Tanzania HIV/AIDS and Malaria Indicator Survey ... - Measure DHS
Tanzania HIV/AIDS and Malaria Indicator Survey ... - Measure DHS
Tanzania HIV/AIDS and Malaria Indicator Survey ... - Measure DHS
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
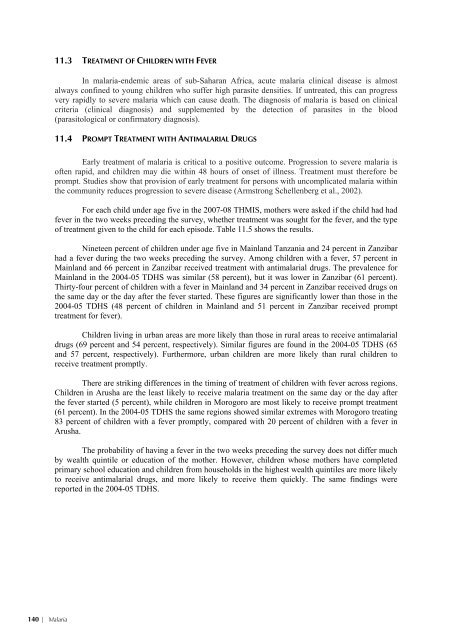
11.3 TREATMENT OF CHILDREN WITH FEVERIn malaria-endemic areas of sub-Saharan Africa, acute malaria clinical disease is almostalways confined to young children who suffer high parasite densities. If untreated, this can progressvery rapidly to severe malaria which can cause death. The diagnosis of malaria is based on clinicalcriteria (clinical diagnosis) <strong>and</strong> supplemented by the detection of parasites in the blood(parasitological or confirmatory diagnosis).11.4 PROMPT TREATMENT WITH ANTIMALARIAL DRUGSEarly treatment of malaria is critical to a positive outcome. Progression to severe malaria isoften rapid, <strong>and</strong> children may die within 48 hours of onset of illness. Treatment must therefore beprompt. Studies show that provision of early treatment for persons with uncomplicated malaria withinthe community reduces progression to severe disease (Armstrong Schellenberg et al., 2002).For each child under age five in the 2007-08 THMIS, mothers were asked if the child had hadfever in the two weeks preceding the survey, whether treatment was sought for the fever, <strong>and</strong> the typeof treatment given to the child for each episode. Table 11.5 shows the results.Nineteen percent of children under age five in Mainl<strong>and</strong> <strong>Tanzania</strong> <strong>and</strong> 24 percent in Zanzibarhad a fever during the two weeks preceding the survey. Among children with a fever, 57 percent inMainl<strong>and</strong> <strong>and</strong> 66 percent in Zanzibar received treatment with antimalarial drugs. The prevalence forMainl<strong>and</strong> in the 2004-05 T<strong>DHS</strong> was similar (58 percent), but it was lower in Zanzibar (61 percent).Thirty-four percent of children with a fever in Mainl<strong>and</strong> <strong>and</strong> 34 percent in Zanzibar received drugs onthe same day or the day after the fever started. These figures are significantly lower than those in the2004-05 T<strong>DHS</strong> (48 percent of children in Mainl<strong>and</strong> <strong>and</strong> 51 percent in Zanzibar received prompttreatment for fever).Children living in urban areas are more likely than those in rural areas to receive antimalarialdrugs (69 percent <strong>and</strong> 54 percent, respectively). Similar figures are found in the 2004-05 T<strong>DHS</strong> (65<strong>and</strong> 57 percent, respectively). Furthermore, urban children are more likely than rural children toreceive treatment promptly.There are striking differences in the timing of treatment of children with fever across regions.Children in Arusha are the least likely to receive malaria treatment on the same day or the day afterthe fever started (5 percent), while children in Morogoro are most likely to receive prompt treatment(61 percent). In the 2004-05 T<strong>DHS</strong> the same regions showed similar extremes with Morogoro treating83 percent of children with a fever promptly, compared with 20 percent of children with a fever inArusha.The probability of having a fever in the two weeks preceding the survey does not differ muchby wealth quintile or education of the mother. However, children whose mothers have completedprimary school education <strong>and</strong> children from households in the highest wealth quintiles are more likelyto receive antimalarial drugs, <strong>and</strong> more likely to receive them quickly. The same findings werereported in the 2004-05 T<strong>DHS</strong>.140 | <strong>Malaria</strong>





![Obtaining Informed Consent for HIV Testing [QRS4] - Measure DHS](https://img.yumpu.com/49850117/1/190x245/obtaining-informed-consent-for-hiv-testing-qrs4-measure-dhs.jpg?quality=85)