Critical Illness Claim Form - ACE Group
Critical Illness Claim Form - ACE Group
Critical Illness Claim Form - ACE Group
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
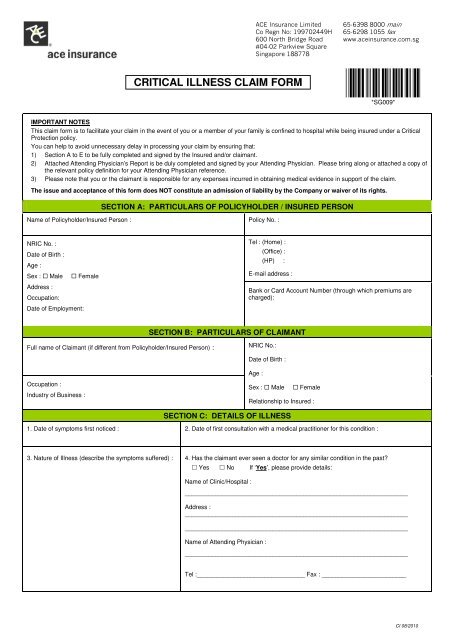
!"#$%&'( ')***CRITICAL ILLNESS CLAIM FORM+",** +"*++-.&&&/ / /*SG009*IMPORTANT NOTESThis claim form is to facilitate your claim in the event of you or a member of your family is confined to hospital while being insured under a <strong>Critical</strong>Protection policy.You can help to avoid unnecessary delay in processing your claim by ensuring that:1) Section A to E to be fully completed and signed by the Insured and/or claimant.2) Attached Attending Physician’s Report is be duly completed and signed by your Attending Physician. Please bring along or attached a copy ofthe relevant policy definition for your Attending Physician reference.3) Please note that you or the claimant is responsible for any expenses incurred in obtaining medical evidence in support of the claim.The issue and acceptance of this form does NOT constitute an admission of liability by the Company or waiver of its rights.SECTION A: PARTICULARS OF POLICYHOLDER / INSURED PERSONName of Policyholder/Insured Person : Policy No. :NRIC No. :Date of Birth :Age :Sex : Male FemaleAddress :Occupation:Date of Employment:Tel : (Home) :(Office) :(HP) :E-mail address :Bank or Card Account Number (through which premiums arecharged):SECTION B: PARTICULARS OF CLAIMANTFull name of <strong>Claim</strong>ant (if different from Policyholder/Insured Person)NRIC No.:Date of Birth :Age :Occupation :Industry of Business :Sex : Male FemaleRelationship to Insured :SECTION C: DETAILS OF ILLNESS1. Date of symptoms first noticed : 2. Date of first consultation with a medical practitioner for this condition :3. Nature of <strong>Illness</strong> (describe the symptoms suffered) : 4. Has the claimant ever seen a doctor for any similar condition in the past? Yes No If ‘Yes’, please provide details:Name of Clinic/Hospital :__________________________________________________________________Address :____________________________________________________________________________________________________________________________________Name of Attending Physician :__________________________________________________________________Tel :________________________________ Fax : _________________________CI 08/2010
5. Name of Hospital : 6. Period of Hospitalization :From : a) ________________________ To : _______________________b) ________________________ _______________________c) ________________________ _______________________7. If claimant to whom this claim relates is/was hospitalized outside Singapore. Please advise :a) <strong>Claim</strong>ant’s usual Address in Overseas : b) Purpose of Overseas Trip :c) Duration of Overseas Trip : d) Name & Address of Hospital & usual Attending Physician and Telephone & Fax No.SECTION D: ANY OTHER INSURANCESAre you claiming from any other insurance company or other insurance company or other sources in respect of this condition?If Yes, please state :Name of Insurance Company Policy No. Amount of Benefits Date Insurance EffectedSECTION E: GENERAL DETAILSHave any of your blood relatives suffered from a similar or related illness? If Yes, please give full details.Relationship of kin Nature of illness Date of diagnosis1) I/We do solemnly and sincerely declare that the foregoing particulars are true and correct in every detail and I/we agree that I/we have madeor in any further declaration in respect of the said claim shall make any false or fraudulent statements of suppress conceal or falsely stateany material fact whatsoever the Policy shall be void and all rights to recover thereunder in respect of past or future claims shall be forfeited.2) I/We hereby authorize and hospital physician, other person who has attended or examined me/us, to furnish the company, or its authorizedrepresentatives, any and all information with respect to any illness or injury, medical history, consultation, prescriptions or treatment, andcopies of all hospital or medical records . A photostatic copy of this authorization shall be considered as effective and valid as the original.Signature of Insured : ___________________________Date : ______________________Signature of Insured Person : _____________________Date : ______________________CI 08/2010
!"#$%&'( ')****+",** +",++-.&&&/ / /CRITICAL PROTECTION CLAIM<strong>Claim</strong>ant’s Attending Physician’s ReportThe issue and acceptance of this form does NOT constitute an admission of liability by the Company or waiver of its rights.Name of claimant :I/C NO.This <strong>Claim</strong>ant has submitted a claim in relation to the following illness : (Please tick [] in the appropriate box)<strong>Critical</strong> ConditionsSections to be completed:1. Amyotrophic Lateral Sclerosis 1, 2, 3 & 342. Aplastic Anaemia 1, 2, 4 & 343. Bacterial Meningitis 1, 2, 5 & 344. Benign Brain Tumour 1, 2, 6 & 345. Blindness 1, 2, 7 & 346. Cancer 1, 2, 8 & 347. Coma 1, 2, 9 & 348. Coronary Artery Bypass Surgery 1, 2, 10 & 349. Fulminant Viral Hepatitis 1, 2, 11 & 3410. Heart Valve Replacement 1, 2, 12 & 3411. Kidney Failure 1, 2, 13 & 3412. Liver Failure 1, 2, 14 & 3413. Loss of Hearing 1, 2, 15 & 3414. Loss of Limbs 1, 2, 16 & 3415. Loss of Speech 1, 2, 17 & 3416. Major Burns 1, 2, 18 & 3417. Major Organ Transplantation 1, 2, 19 & 3418. Motor Neuron Disease 1, 2, 20 & 3419. Muscular Dystrophy 1, 2, 21 & 3420. Myocardial Infarction 1, 2, 22 & 34 21. Paralysis 1, 2, 23 & 3422. Parkinson’s Disease 1, 2, 24 & 3423. Poliomyelitis 1, 2, 25 & 3424. Primary Pulmonary Arterial Hypertension 1, 2, 26 & 3425. Progressive Bulbar Palsy 1, 2, 27 & 3426. Progressive Muscular Atrophy 1, 2, 28 & 3427. Severe Brain Damage 1, 2, 29 & 3428. Stroke 1, 2, 30 & 34 29. Surgery to Aorta 1, 2, 31 & 3430. Terminal <strong>Illness</strong> 1, 2, 32 & 3431. Total and Permanent Disability 1, 2, 33 & 34CI 08/2010
SECTION 1GENERAL INFORMATION1. Are you the <strong>Claim</strong>ant’s usual medical physician? Yes NoIf Yes, do you keep full record of all his consultations? Yes No2. When you were first consulted for this illness? _____________________(DD/MM/YY)3. What were the symptoms complained by the <strong>Claim</strong>ant?__________________________________________________________________________________________________________________________________________________________4. For how long had the <strong>Claim</strong>ant been experiencing these symptoms?__________________________________________________________________________________________________________________________________________________________5. For how long do you think these symptoms had lasted?__________________________________________________________________________________________________________________________________________________________6. What is the diagnosis?_____________________________________________________________________________7. When is the diagnosis made?_________________________________(DD/MM/YY)When is the <strong>Claim</strong>ant first aware of the diagnosis _________________(DD/MM/YY)8. Is this diagnosis related to any previous illnesses? Yes NoIf Yes, please give dates of consultation and the illnesses being diagnosed_________________________________________________________________________________________________________________________________________________________9. If a surgery is performed, when was it carried out? ________________ (DD/MM/YY)10. Is there any factor(s) such as the <strong>Claim</strong>ant’s family medical history which would haveincreased the risk of the <strong>Claim</strong>ant’s illness? Yes NoIf Yes, please give details on the family medical history._______________________________________________________________________________________________________________________________________________________________________________________________________________________________________TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side.SECTION 2 DETAILS OF DIAGNOSIS1. Please provide full and exact details of the diagnosis and its clinical records.____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________CI 08/2010
SECTION 3AMYOTROPHIC LATERAL SCLEROSISDefinition: Amyotrophic Lateral Sclerosis means unequivocal diagnosis by a consultantneurologist confirming well defined neurological deficit with persistent signs of involvement of thespinal nerve columns and the motor centers in the brain and with specific weakness and atrophyof the muscles of the extremities.1. How is the diagnosis made and by whom?____________________________________________________________________2. Please describe the permanent neurological deficit.____________________________________________________________________3. ____________________________________________________________________4. Is there involvement of spinal column and motor centre of the brain? Yes No5. Is there atrophy of muscles of the extremities? Yes No6. Please provide each copy of investigation result and laboratory evidence including(but not limited to) X-Ray, CT Scan, MRI etc.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideSECTION 4APLASTIC ANAEMIADefinition: Aplastic Anaemia means chronic persistent bone marrow failure which results inanaemia, neutropenia and thrombocytopenia requiring treatment with at least one of thefollowing:i. blood product transfusion;ii. immunosuppressive agents; oriii. bone marrow transplantation.1. Please describe the extent of the disease.________________________________________________________________________________________________________________________________________2. What is the haemoglobin level, red cell count, white cell count and platelet count?____________________________________________________________________3. What is the nature of treatment?a. blood product transfusion Yes Nob. immunosuppressive agents Yes Noc. bone marrow transplantation Yes No4. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT Scan, other imaging procedures etc.SECTION 5BACTERIAL MENINGITISDefinition: Bacterial Meningitis means bacterial meningitis causing inflammation of themembranes of the brain or spinal cord resulting in permanent neurological deficit persisting for atleast six (6) consecutive months, such diagnosis to be confirmed by a licensed consultantneurologist.1. Please specify is there any underlying cause/predisposition e.g. Diabetes, Cancer, HIVleading to this disease.________________________________________________________________________2. Has the <strong>Claim</strong>ant returned to normal activities? Yes NoIf yes, please advise the date of return _______________________(DD/MM/YY)3. What are the patient’s present limitations both physical and mental?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________4. Were there any neurological deficit which lasted for more than 3 months? Yes No5. What are the neurological deficits?________________________________________________________________________________________________________________________________________________________________________________________________________________________6. Are these neurological deficits permanent? Yes No7. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT Scan, other imaging procedures, CSF culture etc.CI 08/2010
SECTION 6BENIGN BRAIN TUMORDefinition: Benign Brain Tumor means a non-cancerous tumor in the brain which eitherrequires surgical excision or causes significant permanent neurological deficit persisting for atleast six (6) consecutive months. For the avoidance of doubt, the following shall not fall within thedefinition of Benign Brain Tumor and are not covered under this Policy:i. cysts, granulomas, malformations in, or of the arteries or veins of the brain; orii. haematomas and tumors in the pituitary gland or spine.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side.1. Please describe the extent and nature of the Benign Brain Tumor.a. Was surgical excision performed? Yes Nob. Are there any significant permanent neurological deficit? Yes Noc. Please provide detailed location of the tumor.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Is the tumor in the brain confirmed by imaging studies such as CT Scan or MRI? Yes No3. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT Scan, other imaging procedures etc.SECTION 7BLINDNESSDefinition: Blindness means total and irrecoverable loss of all sight of both eyes due to injury ordisease. The diagnosis must be clinically confirmed by a licensed medical specialist.1. What is the cause of Blindness?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Please describe the extent of the blindnessa. What is the visual actuity of both eyes at present?Left: ___________________________ Right: ___________________________b. What forms of treatment were rendered?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________c. Will further surgery improve his/her sight? Yes NoIf Yes, what kind of surgery will be necessary.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report including (but not limited to)ophthalmologist’s reports, CT scans etc.CI 08/2010
SECTION 8CANCERDefinition: Cancer means the presence of uncontrolled growth and spread of malignant cellsand invasion of tissue. Incontrovertible evidence of such invasion of tissue or definite histology ofa malignant growth must be produced. It includes leukaemia, Hodgkin’s Disease and invasivemelanoma which exceeds a depth of 0.75 millimetre. For the avoidance of doubt, the followingshall not fall within the definition of ‘Cancer’ and are not covered under this Policy :i. localized/non-invasive carcinoma in situ;ii. localized/non-invasive tumors showing only early malignant changes;iii. tumors in the presence of Human Immunodeficiency Virus;iv. Karposi’s Sarcoma and AIDS related cancers; andv. any skin cancer other than malignant melanoma exceeding 0.75 mm indepth.1. Please describe the extent of the disease.a. How was the diagnosis confirmed?TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side.________________________________________________________________________________________________________________________________________________b. What is the histological diagnosis of the disease?________________________________________________________________________________________________________________________________________________c. What is the staging of the Tumor? _________________________________d. Was the disease completely localized? Yes Noe. Was there spread of malignant cells to lymph nodes or distant parts of the body? Yes NoIf Yes, please describe degree of regional nodal involvement, and/or spread to distantparts of the body________________________________________________________________________________________________________________________________________________________________________________________________________________________2. What is the nature of treatment? Surgical Chemotherapy Radiotherapy PalliativePlease provide details of procedure(s)________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Investigations :a. Was a biopsy of the tumor performed? Yes No4. Please provide each copy of related report including (but not limited to) laboratoryevidence including (but not limited to) biopsy reports, cytology reports, surgical report,X-rays, CT Scan, other imaging studies etc.SECTION 9COMADefinition: Coma means a state of unconsciousness with no reaction to external stimuli orinternal needs, persisting continuously with the use of life support systems for a period of at leastninety-six (96) hours, and resulting in a neurological deficit which in the opinion of the Company’sChief Medical Officer is of the permanent nature.Coma resulting directly from alcohol or drug abuse is excluded.1. Please describe the extent of the coma.a. Is there any reaction or response to external stimuli or internal needs persistingcontinuously with the use of a life support system for at least 96 hours? Yes No2. What was the cause of the coma?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report including (but not limited to) laboratoryevidence including (but not limited to) surgical report, X-rays, CT Scan, other imagingstudies etc.CI 08/2010
SECTION 10CORONARY ARTERY BYPASS SURGERYDefinition: Coronary Artery Bypass Surgery means open heart surgery undergone to correctnarrowing or blockage of two or more coronary arteries by the use saphenous vein grafts orinternal mammary grafting. Angiographic evidence of the underlying disease must be provided.For the avoidance of doubt, non-surgical procedures such as balloon angioplasty or lasertechniques shall not fall within the definition of ‘Coronary Artery Bypass Surgery’ and are notcovered under this Policy.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side.1. Please describe the extent of the disease.a. Which arteries are involved and what is the degree of narrowing (%) in respectof each involved artery?________________________________________________________________________________________________________________________________________________________________________________________________________________________b. Was coronary arteriography performed? Yes NoWhat was the result of coronary angiography?________________________________________________________________________________________________________________________________________________________________________________________________________________________2. What is the nature of treatment?a. Was open heart surgery performed? Yes Nob. If Yes, state the number and sites of grafts inserted.________________________________________________________________________________________________________________________________________________c. What other forms of treatment were rendered?________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report and laboratory evidence including(but notlimited to) Thallium scan, X-Rays, CT sacan, surgical report, any other imagingstudies, angiograms etcSECTION 11FULMINANT VIRAL HEPATITISDefinition: Fulminant Viral Hepatitis means a submassive to massive necrosis of the livercaused by the hepatitis virus, leading precipitously to liver failure. All following must bediagnosed :i. a rapidly decreasing liver size;ii. necrosis involving entire lobules, leaving only a collagen reticular framework;iii. rapidly degenerating liver function tests; andiv. deepening jaundice.Liver failure due to other causes e.g. alcohol induced or drugs abused are excluded.1. Please describe the extent of the illness.a. What is the diagnosis and etiological agent________________________________________________________________________________________________________________________________________________________________________________________________________________________b. Is there a rapidly decreasing liver size? Yes Noc. Is there a submassive to massive necrosis of the liver? Yes Nod. Is there a rapidly determination of liver function? Yes Noe. Was there deepening jaundice? Yes No2. What is the current condition of the Insured?________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each of related report and laboratory evidence including (but notlimited to) liver function test, coagulation profile, ultrasound, MR and other imagingstudies etc.CI 08/2010
SECTION 12HEART VALVE REPL<strong>ACE</strong>MENTDefinition: Heart Valve Replacement means the actual undergoing of the replacement of oneor more heart valves with artificial valves due to stenosis or incompetence. For the avoidance ofdoubt, heart valve repair and valvotomy shall not fall within the definition of ‘Heart ValveReplacement’ and are not covered under this Policy.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side.1. Please describe the extent of the disease.a. What was the cause of the heart valve defect?________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Was open heart surgery performed?If Yes, state the surgical procedure used to correct the valvular problem.________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report and laboratory evidence including (but notlimited to) surgical reports, X-rays, CT Scans, any other imaging studies, angiogramsetc.SECTION 13KIDNEY FAILUREDefinition: Kidney Failure means end stage renal disease which presents chronic andirreversible loss of function of both kidneys as a result of which the Insured Person is required toundergo regular renal dialysis or kidney transplantation.1. Please describe the extent of the kidney failure.a. Has the Insured’s renal disease reach end stage? Yes Nob. Are both kidneys involved? Yes Noc. Is the Insured undergoing regular peritoneal dialysis or haemodialysis? Yes No If Yes, start date : _________________ (DD/MM/YY)d. Has renal transplantation been advised or performed? Yes No2. Please provide each copy of related report and laboratory evidence including (but notlimited to) blood test, X-rays, cystoscopy report, pyelograms, ultrasound, biopsyreports, surgical procedures and etc.SECTION 14LIVER FAILUREDefinition: Liver Failure means chronic end stage liver failure which is permanent andirreversible and characterized by permanent jaundice, oesophageal varices, ascites and hepaticencephalopathy. For the avoidance of doubt, liver disease secondary to drug or alcohol abuseshall not fall within the definition of ‘Liver Failure’ and is not covered under this Policy.1. Please describe the extent of the disease.________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Has the Insured’s liver failure reach end stage? Yes NoIf yes,a. Is there permanent jaundice? Yes Nob. Is there ascities? Yes Noc. Is there hepatic encephalpoathy? Yes Nod. Are there oesophageal varices? Yes No3. What was the cause of the chronic liver disease?________________________________________________________________________________________________________________________________________________________________________________________________________________________4. What is the current condition of the Insured?________________________________________________________________________________________________________________________________________________5. Please provide each copy of related report and laboratory evidence including (but notlimited to) liver function tests, ultrasound, MR, other imaging studies etc.CI 08/2010
SECTION 15LOSS OF HEARINGDefinition: Loss of Hearing means total, bilateral and irreversible loss of hearing in both earsfor all sounds as a result of acute sickness or accident. Medical evidence must be supplied by alicensed. (Ear, Nose and Throat) specialist to confirm the loss of hearing and must includeaudiometric and sound-threshold test.1. Please describe the extent of the loss of hearing.________________________________________________________________________________________________________________________________________________a. Was the diagnosis confirmed by an audiometric and sound-threshold test? Yes Nob. Is the loss of hearing considered total and irreversible? Yes No2. What was the cause of the loss of hearing?________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report and laboratory evidence including (but notlimited to) audiometric, sound-threshold reports, X-rays, surgical reports etc.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideSECTION 16LOSS OF LIMBSDefinition: Loss of Limbs means loss by complete physical severance from the body of two (2)or more limbs where severance is above the wrist or ankle joint.1. What was the cause?________________________________________________________________________________________________________________________________________________2. Which limbs were involved?________________________________________________________________________3. At which part of the limb did the severance take place?________________________________________________________________________4. Is this loss of limb permanent?________________________________________________________________________5. Please provide each copy of related report and laboratory evidence including (but notlimited to) surgical report, X-Ray etc.SECTION 17LOSS OF SPEECHDefinition: Loss of Speech means total and irrecoverable loss of the ability to speak due todamage to vocal cords which must be established for a period of twelve (12) consecutivemonths. Medical evidence is to be supplied by a licensed (Ear, Nose and Throat) specialist toconfirm permanent loss of speech and damage to vocal cords. For avoidance of doubt, loss ofspeech directly or indirectly due to psychiatric related causes shall not fall within the definition of ‘Loss of Speech’ and is not covered under this Policy.1. Please describe the extent of loss of speech.________________________________________________________________________________________________________________________________________________a. Duration of the loss of speech?________________________________________________________________________b. Is the loss of speech considered total and irrecoverable? Yes No2. Was the loss of speech due to vocal cord damage? Yes No3. Please provide each copy of related reports(Ear, Nose and Throat) and laboratoryevidence including X-rays, surgical reports etc.SECTION 18MAJOR BURNSDefinition: Major Burns means burns which results in full thickness skin destruction of at leasttwenty percent (20%) of the total skin area of the body of the Insured Person.1. Please describe the extent of the major burns.________________________________________________________________________a. Is the burns considered Third Degree Burns? If so, describe the extent (inpercentages) of the burns covering the body surface.________________________________________________________________________2. What was the cause of the major burns?________________________________________________________________________3. Please provide each copy of related report including (but not limited to) surgicalreports etc.CI 08/2010
SECTION 19MAJOR ORGAN TRANSPORTATIONDefinition: Major Organ Transplantation means the actual undergoing of a transplant of theheart, lung, liver, pancreas or bone marrow as a recipient. For the avoidance of doubt,transplantation of isolated pancreatic islets shall not fall within the definition of of ‘Major OrganTransplantation’ and is not covered under this Policy.1. What is the diagnosis before transplant?________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Please describe the transplant operation.a. Which part of the organ is involved?________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report and laboratory evidence including (but notlimited to) surgical report, X-rays, CT Scans, ultrasound or other imaging studies,ECG, surgical etc.SECTION 20MOTOR NEURON DISEASEDefinition: Motor Neuron Disease means unequivocal diagnosis of Motor Neuron Disease by aconsulting neurologist supported by obvious and definitive evidence of appropriate and relevantneurological signs with permanent neurological deficits.1. Please describe the extent of the disease.________________________________________________________________________________________________________________________________________________________________________________________________________________________a. Are there definitive evidence of permanent neurological deficits resulting from thedisease? Yes NoIf Yes, please elaborate.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT scan, other imaging procedures etc.SECTION 21MUSCULAR DYSTROPHYDefinition: Muscular Dystrophy means a hereditary muscular dystrophy confirmed by aconsulting neurologist resulting in the inability of the Insured Person to perform withoutassistance in respect of three or more of the following:i. bathingii. dressingiii. using the lavatoryiv. eatingv. movement in or out of bed or chair1. Is the <strong>Claim</strong>ant able to perform the following activities independently without anyassistance from any other sources:-a. Ability to wash and bathe Yes Nob. Ability to dress/undress Yes Noc. Ability to attend to toilet needs Yes Nod. Ability to eat Yes No2. Is there evidence of sensory disturbance, abnormal cerebrospinal fluid, or diminishedtendon reflex? If Yes, please describe findings.________________________________________________________________________________________________________________________________________________3. Which are the muscles involved?________________________________________________________________________________________________________________________________________________4. Was the diagnosis confirmeda. by electromyogram? Yes Nob. by muscle biopsy? Yes No5. Please provide each copy of related report and laboratory evidence including (but notlimited to) all neurological reports, electromyogram studies, muscle biopsy etc.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideCI 08/2010
SECTION 22MYOCARDIAL INFARCTIONDefinition: Myocardial Infarction means the death of a portion of the heart muscle as a resultof inadequate blood supply to the areas. The diagnosis must be based on all of the following:i. a history of typical chest pain;ii. new electrocardiographic changes; andiii. elevation of cardiac enzyme levels.1. Was he admitted to the Coronary Care Unit/Intensive Care Unit (CCU/ICU)? Yes NoIf Yes, please state date of admission and duration of stay in CCU/ICU.____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Was any thrombolytic therapy given? Yes No3. Please describe the heart attack_______________________________________________________________________________________________________________________________________________________________________________________________________________________________________a. When did the attack happen? _________________________ (DD/MM/YY)b. Was there a current history of typical chest pain? Yes Noc. Was there a serial elevation of cardiac enzymes documented? Yes Nod. Were there any changes in the ECG typical of an acute myocardial infarction? Yes Noe. For how long did this acute symptoms exist?_____________________________________________________________________________f. Has the <strong>Claim</strong>ant return to normal activities? Yes NoIf Yes, please advise the date: _______ _________________ (DD/MM/YY)g. What is the <strong>Claim</strong>ant’s present limitation, both physical and mental?_____________________________________________________________________________4. Was there death of a portion of the hear muscle? Yes No5. Please provide each copy of report including (but not limited to) resting ECGs, exercisestress tests, enzymes assays, isotope studies, imaging (echocardiograms), coronaryangiography etc.SECTION 23PARALYSISDefinition: Paralysis means complete and permanent loss of use of two (2) or more limbsthrough neurological damage for the remainder of the Insured Person’s life.1. Please describe the extent of the paralysis.____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________a. Which areas were involved?_______________________________________________________________________________________________________________________________________________________________________________________________________________________________________b. Is the loss of use of the involved limbs considered complete and permanent? Yes No If Yes, please provide basis for diagnosis_______________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. What was the cause of the paralysis?_______________________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related report and laboratory evidence including (but notlimited to) neurological reports, X-rays, CT scans, MR, other imaging studies, surgicalreports etc.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideCI 08/2010
SECTION 24PARKINSON’S DISEASEDefinition : Parkinson’s Diseases means unequivocal diagnosis of Parkinson’s Disease by aconsultant neurologist where all the following conditions of the disease are fulfilled :i. it cannot be controlled with medication;ii. it is idiopathic in nature (all other forms of Parkinsonism are excluded);iii. it shows signs of progressive impairment; andiv. the inability of the Insured Person to perform without assistance in respect ofthreev. or more of the following: bathing, dressing, using the lavatory, eating andmovementvi. in or out of bed or a chair.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side1. Please describe the extent of the disease.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________a. What is the cause of the disease?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Is the <strong>Claim</strong>ant able to perform the following activities independently without anyassistance from any other sources:-a. Ability to wash and bathe Yes Nob. Ability to dress/undress Yes Noc. Ability to attend to toilet needs Yes Nod. Ability to eat Yes Noe. Ability to move in or out of a bed or a chair Yes No3. Please provided each copy of related report and laboratory evidence including (but notlimited to) radiological procedure, CT scanning, other imaging procedures etc.SECTION 25POLOIOMYELITISDefinition : Poliomyelitis means unequivocal diagnosis by a consultant neurologist of infectionby the polio virus leading to paralytic disease as evidenced by impaired motor function orrespiratory weakness. Cases other than the foregoing shall not be regarded as poliomyelitis. Forthe avoidance of doubt, poliomyelitis not involving paralysis and other cases of paralysis shall notfall within the definition of ‘Poliomyelitis’ and are not covered under this Policy.1. How was the diagnosis made and by whom?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Is there impaired motor function or respiratory weakness? Yes No3. Are there any other causes of paralysis or weakness? Yes NoIf Yes, please elaborate.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________4. Please provide each copy of related report and laboratory including (but not limited to)X-rays, CT Scans, MRI and investigation results etc.CI 08/2010
SECTION 26PRIMARY PULMONARY ARTERIAL HYPERTENSIONDefinition : Primary Pulmonary Arterial Hypertension means primary pulmonary arterialhypertension as established by clinical and laboratory investigations include cardiaccatheterization. All of the following diagnostic criteria must be met :i. dyspnea and fatigueii. increase left atrial pressure (by at least 20 units);iii. pulmonary resistance of at least 3 units above normal;iv. pulmonary artery pressures of at least 40 mm Hg;v. pulmonary wedge pressure of at least 8 mm Hg; andvi. right ventricular end-diastolic pressure of at least 8 mm Hg; andvii. right ventricular hypertrophy, dilation and signs of right heart failure anddecompensation.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand side1. What was the extent of the primary pulmonary arterial hypertension?________________________________________________________________________________________________________________________________________________a. Was there dyspnea and fatigue Yes Nob. Was there increase left atrial pressure of at least at least 20 units or more? Yes Noc. Was there pulmonary resistance of at least 3 units above normal? Yes Nod. Was there pulmonary artery pressure of at least 40mm Hg? Yes Noe. Was there pulmonary wedge pressure of at least 8mm Hg? Yes Nof. Was there right ventricular end-diastolic pressure of at least 8mm Hg? Yes Nog. Was there right ventricular hypertrophy, dilation and signs of right heart failure anddecompensation? Yes No2. in your medical opinion, what was the cause of the primary pulmonary arterialhypertension?________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Please provide each copy of related reports and laboratory evidence including (but notlimited to) ECGs, X-rays, ultrasound, cardiac catherization, pulmonary function studiesetc.SECTION 27PROGRESSIVE BULBAR PALSYDefinition: Progressive Bulbar Palsy means degenerative wasting of the muscles including thebulbar muscles as diagnosed by a consultant neurologist and agreed to by the Company’s ChiefMedical Officer.1. How was the diagnosis made and by whom?________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Is there degenerative wasting of muscles including bulbar muscles? Yes No3. Please provide each copy of related report and laboratory evidence including (but notlimited to) investigation results, X-ray, CT Scanning, MRI etc.SECTION 28PROGRESSIVE MUSCULAR ATROPHYDefinition: Progressive Muscular Atrophy means involving the wasting of muscles andincreased spasticity as diagnosed by a consultant neurologist and agreed by theCompany’s Chief Medical Officer.1. How was the diagnosis made and by whom?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Is there wasting of muscles? Yes No3. Is there increased spasticity of muscles? Yes No4. Please provide each copy of related report and laboratory evidence including (but notlimited to) investigation results, X-ray, CT Scanning, MRI etc.CI 08/2010
SECTION 29SEVERE BRAIN DAMAGEDefinition: Severe Brain Damage means impairment or loss of intellectual capacity as a resultof brain damage sustained in an accident, following which permanent and constant supervisionor assistance is required to maintain existence of the Insured Person.1. Date of Accident _________________ (DD/MM/YY)2. What was the injury to the brain?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________3. Was the brain damage directly caused by the accident? Yes NoIf No, please elaborate.________________________________________________________________________________________________________________________________________________________________________________________________________________________4. Is there permanent loss of intellectual capacity such that he requires constantsupervision or assistance? Yes No5. Please provide each copy of related report and laboratory evidence including (but notlimited to) investigation results, X-ray, CT Scanning, MRI etc.SECTION 30STROKETO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideDefinition: Stroke means any cerebrovascular incident producing neurological sequelae lastingfor more than twenty four (24) hours and including infarction of brain tissue, haemorrhage of anintracranial vessel, or embolization from an extra cranial source. Evidence of permanentneurological deficit must be produced. For the avoidance of doubt, transient ischemic attacksshall not fall within the definition of ‘Stroke’ and is not covered under this Policy.1. What is the pathological diagnosis?________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Please describe the initial episode.a. Date of episode _________________ (DD/MM/YY)b. Nature of episode _________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________c. Duration of the acute symptoms ___________________________________d. Date of return to normal activities _______________________ (DD/MM/YY)3. Please comment on any neurological sequelae which lasted more than 24 hours.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________a. Are these sequelae permanent? Yes Nob. How long have these sequelae been present since the initial episode?Please give the number of days/months________________________________d. What are the Insured’s present limitations both physical and mental?________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________4. Has there been an infarction of brain tissue, cerebral haemorrhage, or embolizationform an extracranial source? Yes No5. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT Scanning, other imaging procedures, etc.CI 08/2010
SECTION 31SURGERY OF AORTADefinition: Surgery to Aorta means the actual undergoing of an open heart surgery fordisease of the aorta needing excision and surgical replacement of the diseased aorta witha graft. For the purposes of this definition, aorta shall mean the thoracic and abdominalaorta, but not its branches. A surgery performed to cure traumatic injury to the aorta shallnot be regarded as ‘Surgery to Aorta’ and is not covered under this Policy.1. Please describe the extent of the disease.________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Was excision and surgical replacement of the diseased aorta with a graft performedthrough open surgery? Yes No3. Please provide each copy of related report and laboratory evidence including (but notlimited to) surgical reports, X-rays, CT scans, any other imaging studies, angiogramsetc.TO: ATTENDING PHYSICIANYou may use the following space if yourequire additional column to answer any ofthe questions as stated on the left hand sideSECTION 32TERMINAL ILLNESSDefinition: Terminal illness means the Insured Person must be suffering from a disease which inthe opinion of a licensed medical consultant and supported by the Company’s Chief MedicalOfficer, is likely to lead to death within six (6) months from the date of notification of a claimunder this Policy.1. Please describe the terminal illness.________________________________________________________________________________________________________________________________________________________________________________________________________________________a. What is the nature of treatment?________________________________________________________________________________________________________________________________________________________________________________________________________________________b. In your opinion is the condition highly likely to lead to death within 6 months? Yes No2. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedures, CT scanning, X-ray, other imaging procedures etc.SECTION 33TOTAL AND PERMANENT DISABILITYDefinition : Total and Permanent Disability means the inability of the Insured Person toengage in any occupation or employment for remuneration or profit as a result of bodily injury orsickness and the inability of the Insured Person to perform without assistance in respect ofthree or more of the following : bathing, dressing, using the lavatory, eating and movement in orout of bed or a chair. The ‘Total and Permanent Disability’ must have continued withoutinterruption for at least six (6) consecutive months, or for such longer period as the Companymay reasonably require to establish that such disability is and will be total, continuous andpermanent for the remainder of the Insured Person’s life.1. What is the cause of the disability?________________________________________________________________________________________________________________________________________________2. Is the Insured Person able to perform the following activities independently without anyassistance from any other sources:-a. Ability to wash and bathe Yes Nob. Ability to dress/undress Yes Noc. Ability to attend to toilet needs Yes Nod. Ability to eat Yes Noe. Ability to move in or out of a bed or a chair Yes No3. Is this disability total, continuous and permanent for the remainder of the InsuredPerson’s life? Yes NoIf Yes, please elaborate.________________________________________________________________________________________________________________________________________________4. Please provide each copy of related report and laboratory evidence including (but notlimited to) radiological procedure, CT scanning, other imaging procedures etc.CI 08/2010
SECTION 34DETAILS OF INSURED’S ILLNESS1. Please provide Name, Address and Contact No. of the Doctor(s) who referred the <strong>Claim</strong>ant to you._____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________2. Has the <strong>Claim</strong>ant been suffering from/been treated for any other illness(es)/complaints other than this <strong>Critical</strong> illness? Yes No3. Is there any further information which is in your opinion, will assist us in assessing this claim? Yes NoIf there is, please furnish such information.4. In your opinion, does the patient’s medical condition fulfill our policy definition in respect of the critical illness as diagnosed by you in thisepisode? Yes NoTO BE COMPLETED BY ATTENDING PHYSICIAN / SPECIALISTName of Attending Physician: _______________________________________________________________________________________Qualifications: ___________________________________________________________________________________________________Address of Physician’s Hospital/Clinic: _______________________________________________________________________________________________________________________________________________________________________________________________Signature of Physician with Official Stamp of Hospital/Clinic: ______________________________________ Date: ___________________CI 08/2010