Compliance made easy with BCBSGa COBRA Solutions
Compliance made easy with BCBSGa COBRA Solutions
Compliance made easy with BCBSGa COBRA Solutions
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Compliance</strong><strong>made</strong> <strong>easy</strong> <strong>with</strong><strong>BCBSGa</strong> <strong>COBRA</strong><strong>Solutions</strong>
INSIDE FRONT COVERDOES NOT PRINT
For over 67 years, Blue Cross Blue Shieldof Georgia (<strong>BCBSGa</strong>) has been providingGeorgia companies <strong>with</strong> the choice ofquality affordable health care coveragefor their associates. As the largesthealth care insurer in the state, we offeryou the stability that you can trustand the solutions to make your <strong>COBRA</strong>compliance Easy.What is <strong>COBRA</strong>?The Consolidated Omnibus Budget Act of 1985 (<strong>COBRA</strong>) requiresthat employers <strong>with</strong> at least 20 or more employees in the last calendaryear, sponsoring group health plans, offer employees and theirfamilies the opportunity for a temporary extension of health coverage(called “continuation of coverage”). Companies that fall into thiscategory are required to extend <strong>COBRA</strong> continuation rights, benefitsor coverage to any employee and their dependent covered underthe group health plan that has a qualifying event during the calendaryear of which the company is eligible. It is required that continuationof coverage be at group rates in certain instances where coverageunder the plan would otherwise end. Qualifying events include:• Termination• Reduction of hours• Death of the employee• Divorce or legal separation• Dependent children ceasing to meet eligibility requirements• Dependent coverage is lost because the active employeebecomes entitled to Medicare• Retiree or retiree’s spouse or child loses coverage <strong>with</strong>in oneyear before or after commencement proceedings under Title 11(bankruptcy), United States Code.<strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong><strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong> offers you accurate and precise <strong>COBRA</strong>administration to reduce unnecessary claims cost and the convenienceof handling your <strong>COBRA</strong> compliance.<strong>COBRA</strong> <strong>Solutions</strong> will administer <strong>COBRA</strong> for you and provide thefollowing services:• Notify all eligible employees about <strong>COBRA</strong> continuation• Handle billing, collecting and remitting monthly premiums• Notify <strong>COBRA</strong> beneficiaries when benefits are scheduled to end• Provide a monthly report to you, the employer, about your<strong>COBRA</strong> membership• Online Access to send <strong>COBRA</strong> notifications to <strong>COBRA</strong> <strong>Solutions</strong><strong>COBRA</strong> <strong>Solutions</strong> does not provide:• Annual employee notices or notices to newly hired employeesregarding <strong>COBRA</strong> services. In the event that you need noticesfor this purpose, copies can be obtained by calling <strong>BCBSGa</strong><strong>COBRA</strong> <strong>Solutions</strong>.• Memos or notices to employees regarding benefit changes orpremiums as well as the benefit booklets or contracts associated.Your company should send these documents to the <strong>COBRA</strong>members at the same time that active employees are notified.• Open enrollment information1
<strong>COBRA</strong> <strong>Compliance</strong> Requirements• If you maintain an employee health plan which you sponsorfor your employees and you averaged 20 or more employees inthe last calendar year, you are required to offer <strong>COBRA</strong> to youremployees.• Employees only need to be covered under the health plan for oneday to be eligible for <strong>COBRA</strong> continuation.• Every employer <strong>with</strong> 20 or more employees is required to notifyeach employee and their eligible dependent(s) about their <strong>COBRA</strong>rights when they first become covered under the group health plan.• Each time coverage is lost due to a “Qualifying Event” employersare required by federal law to notify the employee <strong>with</strong>in 30 daysof the “qualifying event” even if the employee states that he orshe does not want or need to continue benefits under <strong>COBRA</strong>.This notice must be sent to the last known address and separatenotifications must be sent to the employees eligible dependentsshould they live at a separate address.• Employers must allow continued coverage for employees andtheir eligible dependents for up to 18 months as a result ofunemployment or reduction in hours. Additionally, an employermay elect to continue coverage for up to 36 months for otherQualifying Events such as:- death of the employee- divorce or legal separation- dependents that cease to be a “dependent” under the terms ofthe group health plan- an employee losing coverage because of Medicare eligibility• Qualified dependents (an employee’s spouse or dependentchild who is covered on the day before the Qualifying Event) areentitled to elect to continue their coverage, <strong>with</strong>in 60 days ofreceipt of the <strong>COBRA</strong> notification.• The same health benefits offered to active employees must beavailable to <strong>COBRA</strong> qualified dependents. Dependents may alsochoose from the “core” coverage or other health benefit optionsoffered to active employees.• Employees who elect to continue benefits after a qualifying eventmay be allowed to add new dependents under their extendedcoverage and also change benefits annually if the option isavailable to active employees. This continued coverage must beoffered to eligible employees even if the group falls below 20full or part-time employees.• Initial premium payment for continuation must be received<strong>with</strong>in 45 days after the date of election by <strong>COBRA</strong> participants.A grace period of no less than 30 days would be required forall subsequent premiums.• <strong>COBRA</strong> qualified employees are billed the group’s active healthplan rates plus an additional 2% administrative expense allowedby the <strong>COBRA</strong> regulation.• If the Social Security Administration determines that the qualifiedbeneficiary is considered disabled under Title II or XVI of the SocialSecurity Act <strong>with</strong>in 60 days of the qualifying event, the continuationperiod must be extended for 29 months from the qualifying eventrather than 18 months. Once the beneficiary is eligible for Medicare,<strong>COBRA</strong> coverage will cease.• <strong>COBRA</strong> coverage must be continued even if an exclusion orlimitation <strong>with</strong> respect to any pre-existing condition affects acontinuant’s current coverage.• Following the expiration of <strong>COBRA</strong> coverage, the qualifiedcontinuee must be offered continuation coverage under anyconversion plan that is available to the groups employees.• <strong>COBRA</strong> compliance is serious, therefore, it is advised that legalconsultation supersede any <strong>COBRA</strong> compliance overview providedin this brochure. Judicial decisions are subject to change at anytime. If you are ever in doubt, please contact an attorney.2
How to Enroll Your GroupTo utilize <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong>, simply complete the top portionof the <strong>COBRA</strong> Administration group application. A copy isincluded in this brochure for your use. List your name as it appearson your <strong>BCBSGa</strong> group application. The contact person should bethe name of the employee or group administrator who is appointedto discuss benefit or <strong>COBRA</strong> questions from <strong>BCBSGa</strong> <strong>with</strong> youremployees. Your <strong>BCBSGa</strong> marketing representative will completethe remainder of the form <strong>with</strong> you. Additional information willbe required if your company currently has <strong>COBRA</strong> participants priorto joining/enrolling <strong>with</strong> <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong>. A <strong>COBRA</strong><strong>Solutions</strong> Member Notification Form must also be completedfor any/all future eligible participants, submitted either hard copyor via the Internet. A sample copy of this form along <strong>with</strong> instructionson how to complete it are included in this brochure for youruse. The <strong>COBRA</strong> effective date is the date this service should gointo effect <strong>with</strong> <strong>BCBSGa</strong>. Additionally , you also have the option ofenrolling your associates online via <strong>COBRA</strong> <strong>Solutions</strong> Web Access(CSWA) see page 9 for more information.Contact your marketing representative if you have any questionsregarding the <strong>COBRA</strong> enrollment process.Please note: A service agreement (a copy is included in this brochure)must also be completed at the time of your enrollment. This formprovides an overview of the services performed by <strong>COBRA</strong> <strong>Solutions</strong> andoutlines the obligation of your group in the provision of informationto us for the purpose of <strong>COBRA</strong> administration for you.How to Handle a Qualifying EventAn employee or any dependent needs to be covered by yourgroup health plan for only one day to become eligible for <strong>COBRA</strong>continuation of coverage.Any of the following events that would cause the employee to losehealth care coverage is considered a qualifying event:• Termination of the employee’s employment for any reasonother than “gross misconduct.”• Reduction of the employee’s work hours that would result in theloss of health coverage.• Death of the employee.• Divorce or legal separation.• Dependent child ceases to meet the eligibility requirementsto continue health coverage under the regular health plan.• Dependent coverage is lost because the active employee or<strong>COBRA</strong> continuee becomes eligible for Medicare.The <strong>COBRA</strong> <strong>Solutions</strong> Member Notification Form must be completedwhenever one of the qualifying events occurs, or you may use CSWA.This form can be sent to the <strong>COBRA</strong> <strong>Solutions</strong> office at any time.However, you should not wait longer than 30 days after a qualifyingevent to notify <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong>.<strong>COBRA</strong> <strong>Solutions</strong> will notify the qualified beneficiaries <strong>with</strong>in 14days following the receipt of this form from you. If you use <strong>COBRA</strong><strong>Solutions</strong> Web Access, the notifications are mailed the followingbusiness day. It is important that this form be completed fully.<strong>COBRA</strong> Notice to EmployeesAs an employer, you are required to notify new and all activeemployees and their dependents, covered on the health plan, oftheir <strong>COBRA</strong> rights. The <strong>COBRA</strong> notices should be given to eachemployee when he or she is hired and should be addressed tothe employee, their spouse and eligible dependents.If you have not provided this notice, please be sure to send it tothe employee’s current home address. Please note: If you havequestions regarding the “<strong>COBRA</strong> Notice to Employees”, pleasecontact your attorney for legal advice. If you need a copy of thisnotice, please contact <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong> at 1-800-292-5615or via email at cobrasolutions@bcbsga.com.3
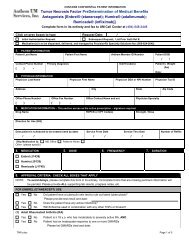
Employer Instructions for Completing the<strong>COBRA</strong> <strong>Solutions</strong> Qualifying Event Notification Form<strong>COBRA</strong> SOLUTIONS MEMBER NOTIFICATION FORMDATE:SEQUENTIAL FORM #1 2 3YOUR GROUP NAME:4YOUR GROUP NUMBER:PLEASE COMPLETE ALL INFORMATION REQUESTEDEMPLOYEE NAME5DOB HCID #/ SSN #TYPECOV-ERAGE6 7 8ADDRESSEVENTCODEQUALIFYINGEVENT DATE(A)BILLINGSTART DATE9 10 11 12EVENT CODES:Please Explain01 - Termination02 – Retirement03 - Medicare04 - Death05 - No Longer an Eligible Dependent06 - Reduce Hours07 – Leave of Absence08 - Divorce/Separation09 – Other(A) Please provide the date to which premiums have been paid.<strong>COBRA</strong> <strong>Solutions</strong> will bill from this date.THIS <strong>COBRA</strong> NOTIFICATION FORM IS TO BE USED TO NOTIFY <strong>COBRA</strong> ADMINISTRATIONOF ELIGIBLE MEMBERS. PLEASE COMPLETE AND MAIL OR FAX TO:<strong>COBRA</strong> SOLUTIONSBlue Cross Blue Shield of GeorgiaP.O. BOX 404145ATLANTA, GEORGIA 30384-4145EMAIL: <strong>COBRA</strong>SOLUTIONS@BCBSGA.COMPHONE: 800-292-5615FAX: 404 842-8040NAME OF PERSON COMPLETING FORMPHONE # AND EXTENSIONPLEASE COMPLETE ALL SECTIONS. PLEASE CALL <strong>COBRA</strong> SOLUTIONS IF YOU HAVE ANY QUESTIONSG-AAD-001976 10/031. The date (month/day/year) that you are sending this form. This formmust be sent to <strong>COBRA</strong> <strong>Solutions</strong> <strong>with</strong>in 30 days of the qualifying event.2. Your full group name as it appears on your regular membership billing.3. Your group number as it appears on your billing. Please submit aseparate form for each group that you report <strong>COBRA</strong> qualifying events.4. Assign a sequential number that will help you identify the forms that yousend to our office should reference be needed to a particular form.5. Give the employee’s full name. Should a qualifying event occur for adependent, please give us the employee information first, followed by thedependent information on the next line.6. Please give the date of birth for the employee or dependent.7. Give us the contract or member number of the employee followed by thesocial security number for any dependents having qualifying events.8. Indicate the type of coverage the qualified beneficiary has <strong>with</strong> yourgroup at the time of the event. Please select from:S – Single CoverageSP – Two Person CoverageF – Family CoverageE&C – Employee and Child CoverageE&C+ – Employee and Children CoveredE&S – Employee and Spouse Coverage9. Give the current address of the employee or dependent10. The code should be selected from those shown on the <strong>COBRA</strong> <strong>Solutions</strong>Qualifying Event Notification Form.11. Give the date of the qualifying event.12. If the member is disabled as determined by the Social SecurityAdministration.Please be sure to mail or fax this form to the address and fax number shownat the bottom.4
PremiumsAs a new group to <strong>COBRA</strong> <strong>Solutions</strong>, we will begin billing your<strong>COBRA</strong> participants the appropriate premium following your group’senrollment and the members being placed in the <strong>COBRA</strong> <strong>Solutions</strong>system. <strong>COBRA</strong> <strong>Solutions</strong> will begin sending a set of premium paymentcoupons to the members who enroll. If you have been billingpremiums for <strong>COBRA</strong> participants, please discontinue, as <strong>COBRA</strong><strong>Solutions</strong> will do this for you.All members utilizing <strong>COBRA</strong> continuation coverage at the timeyou enroll on the service (existing <strong>COBRA</strong> participants) will receivepremium payment coupons to pay future months’ premiums. Shouldyou receive premium payments from these members, please returnthe payment to them and inform them that <strong>COBRA</strong> <strong>Solutions</strong> willbill them directly. As new members enroll in <strong>COBRA</strong> continuationcoverage, they will receive premium payment coupons. Thesecoupons will reflect your applicable group premium plus the administrativepercentage allowed by <strong>COBRA</strong> regulation, which is usually2%.The members will be required to pay premiums on the first ofeach month <strong>with</strong> premiums considered past due after the 30th ofeach month. Coverage is automatically cancelled if premiums are notpaid by the 30th of the month. This is in accordance <strong>with</strong> the <strong>COBRA</strong>regulation and strictly adhered to by <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong>.Exceptions occur when premiums are received in our office after the30th but postmarked on or prior to that date.Monthly premium payments must be paid in full. <strong>BCBSGa</strong> <strong>COBRA</strong><strong>Solutions</strong> does not allow premiums to be broken into smaller increments.However, should a qualified beneficiary desire, they maymake payment for multiple months at one time. Any amounts paidin advance will be subject to rate increases that may occur in yourgroups rate. Should a premium increase occur, the member will berequired to pay the additional premium. Likewise, should a ratedecrease occur, a credit will be given to the member.The first month’s premium may be prorated if cancellation of coverageoccurs other than the first of the month. If you allow coverageto continue through the end of the month in which cancellationoccurs for your active employees, <strong>COBRA</strong> <strong>Solutions</strong> will reflect thesame. The first month’s premium will be adjusted accordingly.For Fully Insured GroupsIf you are a fully insured group <strong>with</strong> <strong>BCBSGa</strong>, we will take care ofyour membership billing for you. As premiums are received by us foryour <strong>COBRA</strong> participants, we will update our membership files foryou. No bill will be sent to you for these members. The monthlyreport furnished on the 15th of the month will show which membersare paying for coverage.Coverage<strong>COBRA</strong> continuation coverage participants are entitled to the samecoverage offered to active employees. Any previously satisfieddeductibles, stop loss amount or coinsurance will be credited tothe members record. The <strong>COBRA</strong> participant usually has the samecontact or member number that was assigned under the groupprogram. The group number will change to reflect that the memberis now covered through <strong>COBRA</strong>. This will have no affect on benefitor benefit levels.The member is entitled to continue the same health benefits thatwere available through active employment. A member may elect tocontinue health coverage only. This option will be available if themember desires. <strong>COBRA</strong> <strong>Solutions</strong> will help the member <strong>with</strong> thiselection. If there are any questions about this procedure, pleasecontact <strong>BCBSGa</strong> <strong>COBRA</strong> <strong>Solutions</strong>.Should a member decline coverage during their 60-day electionperiod, and later decide that they would like <strong>COBRA</strong> continuationcoverage <strong>with</strong>in the 60-day period, coverage will only be extendedfrom the date the member affirms their decision to continuecoverage. This means that a lapse in coverage may occur. In thissituation, a member may have pre-existing waiting periods apply orother contract obligations that occur when a lapse in coverageoccurs. Please see your contract for information concerning lapsesin coverage.Prior to the cancellation of <strong>COBRA</strong> coverage, a member and theirdependents will be notified if they can continue coverage on a<strong>BCBSGa</strong> conversion contract. If no conversion contract is availablethrough your group, benefits will end at that time.<strong>COBRA</strong> benefits are considered group benefits. <strong>COBRA</strong> benefits mustbe exhausted before members are allowed to enroll in a conversioncontract <strong>with</strong> <strong>BCBSGa</strong>.At any time, a member may elect to enroll in an individual <strong>BCBSGa</strong>health care coverage product. Should a member want to examineour individual products, they should contact the <strong>BCBSGa</strong> officenearest them for more information. These health care coverageproducts may be chosen instead of <strong>COBRA</strong> continuation coverage.Medical Underwriting and pre-existing condition waiting periodswill apply.<strong>COBRA</strong> continuation coverage is not allowed when other groupcoverage is elected following the <strong>COBRA</strong> continuation coverageelection. This also includes Medicare coverage following the <strong>COBRA</strong>effective date. Please contact <strong>COBRA</strong> <strong>Solutions</strong> at 1 (800) 292-5615for more information.For Self Funded GroupsIf you are a self-funded group or have coverage <strong>with</strong> another carrier,<strong>BCBSGa</strong> will refund premiums received for your members to you ona monthly basis. These refunds are sent out around the 15th of thefollowing month when reports are generated.If you have a renewal premium increase or decrease, please notify<strong>COBRA</strong> <strong>Solutions</strong> of the new amount. Following this notice, <strong>COBRA</strong><strong>Solutions</strong> will bill your members accordingly.6
<strong>COBRA</strong> <strong>Solutions</strong>Web Access<strong>BCBSGa</strong> is making it easier for you to do business <strong>with</strong> us. Inaddition to the helpful resources already available on our Web site,www.bcbsga.com, we are excited to offer <strong>COBRA</strong> <strong>Solutions</strong>Web Access (CSWA). CSWA allows you to perform changes to youremployees’ records 24-hours-a-day, 7-days-a- week.With <strong>COBRA</strong> <strong>Solutions</strong> Web Accessyou can:1. Enter New <strong>COBRA</strong> Notifications2. Make Changes to <strong>COBRA</strong> Eligibility3. Save Time and Money by using the Internet to transmit <strong>COBRA</strong>NotificationsWith CSWA you can quickly make additions and changes <strong>with</strong> ourpaper-free, electronic enrollment service that uses the speed andconvenience of the Internet. It’s <strong>easy</strong>, efficient and saves you time incompleting your daily tasks. All you need is Internet Explorer version5.0 or later to get started.With <strong>COBRA</strong> <strong>Solutions</strong> Web Access it’seven easier to get what you want• Process <strong>COBRA</strong> Notifications faster than ever <strong>with</strong> the click ofa mouse• Quickly make additions, changes and cancellations• Embedded hotlinks and convenient drop-down menus reducetyping• ‘Steps’ help to track information input• Error messages ensure accuracy of informationCSWA offers you more control: control over employee informationand control over accuracy of information. Error messages signal thatmissing or incomplete information was keyed in, while electronicprompts guide you from one step to the next, from screen to screen.A copy of the CSWA agreement form is included in this brochure.To find out how your company can begin taking advantage of CSWA,please contact your Account Representative or <strong>COBRA</strong> <strong>Solutions</strong> atcobrasolutions@bcbsga.com.CSWA Agreement next page7
<strong>COBRA</strong> <strong>Solutions</strong> Web Access (CSWA)Get the Power of Blue SMworking for you.Access Code Policy and Usage AgreementAccess Code Policy:In order to ensure data security, those individuals receiving Access Codes and accessing the computer resources ofBlue Cross Blue Shield of Georgia (<strong>BCBSGa</strong>), including those of its various affiliates, will adhere to the following methodsof operation:1. Access Codes and passwords will not be revealed by the owner to other individuals.2. No one will use any Access Code and password other than the one issued to him/her.3. CSWA users will not disclose, use, or appropriate confidential or proprietary information beyond which is reasonablynecessary to perform assigned jobs.4. Confidential or proprietary information includes, but is not limited to, the following: medical information, personalinformation regarding members or providers, computer systems or programs, processing techniques, trade secretsand corporate strategies.Violation of this policy by non-<strong>BCBSGa</strong> personnel will result in immediate termination of the person’s Access Code andreporting of the violation to appropriate <strong>BCBSGa</strong> management. <strong>BCBSGa</strong> reserves the right to pursue legal prosecutionunder applicable local, state and federal statutes. Such remedy shall not be exclusive, but shall be cumulative <strong>with</strong> allother remedies at law or in equity.Usage Agreement:I will accept an Access Code and password that allows me to utilize <strong>BCBSGa</strong>’s CSWA System.I have read and agree to the <strong>BCBSGa</strong> Access Code Policy and Usage Agreement as stated above.Name (please print)Signature of UserDate of SignatureCompany NameGroup NumberCompany AddressCity, State, ZIPUsername Email AddressUsername Phone NumberInternal Use OnlyEmployer Group : _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Employer Group #: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Date Agreement Signed: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Access Code Assigned: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Password Assigned: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _Effective Date: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
<strong>COBRA</strong> <strong>Solutions</strong> ApplicationGroup Name:Street Address:Mailing Address:City: State: Zip Code:Contact Person, Title:Email Address:Telephone Number:Fax Number:Alternate if possible:<strong>COBRA</strong> Effective Date:Do not add the 2 percent administrative fee to the rate.Please list all of your health insurance group numbers <strong>with</strong> the appropriate suffix or subgroups. If there is a different group number<strong>with</strong> each group number, please specify along <strong>with</strong> the type coverage offered i.e., health, dental, vision, etc. Please give the appropriaterates that are to be billed to <strong>COBRA</strong> eligible members. (Use additional sheets if more space is needed for the group numbers.)GROUP NUMBER GROUP NAME TYPE OF COVERAGE RATESEmp.Emp. +1Emp. + SPEmp. + Ch(ren)FamilyEmp.Emp. +1Emp. + SPEmp. + Ch(ren)FamilyEmp.Emp. +1Emp. + SPEmp. + Ch(ren)Family
What is your Blue Cross Blue Shield health insurance renewal date?Do you wish to use this same date as the <strong>COBRA</strong> renewal date? ■ Yes ■ NoIf No,please specify the reason for your requestI am aware that the services provided by <strong>COBRA</strong> <strong>Solutions</strong> will commence when I notify <strong>COBRA</strong> <strong>Solutions</strong> of a “qualifying event.”I take responsibility to notify all employees of benefit changes,provide benefit descriptions, and rate changes and will also beresponsible for notifying new employees of <strong>COBRA</strong>.I will notify <strong>COBRA</strong> as employees or their dependents become eligible under the<strong>COBRA</strong> regulations by completing the <strong>COBRA</strong> <strong>Solutions</strong> Member Notification form.I am aware that <strong>COBRA</strong> will bill eligible members based on the information that I furnish.The premium billed to the member(s) willinclude a 2 percent or applicable administrative allowance which will be used by <strong>COBRA</strong> for this program.If my group health benefitsare fully insured, Blue Cross Blue Shield of Georgia will retain the premium and update the appropriate subscriber/member files.If other than a fully insured, Blue Cross Blue Shield of Georgia will refund premium collected.SignatureDateTitleGroup Name (as used by Blue Cross Blue Shield of Georgia)Blue Cross Blue Shield Representative Name
Blue Cross Blue Shield of Georgia3350 Peachtree Road, NEAtlanta, GA 30326(706) 257-1300www.bcbsga.comUnderwritten by Blue Cross Blue Shield of Georgia,an Independent Licensee of the Blue Cross Blue ShieldAssociation11078 03/05SSMEB-0200-00