Building Hope: Taking Cancer Care to the Next Level
Building Hope: Taking Cancer Care to the Next Level
Building Hope: Taking Cancer Care to the Next Level
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
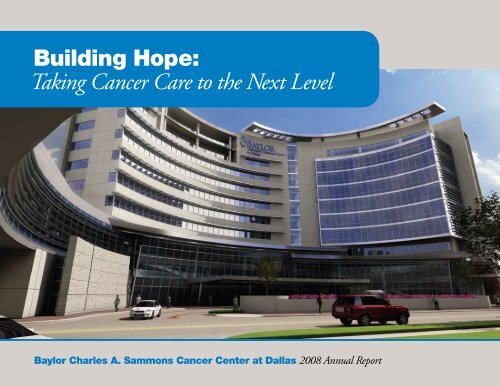
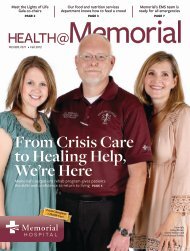
Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas2008 Annual ReportContentsLetter from <strong>the</strong> Direc<strong>to</strong>r .............................................. 1Leadership Changes.................................................. 2The New <strong>Cancer</strong> Center Unveiled ...................................... 3Profile: Donna Bowers<strong>Building</strong> <strong>Hope</strong> Through Specialized <strong>Care</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8Blood and Marrow Transplant Unit UpdateBreast <strong>Cancer</strong> Update<strong>Building</strong> <strong>Hope</strong> One Patient at a Time . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11Patient Navigation ProgramVirginia R. Cvek<strong>to</strong> Patient Education CenterPromoting Prevention and <strong>Cancer</strong> ScreeningsKitchens Lectureship: Music and <strong>the</strong> MindProfile: Andrew Janke<strong>Building</strong> <strong>Hope</strong> Through Quality Improvement Efforts. . . . . . . . . . . . . . . . . . . . . 16Commission on <strong>Cancer</strong> Accreditation<strong>Cancer</strong> Registry UpdateSummary of 2007 <strong>Cancer</strong> Registry DataPCE: 10-Year Experience with Prostate Brachy<strong>the</strong>rapyat Baylor Sammons <strong>Cancer</strong> Center<strong>Building</strong> <strong>Hope</strong> Through Research . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25Personalized MedicineTherapeutic <strong>Cancer</strong> VaccinesEarly Detection for Lung <strong>Cancer</strong>Aquatic Exercise for Breast <strong>Cancer</strong> PatientsEarly Detection of Ovarian <strong>Cancer</strong>Site Tumor Conference Case Reports2008 Publications<strong>Building</strong> <strong>Hope</strong> Through Philanthropy .................................. 30$5 Million Gift for Blood <strong>Cancer</strong> Research2008 Celebrating WomenGift for Imaging Center TechnologyEveryMan Event for Prostate <strong>Cancer</strong>Telephone Direc<strong>to</strong>ry................................................ 32Location Maps .........................................Inside back coverOn <strong>the</strong> cover: Rendering of <strong>the</strong> new 450,000-square-foot outpatient cancer center.Above: Rendering of <strong>the</strong> Healing Garden at<strong>the</strong> new cancer center.<strong>Cancer</strong> research studies on <strong>the</strong> campus of Baylor University Medical Center atDallas are conducted through Baylor Research Institute, Mary Crowley MedicalResearch Center, Texas Oncology, and US Oncology. Each reviews, approves,and conducts clinical trials independently. Their clinical trials are listed <strong>to</strong>ge<strong>the</strong>r,in this publication, for <strong>the</strong> convenience of patients and physicians.Physicians are members of <strong>the</strong> medical staff at one of Baylor Health <strong>Care</strong>System’s subsidiary, community, or affiliated medical centers and are nei<strong>the</strong>remployees nor agents of those medical centers, Baylor University MedicalCenter, or Baylor Health <strong>Care</strong> System. Copyright © 2009, Baylor Health <strong>Care</strong>System. All rights reserved. DH-BH1000-02/09
Letter from <strong>the</strong> Direc<strong>to</strong>rThe year 2008 was a turning point for Baylor Sammons <strong>Cancer</strong> Center. After 3 years of strategic planning, <strong>the</strong> new cancer centerproject was approved by <strong>the</strong> Baylor board of trustees. The three-phase, 5-year project will include a new 450,000-square-foo<strong>to</strong>utpatient cancer center, conversion of <strong>the</strong> Collins building in<strong>to</strong> a dedicated cancer hospital, and renovation of <strong>the</strong> Sammonsbuilding. All of us are excited about this major expansion of oncology at Baylor Dallas! The project was formally announced inSeptember at a ceremony featuring Governor Rick Perry and Mayor Tom Leppert. In November, we were pleased <strong>to</strong> welcomeAlan M. Miller, MD, PhD, as <strong>the</strong> new direc<strong>to</strong>r of <strong>the</strong> Sammons <strong>Cancer</strong> Center and chief of oncology. Dr. Miller was selected for<strong>the</strong>se positions on <strong>the</strong> recommendation of a search committee headed by Dr. Pick Scruggs. Dr. Miller is an expert on blood andstem cell regulation. He was <strong>the</strong> founding direc<strong>to</strong>r of <strong>the</strong> bone marrow transplant program at Tulane. He also served as associatesenior vice president for health sciences at Tulane and headed a Louisiana Board of Regents–funded clinical and translationalresearch, education, and commercialization program. The announcement of <strong>the</strong> new cancer center project and arrival of Dr.Miller ushered in a new era in oncology at Baylor University Medical Center and Baylor Health <strong>Care</strong> System.Dr. Scruggs announced his retirement in November and will be sorely missed. In addition <strong>to</strong> directing radiation oncology atBaylor, Pick served as chair of <strong>the</strong> <strong>Cancer</strong> Center Medical Committee for 18 years. Fortunately, <strong>the</strong> medical committee chair hasbeen assumed by Dr. John Preskitt, our longstanding division direc<strong>to</strong>r of surgical oncology and immediate past president of <strong>the</strong>Baylor Dallas medical staff.Excellence in patient care, research, and education continues <strong>to</strong> be our goal. Advances in molecular biology, genetics, and immunologyhave identified new pathways that make targeted <strong>the</strong>rapy <strong>to</strong> <strong>the</strong> cancer cell increasingly effective. Oncology has emergedas one of <strong>the</strong> most exciting fields in medicine, in large part because progress in <strong>the</strong> basic sciences is being rapidly translated <strong>to</strong> <strong>the</strong>bedside and clinic. The result will be improved outcomes for patients. We will bring <strong>the</strong>se new advances <strong>to</strong> our patients as swiftlyand safely as possible.This is my final direc<strong>to</strong>r’s letter. It has been a privilege <strong>to</strong> serve in this position for <strong>the</strong> past 32 years, and I thank my physiciancolleagues and Baylor staff for <strong>the</strong>ir support and encouragement.Sincerely yours,Marvin J. S<strong>to</strong>ne, MD, MACP<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 1
Leadership ChangesAlan M. Miller, MD, PhDAlan M. Miller, MD, PhD, becamedirec<strong>to</strong>r of <strong>the</strong> Baylor Charles A.Sammons <strong>Cancer</strong> Center and chiefof oncology for Baylor Health <strong>Care</strong>System in November 2008. Beforecoming <strong>to</strong> Baylor he served as associatesenior vice president for health sciencesat Tulane University Health SciencesCenter and in 2007 as interim seniorvice president for health sciences atTulane University. He is a practicingmedical oncologist and previously servedas direc<strong>to</strong>r of <strong>the</strong> bone marrow transplantprogram and vice president and associatedean for clinical affairs at Tulane.Dr. Miller received his PhD in physiologyfrom <strong>the</strong> Roswell Park Division of<strong>the</strong> State University of New York atBuffalo and his MD from <strong>the</strong> Universityof Miami. He did his residency in internalmedicine and fellowship in medicaloncology at <strong>the</strong> University of Florida. Dr.Miller’s research and clinical activity havefocused on blood and stem cell regulation.He has published numerous articlesin peer-reviewed journals on this subject.While at Tulane, Dr. Miller served asprincipal investiga<strong>to</strong>r of a LouisianaBoard of Regents–funded clinical andtranslational research, education, andcommercialization program. For 10years he led <strong>the</strong> National Institutesof Health–funded Tulane SouthwestOncology Group efforts. Dr. Miller hasstrong interests in health care policy andserves on <strong>the</strong> Association of AmericanMedical Colleges Healthcare AdvisoryPanel and was formerly vice chairman of<strong>the</strong> Louisiana Health <strong>Care</strong> Commission.“It is an exciting time <strong>to</strong> be joiningBaylor Sammons <strong>Cancer</strong> Center,” Dr.Miller stated. “The next few years willsee a tremendous growth in <strong>the</strong> center’sprograms and facilities. We have atremendous opportunity <strong>to</strong> build on <strong>the</strong>foundation established by Dr. MarvinS<strong>to</strong>ne and <strong>the</strong> leaders of <strong>the</strong> cancer center<strong>to</strong> grow our reputation as a regionaland national destination cancer centerthrough patient care, education, andresearch.”Dr. Alan M. MillerJohn T. Preskitt, MD,FACPJohn T. Preskitt, MD, FACP,was named chair of <strong>the</strong> Sammons<strong>Cancer</strong> Center MedicalCommittee in September 2008.Dr. Preskitt replaces Robert“Pick” Scruggs, MD, whoretired after serving as chairsince 1990. Dr. Scruggs was a leader at BaylorUniversity Medical Center at Dallas for morethan 30 years, serving as medical direc<strong>to</strong>r ofradiation oncology and assistant chief of <strong>the</strong>Department of Oncology since 1995, presiden<strong>to</strong>f <strong>the</strong> medical staff in 2001, and chairman of<strong>the</strong> medical board of Baylor Dallas in 2002.Dr. John T. PreskittDr. Preskitt joined <strong>the</strong> Baylor Dallas medicalstaff in 1981 after completing his internshipand residency at Baylor Dallas and a surgicaloncology fellowship at M. D. Anderson. He isactive in <strong>the</strong> teaching of surgical residents andhas served as medical direc<strong>to</strong>r of surgical oncologyof <strong>the</strong> Department of Oncology, presiden<strong>to</strong>f <strong>the</strong> medical staff in 2007, and chairman of<strong>the</strong> medical board of Baylor Dallas in 2008.Dr. Preskitt is a regent of <strong>the</strong> American Collegeof Surgeons and has served on several committees,including <strong>the</strong> Executive Committee of <strong>the</strong>Commission on <strong>Cancer</strong>.2 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
The New <strong>Cancer</strong> Center UnveiledWith goals of reducing cancer <strong>to</strong> achronic disease and ultimately finding acure, Baylor University Medical Centerat Dallas announced that it is developingNorth Texas’ first dedicated cancerhospital along with a new outpatientcancer center that will be <strong>the</strong> largest inNorth Texas. The new 450,000-squarefootcancer center is scheduled <strong>to</strong> openin 2011. Work on <strong>the</strong> dedicated cancerhospital will begin in 2010 with completionscheduled for 2013.“When completed in 2013, it will be ourgoal <strong>to</strong> be a nationally and internationallyrenowned cancer care destination,building on Baylor Dallas’ commitment<strong>to</strong> providing advanced cancer treatmentsand leading <strong>the</strong> charge of improvementin cancer care through research,” saidJoel Allison, president and CEO ofBaylor Health <strong>Care</strong> System.An aerial view shows <strong>the</strong> planned location of<strong>the</strong> new 10-s<strong>to</strong>ry outpatient cancer centeron <strong>the</strong> south side of <strong>the</strong> Baylor Dallas campus(at <strong>the</strong> <strong>to</strong>p of <strong>the</strong> illustration above). Theexisting Collins building will be renovatedin<strong>to</strong> a 120-bed inpatient cancer center. Anew circular sky bridge will connect all of<strong>the</strong> buildings housing cancer services.Collins HospitalSammons Tower<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 3
The 120-bed inpatient cancer hospital will be <strong>the</strong> first in North Texas and only <strong>the</strong> second in Texas.The outpatient cancer center and inpatientcancer hospital are a $350 millioninvestment.“Baylor Dallas has his<strong>to</strong>rically been <strong>the</strong>leader in cancer care in North Texas,and we feel a great responsibility <strong>to</strong> offer<strong>the</strong> best cancer care in <strong>the</strong> country,”said John B. McWhorter, <strong>the</strong> hospital’spresident and senior vice president atBaylor Health <strong>Care</strong> System. “We wantpeople <strong>to</strong> be cared for in a compassionatemanner. And we want <strong>to</strong> continue <strong>to</strong>be <strong>the</strong> destination center for cancer carefor citizens of North Texas.”Based on feedback from patients,families, physicians, and staff, <strong>the</strong> newcancer center will be a patient-centeredfacility designed <strong>to</strong> anticipate needsthroughout <strong>the</strong> continuum of care.Activities of <strong>the</strong> Virginia R. CvetkoPatient Education Center will be expanded,and additional complementarymedicine programs will be offered,including programs for massage,acupuncture, music, and art.In addition <strong>to</strong> <strong>the</strong> comprehensive cancerservices already offered at Baylor Dallas,<strong>the</strong> outpatient cancer center will offereasy access and convenient parking; acomfortable and calming atmosphere;a new chapel; an urgent care clinicespecially for cancer patients; an outdoorhealing garden providing a peacefulrespite; and a patient navigation program4 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
News CoverageThe September 26th announcement of Baylor Dallas’ new cancer facility receivednational attention. Baylor made news across <strong>the</strong> country, including an appearance on<strong>the</strong> big screen in New York City’s Times Square.Dallas Mayor Tom Leppert and Texas Governor Rick Perry were featured speakers at<strong>the</strong> announcement. Under <strong>the</strong> governor’s leadership, voters recently approved a $3billion bond package <strong>to</strong> establish <strong>the</strong> <strong>Cancer</strong> Prevention and Research Institute ofTexas, which will create and expedite innovation in <strong>the</strong> area of cancer research andprevention. “We’re moving closer <strong>to</strong> <strong>the</strong> cure, we’re moving closer <strong>to</strong> <strong>the</strong> day whencancer’s deadly role in our society, in our lives, has been eliminated,” Governor Perrystated.<strong>to</strong> help guide patients through <strong>the</strong>ircancer journey.“We’re entering a new era in cancer careat Baylor Dallas,” said Marvin J. S<strong>to</strong>ne,MD, direc<strong>to</strong>r of <strong>the</strong> Baylor Charles A.Sammons <strong>Cancer</strong> Center. “We’ve madeenormous progress during <strong>the</strong> past 32years, but now we’re ready <strong>to</strong> rise <strong>to</strong><strong>the</strong> next level, paralleling <strong>the</strong> strikingadvancements we’ve seen in <strong>the</strong> field,”he said.Baylor conducted a thorough analysis ofnational cancer rates, as well as regionaland local needs, in planning <strong>the</strong> newcancer center and cancer hospital. InTexas, 97,281 new cancer cases wereprojected <strong>to</strong> be diagnosed in 2008,according <strong>to</strong> <strong>the</strong> Texas <strong>Cancer</strong> Registry.In Dallas County, 8,451 new cancercases were projected in 2008. According<strong>to</strong> <strong>the</strong> American <strong>Cancer</strong> Society, <strong>the</strong>lifetime risk of developing cancer is 1 in2 for men and 1 in 3 for women.Announcement of <strong>the</strong> new cancer center in Times Square, New York City.The new cancer center will allow fora more comprehensive, personalizedmedicine program, including areasof research such as targeted <strong>the</strong>rapy.Targeted <strong>the</strong>rapy allows physicians <strong>to</strong>analyze a patient’s genes and determinewhat type of treatment will work best forthat particular patient. The new cancercenter will also allow clinicians <strong>to</strong> engagein fur<strong>the</strong>r cancer research, focusing onbreakthroughs that directly affect patients,whe<strong>the</strong>r through a more accuratediagnosis or more effective treatment. Inaddition, clinical trial participation willbe expanded beyond <strong>the</strong> more than 150studies already offered <strong>to</strong> Baylor patients.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 5
Profile: Donna BowersWhen Donna Bowers talks about <strong>the</strong>plans and vision for <strong>the</strong> new cancer facilitiesat Baylor University Medical Centerat Dallas, she is not just speaking as <strong>the</strong>vice president of <strong>the</strong> oncology programfor Baylor Health <strong>Care</strong> System. Ra<strong>the</strong>r,her words carry a deeper meaning—no<strong>to</strong>nly as a proud, long-time Baylor employee,but as a cancer survivor herself.Like many Baylor employees, Ms.Bowers’ life journey revolves around <strong>the</strong>hospital. She began her career in <strong>the</strong>medical records department at BaylorDallas, now known as health informationmanagement (HIM), while still inhigh school. She went on <strong>to</strong> obtain herbachelor’s degree in health informationmanagement at Texas Woman’s Universitywhile continuing <strong>to</strong> work full-timeat Baylor. At age 19, while still attendingcollege full-time, she was named eveningmanager for <strong>the</strong> HIM department.Upon graduation from Texas Woman’sUniversity, she returned <strong>to</strong> <strong>the</strong> day shift,taking over HIM responsibilities for<strong>the</strong> Baylor Charles A. Sammons <strong>Cancer</strong>Center, and met her husband, Steven6 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Bowers, MD. After a short stint living in Colorado, <strong>the</strong> couple moved back <strong>to</strong>Dallas <strong>to</strong> attend law school at Texas Wesleyan Law School and <strong>to</strong> begin a family.In 1992, she worked at Baylor Dallas as associate direc<strong>to</strong>r of HIM and <strong>the</strong>n spent 5years as <strong>the</strong> direc<strong>to</strong>r leading <strong>the</strong> department. In 2001, she moved in<strong>to</strong> administrationat Baylor Dallas. She became vice president of oncology for Baylor Health <strong>Care</strong>System in 2005. She jumped at <strong>the</strong> chance <strong>to</strong> oversee <strong>the</strong> design and building of<strong>the</strong> new cancer facilities at Baylor Dallas and develop <strong>the</strong> oncology strategy for <strong>the</strong>system, but this was more than a career opportunity—this was a chance <strong>to</strong> give backin a very personal way.In 1999, during her rise <strong>to</strong> career success, Ms. Bowers, <strong>the</strong>n 38, direc<strong>to</strong>r of HIM andmo<strong>the</strong>r <strong>to</strong> 4-year-old Josh and 5-year-old Carli, felt a lump during a breast self-exam.When she didn’t feel any changes after a week, she began rounds of doc<strong>to</strong>r visits. “Iwas <strong>to</strong>ld <strong>the</strong>re was a 99% chance it was cancer,” she said. “I <strong>to</strong>ld <strong>the</strong>m those weren’tvery good odds, but that is how sure <strong>the</strong>y were. Once my breast cancer diagnosis wasconfirmed, I chose <strong>to</strong> undergo a mastec<strong>to</strong>my. I also had 6 months of chemo<strong>the</strong>rapyand radiation and reconstructive surgery.”Ms. Bowers, cancer free for 9 years, looked for a way <strong>to</strong> give back <strong>to</strong> those whohelped her during her fight. It came with her chance <strong>to</strong> help develop <strong>the</strong> new cancerfacilities at Baylor Dallas and through a system-wide initiative <strong>to</strong> grow <strong>the</strong> oncologyservice line. “I knew I could truly understand what a patient needed when <strong>the</strong>y camein<strong>to</strong> <strong>the</strong> organization,” she said. “We did numerous focus groups with patients and<strong>the</strong>ir families <strong>to</strong> find out what <strong>the</strong>y wanted, and each time I knew what <strong>the</strong>y said wasright because that is what I would want as a patient. It offered validity—I could feelit <strong>to</strong>o.”“The outpatient center will be 450,000 square feet and definitely designed around<strong>the</strong> patients and <strong>the</strong>ir families,” she said. “We will keep it very beautiful and elegant—a timeless elegance. We also want it light, bringing in as much of <strong>the</strong> outdoors aswe can.”The new cancer hospital will also have many of <strong>the</strong> features that patients and <strong>the</strong>irfamilies want. “We will have bigger patient rooms with more access for familymembers, more eating places, and special places like <strong>the</strong> healing gardens,” said Ms.Bowers. “We are also focusing more on <strong>the</strong> caregivers. We become very attached <strong>to</strong>our patients and it can be an emotionally difficult job. We want <strong>to</strong> provide a placefor healing, calming, and spirituality for everyone involved in <strong>the</strong> cancer journey.”“At Baylor Dallas and across <strong>the</strong> system, we lead <strong>the</strong> Dallas–Fort Worth area inproviding quality cancer care,” said Ms. Bowers. “I know that as an administra<strong>to</strong>r,but also as a patient. There is no place in <strong>the</strong> area I would ra<strong>the</strong>r be treated for cancerthan at Baylor. We will soon have <strong>the</strong> physical space <strong>to</strong> allow us <strong>to</strong> offer all of <strong>the</strong>services our patients trust us <strong>to</strong> have, including quality and compassionate care,research and clinical trials, education, support, chapel, specialized cancer treatmentprograms, integrated services, specialty boutique, and all o<strong>the</strong>r amenities that ourpatients need and want in a beautiful environment focused on <strong>the</strong> cancer patient and<strong>the</strong>ir families.”“The oncology service line across Baylor is growing and developing,” she added.“Most Baylor facilities offer cancer care <strong>to</strong> patients. We are working with each facility<strong>to</strong> develop new oncology services as well as expand <strong>the</strong> quality services currentlyprovided. <strong>Cancer</strong> <strong>to</strong>uches all of us in some way. Baylor Health <strong>Care</strong> System is <strong>the</strong>place <strong>to</strong> go for quality, compassionate, and innovative live-saving treatments. ForBaylor, <strong>the</strong> patient and <strong>the</strong>ir families come first, and <strong>the</strong> growth and development isdedicated <strong>to</strong> <strong>the</strong>m.”<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 7
<strong>Building</strong> <strong>Hope</strong> Through Specialized <strong>Care</strong>Blood and Marrow TransplantUnit UpdateSymposiumOn Saturday, April 5, 2008, BaylorDallas sponsored “Hema<strong>to</strong>poietic StemCell Transplantation: Past, Present,and Future,” a day-long symposiumon blood and marrow transplantationmedicine. The symposium, attended by97 physicians, nurses, social workers,and o<strong>the</strong>r health care professionals, wasdesigned <strong>to</strong> provide a comprehensiveoverview of blood and marrow transplantationmedicine over <strong>the</strong> last 25years and current and new approaches <strong>to</strong>hema<strong>to</strong>poietic cell transplantation andcellular <strong>the</strong>rapy. The program addressednew developments in hema<strong>to</strong>poietictransplantation biology.The program was chaired by Joseph W.Fay, MD, and Edward D. Agura, MD,acted as modera<strong>to</strong>r. Along with an introductionby Marvin J. S<strong>to</strong>ne, MD, andclosing remarks by Dr. Fay, presentationswere given by international leaders in<strong>the</strong> field, including Rainer F. S<strong>to</strong>rb,MD, Bruce R. Blazar, MD, Fred R.Members of <strong>the</strong> accreditation team for <strong>the</strong> Foundation for <strong>the</strong> Accreditation of Cellular Therapy (FACT). Standing, left <strong>to</strong> right: Laura Brougher,RN, BSN, OCN; Lowell Anderson-Reitz, RN, MS, ANP, AOCN; Shawnette Graham, RN, BSN, OCN; and Deb Spitzer, RN, MSN, OCN. Seated:Pam Carnevale, MHSA; Edward Agura, MD; Jane Golinski, MT(ASCP), BB; and Josephine Murphy, MT(ASCP).8 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Appelbaum, MD, John R. Wingard,MD, and Karolina Palucka, MD.FACT AccreditationIn 1998, Baylor Dallas’ Blood and MarrowTransplantation Program receivedits initial accreditation from <strong>the</strong> Foundationfor <strong>the</strong> Accreditation of CellularTherapy (<strong>the</strong>n known as Foundation for<strong>the</strong> Accreditation of Hema<strong>to</strong>poietic CellTherapy). The program has maintainedFACT accreditation since that time.On July 8, 2008, Baylor receivednotification that <strong>the</strong> program earnedreaccreditation for 3 years. The accreditationapplies <strong>to</strong> all services and facilitiesinspected by FACT, specifically adultau<strong>to</strong>logous and allogeneic hema<strong>to</strong>poieticprogeni<strong>to</strong>r cell transplantation, bonemarrow and peripheral blood cellular<strong>the</strong>rapy product collection, and cellular<strong>the</strong>rapy processing.Graft-Versus-Host Disease ClinicMany complications can be associatedwith a blood and marrow transplant.One of <strong>the</strong> most difficult <strong>to</strong> treat is graftversus-hostdisease (GVHD). To combatthis disease, Baylor Charles A. Sammons<strong>Cancer</strong> Center at Dallas established amultidisciplinary clinic.GVHD occurs after an allogeneictransplant, when a donor’s immune cellsattack <strong>the</strong> recipient’s body. The acuteform often appears within 100 days oftransplant and may cause a skin rash,cramping, nausea, diarrhea, or a suddenrise in liver function test results. Inchronic cases, which tend <strong>to</strong> occur muchlater following bone marrow transplantation,symp<strong>to</strong>ms can mimic o<strong>the</strong>rmedical problems, making diagnosisdifficult. Common symp<strong>to</strong>ms includechanges in <strong>the</strong> patient’s skin, dry eyes,mouth dryness and pain, weight loss,and low blood counts.“We simply cannot predict whichpatient will present with GVHD,” saidEstil Vance, MD, hema<strong>to</strong>logic oncologis<strong>to</strong>n <strong>the</strong> medical staff at Baylor Dallas.“This disease can be disabling. The comprehensivecare provided by a multidisciplinaryteam like <strong>the</strong> one at Baylor Dallasenables patients <strong>to</strong> make remarkablegains and enjoy a better quality of life.”James Chippendale (left front in red parka) and <strong>the</strong> Love <strong>Hope</strong> Strength Foundationteam at <strong>the</strong> base camp of Mount Everest.One Patient’s Journey: James ChippendaleJames Chippendale of Dallas was diagnosed with acute myelogenous leukemia in2000. After three rounds of intense chemo<strong>the</strong>rapy, radiation, and a bone marrowtransplant at Baylor, Mr. Chippendale came back healthier, stronger, and ready <strong>to</strong>join <strong>the</strong> battle against leukemia.Mr. Chippendale, president of CSI Entertainment Insurance headquartered inDallas, teamed with musician and cancer survivor Mike Peters of The Alarm, analternative rock band from Wales, <strong>to</strong> found <strong>the</strong> Love <strong>Hope</strong> Strength Foundation(LHSF) in 2006. The foundation works <strong>to</strong> raise funds through innovative concertsand climbs—including climbs <strong>to</strong> <strong>the</strong> <strong>to</strong>p of <strong>the</strong> Empire State <strong>Building</strong> and<strong>the</strong> base camp of Mount Everest. “The efforts of so many have allowed LHSF <strong>to</strong>provide critical funding for cancer centers worldwide so that all people have access<strong>to</strong> information, quality cancer treatment, and medication and, <strong>the</strong>refore, have <strong>the</strong>best chance for survival,” said Mr. Chippendale.LHSF raised approximately $700,000 its first year and hosts chapters in <strong>the</strong>United States, Australia, <strong>the</strong> United Kingdom, and Peru.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 9
Brenda Bailey, RN, BSN, OCN, CCRNThe Best Are at BaylorThe Texas Nursing Associationand <strong>the</strong> Dallas–Fort Worth NurseExecutives’ annual list of “Great 100Nurses” in <strong>the</strong> Metroplex includedone of Baylor Charles A. Sammons<strong>Cancer</strong> Center at Dallas’ own in2008: Brenda Bailey, RN, BSN,OCN, CCRN, blood and marrowtransplant unit supervisor.Of <strong>the</strong> 100 nurses honored for beingrole models in leadership, service<strong>to</strong> <strong>the</strong> community, compassion as acaregiver, and significant contributions<strong>to</strong> nursing, 20 work withinBaylor Health <strong>Care</strong> System. “Wordscannot express <strong>the</strong> honor that I feelwith this recognition,” Ms. Baileysaid.Breast <strong>Cancer</strong> UpdateBreast MRI for Breast ImagingBreast magnetic resonance imaging(MRI) is an additional procedure thataids in <strong>the</strong> detection of breast cancerat Baylor University Medical Center atDallas. The advanced technology of<strong>the</strong> breast MRI unit works in concertwith both <strong>the</strong> dedicated breast biopsyconsole and <strong>the</strong> computer-aided detectiontechnology. Also, breast MRI aidsin differentiating between benign andmalignant lesions and is key in confirming<strong>the</strong> extent of <strong>the</strong> disease.This advanced technology allows breastMRI-guided biopsies <strong>to</strong> be performedwith great accuracy and ease and reduces<strong>the</strong> overall biopsy exam time. With breastMRI-guided biopsy, most women can resumenormal daily activity immediately.10th Anniversary of Hereditary<strong>Cancer</strong> Risk Program2008 marked <strong>the</strong> Hereditary <strong>Cancer</strong>Risk Program’s 10th anniversary. Since1998, this service has provided cancerrisk assessment and genetic counseling <strong>to</strong>Table 1. Results of Genetic Testing in 1555 Patients, 1998–2008Category Result n N (%)Positive Mutation 142 204 (13%)p53 1Single site 56Ashkenazi multisite 5Negative Comprehensive 1039 1243 (80%)Single site 71Ashkenazi multisite 30Comprehensive and LRP 25Comprehensive and BART 39Comprehensive and p53 5Previous variant amended 33Single site–polymorphism 1O<strong>the</strong>r genetic variant Uncertain significance 70 93 (6%)Favor polymorphism 17And negative BART 5And negative p53 1Pending 15 15 (1%)Total 1555participants at risk for breast and/or ovariancancer. Genetic testing for BRCA1and/or BRCA2 is offered if indicated by<strong>the</strong> pedigree analysis.The program meets all guidelines establishedby <strong>the</strong> American Society of ClinicalOncologists, in which cancer predispositiontesting should be offered when(1) <strong>the</strong> person has a strong family his<strong>to</strong>ryof cancer or very early onset of disease;(2) <strong>the</strong> test can be adequately interpreted;and (3) <strong>the</strong> results will influence <strong>the</strong>medical management of <strong>the</strong> patient orfamily member.Since 1998, <strong>the</strong> program has seen 1,692high-risk individuals (1,659 women and33 men), and 1,555 (92%) chose <strong>to</strong> havegenetic testing. Families learn about <strong>the</strong>Hereditary <strong>Cancer</strong> Risk Program throughcommunity education programs, Internetresources, and physician referrals. Testingresults are shown in Table 1.10 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
<strong>Building</strong> <strong>Hope</strong> One Patient at a TimePatient Navigation ProgramIn 2008, <strong>the</strong> Baylor Charles A.Sammons <strong>Cancer</strong> Center at BaylorUniversity Medical Center at Dallaslaunched a patient navigation programas part of its ongoing commitment <strong>to</strong>provide advanced cancer patient care.The program, led by Cynthia RobinsonHawkins, RN, offers cancer patientsand <strong>the</strong>ir families guidance throughoutStreamlining Treatment for <strong>Cancer</strong> Patients1Physicianreferralor self-referral<strong>to</strong> Baylor2Naviga<strong>to</strong>rcontactspatient <strong>to</strong>ga<strong>the</strong>rinformation,demographics,insurance, etc.3Naviga<strong>to</strong>rcontactspatient <strong>to</strong> relayappointmentinformation;provide patientwith details,directions,campus mapNaviga<strong>to</strong>rreviews patientinformation;interfaces withphysician on <strong>the</strong>Baylor Dallasmedical staff <strong>to</strong>discuss caseand arrangeappointments4 5<strong>the</strong> continuum of care. Patient naviga<strong>to</strong>rscan expedite access <strong>to</strong> services bycoordinating logistics, appointments,educational resources, and o<strong>the</strong>r services.The patient naviga<strong>to</strong>rs serve as part of<strong>the</strong> care team alongside <strong>the</strong> physician,nurse, social worker, and o<strong>the</strong>r allied staffoffering referring physicians a point ofcontact for information, communication,and follow-up. The naviga<strong>to</strong>r is <strong>the</strong>re <strong>to</strong>Naviga<strong>to</strong>rmaintainsregular contactwith patientduringtreatments,appointments,return visits6Naviga<strong>to</strong>rprovidesongoingfollow-up withreferringphysician7Naviga<strong>to</strong>rsendsfollow-up letter<strong>to</strong> patient twoweeks aftertreatmentbegins8Naviga<strong>to</strong>rcontactspatient asneeded aftertreatments, forfollow-upassist referring physicians in getting <strong>the</strong>irpatients care from initial appointmentthrough diagnosis, treatment, and recovery.This program alleviates stress andhelps simplify <strong>the</strong> organization of carefor <strong>the</strong> patients and <strong>the</strong>ir loved ones.Virginia R. Cvek<strong>to</strong> PatientEducation CenterHugs, tears, laughter, creativity, andrelaxation all come <strong>to</strong>ge<strong>the</strong>r <strong>to</strong> helpcancer patients and <strong>the</strong>ir caregivers healat <strong>the</strong> Virginia R. Cvetko Patient EducationCenter at Baylor Sammons <strong>Cancer</strong>Center. For almost 30 years, <strong>the</strong> CvetkoCenter has been an important resourcefor cancer patients and <strong>the</strong>ir loved ones.The center bears <strong>the</strong> name of cancerpatient Virginia Cvetko, and her beliefthat <strong>the</strong>re is life and hope with cancerremains <strong>the</strong> center’s guiding principle.The Cvetko Center offers Internet accessand information about cancer and associatedhealth issues in patient educationand resource rooms. The resource roomsoffer cancer medical guides, inspirationalbooks, cookbooks, videos, and DVDs.Refurbished wigs may be available at nocost <strong>to</strong> patients in need who are undergoingcancer treatment.Whenever possible, <strong>the</strong> Cvetko Centercollaborates with community organizations<strong>to</strong> provide a greater offering ofprograms. Many Cvetko Center activitiesare cosponsored by <strong>the</strong> American <strong>Cancer</strong>Society (ACS). One long-time and verysuccessful program is <strong>the</strong> <strong>Cancer</strong> SurvivorsNetwork program. In this program,cancer survivors visit patients currentlyundergoing treatment for cancer <strong>to</strong>provide support and <strong>to</strong> listen. In 2008,1,140 visits were made by dedicatedvolunteers.ACS also collaborates on <strong>the</strong> Look Good. . . Feel Better program, a quarterly programthat teaches women make-up andhair tips during chemo<strong>the</strong>rapy treatment.In addition, Cvetko Center social workerswork with ACS <strong>to</strong> obtain equipment forpatients and transportation <strong>to</strong> and from<strong>the</strong>ir treatment appointments.The ACS also regularly has a representativepresent in <strong>the</strong> lobby of BaylorSammons <strong>Cancer</strong> Center providing<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 11
patients with information and <strong>the</strong> ACSPersonal Health Manager, an informationresource for patients.<strong>Cancer</strong> Support, Education, andSpecial ProgramsEducation and support are <strong>the</strong> corners<strong>to</strong>nes<strong>to</strong> <strong>the</strong> many programs offeredthrough <strong>the</strong> Cvetko Center. The centeroffers seven ongoing disease-specificgroups along with many special diseasespecificprograms throughout <strong>the</strong> year.In addition, <strong>the</strong> Cvetko Center providescomplementary care programs suchas Journaling for Health and ExpressYourself, a program that helps patientsand <strong>the</strong>ir families express emotions andanxiety through art. More than 3,450participants attended <strong>the</strong> ongoingand special programs presented by <strong>the</strong>Cvetko Center in 2008, an increase of20% over 2007.Celebrating <strong>Cancer</strong> Survivorsand Barrett LectureshipThe Virginia R. Cvetko Patient EducationCenter and US Oncology <strong>to</strong>ge<strong>the</strong>rsponsored Baylor Dallas’ celebration ofNational <strong>Cancer</strong> Survivors Day, June 2through 6, 2008. Refreshments andinformation were available in <strong>the</strong> lobbyof <strong>the</strong> Baylor Sammons <strong>Cancer</strong> Centerall week. Tables were staffed by CvetkoCenter volunteers and staff, as well asrepresentatives from many local cancersupport organizations, including <strong>the</strong>American <strong>Cancer</strong> Society, Gilda’s ClubNorth Texas, and <strong>the</strong> Leukemia andLymphoma Society. Information wasavailable on survivorship issues, earlydetection and prevention, and <strong>the</strong> manysupport groups and programs offered atBaylor Sammons <strong>Cancer</strong> Center and in<strong>the</strong> Dallas area.In conjunction with <strong>the</strong> celebration, <strong>the</strong>annual Charlotte Johnson Barrett Lectureshipwas held on June 5. This year’sguest speaker, Cornelius O. “Skip” GranaiIII, MD, asked, “Are commonly heldbeliefs—dogs bark, cats meow, birds livein <strong>the</strong> sky—and unquestioned answersalways fact?” Dr. Granai believes that patientscount on doc<strong>to</strong>rs <strong>to</strong> hold a certainplace in <strong>the</strong>ir lives. “Perceived for Birds”explored <strong>the</strong> needs of patients and physiciansand <strong>the</strong> vital relationship between<strong>the</strong> two. In addition <strong>to</strong> <strong>the</strong> noon lecture,Dr. Granai met with oncology staff on<strong>the</strong> fourth floor of Hoblitzelle Hospital,<strong>the</strong> sixth floor of Roberts Hospital, and<strong>the</strong> Blood and Marrow Transplant Unit.Waldenström’s MacroglobulinemiaProgramThe Cvetko Center hosted a specialprogram on myeloma and macroglobulinemiaon August 23, 2008, in collaborationwith <strong>the</strong> Leukemia and LymphomaSociety of North Texas. The programfeatured Marvin J. S<strong>to</strong>ne, MD, medicaldirec<strong>to</strong>r of Baylor Sammons <strong>Cancer</strong>Center at Dallas. Dr. S<strong>to</strong>ne presented“Myeloma and Macroglobulinemia:Similarities and Differences.” His presentationwas followed by “Update onWaldenström’s Macroglobulinemia andMultiple Myeloma” presented by StevenP. Treon, MD, PhD, program direc<strong>to</strong>rfor <strong>the</strong> Bing Center for Waldenström’sResearch at Dana-Farber <strong>Cancer</strong> Institutein Bos<strong>to</strong>n. The program was attended bymore than 50 people, including membersof <strong>the</strong> Waldenström’s MacroglobulinemiaSupport Group and <strong>the</strong> North TexasMyeloma Support Group.At <strong>the</strong> Barrett Lectureship, left <strong>to</strong> right:speaker Skip Granai III, MD, C. Allen Stringer,Jr., MD, and Marvin J. S<strong>to</strong>ne, MD.12 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Neil Senzer, MD, and C. Allen Stringer, Jr.,MD, at <strong>the</strong> Ovarian <strong>Cancer</strong> SurvivorCelebration.Survivor Celebrations for Ovarian<strong>Cancer</strong> and Breast <strong>Cancer</strong>On September 22, 2008, <strong>the</strong> centerhosted <strong>the</strong> Second Annual Ovarian <strong>Cancer</strong>Survivor Celebration. The celebrationincluded an update from <strong>the</strong> NationalOvarian <strong>Cancer</strong> Coalition and a presentationby Neil Senzer, MD, entitled“Current Ovarian <strong>Cancer</strong> Research.”The presentation was followed by lunchfor <strong>the</strong> more than 160 people present.The First Annual Breast <strong>Cancer</strong> SurvivorCelebration was held on Oc<strong>to</strong>ber 14,2008. Ebony Steele, nationally knownsyndicated radio host and breast cancersurvivor, shared her experience withbreast cancer and emceed <strong>the</strong> event.John Pippen, MD, was <strong>the</strong> featuredspeaker with his presentation, “ExcitingNew Targeted Therapies for Breast<strong>Cancer</strong>.” The event drew more than 140participants.Complementary <strong>Care</strong> WorkshopAgain this year, <strong>the</strong> Cvetko Center and<strong>the</strong> Healing Environment at BaylorUniversity Medical Center presented“Complementary Methods for Healthand Relaxation,” a half-day workshopfor oncology patients, families, andprofessionals. The event was held onNovember 15, 2008, with Mark A.Casanova, MD, giving <strong>the</strong> keynoteaddress, “Enhancing Quality of LifeFocusing on <strong>the</strong> Whole Person.” Breakoutsessions covered art, <strong>to</strong>uch <strong>the</strong>rapies,Tai Chi, Qigong, and organic versusnatural foods. Almost 100 peopleattended this year’s program.Promoting Prevention and<strong>Cancer</strong> ScreeningsBaylor Dallas hosted a community prostatecancer screening on September 20,2008. The free screening was for men50 years and older and men 40 and olderin high-risk groups (African Americans,Hispanics, and those with a family his<strong>to</strong>ryof prostate cancer). Of <strong>the</strong> 271 menscreened, 10% had abnormal prostatespecificantigen levels.Ebony Steele, Pam Carnevale, MHSA, manager of <strong>the</strong> Cvetko Center, and John Pippen, MD,enjoying <strong>the</strong> Breast <strong>Cancer</strong> Survivor Celebration.It’s a Guy Thing, a morning devotedsolely <strong>to</strong> men’s health, was on Saturday,June 7, 2008. The free event drew morethan 125 attendees from <strong>the</strong> community.Baylor Dallas also served as a host site fora free community melanoma/skin cancerscreening on May 10, 2008. Among <strong>the</strong>222 people who were screened, physiciansfound three cases of melanoma,15 cases of basal cell carcinoma, and sixcases of squamous cell carcinoma.Kitchens Lectureship: Musicand <strong>the</strong> MindOn March 18, 2008, Dr. Richard Kogangave <strong>the</strong> Lloyd Wade Kitchens Lecture atinternal medicine grand rounds. The titleof Dr. Kogan’s presentation was “Musicand <strong>the</strong> Mind: George Gershwin.” Dr.Kogan has had an active career both as aconcert pianist and psychiatrist. He hasbeen praised for his “exquisite playing”by <strong>the</strong> New York Times. He won firstprize in <strong>the</strong> Chopin Competition of<strong>the</strong> Kosciuszko Foundation and hasperformed throughout <strong>the</strong> world asa recitalist and orchestral soloist. Dr.Kogan is a graduate of Juilliard Pre-College, Harvard College, and HarvardMedical School. He is affiliated withWeill-Cornell Medical School as direc<strong>to</strong>rof its Human Sexuality Program.The lecture was given in memory of Dr.Kitchens, who remained at Baylor forhis entire career, practicing with TexasOncology, PA. Dr. Kitchens also servedas medical direc<strong>to</strong>r of <strong>the</strong> Virginia R.Cvetko Patient Education Center from1980 until his death in 2001. He wasan accomplished pianist, and GeorgeGershwin was one of his favoritecomposers.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 13
Profile: Andrew JankeWorking with <strong>the</strong> Cvek<strong>to</strong>Center <strong>to</strong> Help <strong>Cancer</strong>SurvivorsThe impact of a cancer diagnosis on one’ssoul never goes away. Andrew Janke, a27-year-old Dallasite and a testicularcancer survivor, has discovered this firsthand. He’s determined <strong>to</strong> help o<strong>the</strong>rs whohave successfully gone through cancertreatment find answers <strong>to</strong> <strong>the</strong>ir questionsand form a cancer survivor’s network.When he was 23, Mr. Janke discovered asuspicious lump on his testicle. His primarycare physician immediately referredhim <strong>to</strong> a urologist on <strong>the</strong> medical staffat Baylor University Medical Center atDallas. “After my appointment,” Mr.Janke said, “I really had no reaction.I went <strong>to</strong> work and sat in <strong>the</strong> parkinggarage for 15 minutes thinking, ‘Hedidn’t just say that I have cancer, did he?’”Mr. Janke underwent a radical inguinalorchiec<strong>to</strong>my, a procedure <strong>to</strong> remove <strong>the</strong>entire testicle, 3 days after his diagnosisby <strong>the</strong> urologist. A biopsy of <strong>the</strong> tissue <strong>to</strong>verify <strong>the</strong> type of testicular cancer helped14 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
determine a follow-up treatment plan. “Within 2 weeks of my initial operation,” saidMr. Janke, “I underwent <strong>the</strong> first of four rounds of chemo<strong>the</strong>rapy.”During his chemo<strong>the</strong>rapy treatments, his girlfriend—now fiancée—and family andfriends were all <strong>the</strong>re <strong>to</strong> support him. His bro<strong>the</strong>r moved in <strong>to</strong> help him with everydaychores, and his parents, who live in Tennessee, rotated visits. “My folks wouldcome when my chemo treatments were <strong>the</strong> heaviest. It was so nice <strong>to</strong> know someonewas at my apartment, that I wasn’t alone,” he remembered.Following his chemo<strong>the</strong>rapy treatment, a successful second operation <strong>to</strong>ok placebecause <strong>the</strong> cancer had spread <strong>to</strong> his lymph nodes. Six months after being diagnosed,he began <strong>to</strong> recover. “The tests show I’m cancer free now,” said Mr. Janke. But somehow,Mr. Janke can’t quite believe, deep in his soul, that that’s truly <strong>the</strong> case.address <strong>the</strong>ir fear of recurrence, psychosocial issues, long-time side effects, and qualityof life issues,” explained Pam Carnevale, Cvetko Center manager. “Physicians,social workers, dietitians, and chaplains will all take active roles in this program <strong>to</strong>help develop a cancer survivor’s network.”To help with funding <strong>to</strong> get <strong>the</strong> program off <strong>the</strong> ground, Mr. Janke organized alocal car show with <strong>the</strong> proceeds going <strong>to</strong> <strong>the</strong> Cvetko Center. “I’ve always enjoyedanything with four wheels,” laughed Mr. Janke. “I’ve always been a big Chevy fan.”With help from local vendors, he registered 30 cars for his car show, which wascarefully timed <strong>to</strong> coincide with National <strong>Cancer</strong> Survivor’s Day in June 2008.While he’s required <strong>to</strong> have frequent checkups for <strong>the</strong> rest of his life, he’s found thatmuch of <strong>the</strong> support network he had when he was going through treatment is nolonger <strong>the</strong>re. “Once I finished my second operation and was back on my feet, noone mentioned ‘it’ anymore,” he commented. “I felt like people heard I’m ‘cancerfree’and thought, ‘Okay, it’s no longer a big deal.’” What Mr. Janke wants people <strong>to</strong>understand is that even though someone is determined by physicians <strong>to</strong> be “cancerfree,”it is still a very big deal. “There are all sorts of side effects that come about aftercancer treatment,” he said. “Three years later I still have a lot of questions: Is thisnormal? Does this mean <strong>the</strong> cancer is coming back? There are always questions thatcrop up.”To help himself and o<strong>the</strong>rs like him deal with <strong>the</strong> issues and questions that face survivorsof cancer, Mr. Janke volunteered <strong>to</strong> work with <strong>the</strong> Virginia R. Cvetko PatientEducation Center at Baylor Dallas <strong>to</strong> develop a transition program called Life After<strong>Cancer</strong>. “This program will help people who’ve gone through cancer treatmentAndrew Janke, left, with Cvetko Center and event staff at <strong>the</strong> car show organized <strong>to</strong> raisemoney for <strong>the</strong> Life After <strong>Cancer</strong> program.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 15
<strong>Building</strong> <strong>Hope</strong> Through Quality Improvement EffortsCommission on <strong>Cancer</strong> AccreditationIn 2008, <strong>the</strong> Baylor Charles A. Sammons <strong>Cancer</strong> Center received renewal of accreditationfrom <strong>the</strong> Commission on <strong>Cancer</strong>. The Teaching Hospital <strong>Cancer</strong> Program atBaylor Dallas was awarded approval with commendation for <strong>the</strong> next 3 years. Thereare 36 standards in <strong>the</strong> accreditation process, of which nine are eligible for a commendationrating. Baylor received seven commendations on <strong>the</strong> survey.Approximately one-fourth of <strong>the</strong> nation’s hospitals treating cancer patients receiveCommission on <strong>Cancer</strong> approval. Only 31% of teaching hospital cancer programsreceive approval without contingencies.<strong>Cancer</strong> Registry UpdateBy Laura Siciliano, RN, OCNThe year 2008 was one of achievementas well as growth and development for<strong>the</strong> Baylor University Medical Center<strong>Cancer</strong> Registry. The registry staff grewin 2008 with <strong>the</strong> addition of DeliaMoncada, CTR, cancer registry supervisor,and registrars Lydia Vega, CTR,Elizabeth Teter, RHIA, and AliciaMoreno, RN, CTR. Two members ofour staff, Takisha Brown and Gary Vogt,were successful in obtaining credentialingas certified tumor registrars.The goals of <strong>the</strong> cancer registry focuson accuracy and efficiency of data collection,abstracting, casefinding, andfollow-up. The priority goals achievedin 2008 were abstracting data within 5months of date of initial patient contact,increasing and maintaining follow-uppercentages above <strong>the</strong> required Commissionon <strong>Cancer</strong> standards, and submittingerror-free data <strong>to</strong> <strong>the</strong> National<strong>Cancer</strong> Data Base’s Annual Call for Datafor <strong>the</strong> years 2002 and 2007 prior <strong>to</strong> <strong>the</strong>November 4 deadline.The registry continues <strong>to</strong> facilitate andparticipate in <strong>the</strong> Hospital RegistryWebinar Educational Series conductedby <strong>the</strong> North American Association ofCentral <strong>Cancer</strong> Registries. In addition,two registry staff members attended <strong>the</strong>annual Texas Tumor Registrars Associationeducational conference in SanAn<strong>to</strong>nio. A monthly physician-driven“lunch and learn” program has beenimplemented <strong>to</strong> meet <strong>the</strong> needs of<strong>the</strong> cancer registrar in answering keysite-specific questions. The kickoff ofthis program began with Dr. GrangerScruggs, who guided staff memberson a <strong>to</strong>ur of <strong>the</strong> radiation oncologydepartment followed by a review of<strong>the</strong> charting process, which led <strong>to</strong> anunderstanding of <strong>the</strong> intricacies of <strong>the</strong>radiation treatment planning and deliveryprocesses.In Oc<strong>to</strong>ber 2008, Baylor Sammons<strong>Cancer</strong> Center hosted its seventhannual Regional <strong>Cancer</strong> Registry EducationalConference entitled “Value ofQuality Data: Focus on Head and Neckand Central Nervous System <strong>Cancer</strong>s.”Over 60 cancer registrars from around<strong>the</strong> state attended <strong>the</strong> all-day sessionfeaturing physicians on <strong>the</strong> medical staffat Baylor as speakers who covered <strong>to</strong>picsfrom diagnosis through treatment of<strong>the</strong>se cancers.Summary of 2007 <strong>Cancer</strong>Registry DataBy R. Pickett Scruggs, MDDuring reporting year 2007, <strong>the</strong> <strong>Cancer</strong>Registry at Baylor University MedicalCenter at Dallas abstracted 3,137 analyticalcases (cases in which patients werefirst diagnosed or initially treated atBaylor Dallas). Females accounted for59% of <strong>the</strong> patients. Data on age andstage are summarized in Figures 1 and 2.The <strong>to</strong>p five sites of diagnosis were similar<strong>to</strong> those of <strong>the</strong> previous year. Theseincluded breast (690), lung (291), colorectal(248), prostate (203), and liver/biliary (152). Comparing 2007 datawith 2006 data showed that colorectal,prostate, and liver/biliary cases remainedvery similar in number. The numberof breast cases increased by 87 (14%).Contributing <strong>to</strong> this increase was <strong>the</strong>relocation of <strong>the</strong> breast imaging center<strong>to</strong> a new location on <strong>the</strong> Baylor Dallascampus. The Darlene G. Cass Women’sImaging Center is larger and more easilyaccessible <strong>to</strong> patients. In addition, BaylorDallas began operating a full-service16 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Figure 1. Age by Gender of 3,137 Analytic Cases90–9980–8970–7960–6950–5940–4930–3920–2910–190–90% 2% 4% 6% 8% 10% 12% 14% 16%FemaleMalebreast imaging center in North Dallas.Baylor Dallas has a well-known and veryactive medical and surgical digestivedisease service, which contributed <strong>to</strong>an increase of more than 100% in <strong>the</strong>number of esophageal cancers reported.Baylor Dallas is in Texas Health ServiceRegion 3, with 117 reporting facilitiesin 19 counties. A comparison of BaylorDallas’ 2007 registry data with data onexpected new cases in Region 3 for 2007revealed that Baylor Dallas saw almost13% of all cancers in <strong>the</strong> region. BaylorDallas’ cancer registry reported 46% of<strong>the</strong> new cases of liver, 24% of pancreas,17% of breast, 18% of esophageal, 19%of thyroid, 18% of kidney, and 19% ofgynecologic cancer in <strong>the</strong> region.Baylor Dallas’ <strong>to</strong>p 10 sites are comparedwith estimated new cases from <strong>the</strong>National <strong>Cancer</strong> Data Base in Figure 3.The distribution of cases at Baylor Dallasis similar <strong>to</strong> <strong>the</strong> national distribution,with <strong>the</strong> exception of prostate, lung, andbladder cancers, which made up a smallerpercentage of overall Baylor Dallas cases,whereas breast, liver, and pancreas cancersmade up a greater percentage of cases.Figure 2. 2007 Analytic Cases by General Stage16001400149312001000800600400537487Figure 3. Baylor Dallas Top 10 Sites Compared <strong>to</strong> National StatisticsBaylor Dallas Top 10 USA National Top 10BreastProstateLungLungColon/RectumBreastProstateColon/RectumLiverBladderPancreasNon-Hodgkin’s Lymphoma2000212In Situ Localized Regional Distant Benign UnknownStage**From SEER: Surveillance, Epidemiology, and End Results Program186227Corpus UteriKidneyNon-Hodgkin’s LymphomaLeukemiaMelanomaKidneyLeukemiaCorpus Uteri<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 17
SexGeneral StagePrimary Site Total Male Female In Situ Local Regional Distant Benign UnknownAll Sites 3137 1297 1840 212 1493 537 487 186 222Baylor UniversityMedical Center at Dallas2007 Analytic CasesHead and Neck 44 32 12 1 15 18 5 1 4Lip 2 2 0 0 0 0 0 0 2Tongue 20 15 5 0 8 10 2 0 0Oropharynx 1 1 0 0 0 0 0 0 1Hypopharynx 2 1 1 0 0 2 0 0 0O<strong>the</strong>r 19 13 6 1 7 6 3 1 1Digestive System 691 421 270 15 319 174 94 12 77Esophagus 41 31 10 5 17 10 3 0 6S<strong>to</strong>mach 46 32 14 1 19 7 8 5 6Colon 136 70 66 1 60 42 22 1 10Rectum 112 60 52 2 55 33 9 0 13Anus/Anal Canal 16 10 6 3 6 3 2 0 2Liver 152 121 31 0 100 22 16 2 12Pancreas 129 67 62 1 42 39 26 1 20O<strong>the</strong>r 59 30 29 2 20 18 8 3 8Respira<strong>to</strong>ry System 310 158 152 2 121 75 89 2 21Nasal/Sinus 2 1 1 0 2 0 0 0 0Larynx 13 9 4 1 3 5 1 0 3Lung/Bronchus 291 145 146 1 112 70 88 2 18O<strong>the</strong>r 4 3 1 0 4 0 0 0 0Bone 14 9 5 0 8 3 2 1 0Connective/Soft Tissue 20 12 8 0 12 5 1 0 2Skin 73 40 33 4 48 11 5 1 4Melanoma 65 34 31 4 43 9 5 0 4O<strong>the</strong>r 8 6 2 0 5 2 0 1 0Breast 690 11 679 139 414 116 14 2 518 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
SexGeneral StagePrimary Site Total Male Female In Situ Local Regional Distant Benign UnknownFemale Genital 283 0 283 20 143 53 42 7 18Cervix Uteri 32 0 32 2 22 5 1 0 2Corpus Uteri 127 0 127 0 85 27 7 1 7Ovary 89 0 89 0 23 19 34 5 8Vulva 28 0 28 15 12 1 0 0 0O<strong>the</strong>r 7 0 7 3 1 1 0 1 1Male Genital 213 213 0 0 168 30 5 0 10Prostate 203 203 0 0 162 28 3 0 10Testis 9 9 0 0 6 2 1 0 0O<strong>the</strong>r 1 1 0 0 0 0 1 0 0Baylor UniversityMedical Center at Dallas2007 Analytic Cases(Continued)Urinary System 175 127 48 31 108 22 10 1 3Bladder 59 45 14 28 23 8 0 0 0Kidney/Renal 113 80 33 2 83 14 10 1 3O<strong>the</strong>r 3 2 1 1 2 0 0 0 0Brain and CNS 149 60 89 0 26 3 3 114 3Brain (Benign) 9 4 5 0 0 0 0 9 0Brain (Malignant) 43 24 19 0 24 3 3 10 3O<strong>the</strong>r 97 32 65 0 2 0 0 95 0Endocrine 107 28 79 0 56 17 3 22 9Thyroid 83 21 62 0 56 17 2 0 8O<strong>the</strong>r 24 7 17 0 0 0 1 22 1Blood and Bone Marrow 156 86 70 0 0 0 156 0 0Leukemia 98 51 47 0 0 0 98 0 0Multiple Myeloma 41 24 17 0 0 0 41 0 0O<strong>the</strong>r 17 11 6 0 0 0 17 0 0Lymphoma 114 63 51 0 39 5 53 0 17Hodgkin’s Disease 8 3 5 0 4 0 4 0 0Non-Hodgkin’s 106 60 46 0 35 5 49 0 17Unknown Primary 77 31 46 0 5 0 4 22 46O<strong>the</strong>r/Ill-Defined 21 6 15 0 11 5 1 1 3<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 19
Patient <strong>Care</strong> EvaluationStudy: 10-Year Experiencewith Prostate Brachy<strong>the</strong>rapyat Baylor Sammons <strong>Cancer</strong>CenterBy Barry N. Wilcox, MD, FACRO,and Janet Reynolds, CTRProstate cancer afflicts one in six menin this country. Approximately 186,320cases will be diagnosed in 2008. Outsideof skin cancer, it is <strong>the</strong> most commoncancer diagnosed in men and <strong>the</strong> secondleading cause of cancer death, behindlung cancer. In 2008, 28,660 men willdie of this disease, accounting for 10%of all cancer-related deaths in men. 1Patients with prostate cancer have avariety of treatment options available<strong>to</strong> <strong>the</strong>m, especially if <strong>the</strong>y have earlydisease. The choices are watchful waiting(primarily in selected older patients orthose with significant health problems),surgery, and radiation. New treatments,such as cryo<strong>the</strong>rapy, are being explored;however, long-term follow-up data arelimited.Dr. Barry Wilcox and Janet ReynoldsProstatec<strong>to</strong>my is <strong>the</strong> definitive surgicaloption. It can be done in several ways:radical retropubic prostatec<strong>to</strong>my, radicalperineal prostatec<strong>to</strong>my, laparoscopicradical prostatec<strong>to</strong>my, or robotic-assistedlaparoscopic radical prostatec<strong>to</strong>my.Radiation <strong>the</strong>rapy can be administeredusing ei<strong>the</strong>r external beam radiation orbrachy<strong>the</strong>rapy (internal radiation) and,in certain circumstances, as a combinationof both. When used appropriately,all three approaches are effective.External beam radiation can be deliveredby a number of different techniques:three-dimensional conformal radiation<strong>the</strong>rapy (<strong>the</strong> planned dose conforms<strong>to</strong> a tumor with a convex surface);intensity-modulated radiation <strong>the</strong>rapy(<strong>the</strong> planned dose conforms <strong>to</strong> a tumorwith a concave component <strong>to</strong> its surface,e.g., <strong>the</strong> interface of <strong>the</strong> prostate with <strong>the</strong>rectum); image-guided radiation <strong>the</strong>rapy(using <strong>the</strong> previous techniques withdaily visualization of <strong>the</strong> prostate <strong>to</strong>more accurately track organ movement);stereotactic body radiation <strong>the</strong>rapy(delivering a smaller number of high-dosetreatments requiring image guidance);or conformal pro<strong>to</strong>n beam radiation<strong>the</strong>rapy (minimizing radiation <strong>to</strong>surrounding organs).Brachy<strong>the</strong>rapy is radiation given withinor next <strong>to</strong> <strong>the</strong> tumor from an internalsource ra<strong>the</strong>r than from an externalsource. Arguably, despite all <strong>the</strong> advancesin external beam technology, this represents<strong>the</strong> most conformal way <strong>to</strong> deliverradiation <strong>to</strong> <strong>the</strong> prostate. It can bedone using permanent implantation ofinterstitial seeds (using I-125 or Pd-103)or temporary implantation of high-20 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
dose-rate seeds (using Ir-192). Whenused as a single modality treatment,<strong>the</strong>re are restricted stage- and pathologydependentcriteria of applicability.The Baylor Brachy<strong>the</strong>rapyExperienceBaylor University Medical Center atDallas was one of <strong>the</strong> first cancer centersin Nor<strong>the</strong>ast Texas <strong>to</strong> offer prostatebrachy<strong>the</strong>rapy beginning in February1997. As a consequence, a significantclinical experience with <strong>the</strong> procedurehas developed. The 400 patients treatedover this decade have a 5.5-year medianfollow-up. All <strong>the</strong> cases were done ei<strong>the</strong>rby Neil Senzer, MD, or Barry Wilcox,MD, collaborating with a urologist on<strong>the</strong> Baylor Dallas medical staff. WhileI-125 was <strong>the</strong> preferred iso<strong>to</strong>pe at ourinstitution, 13% of <strong>the</strong> cases were donewith Pd-103 (based on tumor growthrate selection fac<strong>to</strong>rs) during <strong>the</strong> earlyyears of <strong>the</strong> experience. All patientsoffered implants alone were low risk,defined as patients with a Gleason score≤6, a prostate-specific antigen (PSA)level ≤10, and clinical stage ≤T2b. A fewpatients with Gleason scores of 7 wereallowed <strong>to</strong> have <strong>the</strong> implant alone if<strong>the</strong>ir predominant pathology was grade3 (3+4) ra<strong>the</strong>r than poorly differentiatedgrade 4 (4+3) and if <strong>the</strong>y had minimalunilateral disease on biopsy specimen.Some patients received preimplantationexternal beam radiation of 45 Gray (Gy)<strong>to</strong> <strong>the</strong> pelvis; however, this group ofpatients had intermediate-risk or highriskdisease.The registry data show that <strong>the</strong> medianage at diagnosis and treatment was67 years. Eighty-eight percent of <strong>the</strong>patients were Caucasian, 8% were AfricanAmerican, and 3% were Hispanic.Of <strong>the</strong> 400 patients, 314 (79%) hadbrachy<strong>the</strong>rapy without <strong>the</strong> addition ofsupplemental external beam radiation.The median PSA level was 6.1, and 79%of tumors were ei<strong>the</strong>r well or moderatelydifferentiated (18 were well differentiated,299 were moderately differentiated,and 83 were poorly differentiated).Thirty-five percent of patients receiveda short-term (mean, 4 months) courseof androgen blockade, usually <strong>to</strong> shrink<strong>the</strong> gland below 60 cc but sometimes <strong>to</strong>defer treatment for o<strong>the</strong>r reasons, such asallowing time for a treatment decision,waiting for iso<strong>to</strong>pe availability, or travel.The average-size gland at implant was 38cc, and <strong>the</strong> median target dose was 145Gy for I-125 and 115 Gy for Pd-103.Those who received external beam radiationwere <strong>the</strong>n implanted with I-125 <strong>to</strong>a dose of 110 Gy.Our technique included a pubic archand ultrasound volume study from whicha dosimetric preplan was rendered. Over<strong>the</strong> ensuing decade, various incrementalimprovements were adopted as technologicadvances permitted. These includedcomputer preoperative dosimetry,pos<strong>to</strong>perative dosimetry (day of <strong>the</strong>procedure), conversion from an analogue<strong>to</strong> digital transducer, and use of strandedseed sources ra<strong>the</strong>r than loose seeds.ResultsSurvival. The actuarial survival rate for<strong>the</strong> 400 patients treated at <strong>the</strong> BaylorSammons <strong>Cancer</strong> Center with brachy<strong>the</strong>rapyis shown in Figure 1. Thedisease-specific survival for <strong>the</strong>se patientswas 99%, with only four of 400 patientsexpiring from <strong>the</strong>ir disease, while a fifthpatient with active prostate cancer expiredsecondary <strong>to</strong> lung cancer (Table 1).Figure 1. Baylor Dallas Observed (Actuarial) 5-Year Survival in Stage IIProstate <strong>Cancer</strong> Patients Treated with Brachy<strong>the</strong>rapy100%90%80%70%60%50%40%30%20%10%0%Diagnosis 1 Year 2 Years 3 Years 4 Years 5 Years<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 21
Table 1. 5-Year Status of 400 Patientswith Prostate <strong>Cancer</strong> Treated withBrachy<strong>the</strong>rapyEvidence ofStatus Prostate <strong>Cancer</strong> No. (%)Alive No 349 (87%)Yes 5 (1%)Died No 39 (10%)Yes 5 (1%)Unknown 2 (0.5%)Table 2. Recurrences Occurring1–10 Years after Brachy<strong>the</strong>rapy forProstate <strong>Cancer</strong> in 400 PatientsRecurrence No. (%)None 385 (96%)Local 5 (1%)Biochemical 5 (1%)Distant Metastasis 5 (1%)Using statistical extrapolation, <strong>the</strong>projected 10-year actuarial survival ratewas 90%. Fur<strong>the</strong>r analysis of <strong>the</strong> recurrencesat Baylor Dallas suggested tha<strong>to</strong>nly 1.5% <strong>to</strong> 2.5% had local-only recurrences,which confirms excellent localcontrol of this disease with this technique(Table 2). Our rate of a transientPSA rise after implantation, what isreferred <strong>to</strong> as “PSA bounce,” was 3%.This rate is lower than that reported insome series and can probably be attributed<strong>to</strong> our older patient population.Side effects and complications. Sideeffects from radiation are well documentedand, with <strong>the</strong> exception offatigue, are confined <strong>to</strong> <strong>the</strong> pelvic area.This is a consequence of bladder andrectal irritation. All of our patients experiencedgrade 1 <strong>to</strong> 2 urinary and rectalsymp<strong>to</strong>ms. These symp<strong>to</strong>ms generallylasted 4 <strong>to</strong> 6 months after implantation.Late urinary complications such as persisten<strong>to</strong>bstruction or retention (grade 3) 2from brachy<strong>the</strong>rapy occurred in 4% of<strong>the</strong> patients. There were no grade 4 complications.Of <strong>the</strong> 13 patients afflicted,a transurethral resection of <strong>the</strong> prostate(TURP) was required in 11, while 2patients required prolonged use of anindwelling Foley ca<strong>the</strong>ter or intermittentself-ca<strong>the</strong>terization. Two patients becameincontinent after <strong>the</strong> TURP procedure,which is consistent with <strong>the</strong> 18% <strong>to</strong> 25%risk 3 in published reports. Of <strong>the</strong> twopatients who had ca<strong>the</strong>terizations ra<strong>the</strong>rthan TURP, one was able <strong>to</strong> regain continencethrough bladder training, while<strong>the</strong> o<strong>the</strong>r did not. In <strong>to</strong>tal, only threepatients experienced permanent urinaryincontinence—a rate of 0.75%.Grade 3 rectal complications, which canmanifest in persistent or recurrent bleedingrequiring surgical correction, are alsoa concern for anyone contemplatingprostate brachy<strong>the</strong>rapy. In our series,such complications occurred in only fourpatients (1%). This percentage is belowthat of some published studies, whichshow a rate of 5% <strong>to</strong> 11%. 4,5 No grade 4complications (fistulas/colos<strong>to</strong>my) werereported.The rate of potency preservation,unfortunately, was not consistentlydocumented prior <strong>to</strong> or following implantation,but his<strong>to</strong>rically it has beenabout 50% <strong>to</strong> 80% depending on whichseries is being reported. These numbersare often subject <strong>to</strong> patient selection bias(potent patients gravitate <strong>to</strong>ward physiciansthat publish good numbers) andage bias (not actuarially adjusted <strong>to</strong> <strong>the</strong>natural decline in potency that occurswith aging). Fur<strong>the</strong>r complicating collectionof this data is <strong>the</strong> fact that manyTable 3. Subsequent <strong>Cancer</strong>s Occurring1–10 Years after Brachy<strong>the</strong>rapy forProstate <strong>Cancer</strong> in 400 Patients<strong>Cancer</strong> TypeNo.Bladder 3Colon/rectum 3Kidney 1Leukemia 2Lung 3Melanoma 1Oral cavity 1Pancreas 1S<strong>to</strong>mach 1older patients refuse <strong>to</strong> answer <strong>the</strong>sequestions or answer <strong>the</strong>m inconsistentlydepending on who is present with <strong>the</strong>min <strong>the</strong> room.Risk of radiation-induced cancer.Much is known about complicationsrelated <strong>to</strong> rectal bleeding; less is knownabout <strong>the</strong> risks of inducing a secondarycancer from radiation. Table 3 documentssome of <strong>the</strong> subsequent cancers that havedeveloped in this group of patients.It has been postulated that someonewho has developed one cancer may bepredisposed genetically or from exposurehis<strong>to</strong>ry <strong>to</strong> developing o<strong>the</strong>r cancers.Many cancers share similar risk fac<strong>to</strong>rs.22 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
It is also well documented that ionizingradiation can induce some cancers years<strong>to</strong> decades later. Our own data showfour cancers found in <strong>the</strong> pelvic area,which include three bladder cancers andone rectal cancer. Since <strong>the</strong> minimumtime requirement for attributing an inducedcancer <strong>to</strong> radiation is 5 years afterradiation exposure, only one case wouldsatisfy <strong>the</strong> time requirement (a bladdercancer) and be reasonably attributed <strong>to</strong>radiation treatment due <strong>to</strong> its location.This translates in<strong>to</strong> a risk of 1 in 400.Given <strong>the</strong> prevalence of bladder cancersin men of this age group, this may possiblyoverestimate <strong>the</strong> risk.Comparison of Resultswith National BenchmarksWe compared <strong>the</strong> results of our experiencewith stage II prostate cancertreatment <strong>to</strong> that of <strong>the</strong> large National<strong>Cancer</strong> Data Base (NCDB) for prostatecancer survival. NCDB, a joint programof <strong>the</strong> Commission on <strong>Cancer</strong> and <strong>the</strong>American <strong>Cancer</strong> Society, is a nationwideoncology outcomes database formore than 1,400 Commission-approvedcancer programs in <strong>the</strong> United Statesand Puer<strong>to</strong> Rico. Some 75% of all newlydiagnosed cases of cancer in <strong>the</strong> UnitedStates are captured at <strong>the</strong> institutionallevel and reported <strong>to</strong> <strong>the</strong> NCDB. TheNCDB data show a 5-year observed(actuarial) survival rate of 89% nationally6 (Figure 2) compared with 91% forour brachy<strong>the</strong>rapy patients (Figure 1).ConclusionOur results in treating prostate cancerwith brachy<strong>the</strong>rapy compare wellwith those of <strong>the</strong> 1,400 Commissionapprovedcancer programs reporting <strong>to</strong><strong>the</strong> NCDB registry. Baylor Sammons<strong>Cancer</strong> Center has achieved an experienceunique <strong>to</strong> <strong>the</strong> Nor<strong>the</strong>ast Texas areain its volume, duration, and follow-up.The results reaffirm <strong>the</strong> effectivenessof brachy<strong>the</strong>rapy, <strong>the</strong> appropriatenessof selection criteria, and <strong>the</strong> qualityof application as practiced at BaylorSammons <strong>Cancer</strong> Center. In <strong>the</strong> future,our experience will continue <strong>to</strong> provideinsight on <strong>the</strong> long-term results of <strong>the</strong>procedure as well as elucidate how <strong>the</strong>continual incremental improvementsthat have been adopted impact outcomes.A good cancer registry is essentialFigure 2. NCDB Prostate <strong>Cancer</strong> Observed (Actuarial) Survival by Stage100%90%80%70%60%50%40%30%20%10%0%Diagnosis 1 Year 2 Years 3 Years 4 Years 5 YearsStage I Stage II Stage III Stage IVn=11,863 n=268,174 n=33,037 n=20,493for an advanced cancer center andenormously beneficial in helping <strong>to</strong>determine where opportunities forimprovement lie. It is also invaluable incompiling national trends and statisticsand serves as a benchmark for comparisonof a cancer center’s results with thoseof o<strong>the</strong>r accredited centers throughout<strong>the</strong> nation. 7AcknowledgmentsWe would like <strong>to</strong> thank Dr. Neil Senzerfor his valuable input and acknowledgehis efforts in starting <strong>the</strong> brachy<strong>the</strong>rapyprogram at Baylor Dallas. Also, we expressour gratitude <strong>to</strong> Joshua Fine, MD, JohnWare, MD, Michael Goldstein, MD,Myron Fine, MD, George Hurt, MD,James Sandin, MD, Bob Schoenvogel,MD, Ben Schnitzer, MD, and SteveFrost, MD, along with <strong>the</strong> many o<strong>the</strong>rurologists and internists who referred<strong>the</strong>ir patients <strong>to</strong> our center and providedfollow-up information for this project.Finally, we want <strong>to</strong> thank our dedicatedbrachy<strong>the</strong>rapy nurses, Carol Motley, RN,and Robin Wilks, RN, for <strong>the</strong>ir professionalismand selfless dedication.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 23
Notes1. American <strong>Cancer</strong> Society. <strong>Cancer</strong> Facts &Figures 2008. Atlanta, GA: American <strong>Cancer</strong>Society, 2008.2. All <strong>to</strong>xicities are expressed using <strong>the</strong> RadiationTherapy Oncology Group/EuropeanOrganisation for Research and Treatment of<strong>Cancer</strong> Late Radiation Morbidity ScoringScheme.3. Kollmeier MA, S<strong>to</strong>ck RG, Cesaretti J, S<strong>to</strong>neNN. Urinary morbidity and incontinencefollowing transurethral resection of <strong>the</strong>prostate after brachy<strong>the</strong>rapy. J Urol 2005;173(3):808–812.4. Mueller A, Wallner K, Merrick G, Ford E,Sutlief S, Cavanagh W, Butler W. Perirectalseeds as a risk fac<strong>to</strong>r for prostate brachy<strong>the</strong>rapy-relatedrectal bleeding. Int J RadiatOncol Biol Phys 2004;59(4):1047–1052.5. Kao J, S<strong>to</strong>ne NN, Lavaf A, Dumane V,Cesaretti JA, S<strong>to</strong>ck RG. 125 I mono<strong>the</strong>rapyusing D90 implant doses of 180 Gyor greater. Int J Radiat Oncol Biol Phys2008;70(1):96–101.6. American College of Surgeons. National<strong>Cancer</strong> Data Base/Commission on <strong>Cancer</strong>Survival Reports. Chicago: ACS, 2008.7. Our experience with brachy<strong>the</strong>rapy alone(i.e., without external beam radiation) comparedwith <strong>the</strong> results of published data frommajor brachy<strong>the</strong>rapy cancer canters willbe <strong>the</strong> subject of a future publication since<strong>the</strong> Commission on <strong>Cancer</strong> accreditationprocess requires comparison of site-specificresults of our cancer center with results fromNCDB.Future Developments for Prostate <strong>Cancer</strong> at SammonsThe Baylor Sammons <strong>Cancer</strong> Center, along with <strong>the</strong> Mary Crowley <strong>Cancer</strong>Research Center, Texas Oncology, US Oncology, and <strong>the</strong> National <strong>Cancer</strong>Institute, offer a number of pro<strong>to</strong>cols for prostate cancer. Clinical trials havecontinued <strong>to</strong> evolve based on new insights and technologies. Given that <strong>the</strong>cure rate for low-risk prostate cancer patients treated with radiation or surgeryis above 80% at 10 years and that prostate cancer typically afflicts men in <strong>the</strong>iradvanced years, most, but not all, of <strong>the</strong> new and innovative studies tend <strong>to</strong>focus on intermediate-risk or high-risk patients, patients who have metastaticdisease at presentation, or patients in whom conventional treatment has failed.As a result, exploring new or innovative treatments for low-risk prostate cancerpatients poses an ethical dilemma. Is it reasonable or even ethical, for example,<strong>to</strong> try something novel and unconventional when well-established, relatively safetreatments that are highly effective are available? This is really for <strong>the</strong> patient <strong>to</strong>determine.Patients who want <strong>to</strong> try a new approach or explore adding a new adjunctive<strong>the</strong>rapy <strong>to</strong> <strong>the</strong> more established treatments have choices at Baylor Sammons<strong>Cancer</strong> Center. For example, stereotactic body radiation <strong>the</strong>rapy is now beingoffered <strong>to</strong> patients with early stage disease. In this approach, patients are givenfive high-dose fractions of very precisely focused radiation ra<strong>the</strong>r than <strong>the</strong> typical8- <strong>to</strong> 9-week daily course of treatment. Early data suggest that stereotactic bodyradiation <strong>the</strong>rapy may be as effective as standard radiation <strong>the</strong>rapy and haveacceptable side effects. O<strong>the</strong>r improvements in <strong>the</strong> treatment of prostate cancerwith radiation will take place as we increase our understanding of preservationof erectile function, determine who has micrometastatic disease at presentation,and improve our imaging and increase our dose conformality with <strong>the</strong> implementationof “dose painting.”24 Baylor Charles A. Sammons <strong>Cancer</strong> Center at DallasAdjuvant treatments—such as giving radiation with selenium, celecoxib, docetaxel,or a vaccine—are currently being studied in clinical trials. In addition,investigational drugs, such as abiraterone acetate, have shown favorable results inmetastatic prostate cancer and are now being considered for study in earlier-stagedisease.
<strong>Building</strong> <strong>Hope</strong> Through ResearchPersonalized MedicineThe Center for Personalized Medicine,which began in 2001 and is ledby Damien Chaussabel, PhD, brings<strong>to</strong>ge<strong>the</strong>r modern blood banking technology,novel genome analysis, and advanceddata mining <strong>to</strong>ols. From one small tubeof blood, Dr. Chaussabel’s group canmeasure <strong>the</strong> expression level of 48,000different gene transcripts.What began as an ambitious plan hasdeveloped in<strong>to</strong> an international programin which scientists and physicians fromBaylor Health <strong>Care</strong> System collaborateon studies with <strong>the</strong>ir peers from around<strong>the</strong> globe.Not only can this research help diagnosediseases, but it also can be used <strong>to</strong> see ifa patient is responding <strong>to</strong> <strong>the</strong>rapy andmedication. “We have made tremendousprogress over <strong>the</strong> last 7 years in identifying<strong>the</strong> unique ‘signatures’ of manydiseases and translating this informationin<strong>to</strong> useful clinical data,” explainedJacques Banchereau, PhD, direc<strong>to</strong>r of<strong>the</strong> Baylor Institute for ImmunologyResearch. “By knowing <strong>the</strong> signatureof a specific illness and what a healthysignature should be, we can moni<strong>to</strong>r <strong>the</strong>effectiveness of a treatment plan.”Therapeutic <strong>Cancer</strong> VaccinesBaylor Research Institute and <strong>the</strong> MountSinai School of Medicine are collaborating<strong>to</strong> develop <strong>the</strong>rapeutic cancer vaccinesfor patients with lymphoma andmyeloma. Additionally, <strong>the</strong> researcherswill investigate ways <strong>to</strong> better diagnoseau<strong>to</strong>immune disorders such as arthritisand lupus.Unlike traditional vaccines used <strong>to</strong>prevent diseases, <strong>the</strong> <strong>the</strong>rapeutic vaccinesbeing created by Baylor Research Instituteand Mount Sinai will be designed aspersonalized cancer treatments using cellsfrom <strong>the</strong> patient’s own immune system.To develop <strong>the</strong> vaccines, Baylor researcherswill cultivate dendritic cells, a class ofwhite blood cells that initiate and control<strong>the</strong> body’s overall immune responseagainst foreign invaders, and manipulate<strong>the</strong>m <strong>to</strong> attack <strong>the</strong> cancer. BaylorInstitute for Immunology Research hasmade significant advances in <strong>the</strong> studyof dendritic cells. It is currently applyingthis technique <strong>to</strong> develop and test vaccinesfor o<strong>the</strong>r diseases, such as malignantmelanoma, breast cancer, and dangerousinfectious diseases.Early Detection for Lung<strong>Cancer</strong>The Baylor Sammons Lung <strong>Cancer</strong>Center has joined <strong>the</strong> InternationalEarly Lung <strong>Cancer</strong> Action Program, agroup of lung cancer experts dedicated <strong>to</strong>achieving early diagnosis, treatment, andeventual cure of lung cancer.Richard Wood,MD, medicaldirec<strong>to</strong>r of <strong>the</strong>Baylor SammonsLung <strong>Cancer</strong> Centerand a physicianon <strong>the</strong> medicalstaff at BaylorDr. Richard WoodDallas, said this is asignificant step <strong>to</strong> establish early detectionthrough low-dose computed <strong>to</strong>mography(CT) screening as an accepted practice.“We’re trying <strong>to</strong> move <strong>the</strong> paradigm<strong>to</strong>ward earlier detection of lung cancer,instead of waiting until a patient presentswith symp<strong>to</strong>ms of <strong>the</strong> disease,” Dr. Woodsaid. “The key is <strong>to</strong> find <strong>the</strong> people whoare asymp<strong>to</strong>matic. Patients who havesmoked 20 years or more or who havehad heavy exposure <strong>to</strong> second-handsmoke or occupational exposure <strong>to</strong>asbes<strong>to</strong>s, beryllium, uranium, or radonare primary candidates.”The Baylor Sammons Lung <strong>Cancer</strong>Center started enrolling patients for thisstudy in 2008. CT scans are provided ata reduced cost <strong>to</strong> high-risk patients, and<strong>the</strong> center is tracking <strong>the</strong> results.“While CT screening for lung canceris still considered experimental, we aredocumenting our findings and will continue<strong>to</strong> push for insurance companies <strong>to</strong>cover <strong>the</strong> cost,” Dr. Wood said.Aquatic Exercise for Breast<strong>Cancer</strong> PatientsBaylor’s commitment <strong>to</strong> research forpatients does not end in <strong>the</strong> labora<strong>to</strong>ry.A study led by Michael Grant, MD,examines <strong>the</strong> potential effectiveness ofaquatic exercise <strong>the</strong>rapy for breast cancerpatients suffering from lymphedema, a<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 25
Site Tumor Conference Case ReportsBy Marvin J. S<strong>to</strong>ne, MDWhen <strong>the</strong> Baylor Charles A. Sammons <strong>Cancer</strong> Center opened on May 1, 1976, one siteconference on gynecologic oncology was already in place. There was also a “tumor board.”Many physicians felt that <strong>the</strong> older concept of a tumor board, where a small group of physiciansheard about patients with a variety of different types of cancer, was outmoded. Newadvances in multidisciplinary and combined-modality approaches created <strong>the</strong> need forseparate committees for <strong>the</strong> major sites. Each site tumor committee in turn was responsiblefor organizing and running a site tumor conference.Back row, left <strong>to</strong> right: Elaine Lagow, RN, BS, CNA, CCRC, Linda Miller, and Nancy Hawkins,RN, MEd, with Carol Cruz, <strong>the</strong> 300th participant in <strong>the</strong> Ovarian Study.condition characterized by inflammationof a limb due <strong>to</strong> an excess collection oftissues and fluids. Approximately 15% <strong>to</strong>20% of breast cancer survivors developlymphedema as a result of <strong>the</strong>ir cancertreatments.The effectiveness of aquatic <strong>the</strong>rapy isbased on <strong>the</strong> idea that water pressurehelps compress <strong>the</strong> swollen limb and aids<strong>the</strong> movement of blood and fluids. Inaddition, water exercises relax muscles,decrease impact on joints, and promotedeep breathing, which collectivelydecrease pain and allow participants <strong>to</strong>have better exercise experiences.Early Detection of Ovarian<strong>Cancer</strong>Baylor Sammons <strong>Cancer</strong> Center is participatingin a multicenter trial focusedon early detection of ovarian cancer inlow-risk women. This 3-year study looksat postmenopausal women aged 50 <strong>to</strong>74 who have at least one ovary and arecancer free, having had no chemo<strong>the</strong>rapyor radiation <strong>the</strong>rapy for at least a year.The goal for <strong>the</strong> Baylor site is <strong>to</strong> accrue600 patients over a 3-year period. Since<strong>the</strong> study started in December 2007,310 women have joined.The site tumor conferences have developed in<strong>to</strong> successful endeavors. Baylor Sammons <strong>Cancer</strong>Center now holds 220 multidisciplinary and educational site-specific conferences each year,with case discussions of about 700 patients. Individual conferences focus on bone and softtissue, breast, chest, skin, head and neck, <strong>the</strong> endocrine system, <strong>the</strong> gastrointestinal system,neurology, urology, gynecology, and hema<strong>to</strong>poietic diseases. Attendance has grown each year <strong>to</strong>more than 6,000 attendees in 2007, including representatives from multiple medical disciplinesas well as fellows, residents, interns, nurses, and allied health professionals. Continuing medicaleducation credit is provided.All conferences are sponsored, planned, and implemented by Baylor Sammons <strong>Cancer</strong> Centersite tumor committees, which report <strong>to</strong> <strong>the</strong> cancer center medical committee. These conferenceshave become <strong>the</strong> “nuts and bolts” of <strong>the</strong> cancer center and oncology activities at Baylor.They directly contribute <strong>to</strong> high-quality patient care and learning at multiple levels.I know of no o<strong>the</strong>r cancer center or institution that conducts a similar scope of regularmultidisciplinary oncology conferences. The success of our conferences is a result of activeparticipation by numerous physicians. These conferences continue <strong>to</strong> thrive because of <strong>the</strong>enthusiasm and devotion <strong>to</strong> clinical excellence of many members of our medical staff.Baylor University Medical Center Proceedings began publishing one case report in eachquarterly issue, starting in April 2008. The first three published cases were as follows:• Adair CF, Preskitt JT, Joyner KL, Dobson RW. Enlarged thyroid gland with normalthyroid function tests. Proc (Bayl Univ Med Cent) 2008;21(2):179–182.• Mittal A, Felter D, Shiller SM, McCollum AD, Lamont JP, Mallat D. Gastrointestinalbleeding and cutaneous nodules. Proc (Bayl Univ Med Cent) 2008;21(3):331–334.• Oh J, Karunanayake M, Stringer CA Jr. Invasive endometrial lesion in a patient withmental retardation. Proc (Bayl Univ Med Cent) 2008;21(4):426–429.26 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
2008 Publications1. Abair T, Card P, O’Shaughnessy J. Highlightsfrom: The 33rd European Society ofMedical Oncology Congress: September2008; S<strong>to</strong>ckholm, Sweden. Clin Breast<strong>Cancer</strong> 2008;8(6):481–486.2. Adair CF, Preskitt JT, Joyner KL, DobsonRW. Enlarged thyroid gland with normalthyroid function tests [site tumor conferencereport]. Proc (Bayl Univ Med Cent)2008;21(2):179–182.3. Albain KS, Nag SM, Calderillo-Ruiz G,Jordaan JP, Llombart AC, Pluzanska A,Rolski J, Melemed AS, Reyes-Vidal JM,Sekhon JS, Simms L, O’Shaughnessy J.Gemcitabine plus paclitaxel versus paclitaxelmono<strong>the</strong>rapy in patients with metastaticbreast cancer and prior anthracycline treatment.J Clin Oncol 2008;26(24):3950–3957.4. An<strong>to</strong>niou AC, Spurdle AB, SinilnikovaOM, Healey S, Pooley KA, Schmutzler RK,Versmold B, Engel C, Meindl A, ArnoldN, Hofmann W, Sutter C, Niederacher D,Deissler H, Caldes T, Kämpjärvi K, NevanlinnaH, Simard J, Beesley J, Chen X; KathleenCuningham Consortium for Researchin<strong>to</strong> Familial Breast <strong>Cancer</strong>, Neuhausen SL,Rebbeck TR, Wagner T, Lynch HT, IsaacsC, Weitzel J, Ganz PA, Daly MB, TomlinsonG, Olopade OI, Blum JL, Couch FJ,Peterlongo P, Manoukian S, Barile M, RadiceP, Szabo CI, Pereira LH, Greene MH,Rennert G, Lejbkowicz F, Barnett-GrinessO, Andrulis IL, Ozcelik H; OCGN, GerdesAM, Caligo MA, Laitman Y, KaufmanB, Milgrom R, Friedman E; SwedishBRCA1 and BRCA2 study collabora<strong>to</strong>rs,Domchek SM, Nathanson KL, Osorio A,Llort G, Milne RL, Benítez J, Hamann U,Hogervorst FB, Manders P, Ligtenberg MJ,van den Ouweland AM; DNA-HEBONcollabora<strong>to</strong>rs, Peock S, Cook M, Platte R,Evans DG, Eeles R, Pichert G, Chu C,Eccles D, Davidson R, Douglas F;EMBRACE, Godwin AK, Barjhoux L,Mazoyer S, Sobol H, Bourdon V, EisingerF, Chompret A, Capoulade C, Bressac-dePaillerets B, Lenoir GM, Gauthier-VillarsM, Houdayer C, S<strong>to</strong>ppa-Lyonnet D;GEMO, Chenevix-Trench G, Eas<strong>to</strong>n DF;CIMBA. Common breast cancer-predispositionalleles are associated with breastcancer risk in BRCA1 and BRCA2 mutationcarriers. Am J Hum Genet 2008;82(4):937–948.5. Arnold CN, Nagasaka T, Goel A, ScharfI, Grabowski P, Sosnowski A, Schmitt-Gräff A, Boland CR, Arnold R, Blum HE.Molecular characteristics and predic<strong>to</strong>rsof survival in patients with malignantneuroendocrine tumors. Int J <strong>Cancer</strong>2008;123(7):1556–15646. Ballen KK, King RJ, Chitphakdithai P, BolanCD Jr, Agura E, Hartzman RJ, KernanNA. The national marrow donor program:20 years of unrelated donor hema<strong>to</strong>poieticcell transplantation. Biol Blood MarrowTransplant 2008;14(9 Suppl):2–7.7. Barve M, Bender J, Senzer N, CunninghamC, Greco FA, McCune D, Steis R, KhongH, Richards D, Stephenson J, GanesaP, Nemunaitis J, Ishioka G, Pappen B,Nemunaitis M, Morse M, Mills B, MaplesPB, Sherman J, Nemunaitis JJ. Inductionof immune responses and clinical efficacyin a phase II trial of IDM-2101, a 10-epi<strong>to</strong>pe cy<strong>to</strong><strong>to</strong>xic T-lymphocyte vaccine, inmetastatic non-small-cell lung cancer. J ClinOncol 2008;26(27):4418–4425.8. Becerra CR, Verma UN, Tran HT, TavanaD, Williams NS, Frenkel EP. Phase I doseescalation study with irinotecan, capecitabine,epirubicin, and granulocyte colonystimulatingfac<strong>to</strong>r support for patientswith solid malignancies. Am J Clin Oncol2008;31(3):219–225.9. Boland CR. The molecular biology ofgastrointestinal cancer: implications fordiagnosis and <strong>the</strong>rapy. Gastrointest EndoscClin N Am 2008;18(3):401–413.10. Boland CR, Koi M, Chang DK, <strong>Care</strong><strong>the</strong>rsJM. The biochemical basis of microsatelliteinstability and abnormal immunohis<strong>to</strong>chemistryand clinical behavior in Lynchsyndrome: from bench <strong>to</strong> bedside. Fam<strong>Cancer</strong> 2008;7(1):41-52.11. Brim H, Mokarram P, NaghibalhossainiF, Saberi-Firoozi M, Al-Mandhari M,Al-Mawaly K, Al-Mjeni R, Al-Sayegh A,Raeburn S, Lee E, Giardiello F, Smoot DT,Vilkin A, Boland CR, Goel A, Hafezi M,Nouraie M, Ashk<strong>to</strong>rab H. Impact of BRAF,MLH1 on <strong>the</strong> incidence of microsatelliteinstability high colorectal cancer in populationsbased study. Mol <strong>Cancer</strong> 2008;7:68.12. Burdick JS. Intraductal papillary mucinousneoplasms. Gastrointest Endosc Clin N Am2008;18(3):523–533.13. Davis GL, Dempster J, Meler JD, OrrDW, Walberg MW, Brown B, Berger BD,O’Connor JK, Goldstein RM. Hepa<strong>to</strong>cellularcarcinoma: management of an increasinglycommon problem. Proc (Bayl UnivMed Cent) 2008;21(3):266–280.14. Dhodapkar MV, Dhodapkar KM, PaluckaAK. Interactions of tumor cells with dendriticcells: balancing immunity and <strong>to</strong>lerance.Cell Death Differ 2008;15(1):39–50.15. Dirix LY, Ignacio J, Nag S, Bapsy P, GomezH, Raghunadharao D, Paridaens R, JonesS, Falcon S, Carpentieri M, Abbattista A,Lobelle JP. Treatment of advanced hormone-sensitivebreast cancer in postmenopausalwomen with exemestane alone or incombination with celecoxib. J Clin Oncol2008;26(8):1253–1259.16. Eager R, Harle L, Nemunaitis J. Ad-MDA-7; INGN 241: a review of preclinicaland clinical experience. Expert Opin BiolTher 2008;8(10):1633–1643.17. Fazel P, Ganesa P, Mennel RG, Austin NA.The ec<strong>to</strong>pic adrenocorticotropic hormonesyndrome in carcinoid tumors. Proc (BaylUniv Med Cent) 2008;21(2):140–143.18. Fini L, Hotchkiss E, Fogliano V, GrazianiG, Romano M, De Vol EB, Qin H, SelgradM, Boland CR, Ricciardiello L. Chemopreventiveproperties of pinoresinol-richolive oil involve a selective activation of <strong>the</strong>ATM-p53 cascade in colon cancer cell lines.Carcinogenesis 2008;29(1):139–146.19. George S, Hutson TE, Mekhail T, Wood L,Finke J, Elson P, Dreicer R, Bukowski RM.Phase I trial of PEG-interferon and recombinantIL-2 in patients with metastatic renalcell carcinoma. <strong>Cancer</strong> Chemo<strong>the</strong>r Pharmacol2008;62(2):347–354.20. Ginsburg A. <strong>Cancer</strong>-related depression andpotential pharmacologic <strong>the</strong>rapies. Proc(Bayl Univ Med Cent) 2008;21(4):439–441.21. Gralow J, Rugo H, Gradishar W,O’Shaughnessy JA, Jahanzeb M, Perez E,Tripathy D. Novel taxane formulations in<strong>the</strong> treatment of breast cancer: a thoughtleader discussion and consensus roundtable.Clin Breast <strong>Cancer</strong> 2008;8(1):33–37.22. Haugen AC, Goel A, Yamada K, Marra G,Nguyen TP, Nagasaka T, Kanazawa S, KoikeJ, Kikuchi Y, Zhong X, Arita M, ShibuyaK, Oshimura M, Hemmi H, Boland CR,Koi M. Genetic instability caused by lossof MutS homologue 3 in human colorectalcancer. <strong>Cancer</strong> Res 2008;68(20):8465–8472.23. Hecht JR, Mitchell E, Chidiac T, ScrogginC, Hagenstad C, Spigel D, MarshallJ, Cohn A, McCollum D, Stella P, DeeterR, Shahin S, Amado RG. A randomizedphase IIIB trial of chemo<strong>the</strong>rapy, bevacizumab,and panitumumab compared withchemo<strong>the</strong>rapy and bevacizumab alone formetastatic colorectal cancer. J Clin Oncol2008 Dec 29 [Epub ahead of print].<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 27
24. Hutson TE. Renal cell carcinoma:what does <strong>the</strong> future hold? BJU Int2008;102(1):5–6.25. Hutson TE. Sunitinib (SUTENT) for<strong>the</strong> treatment of metastatic renal cellcarcinoma. Expert Rev Anticancer Ther2008;8(11):1723–1731.26. Hutson TE, Figlin RA. Experimental<strong>the</strong>rapy for advanced renal cell carcinoma.Expert Opin Investig Drugs 2008;17(11):1693–1702.27. Hutson TE, Figlin RA, Kuhn JG,Motzer RJ. Targeted <strong>the</strong>rapies for metastaticrenal cell carcinoma: an overview of<strong>to</strong>xicity and dosing strategies. Oncologist2008;13(10):1084–1096.28. Hutson TE, Vukelja S, Atienza D, AwasthiS, Delaune R, Deutsch M, Dien PY,Gregory TF, Kolodziej MJ, Musca<strong>to</strong> JJ,Raju RN, Ruxer RL Jr, Mull S, Ilegbodu D,Hood K, Nicol S, Berry W. Phase I study ofa 3-drug regimen of gemcitabine/cisplatin/pemetrexed in patients with metastatic transitionalcell carcinoma of <strong>the</strong> uro<strong>the</strong>lium.Invest New Drugs 2008;26(2):151–158.29. Jones SE. Considerations in treatmentchoice for metastatic breast cancer. Breast<strong>Cancer</strong> 2008;15(1):35–39.30. Jones SE. Metastatic breast cancer: <strong>the</strong>treatment challenge. Clin Breast <strong>Cancer</strong>2008;8(3):224–233.31. Jones S, S<strong>to</strong>koe C, Sborov M, Braun M,Ethirajan S, Kutteh L, Pippen J, Patel M,Paul D, Blum JL, Holmes FA, Myron MC,Cantrell J, Hartung NL, Look RM, DiSalle E, Davis JC, Ilegbodu D, Asmar L.The effect of tamoxifen or exemestane onbone mineral density during <strong>the</strong> first 2 yearsof adjuvant treatment of postmenopausalwomen with early breast cancer. Clin Breast<strong>Cancer</strong> 2008;8(6):527–532.32. Karanes C, Nelson GO, Chitphakdithai P,Agura E, Ballen KK, Bolan CD, Porter DL,Uberti JP, King RJ, Confer DL. Twentyyears of unrelated donor hema<strong>to</strong>poieticcell transplantation for adult recipientsfacilitated by <strong>the</strong> National Marrow DonorProgram. Biol Blood Marrow Transplant2008;14(9 Suppl):8–15.33. Kauff ND, Domchek SM, Friebel TM,Robson ME, Lee J, Garber JE, Isaacs C,Evans DG, Lynch H, Eeles RA, NeuhausenSL, Daly MB, Matloff E, Blum JL, SabbatiniP, Barakat RR, Hudis C, Nor<strong>to</strong>n L,Offit K, Rebbeck TR. Risk-reducingsalpingo-oophorec<strong>to</strong>my for <strong>the</strong> preventionof BRCA1- and BRCA2-associated breastand gynecologic cancer: a multicenter,prospective study. J Clin Oncol 2008;26(8):1331–1337.34. Kuhn JA, Fisher T, Livings<strong>to</strong>n S. Innovationsin surgical oncology at Baylor UniversityMedical Center. Proc (Bayl Univ MedCent) 2008;21(1):33–36.35. Laheru D, Lutz E, Burke J, Biedrzycki B,Solt S, Onners B, Tartakovsky I, NemunaitisJ, Le D, Sugar E, Hege K, JaffeeE. Allogeneic granulocyte macrophagecolony-stimulating fac<strong>to</strong>r-secreting tumorimmuno<strong>the</strong>rapy alone or in sequence withcyclophosphamide for metastatic pancreaticcancer: a pilot study of safety, feasibility,and immune activation. Clin <strong>Cancer</strong> Res2008;14(5):1455–1463.36. Lamborn KR, Yung WK, Chang SM, WenPY, Cloughesy TF, DeAngelis LM, RobinsHI, Lieberman FS, Fine HA, Fink KL,Junck L, Abrey L, Gilbert MR, Mehta M,Kuhn JG, Aldape KD, Hibberts J, PetersonPM, Prados MD; North American BrainTumor Consortium. Progression-free survival:an important end point in evaluating<strong>the</strong>rapy for recurrent high-grade gliomas.Neuro Oncol 2008;10(2):162–170.37. Laport GG, Sandmaier BM, S<strong>to</strong>rer BE,Scott BL, Stuart MJ, Lange T, Maris MB,Agura ED, Chauncey TR, Wong RM, FormanSJ, Petersen FB, Wade JC, Epner E,Bruno B, Bethge WA, Curtin PT, MaloneyDG, Blume KG, S<strong>to</strong>rb RF. Reduced-intensityconditioning followed by allogeneichema<strong>to</strong>poietic cell transplantation for adultpatients with myelodysplastic syndromeand myeloproliferative disorders. Biol BloodMarrow Transplant 2008;14(2):246–255.38. Larsen F, Menter A, Cockerell CJ, WilcoxBN. Verrucous linear (segmental) psoriasisof <strong>the</strong> right leg responding <strong>to</strong> radiation<strong>the</strong>rapy. J Drugs Derma<strong>to</strong>l 2008;7(10):969–971.39. Loesch D, Asmar L, McIntyre K, DoaneL, Monticelli M, Paul D, Vukelja S,Orlando M, Vaughn LG, Zhan F, BoehmKA, O’Shaughnessy JA. Phase II trial ofgemcitabine/carboplatin (plus trastuzumabin HER2-positive disease) in patients withmetastatic breast cancer. Clin Breast <strong>Cancer</strong>2008;8(2):178–186.40. Mi Z, Holmes FA, Hellerstedt B, PippenJ, Collea R, Backner A, Bush JE, GallionHH, Wells A, O’Shaughnessy JA. Feasibilityassessment of a chemoresponse assay <strong>to</strong>predict pathologic response in neoadjuvantchemo<strong>the</strong>rapy for breast cancer patients.Anticancer Res 2008;28(3B):1733–1740.41. Mittal A, Felter D, Shiller SM, McCollumAD, Lamont JP, Mallat D. Gastrointestinalbleeding and cutaneous nodules [site tumorconference report]. Proc (Bayl Univ MedCent) 2008;21(3):331–334.42. Motzer RJ, Bukowski RM, Figlin RA,Hutson TE, Michaelson MD, Kim ST,Baum CM, Kattan MW. Prognosticnomogram for sunitinib in patients withmetastatic renal cell carcinoma. <strong>Cancer</strong>2008;113(7):1552–1558.43. Motzer RJ, Escudier B, Oudard S, HutsonTE, Porta C, Bracarda S, Grünwald V,Thompson JA, Figlin RA, Hollaender N,Urbanowitz G, Berg WJ, Kay A, LebwohlD, Ravaud A; RECORD-1 Study Group.Efficacy of everolimus in advanced renalcell carcinoma: a double-blind, randomised,placebo-controlled phase III trial. Lancet2008;372(9637):449–456.44. Nagasaka T, Goel A, No<strong>to</strong>hara K, TakahataT, Sasamo<strong>to</strong> H, Uchida T, Nishida N,Tanaka N, Boland CR, Matsubara N.Methylation pattern of <strong>the</strong> O6-methylguanine-DNAmethyltransferase gene in colonduring progressive colorectal tumorigenesis.Int J <strong>Cancer</strong> 2008;122(11):2429–2436.45. Nagasaka T, Koi M, Kloor M, Gebert J,Vilkin A, Nishida N, Shin SK, Sasamo<strong>to</strong>H, Tanaka N, Matsubara N, Boland CR,Goel A. Mutations in both KRAS andBRAF may contribute <strong>to</strong> <strong>the</strong> methyla<strong>to</strong>rphenotype in colon cancer. Gastroenterology2008;134(7):1950–1960.46. Nemunaitis JJ. Are vaccines making acomeback in non-small-cell lung cancer? JClin Oncol 2008;26(9):1402–1403.47. Nemunaitis JM, Nemunaitis J. Potential ofAdvexin: a p53 gene-replacement <strong>the</strong>rapyin Li-Fraumeni syndrome. Future Oncol2008;4(6):759–768.48. Nishida N, Nagasaka T, Nishimura T,Ikai I, Boland CR, Goel A. Aberrantmethylation of multiple tumor suppressorgenes in aging liver, chronic hepatitis,and hepa<strong>to</strong>cellular carcinoma. Hepa<strong>to</strong>logy2008;47(3):908–918.49. O’Brien JC. Advances in <strong>the</strong> care of headand neck cancer patients at Baylor UniversityMedical Center. Proc (Bayl Univ MedCent) 2008;21(1):27–32.50. O’Shaughnessy JA, Brufsky AM. RiBBON1 and RiBBON 2: phase III trials of bevacizumabwith standard chemo<strong>the</strong>rapy formetastatic breast cancer. Clin Breast <strong>Cancer</strong>2008;8(4):370–373.51. Oh J, Karunanayake M, Stringer CA Jr.Invasive endometrial lesion in a patient withmental retardation [site tumor conferencereport]. Proc (Bayl Univ Med Cent)2008;21(4):426–429.28 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
52. Rana S, Maples PB, Senzer N, NemunaitisJ. Stathmin 1: a novel <strong>the</strong>rapeutic target foranticancer activity. Expert Rev AnticancerTher 2008;8(9):1461–1470.53. Reardon DA, Fink KL, Mikkelsen T,Cloughesy TF, O’Neill A, Plotkin S, GlantzM, Ravin P, Raizer JJ, Rich KM, Schiff D,Shapiro WR, Burdette-Radoux S, DropchoEJ, Wittemer SM, Nippgen J, Picard M,Nabors LB. Randomized phase II study ofcilengitide, an integrin-targeting arginineglycine-asparticacid peptide, in recurrentglioblas<strong>to</strong>ma multiforme. J Clin Oncol2008;26(34):5610–5617.54. Rezvani AR, Norasetthada L, Gooley T,Sorror M, Bouvier ME, Sahebi F, Agura E,Chauncey T, Maziarz RT, Maris M, ShizuruJ, Bruno B, Bredeson C, Lange T, Yeager A,Sandmaier BM, S<strong>to</strong>rb RF, Maloney DG.Non-myeloablative allogeneic haema<strong>to</strong>poieticcell transplantation for relapsed diffuselarge B-cell lymphoma: a multicentreexperience. Br J Haema<strong>to</strong>l 2008;143(3):395–403.55. Rezvani AR, S<strong>to</strong>rer B, Maris M, Sorror ML,Agura E, Maziarz RT, Wade JC, ChaunceyT, Forman SJ, Lange T, Shizuru J, Langs<strong>to</strong>nA, Pulsipher MA, Sandmaier BM, S<strong>to</strong>rb R,Maloney DG. Nonmyeloablative allogeneichema<strong>to</strong>poietic cell transplantation in relapsed,refrac<strong>to</strong>ry, and transformed indolentnon-Hodgkin’s lymphoma. J Clin Oncol2008;26(2):211–217.56 . Richards D, McCollum D, Wilfong L,Sborov M, Boehm KA, Zhan F, Asmar L.Phase II trial of docetaxel and oxaliplatin inpatients with advanced gastric cancer and/or adenocarcinoma of <strong>the</strong> gastroesophagealjunction. Ann Oncol 2008;19(1):104–108.57. Richey DS, Welch BJ. Concurrent primaryhyperparathyroidism and humoral hypercalcemiaof malignancy in a patient withclear cell endometrial cancer. South Med J2008;101(12):1266–1268.58. Rini BI, Michaelson MD, Rosenberg JE,Bukowski RM, Sosman JA, Stadler WM,Hutson TE, Margolin K, Harmon CS,DePrimo SE, Kim ST, Chen I, George DJ.Antitumor activity and biomarker analysisof sunitinib in patients with bevacizumabrefrac<strong>to</strong>rymetastatic renal cell carcinoma. JClin Oncol 2008;26(22):3743–3748.59. Rotta M, S<strong>to</strong>rer BE, Sahebi F, Shizuru JA,Bruno B, Lange T, Agura ED, McSweeneyPA, Pulsipher MA, Hari P, Maziarz RT,Chauncey TR, Appelbaum FR, SorrorML, Bensinger W, Sandmaier BM, S<strong>to</strong>rbRF, Maloney DG. Long-term outcome ofpatients with multiple myeloma after au<strong>to</strong>logoushema<strong>to</strong>poietic cell transplantationand nonmyeloablative allografting. Blood2008 Nov 17 [Epub ahead of print].60. Selgrad M, Koornstra JJ, Fini L, Blom M,Huang R, Devol EB, Boersma-van Ek W,Dijkstra G, Verdonk RC, de Jong S, GoelA, Williams SL, Meyer RL, Haagsma EB,Ricciardiello L, Boland CR. JC virus infectionin colorectal neoplasia that developsafter liver transplantation. Clin <strong>Cancer</strong> Res2008;14(20):6717–6721.61. Selgrad M, Malfer<strong>the</strong>iner P, Fini L, GoelA, Boland CR, Ricciardiello L. The role ofviral and bacterial pathogens in gastrointestinalcancer. J Cell Physiol 2008;216(2):378–388.62. Sequist LV, Martins RG, Spigel D,Grunberg SM, Spira A, Jänne PA, JoshiVA, McCollum D, Evans TL, MuzikanskyA, Kuhlmann GL, Han M, GoldbergJS, Settleman J, Iafrate AJ, Engelman JA,Haber DA, Johnson BE, Lynch TJ. Firstlinegefitinib in patients with advancednon-small-cell lung cancer harboringsomatic EGFR mutations. J Clin Oncol2008;26(15):2442–2449.63. Sonpavde G, Fleming MT, Hutson TE,Galsky MD. Trial design for metastaticcastration-resistant prostate cancer. J ClinOncol 2008;26(21):3647–3648.64. Sonpavde G, Galsky MD, Hutson TE.Current optimal chemo<strong>the</strong>rapy foradvanced uro<strong>the</strong>lial cancer. Expert RevAnticancer Ther 2008;8(1):51–61.65. Sonpavde G, Hutson TE. Novel antiangiogenicagents in <strong>the</strong> treatment of refrac<strong>to</strong>ryrenal cell carcinoma. Clin Geni<strong>to</strong>urin <strong>Cancer</strong>2008;6(3):s29–s36.66. Sonpavde G, Hutson TE, Berry WR, BoehmKA, Asmar L. Phase II trial of sunitinibfor <strong>the</strong> <strong>the</strong>rapy of progressive metastaticcastration-refrac<strong>to</strong>ry prostate cancer afterprevious docetaxel chemo<strong>the</strong>rapy. ClinGeni<strong>to</strong>urin <strong>Cancer</strong> 2008;6(2):134–137.67. Sonpavde G, Hutson TE, Rini BI. Axitinibfor renal cell carcinoma. Expert Opin InvestigDrugs 2008;17(5):741–748.68. Sonpavde G, Hutson TE, Sternberg CN.Pazopanib, a potent orally administeredsmall-molecule multitargeted tyrosinekinase inhibi<strong>to</strong>r for renal cell carcinoma.Expert Opin Investig Drugs 2008;17(2):253–261.69. Sonpavde G, Ross R, Powles T, SweeneyCJ, Hahn N, Hutson TE, Galsky MD,Lerner SP, Sternberg CN. Novel agents formuscle-invasive and advanced uro<strong>the</strong>lialcancer. BJU Int 2008;101(8):937–943.70. Sorror ML, S<strong>to</strong>rer BE, Sandmaier BM,Maris M, Shizuru J, Maziarz R, Agura E,Chauncey TR, Pulsipher MA, McSweeneyPA, Wade JC, Bruno B, Langs<strong>to</strong>n A,Radich J, Niederwieser D, Blume KG,S<strong>to</strong>rb R, Maloney DG. Five-year follow-upof patients with advanced chronic lymphocyticleukemia treated with allogeneichema<strong>to</strong>poietic cell transplantation afternonmyeloablative conditioning. J ClinOncol 2008;26(30):4912–4920.71. Steen S, Nemunaitis J, Fisher T, Kuhn J.Circulating tumor cells in melanoma: areview of <strong>the</strong> literature and description of anovel technique. Proc (Bayl Univ Med Cent)2008;21(2):127–132.72. Steen S, Stephenson G. Current treatmen<strong>to</strong>f soft tissue sarcoma. Proc (Bayl Univ MedCent) 2008;21(4):392–396.73. S<strong>to</strong>ne MJ. Waldenström’s macroglobulinemia.In Land F, ed. Encyclopedic Reference ofMolecular Mechanisms of Disease. Heidelberg,Germany: Springer-Verlag, 2008.74. Thompson JL, Duffy J. Nutrition supportchallenges in hema<strong>to</strong>poietic stemcell transplant patients. Nutr Clin Pract2008;23(5):533–546.75. Tong AW, Fulgham P, Jay C, Chen P, KhalilI, Liu S, Senzer N, Eklund AC, Han J,Nemunaitis J. MicroRNA profile analysis ofhuman prostate cancers. <strong>Cancer</strong> Gene Ther2008 Oct 24 [Epub ahead of print].76. Tong AW, Nemunaitis J. Modulation ofmiRNA activity in human cancer: a newparadigm for cancer gene <strong>the</strong>rapy? <strong>Cancer</strong>Gene Ther 2008;15(6):341–355.77. Urba WJ, Nemunaitis J, Marshall F, SmithDC, Hege KM, Ma J, Nguyen M, SmallEJ. Treatment of biochemical recurrenceof prostate cancer with granulocyte-macrophagecolony-stimulating fac<strong>to</strong>r secreting,allogeneic, cellular immuno<strong>the</strong>rapy. J Urol2008;180(5):2011–2017.78. Wallraven G, Maples PB, Nemunaitis J.Emergency use regula<strong>to</strong>ry approval processfor experimental gene-based <strong>the</strong>rapy. J ClinOncol 2008;26(33):5488–5489.79. Wallraven G, Nemunaitis JJ, Maples PB.Compassionate approval process for experimentalgene-based products. J Clin Oncol2008;26(11):1899–1900.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 29
<strong>Building</strong> <strong>Hope</strong> Through PhilanthropyNorth Texas is expected <strong>to</strong> see a 21%increase in <strong>the</strong> number of cancer patientsin <strong>the</strong> next 5 years. To meet that growingneed, Baylor Health <strong>Care</strong> System is building<strong>the</strong> area’s premier dedicated cancercenter at Baylor University MedicalCenter at Dallas. The new cancer centerwill include a 10-s<strong>to</strong>ry, 450,000-squarefoo<strong>to</strong>utpatient building and renovationof Collins Hospital and Sammons Towerat a cost of $350 million. Baylor Health<strong>Care</strong> System Foundation is spearheading<strong>the</strong> campaign <strong>to</strong> raise <strong>the</strong> funds <strong>to</strong> makethis project a reality.$5 Million Gift for Blood<strong>Cancer</strong> ResearchThe Pauline Allen Gill Foundationrecently gave $5 million in memoryof Pauline Gill Sullivan <strong>to</strong> support <strong>the</strong>new cancer center at Baylor UniversityMedical Center at Dallas. Nancy Seay,president of <strong>the</strong> Pauline Allen GillFoundation, helped orchestrate <strong>the</strong>gift, which will support hema<strong>to</strong>logicalresearch at Baylor Dallas and establishThe Pauline Allen Gill DistinguishedChair in Hema<strong>to</strong>logical <strong>Cancer</strong>Research.Pauline Gill SullivanMrs. Sullivan’s oncologist, BrianBerryman, MD, will be instrumentalin establishing <strong>the</strong> program. “Through<strong>the</strong> generosity of <strong>the</strong> foundation and<strong>the</strong> family of Pauline Gill Sullivan,physicians and researchers at Baylor willbe able <strong>to</strong> conduct more clinical trialsfor patients with hema<strong>to</strong>logical cancers,helping us identify <strong>the</strong> most effectivetreatments for <strong>the</strong>se diseases and,ultimately, bringing advanced care <strong>to</strong>Baylor patients,” stated Dr. Berryman.Darlene G. Cass and keynote speaker Geralyn Lucas at <strong>the</strong> Celebrating Women luncheon,which raised $2.2 million <strong>to</strong> battle breast cancer.2008 Celebrating WomenBaylor Health <strong>Care</strong> System Foundationhonored women fighting breast cancerat <strong>the</strong> ninth annual Celebrating Womenluncheon on Oc<strong>to</strong>ber 16, 2008, at <strong>the</strong>Hil<strong>to</strong>n Ana<strong>to</strong>le in Dallas. The eventraised $2.2 million for breast cancerresearch, community outreach, andexpanded technology for early detectionand treatment throughout Baylor Health<strong>Care</strong> System.More than 1,350 guests heard s<strong>to</strong>ries ofwomen’s struggles with <strong>the</strong> disease fromkeynote speaker Geralyn Lucas, author ofWhy I Wore Lipstick <strong>to</strong> My Mastec<strong>to</strong>my.The Circle of <strong>Care</strong> Award, which honorscommunity heroes active in <strong>the</strong> fightagainst breast cancer, was given <strong>to</strong> Nancyand David Burgher and Highland HillsUnited Methodist Church Senior Pas<strong>to</strong>rSheron C. Patterson.30 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Dr. Thomas Hutson, Tony Romo, and Carolyn Berry at <strong>the</strong> EveryMan dinner, which promoted prostate cancer awareness and raised money <strong>to</strong>support expanded technology, research, and community outreach.The Foundation will host its 10thannual Celebrating Women luncheonon Oc<strong>to</strong>ber 22, 2009, at <strong>the</strong> Hil<strong>to</strong>nAna<strong>to</strong>le. Actress Christina Applegatewill be <strong>the</strong> featured speaker.Gift for Imaging CenterTechnologyDavid Winter, MD, president of <strong>the</strong>Discovery Foundation, announced that<strong>the</strong> board of direc<strong>to</strong>rs approveda $350,000 grant for new technology in<strong>the</strong> Darlene G. Cass Women’s ImagingCenter. The Discovery Foundation grantwill allow Baylor <strong>to</strong> acquire positronemission mammography, or PEM, whichuses a high-resolution gamma camera.Sometimes referred <strong>to</strong> as molecular breastimaging, this technology can pick upsubtle differences in <strong>the</strong> appearance oftumor versus normal tissue. Conventionalmammography can have a falsenegativerate of up <strong>to</strong> 10%—partly due<strong>to</strong> dense breast tissues obscuring <strong>the</strong>cancer and <strong>the</strong> large overlap between <strong>the</strong>appearance of tumor and normal tissue.PEM will help reduce <strong>the</strong> instances offalse-negative readings. Baylor will be <strong>the</strong>first imaging facility in <strong>the</strong> Southwest <strong>to</strong>have this technology.EveryMan Event for Prostate<strong>Cancer</strong>On April 30, 2008, Ramiro and TonyRomo joined Baylor Health <strong>Care</strong> SystemFoundation at <strong>the</strong> first EveryMan dinnerat <strong>the</strong> Ritz-Carl<strong>to</strong>n Hotel in Dallas.Ramiro Romo, who was diagnosed withprostate cancer in 2007, addressed <strong>the</strong>250 guests attending <strong>the</strong> event designed<strong>to</strong> promote awareness of prostate cancerand raise money <strong>to</strong> support expandedtechnology, research, and communityoutreach. Panelists Steven Frost, MD, andPick Scruggs, MD, provided details about<strong>the</strong> importance of early detection andavailable treatment options. Thomas Hutson,DO, PharmD, shared insights in<strong>to</strong><strong>the</strong> comprehensive research program atBaylor Health <strong>Care</strong> System and its visionfor <strong>the</strong> future. Mat<strong>the</strong>w Shuford, MD,also provided attendees an opportunity<strong>to</strong> interact directly with <strong>the</strong> da Vinci ®surgical robot, used for advanced surgicalprocedures such as prostatec<strong>to</strong>mies.The Foundation will host EveryMan2009 on May 13, 2009, at <strong>the</strong> Ritz-Carl<strong>to</strong>n.Former New York City Mayor RudyGiuliani will be <strong>the</strong> keynote speaker.<strong>Building</strong> <strong>Hope</strong>: <strong>Taking</strong> <strong>Cancer</strong> <strong>Care</strong> <strong>to</strong> <strong>the</strong> <strong>Next</strong> <strong>Level</strong> 31
Telephone Direc<strong>to</strong>ryReferralsBaylor Sammons <strong>Cancer</strong> Center at DallasPatient Navigation Program (214) 820-3535Baylor Physician ConsultLine1-800-9BAYLORBaylor Patient HelpLine1-800-4BAYLORAdministration<strong>Cancer</strong> Center AdministrationAlan M. Miller, MD, PhDDirec<strong>to</strong>r/Chief of Oncology (214) 820-2881Marvin J. S<strong>to</strong>ne, MD, Direc<strong>to</strong>r of OncologyMedical Education, Quality, and Safety (214) 820-3445Donna Bowers, JD, RHIA, CHP,Baylor Health <strong>Care</strong> SystemVice President/Oncology (214) 820-2800Sylvia Coats, Direc<strong>to</strong>r of Administration (214) 820-3433Ryan T. Seymour, MBA, RHIA,BHCS Direc<strong>to</strong>r/Oncology (214) 820-6322John McWhorter, MHA, President,Baylor University Medical Center at Dallas (214) 820-4141Texas Oncology, PA (214) 370-1000R. Steven Paulson, MD, President andChairman of <strong>the</strong> BoardJoni Mokry, RN, OCN, Practice Direc<strong>to</strong>rBaylor Health <strong>Care</strong> System Foundation (214) 820-3136Department of OncologyAlan M. Miller, MD, PhD, Chief (214) 820-2881DivisionsGynecologic Oncology (214) 370-1300C. Allen Stringer, Jr., MD, Direc<strong>to</strong>rMedical Oncology and O<strong>the</strong>rInternal Medical Subspecialties (214) 370-1000Robert G. Mennel, MD, Direc<strong>to</strong>rOncologic Pathology (214) 820-2251Daniel A. Savino, MD, Direc<strong>to</strong>rRadiation Oncology (214) 370-1400R. Pickett Scruggs, III, MD, Direc<strong>to</strong>rSurgical Oncology (214) 826-6270John T. Preskitt, MD, Direc<strong>to</strong>r<strong>Cancer</strong> Center ProgramsGraft-vs-Host Disease Clinic (GVHD) (214) 370-1500Blood and Marrow TransplantInpatient Services (214) 820-2619Blood and Marrow TransplantOutpatient Center (214) 370-1500National Marrow Donor Program (214) 820-4279Darlene G. Cass Women’s Imaging Center (214) 820-2430• Diagnostic mammography• Screening mammography• O<strong>the</strong>r breast imagingW. H. & Peggy Smith Baylor SammonsBreast Center (214) 820-9600• Breast cancer prevention research trials• Breast <strong>Care</strong> for a Lifetime • Breast health education• Personal risk evaluationCutaneous Lymphoma Clinic (214) 370-1500Hereditary <strong>Cancer</strong> Risk Program• Breast and ovarian (214) 820-9600• Gastrointestinal (214) 820-2692Liver and Pancreas Disease Center (214) 820-1756Lung <strong>Cancer</strong> Center (214) 820-6767Lymphedema Program (214) 820-1931• Lymphedema prevention and treatment servicesRadiosurgery Center (214) 820-7285ResearchBaylor Institute for Immunology Research (214) 820-7450Jacques Banchereau, PhD, Direc<strong>to</strong>rBaylor Research Institute (214) 820-2687Michael A. E. Ramsay, MD, PresidentBreast <strong>Cancer</strong> Prevention Research Trials (214) 820-9600Joyce A. O’Shaughnessy, MD, Direc<strong>to</strong>r<strong>Cancer</strong> Immunology Research Labora<strong>to</strong>ry (214) 820-4123Marvin J. S<strong>to</strong>ne, MD, Direc<strong>to</strong>rMary Crowley Medical Research Center (214) 370-1870John Nemunaitis, MD, Executive Medical Direc<strong>to</strong>rNational Surgical AdjuvantBreast and Bowel Project (214) 820-9600Michael D. Grant, MD, Direc<strong>to</strong>rUS Oncology/Texas Oncology Research (214) 370-1000Joanne L. Blum, MD, PhD, Site LeaderSupport ServicesErnie’s Appearance Center (214) 820-8282• Pros<strong>the</strong>ses and specialty care items for cancer patientsScreenings1-800-4BAYLOR• Skin/melanoma (May)• Prostate cancer (Sept)Smoking Cessation Program (214) 820-9791• Martha Foster Lung <strong>Care</strong> CenterVirginia R. Cvetko Patient Education Center (214) 820-2608• Barrett Lectureship• Community resource referrals• Individual counseling• Nutrition education/support• Patient/family education and support programs:> Amyloid Support North Texas> Blood and Marrow Transplant Inpatient Support Group> Breast <strong>Cancer</strong> Support Group> Carcinoid <strong>Cancer</strong> Texas Survivors> North Texas Myeloma Support Group> Oncology Inpatient Support Group> Ovarian <strong>Cancer</strong> Support Group> Prostate <strong>Cancer</strong> Education and Support Group> Support for People with Oral and Head and Neck <strong>Cancer</strong>> Virginia R. Cvetko Living with <strong>Cancer</strong> Series> Waldenström’s Macroglobulinemia Support Group• Patient resource centers/oncology libraries> 6 Collins Hospital> 6 Roberts HospitalWorth Street Valet Parking (214) 820-8077Patient Transport (214) 818-640032 Baylor Charles A. Sammons <strong>Cancer</strong> Center at Dallas
Location MapsHall StreetBaylorCollege ofDentistryRobertsHospitalTruettHospitalJunius StreetBaylor Sammons<strong>Cancer</strong> CenterLot 23Gas<strong>to</strong>n AvenueHoblitzelleHospitalWadleyTowerBarnettTowerLot 25 UndergroundParking Garage 8Garage 30UndergroundParking Garage 3CoveredParkingLot 4ParkingGarage 5Lot 46ParkingGarage 6(Staff)Washing<strong>to</strong>n AvenueI-35EDALLAS N. TOLLWAYI-35ELEMMONWOODALL RODGERS FWY.US 75 N. CENTRAL EXPY.LIVE OAKWASHINGTONGASTONHASKELLPEAKWORTHLIVE OAKI-30GASTONCARROLLWORTHMAINPEAKFITZHUGHHALLMALCOLM XLot 12HASKELLFuture Siteof <strong>the</strong> New<strong>Cancer</strong> CenterWorth StreetBass HallBaylorSchool ofNursingLot 14ELMCOMMERCEDOWNTOWN DALLASI-30FIRSTBAYLOR UNIVERSITYMEDICAL CENTERAT DALLAS CAMPUSSTATE FAIRGROUNDSROBERT B. CULLUMSelf ParkingValet ParkingI-30BAYLOR SAMMONSCANCER CENTERI-45MALCOLM XI-35EUS 175Baylor Sammons <strong>Cancer</strong> Center is located on <strong>the</strong> campus ofBaylor University Medical Center at Dallas and is accessiblefrom U.S. 75 (North Central Expressway)/I-45 and 1-30.Valet parking is available at <strong>the</strong> front entrance and o<strong>the</strong>r nearbylocations. Self parking is conveniently located adjacent <strong>to</strong> <strong>the</strong>Baylor Sammons <strong>Cancer</strong> Center.
Baylor UniversityMedical Center at Dallas3500 Gas<strong>to</strong>n AvenueDallas, Texas 752461-800-4BAYLOR(214) 820-3535BaylorHealth.com/Dallas<strong>Cancer</strong>Baylor Health <strong>Care</strong> System wantscancer patients in North Texas <strong>to</strong>have access <strong>to</strong> advanced cancerprevention, screening, diagnosis,treatment and research—close <strong>to</strong>home where <strong>the</strong>y can be supportedby <strong>the</strong>ir loved ones. Baylor Health<strong>Care</strong> System Foundation supportsthat vision, and <strong>to</strong> that end, it israising funds for Baylor’s new, $350million cancer center project. Tolearn more about giving opportunities,please contact <strong>the</strong> Foundationat (214) 820-3136 or Foundation@BaylorHealth.edu.