PDF(168 KB)
PDF(168 KB)
PDF(168 KB)
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
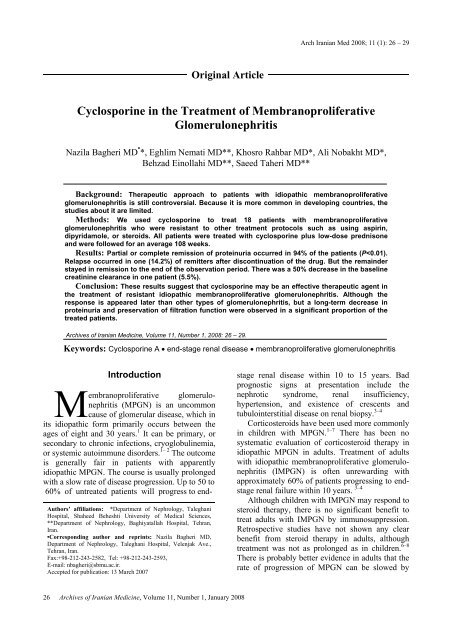
Arch Iranian Med 2008; 11 (1): 26 – 29Original ArticleCyclosporine in the Treatment of MembranoproliferativeGlomerulonephritisNazila Bagheri MD • *, Eghlim Nemati MD**, Khosro Rahbar MD*, Ali Nobakht MD*,Behzad Einollahi MD**, Saeed Taheri MD**Background: Therapeutic approach to patients with idiopathic membranoproliferativeglomerulonephritis is still controversial. Because it is more common in developing countries, thestudies about it are limited.Methods: We used cyclosporine to treat 18 patients with membranoproliferativeglomerulonephritis who were resistant to other treatment protocols such as using aspirin,dipyridamole, or steroids. All patients were treated with cyclosporine plus low-dose prednisoneand were followed for an average 108 weeks.Results: Partial or complete remission of proteinuria occurred in 94% of the patients (P
N. Bagheri, E. Nemati, K. Rahbar, et alantiplatelet agents. 9–11Preliminary study suggests that in the shortterm, the combination of mycophenolate mofetil(MMF) and prednisolone can significantly reduceproteinuria and may preserve renal function inpatients with IMPGN. 11 In this study, five patientsreceived MMF in combination with oralprednisolone and a significant reduction inproteinuria from a baseline of 5.09 to 1.97 g/24 hr(P=0.003) at six months, to 1.96 g/24 hr (P=0.003)at 12 months, and to 2.59 g/24 hr (P=0.015) at 18months was reported. 12Cyclosporine is a well-known and effectiveimmunosuppressive agent, which has been used inmost solid organ transplantation and as treatmentof different types of glomerular diseases. 13 Thedrug-receptor complex specifically andcompetitively binds to and inhibits calcineurin, acalcium and calmodulin-dependent phosphatase. 14This process inhibits the translocation of a familyof transcription factors and nuclear factor ofactivated T cells (NF-AT), leading to reducedtranscriptional activation of early cytokine genesfor interleukin 2, tumor necrosis factor alpha(TNF-alpha), interleukin 3, interleukin 4, CD40L,granulocyte-macrophage colony-stimulating factor,and interferon γ. It seems that this drug has someeffects on the permeability of glomeruli and causesglomerular vasoconstriction. 14 It has been used astreatment in different types of glomerulonephritisespecially in resistant cases but not many studiesabout its effect on MPGN have been done.We report a trial using cyclosporine in adultswith biopsy-proven MPGN resistant to antiplateletagents and corticosteroids.Materials and MethodsPatients with primary MPGN were included inthis study. At the entry, the mean age of thepatients was 27±9 years ranging from 18 – 50years. All patients had failed to achieve aremission of proteinuria after a course of treatmentwith prednisone or antiplatelet agents andangiotensin-converting enzyme (ACE) inhibitors.Exclusion criteria were serum creatinine level>2.5 mg/dL, comorbid condition with expectedsurvival of less than two years, any serioussystemic infection, secondary form of MPGN, andassociated disorders requiring daily NSAIDs.Proteinuria equal or greater than 3.5 g/day wasconsidered nephrotic. A partial remission wasdefined as a 50% reduction of initial proteinuriaand equal or less than 3.5 g/day with stable renalfunction. Complete remission was defined asproteinuria equal or less than 0.2 g/d accompaniedby stable renal function.DiagnosisDiagnosis of MPGN was made based on theclinical and laboratory findings such as nephritic ornephrotic range proteinuria, hematuria,hypertension, serum C3 and CH50 levels, andsometimes mild renal function impairment. Renalbiopsy was performed for confirmation ofdiagnosis.MPGN was characterized by its peculiarhistologic findings such as lobular appearance,cellular and mesangial matrix proliferation, doublecontoured capillary loops in light microscopy,presence of C3, IgG, or IgM deposits inimmunofluorescent (IF) study, and existence ofelectron-dense deposits within the glomerularbasement membrane and/or subendothelium andmesangium in electron microscopy.In all the patients, the initial diagnosis wasconfirmed by pathologic findings in light and IFmicroscopy. We also had electron microscopyreports for five patients. Decreased complementlevel was reported in 14 patients.ProtocolsCyclosporine-neoral (CsA-Neoral) was startedat a dose of 4-5mg/kg/day (divided doses). Allpatients received prednisone at 0.15 mg/kg/day upto maximum of 15 mg and ACE inhibitors. Thepatients’ clinical status and vital signs, renal andliver function tests, lipid profiles, serum creatinine,and 24-hr urine excretion rates of creatinine andprotein were measured at 0, 1, 3, 6, and 12 monthsafter starting cyclosporine. Early stop pointsincluded a confirmed rise equal or >30% inbaseline serum creatinine, doubling of baselineliver enzymes, and intolerable side effects.Cyclosporine was discontinued gradually ifcomplete remission of proteinuria was achieved.Statistical analysisQuantities were shown as mean±SD. TheStudent’s t-test was used for evaluation of changesin proteinuria and creatinine before and after thestudy. P
Cyclosporine in the treatment of MPGN1.000.8083.30%0.600.400.200.005.50%Cyclosporinefailure0%Cyclosporineresponse11.20%Positive Hx of the treatment withother regimensNegative Hx of treatment with otherregimensFigure 1. Response to cyclosporine in patients who did not respond to other regimens.Of them, 16 patients (88.8%) had failed to achieveremission with other regimens.Seventeen patients (94.5%) were responsive tocyclosporine. Twelve of responders achievedcomplete remission and the remainder achievedpartial remission. There was failure to treatment inone patient who had been nonresponder to otherregimens either. Only in this patient there was asignificant decrease in renal function (Figure 1).Duration of disease was less than one year ineight patients (44.5%), between one to two years infour patients (22.2%), and more than two years insix patients (33.3%).Complete remission was achieved in sixpatients during six months, in three patients (25%)between six to 12 months, and in three patients(25%) after 12 months. The mean time forachievement of remission was 3.8 months. Duringthe two-year follow-up, cyclosporine wasdiscontinued in seven patients (41.1%) and only inone patient (14.2%) relapse occurred (Figure 2).DiscussionMPGN was defined as a distinct histologicvariant of glomerulonephritis. Although it wasmost common during the 1970s – 1980s and isnow a rare finding in adults but in some countriesit occurs more frequently. It has been suggestedthat chronic infections are responsible for thedisease in many of these cases. 2Treatment of MPGN depends in part upon theunderlying cause. Compared with secondaryforms, the outcome is generally fair in patientswith apparently IMPGN. 3 The course is usuallyprolonged with a slow rate of disease progression.Antiplatelet agents and corticosteroids havebeen evaluated in the treatment of those patientswith apparently IMPGN who are at risk forprogressive disease. 6 – 8 There is probably betterevidence in adults compared to children that therate of progression of MPGN can be slowed byantiplatelet agents. 8 – 9 Despite this short-term45.00%40.00%35.00%30.00%25.00%20.00%DependencyTaperingStop DrugRelapse15.00%10.00%5.00%0.00%Figure 2. Result of treatment with cyclosporine28Archives of Iranian Medicine, Volume 11, Number 1, January 2008
N. Bagheri, E. Nemati, K. Rahbar, et albenefit, there was no difference in 10 yearsoutcome, and these studies generally had notcontrol groups. 15There are only limited data on the use ofcytotoxic drugs in MPGN too. No benefit wasobserved when compared with a control group. 9 Nocontrolled study has been performed for evaluationof cyclosporine treatment in MPGN.There are a few case reports about usage of thisagent in MPGN but the final result of theirtreatment was not mentioned clearly. 16 In ourstudy, proteinuria was decreased from 4.5±2.8g/day to 0.7±2.2 g/day after initiation ofcyclosporine (P