7djtK7kw4
7djtK7kw4 7djtK7kw4
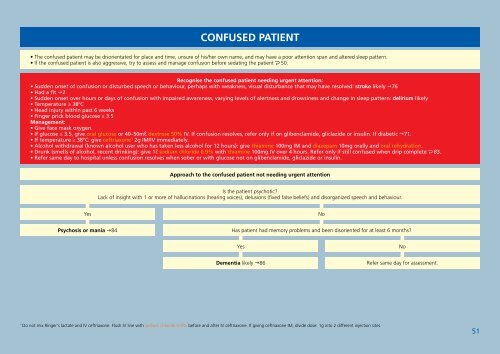
CONFUSED Patient• The confused patient may be disorientated for place and time, unsure of his/her own name, and may have a poor attention span and altered sleep pattern.• If the confused patient is also aggressive, try to assess and manage confusion before sedating the patient 50.Recognise the confused patient needing urgent attention:• Sudden onset of confusion or disturbed speech or behaviour, perhaps with weakness, visual disturbance that may have resolved: stroke likely 76• Had a fit 2• Sudden onset over hours or days of confusion with impaired awareness, varying levels of alertness and drowsiness and change in sleep pattern: delirium likely• Temperature ≥ 38ºC• Head injury within past 6 weeks• Finger prick blood glucose ≤ 3.5Management:• Give face mask oxygen.• If glucose ≤ 3.5, give oral glucose or 40–50ml dextrose 50% IV. If confusion resolves, refer only if on glibenclamide, gliclazide or insulin. If diabetic 71.• If temperature ≥ 38ºC: give ceftriaxone 1 2g IM/IV immediately.• Alcohol withdrawal (known alcohol user who has taken less alcohol for 12 hours): give thiamine 100mg IM and diazepam 10mg orally and oral rehydration.• Drunk (smells of alcohol, recent drinking): give 1l sodium chloride 0.9% with thiamine 100mg IV over 4 hours. Refer only if still confused when drip complete 83.• Refer same day to hospital unless confusion resolves when sober or with glucose not on glibenclamide, gliclazide or insulin.Approach to the confused patient not needing urgent attentionIs the patient psychotic?Lack of insight with 1 or more of hallucinations (hearing voices), delusions (fixed false beliefs) and disorganized speech and behaviour.YesNoPsychosis or mania 84Has patient had memory problems and been disoriented for at least 6 months?YesNoDementia likely 86Refer same day for assessment.1Do not mix Ringer's lactate and IV ceftriaxone. Flush IV line with sodium chloride 0.9% before and after IV ceftriaxone. If giving ceftriaxone IM, divide dose: 1g into 2 different injection sites.51
STRESSED OR MISERABLE Patient• Assess the patient with suicidal thoughts 49.Recognise the stressed/miserable patient needing urgent attentionAssess the stressed/miserable patient• The patient may have headache, dizziness, fatigue, abdominal pain. S/he may have poor eye contact, cry easily, be agitated or communicate poorly.Screen for mental problem• If low mood or sadness, loss of interest or pleasure, feeling tense, worrying a lot or not coping as well as before, consider depression/anxiety 81.• If > 21 drinks/week (man) or > 14 drinks/week (woman) and/or > 5 drinks/session or misuses illicit or prescription drugs consider substance abuse 83.• If hallucinations, delusions and abnormal behaviour, consider psychosis 84.• If memory problems, screen for dementia 86.Identify the traumatised/abused patient• Ask ‘Are you unhappy in your relationship? Has anything happened to you which changed your life?’ If yes to either 53.Try to identify a cause to focus on a solution• Ask about financial difficulty, bereavement, post-natal 97, menopause 98 or chronic ill-health (is HIV status known? 60).• Review medication: oral corticosteroids, oestrogen-containing oral contraceptives ( 91), theophylline, efavirenz can cause mental side effects. Reassure patient on efavirenz that low mood isusually self-limiting and resolves within 6 weeks on ART. If > 6 weeks doctor to change to NVP 200mg 12 hourly.Advise the stressed/miserable patient• Encourage patient to take time to relax:--Do a relaxing breathing exercise each day.--Find a creative or fun activity to do.--Spend time with supportive friends or family.• Regular exercise might help.• Advise patient to get adequate sleep. If patient has difficulty sleeping 54.• Link patient to available psychosocial services: counsellor, psychologist, support group, social worker, helpline back page.• Deal with negative thinking--The patient may often predict the worst, generalise, exaggerate the problem, inappropriately take the blame, or take things personally.--Encourage the patient to question his/her way of thinking (like changing ‘I am a failure’ to ‘I am not a failure, I have achieved many good things in the past’), examine the facts realisticallyand look for strategies to get help and cope.• See communicating effectively see Preface.Offer to review the patient in 1 month.52TB HIV CHRONIC RESPIRATORYDISEASECHRONIC DISEASESOF LIFESTYLEMENTAL HEALTH EPILEPSY MUSCULOSKELETALDISORDERSWOMEN'S HEALTH
- Page 6 and 7: THE UNCONSCIOUS PatientManage the u
- Page 8 and 9: WEIGHT LOSSRecognise the patient wi
- Page 10 and 11: LYMPHADENOPATHY (enlarged lymph nod
- Page 12 and 13: COLLAPSE• Unconscious 1• Fit 2
- Page 14 and 15: HEADACHE• Sudden onset of severe
- Page 16 and 17: FACE SYMPTOMSRecognize the patient
- Page 18 and 19: NOSE SYMPTOMSRunny or blocked noseA
- Page 20 and 21: CHEST PAINRecognise the patient wit
- Page 22 and 23: WHEEZE/TIGHT CHESTInitial Managemen
- Page 24 and 25: ABDOMINAL PAIN WITH OR WITHOUT SWEL
- Page 26 and 27: DIARRHOEARecognise the ill patient
- Page 28 and 29: GENITAL SYMPTOMSAssess the patient
- Page 30 and 31: VAGINAL DISCHARGE• It is normal f
- Page 32 and 33: OTHER GENITAL SYMPTOMSFirst assess
- Page 34 and 35: ABNORMAL VAGINAL BLEEDING• BP < 9
- Page 36 and 37: URINARY SYMPTOMSRecognise patient w
- Page 38 and 39: JOINT SYMPTOMSRecognise the patient
- Page 40 and 41: NECK PAINRecognise the patient with
- Page 42 and 43: FOOT SYMPTOMS• If the problem is
- Page 44 and 45: BURNSAttend urgently to the patient
- Page 46 and 47: PAINFUL SKINFirm, red lump which so
- Page 48 and 49: GENERALISED ITCHY RASHIf status unk
- Page 50 and 51: GENERALISED NON ITCHY RED RASHIs pa
- Page 52 and 53: CHANGES IN SKIN COLOURYellow skinDa
- Page 54 and 55: SUICIDAL PatientRecognise the patie
- Page 58 and 59: TRAUMATISED/ABUSED PatientRecognize
- Page 60 and 61: TB: DIAGNOSISExclude TB in the pati
- Page 62 and 63: TB: ROUTINE CAREAssess the patient
- Page 64 and 65: Manage the patient with a positive
- Page 66 and 67: HIV: ROUTINE CAREAssess the patient
- Page 68 and 69: Advise the patient with HIV• Supp
- Page 70 and 71: ASTHMA AND COPD: DIAGNOSIS• The p
- Page 72 and 73: CHRONIC OBSTRUCTIVE PULMONARY DISEA
- Page 74 and 75: CARDIOVASCULAR DISEASE (CVD) RISK:
- Page 76 and 77: DIABETES: ROUTINE CAREAssess the pa
- Page 78 and 79: HYPERTENSION: DIAGNOSISCheck blood
- Page 80 and 81: HEART FAILURE: ROUTINE CARE• The
- Page 82 and 83: ISCHAEMIC HEART DISEASE (IHD): DIAG
- Page 84 and 85: PERIPHERAL VASCULAR DISEASE (PVD)
- Page 86 and 87: DEPRESSION AND ANXIETY: DIAGNOSISAs
- Page 88 and 89: SUBSTANCE ABUSEIdentify the patient
- Page 90 and 91: Advise the patient with psychosis
- Page 92 and 93: EPILEPSYDr• If the patient is fit
- Page 94 and 95: GOUT• Gout is a metabolic disease
- Page 96 and 97: CONTRACEPTIONGive emergency contrac
- Page 98 and 99: THE PREGNANT Patient• Fitting•
- Page 100 and 101: ROUTINE ANTENATAL CAREAssess the pr
- Page 102 and 103: POSTNATAL CAREAssess the mother and
- Page 104 and 105: PREP ROOM ASSESSMENT OF THE Patient
CONFUSED Patient• The confused patient may be disorientated for place and time, unsure of his/her own name, and may have a poor attention span and altered sleep pattern.• If the confused patient is also aggressive, try to assess and manage confusion before sedating the patient 50.Recognise the confused patient needing urgent attention:• Sudden onset of confusion or disturbed speech or behaviour, perhaps with weakness, visual disturbance that may have resolved: stroke likely 76• Had a fit 2• Sudden onset over hours or days of confusion with impaired awareness, varying levels of alertness and drowsiness and change in sleep pattern: delirium likely• Temperature ≥ 38ºC• Head injury within past 6 weeks• Finger prick blood glucose ≤ 3.5Management:• Give face mask oxygen.• If glucose ≤ 3.5, give oral glucose or 40–50ml dextrose 50% IV. If confusion resolves, refer only if on glibenclamide, gliclazide or insulin. If diabetic 71.• If temperature ≥ 38ºC: give ceftriaxone 1 2g IM/IV immediately.• Alcohol withdrawal (known alcohol user who has taken less alcohol for 12 hours): give thiamine 100mg IM and diazepam 10mg orally and oral rehydration.• Drunk (smells of alcohol, recent drinking): give 1l sodium chloride 0.9% with thiamine 100mg IV over 4 hours. Refer only if still confused when drip complete 83.• Refer same day to hospital unless confusion resolves when sober or with glucose not on glibenclamide, gliclazide or insulin.Approach to the confused patient not needing urgent attentionIs the patient psychotic?Lack of insight with 1 or more of hallucinations (hearing voices), delusions (fixed false beliefs) and disorganized speech and behaviour.YesNoPsychosis or mania 84Has patient had memory problems and been disoriented for at least 6 months?YesNoDementia likely 86Refer same day for assessment.1Do not mix Ringer's lactate and IV ceftriaxone. Flush IV line with sodium chloride 0.9% before and after IV ceftriaxone. If giving ceftriaxone IM, divide dose: 1g into 2 different injection sites.51