23/4Mon30/4Tue08/054636Mon14/05309122Mon28/051017564 64484538281911Mon21/0542Wed06/06111127 1279Mon11/069076522532208 3Mon18/06Mon25/06Source: validated internal ED data <strong>and</strong> <strong>Trust</strong> B2 report * Type 1 attendances for adults
No RATing is taking place at KGH, however reduction ofbreaches is evident300KGH’s daily attendances <strong>and</strong> type 1 breaches in major/UCC,number of patientsAttendancesBreaches in main EDBreaches in UCC255270200231211207 206196186 187180160234 232 232222 223226224226217221217 216211214209 209206209203206<strong>2012</strong>0<strong>2012</strong>02196199186 19019318818317717723022220718110003735 341819 16 17 141Mon16/4Mon23/4463438 3626 2328156 7 101227 5 8482Mon30/4Tue08/05Mon14/05Mon21/05Source: validated internal ED data <strong>and</strong> <strong>Trust</strong> B2 report * Type one attendances2234044Mon28/05201057Wed06/0664727Mon11/06114194 7Mon18/0664193 6Mon25/06
Medicine <strong>and</strong> care of the elderly update• Achievements• Ward sponsor reports <strong>and</strong> meetings under way• Increased total number of discharges, exceeding the number of admissions <strong>and</strong>creating capacity on the wards for weekends• Held key 1 to 1 meetings for reducing the number of long-stay patients• Weekly performance feedback ongoing – increased attendance as part ofgovernance meeting• Challenges• Weekend discharges low <strong>and</strong> resulted in high number of breeches on Monday• Pre-11am reporting not systematic, still relying on manual processes• Simple observations reveal wards not embedding all practices• No agreement on how to achieve consistent consultant input into the wards• Priorities• Challenge established ways of working on wards• Establish rotation for ward sponsor observations so that they can work onembedding the components to pre-11am discharges• Kick-off long stay patient workstream <strong>and</strong> agree workplans
Last week we admitted 8 fewer patients thanwe discharged in medicine……Queens non-elective medical admissions <strong>and</strong> discharges,Number of patientsMedical admissionsMedical dischargesTotalNet80-4 -16 -8 -4 +9 -1 +14-860516759625640373522820Mon-18Tues-19Wed-20Thurs-21Fri-22Sat-23Sun-24360Source: Discharges by week by ward, <strong>Trust</strong> status summary admissions
.. versus the preceding week (11 th –17 th June) whenwe admitted 49 more patients than we dischargedQueens non-elective medical admissions <strong>and</strong> discharges,Number of patientsMedical admissionsMedical dischargesTotalNet800 -5 16 12 -1 7 2049605757505652404138620Mon-11Tues-12Wed-13Thurs-14Fri-15Sat-1624Sun-17337Source: BHRUT bed management team <strong>and</strong> information department
EXECUTIVE SUMMARYTITLE:Maternity Update – May <strong>2012</strong>BOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong>DATE:The purpose of this report is to provide the <strong>Trust</strong><strong>Board</strong> with an update on the monthly performancefor maternity services.The key areas to note are:• In May the <strong>Trust</strong> went over the cap on sixoccasions however the units remainedclinically safe. Two women were divertedin the month.• Average of 78% of women were seen by amidwife in triage within 15 minutes <strong>and</strong>91% within 30 minutes.• 99% of women in May were seen by adoctor in the OAU.• Data capture in OAU out of hours hasfound to be calculated incorrectly this isbeing rectified.• 100% women received pethidine within 15minutes of the request <strong>and</strong> 91% womenreceived an epidural with 30 mins of therequest.• 2 SIs were reported in May.• 75% of the grade1 LSCS were performedwithin 30 mins from decision, at Queen’s<strong>and</strong> 100% at KGH. The Clinical Director isundertaking an audit of the records toascertain if the records have been gradedappropriately• The cap on the number of births has beenremoved from BHRUT with effect fromJune <strong>2012</strong>.• The escalation process continues in linewith other maternity units <strong>and</strong> inconjunction with the PAN Londonescalation policy.• Weekly reporting to NELC has nowceased.• Monthly reporting will continue.• A draft BHRUT assurance framework hasbeen developed <strong>and</strong> under discussion withNELC.□ PBE ……………..….. □STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT……………………□ QUALITY & STRATEGY…………..………….....……□ CHARITABLE FUNDS………………………………...…□ TRUST BOARD……………………………….………….□ REMUNERATION………………………………….…...□ OTHER …………………………..…….(please specify)2. DECISION REQUIRED: CATEGORY:The <strong>Board</strong> are asked to note the content of the □ NATIONAL TARGET □ RMS
eport.□ CQC REGISTRATION □ HEALTH &SAFETY□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROMCOMMISSIONERS□ CORPORATE OBJECTIVE……………………………....□ OTHER …………………….. (pleasespecify)AUTHOR/PRESENTER: W MatthewsPresenter: D WheelerDATE: 27 th June <strong>2012</strong>3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:N/A4. DELIVERABLESMaternity Improvement plan.5. KEY PERFORMANCE INDICATORS91% of women seen within 30 minutes of arrival within Triage99% of women seen within an hour of referral to an obstetrician within the obstetric assessmentunit.100% of women received pethidine within st<strong>and</strong>ard.AGREED AT ______________________MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
Maternity Services Monthly Performance Report<strong>Trust</strong> Name<strong>Barking</strong>, <strong>Havering</strong> & <strong>Redbridge</strong> University HospitalsNHS <strong>Trust</strong>Reporting monthThis report covers the period:1 st May to 31 st May <strong>2012</strong>Completed byMr Dele OlorunsholaClinical Director of Obstetrics, Gynaecology <strong>and</strong>Sexual HealthReviewed byDeborah WheelerDirector of NursingNeill MoloneyDirector of Planning & PerformanceContact Details<strong>Barking</strong>, <strong>Havering</strong> & <strong>Redbridge</strong> University HospitalsNHS <strong>Trust</strong>1st Floor Green ZoneMaternity Services, Queens HospitalRom Valley Way, Romford, RM7 0AGTel: 01708 435 000 x 3894A monthly report will be provided to; monitor the progress made against the maternity servicesimprovement plan, provide assurance that the safety <strong>and</strong> quality of maternity services areimproving within BHRUT. It will summarise the themes <strong>and</strong> actions that have arisen from theweekly analysis of activity within the unit.Monthly maternity report May <strong>2012</strong> v1.1. DOPage 1 of 9Compiled by C Frisby 13.06.<strong>2012</strong>1
1. IntroductionThe purpose of this report is to summarise the progress made In May <strong>2012</strong> against the maternityservice improvement plan <strong>and</strong> the KPIs agreed with the commissioning team within ONEL.2. Total Number of Births at BHRUT for May <strong>2012</strong>KGHQueensElectiveLSCSEmergencyLSCSOtherTotalEmergencyLSCSElectiveLSCSOtherTotal5 7 154 166 112 45 464 6213. Weekly Activity (excluding elective LSCS)Weekly Delivery Activity KGH/QHTotal Deliveries18016014012010080604020005/09/201112/09/201119/09/201126/09/201103/10/201110/10/201117/10/201124/10/201131/10/201107/11/201114/11/201121/11/201128/11/201105/12/201112/12/201119/12/201126/12/201102/01/<strong>2012</strong>09/01/<strong>2012</strong>16/01/<strong>2012</strong>23/01/<strong>2012</strong>30/01/<strong>2012</strong>06/02/<strong>2012</strong>13/02/<strong>2012</strong>20/02/<strong>2012</strong>27/02/<strong>2012</strong>05/03/<strong>2012</strong>12/03/<strong>2012</strong>19/03/<strong>2012</strong>26/03/<strong>2012</strong>02/04/<strong>2012</strong>09/04/<strong>2012</strong>16/04/<strong>2012</strong>23/04/<strong>2012</strong>30/04/<strong>2012</strong>07/05/<strong>2012</strong>14/05/<strong>2012</strong>21/05/<strong>2012</strong>28/05/<strong>2012</strong>Queens Deliveries(optimum 140)KGH DeliveriesWeek ending (optimum 49) DateOptimum Queens4. EscalationsAs part of the capacity management plan the escalation process has been reviewed. The status goesto ‘red’ when there are 15 deliveries or equivalent of labouring women at Queen’s <strong>and</strong> 5 at KGH.Site Red Amber Green EscalationsQH 17 31 31 2KGH 16 0 31 1Monthly maternity report May <strong>2012</strong> v1.1. DOPage 2 of 9Compiled by C Frisby 13.06.<strong>2012</strong>2
4.1 CappingThe capping is currently set to 20 births for Queen’s Hospital <strong>and</strong> 7 births for King George Hospital(optimum delivery rate) 27 in total. This is an accrued total which is calculated from 6pm of day one to5:59pm of day two. These figures are calculated excluding elective caesarean sections.In May <strong>2012</strong> the <strong>Trust</strong> went over the cap on 6 occasions in total.DateNo of BirthstotalNo. abovecap01/05/<strong>2012</strong> to 02/05/<strong>2012</strong> 29 203/05/<strong>2012</strong> to 04/05/<strong>2012</strong> 29 204/05/<strong>2012</strong> to 05/05/<strong>2012</strong> 28 111/05/<strong>2012</strong> to 12/05/<strong>2012</strong> 28 122/05/<strong>2012</strong> to 23/05/<strong>2012</strong> 28 128/05/<strong>2012</strong> to 29/05/<strong>2012</strong> 29 2The maternity unit remained clinically safe on these six occasions4.2 DivertsThere were two diverts in May, one to Homerton Hospital <strong>and</strong> one to Basildon.5.0 TriageThe agreed st<strong>and</strong>ard is that 98% of women will be seen by a midwife within 15 minutes of arrival attriage. In May, overall 76% of women were seen within 15 minutes of arrival <strong>and</strong> 91% were seenwithin 30 minutes.Triage - % of Patients Seen within 15 Minutes of Arrival110100908070605040302010001/03/<strong>2012</strong>06/03/<strong>2012</strong>11/03/<strong>2012</strong>16/03/<strong>2012</strong>21/03/<strong>2012</strong>26/03/<strong>2012</strong>31/03/<strong>2012</strong>05/04/<strong>2012</strong>10/04/<strong>2012</strong>15/04/<strong>2012</strong>20/04/<strong>2012</strong>Number of Patients25/04/<strong>2012</strong>30/04/<strong>2012</strong>05/05/<strong>2012</strong>10/05/<strong>2012</strong>15/05/<strong>2012</strong>20/05/<strong>2012</strong>25/05/<strong>2012</strong>30/05/<strong>2012</strong>Day% of patients Seen within 15 minutesMonthly maternity report May <strong>2012</strong> v1.1. DOPage 3 of 9Compiled by C Frisby 13.06.<strong>2012</strong>3
Triage WaitingtimesNumber ofWomen% of TotalwomenUp to 15 minutes 888 76%15-30 minutes 169 15%31-60 minutes 85 7%61 minutes + 21 2%6.0 OAU ActivityIt has been agreed that 98% of women should be seen by an obstetrician, where this is deemedclinically appropriate, within 1 hour of their arrival to the Obstetric Assessment Unit (OAU) in hours.The <strong>Trust</strong> average for May <strong>2012</strong> was 99%.% of Patients seen within 1 hour on OAU by an Obstetrician110100908070605040302010001/03/<strong>2012</strong>06/03/<strong>2012</strong>11/03/<strong>2012</strong>16/03/<strong>2012</strong>21/03/<strong>2012</strong>26/03/<strong>2012</strong>31/03/<strong>2012</strong>% of patients seen05/04/<strong>2012</strong>10/04/<strong>2012</strong>15/04/<strong>2012</strong>20/04/<strong>2012</strong>25/04/<strong>2012</strong>30/04/<strong>2012</strong>05/05/<strong>2012</strong>10/05/<strong>2012</strong>15/05/<strong>2012</strong>20/05/<strong>2012</strong>25/05/<strong>2012</strong>30/05/<strong>2012</strong>% of Patients seen within 1HourDateMonthly maternity report May <strong>2012</strong> v1.1. DOPage 4 of 9Compiled by C Frisby 13.06.<strong>2012</strong>4
7.0 Out of Hours OAU98% of patients attending the Out of Hours OAU should be seen by an Obstetrician, where itis deemed clinically appropriate, within one hour of their arrival to this unit.The Out of Hours OAU is currently under review by Clinical Fellows <strong>and</strong> department leadsowing to consistently higher waiting times than it’s counterparts. This OAU is governed by thesame st<strong>and</strong>ard as the main OAU, however, the data collection for this area reflects a twentyfourhour period rather than 8pm to 8am when the main OAU is closed. Until the data isrefreshed a % is not available. Several changes are being piloted in this area to achieveshorter waiting times for clients. Changes have already taken place in OAU in hours whichhas improved waiting times. Once the planning phase is complete for out of hours OAU, themost appropriate pathway will be implemented.% of Patients seen within 1 Hour of Referral12010080604020001/03/<strong>2012</strong>08/03/<strong>2012</strong>15/03/<strong>2012</strong>22/03/<strong>2012</strong>29/03/<strong>2012</strong>05/04/<strong>2012</strong>12/04/<strong>2012</strong>19/04/<strong>2012</strong>26/04/<strong>2012</strong>03/05/<strong>2012</strong>10/05/<strong>2012</strong>17/05/<strong>2012</strong>24/05/<strong>2012</strong>31/05/<strong>2012</strong>% of Patients seen within 1Hour of Referral Target8.0 Analgesia AuditSome additional information is at the base of this report, titled ‘Additional Information’ <strong>and</strong>contains some references to analgesia administrations.On a weekly basis, as part of visible leadership, an audit is undertaken to monitor theamount of time women are waiting for their analgesia. The agreed st<strong>and</strong>ard is:• If a woman requests pethidine she should receive this within 15 minutes of the request.The <strong>Trust</strong> achieved 100% against this st<strong>and</strong>ard in May <strong>2012</strong> of those cases audited.• If a woman requests an epidural she should receive this within 30 minutes of therequest. The <strong>Trust</strong> achieved 91% against this st<strong>and</strong>ard for May <strong>2012</strong> of those casesaudited.Monthly maternity report May <strong>2012</strong> v1.1. DOPage 5 of 9Compiled by C Frisby 13.06.<strong>2012</strong>5
9. Serious Untoward Incidents ReportedSUI’s are reported on a weekly basis, in retrospect, therefore the information below issummarised weekly but may include overlapping information from post <strong>and</strong> priormonth.ReportNo of Date of Details ofWeek Commencing Incidents Incident Incident7 th May 014 th May 021 st May 028 th May 2 06/05/<strong>2012</strong> Unexpectedadmission to theneonatal intensivecare unit – infant>37 completedweeks gestationthat have a suddenor unexpectedcollapse followingdelivery.28 th May 16/05/<strong>2012</strong> Unexpectedadmission to theneonatal intensivecare unit – infant>37 completedweeks gestationthat have a suddenor unexpectedcollapse followingdelivery.Site ofIncidentKing GeorgeHospitalKing GeorgeHospitalMonthly maternity report May <strong>2012</strong> v1.1. DOPage 6 of 9Compiled by C Frisby 13.06.<strong>2012</strong>6
Caesarean Deliveries including Elective ActivitySome additional information is at the base of this report, titled ‘Additional Information’<strong>and</strong> contains some references to anaesthetics.When a decision is made to perform an emergency LSCS, the timing for this is dictated by theacuity of each case which is graded from 1-4.Grade 1Caesarean section is considered as urgent <strong>and</strong> has an immediate threat to the life of the woman<strong>and</strong> foetus. To be performed within 30 minutes.At Queen’s hospital 79% of the audited grade 1 C/S were performed within 30 minutes.At KGH, the average based on the notes audited was 100%.Grade 2Caesarean section is considered urgent with maternal or foetal compromise which is notimmediately life threatening. To be performed within 60 minutesAt Queen’s hospital of 78% the audited grade 2 emergency C/S were performed within 60 minutes.At KGH the average was for the notes audited 100%Grade 3 & 4Caesarean section is an emergency with no maternal or foetal compromise, but requires earlydelivery. To be performed at a time to suit the mother <strong>and</strong> the department.At Queen’s hospital, 100% of the audited grade 3/4 emergency C/S were performed within time.At KGH hospital 100% of the audited grade 3/4 emergency C/S were performed within time.Top 3 reasons for delays for all grades of LSCS like the previous month were:1. Clinicians required elsewhere due to busy Labour Ward <strong>and</strong> theatres2. Theatre capacity3. Delayed consent (by mother)Monthly maternity report May <strong>2012</strong> v1.1. DOPage 7 of 9Compiled by C Frisby 13.06.<strong>2012</strong>7
Quarterly workforce report for May <strong>2012</strong>RecruitmentCurrently there are 16 midwives in the recruitment process that are due to qualify in Septemberthat have been offered posts at BHRUT.6 midwives commenced employment in May <strong>and</strong> are currently on their induction programme2 nurses have been appointed <strong>and</strong> remain within the recruitment process.With have further interviews in June for the remaining MCA vacanciesWe interviewed for a Midwifery Placement Facilitator <strong>and</strong> successfully appointed, however shedeclined to take the post. This post was re-advertised <strong>and</strong> has already been shortlistedNew starters in May6 midwivesAdvertsWe are going out to advert for an 8a patient satisfaction/ lead midwife in BereavementThere is 2.74WTE vacancy in b<strong>and</strong> 7; we are currently waiting for the review of the JD with theA4C panelLeavers9 midwives left the trust, some of which have returned to their own country <strong>and</strong> others who havegone to work in a surrounding low risk unit. Discussions took place with these midwives regardingBHRUT co-located birthing centre opening in the autumn however the midwives could not beretainedHow are we maintaining the 1:29 midwife to birth ratioWithin the wards the staffing is done on a monthly basis <strong>and</strong> temporary staff are booked for thevacant shifts. Every day this is reviewed <strong>and</strong> amended.% of bank <strong>and</strong> agencyThe % of bank <strong>and</strong> agency currently used within the month of May is:Midwife• 28.47 WTE = 8.9 % bank- this is an increase of 1%, due the increased number of midwivesthat left the trust in May.• 7.14 WTE = 2% agency- this is a reduction of 0.9 % on last monthNurses• 0.78WTE = 2% agency• 2.8 WTE = 10% bankMaternity Support Workers• 16.89 WTE = 22% bankMonthly maternity report May <strong>2012</strong> v1.1. DOPage 8 of 9Compiled by C Frisby 13.06.<strong>2012</strong>8
Medical recruitmentWe have 2 Consultant vacancies, one left in June <strong>and</strong> one in March <strong>and</strong> we have 2 full timelocums covering these posts.Balanced ScorecardThe balanced scorecard for May <strong>2012</strong> is attached as Appendix 1. Please note that the scorecard isunder review <strong>and</strong> not all information was available at the time of submission of this report.Additional InformationDr R Pilling, has as part of his Clinical Fellow duties, has undertaken an audit into the impact of asecond anaesthetist being available out of hours. His conclusions are below.Conclusions from audit undertaken to ascertain the impact of a second anaesthetist beingavailable out of hours: Clearly extremely busy maternity unit Unpredictable nature of obstetric shifts 40% of shifts well above the average number of anaesthetic interventions required. Increased opening of 2nd theatre since the increased anaesthetic presence Several occasions of a few minutes overlap time Are the indications for a 2nd theatre becoming more relaxed? Or…are we now more compliant with target times for emergency LSCS? Sharing of the workload has definately eased the pressure on the labour ward anaesthetist What evidence do we have of an improvement in patient care?Conclusions from audit in relation to epidural waiting times…. Clear benefit from 2nd anaesthetist Improved epidural waiting times More time available to take an active role on maternity HDU Improved working conditions for duty anaesthetistRecommendations from same audit… Definate need for 2nd anaesthetist on labour ward Needs a separate audit of the indications for the use of 2 theatres Better epidural data(should improve with the imminent introduction of computerised data collection) Reaudit to ensure maintainance of high st<strong>and</strong>ardsMonthly maternity report May <strong>2012</strong> v1.1. DOPage 9 of 9Compiled by C Frisby 13.06.<strong>2012</strong>9
EXECUTIVE SUMMARYTITLE:BOARD/GROUP/COMMITTEE:Learning Disability Progress Report <strong>Trust</strong> <strong>Board</strong> - 4 th <strong>July</strong> <strong>2012</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) &DATEThe report provides the <strong>Trust</strong> <strong>Board</strong>□ PBE ……………..…..with an update on the delivery of theLD agenda, particularly in relation to: □ STRATEGY……….….…….• Health for All (2008)• Six Lives report (2010)• Death by Indifference (2007)• Learning disabilities St<strong>and</strong>ardAssessment Framework (<strong>2012</strong>)(SAF)The report also contains an LD actionplan for <strong>2012</strong>/13, which has beendiscussed <strong>and</strong> approved at the <strong>Trust</strong>’sLD, Safeguarding Adults <strong>and</strong> Quality &Safety Committees.Actions identified in plan have been setin line with national guidance <strong>and</strong> localidentified need.As part of the Learning Disabilities week(18 th - 22 nd June <strong>2012</strong>), the <strong>Trust</strong> signedup to the Mencap Charter.□ FINANCE ……..………□ AUDIT ……………………□ QUALITY & STRATEGY …………..……□ CHARITABLE FUNDS ……………………...…□ TRUST BOARD…………………….………….□ REMUNERATION……………………………...□ OTHER:BHRUT Safeguarding Adults CommitteeBHRUT Learning Disabilities CommitteeBHRUT Quality & Safety Committee - 12 thJune <strong>2012</strong>2. DECISION REQUIRED: CATEGORY:For information <strong>and</strong> noting.□ NATIONAL TARGET□ CNST* CQC REGISTRATION (Outcome 7)□ HEALTH & SAFETY□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE……………………………....□ OTHER …………………….. (please specify)AUTHOR:Gary Etheridge, Deputy Director of NursingPRESENTER:Deborah Wheeler, Director of NursingDATE: <strong>July</strong> <strong>2012</strong>1
3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:N/A4. DELIVERABLESEnsure that the st<strong>and</strong>ards set within the LD Self Assessment Framework are achieved.Maintain the multidisciplinary collaboration within the local economy.Ensure that the relevant recommendations set in both Healths for All <strong>and</strong> Six Lives areimplemented within the organisation.5. KEY PERFORMANCE INDICATORSCQC Outcome 4 - Care <strong>and</strong> welfare of people using the serviceCQC Outcome 6 - Co-operate with other providesCQC Outcome 7 - Safeguarding people from abuseAGREED AT ___________MEETINGORREFERRED TO: _________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
LEARNING DISABILITIES PROGRESS REPORT - JULY <strong>2012</strong>1. IntroductionEquality in accessing healthcare is the central principle in the delivery of care within the NHS. The‘Death by Indifference’ (2007) report from Mencap highlighted significant evidence that equality forpatients with a learning disability who use NHS services was sadly lacking <strong>and</strong> identified patientstories of six deaths whilst in NHS care. In response to this report Sir Jonathan Michael wascommissioned to review the care delivered to these six patients. Following on from this inquiry, tenrecommendations were identified <strong>and</strong> published in the report ‘Healthcare for All’ (2008).The Ombudsmen Report ‘Six Lives’ (2009) supported the recommendations from Healthcare forAll. All of the recommendations were accepted by Government <strong>and</strong> were set out in Valuing PeopleNow: Delivery Plan in January 2009.The publication of the Death by Indifference report prompted a number of families to contactMencap, <strong>and</strong> they continued to do so in the weeks, months <strong>and</strong> years that followed. It is thesecases - a total of 74 to date that form the basis of the article published in the Guardian on 3 rdJanuary <strong>2012</strong>.A further report was produced by Mencap (<strong>2012</strong>), ‘Death by Indifference: 74 deaths <strong>and</strong> counting.A progress report 5 years on’, which considers the steps that have been taken, the progress madeas a consequence <strong>and</strong> what they believe still remains to be done for LD patients. The report paysparticular attention to deaths that have been reported to Mencap between 2009 <strong>and</strong> 2011. Thesecases illustrate Mencap’s serious ongoing concerns that not enough progress has yet been madein addressing the health inequalities experienced by people with a learning disability.Joint working between the local learning disability population, community learning disability teams<strong>and</strong> the <strong>Trust</strong>’s safeguarding team is constantly improving, with strong links now being formedacross all groups’ services <strong>and</strong> departments in the community <strong>and</strong> within BHRUT.2. Local ActionThe <strong>Trust</strong> has made significant progress in implementing a range of local measures to ensure thatpeople with a learning disability receive services/care that takes account of their healthcare needs<strong>and</strong> are proactive in helping them access the healthcare they need.A detailed learning disabilities action plan is regularly updated <strong>and</strong> presented at the <strong>Trust</strong>’sSafeguarding Adults <strong>and</strong> Learning Disabilities Committees.LD actions achieved to date are identified in Appendix I.There are still areas that require additional development during <strong>2012</strong>/13 <strong>and</strong> these are contained inAppendix II.3. Mencap Charter LaunchAs part of the learning disabilities week (18 th June to 22 nd June <strong>2012</strong>) st<strong>and</strong>s were set up in themain entrances of King George’s <strong>and</strong> Queens Hospitals to showcase the current work that hasbeen progressed within the <strong>Trust</strong> to improve access to people with a learning disability, <strong>and</strong> toraise awareness of their needs when they come into hospital.3
Key stakeholders, including service users from the charity “People First” as well as staff from thelocal community learning disability teams of <strong>Havering</strong>, <strong>Barking</strong> & Dagenham, Waltham Forrest <strong>and</strong><strong>Redbridge</strong>, supported by BHRUT, were involved in hosting the st<strong>and</strong>s.To emphasise the commitment to real partnership working the <strong>Trust</strong> signed up to the MencapCharter at a launch event on the 22 nd June <strong>2012</strong>.The nine key charter pledges that the <strong>Trust</strong> has signed up to are outlined below:4. RecommendationsMembers of the <strong>Trust</strong> <strong>Board</strong> are asked to note the content of this report.Gary EtheridgeDeputy Director of Nursing<strong>July</strong> <strong>2012</strong>4
Appendix IHEALTHCARE FOR ALL - INITIATIVES ACHIEVEDRECOMMENDATIONRecommendation 1Those with responsibility for the provision <strong>and</strong> regulation of undergraduate<strong>and</strong> postgraduate clinical training must ensure that curricula includem<strong>and</strong>atory training in Learning disabilities. It should be competence-based<strong>and</strong> involve people with learning disabilities <strong>and</strong> their carers in providingtraining.Recommendation 2All healthcare organisations should ensure they collect the data <strong>and</strong>information necessary to allow people with a learning disability to beidentified by the health service <strong>and</strong> their pathways of care tracked.Recommendation 3Family <strong>and</strong> other carers should be involved as a matter of course aspartners in provision of treatment <strong>and</strong> care, unless good reason is given,<strong>and</strong> <strong>Trust</strong> <strong>Board</strong>s should ensure that reasonable adjustments are made toenable them to do this effectively. This will include the provision ofinformation, but may also involve practical support <strong>and</strong> service coordination.ACHIEVEMENTS• As part of the 90 minute <strong>Trust</strong>’s statutory <strong>and</strong> m<strong>and</strong>atory safeguarding adults training a 30minute session on the care <strong>and</strong> management of patients with learning disabilities is included.• People with learning disabilities <strong>and</strong> their carers contribute to teaching on <strong>Trust</strong> wide in-housestudy days, which has given staff the tools to underst<strong>and</strong> the complexity of the patient’sneeds.• Each ward/department has a safeguarding adult’s link nurse.• The <strong>Trust</strong>’s PAS system contains a learning disability code. This enables patients with a LD tobe flagged. This information is shared internally/externally.• The <strong>Trust</strong>’s LD sub-group has LD representation, to advice on the needs of people with LD.This includes peer reviewing any information to ensure that it meets the needs of the patientwith learning disabilities.• <strong>Trust</strong> Internet site contains patient information leaflets designed for <strong>and</strong> giving appropriateinformation for people with LD.• There is a signposting reception area to allow patients <strong>and</strong> their relatives to seek advice onwhere a department or ward is at the Queen’s site entrance. A member of staff in thereception will walk with the patient to ensure that they get to their destination within thehospital setting.5
RECOMMENDATIONRecommendation 4Primary Care <strong>Trust</strong>s should identify <strong>and</strong> assess the needs of people withLearning disabilities <strong>and</strong> their carers as part of their Joint Strategic NeedsAssessment. They should consult with the Local Strategic Partnership, theLearning Disability Partnership <strong>Board</strong>s <strong>and</strong> relevant voluntary user-ledLearning Disability organisations <strong>and</strong> use the information to inform thedevelopment of Local Area Agreements.Recommendation 5To raise awareness in the health service of the risk of premature avoidabledeath, <strong>and</strong> to promote sustainable good practice in local assessment,management <strong>and</strong> evaluation of services, the Department of Health shouldestablish a learning disabilities Public Health Observatory.Recommendation 6The Department of Health should immediately amend Core St<strong>and</strong>ards forBetter Health, to include an explicit reference to the requirement to make‘reasonable adjustments’ to the provision <strong>and</strong> delivery of services forvulnerable groups, in accordance with the disability equality legislation. Theframework that is planned to replace these core st<strong>and</strong>ards in 2010 shouldalso include a specific reference to this requirement.Recommendation 7Inspectors <strong>and</strong> regulators of the health service should develop <strong>and</strong> extendtheir monitoring of the st<strong>and</strong>ard of general health services provided forpeople with Learning disabilities, in both the hospital sector <strong>and</strong> in thecommunity where primary care providers are located. The aim is to supportappropriate, reasonable adjustments to general health services for adults<strong>and</strong> children with learning disabilities <strong>and</strong> their families to ensurecompliance with <strong>and</strong> enforcement of all aspects of the DisabilityDiscrimination Act.• N/A for acute <strong>Trust</strong>.• N/A for acute <strong>Trust</strong>.ACHIEVEMENTS• The <strong>Trust</strong> participated <strong>and</strong> completed the Learning Disability St<strong>and</strong>ard AssessmentFramework (SAF) in 2011.• The <strong>Trust</strong> is compliant with relevant recommendations in Outcome 4, 6 & 7.• There are commissioning representatives on the LD Committee. Completed SAF is sharedwith NHS London who analyses <strong>and</strong> identifies gaps in service provision in relation to LDpatients receiving care within the <strong>Trust</strong>.6
RECOMMENDATIONRecommendation 8The Department of Health should direct Primary Care <strong>Trust</strong>s (PCTs) tosecure general health services that make ‘reasonable adjustments’ forpeople with Learning disabilities through a Directed Enhanced Service. Inparticular, the Department should direct PCTs to commission enhancedprimary care services which include regular health checks provided by GPpractices <strong>and</strong> improve data, communication <strong>and</strong> cross boundary partnershipworking. This should include liaison staff who work with primary careservices to improve the overall quality of health care for people with learningdisabilities across the spectrum of care.Recommendation 9Section 242 of the National Health Service Act 2006 requires NHS bodies toinvolve <strong>and</strong> consult patients <strong>and</strong> the public in the planning <strong>and</strong> developmentof services, <strong>and</strong> in decision affecting the operation of services. All <strong>Trust</strong><strong>Board</strong>s should ensure that the views <strong>and</strong> interests of people with learningdisabilities <strong>and</strong> their carers are included.Recommendation 10All <strong>Trust</strong> <strong>Board</strong>s should demonstrate in routine public reports that they haveeffective systems in place to deliver effective, ‘reasonably adjusted’ healthservices for those people who happen to have a Learning Disability. This‘adjustment’ should include arrangements to provide advocacy for all thosewho need it <strong>and</strong> arrangements to secure effective representation on PALSfrom all client groups including people with learning disabilities.• N/A for acute care.ACHIEVEMENTS• There is LD representation at the LD Sub-Committee. All workstreams in relation to the LDagenda are discussed at this group. Further discussion will take place at the <strong>Trust</strong>’s LDCommittee.• Safeguarding issues/actions are included in a bi-monthly safeguarding adult’s progress report.• PALS have a LD lead for the team who is made aware of all PALS issues relating to LDpatients. This information is also submitted to the Deputy Director of Nursing.• Information relating to PALS issues is submitted to the Safeguarding Lead for inclusion in herbi-monthly report.7
Appendix IICARE OF PATIENTS WITH A LEARNING DISABILITYACTION PLAN - <strong>2012</strong>/13RECOMMENDATION LEAD TIMESCALE ACTIONS PROGRESS EVIDENCE RAG1.Creation of Learning Disability(LD) champions to ensure thatthe workforce are givenappropriate support <strong>and</strong> trainingto equip them to deliver the LDagenda.2.Special arrangements to be putin place to ensure reasonableadjustments are included in thejourney of a patient with LD.3.The development / review of atransition protocol for patientswith LD from children servicesto either adult services or anyother specialist service.NamedNurseNamedNurseNamedNurse &MatronsNamedNurseNamedNursesNamedNurseApril <strong>2012</strong>April <strong>2012</strong>March 2013March 2013September<strong>2012</strong>December<strong>2012</strong>LD champions to be agreed <strong>and</strong> roleprofile to be developed.Develop <strong>and</strong> implement LD championtraining as part of the Safeguarding Linkworker programme. Learning disabilityleads in the community to participate in thetraining day.Clinical leads to review all current patientpathways <strong>and</strong> bundles to ensure thatreasonable adjustments have beenconsidered for LD patients <strong>and</strong> patientsat risk including timings of appointments,facilities <strong>and</strong> suitable support.Equality impact assessment to becompleted when implementing <strong>and</strong>reviewing these pathways <strong>and</strong> carebundles.Protocols to be reviewed to see whethera st<strong>and</strong> alone eclectic policy would beappropriate.Protocol to be signed off by appropriateCommittee as per the <strong>Trust</strong>s policy onpolicies <strong>and</strong> protocols.Existing safeguarding adultchampions in place. Role to beextended to incorporate LD.Training day held on the 26 thApril <strong>2012</strong>.Agenda8
RECOMMENDATION LEAD TIMESCALE ACTIONS PROGRESS EVIDENCE RAG4.Ensure carer engagement ismaintained <strong>and</strong> that supportarrangements are shared <strong>and</strong>available at all times.5.PALS <strong>and</strong> complaints servicesmakes reasonable adjustmentsto ensure that patients <strong>and</strong>carers with LD have a voice are<strong>and</strong> are aware of the servicesavailable.NamedNurseNamedNurseDeputyDirector ofNursingPALS &ComplaintsMgrsNamedNurseDeputyDirector ofNursingPALSManagerDeputyDirector ofNursingPALSManagerDeputyDirector ofNursingPALS MgrMay <strong>2012</strong>& Nov <strong>2012</strong><strong>July</strong> <strong>2012</strong>August <strong>2012</strong>Bi-monthlyOctober <strong>2012</strong>Bi-monthlyMay <strong>2012</strong>LD patient surveys to be conducted twiceyearly.LD representation to be included on LDsub-committee.May <strong>2012</strong> Survey currently beingundertaken. Results will beavailable early June <strong>2012</strong>.A LD sub-committee has LDrepresentation, to advice on theneeds of people with Learningdisabilities. This includes peerreviewing any information toensure that it meets the needs ofthe patient with LD.Complaints & PALS information to bemade available in easy read versions. .Bi-monthly reports to be produced oncomplaints & PALS issues raised inrelation to adults at risk.PALS to be advised of all in-patientadmissions of patients with LD <strong>and</strong> tomake pro-active contact with patient <strong>and</strong>family to introduce service.PALS information relating to LD patientexperience will be reported inSafeguarding Adult Committee reports.PALS staff to provide signposting to LSpatients <strong>and</strong> family members toadvocacy <strong>and</strong> support organisations.Bi-monthly reports presented atthe Quality & Safety Committee.In place.MinutesMinutesReports9
RECOMMENDATION LEAD TIMESCALE ACTIONS PROGRESS EVIDENCE RAG6.The <strong>Trust</strong> should align itscomplaints procedures withother partner agencies.7.Whilst the patient is under thecare of the <strong>Trust</strong> the needs ofthe patient with learningdisabilities are assessedcorrectly in order to reduce therisk of diagnostic oversight.(CQC Outcome 4).8.<strong>Trust</strong> needs to be assured that itis compliant with the coreaspects of the LD SAF.9.The <strong>Trust</strong> must be assured that20% of the workforce aretrained in the care <strong>and</strong>management of patientsdiagnosed with Autism. (LDSAF requirement).DeputyDirector ofNursingAssistantDirector ofNursing &NamedNurseNamedNurse &externalpartnersNamedNurse &externalpartnersNamedNurseNamedNurseDeputyDirector ofNursingNamedNurseDeputyDirector ofNursingNamed<strong>July</strong> <strong>2012</strong>Meeting to be arranged to identify if thisprocess is in place <strong>and</strong> next steps.August <strong>2012</strong> Development <strong>and</strong> review of nursingdocumentation to take into account LDneeds. LD sub-committee members to beinvolved in process.October <strong>2012</strong>March 2013June <strong>2012</strong>September<strong>2012</strong>September<strong>2012</strong>March 2013<strong>Trust</strong> health record for a patient with LDto be devised.Training to be coordinated to ensure staffknow the process of acquiring acompleted health passport or completethe <strong>Trust</strong> LD learning passport oncedevised.Complete Annual LD Self AssessmentFramework.Following SAF assessment, identifiedgaps to be included in LD action plan.Outcome of the review of the LD SAF tobe shared with the LD Committee <strong>and</strong>Quality & Safety Committee.<strong>Trust</strong> to liaise with the borough educationteams to ascertain local economyapproach to achieving this target.March 2013 Investigate other forms of training i.e. e-learning as a way of achieving targetaudience.<strong>Trust</strong> health record for a patientwith LD currently is currentlybeing devised with theassistance of the external LDlead nurses.<strong>Trust</strong> currently waiting for SAFdocument.10
RECOMMENDATION LEAD TIMESCALE ACTIONS PROGRESS EVIDENCE RAG10.Review <strong>and</strong> raise awarenesswithin the <strong>Trust</strong> of the risk ofpremature death <strong>and</strong> promotesustained good practice in theassessment, decision making<strong>and</strong> implementation of care forLD patients who are at risk oflife threatening conditions <strong>and</strong>end of life provision (Death byIndifference 2007).11.Implementation of the MencapCharter.12.Review safeguarding adult’sintranet/internet site.NurseDeputyDirector ofNursingNamedNurseMarch 2013Compliance to be reported quarterly atLD Committee.Named Dr <strong>July</strong> <strong>2012</strong> Review DNR <strong>and</strong> End of Life Policy.Named <strong>July</strong> <strong>2012</strong>NurseNamedNurseDeputyDirector ofNursingNamedNurseEnsure that staff are aware of the MentalCapacity Act 2005 <strong>and</strong> Deprivation ofLiberties process in relation to the LDpatient.<strong>July</strong> <strong>2012</strong> Review the <strong>Trust</strong>s Mental Capacity,Restraint <strong>and</strong> Deprivation of Libertiesprotocol to ensure the LD patient’s needsare covered within them.<strong>July</strong> <strong>2012</strong>Implementation of Charter within agreedtimeframe.June <strong>2012</strong> Safeguarding site to be reviewed.Designated site for LD to be established.Gary EtheridgeDeputy Director of NursingProduced in May <strong>2012</strong>Reviewed in June <strong>2012</strong>11
EXECUTIVE SUMMARYTITLE:Maternity Update – May <strong>2012</strong>BOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong>DATE:The purpose of this report is to provide the <strong>Trust</strong><strong>Board</strong> with an update on the monthly performancefor maternity services.The key areas to note are:• In May the <strong>Trust</strong> went over the cap on sixoccasions however the units remainedclinically safe. Two women were divertedin the month.• Average of 78% of women were seen by amidwife in triage within 15 minutes <strong>and</strong>91% within 30 minutes.• 99% of women in May were seen by adoctor in the OAU.• Data capture in OAU out of hours hasfound to be calculated incorrectly this isbeing rectified.• 100% women received pethidine within 15minutes of the request <strong>and</strong> 91% womenreceived an epidural with 30 mins of therequest.• 2 SIs were reported in May.• 75% of the grade1 LSCS were performedwithin 30 mins from decision, at Queen’s<strong>and</strong> 100% at KGH. The Clinical Director isundertaking an audit of the records toascertain if the records have been gradedappropriately• The cap on the number of births has beenremoved from BHRUT with effect fromJune <strong>2012</strong>.• The escalation process continues in linewith other maternity units <strong>and</strong> inconjunction with the PAN Londonescalation policy.• Weekly reporting to NELC has nowceased.• Monthly reporting will continue.• A draft BHRUT assurance framework hasbeen developed <strong>and</strong> under discussion withNELC.□ PBE ……………..….. □STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT……………………□ QUALITY & STRATEGY…………..………….....……□ CHARITABLE FUNDS………………………………...…□ TRUST BOARD……………………………….………….□ REMUNERATION………………………………….…...□ OTHER …………………………..…….(please specify)2. DECISION REQUIRED: CATEGORY:The <strong>Board</strong> are asked to note the content of the □ NATIONAL TARGET □ RMS
eport.□ CQC REGISTRATION □ HEALTH &SAFETY□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROMCOMMISSIONERS□ CORPORATE OBJECTIVE……………………………....□ OTHER …………………….. (pleasespecify)AUTHOR/PRESENTER: W MatthewsPresenter: D WheelerDATE: 27 th June <strong>2012</strong>3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:N/A4. DELIVERABLESMaternity Improvement plan.5. KEY PERFORMANCE INDICATORS91% of women seen within 30 minutes of arrival within Triage99% of women seen within an hour of referral to an obstetrician within the obstetric assessmentunit.100% of women received pethidine within st<strong>and</strong>ard.AGREED AT ______________________MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
Maternity Services Monthly Performance Report<strong>Trust</strong> Name<strong>Barking</strong>, <strong>Havering</strong> & <strong>Redbridge</strong> University HospitalsNHS <strong>Trust</strong>Reporting monthThis report covers the period:1 st May to 31 st May <strong>2012</strong>Completed byMr Dele OlorunsholaClinical Director of Obstetrics, Gynaecology <strong>and</strong>Sexual HealthReviewed byDeborah WheelerDirector of NursingNeill MoloneyDirector of Planning & PerformanceContact Details<strong>Barking</strong>, <strong>Havering</strong> & <strong>Redbridge</strong> University HospitalsNHS <strong>Trust</strong>1st Floor Green ZoneMaternity Services, Queens HospitalRom Valley Way, Romford, RM7 0AGTel: 01708 435 000 x 3894A monthly report will be provided to; monitor the progress made against the maternity servicesimprovement plan, provide assurance that the safety <strong>and</strong> quality of maternity services areimproving within BHRUT. It will summarise the themes <strong>and</strong> actions that have arisen from theweekly analysis of activity within the unit.Monthly maternity report May <strong>2012</strong> v1.1. DOPage 1 of 9Compiled by C Frisby 13.06.<strong>2012</strong>1
1. IntroductionThe purpose of this report is to summarise the progress made In May <strong>2012</strong> against the maternityservice improvement plan <strong>and</strong> the KPIs agreed with the commissioning team within ONEL.2. Total Number of Births at BHRUT for May <strong>2012</strong>KGHQueensElectiveLSCSEmergencyLSCSOtherTotalEmergencyLSCSElectiveLSCSOtherTotal5 7 154 166 112 45 464 6213. Weekly Activity (excluding elective LSCS)Weekly Delivery Activity KGH/QHTotal Deliveries18016014012010080604020005/09/201112/09/201119/09/201126/09/201103/10/201110/10/201117/10/201124/10/201131/10/201107/11/201114/11/201121/11/201128/11/201105/12/201112/12/201119/12/201126/12/201102/01/<strong>2012</strong>09/01/<strong>2012</strong>16/01/<strong>2012</strong>23/01/<strong>2012</strong>30/01/<strong>2012</strong>06/02/<strong>2012</strong>13/02/<strong>2012</strong>20/02/<strong>2012</strong>27/02/<strong>2012</strong>05/03/<strong>2012</strong>12/03/<strong>2012</strong>19/03/<strong>2012</strong>26/03/<strong>2012</strong>02/04/<strong>2012</strong>09/04/<strong>2012</strong>16/04/<strong>2012</strong>23/04/<strong>2012</strong>30/04/<strong>2012</strong>07/05/<strong>2012</strong>14/05/<strong>2012</strong>21/05/<strong>2012</strong>28/05/<strong>2012</strong>Queens Deliveries(optimum 140)KGH DeliveriesWeek ending (optimum 49) DateOptimum Queens4. EscalationsAs part of the capacity management plan the escalation process has been reviewed. The status goesto ‘red’ when there are 15 deliveries or equivalent of labouring women at Queen’s <strong>and</strong> 5 at KGH.Site Red Amber Green EscalationsQH 17 31 31 2KGH 16 0 31 1Monthly maternity report May <strong>2012</strong> v1.1. DOPage 2 of 9Compiled by C Frisby 13.06.<strong>2012</strong>2
4.1 CappingThe capping is currently set to 20 births for Queen’s Hospital <strong>and</strong> 7 births for King George Hospital(optimum delivery rate) 27 in total. This is an accrued total which is calculated from 6pm of day one to5:59pm of day two. These figures are calculated excluding elective caesarean sections.In May <strong>2012</strong> the <strong>Trust</strong> went over the cap on 6 occasions in total.DateNo of BirthstotalNo. abovecap01/05/<strong>2012</strong> to 02/05/<strong>2012</strong> 29 203/05/<strong>2012</strong> to 04/05/<strong>2012</strong> 29 204/05/<strong>2012</strong> to 05/05/<strong>2012</strong> 28 111/05/<strong>2012</strong> to 12/05/<strong>2012</strong> 28 122/05/<strong>2012</strong> to 23/05/<strong>2012</strong> 28 128/05/<strong>2012</strong> to 29/05/<strong>2012</strong> 29 2The maternity unit remained clinically safe on these six occasions4.2 DivertsThere were two diverts in May, one to Homerton Hospital <strong>and</strong> one to Basildon.5.0 TriageThe agreed st<strong>and</strong>ard is that 98% of women will be seen by a midwife within 15 minutes of arrival attriage. In May, overall 76% of women were seen within 15 minutes of arrival <strong>and</strong> 91% were seenwithin 30 minutes.Triage - % of Patients Seen within 15 Minutes of Arrival110100908070605040302010001/03/<strong>2012</strong>06/03/<strong>2012</strong>11/03/<strong>2012</strong>16/03/<strong>2012</strong>21/03/<strong>2012</strong>26/03/<strong>2012</strong>31/03/<strong>2012</strong>05/04/<strong>2012</strong>10/04/<strong>2012</strong>15/04/<strong>2012</strong>20/04/<strong>2012</strong>Number of Patients25/04/<strong>2012</strong>30/04/<strong>2012</strong>05/05/<strong>2012</strong>10/05/<strong>2012</strong>15/05/<strong>2012</strong>20/05/<strong>2012</strong>25/05/<strong>2012</strong>30/05/<strong>2012</strong>Day% of patients Seen within 15 minutesMonthly maternity report May <strong>2012</strong> v1.1. DOPage 3 of 9Compiled by C Frisby 13.06.<strong>2012</strong>3
Triage WaitingtimesNumber ofWomen% of TotalwomenUp to 15 minutes 888 76%15-30 minutes 169 15%31-60 minutes 85 7%61 minutes + 21 2%6.0 OAU ActivityIt has been agreed that 98% of women should be seen by an obstetrician, where this is deemedclinically appropriate, within 1 hour of their arrival to the Obstetric Assessment Unit (OAU) in hours.The <strong>Trust</strong> average for May <strong>2012</strong> was 99%.% of Patients seen within 1 hour on OAU by an Obstetrician110100908070605040302010001/03/<strong>2012</strong>06/03/<strong>2012</strong>11/03/<strong>2012</strong>16/03/<strong>2012</strong>21/03/<strong>2012</strong>26/03/<strong>2012</strong>31/03/<strong>2012</strong>% of patients seen05/04/<strong>2012</strong>10/04/<strong>2012</strong>15/04/<strong>2012</strong>20/04/<strong>2012</strong>25/04/<strong>2012</strong>30/04/<strong>2012</strong>05/05/<strong>2012</strong>10/05/<strong>2012</strong>15/05/<strong>2012</strong>20/05/<strong>2012</strong>25/05/<strong>2012</strong>30/05/<strong>2012</strong>% of Patients seen within 1HourDateMonthly maternity report May <strong>2012</strong> v1.1. DOPage 4 of 9Compiled by C Frisby 13.06.<strong>2012</strong>4
7.0 Out of Hours OAU98% of patients attending the Out of Hours OAU should be seen by an Obstetrician, where itis deemed clinically appropriate, within one hour of their arrival to this unit.The Out of Hours OAU is currently under review by Clinical Fellows <strong>and</strong> department leadsowing to consistently higher waiting times than it’s counterparts. This OAU is governed by thesame st<strong>and</strong>ard as the main OAU, however, the data collection for this area reflects a twentyfourhour period rather than 8pm to 8am when the main OAU is closed. Until the data isrefreshed a % is not available. Several changes are being piloted in this area to achieveshorter waiting times for clients. Changes have already taken place in OAU in hours whichhas improved waiting times. Once the planning phase is complete for out of hours OAU, themost appropriate pathway will be implemented.% of Patients seen within 1 Hour of Referral12010080604020001/03/<strong>2012</strong>08/03/<strong>2012</strong>15/03/<strong>2012</strong>22/03/<strong>2012</strong>29/03/<strong>2012</strong>05/04/<strong>2012</strong>12/04/<strong>2012</strong>19/04/<strong>2012</strong>26/04/<strong>2012</strong>03/05/<strong>2012</strong>10/05/<strong>2012</strong>17/05/<strong>2012</strong>24/05/<strong>2012</strong>31/05/<strong>2012</strong>% of Patients seen within 1Hour of Referral Target8.0 Analgesia AuditSome additional information is at the base of this report, titled ‘Additional Information’ <strong>and</strong>contains some references to analgesia administrations.On a weekly basis, as part of visible leadership, an audit is undertaken to monitor theamount of time women are waiting for their analgesia. The agreed st<strong>and</strong>ard is:• If a woman requests pethidine she should receive this within 15 minutes of the request.The <strong>Trust</strong> achieved 100% against this st<strong>and</strong>ard in May <strong>2012</strong> of those cases audited.• If a woman requests an epidural she should receive this within 30 minutes of therequest. The <strong>Trust</strong> achieved 91% against this st<strong>and</strong>ard for May <strong>2012</strong> of those casesaudited.Monthly maternity report May <strong>2012</strong> v1.1. DOPage 5 of 9Compiled by C Frisby 13.06.<strong>2012</strong>5
9. Serious Untoward Incidents ReportedSUI’s are reported on a weekly basis, in retrospect, therefore the information below issummarised weekly but may include overlapping information from post <strong>and</strong> priormonth.ReportNo of Date of Details ofWeek Commencing Incidents Incident Incident7 th May 014 th May 021 st May 028 th May 2 06/05/<strong>2012</strong> Unexpectedadmission to theneonatal intensivecare unit – infant>37 completedweeks gestationthat have a suddenor unexpectedcollapse followingdelivery.28 th May 16/05/<strong>2012</strong> Unexpectedadmission to theneonatal intensivecare unit – infant>37 completedweeks gestationthat have a suddenor unexpectedcollapse followingdelivery.Site ofIncidentKing GeorgeHospitalKing GeorgeHospitalMonthly maternity report May <strong>2012</strong> v1.1. DOPage 6 of 9Compiled by C Frisby 13.06.<strong>2012</strong>6
Caesarean Deliveries including Elective ActivitySome additional information is at the base of this report, titled ‘Additional Information’<strong>and</strong> contains some references to anaesthetics.When a decision is made to perform an emergency LSCS, the timing for this is dictated by theacuity of each case which is graded from 1-4.Grade 1Caesarean section is considered as urgent <strong>and</strong> has an immediate threat to the life of the woman<strong>and</strong> foetus. To be performed within 30 minutes.At Queen’s hospital 79% of the audited grade 1 C/S were performed within 30 minutes.At KGH, the average based on the notes audited was 100%.Grade 2Caesarean section is considered urgent with maternal or foetal compromise which is notimmediately life threatening. To be performed within 60 minutesAt Queen’s hospital of 78% the audited grade 2 emergency C/S were performed within 60 minutes.At KGH the average was for the notes audited 100%Grade 3 & 4Caesarean section is an emergency with no maternal or foetal compromise, but requires earlydelivery. To be performed at a time to suit the mother <strong>and</strong> the department.At Queen’s hospital, 100% of the audited grade 3/4 emergency C/S were performed within time.At KGH hospital 100% of the audited grade 3/4 emergency C/S were performed within time.Top 3 reasons for delays for all grades of LSCS like the previous month were:1. Clinicians required elsewhere due to busy Labour Ward <strong>and</strong> theatres2. Theatre capacity3. Delayed consent (by mother)Monthly maternity report May <strong>2012</strong> v1.1. DOPage 7 of 9Compiled by C Frisby 13.06.<strong>2012</strong>7
Quarterly workforce report for May <strong>2012</strong>RecruitmentCurrently there are 16 midwives in the recruitment process that are due to qualify in Septemberthat have been offered posts at BHRUT.6 midwives commenced employment in May <strong>and</strong> are currently on their induction programme2 nurses have been appointed <strong>and</strong> remain within the recruitment process.With have further interviews in June for the remaining MCA vacanciesWe interviewed for a Midwifery Placement Facilitator <strong>and</strong> successfully appointed, however shedeclined to take the post. This post was re-advertised <strong>and</strong> has already been shortlistedNew starters in May6 midwivesAdvertsWe are going out to advert for an 8a patient satisfaction/ lead midwife in BereavementThere is 2.74WTE vacancy in b<strong>and</strong> 7; we are currently waiting for the review of the JD with theA4C panelLeavers9 midwives left the trust, some of which have returned to their own country <strong>and</strong> others who havegone to work in a surrounding low risk unit. Discussions took place with these midwives regardingBHRUT co-located birthing centre opening in the autumn however the midwives could not beretainedHow are we maintaining the 1:29 midwife to birth ratioWithin the wards the staffing is done on a monthly basis <strong>and</strong> temporary staff are booked for thevacant shifts. Every day this is reviewed <strong>and</strong> amended.% of bank <strong>and</strong> agencyThe % of bank <strong>and</strong> agency currently used within the month of May is:Midwife• 28.47 WTE = 8.9 % bank- this is an increase of 1%, due the increased number of midwivesthat left the trust in May.• 7.14 WTE = 2% agency- this is a reduction of 0.9 % on last monthNurses• 0.78WTE = 2% agency• 2.8 WTE = 10% bankMaternity Support Workers• 16.89 WTE = 22% bankMonthly maternity report May <strong>2012</strong> v1.1. DOPage 8 of 9Compiled by C Frisby 13.06.<strong>2012</strong>8
Medical recruitmentWe have 2 Consultant vacancies, one left in June <strong>and</strong> one in March <strong>and</strong> we have 2 full timelocums covering these posts.Balanced ScorecardThe balanced scorecard for May <strong>2012</strong> is attached as Appendix 1. Please note that the scorecard isunder review <strong>and</strong> not all information was available at the time of submission of this report.Additional InformationDr R Pilling, has as part of his Clinical Fellow duties, has undertaken an audit into the impact of asecond anaesthetist being available out of hours. His conclusions are below.Conclusions from audit undertaken to ascertain the impact of a second anaesthetist beingavailable out of hours: Clearly extremely busy maternity unit Unpredictable nature of obstetric shifts 40% of shifts well above the average number of anaesthetic interventions required. Increased opening of 2nd theatre since the increased anaesthetic presence Several occasions of a few minutes overlap time Are the indications for a 2nd theatre becoming more relaxed? Or…are we now more compliant with target times for emergency LSCS? Sharing of the workload has definately eased the pressure on the labour ward anaesthetist What evidence do we have of an improvement in patient care?Conclusions from audit in relation to epidural waiting times…. Clear benefit from 2nd anaesthetist Improved epidural waiting times More time available to take an active role on maternity HDU Improved working conditions for duty anaesthetistRecommendations from same audit… Definate need for 2nd anaesthetist on labour ward Needs a separate audit of the indications for the use of 2 theatres Better epidural data(should improve with the imminent introduction of computerised data collection) Reaudit to ensure maintainance of high st<strong>and</strong>ardsMonthly maternity report May <strong>2012</strong> v1.1. DOPage 9 of 9Compiled by C Frisby 13.06.<strong>2012</strong>9
EXECUTIVE SUMMARYTITLE:Milestone Tracker/Composite PlanBOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:Attached is the monthly progress report forperformance against the requirements included in theMilestone Tracker. There are a number of process <strong>and</strong>outcome requirements included in the milestonetracker under the following headings:• Corporate Governance <strong>and</strong> Assurance• Service Quality <strong>and</strong> Performance• Finance, Productivity <strong>and</strong> ReconfigurationEach criterion is RAG rated Green, Amber/Green,Amber/Red or Red. Included in the report is the <strong>Trust</strong>RAG rating.□ TEC ……………..….. □ STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT ………….……..….□ QUALITY & SAFETY …………..………….....……□ WORKFORCE□ CHARITABLE FUNDS ………………………………...… TRUST BOARD ……………………………….………….□ REMUNERATION ………………………………….…...□ OTHER …………………………..……. (please specify)Whilst there has been considerable progress againstthe requirements there are a number of areas whichhave been rated as RED or Amber/Red• Complaints• Emergency access st<strong>and</strong>ard• Cancer performance• CIP Plan <strong>and</strong> deliveryThis report only provides a summary of the document.The attachments, providing detailed progress <strong>and</strong>evidence of compliance, can be provided to <strong>Trust</strong><strong>Board</strong> members if requested.In addition to the May report the <strong>Trust</strong> has now agreeda revised Composite Plan with the cluster <strong>and</strong> NHSLondon. This is report is also attached.2. DECISION REQUIRED: CATEGORY:Report for noting. NATIONAL TARGET □ CNST CQC REGISTRATION □ HEALTH & SAFETY ASSURANCE FRAMEWORK CQUIN/TARGET FROM COMMISSIONERS CORPORATE OBJECTIVE ……………………………....□ OTHER …………………….. (please specify)AUTHOR/PRESENTER: Neill MoloneyDATE: 28 June <strong>2012</strong>3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:The milestone tracker highlights the importance of delivering the £23m cost reduction within the QIPP programme.4. DELIVERABLES
There are a number of process <strong>and</strong> outcome requirements included in the milestone tracker under the followingheadings:• Corporate Governance <strong>and</strong> Assurance• Service Quality <strong>and</strong> Performance• Finance, Productivity <strong>and</strong> Reconfiguration•5. KEY PERFORMANCE INDICATORSIncluded in the milestone tracker report.AGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
BHRUT TFA: Corporate Governance <strong>and</strong> Assurance -FF0000 WORKING DRAFT (20 June <strong>2012</strong>)Itemno.Activities <strong>and</strong> deliverablesBHRUT / NELC/JOINTdeliverableBHRUT accountable DirectorLeadNELC Director LeadComments:(1) Dependencies(2) RisksRAG rating Start date End date Apr‐12 May‐12 Jun‐12 Jul‐12 Aug‐12 Sep‐12 Oct‐12 Nov‐12 Dec‐12 Jan‐13 Feb‐13 Mar‐13Key# = transitional financial support <strong>and</strong> / or consultancy support provided to BHR to support delivery1 leadership, <strong>Board</strong> Development <strong>and</strong> WorkforceLeadership <strong>and</strong> <strong>Board</strong> developmentStrengthen <strong>Board</strong> leadership <strong>and</strong> governanceNote: Averil Dongworth, Alwen Williams <strong>and</strong> NHS London to discuss <strong>and</strong> agree approach <strong>and</strong>milestonesBHRUT Averil Dongworth Alwen Williams‐ OD PlanOD Plan at leadership levels (<strong>Board</strong> level, senior management team <strong>and</strong> Senior Clinicians) withagreed deliverables / milestonesBHRUT Dorothy Hosein Helen BullersApr‐1201‐Dec‐12‐ Workforce Reduction PlanWorkforce reduction <strong>and</strong> transition plan (ahead of Workforce Strategy)BHRUT HRD Helen BullersDependency with CIPdeliveryMay‐12Jul‐12‐ Workforce Strategy<strong>Board</strong> approved workforce strategy <strong>and</strong> education <strong>and</strong> training plan from <strong>2012</strong>/13 to 2015/16. Thisneeds to have been reviewed with NELC <strong>and</strong> NHSL (link to LTFM & CIP)BHRUT HRD Helen BullersDependency withclincial strategy IBP /LTFMMay‐1201‐Dec‐12‐ National Workforce Assurance ToolBHRUT participates in National Workforce Assurance Tool <strong>and</strong> use data outputsMay‐12 OngoingBHRUT HRD Helen Bullers‐ Equality <strong>and</strong> Diversity Plan<strong>Board</strong> approved Equality <strong>and</strong> Diversity plan BHRUT HRD Helen Bullers May‐12 31‐Jul‐12‐ <strong>Board</strong> reportingWorkforce report to be provided to all <strong>Board</strong> meetings to include Workforce metrics, key risks <strong>and</strong>mitigating actions to support <strong>Board</strong> assurance.BHRUT HRD Helen BullersApr‐12 Ongoing2 Clinical governance <strong>and</strong> risk managementBHRUT clinical improvement planHigh‐level approach to the development of an improvement strategy clearly definedBHRUT MD Caroline Alex<strong>and</strong>er01‐Aug‐12‐ Improvement Strategy is finalised following internal engagement <strong>and</strong> OD process.BHRUT MD Caroline Alex<strong>and</strong>erBuilds on learningfrom the developmentof scorecards31‐Oct‐12BHRT corporate <strong>and</strong> directorate quality <strong>and</strong> safety scorecard <strong>and</strong> improvement trajectories to beagreed with NELC Director of Quality, evidence of escalation to <strong>Board</strong> <strong>and</strong> regular review via CQRM.RAG ratings <strong>and</strong> improvement trajectories to be monitored for all 11 directoratesNote: metrics to be included <strong>and</strong> not limited to those in appendix 2BHRUT MD Caroline Alex<strong>and</strong>erApr‐12‐ 1st iteration of scorecards BHRUT MD Caroline Alex<strong>and</strong>er May‐12 01‐Jul‐12‐ Scorecards finalised BHRUT MD Caroline Alex<strong>and</strong>er 01‐Jul 01‐Oct‐12
BHRUT TFA: Service Quality <strong>and</strong> Performance - FF0000WORKING DRAFT (20 June <strong>2012</strong>)Itemno.Activities <strong>and</strong> deliverablesBHRUT / NELC/JOINTdeliverableBHRUT accountable DirectorLeadNELC Director LeadComments:(1) Dependencies(2) RisksRAG rating Start date End date Apr‐12 May‐12 Jun‐12 Jul‐12 Aug‐12 Sep‐12 Oct‐12 Nov‐12 Dec‐12 Jan‐13 Feb‐13 Mar‐13Key# = transitional financial support <strong>and</strong> / or consultancy support provided to BHR to support delivery1 Emergency CareBHRUT Cathy Geddes Helen Brown OngoingMonth on month improvement against emergency access st<strong>and</strong>ards‐ Trajectory for improvement to 95% to be agreed. Evidence of plans in place to sustain BHRUT Cathy Geddes Helen Brown Jun‐12improvement.‐ Clear assessment of risk <strong>and</strong> mitigations of performance deteriorating BHRUT Cathy Geddes Helen Brown Jun‐122 MaternityEliminate 60 minute plus ambulance h<strong>and</strong>overs monitored via the hospital alert system(HAS)Month on month improvement to eliminate all mixed sex accommodation breaches on asustainable basis.BHRUT Cathy Geddes Helen Brown Dependency ondelivery of LOS <strong>and</strong>DTOCsBHRUT Cathy Geddes Helen Brown Links to emergencycare st<strong>and</strong>ardsimprovementOngoingOngoingEscalation <strong>and</strong> divertion approach to conform with policy agreed with all providers BHRUT Cathy Geddes Caroline Alex<strong>and</strong>er Jun‐12 OngoingReduction of 2,100 births being delivered across all sites including a reduction in bookingsin September <strong>2012</strong> <strong>and</strong> deliveries by 2013/14NELC Cathy Geddes Helen Brown May‐12 Ongoing3 Planned CareNote: Quality <strong>and</strong> Safety metrics to be monitored through directorate scorecard <strong>and</strong>improvement process. Exception reporting through CQRMContinue to sustain the aggregated position against the admitted, non‐admitted <strong>and</strong>incomplete RTT pathways. Maximum target timeframe for diagnostic is 6 weeksBHRUT Cathy Geddes Helen Brown OngoingCancer – continue to meet cancer targets in line with national <strong>and</strong> contractual reportingst<strong>and</strong>ardsContinue to maintain or improve against all existing st<strong>and</strong>ards as outlined in NHSPerformance FrameworkBHRUT Cathy Geddes Helen Brown OngoingBHRUT Cathy Geddes Helen Brown OngoingAssurance meetingsKey BHRUT assurance meetings (tbc)External assurance Meetings
BHRUT TFA: Finance, Productivity, Reconfiguration -FF0000 WORKING DRAFT (20 June <strong>2012</strong>)Itemno.Activities <strong>and</strong> deliverablesBHRUT / NELC/ JOINTdeliverableBHRUT accountable DirectorLeadNELC Director LeadComments:(1) Dependencies(2) RisksRAG rating Start date End date Apr‐12 May‐12 Jun‐12 Jul‐12 Aug‐12 Sep‐12 Oct‐12 Nov‐12 Dec‐12 Jan‐13 Feb‐13 Mar‐13Key# = transitional financial support <strong>and</strong> / or consultancy support provided to BHR to support delivery1 FinanceFinancial performance <strong>2012</strong>/13: Delivery of CIP & Control TotalFinancial return surplus/deficit at month end is in‐line with or better than the trajectory in the annual BHRUT FD Stuart Saw <strong>Trust</strong> month 1 reporting only formallyplan (YTD <strong>and</strong> forecast outturn).available in month 2Apr‐12 OngoingGovernance <strong>and</strong> monitoring arrangements<strong>Board</strong> to agree, approve <strong>and</strong> sign‐off directorate budgets with the delegated budget holder. BHRUT FD Stuart Saw Dependent on CIP review Apr‐12 15‐Jun‐12An internal policy covering financial failure <strong>and</strong> escalation is produced. This is endorsed by the <strong>Board</strong><strong>and</strong> agreed with NHS London.BHRUT FD Stuart Saw Approved by BHRUT <strong>Board</strong> in May <strong>and</strong> finalrevisions to be made following NHS LondonfeedbackBudget holders are held accountable for adverse performance; they produce monthly variance analysisBHRUT FD Stuart Saw Apr‐12 Ongoingreports which clearly sets out favourable <strong>and</strong> adverse variances from budget (YTD <strong>and</strong> FOT), thecausality of those variances <strong>and</strong> mitigating actions being taken. The reports are evidenced <strong>and</strong>presented to, reviewed <strong>and</strong> challenged by the <strong>Board</strong>; recovery plans agreed with budget holders whereapplicable.Apr‐12Jun‐122 Productivity‐ CIP Plan & delivery# BHRUT to develop a robust CIP plan for <strong>2012</strong>/13. min 80% green rated <strong>and</strong> min 80% recurrent.Note: definition of RAG ratings to be agreedBHRUT FD Stuart Saw 1.05.<strong>2012</strong> 29.05.<strong>2012</strong># Interim review of CIPs to be completed by external consultants <strong>and</strong> mitigating actions identified. NELC BHRUT FD Stuart Saw 18.05.<strong>2012</strong>to review <strong>and</strong> sign‐off refreshed plans.# Delivery of CIP Plan. Financial return CIP at month end is in‐line with or better than the annual plantrajectory (YTD <strong>and</strong> forecast outturn).BHRUT FD Stuart Saw Apr‐12 Ongoing‐ Commissioner QIPP Delivery‐Clearly quantify acute activity reduction embedded into BHRUT contract & associated QIPP schemes. NELC Conor Burke / Helen Brown May‐12 Jun‐12Ensure green rated Commissioner delivery plans in place with trajectories for delivery: i) unplannedcare 2) planned care‐ track <strong>and</strong> report delivery against trajectory as outlined in delivery plans 1) unplanned care 2) planned NELC Conor Burke / Helen Brown May‐12 ongoingcareClear delivery mechanism in place between CCGs <strong>and</strong> BHRT to support delivery NELC Conor Burke / Helen Brown Jul‐12‐ LOS improvement & deliveryAgree annual plan for delivery of LOS improvement/ bed reduction (BHR internal opportunity) BHRUT Cathy Geddes Helen Brown Dependency on LTFM <strong>and</strong> H4NEL Jun‐12including monthly phasing plan‐ Deliver to phased programme of LOS improvement/ bed reduction BHRUT Cathy Geddes Helen Brown 1.06.<strong>2012</strong> OngoingIdentify baseline <strong>and</strong> agree a delivery plan <strong>and</strong> improvement trajectory with NELFT <strong>and</strong> other partners NELCHeather Mullins / Helento support reduction in DTOC health delays (external factors).Brown‐ Ongoing delivery of reduction in DTOC health delays NELC Heather Mullins / HelenBrownDependency on LTFM <strong>and</strong> H4NEL15.06.<strong>2012</strong> OngoingJun‐12Develop plan for reduction in first to follow‐up ratios BHRUT Cathy Geddes Will Huxter / Helen Brown Dependency on LTFM <strong>and</strong> H4NEL 29.06.<strong>2012</strong>‐ Deliver plan for reduction in first to follow‐up ratios BHRUT Cathy Geddes Will Huxter / Helen Brown Dependency on LTFM <strong>and</strong> H4NEL 29.06.<strong>2012</strong> Ongoing3 Reconfiguration‐ Clinical Strategy <strong>and</strong> LTFM# Development of LTFM Model: base case / gap analysis BHRUT FD Stuart Saw LTFM dependent on Health4NEL <strong>and</strong>Jun‐12 15.06.<strong>2012</strong>reconfiguration strategy# Detailed plan outlining schedule of events supporting delivery of LTFM <strong>and</strong> clearly describing process BHRUT 29/06/<strong>2012</strong><strong>and</strong> deliverables (including clincial service review)# LTFM <strong>and</strong> Clinical Service Review: scenarios for viablity, timeline to deliver, estimate of transitional BHRUT FD Stuart Saw LTFM dependent on Health4NEL <strong>and</strong>Jul‐12 21/09/<strong>2012</strong>support required, multi‐year productivity programmereconfiguration strategy# Ensure jointly agreed Transitional Financial Plan NELC / BHRUT tbc 3.09.<strong>2012</strong>‐ Recofiguration planningRefresh Health4 NEL dem<strong>and</strong> <strong>and</strong> capacity model ‐ jointly agreed BHR <strong>and</strong> Commissioner position BHRUT Nick Hulme Geoff Sanford Dependency with LTFM <strong>and</strong> LOSimprovement planOutline Business Case to BHRUT <strong>Trust</strong> <strong>Board</strong> BHRUT Nick Hulme Geoff Sanford see Appendix for current draft plan to bereviewed by Nick Hulme / Rob Royce06/07/<strong>2012</strong>01/08/<strong>2012</strong>Outline Business Case to NHS L CIC BHRUT 27/09/<strong>2012</strong>Clinical Strategy, LTFM <strong>and</strong> Reconfiguration 'checkpoint'Review alignment of outputs from clincial Strategy / LTFM work with H4N OBC <strong>and</strong> whether any BHRUT / NELC / NHS L 10/10/<strong>2012</strong>revisions to the approach are required. Review readiness to initate PFI negotiations <strong>and</strong> capital funding‐ System‐wide strategic vision for out of hospital services including future of King George'sDevelop 'integrated care' business case including options for reconfiguration of out of hospital services NELC / CCGs Heather Mullin / Helen Brown Jul‐12 Oct‐12(including future vision for KGH), with clear linkages to BHRUT clinical strategy / LTFM <strong>and</strong> update CCGCSPs. Outputs to feed into Clinical Strategy <strong>and</strong> reconfiguration checkpoint in mid October.OBC / PCBC for proposed changes 31/10/<strong>2012</strong>Assurance meetingsKey BHRUT assurance meetingsBHRUT Financial Recovery Programme <strong>Board</strong> (monthly) BHRUT Averil Dongworth Apr‐12 OngoingExternal assurance MeetingsFinance <strong>and</strong> LTFM Steering Group JOINT BHRUT & NELC FD Stuart Saw TBC‐ Appointment of steering group JOINT BHRUT & NELC FD Stuart Saw 11.05.<strong>2012</strong> 18.05.<strong>2012</strong>Reconfiguration Programme Exec JOINT BHRUT & NELC Nick Hulme Helen Brown / David ButcherCommissioner QIPP delivery NELC Nick Hulme Will Huxter
BHRUT TFA Appendix 1: Reconfiguration planning - subject to review by Nick Hulme FF0000- WORKING DRAFT (20 June <strong>2012</strong>)Reconfiguration planning ‐ First draft completed by Rob Royce <strong>and</strong> David Butcher subject to review by Nick HulmeItem no. Activities <strong>and</strong> deliverables BHRUT / NELC/ BHRUTJOINTdeliverableaccountableDirector LeadNELC Director Lead Comments:(1) Dependencies(2) RisksRAGratingStart date End date Apr‐12 May‐12 Jun‐12 Jul‐12 Aug‐12 Sep‐12 Oct‐12 Nov‐12 Dec‐12 Jan‐13 Feb‐13 Mar‐13Relocate KGH A&EPhase 1: Develop FBC for Estate changes that support Consolidation A&E <strong>and</strong> obstetric delvieries onto Queens HospitaTo be reviewed by NickHulme by 8 June <strong>2012</strong>.Timeframes <strong>and</strong> activitiesare subject to his review# Submit design brief for to HealthPlannersBHRUT Rob Royce David Butcher 26.04.<strong>2012</strong>[Complete?]# Confirm service map <strong>and</strong> productivityassumptionsBHRUT Rob Royce David Butcher 27.04.<strong>2012</strong>[Complete?]# Submit detailed plan to Catalyst for TVE BHRUT Rob Royce David Butcher 25.05.<strong>2012</strong>production# Agree architect's plan BHRUT Rob Royce David Butcher 31.05.<strong>2012</strong># Produce TVEs BHRUT Rob Royce David Butcher 20.07.<strong>2012</strong># Confirm capital cost estimates <strong>and</strong> nonfinanceBHRUT Rob Royce David Butcher 20.07.<strong>2012</strong>sections# Complete options appraisal BHRUT Rob Royce David Butcher 20.07.<strong>2012</strong># Produce forecast revenue assumptions BHRUT Rob Royce David Butcher 31.07.<strong>2012</strong><strong>and</strong> Queen's main case# Confirm Queen's main case approval BHRUT Rob Royce David Butcher 31.08.<strong>2012</strong>Confirm plans for SCBU expansion /include within Queens capital businesscaseBHRUT Rob Royce David ButcherPhase 2: Deliver estates changesTo be reviewed by NickHulme by 8 June <strong>2012</strong>.Timeframes <strong>and</strong> activitiesare subject to his reviewUndertake development of co‐locatedMLUUndertake SCBU expansionDevelop Sexual Health scheme design 30.06.<strong>2012</strong>Undertake Sexual Health capital work<strong>and</strong> relocationUndertake UCC <strong>and</strong> GP OOH works <strong>and</strong>relocationUndertake work for Paeditrician A & EexpansionUndertake work for Radiology A&EexpansionUndertake works for Majors/ MinorsAssesment Unit re‐designIncorporate other agree capital works(e.g. Cath Lab, Resus <strong>and</strong> CC expansion)31.10.<strong>2012</strong>31.01.201331/05.201331/05.201330.09.201330.09.2013Phase 3: Decision makingTo be reviewed by NickHulme by 8 June <strong>2012</strong>.Timeframes <strong>and</strong> activitiesare subject to his reviewAgree System Readiness Indicators NELC 30.09.<strong>2012</strong>obstetricsAgree System Readiness Indicators NELCemergency care pathwayConfirmation of Queen's readiness NELC / BHRUT 31.10.2013provided by BHRUT <strong>and</strong> CCG <strong>Board</strong>s <strong>and</strong>consoidation of obstetricsConfirmation of Queen's readinessprovided by BHRUT <strong>and</strong> CCG <strong>Board</strong>s <strong>and</strong>consolidation of a&e / acute elementsof emergency care pathway ontoQueen's Hospital siteNELC / BHRUT
BHRUT TFA Appendix 2: Metrics <strong>and</strong> improvement trajectories to be agreed <strong>and</strong> monitored during the CQRM programme (Metrics to be included <strong>and</strong> not limited to those listed below) FF0000- WORKING DRAFT (20 June <strong>2012</strong>)Metrics <strong>and</strong> improvement trajectories to be agreed <strong>and</strong> monitored during the CQRM programme ‐ Metrics to be included <strong>and</strong> not limited to those listed below14 June <strong>2012</strong>: Quality KPIs /trajectories agreed with the trust (as below) with exception of NICU awaiting confirmation from Director of Midwifery. Rag rate: AMBERNote: update provided by Eirlys Evans 14 June <strong>2012</strong>Activities <strong>and</strong> deliverables‐ Compliance with patient experience CQUIN targetFollowing review of plan in <strong>July</strong> meet agreed milestones for improvement‐ Complaints metrics being monitored:(1) Backlog of complaints resolved by September(2) Evidence of consistent reporting to board on complaints:· Numbers· Response rates· Themes <strong>and</strong> trend analysis· Actions/learning(3) Month on month reduction in the number of serious complaintsBHRUT / NELC/JOINT deliverableBHRUT accountable DirectorLeadBHRUT ND Caroline Alex<strong>and</strong>erBHRUT ND Caroline Alex<strong>and</strong>erNELC Director Lead Progress update RAGTrajectories have now been agreed:No overdue complaints more than 3 months oldby September <strong>2012</strong>. 80% within 30 days *(Review to aim for 25 days.)Trajectory for responses within agreedtimescales:April complaints target 60%May complaints target 70%June complaints target 80%Then minimum 80% sustained monthlyAmberRED‐ Serious incidents being monitored, investigated <strong>and</strong> improvement in staff knowledge/awareness. Compliance with:(1) agreed CQUIN (timeliness of reporting <strong>and</strong> quality or reports) target(2) Backlog completed by end of <strong>July</strong>‐ Never events no repeated themes based on last year’s cases. Never events reported to NELCthrough SI reporting‐ HCAI rates monitored <strong>and</strong> reported daily to NELC. Participation in HCAI peer review.Completion of NELC site visits.Key metrics to be monitored:(1) MRSA <strong>and</strong> Cdiff ‐ meet agreed annual targets/trajectory(2) Bed closures – reduced in relation to last year’s monthly rates(3) Annual infection control plan meets expected milestones <strong>and</strong> embeds the learning from theHCAI peer review processBHRUT MD Caroline Alex<strong>and</strong>erBHRUT MD Caroline Alex<strong>and</strong>erBHRUT DN Caroline Alex<strong>and</strong>erFurther assurance requested on status ofmaternity SI backlogNo Never Events reported.<strong>Trust</strong> are above trajectory for MRSA objective.Currently 2 cases (1 in April & 1 in May) againstannual objective of 7 cases.C.diff current position is 15 against an annualobjective of 59.Ward closures <strong>and</strong> bed days lost are morethan in the same period 2011 i.e. 9 wardsclosed ,195 bed days lost April <strong>2012</strong> comparedto 0 in 2011May 3 wards closed 116 bed days lost anincrease of 32 bed days lost for same periodlast year ( 84).Red/AmberGreenRED‐ Hospital acquired pressure monitored <strong>and</strong> reported to NELC. Key metrics to be monitored:(1) Month on month reduction in grade 3 <strong>and</strong> 4 pressure ulcers(2) Reporting on safety thermometer CQUIN achieved(3) Actions agreed at June CQRM following review of trends <strong>and</strong> root causes are fullyimplemented according to the agreed milestones‐ Falls monitored <strong>and</strong> reported to NELC. Key metrics to be monitored include:(1) Month on month reduction in falls resulting in harm(2) Actions agreed at June CQRM following review of trends <strong>and</strong> root causes are fullyimplemented according to the agreed milestones(3) Reporting on safety thermometer CQUIN achieved‐ Falls resulting in fractures achieve reduction‐ Safeguarding children <strong>and</strong> adults. Key metrics to be monitored:(1) Training requirements met for safeguarding children at levels 1, 2 <strong>and</strong> 3 <strong>and</strong> an upwardtrajectory in safeguarding adults training(2) Implementation of annual safeguarding plan according to key milestones(3) Consistent attendance at LSCBs <strong>and</strong> SABs by senior leaderBHRUT DN Caroline Alex<strong>and</strong>erBHRUT DN Caroline Alex<strong>and</strong>erBHRUT DN Caroline Alex<strong>and</strong>erBHRUT DN Caroline Alex<strong>and</strong>erTrajectory AgreedZero grade 4s by end of Sept30% reduction of grade 3s by September <strong>and</strong>performance maintainedCurrent position since April <strong>2012</strong>:2 grade 4 <strong>and</strong> 8 grade 3 .Current position:April 2 severe harm. 1 deathMay 1 severe harm.More Detail on action plan required.Implementing Safety Themometer (CQUIN) formonitoring fallsOFSTED CQC report will be issued on 22 June<strong>2012</strong> (to be updated following this beingissued)REDREDAmberAmber
BHRUT TFA -FF0000FINAL WORKING DRAFT (18 May <strong>2012</strong>)BHRUT: TFADate of draft: 18 May <strong>2012</strong>TFA focus areaAuthors <strong>and</strong> reviewersStage of draftSign‐off stage(1) Finance, Productivity, Reconfiguration Section Reviewer Role <strong>and</strong> organisation Input receivedMilestone planFinance Stuart Saw NELC 11.05.<strong>2012</strong>Will Huxter NELC 11.05.<strong>2012</strong>Dave Wragg FD BHRUT 11.05.<strong>2012</strong>Neil Moloney Director of Planning <strong>and</strong> Performance (BHRUT) 11.05.<strong>2012</strong>Productivity Heather Mullins NELC 02.05.<strong>2012</strong>Nick Hulme BHRUT 18.05.<strong>2012</strong>Cathy Geddes Chief Operating Officer (BHRUT) 18.05.<strong>2012</strong>Reconfiguration Geof Sanford NELC 15.05.<strong>2012</strong>(2) Service quality <strong>and</strong> performanceMilestone planQualityCaroline Alex<strong>and</strong>er 17.05.<strong>2012</strong>Eirlys Evans Deputy Director of Nursing (NELC) 14.05.<strong>2012</strong>Christina McKenzie External contractor (NELC) 14.05.<strong>2012</strong>Helen Bullers Director of HR (NELC) 15.05.<strong>2012</strong>Deborah Wheeler Director of Nursing (BHRUT) 17.05.<strong>2012</strong>(3) Corporate Governance <strong>and</strong> AssuranceMilestone planCorporateGovernance <strong>and</strong>AssuranceHelen Brown Director of Performance <strong>and</strong> Delivery (NELC) 17.05.<strong>2012</strong>Caroline Alex<strong>and</strong>er Director of Nursing <strong>and</strong> Quality (NELC) 17.05.<strong>2012</strong>Alwen Williams CEO (NELC) 17.05.<strong>2012</strong>Averil Dongworth CEO (BHRUT) 17.05.<strong>2012</strong>
EXECUTIVE SUMMARYTITLE:BOARD/GROUP/COMMITTEE:Finance Report – Month Two (May) <strong>2012</strong>/131. KEY ISSUES: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong>DATE:• Year to date deficit of (£10.9m) (excludingimpairments & IFRS), an adverse variance of£2.4m against profiled budget• Deficit in Month Two of (£3.2m) (excludingimpairments & IFRS), an adverse variance of(£1.7m) against profiled budget for the Month.• The adverse variance to date is mainly related toa QIPP/Cost Reduction shortfall of (£1.6m) –partly related to unidentified schemes of (£0.6m).• In addition there is a shortfall against incometargets of £0.8m. This includes £0.4m on centralPCT contract income, although it is anticipatedthat this shortfall will be recovered in futureMonths.• The risk assessment at Month Two of the QIPP/Cost reduction programme is £12.0m at Red,£2.4m Amber, £3.1m Green <strong>and</strong> £5.6m blue (i.e.implemented). The PMO team, with support fromErnst & Young are planning to report by the end ofthe week ending 22 nd June on the revisedprogramme for delivery of the full £23.1m target. Afurther update will be provided at the meeting.• There are also some emerging overspendings onpay described in the report, notably in theEmergency Care/Acute Medicine/NeurosciencesDirectorates, which require further action.□ S&SIB ………………□ EPB…...…………..□ FINANCE ……………□ AUDIT ….……..….□ CLINICAL GOVERNANCE …………..…......□ CHARITABLE FUNDS ……………………….TRUST BOARD ………………………………□ REMUNERATION ……………………………□ OTHER ………………………(please specify)CATEGORY:□ NATIONAL TARGET □ CNST□ STANDARDS FOR BETTER HEALTH□ ASSURANCE FRAMEWORK□ TARGET FROM COMMISSIONERS CORPORATE OBJECTIVE To monitor the<strong>Trust</strong>’s progress in achieving its financialturnaround, achieving control targets <strong>and</strong> meetingits statutory financial duties going forward.□ OTHER …………………….. (please specify)AUTHOR/PRESENTER:Alan Davies, Deputy Director of Finance / DavidWragg, Director of FinanceDATE:2. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:Set out under key issues3. ALTERNATIVES CONSIDERED/REASONS FOR REJECTION:N/A4. DELIVERABLES:N/A5. EVIDENCE :N/A6. RECOMMENDATION/ACTION REQUIRED:AGREED AT ______________________MEETING, ORREFERRED TO: ______________________DATE: ____________________________DATE: ____________________________REVIEW DATE _________________________(if applicable)1
1. EXECUTIVE SUMMARYMonthly I&E Run rate comparison.Monthly Net I&E PositionKey month 2 variances:2.00.0-2.0-4.0M01AprM02MayM03JunM04<strong>July</strong>M05AugM06SepM07OctM08NovM09DecM10JanM11FebM12Mar• Surgical Services (£587k adverse). Within this the majoradverse variances are: (£580k) unidentified QIPP/costreduction, mostly in Anaesthetics (£249k) which also has nonpayoverspending of (£67k – 5%, against an increase inTheatre activity of 9% against 11/12 average). There is also anoverspending on pay of (£96k), primarily a remnant of the backdatedsessions paid in M1 (as reported in M1).-6.0m£-8.0-10.0-12.0<strong>Trust</strong> I&E Summary<strong>2012</strong>/13 - Net I&E Deficit (-)/ Surplus<strong>2012</strong>/13 - Plan2011/12 - Net I&E Deficit (-)/ SurplusPrior 2 Yrs Average - Net I&E Deficit (-)/ Surplus*Febuary & March have been adjusted to show the underlying run rate position.<strong>2012</strong>/13 In Month (£'000) <strong>2012</strong>/13 Year to date (£'000)Actual £'000 Var £'000 Var % Actual £'000 Var £'000 Var %2011/12 YTDActual £'000(36,771) (508) -1.36% Income inc. Divisional (67,790) (803) -1.17% (64,736) (412,888)Expenditure24,951 (391) -1.59% - Pay 49,233 (305) -0.62% 47,625 290,89911,374 (63) -0.56% - Non-pay 22,287 113 0.50% 22,768 133,687(749) -100.00% - QIPP/Cost Reduction (1,428) (14,536)44 100.00% - Reserves (17) 1,193(446) (1,668) -78.89% EBITDA 3,730 (2,439) -189.03% 5,657 11,698ITDA1,186 22 1.79% - Depreciation 2,373 43 1.79% 2,319 14,494355 0.00% - Capital Dividends 711 0.00% 647 4,2632,093 (15) -0.70% - Net Interest 4,084 7 0.16% 3,425 23,8223,189 (1,661) -108.70% Net position 10,896 (2,389) -28.09% 12,048 54,277(2,005) Impairments (2,005) (2,005)1,184 (1,661) -348.06% Net position 8,891 (2,389) -36.75% 12,048 52,2722AnnualBudget £'000• Emergency Care, Acute Medicine & Neurosciences (£395kadverse), with overspending of £438k in May related to;slippage in ward closure programme (£110k); Emergency Carepay overspending in month of (£153k) related to RESETprogramme <strong>and</strong> additional staffing levels; <strong>and</strong> overspending inNeurosciences pay of (£102k) related to CIP slippage <strong>and</strong>increased Stroke Therapy staffing costs (linked to increasedactivity)• Diagnostics & Specialist Medicine (£605k adverse), including(£170k) unidentified QIPP/cost reduction. In addition: Pathologynon-pay overspending of (£136k) relating to reagents/chemicalson new MES contract; Radiology (£129k) on pay, relating toagency/locum cover for Radiologist vacancies <strong>and</strong> (£106k) onnon-pay, related to High Cost Devices, which will be offset bybilling to PCTs.• Women, Children & Support Services (£194k overspent), withan overspending of (£160k) in Month, related to SupportServices pay (£50k in month – Healthcare Records <strong>and</strong> MedicalSecretaries) , Womens pay (£75k in month – increased agencyMidwives), <strong>and</strong> Womens non-pay (£71k – increase in HIV drugexpenditure)• Corporate Directorates overall were £80k favourable YTD.Reserves show a negative variance of £541k, which primarilyrepresents the unidentified Central CIP target.
<strong>Trust</strong> I&E summary by division:<strong>2012</strong>/13 In Month <strong>2012</strong>/13 In Month <strong>2012</strong>/13 Year to date (£'000) 2011/12<strong>2012</strong>/13Actual£'000 Var £'000 Var %Adj ActualWTEVarianceWTE Actual £'000 Var £'000 Var %Adj AverageActual WTEAverageActual £'000AnnualBudget £'000(34,338) (366) -1.05% Central Income (62,969) (449) -0.71% (32,119) (381,504)Surgical Services Division3,553 (95) -2.74% 599.58 8.94 Anaesthetics 7,181 (425) -6.29% 613.40 3,507 39,8751,444 (73) -5.30% 250.70 8.35 Specialist Surgery 2,801 (36) -1.29% 250.26 1,340 16,4301,621 (101) -6.63% 369.59 -4.57 Surgery 3,155 (127) -4.18% 384.78 1,624 18,2856,619 (268) -4.22% 1,219.87 12.72 Total 13,138 (587) -4.68% 1,248.44 6,472 74,590Emergency Care, Gen Med & Neurosciences3,773 (153) -4.22% 950.41 -21.54 Medicine 7,413 (208) -2.89% 1,033.10 3,829 41,6092,942 (216) -7.93% 582.67 8.37 Emergency Care 5,588 (154) -2.83% 583.37 2,573 32,1131,208 (69) -6.02% 232.30 3.35 Neurosciences 2,304 (33) -1.44% 230.86 1,136 13,5237,923 (438) -5.85% 1,765.38 -9.82 Total 15,305 (395) -2.65% 1,847.33 7,538 87,245Women's, Children & Support Services1,170 28 2.33% 243.33 13.11 Children 2,340 12 0.50% 263.71 1,188 14,050905 (50) -5.85% 385.69 -16.30 Support Services 1,819 (94) -5.43% 382.87 887 10,0773,012 (138) -4.81% 659.38 -0.84 Women 5,940 (112) -1.93% 678.97 3,124 35,4905,086 (160) -3.25% 1,288.40 -4.03 Total 10,099 (194) -1.96% 1,325.55 5,200 59,617Diagnostics & Specialist Medicine1,720 32 1.84% 285.98 0.90 Pathology 3,752 (240) -6.85% 284.06 1,777 20,5101,629 (88) -5.69% 290.43 -6.75 Radiology 3,320 (239) -7.74% 287.38 1,543 17,7203,712 (304) -8.92% 598.31 -6.36 Specialist Medicine 6,955 (126) -1.85% 605.48 3,441 39,8027,061 (359) -5.36% 1,174.72 -12.21 Total 14,027 (605) -4.51% 1,176.92 6,762 78,0317,230 93 1.27% 750.91 26.94 Corporate 14,317 80 0.55% 728.52 6,777 84,551(419) (1,499) -78.15% 6,199.28 13.60 - Sub-total Divisions 3,916 (2,151) -121.89% 6,326.76 630 2,530(27) 178 117.92% Central adjustment including provisio (187) 255 372.96% 134 410(346) Reserves (541) (4,576)1,186 22 1.79% Depreciation 2,373 43 1.79% 1,169 14,4942,448 (15) -0.63% PDC & Net Interest 4,794 5 0.11% 2,209 28,0753,189 (1,661) -108.70% Total 10,896 (2,389) -28.09% 6,326.76 3,512 40,933(2,005) Impairments (2,005) (2,005)1,184 (1,661) -348.06% Net position 8,891 (2,389) -36.75% 6,326.76 3,512 38,9283
2. CLINICAL INCOMEKey points:• Income for Month 2 has been forecasted using first cut activityfor the Month. Activity for A&E was taken at Day 30 <strong>and</strong> activityfor Inpatients, Out Patients <strong>and</strong> Daycases were taken at Day 29,<strong>and</strong> then extrapolated to a full month. This has ensured thatactivity is more accurate <strong>and</strong> gives greater assurance aroundIncome for the current month.• There was an under- performance of £0.2m in month, with a yearto date under-performance to £0.4m. At month 2, the <strong>Trust</strong>forecasts a breakeven position for the year. The expectation isthat the <strong>Trust</strong> will achieve the contracted activity by the year end,for each individual contract.• The over-performance for Acute Medicine is mainly as a result ofNon- elective activity. Some of this over-performance will beoffset by the transitional income from ONEL.Business UnitPerformanceIn Month Year to date ForecastActual Var Actual Var Actual Var(7,247) 325 Acute Medicine (14,226) 645 (82,308) 645(1,878) (1) Anaesthetics (3,529) (197) (22,180) (197)(2,029) 8 Children (3,877) (128) (23,928) (128)(2,463) 84 Emergency Care (4,800) 47 (28,569) 47(2,343) (113) Neurosciences (4,592) (217) (28,706) (217)(765) (62) Pathology (1,530) (123) (9,795) (123)(991) 74 Radiology (1,983) 148 (11,154) 148(2,369) (78) Specialist Medicine (4,729) (15) (28,552) (15)(3,595) 60 Specialist Surgery (6,892) 172 (40,729) 172(3,605) (112) Surgery (7,130) (9) (43,025) (9)(4,340) (2) Women (8,478) 51 (50,783) 51(636) (377) Corp (1,201) (824) (11,776) (374)(32,261) (194) Total (62,969) (449) (381,504) 0• Outpatients is over performing by £403k YTD, this is an area ofconcern as if the over-performance continues on the sametrajectory, the <strong>Trust</strong> runs the risk of not meeting the PCT plans,which exposes the <strong>Trust</strong> to risk of non-payment of overperformanceincome because of the Cap <strong>and</strong> Collar contract. Todate, the <strong>Trust</strong> has not received the Commissioning StrategyPlans from the PCTs, thus it is unclear when activity reductionsare likely to occur.• Contract Variations: The <strong>Trust</strong> is currently negotiating for extraincome for Best Practice Tariff, Breast Screening <strong>and</strong>Commissioners’ failure to move births to other providers• The activity table below compares current year YTD activity withthe same period last year. A&E activity has grown by 8% yearon year. This is mainly as a result of the UCC; the <strong>Trust</strong>acquired the UCC in month 4 last year.• There is a growth of 7% in Day cases year on year as a result ofthe achievement of the 18weeks targets, coupled with the <strong>Trust</strong>undertaking work that went to the ISTC last year.• Non Elective activity appears to have declined by 2%, this isbeing reviewed to confirm whether the reduction is as a result ofthe PCT QIPP plans being achieved.• Month 1 actual income came in at £30.7m; £2.1m more than wasforecasted, as such, the YTD position reflects the actual activityat Month 1 <strong>and</strong> the current month forecast.4
Income by PODIn Month Year to date ForecastActual Var Actual Var Actual Var(1,749) 37 A <strong>and</strong> E (3,450) 26 (20,571) 26(71) (4) Ambulatory Care (157) 6 (908) 6(192) 5 Breast Screening (384) 10 (2,252) 10(217) 0 Challenge <strong>Trust</strong> <strong>Board</strong> (433) 0 (2,600) 0(378) 0 CQUIN (756) 0 (4,536) 0(2,256) 18 Critical Care (4,353) (123) (26,731) (123)(2,828) (10) Daycases (5,393) 105 (32,091) 105(904) 31 Devices & Drugs (1,807) 61 (10,538) 61(1,186) (68) Direct Access (2,371) (137) (14,912) (137)(1,957) (125) Elective (3,839) (41) (23,428) (41)(355) 0 HIV Contract (711) 0 (4,264) 0(33) (12) ISTC Contract (62) (28) (512) (28)(11,419) 548 Non Elective (22,135) 392 (130,849) 392(2,598) (64) OP First Attendances (5,122) 162 (30,168) 162(2,684) (117) OP Follow Ups (5,449) 229 (31,804) 229(471) (0) OP Procedures (890) 13 (5,323) 13(1,552) 79 Other (3,104) 158 (17,836) 158(263) (18) Patient Transport Services (525) (36) (3,330) (36)(323) 1 Radiotherapy (645) 2 (3,862) 2496 0 Readmissions 992 0 5,953 0(470) 1 Regular Day Attenders (907) (32) (5,601) (32)(238) (1) Road Traffic Accidents (409) (68) (2,796) (68)0 (358) Support 0 (717) (4,033) (267)(614) (136) XBD (1,058) (432) (8,513) (432)(32,261) (194) Total (62,969) (449) (381,504) 0ActivityPOD Group 2011-12 <strong>2012</strong>-13 Var%ChangeA<strong>and</strong>E 31,117 36,809 5,692 8%Ambulatory Care 529 578 49 4%Breast Screening 3,692 3,878 186 2%Critical Care 4,379 4,290 (89) -1%Daycases 6,291 7,248 957 7%Direct Access 759,868 769,176 9,308 1%Elective 1,159 1,271 112 5%Non Elective 12,787 12,348 (439) -2%OP First Attendances 27,134 29,990 2,856 5%OP Follow Ups 63,589 68,307 4,718 4%OP Procedures 5,106 5,497 391 4%Other 13,642 13,146 (496) -2%Radiotherapy 3,040 3,308 268 4%Regular Day Attenders 2,171 2,166 (5) 0%XBD 7,043 3,269 (3,774) -37%Total 941,547 961,281 19,734 1%5
2. PAY EXPENDITUREPay & Headcount Position2011/12M12ActualWTE2011/12M12Actual£0002011/12 FYAv WTE2011/12FY Av£'000• The above WTE has been restated for M01 due to changes in the process of reporting agency <strong>and</strong> the capturing of the WTE.• M2 headcount (FTE), shows a further reduction, of 24 FTE from the M1 position.• Average pay costs were up in M2 compared to M1, partly due to enhanced payments for the April bank holidays, paid in May (impacting onpermanent <strong>and</strong> bank staffing).<strong>2012</strong>/13M1ActualWTE<strong>2012</strong>/13M1Actual£000<strong>2012</strong>/13M2ActualWTE<strong>2012</strong>/13M2Actual£000Mov'tfrompriormonthWTEMov'tfrompriormonth£'000M2 12/13v 11/12Av WTEM2 12/13v 11/12Av £'000Sum m ary LevelS taff TypeMedical StaffPerm anent 835 6,080 814 5,919 836 5,941 822 5,984 ‐ 15 43 7 65Bank 50 570 48 562 59 683 54 574 ‐ 5 (109) 6 12Agency 72 1,026 67 889 70 680 79 961 10 281 12 72Medical S taff Total 958 7,676 930 7,369 966 7,304 955 7,519 ‐ 10 215 26 150Scientific, Therap & TechnicalPerm anent 877 3,191 868 3,162 877 3,191 879 3,230 ‐ 1 0 ‐ 8 29Bank 21 87 25 60 19 73 18 72 ‐ 2 (15) ‐ 6 12Agency 41 287 30 200 34 176 41 251 ‐ 7 (111) ‐ 8 (24)Scientific, Therap & Technical Total 940 3,566 923 3,422 930 3,440 937 3,553 ‐ 10 (125) ‐ 22 18Nursing & Midwifery - Qual.Perm anent 1919 6,883 1909 6,846 1919 6,980 1920 7,231 0 251 11 385Bank 258 818 225 702 200 682 195 630 ‐ 5 (52) ‐ 30 (72)Agency 50 319 70 433 48 330 40 261 ‐ 8 (69) ‐ 30 (172)Nursing & Midwifery - Qual. Total 2227 8,021 2203 7,980 2166 7,993 2154 8,122 ‐ 12 129 ‐ 49 142Nursing & Midwifery - Unqual.Perm anent 691 1,420 669 1,374 679 1,434 662 1,507 ‐ 16 73 ‐ 6 133Bank 159 349 177 332 130 304 127 282 ‐ 3 (22) ‐ 50 (50)Nursing & Midwifery - Unqual. Total 850 1,769 846 1,706 809 1,737 789 1,789 ‐ 19 52 ‐ 57 83Ancillary StaffPerm anent 288 771 282 753 285 694 288 817 3 123 6 64Agency 0 3 0 3 0 1 - 0 (1) 0 (3)Ancillary S taff Total 288 773 282 756 285 695 288 817 3 122 6 61Managem ent & Adm in StaffPerm anent 987 2,767 1063 2,826 1002 2,887 1000 2,854 ‐ 2 (33) ‐ 63 28Bank 74 143 82 157 61 131 67 143 6 12 ‐ 15 (14)Agency 4 183 2 108 5 95 9 153 4 58 7 45Managem ent & Adm in Staff Total 1065 3,094 1146 3,092 1067 3,112 1076 3,150 8 38 ‐ 71 58N et D eficit / (Surplus) 6327 24,899 6330 24,325 6223 24,282 6199 24,950 ‐ 24 668 ‐ 130 625Total Perm anent 5597 21,112 5605 20,879 5598 21,127 5570 21,623 ‐ 29 496 ‐ 35 744Bank 562 1,969 556 1,814 469 1,873 461 1,701 ‐ 8 (172) ‐ 95 (113)Agency 167 1,818 168 1,632 156 1,282 169 1,626 13 344 0 (6)Total 6327 24,899 6330 24,325 6223 24,282 6199 24,950 ‐ 24 668 ‐ 130 6256
Monthly pay trend comparison:M£26.025.024.023.022.021.020.0Expenditure by pay groupMonthly Pay ExpenditureApr May Jun Jul Aug Sep Oct Nov Dec Jan Feb MarActual Budget Prior Yr Actual*March has been adjusted to show the underlying run rate position.<strong>2012</strong>/13 In Month <strong>2012</strong>/13 In Month <strong>2012</strong>/13 Year to date 2011/12Actual£'000 Var £'000 Var % Paid WTEAdj ActualWTEAdjVarianceWTE Actual £'000 Var £'000 Var %Adj AverageActual WTEAverage£'0007,519 (58) -0.78% 972.86 933.67 39.19 Medical 14,824 (116) -0.79% 957.51 7,6768,122 (58) -0.72% 2,157.60 2,142.78 14.82 Nursing - Qualified 16,115 66 0.41% 2,226.74 8,0211,789 (206) -13.01% 731.69 789.45 -57.76 Nursing - Unqualified 3,526 (404) -12.95% 849.88 1,7693,553 (71) -2.05% 939.61 921.30 18.31 ST&T 6,993 (43) -0.62% 939.82 3,5663,150 13 0.42% 1,083.62 1,073.25 10.37 Management & Admin 6,262 118 1.84% 1,064.91 3,094818 (11) -1.32% 327.00 287.86 39.14 Ancillary 1,513 74 4.68% 287.90 77324,951 (391) -1.59% 6,212.38 6,148.31 64.07 Total 49,233 (305) -0.62% 6,326.76 24,899(743) -100.00% 0.50 0.00 0.50 Divisional Unallocated CIP (1,320) -100.00%50 100.00% 0.00 0.00 0.00 Reserves (11) -100.00%24,951 (1,085) -4.55% 6,212.88 6,148.31 64.57 Total 49,233 (1,636) -3.44% 6,326.76 24,899Key points:• Adjusted Actual WTE uses contracted for permanent staff <strong>and</strong> confirmedbooked hours on the IHB system for bank & agency in the month.• Pay costs in M02 show a reduction of £0.6m from the previous month <strong>and</strong> areabove the monthly average for 2011/12. The profiled pay budget (net of CIPtarget) for M02 is £24.6m. Actual pay was (£0.4m) over spent against this.Mostly on nursing <strong>and</strong> largely due to the 2 bank holidays that would have hitthis payroll for permanent <strong>and</strong> bank staff. There are a number of over spendsthat are mitigated by under spends elsewhere the key ones are describedbelow.• Pay over spent by £305k, driven by in month overspending of £391k. Mainpressures from:Emergency Care, Neurosciences & Acute Medicine division (£353k) advin month / (£283k) adv YTD month),A&E staffing - (£153k) M02 <strong>and</strong> (£41k) YTD. Mostly medical staff of which(£30k) is retrospective bookings <strong>and</strong> (£80k) is associated with vacancycover <strong>and</strong> the Reset project (plan to be submitted). (£30k) in month is arealignment from Medicine;Neurosciences - (£102k) M02 / (£54k) YTD mostly associated withadditional stroke activity;Medicine - (£98k) M02 / (£193k) YTD mostly from CIP ward closureslippage, additional Endoscopy Sessions to cover the growth in activityfrom bowel cancer screening extension <strong>and</strong> booking to e-rostering ratiosthat are being reviewed.Women, Children & Support ServicesMidwifery has a (£100k) a month over spend due to the operational ratiomethodology being used for bookings (paper being taken to TEC). Aprilbirths were significantly under budgeted plan.Support Services have A&C pressures (£24k) a month relating to -recruitment, prior year non recurrent CIP pressures <strong>and</strong> activity. Capacity,dem<strong>and</strong> <strong>and</strong> recovery plan being developed.Diagnostics & Specialist MedicineRadiology is overspending bv (£65k) a month due to the continued use ofhigh cost temporary staffing for cover <strong>and</strong> vacancies.Surgical ServicesIn month break even is largely due to 2 months funding of additionaldedicated obstetrics cover which requires a long term signed off model ofcare <strong>and</strong> a recruitment/operational change plan. Anaesthetics continues toover spend on medical staff <strong>and</strong> there are small over spends withinUrology <strong>and</strong> General Surgery (medical <strong>and</strong> nursing staff) <strong>and</strong> Theatres(nursing).7
4. NON-PAY EXPENDITUREExpenditure by Non Pay category:<strong>2012</strong>/13 In Month <strong>2012</strong>/13 Year to dateActual £'000 Var £'000 Var % Actual £'000 Var £'000 Var %2011/12Average£'0002,663 (141) -5.57% Drugs 5,025 35 0.69% 2,4672,845 (158) -5.88% Clinical supplies & services 5,707 (365) -6.83% 2,7401,402 61 4.15% General supplies & services 2,956 14 0.48% 1,5021,617 (125) -8.39% Premises & fixed plant 2,800 203 6.77% 1,5181,079 88 7.54% Other - PFI 2,284 33 1.42% 1,1471,026 (25) -2.55% Other - CNST 2,001 1 0.05% 900741 237 24.25% Other 1,515 191 11.21% 1,10911,374 (63) -0.56% Total 22,287 113 0.50% 11,382Non-pay expenditure by Business Unit:<strong>2012</strong>/13 In Month 2011/12 <strong>2012</strong>/13 Year to date (£'000)Monthly ActualActual £'000 Var £'000 Var %Average £'000 £'000 Var £'000 Var %Surgical Services Division985 (22) -2.33% Anaesthetics 1,009 1,961 (67) -3.55%244 (13) -5.49% Specialist Surgery 211 427 29 6.35%191 (12) -6.71% Surgery 168 337 15 4.33%1,420 (47) -3.44% Total 1,388 2,725 (23) -0.85%Emergency Care, Gen Med & Neurosciences675 (48) -7.62% Medicine 631 1,202 32 2.62%249 2 0.79% Emergency Care 258 492 14 2.76%239 (18) -8.13% Neurosciences 215 411 27 6.13%1,163 (64) -5.80% Total 1,103 2,105 73 3.36%Women's, Children & Support Services115 (42) -57.90% Children 106 210 (46) -27.84%39 (6) -18.29% Support Services 35 67 (2) -3.58%583 (71) -13.81% Women 553 1,102 (28) -2.58%736 (119) -19.23% Total 693 1,379 (76) -5.81%Diagnostics & Specialist Medicine626 71 10.14% Pathology 674 1,530 (136) -9.77%295 (21) -7.79% Radiology 285 654 (106) -19.32%1,931 (136) -7.55% Specialist Medicine 1,765 3,478 113 3.15%2,853 (86) -3.12% Total 2,724 5,661 (129) -2.33%Trend overview:M£12.011.511.010.510.09.59.08.58.0Non-pay expenditureApr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<strong>2012</strong>/13 Actual<strong>2012</strong>/13 Budget2011/12 Prior Yr Actual2010/11 Prior Yr Actual*Feb <strong>and</strong> Mar have been adjusted to show the underlying run rate.Key points:• Non pay overall is down against last years average. However most categories of spendare higher with the exception of other non pay which is due to a reduction in ExternalConsultancy <strong>and</strong> Legal & Professional related fees.• Pathology (£0.1m) <strong>and</strong> Radiology (£0.1m) are the main areas of concern as these are13% <strong>and</strong> 14% up on last year’s average. Pathology is mostly re-agents <strong>and</strong> bloodproducts, some of which is suspected to be around Olympic stock preparation.Radiology is due to supplies <strong>and</strong> appliances mostly on the interventional side. Howeverreviews are under way for both by M03. Anaesthetics is also (£0.1m) over YTD largelyfrom doing additional Theatre cases.• Drugs has over spent in month bringing the YTD position on plan. Within the YTDposition though High Cost Drugs in specialist areas are causing pressures particularlyoncology £0.1m YTD <strong>and</strong> circa £0.5m FYE.• Clinical Supplies & Appliances over spent by (£0.4m) is the main category of overspendas discussed above by specialty analysis.6,172 (316) -5.40% - Sub-total 5,908 11,870 (154) -1.32%5,114 228 4.27% Corporate 5,252 10,395 163 1.54%88 25 21.92% Central I&E inc. Reserves 222 22 104 82.92%11,374 (63) -0.56% Net position 11,382 22,287 113 0.50%8
<strong>Trust</strong> Wide Perfomance Summary at 31st May <strong>2012</strong>, And Forecast Overview to 31st March 20135. CIP <strong>and</strong> QIPP Programme Summary1. Annual Savings Forecast (part year <strong>and</strong> full year effect).Apr 12 May 12 Jun 12 Jul 12 Aug 12 Sep 12 Oct 12 Nov 12 Dec 12 Jan 13 Feb 13 Mar 13 Total PYE 2013/14 FYE£'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000Target 898 1,567 1,621 1,803 1,864 2,066 2,179 2,179 2,194 2,273 2,283 2,227 23,155IN MONTH Implemented ‐ 'Blue' 350 550 440 444 449 467 477 477 477 477 476 477 5,563 5,625Variance from <strong>Trust</strong> target -548 -1,016 -1,180 -1,359 -1,415 -1,599 -1,702 -1,702 -1,717 -1,796 -1,807 -1,750 -17,592Cumulative Target 898 2,464 4,085 5,888 7,752 9,819 11,998 14,177 16,371 18,645 20,928 23,155 23,155 This is the original CIP targetBLUE Schemes Actual / forecast Savings 350 900 1,341 1,785 2,234 2,701 3,179 3,655 4,132 4,610 5,086 5,563 5,563 5,625GREEN Schemes Actual / forecast Savings 0 0 85 359 590 910 1,276 1,638 2,000 2,365 2,735 3,111 3,111 2,677 This forecast includes only green schemesAMBER Schemes Actual / forecast Savings 0 0 15 120 255 508 828 1,149 1,470 1,791 2,111 2,437 2,437 3,367 This forecast includes only amber schemesRED Schemes Actual / forecast Savings 0 0 5 291 582 1,924 3,498 5,072 6,649 8,304 9,855 12,043 12,043 7,591 This forecast includes only red schemesBEST CASE Forecast Cumulative Target 898 2,464 4,085 5,888 7,752 9,819 11,998 14,177 16,371 18,645 20,928 23,155 23,155(includes all schemes) Actual / forecast Savings 350 900 1,446 2,556 3,661 6,044 8,781 11,515 14,252 17,069 19,788 23,155 23,155 19,260Variance from <strong>Trust</strong> target -548 -1,564 -2,639 -3,332 -4,091 -3,775 -3,217 -2,662 -2,120 -1,576 -1,140 0 0LIKELY CASE Forecast Cumulative Target 898 2,464 4,085 5,888 7,752 9,819 11,998 14,177 16,371 18,645 20,928 23,155 23,155(includes Blue, Green Actual / forecast Savings 350 900 1,441 2,265 3,079 4,120 5,283 6,443 7,603 8,765 9,933 11,111 11,111 11,669<strong>and</strong> Amber Schemes Variance from <strong>Trust</strong> target -548 -1,564 -2,644 -3,623 -4,673 -5,699 -6,715 -7,734 -8,769 -9,880 -10,995 -12,043 -12,043WORST CASE Forecast Cumulative Target 898 2,464 4,085 5,888 7,752 9,819 11,998 14,177 16,371 18,645 20,928 23,155 23,155(includes Blue <strong>and</strong> Actual / forecast Savings 350 900 1,426 2,145 2,825 3,612 4,455 5,294 6,133 6,974 7,821 8,674 8,674 8,302Green Schemes Variance from <strong>Trust</strong> target -548 -1,564 -2,659 -3,743 -4,928 -6,207 -7,543 -8,884 -10,239 -11,670 -13,106 -14,480 -14,480£'00025,00020,00015,00010,0005,000-Definitions8982,4649004,085<strong>Trust</strong> target: The efficiency required to meet the CIP plan.1,4461,3411,441Savings plan: Original savings potential (local estimate of savingsto allow performance management of project)Savings actual / forecast: In month / cumulative actual savings<strong>and</strong> forecast savings for future periods.PYE: Part Year Effect: Benefit of saving in current financial year.FYE: Full Year Effect: Benefit of saving running for full 12 months.Forecast CIP Savings vs <strong>Trust</strong> Target Profile £0005,8882,5562,2652,1451,7857,7523,6613,0792,825 2,2349,8196,0443,6122,701Bed Review to be determined4,120Worst Green ForecastLikely Amber ForecastBest Red ForecastCIP TargetCumulative ImplementedUnlikely to deliver11,998Unlikely to deliverUnlikely to deliver8,7815,2834,4553,179Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb MarRisk Ratings for Projects14,17711,5155,2946,4433,65516,37114,2526,1337,6034,132BLUEScheme implemented <strong>and</strong> savings removed from budgets.GREENInitiative is delivering on plan <strong>and</strong> to the full value.AMBERInitiative is off trajectory or there are risks to delivery butassured that recovery/mitigation plans are adequate.May also be used if scheme has been actioned but it isachieving less than 90% of the cash value.REDInitiative is off trajectory <strong>and</strong>/or a significant risk to delivery<strong>and</strong> not sufficiently assured that recovery/mitigation plansin place. There is a 50% or greater risk of non delivery.18,64517,0696,9748,7654,61020,92819,7887,82123,1559,9335,08623,15511,1118,6745,563Unidentified52%Unidentified63%Best CaseUnidentified0%Identified100%Likely CaseWorst CaseIdentified37%Identified48%This forecast includes all green, amber & red schemesThis forecast includes all green & amber schemesThis forecast includes only green schemesCIP Monthly Headlines May• Overall unfavourable variance to budget YTD was £1,564k, of which£582k relates to unallocated CIP which is phased evenly in 1/12ths.The <strong>Trust</strong> has taken into account the findings of the external review<strong>and</strong> is developing the CIP Delivery Plrogramme to identify furthersavings to meet the target.Scheme Narrative - Business Unit Overview• Acute Medicine - £105k achieved as per plan, £130k unfavourabledue to unachieved planned ward closures (£97k) <strong>and</strong> £33k fromadditional endoscopy costs <strong>and</strong> temporary staff costs not confirmed asCIP.• Emergency Care - £17k achieved as per plan, £86k shortfall due tobudget phasing of unidentified CIP• Neurosciences - £3k achieved, £94k variance due to £70k in tempmedical staff reduction not achieved <strong>and</strong> phasing of unidentified target.• Bed <strong>and</strong> Site - £0 achieved, £25k variance due to unidentified CIPtarget• Anaesthetics - £39k achieved, of which £22k from Amber B ward.£267k unidentified CIP target unachieved• Surgery - £35k achieved, of which £22k from closing Amber B ward.£80k unachieved from unidentified CIP allocation.• Specialist Surgery - £88k achieved from apportioned savings fromthe closure of Amber B, against a target of £134k. Includes £80kunidentified target <strong>and</strong> £33k not recognised relating to best practisetariffs.• Women - £205k achieved, of which £133k due to reduction onMidwifery temporary staff usage <strong>and</strong> £42k from HIV Home Care drugssavings. £30k shortfall due to unidentified CIP.• Children - £102k achieved, of which £83k from reduction intemporary staff usage. £24k shortfall due to unidentified CIP target.• Support Services - £0k achieved, £41k shortfall from unidentifed CIPtarget• Pathology - £41k achieved, £10k shortfall arising from delays inrevised consultant PA's <strong>and</strong> £40k unidentied CIP target.• Radiology - £25k achieved as per plan• Specialist Medicine - £38k achieved, of which £17k from Outpatientprescribing. £102k shortfall arising from failure to recognised savingsfrom manpower planning review (£67k), medicines management (£20k)<strong>and</strong> oncology drugs £(17)k .• Corporate - £203k achieved from actions identified in the plan, butshortfall of £96k arising due to not freezing recruitment - £37k,procurement plans - £15k , R&D cost savings of £13k <strong>and</strong> unidentifiedtarget of £5k.• Central - no planned schemes due for delivery for May12, but £127kunachieved as a result of unidetified CIP target phasing.9
<strong>Trust</strong> Wide Perfomance Summary at 31st May <strong>2012</strong>, And Forecast Overview to 31st March 20131. Annual Workforce Savings Forecast (part year <strong>and</strong> full year effect).Apr 12 May 12 Jun 12 Jul 12 Aug 12 Sep 12 Oct 12 Nov 12 Dec 12 Jan 13 Feb 13 Mar 13 Total PYE 2013/14 FYE£'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000 £'000Target 53.0 81.0 96.8 107.8 108.8 126.1 171.1 170.1 170.1 169.1 169.1 170.1 170.1IN MONTH Implemented ‐ 'Blue' 46.5 42.1 51.1 49.4 48.4 56.4 59.4 59.4 59.4 59.4 59.4 60.4 60.4 60.4Variance from <strong>Trust</strong> target -6.5 -38.8 -45.7 -58.4 -60.4 -69.7 -111.7 -110.7 -110.7 -109.7 -109.7 -109.7 -109.7Target 53.0 81.0 96.8 107.8 108.8 126.1 171.1 170.1 170.1 169.1 169.1 170.1 170.1 This is the original CIP targetBLUE Schemes Actual / forecast Savings 46.5 42.1 51.1 49.4 48.4 56.4 59.4 59.4 59.4 59.4 59.4 60.4 60.4 60.4GREEN Schemes Actual / forecast Savings 0.1 7.6 14.6 21.4 17.4 13.4 17.4 16.4 16.4 11.4 11.4 11.4 11.4 11.4 This forecast includes only green schemesAMBER Schemes Actual / forecast Savings 0.0 26.4 25.2 21.7 21.7 31.7 31.7 31.7 31.7 31.7 31.7 31.7 31.7 31.7 This forecast includes only amber schemesRED Schemes Actual / forecast Savings 0.0 0.0 1.1 14.7 26.2 35.4 67.5 67.5 67.5 71.5 71.5 71.5 71.5 71.5 This forecast includes only red schemesBEST CASE Forecast Cumulative Target 53.0 81.0 96.8 107.8 108.8 126.1 171.1 170.1 170.1 169.1 169.1 170.1 170.1(includes all schemes) Actual / forecast Savings 46.6 76.2 92.0 107.2 113.7 137.0 176.0 175.0 175.0 174.0 174.0 175.0 175.0 175.0Variance from <strong>Trust</strong> target -6.4 -4.8 -4.8 -0.6 4.9 10.9 4.9 4.9 4.9 4.9 4.9 4.9 4.9LIKELY CASE Forecast Cumulative Target 53.0 81.0 96.8 107.8 108.8 126.1 171.1 170.1 170.1 169.1 169.1 170.1 170.1(includes Blue, Green Actual / forecast Savings 46.6 76.2 90.9 92.6 87.6 101.6 108.6 107.6 107.6 102.6 102.6 103.6 103.6 103.6<strong>and</strong> Amber Schemes Variance from <strong>Trust</strong> target -6.4 -4.8 -5.9 -15.3 -21.3 -24.5 -62.6 -62.6 -62.6 -66.6 -66.6 -66.6 -66.6WORST CASE Forecast Cumulative Target 53.0 81.0 96.8 107.8 108.8 126.1 171.1 170.1 170.1 169.1 169.1 170.1 170.1(includes Blue <strong>and</strong> Actual / forecast Savings 46.6 49.7 65.7 70.8 65.8 69.8 76.8 75.8 75.8 70.8 70.8 71.8 71.8 71.8Green Schemes Variance from <strong>Trust</strong> target -6.4 -31.2 -31.1 -37.0 -43.0 -56.3 -94.3 -94.3 -94.3 -98.3 -98.3 -98.3 -98.3WTE250.0150.050.0-50.0Definitions76.292.0<strong>Trust</strong> target: The efficiency required to meet the CIP plan.Savings plan: Original savings potential (local estimate of savingsto allow performance management of project)Savings actual / forecast: In month / cumulative actual savings<strong>and</strong> forecast savings for future periods.PYE: Part Year Effect: Benefit of saving in current financial year.FYE: Full Year Effect: Benefit of saving running for full 12 months.Forecast CIP Staff Reductions vs <strong>Trust</strong> Target107.290.9 92.670.8113.765.851.1 49.4 48.487.6137.069.8101.6Worst Green ForecastLikely Amber ForecastBest Red ForecastCIP TargetCumulative Implemented176.0 175.0 175.0 174.0 174.0 175.0Bed Review to be determinedUnlikely to deliverUnlikely to deliver76.8 75.8 75.8Unlikely to deliverRisk Ratings for Projects108.6 107.6 107.6BLUEScheme implemented <strong>and</strong> savings removed from budgets.GREENInitiative is delivering on plan <strong>and</strong> to the full value.AMBERInitiative is off trajectory or there are risks to delivery butassured that recovery/mitigation plans are adequate.May also be used if scheme has been actioned but it isachieving less than 90% of the cash value.REDInitiative is off trajectory <strong>and</strong>/or a significant risk to delivery<strong>and</strong> not sufficiently assured that recovery/mitigation plansin place. There is a 50% or greater risk of non delivery.102.6 102.6 103.670.8 70.8 71.856.4 59.4 59.4 59.4 59.4 59.4 60.4Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar10Unidentified89%Unidentified94%Unidentified95%Best CaseIdentified11%Likely Case Identified6%Worst Case Identified5%This forecast includes all green, amber & red schemesThis forecast includes all green, amber & red schemesThis forecast includes only green schemesCIP Monthly Headlines May• Overall unfavourable variance to budget increased to 38.8 primarilyas a result of the planned ward closure not occuring, with the schemenow being removed.• Ongoing temporary staff cost reductions in the month were inprimarily as a result of the premium reduction of recruitment activity,rather than actual consumption reduction beyond the reductions seen inApril• Unidentified CIP requires a corresponding WTE reduction wherepotential workforce reductions will be required. The outcome of thecurrent external review will need to be detailed at a workforce level.Scheme Narrative - Business Unit Overview• Acute Medicine - 9.6 planned WTE reductions achieved.• Emergency Care - No planned reductions in the month.• Neurosciences - Although planned temporary staff cost reductionswere targeted from temp to perm price premium, these reductions arenot being achieved.• Bed <strong>and</strong> Site - No planned reductions in the month.• Anaesthetics - 7.4WTE planned, 4.4WTE achieved. Shortfallcontinues to be due to inability to remove additional lists resulting inadditional session costs.• Specialist Surgery - No planned reductions in the month.• Surgery - 0.6 planned WTE reductions achieved.• Women - 30.5WTE planned - 31.5WTE reported achieved - nochange from April• Children - Planned temporary staff cost reductions arising from tempto perm price premium reduction. No planned overall WTE reductionsin the month.• Support Services - No planned reductions in the month.• Pathology - 0.6 planned WTE reductions from changes to PA's notachieved• Radiology - No net headcount reduction. Financial Savings fromrecruitment displacing temporary staff.• Specialist Medicine - 5WTE included in plan as part of workforcereview not achieved up to end of May.• Corporate - 0.5WTE reduction in Estates implemented• Central - no planned schemes due for delivery from May 12.
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Annual Statement In Month Statement Ytd StatementWTE ReductionsDataDivision CIP Scheme Scheme Expenditure Type12/13 Target12-13 12-13 In Mth In Mth In Mth Ytd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTEGreen Amber RedF-cast Variance Target Delivery VarianceAcute Medicine Divisional CIP Endoscopy 4th Room Pay 138 - 96 - 96 (42) 13 - (13) 13 - (13) - - -FYE Angelica Pay 390 390 - - 390 - 33 33 - 65 65 - 8.6 8.6 -Perfusion Scans Pay 40 40 - - 40 - 3 3 - 7 7 - - - -Staff Secondment Opportunity Pay 81 81 - - 81 - 7 7 - 14 14 - 1.0 1.0 -Overseas Nursing Recruitment Non-Pay 120 120 - - 120 - 10 10 - 20 20 - - - -Temporary staff reduction Pay 120 110 - - 110 (10) 10 - (10) 20 - (20) - - -Income Opportunities Cardiology Direct Access Non-Pay - - - - - - - - - - - - - - -Length of stay / Ward closures LOS to national mean 95% (Discharge Co-Or) Pay 264 - - - - (264) 24 - (24) 24 - (24) - - -LOS to national mean 95% (5/7 Day Wrk) Pay 583 - - - - (583) 53 - (53) 53 - (53) - - -LOS to national mean 95% (CofE Physician) Pay 189 - - - - (189) - - - - - - - - -LOS to national mean 95% (Card) Pay 90 - - - - (90) - - - - - - - - -LOS to national mean 95% (Resp) Pay 224 - - - - (224) 20 - (20) 20 - (20) - - -LOS to national mean 95% (Amb) Pay 90 - - - - (90) - - - - - - - - -LOS to national mean 95% (EDS) Pay 30 - - - - (30) - - - - - - - - -LOS to national mean 95% (DTOC) Pay 206 - - - - (206) - - - - - - - - -LOS to national mean 95% (Ward 1 + Surge) Pay - - 207 207 207 - - - - - - - -LOS to national mean 95% (Ward 2 + Surge) Pay - - 415 415 415 - - - - - - - -To be identified Total Divisional Target Pay - - - 1,106 1,106 1,106 - - - - - - - -Acute Medicine Total 2,565 741 96 1,728 2,565 1 172 53 (120) 235 105 (130) 9.6 9.6 -Neurosciences Divisional CIP Neurosciences Temp Staff Reduction Pay 420 - 100 - 100 (320) 35 - (35) 70 - (70) - - -Head of Neuropsychology regrade Pay 20 20 - - 20 - 2 2 - 3 3 - - - -Develop Spinal Elective Service West essex Ext Income - - - 48 48 48 - - - - - - - - -Neurosciences permanent recruitment Pay 100 - - - - (100) - - - - - - - - -To be identified Total Divisional Target Pay 146 - - 518 518 372 12 - (12) 24 - (24) - -Neurosciences Total 686 20 100 566 686 - 49 2 (47) 98 3 (94) - - -Emergency Care Divisional CIP Advanced Nurse Practiitioner Pay 80 - 56 - 56 (24) - - - - - - - - -PELC VAT Pay 100 100 - - 100 - 8 8 - 17 17 - - - -Temp Medical Staff Reduction -A&E Pay 105 105 - - 105 - - - - - - - - - -ED Skills for Health Review Pay 250 - - - - (250) - - - - - - - - -To be identified Total Divisional Target Pay 515 - - 789 789 274 43 - (43) 86 - (86) - -Emergency Care Total 1,050 205 56 789 1,050 - 51 8 (43) 102 17 (86) - - -Bed <strong>and</strong> Site To be identified Total Divisional Target Pay 152 - - 152 152 - 13 - (13) 25 - (25) - -Bed <strong>and</strong> Site Total 152 - - 152 152 - 13 - (13) 25 - (25) - -11
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTEAnaesthetics Divisional CIP Invest in Gambro Dialysis Devices for ITU Non-Pay 44 32 - - 32 (12) 4 - (4) 4 - (4) - - -Procurement moving from Supply Chain to BMIfor consumablesNon-Pay 67 67 - - 67 - - - - - - - - - -Procurement reduction in Prothesis spend Non-Pay 67 67 - - 67 - - - - - - - - - -Sevoflurane Reduction Non-Pay 26 30 - - 30 3 2 2 0 4 5 1 - - -Key Recruitment Recruitment into Vacant ITU nursing posts Pay 40 - 40 - 40 - - - - - - - - - -Length of stay / Ward closures Closure Amber B Pay 241 - - 241 241 - 22 22 - 22 22 - -Medical staffing productivity Match Theatres plan to Outturn Pay 42 42 - - 42 - 3 3 - 7 7 - 1.0 1.0 -Reduction of Study Leave for AnaestheticDoctorsPay - - - - - - - - - - - - -Reduction of Study Leave within Theatres forNursing StaffPay 14 14 - - 14 - 1 1 - 2 2 - 1.9 1.9 -Recruitment - Temp to Perm Pay - - - - - - - - - - - - - - -Senior Nurse staffing Reduction of Study Leave in ITU Pay 3 - - 3 3 - - - - - - 0.1 0.1Theatre productivityRecruitment of Locum Doctor into DR Jonesposition on 10 PasPay 23 23 - - 23 - - - - - - - - - -Recruitment of Specialty Doctors Pay 20 20 - - 20 - - - - - - - - - -Remove weekend Initiative list <strong>and</strong> use vacanttheatre list due to A/L (Bhargava)Pay 19 19 - - 19 - 2 2 - 3 3 - 1.4 1.4 -Remove weekend Initiative list <strong>and</strong> use vacanttheatre list due to A/L (Ojo)Pay 16 - - - - (16) - - - - - - 1.4 - (1.4)Remove weekend Initiative list <strong>and</strong> use vacanttheatre list due to A/L (Pittathankal)Pay 16 - - - - (16) - - - - - - 0.4 - (0.4)Run HCA Lists wintin current schedule <strong>and</strong> staffPayon duty- - - - - - - - - - - - 1.0 - (1.0)Recruitment - Temp to Perm Pay - - - - - - - - - - - - - - -Ward productivity Reduction of Study Leave in ITU Pay 3 - - - - (3) 0 - (0) 1 - (1) 0.1 (0.1)To be identified Total Divisional Target (blank) 1,638 - - 1,439 1,439 (199) 133 - (133) 267 - (267) - -Anaesthetics Total 2,035 556 40 1,439 2,035 0 146 31 (116) 288 39 (249) 7.2 4.4 (2.8)SurgeryDivisional CIPRepatriate Lower GI physiology tests fromBARTSExt Income 26 - - 12 12 (15) - - - - - - - - -Income Opportunities Best Practice Tariff Ext Income 200 - - - - (200) 17 - (17) 33 - (33) - - -Length of stay / Ward closures Closure Amber B Pay 241 - - 241 241 - 22 22 - 22 22 - -Management Structure Management Restructure Pay 83 - - 83 83 - - - - - - - -Surgical Management Restructure Pay 83 - - - - (83) - - - - - - - -Medical staffing productivity Urology Consultant Saving (CZI) Pay 79 79 - - 79 - 7 7 - 13 13 - 0.6 0.6 -Junior Doctor B<strong>and</strong>ing Pay - - - - - - - - - - - - -KGH Specialty Doctor On Call Rota - 13 to 10PA'sPay 41 41 - - 41 - - - - - - - - - -Outpatient productivity Breast One Stop Clinics Pay - - - - - - - - - - - - - - -Surgical Hot Clinics Pay - - - - - - - - - - - - - - -Best Practice Tariff Breast Best Practice Tariff Breast (blank) - - - - - - - - - - - - - - -To be identified Total Divisional Target (blank) 562 - - 536 536 (26) 40 - (40) 80 - (80) - -Surgery Total 991 443 - 548 991 (0) 63 28 (35) 126 35 (91) 0.6 0.6 -Specialist Surgery Divisional CIP Max Fax Bipolar (blank) - - - - - - - - - - - - - - -Length of stay / Ward closures Closure Amber B Pay 802 321 - - 321 (481) 67 22 (45) 134 88 (46) - - -Procurement - other Siemens Audiology Contract Pay 49 - - 49 49 - - - - - - - -ISTC Activity Retention ISTC Activity Retention Ext Income - - - - - - - - - - - - - - -To be identified Total Divisional Target (blank) 106 - - 538 538 432 9 - (9) 18 - (18) - -Specialist Surgery Total 908 370 - 538 908 (0) 76 22 (54) 151 88 (64) - - -12
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTEWomenDivisional CIPBest Practice Tariff - Gynae OPD procedures(MA10z <strong>and</strong> MA21Z)Pay - - - - - - - - - - - - (1.0) - 1.0Ext Income 200 - - - - (200) - - - - - - - - -Unidentified Non-Pay - - 50 50 50 - - - - - -ISH increase in income including due toOlympics Net of all costPay - - - - - - - - - - - - - - -Ext Income - - - - - - - - - - - - - - -Renegotiated contract with BLT Non-Pay 25 25 - - 25 - 2 2 - 4 4 - - - -Terminated psycho sexual contract) Non-Pay 50 50 - - 50 - 4 4 - 8 8 - - - -ISH stopped using Drs lab Non-Pay 10 10 - - 10 - 1 1 - 2 2 - - - -Gynae OPD Productivity Non-Pay - - - - - - - - - - - - - - -Gynae Theatre Productivity Non-Pay 30 - 30 - 30 - - - - - - - - - -Midwifery temp staff removal due to recruitmentPay<strong>and</strong> rota managemnet -17.8 less staff900 800 - 100 900 - 67 67 - 133 133 - 31.5 31.5 -Maternity Consumables Non-Pay 50 - - 50 50 - - - - - - - - - -IT savings in ISH Non-Pay 10 10 - - 10 - 1 1 - 2 2 - - - -ISH Workforce reconfiguration Non-Pay 160 160 - - 160 - 1 1 - 14 14 - - - -HIV - Home Care drugs savings Non-Pay 250 250 - - 250 - 21 42 21 42 42 0 - - -Drugs Savings Non-Pay 25 - 25 - 25 - - - - - - - - - -To be identified Total Divisional Target (blank) 169 - - 319 319 150 21 - (21) 30 - (30) - -Women Total 1,879 1,305 55 519 1,879 - 118 117 (1) 235 205 (30) 30.5 31.5 1.0Children Divisional CIP Best Practice Tariff - Paediatric Diabetes Ext Income - - - - - - - - - - - - - - -Cardiology visiting consultants from GOS Non-Pay - - - - - - - - - - - - - - -PAU Pay - - - - - - - - - - - - - - -Paeds nursing recruitment - temp staffingremovalPay 500 500 - - 500 - 42 83 42 83 83 0 - - -Paediatric Drugs Non-Pay 25 25 - - 25 - - - - - - - - - -Paediatric Consumables Non-Pay 10 10 - - 10 - - - - - - - - - -Remove External Consultancy Non-Pay 110 - - 110 110 18 18 18 18 - -To be identified Total Divisional Target (blank) 170 - - 60 60 (110) 8 - (8) 24 - (24) - -Children Total 705 645 - 60 705 0 49 102 53 107 102 (5) - - -Support Services Divisional CIP Outpatient productivity Pay 200 - - 200 200 - - - - - - - - - -Outpatients - Efficiency Savings Non-Pay - - - - - - - - - - - - - - -Medical Secretaries Pay 80 - - 80 80 - - - - - - - - - -Medical Records Pay - - - - - - - - - - - - - - -To be identified Total Divisional Target Pay 247 - - 247 247 - 21 - (21) 41 - (41) - - -Support Services Total 527 - - 527 527 - 21 - (21) 41 - (41) - - -13
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTESpecialist Medicine Divisional CIPPharmacy Production Unit - MaximiseContributionExt Income 60 - - - - (60) - - - - - - - -Ext Income 60 - - 60 60 - - - - - -Additional Income Radiotherapy Chemotherapy (blank) - - - - - - - - - - - - - - -Therapies In House Non-Pay 30 - - - - (30) 3 - (3) 5 - (5) - -Non-Pay 28 - - 28 28 3 3 3 3 - -Pharmacy Efficiencies - Medicines management Non-Pay 390 - - 135 135 (255) 10 - (10) 20 - (20) - - -Non-Pay 245 - - 245 245 10 10 10 10 - -Junior Doctor B<strong>and</strong>ing Pay 27 - - - - (27) 2 - (2) 5 - (5) - -Pay 27 - - 27 27 2 2 5 5 - -Bone marrow pathway Ext Income 24 - - - - (24) - - - - - - - -Ext Income - 24 - 24 24 - - - - - -Non Pay Drug Saving (Onc Pharm) Non-Pay 100 - - - - (100) 8 - (8) 17 - (17) - -Non-Pay - - - - - - - - - - -Review MDT <strong>and</strong> CRO structure to increasesupport <strong>and</strong> reduce costsExt Income 25 - - - - (25) 2 - (2) 4 - (4) - -Ext Income 25 - - 25 25 2 2 4 4 - -Manpower Planning review Pay 700 - - 650 650 (50) 33 - (33) 67 - (67) 5.0 - (5.0)Outpatient Prescribing Non-Pay 100 - - - - (100) 8 - (8) 17 - (17) - -Non-Pay 100 - - 100 100 8 8 17 17 - -Pharmacy Robot Pay 48 - - - - (48) - - - - - - - -Pay 48 - - 48 48 - - - - - -Wastage Saving Non-Pay 54 - - - - (54) - - - - - - - -Non-Pay 54 - - 54 54 - - - - - -Rapid Arc - Ext Income 100 - 100 - 100 - - - - - - - - - -Therapies Reduction in Premium Cost Pay 160 80 80 - 160 - - - - - - - - - -Agency Bank Reduction - Through on call review Pay 158 - 79 - 79 (79) - - - - - - - - -Pay 79 - - 79 79 - - - - - -To be identified Total Divisional Target (blank) 35 - - 198 198 163 3 - (3) 6 - (6) - -Specialist Medicine Total 2,011 745 283 983 2,011 - 70 25 (45) 139 38 (102) 5.0 - (5.0)14
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTERadiologyDivisional CIPCo-ordination of MRI scanning - ClaustrophobicNon-Paypatients10 10 - - 10 - 1 1 - 2 2 - - - -Dem<strong>and</strong> Management - Through Cross ChargingNon-Payetc Pathology42 - - - - (42) - - - - - - - -Dem<strong>and</strong> Management - Through Cross ChargingNon-Payetc Radiology550 - 200 350 550 - - - - - - - - - -Electronic Request to GPs - Saving on A&C Pay 16 - 16 - 16 - - - - - - - - - -Employment of Additional Radiographers -Reduce outsourcingPay 54 25 - 35 60 6 2 2 (0) 4 4 (0) - - -Employment to full establishment forRadiologistsPay 96 96 - - 96 - 8 8 - 16 16 - - - -Recruitment of CT & MRI Staff Pay 26 - - - - (26) - - - - - - - -Pay 26 - - 26 26 - - - - - -Sign off of remuneration rate towards activitybasedPay - - - - - - - - - - - - - - -Total Implementation of Voice Recognition Non-Pay 16 16 - - 16 - 1 1 - 3 3 - - - -Recruitment Drive for Sonographers Pay 100 100 - - 100 - - - - - - - - - -To be identified Total Divisional Target (blank) - - - 36 36 36 - - - - - - - -Radiology Total 910 273 216 421 910 - 12 12 - 25 25 - - - -PathologyDivisional CIPDem<strong>and</strong> Management - Through Cross ChargingNon-Payetc Pathology98 - 42 98 140 42 - - - - - - - - -Pathology Investment Programme Pay 90 50 40 - 90 - - - - - - - - - -MRSA Screening Pay 75 75 - - 75 - 6 6 - 13 13 - - - -Blood Products Ext Income 50 - - - - (50) 4 - (4) 8 - (8) - -Ext Income 50 - - 50 50 4 4 8 8 - -Pathology Investment Programme - MicroAutomationPay 287 - 150 137 287 - - - - - - - - - -Pathology Investment Programme - OrderCommsPay 45 45 - - 45 - - - - - - - - - -Pathology Investment Programme - OtherWorkforce PlanningPay 38 38 - - 38 - - - - - - - - - -Consultant PAs Pay 60 - - - - (60) 5 - (5) 10 - (10) 0.6 (0.6)Pay 55 - - 55 55 5 5 5 5 - -Bring Vitamin D in house Non-Pay 40 - - - - (40) 3 - (3) 7 - (7) - -Non-Pay 40 - - 40 40 3 3 7 7 - -M.E.S. - Full year effect in 11/12 Non-Pay 50 - - - - (50) 4 - (4) 8 - (8) - -Non-Pay 50 - - 50 50 4 4 8 8 - -To be identified Total Divisional Target (blank) 240 - - 203 203 (37) 20 - (20) 40 - (40) - -Pathology Total 1,073 403 232 438 1,073 - 43 23 (20) 86 41 (45) 0.6 - (0.6)15
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTECorporate Divisional CIP Investment in KGH Bleeps (stbc) Non-Pay 24 - - 24 24 2 2 2 2 - -24 - - - - (24) 2 - (2) 4 - (4) - -McKesson Contract Change Non-Pay 90 45 45 - 90 - - - - - - - - - -Pagers - reduced operating costs Non-Pay 15 - - 15 15 1 1 1 1 - -30 - - - - (30) 3 - (3) 5 - (5) - -Procurement Non-Pay 89 - - - - (89) 7 - (7) 15 - (15) - - -Reduced McKesson Payroll Cost - weekly tomonthly payrollNon-Pay 72 - 72 - 72 - - - - - - - - - -Review of Payphones at KGH Non-Pay 3 - - 3 3 0 0 0 0 - -6 - - - - (6) 1 - (1) 1 - (1) - -Rollover NEPT Contract Non-Pay 60 38 - - 38 (22) 5 6 1 10 6 (4) - - -Consolidation of PCT Transport SLA's Non-Pay 66 - 60 - 60 (6) - - - - - - - - -Reduction to Outturn on Fixtures <strong>and</strong> Fittings(non-capital)Non-Pay 72 36 - - 36 (36) 6 3 (3) 12 3 (9) - - -Reduce Non-Capital Minor Works Non-Pay 30 30 - - 30 - 3 3 - 5 5 - - - -Activity Reduction - NEPT Usage Non-Pay - - - - - - - - - - -Bad Debt Charge Reduction - <strong>2012</strong>1/3 Non-Pay 129 - - - - (129) - - - - - - - -- - - - - - - - - - -Reduced External Consultancy Fees Pay 99 (5) - - (5) (104) 8 (5) (13) 17 (5) (22) - - -Removal of Seconded Staff Pay - - - - - - - - - - - - 1.0 - (1.0)HR - Staff Efficiencies Non-Pay 25 - - 25 25 - - - - - - - - - -E-Rostering - Consolidated Med Staff RotaPlanning SavingsPay 140 - 140 - 140 - - - - - - - - - -R&D Enhanced Income/Cost Efficiency Non-Pay 76 - - - - (76) 6 - (6) 13 - (13) - - -London/Quadrant Room Rduction FYE Non-Pay 39 39 - - 39 - 3 3 - 7 7 - - - -ISTC 3rd Party Income Share Non-Pay 20 20 - - 20 - 2 2 - 3 3 - - - -RO Water Testing Contract FYE Non-Pay 120 120 - - 120 - 10 10 - 20 20 - - - -Goodmayes Rental Non-Pay 86 86 - - 86 - 7 7 - 14 14 - - - -Car Park Expansion - 50 Spaces KGH Ext Income 46 46 - - 46 - 4 4 - 8 8 - - - -Waste Contract Review of Service Spec KGH Non-Pay 40 40 - - 40 - 3 3 - 7 7 - - - -Clinical Engineering Post Reduction - 8d0.5WTEPay 58 58 - - 58 - 5 5 - 10 10 - 0.5 0.5 -Food/Meal Spc Change <strong>Trust</strong>wide FYE Non-Pay 243 243 - - 243 - 20 20 - 41 41 - - - -DOV12 KGH FM Element Non-Pay 50 25 - - 25 (25) 4 - (4) 8 4 (4) - - -Laundry Lease Non-Pay 170 170 - - 170 - 14 14 - 28 28 - - - -Clincal Engineering SLA Non-Pay 8 8 - - 8 - 1 1 - 1 1 - - - -Medical Gases Non-Pay - - - - - - - - - - - - - - -SBS Contract & Debt Mgt Resource Non-Pay 118 108 - - 108 (10) 10 59 49 20 59 39 - - -Pay (67) (67) - - (67) 0 (6) (11) (6) (11) (11) - (2.0) - 2.0Freeze recruitment for first 3months of the yearfor 2wte b<strong>and</strong> 8a Snr MgrsPay 36 36 - - 36 - 21 - (21) 21 - (21) - - -Freeze recruitment for first 3months of the year Pay 29 29 - - 29 - 16 - (16) 16 - (16) - - -Staff member on long term sickness. Will not beback to work for the last six months of the year. Pay 16 16 - - 16 - 7 - (7) 7 - (7) - - -Give up budget as CIPMember of staff retiring. Do not replace 5 monthsPayCIP24 24 - - 24 - 8 - (8) 8 - (8) - - -remove the DBA Pay 33 33 - - 33 - 7 - (7) 7 - (7) 1.0 - (1.0)Medical staffing productivity Recruitment - Temp to Perm Pay - - - - - - - - - - - - - - -Theatre productivity Recruitment - Temp to Perm Pay - - - - - - - - - - - - - - -To be identified Total Divisional Target (blank) 29 - - 544 544 515 2 - (2) 5 - (5) - -Corporate Total 2,106 1,219 317 569 2,105 (1) 179 128 (52) 300 203 (96) 0.5 0.5 -16
Workstream Summary <strong>2012</strong>-13 - May <strong>2012</strong>(all figures in £'000)Division CIP Scheme Scheme Expenditure TypeData12/13 TargetAnnual Statement In Month Statement Ytd StatementGreen Amber Red12-13F-cast12-13VarianceIn MthTargetIn MthDeliveryIn MthVarianceWTE ReductionsYtd Target Ytd Delivery Ytd Variance WTE Target WTE YTD Var WTECentral Divisional CIP Stafflow Pay 506 506 - - 506 - 46 - (46) 46 - (46) - - -Jnr Doctors Rotas Pay 150 150 - - 150 - 14 - (14) 14 - (14) - - -Vacancy Restriction to review up to 100WTErelative to 12/13 budgetsPay - - - - - - - - - - - - - - -CNS Pay - - - - - - - - - - - - - - -SNR Nursing Pay 100 - - 100 100 - 9 - (9) 9 - (9) - - -Pharmacy - 5% Staff Pay 125 - - 125 125 - 11 - (11) 11 - (11) - - -Radiology Pay - - - - - - - - - - - - - - -ARMD Non-Pay 150 - - 150 150 - 14 - (14) 14 - (14) - - -Drugs Non-Pay - - - - - - - - - - - - - - -Management & Admin Pay 250 - - 250 250 - 23 - (23) 23 - (23) - - -Capital Driven Efficiences Non-Pay - - - - - - - - - - - - - - -PMO Driven Efficiences Non-Pay - - - - - - - - - - - - - - -Direct Access Non-Pay - - - - - - - - - - - - - - -Income Opportunities Capital project mgt Non-Pay 500 500 - - 500 - 45 - (45) 45 - (45) - - -Outpatient productivity OP Nursing Pay - - - - - - - - - - - - - - -OP Diagnostics Pay - - - - - - - - - - - - - - -Procurement - other Consumables Non-Pay 292 292 - - 292 - 27 - (27) 27 - (27) - - -Ward Consumables Non-Pay 225 - 225 - 225 - 20 - (20) 20 - (20) - - -Vat on Energy Non-Pay 230 - 230 - 230 - 21 - (21) 21 - (21) - - -Project / External Consultancy Non-Pay 188 - 188 - 188 - 17 - (17) 17 - (17) - - -Bed Contract - KGH (Cap'n) Non-Pay 50 50 - - 50 - 5 - (5) 5 - (5) - - -HCA Non-Pay - - - - - - - - - - - - - - -VAT on IT Managed Service Non-Pay 150 - 150 - 150 - 14 - (14) 14 - (14) - - -A&E A&E KGH @ night Non-Pay 750 - - 750 750 - 68 - (68) 68 - (68) - - -Staff Absence IHB Bookings Sickness cover Pay - - - - - - - - - - - - - - -IHB Bookings Additional Sessions Pay - - - - - - - - - - - - - - -IHB Bookings Additional Resource Pay - - - - - - - - - - - - - - -Procurement automation Procurement Automation Non-Pay 500 250 250 - 500 - 45 - (45) 45 - (45) - - -To be identified Total Divisional Target (blank) 1,392 - - 1,392 1,392 - 127 - (127) 127 - (127) - -Central Total 5,557 1,748 1,043 2,767 5,557 - 505 - (505) 505 - (505) - - -Gr<strong>and</strong> Total 23,155 8,674 2,437 12,043 23,155 0 1,567 550 (1,016) 2,464 900 (1,564) 54.0 46.6 (7.4)17
Workstream Summary <strong>2012</strong>-13 - April <strong>2012</strong>(all figures in £'000)Data12/13 TargetAnnual StatementIn Month StatementDivision CIP Scheme SchemeM<strong>and</strong>ated12-13 12-13 In Mth In MthExpenditure Type Project ManagerY/NGreen Amber RedF-cast Variance Target DeliveryCorporate Divisional CIP Investment in KGH Bleeps (stbc) Y Non-Pay S Adams 24 22 - - 22 (2) 2 - (2)McKesson Contract Change N Non-Pay G Perry 90 45 45 - 90 - - - -Pagers - reduced operating costs Y Non-Pay S Adams 30 - 28 - 28 (3) 3 - (3)Reduced McKesson Payroll Cost - weekly tomonthly payrollN Non-Pay L Malyon 72 - 72 - 72 - - - -Review of Payphones at KGH N Non-Pay S Adams 6 - 6 - 6 (1) 1 - (1)Rollover NEPT Contract N Non-Pay L Kruse 75 75 - - 75 - - - -Consolidation of PCT Transport SLA's N Non-Pay L Kruse 60 - 60 - 60 - 5 - (5)Reduction to Outturn on Fixtures <strong>and</strong>Fittings (non-capital)N Non-Pay J Doyle 72 66 - - 66 (6) 6 - (6)Reduce Non-Capital Minor Works N Non-Pay J Doyle 30 30 - - 30 - 3 3 -Activity Reduction - NEPT Usage N Non-Pay L Kruse 45 - - 45 45 - - - -Bad Debt Charge Reduction - <strong>2012</strong>1/3 N Non-Pay D Wragg 150 - 150 - 150 - - - -Reduced External Consultancy Fees N Pay N Moloney 99 61 - - 61 (38) 8 5 (3)Removal of Seconded Staff N Pay D Wragg - - - - - - - - -HR - Staff Efficiencies N Non-Pay R McAll 25 - - 25 25 - - - -E-Rostering - Consolidated Med Staff RotaPlanning SavingsN Pay G Perry 140 - 140 - 140 - - - -R&D Enhanced Income/Cost Efficiency N Non-Pay J Alcolada 76 - - - - (76) 6 - (6)London/Quadrant Room Rduction FYE N Non-Pay J Doyle 39 39 - - 39 - 3 3 -ISTC 3rd Party Income Share N Non-Pay J Doyle 20 20 - - 20 - 2 2 -RO Water Testing Contract FYE N Non-Pay J Doyle 120 120 - - 120 - 10 10 -Goodmayes Rental N Non-Pay J Doyle 86 86 - - 86 - 7 7 -Car Park Expansion - 50 Spaces KGH N Ext Income J Doyle 46 46 - - 46 - 4 4 -Waste Contract Review of Service SpecN Non-Pay J Doyle 40 40 - - 40 - 3 3 -KGHClinical Engineering Post Reduction - 8dN Pay J Doyle 58 58 - - 58 - 5 5 -0.5WTEFood/Meal Spc Change <strong>Trust</strong>wide FYE N Non-Pay J Doyle 243 243 - - 243 - 20 20 -DOV12 KGH FM Element N Non-Pay J Doyle 50 50 - - 50 - 4 4 -Laundry Lease N Non-Pay J Doyle 170 170 - - 170 - 14 14 -Clincal Engineering SLA N Non-Pay J Doyle 8 8 - - 8 - 1 1 -Medical Gases N Non-Pay J Doyle - - - - - - - - -SBS Contract & Debt Mgt Resource Y Non-Pay A De Swarte 100 92 - - 92 (8) 8 - (8)Pay A De Swarte (60) (55) - - (55) 5 (5) - 5Medical staffing productivity Recruitment - Temp to Perm Y Pay (blank) - - - - - - - - -Theatre productivity Recruitment - Temp to Perm Y Pay (blank) - - - - - - - - -To be identified Total Divisional Target (blank) (blank) (blank) 54 - - 182 182 128 5 - (5)Corporate Total 1,968 1,216 500 252 1,968 (0) 114 81 (33)In MthVariance18
Workstream Summary <strong>2012</strong>-13 - April <strong>2012</strong>(all figures in £'000)Data12/13 TargetAnnual StatementIn Month StatementDivision CIP Scheme SchemeM<strong>and</strong>ated12-13 12-13 In Mth In MthExpenditure Type Project ManagerY/NGreen Amber RedF-cast Variance Target DeliveryCentral Divisional CIP Stafflow N Pay (blank) 506 506 - - 506 - - - -Jnr Doctors Rotas N Pay (blank) 150 150 - - 150 - - - -Vacancy Restriction to review up to 100WTErelative to 12/13 budgetsN Pay (blank) - - - - - - - - -CNS N Pay (blank) - - - - - - - - -SNR Nursing N Pay (blank) 100 - - 100 100 - - - -Pharmacy - 5% Staff N Pay (blank) 125 - - 125 125 - - - -Radiology N Pay (blank) - - - - - - - - -ARMD N Non-Pay (blank) 150 - - 150 150 - - - -Drugs N Non-Pay (blank) - - - - - - - - -Management & Admin N Pay (blank) 250 - - 250 250 - - - -Capital Driven Efficiences N Non-Pay (blank) - - - - - - - - -PMO Driven Efficiences N Non-Pay (blank) - - - - - - - - -Direct Access N Non-Pay (blank) - - - - - - - - -Income Opportunities Capital project mgt N Non-Pay (blank) 500 500 - - 500 - - - -Outpatient productivity OP Nursing N Pay (blank) - - - - - - - - -OP Diagnostics N Pay (blank) - - - - - - - - -Procurement - other Consumables N Non-Pay (blank) 292 292 - - 292 - - - -Ward Consumables N Non-Pay (blank) 225 - 225 - 225 - - - -Vat on Energy N Non-Pay (blank) 230 - 230 - 230 - - - -Project / External Consultancy N Non-Pay (blank) 188 - 188 - 188 - - - -Bed Contract - KGH (Cap'n) N Non-Pay (blank) 50 50 - - 50 - - - -HCA N Non-Pay (blank) - - - - - - - - -VAT on IT Managed Service N Non-Pay (blank) 150 - 150 - 150 - - - -A&E A&E KGH @ night N Non-Pay (blank) 750 - - 750 750 - - - -Staff Absence IHB Bookings Sickness cover N Pay (blank) - - - - - - - - -IHB Bookings Additional Sessions N Pay (blank) - - - - - - - - -IHB Bookings Additional Resource N Pay (blank) - - - - - - - - -Procurement automation Procurement Automation N Non-Pay (blank) 500 250 250 - 500 - - - -To be identified Total Divisional Target (blank) (blank) (blank) 1,604 - - 1,604 1,604 - 134 - (134)Central Total 5,769 1,748 1,043 2,979 5,769 - 134 - (134)In MthVarianceGr<strong>and</strong> Total 23,145 8,693 4,231 10,221 23,145 0 1,027 355 (672)19
6. Business Unit SummariesBelow are the summaries for each of the Clinical Business Units. They show the Direct Central Income position <strong>and</strong> their local Income <strong>and</strong> Expenditureposition, giving an overall Net Deficit (+) / Surplus (‐) position. All Income is shown as a credit (‐) <strong>and</strong> all variances are expressed as Adverse (‐) or Favourable(+). This is not an SLR report as none of the central income has been apportioned out to the activities that are supporting it, rather it represents where theincome is coded to. They do show the movement in the relation ship between coded income <strong>and</strong> expenditure between current year to date <strong>and</strong> prior yearaverage for expenditure <strong>and</strong> actual reported income.Anaesthetics.Description 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthAnaesthetics(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Critical Care 2,144 2,121 (18,634) (2,679) (29) 2,485 2,194 (3,264) (3,042) (222) 19,583Daycases 275 324 (1,865) (270) 41 409 388 (334) (330) (4) 2,023Devices & Drugs - - (6) 0 - - (18) (44) 26 107Elective 5 - (24) (4) 6 - (5) (3) (2) 28Non Elective - - (7) 0OP First Attendances 515 311 (470) (57) (37) 442 432 (84) (85) 1 506OP Follow Ups 272 120 (142) (11) (15) 206 295 (21) (25) 3 130OP Procedures 0 - (0)Direct Central ActivityIncome3,211 2,876 (21,148) (3,017) (45) 3,549 3,309 (3,726) (3,529) (197) 22,377Divisional/Local income (1,112) (169) (16) (174) (161) (13) (1,041)Pay- Permanent 529.29 29,272 4,377 502 602.28 538.17 5,176 4,529 647 31,056- Bank 42.88 772 589 (461) - 49.02 10 664 (653) 63- Agency 16.70 165 200 (172) 6.24 12.39 98 188 (90) 154Pay Total 588.87 30,209 5,166 (132) 608.52 599.58 5,285 5,381 (96) 31,273Non Pay 10,559 2,018 (258) 1,894 1,961 (67) 11,332CIP / Turnaround Target 0 (249) - (249) (1,690)Net Divisional I&E 39,656 7,015 (406) 6,756 7,181 (425) 39,875Net Deficit 18,508 3,998 (450) 3,030 3,653 (622) 62,25220
Specialist SurgeryDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthSpecialist Surgery(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Daycases 1,402 1,127 (9,984) (1,136) (268) 1,540 1,505 (1,673) (1,669) (4) 10,119Devices & Drugs - - (344) (39) 39 - - (89) (71) (17) 532Elective 274 226 (6,048) (851) (169) 249 241 (965) (959) (6) 5,835Non Elective 560 455 (7,796) (1,250) (208) 486 539 (1,188) (1,328) 140 7,129OP First Attendances 6,694 5,863 (6,122) (879) (111) 6,203 7,118 (905) (953) 48 5,474OP Follow Ups 10,985 11,825 (6,397) (1,013) 72 10,843 12,862 (936) (997) 60 5,662OP Procedures 1,726 1,748 (1,691) (289) (1) 1,710 1,787 (280) (292) 12 1,693Other 2,632 2,692 (3,528) (271) 0 2,454 2,256 (600) (553) (47) 3,602Regular Day Attenders 1 2 (3) (1) 1XBD 340 239 (486) (65) (28) 314 226 (85) (71) (14) 512Direct Central ActivityIncome24,615 24,179 (42,399) (5,796) (672) 23,799 26,534 (6,721) (6,892) 172 40,558Divisional/Local income (943) (151) (6) (158) (142) (16) (945)Pay- Permanent 220.90 14,251 2,090 285 258.90 230.36 2,530 2,248 282 15,227- Bank 11.26 359 205 (145) - 16.74 - 210 (210) -- Agency 7.05 62 114 (104) 0.15 3.60 1 57 (56) 7Pay Total - 239.21 14,672 2,409 36 259.05 250.70 2,531 2,516 15 15,234Non Pay - 2,698 419 31 456 427 29 2,728CIP / Turnaround Target 0 (64) - (64) (587)Net Divisional I&E 16,427 2,677 61 2,766 2,801 (36) 16,430Net Deficit (25,972) (3,118) (612) (3,955) (4,091) 136 56,98721
SurgeryDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthSurgery(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WT E) WTE)£000 £000 £000 £000Daycases 1,880 1,750 (6,981) (1,062) (109) 1,758 1,916 (985) (1,059) 74 5,960Devices & Drugs - - 631 (23) 23 - - (60) (73) 12 361Elective 611 572 (9,726) (1,540) 12 626 610 (1,650) (1,596) (54) 9,982Non Elective 1,187 1,314 (16,569) (2,804) 263 1,290 1,118 (2,751) (2,522) (229) 16,504OP First Attendances 3,177 3,282 (4,287) (684) 12 3,201 3,649 (654) (682) 28 3,955OP Follow Ups 5,590 5,528 (3,974) (618) (30) 5,184 6,070 (571) (596) 25 3,456OP Procedures 387 285 (1,058) (92) (61) 476 550 (120) (122) 2 724Other - - (280) (25) 0 - - (181) (328) 147 1,087Regular Day Attenders 95 117 (132) (27) 6 94 84 (38) (37) (1) 227XBD 531 595 (842) (140) (0) 493 402 (129) (115) (14) 779Direct Central ActivityIncome13,458 13,443 (43,218) (7,013) 114 13,122 14,400 (7,140) (7,130) (9) 43,035Divisional/Local income (1,680) (294) 14 (292) (282) (10) (1,749)Pay- Permanent 331.99 18,805 2,825 309 364.02 333.00 3,046 2,810 236 18,259- Bank 46.10 (4,506) 310 (1,061) 1.00 33.67 11 261 (250) 162- Agency 5.96 - 71 (71) - 2.92 2 29 (27) 13Pay Total - 384.05 14,300 3,205 (822) 365.02 369.59 3,060 3,100 (41) 18,434Non Pay - 2,102 337 13 352 337 15 2,107CIP / Turnaround Target 0 (91) - (91) (506)Net Divisional I&E 14,721 3,249 (795) 3,029 3,155 (127) 18,285Net Deficit (28,497) (3,764) (681) (4,111) (3,975) (136) 61,320MedicineDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthMedicine(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Daycases 1,562 2,015 (8,734) (1,310) 290 2,130 2,319 (1,482) (1,549) 67 8,964Devices & Drugs - - (115) (1) 1 - - (180) (172) (8) 1,080Elective 92 96 (1,052) (183) 17 92 92 (185) (170) (15) 1,117Non Elective 3,510 4,250 (61,608) (9,955) 1,386 3,927 4,376 (8,840) (9,722) 882 53,038OP First Attendances 3,195 4,005 (5,264) (879) 112 3,521 3,515 (864) (863) (1) 5,228OP Follow Ups 7,330 7,842 (5,759) (920) 49 7,671 7,763 (863) (849) (14) 5,218OP Procedures 813 98 (664) (15) (112) 842 772 (146) (140) (5) 881Other 1,448 2,205 33 (317) (23) 2,065 1,940 (130) (123) (7) 781Regular Day Attenders 1 - (6) (0) 1 - () () () 2XBD 3,734 3,164 (6,268) (758) (196) 3,475 2,077 (892) (638) (254) 5,354Direct Central ActivityIncome21,684 23,674 (89,436) (14,338) 1,523 23,723 22,854 (13,581) (14,226) 645 81,663Divisional/Local income (5,579) (903) (27) (844) (817) (27) (5,001)Pay- Permanent 837.51 41,353 6,108 784 913.69 810.35 6,735 5,968 767 40,038- Bank 133.69 180 813 (783) 4.93 118.62 (10) 741 (751) (1,161)- Agency 23.19 611 379 (277) 10.25 20.14 110 319 (209) 525Pay Total - 994.39 42,145 7,300 (276) 928.87 949.11 6,835 7,028 (193) 39,402Non Pay - 7,117 1,262 (75) 1,234 1,202 32 7,328CIP / Turnaround Target 0 (20) - (20) (120)Net Divisional I&E 43,683 7,659 (378) 7,205 7,413 (208) 41,609Net Deficit (45,753) (6,679) 1,145 (6,376) (6,813) 437 123,27222
Emergency CareDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthEmergency care(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000A<strong>and</strong>E 27,887 30,738 (19,761) (3,102) 228 35,330 36,809 (3,424) (3,450) 26 20,545Ambulatory Care 333 484 (953) (145) 45 510 578 (150) (157) 6 902Daycases - - (1) 0Elective 7 4 (93) (4) (8) 12 - (21) (12) (9) 130Non Elective 964 1,338 (5,656) (970) 258 1,379 1,306 (1,070) (1,094) 23 6,421OP First Attendances 558 518 (258) (48) (4) 477 503 (57) (57) 346OP Follow Ups 49 48 (30) (5) (0) 38 56 (1) (2) 9Other - - (243) (28) 0 - - (28) (28) 169XBD 3 - (116) (1) 0 - () () ()Direct Central ActivityIncome29,801 33,130 (27,111) (4,303) 518 37,746 39,252 (4,753) (4,800) 47 28,522Divisional/Local income (769) (101) (27) (119) (104) (16) (688)Pay- Permanent 455.78 25,791 3,375 923 555.28 477.62 4,537 3,638 900 27,182- Bank 44.68 91 362 (346) 7.42 45.01 77 375 (298) 461- Agency 48.17 1,872 996 (684) 28.34 54.13 544 1,187 (643) 2,823Pay Total - 548.63 27,755 4,733 (107) 591.04 576.76 5,159 5,200 (41) 30,466Non Pay - 2,788 515 (50) 505 492 14 3,002CIP / Turnaround Target 0 (111) - (111) (667)Net Divisional I&E 29,774 5,147 (184) 5,434 5,588 (154) 32,113Net Deficit 2,663 844 334 681 788 (107) 60,635NeurosciencesDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthNeurosciences(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Daycases 42 61 (413) (57) 1 70 72 (73) (60) (12) 439Devices & Drugs - - (1,679) (338) 29 - - (298) (254) (44) 1,791Elective 147 168 (3,344) (643) 26 147 166 (679) (706) 27 4,110Non Elective 299 374 (9,822) (1,629) 66 388 373 (1,678) (1,575) (103) 10,067OP First Attendances 1,138 890 (1,794) (223) (90) 1,046 1,135 (322) (339) 17 1,950OP Follow Ups 1,549 1,611 (1,480) (199) (14) 1,643 1,895 (250) (263) 13 1,513OP Procedures 228 337 (292) (47) 14 365 292 (54) (49) (5) 326Other 899 1,333 (8,092) (1,459) 241 1,078 936 (1,301) (1,303) 2 7,804XBD 603 385 (794) (97) (68) 571 22 (153) (42) (111) 923Direct Central ActivityIncome4,905 5,158 (27,711) (4,692) 206 5,308 4,891 (4,809) (4,592) (217) 28,923Divisional/Local income (935) (123) (33) (90) (108) 19 (538)Pay- Permanent 201.45 11,252 1,685 191 229.42 198.77 1,967 1,757 210 11,804- Bank 31.32 66 199 (188) 4.74 29.05 28 179 (151) 167- Agency 4.75 - 81 (81) 1.49 4.48 (48) 65 (113) (386)Pay Total - 237.52 11,318 1,965 (78) 235.65 232.30 1,947 2,001 (54) 11,584Non Pay - 2,789 430 35 438 411 27 2,624CIP / Turnaround Target 0 (24) - (24) (146)Net Divisional I&E 13,171 2,271 (76) 2,272 2,304 (33) 13,523Net Deficit (14,539) (2,421) 130 (2,537) (2,288) (249) 42,44623
PathologyDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthPathology(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Direct Access 738,864 754,371 (10,274) (1,644) 3 783,818 749,546 (1,653) (1,530) (123) 9,918Direct Central ActivityIncome738,864 754,371 (10,274) (1,644) 3 783,818 749,546 (1,653) (1,530) (123) 9,918Divisional/Local income (1,162) (139) (55) (139) (125) (15) (835)Pay- Permanent 276.99 14,106 2,261 90 286.88 278.02 2,325 2,284 41 13,656- Bank 2.04 68 17 (5) - 4.07 - 24 (24) -- Agency 6.01 (404) 68 (136) - 3.89 (13) 38 (50) (75)Pay Total - 285.04 13,770 2,346 (51) 286.88 285.98 2,313 2,347 (34) 13,581Non Pay - 8,281 1,348 32 1,394 1,530 (136) 8,363CIP / Turnaround Target 0 (56) - (56) (598)Net Divisional I&E 20,888 3,555 (74) 3,511 3,752 (240) 20,510Net Deficit 10,614 1,911 (71) 1,858 2,222 (364) 30,428RadiologyDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthRadiology(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WT E) WTE)£000 £000 £000 £000Breast Screening 3,370 3,794 (2,221) (376) 42 3,774 3,878 (374) (384) 10 2,241Devices & Drugs (1,189) 0 - - (161) (302) 141 968Direct Access 14,049 14,297 (3,985) (637) 38 14,679 13,920 (650) (645) (5) 3,900OP First Attendances 397 33 (38) (5) (61) 36 45 (6) (6) 1 36OP Follow Ups 87 - (7)OP Procedures 12 - (3)Radiotherapy 3,263 3,190 (2,977) (530) (12) 3,169 3,308 (643) (645) 2 3,860Other (163) 0Direct Central ActivityIncome21,177 21,314 (10,571) (1,547) (4) 21,657 21,151 (1,834) (1,983) 148 11,005Divisional/Local income (395) (67) 1 (67) (62) (5) (400)Pay- Permanent 248.03 13,867 2,088 224 283.68 256.21 2,599 2,130 469 15,467- Bank 11.22 27 183 (178) - 20.36 - 242 (242) -- Agency 10.83 155 314 (289) - 13.86 - 356 (356) -Pay Total - 270.08 14,048 2,585 (243) 283.68 290.43 # 2,599 2,728 (129) 15,467Non Pay - 2,964 569 (75) 548 654 (106) 3,273CIP / Turnaround Target 0 1 - 1 (620)Net Divisional I&E 16,617 3,087 (317) 3,081 3,320 (239) 17,720Net Deficit 6,046 1,539 (321) 1,247 1,337 (90) 28,72524
Specialist MedicineDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthSpecialist Medicine(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Daycases 357 355 (1,713) (217) (7) 411 479 (254) (275) 20 1,539Devices & Drugs - - (511) (91) 21 - - (920) (867) (52) 5,519Direct Access 4,221 4,625 (1,234) (254) 22 5,942 5,710 (205) (196) (9) 1,231Elective 34 28 (290) (25) (26) 34 24 (59) (56) (2) 355Non Elective 129 171 (3,330) (509) 125 185 170 (536) (524) (12) 3,215OP First Attendances 3,200 2,564 (3,364) (476) (121) 2,803 3,007 (533) (538) 5 3,223OP Follow Ups 13,997 15,607 (7,471) (1,172) 63 14,413 16,170 (1,072) (1,120) 48 6,482OP Procedures 108 1,256 (753) (118) 101 1,382 1,417 (124) (129) 5 751Other - - (326) (115) (7) - - (132) (147) 15 792Regular Day Attenders 1,892 2,009 (4,956) (771) (5) 2,172 2,016 (875) (844) (31) 5,252XBD 176 506 (332) (123) 77 131 91 (35) (32) (3) 209Direct Central ActivityIncome24,114 27,120 (24,281) (3,872) 244 27,472 29,084 (4,744) (4,729) (15) 28,566Divisional/Local income (5,661) (1,137) 194 (1,182) (1,072) (110) (7,090)Pay- Permanent 546.32 27,092 4,101 414 591.95 558.98 4,534 4,196 338 27,254- Bank 17.50 5 118 (117) - 15.87 - 100 (100) -- Agency 22.18 (494) 270 (353) - 24.56 - 253 (253) -Pay Total - 586.00 26,602 4,489 (56) 591.95 599.41 4,534 4,549 (15) 27,254Non Pay - 19,280 3,530 (317) 3,591 3,478 113 21,598CIP / Turnaround Target 0 (114) - (114) (1,960)Net Divisional I&E 40,222 6,882 (179) 6,829 6,955 (126) 39,802Net Deficit 15,941 3,011 65 2,085 2,226 (141) 68,368ChildrenDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthChildren(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Critical Care 2,025 1,856 (7,502) (1,133) (133) 2,020 2,096 (1,212) (1,311) 99 7,271Daycases 38 83 (594) (69) 42 114 99 (87) (79) (9) 528Devices & Drugs (6) 0 - - (20) (25) 5 119Elective 8 17 (155) (30) 20 14 13 (25) (42) 18 148Non Elective 2,361 2,617 (11,841) (1,646) 245 2,837 2,329 (1,898) (1,605) (293) 11,389OP First Attendances 807 712 (1,250) (182) (20) 800 1,361 (216) (276) 60 1,305OP Follow Ups 1,465 1,158 (1,028) (168) (37) 1,120 1,286 (173) (186) 13 1,048Other - - 208 (129) (0) - - (210) (210) 1,260Regular Day Attenders 60 43 (17) (4) (28) 61 66 (25) (26) 152XBD 128 979 (713) (167) 125 435 360 (139) (119) (20) 835Direct Central ActivityIncome6,892 7,465 (22,897) (3,528) 214 7,402 7,610 (4,005) (3,877) (128) 24,056Divisional/Local income (1,136) (161) (28) (162) (154) (8) (973)Pay- Permanent 217.88 12,117 1,962 58 256.44 217.63 2,339 2,045 294 14,035- Bank 25.86 279 223 (176) - 21.78 16 173 (156) 98- Agency 9.74 (33) 141 (146) - 3.92 - 66 (66) -Pay Total - 253.48 12,363 2,325 (265) 256.44 243.33 2,355 2,284 71 14,132Non Pay - 1,029 211 (40) 164 210 (46) 950CIP / Turnaround Target 0 (5) - (5) (60)Net Divisional I&E 12,257 2,376 (333) 2,352 2,340 12 14,050Net Deficit (10,640) (1,152) (119) (1,653) (1,537) (116) 38,10625
Support ServicesDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthSupport Services(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Average Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE) £000 £000 £000 £000Direct Central ActivityIncome- - - 0 - 0 0.00 0.00 0Divisional/Local income (123) (22) 2 (25) (20) (5) (147)Pay- Permanent 346.44 10,832 1,596 209 369.39 368.14 1,727 1,699 28 10,361- Bank 31.44 (299) 117 (167) - 17.55 (0) 72 (72) -- Agency 3.31 - 14 (14) - - - 0 (0) -Pay Total - 381.19 10,532 1,727 28 369.39 385.69 1,727 1,771 (45) 10,361Non Pay - 399 69 (3) 65 67 (2) 391CIP / Turnaround Target 0 (42) - (42) (528)Net Divisional I&E 10,809 1,774 27 1,725 1,819 (94) 10,077Net Deficit 10,809 1,774 27 1,725 1,819 (94) 10,077WomenDescription 2011/12 2011/12 2011/12 2011/12 2011/12 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13 <strong>2012</strong>/13YTDActualIn Month In monthWomen(Activity / AnnualBudget ActualYTD YTD AnnualYTD Budget Av e rage Budget Actual Varianc (Activity (Activity / YTD Budget Actual Variance BudgetActivity WTE) £000 £000 e £000 / WTE) WTE)£000 £000 £000 £000Daycases 582 516 (2,739) (457) (45) 542 470 (399) (372) (27) 2,414Devices & Drugs (36) 0Elective 130 126 (1,855) (297) (12) 130 125 (292) (295) 4 1,765HIV Contract - - (4,316) (719) 0 - - (711) (711) 4,264Non Elective 2,144 2,285 (24,887) (4,188) 305 2,143 2,137 (3,782) (3,765) (17) 22,692OP First Attendances 8,318 9,172 (8,463) (1,377) 132 8,886 9,223 (1,320) (1,322) 2 7,983OP Follow Ups 17,829 20,494 (9,691) (1,532) 187 18,035 21,911 (1,332) (1,411) 79 8,057OP Procedures 694 736 (876) (151) 10 721 678 (155) (158) 3 936Other 7,647 8,138 (2,917) (418) 24 7,574 8,014 (381) (403) 22 2,287XBD 149 112 (389) (47) (13) 134 90 (55) (41) (15) 333Direct Central ActivityIncome37,493 41,579 (56,168) (9,187) 587 38,165 42,649 (8,427) (8,478) 51 50,732Divisional/Local income (2,303) (387) 3 (380) (374) (6) (2,281)Pay- Permanent 604.54 30,201 4,699 335 655.54 591.40 5,047 4,657 390 30,911- Bank 59.95 (160) 410 (436) 2.50 59.52 117 403 (287) 990- Agency 31.44 10 421 (420) - 8.46 - 153 (153) -Pay Total 695.93 30,051 5,530 (521) 658.04 659.38 5,164 5,212 (49) 31,901Non Pay 5,956 1,106 (113) 1,074 1,102 (28) 6,444CIP / Turnaround Target 0 (30) - (30) (574)Net Divisional I&E 33,705 6,249 (631) 5,827 5,940 (112) 35,490Net Deficit (22,464) (2,938) (44) (2,600) (2,538) (61) 86,22126
7. BALANCE SHEETCurrent Previous Last(£m) Period Period Yr EndMay-12 Apr-12 Mar-12Non-current assets £390.4 £387.5 £389.1Current assetsInventories £5.8 £5.8 £7.0Trade <strong>and</strong> other receivables £37.3 £55.8 £29.5Cash <strong>and</strong> cash equivalents £26.6 £11.2 £2.8£69.6 £72.8 £39.3Current liabilitiesTrade <strong>and</strong> other payables (£79.6) (£79.8) (£48.2)PFI \ Borrowings (£6.3) (£6.3) (£5.5)Provisions (£1.9) (£2.1) (£1.8)Net current assets/(liabilities) (£18.2) (£15.4) (£16.2)Non-current liabilities:PFI \ Borrowings (£257.1) (£257.1) (£259.9)Trade <strong>and</strong> other payables (£4.9) (£4.9) (£4.9)Provisions (£5.8) (£5.6) (£5.0)Total assets employed £104.5 £104.5 £103.0Financed by taxpayers' equity:Public dividend capital £365.7 £365.7 £307.3Retained Earnings - P&L (£272.7) (£271.5) (£216.4)Retained Earnings - Donated Assets - - -Revaluation reserve £11.5 £10.3 £11.3Donated asset reserve £0.0 £0.0 £0.8Total taxpayers' equity £104.5 £104.5 £103.0• oCurrent Prior LastKPIs Period Period Yr EndMay-12 Apr-12 Mar-12Average Debtors days 18 21 21Debtors >90 days (£'000s) £451 £776 £592Debtors >180 days (£'000s) £1,023 £823 £1,536Debtors >365 days (£'000s) £2,104 £2,021 £2,825Total Bad Debt Provision (£'000s) £2,521 £2,431 £1,926>365 days provided (£'000s) £1,857 £1,755 £1,293Average creditor days 54 80 58Current ratio 74% 78% 71%Better payment practice code performance:- Non-NHS- Volume - paid on time 3,127 1,659 2,773- Volume - % paid on time 66.19% 82.66% 27.96%- Value - paid on time (£'000s) £7,167.00 £16,910.00 £5,150- Value - % paid on time 75.70% 98.34% 35.85%- NHS- Volume - paid on time 65 7 316- Volume - % paid on time 34.95% 22.58% 34.39%- Value - paid on time (£'000s) £170 £116 £1,630- Value - % paid on time 22.13% 6.06% 30.52%Key points:• The overall balance sheet position shows an increase of £15m in cash <strong>and</strong> cash equivalentscompared with April <strong>2012</strong>. This is from the reduction in debtors with PCT’s paying June’sSLA invoices in advance. The cash balance has been left in order to pay the PFI invoice in<strong>July</strong>.Key points:• Average creditor days decreased from 80 in April to 54in May. The reason for this is due to the PCT’s payingfurther invoices in advance to enable creditors to bepaid.27
8. CAPITAL AND CASHFLOWo2Summary Cashflow - Year to date£000'sOperating Deficit (4,300)Interest Paid (6,164)PDC Dividend Paid 0Interest received 10Impairments (1,786)Transfers -Net I&E deficit (cash impact) (12,240)Capital Programme SummaryMay-12TotalApproved <strong>2012</strong>-13TotalProposed <strong>2012</strong>-13TotalFunding<strong>2012</strong>-13YTDExpenditureInternally Funded AssetsMedical Equipment 1,282 2,130 3,412 829IT – Hardware 1,119 659 1,778 343IT – S o ftwa re 0 0 0 36Other Plant & Machinery 500 0 500 0E s ta te s 2,782 382 3,164 259sub-Total 5,683 3,171 8,854 1,467Depreciation <strong>and</strong> Amortisation 2,373Movements in working balances:Decrease in Inventories 53Increase in Trade <strong>and</strong> Other Receivables 207Increase in Trade <strong>and</strong> Other Payables 36,611Decrease in Provisions (11)- sub-total 26,993Capital expenditure (3,467)Revenue Rental Income 207Net cashflow before financing 23,733Capital Element of Finance Leases <strong>and</strong> PFI (1,488)Loans repaid -Public Dividend Capital Received -Externally Funded AssetsP a tho lo g y 4,194 900 5,094 208SAN 967 0 967 249MLU 2,576 0 2,576 51Access Funded Assets 117 0 117 11sub-Total 7,854 900 8,754 519<strong>Trust</strong> Variation Enquiries 0 2,966 2,966 161Total <strong>Trust</strong> - Funded 13,538 7,037 20,575 2,146Subject to External Approval & FundingCardiac Cath Lab 0 1,700 1,700 0CT Scanners 0 2,000 2,000 0A&E Reconfiguration 0 3,000 3,000 0Digital Mammography 0 1,548 1,548 0PAS Replacement 0 10,000 10,000 0sub-Total 0 18,248 18,248 0Total Capital Plan to Date 13,538 25,285 38,823 2,146Net Increase/(Decrease) in Cash <strong>and</strong> CashEquivalents22,246Opening cash balance 4,343Closing cash balance 26,589Cashflow - Key points:• The year to date cash deficit arising from the I&E position st<strong>and</strong>s at £12,240k.• The closing cash balance has increased to £26,589 as the <strong>Trust</strong> is building upfunds to pay the next PFI instalment in <strong>July</strong>.• The increase in trade payables includes the £23m PCT advances, which wasreceived close to Month end, accounting for the high closing cash balances.Total <strong>Trust</strong> Submitted Plan 40,011Balance to Submitted Plan 1,188Assets to be Considered via Charitable FunDa Vinci Robot 0 2,400 2,400Capital - Key points:• Year to date capital expenditure is £2,146k• Subject to external funding is £25,285k which has yet to be finalised.The additional funding is required for the <strong>Trust</strong> reconfigurationFoundation <strong>Trust</strong> application.28
9. Financial Risk Rating (Using Dept of Health’s risk b<strong>and</strong>ings between 1.0 <strong>and</strong> 3.0 where riskier organisations score closer to 1)The weighted financial risk score for May is 1.38, (April 1.55). Although creditor days has improved the score by 0.05, the score as a whole worsens inmonth because the operating deficit to date now exceeds 2% of planned income. April’s rating would have been artificially high.Overall movement in Risk Rating29
Appendix 7Financial indicators for acute & ambulance trusts : BHRUT May 12SCORINGCriteriaInitial PlanningMetricPlanned Outturn as a proportion ofTurnoverFormula for organisations with aplanned operating breakeven orsurplusSHA expected operating surplus orbreakeven -planned operating surplus or breakevenPlanned IncomeFormula for organisations with aplanned operating deficitx 100 x 100Planned operating deficitPlanned IncomeWeight (%)5 5Measure-9.4%3 2 1Planned operating breakeven or surplus that iseither equal to or at variance to SHAexpectations by no more than 3% of income.Any operating deficit less than 2% of income ORan operating surplus/breakeven that is atvariance to SHA expectations by more than 3%of planned income.Operating deficit more than or equal to 2% ofplanned incomeBHRUTBHRUT RawWeightedScore APR 12Score APR 1210.05Year to DateYTD Operating PerformanceFormula for organisations with a YTD Formula for organisations with a YTDactual operating breakeven or surplus actual operating deficitYTD planned operating breakeven/surplus/deficit - YTD actual operatingbreakeven or surplusForecast Incomex 100YTD operating deficitForecast Incomex 1002520-2.6%YTD operating breakeven or surplus that iseither equal to or at variance to plan by no morethan 3% of forecast income.Any operating deficit less than 2% of income ORan operating surplus/breakeven that is atvariance to plan by more than 3% of forecastincome.Operating deficit more than or equal to 2% offorecast income10.20YTD EBITDAYTD EBITDAActual YTD Incomex 1005-5.5%Year to date EBITDA equal to or greater than 5%of actual year to date incomeYear to date EBITDA equal to or greater than1% but less than 5% of year to date incomeYear to date EBITDA less than 1% of actual yearto date income.10.05Forecast OutturnForecastForecast Operating PerformanceEBITDAFormula for organisations with aforecast operating breakeven orsurplusPlanned operating breakeven/surplus/deficit - Forecast operatingbreakeven or surplusForecast Incomex100Forecast EBITDAForecast IncomeFormula to be used for organisationswith a forecast operating deficitForecast operating deficitForecast Incomex100x 10040205-9.9%-0.4%Forecast operating breakeven or surplus that iseither equal to or at variance to plan by no morethan 3% of forecast income.Forecast EBITDA equal to or greater than 5% offorecast income.Any operating deficit less than 2% of income ORan operating surplus/breakeven that is atvariance to plan by more than 3% of income.Forecast EBITDA equal to or greater than 1%but less than 5% of forecast income.Operating deficit more than or equal to 2% ofincomeForecast EBITDA less than 1% of forecastincome.110.200.05Rate ofChange inForecastSurplus orDeficit.(Current period forecast surplus/deficit) - (Prior period forecast surplus/deficit)Forecast Incomex 100150.0%Forecasting an operating deficit with aStill forecasting an operating surplus with amovement less than 2% of forecast income ORmovement equal to or less than 3% of forecastan operating surplus movement more than 3% ofincomeincome.Forecasting an operating deficit with amovement of greater than 2% of forecastincome.20.30Underlying FinancialPositionUnderlyingPosition %EBITDA Margin (%)Underlying Breakeven/Surplus/DeficitUnderlying IncomeUnderlying EBITDAUnderlying Incomex 100510x 100 5-12.7%3.1%Underlying breakeven or SurplusUnderlying EBITDA equal to or greater than 5%of underlying incomeAn underlying deficit that is less than 2% ofunderlying income.Underlying EBITDA equal to or greater than 5%but less than 1% of underlying incomeAn underlying deficit that is greater than 2% ofunderlying incomeUnderlying EBITDA less than 1% of underlyingincome110.050.05Processes & Balance Sheet EfficiencyBetter BetterPayment PaymentDebtor Days Current Ratio Practice PracticeCode Volume Code Value%%Value of ALL Bills paid within targetValue of ALL Bills paid within the yearVolume of ALL Bills paid within targetVolume of ALL Bills paid within the yearDebtors as at current periodForecast Incomex 100x 100Current AssetsCurrent Liabilities202.52.5561%54%0.7495% or more of the value of NHS <strong>and</strong> Non NHSbills are paid within 30days95% or more of the volume of NHS <strong>and</strong> NonNHS bills are paid within 30daysLess than 95% but more than or equal to 60% ofthe value of NHS <strong>and</strong> Non NHS bills are paidwithin 30daysLess than 95% but more than or equal to 60% ofthe volume of NHS <strong>and</strong> Non NHS bills are paidwithin 30daysLess than 60% of the value of NHS <strong>and</strong> NonNHS bills are paid within 30 daysLess than 60% of the volume of NHS <strong>and</strong> NonNHS bills are paid within 30 daysCurrent ratio is anything less than 1 <strong>and</strong> greaterCurrent Ratio is equal to or greater than 1. A current ratio of less than 0.5than or equal to 0.5Debtor days greater than 30 <strong>and</strong> less than orx365 518Debtor days less than or equal to 30 daysDebtor days greater than 60equal to 60 days2 0.051 0.032 0.103 0.1530
EXECUTIVE SUMMARYTITLE:Workforce Key Performance IndicatorsBOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong> & TEC1. KEY ISSUES: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:• For the month of May <strong>2012</strong> the overall number ofFTE's in post across the <strong>Trust</strong> increased by31.13 FTE's on the April position <strong>and</strong> hasincreased by 185.40 FTE's across the 12 monthperiod.• The number of starters in month was 49.48FTE's compared to 45.04 FTE's in the previousmonth. Following a period of focussedrecruitment activity, a total of 617.99 FTE's havestarted in the <strong>Trust</strong> since June 11. Maydemonstrated another decrease in the number ofleavers with 32.33 fte leavers compared to 45.83in April.• Starters & leavers data analysis over the sameperiod differs from the staff in post growth for thesame 3 reasons as in previous reports.1. If new starters commence employment or leaveafter the payroll cut off date (midmonth) they will notbe entered or removed onto/off ESR until month end– therefore they will not appear on the staff in postreport generated from ESR until the following month.2. Staff who increase or decrease their hours willaffect the reported FTE’s in post but not the starters<strong>and</strong> leavers3. Timliness of managers completing <strong>and</strong> submittingthe appropriate forms to HR - for entering onto ESR.• In addition to the overall <strong>Trust</strong> Bank & Agencyspend increasing by £713,527 in month, dataalso shows that May <strong>2012</strong> produced the highesttemporary staffing spend over the 12 monthperiod . The bank <strong>and</strong> agency spend for Mayaccounts for 16.32% of the pay bill, an increaseof 3.12% on the April position.• The fact that temporary staff spend in Mayincreased significantly yet FTE usage decreasedis likely to be attributed to accrual of invoices atyear end.• Despite the significant increase in spend, overall<strong>Trust</strong> bookings of Bank & Agency remainedrelatively static on the April position with a 0.39FTE increase from the previous month. Thenumber of agency bookings increased by 7.37FTE's in month - bank bookings decreased by7.76 FTE's over the same period.1. Midwifery bank <strong>and</strong> agency FTE bookingsdecreased in May by 3.10 FTE's on the Aprilposition.√ TEC June <strong>2012</strong> □ EPB………..…….□ FINANCE …………… □ AUDIT ………..….□ CLINICAL GOVERNANCE …………..…...……□ CHARITABLE FUNDS ………………………...…√ TRUST BOARD <strong>July</strong> <strong>2012</strong>□ REMUNERATION ………………………….…...□ OTHER ………………………. (please specify)CATEGORY:□ NATIONAL TARGET□ CNST□ STANDARDS FOR BETTER HEALTH□ HEALTH & SAFETY□ ASSURANCE FRAMEWORK□ TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE …………………..……………………………………………………..□ OTHER …………………….. (please specify)AUTHOR/PRESENTER:Author – Linda Baker – Head of workforcePlanningPresenter – Ruth McAll – Director of WorkforceDATE: 22 June <strong>2012</strong>1
2. Registered Nursing temporary staff bookingsdecreased in May by 14.57 FTE's on theApril position.3. We have seen an increase this month to thetemporary staffing usage in the Medical &Dental staff group by 9.64 FTE whencompared to April <strong>2012</strong>.4. Admin & Clerical have seen the biggestincrease in Bank <strong>and</strong> Agency usage thismonth, rising from 64.24 FTE in April to76.98 in May. An overall increase of 12.74FTE• Feedback from the Divisions & AssociateDirector IHB have identified that there continuesto be a high number of requests for specialistagency bookings• For the month of May, <strong>Trust</strong> annualised turnoverremained the same at 10.9% - this is 1.1% belowthe average of other large Acute <strong>Trust</strong>s.• The overall reported sickness absence rates forthe month of May has increased slightly by0.22% on the April position, rising from 4.29% to4.51% across the month.• The sickness absence rate has decreased by0.31% when compared to the same period lastyear.• HR have repeated the pan Londonbenchmarking exercise against other acuteLarge London <strong>Trust</strong>s this shows that thecombined average sickness absence rate for thisgroup is 3.59% - as such the graph has beenrevised to reflect this. Based upon this revisedinformation BHRUT's benchmarked positionshows us as currently sitting 0.92% above the3.59% average of all other large acute London<strong>Trust</strong>s. The <strong>Trust</strong>'s target has been left at 3.6%• The estimated costs associated with sicknessabsence has increased this month, in line withoverall percentage. It is estimated that the costto the <strong>Trust</strong> for April was £645,566. This figurehas risen by an estimated £26,612 on the sameperiod last year.• When the number of FTE's lost due to sicknessabsence is analysed by reason for absence, thehighest loss is seen in 'Unknown causes - notspecified' with 52.39 fte lost• In order to further improve the accuracy ofsickness absence reporting <strong>and</strong> recording, HRhave incorporated ‘effective recording processes'in their ' Essential skills for managers ' trainingprogramme. The effects of this training on theactual reported data may take time to show ademonstrable change2. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:None3. ALTERNATIVES CONSIDERED/REASONS FOR REJECTION:N/A2
4. DELIVERABLES:Continuous measurement <strong>and</strong> monitoring of workforce performance against NHS <strong>and</strong> local agreedtargets5. EVIDENCE :ESR dataIView DataNHSIE data6. RECOMMENDATION/ACTION REQUIRED:No action for information onlyAGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE ___________________________(if applicable)3
TRUST - WORKFORCE KEY PERFORMANCE INDICATORS - MAY <strong>2012</strong>Indicator Target May-11 Jun-11 Jul-11 Aug-11 Sep-11 Oct-11 Nov-11 Dec-11 Jan-12 Feb-12 Mar-12 Apr-12 May-12 YTDStaff In Post 5192.63 5215.55 5223.68 5250.52 5263.48 5313.23 5363.19 5353.99 5355.45 5350.71 5366.64 5366.82 5397.95 182.40Starters *¹ 55.83 46.59 40.73 59.29 70.57 78.23 55.37 31.24 44.46 38.74 58.25 50.44 49.48 623.39Leavers *¹ 32.60 35.25 44.96 46.70 49.75 38.32 40.87 42.38 39.15 41.19 52.31 45.83 32.33 509.04Turnover (Annualised)*¹12.0% 11.0% 11.0% 11.65% 10.88% 10.69% 10.60% 10.70% 10.78% 10.82% 11.0% 10.9% 10.9% 10.9%<strong>Trust</strong> SicknessAbsence % for month4.5% 4.82 3.63 5.05 5.35 4.80 5.46 5.13 6.00 5.15 5.81 4.41 4.29 4.51<strong>Trust</strong> SicknessAbsence Rolling 12Month Period<strong>Trust</strong> Estimated Cost ofSickness Absence(Month)3.6% 4.38 4.30 4.38 4.46 4.49 4.63 4.31 4.77 4.76 4.87 4.92 4.99 4.97£672,178 £482,909 £668,946 £704,259 £618,998 £760,710 £707,395 £903,771 £756,866 £764,730 £594,960 £582,757 £645,566 £8,191,867Appraisals 80.0% 78.60% 72.40% 72.09% 76.72% 76.03% 76.42% 72.25% 73.74% 77.80% 79.3% 74.3% 77.9% 78.49%Resus 80.0% 80.26% 78.42% 77.38% 72.62% 69.04% 68.22% 68.26% 72.15% 75.69% 77.8% 78.6% 76.3% 77.86%Paybill Budget £22,735,275 £22,223,328 £22,030,665 £22,326,245 £21,393,649 £21,806,873 £22,000,988 £21,907,263 £22,422,582 £22,276,976 £25,028,069 £23,895,905 £23,701,154 £271,013,698Paybill £23,999,750 £24,005,808 £24,058,435 £24,665,197 £24,012,335 £24,085,519 £24,357,038 £24,267,150 £24,857,841 £24,430,745 £24,518,224 £24,282,126 £24,950,935 £292,491,353Bank/Agency Spend £3,437,137 £3,361,872 £3,662,378 £3,653,979 £3,259,189 £3,179,473 £3,176,222 £3,079,296 £3,527,427 £3,053,265 £3,584,109 £3,155,363 £3,868,890 £40,561,463% Paybill Budget spenton bank & Agency staff15.12% 15.13% 16.62% 16.37% 15.23% 14.58% 14.44% 14.06% 15.73% 13.71% 14.32% 13.20% 16.32% 14.97%Overtime Spend (£) £131,254 £93,063 £104,179 £112,130 £116,637 £67,772 £65,940 £58,911 £69,768 £70,658 £62,666 £53,941 £61,881 £937,546IHB FTE Bookings 663.81 637.33 677.85 688.47 646.05 663.25 661.31 600.15 667.76 672.17 714.77 587.37 586.98 7803.46IHB FTE Booked as a %of Substantive SIP12.78% 12.22% 12.98% 13.11% 12.27% 12.48% 12.33% 11.21% 12.47% 12.56% 13.32% 10.94% 10.87% 12.23%*¹ Starters, Leavers & Turnover figures excludes junior doctors on rotationFinancial value in month of February <strong>2012</strong> for Bank/Agency spend has been adjusted by a £353,356 reduction relating to prior period accruals. This has come about from: an improved system between IHB <strong>and</strong> Finance creating a more accuratebase resulting in an downward adjustment of £182,354 for agency; a further reduction to the agency accrual due to writing off of old year agency accruals from the system of £51,186 as part of an aged analysis; <strong>and</strong> as a reduction for ageing to theBank Accrual of £119,816.1
Staff in PostStarters & LeaversFTE's5500.005400.005300.005200.005100.00FTE's90.0080.0070.0060.0050.0040.0030.0020.0010.000.005000.00May-11Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11Dec-11MonthJan-12Feb-12Mar-12Apr-12May-12May-11Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11Dec-11MonthJan-12Feb-12Mar-12Apr-12May-12Staff in PostStartersLeaversStaff in Post ( SIP )For the month of May <strong>2012</strong> the overall number of FTE's in post across the <strong>Trust</strong> increased by 31.13 FTE's on the April position <strong>and</strong> has increased by 185.40 FTE's across the 12month period.Starters & leaversThe number of starters in month was 49.48 FTE's compared to 45.04 FTE's in the previous month. Following a period of focussed recruitment activity, a total of 617.99 FTE's havestarted in the <strong>Trust</strong> since June 11. May demonstrated another decrease in the number of leavers with 32.33 fte leavers compared to 45.83 in April. Supported by the HR Advisors,Divisions have been tasked to actively promote Exit interviews so that 'reasons for leaving' can be truly understood. Findings of this piece of work will be reported within futurescorecards once the data has been analysed in a meaningful way.Starters & leavers data analysis over the same period differs from the staff in post growth for the same 3 reasons as in previous reports.1. If new starters commence employment or leave after the payroll cut off date (midmonth) they will not be entered or removed onto/off ESR until month end – therefore they will notappear on the staff in post report generated from ESR until the following month.2. Staff who increase or decrease their hours will affect the reported FTE’s in post but not the starters <strong>and</strong> leavers3.Timliness of managers completing <strong>and</strong> submitting the appropriate forms to HR - for entering onto ESR.<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Temporary staff Use <strong>and</strong> Spend4500000Bank/Agency Spend ( Provided by Finance)800IHB Bookings - FTE3750000700Spend (£'s)3000000225000015000007500000May-11Jun-11Jul-11Bank/Agency SpendAug-11Sep-11Oct-11Nov-11Dec-11MonthJan-12Feb-12Mar-12Apr-12May-12FTE6005004003002001000Apr-11May-11Jun-11Jul-11Aug-11Sep-11Oct-11DateNov-11Dec-11Jan-12Feb-12Mar-12Apr-12May-12AgencyBankBank & Agency SpendIn addition to the overall <strong>Trust</strong> Bank & Agency spend increasing by £713,527 in month, data also shows that May <strong>2012</strong> produced the highest temporary staffing spend over the 12month period . The bank <strong>and</strong> agency spend for May accounts for 16.32% of the pay bill, an increase of 3.12% on the April position.. The fact that temporary staff spend in Mayincreased significantly yet FTE usage decreased is likely to be attributed to accrual of invoices at year end.Bank & Agency UsageDespite the significant increase in spend, overall <strong>Trust</strong> bookings of Bank & Agency remained relatively static on the April position with a 0.39 FTE increase from the previous month.The number of agency bookings increased by 7.37 FTE's in month - bank bookings decreased by 7.76 FTE's over the same period.Midwifery bank <strong>and</strong> agency FTE bookings decreased in May by 3.10 FTE's on the April position.Registered Nursing temporary staff bookings decreased in May by 14.57 FTE's on the April position.We have seen an increase this month to the temporary staffing usage in the Medical & Dental staff group by 9.64 FTE when compared to April <strong>2012</strong>.Admin & Clerical have seen the biggest increase in Bank <strong>and</strong> Agency usage this month, rising from 64.24 FTE in April to 76.98 in May. An overall increase of 12.74 FTE<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
TURNOVERActual Versus Target Annualised Turnover14.012.0Turnover %10.08.06.04.0TurnoverFor the month of May, <strong>Trust</strong> annualised turnover remained the same at 10.9% -this is 1.1% below the average of other large Acute <strong>Trust</strong>s.2.00.0May-11Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11Dec-11Jan-12Feb-12Mar-12Apr-12May-12Actual TurnoverTarget TurnoverMonthA&E Registered Nursing Turnover, recruitment <strong>and</strong> temporary staff use - Hotspot monitoringCombined A&E Qualified Nursing - Staff in Post v IHB Booking v Annualised TurnoverA&E detailed turnover <strong>and</strong> leavers update formonitoring purposes20025.00%The overall effects of the registered nurse b<strong>and</strong> 5recruitment & over-recruitment strategy is demonstrated tothe right.17515020.00%N&M Qual(IHB)For the month of May the combined QH & KGH A&Eregistered nursing turnover rate fell from 20.63% to 19.51%.There were no registered nursing leavers across either sitein month. The graph to the right shows the number of FTE's,turnover <strong>and</strong> temporary staff usage for all registered nursingb<strong>and</strong>s within both A&E's. The overall number of registerednursing FTE's in post increased by 4.36 FTE this month <strong>and</strong>we have seen an decrease in temporary staff bookings by0.66 FTE's.FTE's12510075502515.00%10.00%5.00%Turnover %N&M Qual(SIP)N&M Qual(Turnover)00.00%May-11Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11MonthDec-11Jan-12Feb-12Mar-12Apr-12May-12<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
SICKNESS ABSENCEReal - Time Sickness AbsencePercentage (%)6.506.005.505.004.504.003.503.002.502.001.501.000.500.00May-11£1,000,000Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11MonthDec-11Jan-12Feb-12BHRUT Target Other Large Acute London<strong>Trust</strong> Estimated Cost of Sickness Absence (Month)Mar-12Apr-12May-12Sickness AbsenceReported sickness absence rates for the month of May has increased slightlyby 0.22% on the April position, rising from 4.29% to 4.51% across the month.The sickness absence rate has decreased by 0.31% when compared to thesame period last year. HR have repeated the pan London benchmarkingexercise against other acute Large London <strong>Trust</strong>s this shows that thecombined average sickness absence rate for this group is 3.59% - as suchthe graph has been revised to reflect this. Based upon this revisedinformation BHRUT's benchmarked position shows us as currently sitting0.92% above the 3.59% average of all other large acute London <strong>Trust</strong>s. The<strong>Trust</strong>'s target has been left at 3.6%£900,000Estimated costs of sickness absenceEstimated Cost (£'s)£800,000£700,000£600,000£500,000£400,000£300,000£200,000The estimated costs associated with sickness absence has increased thismonth, in line with overall percentage. It is estimated that the cost to the<strong>Trust</strong> for April was £645,566. This figure has risen by an estimated £26,612on the same period last year.£100,000£0May-11Jun-11Jul-11Aug-11Sep-11Oct-11Nov-11Dec-11MonthJan-12Feb-12Mar-12Apr-12May-12<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Sickness Absence - FTE LostReason for AbsenceS10 Anxiety/stress/depression/other psychiatric illnessesS11 Back ProblemsS12 Other musculoskeletal problemsS13 Cold, Cough, Flu - InfluenzaS14 AsthmaS15 Chest & respiratory problemsS16 Headache / migraineS17 Benign <strong>and</strong> malignant tumours, cancersS18 Blood disordersS19 Heart, cardiac & circulatory problemsS20 Burns, poisoning, frostbite, hypothermiaS21 Ear, nose, throat (ENT)S22 Dental <strong>and</strong> oral problemsS23 Eye problemsS24 Endocrine / gl<strong>and</strong>ular problemsS25 Gastrointestinal problemsS26 Genitourinary & gynaecological disordersS27 Infectious diseasesS28 Injury, fractureS30 Pregnancy related disordersS31 Skin disordersS98 Other known causes - not elsewhere classifiedS99 Unknown causes / Not specifiedReasons for Sickness Absence vFTE's lostWhen the number of FTE's lost due tosickness absence is analysed by reasonfor absence, the highest loss is seen in'Unknown causes - not specified' with52.39 fte lost. HR acknowledge thiscreates concern as it means that staffare not providing their absence reasonor it isn't being recorded by theirmanager/supervisor. In order to furtherimprove the accuracy of sicknessabsence reporting <strong>and</strong> recording, HRhave incorporated 'effective recordingprocesses' in their ' Essential skills formanagers ' training programme. Theeffects of this training on the actualreported data may take time to show ademonstrable change. Directoratesmust not only ensure that managersrecord absence correctly within theweekly absence returns but also thatreturns are submitted in a timely way.0 10 20 30 40 50 60FTE LostWORKFORCE DEVELOPMENTS<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
1. Skills for Health projectsSupported by CTB funding, earlier in the year the <strong>Trust</strong> commissioned Skills for Health (SfH) to assist us in addressing key actions identified within the CQC action plan relating to:- Improving workforce planning capacity <strong>and</strong> capability across the <strong>Trust</strong>- completion of a systematic skill mix review of identified clinical areasImproving workforce planning capacity <strong>and</strong> capability across the <strong>Trust</strong>The <strong>Trust</strong> <strong>and</strong> SfH identified <strong>and</strong> agreed that Directorates <strong>and</strong> Business Units should receive introductory training sessions on workforce planning in order to support the businessplanning process ( bottom up approach) <strong>and</strong> improve capacity <strong>and</strong> capability at service level.The main purpose of these sessions is to increase awareness of <strong>and</strong> raise the profile of workforce planning across the Directorates, demonstrating how it supports the development ofbusiness plans <strong>and</strong> ultimately ensuring optimum patient care. The main focus of these sessions relates to supporting the required shift in behaviours as well as technical abilities toeffectively workforce plan <strong>and</strong> secure the Directorates engagement with the principles of workforce planning <strong>and</strong> getting participants to think about their role <strong>and</strong> ways of taking thelearning forward. . SfH's experience shows that these sessions are a good way of engaging a large number of people within organisations <strong>and</strong> starts the process of “doing thingsdifferently”.The first session took place on the 19th June with the next booked for 11th <strong>July</strong> - initial feedback has been very positive.Systematic skill mix reviewAs already highlighted BHRUT commissioned SfH to carry out a systematic Skill Mix Review - initially within A&E on the QH site, this piece of work was completed at end May <strong>and</strong> SfHhave provided a report of their findings <strong>and</strong> recommendations. The next phase is for the A&E department to take this piece of work forward through developing an action plan forimplementation. In the original SfH brief the skill mix review was to be preceded <strong>and</strong> informed by a Functional Mapping Exercise but this was removed from the brief to avoid overlap withthe new McKinsey project.Skill mix matters because it affects service delivery, performance <strong>and</strong> financial out-turn <strong>and</strong> a Skill Mix Review forms part an important part of any strategic workforce developmentprogramme. SfH's approach was to utilise service, workforce <strong>and</strong> finance information <strong>and</strong> data to determine how closely the current skill mix matches the <strong>Trust</strong>’s future skills requirement.Evidence was gained from interviews with staff <strong>and</strong> Directors, other information provided by the <strong>Trust</strong>, external reports, guidelines <strong>and</strong> comparative sources. information provided hasthen been analysed using Skills for Health’s expertise, tools & workforce analysis techniques in order to:- Assess the skill mix requirements in the Queens’ Hospital A&E Department.- Analyse how staff resources are used in the Department.- Review benchmarking data relevant to the project brief.- Triangulate the findings <strong>and</strong> make recommendations for the <strong>Trust</strong> to skill mix improvements in order to overcome problems identified in the delivery of A&Eservices.Key findings as to the workforce <strong>and</strong> skills mix challenges identified include:- Skills mix change is an imperative in the context within which the <strong>Trust</strong> is operating- New ways of working have been trialled but there is no consistent approach to the development <strong>and</strong> deployment of new roles- Rotas are not aligned with workload <strong>and</strong> staff lack information to improve performance- There are significant recruitment <strong>and</strong> retention difficulties for medical <strong>and</strong> other staff- Activity indicators highlight systemic local challenges that need to be addressed- Current staffing is expensive <strong>and</strong> over reliant on B<strong>and</strong> 5&6 nursing staff <strong>and</strong> on locum medical staff- Nursing staff hours are less closely aligned to A&E attendances than medical staff hours.WORKFORCE DEVELOPMENTS - continued<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Key opportunities identified for the <strong>Trust</strong> to improve quality <strong>and</strong> productivity through workforce change include:- Changing skill mix to achieve a more effective deployment of support staff <strong>and</strong> advanced practitioners the A&E Department- Ensuring that HCAs achieve competence in a more structured way.- Underst<strong>and</strong>ing <strong>and</strong> utilising skill sets more fully to improve productivity <strong>and</strong> ensure more effective planning for supply shortages in qualified nursing staff.- Using skill sets more effectively to increase role satisfaction <strong>and</strong> improve staff retention, thereby reducing staff turnover <strong>and</strong> temporary staff usage- Reviewing the alignment of staff rotas to workload.- Giving more systematic information to staff to enable them to take responsibility for improving performance.Main issues identified regarding current staffing <strong>and</strong> skill mix:- Skill mix. The staffing appears to be light on B<strong>and</strong>s 2, 3 <strong>and</strong> 4. This is particularly so in the sense that A&E at Queen’s is like a “ward”, <strong>and</strong> you expect to use HCAs heavily in wards.Also, light on advanced nurse practitioners, who could replace some of the vacant staff grade posts currently filled by locums who appear to be almospermanent (but at twice the cost, <strong>and</strong> with some quality issues).- Workforce planning issues. There are some serious recruitment difficulties for doctors <strong>and</strong> recruitment/retention issues for nurses. The supply of qualified nursesmay in fact get tighter by 2014/15 as the number of nurses in training has been cut by 25% in 2011/12. The <strong>Trust</strong> may face continuing difficulties in recruiting staff gradedoctors. However, the supply of local people capable of developing “assistant practitioner” HCA skills may be significant, <strong>and</strong> they will be much less likely to leave.- Cost. It may be more cost effective to deploy advanced nurse practitioners to replace some staff grade doctor posts, <strong>and</strong> to replace some qualified nurse posts withcompetent HCAs.Key recommendations for action for the <strong>Trust</strong> to consider are:1. To develop <strong>and</strong> implement a support staff & advanced practitioner strategy for A&E incorporating:• a clear competence framework for A&E roles supporting role clarity <strong>and</strong> progression opportunities from B<strong>and</strong> 3 onwards• a system for recognizing <strong>and</strong> rewarding the achievement of competence• accessible learning opportunities to facilitate staff development2. To design <strong>and</strong> implement a programme for the systematic introduction of new roles <strong>and</strong> skill mix change ensuring effective communication <strong>and</strong> governance arrangements are in place3. To put in place a process to ensure that A&E performance data is systematically made available to staff enabling teams <strong>and</strong> individuals to take personal responsibility for performance4. To arrange a process for dialogue with commissioners <strong>and</strong> GPs to develop an integrated strategy for reducing dem<strong>and</strong> pressuresThe General Manager A&E is currently developing an action plan for implementation of the SfH recommendations in addition to other recommendations concerning staffing. Thefindings <strong>and</strong> resulting action plan are being presented to the Workforce Committee on 25th June <strong>2012</strong> followed by the Joint Staff Committee in <strong>July</strong> before discussions then take placewith staff in the Department.WORKFORCE DEVELOPMENTS - continued<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
2. Essential Skills for Managers TrainingIn April <strong>2012</strong> the Education Department in conjunction with Human Resources launched the second Essential Skills for Mangers Programme. For 12/13 there are 2 separate Cohortsrunning each consisting of 10 days study - with attendance to all 10 being m<strong>and</strong>atory. The programme will cover the following components:Confident delegation Effective team leadership Effective communicationDealing with poor performance Recruitment <strong>and</strong> Selection of the right staff appraisal, development <strong>and</strong> trainingWork load planning, prioritisation & organisation Interpretation <strong>and</strong> application of HR Policy <strong>and</strong> ProceduresDIRECTORATE WORKFORCE KPI'sDIAGNOSTICS & SPECIAL MEDICINE DIRECTORATE -WORKFORCE KEY PERFORMANCE INDICATORS - MAY <strong>2012</strong><strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Indicator Target Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 YTDStaff In Post 1094.28 1104.66 1099.47Starters *¹ 9.43 12.66 22.09Leavers *¹ 6.12 4.46 10.58Turnover (Annualised) *¹ 12.0% 9.1% 8.6%<strong>Trust</strong> Sickness Absence %for month3.6% 4.29% 4.51%Directorate SicknessAbsence For Month3.6% 5.11% 5.03%Directorate SicknessAbsence Rolling 12 MonthPeriodDirectorate Estimated Costof Sickness Absence(Month) *²3.6%£151,450 £162,189 £313,639Appraisals Compliance 80.0% 71.95% 71.96%Resus Compliance 80.0% 77.57% 77.13%Paybill Budget£4,719,045 £4,655,044 £9,374,089Paybill £4,763,991 £4,859,576 £9,623,567Bank/Agency Spend £496,296 £189,999 £686,295% Paybill Budget spent onbank & Agency staff10.52% 4.08% 7.32%Overtime Spend (£) £15,913 £22,366 £38,279IHB FTE Bookings 77.34 75.64 152.98IHB FTE Booked as a % ofSubstantive SIP7.07% 6.85% 6.96%*¹ Starters, Leavers & Turnover figures excludes junior doctors on rotationEMERGENCY, GEN. MEDICINE & NEUROSCIENCES DIRECTORATE -WORKFORCE KEY PERFORMANCE INDICATORS - MAY<strong>2012</strong>Indicator <strong>Trust</strong> Overall Scorecard Target - May <strong>2012</strong> Apr-12 - Workforce Information May-12DepartmentJun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 YTD
Indicator Target Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 YTDStaff In Post 1497.50 1488.89 1493.20Starters *¹ 24.47 16.48 40.95Leavers *¹ 16.71 5.00 21.71Turnover (Annualised)*¹12.0% 12.3% 12.4%<strong>Trust</strong> SicknessAbsence % for month3.6% 4.29% 4.51%Directorate SicknessAbsence For Month3.6% 3.71% 3.88%Directorate SicknessAbsence Rolling 12Month PeriodDirectorate EstimatedCost of SicknessAbsence (Month) *²3.6%£128,632 £143,589 £272,221Appraisals Compliance 80.0% 74.07% 75.21%Resus Compliance 80.0% 76.26% 78.64%Paybill Budget£6,897,802 £6,887,836 £13,785,638Paybill £6,945,598 £7,283,477 £14,229,075Bank/Agency Spend £1,351,514 £1,514,580 £2,866,094% Paybill Budget spenton bank & Agency staff19.59% 21.99% 20.79%Overtime Spend (£) £4,331 £6,229 £10,560IHB FTE Bookings 247.95 261.02 508.97IHB FTE Booked as a %of Substantive SIP16.56% 17.53% 17.04%*¹ Starters, Leavers & Turnover figures excludes junior doctors on rotationSURGICAL DIRECTORATE - WORKFORCE KEY PERFORMANCE INDICATORS - MAY <strong>2012</strong>Indicator Target Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 YTD<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Staff In Post 1122.50 1151.10 1136.80Starters *¹ 7.00 3.60 10.60Leavers *¹ 10.67 7.43 18.10Turnover (Annualised)*¹12.0% 8.5% 8.9%<strong>Trust</strong> SicknessAbsence % for month3.6% 4.29% 4.51%Business Unit SicknessAbsence For Month3.6% 3.44% 3.90%Business Unit SicknessAbsence Rolling 12Month PeriodBusiness UnitEstimated Cost ofSickness Absence(Month) *²3.6%£99,908 £120,250 £220,158Appraisals Compliance 80.0% 85.65% 86.14%Resus Compliance 80.0% 76.42% 78.59%Paybill Budget£5,182,485 £5,288,767 £10,471,252Paybill £5,501,762 £5,495,357 £10,997,119Bank/Agency Spend £753,584 £655,882 £1,409,466% Paybill Budget spenton bank & Agency staff14.54% 12.40% 13.46%Overtime Spend (£) £25,315 £22,791 £48,106IHB FTE Bookings 137.79 112.35 250.14IHB FTE Booked as a %of Substantive SIP12.28% 9.76% 11.02%*¹ Starters, Leavers & Turnover figures excludes junior doctors on rotationWOMEN, CHILDREN & SUPPORT SERVICES DIRECTORATE -WORKFORCE KEY PERFORMANCE INDICATORS - MAY <strong>2012</strong>Indicator Target Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 Apr-13 YTDStaff In Post 1181.94 1180.51 1181.23Starters *¹ 3.40 11.00 14.40<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
Leavers *¹ 12.33 12.00 24.33Turnover (Annualised)*¹12.0% 11.4% 11.7%<strong>Trust</strong> SicknessAbsence % for month3.6% 4.29% 4.51%Directorate SicknessAbsence For Month3.6% 5.24% 5.57%Directorate SicknessAbsence Rolling 12Month Period3.6%Directorate EstimatedCost of SicknessAbsence (Month) *²£140,926 £149,545 £290,471Appraisals Compliance 80.0% 85.03% 86.20%Resus Compliance 80.0% 76.40% 77.79%Paybill Budget£4,559,907 £4,562,188 £9,122,095Paybill £4,627,315 £4,640,770 £9,268,085Bank/Agency Spend £444,148 £266,534 £710,682% Paybill Budget spenton bank & Agency staff9.74% 5.84% 7.79%Overtime Spend (£) £2,542 £3,422 £5,964IHB FTE Bookings 103.68 108.89 212.57IHB FTE Booked as a %of Substantive SIP8.77% 9.22% 9.00%*¹ Starters, Leavers & Turnover figures excludes junior doctors on rotation<strong>Trust</strong> Overall Scorecard - May <strong>2012</strong> - Workforce Information Department
EXECUTIVE SUMMARYTITLE:Transformation <strong>Board</strong> UpdateBOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:Provide an update to the <strong>Trust</strong> <strong>Board</strong>.□ TEC ……………..….. □ STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT ………….……..….□ QUALITY & SAFETY …………..………….....……□ WORKFORCE□ CHARITABLE FUNDS ………………………………...…√ TRUST BOARD ……………………………….………….□ REMUNERATION ………………………………….…...□ OTHER …………………………..……. (please specify)2. DECISION REQUIRED: CATEGORY:For Information□ NATIONAL TARGET □ CNST□ CQC REGISTRATION □ HEALTH & SAFETY√ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE ……………………………....□ OTHER …………………….. (please specify)3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:AUTHOR/PRESENTER: Dorothy Hosein, Director ofTransformationDATE: June <strong>2012</strong>There is currently a significant gap between the CIP programme <strong>and</strong> <strong>Trust</strong> required position. The TransformationProgramme is necessary to bridge that gap <strong>and</strong> ensure financial stability.Twelve Corporate Workstreams have been established which will support <strong>Trust</strong>’s cost improvement programme. Each ofthese Workstreams is led by a senior Executive <strong>and</strong> at the time of writing this report, targets are being confirmed. EachWorkstream will have a number of clinical indicators <strong>and</strong> quality measurements to ensure there is no adverse effect tothe quality of care that we provide to our patients. The above is described in more detail within the attached report.In addition, a rigorous structure of accountability <strong>and</strong> performance management is being introduced, together with closemonitoring of performance. The Programme will be supported by a Project Management Office, described in theattached report.4. DELIVERABLES1, End of June <strong>2012</strong> all short term measures in the attached report initiated.Emergency Pay controls all in place.2. First week of <strong>July</strong> <strong>2012</strong> all Workstreams together with targets established.3. End <strong>July</strong> <strong>2012</strong> Improvement in the <strong>Trust</strong> increment expenditure position by (tbc)Key Performance Indicators1. Status of Workstream2. Status of Cost improvement Programme3. Monitoring of clinical risks associated with plans.Agreed at Transformational <strong>Board</strong> Meeting.
5. KEY PERFORMANCE INDICATORSAGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________2
<strong>2012</strong>/13 Cost Improvement Strategy: High level approach<strong>Trust</strong> <strong>Board</strong> Update: 4 th <strong>July</strong> <strong>2012</strong>Dorothy HoseinJan BergmanPaul McAuliffeProgramme Management Office
IntroductionThe <strong>Trust</strong> needs to identify <strong>and</strong> deliver a £23m costimprovement strategy in <strong>2012</strong>/13 <strong>and</strong> there is a further£4m of recurrent cost pressures. The resulting totalfinancial challenge for <strong>2012</strong>/13 is £27m. Thepurpose of this paper is to provide an overview of thedelivery strategy to the Finance Committee <strong>and</strong>confirm support for implementation.The paper is broken down into the following foursections:1)Workstream targets2)Workstream scope <strong>and</strong> delivery timescales3)CIP governance framework4)Short term tactical controlsThe PMO have identified FYE saving opportunities ofup to £29m facilitated through twelve coreworkstreams (see table opposite <strong>and</strong> described inmore detail on pages 4-6). Each workstream has anaccountable officer to drive <strong>and</strong> ensure delivery, withadditional support from the newly established ProjectManagement Office (PMO).Work streamAccountable officer1. Medical staff costs Medical Director2. Nursing staff costs Nursing Director3. Allied Health Professional staff costs Nick Hulme - Project Director ofReconfiguration4. Admin & Clerical staff costs <strong>and</strong> T&C Dorothy Hosein - Director ofTransformation5. Beds Cathy Geddes - Chief Operating Officer6. Theatres Eileen Moore - Associate Director ofSurgery7. Outpatients Arshiya Khan - Associate Director ofWomen & Children & Support Services8. Diagnostics Elizabeth Lyons - Associate Director ofCDT9. Non pay/procurement Director of Finance10. Medicines management Portia Omo-Bare - Chief Pharmacist11. Estates <strong>and</strong> facilities Jackie Doyle - Head of Estates &Facilities12. Corporate costs Jan Bergman - Head of PMO2
Breakdown of suggested opportunity by workstreamNote: Top down analysis has identified some initial savingsopportunities, as more detailed analysis is completed within eachworkstream, there will be some redistribution of some parts of theworkforce targets(medical, nursing, AHP, A&C) into the crosscutting schemes (theatres, outpatients, diagnostics).Amber / Green schemes M2Current gap3
High level projection of the opportunities in <strong>2012</strong>/13Workstreama. Opportunitiesidentified FYE - £mb. Opportunities identifiedPYE (estimated*) - £mc. Green / Amber schemes(M2 tracker) - £md. PYE + Green / Amberschemes (b+c) - £m1. Medical staff costs 7.67 1.85 1.06 2.902. Nursing staff costs 5.69 3.29 2.01 5.303. Allied Health Professionalstaff costs4. Admin & Clerical staffcosts <strong>and</strong> T&C1.42 0.71 0.41 1.121.39 0.59 0.38 0.965. Beds 4.30 1.08 0.80 1.886. Theatres 0.55 0.18 0.09 0.277. Outpatients 0.40 0.13 0.22 0.368. Diagnostics 0.00 1.03 1.039. Non pay/procurement 2.24 0.95 1.34 2.3010. Medicines management 1.19 0.40 0.63 1.0211. Estates <strong>and</strong> facilities 2.16 0.72 1.67 2.3912. Corporate costs 2.04 0.68 1.42 2.10Total 29.03 10.58 11.05 21.63CIP target 27.00Gap to CIP target -5.37Workforce impact: Delivering savings of £29m approximates to c450 WTE (based on average WTE cost); in practice a proportion of the savings will befrom changes to skill mix <strong>and</strong> reductions in agency usage. Therefore, further work is needed to be completed with accountable officers to underst<strong>and</strong> the fullstaffing implications.*Some elements of the opportunities may already be accounted for in the <strong>Trust</strong>’s schemes in progress (column c). Further analysis is required on this area as workstreamsprogress.4
Workstream scope <strong>and</strong> required action (1)Workstream Scope Outcomes to deliver £10.6m PYE Savings tocommence*1. Medical staffcosts2. Nursing staffcosts3. Allied HealthProfessional staffcosts4. Admin & Clericalstaff costs <strong>and</strong> T&C►All medical pay savings throughreduction in staff, staff skill mix,rotas <strong>and</strong> reductions in bank /agency usage► All Nursing pay savings throughreduction in staff, staff skill mix ,rotas <strong>and</strong> reductions in bank /agency usageNB: Bed reduction strategies are notincluded in this workstream.►►►All AHP / scientific / technical paysavings through reduction in staff,staff skill mix , rotas <strong>and</strong>reductions in bank / agencyusageAll admin & clerical pay savingsthrough reduction in staff, staffskill mix , rotas <strong>and</strong> reductions inbank / agency usageTerms & conditions (all staffgroups)5. Beds ► Ward costs saved throughreducing LoS• Removal of bank/agency spend over budget.• Conversion of 75% agency usage to bank• 10% reduction in agency costs through reduced supplierlist <strong>and</strong> st<strong>and</strong>ardised rates for internal/external sessions.• Removal of bank/agency spend over budget.• Conversion of 75% agency usage to bank• 10% reduction in agency costs through reduced supplierlist <strong>and</strong> st<strong>and</strong>ardised rates.• Release of £1.95m pay costs from Jan 13 through skill mixreviews focussing on b<strong>and</strong> 6+ <strong>and</strong> non ward roles.• Removal of all bank/agency over budget.• Conversion of 75% agency usage to bank• 10% reduction in agency costs through reduced supplierlist <strong>and</strong> st<strong>and</strong>ardised rates.• Release of £158k therapy, £266 Radiology, £282mpharmacy pay costs from Jan 13 through skill mix reviews.• Removal of all bank/agency over budget.• Conversion of 75% agency usage to bank• 10% reduction in agency costs through reduced supplierlist <strong>and</strong> st<strong>and</strong>ardised rates.• Release of £909k pay costs from Jan 13 through skill mixreviews.• Closure of 134 non elective beds from Jan 13 across bothsites.Jul 12Jul 12 (bank <strong>and</strong>agency)Jan 13 (skill mix)Jul 12 (bank <strong>and</strong>agency)Jan 13 (skill mix)Jul 12 (bank <strong>and</strong>agency)Jan 13 (skill mix)Jan 13*Enables consultation where required. However the <strong>Trust</strong> pay protection policy will need to be considered.5
Workstream scope <strong>and</strong> required action (2)Workstream Scope Outcomes to deliver £10.6m PYE Savings tocommence*6. Theatres ► Theatres costs saved throughincreasing the productivity of theatres► Theatre workforce efficiencies► Theatre non pay efficiencies7. Outpatients ► OP costs saved through increasing theproductivity of clinic usage► OP workforce efficiencies8. Diagnostics ► All Diagnostics costs (pay <strong>and</strong> nonpay) saved through increasingefficiency <strong>and</strong> decreasing dem<strong>and</strong>.9. Nonpay/procurement10. Medicinesmanagement►►All costs saved through decreasing theusage <strong>and</strong> unit price of in scope nonpayspend (excludes theatres,diagnostics)All costs saved through decreasing theusage <strong>and</strong> unit price of medicines(includes outsourcing opportunities)• Reduction of 348 theatre lists per annum from Jan 13through achievement of 90% utilisation (auditcommission calculation)• Reduction in 1,375 OP clinics per annum from Dec 12through reduced DNA rates to 5% for new <strong>and</strong> followup patients.•N/A• £500k reduction in non pay spend through ‘red pen’exercise with Business Unit Managers. Further 5%reduction in remaining non pay spend (£1.7m)through tactical/strategic schemes from Dec 12.• 4% reduction in drug costs (£1.2m FYE ) from Dec12 through tactical <strong>and</strong> strategic schemes.Jan 13Dec 12N/ADec 12Dec 1211. Estates <strong>and</strong>► All Estates costs, PFI & non-PFIfacilities• 5% reduction in corporate costs (4.2m FYE) fromDec 12Dec 12.12. Corporate costs ► All Corporate costs excluding estates Dec 126
Programme GovernanceWorkstream & Divisional AccountabilityProgramme Governance StructureWorkstream 1Workstream 12<strong>Trust</strong> <strong>Board</strong>Transformation<strong>Board</strong>Chair: CEO+ External partnersMonthlyQuality & SafetyCommitteeFinance Committee<strong>Trust</strong> ExecutiveCommitteeChair: CEOFormal ClinicalAgreementMonthlyProject Management Planning & ReportingID Task NameNov '10 Dec '10 Jan '11 Feb '11 Mar '101 08 15 22 29 06 13 20 27 03 10 17 24 31 07 14 21 28 0741 Develop Finance training material to train budget holders staProgramme SteeringGroupChair: Director ofTransformationDeputy: QIPPProgramme DirectorFortnightly42 Finance induction training43 Agree induction training content with Clare Stafford44 Present plan for training material to FMs meeting45 Talk to HR to get a place on induction agenda46 Develop training material47 First induction training session held48 Budget holder training49 Review current training <strong>and</strong> define improvement areas50 Agree training content with Clare Stafford51 Present plan for training material to FMs meeting52 Develop training material53 Specialist finance trainingWorkstreamsPMOClinical ReviewGroup54 Define specialist training content55 Agree training content with Clare Stafford56 Present plan for training material to FMs meeting57 Develop training materialChair: AccountableOfficerProject TeamPMO SupportWeeklyDelivery SupportUnitWeeklyClinical Review7
Additional short term tactical measures to close the£5.4m gapA number of short term measures are being planned <strong>and</strong>implemented to decrease the current rate of expenditure acrossthe <strong>Trust</strong>. These include:1) Additional Pay controlsa) Increased authorisation levels for booking bank <strong>and</strong> agencystaff across all staff Groups.a) Nursing: Matron <strong>and</strong> General Manager approval nowrequired; Out of Hours authorisation by Site manager.Short notice sign off by Associate Directorsb) Medical: Associate Director sign off. Off frameworkrates for locums require COO approvalc) AHP: Associate Director sign offd) A&C : Can only be approved by COO.2) Red pen reviewDetailed analysis of General Ledger data (expenditure, budgets <strong>and</strong>trends) to identify opportunities for rapid cost reduction with a robust, wellgoverned process which gives leaders in the <strong>Trust</strong> the opportunity to holdmanagement to account for delivery.b) Weekly Pay Controls group led by the Transformation Directorto monitor spend against budget. Budget holders challengedwhere spend £/ WTE is over funded levels.8
1REPORT TO:REPORT FROM:<strong>Trust</strong> <strong>Board</strong>Chief ExecutiveDATE: 23 June <strong>2012</strong>SUBJECT:FOR:INTERIM CHAIR & CHIEF EXECUTIVE’S REPORTInformation______________________________________________________________1. INTRODUCTIONThis report contains a summary of:• Actions taken under emergency powers• Executive decisions• National Issues/News• Local Issues/News2. RECOMMENDATIONThe <strong>Board</strong> is asked to note this report.3. ACTIONS TAKEN UNDER EMERGENCY POWERSNo actions have been taken by the Interim Chairman or Chief Executiveacting under emergency powers.4. EXECUTIVE DECISIONSThe <strong>Trust</strong> Executive Committee has been meeting on a monthly basis <strong>and</strong>have reviewed <strong>and</strong> inputted into several reports prior to their submissionto the <strong>Trust</strong> <strong>Board</strong>, such as the Care Quality Commission Report,Learning Disability Progress Report, Milestone Tracker/TFA <strong>and</strong> theTransformation <strong>Board</strong> update.Interim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
25.NATIONAL ISSUES/NEWSHealth Secretary sets objectives for NHS Commissioning <strong>Board</strong>Authority:Andrew Lansley has set out the Government’s strategic objectives for theNHS Commissioning <strong>Board</strong> Authority <strong>and</strong> the basis against which theAuthority will be held to account. The Department of Health will hold theAuthority to account for its performance against our strategic objectives,relating to: transferring power to local organisations, establishing thecommissioning l<strong>and</strong>scape, developing specific commissioning <strong>and</strong>financial management capabilities, <strong>and</strong> developing excellent relationships.For more information go to: http://www.dh.gov.uk/health/<strong>2012</strong>/04/authorityobjectives/Sir Peter Carr confirmed as Chair of NHS <strong>Trust</strong> DevelopmentAuthority:Sir Peter, currently Vice Chair NHS North of Engl<strong>and</strong>, will head up theNHS <strong>Trust</strong> Development Authority, the new organisation that will supportNHS <strong>Trust</strong>s to achieve foundation status, when it is established in June<strong>2012</strong>. The NTDA will be accountable for the performance managementof NHS <strong>Trust</strong>s, driving up quality <strong>and</strong> delivering value for money, whiledeveloping <strong>and</strong> supporting NHS organisations to achieve Foundation<strong>Trust</strong> status. Sir Peter Carr stepped down from his role with NHS Northof Engl<strong>and</strong> <strong>and</strong> took up post as NTDA Chair from 1 June <strong>2012</strong>.For further information go to: http://mediacentre.dh.gov.uk/<strong>2012</strong>/04/25/sirpeter-carr-confirmed-as-chair-of-nhs-trust-development-authority/New guidance to speed up access to the drugs patients need:Lord Howe has announced new guidance on the Cancer Drugs Fund,which will help speed up access to the drugs patients need. In mostcases, patients will be able to access drugs within a matter of days ofapplication to the Fund. The Department has worked with NHScolleagues to review the guidance issues in 2011, taking into accountpublic feedback from cancer charities.For further information to: http://mediacentre.dh.gov.uk/<strong>2012</strong>/04/23/newguidance-to-speed-up-access-to-the-drugs-patients-need/Clinical Commissioning Group Authorisation : Final Draft Guide:The Clinical Commissioning Group Authorisation : Final Draft Guide forapplicants has been published following formal ratification at the <strong>Board</strong>meeting of the NHS Commissioning <strong>Board</strong> Authority on 13 April <strong>2012</strong>.This document is designed to help emerging Clinical CommissioningGroups (CCGs) develop clear plans to progress through the authorisationprocess <strong>and</strong> become authorised CCGs.Link: http://www.commissioningboard.nhs.uk/files/<strong>2012</strong>/04/ccg-auth-appguide.pdfInterim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
3Raising the bar on patient safety: the journey of ‘harm free’ care:On 17 May <strong>2012</strong>, Maxine Power, QIPP Safe Care National WorkstreamLead, gave an overview of Safety Express, an initiative that aims to deliverhigher quality ‘harm free’ care at lower cost. It plans to do this byreducing the number of patients who experience harm from pressureulcers, falls, infections in patients with urinary catheters <strong>and</strong> blood clots.Link: http://bit.ly/Js4rLGSir Keith Pearson confirmed as Chair of Health Education Engl<strong>and</strong>:Sir Keith Pearson has been confirmed as Chair of Health EducationEngl<strong>and</strong> (HEE). Sir Keith, currently Chair of the NHS Confederation, willhead up Health Education Engl<strong>and</strong>, the organisation that will providenational leadership to the new system of education <strong>and</strong> training inhealthcare, established in June <strong>2012</strong>.For further information, go to: http://mediacentre.dh.gov.uk/<strong>2012</strong>/05/02/sirkeith-pearson-confirmed-as-chair-ofhealth-education-engl<strong>and</strong>/Situations vacant in the new NHS:Leadership, innovation <strong>and</strong> the ability to inspire confidence in others arejust some of the qualities sought by the Secretary of State for Health as heseeks to recruit high calibre c<strong>and</strong>idates to the new NHS structure.Vacancies are currently advertised for two Chairs <strong>and</strong> three Non-Executive Directors of the Independent Reconfiguration Panel,Healthwatch Engl<strong>and</strong> <strong>and</strong> the NHS Commissioning <strong>Board</strong> Authorityrespectively.For further information, go to: http://cno.dh.gov.uk/<strong>2012</strong>/05/01/situationsvacant-in-the-new-nhs/Guidance on new National CQUIN goals:Two new National Commissioning for Quality <strong>and</strong> Innovation (CQUIN)goals, on dementia <strong>and</strong> on the use of the NHS safety thermometer, havebeen introduced for use in <strong>2012</strong>/13. This guidance is designed to assistCommissioners <strong>and</strong> Providers when including CQUINs in contracts.Link: http://www.dh.gov.uk/health/<strong>2012</strong>/05/guidance-on-new-nationalcquin-goals/Department teams up with doc2doc forum to gather views on longterm conditions:-The Department of Health is working with doc2doc, the BMJ Group’sonline community for health professionals, on its long term conditionsstrategy. This is a cross government strategy being drafted by theDepartment of Health.For further information, go to:http://www.dh.gov.uk/health/<strong>2012</strong>/05/doc2doc/Interim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
4How to maintain quality during the transition: preparing forh<strong>and</strong>over:To help organisations maintain quality during the transition, the NationalQuality <strong>Board</strong> has produced guidance for all sending <strong>and</strong> receiving bodieson how to prepare for h<strong>and</strong>over during the transition. PCT <strong>and</strong> SHAClusters were asked to produce plans by the 23 <strong>and</strong> 30 June <strong>2012</strong>respectively, setting out how they intend to produce <strong>and</strong> h<strong>and</strong>over thenecessary quality information to their successor bodies.Link: http://www.dh.gov.uk/health/category/policy-areas/nhs/nqb/NHS companion document – Chronic Obstructive PulmonaryDisease <strong>and</strong> Asthma:Improving outcomes for people with respiratory disease is a key priority forthe NHS. To support the Outcomes Strategy for Chronic ObstructivePulmonary Disease <strong>and</strong> Asthma, published last <strong>July</strong>, a companiondocument has been published that sets out 46 key recommended actionsfor the NHS, to help deliver on the five domains in the NHS OutcomesFramework.Link: http://www.dh.gov.uk/health/<strong>2012</strong>/05/nhs-companion-copd/Making medical tests work for you: offering patients more choice:For the first time, patients will now have more choice about where, when<strong>and</strong> how they receive some of the most common medical tests. Newproposals published during May outlined how patients will be able tochoose where they receive essential tests, including blood tests <strong>and</strong> heartscans. From April 2013, patients will be able to pick somewhere closer tohome, or near where they work, instead of having to accept the nearerlocation offered.For further information, go to:http://mediacentre.dh.gov.uk/<strong>2012</strong>/05/23/offering-patients-more-choice/NHS Commissioning <strong>Board</strong> Authority Update:The NHS Commissioning <strong>Board</strong> Authority (<strong>Board</strong> Authority) has publishedthe proposed configuration, member practices, indicative running costsallowances, <strong>and</strong> the complete list of authorisation waves, for 212proposed Clinical Commissioning Groups (CCGs). There are nowproposed CCGs covering the whole of Engl<strong>and</strong>. The geographicalboundaries have been drawn for each of them for the first time. Thepractice information provides the planning assumptions about the memberpractices in each proposed CCG. The <strong>Board</strong> Authority has also publishedNational <strong>and</strong> Regional CCG maps.Links: www.commissioningboard.nhs.uk/<strong>2012</strong>/05/24/board-meet-21012/Interim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
5Friends <strong>and</strong> family test:An NHS ‘friends <strong>and</strong> family’ test to improve patient care <strong>and</strong> identify thebest performing hospitals in Engl<strong>and</strong> has been announced by the PrimeMinister. From April 2013, patients will be asked a simple question;whether they would recommend hospital wards, accident <strong>and</strong> emergencyunits to a friend or relative based on their treatment.Link: http://www.dh.gov.uk/health/<strong>2012</strong>/05/friends-family/Transfer of patient safety function to the NHS Commissioning <strong>Board</strong>Special Health Authority:On 1 June this year, the key functions <strong>and</strong> expertise for patient safetydeveloped by the National Patient Safety Agency (NPSA) transferred tothe NHS Commissioning <strong>Board</strong> Special Health Authority. This ensurespatient safety is at the heart of the NHS <strong>and</strong> builds on the learning <strong>and</strong>expertise developed by the NPSA, driving patient safety improvement.Link: http://www.npsa.nhs.uk/corporate/news/transfer-of-patient-safetyfunction/World class procurement in the NHS – call for evidence <strong>and</strong> ideas:Sir Ian Carruthers, on behalf of the NHS Chief Executive, has issued a callfor evidence on how procurement in the NHS can be transformed todeliver the highest quality patient care, offer value for money, supportinnovation <strong>and</strong> stimulate growth in the UK. This is part of a widerengagement process that will report in December <strong>2012</strong>.Link: www.dh.gov.uk/health/<strong>2012</strong>/05/procurement-review/NHS procurement guidance <strong>and</strong> the NHS st<strong>and</strong>ards of procurement:The guidance aims to start the journey to world class procurement byidentifying actions which require immediate attention <strong>and</strong> to layfoundations for a fuller <strong>and</strong> further reaching procurement strategy later inthe year, following a wider call for evidence, as mentioned above.Link: www.dh.gov.uk/health/category/qipp-procurement/PCT Estate – planning for property transfers:On 1 April 2013 PCTs <strong>and</strong> SHAs will be abolished. On, or beforeabolition, it is imperative that all PCT <strong>and</strong> SHA estates, <strong>and</strong> associatedassets rights <strong>and</strong> liabilities, are properly dealt with. It is proposed that alltransfers to successor bodies will take place at a single point on 31 March2013. The aim is to have all documentation prepared <strong>and</strong> signed off bythe 31 December <strong>2012</strong>, with an effective date of 31 March 2013. Thedocuments describe the actions <strong>and</strong> timetable required to prepare forthese transfers.Link: http://www.dh.gov.uk/health-category/publications/letters-circulars/Interim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
6David Behan CBE appointed CQC Chief Executive:David Behan CBE, the Department’s Director General of Social Care,Local Government <strong>and</strong> Care Partnerships, has announced his departureto take up the role of Chief Executive at the Care Quality Commission(CQC).For further information, go to: http://www.dh.gov.uk/health/<strong>2012</strong>/06/davidbehan-cqc/NHS Chief Executive’s annual report published:The Department of Health has published ‘the year’, NHS Chief ExecutiveSir David Nicholson’s annual report for 2011/12, in which he reviews theachievements of the previous 12 months <strong>and</strong> considers the challenges tocome. This edition also includes ‘the quarter’, which provides thedefinitive account of how the NHS is performing at National level againstthe requirements <strong>and</strong> indicators set out in the NHS Operating Framework2011/12.For further information, go to: http://www.dh.gov.uk/health/<strong>2012</strong>/06/theyear-2011_12/NHS patient feedback challenge – expert panel announced:The NHS patient feedback challenge, created <strong>and</strong> managed by the NHSInstitute for Innovation <strong>and</strong> Improvement <strong>and</strong> funded by the Department ofHealth, is a one year programme to find <strong>and</strong> spread great approaches toimproving services, using patients’ feedback. It is an opportunity tomeasure how we are doing <strong>and</strong> share ways to improve the patientexperience across the NHS. The NHS patient feedback challenge isbacked by a £1m fund.For further information, go to:http://www.dh.gov.uk/health/<strong>2012</strong>/06/feedback-challenge-panel/Ambulance h<strong>and</strong>over delays:This letter from David Flory focuses on the increased concern about theongoing problem of patient h<strong>and</strong>overs from ambulances to hospitals.While this is not a widespread problem, the unacceptably long h<strong>and</strong>overtimes in a number of places are sufficient to warrant focused attention.Link: http://www.dh.gov.uk/health/<strong>2012</strong>/06/patient-h<strong>and</strong>over-delays/Accelerating the release of public sector l<strong>and</strong> for development:This letter from David Flory updates the NHS on progress with theircontribution to the Government’s plans to build 100,000 new homes onpublic sector l<strong>and</strong>. Further information on guidance <strong>and</strong> support availableto the NHS is included at the link below.Link: http://www.dh.gov.uk/health/<strong>2012</strong>/06/update-surplus-l<strong>and</strong>/Interim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
7Delivering safe <strong>and</strong> sustainable Cost Improvement Programmes(CIPs) Conference:On 11 September <strong>2012</strong>, David Bennett, Chair <strong>and</strong> acting Chief Executive,Monitor, in partnership with the Healthcare Financial ManagementAssociation (HFMA), will deliver a keynote speech. The Conference aimsto provide a high level forum for learning, discussion <strong>and</strong> debate between<strong>Board</strong> members around the <strong>Board</strong>’s role in delivering safe <strong>and</strong> sustainableCost Improvement Programmes. Jim Easton, Director of ImprovementTransformation, NHS Commissioning <strong>Board</strong> Authority, will speak, as willothers. The Conference chair is Eric Morton, Interim Chief Executive,Morecambe Bay NHS Foundation <strong>Trust</strong>.Link: http://www.hfma.or.uk/events-<strong>and</strong>-conferences/national/cip.htmInterim Chair & Chief Executive’s Report – <strong>July</strong> <strong>2012</strong>
EXECUTIVE SUMMARYTITLE:Declaration of Member’s Interests for <strong>2012</strong>/13BOARD/GROUP/COMMITTEE:<strong>Trust</strong> <strong>Board</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:Each Executive Director <strong>and</strong> Non-ExecutiveDirector must declare annually any Membershipof Professional Associations <strong>and</strong> Charitablebodies, <strong>and</strong> whether they hold Directorship <strong>and</strong>Shareholdings in Public <strong>and</strong> Private companies□ TEC ……………..….. □ STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT ………….……..….□ CLINICAL GOVERNANCE …………..………….....……□ CHARITABLE FUNDS ………………………………...…□ TRUST BOARD ……………………………….………….□ REMUNERATION ………………………………….…...□ OTHER …………………………..……. (please specify)2. DECISION REQUIRED: CATEGORY:The <strong>Board</strong> is asked to note this report.□ NATIONAL TARGET□ CQC REGISTRATION□ CNST□ HEALTH & SAFETY3. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:NA□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROM COMMISSIONERS CORPORATE OBJECTIVE Compliance withstatutory obligation under the Code ofAccountability for NHS <strong>Board</strong>s.□ OTHER …………………….. (please specify)AUTHOR/PRESENTER:Sue Williams, Executive Assistant to CEO & ChairmanDATE: 25 June <strong>2012</strong>4. DELIVERABLESNA5. KEY PERFORMANCE INDICATORSNAAGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________
DECLARATION OF INTERESTS <strong>2012</strong>/13Interests Declared<strong>Board</strong> MemberCharitable Bodies<strong>Trust</strong>ee, Sight Action (<strong>Havering</strong>)National Development Lead, The Health Quality Improvement Partnership (HQIP)Vice President (to March 2013) President (March 2013/15), British Transplant SocietyChair of Council (2007 onwards), London School of Jewish StudiesGovernor (Secondary School 2009), Immanuel College, Bushey, HertsWilliam LangleyElaine Young (Wife - David Wragg)Prof Anthony WarrensProf Anthony WarrensProf Anthony WarrensStatutory BodiesMember, Advisory Committee for Safety in Blood, Tissues <strong>and</strong> Organs (2008 onwards)Member, UK (Transplant) Donation Ethics Committee (2009 onwards)Prof Anthony WarrensProf Anthony WarrensDirectorships:Private CompaniesDirector, Protopack (Food Packaging Design Company)Director, Tranquil Training (Inl<strong>and</strong> Waterways RYA Training School)Executive Director, LUDO Management LtdKeith MahoneyKeith MahoneyWilliam LangleyJune <strong>2012</strong>
Associate, Zenon ConsultingDirector, MD Heath Consultancy Ltd (2004)Company Secretary, MD Health Consultancy Ltd (2004)Dr Maureen DalzielDr Maureen DalzielIan Dalziel (Husb<strong>and</strong> – Dr Maureen Dalziel)OtherConsultant, Private Practice at Hartswood Hospital, BrentwoodConsultant, Hunter HealthcareLeader (Member), London Borough of <strong>Havering</strong>Non Executive Director, London Thames Gateway Urban Development CorporationChairman, East <strong>and</strong> South East London Transport Partnership<strong>Board</strong> Member, London Enterprise Partnership<strong>Board</strong> Member, LGA Improvement <strong>Board</strong><strong>Board</strong> Member, Capital Ambition<strong>Board</strong> Member, NHS Supply Chain Customer <strong>Board</strong>Company Director, Caroline Wright Communications LtdDirector, British Education Supplies AssociationConsultant, Private Clinical Practice at Wellington, Garden <strong>and</strong> London Independent Hospitals (2009 onwards)<strong>Board</strong> Member, Intensive Care National Audit Research Centre (ICNARC) (1994)<strong>Board</strong> Member, British Pregnancy Advisory Service (BPAS) (2007)Mr Stephen BurgessDr Robert RoyceMichael WhiteMichael WhiteMichael WhiteMichael WhiteMichael WhiteMichael WhiteKeith MahoneyCaroline WrightCaroline WrightProf Anthony WarrensDr Maureen DalzielDr Maureen DalzielJune <strong>2012</strong>
Shareholdings:Private CompaniesJune <strong>2012</strong>
EXECUTIVE SUMMARYTITLE:BOARD/GROUP/COMMITTEE:Infection Control annual report <strong>Trust</strong> <strong>Board</strong> 4 <strong>July</strong> <strong>2012</strong>1. PURPOSE: REVIEWED BY (BOARD/COMMITTEE) <strong>and</strong> DATE:Attached is the annual infection control reportfor 2011/12, which will be published on the <strong>Trust</strong>website.The June Infection Control Committee alsoreviewed the plans for <strong>2012</strong>/13. keydeliverables are:- implementation of the ANTT programme,due for launch in <strong>July</strong>- re-launch of a <strong>Trust</strong>-wide “clan yourh<strong>and</strong>s” campaign- review of the management of norovirusoutbreaks, following the external reviewby Dr Hosein <strong>and</strong> the recent publicationof best practice guidance by the HPAfrom the Norovirus Working Partyx□ TEC…26.6.12….. □ STRATEGY……….….…….□ FINANCE ……..……… □ AUDIT ………….……..….□ QUALITY & SAFETY …………..………….....……□ CHARITABLE FUNDS ………………………………...…□ TRUST BOARD ……………………………….………….□ REMUNERATION ………………………………….…...x□ OTHER …Infection Control Committee 12.6.122. DECISION REQUIRED: CATEGORY:Ratification of the annual report. Agreement tosupport the highlighted initiatives for <strong>2012</strong>/13x□ NATIONAL TARGET □ CNST□ CQC REGISTRATION □ HEALTH & SAFETY□ ASSURANCE FRAMEWORK□ CQUIN/TARGET FROM COMMISSIONERS□ CORPORATE OBJECTIVE ……………………………....□ OTHER …………………….. (please specify)PRESENTER: Deborah Wheeler, Director ofNursing/DIPCDATE: 26.6.123. FINANCIAL IMPLICATIONS/IMPACT ON CURRENT FORECAST:4. DELIVERABLES5. KEY PERFORMANCE INDICATORSAGREED AT ______________________ MEETINGORREFERRED TO: __________________________DATE: ____________________________DATE: ____________________________REVIEW DATE (if applicable) ___________________________
Director of Infection Prevention <strong>and</strong> ControlAnnual ReportApril 2011 – March <strong>2012</strong>Authors:Sheila O’MahonyMatron Infection Prevention & ControlDr Lindsey BainInfection Control Doctor/Consultant MicrobiologistMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM1
CONTENTS1.0 EXECUTIVE SUMMARY 52.0 BACKGROUND INFECTION PREVENTION AND CONTROLARRANGEMENTS2.1 Infection Prevention <strong>and</strong> Control Team structure 72.2 Budget allocation for infection prevention <strong>and</strong> control staffing 72.3 Infection Control Committee 82.4 Infection Prevention <strong>and</strong> Control Annual Plan 82.5 Training/Education delivered by the Infection Prevention <strong>and</strong> Control Team 92.6 IPCT Training <strong>and</strong> Development 103.0 HEALTH CARE ASSOCIATED INFECTION RATES & OTHER IPCSURVEILLANCE3.1 Results of M<strong>and</strong>atory HCAI Reporting 103.1.1 MRSA Bacteraemia 103.1.2 Clostridium difficile 123.1.3 GRE Bacteraemia 133.1.4 Orthopaedic Surgical Site Infections 133.2 Trends in Health Care Associated Infections Statistics 143.2.1 Urinary catheter associated bacteraemia (CAUTI) 143.3 Outbreaks <strong>and</strong> incidents 143.3.1 Outbreaks of Norovirus (or presumed Norovirus) infection leading toclosure of wards3.3.2 Other outbreaks/incidents of infectionQueen’s Hospital3.3.3 Neonatal Intensive Care Unit 153.3.4 Harvest B Ward outbreak of Mupirocin Resistant MRSA3.3.5 Neurosciences Unit Patient with Sporadic Creutzfeldt Jacob DiseaseKing George Hospital3.3.6 Ante Natal Chicken pox incident 163.3.7 ITU - Vancomycin resistant Enterococcus/ Klebsiella 164.0 HAND HYGIENE 165.0 DECONTAMINATION 175.1 Arrangements 175.1.1 Decontamination Committee Activities 176.0 CLEANING SERVICES 17Page71014151516Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM2
6.1 Management Arrangements Queen’s Hospital 176.1.1 Monitoring Arrangements 176.2 Management Arrangements KGH 186.2.1 Monitoring Arrangements 186.3 Patient Environment Action Team Audits (PEAT) Results 2011 187.0 AUDITS AND EXTERNAL PEER REVIEW 197.1 Audit Programme 197.2 Quality of care audits – improving the quality of nursing care using acontinuous audit cycle207.2.1 Process 207.2.2 Results 207.2.3 Health care associated Infections (HCAI’s) peer review 207.3 Report from Antimicrobial Pharmacists/Consultant Microbiologists 227.3.1 Background 227.3.2 Guideline development <strong>and</strong> implementation 227.3.3 Development of the <strong>Trust</strong> Antimicrobial Management Code.237.3.4 Implementation of the <strong>Trust</strong> Antimicrobial Management Code237.3.5. Formation of the Antimicrobial Stewardship Committee 237.3.6 Education <strong>and</strong> Training 247.3.7. Adult Pocket Antimicrobial Guide for Common Infections 247.3.8 Audits 248.0 ACTION PLAN FOR <strong>2012</strong>/3013 258.1. Audits 258.2 Education <strong>and</strong> training 258.3 Guidelines 258.4 Paediatric Antimicrobial guidelines 258.5 Miscellaneous 259.0 CONCLUSIONS 2610.0 REFERENCES 26APPENDICESMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM3
Appendix 1 Clinical Governance reporting chart 27Appendix 2Infection Prevention & Control Team organisational chart…………………………………………………….Appendix 3 IPC Annual <strong>Trust</strong> Action Plan 2011-<strong>2012</strong> 29Appendix 4IPC Annual <strong>Trust</strong> Action Plan <strong>2012</strong>-2013 including the annual plan foreducation <strong>and</strong> the annual plan of audit2834Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM4
1.0 EXECUTIVE SUMMARYThis report covers the period from April 1 st 2011 to March 31 st <strong>2012</strong> <strong>and</strong> informs the <strong>Board</strong> ofthe progress being made to reduce Health care associated infections HCAI <strong>and</strong> to agree theAnnual Plan for sustained reduction <strong>and</strong> improvements in infection control practices for<strong>2012</strong>/13. In December 2010 a revised code of practice was introduced for the prevention<strong>and</strong> control of health care associated infections (HCAI); The Health Act (2008), Code ofPractice on the Prevention <strong>and</strong> Control of Infections <strong>and</strong> Related Guidance. The code ofpractice is also referred to as the Hygiene Code <strong>and</strong> is regulated by the Care QualityCommission the <strong>Trust</strong> remains fully compliant with the Hygiene Code. The Hygiene Coderequires the Director of Infection Prevention <strong>and</strong> Control (DIPC) to produce an annual reporton the state of healthcare associated infections in the organisation.This report includes:‣ A description of the Infection Prevention <strong>and</strong> Control infrastructure‣ An update on the <strong>Trust</strong>'s performance against key targets for infection prevention <strong>and</strong>control‣ A summary of initiatives <strong>and</strong> activities‣ Detail of key successes <strong>and</strong> areas for future developmentThe final plan for year 2011-<strong>2012</strong> is in Appendix 3. Actions outst<strong>and</strong>ing are added into theannual plan for <strong>2012</strong>-2013 which is in appendix 4.The <strong>Trust</strong> achieved the annual Clostridium difficile (C.diff) improvement objectives. Therewere 43 cases against a target of no more than 81. Last year there were 111 cases against atarget of no more than 128.The <strong>Trust</strong> unfortunately exceeded the annual target for MRSA bacteraemias which was 10cases against a target of 8. Last year there were 14 cases against a target of no more than11. However, on 2 occasions the <strong>Trust</strong> went over 100 days without a bacteraemia.As the <strong>Trust</strong> breached the annual objective of 8 cases of MRSA bacteraemia with 4 cases inNovember taking the year to date total to 9 the improvement team from NHS Londonundertook a peer review. The performance team at NHS London had set up project groupsacross London to review processes <strong>and</strong> systems in place to enhance the Government’saspiration that all NHS organisations adopt a zero tolerance approach to all avoidablehealthcare associated infections. The review was done in January <strong>2012</strong> at Queens Hospital.The review team concluded that BHRUT had most of the actions required to reduce HCAI inplace <strong>and</strong> a desire to create much stronger local accountability, assurance <strong>and</strong> governanceprocesses to sustain reductions in HCAI. They had nothing new to recommend in terms ofMRSA, <strong>and</strong> its control but, suggested the focus should continue to be on: antibioticstewardship; prompt diagnosis <strong>and</strong> isolation; competent clinical practice <strong>and</strong> cleaning <strong>and</strong>environmental hygiene. Recommendations have been added to the infection control annualplan.The Infection Prevention & Control Team (IPCT) had a busy year with yet again a particularlychallenging Norovirus season that resulted in BHRUT being an outlier in the region foroutbreaks of diarrhoea <strong>and</strong> vomiting. The ward based ward outbreak management trainingMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM5
that was delivered from August to December demonstrated continuing improvement in staffawareness <strong>and</strong> prompt reporting of potential outbreaks of infection.There were 42 ward closures resulting in 1,360 bed days lost <strong>and</strong> 30 wards had positivenorovirus results. During last years norovirus season there were 28 wards closed with 1,092bed days lost <strong>and</strong> only 7 wards confirmed norovirus positive. This was a significant increasein closures to last year’s norovirus season <strong>and</strong> posed challenges for all services involved toensure minimum disruption to planned <strong>and</strong> emergency activity. Reviews of the outbreaks didnot suggest any one reason why this was a particularly bad season. The IPCT willsummarise common themes that occurred during the outbreaks <strong>and</strong> ensure the pre norovirusseason training reflects the themes.As well as wards that were closed a further 48 wards reporting diarrhoea <strong>and</strong> vomiting wereinvestigated but NOT closed initially. From the 48 wards 40% were confirmed noroviruspositive. Five of the 48 wards were closed after 24 hours observation because more patientsdeveloped symptoms of D&V presenting like norovirus.From September 2011 the IPCT held monthly outbreak review meetings with ward staff,domestic services, <strong>and</strong> representatives from the Health Protection Agency (HPA) <strong>and</strong>Primary Care <strong>Trust</strong>s. The meetings were based around the HPA‘s Top Ten Tips (TTT) fornorovirus management <strong>and</strong> proved useful in identifying any issues that occurred during theoutbreak for action. Common themes were delay in isolating patients with diarrhoea,inappropriate use of gloves <strong>and</strong> staff working whilst symptomatic. However the meetings alsohighlighted areas of good practice including prompt reporting of patients, excellent nursingcare of sick patients <strong>and</strong> high st<strong>and</strong>ards of cleaning.Other outbreaks/incidents of infection included:-The Neonatal Intensive Care Unit (NICU) QH had clusters of neonates with multi resistantorganisms.Harvest B ward at Queen’s Hospital had an outbreak of Mupirocin resistant MeticillinResistant Staphylococcus Aureus (MRSA)1 chicken pox incident in the Maternity unit at KGHITU –KGH Vancomycin resistant Enterococcus/ Klebsiella1 Patient identified with Sporadic Creutzfeldt Jakob Disease (CJD)Work continued to complete root cause analyses (RCA) of Meticillin Resistant StaphylococcalAureus bacteraemias. From April 2011 all Meticillin Sensitive Staphylococcus Aureus(MSSA) bacteraemias were also investigated using the RCA tools. In January <strong>2012</strong> the IPCTdevised a rapid review tool to review the MSSA’s because of the large number <strong>and</strong> amount oftime it took to complete the RCA’s. This, in addition to completion of other priority RCA’s wasputting pressure on the clinical areas which delayed the opportunity to ascertain the rootcause <strong>and</strong> the implementation of any actions required.The continuing compliance with Saving Lives formed the basis of the infection control annualplan. Further work is required to achieve robust information to monitor against but inconjunction with the quality of care programme, which was previously known as the visibleleadership programme, significant improvements have been made to clinical practice.Training in infection prevention & control included the very popular passport study days, linknurse programme, general staff induction, registered nurse <strong>and</strong> support workers induction. InMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM6
January <strong>2012</strong> consultant’s m<strong>and</strong>atory training commenced: On a monthly basis the IPCTdelivered h<strong>and</strong> hygiene session using the ‘glo germ’ kit.Audits undertaken include environmental, personal protective equipment audits <strong>and</strong> isolationaudits.The key risks during this period were exceeding the MRSA target. <strong>and</strong> managing theNorovirus outbreaks.2.0 BACKGROUND INCLUDING INFECTION PREVENTION & CONTROLARRANGEMENTSThe work of the infection prevention & control department supports the <strong>Trust</strong> in minimisingthe risk of healthcare acquired infection to patients in accordance with <strong>and</strong> taking intoaccount the duties of the Hygiene Code, NHS Litigation Authority (NHSLA) <strong>and</strong> the CareQuality Commission’s Core st<strong>and</strong>ards. The <strong>Trust</strong> is compliant with the Health <strong>and</strong> SocialCare Act 2010 Outcome 8: Improve cleanliness <strong>and</strong> infection control compliance levels whichis regulated by the Care Quality Commission2.1 Infection Prevention & Control Team structure (IPCT)Deborah Wheeler, Executive Director of Nursing is in her 3 rd year at the <strong>Trust</strong> <strong>and</strong> remainsthe Director of Infection Prevention & Control (DIPC). The DIPC is accountable to the ChiefExecutive <strong>and</strong> is responsible for the strategy, policy development, implementation <strong>and</strong>performance relating to all aspects of infection prevention <strong>and</strong> control. Appendix 1 shows thereporting line for the team through to <strong>Trust</strong> board; Appendix 2 shows the team structure.The Infection Control Doctor (ICD) is Dr Lindsey Bain, who meets with the IPCT fortnightly toreview infection control issues <strong>and</strong> review any new guidance or policy changes. Dr Bain waspreviously allocated 4 professional activities (PA’s) for infection control per week. This wasnot achievable after one of the 4 microbiologists left the <strong>Trust</strong> in December 2011. As a resultof this Dr Bain now has only 2 PA’s for infection control distributed across the weekThe infection prevention & control team operate during normal working hours, <strong>and</strong> consist of:• 1 wte b<strong>and</strong> 8b Matron• 2 wte b<strong>and</strong> 7 senior infection prevention <strong>and</strong> control nurses (SIPCN’s)• 1 wte b<strong>and</strong> 7 practice facilitator• 2 wte b<strong>and</strong> 6 infection prevention & control nurses (IPCN’s)• 1.67 wte b<strong>and</strong> 4 administrative support.One of the b<strong>and</strong> 7 nurses was on maternity leave until March <strong>2012</strong> <strong>and</strong> had a phased returnto work. The team were able to recruit a b<strong>and</strong> 2 Health Care Assistant from King Georgemedical assessment unit on a secondment basis for 4 months. This secondment ceases inJune <strong>2012</strong>. The secondee was trained to undertake audits of h<strong>and</strong> hygiene, isolation <strong>and</strong>personal protective equipment. She also did ward to ward h<strong>and</strong> hygiene training <strong>and</strong> followedup practice after outbreaks of D&V. <strong>and</strong> was well received by clinical colleagues. Thissecondment proved to be an advantage for the IPCT as it enabled them to concentrate onother clinical duties <strong>and</strong> policy development.Matron Sheila O’Mahony <strong>and</strong> Dr Lindsey Bain are taking early retirement in <strong>July</strong> <strong>and</strong> Augustrespectively so the <strong>Trust</strong> is recruiting to these posts.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM7
2.2 Budget allocation for infection prevention <strong>and</strong> control staffingSUMMARYStaff Group Amount £Administrative support 46,773.00Nursing 312,316.00Total 359,089.00The IPCT does not have a dedicated budget for consumables or other overheads required todeliver infection prevention <strong>and</strong> control training to staff. Tools for teaching <strong>and</strong> managingoutbreaks have been sourced by BHRUT charity money <strong>and</strong> support from companyrepresentatives. The IPCT won the £200 first prize for the Annual Clinical Audit competitionby presenting an audit on improvements on implementation of the Clostridium difficile policyusing exception reports. The team used the prize money to purchase h<strong>and</strong> held monitors thatcan be used for audit purposes <strong>and</strong> verification that cleaning procedures are working. Theuse of the monitors will progress through <strong>2012</strong>-2013The Infection prevention <strong>and</strong> control service delivery is supported by many other staff <strong>and</strong>departments, but specifically by consultant microbiologists, antibiotic pharmacists, facilitiesdept, occupational health team <strong>and</strong> clinical matrons. The core infection prevention & controlservice is advisory <strong>and</strong> educational whilst maintaining programmes of audit, surveillance <strong>and</strong>management of outbreaks, both seasonal <strong>and</strong> unexpected.2.3 Infection Control CommitteeThe <strong>Trust</strong> Infection Control Committee (ICC) met bi monthly chaired by the Director ofNursing in her role as DIPC. The ICC agenda reflected the infection control annual plan <strong>and</strong>therefore ensured compliance with the Saving Lives High Impact Actions Programme <strong>and</strong>compliance with the Health Act. All MRSA <strong>and</strong> Clostridium.difficile RCAs are signed off bythe DIPC <strong>and</strong> are presented as a summary action plan at each Infection Control Committee(ICC). The MRSA RCAs this year were also signed off by the Chief Executive <strong>and</strong> MedicalDirector. Attendance at the ICC is variable but with the development of the newly appointedclinical business units there will be designated clinical leads for infection prevention & control.The proposal is that the leads attend the committee <strong>and</strong> participate in championing the highimpact interventions within their own units. They will also be involved in audit programmeslinking into the infection prevention annual plan. As the role is new it will be progressed <strong>and</strong>developed through the year.Infection control policies were reviewed <strong>and</strong> updated as necessary including:-‣ The Control <strong>and</strong> Management of Panton Valentine Leukocidin (PVL) AssociatedStaphylococcus Infections Policy‣ The Management of Patients with suspected or confirmed Transmissible SpongiformEncephalopathy TSE/CJD‣ The Infection Prevention & Control policy‣ Isolation Policy‣ Varicella Vaccination for health care staff policy (Occupational Health)‣ Policy for the Control <strong>and</strong> Management of Norovirus Policy‣ Guidelines for taking blood culturesMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM8
The implementation of the Root Cause Analysis (RCA) policy proved useful to get theprocess embedded into clinical areas. The investigation tools for MRSA <strong>and</strong> Clostridiumdifficile were amended so they were easier to complete. Further review of the policy isscheduled for June <strong>2012</strong> to ensure the RCA process is consistent throughout the <strong>Trust</strong>.2.4 Infection Prevention <strong>and</strong> Control (IPCT) Annual PlanThe 2011-<strong>2012</strong> annual plan focussed on achieving MRSA <strong>and</strong> Clostridium difficile targets,implementing the emergency MRSA screening, Saving Lives high impact interventions <strong>and</strong>compliance with the Health & Social Care Act <strong>and</strong> requirements of the Care QualityCommission. The year end updated plan is attached at Appendix 3The annual plan for <strong>2012</strong>-2013 is attached in Appendix 4. Implementation of the annual planis monitored by the Infection Control Committee <strong>and</strong> reported to the Quality & SafetyCommittee, which is a committee of the <strong>Trust</strong> <strong>Board</strong> (Appendix 1).2.5 Training/Education delivered by the IPCTThe IPCT maintained the monthly infection prevention & control passport study day for 8months of the year; 398 staff attended in this year. The February passport study day wascancelled due to organisational pressures. The infection prevention <strong>and</strong> control link nursesmet quarterly <strong>and</strong> held an annual study day in November 2011. The link nurse programmehas been successful in training them to undertake the passport assessments in their ownareas. This has been achieved in 10 areas to date. The aim is for all the link nurses to beable to assess staff but priority areas are where outbreaks or other infection prevention orcontrol incidents occur.The IPCT also contribute to the following training sessions:‣ General induction twice a month‣ RGN induction 2 weekly‣ Healthcare Assistant induction monthly‣ Junior doctor Induction twice a year‣ IV cannulation <strong>and</strong> venepuncture monthly‣ <strong>Trust</strong> m<strong>and</strong>atory training sessions weekly‣ <strong>Trust</strong> Midwifery m<strong>and</strong>atory training monthly‣ Neonatal & Paediatric m<strong>and</strong>atory including doctors monthly‣ Contracted services as required‣ Principles & Practices at London South Bank University twice a year totalling 30 hoursof teaching This has been upgraded to Masters degree level for this year‣ Ward based training as requested <strong>and</strong> after all outbreaks of infection‣ Student nurse passport. This year 1 st .2 nd <strong>and</strong> 3 rd students attended the half daysessions monthly‣ 6 sessions a year on st<strong>and</strong>ard infection control precautions are dedicated toprofessions allied to medicineMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM9
Comparasion of Attendance at Formal Infection Prevention & Control Education & Trainingpresented at the <strong>Trust</strong> between:April 2010 - March 2011 & April 2011 - March <strong>2012</strong>120010008006004002002010/ <strong>2012</strong>011/<strong>2012</strong>0M<strong>and</strong>atory Registered NursesInduction Registered NursesInfection Control Link NursesPassport Registered NursesM<strong>and</strong>atory MidwiferyPassport HCSWM<strong>and</strong>atory HCSWInduction HCSW2.6 IPCT training <strong>and</strong> developmentThe IPCT Matron attended the national Infection Prevention Society Annual Conference inSeptember 2011. From the conference the team have implemented a new stool assessmentchart that supports investigation during outbreaks of diarrhoea <strong>and</strong> vomiting. This hasenabled staff to properly assess patients with diarrhoea <strong>and</strong> implement appropriate isolation,treatment <strong>and</strong> management.The Infection Prevention & Control Practice Facilitator is in the last semester of the MA Edwhich finishes in September <strong>2012</strong>3.0 HCAI RATES AND OTHER IPC SURVEILLANCE3.1 Results of M<strong>and</strong>atory HCAI Reporting3.1.1 MRSA BacteraemiaOccurrences of MRSA bacteraemia are displayed in the graph below.For 2011/12 the target given to the <strong>Trust</strong> applied only to ‘hospital acquired’ cases (diagnosedmore than 48 hours after admission). The target set was to reduce our rate to the median ofall trusts’ rates the previous year. This was not more than 8 cases. We ended the year with10 cases.Although we did not achieve the target set, we did see a 29% reduction in cases comparedwith 2010/11. This was the second successive year we saw a reduction of this magnitude,having reduced cases by 25% the previous year.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM10
During 2010/11 the process of root cause analysis of each case was devolved to thedivisions, who report outcomes <strong>and</strong> actions to the ICC. On review of the individual cases, 6were judged to have been potentially preventable: 1 post-operative infection, 3 venouscannula associated infections <strong>and</strong> 2 cases where the blood culture was potentiallycontaminated, although this is always difficult to prove. As previously seen, most infectionsoccur in medical patients, but the potentially preventable infections were mostly surgical.No. of cases14121086420MRSA Bacteraemias 2011/12diagnosed >48 hours since admissionApr May Jun Jul Aug Sep Oct Nov Dec Jan Feb MarMedCTDCummulative totalSurgW&CTargetThe graph below shows how BHRUT compares with other hospitals locally <strong>and</strong> nationally.For several years our improvement correlated with national figures, but then fell away. Oneobvious difference between BHRUT <strong>and</strong> other trusts is that we were late to implementscreening of emergency admissions. Screening of emergency patients according to DoHguidance commenced in December 2010 <strong>and</strong> has now been in place for 16 months. This ismonitored by monthly audit of wards. Across the <strong>Trust</strong> the compliance for the year was 75%.Recently a lot of work has gone into improving compliance <strong>and</strong> ensuring that the datagathered is as accurate as possible. National st<strong>and</strong>ards for compliance with emergencyadmissions have not been set, however preliminary results of the ‘National One Week’(NOW) prevalence audit of English trusts showed that the average compliance acrossEnglish trusts was only 61%. Further results from this study, which should show thecomparative prevalence of MRSA colonisation in BHR hospitals compared with the rest of thecountry, are expected in the coming summer.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM11
16.014.0<strong>Trust</strong>-apportioned MRSA bacteraemia rate, with <strong>Trust</strong>-apportionednational & regional rate<strong>Trust</strong>LondonEngl<strong>and</strong>12.0rate per 10,000 bed days10.08.06.04.02.00.0Oct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - DecJan -Apr - JunJul - SepOct - Dec2006 2007 2008 2009 2010 2011 <strong>2012</strong><strong>Barking</strong>, <strong>Havering</strong> & <strong>Redbridge</strong> Hospitals NHS <strong>Trust</strong>MRSA screening of elective <strong>and</strong> day case patients has been in place since April 2009.Compliance this year across the trust was only 69%. The infection prevention team haveworked with the information <strong>and</strong> surgical management teams to improve this. Development ofa computer programme by the information team identifies expected admissions that have notbeen screened, thereby enabling pre-emptive action. We have also done further work toclarify which groups of patients do not need screening. This has been made clear to theclinical units who can now focus on the screening of the correct patient group.3.1.2 Clostridium difficileCases of this infection are shown in the graph below. The target applied only to those caseswhich occurred more than 3 days after admission.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM12
No. of new cases80706050403020100Clostridium difficile 2011/12diagnosed >72 hours after admissionApr May Jun Jul Aug Sep Oct Nov Dec Jan Feb MarMedCTDCummulative totalSurgW&CTargetAs can be seen, BHRUT was well within the target of not more than 81 cases, ending theyear with 44 cases. This was a considerable improvement on results in 2010/11 when wehad 111 cases. We consider this is due to continuing the process of immediate individualpatient review against a set of st<strong>and</strong>ards produced from our existing policy, which we startedin October 2010 <strong>and</strong> have continued since. A summary of results is produced for review ateach infection control committee. The most common failing continues to be immediateisolation of patients who develop diarrhoea.3.1.3 GRE BacteraemiaThese are enterococci which are resistant to glycopeptide antibiotics (vancomycin <strong>and</strong>teicoplanin).There were 12 cases this year, a considerable increase in cases compared with the previoustwo years. There was no obvious connection between any of the cases <strong>and</strong> it is clear thatdifferent species of are enterococci involved. The most likely explanation is increased use ofantibiotics such as levofloxacin (introduced to comply with guidance for treating pneumonia)<strong>and</strong> meropenem (required for treatment of multi-resistant organisms) may have encouragedthe selection of these organisms; however this needs to be confirmed by audit or systematicreview. This will be implemented in <strong>2012</strong>. No actual date has been agreed for this to happenyet.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM13
GRE Bacteraemia at BHRUTOctober 2003 to March <strong>2012</strong>No. of cases876543210Oct-Dec 04Apr-Jun 05Oct-Dec 05Apr-Jun 06Oct-Dec 06Apr-Jun 07Oct-Dec 07Apr-Jun 08Oct-Dec 08Apr-Jun 09Oct-Dec 09Apr-Jun 10Oct-Dec 10Apr-Jun 11Oct-Dec 11KGH OCH/HWH/QH Total3.1.4 Orthopaedic Surgical Site InfectionsThe surgical division are responsible for collection of the data <strong>and</strong> have been reporting therepair of fractured neck of femur for the 3 periods to date. The data is uploaded to the HealthProtection Agency for Surgical Site Surveillance (SSIS) web site by the Trauma Co-ordinator.There are still some operational difficulties in collecting the information, however, there hasbeen a recent improvement with data collection as the trauma Co Ordinator now also ringsElm <strong>and</strong> Erica Ward at KGH on a daily basis where the orthopaedic patients who have beenoperated on at Queen’s Hospital for fractured neck of femur have their rehabilitation ifrequired. The Community Orthopaedic Project in Essex (COPE) Team also report any woundinfections following discharge.Within this period there have been 6 surgical site infections of which 4 were during admission<strong>and</strong> 2 after discharge that were identified by the COPE team. All these patients wereappropriately treated. In future the infection control lead for orthopaedics will report suchpatients <strong>and</strong> their management at the infection control committees.For the forthcoming year the surgical division have agreed to commence surveillance onpatients following elective hip or knee replacement. The start date has yet to be agreed.3.2 Trends in Health Care Associated Infection Statistics3.2.1 Urinary catheter associated bacteraemia (CAUTI )During 2010/11 we managed to achieve a 10% reduction in cases <strong>and</strong> the target for 2011/12was set at no more than 38 however the final figure for the year is 43. Whilst RCA processeshave not been initiated for this, the quality of care audits suggest that the introduction ofAseptic Non-touch Technique (ANTT) will address the asepsis on insertion of a urinarycatheter Further training will be given on the importance of continual aseptic managementduring the daily care of catheterised patients whilst maintaining a closed circuit As the rate ofcatheterisation reduces it is hoped that the CAUTI will also reduce.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM14
50Urinary Catheter Associated BacteraemiaApril 2011 - March <strong>2012</strong>No. of cases403020100Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb MarMed Clin Supp SurgW&C Target Cumm3.3 Outbreaks <strong>and</strong> incidents3.3.1 Outbreaks of Norovirus (or presumed Norovirus) infection leading to closure ofwardsThe total number of wards affected was more than in 2010/11 which puts BHRUT as anoutlier in the region. The ward staff did identify patients with sudden onset vomiting ordiarrhoea quickly which enabled the IPCT to implement outbreak management policy toensure tight control ensuring minimal transmission. Despite these measures Norovirus wasparticularly virulent. Prior to next years norovirus season the IPCT will summarise theoutbreak management review meetings <strong>and</strong> present the overall findings to the ICC <strong>and</strong>debate as to whether any other measures should be in place.18BHRUHT Wards closed due to Diarrhoea includingNorovirus 2006 - March <strong>2012</strong>1614No. of wards closed121086420Nov-06Mar-07Jul-07Nov-07Mar-08Jul-08Nov-08Mar-09Jul-09Nov-09Mar-10Jul-10Nov-10Mar-11Jul-11Nov-11Mar-12Wards closed due presumed Norovirus KGHWards closed due presumed Norovirus Queen's3.3.2 Other outbreaks/incidents of infectionMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM15
Queen’s Hospital3.3.3 Neonatal Intensive Care UnitIn January <strong>and</strong> September the Neonatal Intensive Care Unit (NICU) had clusters of neonatescolonised with multi resistant organisms but no clinical .infection. These clusters wereinvestigated <strong>and</strong> led to further environmental investigation of the tap water in the unit. Thisinvolved sampling of water used for h<strong>and</strong> hygiene. Following inconclusive results of the watersamples it was agreed to put in place a programme whereby the unit taps were ‘flushed’through <strong>and</strong> removal of any lime scale, prior to re sampling. Flushing simply means lettingthe taps run freely for 10-20 minutes twice a week. This was performed by the estatesdepartment. To ensure safety of the neonates a decision was taken to bathe the babies insterile water. After further water testing the IPCT was assured the tap water was safe but theuse of sterile water for bathing continues for level 2 neonates in the Queen’s NICU in theshort term until the newly formed Water Safety Group** (explained below) agree aprogramme of regular testing to be dictated by the department of Health. The method ofcleaning taps to ensure no recontamination was also reviewed <strong>and</strong> found to be satisfactory.Subsequent to this outbreak an incident occurred regarding Pseudomonas aeruginosa in aHospital in Northern Irel<strong>and</strong> <strong>and</strong> whilst the review is outst<strong>and</strong>ing guidance on management ofwater in critical care units has been updated <strong>and</strong> re issued. BHRUT is compliant with thisguidance <strong>and</strong> the IPCT, estates, domestic services <strong>and</strong> relevant clinical staff have formed a**Water Safety Group to progress future actions.3.3.4 Harvest B ward outbreak of Mupirocin resistant MRSASix patients from Harvest B ward were identified as being colonised with Mupirocin resistantMRSA between 13/04/2011 <strong>and</strong> 25/05/2011. The index case was identified on admission toBeech ward where MRSA screening was done. Although the first patient was identified inApril, no further cases were identified until a cluster of four patients in the week of 16/05/2011Actions were taken to minimise further spread including blitz cleaning, weekly MRSAscreening for 3 weeks <strong>and</strong> a 3 week long audit programme of st<strong>and</strong>ard infection controlprecautions. No further clusters of patients were identified as MRSA positive. There were noclinical infections associated with this episode.3.3.5 Neurosciences Unit- Patient with Sporadic Creutzfeldt Jakob Disease. (CJD)A patient was admitted to Neurosurgery with a diagnosis of Sporadic CJD. Followingoutbreak meetings including representatives from the Health Protection Agency <strong>and</strong> theirCJD section it was agreed that the patient had not had any procedures in BHRUT that poseda risk to other patients or staff.3.3.6 Ante Natal Chicken pox incidentA pregnant patient attended the ante natal clinic at KGH unaware she had chicken pox whichwas subsequently diagnosed by her GP the following day. As a significant exposure riskoccurred, a list of all patients <strong>and</strong> staff that were in direct contact with the infectious personwas compiled. Clinical advice about management of infected patients was obtained from theConsultant Microbiologist covering the relevant area. Staff were advised to contactOccupational Health if they did not know their immune status. 53 patients who were possiblecontacts were tested as soon as possible. Five of the 53 patients were found to be non-Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM16
immune. As a result of this incident a leaflet explaining Chicken Pox is being prepared for theante natal clinic to be given at the patient’s first visit.3.3.7 King George ITU - Vancomycin resistant Enterococcus/ KlebsiellaBetween 21/08/2011 <strong>and</strong> 29/08/2011 five patients in King George ITU became colonised withExtended Spectrum Beta Lactamase (ESBL) producing Klebsiella pneumoniae, two of whomsubsequently developed Vancomycin Resistant Enterococcus (VRE), <strong>and</strong> one patient wasidentified with VRE without a history of Klebsiella pneumoniae. A meeting was held toestablish any risks or contributing factors <strong>and</strong> links (medical /surgical l/geographical/prescribed antibiotics) between the affected patients <strong>and</strong> to determine any areas of deviationfrom best practice. It was found that the VRE was of different strains however 5 patients hadthe same Klebsiella strain. An action plan was put in place to ensure a safe environment <strong>and</strong>no further transmission occurred.4.0 HAND HYGIENEThe IPCT held h<strong>and</strong> hygiene awareness days in April <strong>and</strong> November 2011 <strong>and</strong> January2102. They had support from the Contract services Sodexo <strong>and</strong> the infection prevention &control Link nursesThe promotion of h<strong>and</strong> hygiene was achieved by a variety of ways including:-‣ Infection prevention & control Link nurses attending sessions at the Atriums of theboth hospitals <strong>and</strong> demonstrating the glo germ machine to members of the public <strong>and</strong>staff‣ Infection prevention & control Link nurses going to individual wards with a member ofthe IPCT promoting h<strong>and</strong> hygiene with the glo germ machines‣ Screen saver on PC desktops to remind staff about h<strong>and</strong> hygieneThe IPCT purchased 2 new Ultraviolet h<strong>and</strong> hygiene training kits.5.0 DECONTAMINATION5.1 ArrangementsThe DIPC is the executive lead for decontamination. The Matron of IPCT investigates <strong>and</strong>escalates any operational issues. The Sterile Services Department (SSD) is fully accredited<strong>and</strong> is overseen by a hard facilities contracts manager in BHRUT, who manages any noncompliances.5.1.1 Decontamination Committee ActivitiesDecontamination <strong>Trust</strong> wide audit was undertaken by an external consultant. Reports weresent to individual managers to progress any actions. These were followed up at the Medicaldevices/decontamination committee with an overall action plan that is monitored by thecommittee. The external auditor also visited the Sterile Service Department which ismanaged by the company Synergy. The audit findings were excellent other than a fewenvironmental issues which were dealt with at the time of the audit.6.0 CLEANING SERVICESMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM17
6.1 Management Arrangements Queens Hospital‣ Queens’s hospital is a 939 bed PFI hospital. The hospital building is operated by aprivate sector partner (Catalyst Healthcare Management) who manage theFacilities Management Company, Sodexo.‣ Sodexo are responsible for providing the cleaning, 24hrs a day with workschedules for each ward/department. Queens is cleaned to National St<strong>and</strong>ards ofCleanliness 2007, this was introduced in October 2011, all work schedules havebeen updated to reflect the enhanced cleaning, as previously the hospital wascleaned to 2002 st<strong>and</strong>ards.‣ Regular operations meetings continue to be held monthly between the <strong>Trust</strong>,Sodexo <strong>and</strong> Catalyst; the format of these meetings is to discuss <strong>and</strong> resolve anyoperational issues during that period. Any issues that cannot be resolved at thismeeting are escalated to the PFI <strong>Board</strong> meeting which again is held monthly, <strong>and</strong>the membership includes senior management from the <strong>Trust</strong>, Sodexo <strong>and</strong> Catalyst.‣ Catalyst issue a monthly report to the <strong>Trust</strong> to coincide with the PFI <strong>Board</strong> whichincorporates the Key Performance Indicators, along with the cleaning scoresachieved for the month.6.1.1 Monitoring Arrangements‣ Weekly walk around (environmental audit), which includes Soft <strong>and</strong> Hard FacilitiesManager for the <strong>Trust</strong>, Sodexo Domestic Manager, Sodexo Estates Manager &representation from Catalyst The Deputy Director of Nursing, <strong>and</strong> a member of theInfection Control Team now join the walk around.‣ The format for the walk around is to visit a specific area, <strong>and</strong> monitor the wholeenvironment.‣ Matrons’ audit Includes Soft Facilities Manager for the <strong>Trust</strong>, Sodexo Manager <strong>and</strong><strong>Trust</strong> Matrons, including the IPCT Matron. The format for the audit is to visit aspecific area, with the relevant matron, <strong>and</strong> use the NSC audit tool (49 point audittool).‣ Cleaning Audits: Sodexo Domestic Supervisors undertake audits using the NSCaudit tool, inline with the recommended frequencies for audit.6.2 Management Arrangements KGHThe <strong>Trust</strong> awarded a Total Facilities Contract to Sodexo in August 2009 for a period of 5years. There is a Contracts Manager to monitor the service provision.‣ Monthly TFM operational meetings are held with Sodexo Management Team <strong>and</strong>the <strong>Trust</strong> TFM Management team whereby any operational issues are dealt with..‣ The Domestic KPI report gives cleaning checklist scores for the month.‣ A TFM User Group meeting is also held monthly which comprises of DepartmentLeads for Sodexo, the <strong>Trust</strong> Contracts Managers, Infection Control <strong>and</strong> aMatron/s to discuss the day to day issues on the wards <strong>and</strong> departments <strong>and</strong> anychanges in procedures etc.‣ A quarterly review meeting is held between Senior Management of the <strong>Trust</strong> <strong>and</strong>Sodexo where issues have been escalated from the Operational meetings.6.2.1 Monitoring ArrangementsMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM18
‣ Domestic Service - Monitoring of the domestic service provision is carried out usingthe National St<strong>and</strong>ards of Cleanliness 49 point audit tool. The contractrequirement states that the cleaning of the hospital must be carried out to 2007st<strong>and</strong>ards <strong>and</strong> frequencies.‣ Monthly combined audits are carried out with Deputy Director of Nursing, InfectionControl <strong>and</strong> Soft Services Manager,‣ Matrons Audits are held bi-weekly <strong>and</strong> Infection Control <strong>and</strong> Nursing audit held biweekly.‣ The Soft Services Manager monitors Sodexo cleaning audits ward areas weekly.This year the <strong>Trust</strong> submitted total cleaning scores for the whole year. They are asfollows:-King George 96.6%- Queen’s Hospital 95.6%6.3 Patient Environment Actions Team Audits (PEAT) Results for <strong>2012</strong>-2011-2010-2009Scores for <strong>2012</strong>EnvironmentPrivacy & DignityFood ScoreSite NameScoreScoreKing George Hospital Good Excellent GoodQueen's Hospital Good Excellent GoodScores for 2011EnvironmentPrivacy & DignityFood ScoreSite NameScoreScoreKing George Hospital Good Excellent GoodQueen's Hospital Good Excellent GoodScores for 2010EnvironmentPrivacy &Food ScoreSite NameScoreDignity ScoreKing George Hospital Good Excellent GoodQueen's Hospital Good Good GoodScores for 2009EnvironmentPrivacy &Food ScoreSite NameScoreDignity ScoreKing George Hospital Good Acceptable AcceptableQueen's Hospital Good Excellent Good7.0 AUDIT AND EXTERNAL REVIEWS7.1 Audit ProgrammeThe IPCT undertake audits on an annual basis <strong>and</strong> as required due to an outbreak, incidentor untoward event.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM19
The audits <strong>and</strong> results are as follows:-AuditNo. of Wards/departmentsaudits2010-2011Results% Range2010-2011No. ofWards/departmentsauditedResults% Range.2011-<strong>2012</strong>2011-<strong>2012</strong>Environment 62 86-100 74 88-100Isolation 63 93-100 61 93-100Personal ProtectiveEquipment (PPE)69-98-100 74 87-100Written feed back is given to all wards /departments following an audit session. However,those who achieved a score below 90% are re audited within two weeks of the original audit.If there is no improvement a meeting is arranged with the Ward manager <strong>and</strong> Matron <strong>and</strong> theoutcomes are emailed to the Deputy Directors of Nursing.7.2 Quality of care – improving the quality of nursing care using a continuousaudit cycle.7.2.1 ProcessOn the timetabled days each clinical area is assessed by a staff member <strong>and</strong> the datacollected <strong>and</strong> analysed on the day. A third of the patients in every relevant clinical area areaudited. This enables immediate feedback to be given to the nurse in charge who identifieswith the auditor areas of good practice <strong>and</strong> areas which need to be improved before the areais audited again. .7.2.2 ResultsThese are presented on a dashboard which is sent monthly to ward teams, matrons, clinicaldirectors <strong>and</strong> senior nursing team <strong>and</strong> is RAG rated. Areas score green with 100%compliance, amber if above 90%, red if 89% or below, <strong>and</strong> pink if below 60%.H<strong>and</strong> hygiene Quarterly <strong>Trust</strong> percentagesJun-11 Aug-11 21.11.11 13.02.1267.50 76.93 69.67 66.51Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM20
IV cannula Quarterly <strong>Trust</strong> percentages05.05.11 18.07.11 31.10.11 30.01.1252.91 57.27 60.53 57.75Urinary Catheters Quarterly <strong>Trust</strong> percentages27.06.11 Sep-11 09.01.1278.84 83.23 80.24Action plans are written for areas that require assistance <strong>and</strong> this is monitored by thematrons, assistant director of nursing or Director of Nursing.7.2.3 Health Care Associated Infections (HCAI’s) Peer ReviewColleagues from NHS London undertook a review at BHRUT in January <strong>2012</strong> The purposewas to determine if the systems <strong>and</strong> processes in place were sufficiently robust <strong>and</strong> to beable to advise if there are additional actions the organisation could take. The team revieweda range of documentation provided by the IPCT The review team also observed theenvironment <strong>and</strong> practice by visiting a number of wards, <strong>and</strong> interviewed a range of staff.including the IPCT, Matrons, ward staff, cleaning staff <strong>and</strong> some medical staff. The full reporthas been shared with clinical staff, below are the key areas noted during the review.Key areas of action focus on the following risks:‣ <strong>Board</strong> to ward accountability‣ Staff having the necessary competence to assure consistent application of evidencebased practice when inserting lines <strong>and</strong> catheters <strong>and</strong> following agreed guidelines <strong>and</strong>protocols consistently‣ Assuring prudent antimicrobial practices are in place‣ Governance <strong>and</strong> assurance processes being robust enough to inform the <strong>Board</strong> ofprogress <strong>and</strong> alert the <strong>Board</strong> to any further risks.Culture <strong>and</strong> Ownership‣ To enhance medical engagement:Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM21
‣ Set objectives for HCAI with each clinical director‣ Identify medical leads for infection prevention within each speciality‣ Agree four or five specific actions <strong>and</strong> outcomes that BHRUT seek from the lead e.g.‣ RCA involvement‣ Antimicrobial prescribing‣ Training <strong>and</strong> competence‣ Involvement of juniors in HCAI/antibiotic audits‣ H<strong>and</strong> hygiene/BBE‣ Include objectives for HCAI in consultant job plans‣ Ensure this features in Consultant appraisalsRole of Infection Prevention & Control Team‣ The team work with “positive alerts.”‣ Explore ways to develop roles <strong>and</strong> seek ways to balance being reactive with aproactive approach that focuses on the strategic goals of the team<strong>Board</strong> Assurance‣ Build stronger relationships with specific directorates.‣ Review The <strong>Board</strong> how receives success a report of the on incumbent the Quality robust <strong>and</strong> “link Safety worker Performance role” can indicators. be measured Thisincludes a graph demonstrating compliance to agreed performance measures includingTraining HCAI’s <strong>and</strong> then has a section titled “Mitigating Actions”. Review this section to ensurethat the report articulates the risks to delivery <strong>and</strong> the actions required to minimise or‣ Reviewmitigateassessmentthese, in orderofthatcompetence,the <strong>Board</strong>particularlycan seek assurancefor clinicalonskillsthe effectivenesssuch as asepticof thesetechnique,controls.line insertion, <strong>and</strong> taking blood culture.‣ Build on existing work achieved on ensuring all staff inserting central lines are trainedRoot Cause Analysis<strong>and</strong> assessed.‣ Continue to undertake RCA’s <strong>and</strong> review by by the DIPC <strong>and</strong> Medical DirectorCleaning‣ ensure<strong>and</strong><strong>Trust</strong>Environmenthave a slightly more robust process for tracking progress <strong>and</strong> ensuring therequired changes are made‣ Ensure BHRUT these RCA’s have are copies owned of by all the the Clinical 2007 cleaning Business specificationsUnits‣ Review who is responsible for cleaning specific items of equipmentClinical The Audits IPCT have set up training sessions for ward managers <strong>and</strong> Sodexo to underst<strong>and</strong>roles <strong>and</strong> responsibilities <strong>and</strong> details of the 2007 cleaning st<strong>and</strong>ards‣ Test the effectiveness of the current methods of undertaking the audits required toAntimicrobial populate Stewardshipthe dashboard to be assured the controls are effective‣ As audits are weekly <strong>and</strong> staff generally know when they are taking place. Consider staff‣ Place auditing clear in areas responsibility they do not <strong>and</strong> normally expectation work in for or improvement getting other with staff the or volunteers senior leadership toteam undertake of the audits Clinical at different Business times. Units‣ Ensure this is underpinned with an effective governance <strong>and</strong> assurance process thatFunction articulates of Infection the risks Control to delivery Committee <strong>and</strong> the actions necessary to minimise or mitigate thoserisks.Review scope <strong>and</strong> assurance processes of ICC, including setting clear expectation‣ Undertake smaller audits more frequently until <strong>Trust</strong> is assured good practice isregarding attendance as there is an absence of medical staff (many sending apologies toembedded.the last two quarterly meetings).‣ ReviewUse formalcontent<strong>and</strong>ofinformalthe meetingmethods<strong>and</strong> review(such asto makejunioritdoctorsmore compelling,undertaking(suchaudits,as clinicians<strong>and</strong> seniormedicalbringingstaffrelevantcheckingtopicscomplianceto discuss) butduringalsowardensuringrounds)it adequatelyConsultantfulfils<strong>and</strong>itsseniorrole ofmedicalstaff providing need assurance. to regularly check <strong>and</strong> review antibiotic prescribing during their ward roundsPlansMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM22
Action plans are in place but to help in <strong>Trust</strong>’s desire to create greater local ownership<strong>and</strong> clarity of outcome, review them in order to:‣ Clearly identify <strong>and</strong> separate the corporate actions from the Directorate ones.‣ Identify the outcomes BHRUT are seeking rather than just the processes (e.g. highcompliance to antimicrobial prescribing) <strong>and</strong> align the actions to delivering those.‣ Clearly identify the person(s) accountable for the action(s) <strong>and</strong> the timescales fordelivery.‣ Put in place an effective process for tracking progress <strong>and</strong> identifying anyslippage to timescales so that issues are escalated <strong>and</strong> addressed.7.3 Report from Antimicrobial Pharmacists/Consultant MicrobiologistsThis report details the activities that have been carried by pharmacy <strong>and</strong> microbiology indeveloping a robust antimicrobial stewardship programme throughout BHRUHT in2011/<strong>2012</strong>.7.3.1 BackgroundThe point-prevalence baseline audit carried out in October 2010 highlighted that improvingthe documentation of antimicrobial prescribing is essential to allow monitoring of adherenceto guidelines <strong>and</strong> the appropriateness of antimicrobial prescribing. Based on the results, anumber of recommendations were made which led to the implementation of the antimicrobialstewardship programme at BHRUHT in 2011/<strong>2012</strong>. The programme included the followingelements:7.3.2 Guideline development <strong>and</strong> implementationThe process of reviewing antimicrobial guidelines was reviewed which included theimportance of communicating <strong>and</strong> cascading information to all prescribers <strong>and</strong> educatingstaff about them.The following guidelines approved by the Drugs <strong>and</strong> Therapeutics Committee have beenwritten in conjunction with consultant microbiologists <strong>and</strong> with the involvement of theappropriate senior medical staff:• Gastro-Intestinal Infections– May 2011• Lower Respiratory Tract Infections- June 2011• Updated Gentamicin Guidelines- Oct 2011• Obstetrics <strong>and</strong> Gynaecology Antimicrobial Guidelines- Nov 11• Adult pocket antimicrobial guide for common acute infections. Dec 2011• Amikacin once daily dosing <strong>and</strong> monitoring guidelines- Jan <strong>2012</strong>• Vancomycin dosing <strong>and</strong> monitoring guidelines -Jan <strong>2012</strong>• Gentamicin Multiple Daily Dosing Guidelines for the Treatment of Endocarditis-Jan <strong>2012</strong>• Treatment <strong>and</strong> prophylaxis of Influenzae- Jan <strong>2012</strong>• Gentamicin guidelines for paediatrics – Jan <strong>2012</strong>• Update of the Restricted Antimicrobial list- February <strong>2012</strong>7.3.3 Development of the <strong>Trust</strong> Antimicrobial Management CodeMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM23
This was written to avoid situations where patients are inappropriately exposed to longcourses of either intravenous or oral antibiotics <strong>and</strong> to allow monitoring of adherence toguidelines.The antimicrobial management code includes four antimicrobial prescribing indicators (APIs):‣ API- Indication of antimicrobial to be documented on drug chart <strong>and</strong> medicalnotes‣ AP2- Duration/stop date or review date documented on drug chart <strong>and</strong> medicalnotes‣ AP3- All IV antimicrobial therapy to be reviewed at 48 hours‣ AP4- Restricted antibiotics approved by microbiologists must be documentedon the drug chart7.3.4 Implementation of the <strong>Trust</strong> Antimicrobial Management CodeA multipronged awareness programme to implement the Antimicrobial Management codewas launched in April 2011 which comprised of:(i)(ii)(iii)(iv)(v)(vi)(vii)(viii)The distribution of the code to all medical, nursing <strong>and</strong> pharmacy staff via email.Display of policy poster on wards;A series of announcements at clinical team meetingsInduction for medical staffAn article on the hospital’s staff information bulletinDesktop image of the code on all <strong>Trust</strong> computersRedesign of a new drug chart to include dedicated antimicrobial prescribingsection to prompt prescribers to document the indication <strong>and</strong> durationA sticker designed to be used by clinical pharmacist to notify prescribers if therewas non compliance to the code.7.3.5. Formation of the Antimicrobial Stewardship CommitteeAn assessment of the trust against a published national evidence-based Antimicrobial Selfassessment tool recommended by the DOH was carried out in 2010 As a result of theassessment the following specific actions were completed:• A formal Antimicrobial Stewardship Committee with representation frompharmacy, microbiology, senior nursing staff <strong>and</strong> consultant from otherspecialities which reports to the Drugs <strong>and</strong> Therapeutics <strong>and</strong> Infection ControlCommittees was established, the first meeting was held on 28 th2011.A written audit strategy on antimicrobials.• Written strategy for Antimicrobial Education <strong>and</strong> Training.7.3.6 Education <strong>and</strong> TrainingSeptemberThe antimicrobial pharmacists <strong>and</strong> the consultant microbiologists were actively involved inclinical education. A m<strong>and</strong>atory antimicrobial stewardship training competency package wasdeveloped <strong>and</strong> was delivered to all junior doctors via hard copy <strong>and</strong> a one hour face-to-facetraining session. We have focussed our efforts not just on policy change but also educatingall staff across all disciplines to improve antibiotic prescribing. We have delivered over 30sessions of teaching to medical staff, nurses <strong>and</strong> pharmacists. As part of the antimicrobialMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM24
education <strong>and</strong> training package at BHRH we have set up an antimicrobial accompanied wardvisits for junior pharmacists. The main aim of these visits will be to aid their antimicrobiallearning <strong>and</strong> build on their confidence of dealing with antimicrobials whilst on the wards.7.3.7. Adult Pocket Antimicrobial Guide for Common InfectionsThe first edition of adult pocket guide was launched in January <strong>2012</strong>. The cards have beendistributed to all doctors <strong>and</strong> pharmacists7.3.8 AuditsThis financial year saw the 2 nd point prevalence study conducted at BHRH, providing afurther snapshot view of prescribing patterns within the trust. Consequently, this has allowedcomparisons to be drawn against last year’s audit conducted. (Table 1).Table 1 Point Prevalence Audit2010 2011No of charts seen 649 868No of antimicrobials prescribed 378 409Allergy Documented 99.5% 99.7%Nature of Allergy documented 21% 33%Indication documented in Drug Chart 7% 53.3%Indication documented in medical notes or 67% 84.1%drug chartDocumentation of duration/course length 32% 51%on drug chartFollowing regular teaching to doctors <strong>and</strong> the greater awareness that has been raised aroundthe documentation of course lengths, indication there has been significant improvement withthese indicators (table 1). These along with extra efforts by pharmacy staff to focusprescribers on the quality of antibiotic prescribing have been successful in improving the useof antibiotics <strong>and</strong> reducing unneccessary prescriptions.The point prevalence audit for 2011 was awarded a 2 nd prize in the annual clinical auditcompetition.A trust-wide gentamicin prescribing, administration <strong>and</strong> therapeutic monitoring was carriedout in August 2011 <strong>and</strong> was awarded the first prize for the Tony Fuller Award in patientsafety.A poster on quality improvement programme to improve antimicrobial stewardship <strong>and</strong>patient safety at BHRH was presented at the Research <strong>and</strong> Development Annual conferencein November 2011Our work has shown that proactively developing an Antimicrobial stewardship programmehas improved documentation of antimicrobial prescribing as per the management code. It hasalso improved engagement of prescribers on antibiotic issues <strong>and</strong> raised the profile ofprudent antibiotic prescribing within the <strong>Trust</strong>. There has also been a decrease in Clostridiumdifficile cases within the <strong>Trust</strong>. The antibiotic stewardship programme will be continued ondeveloping guidelines with more emphasis on education <strong>and</strong> training <strong>and</strong> awareness <strong>and</strong>compliance to guidelines will continued to be audited.8.0 ACTION PLAN FOR <strong>2012</strong>/2013Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM25
The action plans identified in 2011/<strong>2012</strong> report were all met. The plans for <strong>2012</strong>/2013 are asfollows:8.1. Auditsa) 3 rd Point prevalence Auditb) Monthly audit of the management code in different specialist area <strong>and</strong> report to therelevant clinical directorate meetings- May <strong>2012</strong>c) <strong>Trust</strong>-wide antibiotic prophylaxis audit in surgery April <strong>2012</strong>d) Audit the appropriateness of use of antibiotics in respiratory infectionse) Audit the use of restricted antibiotics8.2. Education <strong>and</strong> traininga) Convert the current antimicrobial stewardship competency package to an E-Learningmoduleb) Continue Antimicrobial Stewardship training for doctors, nurses <strong>and</strong> pharmacists8.3 GuidelinesUpdate/review the following guidelines:a) Malariab) Infective Endocarditisc) Sexually Transmitted Diseased) Urinary Tract Infectionse) Clostridium difficilef) Neutropenic sepsisg) Antibiotic prophylaxis for surgeryh) Tuberculosisi) Eye <strong>and</strong> Dental Infectionsj) Osteomyelitis <strong>and</strong> septic arthritisk) Central Nervous infectionsl) Opportunistic infections associated with HIVI8.4) Paediatric Antimicrobial Guidelinesa) Set up a working group to develop the first edition of paediatric antimicrobial guidelinesb) The guidelines identified for paediatrics are:1) pneumonia (community acquired <strong>and</strong> hospital acquired), 2) UTI (Nice guideline) 3)Meningitis (NICE guideline) 4) Soft tissue infection 5) orbital cellulitis 6) Osteomyelitis7) Eczema herpeticum 8) peritonitis 9) suspected sepsis (< 3 months <strong>and</strong> >3 months),10) TB8.5 Miscellaneousa) Design <strong>and</strong> distribute penicillin allergy posters to all wardsb) Distribute pocket size antimicrobial guidelines to all new doctors in August <strong>2012</strong>9.0 CONCLUSIONSMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM26
It has been another challenging year for the <strong>Trust</strong>, which missed out on achieving the MRSAtarget but did achieve the Clostridium difficile target. The quality of care programme hasbeen successful in engaging clinical staff <strong>and</strong> raising the expectations <strong>and</strong> st<strong>and</strong>ards ininfection prevention <strong>and</strong> control practices. Overall it was a successful year except fornorovirus which as previously mentioned was present for a long period of time this year <strong>and</strong>had a significant effect on the <strong>Trust</strong>s activity due to closed beds. A peer review of thenorovirus management at BHRUT by an external Microbiologist/ Director of InfectionPrevention & Control has been requested <strong>and</strong> took place in May <strong>2012</strong>.The priorities for <strong>2012</strong>-2013 are to reduce the number of MRSA bacteraemias <strong>and</strong> C.diffs, toprogress with the annual plan, ensuring a more robust process for root cause analysistraining <strong>and</strong> the implementation of the Aseptic No Touch Technique (ANTT) programme.10. 0 REFERENCESo Winning ways (DH 2003),o Towards Cleaner Hospitals <strong>and</strong> lower rates of infection (DH 2004)o A Matron’s Charter: an action plan for cleaner hospitals (DH 2004),o Revised guidance on contracting for cleaning (DH 2004),o Saving Lives: A delivery program to reduce healthcare associated infection (HCAI)including MRSA (DH 2005).o Going further faster: implementing the Saving Lives delivery program (DH 2006)o The Health <strong>and</strong> Social Care Act 2008 (2010 ) Code of Practice for the Prevention <strong>and</strong>Control of Health Care Associated Infections (DH 2006)o The National Specifications for Cleanliness in the NHS: a framework for setting <strong>and</strong>measuring performance outcomes. (NPSA 2007)o Essential steps to safe clean care (DH 2007)o Clean, safe care: reducing infections <strong>and</strong> saving lives (DH 2008)o <strong>Board</strong> to ward how to embed a culture of HCAI prevention in acute trusts (DH 2008)o Clostridium difficile infection: How to deal with the problem (HPA& DH 2009)**The front page picture was taken during a h<strong>and</strong> hygiene awareness day whenvisitors joined in with the ‘glo germ’ demonstration of h<strong>and</strong> hygiene.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM27
Appendix 1CLINICAL GOVERNANCE REPORTING – JUNE 2011TRUST BOARDQuality <strong>and</strong> Safety CommitteeAudit CommitteePatient Experience CommitteeStatutory Safety CommitteeSafeguarding Children CommitteeSafeguarding Adults CommitteeClinical Risk Management CommitteeEvidence Based Practice CommitteeDrugs <strong>and</strong> Therapeutic CommitteeInfection Control CommitteeClinical Audit CommitteeTerms of Reference – risk topicscovered:• Mortality• Patient experience• External Clinical Accreditations• CQC Registration• Clinical Effectiveness <strong>and</strong>outcomes• Quality Account• Complaints• Incidents <strong>and</strong> Serious Incidents• Closed claims review• Key <strong>Trust</strong> Objectives• Risks to Reputation• Service Changes• Horizon scanningBAF & Risk RegisterCQC RegistrationResearch <strong>and</strong> DevelopmentNursing & Midwifery <strong>Board</strong>Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM28
Appendix 2Infection Prevention & Control Staff ChartDeborah WheelerDirector of Infection Prevention & Control& Director of NursingLesley MarshAssociate Director of NursingDr Lindsey BainInfection Control DoctorSheila O’MahonyMatron, Infection Prevention & ControlKate MartinSenior Infection Control NurseCorinne Cameron-WatsonSenior Infection Control NursesMercia WilliamsIC Practice FacilitatorTracey MortonInfection Control NurseLynne SmithAdministrative Co-ordinatorLucy EllisInfection Control NurseSheree BlackAdministrative Co-ordinatorMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM29
Appendix 3Annual <strong>Trust</strong> Action Plan to Prevent <strong>and</strong> Reduce Health Care AcquiredInfections 2011-<strong>2012</strong>Updated March <strong>2012</strong> Sheila O'Mahony Matron IPCTKey:Appendix 3W = Not yet startedG = CompleteA = In progress, on trackR = Overdue*Leads are responsible for action <strong>and</strong> supported by the infection prevention & control team asrequiredAim Actions Required Lead ReviewDateRAGrating1. Reduction in Maintain compliancenumber of MRSA with Intravenous <strong>and</strong>Bacteraemias <strong>and</strong> central venous carestaying within target bundlesof 8 bacteraemiasRCA investigation ofeach MRSAbacteraemiaAgreed target of 8bacteraemias for wholeyear 1.4.11 - 31.3.12Audit through qualityof care audits.Monitor eachbacteraemiaundertake RCA <strong>and</strong>report to ICC.Improvementsidentified from RCAsto be taken forward<strong>and</strong> monitored viaaction plansRCA investigationtool <strong>and</strong> policy is to beupdated <strong>and</strong> adaptedto ensure it is robustMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM30Progress at March 15 th <strong>2012</strong>DIPC/IPCT/DND's RED Target to date is 10 which is 2above trajectoryICDDND to designateleadMarch31 st<strong>2012</strong>March31 st<strong>2012</strong>AMBERAMBER5 RCA’s have been signed off <strong>and</strong>action plans presented to ICCDates set for sign of remainingRCA’s by 31 st March <strong>2012</strong>RCA tool has been adapted <strong>and</strong>used successfully on 4/5 RCA’sUpdated policy remains
2. To monitorincidence <strong>and</strong> reducenumber of MeticillinSensitiveStaphylococcusAureusNo target has been setfor MSSA65 HCAI were reportedin 2010 -2011<strong>and</strong> 72CAI3. To monitor <strong>and</strong>reduce the number ofE.coli bacteraemia<strong>and</strong> to be approvedat ICCAll RCA's to be signedoff by DIPC <strong>and</strong> CEO<strong>and</strong> added tosummary action plan<strong>and</strong> presented to ICCMaintain compliancewith care bundlesAudit through qualityof care auditsSet local trust targetto reduce currentbacteraemia figureMonitor each infection<strong>and</strong> complete RCAImprovementsidentified from RCAsto be takenforward <strong>and</strong>monitored via actionplansSummary action planto be collated <strong>and</strong>presentedat ICC <strong>and</strong> signed offby DIPC <strong>and</strong> CEOAll E coli bacteraemiato be manuallyrecorded on MESSHealth ProtectionAgency data base<strong>and</strong> reported throughICCIPCTIPCT/MatronsDIPC/CEOInfection ControlDoctorMarch31 st<strong>2012</strong>March31st<strong>2012</strong>March31 st<strong>2012</strong>March31 st<strong>2012</strong>AMBERGREENoutst<strong>and</strong>ing to be carried forwardto annual plan for <strong>2012</strong>-20135 RCA’s awaiting sign off beforeMarch 31 st <strong>2012</strong>Local targets to be set afterbenchmark data completed for2010-2011. NO targets set by DHfor <strong>2012</strong>-2013MSSA RCA's beingundertaken since 1st April 20112 HAI - 2 CAI April 20112 HAI – 5 CAI May 20115 HAI – 7 CAI June 20118 HAI - 7 CAI <strong>July</strong> 20113 HAI – 7 CAI August 20113 HAI - 5 CAI September 20113 HAI – 6 CAI October 20113 HAI- 8 CAI November 20111 HAI - 6 CAI December 20112 HCAI 9 CAI January <strong>2012</strong>2 HCAI 8 CAI February <strong>2012</strong>Total HA1 to end of February <strong>2012</strong>= 31GREEN Reported from June 1 st 20117 HAI - 15 CAI June 201110 HAI - 42 CAI <strong>July</strong> 20115 HAI - 28 CAI August 20118 HAI - 29CAI September 201111 HAI – 25 CAI October 20116 HAI – 20 CAI November 201110 HAI – 31 CAI December 201111 HCAI 28 CAI January <strong>2012</strong>Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM31
No target has been setfor E coli's - no dataavailable for 2010-2011as not collected byPathology4. H<strong>and</strong> HygieneAll staff working inclinical areas to meet aminimum of 95%compliance againstst<strong>and</strong>ardSet local trust targetto reduce currentbacteraemia figureDeliver h<strong>and</strong> hygienetraining for all staff onan annual basis asper separate h<strong>and</strong>hygiene training plan.Carry out ongoing 6weekly audits tomonitor compliance.Feedback <strong>and</strong> reporton compliance byward <strong>and</strong> specialityIPCTDND's/ Matrons /Infection ControlTeamMarch31st<strong>2012</strong>March31 st<strong>2012</strong>GREENGREEN9 HCAI 20 CAI February <strong>2012</strong>Total HAI to date = 77Local targets to be set afterbenchmarkdata completed for 2010-2011.Training sessions rolled out trustwide.Monthly audits undertakenby senior nursing team as part ofVisible Leadership Initiative.Results of audits shared atexecutive <strong>and</strong> local level, <strong>and</strong>reported to ICC Performance asappropriate.H<strong>and</strong> Hygiene awareness dayheld on January 24 th both sites5. Adherence to Saving Lives High Impact Interventions5.1 Central VenousLine Management HII1All CVC lines to beinserted <strong>and</strong> managedin accordance withSaving Lives CareBundle Guidance5.2 Care ofIntravenous Lines HII2All peripheral lines to beinserted <strong>and</strong> managedin accordance withCarry out weeklyaudits to monitorcompliance with allrelevant Saving LivesCare Bundles.Feedback findings toclinical care /wardteams. Report to ICCtwice annually as peragreed timetable.Report to ICC twiceannually as peragreed timetable to beagreed with DND's aspart of quality careDND's for allSaving Livesitems. ITU clinicallead Matrons,ward sistersDND'sMarch31 st<strong>2012</strong>March31 st<strong>2012</strong>AMBERAMBERCentral line policy updateoutst<strong>and</strong>ing plan to be discussedwith infection control lead whennominated by clinical directorMore work required on insertion ofperipheral lines plan to bediscussed with infection controllead when nominated by clinicaldirectorMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM32
Saving Lives Care programmeBundle Guidance Ward managers <strong>and</strong>senior consultants toaccount for noncompliancePerformancemanagement ofpersistently noncompliantstaff5.3 Prevention of Report to ICC twiceSurgical Siteannually as perInfections HII4agreed timetableAll surgical sites to becared for using aseptictechnique in accordancewith Saving Lives CareBundle Guidance<strong>Trust</strong> to participate inthe Health ProtectionAgency's Surgical SiteInfection SurveillanceScheme(SISS) currentlyreporting fractured neckof femursAll ventilated <strong>and</strong>tracheostomy patients tobe managed inaccordance with theSaving Lives CareBundle GuidanceNeed more robustreporting withclinician’sengagement. Need toagree other modulesof SSISNo progress with thisHII - roll over to <strong>2012</strong>-2013 planDND's GREEN Ward level audits continue to becarried out as part of Quality CareProgrammeSurgical DNDSurgical DNDITU Clinical Lead/Critical CareMatronsMarch31 st<strong>2012</strong>March31 st<strong>2012</strong>March31 st<strong>2012</strong>AMBERAMBERAMBERNo report/action to date Plan forfuture SSIS reporting to bediscussed with infection controllead when nominated by clinicaldirectorTo be carried forward to next yearsaction plan5.5 Urinary CatheterCare HII6 &Report to CQUINquarterly <strong>and</strong> at ICCICD/IPCTMarch GREEN April 2011 HAI =131 st May 2011 HAI =2Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM33
Agreed target of 38urinary catheterassociated bacteraemiafor whole year 1.4.11 -31.3.12meetings <strong>2012</strong> June 2011 HAI = 0<strong>July</strong> 2011 HAI = 4August 2011 HAI = 3September 2011 HAI = 2October 2011 HAI = 9November 2011 HAI = 6December 2011 HAI = 4January <strong>2012</strong> HAI = 3Total to February <strong>2012</strong>= 345.6 Clostridiumdifficile ManagementHII7To meet annual target of81 cases of C.diffinfectionsPrescribing practice tomeet a minimum of 90%compliance with policy.Prevent C.diff spread byadherence to carebundle guidance at alltimesAgreed target of 81infections for wholeyear 1.4.11 - 31.3.12.Monitor eachinfection, complete anexception report <strong>and</strong>undertake RCA ifdeath occurred <strong>and</strong> isstated on part 1a ofdeath certificate <strong>and</strong>report to ICC.Improvementsidentified from RCAsto be taken forward<strong>and</strong> monitored viaaction plansCarry out ongoing 6monthly audits tomonitor compliancewith Policy. WardPharmacists to check<strong>and</strong> challengeprescribing practiceDND's ICDMarch31 st<strong>2012</strong>GREENApril 2011 HAI = 6 .Two cases oneHarvest B underwent RCAMay 2011 HAI = 5June 2011 HAI = 3<strong>July</strong> 2011 HAI = 2August 2011 HAI = 5September 2011 HAI = 5October 2011 HAI = 5November 2011 = HAI =3December 2011= HAI 2January <strong>2012</strong> = 2February <strong>2012</strong> = 1Total to February = 39Await report date6. Screening (Saving Monitor <strong>Trust</strong> ICD/IPCT GREEN IPCT provide positive results toMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM34
Lives - A strategy forNHS <strong>Trust</strong>s: asummary of bestpractice)Screening Protocol toinclude all patientsEnsure positiveresults arecommunicated <strong>and</strong>acted uponwardsMonthly reports sent to divisionsfor action re complianceEnsure all patients arescreened for MRSA7. Death associatedwith HCAI'sTo monitor screeningrates with feedback torelevant areaAll patient deathsassociated withHCAI's should bechecked to ensurethat the HCAI isaccurately recordedas a cause of death orcontributor factorUndertake review ofjunior doctors trainingfor death certificationIPCTIPCT / MedicalDirectorMedical DirectorMarch31 st<strong>2012</strong>March31 st<strong>2012</strong>AMBERAMBERAMBERInformation departmentdeveloping data warehouseinformation reports will begenerated from this system whenup <strong>and</strong> running.Awaiting date of meeting.If dealt with by medical educationremove from annual plan8. Antibiotic actionplan 2011-<strong>2012</strong> Seeseparate planAnti MicrobialManagement Codeapproved at ICC <strong>and</strong>implemented May2011 to be auditedweek commencing25th <strong>July</strong> <strong>and</strong> resultsto Sept ICCManisha Madhani/ Dr Diane OshiruMarch31 st<strong>2012</strong>GREEN9. Environmental issues supporting h<strong>and</strong> hygiene <strong>and</strong> management of wards closeddue to outbreaks of infectionAudit completedReported at Nov ICCMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM35
Review all signageFloor signsTalking KonesExternal BannerInstallation of Saniposth<strong>and</strong> hygiene stations(both sites)Review ward postersrolling over from cleanyour h<strong>and</strong>s campaignto the five moment’scampaign. Replaceold postersAssess current stateof floor signs <strong>and</strong>liaise with Sodexo toremove tatty stainedsigns. Reviewpossibility <strong>and</strong> costsof replacement ofsigns.Establish whichKones are stillfunctionalCheck condition ofexternal clean yourh<strong>and</strong>s banner.Remove if tatty orsoiled beyondreasonable repair.Review costs ofreplacement if bannernot suitable.IPCTIPCTMarch31 st<strong>2012</strong>March31 st<strong>2012</strong>IPCT March31 st<strong>2012</strong>IPCTIPCT/<strong>Trust</strong>Contract ManagerSoft FM Estates &FacilitiesMarch31 st<strong>2012</strong>January<strong>2012</strong>GREENGREENAMBERGREENAMBERWard entrance posters changed tofive momentsSome floor signage removedreview <strong>2012</strong>4 Kones in need of repair/replacement no action to dateIPCT to decide if cost effective tohave repairedRemains in good conditionCompany who provide sanipostceased trading remove from planMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM36
Appendix 4Key:W = Not yet startedG = CompleteA = In progress, on trackR = OverdueAnnual <strong>Trust</strong> Plan to Prevent <strong>and</strong> Reduce Health Care Acquired InfectionsApril <strong>2012</strong> - March 2013Updated 01/05/<strong>2012</strong>*Leads are responsible for action <strong>and</strong> supported by the infection prevention & control team as requiredAim Actions Required Lead Review Date RAG rating Progress at 1.5.121. Reduction in number of MRSABacteraemias <strong>and</strong> stay within targetof 7 bacteraemiasRCA investigation of each MRSAbacteraemiaMaintain compliance withIntravenous <strong>and</strong> central venouscare bundlesApproved business case for theintroduction of Biopatch dressingto be used post insertion ofperipheral, central lines to aid inthe reduction of bacteraemiasAudit through quality of careaudits – appendix oneMonitor each bacteraemiaundertake RCA <strong>and</strong> report to ICC.Report using SI STEIS process ifdeath occurred <strong>and</strong> is stated onpart 1a of death certificateDIPC/IPCT/ AllBusiness UnitClinical DirectorsDr OdejinmiAll Business UnitClinical DirectorsICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCREDAMBER1 MRSA bacteraemia12/04/<strong>2012</strong>Round table scheduled for2.5.12All RCA's to be signed off byDIPC <strong>and</strong> CEODIPC4 weeks postRCAMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM37
All RCA’s to be added tosummary action plan <strong>and</strong>presented to ICCReduction in trends <strong>and</strong> demonstratelearning across the organisation followingcompletion of each RCA2. To monitor incidence <strong>and</strong> reducenumber of Meticillin SensitiveStaphylococcus AureusBusiness units to demonstrateimplementation of findingsthrough action plan at ICCQuality of care auditsdemonstrate a consistent upwardtrend across <strong>Trust</strong> in relation toinfection control.Maintain compliance with carebundlesAudit through quality of careaudits – appendix oneAll Business UnitClinical DirectorsIPCT/MatronsICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCMarch 31st2013REDCatheter audit results in April<strong>2012</strong> = 77.4%AMBER 3 hospital apportioned – 1RCA analysis completed. 2being completedLocal targets to be set after benchmarkdata completed for <strong>2012</strong>-2013.Set local trust target to reducecurrent bacteraemia figureMonitor each infection <strong>and</strong>complete simple RCA analysisImprovements identified fromRCAs to be taken forward <strong>and</strong>monitored via action plans3. To monitor <strong>and</strong> reduce the numberof E.coli bacteraemiaLocal targets to be set after benchmarkdata completed for 2011-<strong>2012</strong>Summary action plan to becollated <strong>and</strong> presentedat ICC <strong>and</strong> signed off by DIPCAll E coli bacteraemia to bemanually recorded on MESSHealth Protection Agency database <strong>and</strong> reported through ICCSet local trust target to reducecurrent bacteraemia figureInfection ControlDoctorIPCTJanuary 2013March 31st2013AMBER12 hospital apportionedMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM38
4. H<strong>and</strong> HygieneDeliver h<strong>and</strong> hygiene training for allclinical staff on an annual basis (seeappendix 2).Support h<strong>and</strong> hygiene complianceTraining sessions rolled out trustwide.Through train the trainer<strong>and</strong> link nurse programsIPCT to record attendees onESR <strong>and</strong> follow-up nonattendance by notifying linemanager for actionH<strong>and</strong> Hygiene awareness daysplanned for 2013 May <strong>2012</strong>,October <strong>and</strong> February 2013IPCTTwice yearly toICC in Sept <strong>and</strong>MarchIPCT May 12October 12Feb 13AMBERAMBERImplement World HealthOrganisation (WHO) 5 MomentscampaignAll staff working in clinical areas to meeta minimum of 95% compliance againstst<strong>and</strong>ardReview poster placements <strong>and</strong>update where necessaryAudit h<strong>and</strong> hygiene quarterly aspart of the Quality of Careprogramme to monitorcomplianceADNQuarterly to ICCin <strong>July</strong> <strong>and</strong> JanAMBERFeedback <strong>and</strong> report oncompliance by ward <strong>and</strong>speciality to ICC.5. Adherence to Saving Lives High Impact Interventions5.1 AsepsisDeliver ANTT for all clinical staffAll staff undertaking clinical procedures as per separate ANTT projectmust use Aseptic Non Touch Technique plan through train the trainer <strong>and</strong>(ANTT) to reduce risk of crossrecord training on ESRcontaminationIPCT/train thetrainerICC31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBERANTT project plan presentedto ICC on 2.5.12 <strong>and</strong>approved. Roll out in August<strong>2012</strong> following training in<strong>July</strong>.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM39
5.2 Central Venous Line ManagementHII1Policy on CVC insertion <strong>and</strong>management to be writtenConsultant lead foranaesthetics1.7.12All CVC lines to be inserted <strong>and</strong>managed in accordance with SavingLives Care Bundle GuidanceImplementation of the approvedpolicyAgree tool to be used to audit theeffect of the policy5.3 Care of Intravenous Lines HII2All peripheral lines to be inserted <strong>and</strong>managed in accordance with SavingLives Care Bundle GuidanceStaff follow policy for insertion <strong>and</strong>management of peripheral lines.The process of insertion <strong>and</strong>care of peripheral lines is auditedquarterly using quality of careaudit toolFeedback <strong>and</strong> report oncompliance by ward <strong>and</strong>speciality to ICC.PCT / MatronsADNICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBER5.4 Prevention of Surgical SiteInfections HII4All surgical sites to be cared for usingANTT in accordance with Saving LivesCare Bundle Guidance.1. fractured neck of femurs –ongoing2. commence surveillance for postoperative surgical wounds in Q23. commence surveillance for postoperative caesarean wounds inQ34. commence surveillance for longbone surgery in Q4Results are discussed withinbusiness units <strong>and</strong> learning isshare across the <strong>Trust</strong><strong>Trust</strong> to participate in the HealthProtection Agency's Surgical SiteInfection Surveillance Scheme(SISS) currently reportingfractured neck of femursImplement an additional siteeach quarter.Use Health Protection AgencySurgical Site Surveillance toolReport compliance <strong>and</strong> findingsat business unit meetings <strong>and</strong>ICCIdentify actions required <strong>and</strong>report on completion onceMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM40All ClinicalDirectors MatronsCD specialistsurgeryCD general surgeryCD womenSee attachedaudit plan12/06/<strong>2012</strong>02/10/<strong>2012</strong>Feb 2013 TBCAMBER
5.5 Ventilation <strong>and</strong> TracheostomiesHII5All ventilated <strong>and</strong> tracheostomy patientsto be managed in accordance with theSaving Lives Care Bundle Guidance5.6 Urinary Catheter Care HII6Target for 2011 – 12 was 38 <strong>and</strong> 44occurred.This is now incorporated in the safetythermometer work whereby 95% ofpatients receive harm free care by Dec12 relating to pressure ulcers grade 3+4,falls, CA-UTI <strong>and</strong> VTE.implemented.Collect data in accordance withnational reporting guidance fromIntensive Care National AuditResearch centre (ICNARC)Present findings every quarter toICC with associated actionsrequired <strong>and</strong> progress againsttarget.Complete safety thermometerevery month for al patients in thetrust.Rapid review of all CAUTIbacteraemia within 1 week ofnotification to IPCT. Developaction plan <strong>and</strong> implement asrequired.Feedback findings to relevantstaff.Clinical Director -AnaestheticsQuarterly to ICC31/07/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCICD/IPCT 01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBERAMBERCurrent position in April 12 is87%Report to CQUIN quarterly <strong>and</strong>at ICC meetings5.7 Clostridium difficile ManagementHII7To meet annual target of 59 cases of C.difficile infections 1.4.12 - 31.3.13Complete quality of care urinarycatheter & continence auditsevery quarterComplete an exception reportwith ward manager followingeach case of C. difficile within 1working day of infection controlbeing notified to monitorcompliance with C.difficile policy.ICT provide immediate feedbackof results to ward followed byIPCT/wardmanagersICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBER5 hospital apportionedMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM41
written report including actionsrequired (if any) sent to businessunits <strong>and</strong> DIPCReport compliance <strong>and</strong> findingsat business unit meetings <strong>and</strong>ICCIdentify actions required <strong>and</strong>report on completion onceimplemented.Wardmanagers/MatronsMatronsUndertake Root Cause Analysisif death occurred <strong>and</strong> is stated onpart 1a of death certificate or ifmore than 2 C.difficile infectionsin a month in one ward <strong>and</strong>report to ICC.MatronsPrescribing practice to meet a minimumof 95% compliance with antibiotic policy.Improvements identified fromRCAs to be taken forward <strong>and</strong>monitored via action plans <strong>and</strong>reported through ICCUndertake annual audit tomonitor compliance withantibiotic prescribing Policy.AntibioticPharmacistOct <strong>2012</strong> AMBERWard Pharmacists to check <strong>and</strong>challenge prescribing practicewhen they review a drug chart.Report findings from the annualaudit to business units <strong>and</strong>infection control committee toagree actions requiredShare learning regarding practicechanges requiredMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM42
6. Screening for MRSA (Saving Lives -A strategy for NHS <strong>Trust</strong>s: a summaryof best practice)Ensure 100% of inpatients are screenedfor MRSAAll patients who fit the criteria arescreened for MRSA within 24hours of admission.Monitor <strong>Trust</strong> Screening Protocolto include all patients using datawarehouse information.ICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBERMonthly compliance reports aresent to the business units. Eachunit not achieving 100% need toreview <strong>and</strong> action appropriately.ICC review <strong>Trust</strong> compliance.Positive results arecommunicated by IPCT to therelevant clinical area within 1working day of notificationIPCT advise treatment plan <strong>and</strong>review accordingly7. Implement recommendations fromHCAI Peer Review January <strong>2012</strong>The recommendations were:• <strong>Board</strong> to ward accountability• Staff having the necessarycompetence to assure consistentapplication of evidence basedpractice when inserting lines <strong>and</strong>catheters <strong>and</strong> following agreedguidelines <strong>and</strong> protocols consistently(see ANTT in section 5.1)• Assuring prudent antimicrobialIPCT monitor compliance ofpatients positive with MRSA <strong>and</strong>report trends to ICCAll clinical business units tonominate a consultant lead forInfection Prevention & Control tochampion High ImpactInterventions <strong>and</strong> ensure ward toboard responsibility <strong>and</strong>accountabilityClinical Directors to ensure IP&Cis included in PDP/AppraisalsIPC Consultant Leads <strong>and</strong>matrons to take forward <strong>and</strong>Clinical DirectorsClinical DirectorsIPC ConsultantLeads01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBERAMD for has sent a letter toconsultants calling forchampions.Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM43
practices are in place (see section 8)• Governance <strong>and</strong> assuranceprocesses being robust enough toinform the <strong>Board</strong> of progress <strong>and</strong>alert the <strong>Board</strong> to any further risksreport progress to own businessunit <strong>and</strong> ICCChange working practices withinIPCT to promote proactiveworkingQuality of Care dashboardsubmitted monthly to BusinessunitsIPCTADN8. Antibiotic action plan <strong>2012</strong>-2013 Adhere to antibiotic plan -summary in appendix 39. Isolating patients with health careassociated infection -NorovirusReduce the risk of transmission ofnorovirus during the anticipated seasonalsurge from September onwardsDeliver training sessions to keyclinical staff in non outbreakmonths in preparation foroutbreak management (seeattached education plan).IPCT attendance at morning bedmeetings to give situation reportPromote the safer clinical care ofan individual or group of patientswith norovirus by isolation or cohortcontrol.Hold monthly outbreak reviewmeetings with managers fromaffected wards, bed teams,domestic services, HPA. <strong>and</strong>commissioners using the HPATop Ten Tips for norovirusmanagement <strong>and</strong> summary ofexception report findingsAudit outbreak control on wardre-opening using exceptionAntibioticpharmacistIPCTOctober <strong>2012</strong> AMBERICC01/05/<strong>2012</strong>12/06/<strong>2012</strong>31/07/<strong>2012</strong>02/10/<strong>2012</strong>04/12/<strong>2012</strong>Feb 2013 TBCAMBERMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM44
eports <strong>and</strong> feed back findings toward staff <strong>and</strong> summary to ICCAction recommendations fromexternal review to occur in May<strong>2012</strong>.10. Policies relating to Infectioncontrol are evidence based <strong>and</strong> valid.Policies are reviewed by IPCTevery quarter.Policies due for review this yearare:• Meningitis• H<strong>and</strong> Hygiene• Tuberculosis staffscreening• C Difficile• RCA policyIPCT June 12Sept 12Dec 12Mar 13AMBERANTT, h<strong>and</strong> hygiene, TBstaff screening <strong>and</strong> C.diff aredue to be present at ICC inJune 12RCA policy away dayscheduled for 16.5.12New policies to be written• ANTTSheila O'Mahony Matron IPCTPlease note:Recommendations from the Tuberculosis Look back exercise will be added once the look back process is completed - anticipated completion date is<strong>July</strong> <strong>2012</strong>.KEY:DIPC – Director of Infection Prevention & ControlICD- Infection Control DoctorIPCT – Infection prevention & Control TeamHAI – Health Care Acquired InfectionsCAI – Community Acquired InfectionsAND – assistant Director of NursingAMD – associate medical directorMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM45
Title:Infection Control Annual Programme of Audits incorporating Criterion 8 of the Health <strong>and</strong> Social Care Act & HighImpact Interventions (HII’s) for <strong>2012</strong>– 2013Purpose: To improve Infection Prevention & Control practice <strong>and</strong> compliance at BHRUT targeting all clinical practitioners <strong>and</strong>setting st<strong>and</strong>ards for those practitioners to teach non-clinical staffAim: To audit all clinical areas thereby ensuring compliance with Infection Prevention & Control practice.Objective: To achieve compliance rates of greater than 95% in all clinical areas.Plan Owner:Matron for the Infection Prevention & Control Team (IPCT)Project manager: Infection Prevention & Control FacilitatorMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM46
Infection Control Annual Programme of Audits incorporating Criterion 8 of the Health <strong>and</strong> Social Care Act & High Impact Interventions (HII’s) for<strong>2012</strong>/2013Topic Saving Lives Audit Timescale LeadpersonTo ensure all staff comply with proper h<strong>and</strong> hygiene practice to reduce the April <strong>2012</strong>IPCTrisk of cross infection <strong>and</strong> to enable the <strong>Trust</strong> to adhere to a compliance Nov <strong>2012</strong>rate of 95% <strong>and</strong> above.H<strong>and</strong> Hygiene using the InfectionPrevention Society (IPS) ToolEnvironmental audit policy usingthe IPS toolPPE audit using the IPS toolIsolation audit using the IPS toolTo ensure st<strong>and</strong>ards of cleanliness <strong>and</strong> hygiene are complied with tomaintain a safe environment for patients/ staff/ visitors in prevention ofinfection.To ensure clinical practices are based on best practice <strong>and</strong> reflect infectioncontrol principles to reduce the risk of cross infection to patients’ whilstproviding appropriate protection to staff.To ensure compliance with the appropriate isolation precautions to promotesafer clinical care of an individual with an infectionMay <strong>2012</strong>March 2013 <strong>and</strong> followingany outbreak of infectionJune <strong>2012</strong>February 2013 <strong>and</strong>following any outbreak ofinfection<strong>July</strong> <strong>2012</strong>March 2013 <strong>and</strong> followingany outbreak of infectionIPCTIPCTIPCTHII7 Reduce the risk fromClostridium difficileScreening for meticillin – resistantStaphylococcus Aureus (MRSA)colonisationAudit compliance with the ‘Control of Clostridium difficile Policy &procedures’ through the use of exception reports following every case ofC.diffTo ensure compliance with the MRSA policy on Screening of ElectiveAdmissions <strong>and</strong> EmergenciesFeedback given at time ofaudit to wardmanagers/matrons withaction identified<strong>Trust</strong> results feedback toevery ICC<strong>Trust</strong> results feedback toevery ICCIPCTIPCT/ICDGeneralManagersQuality of Care Programme infection Control AuditMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM47
H<strong>and</strong> Hygiene (observationalTool)Continence including UrinarycathetersIntravenous CannulaePressure UlcersTo ensure all staff comply with proper h<strong>and</strong> hygiene practices <strong>and</strong> togive feedback on individual ward compliance ensuring rate the <strong>Trust</strong>to adhere to a compliance rate of 95% <strong>and</strong> above.To ensure staff comply with the policy on ‘Urethral Catheterisation inAdult Patients’To ensure all peripheral lines are inserted <strong>and</strong> managed inaccordance with the ANTT guidelines <strong>and</strong> ‘Policy for Reducing theRisk of Infections Associated with Intravascular Devices’To ensure the Skin bundle pathway are being followed <strong>and</strong> correctpressure grading <strong>and</strong> equipment are used.14 th May <strong>2012</strong>13 th August <strong>2012</strong>23 rd April <strong>2012</strong>23 rd <strong>July</strong> <strong>2012</strong>30 th April <strong>2012</strong>30 th <strong>July</strong> <strong>2012</strong>2 nd April <strong>2012</strong>2 nd <strong>July</strong> <strong>2012</strong>ADN/Matrons/IPCTADN/Matrons/IPCTADN/Matrons/IPCTADN/Matrons/TVNDepartmental Infection Control AuditsAntimicrobial prescribing To ensure staff comply with the <strong>Trust</strong> Antibiotic policies Proposed for October <strong>2012</strong> antibioticpharmacistManagement of the antimicrobialprescribing codeTo ensure staff comply with the code Annual antibioticpharmacistHII1 Central Line care bundle To ensure all CVC lines are inserted <strong>and</strong> managed in accordancewith the ANTT guidelines <strong>and</strong> the Policy for Reducing the Risk ofInfections Associated With Intravascular Devices.September / October AnaestheticleadHII5 Care bundle from ventilatedpatients (or tracheotomy whereappropriate)HII4 Care bundle to preventsurgical site infections (SSIS)To ensure staff compliance with the NICE guidelines <strong>and</strong> theventilator care bundle.The aim of SSIS is to enhance the quality of patient care byencouraging hospitals to use data obtained from surveillance tocompare their rates of SSI over time <strong>and</strong> against a benchmark rate,<strong>and</strong> to use this information to review <strong>and</strong> guide clinical practice.Company AuditsSeptember <strong>2012</strong>March 2013April - June12<strong>July</strong> - September12Oct - December 12Jan – March 13ITU MatronsOrthopaedictrauma CoordinatorCommodesTaking blood cultures (HII as bestpractice)HII2 Peripheral line as bestpractice(Product <strong>and</strong> usage)HII6 Urinary catheter audit(Products <strong>and</strong> usage)To ensure the commodes used are in a good state of repair <strong>and</strong> clean<strong>and</strong> to make recommendations as required.March 2013Verna careCompanyTo review the correct product usage <strong>and</strong> make recommendations as Nov <strong>2012</strong>Greiner /IPCTrequired.To ensure all peripheral lines are inserted <strong>and</strong> managed inOctober <strong>2012</strong>B Braun/IPCTaccordance with the ANTT guidelines <strong>and</strong> ‘Policy for Reducing theRisk of Infections Associated With Intravascular Devices’To review the product usage <strong>and</strong> make commendations as needed. <strong>July</strong> <strong>2012</strong> Bard/ IPCTMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM48
Safe H<strong>and</strong>ling <strong>and</strong> disposal ofsharpsH<strong>and</strong> Hygiene i.e. Spirigelplacement <strong>and</strong> usage AuditMattress AuditsPressure UlcersTo review the product usage, do spot training as required <strong>and</strong> tomake recommendations as needed.To ensure correct usage of the product <strong>and</strong> do spot training asneeded.To ensure that mattresses purchased are for the provision of safe <strong>and</strong>effective patient careTo ensure the Skin bundle pathways are being followed <strong>and</strong> correctpressure grading <strong>and</strong> equipment are used.19 th & 20 th April <strong>2012</strong> Daniels/ IPCTMarch 2013Ecolab/IPCTNovember/December <strong>2012</strong> NurseConsultantTVN/Hill-Rom &Huntleigh21 st May <strong>2012</strong> NurseConsultantTVN/ Hill-Rom& HuntleighKEY:IPCT - Infection Prevention & Control TeamICD - Infection Control DoctorADN - Assistant Director of NursingTVN – Tissue Viability NurseMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM49
Title Annual Infection Prevention <strong>and</strong> Control Education Programme for <strong>2012</strong> -2013Purpose:To ensure the education plan incorporates the NHSLA Risk Management St<strong>and</strong>ards, Criterion 8 of the Health <strong>and</strong>Social Care Act & High Impact Interventions (HII’s) <strong>and</strong> that it is based on the principles of <strong>and</strong>ragogics.Aim: To ensure all staff attend <strong>and</strong> are competent with infection prevention & control practices.Objective: To ensure all staff are able to correlate theory with practice enabling them to render safe patient carePlan Owner: Matron Infection Prevention & Control Team (IPCT)Project manager:Mercia Williams Infection Prevention & Control FacilitatorMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM50
Annual Infection Prevention <strong>and</strong> Control Education Programme for <strong>2012</strong>-2013Course Name Objectives Content TargetaudienceInfectionPrevention &ControlPassportPrinciples <strong>and</strong>Practices ofInfectionControlLondon SouthBank• Through 9 all daysessions with a capacityof 450 places for <strong>2012</strong>/13raise awareness withregard to prevention <strong>and</strong>control of HAI• To discuss the causesspread <strong>and</strong> treatment ofHospital AssociatedInfection (HAI)• To discuss the basicinfection prevention <strong>and</strong>control strategies to beimplemented in theclinical environment tominimise transmission ofinfection.• The <strong>Trust</strong> hascommissioned 12 placesfor BHRUT staff to givean overview of infectionprevention & controlpractices• St<strong>and</strong>ard InfectionControl Precautions(SICP)• Specimen Collection• Decontamination ofequipment• H<strong>and</strong> Hygiene• Safe H<strong>and</strong>ling <strong>and</strong>disposal of Sharps• Protocol for NSI• Infectious diseases e.g.TB• HAI’s• Clinical audit results• Introduction to Infectioncontrol• SICP• Food Safety• Specimen Collection• Care QualityMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM51AllHealthcareWorkersRGN’s <strong>and</strong>Degreepathway &MasterslevelstudentsAssessmentmethodFormalassessment:6 weeks postdate ofattending thestudy day.Tool used isInfectionControlPassportBookletAssignmentas per LSBUcurriculumStudy Dates Duration ProgressReport toICCSeptember<strong>2012</strong> <strong>and</strong>March 201317 th April 12 Full Day25 attendees22 nd May 1221 st June 1220 th Sept 1225 th Oct 1222 nd Nov 12Bi-annuallywith anexpectationof 6attendeesper course7 hours
University(LSBU)M<strong>and</strong>atoryTraining forSpecialist staffSocial WorkersIntegratedTherapiesRadiologyPharmacySiemens(Medicalequipmentservice staff)• To update staff oncurrent developments inInfection Prevention &Control practicesspecific to their workingenvironmentcommission• Root Cause Analysis(RCA) & SeriousIncidences• Audits• Environmental Hygiene<strong>and</strong> Safety• Legislation• SICP• Statistical analysis ofcurrent HAI’s within thetrust<strong>and</strong> othermultidisciplinary staffAll SocialworkersAll Physio’s&OccupationalTherapistsAllRadiographer<strong>and</strong> RadiologiAll pre <strong>and</strong>postregistrationPharmacystudentsFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightAnnually 2 hours (x 1session)2 hours (x 4sessions)1 hour (x 2sessions)1 hour asrequired1 hourInfectionPrevention &Control LinkPractitionersTrainingProgramme• To implement evidencebased practice which iscentral to clinicaleffectiveness• To improve quality ofcare• To improvecommunication with themulti-professional team(MPT).• St<strong>and</strong>ard infectioncontrol precautions;• Specimen collection.• Decontamination ofward equipment.• H<strong>and</strong> hygiene.• Safe h<strong>and</strong>ling <strong>and</strong>disposal of sharps.• Protocols for needlestick injuries.AllEngineersInfectionPrevention<strong>and</strong> ControlLinkPractitionersFormalassessment;1. Train thetrainerprogramme2. WardbasedAudits3. Case14 th Feb<strong>2012</strong>28 th May<strong>2012</strong>17 th <strong>July</strong><strong>2012</strong>13 th Nov<strong>2012</strong>Full dayMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM52
• To bridge the gapbetween theory <strong>and</strong>practice• To share effective <strong>and</strong>ineffective strategies withthe MPT• To share knowledge <strong>and</strong>expertise with themembers of the MPT• Infectious diseases i.e.TB.• Healthcare associatedinfections.• Clinical audits.• Link Practitionertraining• Train the trainerprojects i.e. passportassessments• Case presentationsstudypresentation4. AnnualconferencepresentationsOutbreakManagementPre <strong>and</strong> duringNorovirusseason• To update staff of theprinciples of outbreakmanagement• To discuss thelegislation <strong>and</strong> policiesrelating to outbreakmanagement.• To discuss theprinciples of outbreakmanagement includingthe lines ofcommunication to befollowed in the event ofan outbreak.• To discuss the timelines within which thedocument has to becompleted.• Discuss the documentsto be completedAll StaffQuestion <strong>and</strong>answersessionAugustthrough toMarch½ hrsession oneach shiftGeneralInduction• To ensure all staff areaware of <strong>and</strong> able todemonstrate proper h<strong>and</strong>hygiene technique <strong>and</strong>safe h<strong>and</strong>ling <strong>and</strong>disposal of sharpsincluding management of• H<strong>and</strong> Hygiene theory &practiceMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM53AllHealthcareWorkersFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightMonthly asper <strong>Trust</strong>inductionprogramme.½ hour
needle stick injuries.RegisteredNursesInductionProgramme• To ensure adherence toinfection control practicerelating to IV therapy isadhered to.• Legislation• Micro-organismsresponsible for IVdevice relatedinfections• Causes of IV devicerelated infections• Prevent IV devicerelated infection• VIP scoring• Complicationsassociated with IVdevices• H<strong>and</strong> hygieneRGN’sFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightMonthly asper trustinductionprogramme1 hourM<strong>and</strong>atoryTraining forRGN’s, HCWS,& ODP’s• To update staff oncurrent developments inInfection Prevention &Control practices• Legislation• SICP• Statistical analysis ofcurrent HAI’s within thetrustAllattendeesFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightTri-weekly asper trusteducationprogrammeMon &Fridays:50 minutesM<strong>and</strong>atoryTraining forSpecialistAreas;Midwives’ <strong>and</strong>Medical StaffNeonatal <strong>and</strong>PaediatricNurses• To update staff oncurrent developments inInfection Prevention &Control practices asapplied to Midwifery,Obstetrics <strong>and</strong> Gynae• Legislation• SICP• Statistical analysis ofcurrent HAI’s within thetrust as applied toMaternityMidwives,Gynaecologists, &ObstetriciansNeonatalNurses;NurseryNurses, &MaternityH<strong>and</strong> hygieneassessmentusing UV lightMonthly asper speciallyeducationprogrammeTuesdays1 hourTuesdays 1hourMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM54
M<strong>and</strong>atoryH<strong>and</strong> HygieneTraining forclinical <strong>and</strong>non clinicalstaffConsultantsM<strong>and</strong>atoryH<strong>and</strong> HygieneTrainingCannulation &VenepunctureTrainingHealth CareSupportWorker’sInductionProgramme• To demonstrate <strong>and</strong>discuss proper h<strong>and</strong>hygiene practice• To demonstrate <strong>and</strong>discuss proper h<strong>and</strong>hygiene practiceTo ensure best infectioncontrol practice relating to IVtherapy is adhered to.To discuss the generalprinciples of Infectionprevention <strong>and</strong> control• Legislation• Indication for h<strong>and</strong>washing (5 moments)• The correct steps tofollow when washingh<strong>and</strong>s• Areas frequentlymissed• Indications for h<strong>and</strong>washing (5 moments)• The correct steps tofollow when washingh<strong>and</strong>s• Areas frequentlymissed• Legislation• Principles of infectionprevention relating toCannula insertion <strong>and</strong>care• Audits• H<strong>and</strong> hygiene• Legislation• St<strong>and</strong>ard InfectionControl Precautions• Specimen Collection• Decontamination ofequipment• H<strong>and</strong> Hygiene• Safe H<strong>and</strong>ling <strong>and</strong>disposal of Sharps• Protocol for NSI• Infectious diseases e.g.CareAssistants.All clinical<strong>and</strong> nonclinical staffAllConsultantsRGN’sNewlyappointedHCSW’sFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightFormalassessmentmodule as pertrusteducationdepartmentFormal h<strong>and</strong>hygieneassessment:Simulationusing the UVlightWeekly asper trustm<strong>and</strong>atoryprogrammeBi-weekly asper trusteducationprogramme3 rd March 1227 th April 1215 th June 1213 th Aug 1228 th Aug 1212 th Oct 1210 th Dec 1230 th Dec 1214 th Dec 12Monthly asper trusteducationprogrammeWeds:½ hourMondays½ hour1 hour2 hoursMelis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM55
TBM Williams 1.5.12Melis<strong>and</strong>e/ Annual reports /DIPC Annual Report 2011-<strong>2012</strong> SMOM56
Approved at Quality & SafetyCommittee 12.06.12QUALITY & SAFETY COMMITTEEPart IMinutes of the meeting held on Tuesday 17 th April <strong>2012</strong> at 14.00 hrs in <strong>Board</strong> Rooms 1&2,<strong>Trust</strong> Headquarters, Queen’s Hospital, Romford.Present:Prof. Anthony Warrens, Non Executive Director (Joint Chair) (Chair)Averil Dongworth, Chief Executive (AD)Magda Smith, Associate Medical Director – Emergency Care, Medicine &Neurosciences (MS)Stephen Burgess, Medical Director (SB)Cathy Geddes, Chief Operating Officer (CG)Arshiya Khan, Associate Director – Women & Children <strong>and</strong> Support Services(AK)Portia Omo-Bare, Chief Pharmacist (POB)Pam Strange, Clinical Governance Director (PS)Imogen Shillito, Director of Communications (IS)Gary Etheridge, Deputy Director of Nursing (GE)Geraldine Soosay, Clinical Director – Pathology (GS)Michael White, Non Executive Director (MW)Elaine Clark, Patient Representative / Chair of IPEG (EC)Cris Robinson, Committee Coordinator (Minutes) (CR)Action32/<strong>2012</strong> ApologiesApologies were noted for Caroline Wright, Non Executive Director; JohnAlcolado, Associate Medical Director – Academia; Alison Crombie, Director ofEducation; Ian Grant, Associate Medical Director – Diagnostics & SpecialistMedicine; Tan V<strong>and</strong>al, Associate Medical Director – Surgery & Anaesthetics;Deborah Wheeler, Director of Nursing; Richard Howard, Associate MedicalDirector - Women’s & Children’s <strong>and</strong> Support Services; Jane Moore, ONEL.33/<strong>2012</strong> Minutes of the Meeting held on 14 th February <strong>2012</strong> (Part I)The minutes were agreed as a true record of the discussions with the followingcaveats:• 15/<strong>2012</strong> - The figures relating to the number of sickle cell patients tobe clarified as they appear very high.• 09/<strong>2012</strong> – The wording in the last sentence to be changed to show that<strong>Havering</strong> Chief Executive leads on safeguarding children acrossLondon, not <strong>Havering</strong>.IGCR1
34/<strong>2012</strong> Matters ArisingCriticism of the late arrival of agenda <strong>papers</strong> was made by MW, with othermembers agreeing that it hindered a thorough review of the large number ofdocuments for discussion. AD advised this was also a problem with other<strong>Trust</strong> committees which required a rigorous approach to ensuring <strong>papers</strong> weresubmitted on time to the committee administrators. It was agreed that in futurereports must be submitted no later than 1 week in advance of the meeting orthe <strong>papers</strong> would be produced without them. The Committee’s terms ofreference would be checked to ensure this was included.Action LogAll actions were reported to be either in h<strong>and</strong> or completed with the followingexceptions that require further follow up:04/<strong>2012</strong> – The importance of narrative for the Quality Dashboard to beemphasised to the Clinical Directors.06/<strong>2012</strong> – The roll out plans for increasing ward round Consultant cover todeliver improved senior medical review of patients was not an agenda item<strong>and</strong> there was no one present to talk to the item. A written response includingan early unpopulated action plan was noted, but this was felt to be insufficientto satisfy the Committee <strong>and</strong> a detailed report should be presented to the nextmeeting; this to be requested from the Associate Medical Director.16/<strong>2012</strong> – In the absence of the Director of Nursing it was unclear whether theproposed separate meeting to discuss Health Care Assistant development,planned to address the findings from the <strong>Havering</strong> Enter & View visit had takenplace. An update on this was requested for the next meeting.18/<strong>2012</strong> – SB advised that this outst<strong>and</strong>ing item remained unresolved as a fullconversation had not been held to discuss the contractual arrangementsbetween the <strong>Trust</strong> <strong>and</strong> the ISTC. AD explained that a meeting has beenrequested but this has not yet taken place.Rolling ProgrammeThe rolling programme was noted, <strong>and</strong> no items were added by members.However, an initial meeting has taken placed between AD, SB <strong>and</strong> PS toreview the future direction for the Quality & Safety Committee <strong>and</strong>consideration is being given to using the Rolling Programme to capture thework of the Clinical Directors <strong>and</strong> other committees.STRATEGY35/<strong>2012</strong> Divisional Quality DashboardSB advised that the report included two sections: one the quality dashboard<strong>and</strong> the other the East Midl<strong>and</strong>s Observatory report which came with a healthwarning due to the majority of the data being somewhat out of date. Heexplained that the SHMI data in the Observatory report has been supersededwith the latest <strong>Trust</strong> position being 94.1. Furthermore the <strong>Trust</strong> was not anoutlier for pneumonia as shown by the Observatory but was in fact performingon average with other <strong>Trust</strong>s. PS assured CG that a full mortality report isbrought to every other Committee that provides clear mortality data based onDr Foster <strong>and</strong> the dashboard contained a summary only. However, SB didpoint out that some areas do appear to be outliers such as cancer deaths, <strong>and</strong>these required further review.A debate then ensued as to the value of the Observatory data. MS felt that theObservatory format was very easy to scan <strong>and</strong> would like to see other datapresented in that way to the Committee. PS <strong>and</strong> SB were asked to considerhow the data could be usefully used <strong>and</strong> to bring a report to the next meeting.ActionAllCRSBCRDCWSBSB / PS2
The main quality dashboard was then discussed <strong>and</strong> it was stressed that itwould be important for the Clinical Directors to own the dashboard <strong>and</strong> toprovide the necessary data for their Directorate. This triggered a query by CGregarding the level of clinical governance support available to the Directorates<strong>and</strong> it was explained that PS <strong>and</strong> MS are meeting with each Clinical Director toexplain what was required of them, but the intention was to move from acentral clinical governance structure to one that was embedded into therevised structure. In addition a Clinical Governance H<strong>and</strong>book had beenprovided to each Clinical Director.There was a general level of concern that due to annual leave, some datawere missing from the dashboard <strong>and</strong> if read externally, this could lead othersto assume this was unavailable or not being adequately covered, which wasincorrect. It was agreed that SB would discuss outside the meeting, whatother arrangements can be put in place to ensure future access to PMO datawhen staff are on leave. AD felt strongly that operational managers need toensure the information required to populate the dashboard is available <strong>and</strong> CGoffered to take this back through the operational structure.Questions were raised about the breakdown between hospital acquired <strong>and</strong>community acquired pressure damage cases shown in the dashboard <strong>and</strong> GEconfirmed that the figure shown was a combined figure but explained that inthe Energise for Excellence report appearing later on the agenda, thisbreakdown was shown.MW felt that the narrative relating to single sex breaches did not address thequery raised by the Committee in February for more information on the plansto address the problem. GE explained that he had visited Whipps Cross <strong>and</strong>other <strong>Trust</strong>s to review how they were managing the breaches occurring inITU/HDU <strong>and</strong> as a result costed plans have been drawn up for physicalchanges amounting to approximately £1m. However, he felt that no workshould be undertaken until the McKinsey emergency access work hadprogressed as improving the bed flow would result in greater ability to ‘stepdown’ ITU/HDU patients to general wards thus reducing the number ofbreaches. CG concurred feeling that more time should be allowed before adecision was made. SB added that the Health4NEL <strong>and</strong> re-jigging of criticalcare across London would also impact on the <strong>Trust</strong>’s single sex breaches. GEconfirmed in response to a query by AD, that to ensure full transparency thetopic was on the agenda for the next Improving Patient Experience Group.36/<strong>2012</strong> Items for Escalation from Feeder CommitteesPS explained the key issues that were being escalated by the Quality & SafetyCommittee’s feeder committees. These were from the Clinical AuditCommittee where information on National audits has not been forthcomingfrom the clinical leads; this issue together with the tardiness in completing theaudit registration procedures has been raised with Clinical Leads.The Clinical Risk Committee raised the issues of poor record tracking by wardbased staff <strong>and</strong> the lack of a suitable system for maternity health records. Ofconcern was the extremely poor compliance by doctors to include their GMCnumbers on prescription charts. The final item for escalation was theperceived lack of accountability across the organisation. SB suggested thatthe previous requirement for presentations by the relevant areas would, ifreintroduced, go some way to dealing with this issue. It was proposed that thissuggestion would be considered further by MS, SB <strong>and</strong> PS.ActionSBCGMS / PS/ SB3
In relation to the GMC concern, SB advised that he has written out on 3separate occasions stressing the requirement to comply but this has not led tothe expected improvements. It was generally felt that taking a tough stance byrejecting the request for drugs if the GMC information was not provided mightbe a way of delivering a strong message to doctors, but the potential impact onpatient care was a major concern. EC felt that if patients understood thereason for delays this would be understood. POB agreed with EC butconsidered the GMC issue to be a separate one to the TTAs (drugs to takeaway). A solution to improving untracked patient notes <strong>and</strong> doctors complyingwith the GMC requirement would be sought by MS, PS <strong>and</strong> POB outside themeeting.37/<strong>2012</strong> Corporate Accreditation Quarter 4 RegisterSB reported on the 3 visits that had taken place during the last quarter of2011/12, explaining that informal feedback from the HFEA visit was good <strong>and</strong>their report was expected.GS advised that both Haematology <strong>and</strong> Biochemistry had been reviewed <strong>and</strong>had high levels of critical non-compliances. This appears to be because of arebasing of the criteria being applied to ‘critical’ <strong>and</strong> did not take account of theresource implications for ensuring compliance. Due to the rebasing, GSstressed that the <strong>Trust</strong>’s preparations will be reviewed very carefully before thenext inspection for Microbiology. At the present time Cellular Pathology is theonly area fully accredited. GS went on to explain that within pathology theyare reconsidering how quality is being managed <strong>and</strong> are looking at roles,responsibilities <strong>and</strong> support mechanisms with the intention of appointing aQuality Manager.Since the detailed action plans for Haematology <strong>and</strong> Biochemistry had notbeen provided to enable the Committee to review the intended actions to moveforward towards full compliance, GS was asked to send these to CR forcirculation.PATIENT SAFETY38/<strong>2012</strong> Care Quality Commission Update & Action PlanThe latest iteration of the action plan, together with the March report to NHSLondon had been included with the agenda <strong>papers</strong>, <strong>and</strong> are also being sharedwith the Audit Committee, <strong>Trust</strong> <strong>Board</strong> <strong>and</strong> <strong>Trust</strong> Executive Committee.Progress against the 81 actions is being closely monitored by the Project<strong>Board</strong> <strong>and</strong> PMO, with updates every 2 weeks to NHS London <strong>and</strong> theCommissioners. The <strong>Trust</strong> <strong>Board</strong> was being kept informed.SB advised that whilst progress was on course, there were a number of longerterm actions that will not achieve full compliance for some time but, at thecurrent time, only 6 of the outst<strong>and</strong>ing ‘red’ items had 2 or more elementsrequiring completion with the potential to lead to delays <strong>and</strong> these were beingdiscussed with the Operational <strong>and</strong> Executive leads. All other actions arenearing completion with many of their under-pinning individual actionscompleted <strong>and</strong> evidence collected.The position with the <strong>Trust</strong> wide review <strong>and</strong> progress against the WarningNotices were also summarised within the executive summary to the report.There was some debate about the timing of positive outcomes on the CQCwebsite where there appeared to be a delay between what is being told to the<strong>Trust</strong> <strong>and</strong> what is actually being shown. SB suggested he discuss this with ADso that this could be raised informally with the CQC at a future meeting.ActionMS / PS/ POBGSSB4
39/<strong>2012</strong> Maternity Implementation Plan UpdateAK explained that the plan had been agreed with NHS London <strong>and</strong> theCommissioners in September 2011 <strong>and</strong> capped daily deliveries at Queen’s at20 <strong>and</strong> 7 at King George; the initial plan was for this to continue until the 31 stMarch <strong>2012</strong>. At a meeting last week the <strong>Trust</strong> was offered assurances <strong>and</strong> isawaiting confirmation that the capping of deliveries will stop from the 1 st May<strong>and</strong> the <strong>Trust</strong> will resume its activity. An internal review has shown that onaverage the <strong>Trust</strong> is currently delivering 17-19 births a day at Queens <strong>and</strong> 4-5at King George which with the average of 4-5 labour rooms empty each day<strong>and</strong> good levels of staffing would ensure the <strong>Trust</strong> can maintain a safe service.However, to ensure there are no future problems there is now a clear definitionof excessive levels <strong>and</strong> a London-wide Escalation Policy is in place with clearSt<strong>and</strong>ard Operating Procedures to follow.The Chair, on behalf of the Committee, praised the significant progress thathas been made. AD advised the improvements have been recognised by boththe CQC <strong>and</strong> NHS London.AK went on to explain that the elective caesarean sections that had beendiverted in early October were now being performed by the <strong>Trust</strong>. Memberswere asked to note that the Essex Overview & Scrutiny Committee has askedthat the diverted Essex women are allowed back <strong>and</strong> the intention is to resumeelective caesarean sections for an average of 30-40 Essex women per week.40/<strong>2012</strong> Vascular & Stroke Network St<strong>and</strong>ards – 6 monthly updateSB presented this report explaining that the <strong>Trust</strong>’s Stroke Unit <strong>and</strong> HyperAcute Stroke Unit were accredited. The report details the pressures that arebeing experienced when non stroke emergency admissions are placed inthese units. The Stroke Network are aware of these pressures which arebeing experienced at other stroke units. Patients are currently being escalatedto the Network for repatriation to their local stroke unit as required.Since the centralisation of vascular services from both the <strong>Trust</strong>’s main sites toQueen’s Hospital in March 2011 evidence is available to demonstrate that the<strong>Trust</strong> has achieved 14 of the 22 st<strong>and</strong>ards in a short period, however evidenceagainst the remaining 8 required before approval as a complex vascular centrehave been deferred. The requirements to ensure each consultant to enterdata onto the National Vascular database <strong>and</strong> that a 24/7 interventionalradiology rota should be in place have now been demonstrated. Finalevidence was submitted to an external peer review on the 30 th March <strong>and</strong> theoutcome has yet to be communicated to the <strong>Trust</strong> although it is expected wewill be accredited as a Vascular Unit. SB advised there had been issues aboutvolume <strong>and</strong> numbers but case loads are being met, <strong>and</strong> the <strong>Trust</strong> feelsconfident it will do so in future.41/<strong>2012</strong> Medicines Security Assurance ReportPOB asked for it to be noted that the Governance of Medicines Managementreport was still to be completed, <strong>and</strong> the paper circulated is Medicines SecurityAssurance Report. The need for this report arose following Freedom ofInformation requests about medicines security that led the Department ofHealth to ask for an audit by all <strong>Trust</strong>s to be completed by the 31 st March<strong>2012</strong>. The report is attached <strong>and</strong> although it has not yet been ratified by theDrugs & Therapeutic Committee, it was signed off by the Chief Executive toenable compliance by the deadline.The audit was based on retrospective information from Visible LeadershipAction5
audits carried out quarterly on the storage of medicines, the controlled drug 3-monthly audits <strong>and</strong> patient drugs 3-monthly audits. 25 different areas werereviewed <strong>and</strong> the findings showed compliance in 13 areas, with 12 areas thatwere non-compliant. POB cautioned that the criteria was set very high <strong>and</strong> a10% failure resulted in a finding of non-compliant. The key issues found werethat drugs in some areas were being left outside of the lockable cupboards;fridges were not locked <strong>and</strong> temperature recording was not consistently beingcarried out. The third area was that in some departments patients’ TTA drugswere found, which should have been returned to pharmacy to reduce the riskof them being given to another patient or being misused <strong>and</strong> to allowpharmacy, where appropriate, to return the drugs to the pharmacy stock.ActionAn action plan has been prepared <strong>and</strong> will be taken with the report to theDrugs & Therapeutic Committee. Further audits are planned <strong>and</strong> a jointpharmacy / nursing group has been asked to look at the issues. Newsletterswill be used to ensure the key messages from the review are shared.GE felt the report was excellent, <strong>and</strong> confirmed with POB that it was beingtaken to this week’s Nursing & Midwifery <strong>Board</strong>. GE offered his support.AW felt that most of the areas of non-compliance were relatively easy to dealwith.42/<strong>2012</strong> Infection Control Annual PlanGE presented the draft infection control annual plan that has been reviewed bythe Infection Control Committee, explaining that relevant staff had beeninvolved in its development. The Committee was asked to comment on theplan by providing feedback to the Director of Nursing.SB reported that the <strong>Trust</strong>’s MRSA bacteraemia target for 2011/12 had been 8<strong>and</strong> the final number of actual cases had been 10. The target for <strong>2012</strong>/13 hasbeen set at 7 <strong>and</strong> the <strong>Trust</strong> has already had 1 confirmed case. It is importantthat a rigorous root cause analysis be applied <strong>and</strong> the findings used toreinvigorate the infection control strategy. It was also felt that the <strong>Trust</strong>’sMRSA policy needed to be rigorously applied. IS stressed the need for sharedlearning from the root cause analysis <strong>and</strong> GE explained that the LearningLessons Group will have a regular item on their agenda. The groupmembership includes an Infection Control Nurse.43/<strong>2012</strong> MRSA Screening PerformancePATIENT OUTCOMESAt the February meeting DCW had been asked to provide an update on thepoor MRSA screening data. The report confirmed that there has been anoverall improvement in compliance with screening elective admissions acrossall Divisions, but emergency screening was static. In addition, there has beenconfusion in some areas about the need to screen or not; particularly forgynaecology patients admitted for very short stays. Actions are in h<strong>and</strong> tomake improvements through the exclusion of those patients that do not needscreening.44/<strong>2012</strong> AEU Expansion ReportMS provided a report on the acute elderly service which showed that followingthe launch of the Acute Elderly Unit in June 2010, Phase 1 had beencompleted with various actions being completed between opening <strong>and</strong>December 2011. Two of the Phase 2 actions have been completed with 36All
items at ‘amber’ <strong>and</strong> 2 at ‘red’ requiring completion in <strong>2012</strong>.Further plans include increased specialist input to older persons at the ‘frontdoor’, consultant geriatrician input to all older persons admitted, improvedskills <strong>and</strong> knowledge in the care of patients with dementia, delirium <strong>and</strong>depression, <strong>and</strong> consistent care across the whole week. There were noquestions on the report, which was felt to be both informative <strong>and</strong> helpful.45/<strong>2012</strong> Emergency LSCS Performed within Graded TimeAK advised there were ongoing concerns relating to the timeframes foremergency caesarean sections. She explained the different timeframes forthe different grades. The high number of Grade 1 cases which are those withlife threatening consequences <strong>and</strong> which should be within 30 minutes havebeen discussed with Commissioners <strong>and</strong> bench marked against other <strong>Trust</strong>s.It would appear that our Consultant <strong>and</strong> medical staff are grading some casesincorrectly <strong>and</strong> this has been discussed at an internal meeting. AK stressedthat any changes to the way patients are graded requires very carefulassessment <strong>and</strong> review with appropriate training to avoid confusion <strong>and</strong> risk topatients.Discussions with Commissioners are also reviewing the target to ensure it ismore realistic, but AK advised that last year the <strong>Trust</strong> achieved 77% for Grade1 cases <strong>and</strong> this year the rate is 95.5%; this has been achieved throughimproved cover in the labour ward. Following a query by AW about themedian value <strong>and</strong> range, AK explained that the delays in Grade 1 cases beingachieved within 30 minutes was often only delayed by 1 or 2 minutes <strong>and</strong>where the delay was over 10 minutes, this was frequently because of clinicalreasons. AK agreed to provide AW with an estimate of the range.AD pointed out that there were lessons to be learnt, stressing that staff need tobe aware of what other <strong>Trust</strong>s are doing <strong>and</strong> bench-marking their ownperformance. SB felt the <strong>Trust</strong> was actually being bench-marked by NHSLondon against a wide range of parameters that other <strong>Trust</strong>’s are not beingmeasured against, <strong>and</strong> which are highlighting some areas for improvement. Itwas felt that SB should consider whether the positives of the bench-markingprocess could be used in a positive journal article.46/<strong>2012</strong> Energise for ExcellenceGE presented the report prepared by the Assistant Director of Nursing. Thereport showed there were high numbers of pressure ulcers reported duringQuarter 3 <strong>and</strong> steps were being taken to carry out root cause analysis to clearthe backlog <strong>and</strong> ensure lessons are learnt.GE asked members to note there had been 3 deaths from falls during 2011<strong>and</strong> again, root cause analysis investigations were being conducted <strong>and</strong> thefindings would come to this Committee when they are signed off. POB felt thatreviews of patient falls should consider appropriate prescribing.Concerns were raised by AW that the pressure ulcer situation was gettingworse but SB advised that better reporting was partly responsible for theincrease <strong>and</strong> the <strong>Trust</strong> was getting better at recognising hospital <strong>and</strong>community acquired pressure damage. He also explained that seriousincidents are now a CQUIN target <strong>and</strong> the <strong>Trust</strong> was meeting its trajectoryalthough it was important to continue looking closely at them. MS felt the rawdata showed that community acquired pressure damage accounts for a highproportion of the cases, <strong>and</strong> she advised there is a lot of work going on withthe community to develop a ‘no blame’ framework for the recording <strong>and</strong>management of pressure damage. It was agreed the report needs additionalnarrative to explain the reasons for the high numbers <strong>and</strong> the actions beingActionAKSBGE7
taken. GE was asked to take this comment back to the author.SB commented that falls <strong>and</strong> catheter related incidents are included as part ofthe Milestone Tracker, <strong>and</strong> these were currently graded as ‘amber/red’ <strong>and</strong> sogave cause for concern.47/<strong>2012</strong> Safeguarding Adults Update ReportPATIENT EXPERIENCEGE presented the Safeguarding Adults report, highlighting the key points thatthe safeguarding team is now fully established; safeguarding adults trainingneeds analysis <strong>and</strong> strategy have been produced, <strong>and</strong> the <strong>Trust</strong>’s draftSafeguarding Adults Policy has been developed. In addition the safeguardingadult link worker scheme has been reinvigorated. GE advised there had beena total of 82 safeguarding adult referrals to the safeguarding team between 1 stDecember <strong>and</strong> 18 th March.It was noted that from the 1 st April the national dementia CQUIN comes intoforce <strong>and</strong> the <strong>Trust</strong>’s Dementia Committee is looking at its existing dementiapathway to ensure it meets the CQUIN requirements.GE reported that a comprehensive plan is in place to deliver CQC Outcome 7targets <strong>and</strong> is on target to meet all of the deadlines, this is now ‘blue’ on theCQC action plan as the supporting evidence has been provided.Whilst providing an update to the Committee, GE advised that there will be aLearning Disability week commencing the 18 th June with a number of eventsplanned to launch the MenCap Charter with lots of st<strong>and</strong>s to generateengagement.48/<strong>2012</strong> National Outpatient SurveyThe report provided members with an update against the 2009-2011 resultswith the results appropriately RAG-rated. In essence, the results show nochange despite the plan put in place following the last survey to generateimprovements. It was felt important the a multi-disciplinary approach wasneeded to ensure ownership across the organisation with each ClinicalDirector mapping their own area’s performance.MS stressed the need for there to be a clear strategy for engaging with teamsin Outpatient Clinics with more innovative ways of recording patients’ views;suggesting a simple red ball/green ball being given to patients for them to putinto tubs at the end of their visit to record how they felt about the visit.GE agreed to contact the Committee responding to the survey to convey theCommittee’s views <strong>and</strong> would feedback to the next meeting.49/<strong>2012</strong> National Inpatient SurveyThe Inpatient Survey was based on the views of patients discharged during<strong>July</strong> 2011. A similar review of the Inpatient Survey to the one for theOutpatient survey shows there has been a deterioration since the 2009-11survey <strong>and</strong> this aligns to CQUIN questions being asked through the real timesurvey. The report will be made public on the 24 th April by the CQC so untilthat date, there should be no onward transmission of the report. Oncereleased the CQC will identify where the <strong>Trust</strong> sits in relation to other <strong>Trust</strong>s inthe country.The members again debated how the organisation can own the findings <strong>and</strong>turn them around with additional concerns raised about changing patientperceptions; citing mixed sex ward responses as an example of whereActionGE8
communications could be better used. It was suggested that Executives couldgive presentations at different forums to stress the importance of ensuringattitudes <strong>and</strong> beliefs are changed <strong>and</strong> patients remain the central focus ofperformance. The similarity between the themes from this report, theoutpatient report <strong>and</strong> the staff survey was stressed by IS. GE explained that abid has been made for 10 more feedback kiosks, new comment cards arebeing printed <strong>and</strong> big banners have been ordered to inform patients how theycan have their views heard.GE was asked to bring an action plan to the next meeting.50/<strong>2012</strong> Update on Surgical ComplaintsA short briefing paper on responding to surgical complaints was presentedacknowledging the backlog <strong>and</strong> the poor response times. MS advised that theSurgical Division’s backlog had been considerable <strong>and</strong> had proved challenginghowever with a lot of effort all but 3 of the complaints up to the end ofDecember had been cleared. The team felt they were now on track to achievethe expected 80% by the end of March; the figures are yet to be finalised.MS explained that additional support was needed to manage the complaints inemergency care. However, because of the level of scrutiny of the complaintresponses the number of complainants returning unsatisfied has reduced.It was felt by AW that the additional efforts had produced positive results thatshould receive praise.51/<strong>2012</strong> Implementing Patient StoriesGE told the Committee how in previous employments it had been st<strong>and</strong>ardpractice for patients to be invited to <strong>Trust</strong> <strong>Board</strong> meetings to tell their stories.The executive summary to the report listed how this could be achieved atBHRUT.POB felt this was a good initiative but questioned how front line staff wouldbecome involved. This was also a view held by MS who said that whilstaddressing <strong>Trust</strong> <strong>Board</strong>, it also needed to be cascaded to the rest of theorganisation through Directorate teams. EC explained how a film had beenmade of her own experiences <strong>and</strong> how this, <strong>and</strong> other similar patient videos,had proved highly effective tools; she was happy to offer her services if thisidea was taken forward. IS felt the idea was very good <strong>and</strong> advised that acouple of patients were currently being filmed but she cautioned the need toensure both good <strong>and</strong> bad experiences needed to be included in any Part I<strong>Trust</strong> <strong>Board</strong>. The importance of subsequent patient feedback was alsohighlighted by EC.52/<strong>2012</strong> Equality ObjectivesIn the absence of AD, IS reported there is a new legal requirement on the<strong>Trust</strong> to have measurable indicators for equality <strong>and</strong> the three shown in thereport are those proposed by the <strong>Trust</strong>. Members were asked to providefeedback <strong>and</strong> the consensus was that they were reasonable.ActionGE53/<strong>2012</strong> Any Other BusinessNo other business was proposed.54/<strong>2012</strong> Summary of Issues for Escalation to <strong>Trust</strong> <strong>Board</strong>• The suggestion of patients attending <strong>Trust</strong> <strong>Board</strong> to tell their patient storyshould be escalated to the <strong>Trust</strong> <strong>Board</strong>.SB9
20/<strong>2012</strong> Date of Next MeetingThe next meeting will be held at 14.00 hrs on the 12 th June <strong>2012</strong> in MeetingRooms 1&2ActionACTION LOG – PART I33/<strong>2012</strong> MINUTES OF THE MEETING – 14.2.12The figures relating to the number of sickle cell patients to be clarified as theyappear very high. (15/<strong>2012</strong>)Wording in the last sentence of 09/<strong>2012</strong> to be changed to show that <strong>Havering</strong>Chief Executive leads on safeguarding children across London, <strong>and</strong> not <strong>Havering</strong>.ResponsibilityIGCRQSC terms of reference to be checked in relation to the time for submission ofreports for meetings.34/<strong>2012</strong> MATTERS ARISING / ACTION LOGAll reports to future meetings to be submitted no later than 1 week in advance ofmeeting.The importance of narrative for the Quality Dashboard to be emphasised toClinical Directors. (04/<strong>2012</strong>)A detailed report providing detail of the roll out plans for increasing ward roundConsultant cover to deliver improved senior medical review of patients is requiredfor the next meeting. This to be requested from the Associate Medical Director.(06/<strong>2012</strong>)Information to be provided at the next meeting on whether the proposed separatemeeting to discuss HCA development as a result of the <strong>Havering</strong> Enter & Viewvisit has taken place. (16/<strong>2012</strong>)The contractual arrangement between the <strong>Trust</strong> <strong>and</strong> ISTC remains an outst<strong>and</strong>ingitem requiring feedback at the next meeting.35/<strong>2012</strong> DIVISIONAL QUALITY DASHBOARDValue <strong>and</strong> use of the East Midl<strong>and</strong>s Observatory data to be considered <strong>and</strong>reported to the next meeting.Action to be taken to ensure data is available even during PMO annual leave.Operational managers’ responsibilities to provide requested data / information ontime to be raised.36/<strong>2012</strong> ITEMS FOR ESCALATION FROM FEEDER COMMITTEESThe reintroduction of presentations from feeder committees on areas of concern tobe discussed <strong>and</strong> fed back to the Committee.Explore options to improve untracked patient notes <strong>and</strong> ensure doctors complywith the <strong>Trust</strong> requirement to quote GMC number on prescription charts.37/<strong>2012</strong> CORPORATE ACCREDITATION QUARTER 4 REGISTERThe Haematology <strong>and</strong> Biochemistry action plans to be sent to CR for onwardcirculation to members.CRAll membersSBCRDCWSBSB / PSSBCGMS / PS / SBMS / PS / POBGS10
38/<strong>2012</strong> CARE QUALITY COMMISSION UPDATE AND ACTION PLANThe delay between CQC verbal reports on improvements <strong>and</strong> the changesbecoming evident on their website to be discussed with the Chief Executive <strong>and</strong>raised informally with the CQC.42/<strong>2012</strong> INFECTION CONTROL ANNUAL PLANFeedback to be provided to the Director of Nursing on the draft Annual Plan.45/<strong>2012</strong> EMERGENCY LSCS PERFORMED WITHIN GRADED TIMEAn estimate of the range used for this data to be provided to AW.Consideration to be given to producing a positive journal article about the benefitsof measuring <strong>and</strong> meeting the NHS London performance indicators.46/<strong>2012</strong> ENERGISE FOR EXCELLENCEQSC comments on the report to be relayed to the Assistant Director of Nursing48/<strong>2012</strong> NATIONAL OUTPATIENT SURVEYFeedback from the Quality & Safety Committee to be made to the OutpatientSurvey Response Committee with feedback to next QSC.49/<strong>2012</strong> NATIONAL INPATIENT SURVEYAn action plan to address the Inpatient Survey findings to be brought to the nextmeeting.54/<strong>2012</strong> SUMMARY OF ISSUES FOR ESCALATION TO TRUST BOARDThe suggestion of patients attending <strong>Trust</strong> <strong>Board</strong> to tell their patient story to beescalated to <strong>Trust</strong> <strong>Board</strong>.SBAll membersAKSBGEGEGESB11
Charitable Funds CommitteeMinutes from meeting held onMonday 27 th March <strong>2012</strong>Attendees: Keith Mahoney KM Non- Executive Director, ChairmanDavid Wragg DIW Director of FinanceDeborah Wheeler DCW Director of NursingBill Langley WL Non-Executive DirectorJackie Doyle JD Divisional Manager-Estates, Facilities & CapitalLinda George LG Charitable Funds AccountantChris Stevens CS Head of Fundraising1 Charity Br<strong>and</strong>ing – Superfantastic PresentationRepresentatives from Superfantastic attended the meeting to present their suggestionson different types of br<strong>and</strong>ing, including logos, colour schemes <strong>and</strong> promotionalleaflets. The Committee was informed that the representatives would also show theseideas to some focus groups for their input <strong>and</strong> feedback2 ApologiesNone3. Minutes of the Previous Meeting & Matters ArisingThe minutes from the previous meeting held on 28th February <strong>2012</strong> were agreed as acorrect record.Investment presentationsThe Committee members were informed that the proposed Investment Managers’representatives attended the presentations on 22 nd March <strong>and</strong> it was agreed thatShroders would be our new Investment Managers.Application for the Complementary Therapy Co-ordinatorThe Committee approved an extension to support the Complementary Therapist for afurther year once the current period has ended in June.Application for Positive Patient IDThe Committee was informed that DIW had met with Campaign. DIW report that, froma personal perspective, there would be an upfront cost with a large administrationInterim Chairman: George WoodChief Executive: Averil Dongworth
urden <strong>and</strong> he was not in agreement with this being charitable. It was also agreed thatit seemed a big investment for what it was. This was not approved.Usage of KGH PharmacyDCW <strong>and</strong> JD were communicating about ambulance transport <strong>and</strong> also reported thatthe waiting room was cold <strong>and</strong> draughty. JD reported that the team inspected thewhole area including the patients’ waiting room <strong>and</strong> suggested that the Outpatientsarea could be placed where it would be warmer, with the ambulance booking in areabeing on the left h<strong>and</strong> side. The ambulance desk would be moved to where theinformation desk currently is <strong>and</strong> that this could then leave a place for aninformation/reception desk. This could also be where keys <strong>and</strong> bleeps were housed<strong>and</strong> could be the main expense. The Committee agreed that Claire McLaughlin shouldsubmit a bid for the work including the reception desk. DCW asked where the PALSoffice would go <strong>and</strong> was informed that this would remain where it was. CS re-iteratedon the commercial aspect of the siting of the PALS office, but it was agreed that thePALS office needed to be accessible. JD to draw up a cost.ACTION JDSenior Sisters’ MeetingCS updated the Committee on the Senior Sisters’ meeting. He reported that peoplewanted to meet up <strong>and</strong> that there were a number of wish lists. The attendees hadheard of the Charity but some were unaware if their wards or departments hadbenefited.Screens for the Multi Faith Room at QHThe Committee was updated on the investigations on the Multi Faith screen application<strong>and</strong> it was agreed that this application would be passed. ApprovedRequest for Toasters <strong>and</strong> MicrowavesIt was noted that microwaves could not have elements in. The pantrys were notclassed as enclosed rooms. CS informed the Committee that he was waiting to hearwhere the toasters <strong>and</strong> microwaves were needed at KGH <strong>and</strong> the idea needed to beconsistent with QH. JD reported that it would not be ideal to go down that route <strong>and</strong>that smaller areas now have toasters <strong>and</strong>/or microwaves. The fire officer will bearranging local training <strong>and</strong> could discuss the need. CS will liaise with him aboutlocations <strong>and</strong> the correct detector heads. JD suggested the approval of microwaves insome relevant areas <strong>and</strong> to see how these go, but reminded the Committee of the highcosts due to the equipment being industrial <strong>and</strong> the need for fire-retardant casings.ACTION CS2
Verbal Request for Patient FaresLG informed the Committee that TfL would not give any concessions for bulk purchasesof Oyster Cards <strong>and</strong> the Committee discussed the possible costs involved. WLsuggested that we should support the costs for a couple of weeks <strong>and</strong> see theoutcome.ACTION LG/CSRefurbishment of DSU Patient Waiting AreaCS sought clarification from the DSU team that the request was just to improve thewaiting area. KM enquired if this needed doing <strong>and</strong> it was reported that there was noset time for some surgical procedures, so patients could be waiting for long periods <strong>and</strong>the improvements would benefit those patients awaiting surgery. This was approved.4 Fundraising – Draft StrategyCS informed the Committee that 5 keys challenges had been added to the draftstrategy <strong>and</strong> that if these could be met there would be more chances of fundsincreasing. KM felt that the wording in section 1.1 needed to be replaced with theemphasis on the growing dem<strong>and</strong> for Charitable Funds. WL suggested that part ofsection 1.2 should be moved to the ‘Objectives’ area <strong>and</strong> to incorporate the use of radio<strong>and</strong> commercial relationships within the opportunities at 1.3. WL also felt that otherareas of weakness could involve the website <strong>and</strong> communications as well as thepossible dilution of the charity as a result of KGH League of Friends being seen to be incompetition, although not directly. WL also felt that Communications should also beincluded within the objectives. It was agreed that CS could focus on Communications<strong>and</strong> seek promotional leaflets etc.ACTION CS/JD5 Statement of Financial Activities <strong>and</strong> Balance Sheet for the period:1 st February <strong>2012</strong> – 29 th February <strong>2012</strong>The Committee received the updated SoFA <strong>and</strong> Balance Sheet for February <strong>2012</strong> <strong>and</strong>the Committee noted the report..6 Income <strong>and</strong> Expenditure from 1 st February <strong>2012</strong> to 29 th February <strong>2012</strong>The Committee was asked to note the report.5 7 Requests for ExpenditureComplementary TherapyCS said that the funding was now in place <strong>and</strong> the Committee agreed to support the3
post for a further additional six months. JD suggested that, after two years, if therewas positive feedback, the post should not continue to be paid by charities <strong>and</strong> thatthere should then be a business case in place <strong>and</strong> a budget available. WL requestingverification of the costs <strong>and</strong> CS explained the some volunteers offer to assist <strong>and</strong> somepatients return after treatment is completed for one more complementary treatment.This request was approved to cover funding until June 2013Additional Cots for Tropical LagoonJD informed the Committee that this equipment as well as mattresses were High Spec<strong>and</strong> would be coming from her budget.TV for Discharge loungeJD explained the benefit to patients waiting to be collected after being released from thewards, who may have a considerable wait to be picked up by relatives or anambulance. There is a requirement for cabling to be put in place to facilitate a TV, butthis would make the patients’ waiting time more pleasurable. This request wasapprovedAfinion HbA1C analysersAn analyser is already being used at QH having been paid for by donations fromDiabetes UK. DCW asked to check with clinical engineers on the full cost. Marinod’Aliessio should be approached to ensure that there are no installation costs. WLasked if this was something that KGH League of friends would pay for. This requestwas not approved until further investigation.ACTION CS/KMBreast Lipo FillingWL <strong>and</strong> DCW asked if we received income from the procedure <strong>and</strong> DIW confirmed thatthe trust charges, but the additional funds are being requested to remove <strong>and</strong> replacethe fat tissue. JD informed the Committee that this was not full reconstruction <strong>and</strong>DCW asked why there was not a tariff. CS informed the Committee that a staffmember had raised just over £10k. JD suggested that Eileen Moore should beapproached for more information. This request was not approved until furtherinformation was receivedACTION CS/LGBreast Ultrasound RoomJD informed the Committee that the area was in poor condition <strong>and</strong> CS reported that hewas also awaiting the cost for a water cooler in the area. This request was approvedwith an additional cost authorised for the water cooler.4
Occupational Health <strong>and</strong> WellbeingWL asked how the equipment would promote the business, how long on average dopeople wait in the waiting area; what types of messages will they be displaying on thescreen <strong>and</strong> who/how would they be produced <strong>and</strong> how many people visit occupationalhealth? JD asked for clarification on the costs.ACTION CSAOBCS informed the Committee that Malcolm Buckley, a councillor from Basildon, wants toraise funds for a neuro stimulator <strong>and</strong> wants to get the Basildon Mayor involved. CSsent details to Mr Low, as the <strong>Trust</strong> is already using one, but not the updated version.WL asked whether this was a necessity or just for the sake of getting a new one. CSexplained that the newer version was faster to use This request was not approveduntil a full bid is received.ACTION CS/LG8. Children’s Wards Charitable AccountsCS reported on the Paediatric accounts <strong>and</strong> explained that the manager wanted all thefunds to go into one charitable account. KM agreed with the objectives, but said thatthis should not stop the play leaders from accessing funds for play items as there wasno budget for these otherwise. The Committee agreed that donations with specificrequests should be spent straight away <strong>and</strong> the holding accounts should be put into thechildren’s wards general purpose accounts but earmarked for the relevant expenditure.It was suggested that the paediatric directorate should have a fundraising workinggroup similar to that in Oncology.ACTION CS9. Lavender Garden UpdateThe Committee were notified that both George <strong>and</strong> Avril were unaware of the officialopening of the Lavender Garden. KM mentioned that he had emailed both George <strong>and</strong>Avril, but this was not entered in Sue William’s diary. CS informed the Committee thatall the invitations had been sent out. Communications recommended that staff shouldbe invited <strong>and</strong> an email sent to matrons to nominate one or two staff members. WLasked how many we would expect to cater for. CS reported the expected numberwhich included local MPs, councillors <strong>and</strong> community groups. He also informed theCommittee that Apex Conference Centre had raised funds <strong>and</strong> asked if they could filmthe event at no cost to the Charity, <strong>and</strong> that they would also like to do interviews.Bedrock would be providing the PA system, <strong>and</strong> marquees had also been organisedwith the decision to buy them as these would be cheaper than hiring. The Committeeagreed that a speaker could inform all the attendees on the difference that the Charitymakes. The Committee approved the use of retained gains proportionately to coverthe balance costs of the garden.5
10. Investment Report <strong>and</strong> TenderingKM, DW <strong>and</strong> WL attended the Investment Manager’s presentations along with PaulGreenshaw on 22 nd March, <strong>and</strong> it was agreed that the shares would be placed in theh<strong>and</strong>s of Schroders. This was duly noted.ACTION DIW/LGLG reported to the Committee that the value in the portfolio as at 27 th March <strong>2012</strong> hadincreased by £162k <strong>and</strong> the report as at 27 th March was distributed.11. Any Other Business – The meeting came to a close at this point.Dates of Future Meetings for <strong>2012</strong>Dates <strong>and</strong> Venues for the Remaining Meetings for <strong>2012</strong>All meetings will take place at 2pm – 4pmTuesday 29 th May – <strong>Board</strong>roomTuesday 26 th June – <strong>Board</strong>roomTuesday 31 st <strong>July</strong> – <strong>Board</strong>roomTuesday 25 th September – Sky Room on 4 th Floor (CS or LG to collect key from Education)Tuesday 30 th October – <strong>Board</strong>roomTuesday 27 th November – <strong>Board</strong>room6


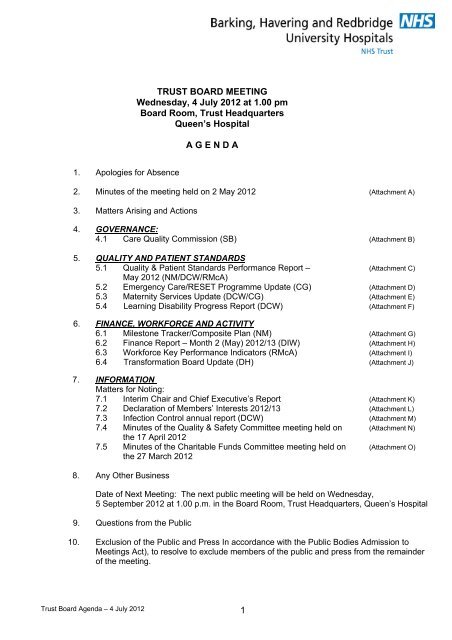
![[4] Biopsy Leaflet.pub - Barking, Havering and Redbridge University ...](https://img.yumpu.com/51285530/1/190x134/4-biopsy-leafletpub-barking-havering-and-redbridge-university-.jpg?quality=85)