Charlotte H. Smith, MD 2009 TCMS President - Travis County ...
Charlotte H. Smith, MD 2009 TCMS President - Travis County ...
Charlotte H. Smith, MD 2009 TCMS President - Travis County ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
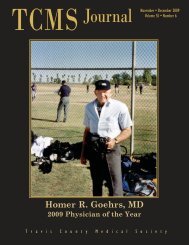
<strong>TCMS</strong> JournalJanuary • February <strong>2009</strong>Volume 55 • Number 1<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong><strong>2009</strong> <strong>TCMS</strong> <strong>President</strong>T r a v i s C o u n t y M e d i c a l S o c i e t y
Bench on Ladybird Lake, Austin. Photo by Ted E. Wallis, <strong>MD</strong>.2 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
<strong>TCMS</strong>Journal<strong>Travis</strong> <strong>County</strong> Medical SocietyOn the Cover<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong><strong>2009</strong> <strong>TCMS</strong> <strong>President</strong>January • February <strong>2009</strong> VOLUME 55 • NUMBER 1FEATURES AND ARTICLESTHE PRESIDENT’S MESSAGEComing Full Circle . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong>HEALTH CARE REFORMThis I Believe . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5Thomas B.Coopwood, <strong>MD</strong>PROJECT ACCESSRaising the Standard of Health . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7Theresa J. Pugh, <strong>MD</strong>Check out<strong>TCMS</strong> eventswww.tcms.comLEGISLATIVE UPDATEHelp Fix Our Broken Health Care System . . . . . . . . . . . . . . . . . . . . . . . . . . .9ON THE COVER<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong>: <strong>2009</strong> <strong>TCMS</strong> <strong>President</strong> . . . . . . . . . . . . . . . . . . . . . .10Merry WheatonTCM ALLIANCEServing Our Community . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13Shelly OzdilPRACTICE MANAGEMENTFailure to Stabilize Before Transfer . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .14TMLT Risk Management DepartmentDEPARTMENTSIn the News . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .14Take 5: Delirium . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .17EDITORIAL:Editor, Owen Winsett, <strong>MD</strong>Managing Editor, Belinda ClarePublication Coordinator, Ron MizeCONTACT: <strong>Travis</strong> <strong>County</strong> Medical Society 4300 N Lamar Blvd.; Austin, Texas 78756; Post Office Box 4679; Austin, Texas 78765Ron Mize (512) 206-1245 or email rmize@tcms.comADVERTISING: Advertising rates and requirements available upon request. <strong>Travis</strong> <strong>County</strong> Medical Society Journal assumes no responsibility for statements made bycontributors. Advertising in the <strong>Travis</strong> <strong>County</strong> Medical Society Journal does not imply approval or endorsement by the <strong>Travis</strong> <strong>County</strong> Medical Society.SECD #277180: <strong>Travis</strong> <strong>County</strong> Medical Society Journal (ISSN 1054-2507) is the official bi-monthly publication of the <strong>Travis</strong> <strong>County</strong> Medical Society and the Seventh Districtof Texas. Periodicals Postage Paid at Austin, Texas. Subscription price $2.00 per year to members. Payment of annual membership dues entitles member to a subscription.POSTMASTER: Send change of address notices to the <strong>Travis</strong> <strong>County</strong> Medical Society Journal; 4300 North Lamar Blvd.; Austin, Texas 78756.MEMBERSHIP: 2,952<strong>TCMS</strong> Journal January • February <strong>2009</strong> 3
FROM THE PRESIDENTComing Full Circle<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong><strong>President</strong>, <strong>Travis</strong> <strong>County</strong> Medical SocietyMay 1975: The case of C.H.A 14 y.o. female presentedto the Brackenridge ERwith a 2 day history ofheadache, neck pain,emesis, diarrhea, and feverafter returning from a highschool band competition in Corpus Christi.Her panicked mother found the girl unresponsiveon the floor of their home andbrought her in the back of the stationwagon to the ER. Unable to carry herinside the hospital, her mother summonedthe staff, who found her lying on thepavement outside of the entrance.Upon assessment, the patient was foundto be in shock with a temperature of 107degrees Fahrenheit, low blood pressure andan elevated WBC suggestive of bacterialinfection. Physical examination was otherwiseunremarkable. Radiographs found noevidence of pneumonia. Cultures of urine,blood and CSF revealed no obvious sourceof infection. No other students that had beenon the band trip on the bus had symptoms ofany illness. Penicillin was administeredintravenously with no improvement. Shortlyafter the penicillin was given, she developed adiffuse, sunburn-like skin rash, followed byextensive desquamation. Presuming apenicillin reaction, a cephalosporin wasadministered intravenously. Shortlythereafter, the patient improved, allowingher to be discharged home one week later.The final diagnosis was “sepsis, undeterminedetiology.”That episode was the first time I hadever been significantly ill. My memory ofit is limited, except from what my parentstold me, from newspaper clippings andfrom cards that were brought home fromthe hospital. This was apparently bignews in Austin, particularly because ofthe early fear that the entire Reagan HighSchool band might come down withspinal meningitis. I was touched to seethat prominent pastors I’d never metfrom churches I’d never attended hadvisited, leaving notes that theircongregations were praying for me.Brackenridge had just opened a brandnew nine story tower, but the ICU wasthe last unit relocated to the newbuilding. Consequently, I was one of thelast patients cared for in the old redbrick building.Seven years later, I was a medicalstudent at Baylor College of Medicine,having dreamed of becoming a physiciansince the sixth grade. During the mandatoryphysical examination for enteringstudents, a heart murmur was found bythe second year medical students. Whenthe attending physician asked if I hadany significant medical history, I toldhim about the episode at Brackenridgeand the lack of a definitive diagnosis. Helater reviewed my medical records andmade a retrospective diagnosis: “ToxicShock Syndrome.”It appeared that I had had one of thefirst cases in the country, before thissyndrome was well known. Dr. TomMcHorse, the young internist caring forme at Brackenridge had saved my life bydoing the exact right thing before therewas a definitive treatment protocol forthis unknown syndrome.In 1986, I returned to Brackenridgeas an intern in the Central Texas MedicalFoundation (CTMF) transitionalprogram. So much had changed. The redbrick building (where I had been treatedin the ICU) was gone. St. David’sMedical Center (where I was born) wasnow a large facility with its own park.Seton Medical Center (where I workedin the lab as a high school student) wasnow a tower. Holy Cross Hospital (whereI did a high school health-professionselective and worked as a physical therapyaide in my pre-med days at UT) wasdestined for demolition. The level ofmedical sophistication in Austin hadimproved and fewer citizens had to go toHouston or Dallas for complex care.What is said about your internshipwas true for me − despite the sleepdeprivation from every-other night call,the busy workload and the steep learningcurve, PGY-1 was the best year of mylife, at least up to that point. Making$13K that year seemed extravagant eventhough it was less than minimum wageconsidering the number of hoursworked. The CTMF faculty and the<strong>Travis</strong> <strong>County</strong> physicians volunteering toeducate us were some of the finestteachers I’d ever encountered. They weretough but encouraging, and their level ofprofessionalism and kindness had a bigimpact on all of us. They allowed (andeven encouraged) me to continue inleadership roles with the TMA andAMA. I developed many wonderful,continued on page 64 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
HEALTH CARE REFORMThis I BelieveThomas B. Coopwood, <strong>MD</strong>That everyone should have access to healthcare. Not a right, just as people have noright to food, housing, clothing, or a job.Understand that I’m no health care expert,administrator, or insurance companyexecutive. I’m just a surgeon who served inthe front lines of providing health care toeveryone, so I can only speak from thisbackground. When I left medical school,physicians were the deciders of the healthcare needs of patients in collaboration withthe patient. By the time I retired, lip servicewas paid to this idea, but hospitals andinsurance companies called the shots andoften patients and physicians got the shortend of the stick.My Grandfather and Father werephysicians in a small town in the dayswhen the profession was highly respected.They gave freely of themselves wheneverand to whomever needed their help.Payment was in cash or produce from thegarden or barnyard. Health care wasn’texpensive then and there was no insurance.Patients received the care they needed whenthey needed it. However medicine wasn’t assophisticated or robust as it is now.All that began to change in the 1940sas companies started to provide health careinsurance and then in the 1960s we gotMedicare and Medicaid. Suddenly therewas another entity, not the patient thatwould pay for the care. This was a boon tothe providers as more and more peoplewere covered and free care decreased. Butwith the increased reimbursement camemedical liability, insurance companies, andthe rapid growth of medical technology.Over time health care expenses have risen somuch that we find our nation in crisis. Manycan’t afford today’s expensive care and even ifthey could there aren’t enough providers.Still, by and large, hospitals andphysicians provide access to care − at least inemergency situations − regardless of abilityto pay. Elective care is often a different story.Many paying patients − Medicare, Medicaidand, even more so the uninsured − havetrouble finding a medical home.Now we are in a fix. Everyone shouldhave access to care, but who should pay forit and who should provide it? Shouldproviders donate their services more andmore as the number unable to pay increases?Maybe insurance companies should beforced to cover everyone in an area regardlessof their ability to pay. Maybe we shouldprovide this access through more governmentprograms raising taxes on the local,state, or national level until all have thisaccess (we would also pay to train a lotmore providers). Or maybe companiesshould be required to pay for the insuranceof all their employees and their families.What can we as a nation do to controlthe rising cost of health care and thelimited access this causes? Should we limitor not pay for new technology, newmedications, or procedures or do we needto look for another way to ration care, aswe must do now? Should we have a twotieredlevel of care with government payingfor “basic care” and the individual paying foranything needed over “basic.” And whodecides what is “basic”? Maybe everyoneshould have “Cadillac” as opposed to“Volkswagen” care. As George Will says,“Americans want 2008 medicine at 1958prices and universal coverage with undiminishedchoice − without mandatory purchasesor government interference with choicesincluding doctor-patient relationships.”This is what we have now, but it is notsustainable. All the payees and providerswill go broke. Or maybe we should notchange the system and continue to rationcare as we do and let the devil take thehindmost. The problem is the cost of careis too high and there are too many that arepriced out of the market.As the national debate continues anddecisions are made, it is just a question ofwhose ox gets gored;− The uninsured limited to basic care− The insured standing in line withthe uninsured: not enoughwilling providers− The taxpayer who foots the bill forhealth care− The physician by taking more cuts inreimbursement− The hospital continuing to providecharity care as well as having more cutsin reimbursements− Big Pharma having to sell all drugs asgeneric or give them away− New innovation not paid for at all orat reduced rate− Employers required to providehealth care insurance for employeesand families− Insurance companies provide morecoverage for less or no premium− Nurses and hospital personnel whowill have to work for less and pay moretaxes.In the end everyone should haveaccess to health care and everyone is goingto feel the pain of providing it. Thereseems to be no easy answer. If thegovernment funds the care there will haveto be massive tax increases or much moredeficit spending.So to me it’s pick your poison: highertaxes, limited access, more charity work, lessincome, fewer jobs. Just about now we needa King Solomon.Thomas B. Coopwood, <strong>MD</strong> is Vice-Chairperson of the <strong>Travis</strong> <strong>County</strong> HealthcareDistrict and a Past <strong>President</strong> of the <strong>TCMS</strong>.<strong>TCMS</strong> Journal January • February <strong>2009</strong> 5
continued from page 4lifelong relationships and friendshipsthat year.Thus it was with sadness when I hadto leave Austin for my Physical Medicineand Rehabilitation residency inHouston. It turned out to be a good tripthough − I met and married a wonderfulsurgery resident, Ames <strong>Smith</strong>, and hadthe opportunity to learn and bementored in one of the best PMRprograms in the country.Flash forward to <strong>2009</strong>Since returning to Austin in 1990 tostart our practices, Ames and I havebecome a family of four, includingZachary (13) and Victoria (6). A big partof our lives now includes balancingwork, marriage, and family.Austin is now a metropolis with morethan 30 hospitals and 3000 physiciansproviding state of the art care that rivalsother big cities. Brackenridge is the busiestlevel two trauma center in the country,with plans to become a level one traumacenter and a neurosciences center ofexcellence. I am now able to offerresources that my SCI patients could notget in many other cities. UTMB-AustinPrograms (formerly CTMF then AMEP)continues to grow in the size, scope, andquality of medical education provided.In so many ways, I have come fullcircle − practicing medicine, teaching,and mentoring in a community that didthe same for me; working atBrackenridge after having been a patientthere. I have served on the <strong>TCMS</strong> Boardwith the physician who saved my life atage fourteen and I’ve treated the pastorwho had prayed for me. I’ve cared for somany people who have been a big part ofmy past. I’m also honored to serve inleadership roles with the <strong>TCMS</strong>, TMA,AMA, and AAPMR − organizationsthat have helped me in my ownprofessional development.What are my hopes for this year? As<strong>TCMS</strong> <strong>President</strong>, I hope I can be asencouraging to you as so many of youhave been to me over the years, especiallyto young physicians starting out andanyone feeling discouraged about thestate of medicine.Most of us would agree that healthcare financing is broken and that changeis needed. With the drumbeat of healthcare reform increasing in Washingtonand in the Texas Legislature, change isinevitable. By working together, we havean opportunity to influence the processin a positive way for our patients and ourprofession. I hope that, together, we will.I encourage you to share with me yourown thoughts, concerns, and hopes.Executive Board<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong>, <strong>President</strong>C. Mark Chassay, <strong>MD</strong>, <strong>President</strong> ElectPhillip C. Collins, <strong>MD</strong>, Immediate Past <strong>President</strong>Brian Sayers, <strong>MD</strong>, Secretary-TreasurerR.Y. Declan Fleming, <strong>MD</strong>, Member At LargeHillary Miller, <strong>MD</strong>, Member At LargePaula S. Oliver, <strong>MD</strong>, Member At LargeAdam J. Schneider, <strong>MD</strong>, Member At LargeSarah I. Smiley, DO, Member At LargeBruce A. Levy, <strong>MD</strong>, JD, Chair, Board of EthicsMichelle A. Berger, <strong>MD</strong>, Delegation RepresentativeStephen S. Clark, <strong>MD</strong>, BTC RepresentativeBoard of EthicsWilliam D. Caldwell, <strong>MD</strong>Toni Funicello, <strong>MD</strong>Bruce A. Levy, <strong>MD</strong>, JD, ChairJeffrey Jekot, <strong>MD</strong>Hillary Miller, <strong>MD</strong>Clifford K. Moy, <strong>MD</strong>Archie Dan <strong>Smith</strong>, <strong>MD</strong>TMA House of DelegatesClifford K. Moy, <strong>MD</strong>, Vice SpeakerTMA Board of TrusteesC. Bruce Malone, <strong>MD</strong>Delegates to AMACharles (Bill) Bailey, <strong>MD</strong>, JDC. Bruce Malone, <strong>MD</strong>Clifford K. Moy, <strong>MD</strong>Alternate Delegates to AMADavid C. Fleeger, <strong>MD</strong><strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong>AMA Board of TrusteesJoseph P. Annis, <strong>MD</strong>AMA Young Physician SectionGoverning CouncilDawn Buckingham, <strong>MD</strong>, Chair-electDelegates to TMAIra Bell, <strong>MD</strong>Michelle A. Berger, <strong>MD</strong>*Robert E. Blais, <strong>MD</strong>Roberta M. Braun, <strong>MD</strong>C. Mark Chassay, <strong>MD</strong>William J. Deaton, <strong>MD</strong>James Eskew, <strong>MD</strong>**Lisa C. Ellis, <strong>MD</strong>Michael L. Gutierrez, <strong>MD</strong>James M. Hicks, <strong>MD</strong>Felix Hull, <strong>MD</strong>Jeffrey M. Jekot, <strong>MD</strong>Thomas D. Kirksey, <strong>MD</strong>Greg M. Kronberg, <strong>MD</strong>Hillary Miller, <strong>MD</strong>Hector E. Morales, <strong>MD</strong>Patrick S. Pevoto, <strong>MD</strong>Peggy M. Russell, DODora L. Salazar, <strong>MD</strong>Catherine L. Scholl, <strong>MD</strong><strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong>Eric S. Tiblier, <strong>MD</strong>Emilio M. Torres, <strong>MD</strong>Dennis E. Welch, <strong>MD</strong>Robert P. Wills, <strong>MD</strong>Guadalupe “Pete” Zamora, <strong>MD</strong>* Chair** Vice-ChairAlternate Delegates to TMASara Austin, <strong>MD</strong>Bruce A. Levy, <strong>MD</strong>, JDTony Aventa, <strong>MD</strong>Jerald A. Mankovsky, <strong>MD</strong>Craig T. Berent, <strong>MD</strong> Carla F. Ortique, <strong>MD</strong>Dawn C. Buckingham, <strong>MD</strong> Paula S. Oliver, <strong>MD</strong>Edward D. Buckingham, <strong>MD</strong> Jack Pierce, <strong>MD</strong>Jane E. Braunstein, <strong>MD</strong> Robina N. Poonawala, <strong>MD</strong>William D. Caldwell, <strong>MD</strong> Melinda Rainey, <strong>MD</strong>Nancy T. Foster, <strong>MD</strong> Stephanie D. Roth, <strong>MD</strong>Leigh A. Fredholm, <strong>MD</strong> Aravind B. Sankar, <strong>MD</strong>Toni Funicella, <strong>MD</strong>Halsey M. Settle, III, <strong>MD</strong>Mary A. Gonzales, <strong>MD</strong> Adam J. Schneider, <strong>MD</strong>Juan Guerrero, <strong>MD</strong>Zoltan Trizna, <strong>MD</strong>Daniel J. Leeman, <strong>MD</strong> Belda Zamora, <strong>MD</strong>6 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
PROJECT ACCESSProject Access - Raising the Standard of HealthTheresa J. Pugh, <strong>MD</strong>When I was a young child, I remembermy father taking me to our area FreeClinic to volunteer. As a family physician,he would see patients while I assisted thestaff in stapling papers and making newpatient charts. The gratitude of thepatients who received care at the clinic isstill a vivid memory. When I chose familypractice as my career path, I wanted tocontinue giving back to the community.So, when a Project Access applicationcame in the mail, I was eager to participate.But, as a new physician with amountain of student loans and otherdebt, I was worried about the financialimpact of participating. I wondered if mypractice would become overloaded withpatients who would not be able to pay fortheir care. I was also concerned that thepatients may have a lot of complicatedchronic illness and need frequent visits. Atthe same time, I was just beginning mypractice and there were very few days thatmy schedule was full. It made sense to usethose empty appointment slots to seepatients who truly needed care. Icompleted the application and agreedto accept ten patients per year, therecommended number.Four years later, I couldn’t be happierabout that decision. My patient load hasbeen well below ten patients per year, andI am surprised at how few visits most ofthe patients require. The patients I seethrough the program are relativelyhealthy, hard-working individuals whosimply do not have access to privateinsurance. The program has even allowedme to continue seeing one of my patientswho used to have private insurance, but isnow a Project Access patient. Without theprogram, he may not have been able toreceive the excellent specialist care hereceived when he was diagnosed with achronic illness. Early in my participationwith the program, it was clear thatpatients would benefit from access toregular health care, but I did not realizethe full extent of the payback that I wouldreceive. My practice is now busy andcontinuing to grow, partly due to myparticipation in the program. Many of myProject Access patients have since transferredto private insurance and continuedseeing me as their primary care physician.They have also referred friends, family,Project Access Physician ParticipationA physician participating in Project Access agrees to either seepatients in their office or volunteer at a community clinic.and co-workers to our practice. While Ihave never calculated the numbers, I amsure that my practice has received morerevenue than I have ever donated in care.Participating in the program is sosimple that my staff prefers Project Accessto most HMOs. The Project Access staff isextremely helpful and handles specialistreferrals and scheduling out-of-officetesting. When we see patients through theprogram, we are able to practice medicinethe way we want, without having to worryabout extra paperwork and insurancecompany denials. Without Project Access,many of these people would be facingfurther financial difficulties frommounting medical bills. By caring forpatients in the appropriate outpatientI will volunteer to see Project Access patients in my office:Primary Care PhysicianOver a 12 month period I pledge to accept up to the following number of patients:10 Other ____________OrSpecialty Care PhysicianOver a 12 month period I pledge to accept up to the following number of patients:10 Other ____________I will volunteer at a Community ClinicOver a 12 month period I pledge to volunteer the following number of hours:24 hours Other ____________Please contact me. I have additional questions regarding my role in Project Access.I am not interested in volunteering for Project Access at this time.Office Contact Name (please print):__________________________________________Physician name: __________________________________ Specialty: ____________Fax this card to 206-1135 or mail to PO Box 4679, Austin, TX 78765For more information, contact Cliff Ames at 206-1165.<strong>TCMS</strong> Journal January • February <strong>2009</strong> 7
setting, the emergency rooms are lesscrowded with patients who do not haveaccess to care. But the most rewardingpart of participating in the program is thegratitude that each patient expresses.Every patient has personally thanked mefor participating in the program, and theyare thankful that such a program exists.Unfortunately, the media usuallyreports on the negative aspects of healthcare. Rising out-of-pocket expenses,increasing numbers of uninsured patientsand limited access to care are colossalissues within our health care system. It istruly wonderful to be involved in aprogram that eliminates these issues andcares for some of the patients who need itmost. This program makes a significantdifference on a local level, and its successmay show other communities that groupsof physicians actually have a lot of powerto combat some of the problems with ourhealth care system. While we are all shorton time, Project Access makes it simple togive back. With so many participatingphysicians, the burden on each of us isquite low; but if more physicians wereinvolved, more patients could receive care.If you are not a participant withProject Access, I urge you to considerjoining us. If you are, thank you for yourparticipation and please encourage yourcolleagues to join us. Together, we can havean amazing impact on raising the standardof health in the Austin community.Theresa J. Pugh, <strong>MD</strong> practices familymedicine at Jefferson Street Family Practicein central Austin. If you have any questionsabout Project Access, please feel free tocontact Dr. Pugh at DrTJPugh@yahoo.com.8 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
LEGISLATIVE UPDATEHelp Fix Our Broken Health Care SystemSimple Things You Can Do for Your PracticeToday’s health care system is broken. Unfortunately, youcannot fix it or protect your practice by working more hoursand taking care of more patients. The only way for you toeffect “real change” is through the legislative process. Here arefour easy things you can do for your practice starting today −right at your desk.Sign up for First Tuesdays at the Capitol: Join hundreds ofyour colleagues at the Capitol the first Tuesday of the month(Feb. 3, March 3, April 7, May 5). Legislators take note whendoctors in white coats walk the halls of the capitol eachsession.Join TEXPAC: The Texas Medical Association PoliticalAction Committee (TEXPAC) is the political arm of TMA.It’s the largest bipartisan political action committee in thestate and ranks first in size among other state medical associationPACs. If you haven’t joined TEXPAC, it’s not too lateto get involved. A small contribution to TMA’s politicalaction committee can make a huge difference.Sign up for TMA Legislative News Hotline: Keep track ofmedicine’s top priority issues throughout the session bysubscribing to the daily or weekly e-newsletter.Use TMA’s Grassroots Action Center: Write, e-mail, or callyour legislator when critical issues arise. TMA makes it easy.All you have to do is respond to a TMA Action Alert usingthe message provided. It only takes a minute.Be A Legislative Key ContactLet <strong>TCMS</strong> know if you have a personal or professionalrelationship with a state or federal legislator and are willingto contact him or her about medical issues – especiallyduring the 81st Texas Legislature.<strong>TCMS</strong> gives you all the information you need to makecontact. A simple phone call, email, or fax can make all thedifference! Contact Stephanie Triggs at 206-1124 orstriggs@tcms.com for more information.GovernorRick PerryLieutenant GovernorDavid Dewhurst(R)(R)State SenatorsKirk Watson(D – District14)Jeff Wentworth (R – District 25)State RepresentativesDawnna Dukes (D – District 46)Valinda Bolton (D – District 47)Donna Howard (D – District 48)Elliott Naishtat (D – District 49)Mark Strama (D – District 50)Eddie Rodriguez (D – District 51)Get more information or register for any or all of the aboveby visiting www.texmed.org and www.texpac.org.US SenatorsKay Bailey HutchisonJohn Cornyn(R)(R)US RepresentativesMichael McCaul (R – District 10)Lamar <strong>Smith</strong> (R – District 21)Lloyd Doggett (D – District 25)<strong>TCMS</strong> Journal January • February <strong>2009</strong> 9
ON THE COVER<strong>Charlotte</strong> H. <strong>Smith</strong>, <strong>MD</strong><strong>2009</strong> <strong>TCMS</strong> <strong>President</strong>Merry WheatonFreelance writerOnce upon a time, before <strong>Charlotte</strong><strong>Smith</strong> became board certified in physicalmedicine with a sub-specialization inspinal cord injury medicine, she was a shypre-med student named <strong>Charlotte</strong>Hoehne, working three or four jobs to putherself through UT-Austin, and laughablyuninformed about organized medicine.Then in 1982, in the face of hugetuition hikes, someone suggested sheapply for a TMA loan to help pay herexpenses at Baylor College of Medicine.“I did, and part of the process was aprivate interview on campus with TMA<strong>President</strong> George Alexander,” sheremembers. “I went in there thinking hewas a banker, and when he said, ‘Inexchange for this loan, I’m going to wantsomething from you,’ I thought, ‘Oh,no, nothing good can follow that!’”In fact, what the Houston familypracticioner wanted was for her to beinvolved in starting a TMA chapter atBaylor. She did, becoming its chapterpresident and initiating her long-terminvolvement with county, state, andnational medical societies.From 1988 to 1990, she was aDelegate to the AMA, as the votingrepresentative for 27,014 US residentphysicians. The issue of resident workhours had been catapulted to the top ofthe AMA’s agenda by the media firestormfollowing Libby Zion’s death in 1984while under the care of an overworkedresident physician, and the State of NewYork’s subsequent legislation restrictingresident working hours. “There I was,representing all the residents in the US;we had one vote,” says Dr. <strong>Smith</strong>. In anorganization which seemed overwhelminglymale and conservative, she was notoptimistic that things would improve forresidents. But it was clearly no place forshyness. She says her voice was probablyshaking, but she testified in the House ofDelegates, and when they finally voted,the support for limiting resident workinghours was unanimous. Her response?“It blew my mind. I thought, ‘Whata democracy!’”Ames, <strong>Charlotte</strong>, Zach, and Victoria enjoying thebiggest snow storm in Seattlein over 40 years!Before the vote was called, however,back at Baylor, Dr. Michael DeBakeyhad decided he could spare one resident− a general surgeon who was doing apathology rotation − to testify before theAMA. That was F. Ames <strong>Smith</strong>, Jr., wholike other Baylor residents, worked sixtythreedays in a row − with work weeksregularly exceeding one hundred hours.“He called and asked me what to wear totestify, and he kept calling me,”<strong>Charlotte</strong> <strong>Smith</strong> remembers with asmile. “I thought maybe I could get himon a committee, since he was so interestedin the AMA and the TMA. It tookabout three months before I realized hemight have other intentions.... Westarted going out, but I wouldn’t let himdrive because he was so exhausted. Onevery date he’d fall asleep and I’d drophim off at his parents’ house....” After amonth of that, he proposed. “So you seeI owe a lot to organized medicine:getting a student loan, overcoming myshyness, meeting my husband, andmaking my best friends from that time,who were all involved in TMA andAMA,” she says.Soon the question became where tosettle. Dr. <strong>Charlotte</strong> <strong>Smith</strong> had grownup in Austin, in a family with a longtradition of advocacy. A great auntstricken with polio in the 1940s hadmanaged to get a college education andlead a productive life; an uncle hadbecame a quadriplegic as the result of adiving accident; and her father, anattorney and lobbyist, had helped writethe American with Disabilities Acttwenty years before it eventually gotenacted. The opportunity to be anadvocate for patients drew her to Austinand reinforced her involvement withmedical associations. “How effectivecould I be for patients by myself? I wasyoung, female, and practicing in a fieldmost people had never even heard of,”she reasoned.Surprisingly, she had started medicalschool intending to specialize in10 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
ophthalmology. When she was twelve,her father took her to the NeuroscienceCenter in Houston, where she met a verykind and gracious ophthalmologistnamed Alice McPherson. Inspired,young <strong>Charlotte</strong> explored medicalcareers throughout high school, rotatingthrough nursing, PT and the ER at HolyCross Hospital, working in the Setonlab, and as a rehabilitation aide at aresidential home for persons withmultiple disabilities. Later, however,when she did her first rotation inophthalmology, she discovered she hatedit. “I like talking to people. I like longtermrelationships,” she explains.Baylor had one of the nation’s topprograms in physical medicine andrehabilitation and that, combined withher family history, took her in adirection she has found stimulating andgratifying. Since physiatrists deal withfunction, the etiologies are varied andthe patients are diverse. She enjoys thescience, the variety, and the relationshipswith patients, who have ranged from atwenty-four-week preemie with cerebralpalsy spasticity to a hundred-and-fouryear-oldman with a fractured hip. “Theonly things you can’t transplant now arethe brain, the spinal cord, and theeyeballs. The survivors of damage tothese parts of the body teach and inspireme. They’re a very upbeat populationand I have lifelong bonds with many ofthem,” she says.Dr. <strong>Smith</strong> is nowhere close toretiring, or wanting to, though shewould prefer to work eight to ten hoursa day, rather than sixteen to twenty. Sheand Ames still have a relatively youngfamily. “Our son Zachary is thirteen andour daughter Victoria just turned six.We had themlate in life, butwe reallywanted them,”she says, whippingout theirschool photos.“Zach told methe other day,‘Mom, you’re inreally goodshape for your age. I mean, you don’tlook twice as old as the other kids’moms.’” Laughing, she adds, “I didn’tknow whether to kiss him or hit him!”As a couple, the two Drs. <strong>Smith</strong>have wrestled with the challenges facingdual professionals. They’ve come out ontop and now offer marriage mentoringthrough their church. “Building up thefamily is so important,” she says, notingthat the biggest predictor of outcomeamong her patients is whether or not theyhave someone who cares about them.Another hidden talent: <strong>Charlotte</strong> occasionally plays clarinet with “Docs of Dixie.”The band will entertain at her installation, March 31, <strong>2009</strong>.Drs. Ames and <strong>Charlotte</strong> help daughter Victoriacross the finish line at Walk With Your Doctor.Dr. <strong>Smith</strong> is Medical Director forRehabilitation Services for Seton’s localnetwork. She teaches through TMA, theAmerican Academy of Physical Medicineand Rehabilitation, Baylor’s Departmentof PMR, and UTMB-Austin’sDepartment of Neurology, and she’sdelighted that two of the three medicalstudents she has worked with through theAustin Medical Education Program havedecided to specialize in her field.With such a full plate, why wouldshe take on the job of <strong>TCMS</strong> <strong>President</strong>?“I have to be strategic, and I’ve made thelocal medical society a priority becauseit’s important. It’s critical. It’s the countysocieties that make up the TMA and ifthe counties are strong and we work welltogether, the whole family is strong....These are historic times. People voted forchange, and we can make the change agood one by really focusing on doing theright things for our patients,” she says.Her experiences in the AMA Houseof Delegates have convinced her thateach voice matters.Noting that the <strong>TCMS</strong> has a strongsphere of influence, she says, “I don’twant to be a single-issue person, but Ibelieve it would be wrong of me not totry to raise awareness about people withdisabilities, so the medical communityand the community-at-large knowwhat’s needed.”She points out that sinceChristopher Reeves, we know thatrecovery (not rehab, but recovery!) canhappen after years. She’s enthusiasticabout the work of the Lone Star ParalysisFoundation and the Brain and SpineRecovery Center at Brackenridge, whichhas fine equipment, like functional electricalstimulation bikes, and which ispushing the envelope on traditionaltherapy and getting great results, even fromsome patients twenty years post-accident.“Austin has so many things you can’tget anywhere else,” Dr. <strong>Smith</strong> says. She’sexcited about the opportunities to growUTMB-Austin’s nursing, therapy, andresidency programs, and predicts that itsmedical residency program is going to bethe best in the country.On the other hand, she notes thatTexas leads the nation in the number ofuninsured people, that the State’sMedicaid program doesn’t cover rehabfor people over twenty-one years of age,and that Workers’ Compensation here isoptional. And she asks pointedly, “Whatgood is great health care without access?”Of her leadership style she says, “For me,it’s all about service. I believe that peoplewho meet needs are people who end upleading. I’m open, I want to listen, and Ihope I can step up in a crisis.”<strong>TCMS</strong> Journal January • February <strong>2009</strong> 11
<strong>Travis</strong> <strong>County</strong> Medical SocietyUpcoming Events01/27-Networking SocialAlamo Drafthouse Cinema02/11-Business Over BreakfastHacking Medical Business Networks02/21-Mens Basketball: UT vs. OUFrank Erwin Center02/26-Networking Social03/11-Women in Medicine03/26-Business of Medicine DinnerSelection and Implementationof EMRs03/31-Joint Installation of OfficersUT Alumni CenterFor additional information visitwww.tcms.com12 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
TCM ALLIANCEServing Our CommunityShelly Ozdil<strong>President</strong>-Elect, <strong>Travis</strong> <strong>County</strong> Medical AllianceJB and Sandy Bike-a-ThonLaurel Hooper and Holly Schneiderwere instrumental in coordinating afavorite project, Hard Hats for LittleHeads, with Mix 94.7’s JB & SandyMorning show’s annual Bikes for Kidsgive-a-way. Thanks to the Alliance, 850children receiving a bike will be able toride it safely with a donated helmet.Committee members made phone calls tofamilies letting them know their child(ren)was selected and were on hand at MellowJohnny’s not only to organize and deliverthese helmets, but also to provide a bit ofholiday cheer by donating and decoratinga beautiful Christmas tree to set the mood.Literacy OutreachThe Literacy Outreach committee ofthe TCMA supports BookSpring, aprogram to launch children into a world ofreading. In March 2008, two literacyprograms, Reading-Is-Fundamental andCapital Area Reach Out and Read mergedand the new organization becameBookSpring. The Alliance is in its thirdyear of involvement with literacy outreach.Our volunteers deliver gently used children’sbooks to four area Austin medical clinics aspart of the program to promote literacy inchildren. At well-checks, doctors encourageparents to read aloud to their children andprovide each child between 6 months and 5years a developmentally appropriate bookto keep. Waiting rooms are stocked withgently used books and often parents andchildren learn the pleasures of looking atbooks together.The Alliance is always looking fordonations to support this program. Wewelcome books, monetary donations, anddonations of your time. Contact MargeneBeckham at mbeckham@austin.rr.com ifyou would like to help!Gala… “Bronze Star Ball”The Gala committee, chaired by LydiaSoldano and Loren Gigliotti, is hard atwork preparing for a night of fun andentertainment. Mark your calendars forFebruary 7, <strong>2009</strong>. The “Bronze Star Ball”will be held from 7:00 pm to 11:30 pm atthe Bob Bullock Texas State HistoryMuseum with musical guest The BellevilleOutfit. Elaine Agatson is hard at workgathering items for the silent auction andwe are so grateful to Duncan & BoydJewelers for their generous donation of a“sparkly” for our raffle. We would also liketo thank 2 Dine 4 Catering for all of thein-kind donations they are providing. Thiscommunity support enables us to make abigger difference in <strong>Travis</strong> <strong>County</strong>.Sponsorships are still available bycontacting Kathy Shelly at 680-1073 orkbshelly@austin.rr.com. A pre-party eventwill be held this year as a special thank youto our sponsors:Gold StarAustin Radiology AssociationClinical Pathology Associates<strong>Travis</strong> <strong>County</strong> Medical SocietySilver StarAustin Anesthesiology Group, LLPAustin GastroenterologyAustin Regional ClinicCapitol Anesthesiology AssociationDr. and Mrs. Phil CollinsRising StarCapital Cardiovascular SpecialistsClinical Pathology Laboratories, Inc.Texas Oculoplastic ConsultantsTMA Insurance TrustMember Spotlight: Lydia Soldano joined the Alliance to become involved in the community, to meet new people, and to make a difference.The Alliance was thrilled when Lydia asked to start a running group. “Austin Fun Run” is a great group of members who walk and run at alllevels and who join together in area races to promote the Alliance by wearing our t-shirts. She didn’t hesitate when she was asked to chair thisyear’s Gala! She, Loren Gigliotti, and their committee have been hard at work for months planning a fabulous night for the Alliance. We lookforward to enjoying their efforts at the Bronze Star Ball! Lydia and her husband, Tony, a dermatopathologist, have a four-year-old daughterMackenzie. Lydia says, “The women in this organization are amazing – no matter that I was new and no one knew of my talents or lack thereof,I was immediately put to work and given the space to shine knowing that someone would be there to help if I needed it.”Joining Lydia in her willingness to give time and talent to the Alliance is Loren Gigliotti. Loren joined the Alliance by way of the <strong>Travis</strong> <strong>County</strong>Medical Society. While at a Society event, she saw information about the Alliance and thought it offered a variety of activities she would enjoy,from social to philanthropic. As a new member, she jumped right in by chairing the Gala this year and has already signed on as secretary fornext year’s board. Loren grew up in Austin and she and her husband Steve, an interventional cardiologist, have three kids Francesca, 5, Isabella,3, and Sadie, 9 months. When asked about her favorite part of the Alliance, Loren says, “I love how kind and down to earth everyone is!”<strong>TCMS</strong> Journal January • February <strong>2009</strong> 13
IN THE NEWSTo the Editor,The November/December <strong>TCMS</strong> Journal“The Great American Smokeout” made methink back . . .to a discussion in the NuclearLaboratory at Rose Memorial Hospital,Denver, Colorado, December, 1957.Jack Benny: “Doctor, is there anythingto this idea that smoking cigarettes causeslung cancer? My doctor told me to quit.”Dr. Bob Ellzey: “Yes, Mr. Benny. Theyhave established that if you smoke as manyas two packs of cigarettes a day for 10years, you likely will get lung cancerwhether or not you quit.”Jack Benny: “I’ve smoked two packs aday since I was thirteen.”Dr. Bob Ellzey: “Well then, it probablydoesn’t make any difference whether youquit or not.”A year or so after this conversation,examination of the bronchi in people whohad quit smoking showed the destroyed ciliato begin to reappear, and the lungs begin toreturn to normal so that quitting does helpprevent smoking-caused lung cancer.The good news, Jack Benny didn’tdevelop lung cancer!Bob Ellzey, <strong>MD</strong>Retired RadiologistJack Benny (center) and(right) Dr. Bob Ellzey, Senior Resident.To the Editor,As a retiree whose status has changed fromthat of one who cared for people, to a seeminglyinsatiable recipient of medical services,I feel as though I’m drawing interest on principleaccumulated over a long time. It seemsinevitable that if one lives long enough he’sbound to become a walking museum, Ibeing no exception. I come down to thepoint that my many colleagues who haveand do care for me do so with inexhaustiblekindness, love, and generosity. This letter ismy feeble attempt to express to them mydeep gratitude.Mathis Blackstock, <strong>MD</strong>Retired Family DoctorRetired Membership is granted to thosephysicians who have retired from theactive practice of medicine. Upon nominationfrom the Board of Ethics, the<strong>TCMS</strong> Executive Board elected thefollowing to Retired Membership:Lynus Brown, <strong>MD</strong>Joseph L. Des Rosiers, <strong>MD</strong>Robert O. Kerr, <strong>MD</strong>Linda J. Litzinger, <strong>MD</strong>Doris M. Robitaille, <strong>MD</strong>Robert B. Teague, <strong>MD</strong>William R.Woodward, <strong>MD</strong>RETIREDJames W. Fox, <strong>MD</strong> passed away onNovember 21, 2008. He was born inTaylor, Texas on October 31, 1941.Dr. Fox was one of the founders of theAustin Smiles Foundation and traveled theworld offering his services. Our condolencesto the family of Dr. Fox.IN MEMORYJames Winston Thomas, <strong>MD</strong> passedaway on December 11, 2008. Dr. Thomaswas born on October 25, 1921 in Mart,Texas. Our condolences to the family ofDr. Thomas.Durward A. Baggett, <strong>MD</strong> passed awayon August 21, 2008. Dr. Baggett wasborn in Kilgore, Texas and attendedthe University of Texas at Austinearning a degree in chemistry in 1949. Dr.Baggett’s desire to become a physician ledhim to move his family to Galveston andmedical school where he graduated fromthe University of Texas Medical Branch atGalveston. They returned to Austin for Dr.Baggett’s internship at Brackenridge andthey remained throughout his career. Hewas Chief of Staff of BrackenridgeHospital and State <strong>President</strong> of the TexasAcademy of Family Physicians. Dr.Baggett was the first physician in <strong>Travis</strong><strong>County</strong> to become a Board CertifiedFamily Physician. Our condolences to thefamily of Dr. Baggett.IN MEMORYByron Phillip Kocen, <strong>MD</strong> passed away onNovember 29, 2008. Dr. Kocen opened hisfirst pediatric practice in 1964 and spent thenext 44 years serving the children of CentralTexas, first as a traditional pediatrician andlater as a pioneer in the field of ADHD andthe treatment of learning differences inchildren as well as adults. Our condolencesto the family of Dr. Kocen.Jerald R. “Doc” Senter, <strong>MD</strong> passed awayon October 31, 2008. Dr. Senter was bornin Sherman, Texas and grew up in Tulsa,Oklahoma. He enlisted in the Army AirForce during WW II and served as acombat officer with the 8th Air Force, 2ndAir Division, 458th Bomb Group, and754th Bomb Squadron in England.Dr. Senter received his <strong>MD</strong> degree fromthe University of Oklahoma and moved toAustin where he had an active practice for51 years before retiring in 2002. Ourcondolences to the family of Dr. Senter.14 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
PRACTICE MANAGEMENTFailure to Stabilize Before TransferTexas Medical Liability TrustRisk Management DepartmentThe following closed claim study is basedon an actual malpractice claim fromTMLT. This case illustrates how action orinaction on the part of physicians led toallegations of professional liability, andhow risk management techniques may haveeither prevented the outcome or increasedthe physician’s defensibility. The ultimategoal in presenting this case is to help physicianspractice safe medicine. An attempthas been made to make the material lesseasy to identify. If you recognize your ownclaim, please be assured it is presented solelyto emphasize the issues of the case.PresentationA 35-year-old man was involved in ahead-on motor vehicle collision. Thedriver of the car that crossed into theman’s lane of traffic died at the scene. Theman and his 11-year-old daughter wereseriously injured. It took 45 minutes toextricate the man from his car.Physician actionThe man and his daughter were taken toa local hospital, which had been designatedas a Level III trauma center. Theman was admitted to the trauma roomby a general surgeon at 2:45 pm. Anemergency medicine physician alsoprovided care to this patient. The initialexam revealed that the patient had aheart rate of 120 bpm and a systolicblood pressure of 110 mm Hg. His respiratoryrate was in the 30s. The generalsurgeon noted blood draining from theleft ear and multiple lacerations andcontusions of the face. An abdominalexam revealed a soft and non-tenderabdomen. An open left tibia and fibulafracture with no distal pulses was present.The right tibia and fibula were alsofractured, but distal pulses were present.Despite the fact that he wasreceiving rapid infusion of saline, thepatient’s blood pressure was falling. Hewas given two units of blood and hisblood pressure increased into the 120s.The patient’s mental status continued todeteriorate. Because the patient hadsymptoms consistent with head trauma,the general surgeon decided that thepatient needed to be transferred to aLevel I trauma center. This decision wasbased in part on the fact that they had noneurosurgeon available to treat thispatient. At 3:20 pm, a neighboringhospital was called and agreed toaccept the patient. A care flight helicopterwas dispatched.At 3:30 pm, during the wait for thehelicopter, a CT scan of the abdomen,pelvis, and head was performed.According to the radiologist, the resultsof the head CT were negative, and theabdominal CT read as follows: “. . . thereis no pneumothorax. No intrahepaticlaceration. No definite splenic laceration.A small amount of fluid is suspectedabout the spleen. There is a smallamount of fluid around the cecum. Nosignificant fluid collection in the paracolicgutters, however. . . There is a smallamount of free pelvic fluid and pelvicwall hematoma.” The radiologistreviewed the CT scan with the generalsurgeon, and both were of the opinionthat there was no evidence of internalorgan damage or bleeding.At 4 pm, the patient’s bloodpressure dropped to 69/30 mm Hg.When the care flight helicopter arrived at4:08 pm, the patient’s blood pressure hadincreased to 88/56 mm Hg, and by 4:20pm, his blood pressure increased to120/103 mm Hg. At 4:40 pm, the careflight helicopter lifted off with thepatient, and his blood pressure was125/34 mm Hg. Three units of bloodwere administered during flight. At 5:01pm, the patient coded while still in theair. CPR was started. The care flighthelicopter landed at the hospital at 5:13pm, and the patient was brought to theED at 5:17 pm without a pulse or bloodpressure. CPR was continued, but thepatient did not respond. He waspronounced dead at 5:28 pm.An autopsy was performed and thefindings included a significant lacerationof the patient’s liver and bladder withsubsequent hemoperitoneum. The patientwas noted to have multiple rib fractureswith lung contusions and bilateral hemothoraces.Approximately 1500 cc ofblood was present in the peritonealcavity as well as 50 cc of blood in bothpleural cavities.The patient’s daughter sustainedseveral bone fractures and a severe scalpwound. She was treated at the Level IIIhospital and recovered from her injuries.AllegationsA lawsuit was filed against the generalsurgeon. The allegations included:<strong>TCMS</strong> Journal January • February <strong>2009</strong> 15
• failure to perform peritoneal lavage;• failure to properly monitor theincreasing hardness of thepatient’s abdomen;• failure to perform a laparotomy todetermine the nature and extent ofthe patient’s bleeding and repair thebleeding; and• failure to stabilize the patient priorto transfer.The emergency medicine physician,the radiologist, and the Level III hospitalwere also sued.Legal implicationsThe plaintiff’s expert, a trauma surgeon,was critical of the general surgeonbecause he did not clearly stabilize thepatient before transfer. He stated that thestandard of care requires that a patientwith persistent hypotension, tachycardia,metabolic acidosis, and altered mentalstatus with no radiological evidence ofintracranial injury be stabilized beforetransfer. It should be clear in the eyes ofthe transferring physician that there is nosurgical source of bleeding that needs tobe controlled before transfer. Accordingto this physician, the defendant shouldhave evaluated the abdomen with aperitoneal lavage. He also stated that ahemoglobin level and a blood gas drawnbefore transfer would have helped thegeneral surgeon determine if the patient’scondition was worsening. This surgeonalso testified that the patient would havesurvived if the defendant had repairedthe bleeding internal organs.The defense expert and the defendantargued that given the patient’s suspectedhead injury and compromised vascularsupply, it was imperative to transfer thepatient since there was no neurosurgeon orvascular surgeon available at the hospital.The plaintiffs asserted that since theresults of the head CT came backnormal, there was no head injury. Thisargument was challenged when the plaintiff’sexperts conceded that a normal headCT does not rule out a head injury andthat a shear type injury to the brain willnot show up initially on a CT scan.The defense also argued that therewas no indication that the patient wasbleeding internally. This is supported bythe negative results from the abdominalCT scan and a documented soft andnon-tender abdomen. Though theautopsy clearly showed a lacerated liverand the abdomen had 1500 cc of blood,the defense expert believed this occurred(along with the broken ribs) duringvigorous CPR efforts. Additionally, itwas also viewed as unlikely that thepatient could have survived three hours(from the time of the collision to thetime of cardiac arrest) if a severe liverlaceration had occurred at the time of thecollision.With regards to the alleged instabilityof the patient, there were some low bloodpressure readings in the hospital record.Specifically, there is a reading at the timethe life flight helicopter arrived of 88/56mm Hg. However, the flight nurse tookblood pressure readings immediatelyafter the patient was on board and thepatient’s blood pressure was 127/103mm Hg. It continued in that rangeduring the flight.One area of weakness for the defenseinvolved a discrepancy in documentation.An ED nurse documented that thepatient had a flat, non-tender abdomen.The general surgeon did not documentserial abdominal exams, but testified thathe was checking the abdomen and foundthat there was no distension. A care flightnurse noted “abdomen veryobese/distended/firm despite NG w 400ccbrown liquid noted from same.” Theemergency medicine physician testifiedand documented on the transfer sheetthat the patient was unstable at the timeof transfer. According to this physician,the patient was “never completely stable”while at the Level III hospital and he wasstabilized as best they could before transfer.DispositionThe emergency medicine physician andthe hospital settled their cases. The caseagainst the radiologist was dropped. Thecase against the general surgeonproceeded to trial. The jury reached averdict in favor of the defendant.Risk management considerationsThe jury verdict in favor of the generalsurgeon validated that the members ofthe panel believed that he acted in aprudent, reasonable manner.The information and opinions in thisarticle should not be used or referred to asprimary legal sources nor construed asestablishing medical standards of care forthe purposes of litigation, including experttestimony. The standard of care is dependentupon the particular facts andcircumstances of each individual case andno generalization can be made that wouldapply to all cases. The informationpresented should be used as a resource,selected and adapted with the advice ofyour attorney. It is distributed with theunderstanding that neither Texas MedicalLiability Trust nor Texas MedicalInsurance Company is engaged inrendering legal services.© Copyright <strong>2009</strong> TMLT.16 January • February <strong>2009</strong> <strong>TCMS</strong> Journal
TAKE FIVEfor yourHEALTHDELIRIU<strong>MD</strong>elirium is a disturbance of consciousness (awareness of the person’s environment) characterized by altered or shiftingmental status and inattention (reduced ability to focus, sustain, or shift attention). There are also changes in cognition (basicmental functions) such as memory impairment, disorientation to time or place, and language disturbance. There also maybe disturbances of perception (accurate appreciation of the environment) such as hallucinations (seeing or hearing thingsthat are not actually there), abnormal speech, abnormal movements (including tremors or picking at clothing), disruptiveor violent behavior, and sudden shifts in emotions. To qualify for a diagnosis of delirium, the signs and symptoms musthave a short onset (over a period of hours or days) and change over the course of the day. It is important to make a cleardistinction between delirium and dementia (such as Alzheimer disease). Dementia is a disturbance in intellectual (thinking)functions that is usually gradually progressive over a long period.Having delirium along with another medical illness can significantly increase a person’s chance of dying from that illness.It is important for doctors to identify delirium so that it can be treated to improve the person’s overall prognosis.DELIRIUMCAUSES OF DELIRIUM• New or worsening medical illnesses such as severe infections or heart failure• Medications, abused drugs, or poisons• Drug withdrawal syndromes, such as delirium tremens (delirium from alcohol withdrawal)• Psychiatric (mental) illnesses• Severe pain, immobilization, or sleep deprivationTREATMENTS FOR DELIRIUM• Identifying and treating the underlying cause of delirium is essential.• Supportive care, including mechanical ventilation and life-support medications, may be necessary.• The need for all medications the patient is receiving should be assessed.• Replacement of vitamin B should be considered for persons with alcoholism or who are malnourished.• Antipsychotic medications may be used to reduce the symptoms of delirium.• Benzodiazepines (antianxiety medications) may be used, particularly in cases of drug withdrawal syndromes.If no other treatments are effective and the patient is at clear risk of harm to self or others, soft restraints may beneeded for a short time.Psychiatric assessment and management are important, particularly in cases of delirium not easily explainable bypoison exposure, medication effects, or medical illness.For More InformationAmerican Psychiatric Associationhttp://www.psych.orgBrain Dysfunction in Critically Ill Patientshttp://www.icudelirium.orgNational Institute of Mental Healthhttp://www.nimh.nih.govMake copies of this article toshare with your patients<strong>TCMS</strong> Journal January • February <strong>2009</strong> 17