Selective Neck Dissection - Vula - University of Cape Town
Selective Neck Dissection - Vula - University of Cape Town
Selective Neck Dissection - Vula - University of Cape Town
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
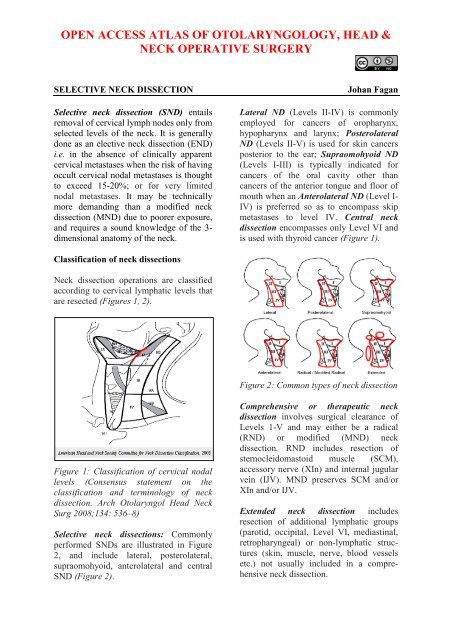
It has been proposed that neck dissectionsbe more logically and precisely describedand classified by naming the structures andthe nodal levels that have been resected.(Ferlito A, Robbins KT, Shah JP, et al.Proposal for a rational classification <strong>of</strong>neck dissections. Head <strong>Neck</strong> 2011 Mar;33(3): 445-50)skin incision can be extended across to theopposite side with bilateral SND, or can beextended superiorly to split the lower lip inthe midline to gain access to the oralcavity, or preauricularly for a parotidectomy(Figure 3). Figure 4 demonstratesthe hockey stick incision.<strong>Selective</strong> <strong>Neck</strong> <strong>Dissection</strong>Anaesthesia, positioning and drapingThe operation is done under generalanaesthesia without muscle relaxation aseliciting muscle contraction on mechanicalor electrical stimulation <strong>of</strong> the marginalmandibular, hypoglossal (XIIn) andaccessory nerves assists with locating andpreserving these nerves. It is a cleanoperation and antibiotics are therefore notrequired unless the upper aerodigestivetract is entered. With an experiencedsurgeon, blood transfusion is rarelyrequired.The patient is placed in a supine positionwith the neck extended and head turned tothe opposite side. Surgical draping mustpermit monitoring for movement <strong>of</strong> thelower lip with irritation <strong>of</strong> the marginalmandibular nerve, and must provide accessto the clavicle inferiorly, the trapeziusmuscle posteriorly, the tip <strong>of</strong> the earlobesuperiorly and the midline <strong>of</strong> the neckanteriorly. The drapes are sutured to theskin.Figure 3: Incision for SND (Red)compared to MND (Yellow); dotted linesindicate extensions for parotidectomy andoral tumour resectionsIncisions and flapsIncisions should take into considerationaccess that may be required to resect theprimary tumour, cosmetic factors, and theblood supply to the flaps. A transverse skincrease incision is placed more inferiorlythan with a MND so as to avoid a verticalskin incision and to facilitate dissection <strong>of</strong>levels III and IV (Figure 3). The transverseFigure 4: Hockey-stick incision forposterolateral SND combined withparotidectomy2
6The hockey-stick incision may be extendedinto a preauricular skin crease and isparticularly useful for combined posterolateralND and parotidectomy. Care has tobe taken in patients who have beenpreviously irradiated as the posteroinferiorcorner <strong>of</strong> the flap has a tenuous bloodsupply and may slough and have to heal bysecondary intention.Total laryngectomy with Lateral ND canbe accessed via a wide apron flap (Figure5).overlying the SCM (Figure 6).EJVGr Aur nFigure 6: Note cut edges <strong>of</strong> platysmamuscle, and the external jugular vein andgreater auricular nerve overlying the SCMFigure 5: Wide apron flapSupraomohyoid SND: Operative steps(Figure 6)The detailed step-by-step description <strong>of</strong>neck dissection that follows refers to aright-sided Supraomohyoid ND (Levels I-III). For a Lateral ND, simply skip dissecttion<strong>of</strong> Level 1 and extend the nodal resectioninferiorly beyond the level <strong>of</strong> the omohyoidmuscle, either by retracting or dividingthe muscle for access.Initial exposureThe neck is opened via a horizontalincision placed in a skin crease just belowthe level <strong>of</strong> the hyoid bone. The incision ismade through skin, subcutaneous fat, andplatysma muscle. Identify the externaljugular vein and greater auricular nerveNext the superior skin flap is elevated withcautery in a subplatysmal plane until thesubmandibular salivary gland is identified.The surgeon then uses electrocautery or ascalpel to raise an inferiorly basedsubplatysmal flap, exposing the neck asfollows: anteriorly up to the omohyoidmuscle (the posterior margin <strong>of</strong> whichcorresponds to the anterior margin <strong>of</strong> thesupraomohyoid or anterolateral neckdissections) and inferiorly, the lateralsurface <strong>of</strong> the SCM almost to the clavicleThe only structure to look out for and notinjure during this step <strong>of</strong> the dissection isthe external jugular vein which lies on thelateral surface <strong>of</strong> the sternomastoid muscle.The recommended subsequent operativesteps <strong>of</strong> a supraomohyoid neck dissecttionare illustrated in Figure 7.Step 1 (Figures 7)The surgeon resects fat and lymph nodesfrom the submental triangle (Level Ia).The skin is elevated in a subplatysmalplane up to the opposite anterior belly <strong>of</strong>digastric muscle, looking out for the3
Step 2 (Figure 7)54663Figure 7: Recommended surgical steps forsupraomohyoid neck dissectionanterior jugular veins. The contents <strong>of</strong> thesubmental triangle are resected withelectrocautery up to the hyoid bone. Thedeep plane <strong>of</strong> dissection is the mylohyoidmuscle (Figures 8, 9).27 41The surgeon next addresses Level Ib <strong>of</strong> theneck. The fascia (capsule) overlying thesubmandibular gland is incised midwayover the gland and is dissected from thegland in a superior direction in a subcapsularplane so as to avoid injury to the marginalmandibular nerve (Figure 10). Usingthis technique the marginal mandibularnerve does not need to be routinelyidentified; the assistant however watchesfor twitching <strong>of</strong> the lower lip as this indicatesproximity to the nerve. The marginalmandibular nerve crosses the facialartery and vein (Figure 11).The facial arteryand vein are identified by blunt dissectionwith a fine haemostat (Figure 11).Figure 8: Resection <strong>of</strong> submental triangleFigure 10: Incision <strong>of</strong> submandibularsalivary gland capsuleFigure 9: Resection <strong>of</strong> submental trianglefrom mylohyoid muscleNext attention is directed to the fat andlymph nodes tucked anteriorly betweenthe anterior belly <strong>of</strong> digastric and mylohyoidmuscle (Figure 11). These nodes areespecially important to resect withmalignancies <strong>of</strong> the anterior floor <strong>of</strong>mouth. To resect these nodes one retractsthe anterior belly <strong>of</strong> digastric anteriorlyand delivers the tissue using electrocauterydissection with the deep dissection planebeing on the mylohoid muscle (Figures 12,13).4
Marg mandibular nFacial vein (ligated)Facial arteryFigure 11: The submandibular gland hasbeen dissected in a subcapsular plane; themarginal mandibular nerve is seencrossing the facial artery and vein; fat andnodes are delivered from the anteriorpocket deep to digastric (white arrow)Figure 12: Dividing the facial vesselsbelow the marginal mandibular nerveOther than the nerve to mylohoid andvessels that pierce the muscle and need tobe cauterized or ligated, there are nosignificant structures until the dissectionreaches the posterior free margin <strong>of</strong> themylohyoid muscle.Next attention is directed at the region <strong>of</strong>the facial artery and vein. The surgeonpalpates around the facial vessels for faciallymph nodes; if present, they are dissectedfree using fine haemostats, taking care notto traumatise the marginal mandibularnerve. The facial artery and vein are thenligated and divided close to the submandibulargland so as not to injure the marginalmandibular nerve (Figure 12). Thisfrees up the gland superiorly, which canthen be reflected away from the mandible(Figure 13).Next the surgeon addresses the lingualnerve, submandibular duct, and XIIn.The mylohyoid muscle is retractedanteriorly with a right-angled retractor.The clearly defined interfascial dissectionplane between the deep aspect <strong>of</strong> thesubmandibular gland and the fasciacovering the XIIn is opened with fingerFigure 13: Marginal mandibular nervevisible over divided facial vessels; glandreflected inferiorly; mylohyoid musclewidely exposeddissection, taking care not to tear the thinwalledveins accompanying XIIn. TheXIIn is now visible in the floor <strong>of</strong> thesubmandibular triangle (Figure 14).Inferior traction on the gland brings thelingual nerve and the submandibular ductinto view (Figure 14). The submandibularduct is separated from the lingual nerve,ligated and divided (Figures 15, 16).5
The submandibular ganglion, suspendedfrom the lingual nerve, is clamped, dividedand ligated, taking care not to cross-clampthe lingual nerve (Figure 16).Figure 14: Finger dissection delivers thesubmandibular gland and duct, and bringsthe lingual nerve into view. The proximalstump <strong>of</strong> the facial artery is visible at thetip <strong>of</strong> the thumb, and the XIIn is seenbehind the nail <strong>of</strong> the index fingerThe facial artery is divided and ligatedjust above the posterior belly <strong>of</strong> digastric(Figure 17). Note: A surgical variation <strong>of</strong>the above technique is to preserve thefacial artery by dividing and ligating the 1-5 small branches that enter the submandibulargland. This is usually simple to do,it reduces the risk <strong>of</strong> injury to the marginalmandibular nerve, and permits the use <strong>of</strong> abuccinator flap based on the facial artery(Figure 18).Figure 15: Submandibular ductFigure 17: Clamping and dividing thefacial artery just above the posterior belly<strong>of</strong> digastricFigure 16: Separating the submandibularganglion from the lingual nerveFigure 18: Facial artery has been keptintact; a branch is being divided6
Step 3 (Figure 7)This step entails identifying the XIIn inLevel IIa, and tracing the XIIn posteriorlyto where it leads the surgeon directly tothe internal jugular vein (IJV).Divide the external jugular vein (Figure19). This is a key step with SND as itimproves access to Levels IIa and IIb. Thegreater auricular nerve is preserved.Figure 20: Dissect along the entire length<strong>of</strong> the digastricFigure 19: Divide the external jugular veinDivide the fascia along the lateral aspect<strong>of</strong> the posterior belly <strong>of</strong> digastric (Figure20). This step is the key to facilitatingsubsequent exposure <strong>of</strong> the IJV and XIn.Expose the posterior belly <strong>of</strong> digastricalong its entire length, taking care not towander above the muscle as this mightjeopardise the facial nerve. No significantstructures cross the posterior belly otherthan the facial vein.Next identify the XIIn below the greatercornu <strong>of</strong> the hyoid bone anterior to whereit crosses the external carotid artery. It isgenerally more superficial than expected,and is located just deep to the veins thatcross the nerve. Carefully dissect along thenerve in a posterior direction and divide allthe veins crossing the nerve to expose thefull length <strong>of</strong> XIIn (Figure 21).Figure 21: Divide the veins that cross theXIInAfter the nerve has crossed posterior to theexternal carotid artery, identify the SCMbranch <strong>of</strong> the occipital artery that tethersthe XIIn (Figure 22). Dividing this arteryreleases the XIIn (Figure 23). The nervethen courses vertically along the anteriorsurface <strong>of</strong> the IJV and hence leads thesurgeon directly to the IJV (Figure 23).Using dissecting scissors or a haemostat topart the fatty tissue behind the IJV in LevelII, the surgeon next identifies the XInwhich may course lateral (commonly),medial (uncommonly) or through (veryrarely) the IJV. The nerve is <strong>of</strong>ten firstlocated by noting movement <strong>of</strong> the7
shoulder due to mechanical stimulation <strong>of</strong>the nerve (Figure 23).a scalpel (Figure 24). This exposes structuresdeep to the SCM i.e. the remainder <strong>of</strong>Levels II and III <strong>of</strong> the neck and the lateralsurface <strong>of</strong> the omohyoid muscle as itcrosses the internal jugular vein. A number<strong>of</strong> small vessels entering the muscle areencountered and cauterized. The dissectionis carried posteriorly along the deep aspect<strong>of</strong> the muscle in a subepimysial plane up tothe posterior edge <strong>of</strong> the SCM.ArteryFigure 22: SCM branch <strong>of</strong> occipital arterytethering the XIInFigure 24: Dissect along the anteriorborder <strong>of</strong> the sternomastoid in asubepimysial plane taking care not toinjure the XIn where it enters the muscleFigure 23: Dividing the SCM branch <strong>of</strong> theoccipital artery frees the XIIn that thenleads directly to IJV. Note the XIn and thetunnel created behind IJVStep 4 (Figure 7)ECAXIInIJVTunnelXInDissect with a scalpel or electrocauteryalong the omohyoid and strip the fattytissue in the anterior parts <strong>of</strong> Levels II andIII from the underlying infrahyoid strapmuscles in a posterior direction towardsthe carotid sheath.Divide the epimysium along the anteriorborder <strong>of</strong> the SCM using electrocautery orStep 5 (Figure 7)Attention is now directed to clearing LevelIIb which is located posterior to the IJVand deep to SCM. Opinions differ as towhether Level IIb (posterior to XIn) needsto be routinely dissected so as to minimisetrauma to the XIn.The upper part <strong>of</strong> the SCM is retractedposteriorly to expose Level IIb. With ahaemostat, create a tunnel immediatelyposterior to the IJV down to theprevertebral muscles (Figure 23). Thismanoeuver speeds up the subsequentdissection <strong>of</strong> Level IIb by clearlydelineating the posterior wall <strong>of</strong> the IJV.The transverse process <strong>of</strong> the C1 vertebracan be palpated immediately posterior tothe XIn and IJV and serves as an additional8
landmark for the position <strong>of</strong> thesestructures in difficult surgical cases.In order to resect Level IIb, identify theXIn in Level IIb, and atraumaticallydissect it free from the surrounding fatwith sharp and blunt dissection up towhere it enters the SCM (Figure 23, 25-27).Figure 26: Pass the fat <strong>of</strong> Level IIbanteriorly under the XInFigure 25: Free the XIn from thesurrounding fatUsing a scalpel (due to proximity <strong>of</strong> XIn),or blunt dissection with a haemostat,proceed to mobilise Level IIb startingposterosuperiorly, with the assistantretracting the fatty tissue in an anteriordirection. The occipital artery passesacross to the top <strong>of</strong> Level IIb; its branchesmay need to be cauterized should they besevered while dissecting the superior part<strong>of</strong> Level IIb. Cut down onto the deepmuscles <strong>of</strong> the neck which are seen tocourse in a posteroinferior direction. Oncethe fat <strong>of</strong> Level IIb has been fullymobilized from the underlying muscles,pass it anteriorly underneath the XIn(Figure 26, 27).Step 6 (Figure 7)To resect Levels II and III, extend theincision along the posterior edge <strong>of</strong> thedeep aspect <strong>of</strong> SCM inferiorly through theFigure 27: Fat <strong>of</strong> Level IIb having beenpassed anteriorlyfatty tissue <strong>of</strong> Level 3. With the assistant(s)retracting the SCM posteriorly and the fat<strong>of</strong> levels II and III anteriorly with sharptoothedrake retractors, dissect the fattytissue <strong>of</strong> Levels II and III in an anterogradedirection. The deep dissection plane is themuscle the floor <strong>of</strong> neck between thebranches <strong>of</strong> the cervical plexus whichneed to be identified and preserved(Figure 28). The phrenic nerve andbrachial plexus are not seen in thisdissection, but are relevant if Level 4 isdissected. Continue the anterogradedissection with a scalpel or scissors untilthe ansa cervicalis, and the carotid sheathcontaining the common and internalcarotid arteries, Xn and IJV aresequentially exposed (Figure 29).9
CervicalplexusStep 7 (Figure 7)Continue stripping the fat and lymphaticsaround the anterior aspect <strong>of</strong> IJV until thecommon carotid artery is again reached.Divide and ligate tributaries <strong>of</strong> the IJVwith silk ties (Figure 31).Figure 28: Anterograde dissection <strong>of</strong>Levels II and III, preserving the cervicalplexusIJVCarotidXnAnsaXInFigure 29: IJV, common carotid artery,Xn, IJV, ansa cervicalis and XInThe carotid sheath is incised along the fullcourse <strong>of</strong> the vagus nerve, and the neckdissection specimen is stripped <strong>of</strong>f the IJVwhile dissecting inside the carotid sheath.The ansa cervicalis, which courses eitherdeep or superficial to the IJV may bepreserved (Figures 29, 30).Figure 31: Divide and ligate tributaries <strong>of</strong>the IJVInferiorly the fatty tissue at the junction <strong>of</strong>Levels III and IV is divided at the level <strong>of</strong>the omohyoid (supraomohyoid neckdissection). Identify and preserve thesuperior thyroid artery where it originatesfrom the external carotid artery (Figure32).DescendenshypoglossiFigure 32: Identify and preserve thesuperior thyroid arteryFigure 30: Further anterior dissectionshowing descendens hypoglossi component<strong>of</strong> ansa cervicalisWith a Lateral ND Level IV is resected byapplying traction to the fatty tissue deep tothe omohyoid in a cephalad direction whiledissecting it from Level IV with a scalpel;the transverse cervical vessels may be10
encountered and need to be ligated; fingerdissection may be used to establish adissection plane between the fat <strong>of</strong> LevelIV and the brachial plexus and phrenicnerve; be vigilant for a chylous leak as thethoracic duct (left neck) or right lymphaticduct may be transected.The final step is to complete stripping theneck dissection specimen <strong>of</strong>f theinfrahyoid strap muscles taking care not toinjure the XIIn and its accompanying veinssuperiorly, and to deliver the neckdissection specimen (Figure 33).Useful referencesRobbins KT, Shaha AR, Medina JE, et al.Consensus statement on the classificationand terminology <strong>of</strong> neck dissection. ArchOtolaryngol Head <strong>Neck</strong> Surg 2008;134:536–8Ferlito A, Robbins KT, Shah JP, et alProposal for a rational classification <strong>of</strong>neck dissections. Head <strong>Neck</strong>. 2011Mar;33(3):445-50Harris T, Doolarkhan Z, Fagan JJ. Timing<strong>of</strong> removal <strong>of</strong> neck drains following headand neck surgery. Ear Nose Throat J. 2011Apr;90(4):186-9Author & EditorFigure 33: Completed supraomohyoid NDClosureThe neck is irrigated with warm water, theanaesthetist is asked to do a valsalvamaneuver so as to elicit unsecuredbleeding vessels and chyle leakage, and a5mm suction drain is inserted. The neck isclosed in layers with continuous vicryl toplatysma and sutures/staples to skinPostoperative careThe drain is maintained on continuoussuction e.g. low pressure wall suction, untilthe drainage volume is