The Ethics and Regulations of Clinical Research - UKM Medical ...
The Ethics and Regulations of Clinical Research - UKM Medical ...
The Ethics and Regulations of Clinical Research - UKM Medical ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Scope <strong>of</strong> Lecture• Case studies• Definitions• General principles <strong>of</strong> ethical researchInformed consentIndependent review• CIOMS Guidelines• Summary4<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Experiments On Prisoners• Nazi experiment on prisoners in concentration camps– Bone, muscle, <strong>and</strong> nerve transplantation experiments– Freezing experiments– Malaria experiments– Sulfonamide experiments– Sea water experiments– Sterilization experiments– Incendiary bomb experiments• Imperial Japanese Army Unit 731– Similar sort <strong>of</strong> experiments.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Principles <strong>of</strong> <strong>Ethics</strong> - Hippocrates• ―Primum non nocere‖• …..Whatever houses I may visit, I will come for thebenefit <strong>of</strong> the sick, remaining free <strong>of</strong> all intentionalinjustice, <strong>of</strong> all mischief <strong>and</strong> in particular <strong>of</strong> sexualrelations with both female <strong>and</strong> male persons, be theyfree or slaves….<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Tuskegee syphilis experiment• A clinical study conducted between 1932 <strong>and</strong> 1972 inTuskegee, Alabama, by the U.S. Public HealthService• 400 impoverished black males who had syphilis, were<strong>of</strong>fered observation by the researchers• At start <strong>of</strong> study, there was no therapy but whenpenicillin became available, the drug was withheld sothey could observe the effects <strong>of</strong> syphilis on thehuman body.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Tuskegee syphilis experiment• By the end <strong>of</strong> the study in 1972, only 74 <strong>of</strong> thetest subjects were alive.– 28 <strong>of</strong> the original 399 men had died <strong>of</strong> syphilis, 100were dead <strong>of</strong> related complications.– 40 <strong>of</strong> their wives had been infected,– 19 <strong>of</strong> their children were born with congenital syphilis.• <strong>The</strong> study was not shut down until 1972,when its existence was leaked to the press,forcing the researchers to stop in the face <strong>of</strong>public outcry.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Scientific misconduct• Dr. SSR, an anesthesiologist, who practiced at B<strong>Medical</strong> Center, has admitted that he neverconducted the clinical trials that he wrote about in 21journal articles dating back to at least 1996.– Company P Inc. underwrote most <strong>of</strong> the trials in whichDr. R found that their painkiller drugs C <strong>and</strong> L wereeffective against post-operative pain.– Questions were raised about two study abstracts thathe filed. BMC determined that he had not receivedapproval to conduct human research for these studies.– This led to the discovery Dr. R had concocted data for21 studies.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
And more…• Company P Inc. acquired WL in 2000, a company that sold―N‖, a medication approved by FDA for the treatment <strong>of</strong>epileptic fit seizures, <strong>and</strong> for pain related to shingles.• P pleaded guilty in 2004, to felony charges that it promotedthe drug for uses that were not approved by the FDA.– P is being sued by consumer groups <strong>and</strong> third-party payers who areseeking $4.9 billion in repayment for fraudulent misrepresentation inpromoting the <strong>of</strong>f-label usage <strong>of</strong> N.• Company P sought to conceal harmful studies <strong>and</strong> clinicaltrials involving ―N‖.– MR, the N team leader wrote in an e-mail in 2000 saying, " I think wecan limit the potential downsides <strong>of</strong> the …. Study by delaying thepublication for as long as possible,".<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
And lastly….• <strong>The</strong> study's scientific manager, wrote in an email toemployees after P had acquired WL that she hadbeen instructed "that we should take care not topublish anything that damages N marketing success.―• In 2002, AC, then N senior marketing manager,emailed an outside firm that was contracted to writeup the study's results, "We are not interested at all inhaving this paper published because it is negative!!".<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
General Ethical Principles• <strong>Research</strong> in human subjects should be done inaccordance to 3 basic principles– respect for persons,– respect for autonomy– protection <strong>of</strong> persons with impaired or diminished autonomy– beneficence– maximize benefits <strong>and</strong> to minimize harms– justiceInternational Ethical Guidelines for Biomedical <strong>Research</strong> Involving Human Subjects Prepared by theCouncil for International Organizations <strong>of</strong> <strong>Medical</strong> Sciences (CIOMS) in collaboration with the WorldHealth Organization (WHO) CIOMS, Geneva 2002<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Codes <strong>and</strong> <strong>Regulations</strong>for Ethical <strong>Clinical</strong> <strong>Research</strong>• Nuremberg Code(1947) - Nazi• Belmont Report(1979) - Tuskegee• U.S. Common Rule (1991)• Declaration <strong>of</strong> Helsinki (2000)• CIOMS (2002)<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
How do you evaluate if a proposedresearch is ethical?
Main Principles <strong>of</strong> Ethical <strong>Clinical</strong> <strong>Research</strong>• Social <strong>and</strong> clinical value• Scientific validity• Fair Subject selection• Favourable risk-benefit ratio• Independent review• Informed consent• Respect for potential <strong>and</strong> enrolled subjects<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
1. Social <strong>and</strong> clinical value• Every research is designed to answer a specificquestion.– should contribute to underst<strong>and</strong>ing <strong>of</strong> health or improveour ways <strong>of</strong> treating a disease.• Consider how research would benefit– <strong>Research</strong> participant– Society– Nation etc• For clinical trials, there should be equipoise ie.uncertainty which is the better treatment.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
2. Scientific validity• A study should be designed in a way that will get anunderst<strong>and</strong>able answer to the research question.– Is the research question answerable?– Is the research methods are valid, rigorous <strong>and</strong> feasible?– Is the study is designed with a clear scientific objective<strong>and</strong> using accepted principles, methods, <strong>and</strong> reliablepractices.• <strong>The</strong> trial should be <strong>of</strong> sufficient power to definitively testthe objective• Invalid research is unethical because it is a waste <strong>of</strong>resources <strong>and</strong> exposes people to risk for no purpose.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
3. Fair subject selection• Who does the study need to include, to answer thequestion it is asking?• <strong>The</strong> basis for recruiting individuals should be thescientific goals <strong>of</strong> the study — not vulnerability,privilege, or other factors.– Participant should be chosen in a way that minimizesrisks <strong>and</strong> enhances benefits to individuals <strong>and</strong> society.• Groups <strong>and</strong> individuals who accept the risks <strong>and</strong>burdens <strong>of</strong> research should be in a position to enjoyits benefits, <strong>and</strong> those who may benefit should sharesome <strong>of</strong> the risks <strong>and</strong> burdens.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Studies on Vulnerable patients• Study done in Nigeria on meningitis• Company X study protocol called for the children to have their• blood tested on arrival <strong>and</strong> then five days later. If a child was notresponding well to the oral Drug T, Company X was to switchthe treatment to Ceftriaxone.• <strong>The</strong> patients claim that Company X neglected to analyze theirblood samples <strong>and</strong> therefore did not determine if a patient had anegative reaction until the manifestation <strong>of</strong> visible <strong>and</strong>permanent injury.• After two weeks, Company X team left Kano <strong>and</strong> did not returnfor any follow-up evaluations.• Five children who received drug T <strong>and</strong> six children who werelow-dosed died. Others suffered paralysis, deafness, <strong>and</strong>blindness. Prior to Kano, only one child had ever been treatedwith T, <strong>and</strong> then only after all other antibiotics failed; no childhad ever received T orally.MA Pagnattaro <strong>The</strong> Journal <strong>of</strong> Legal Studies Education<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
4. Favorable risk-benefit ratio• <strong>Clinical</strong> research should be done in a mannerconsistent with the st<strong>and</strong>ards <strong>of</strong> clinical practice– This may differ between hospitals, states & countries• <strong>The</strong>re is always uncertainty about the degree <strong>of</strong> risks<strong>and</strong> benefits associated with a drug, device, orprocedure• Evaluate1. Risks– Minor or major, short term or long term etc.– Includes physical, psychological, economic, or social– Identify mechanisms to minimize risk eg additionaltests, monitoring etc<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Favorable risk-benefit ratio2. Potential benefits to individuals– Physical, psychological etc.– Consider ONLY benefits from research– Not added services eg payment etc3. If potential benefit outweights risk, proceed4. If risk outweigh benefit to the individual, thenevaluate risk against social benefit <strong>of</strong> knowledge<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
5. Independent review• To minimize potential conflicts <strong>of</strong> interest <strong>and</strong> makesure a study is ethically acceptable, an independentreview panel should review the proposal– Are those conducting the trial sufficiently free <strong>of</strong> bias?– Is the study doing all it can to protect researchvolunteers?– Has the trial been ethically designed <strong>and</strong> is the risk–benefit ratio favorable?• Independent evaluation <strong>of</strong> research projects is donethrough local institutional review boards (IRBs), <strong>and</strong>data <strong>and</strong> safety monitoring boards.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Investigator Conflicts <strong>of</strong> Interest• Pr<strong>of</strong>essional gain: publications/promotion• Financial gain– Patient finder’s fee to collaborators– Recruitment bonuses• Affiliation with/funding from sponsor for future studies,consultant relationships• Other incentives (e.g., travel, presentations)• Per patient payment system presents conflicts <strong>of</strong>interest inherent in capitalist society<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Potential Consequences <strong>of</strong> Investigator COI• Attempting to increase study enrollment• Coercing subjects to enroll <strong>and</strong> discouragingwithdrawal, treatment alternatives• Enrolling fictitious or ineligible patients• Bias trial toward positive results• Failure to report adverse events• Failure to comply with protocol regimens• Alteration <strong>of</strong> outcome data• Data fabrication<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Definition <strong>of</strong> Independent <strong>Ethics</strong>Committee (IEC)An independent body (a review board or acommittee, institutional, regional, national, orsupranational), constituted <strong>of</strong> medical/scientificpr<strong>of</strong>essionals <strong>and</strong> non-medical/non-scientificmembers, whose responsibility it is to ensurethe protection <strong>of</strong> the rights, safety <strong>and</strong> wellbeing<strong>of</strong> human subjects involved in a trial <strong>and</strong>to provide public assurance <strong>of</strong> that protection,by, among other things…<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Definition <strong>of</strong> Independent <strong>Ethics</strong> Committee(IEC), continued……reviewing <strong>and</strong> approving/providing favourable opinion on,the trial protocol, the suitability <strong>of</strong> the investigator (s),facilities, <strong>and</strong> the methods <strong>and</strong> material to be used inobtaining <strong>and</strong> documenting informed consent <strong>of</strong> thetrial subjects28<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Main Tasks <strong>of</strong> EC• Review <strong>of</strong>– Scientific Design <strong>and</strong> Conduct <strong>of</strong> the Study– Recruitment <strong>of</strong> <strong>Research</strong> Participants– Care <strong>and</strong> Protection <strong>of</strong> <strong>Research</strong> Participants– Protection <strong>of</strong> <strong>Research</strong> Participant Confidentiality– Informed Consent Process– Community Considerations<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
EC - Composition• Chairperson– preferably be from outside the Institution <strong>and</strong>not head <strong>of</strong> the same Institution to maintainthe independence <strong>of</strong> the Committee.• Member secretary– who generally belongs to the same institution<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Non-scientific, non-medical members• Members <strong>of</strong> the community who are able toevaluate:– Social views <strong>and</strong> values– Religious issues– Legal implications– Environmental considerations• Age & gender balanced• Must have integrity• Examples:– Clergy, lawyers, environmentalists, pharmacists,dentists, teachers, etc.31<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
PP<strong>UKM</strong> IEC• Chairperson• 1-2 basic medical scientists. (Lab)• 1-2 clinicians from various departments– 1 permanent member, 1 reserve member• One legal expert or retired judge– Appointed by Bar Council• One philosopher / ethicist / theologian– Ustaz / Fakulti Islam• One lay person from the community• Member-Secretary• Co-opted / Ad-hoc member<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Essential documents• Trial protocol/amendments• Investigator’s brochure + safety information• Subject information sheet• Consent form & updates• Indemnity/insurance coverage• Publication policy• Investigators’ current CVs• Payment• Subject recruitment procedures/advertisements33<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
EC Approval• Prompt notification in writing by IEC :– Decisions/Opinions– Reasons for its decisions/ opinions– Procedures for appeal <strong>of</strong> its decisions/opinions• Written approval :Minimum Information Required by ICH - GCP– Date <strong>of</strong> the meeting– Documents reviewed (versions & dates)– List <strong>of</strong> members present <strong>and</strong> quorum complete<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Some comments from MREC MOH<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
NHS REC approval• Ethical advice is required for any research involving:– patients <strong>and</strong> users <strong>of</strong> the NHS.– individuals identified as potential research participantsbecause <strong>of</strong> their status as relatives or carers <strong>of</strong> patients<strong>and</strong> users <strong>of</strong> the NHS, as defined above– access to data, organs or other bodily material <strong>of</strong> past<strong>and</strong> present NHS patients– fetal material <strong>and</strong> IVF involving NHS patients– the recently dead in NHS premises– the use <strong>of</strong>, or access to, NHS premises or facilities– NHS staff – recruited as research participants by virtue<strong>of</strong> their pr<strong>of</strong>essional role.Governance arrangements for NHS<strong>Research</strong> <strong>Ethics</strong> Committees July 2001<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Expedited Review• One experienced IRB member (Chairman)• Reported to full IRB• Study with minimal risk <strong>of</strong> harm, <strong>and</strong>…– 1. Drugs or devices - no IND– 2. Blood - healthy adults; others– 3. Hair, nails, teeth, excreta, secretions– 4. Non-invasive clinical procedures– 5. Data, documents, records– 6. Voice, video, image recordings– 7. Behavior or characteristics<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Issues with IEC• Initial review done:– rarely follow-up review <strong>and</strong> monitoring.• No training in ethics review:– primarily scientific review done.• ECs are not completely independant– do not have any funds / <strong>of</strong>fice allocated– Most members <strong>UKM</strong> staff<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
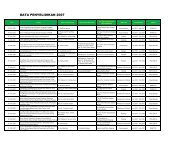
Issues with IEC (2)• Genetic research– Not st<strong>and</strong>ardised– Archiving specimens• Timely review– Too many projects– Varying level <strong>of</strong> projects– SSM– Masters– PhD– International Multicentre trial<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Issues with IEC (3)• Subjects in the study– Incentives?– Cost <strong>of</strong> treatment <strong>of</strong> injury due to trial– Advertisements– How will the patient be looked after the end <strong>of</strong> study– Information sheet <strong>and</strong> consent form– How much detail?<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
6. Informed consent• For research to be ethical, individuals should maketheir own decision about whether they want toparticipate or continue participating in research.• This is done through a process <strong>of</strong> informed consent inwhich individuals– (1) are accurately informed <strong>of</strong> the purpose, methods,risks, benefits, <strong>and</strong> alternatives to the research,– (2) underst<strong>and</strong> this information <strong>and</strong> how it relates totheir own clinical situation or interests, <strong>and</strong>– (3) make a voluntary decision about whether toparticipate.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
7. Respect for potential <strong>and</strong> enrolledsubjects• Individuals should be treated with respect from thetime they are approached for possible participation—even if they refuse enrollment in a study—throughouttheir participation <strong>and</strong> after their participation ends.• This includes:– Respecting their privacy <strong>and</strong> keeping their privateinformation confidential.– Respecting their right to change their mind, to decidethat the research does not match their interests, <strong>and</strong> towithdraw without penalty.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Respect for potential <strong>and</strong> enrolled subjects– Informing them <strong>of</strong> new information that might emerge inthe course <strong>of</strong> research, which might change theirassessment <strong>of</strong> the risks <strong>and</strong> benefits <strong>of</strong> participating.– Monitoring their welfare <strong>and</strong>, if they experienceadverse reactions, untoward events, or changes inclinical status, ensuring appropriate treatment <strong>and</strong>,when necessary, removal from the study.– Informing them about what was learned from theresearch.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Do we need clinical trials?<strong>The</strong> benefit <strong>of</strong> some therapies areobvious!
Evidence vs Eminence Based Medicine• We need good research to advance science<strong>The</strong> Star Dec 12 2010<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Ideas & Trends; Sham Surgery Returns As a<strong>Research</strong> Tool• In 1939, to treat angina, an surgeon named Fieschi devised a simpletechnique. Reasoning that increased blood flow to the heart would easehis patients' pain, he made tiny incisions in their chests <strong>and</strong> tied knotsin two arteries. <strong>The</strong> results were spectacular. Three quarters <strong>of</strong> allpatients improved.'' One third were cured.‖• Two decades later, the National Institutes <strong>of</strong> Health paid a youngcardiologist in Seattle, Dr. LA. Cobb, to conduct a novel test <strong>of</strong> theFieschi technique. Dr. Cobb operated on 17 patients. Eight had theirarteries tied; the other nine got incisions, nothing more. In 1959, theNEMJ published his findings: the phony operations worked just as wellas the real thing.• That was beginning <strong>of</strong> the end <strong>of</strong> the procedure, known as internalmammary artery ligation; within two years, it became a footnote in themedical history texts. It was also the beginning <strong>and</strong> the end, apparently,for sham surgery in this country. By the early 1970's, an ethicsrevolution had transformed human experiments, <strong>and</strong> the idea <strong>of</strong> surgeryas placebo was unthinkable.<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
High dose chemotherapy in Breast CancerPeters WP et al J Clin Oncol 1: 1132-1143. © 1993<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
What we WANT from research<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
What we DON’T want<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
AUDIT FINDINGS – Breast trial• No signed informed consent forms for patientsparticipating in the trial• <strong>The</strong> trial was not approved by the University's InstitutionalReview Board.• <strong>The</strong> study shows little evidence <strong>of</strong> r<strong>and</strong>omization• <strong>The</strong> study protocol was written nine years after the studywas started, <strong>and</strong> only after the investigation intoBezwoda's 1999 study was begun<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
AUDIT FINDINGS (2)• <strong>The</strong>re were at least three possibletreatment-related deaths althoughthe paper stated there were "notreatment-related deaths"• Records for 29 <strong>of</strong> the 90 patientscould not be located• <strong>The</strong>re were insufficient records formany patients, <strong>and</strong> some patientswere treated with regimens <strong>and</strong>hormonal agents not consistentwith the published information<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
<strong>The</strong>re are many whomistrust <strong>Medical</strong> <strong>Research</strong><strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Anti-arrythmic drugs• Flicanide an anesthetic agent was found to help incontrolling arrythmias.• Phase II results indicated excellent control <strong>of</strong>arrythmias• As arrythmias was thought to be a prime cause <strong>of</strong>cardiac death, controlling arrythmias should lead tobetter cardiac outcome.• Flicanide was prescribed in increasing numbers.• A placebo controlled trial was completed <strong>and</strong> shouldmore cardiac deaths in treatment arm<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
It is still happening!!<strong>Ethics</strong> <strong>and</strong> regulation <strong>of</strong> clinical trials
Good clinical research is necessary toadvance our knowledge base in medicineEthical research ensures theprotection <strong>of</strong> subjects whovolunteer to scientific research
In god we trust, ….Everyone else pays cashIn god we trust, … everyone else needsmonitoring
THANK YOU