Gastroschisis-Guidel..
Gastroschisis-Guidel..
Gastroschisis-Guidel..
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
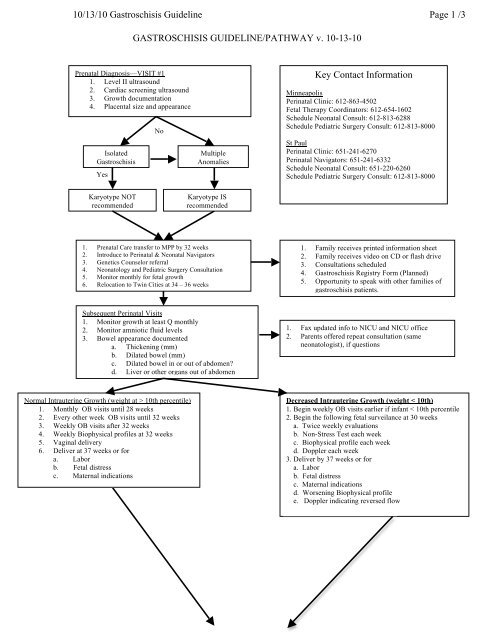
10/13/10 <strong>Gastroschisis</strong> <strong>Guidel</strong>ine Page 1 /3GASTROSCHISIS GUIDELINE/PATHWAY v. 10-13-10Prenatal Diagnosis—VISIT #11. Level II ultrasound2. Cardiac screening ultrasound3. Growth documentation4. Placental size and appearanceIsolated<strong>Gastroschisis</strong>YesNoMultipleAnomaliesKey Contact InformationMinneapolisPerinatal Clinic: 612-863-4502Fetal Therapy Coordinators: 612-654-1602Schedule Neonatal Consult: 612-813-6288Schedule Pediatric Surgery Consult: 612-813-8000St PaulPerinatal Clinic: 651-241-6270Perinatal Navigators: 651-241-6332Schedule Neonatal Consult: 651-220-6260Schedule Pediatric Surgery Consult: 612-813-8000Karyotype NOTrecommendedKaryotype ISrecommended1. Prenatal Care transfer to MPP by 32 weeks2. Introduce to Perinatal & Neonatal Navigators3. Genetics Counselor referral4. Neonatology and Pediatric Surgery Consultation5. Monitor monthly for fetal growth6. Relocation to Twin Cities at 34 – 36 weeks1. Family receives printed information sheet2. Family receives video on CD or flash drive3. Consultations scheduled4. <strong>Gastroschisis</strong> Registry Form (Planned)5. Opportunity to speak with other families ofgastroschisis patients.Subsequent Perinatal Visits1. Monitor growth at least Q monthly2. Monitor amniotic fluid levels3. Bowel appearance documenteda. Thickening (mm)b. Dilated bowel (mm)c. Dilated bowel in or out of abdomen?d. Liver or other organs out of abdomen1. Fax updated info to NICU and NICU office2. Parents offered repeat consultation (sameneonatologist), if questionsNormal Intrauterine Growth (weight at > 10th percentile)1. Monthly OB visits until 28 weeks2. Every other week OB visits until 32 weeks3. Weekly OB visits after 32 weeks4. Weekly Biophysical profiles at 32 weeks5. Vaginal delivery6. Deliver at 37 weeks or fora. Laborb. Fetal distressc. Maternal indicationsDecreased Intrauterine Growth (weight < 10th)1. Begin weekly OB visits earlier if infant < 10th percentile2. Begin the following fetal surveilance at 30 weeksa. Twice weekly evaluationsb. Non-Stress Test each weekc. Biophysical profile each weekd. Doppler each week3. Deliver by 37 weeks or fora. Laborb. Fetal distressc. Maternal indicationsd. Worsening Biophysical profilee. Doppler indicating reversed flow
10/13/10 <strong>Gastroschisis</strong> <strong>Guidel</strong>ine Page 2 /3Resuscitation1. Dry the infant2. Assess respiratory status3. Provide respiratory support4. Attach monitors5. Protect exposed visceraa. Saran wrap followed by Kerlix creating gauze silob. Lateral position to protect silo of wrapped bowel6. Place peripheral IV7. Begin IV glucose infusion – 120/kg8. Fluid bolus-normal saline – 10 ml/kg9. Nasogastric tube, aspirate stomach and low intermittentsuction10. Blood cx11. Temperature stabilizationNICU1. Infant is weighed2. Infants length is measured3. Attach monitors4. Respiratory support5. Call pediatric surgeonsa. Notify surgeon in advance (day/evening only)b. During Night only call when he/she should come tothe NICU6. Blood worka. CBC with differentialb. Glucosec. Type and screen7. Intubated and paralyzed, if clinically indicated8. OG Tube to LIS, #8-#10 Fr. Replogle9. Urinary catheter (Foley)10. Spring loaded silo placed if abd. Closure not possible11. Amp. and Gentamicin until 24 hrs after abd. closure12. PICC line for all infantsa. If PICC line not central Broviac may be placed atclosurePrimary Surgical Closure1) PIP 12 mm Hg. (16 cm H 2 O), notify doctor &consider:a) Elevate HOB to 30 degrees (maximum)b) Remove constricting dressingsc) Neuromuscular blockaded) Vasoactive meds to increase perfusion5) For IAP > 20 mm Hg (27 cm H 2 O), which is the officialdefinition of intra-abdominal compartment syndrome)&/or urine output < 1 ml/kg/hr, consider surgicalinterventionSilo followed by Surgical Closure1) Measure intra-abdominal pressure (IAP)a) Hourly X 1 days or until consistently < 12 mm Hg (16cm H 2 O)b) Hourly X 1 day after each silo reduction untilconsistently < 12 mm Hg (16 cm H 2 O)2) For IAP > 20 mm Hg (27 cm H 2 O) consider undoingsilo reduction3) Monitor SpO 2 on silo every hour (not continuously—can damage the bowel)a) Apply probe to the TOP of the silo outside thetopmost part of bowel.b) Do NOT remove plastic liner from the probe—inother words do not expose and do not apply stickypart of probe to silo (can damage silo). Use tape tokeep probe in place and move as silo is reduced.c) Notify neonatologist if SpO 2 on silo and hand is morethan 10% different
10/13/10 <strong>Gastroschisis</strong> <strong>Guidel</strong>ine Page 3 /3Post-Op. Abd. Wall Closure Management1. Morphine or Fentanyl drip (NICU Sedation PowerPlan)2. Ativan 0.1 mg/kg IV agitation q4H PRN3. OG to LIS4. Monitor IAP hourly. (Should be < 12 mm Hg (16 cm H 2 0)5. Notify MD if IAP > 12 mm Hg (20 cm H 2 O) & consider medicaltreatmenta. N/G suctionb. Remove any constrictive dressingsc. Elevate head of bed to 30 degreesd. Neuromuscular blockadee. Vasoactive meds to keep perfusion pressure adequate6. Notify MD if IAP >20 mm H 2 O (27 cm H 2 O) &/or urine output< 1 ml/kg/hr AND consider surgical decompressionAttempt Feeding1. Assess stooling, OG drainage and OG color2. 2 weeks post operative suppository3. Begin with bolus 20 mL/Kg/day offered by mouthdivided Q3H4. Begin with breast milk, standard formula or ElecareFailure to Progress1. Reassess by 2 months post surgery2. Consider GI patency studies3. Consider exploratory surgerya. Possible obstructionSuccessful FeedingPost-Discharge Follow-Up1. Recommend close monitoring of growth(at least 6, 12, 18 months)(2 X risk of poor growth in first 3 years)2. > 50% chance of re-hospitalization (especially in complicated casesatresiasand bowel resections)3. Slightly higher risk of delayed development (mostly inatresia/resection patients)4. Follow up with primary surgeon 1-2 months.