New Directions In Robotic Surgery UA Surgeons Perform First
New Directions In Robotic Surgery UA Surgeons Perform First
New Directions In Robotic Surgery UA Surgeons Perform First
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
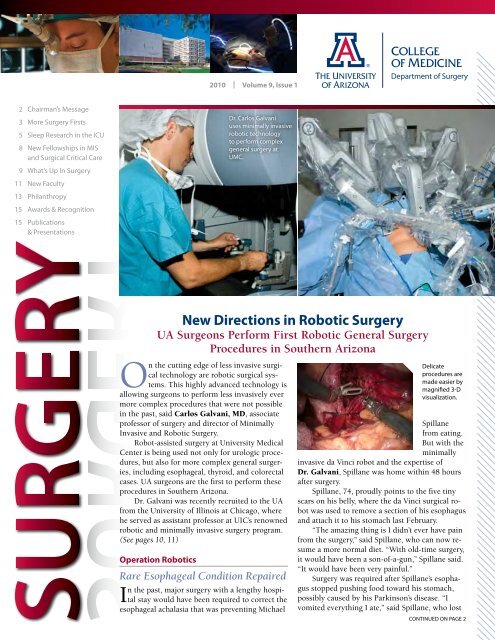
2010 | Volume 9, Issue 12 Chairman’s Message3 More <strong>Surgery</strong> <strong>First</strong>s5 Sleep Research in the ICU8 <strong>New</strong> Fellowships in MISand Surgical Critical Care9 What’s Up <strong>In</strong> <strong>Surgery</strong>11 <strong>New</strong> Faculty13 Philanthropy15 Awards & Recognition15 Publications& PresentationsDr. Carlos Galvaniuses minimally invasiverobotic technologyto perform complexgeneral surgery atUMC.<strong>New</strong> <strong>Directions</strong> in <strong>Robotic</strong> <strong>Surgery</strong><strong>UA</strong> <strong>Surgeons</strong> <strong>Perform</strong> <strong>First</strong> <strong>Robotic</strong> General <strong>Surgery</strong>Procedures in Southern ArizonaOn the cutting edge of less invasive surgicaltechnology are robotic surgical systems.This highly advanced technology isallowing surgeons to perform less invasively evermore complex procedures that were not possiblein the past, said Carlos Galvani, MD, associateprofessor of surgery and director of Minimally<strong>In</strong>vasive and <strong>Robotic</strong> <strong>Surgery</strong>.Robot-assisted surgery at University MedicalCenter is being used not only for urologic procedures,but also for more complex general surgeries,including esophageal, thyroid, and colorectalcases. <strong>UA</strong> surgeons are the first to perform theseprocedures in Southern Arizona.Dr. Galvani was recently recruited to the <strong>UA</strong>from the University of Illinois at Chicago, wherehe served as assistant professor at UIC’s renownedrobotic and minimally invasive surgery program.(See pages 10, 11)Operation <strong>Robotic</strong>sRare Esophageal Condition Repaired<strong>In</strong> the past, major surgery with a lengthy hospitalstay would have been required to correct theesophageal achalasia that was preventing MichaelDelicateprocedures aremade easier bymagnified 3-Dvisualization.Spillanefrom eating.But with theminimallyinvasive da Vinci robot and the expertise ofDr. Galvani, Spillane was home within 48 hoursafter surgery.Spillane, 74, proudly points to the five tinyscars on his belly, where the da Vinci surgical robotwas used to remove a section of his esophagusand attach it to his stomach last February.“The amazing thing is I didn’t ever have painfrom the surgery,’’ said Spillane, who can now resumea more normal diet. “With old-time surgery,it would have been a son-of-a-gun,’’ Spillane said.“It would have been very painful.’’<strong>Surgery</strong> was required after Spillane’s esophagusstopped pushing food toward his stomach,possibly caused by his Parkinson’s disease. “Ivomited everything I ate,’’ said Spillane, who lostcontinued on PAge 2
2Chairman’s MessageThe Department of <strong>Surgery</strong>continues to experience remarkablegrowth through the addition ofinnovative clinical services and therecruitment of nationally recognizedfaculty, both crucial to our missionto provide the highest quality surgicalcare in the Southwest.<strong>In</strong> addition, our researchprograms are growing and oureducational programs are becomingstronger. We continue to attractsuperb candidates for our residencyand fellowship training programs,as well as outstanding faculty members.Through our publications andpresentations, we share our knowledgenationally and internationally.We are happy to welcome newleadership in the department,including two new division chiefs,Dr. Michael Lemole in Neurosurgeryand Dr. Alex Chiu in Otolaryngology,who will build a Center forSinonasal and Skull Base <strong>Surgery</strong>.This multidisciplinary center willprovide the most advanced techniquesin endoscopic management ofsinonasal and skull base diseases.We are especially proud of ourincreasingly multidisciplinaryprograms in robotic and minimallyinvasive surgery; solid-organtransplantation; pancreatic, liver,and upper gastrointestinal cancers;colorectal disease; trauma; and bariatricsurgery – all of which are nowestablished and expanding. <strong>In</strong> manysurgical subfields, we have nowgained the expertise that will allowfor most effectively performing clinicaland translational research.Most exciting is the merging ofUniversity Medical Center (UMC)and the physician practice plan,University Physicians Healthcare(UPH). UMC has significantlyenlarged thetrauma centerand the surgicalintensive careunit (SICU). Andthe beautiful newDiamond Children’s Medical Centerrecently opened.We remain committed to enhancingour teaching activities. <strong>New</strong>fellowships have been approved inminimally invasive surgery and insurgical critical care. General surgeryresidents continue to spend one weekper year in the surgical training labto improve their skills in laparoscopicand minimally invasive procedures.Last year the first two residentsenrolled in the department’s MedicalSciences Graduate Program to worktoward their master of science inmedicine, thanks to an endowment tosupport research and education in theDepartment of <strong>Surgery</strong>. This year, twomore residents will join the program;one of whom will earn a PhD.These are exciting and invigoratingtimes for the University ofArizona. Our Department of <strong>Surgery</strong>encompasses an incredibly vibrantgroup of impressive individuals – facultyand staff, residents and students,research technicians and clinicalcaregivers – dedicated to the very bestin patient care, research, and education.Thank you for your continuedsupport.Sincerely,Rainer W.G. Gruessner, MDProfessor and Chairman<strong>UA</strong> Department of <strong>Surgery</strong><strong>Surgery</strong> is published annually by the Arizona Health Sciences Center Office of Public Affairs,P.O. Box 245066, Tucson, AZ 85724-5066 | (520) 626-7219 | Visit us online: www.surgery.arizona.eduEditor: Jo Marie Gellerman | Design: Arizona Health Sciences Center Biomedical CommunicationsAll contents © 2010 Arizona Board of Regents. All rights reserved. The <strong>UA</strong> is an EEO/AA - M/W/D/V Employer.If you need this information in an accessible format (Braille, digital, tape or large print) please contact Jo Gellerman,(520) 626-7219.Quality Patient Care<strong>Robotic</strong> <strong>Surgery</strong>continued from PAge 130 pounds.The disorder is rare, occurring in one in100,000 people, Spillane said. A gastroenterologistsuggested he find the best surgeonin the country to perform the complicatedprocedure.“This is nothing to fool around with,’’his doctor told him, before recommendingDr. Galvani.A flight nurse during the Vietnam War,Spillane was fascinated by the technologyused to fix his esophagus. He checked outthe da Vinci robot briefly, in the momentsbefore he was sedated for surgery. He wastold that a robotic arm would lift his liver sothat the machine had access to his esophagusandstomach.The arms,directed bysurgeons,removedpart of theesophagusand attachedhisstomach tothe posteriorof hisesophagus,with the robotsuturing the organs.Spillane believes it a bit of a miracle thathe was living in the right place at the righttime.Taking the Scar Out ofThyroid <strong>Surgery</strong>typical open surgery to remove all orA part of the thyroid can leave a visiblescar up to three inches long across the frontof the lower neck. Through an incision madeat the armpit, surgeons at the <strong>UA</strong> Departmentof <strong>Surgery</strong> using the da Vinci SurgicalSystem channeled the instruments to thegland, a delicate procedure made easier bythe three-dimensional visualization andmaneuverability of the robot. The incision iswell hidden, leaving no scar on the patient’sneck.A surgical team led by Marlon Guerrero,MD, assistant professor of surgery anddirector of the Endocrine <strong>Surgery</strong> Center,
assisted by Dr. Galvani, performedSouthern Arizona’s first transaxillaryrobot-assisted thyroid lobectomy on48-year-old Raquel Vizcarra. Doctorsdiscovered two nodules on Vizcarra’sthyroid that turned out to be follicularadenoma. She had a 20 percent risk ofthe tumors being cancerous so she optedfor surgery.“I felt very comfortable choosing therobot,” said Vizcarra. “I was happy tohave no scar on my neck, but I also likedthat the robot can help the surgeon bemore precise.”Vizcarra was discharged the nextday.“<strong>Robotic</strong> thyroid or parathyroid surgeriesare options for most patientswho require surgery for benign orcancerous thyroid disease,” saidDr. Guerrero. “If you don’t want tohave a neck scar, robotic surgery isthe best way to do it.”Rectal Cancer CuredThree days after a robot was usedto remove cancer that had invadedher rectum, Sally Brock receivedthe best news of her life. “The surgerywas 100 percent successful,’’ saidBrock, 60. “The nightmare was over.’’Colorectal surgeon Liana Tsikitis,MD, assistant professor, Division of SurgicalOncology, was the first in SouthernArizona to use the da Vinci surgicalrobot to perform an abdominal perinealresection. With traditional surgery, Brockwould have undergone alengthy procedure, leavinga sizable abdominalscar, a difficult recoveryand greater chance ofinfection. The da Vinciallowed Tsikitis to enterthrough four tiny incisionsin the abdomen, with robotarms removing the diseasedtissue through the anus in adelicate procedure that lasted90 minutes.The use of the da Vinciis new in rectal resections.“It’s a technically demandingMore <strong>Surgery</strong> <strong>First</strong>s in theFight Against CancerExtending Lives of Patients with Deadly Mesothelioma<strong>In</strong> the first successful surgery of its kind in Southern Arizona, <strong>UA</strong> thoracicsurgeon Jonathan C. Daniel, MD, in February performed a highly complexprocedure to treat malignant mesothelioma on Tucsonan James Massie, a formerpresidential interpreter and retired Marine.A rare and deadly form ofcancer associated with asbestosexposure, mesothelioma invadesthe thin lining of the body’s organs,most commonly the lungs.Without treatment, life expectancyis six months. Chemotherapycan extend life by only a few moremonths.But since the arrival lastSeptember of Dr. Daniel, assistantprofessor in the Division of Cardiothoracic<strong>Surgery</strong>, the <strong>UA</strong> hasoffered Arizona patients anotheroption: surgical intervention withextrapleural pneumonectomy orradical pleurectomy.While it is not expected to be a cure, Massie, 65, hopes the procedure willadd years to his life.“We want to truly enjoy life as much as we can – hiking, camping, just enjoyingeach other’s company,’’ Massie said of the time that he and Sherry, his wifeof 35 years, have been given as a result of the surgery.operation,’’ Dr. Tsikitis said, adding thatmost abdominal perineal resections areperformed through traditional surgery.Brock, whohad owned anart gallery in herhometown ofBisbee, discoveredrectal bleeding inAugust 2009. Herprimary care physicianordereda colonoscopy.“Here I was 60,but I had neverhad a colonoscopy,’’Brocksaid. “I put itoff year afteryear.’’Dr. Jonathan Daniel performs a highly complicatedprocedure to treat a deadly form of lung cancer.continued on PAge 4She was shocked at the diagnosis.While the tumor was advanced, it hadnot spread to the lymph nodes. Brockwas certain she wanted to receive treatmentat the <strong>UA</strong> and she was intriguedby the da Vinci. “I was just tickled aboutit,’’ she said of robotic surgery. “You healmuch faster. There’s not as much tissuethat is cut and it’s less disruptive to yourorgans.’’The best news came on Brock’s thirdday in the hospital, when she learnedthe surgery was a success. “I needed nofurther radiation or chemotherapy,’’ shesaid. “It was the best news ever.’’To refer a patient or foran appointment, call(520) 694-10003
Quality Patient Care<strong>Surgery</strong> <strong>First</strong>scontinued from PAge 3After Massie underwent fourrounds of chemotherapy, Dr. Danielremoved the tumor, the lung, the coveringof the heart, and the diaphragm.A new pericardium – or covering ofthe heart – and diaphragm were createdwith the synthetic material Gore-Tex, commonly used in ski gloves.Following surgery, radiation was usedto blast Massie’s chest cavity toprevent the cancer from returning.With preoperative chemotherapyadministered at the Arizona Cancer Centerby nationally recognized mesotheliomaoncologist Linda Garland, MD, and post-op intensity-modulated radiation byAlexander Chi, MD, the <strong>UA</strong> hopes todevelop into the premier center formesothelioma treatment in the Southwest,Dr. Daniel said.Having recently finished gruelingradiation sessions, Massie is gettingstronger. He and his wife are takingshort hikes and walks. They plan totravel later this year.“Our hope is to get as many yearsas we can,’’ Sherry Massie said.4‘Hot Chemo’ Offers Hope for Patients with Advanced Abdominal Cancernew therapy, first offered and only available in Arizona at the <strong>UA</strong> DepartmentA of <strong>Surgery</strong> and University Medical Center, is providing hope to patients withmetastasized abdominal cancers.“Regional and metastatic disease is the new frontier in cancer treatment,” saidEvan S. Ong, MD, <strong>UA</strong> assistant professor of surgery, who has created the Regionaland Metastatic Disease Center to address this challenge. “We deal with patientswith stage IV cancers.”Hyperthermic intraperitoneal chemoperfusion (HIPEC) is a relatively newtreatment for several types of metastasized abdominal cancers, including cancersof the stomach, colon, ovaries, liver, and appendix that have spread but are stilllimited to the abdominal region. Immediatelyfollowing surgery to removecancerous lesions, <strong>UA</strong> surgeonsadminister a heated chemotherapysolution that is circulated throughoutthe abdomen for nearly two hours.Because the chemo drug is retained inthe abdominal cavity and not spreadthroughout the body, the surgeons areable to give 80 to 400 times the usualdose, depending on the drug. Heatingthe chemotherapy to high temperatures(102 degrees) helps it to workmore effectively.“<strong>In</strong> the past, no effective treatmentoptions wereCirculating the heated chemotherapy throughoutthe abdominal cavity allows it to be distributedthoroughly and to penetrate the areas of cancerdirectly. By delivering directly to the tumor, manyof the side effects associated with intravenouschemotherapy can be avoided.available forthese patients,”Dr. Ong said.“<strong>Surgery</strong>would befollowed by chemotherapy treatments, but eventually thecancer became resistant to the chemotherapy. But nowwe’re seeing survival rates of 30 to 40 percent over fiveyears for patients with stage IV colorectal cancer versus0 percent just 10 or 20 years ago.”Dr. Evan Ong is one of only a few surgeons thatoffer the option of combining surgery with theHIPEC procedure for metastasized abdominalcancers.Throughout the treatment, patientslike Richard Mackey, who was diagnosedwith stomach cancer, are surprised byhow little pain they have experienced,said Dr. Ong.“<strong>In</strong> the past, youoften saw cancerpatients who diedin agony. But withnewer, minimallyinvasive surgicaltechniques, plusnew chemotherapiesand betterways to relievepain, that is nolonger the picture.”
Cutting-Edge ResearchUpdate on Transplant <strong>First</strong>sThree Organs forOne-Year-OldLast fall, a one-year-old girl fromGilbert, Ariz., successfully underwenta three-organ multivisceral transplantat University Medical Center. Thefirst procedure of its kind performed inArizona and the Southwestern UnitedStates, Adrianna Martinez’s transplantincluded the liver, small bowel, andpancreas from a deceased baby donor.The organs were transplanted “en bloc”(kept together as a single unit) in a seven-hour operation, a complex procedure thatis rarely performed and requires superb logistical, surgical, and medical coordination.Adrianna was born without a small bowel. Her rare congenital malformationmade it impossible to digest food. She also was born with situs inversus – herabdominal organs were positioned on the wrong side – making her condition evenmore complex.Almost a year later, “Adrianna looks good,” said Khalid Khan, MBChB, MRCP,<strong>UA</strong> associate professor of surgery and a gastroenterologist specializing in pediatricliver and intestine transplants. “It is amazing to see the change in these children followingtheir procedures. Once they have their transplants, they have an exceptionallygood prospect for living a totally normal life.”Tasha Bowman, Adrianna’s mother, said the toddler is starting to catch up developmentallyand is now walking. “People are always so surprised to hear she hadthree of her organs transplanted.”“We continue to achieve levels of excellence in transplant surgery by offeringlifesaving options for children and adults with intestinal failure and liverdysfunction,” said Rainer Gruessner, MD, chief of transplantation and surgerydepartment chairman.Islet Cell Transplants Treat Chronic PancreatitisSince performing the first islet cell autotransplant in the region last summer, <strong>UA</strong>surgeons have transplanted islet cells in seven patients suffering from chronicpancreatitis.The transplantation of the insulin-producing islet cells following the removal of apatient’s pancreas alleviates pain and avoids surgically induced diabetes, said HoracioRilo, MD, director of the department’s <strong>In</strong>stitute for Cellular Transplantation. The <strong>UA</strong>Department of <strong>Surgery</strong>’s Class10,000 clean room, a state-ofthe-artfacility, makes isolatingcells to treat debilitating diseasespossible. Only a handfulof medical centers worldwideare able to offer this procedure.Dr. Horacio Rilo is internationallyknown for his work in cellulartransplantation. His researchlaboratory houses the high-tech,FDA-approved, Class 10,000clean room.Trauma ResearchTargets ImprovingOutcomesHelping ICU Patients Getthe Sleep They NeedSleep is essential for recovery froman illness or injury. Yet, acutely illpatients in hospital intensive care units(ICUs) who need the most rest are gettingthe least.Randall S. Friese, MD, associateprofessor in the Division of Trauma,Critical Care and Emergency <strong>Surgery</strong>, isconducting a study investigating sleeppromotion during critical illness andinjury to help ICU patients get the restthey need to heal.“Beeping monitorsand round-theclocktreatments makegetting restful sleepnearly impossible inthe ICU,” Dr. Friesesaid. “Patients maylook like they aresleeping, but they’re“Ourresearch willdemonstratewhether astrategy topromotesleep inpatients inan ICU settingduringrecoveryfrom a criticalillness orinjury resultsin improvedhealing.”–Dr. Friesenot sleeping well.They are not gettingto the restorative stagesthat are required.”Previous researchconducted by Dr.Friese, one of the firstdoctors to examinesleep patterns ofsurgical and traumapatients, revealedthat while patients inthe ICU received anacceptable amount ofsleep, most of it wasnot a deep sleep. Hefound that patientsin the ICU spent 96percent of their sleepcycle in superficialstages. With normalsleep, as much as 50 percent of the sleepcycle is in the deep, restorative stages.The current study at the Universityof Arizona and University Medical Centeris funded by an Arizona Biomedicalcontinued on PAge 65
Cutting-Edge ResearchSleepcontinued from PAge 5Research Commission grant.“Our research will demonstrate whethera strategy to promote sleep in patientsin an ICU setting during recovery from acritical illness or injury results in improvedhealing,” Dr. Friese explained. “We will approachthe study in three phases: developa manual for sleep promotion and stafftraining; implement and test the protocol;and conduct a pilot trial to determine itseffectiveness.”Some proposed steps to decreasedisturbances in the ICU include adjustingmonitors so that alarms don’t wake up patients,providing ear plugs and eye shields,dimming the lights, and using pharmacologicsleeping aids.“If doctors and ICU directors developand put into practice protocols for promot-in the United States, causing some 50,000deaths and 80,000 new cases of long-termdisability each year.Preliminary studies in the UnitedStates and China have shown that progesingsleep, I believe that outcomes,including infection rates, ICU andhospital lengths of stay, overallcomplication rates and most important,mortality rates, will improve.”new clinicalA trial affectingthe treatmentof Southern Arizona patients withtraumatic head injuries is underway inthe University Medical Center TraumaCenter. UMC is one of 17 major traumacenters around the country participatingin a five-year, $14.5 million researchproject funded by the National <strong>In</strong>stitutesof Health.The Progesterone for the Treatmentof Traumatic Brain <strong>In</strong>jury (ProTECT III)study will determine whether the hormoneprogesterone is useful in improvingoutcomes following severe head injury,as suggested in small preliminary studiesby Atlanta’s Emory University, which isleading the nationwide clinical trial.<strong>In</strong> Tucson, Randall S. Friese, MD,<strong>UA</strong> Department of <strong>Surgery</strong>, and KurtDenninghoff, MD, <strong>UA</strong> Department ofEmergency Medicine, are the principalinvestigators.Traumatic brain injury (TBI) is suddendamage to the brain caused by anoutside force to the head, such as a carcrash, a fall, or any blow to the skull.Traumatic Brain <strong>In</strong>jury StudyBegins in UMC Trauma CenterThe UMC Trauma Center, the only level1 Trauma Center in Southern Arizona,treats approximately 500 patients withmoderate to severe TBI each year, saidDr. Friese, a trauma surgeon.For those who survive, TBI can affecta person’s ability to concentrate andremember as well as cause problems withbalance and coordination, he said. Manysurvivors of TBI are severely disabled. TBIis the leading cause of death and disabilityin children and adults 1 to 44 years of ageterone, when given immediately afterTBI, may reduce brain swelling anddamage. One study showed a 50 percentdecrease in mortality. Progesterone isnaturally present in small amounts inthe brains of both males and females.Progesterone is critical for the normaldevelopment of neurons in the brainand seems to have a protective effect ondamaged brain tissues.As part of the ProTECT III clinicaltrial, brain-injured adults treated in theUMC Trauma Center may receive progesteroneif they are 18 or older, have amoderate to severe brain injury, and canstart the medication within four hoursafter the injury. Patients who meet theseand other criteria will be entered randomly– like flipping a coin – into oneof two study groups: one that receivesan IV mixture with progesterone andone that receives an IV mixture withplacebo.Everyone in the study will be giventhe standard medical care for TBI. Thisis a double-blind study, meaning thatneither the patient nor doctors, nursesor researchers will know whether anyparticular patient received the progesteroneor placebo.6
Researchers Receive $1.2 Million toMonitor Activity of DiabeticsResearchers in the <strong>UA</strong> Department of <strong>Surgery</strong> have been awarded a $1.2 milliongrant to use cutting-edge technology in the form of a simple computerized undershirtto monitor activity among diabetics with foot wounds. The study will determinethe role activity plays in the formation of sores in an effort to better understandhow to prevent wounds.David G. Armstrong, DPM, MD, PhD, professor of surgery and co-founder ofthe <strong>UA</strong> Department of <strong>Surgery</strong> Southern Arizona Limb Salvage Alliance (SALSA), aninternationally renowned center for diabetic wound treatment and amputation prevention,is taking a lead role in the international collaborative. Dr. Armstrong hopesthe study will ultimately result in fewer infections and amputations. It is funded bythe Qatar National Research Foundation.“This is potentially game-changing. The kind of data we’re going to collect on alarge scale will help us better tailor activity for a broad spectrum of patients that gobeyond this one disease,’’ said Dr. Armstrong.The technology being used is a bodywornsensor that will for the first time allowresearchers to accurately monitor activity.Over the course of the three-year study, 112diabetics with foot wounds will be enrolled atthe <strong>UA</strong> and at Hamad Medical Corporation inDoha, Qatar, and monitored through a comfortabletank top. Partnering in the collaborationis the Center for Lower ExtremityAmbulatory Research (CLEAR)in Chicago.“It doesn’t cramp your style at“This could be like ahome security systemfor your body.’’– Dr. Armstrongall,’’ Dr. Armstrong said of the device.“It can assess not just the steps thatwe take, but many other things. It canmeasure if you are standing or sitting,jumping or running, lying down on your stomach oryour back. We are able to gauge, with highly sensitiveequipment, what’s going on with the foot and rest ofthe body based on subtle movements that occur in the trunk.“We used to think that it was the number of steps that people took that mightpredict whether they got a wound or not,’’ Dr. Armstrong said. “The more steps youtook, the more likely you were to get a blister, which would become a wound.’’But Dr. Armstrong now believes that other movements may be responsible: walkingin short bursts around the home may actually be more dangerous than walkinga mile outdoors.“<strong>In</strong>jury might not be occurring during the walking, but during thestarting and stopping.“The great news is that this problem is preventable. And one of the ways it’s preventableis in better assessing activity levels in patients.’’Dr. Armstrong hopes sensors ultimately will be available to all people withdiabetes, possibly embedded in cell phones. If a person is moving in a manner that ismore likely to cause a wound, the person and his or her physician would be alertedelectronically.“This could be like a home security system for your body,’’ Dr. Armstrong said.The study aims to help researchers determine the most effective forms of exerciseand activity for people with diabetes.“We want people to be as active as they can but we don’t want them to be activein a way that hurts them,’’ Dr. Armstrong said. “We think there’s a happy medium.We want to get people back to living their lives.’’<strong>In</strong>novative EducationThe <strong>Surgery</strong>DistinguishedLeadership AwardThe <strong>UA</strong> Department of <strong>Surgery</strong>honored George W. Drach, MD,with the 2010 Distinguished LeadershipAward at the <strong>Surgery</strong> Residentsand Fellows Scientific Research Dayand the Graduation Dinner on June 18.Dr. Drach served as keynote speaker atthe Scientific Research Day, presenting“Follow Your Dreams (With Help),”and at the Graduation Dinner, where hespoke on “An Arizona Boy Grows Up inAcademia.”The <strong>UA</strong> Department of <strong>Surgery</strong> DistinguishedLeadership Award recognizesthe outstanding leadership of individualsin surgery that led to improved surgicalpractices.The founding chief of the Divisionof Urology, Dr. Drach served on thefaculty of the <strong>UA</strong> Department of <strong>Surgery</strong>from 1970 to 1996. From 1996 to1998, he was at the University of TexasSouthwestern Medical School in Dallasas professor of urology and directedthe urology clinic at Parkland MemorialHospital. <strong>In</strong> 1998 he joined the Universityof Pennsylvania and now serves asprofessoremeritus.Dr. Drachhas authoredmore than 112journal articles,33 bookchapters, andthree books ormonographs.Dr. George Drach, foundingchief of Urology, andDr. Mitchell Sokoloff,current chief of UrologyHe receivedthe AmericanUrological Association(A<strong>UA</strong>)Hugh HamptonYoung award (outstanding contributionsto American urology) and A<strong>UA</strong> Research<strong>In</strong>novator (significant contributions toresearch) and Certificate of (Lifetime)Achievement awards. He served as thestudy monitor for the United StatesLithotripter Study (Dornier, <strong>In</strong>c. andthe National Electrical ManufacturersAssociation) from 1982 to 1996 and receivedthe honor of “Father of AmericanLithotripsy” in 1993.7
<strong>In</strong>novative Education<strong>UA</strong>’s <strong>First</strong> SurgicalCritical CareFellowshipThe <strong>UA</strong> Department of <strong>Surgery</strong> receivedaccreditation last March forthe first surgical critical care fellowshipin Tucson. Two fellows per year will beadmitted to a year-long training programfocusing on the treatment of critically illpatients in the newly opened, state-ofthe-art,20-bed intensive care unit (ICU)at University Medical Center.UMC is the only American Collegeof <strong>Surgeons</strong>-verified level I trauma centerin Southern Arizona. Trauma referralscome from Southern Arizona, <strong>New</strong> Mexico,and northern Mexico. More than5,000 trauma evaluations are conductedin the newly built trauma center eachyear, with many patients subsequentlyrequiring admission to the surgical ICU.The fellowship program has beengranted initial accreditation for fouryears, an unusually long period, which isa testament to the commitment and expertiseof the faculty, said Peter Rhee, MD,professor and chief, Division of Trauma,Critical Care and Emergency <strong>Surgery</strong>,and fellowship director.“We are extremely proud of what wehave been able to accomplish with thefellowship program. It is the first part ofour desire to have an internationally recognized‘acute care surgery’ fellowshipprogram, which isthe future of generalsurgery. This programwill generate the nextgeneration of generalsurgeons for Arizona,”said Dr. Rhee.The program’sfirst surgical criticalJorge Con, MDcare fellow, JorgeCon, MD, startedin July. Dr. Con recently completed hisresidency training at the University ofTexas in Austin.<strong>New</strong> Fellowship in MIS a <strong>UA</strong> <strong>First</strong>The <strong>UA</strong> Department of <strong>Surgery</strong> hasbeen accepted by the FellowshipCouncil to offer the first minimally invasivesurgery (MIS) fellowship in Tucson.The fellowship will provide thehighest level of training in advancedminimally invasive surgical techniquesto surgeons interested in an academiccareer in MIS and bariatric surgery.<strong>In</strong> addition to learning how to providetop-quality patient care in minimallyinvasive and robotic surgery, theprogram will prepare fellows to teachphysicians in communities across thecountry. This emphasis makes the <strong>UA</strong>fellowship one of the most distinctiveprograms in the country, said CarlosGalvani, MD, <strong>UA</strong> MIS fellowship programdirector.Starting July 2011, one fellow will beappointed each year following a five-yearresidency in general surgery (UnitedStates, Canada, or abroad).“Minimally invasive surgery hasmuch more to offer patients and so moreand more surgeons are applying to MISfellowship training programs every year,”said Dr. Galvani. “We are pleased to bemembers of the Fellowship Council andparticipate in the annual match.”More information can be found atfellowshipcouncil.org.Residents and Fellows Graduation 2010The <strong>UA</strong> Department of <strong>Surgery</strong> ended another academic year in June with 10graduating residents and fellows.General <strong>Surgery</strong>: Shelly Bansal, MD, accepted a cardiothoracic surgery fellowshipat Ohio State University; LeAnn Chavez, MD, is practicing for the<strong>In</strong>dian Health Service in Anchorage, Alaska; Adam Hansen, MD, is staying atthe <strong>UA</strong> for fellowship training in cardiothoracic surgery; Guillermo Higa, MD,has begun a minimally invasive surgery fellowship at the Cleveland Clinic inWeston, Florida; Rebecca Lyn Klein, MD, has begun a breast surgical oncologyfellowship at the University of Texas Southwestern Medical School in Dallas;Nazhone Yazzie, MD, is working for the Chickasaw Nation in Oklahoma.Neurosurgery: Sergio Rivero, MD, is completing his master’s degree in thenew Medical Sciences Graduate Program, which is being piloted in the <strong>UA</strong>Department of <strong>Surgery</strong>.Urology: Jennifer Linehan, MD, has gone to City of Hope in Duarte, California,to begin a urologic oncology fellowship; Maggie D. Vuturo, MD, wasawarded to a female urology fellowship at Cedars-Sinai in Los Angeles.Vascular <strong>Surgery</strong>: Trung Bui, MD, has joined a private practice in California.2010 Residents and Fellows ScientificResearch Day and Graduation8
What’s Up <strong>In</strong> SURGERYDr. Michael Moulton Named to EndowedChair for Research in Cardiothoracic <strong>Surgery</strong>The <strong>UA</strong> Department of <strong>Surgery</strong> andthe <strong>UA</strong> Sarver Heart Center haveappointed Michael J. Moulton, MD,associate professor of surgery, to theTony A. Marnell Sr. Endowed Chair forResearch in Cardiothoracic <strong>Surgery</strong>. Dr.Moulton is interim chief of the Divisionof Cardiovascular and Thoracic <strong>Surgery</strong>at the <strong>UA</strong> College of Medicine, surgicaldirector of lung transplantation, andprogram director of the CardiothoracicResidency Program.The endowment will enable Dr.Moulton to continue his research inmathematical modeling of the heart.Working closely with fellow Sarver HeartCenter member Timothy Secomb, PhD,professor of physiology and mathematics,Dr. Moulton is developing a novelmathematical model that generates a dynamicsolution of equilibrium equationsfor the contracting heart. This modelwill be used to more precisely diagnosecardiac abnormalities and improve treatmentoptions for heart failure patients.The Chair was established by anestate gift from Mr. Marnell in gratitudeto former cardiothoracic chief Jack G.Copeland, MD, who performed a hearttransplant on Mr. Marnell in 1989, givinghim 12 more years of an active, happylife.“The Marnell Endowed Chair is agreat honor. His generosity and foresightwill allow us to increase our researchactivities. This work will benefit patientswith heart failure and other serious cardiacproblems,” said Dr. Moulton.Dr. Moulton performs bothheart and lung transplants, aswell as coronary artery bypass,heart valve operations, and aortic surgery.According to the Scientific Registryof Transplant Recipients, the one-yearsurvival rate at the <strong>UA</strong> is 84 percent,exceeding the national average of 80percent.Dr. Moulton has published morethan 50 articles and abstracts in peer-reviewedjournals. He is an American Collegeof <strong>Surgeons</strong> fellow and a member ofthe Society of Thoracic <strong>Surgeons</strong> and the<strong>In</strong>ternational Society for Heart and LungTransplantation.Cardiothoracic surgeon Dr. Michael Moultondevelops mathematical models of the heartto more precisely diagnose and treat cardiacabnormalities.Farewell to Dr. Jack Copeland<strong>In</strong> June, Jack Copeland, MD, chief of the Division of Cardiovascularand Thoracic <strong>Surgery</strong>, accepted a position as professor ofadult and pediatric cardiac surgery at the University of California,San Diego (UCSD) Cardiovascular Center in La Jolla, California.An internationally renowned cardiothoracic transplant surgeon,Dr. Copeland performed the first heart transplant in Arizonain 1979. Since then, the <strong>UA</strong> team has performed more than1,000 heart transplants. <strong>In</strong> 1985, Dr. Copeland became the firstsurgeon in the world to perform a successful bridge-to-transplantprocedure using an artificial heart. <strong>In</strong> 2000, the <strong>UA</strong> Department of<strong>Surgery</strong>, <strong>UA</strong> Sarver Heart Center, and University Medical Centerbegan to study the “Berlin Heart,” a ventricular-assist device thatis attached to a child’s heart to provide relief. The device helpsstrengthen heart muscle to overcome congenital cardiomyopathy,eliminating the need for a transplant.Dr. Copeland served as co-director of the <strong>UA</strong> Sarver HeartCenter, as the Michael Drummond Distinguished Professor of <strong>Surgery</strong>,and as the Jack G. Copeland, MD, Endowed Chair of Cardiothoracic<strong>Surgery</strong>.Michael J. Moulton, MD, associate professor of surgery, isserving as interim chief of the Division of Cardiovascular andThoracic <strong>Surgery</strong> and director of the Cardiothoracic <strong>Surgery</strong>Residency Program.UMC-UPH Merges and <strong>Surgery</strong> GrowsLast June, the boards of directors from University MedicalCenter and University Physicians Healthcare agreed tointegrate the two health-care organizations affiliated with theUniversity of Arizona College of Medicine. The combined neworganization will be closer aligned with the <strong>UA</strong> to better servepatients and provide greater efficiencies across the system.The merger also allows for more growth in the <strong>UA</strong> Departmentof <strong>Surgery</strong>. Sincethe rebuilding of thedepartment began threeyears ago, surgeries atUMC have increased fromabout 800 procedures permonth to 1,200 proceduresper month, raisingthe need for more operating rooms. Thedepartment now will add more cases toUniversity Physicians Healthcare Hospital(UPHH) and branch outto the Ambulatory Care<strong>Surgery</strong> Center at 750 N.Alvernon. <strong>In</strong> addition,plans are underwayto establish a Level IIItrauma center at UPHH.9
<strong>UA</strong> CosponsorsTransplant Conferencein Florence, ItalyThe <strong>UA</strong> Department of <strong>Surgery</strong>cosponsored the 5th <strong>In</strong>ternationalConference on “Living DonorAbdominal Organ Transplantation:State of the Art,” heldJune 25-26, in Florence, Italy.The conference is a joint effortbetween the Universityof Arizona, the University ofChicago Medical Center, theUniversity of Illinois at Chicago,University Hospitals Leuven,Ghent University Hospitaland Medical School, and the Departmentof General <strong>Surgery</strong> and Transplantationat the University of Bologna.The <strong>UA</strong> co-chair was Rainer Gruessner,MD, chief, Division of AbdominalTransplantation, and Department of<strong>Surgery</strong> chairman.Presenters from around the globediscussed immunosuppressive strategiesand advanced techniques for livingdonor transplantation.MultidisciplinaryCancer ManagementCourse in Abu DhabiHugo Villar, MD, professor andchief of the Division of Surgical Oncology,served as the American Societyfor Clinical Oncology (ASCO) coursedirector for a Multidisciplinary CancerManagement Course (MCMC) heldin February in Abu Dhabi, United ArabEmirates. The objectives of each MCMCare to enhance understanding of multidisciplinarycancer management concepts.<strong>In</strong> addition, ASCO works togetherwith the host society to determine whatspecific knowledge would benefit courseattendees in the specific region.Dr. Villar has been heavily involvedwith the Commission on Cancer and inthe writing, teaching, and implementationof the MCMC. Under his leadership,the course extended first to Mexico andthen to Latin America and to the rest ofthe world, with an emphasis on underservedareas in Latin America and theMiddle East.<strong>First</strong> <strong>New</strong> e-HealthProgram in AlbaniaRifat Latifi, MD, professorof surgery in the Divisionof Trauma, Critical Care andEmergency <strong>Surgery</strong>, led thefirst Leadership TelemedicineTraining Course on July 15 inTirana, Albania, with a group ofAlbanian health specialists. Thecourse was offered as part of theU.S. Agency for <strong>In</strong>ternational Development(USAID) award to builda sustainable telemedicine programin the country.The <strong>In</strong>tegrated Telemedicineand e-Health Program is a two-year,$750,000 project, with the support ofthe Ministry of Health and the Universityof Tirana Medical School. Implementedby the <strong>In</strong>ternational Virtuale-Hospital Foundation and the AlaskanFoundation, the program includes anational telemedicine center in TiranaUniversity Hospital and 13 regionaltelemedicine centers.The network will help deliverquality health services using informationand communication technologiesfor the exchange of information fordiagnosis, treatment, and prevention ofdiseases and injuries; for research andevaluation; and for the continuingeducation of healthcare providers inAlbania.10<strong>New</strong> Surgical Weight Loss Program at UMCThe <strong>UA</strong> Department of <strong>Surgery</strong> haslaunched a new comprehensivebariatric surgery program at UniversityMedical Center. Aimed at helping obesepatients lose weight, theprogram combines minimallyinvasive and robot-assisted procedureswith diet, nutrition, andsupport services.The program’s director,Carlos Galvani, MD, is aninternationally recognized expertin robot-assisted and otherminimally invasive surgical techniques.He specializes in the three majortypes of weight-reduction surgery:n Gastric banding: a small pouch iscreated by “banding” the top of thestomach to severely restrict foodintake. Digestion is not interrupted.n Laparoscopic gastric bypass surgery:the surgeon makes a smallpouch of the stomach and redirectsthe intestine so food bypasses it.n Laparoscopic sleeve gastrectomy:this relatively new, nonreversibletechnique removes some 80 percentof the stomach, preventing some ofthe hormones that cause hunger tobe released.<strong>In</strong> addition, UMC offers revisionalsurgery to adjust or correct previousbariatric surgeries.As an academic medical center,UMC is able to provide a team of specialiststhat include dieticians, psychologists,critical care specialists, anesthesiologists,gastrointestinal specialists,radiologists, pulmonologists, and sleepdisorder specialists.
<strong>New</strong> FacultyMichael Teodori, MD, arenowned specialist insurgical treatments forhighly complex heartproblems in newbornsand children, has joinedthe <strong>UA</strong> Departmentof <strong>Surgery</strong> as clinicalprofessor of surgery anddirector of Pediatric Cardiovascular <strong>Surgery</strong>.Dr. Teodori spent 19 years in Phoenix,first in private practice, then joining PhoenixChildren’s Hospital in 2002. He is responsiblefor the development of the Children’s HeartCenter at Phoenix Children’s Hospital, wherehe performed 70 percent of Arizona’s pediatricheart surgeries a year.As a pediatric cardiac surgeon, Dr. Teodoriworks with children, from newborn infantsto teens, who have congenital heart defects.He is one of an elite corps of highly skilledpediatric cardiothoracic surgeons nationwidewho are able to perform complex surgeries onsome of the tiniest and most fragile patientswith birth defects like hypoplastic left heartsyndrome and transposition of the greatarteries.A native of Pittsburgh, Dr. Teodori receivedhis undergraduate degree in biology fromthe Massachusetts <strong>In</strong>stitute of Technology(MIT). He earned his medical degree fromUniversity of Pennsylvania School of Medicine,then completed residency training in generalsurgery and cardiothoracic surgery at theUniversity of Pittsburgh.Carlos A. Galvani, MD,is associate professorand director of Minimally<strong>In</strong>vasive and <strong>Robotic</strong><strong>Surgery</strong>. He comes tothe <strong>UA</strong> from the Universityof Illinois at Chicago(UIC), where he servedas assistant professor at UIC’s renowned roboticand minimally invasive surgery program.Dr. Galvani is an internationally recognizedexpert in robot-assisted surgery andother minimally invasive surgical techniques.He was a member of the UIC team thatperformed the world’s first robotic pancreatectomy(removal of the pancreas). He hasextensive experience in bariatric surgery,G. Michael Lemole, Jr., MD, a leading authority on skull basesurgery, has been appointed associate professor of surgery andchief of the Division of Neurosurgery at the <strong>UA</strong> Department of<strong>Surgery</strong>.<strong>In</strong> his previous position at the University of Illinois at Chicago(UIC), Dr. Lemole headed the UIC Skull Base Multidisciplinary Program. He also served asco-director of the Chicago CyberKnife Radiosurgery Center at Advocate Christ MedicalCenter.As the new chief of neurosurgery at the <strong>UA</strong> Department of <strong>Surgery</strong> and UniversityMedical Center, Dr. Lemole is expanding the department’s vascular and endovascular, skullbase, epilepsy, spine, and trauma capabilities. His focus is on creating multidisciplinaryteams of surgeons and specialists working together to offer the full range of leading-edgesurgical, radiosurgical, and medical treatments for patients with brain and spine disorders.Dr. Lemole’s clinical interests include diseases of the cranial base, or skull base,including both malignant and benign tumors, as well as congenital and traumaticanatomic defects. He also treats the wider variety of benign and malignant cranialneoplasms.Working with otolaryngology and oculoplastic surgery, Dr. Lemole will employminimally invasive approaches to remove tumors through the nasal passages andstereotactic radiosurgery for less accessible tumors.Dr. Lemole received his undergraduate degree from Harvard University and his medicaldegree from the University of Pennsylvania. He completed his residency in 2002 inneurological surgery at Barrow Neurological <strong>In</strong>stitute in Phoenix. At Barrow he completedfellowships in complex spinal surgery and cerebrovascular/skull base surgery.He has generated more than 30 peer-reviewed publications and 18 book chapters. He isa member of several medical societies, including the American Association of Neurological<strong>Surgeons</strong>, Congress of Neurological <strong>Surgeons</strong>, and North American Skull Base Society.single-incision laparoscopic surgery (SILS),robotic surgery of the gastrointestinal tract,robotic surgery for gastroparesis, and laparoscopicsolid-organ surgery. <strong>In</strong> addition, heperforms robot-assisted surgery for benignand malignant diseases of the esophagus,robot-assisted living donor nephrectomy androbotic liver resection.Dr. Galvani completed his medicaldegree, internship, and general surgeryresidency in Buenos Aires. He received specialtraining in gastrointestinal surgery at theUniversity of California, San Francisco, andcompleted fellowships in advanced laparoscopicand robotic surgery and in laparoscopicbariatric surgery at the UIC Minimally<strong>In</strong>vasive <strong>Surgery</strong> Center.His research interests include investigatingclinical outcomes of laparoscopic and roboticsurgery for the treatment of esophagealdiseases, living related donor nephrectomies,and bariatric surgery. His studies have dem-onstrated that the use of robotics is highlybeneficial for patients.Dr. Galvani was selected as the Society ofAmerican Gastrointestinal <strong>Surgeons</strong> (SAGES)2006 Traveling Fellowship Award recipient.He has co-authored several book chaptersin surgical textbooks and more than 90publications and abstracts. Dr. Galvani isfluent in both English and Spanish.Stephen Goldstein,MD, has been appointedassociate professor ofsurgery in the Divisionof Otolaryngology. Dr.Goldstein comes to the<strong>UA</strong> from the University ofPennsylvania, where heserved as the director of Facial Plastic <strong>Surgery</strong>in the Department of Otolaryngology.Board-certified as a fellow of the AmericanAcademy of Facial Plastic and Reconstructive11
Alexander G. Chiu, MD, an establishedinternational leader in the treatment ofsinonasal cancers, anterior skull basesurgery, and chronic rhinosinusitis, hasbeen named chief of the Division ofOtolaryngology – Head and Neck<strong>Surgery</strong> and professor of surgery at the<strong>UA</strong> Department of <strong>Surgery</strong>.Prior to his arrival at the <strong>UA</strong>, Dr. Chiuserved as associate professor and directorof the Rhinology and Skull Base <strong>Surgery</strong>Fellowship Program at the University ofPennsylvania. Dr. Chiu specializes in andhas pioneered endoscopic and minimallyinvasive techniques to remove benign andmalignant tumors of the nose, paranasalsinuses, and anterior skull baseDr. Chiu and Dr. Michael Lemole, chiefof the <strong>UA</strong> Division of Neurosurgery, areestablishing the Center for Managementof Sinonasal and Skull Base Tumors, theonly center of its kind in the Southwest.This preeminent multidisciplinary teamof surgeons, radiation oncologists, andmedical oncologists will offer leading-edgeand minimally invasive treatments for benignand malignant tumors of the nose, paranasalsinuses, and skull base.Dr. Chiu’s surgical expertise includes frontalsinus surgery, revision endoscopic sinussurgery, endoscopic repair of cerebrospinalfluid leaks and endoscopic sinonasal tumorsurgery. <strong>In</strong> recognition by his peers andpatients for clinical excellence, Dr. Chiu wasnamed to the Best Doctors of America 2009-2010, Patient’s Choice Award 2008-2010,Best ENT of the Main Line 2009-2010, andBest Doctors of 2010 as listed by SuburbanLife Magazine and Southern Jersey LivingMagazine.Dr. Chiu completed his medical degree atAlbany Medical College and residency trainingin otolaryngology at Georgetown UniversityMedical Center. He completed a fellowship insinonasal and skull base surgery at StanfordUniversity Medical Center.His research interests center on translationalstudies of novel topical medications forthe treatment ofchronic rhinosinusitisrecalcitrant toconventional medicaland surgical therapies.He helped pioneer an animal model forthe study of topical medications and holdsseveral industry and foundation researchgrants on the study of antimicrobialpeptides and sinusitis.Currently, Dr. Chiu is the co-editor-inchiefof the American Journal of Rhinologyand Allergy and serves on the editorial boardof ORL: Journal of Otorhinolaryngology. Hehas been a guest editor for OtolaryngologicClinics of North America on Preventionand Management of Complications inEndoscopic Sinus and Skull Base <strong>Surgery</strong>.He is writing two textbooks on themanagement of sinonasal cancer andsurgical techniques for sinus and skull basesurgery. He has published more than 70peer-reviewed articles and book chapterson sinus and skull base surgery.12<strong>Surgery</strong> and the American Academy ofOtolaryngology – Head and Neck <strong>Surgery</strong>,Dr. Goldstein’s clinical practice focuses onprimary and revision rhinoplasty, cosmeticfacial rejuvenation, facial reconstruction, sinussurgery, and voice disorders.Dr. Goldstein earned his medical degreefrom State University of <strong>New</strong> York (SUNY)Upstate Medical Center in Syracuse andcompleted his residency in otolaryngology atThomas Jefferson University in Philadelphia.He completed fellowship training in facialplastic and reconstructive surgery atBuckhead Facial Plastic <strong>Surgery</strong>, an affiliate ofEmory University in Atlanta.Dr. Goldstein returned to Philadelphiaand joined Robert T. Sataloff, MD, aninternationally prominent laryngologist, asa partner in the world-renowned Center forVoice Disorders. He was the director of facialplastic surgery at the Graduate Hospitalprior to joining the full-time faculty at theUniversity of Pennsylvania in 2005. He waslisted in America’s Top Physicians in 2009and 2010.Dr. Goldstein has published numerousarticles and chapters on nasal and facialplastic surgery. His research interests are theeffects of nasal disorders on the voice andnasal reconstruction.Joel Funk, MD, hasjoined the Division ofUrology as assistantprofessor of surgery.He is a board-eligibleurologist specializingin minimally invasivesurgery and prostateobstruction management. Dr. Funk sees bothadults and children at his practice locatedat the new UPH Clinic in Green Valley andat the UPH <strong>Surgery</strong> Clinic at UPH HospitalOutpatient Clinics.Dr. Funk attended medical school atNorthwestern University Medical School. Hecompleted his general surgery and urologyresidencies at the <strong>UA</strong> Department of <strong>Surgery</strong>.Prior to joining the <strong>UA</strong>, Dr. Funk was aurologic surgeon at Prescott Urology Ltd.Bellal Joseph, MD,has been appointedassistant professor ofsurgery in the Divisionof Trauma, CriticalCare and Emergency<strong>Surgery</strong>.Dr. Joseph is agraduate of the Saba School of Medicine inthe Netherlands-Antilles. He completed hisresidency training at Henry Ford Hospital inDetroit and a trauma critical care fellowshipat the University of Maryland’s renowned R.Adams Cowley Shock Trauma Center.His clinical and research interests areemergency general surgery, penetratingtrauma, international trauma, quality andprocess improvement, and long-term clinicaland functional outcomes after trauma,including how tight blood sugar controlin trauma patients improves perioperativeoutcomes.A member of the American College of<strong>Surgeons</strong> and the Society of Critical CareMedicine, Dr. Joseph has published severalpeer-reviewed publications.
Andrew L. Tang, MD,assistant professor ofsurgery in the Division ofTrauma, Critical Care andEmergency <strong>Surgery</strong>, is a<strong>UA</strong> alumnus, graduatingwith a bachelor’s degree inbiochemistry and a medicaldegree from the College of Medicine.At the University of Southern California, LosAngeles, Dr. Tang completed a foregut researchfellowship and a surgical critical care fellowship.His current research projects include theepidemiology of traumatic spine and spinal cordinjuries, trauma-related complications duringpregnancy, and the long-term outcome oftrauma-related cardiac injuries.Dr. Tang has published more than 20 articles,textbook chapters, and abstracts. He wasawarded the Los Angeles County Sheriff’sDepartment Certificate of Appreciation, theLos Angeles County Department of HealthCertificate of Appreciation, and the St. CalamusGood Samaritan Award.Jodi L. Walters, DPM, hasbeen appointed assistantprofessor of surgery inthe Division of Vascular<strong>Surgery</strong> and the SouthernArizona Limb SalvageAlliance (SALSA). She isa graduate of William M.Scholl College of Podiatric Medicine in Chicago.After completing her podiatric and orthopedicsurgery residency training at the SouthernArizona VA Health Care System (SAVAHCS) inTucson, she served as the program’s assistantdirector and director of podiatry research.Dr. Walters specializes in the diagnosisand treatment of the diabetic foot and itsrelated diseases and complications. She offersaggressive conservative therapy, targetingwounds and ulcers of the lower extremities,complex foot reconstruction, Charcotarthropathy second opinions, and preventivefoot care.Dr. Walters is the recipient of the Researcherof the Year award from the SAVAHCS BiomedicalResearch and Education Foundation of SouthernArizona in 2008. Her research focuses ondiabetic wound care, amputation prevention,and limb salvage.Philanthropy<strong>New</strong> Advisory Board MembersTwo new members have joined the <strong>UA</strong> Department of <strong>Surgery</strong> advisoryboard, announced Richard H. Carmona, MD, the department’s advisoryboard chairman.Businessman Dennis R. Minano is vice chairman of theSonoran <strong>In</strong>stitute and former chairman of the board of <strong>In</strong>tegriGuard.He currently serves on the board of Tucson RegionalEconomic Opportunities, <strong>In</strong>c. (TREO). Mr. Minano retiredfrom General Motors in 2002 after serving as vice presidentand chief environmental officer and board member of theGM Foundation.Benjamin Paz, MD, vice chairman of the DepartmentDennis R. MinanoBenjamin Paz, MDof <strong>Surgery</strong> at the City of Hope Medical Center in Duarte,California, is a renowned leader in surgical oncology and anexpert in minimally invasive and breast cancer surgery. Agraduate of the <strong>UA</strong> General <strong>Surgery</strong> Residency Program,Dr. Paz was named the 2009 <strong>UA</strong> Department of <strong>Surgery</strong>Distinguished Alumnus of the Year.“Dennis Minano and Dr. Benjamin Paz are two stellaradditions to the Department of <strong>Surgery</strong>’s advisory board,”said Dr. Carmona. “Dennis Minano brings outstanding expertisein health care systems and in business developmentand a strong commitment to Tucson. Dr. Paz’s leadership andoutstanding surgical career will make a major contributionto the board.”Dr. Rainer Gruessner, chairman of the <strong>UA</strong> Department of <strong>Surgery</strong>, establishedthe advisory board to help strengthen private support for the department’sclinical, education and research missions. The goal of the board is to generatemore resources for the department so that scientific discoveries can be broughtto the bedside as quickly and safely as possible, including lifesaving techniquesand innovative solutions to surgical problems for the benefit of patientsworldwide.“Dr. Carmona is a superb chair of the advisory board and has been instrumentalin recruiting outstanding leaders,” said Dr. Gruessner.Dr. Carmona is distinguished professor of public health and a professorof surgery at the University of Arizona. He is president and vice chairman ofthe nonprofit Canyon Ranch <strong>In</strong>stitute. He was the 17th Surgeon General of theUnited States.McLane Endowment SupportsMedical Sciences ProgramThanks to a generous donation to the <strong>UA</strong> Department of <strong>Surgery</strong> to supportresearch and education, the University was able to establish the McLaneEndowment for the Department of <strong>Surgery</strong> Medical Sciences Graduate Program.“The entire department is deeply grateful to the McLane family for theirforesight in making this fund possible,” said Rainer Gruessner, MD, departmentchairman.During the 2009-2010 academic year, income from this perpetual fund supportedthe program’s inaugural year with two surgery residents working towardtheir master of science in medicine. The program provides a timely, convenientway to earn a graduate degree – either an MS (master of science) or a PhD(doctor of philosophy) – during the residency training years, so that interestedstudents stay connected with both clinical and research advances in their field,while jump-starting their academic careers.13
Charles F. ZukoskiEndowment forPost-GraduateSurgical EducationFamily and friends of the lateCharles F. Zukoski III, MD, professoremeritus of the Department of<strong>Surgery</strong>, have established an endowmentin his memory to benefit theGeneral <strong>Surgery</strong> ResidencyTraining Program.Last summer, Dr. Zukoskidied at the age of 83in a Salt Lake City hospitalfrom injuries sustainedin a car accident in Utah.He and his wife had beentraveling home to Arizonafrom Washington.A renowned transplantsurgeon-researcher,Dr. Zukoski joined thenewly founded <strong>UA</strong> Department of<strong>Surgery</strong> in 1969 at the two-year-oldCollege of Medicine. He establishedthe renal transplantation center at theVA hospital in Tucson, serving as itschief of surgical services and as thesection chief of renal transplantation.He performed the first kidney transplantin Southern Arizona in 1970.At the University of Arizona, he alsoserved as the chief of general surgery.Dr. Zukoski is best known for hispioneering work in immunosuppressivetherapies. He retired from thedepartment in 1995. He sponsored anaward given every year at the General<strong>Surgery</strong> Residents Graduation forOutstanding Role Model in <strong>Surgery</strong>.<strong>In</strong> MemoriamL. Philip Carter, MD, surgical medical director of UniversityMedical Center Perioperative Services and former chief of theDivision of Neurosurgery in the <strong>UA</strong> Department of <strong>Surgery</strong>, diedJuly 6 after a courageous battle with cancer. He was 71.During most of the 1980s, Dr. Carter served as chief ofCerebrovascular <strong>Surgery</strong> at Barrow Neurological <strong>In</strong>stitute (BNI) inPhoenix. He helped establish a stroke unit and published seminalpapers on intraoperative cerebral blood flow measurements. He co-edited the bookNeurovascular <strong>Surgery</strong>.<strong>In</strong> 1988, he became professor and chief of neurosurgery at the <strong>UA</strong> Collegeof Medicine. The first fully trained neurovascular surgeon in Tucson, Dr. Carterstandardized cortical blood flow monitoring in trauma and vascular neurosurgerypatients in the intensive care unit. He also helped pioneer a joint study on interstitialbrachytherapy for patients with tumors. He was instrumental in creating thepartnership with BNI to train <strong>UA</strong> neurosurgery residents.<strong>In</strong> 1993, Dr. Carter became professor and chairman of the Department of Neurosurgeryand residency program director at the University of Oklahoma School ofMedicine.<strong>In</strong> 1997, he returned to Tucson to join Western Neurosurgery. <strong>In</strong> 2005, he wasappointed surgical medical director of Perioperative Services at UMC and againappointed professor in the Division of Neurosurgery, where he continued to beinvolved in teaching medical students and neurosurgery residents.Throughout his career, Dr. Carter authored more than 100 book chapters andscientific articles and two books. He has given numerous lectures and presentationsat national and international neurosurgical meetings.For his outstanding leadership and unswerving dedication to neurosurgery,Dr. Carter was named this year’s president of the Western Neurosurgical Society, oneof the most senior and prestigious leadership positions in clinical neurosurgery.Robert M. Anderson, MD, an original faculty memberin the Department of <strong>Surgery</strong> and former associate dean of the <strong>UA</strong>College of Medicine, died Jan. 8 in Tucson at the age of 89.A pioneer heart surgeon who performed the first open-heartsurgery in Arizona 50 years ago, Dr. Anderson also was an inventorand the author of more than 60 scientific papers. He served aschief of Cardiothoracic <strong>Surgery</strong> in the Department of <strong>Surgery</strong> from1972 to 1977, and as associate dean of the College of Medicine beginning in 1981.<strong>In</strong> the late 1950s, Dr. Anderson designed one of the earliest and most widelyused heart-lung machines, which made open-heart surgery possible by providingblood and oxygen to the body while the heart was stopped for surgical repair. <strong>In</strong>December 1959, he performed the first open-heart surgery in Arizona at St. Mary’sHospital in Tucson, successfully repairing a hole in the heart of an 8-year-old girl.It was one of thousands of heart operations he performed during his career.Giving OnlineIf you need assistance, please contactKari Schlachtenhaufen at (520) 626-2222 orkaris@surgery.arizona.edu.Each division and program in the <strong>UA</strong> Department of <strong>Surgery</strong> now has online givingcapabilities, either through the University of Arizona Foundation website(www.uafoundation.org) or through the Department of <strong>Surgery</strong> website(www.arizona.surgery.edu), linked to the University of Arizona Foundation.Click on “Give Today” on the Foundation’s website or “Giving” on the <strong>Surgery</strong> home-page andsearch for either “Department of <strong>Surgery</strong>” or the division or program you are interested in (suchas Urology, SALSA, or Trauma).14
NeurosurgeryDivision Establishes<strong>New</strong> Alumni SocietyMichael Lemole, MD, chief of Neurosurgery,recently established theL. Philip Carter, MD, NeurosurgeryAlumni Society for former residentsand fellows, faculty, and friends of theDivision of Neurosurgery. The late Dr. L.Philip Carter and his wife, Colleen, hadgraciously agreed to have the AlumniSociety named in honor of Dr. Carter.Dr. Carter served as surgical medicaldirector of UMC Perioperative Servicesand was the former chief of the Divisionof Neurosurgery in the <strong>UA</strong> Departmentof <strong>Surgery</strong>. Dr. Carter died shortly afterthe inaugural alumni society event heldin his honor on May 21, with more than120 friends and family attending, includingthe Carters’ extended family.The society will support the newNeurosurgery Education Fund to encourageneurosurgery residents’ participationin conferences, research, and training.TOUR SURGERYAwards & RecognitionDavid G. Armstrong, DPM, MD, PhD,professor of surgery and director of theSouthern Arizona Limb Salvage Alliance(SALSA), received the 2010 Roger PecoraroAward from the American DiabetesAssociation. The Pecoraro Award isconsidered the highest honor in the fieldof amputation prevention and woundhealing. The award and lectureship washeld in June at the American DiabetesAssociation’s annual symposium inOrlando. Dr. Armstrong is the youngestaward recipient in its two-decade history.Douglas F. Larson, PhD, professor ofsurgery, Division of Cardiovascular andThoracic <strong>Surgery</strong>, received the VirginiaFurrow Award for Excellence in GraduateStudent Teaching from the <strong>UA</strong> Collegeof Medicine.Joseph Mills Sr., MD, chief of the Divisionof Vascular and Endovascular <strong>Surgery</strong>,received the 2011 Edward James OlmosAward for Advocacy in AmputationPrevention at the DFCon Global DiabeticFoot Conference. Dr. Mills is professor ofsurgery and co-director of the SouthernArizona Limb Salvage Alliance (SALSA).The Olmos Award was presented by theconference co-chairs and by Mr. Olmos,the Academy Award and Tony Awardnomineeat ceremonies at the DFConmeeting in March in Los Angeles.Amy Waer, MD, assistant professorof clinical surgery, has been appointedinterim assistant dean for MedicalStudent Education at the <strong>UA</strong> College ofMedicine. Dr. Waer, a graduate of the<strong>UA</strong> College of Medicine, has been the<strong>Surgery</strong> Clerkship Director, a SocietiesMentor, Block Director for AdvancedTopics in the ArizonaMed curriculum,and <strong>Surgery</strong> Residency Director. Theinterim assistant dean position will bea part-time appointment for Dr. Waer,who will continue in her role as <strong>Surgery</strong>Residency Director.Hugo Villar, MD, professor and chief,Division of Surgical Oncology, has beenappointed to serve as a co-chair of theLatin American Scientific Advisory Boardof the Annals of Surgical Oncology, theofficial journal of the Society of SurgicalOncology.Visit the Department of <strong>Surgery</strong>and learn about the latest advancesin surgery, including the Class10,000 Clean Room, the Center forCellular Transplantation, the PediatricLiver Transplant Program, and theHepatoPancreaticoBiliary (HPB) Center.Tours are regularly available for smallgroups.Contact:Kari Schlachtenhaufen at(520) 626-2222, orkaris@surgery.arizona.edu to geton the mailing list for notices aboutthe next tour.PublicationsArmstrong DG, Wu SC, Crews RT, “PracticalStrategies for Debridement, Off-Loading andHealing the Diabetic Foot Wound,” <strong>In</strong>: RodriguezHE, Pearce WH, and Yao JST, “The IschemicExtremity: <strong>New</strong> Findings and Treatment,”Shelton Connecticut, USA, People’sMedical Publishing, 265-272, 2010.Rogers LC, Bevilacqua N, Armstrong DG,Andros G, “Digital Planimetry Results in MoreAccurate Wound Measurements: A Comparisonto Standard Ruler Measurements,”J Diabetes Sci Technol, 4:799-802, 2010.Bowling FL, Metcalfe SA, Wu S, Boulton AJ,Armstrong DG, “Liquid Silicone to MitigatePlantar Pedal Pressure: A Literature Review,”J Diabetes Sci Technol 4:846-852, 2010.Biswas A, Bharara M, Hurst C, ArmstrongDG, Rilo H, “The Micrograft Concept forWound Healing: Strategies and Applications,”J Diabetes Sci Technol, 4:808-819,2010.Bharara M, Schoess J, Nouvong A, ArmstrongDG, “Wound <strong>In</strong>flammatory <strong>In</strong>dex: A‘Proof of Concept’ Study to Assess WoundHealing Trajectory,” J Diabetes Sci Technol,4:773-779, 2010.Wukich DK, Sung W, Wipf S, ArmstrongDG, “The Consequences of Complacency:Managing the Effects of Unrecognized CharcotFeet,” Diabetic Medicine, 2010, in press.Sumpio BE, Armstrong DG, Lavery LA,Andros G, “The Role of <strong>In</strong>terdisciplinaryTeam Approach in the Management of theDiabetic Foot. A Joint Statement from the15
Society for Vascular <strong>Surgery</strong> and the AmericanPodiatric Medical Association,” J AmerPodiatr Med Assn,100:309-311, 2010.Bharara M, Fitzgerald R, Fisher T, Mills JL,Armstrong DG, “<strong>In</strong>terdisciplinary Team Approachto Targeted Foot Care,” in ArmstrongDG, Lavery LA, editors, “Clinical Care of theDiabetic Foot, 2nd Edition,” Alexandria,American Diabetes Association, 2010.Wu SC, Armstrong DG, “Offloading the DiabeticFoot Wound,” <strong>In</strong>: Armstrong DG, LaveryLA, editors, “Clinical Care of the DiabeticFoot, 2nd Edition,” Alexandria, AmericanDiabetes Association, 2010.Armstrong DG, Lavery LA, editors, “ClinicalCare of the Diabetic Foot, 2nd Edition,” Alexandria,American Diabetes Association, 2010.Rogers LC, Armstrong DG, “Podiatry Care,”in Cronenwett JL and Johnston KW “Rutherford’sVascular <strong>Surgery</strong>,” 7th Edition, Elsevier,1747-1760, 2010.Abbas ZG, Bhansali A, Das BN, ArmstrongDG, Gopalakrishna G, Woo Lee J, HarklessLB, Babu M, Al Derwish M, Sadiq MD, Saraswathi,Pendsey S, Joshi S, Kono S, ViswanathanV, Wadud JR, “Multidisciplinary Consensuson the Diabetic Foot,” Diabetic Foot Societyof <strong>In</strong>dia, 2009.Armstrong DG, Rogers LC, Bevilacqua NC,“Foot Amputations,” <strong>In</strong>: Saxena A, “<strong>In</strong>ternationalAdvances in Foot <strong>Surgery</strong>,” SpringerVerlag, 2010.Bharara M, Schoess J, Nouvong A, ArmstrongDG, “Wound <strong>In</strong>flammatory <strong>In</strong>dex: AProof of Concept Study to Assess WoundHealing Trajectory,” J Diabetes Sci Technol,2010, in press.Scimeca CL, Bharara M, Fisher TK, GiovincoN, Armstrong DG, “Novel Use of Doxycyclinein Continuous-<strong>In</strong>stillation NegativePressure Wound Therapy as ‘Wound Chemotherapy,’” Foot Ankle Spec, 2010 June 8,epub ahead of print.Scimeca C, Bharara M, Fisher TK, ArmstrongDG, “An Update on Pharmacological <strong>In</strong>terventionsfor Diabetic Foot Ulcers,” Foot AnkleSpecialist, 2010, in press.Rogers LC, Andros G, Caporusso J, HarklessLB, Mills J, Armstrong DG, “Toe and Flow:The Team Approach to Amputation Prevention,”J Vasc Surg, 2010, in press.Fisher TK, Scimeca C, Bharara M, Mills JL,Armstrong DG, “A Stepwise Approach toSurgical Management of Diabetic Foot <strong>In</strong>fections,”J Vasc Surg, 2010, in press.Mills JL, Armstrong DG, Andros GA, “CanSynergy Save Sisyphus? The Value of Team inAmputation Prevention,” J Vasc Surg, 2010,in press.Sumpio BE, Armstrong DG, Lavery LA,Andros G, “The Role of <strong>In</strong>terdisciplinaryTeam Approach in the Management of theDiabetic Foot. A Joint Statement from theSociety for Vascular <strong>Surgery</strong> and the AmericanPodiatric Medical Association,” Journalof Vascular <strong>Surgery</strong>, 51:1504-1506, 2010.Fisher TK, Wolcott R, Wolk DM, Bharara M,Armstrong DG, “Diabetic Foot <strong>In</strong>fections: ANeed for <strong>In</strong>novative Assessments,” <strong>In</strong>t J LowerExtremity Wounds, 9:31-36, 2010.Mills JL, Armstrong DG, “Chronic Venous<strong>In</strong>sufficiency,” British Medical Journal - BestPractices Program, March 2010.Crews RC, Bowling F, Boulton AJM, ArmstrongDG, “The Use of SuperoxidizedAqueous Solution vs. Saline as a ReplacementSolution in the Versajet Lavage Systemin Chronic Diabetic Foot Ulcers: A PilotStudy,” J Amer Podiatr Med Assn, 2010,in press.Scimeca CL, Bharara M, Kimbriel HR, ArmstrongDG, “<strong>In</strong>novations in Diabetic FootCare: Using a Wound Healing Timeline forAdvanced Therapies,” Wounds <strong>In</strong>ternational,1:1-4, 2010.Scimeca CL, Bharara M, Armstrong DG,“Diabetic Foot Ulcers,” Expert Opinion onEmerging Drugs, 2010, in press.Scimeca CL, Bharara M, Fisher TK, KimbrielHR, Mills JL, Armstrong DG, “Novel Useof <strong>In</strong>sulin in Continuous-<strong>In</strong>stillation NegativePressure Wound Therapy as ‘WoundChemotherapy,’ ” Diab Technology Therapeutics,2010, in press.Scimeca CL, Fisher TK, Armstrong DG,“Chronic Painful Lower Extremity Wounds:Postoperative Pain Management Through theUse of Continuous <strong>In</strong>fusion Regional AnesthesiaSupplied by a Portable Pump Device,”<strong>In</strong>t Wound J, 7:195-198, 2010.Giovinco N, Fisher TK, Mills JL, ArmstrongDG, “Wound Chemotherapy by Useof Negative Pressure Wound Therapy and<strong>In</strong>fusion,” ePlasty, 10:66-73, 2010.Fisher TK, Armstrong DG, “Partial Calcanectomyin High Risk Patients with Diabetes:Use and Utility of a ‘Hurricane’ <strong>In</strong>cisionalApproach,” ePlasty, 1:10:e17, 2010.Scimeca CL, Bharara M, Fisher TK, KimbrielHR, Armstrong DG, “Novel Use of Platelet-Rich Plasma to Augment Curative DiabeticFoot <strong>Surgery</strong>,” J Diabetes Research and Technology,2010, in press.Leon LR, Pacanowski J, Ranellone E, ArmstrongDG, “Diabetic Limb Salvage: TooMuch of a Good Thing?,” Vasc EndovascSurg, 2010, epub ahead of print.Tussing-Humphreys LM, Nemeth E, FantuzziG, Freels S, Holterman AL, Galvani C,Ayloo S, Vitello, Braunschweig CA, “DecreasedSerum Hepcidin, <strong>In</strong>flammation, andImproved Functional Iron Status Six-monthsPost-restrictive Bariatric <strong>Surgery</strong>,” Obesity(Silver Spring), 2010 January 14, epubahead of print.Galvani C, Gorodner MV, Gallo A, Bueno R,Moser F, Horgan S, “Laparoscopic AdjustableGastric Banding Does Not Adversely AffectEsophageal Dysmotility,” submitted toObesity <strong>Surgery</strong>.Galvani C, Gorodner M, Espat J, “<strong>Robotic</strong>-Assisted Resection of Adrenal Aldosteronoma,”Ann Surg Oncol, 2010 August 24, epubahead of print.Galvani C, Choh M, Gorodner M, “Single<strong>In</strong>cision Sleeve Gastrectomy Using a NovelTechnique for Liver Retraction,” JSLS, 14:228-233, 2010.Galvani C, Gallo A, Gorodner MV, “Single-<strong>In</strong>cision Laparoscopic Adjustable GastricBand (SI-LAGB): Evaluation of the <strong>In</strong>itialExperience,” <strong>Surgery</strong> for Obesity and RelatedDiseases, in press.Sroka I, Anderson T, McDaniel K, Nagle R,Gretzer MB, and Cress A, “The Q1 LamininBinding <strong>In</strong>tegrin alpha-6-beta1 in ProstateCancer Perineural <strong>In</strong>vasion,” J Cell Physiol,2010.Kaplan B, Jie T, Diana R, Renz J, WhineryA, Stubbs N, Bracamonte E, Spier C, SchubartP, Rilo H, Gruessner R, “Histopathol-16
ogy and Immunophenotype of the SpleenDuring Acute Antibody-Mediated Rejection,”Am J Transplant, 2010 May;10(5):1316-20,epub 2010 March 19.Gruessner AC, Sutherland DE, GruessnerRW, “Pancreas Transplantation in the UnitedStates: A Review,” Curr Opin Organ Transplant,2010 February;15(1):93-101.Gruessner RW, “Pancreas Transplantation,”Curr Opin Organ Transplant, 2010 February;15(1):92.Guerrero MA, Suh I, Vriens MR, Shen WT,Gosnell J, Kebebew E, Duh QY, Clark OH,“Age and Tumor Size Predict Lymph Node<strong>In</strong>volvement in Hürthle Cell Carcinoma,”J Cancer, 2010;1:23-26.Guerrero MA, Clark OH, “A ComprehensiveReview of <strong>In</strong>traoperative Parathyroid HormoneMonitoring,” World J Endo Surg,2010;2(1):21-27.Joseph B, Wynne J, Dudrick S, Latifi R,“Nutrition in Trauma and Critically Ill Patients,”European Journal of Trauma andEmergency <strong>Surgery</strong>, 2010, 36(1):25-30.Knatterud ME, “Mayo in May: From MaudMellish to Mod Mannequins,” AMWA [AmericanMedical Writers Association] North CentralChapter <strong>New</strong>sletter [for AMWA membersin Minnesota, North Dakota, South Dakota,and northern Wisconsin], June 2010, pp 2-5.Knatterud ME, Two short book reviews in“Summer Reading Roundup,” Wheat Ridge,CO, Science Editor [Council of Science Editorsjournal], May-June 2010, Vol. 33, No. 3,pp. 90-91, 92.Vol. 33, No. 3, p. 103.Knatterud ME, ed.,“Peer-Renewed” column,Wheat Ridge,CO: Science Editor[Council of ScienceEditors journal],March-April 2010,Vol. 33, No. 2,p. 67.Knatterud ME, ed.,“Peer-Renewed” column,Wheat Ridge,CO: Science Editor[Council of ScienceEditors journal],May-June 2010,Knatterud ME, ed., “Peer-Renewed” column.Wheat Ridge, CO: Science Editor[Council of Science Editors journal], July-August 2010, Vol. 33, No. 4, p. 142.Liu L, Herrinton, LJ, Hornbrook MC, WendelCS, Grant M, Krouse RS, “Early andLate Complications Among Long-TermColorectal Cancer Survivors with Ostomy orAnastomosis,” Dis Colon Rectum 2010 February;53(2):200-12.NIHMS 216735 PMCJournal, in press.Ramirez M, McMullen C, Grant M, AltschulerA, Hornbrook M, Krouse R, “FiguringOut Sex in a Reconfigured Body: Experiencesof Female Colorectal Cancer Survivorswith Ostomies,” Women & Health,2009;49(8):608-624. NIHMS 171961 PMCJournal, in press.Gemmill R, Sun V, Ferrell B, Krouse RS,Grant M, “Going with the Flow: Quality ofLife Outcomes of Cancer Survivors with UrinaryDiversion,” J Wound Ostomy ContinenceNurs, 2010 January/February;37(1):65-72.Jensen V, Prasad AR, Smith A, Raju M, WendelCS, Schmelz M, Leyva W, Warneke J,Krouse RS, “Prognostic Criteria for SquamousCell Cancer of the Skin,” J Surg Res,2010 March;159(1):509-516.Kulvatunyou N, Bender JS, Lees JS, BrightB, Albrecht RM, “Decreased Use of CervicalSpine Clearance in Blunt Trauma: The Implicationof the <strong>In</strong>jury Mechanism and Distracting<strong>In</strong>jury,” Accid Anal, 2010; 42(4): 1151-1155.Kulvatunyou N, “Clinical Examination inComplement with Computed TomographyScan: An Effective Method for Identificationof Cervical Spine <strong>In</strong>jury,” Letter to the editor,J Trauma, 2010; 68(5):1269.Kulvatunyou N and Roberts PR, “GastrointestinalHemorrhage,” <strong>In</strong>: Farmer JC, WallMH, Roberts PR, Pocket ICU Management(2nd Edition). <strong>New</strong> York: PocketMedicine.com, 2010.Joseph B, Wynne JL, Dudrick S, Latifi R,“Nutrition in Trauma and Critically Ill Patients,”European Journal of Trauma andEmergency <strong>Surgery</strong>, Focus on Laprascopaland Abdominal Emergencies. January 2010.Klein RL, Lang JE, Neratinib, “An IrreversiblePan-ErbB <strong>In</strong>hibitor,”Drugs of the Future,accepted 2010, in press.Klein RL, Brown AR, Gomez-Castro CM,Chambers SK, Cragun JM, Grasso-LeBeau L,Lang JE, “Ovarian Cancer Metastatic to theBreast Presenting as <strong>In</strong>flammatory BreastCancer: A Case Report and Literature Review,”Journal of Cancer, accepted 2010,in press.Liang-Chih L, Lang J (co-first authors), LuY, Hwang S, Ewing C, Roe D, Esserman L,Morita E, Treseler P, Leong S, “<strong>In</strong>traoperativeFrozen Section Analysis of Sentinel LymphNodes in Breast Cancer Patients: A Metaanalysisand Single-<strong>In</strong>stitution Experience,”Cancer, accepted 2010, in press.Banerjee PP, Luciano C, Bellotte NJB, RoitbergBZ, Lemole GM Jr, “Learning Retentionof Thoracic Pedicle Screw PlacementUsing a High-Resolution Augmented RealitySimulator with Haptic Feedback,” J Neurosurg(Spine), 2010 (submitted).Latifi R, Poropatich R (ed.), “Telemedicinefor Trauma, Disaster and Emergency Management,”Norwood, MA: Artech HousePublishers, 2010.Mills, JL Sr, Armstrong DG, Andros G,editors of supplement “Rescuing Sisyphus:The Team Approach to Amputation Prevention,”J Vasc Surg 52(3S):1-2S, September2010.Rogers LC, Andros G, Caporusso J, HarklessLB, Mills JL Sr, Armstrong DG, “Toe andFlow: Essential Components and Structureof the Amputation Prevention Team,” J VascSurg 52(3S):23-27S, September 2010.17
Fisher TK, Scimeca CL, Bharara M, Mills JLSr, Armstrong DG, “A Step-Wise Approachfor Surgical Treatment of Diabetic Foot <strong>In</strong>fections,”J Vasc Surg 52(3S): 72-75S, September2010.Ihnat DM, Mills JL Sr, “Current Assessmentof Endovascular Therapy for <strong>In</strong>frainguinalArterial Occlusive Disease in Patientswith Diabetes,” J Vasc Surg 52(3S):92-95S,September 2010.Scimeca CL, Bharara M, Fisher TK, KimbrielH, Mills JL, Armstrong DG, “Novel Use of<strong>In</strong>sulin in Continuous-<strong>In</strong>stillation NegativePressure Wound Therapy as ‘Wound Chemotherapy,’” Journal of Diabetes Science andTechnology, 2010;4(4):820-4.Leon LR; Mills JL, “Diagnosis and Managementof Aortic Mycotic Aneurysms,” Vascularand Endovascular <strong>Surgery</strong>, 2010;44(1):5-13.Giovinco NA, Bui TD, Fisher T, Mills JL,Armstrong DG, “Wound Chemotherapy bythe Use of Negative Pressure Wound Therapyand <strong>In</strong>fusion,” Eplasty 2010;10:66-73.Mills JL Sr., Patel S, “Duplex Surveillance in<strong>In</strong>frainguinal Bypass Grafts: Identificationand Treatment of Graft-Threatening Lesions,”Chapter 4, pp. 43-59, <strong>In</strong>: The Ischemic Extremity:<strong>New</strong> Findings and Treatment, RodriguezHE, Pearce WH and Yao JST (eds),PMPH-USA, Ltd., Shelton, CT, 2010.Mills JL, “<strong>In</strong>frainguinal Bypass,” <strong>In</strong>: Rutherford’sTextbook of Vascular <strong>Surgery</strong>, 7th Edition,Chapter 109, pp. 1682-1701, Saunders,Philadelphia, 2010.Mills JL, “Evaluation and Management ofPeripheral Arterial Disease,” <strong>In</strong>: Clinical Careof the Diabetic Foot, 2nd Edition, Chapter11, pp. 107-116, American Diabetes Association,<strong>In</strong>c., Alexandria, 2010.Bharara M, Fitzgerald R, Fisher, Mills JL,Armstrong DG, “<strong>In</strong>terdisciplinary TeamApproach to Targeted Diabetic Foot Care,”<strong>In</strong>: Clinical Care of the Diabetic Foot, 2ndEdition, Chapter 12, pp. 117-124, AmericanDiabetes Association, <strong>In</strong>c., Alexandria, 2010.Ihnat DM, Mills JL, “Endovascular Managementof <strong>In</strong>frapopliteal Occlusive Disease,”<strong>In</strong>: Endovascular <strong>Surgery</strong>, 4th Edition, eds:Moore WS, Ahn SS, Elsevier, Philadelphia,2010.Rose J, Lucas L, Mills JL, “EndovascularTreatment of a Ruptured Axillary Aneurysmand Large <strong>In</strong>ternal Mammary Artery Aneurysmin a Patient with Marfan Syndrome,”J Vasc Surg, in press.Eidt JF, Mills JL, Rhodes RS, Biester T,Gahtan V, Jordan WD, et al, “Comparison ofSurgical Operative Experience of Traineesand Practicing Vascular <strong>Surgeons</strong>: A Reportfrom the Vascular <strong>Surgery</strong> Board of theAmerican Board of <strong>Surgery</strong>,” J Vasc Surg,in press.Stuke L, Jennings A, Gunst M, Tyner T, FrieseR, O’Keeffe T, Frankel H, “UniversalConsent Practice in Academic <strong>In</strong>tensive CareUnits (ICUs),” J <strong>In</strong>tensive CareMed, 2010 January-February;25(1):46-52.Huebinger RM, Gomez R, Mc-Gee D, Chang L, Bender JE,O’Keeffe T, Burris AM, FrieseSM, Purdue GF, Hunt JL, ArnoldoBD, Horton JW, BarberRC, “Association of MitochondrialAllele 4216C with <strong>In</strong>creasedRisk for Sepsis-RelatedOrgan Dysfunction and Shockafter Burn <strong>In</strong>jury,” Shock, 2010January;33(1):19-23.Warner MA, O’Keeffe T,Bhavsar P, Shringer R, Moore C,Harper C, Madden CJ, Sarode R,Gentilello LM, Diaz-Arrastia R, “Transfusionsand Long-Term Functional Outcomes inTraumatic Brain <strong>In</strong>jury,” J Neurosurg, 2010January 29.Hui DS, Eastman AL, Lang JL, Frankel HL,O’Keeffe T, “A Survey of Critical Care TrainingAmong Surgical Residents: Will They beReady?, J Surg Res, 2010 May 11, epubahead of print.Higa G, Friese R, O’Keeffe T, Wynne J,Bowlby P, Ziemba M, Latifi R, KulvatunyouN, Rhee P, “Damage Control Laparotomy:A Vital Tool Once Overused,” JTrauma, 2010 July;69(1):53-59.Schnüriger B, <strong>In</strong>aba K, Barmparas G, RheeP, Putty B, Branco BC, Talving P, DemetriadesD, “A <strong>New</strong> Survivable Damage ControlModel including Hypothermia, Hemodilution,and Liver <strong>In</strong>jury,” J Surg Res, 2010April 68(4):881-885.Ling GS, Rhee P, Ecklund JM, “Surgical <strong>In</strong>novationsArising from the Iraq and AfghanistanWars,” Annu Rev Med, 2010;61:457-68.<strong>In</strong>aba K, Recinos G, Teixeira PG, BarmparasG, Talving P, Salim A, Brown C, Rhee P, DemetriadesD, “Complications and Death atthe Start of the <strong>New</strong> Academic Year: Is Therea July Phenomenon?,” J Trauma, 2010 January;68(1):19-22.DuBose JJ, Kobayashi L, Lozornio A, TeixeiraPG, <strong>In</strong>aba K, Lam L, Talving P, Branco B,Demetriades D, Rhee P, “Clinical ExperienceUsing 5% Hypertonic Saline as a Safe AlternativeFluid for Use in Trauma,” Journal ofTrauma, May 68(5):1172-1177, 2010.<strong>In</strong>aba K, Branco BC, Rhee P, BlackbourneLH, Holcomb JB, Teixeira PG, Shulman I,Nelson J, Demetriades D, “The Impact ofABO-Identical Versus ABO-Compatible,Non-Identical Plasma Transfusion in TraumaPatients,” Journal of the American College of<strong>Surgeons</strong>, June 2010(6):967-965, 2010.Wen F, Shen A, Shanas R, Bhattacharyya A,Lian F, Hostetter G, and Shi J, “Higher Expressionof the Heterogeneous Nuclear RibonucleoproteinK in Melanoma,” Ann SurgOncol, May 25, 2010, advance onlinepublication.Tsikitis VL, Holubar SD, Dozois EJ, CimaRR, Pemberton JH, Larson DW, “Advantagesof Fast-Track Recovery after LaparoscopicRight Hemicolectomy for Colon Cancer,”Surg Endosc, 2010 August;24(8):1911-6,epub 2010 Jan 28.18
Tsikitis VL, Corning C, Henderson J, Rose J,“Chloroma/Granulocytic Sarcoma: Abdominal& Pelvic Presentation of Acute MyelogenousLeukemia,” J Cancer, 2010; 1:98-100.Tsikitis VL, Khreiss M, “Review Article onCurrent Treatment Options of Colon Cancer:Colon Cancer,” Contemporary Oncolog,in press.Tsikitis V, Popek S, “Preoperative vs. PostoperativePelvic Radiotherapy for Locally AdvancedRectal Cancer,” World Journal of Gastroenterology,in press.Villar H, Update to Chapter Shackelford’s<strong>Surgery</strong> of the Alimentary Tract, 7th Edition,Volume 4 for October 2010.Villar H, Fong Y, Early K, Deane S, JohnsonF, Nogueras J, Finley R, Hoballah J, MichelassiF, “American College of <strong>Surgeons</strong> <strong>In</strong>ternationalScholarship Programs: 40-Year Historyof Support for <strong>In</strong>ternational Surgical Education,”ISSN: 1072-7515/10; jamcollsurg,2010.04.19.Bernas MJ, Cardoso FL, Daley SK, WeinandME, Campos AR, Ferreira AJ, Hoying JB,Witte MH, Brites D, Persidsky Y, RamirezSH, Brito MA, “Establishment of Primary Culturesof Human Brain Microvascular EndothelialCells to Provide an <strong>In</strong> Vitro CellularModel of the Blood-Brain Barrier,” NatureProtocols, 5:1265-1272, 2010.Bernas MJ, Askew RL, Armer JM, CormierJN, “Lymphedema: How Do We Diagnose andReduce the Risk of This Dreaded Complicationof Breast Cancer Treatment?,” CurrBreast Cancer Rep, 2:53-58, 2010.Bernas MJ, Daley SK, Bracamonte E, McKennaM, Carati C, Witte MH, “Use of Low-Level Laser in Treatment of ExperimentalLymphedema,” Proceedings of the 22nd <strong>In</strong>ternationalCongress of Lymphology, Sydney,Australia, September 2009, Lymphology43(Suppl), in press.Bernas, MJ, Daley SK, Summers P, Witte CL,Witte MH, “MLD Monotherapy for Treatmentof Lymphedema,” Proceedings of the 22nd<strong>In</strong>ternational Congress of Lymphology, Sydney,Australia, September 2009, Lymphology43(Suppl), in press.Daley SK, Bernas MJ, Stea BD, BracamonteE, McKenna M, Stejskal A, Hirleman ED,Witte MH, “Radioprotection from Radiation-<strong>In</strong>duced Lymphedema without TumorProtection,”Lymphology43:48-58, 2010.Cormier J, FeldmanJ, Askew R,Beck M, BernasM, Francis K, FuM, Lasinski B,Rodrick J, StewartB, Stewart P, StoutN, Thrift K, TuppoC, Weiss B,Moffatt C, ArmerJ, “ALFP to Updatethe BestPractice Document,”J ofLymphoedema, 5:68-71, 2010.Zhang H, Tse J, Hu X, Witte M, Bernas M,Kang J, Tilahun F, Hong YK, Qiu M, Chen L,“Novel Discovery of LYVE-1 Expression inthe Hyaloid Vascular System,” <strong>In</strong>vest OphthalmolVis Sci, 2010, in press.Ganta VC, Cromer V, Mills GL, Traylor J,Jennings M, Daley S, Clark B, Mathis JM,Bernas M, Jordan P, Witte M, Alexander JS,“Angiopoeitin-2 in Experimental Colitis,”<strong>In</strong>flamm Bowel Dis, 16:1029-1039, 2010.Cherington C, Daley SK, Kurtzman D,Carrasco A, Bernas MJ, Witte MH, “LymphaticDysfunction and Tumor Growth andSpread in a Murine Model: A Pilot Study,”Proceedings of the 22nd <strong>In</strong>ternational Congressof Lymphology, Sydney, Australia, September2009, Lymphology 43(Suppl),in press.Witte MH, Bernas M, “Lymphatic Pathophysiology,”<strong>In</strong>: Rutherford’s Vascular <strong>Surgery</strong>,7th Edition, Chapter 12, pp. 177-201, SaundersCompany, Philadelphia, 2010.Witte MH, M Dellinger, Bernas MJ, JonesKA, Witte CL, “Molecular Lymphology andGenetics of Lymphedema-Angio dysplasiaSyndromes,” <strong>In</strong>: Textbook of Lymphology, 3rdEdition, Chapter 16, Urban & Fischer Verlag,München, Germany, 2010, in press.Campisi, C, Boccardo F, Witte M, BernasM, “Lymphatic <strong>Surgery</strong> and <strong>Surgery</strong> of LymphaticDisorders,” <strong>In</strong>: Venous and LymphaticDisorders, Chapter 41, McGraw-Hill, <strong>New</strong>York, 2010, in press.Dellinger M, Bernas M, Witte M, “LymphaticBiology and Pathobiology,” <strong>In</strong>: Venousand Lymphatic Disorders, Chapter 3,McGraw- Hill, in press.Bernas M, “Review of National and <strong>In</strong>ternationalConsensus on Chronic Lymphedema,”Chapter 20, <strong>In</strong>: LYMPHEDEMA: A ConciseCompendium of Theory and Practice, Springer,in press.Alexander JS, Ganta VC, Jordon PA, WitteMH, “Gastrointestinal Lymphatics in Healthand Disease,” Pathophysiology, 17:315-335,2010.Witte, M, “Standing on the Shoulders ofGiants: The Past, Present, and Future of the<strong>In</strong>ternational Society of Lymphology,” Proceedingsof the 22nd <strong>In</strong>ternational Congressof Lymphology, Sydney, Australia, September2009, Lymphology 43(Suppl), in press andCD-ROM.Witte M, “Translational/Personalized Medicine,Pharmaco/Surgico/Radiogenomics,Lymphatic Spread of Cancer, and MedicalIgnoromes,” J Surg Oncol, in press.Witte M, McDonald D, Dellinger M, BoccardoF, Nathanson D, Sleeman J, GershenwaldJ, “Lymphangiogenesis/Hemangiogenesis:Potential Targets for Therapy,” J Surg Oncol,in press.Leong SPL, Witte M, “Future Perspectives,Unanswered Questions and Research Agenda,”J Surg Oncol, in press.WilliamsW, O’Chart M, Bernas M, WitteCL, Witte M, “Radionuclide Lymphoscintigraphy,”Chapter 7.2 <strong>In</strong>: LYMPHEDEMA: AConcise Compendium of Theory and Practice,Springer, in press.19
20Jones KA, Witte M, “Hereditary and FamilialLymphedema Syndromes,” Chapter 4, <strong>In</strong>:LYMPHEDEMA: A Concise Compendium ofTheory and Practice, Springer, in press.PresentationsArmstrong DG, Podiatry <strong>New</strong> Zealand NationalSymposium, Wellington, <strong>New</strong> Zealand,September 2010:• Keynote lecture, “An Update on WoundHealing”• “Debridement and Offloading”• “Risk Assessment: Toward a TherapeuticLingua Franca”Armstrong DG, Wound Healing Masters’Advisory Board, “The Diabetic Foot: TheState of Play in 2010,” Toronto, Canada (viavideo), August 2010.Armstrong DG, South Africa Diabetic FootStudy Group, “The Diabetic Foot: Building aTeam and Making a Difference,” Cape Town,South Africa, August 2010.Armstrong DG, Advanced Foot and AnkleReconstruction Course, Keynote Presentation,“Models for Amputation Prevention”,La Jolla, July 2010.Armstrong DG, American Podiatric MedicalAssociation National Symposium, “AlphaLipoic Acid and Acetyl-L-Carnitine: PotentAllies in the Fight Against Neuropathy?” and“A Systematic Approach to Diabetic Neuropathy,”Seattle, July 2010.Armstrong DG, WOCN/Diabetic Foot SocietySymposium Keynote Lecture, “The DiabeticFoot: The Next 25 Years,” and “TheDiabetic Foot: Development of Teams,”Tokyo, Japan, July 2010.Armstrong DG, 70th American DiabetesAssociation Scientific Sessions, PecoraroAward Lecture, “Healing the Diabetic Foot:Worth a Life’s Work,” Orlando, June 2010.Armstrong DG, Tissue Repair Masters Symposium,“Theragnostics and Diagnostics:You Can’t Manage What You Can’t Measure,”London, June 2010.Armstrong DG, Tornier Foot and AnkleAdvanced Course, “Tissue Repair and ReconstructionTechniques,” <strong>New</strong> York City,May 2010.Montague MD, Daley SK, Bernas MJ,Cherington C, Witte MH, “The Role ofLymphatics in Metastasis of Melanoma,”Abstract #402, J <strong>In</strong>v Med, 58 (1): 218,2010.Armstrong DG, American Diabetes Association“Step Out” Event to Fight Diabetes: “TheDiabetes Tsunami,” Tucson, May 2010.Armstrong DG, 20th FIP <strong>In</strong>ternationalSymposium, Keynote Presentation: “Podiatryand Diabetes: A Natural Marriage,” Amsterdam,May 2010.Armstrong DG, 13th Malvern <strong>In</strong>ternationalDiabetic Foot Symposium, “Success in AmputationPrevention in the USA” “The ABC’sof Negative Pressure Wound Therapy, and“Debate on Wound Therapies (with Prof.William Jeffcoate),” Great Malvern, UK, May2010.Armstrong DG, EviVenice Cardiovascular/Diabetes Symposium, “Diabetic Foot <strong>Surgery</strong>,”Venice (via video), April 2010.Armstrong DG, <strong>New</strong> York College of PodiatricMedicine: The Academic Physician(Meet the Professor), <strong>New</strong> York City (via video),April 2010.Armstrong DG, Symposium for the Advancementof Wound Care Pre-ConferenceWorkshop: Offloading: Advanced Workshop,“The Team Approach to Amputation Prevention,”Orlando, April 2010.Armstrong DG, Sanofi-Aventis Basic ScienceAdvisory Board Meeting, “The DiabeticFoot,” Orlando, April 2010.Armstrong DG, Diabetes Technologies SocietyAnnual Meeting, “The Diabetic Foot: PersistenceYields <strong>In</strong>novation,” San Antonio,April 2010.Armstrong DG, Diabetic Foot Global Conference2010 (DFCon10), “The Global Soleof the Matter” (moderator), “Non-PoweredNegative Pressure Wound Therapy for theDeveloped and Developing World” (moderator),“Frequency Modulated Electrical Stimulationin the Diabetic Foot” (moderator), “DiabeticFoot <strong>In</strong>fection” (moderator), and “TakingUs Home: Essential Tips for MondayMorning” (moderator), Los Angeles, March2010.Armstrong DG, <strong>In</strong>ternational Diabetic Foot<strong>Surgery</strong> Symposium, “Marrying the Teamwith Technology to Heal Wounds and PreventAmputations in People with Diabetes” “Howto Build a Limb Salvage Team,” and “Risk Factorsfor Diabetic Foot Ulcers,” Jeddah, Kingdomof Saudi Arabia, March 2010.Armstrong DG, Bliss Army Medical CenterGrand Rounds, Fort Huachuca, “The DiabeticFoot,” Ft. Huachuca, February 2010.Armstrong DG, Georgia Podiatric MedicalAssociation Annual Scientific Symposium,“Policy, Prevention, and Procedures: What’s<strong>New</strong> in Healing the Diabetic Foot,” Atlanta,February 2010.Armstrong DG, Texas Podiatric Medical AssociationAnnual Meeting, “Diabetic Foot:The Global State of Play in 2010,” Chairmanand Video Conference Moderator, “MRSA,”Dallas, January 2010.Armstrong DG, Midwestern UniversitySchool of Podiatric Medicine Symposium,“Wound Healing,” Glendale, January 2010.Armstrong DG, University of South Carolina,Department of <strong>Surgery</strong> Grand Rounds,“The Diabetic Foot,” Greenville, South Carolina,January 2010.Bernas B, invited speaker: “Low Level LaserTreatment on an Animal Model of Lymphedema,”Australian Medical Laser AssociationMeeting, Melbourne, May 2010.Bernas B, invited speaker: “<strong>In</strong>terpretation ofLymphatic Imaging,” 8th Australasian LymphologyAssociation Conference, Melbourne,May 2010.Bernas B, invited speaker: “A Whirlwindthrough the Lymphatic System with Imagingand Genetics,” Tauranga Hospital, Tauranga,<strong>New</strong> Zealand, June 2010.Dresner M, “What’s in a Name,” ethicslecture, Tripler Army Medical Center,Honolulu.Galvani C, Gallo A, Gorodner MV, DonahuePE, Horgan S, “Does Previous EndoscopicTreatment Affect the Outcome of <strong>Robotic</strong>-Assisted Heller Myotomy?” MIRA meeting,San Diego, January 2010.Galvani C, “Applications of <strong>Robotic</strong>s in General<strong>Surgery</strong>,” Army Hospital at Fort Huachuca,AZ, March 2010.
Galvani C, “<strong>Robotic</strong> <strong>Surgery</strong> in Tucson Today—andTomorrow,” Pima County MedicalSociety, Tucson, April 2010.Galvani C, “Cirugia Bariátrica con <strong>In</strong>cisiónúnica: Futuro o Fantasia?” and “Hernia Hiatalen Cirugía Bariátrica: Como Reparar? Cono Sin Malla?” IV CONGRESO INTERNA-CIONAL DE ACT<strong>UA</strong>LIZACION ENCIRUGÍA BARIATRICA Y METABOLICA,Enfoque Quirúrgico y Multidisciplinario,Mendoza, Argentina, April 2010.Galvani C, 27° CONGRESO INTERNACIO-NAL DE CIRUGÍA DE CÓRDOBA DEL BI-CENTARIO, Disertante en Jornada de Residentes,Asociación de Residentes de Cirugíade Córdoba, Simposio Cirugía Miniimvasiva,Córdoba, Argentina, July 2010:• “<strong>In</strong>cisión única Generalidades”• “Colecistectomía por <strong>In</strong>cisión única”• “Banda Gastric Adjustable por <strong>In</strong>cisiónúnica”• “Gastrectomía en manga por incisiónúnica”Galvani C, <strong>In</strong>ternational Federation for the<strong>Surgery</strong> of Obesity and Metabolic Disorders(IFSO), Long Beach, September 2010:• “Single-<strong>In</strong>cision Laparoscopic AdjustableGastric Band Placement (SI-LAGB) andHiatal Hernia Repair”• “Single-Port Sleeve Gastrectomy (SG) andHiatal Hernia Repair”• “Trans-Umbilical Gastric BandPlacement: Single-Port vs. Multiple-Port”Guerrero MA, Schreinemakers JA, Suh I,Vriens MR, Shen WT, Gosnell J, Kebebew E,Duh Q, Clark OH, “Tumor Size PredictsLymph Node <strong>In</strong>volvement in Hürthle CellCarcinoma,” Fifth Annual Academic SurgicalCongress, San Antonio, February 2010.Guerrero MA, ShenWT, Gosnell J, et al,“The Number ofNeedle Passes Affectsthe Accuracy of ParathyroidHormoneAssay with <strong>In</strong>traoperativeParathyroidAspiration,” SouthwesternSurgicalCongress 62nd AnnualMeeting, March2010.Gruessner, RWG,“<strong>In</strong>novation, Expansion,and Progress in<strong>Surgery</strong> and Transplantation at the Universityof Arizona,” 260 Club of Green Valley,Green Valley, AZ, February 2010.Gruessner RWG, “Rebuilding the Departmentof <strong>Surgery</strong> and Transplantation at theUniversity of Arizona,” Foothills Forum,Tucson, February 2010.Gruessner RWG, “Pancreas Transplant:Techniques and Management,” The <strong>First</strong>Egyptian Organ Transplant Congress, Cairo,March 2010.Gruessner RWG, “Recent Advances inTransplantation and Complex Abdominal<strong>Surgery</strong>,” Carondelet St. Joseph’s HospitalSymposium, Tucson, April 2010.Gruessner RWG, “Transplant <strong>Surgery</strong>,”Carondelet St. Mary’s Hospital Symposium,Tucson, June 2010.Gruessner RWG, “Living Donor Pancreasand <strong>In</strong>testinal Transplant,” 5th <strong>In</strong>ternationalConference on Living Donor AbdominalOrgan Transplantation: State of the Art,Firenze, Italy, June 2010.Joseph B, Madigan B, Lucas L, O’Keeffe T,Friese R, Kulvatunyou N, Wynne J, LatifiR, Mills J, Rhee P, “Superior MesentericVein Avulsion From Blunt Assault: A Rareand Potentially Lethal <strong>In</strong>jury,” accepted fororal presentation, 40th Annual Meeting ofthe Western Trauma Association, March2010.Joseph B, Hadeed G, Wynne J, KulvatunyouN, O’Keeffe T, Friese R, Latifi R,Rhee P, “Pictures Are Worth a ThousandWords,” accepted for oral presentation,ATACCC Conference, August 2010.Joseph B, Amini A, Houdek M, Friese R,O’Keeffe T, Wynne J, Kulvatunyou N,Latifi R, Rhee P,“Factor IX Complex forCorrection of Traumatic Coagulopathy,” acceptedfor oral presentation, 69th AnnualAmerican Association for the <strong>Surgery</strong> ofTrauma, September 2010.Popek S, Grant M, Gemmill R, Wendel CS,Mohler MJ, Rawl SM, Baldwin CM, Ko CY,Schmidt CM, Krouse RS, “OvercomingChallenges: Life with a Colostomy,” acceptedfor oral presentation, Association of VA <strong>Surgeons</strong>34th Annual Meeting, <strong>In</strong>dianapolis,May 2010.Krouse RS, accepted for oral presentation,the <strong>In</strong>terdisciplinary ColorectalCancer Survivorship Research ProgramSymposium, American PsychosocialOncology Society 7th Annual Conference,<strong>New</strong> Orleans, February 2010:• Grant M, Hornbrook MC, Wendel CS,Coons SJ, Herrinton LJ, Mohler MJ, BaldwinCM, McMullen CK, Altschuler A,Rawl SM, Krouse RS, “Advantages of<strong>In</strong>terdisciplinary Research”• Hornbrook MC, Wendel CS, Coons SJ,Grant M, Herrinton LJ, Mohler J, BaldwinCM, McMullen CK, Green SB, AltschulerA, Rawl SM, Krouse RS, “Predictors ofSF-6D Scores Among Long-term ColorectalCancer Survivors”• Ramirez M, Altschuler A, McMullen C,Hornbrook M, Herrinton L, Grant M,Krouse R, “Sexuality and Partner SupportAmong Female Colorectal CancerSurvivors with Ostomies”• McMullen C, Altschuler A, Grant M,Hornbrook M, Krouse R, “The Risks of<strong>In</strong>dependent Ostomy Care Among FrailCRC Survivors: Lessons From a Study ofFamily Caregiving”• Krouse R, Grant M, McCorkle R, WendelC, Folkman S, Hibbard J, Hornbrook M,“HRQOL-Enhancing Ostomy Self-management<strong>In</strong>tervention for Colorectal CancerSurvivors.”Cobb M, Tallman N, Grant M, McCorkle R,Hornbrook MC, Wendel CS, Folkman S,Hibbard J, Krouse RS, “HRQOL-EnhancingOstomy Self-Management <strong>In</strong>tervention forColorectal Cancer Survivors,” accepted forposter presentation, 2010 WOCN/WCETJoint Conference, Phoenix, June 2010.21
22Krouse RS, accepted for poster presentation,5th Biennial Cancer Survivorship ResearchConference, Washington, D.C., June2010:• Grant M, McMullen CK, Altschuler A,Mohler MJ, Hornbrook MC, HerrintonLJ, Wendel CS, Baldwin CM, Coons SJ,Krouse RS, “Health-Related Quality ofLife in Colorectal Cancer Survivors asIdentified in Focus Groups”• Krouse RS, Grant M, Wendel CS, Mc-Mullen CK, Bulkley JE, Ramirez M,Altschuler A, Coons SJ, Hornbrook MC,Herrinton, LJ, “Dietary and BehavioralAdjustments to Control Bowel Functionfor Long-term Colorectal Cancer Survivors”• Hornbrook MC, McMullen CK, SchneiderJ, Altschuler A, Grant M, LiljestrandP, Krouse RS, “Addressing Age-RelatedDeclines in Survivorship Care Planning:What CRC Patients and Caregivers TellUs About Aging with an Ostomy”• McMullen CK, Schneider J, Altschuler A,Grant M, Hornbrook M, Liljestrand P,Krouse R, “Caregiver Advocacy for theOstomy-related Health of Colorectal CancerSurvivors: Exploring the CaregivingRelationship”Grant M, McMullen CK, Altschuler A, HornbrookMC, Wendel CS, Krouse RS, “LongtermSurvivors of Colorectal Cancer (CRC)with Ostomies: Irrigation Dilemmas,” acceptedfor poster presenation, MASCC/ISOO2010 <strong>In</strong>ternational Symposium on SupportiveCare in Cancer, Vancouver, June 2010.Hornbrook MC, Wendel CS, Coons SJ, GrantM, Herrinton LJ, Mohler J, Baldwin CM, Mc-Mullen CK, Green SB, Altschuler A, RawlSM, Krouse RS, “Predictors of SF-6D ScoresAmong Long-Term Colorectal Cancer Survivors,”accepted for poster presenation, AcademyHealthAnnual Research Meeting, Boston,June 2010.Kulvatunyou N et al, “<strong>In</strong>cidence, Risk Factors,and Clinical Outcome of Contrast-<strong>In</strong>ducedNephropathy Among Trauma Patients,”accepted for poster presentation, SurgicalSouthwest Association Meeting, LoewsVentana Canyon, Tucson, March 2010.Vaughn RC, Joe SA, Pytynia KB, Lemole GMJr, “Surgical Anatomy of the Sphenoid Sinus,<strong>In</strong>ternal Carotid Artery and Distances toCritical Structures,” Chicago Laryngologicand Otologic Society Lederer-Pierce ResearchCompetition, Chicago, April 2010.Lang J, “Breast Cancerand Jewish Heritage,”Temple Emanu-El, Tucson, March2010.Lang J, “Breast Cancerand Genomics,”Breast Surgical OncologyGrand Rounds,Porto Alegre, Brazil,February 2010.Latifi R et al, “<strong>In</strong>tensiveLaparoscopicTraining Course forSurgical Residents:Program Descriptionand <strong>In</strong>itial Results,” 18th <strong>In</strong>ternational Congressof the EAES, Geneva, June 2010.Latifi R, discussant, “Time Critical Conditions– Lessons Learned: Trauma/Acute Care<strong>Surgery</strong>,” Beyond Rationalization: <strong>In</strong>tegratedNetworks of Emergency Care, 2010 AcademicEmergency Medicine Consensus Conference,Phoenix, June 2010.Latifi R, “Establishing Telemedicine in DevelopingCountries – Lessons from the Balkans,”Global Health Salon Series, Washington,DC, May 2010.Latifi R, discussant, Daniel CO, West TA,Craig-Blanco PS, Myers JG, Stewart RM,“Full-Time Trauma Service Leads to ImprovedLevel III Trauma Center Outcomes,”and course director and lecturer, AlbaniaLeadership Telemedicine Training Program,Tirana, Albania, July 2010:• “Telemedicine and e-Health: An <strong>In</strong>troduction”• “Telemedicine Communications TechnologyReview: What Options Are Available?”• “E-Health Education Aspects”• “Telemedicine and Telepresence for Traumaand Emergency Management in ExtremeConditions”• “Establishing Telemedicine in theBalkans: Lessons Learned for OtherCountries”Latifi R, “Enteral Feeding After Blunt AbdominalTrauma: When to Start,” “FulminantColitis, When and How to Operate?,” 11thEuropean Congress of Trauma and Emergency<strong>Surgery</strong>, Brussels, Belgium, May 2010.Latifi R, Hadeed GJ, Mare C, Matter MA,Ridings D, Leyva F, “Prospective Evaluationof a Telemedicine and Telepresence Programfor Trauma,” 11th European Congress ofTrauma and Emergency <strong>Surgery</strong>, Brussels,Belgium, May 2010.Latifi R, “Acute Pancreatitis: When andHow to Operate?,” “Nutritional Aspects of GIEmergency <strong>Surgery</strong>, ” Acute Care <strong>Surgery</strong>Course on Visceral and GastrointestinalEmergencies, European Society for Traumaand Emergency <strong>Surgery</strong>, Graz, Austria, May2010.Latifi R, “Telemedicine for Trauma andEmergencies in Austere Conditions,” HammadMedical Corporation, Doha, Qatar,April 2010.Latifi R, via teleconference, “<strong>In</strong>ternationalVirtual eHospital Telemedicine Programs,”1st <strong>In</strong>ternational Conference on TransformingHealthcare Using <strong>In</strong>formation Technology,<strong>New</strong> Delhi, <strong>In</strong>dia, March 2010.Latifi R, Merrell RC, Doarn CR, Hadeed GJ,Bekteshi F, Lecaj I, “ ‘<strong>In</strong>itiate Build-Operate-Transfer’—A Strategy for Establishing SustainableTelemedicine Programs in DevelopingCountries: <strong>In</strong>itial Lessons from the Balkans,”poster presentation, Prince MahidolAward Conference 2010, Global Health<strong>In</strong>formation Forum, Bangkok, Thailand, January2010.Lemole GM Jr, “Neurosurgery Update:What’s <strong>New</strong> at The University of Arizona?,”Sierra Vista Regional Health Center, BensonHospital, Benson, AZ, May 2010.Herrera SR, Shin JH, Koulumberis PE, ChanM, Hage Z, Alaraj AM, Lemole GM Jr,Amin-Hanjani S, Slavin KV, Charbel FT, “CT
Department of <strong>Surgery</strong>PO Box 245066Tucson AZ 85724-5066NONPROFIT ORGUS POSTAGE PAIDTUCSON AZPERMIT NO. 190To refer a patient or for an appointment, call (520) 694-1000Visit us online: www.surgery.arizona.edu<strong>Surgery</strong> at the University of Arizona –Advancing Care, Achieving Cures24