Under the radar - Centre for Mental Health
Under the radar - Centre for Mental Health
Under the radar - Centre for Mental Health
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
POLICY<strong>Under</strong> <strong>the</strong> <strong>radar</strong>Women with borderlinepersonality disorder in prisonMatt Fossey and Georgia Blacka better way
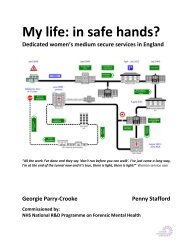
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>2005) (See Box 1). However, this service onlyaccommodates twelve women at a time who aredeemed to be a significant danger to society.Women in o<strong>the</strong>r prisons receive treatment thatfalls short of this standard, and receive far lessthan <strong>the</strong> financial resources given to thosein DSPD services (Barrett et al., 2009). Thispaper ga<strong>the</strong>rs evidence from health, prison andpsychiatric research about women with BPD inprisons.Box 1: Women’s DSPD pilotThe Primrose Project, based at HMP/YOI Low Newton, is a collaborative pilotprogramme serving <strong>the</strong> needs of womenwho primarily pose a risk of seriousharm to <strong>the</strong> public emanating from<strong>the</strong>ir complex clinical presentations.The issues affecting service provision<strong>for</strong> women may be different from thoseof men; <strong>the</strong>re<strong>for</strong>e, <strong>the</strong> Department of<strong>Health</strong> states that <strong>the</strong> project has drawnon best practice to develop a hybridmodel of intervention. Unlike <strong>the</strong> DSPDprogramme <strong>for</strong> male offenders, <strong>the</strong> 12places allocated to <strong>the</strong> Primrose pilotare housed on <strong>the</strong> wings and are notsegregated from <strong>the</strong> rest of <strong>the</strong> prison(Department of <strong>Health</strong>, 2006).When considering <strong>the</strong> provision of services <strong>for</strong>prisoners with personality disorders, politicaldebate and policy decision making seem tobe disproportionately skewed towards thoseoffenders who pose <strong>the</strong> greatest risk to society.A recent report by <strong>the</strong> <strong>Centre</strong> estimates that upto £60 million is spent annually on containingand treating prisoners in services <strong>for</strong> Dangerousand Severe Personality Disorder (DSPD) in onlya small number of prisons and high securityhospitals (Ru<strong>the</strong>r<strong>for</strong>d, 2010), yet DSPD is anon diagnostic term without a clinical meaning(Buchanan & Leese, 2001). An economicevaluation argues that <strong>the</strong>se services are morecostly than prisons and result in a deteriorationin outcomes (Barrett et al., 2009).<strong>Under</strong> 0.5% of prisoners have access to <strong>the</strong>specialist interventions offered by DSPD unitsdue to <strong>the</strong> nature and degree of <strong>the</strong>ir condition,yet research suggests that 78% of male remand,64% of male sentenced and 50% of femaleprisoners have a diagnosis of personalitydisorder (Singleton et al., 1998).Although significant resources are directedtowards interventions <strong>for</strong> male prisoners indangerous and severe personality disorderservices very little resource is used to helpwomen prisoners with debilitating conditionssuch as borderline personality disorder.What is borderline personalitydisorder?The term personality disorder has been usedto describe people who have “an enduringpattern of inner experience and behaviourthat deviates markedly from <strong>the</strong> expectationsof <strong>the</strong> individual’s culture” (DSM-IV, 1994).There are twelve different types of personalitydisorder (Sainsbury <strong>Centre</strong>, 2009a). Borderlinepersonality disorder (BPD) is a diagnosis used todescribe people who show “a pervasive patternof instability of interpersonal relationships,self-image, and affect, and marked impulsivity,beginning by early adulthood and present in avariety of contexts” (DSM-IV, 1994).“It was like as if someone had injected mewith ... I don’t know speed or something, and Iwas just getting out of control. I was told ‘if youdon’t come off <strong>the</strong> ladder you’re going to fall off<strong>the</strong> top, you’re going to run out of rungs’.”Many people with BPD experience a life full ofemotional pain and distress (Perseius et al.,2005). The reality of <strong>the</strong> symptoms described in<strong>the</strong> diagnostic manual is that <strong>the</strong>se difficultiesoften lead to self-harm and self-mutilation,associated with <strong>the</strong> complexity of expressingdifficult emotions (Nehls, 1999). A systematicreview found that over half of people withBPD also fulfilled criteria <strong>for</strong> drug or alcoholdependence (Trull et al., 2000).Many people with borderline personalitydisorder have experienced some <strong>for</strong>m ofchildhood trauma, especially physical abuse(71%), sexual abuse (68%), and witnessingserious domestic violence (62%) (Herman etal., 1989). This leads to some of <strong>the</strong> underlyingcognitions behind borderline personalitydisorder, <strong>for</strong> instance feeling that <strong>the</strong> world ishostile (Silk et al., 1995).2
Treatment <strong>for</strong> BPD in <strong>the</strong> community haschanged in recent years following publicationof government policy implementation guidance(Department of <strong>Health</strong>, 2003). This has beenfur<strong>the</strong>r rein<strong>for</strong>ced by new evidence-basedguidelines, recommending longer treatmentcourses, a reduction in medication prescriptionand continuity of care (NICE, 2009).Borderline personality disorderand women in prisonBPD is very common in prison, with a recentestimate at 30% <strong>for</strong> men and women in <strong>the</strong> US(Black et al., 2007). A decade be<strong>for</strong>e, Jordanet al., (1996) estimated that 28% of femaleprisoners met criteria <strong>for</strong> BPD in <strong>the</strong> US,suggesting this figure is stable. BPD has a highco-morbidity with o<strong>the</strong>r mental health diagnosesand risk factors such as substance use and selfinjury.Women represent one-twentieth of <strong>the</strong> prisonpopulation, with <strong>the</strong> current figure at 4,420(5.4%), of whom one-fifth are on remand (PrisonService, 2010). There was a rapid increase innumbers of women in prison from 1,180 in1992 to 3,340 in 2002 (Councell, 2003) sincewhich time <strong>the</strong> figure has been relatively stable.There are still concerns that <strong>the</strong>re are too manywomen in custody (Corston, 2007; MoJ, 2007).“... to tell <strong>the</strong> truth, <strong>the</strong> first time, I don’t evenremember going into prison, I was so ill. It wasonly … talking to xxx, that she said ‘yeah you’vebeen in prison twice’. I said, Oh!”The female population in custody has differentdemographic characteristics to <strong>the</strong> malepopulation, with 19% being <strong>for</strong>eign nationals,and 29% being of an ethnic minority comparedto 13% and 27% respectively <strong>for</strong> men (PrisonService, 2010). Half <strong>the</strong> women in prison haveexperienced domestic violence, and women aretwice as likely as men to have experienced some<strong>for</strong>m of mental illness in <strong>the</strong> year preceding <strong>the</strong>iradmission to custody (Singleton et al., 1998).Sixty-five per cent of imprisoned women havesubstance use problems, compared to 70%of men (Social Exclusion Task Force, 2009).Worryingly, 83% of women in prison have alongstanding illness, compared with 32% of <strong>the</strong>general female population, and many are onprescription medication (HM Chief Inspector ofPrisons, 2009).The Corston Report suggested an agendaof radical change to provision <strong>for</strong> custodialsentences <strong>for</strong> women. The Governmenthas responded by addressing sentencingrecommendations, alternative custodialarrangements, life skills/learning, hygiene andself-harm programmes (Corston, 2007). Thereport also highlighted that while services in <strong>the</strong>community are targeting women who are at riskof offending, <strong>for</strong> instance by providing ‘one stopshops’ (www.justice.gov.uk) and by monitoringthose with mental ill health, that ethos has nottranslated to prisons.The Corston Report did not mention BPD itself,but it included many vignettes about self-harmwithout recognising it as a key indicator of BPD(See Box 2). Despite only representing 5% of<strong>the</strong> custodial population, women represent halfof all self-harming incidents in prison (HomeOffice, 2009).Box 2: Key indicators of borderlinepersonality disorder“If a person presents in primary carewho has repeatedly self-harmed orshown persistent risk-taking behaviouror marked emotional instability,consider referring <strong>the</strong>m to communitymental health services <strong>for</strong> assessment<strong>for</strong> borderline personality disorder.”(NICE, 2009)In 2009, <strong>the</strong> Bradley Report raised concernsabout <strong>the</strong> provision of mental health carein <strong>the</strong> criminal justice system, particularlyhighlighting that <strong>the</strong>re is no <strong>for</strong>mal provision ofservices <strong>for</strong> people with personality disorder inprison (Bradley, 2009). This is not equivalentto <strong>the</strong> community, where specialist services <strong>for</strong>personality disorder have been in developmentsince 2003 (Department of <strong>Health</strong>, 2003). Thereport recommended that <strong>the</strong> Department of<strong>Health</strong>, <strong>the</strong> National Offender ManagementService (NOMS) and <strong>the</strong> NHS develop a strategy<strong>for</strong> managing personality disorder at all levelsof service, from custody to probation and in <strong>the</strong>community (Bradley, 2009). As <strong>the</strong> new strategytakes hold (Department of <strong>Health</strong>, 2009), it isa good time to address borderline personalitydisorder within <strong>the</strong> general context of femaleoffender mental health.<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>3
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>What is <strong>the</strong> impact of prison onwomen with BPD?It has been recognised that people with BPDhave frequently experienced some <strong>for</strong>m oftrauma during childhood, such as sexual abuse(Herman, et al., 1989). The prison environmentis hostile and punitive, having been designedprimarily <strong>for</strong> <strong>the</strong> male prisoner (Corston, 2007).Prisons are predominantly staffed by men, withonly 35% of prison service staff being female(Fawcett Society, 2008).Women who have experienced abuse are morelikely to feel traumatised by routine prisonprocedures such as body searches (Moloneyet al., 2009). This was found in a study of 800male and female prisoners in a US study, where<strong>the</strong> greatest feelings of unsafety in prison wereexpressed by women with depression, anxiety,post traumatic stress disorder (PTSD) or recentvictimisation (Wolff & Shi, 2009).“Well it’s a bloody awful place. It smells likehorse piss as soon as you walk in that healthcare department ... They’ve got so manypsychiatric patients in <strong>the</strong>re ... They just leaveyou in a cell with a hatch open and keep you in<strong>the</strong>re most of <strong>the</strong> day ... When you go on <strong>the</strong>blocks most of <strong>the</strong>m are mentally ill and <strong>the</strong>y’reall on drugs. They’re all trying to nick your drugs.They’re a nightmare. It’s a horrible place.”The reaction of emotionally vulnerable womenin prison may be to re-experience many of <strong>the</strong>features of childhood sexual abuse, namelytraumatic sexualisation, betrayal, powerlessnessand stigmatisation (Heney & Kristiansen, 1998;Dirks, 2004). This poses a threat to <strong>the</strong>ir mentaland physical wellbeing, and may cause <strong>the</strong>mto adopt maladaptive strategies to address <strong>the</strong>trauma of being in prison such as substanceuse, violence, self-injury and suicide (Heney &Kristiansen, 1998; Zlotnick, 1997).Avoiding trauma in people with a personalitydisorder is important, as it directly affects <strong>the</strong>irgeneral and mental health. One study found thatany type of recent victimisation was significantlyassociated with serious mental disorder <strong>for</strong>48.1% of male prisoners and 47.2% of femaleprisoners (Wolff & Shi, 2009). Poorer healthincreases <strong>the</strong> disruption and ill-effects of prison<strong>for</strong> women with BPD and also raises <strong>the</strong> cost to<strong>the</strong> prison estate. People with BPD cost healthservices three times as much when <strong>the</strong>y developo<strong>the</strong>r health problems as those without BPD(Rendu et al., 2002).“I was self-harming quite, quite a lot. Andanybody who self-harms goes straight to <strong>the</strong>hospital wing, which is horrible ... just sitting<strong>the</strong>re until somebody opens <strong>the</strong> cell door …I think that that was where <strong>the</strong> self-harm gotworse … basically if you didn’t go to work you’dget locked in your cell all day. It goes roundin circles. Because you’d self-harmed as apunishment you’d get locked up, so you selfharmeven more to get out of <strong>the</strong> cell, but <strong>the</strong>ywon’t have you at work because you’ve selfharmed.”Family issuesWomen’s pathways to custody differ greatlyfrom those of men, as <strong>the</strong> majority of offencesare non-violent or property related and as suchrarely pose a threat to public safety (Moloney etal., 2009). Women’s offending patterns are morelikely to be directly affected by <strong>the</strong>ir families,with property crimes such as petty <strong>the</strong>ft beingassociated with family poverty (Taylor, 2004).“Didn’t see my son and daughter <strong>for</strong> sixmonths which broke my heart and killed me.”When mo<strong>the</strong>rs are imprisoned <strong>the</strong> impact ishighly disruptive on <strong>the</strong>ir families, as femaleprisoners are often <strong>the</strong> only carers of <strong>the</strong>irchildren, frequently resulting in custody beingtaken by grandparents or o<strong>the</strong>r female relatives(Caddle & Crisp, 1997; Home Office, 2004).This is not <strong>the</strong> case <strong>for</strong> men, whose children areusually cared <strong>for</strong> by <strong>the</strong>ir female partners during<strong>the</strong>ir incarceration (Taylor, 2004). Fa<strong>the</strong>rs takecustody of female prisoners’ children in just 9%of cases in <strong>the</strong> UK, only marginally higher than<strong>the</strong> number taken into care, at 8% (Caddle &Crisp, 1997). Around two-thirds of women inprison have dependent children under 18, and40% of those are children under 10 years.Women with BPD have potentially difficultfamily situations. This may be dependent on<strong>the</strong> severity of BPD symptoms, as men andwomen with increasingly severe symptomsexperience more marital distress, commit moredomestic violence and have more disruptionin <strong>the</strong>ir marriages (Whisman & Schonbrun,2009). Imprisoned women with more antisocialand borderline traits also show greater4
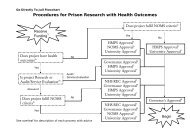
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>to substance use and involvement in <strong>the</strong>sex trade. These factors contribute to <strong>the</strong>likelihood of criminal behaviour.5. Associated stigma: Children of incarceratedparents suffer <strong>the</strong> stigma of criminality, withstaff in <strong>the</strong> criminal justice system beingprone to bias in decision making about <strong>the</strong>child. Some may believe that “<strong>the</strong> apple doesnot fall far from <strong>the</strong> tree” and impose highersanctions <strong>for</strong> criminal behaviour, ra<strong>the</strong>r thangiving <strong>the</strong>m community or social serviceprovision.The potential economic burden of <strong>the</strong>seintergenerational effects could be mitigatedby effective early intervention and parentingprogrammes. A recent report (Sainsbury<strong>Centre</strong>, 2009b) estimates that <strong>the</strong> total cost ofcrime attributable to people who had conductproblems in childhood is approximately £60billion a year in England and Wales.Strategies <strong>for</strong> interventionIn order to tackle a complex mental healthproblem, it first needs to be identified in a timelyfashion, and <strong>the</strong>n treated appropriately, <strong>for</strong> aneffective period of time. In <strong>the</strong> criminal justicesystem, mental health diagnoses are identifiedei<strong>the</strong>r at <strong>the</strong> arrest, court or prison receptionstage, but many mental health problems aremissed due to inadequate screening procedures(Shaw & Humber, 2007). Black et al. (2007)conclude that correctional facilities need tosystematically screen <strong>for</strong> BPD specifically, suchis <strong>the</strong> impact of <strong>the</strong> diagnosis on o<strong>the</strong>r mentalhealth needs in prison.The Corston Report recommended increasedattention to health care, mental health andself-harm, but <strong>the</strong> report does not specificallyaddress BPD. Programmes such as Carousel,which combines group <strong>the</strong>rapy with individualcounselling and o<strong>the</strong>r activities, werementioned. The Government has subsequentlyimplemented <strong>the</strong> CARE (choices, actions,relationships and emotions) programme <strong>for</strong>self-harm at HMP Downview with <strong>the</strong> intentionof widespread use. However, <strong>the</strong>se programmesare inconsistent with NICE guidelines <strong>for</strong> BPD.Simple additions to prison procedure, such ascare in transition periods, could greatly reduce<strong>the</strong> risk <strong>for</strong> women prisoners with BPD. Thecurrent lack of specific provision <strong>for</strong> BPD meansthat evidence-based practice <strong>for</strong> women with thisdiagnosis is ignored, despite <strong>the</strong> high prevalencein <strong>the</strong> prison population. The followinginterventions would help to tackle this problem.ScreeningThe aim of prison mental health services isto screen <strong>for</strong> mental health problems at alllevels of <strong>the</strong> system: from reception screeningand induction or ‘first night’ centres onwards(Department of <strong>Health</strong>, 2005). The earlydetection stage is extremely important as thisdetermines <strong>the</strong> level of care provided in prison.Screening tools used at reception have beencriticised, with many instances of psychiatricmorbidity being missed (Birmingham, 1997). Thissuggests that comprehensive screening at <strong>the</strong>court stage would make a dramatic difference(Shaw et al., 1999; Bradley, 2009).A screening programme <strong>for</strong> BPD at <strong>the</strong> stage ofcourt trial would be able to target <strong>the</strong> 57,875women who were charged with indictableoffences in 2008 (Home Office, 2010). Of <strong>the</strong>se,14.8% are found guilty, leading to 16,440 womenstarting a period in custody (Home Office, 2010).Of <strong>the</strong>se, 12,676 are first receptions into prison,suggesting that a high number of those screenedat reception will not have been screened be<strong>for</strong>e.This may benefit women who have not beendiagnosed outside <strong>the</strong> criminal justice systemand <strong>the</strong>re<strong>for</strong>e have not previously received anysupport <strong>for</strong> <strong>the</strong>ir diagnosis and mental healthneeds. In this way, <strong>the</strong> prison service can play amajor role in increasing <strong>the</strong> number of womenreceiving help <strong>for</strong> BPD.In order to screen and treat women with BPDappropriately, prison health care staff shouldnot be exempt from NICE guidelines, which statethat “mental health professionals working insecondary care services, including communitybasedservices and teams, CAMHS and inpatientservices, should be trained to diagnoseborderline personality disorder, assess risk andneed, and provide treatment and management inaccordance with this guideline” (NICE, 2009).Staff training and recruitmentIt has been widely recognised that lookingafter people with a personality disorder can bedifficult, and some people are better suited to itthan o<strong>the</strong>rs (Bowers et al., 2003). By providingspecialist training and setting up a supportive6
system <strong>for</strong> staff, most will find it easier tocope with and will be able to provide a betterservice. This will also save money in staffingcosts, as positive attitudes towards people withpersonality disorder lead to improved generalhealth and job per<strong>for</strong>mance, decreased burnout,and favourable perception of managers in prisonstaff (Bowers et al., 2006).There are already programmes designedto train staff who are working with peoplewith personality disorders. For example, <strong>the</strong>University of East London provides a part-timepostgraduate certificate entitled Working withPeople with Personality Disorders which isaimed at staff working in statutory or voluntarysector mental health services.The provision of support <strong>for</strong> staff workingwith individuals with a personality disorder isrecommended to include <strong>the</strong> following (Duff,2003):1. Specialised induction2. Mentorship3. Personal development plans and teachingprogrammes linked to organisationaldevelopmental plans4. Support and supervision systems5. DebriefingIn addition, Duff (2003) recommended thatstaff increase <strong>the</strong>ir self-awareness of <strong>the</strong>irvulnerabilities and blind-spots. They shouldalso be more aware of people with a personalitydisorder diagnosis, of <strong>the</strong>ir perspectives andpositive attributes, and be able to build on <strong>the</strong>irexisting skills. It is important <strong>for</strong> staff to haveawareness of potential complications within<strong>the</strong> team due to <strong>the</strong> difficulties of working withpeople who have a diagnosis of personalitydisorder.TransitionsTransition periods in prison custody are highrisk, with increased likelihood of suicide <strong>for</strong>all prisoners (Shaw & Humber, 2007). Prisonsprotect new prisoners from harm by <strong>the</strong>use of a ‘first night’ centre and an inductionwing which are designed to ease transitionalperiods. Care is still lacking in transitions backto <strong>the</strong> community, however, especially <strong>for</strong>prisoners with mental health difficulties. Rapidengagement with community mental healthservices significantly reduces risk during thisperiod (Shaw & Humber, 2007).Equally, a specific NICE target <strong>for</strong> treatment ofBPD is to take added care in transition periods.NICE guidelines say that extra care should betaken when a person with BPD has to make atransition between different sources of care dueto <strong>the</strong> incurred emotional difficulty with thisprocess. The guidelines recommend that:1. Such changes are discussed carefullybe<strong>for</strong>ehand with <strong>the</strong> person (and <strong>the</strong>ir familyor carers if appropriate) and are structuredand phased.2. The care plan supports effective collaborationwith o<strong>the</strong>r care providers during endings andtransitions, and includes <strong>the</strong> opportunity toaccess services in times of crisis.3. When referring a person <strong>for</strong> assessment ino<strong>the</strong>r services (including <strong>for</strong> psychologicaltreatment), <strong>the</strong>y are supported during <strong>the</strong>referral period and arrangements <strong>for</strong> supportare agreed be<strong>for</strong>ehand with <strong>the</strong>m (NICE,2009).We suggest that <strong>the</strong>se detailed arrangementsare made <strong>for</strong> women with BPD, in addition to <strong>the</strong>measures already taken as part of prison policy.Therapeutic interventions in prisonTreatment programmes <strong>for</strong> BPD should bebased on psycho<strong>the</strong>rapeutic principles. Thereis a list of suggested <strong>the</strong>rapeutic approaches in<strong>the</strong> NICE guidelines which includes dialecticaland cognitive behavioural <strong>the</strong>rapy-basedprogrammes, mentalisation-based <strong>the</strong>rapy andpart hospitalisation, cognitive analytical <strong>the</strong>rapyand psychodynamic <strong>the</strong>rapies (NICE, 2009).Dialectical behavioural <strong>the</strong>rapy, which focuseson acceptance and behaviour change, is <strong>the</strong> onlytreatment that has shown consistent benefits<strong>for</strong> people with a borderline personality disorderdiagnosis, according to a Cochrane systematicreview (Binks et al., 2006).In <strong>the</strong> Carousel programme, group <strong>the</strong>rapy iscombined with individual counselling, physicalexercise, relaxation, educational activity and art<strong>the</strong>rapy. Some of this programme con<strong>for</strong>ms to<strong>the</strong> guideline and <strong>the</strong>re<strong>for</strong>e may be beneficial,but it is currently lacking an evidence base. NICEguidelines also suggest that psycho<strong>the</strong>rapeuticinterventions are embedded within a programmeof strategies <strong>for</strong> associated co-morbidities suchas substance use and eating disorders (NICE,2009). It is also stipulated in <strong>the</strong> guidelinesthat <strong>the</strong>rapy should last <strong>for</strong> not less than three<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>7
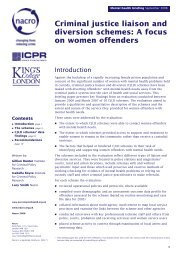
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>months. In remand prisons and with shortsentences this may be difficult (<strong>the</strong>average sentence is just 9.6 months), requiringin-reach/bridge services to continue treatmentin <strong>the</strong> community.Women with BPD frequently have co-morbidmental health problems, including eatingdisorders or substance use issues, andaccording to NICE guidelines <strong>the</strong>se should betreated under <strong>the</strong> same umbrella as BPD. Apractical strategy is to have a care co-ordinatorfacilitating access to BPD treatment in a way thatcomplements substance use programmes. Thisstrategy needs to be introduced into prisonsto enable women to address multiple needsaffecting <strong>the</strong>ir mental health.Alternatives to prisonBy diverting women with BPD from custody,<strong>the</strong> problem of inadequate mental health careprovision in prison may be avoided. There areseveral different schemes that enable women,specifically, to be diverted at any point in<strong>the</strong> criminal justice process. This can includediverting women with a severe mental illnessto hospital under <strong>the</strong> <strong>Mental</strong> <strong>Health</strong> Act (1983)ra<strong>the</strong>r than keeping <strong>the</strong>m in <strong>the</strong> criminal justicesystem.There are also broader schemes supportingprisoners with a variety of mental healthproblems and linking <strong>the</strong>m to communityservices. A review of existing diversion schemesfound that only 2-3% of female offenderscoming through <strong>the</strong> criminal justice systemwere being diverted (Hunter et al., 2005), whichgrossly excludes <strong>the</strong> 50% of female prisonerswith a personality disorder diagnosis.The Primrose Service is <strong>the</strong> only servicedesigned specifically <strong>for</strong> <strong>the</strong> diversion fromprison of women with a personality disorderdiagnosis. But it has just 12 beds, and it ishoused within <strong>the</strong> prison system ra<strong>the</strong>r than asecure hospital.The Bradley Report recommended that <strong>the</strong>Government should evaluate <strong>the</strong> existingtreatment options <strong>for</strong> personality disorder inprison including <strong>the</strong>rapeutic communities, andalso that <strong>the</strong> DSPD units should be assessedto see if <strong>the</strong>y are adequately addressingprisoners’ needs. It also recommended that<strong>the</strong> Department of <strong>Health</strong>, NOMS and <strong>the</strong> NHSshould develop a personality disorder strategythat would cover management from custodial tocommunity services <strong>for</strong> women who are servingshort sentences (Bradley, 2009).Parenting interventionsGiven <strong>the</strong> considerable costs of crimeattributable to conduct disorders (Sainsbury<strong>Centre</strong>, 2009b), and <strong>the</strong> links made betweenmo<strong>the</strong>rs with BPD, incarceration andintergenerational risk factors <strong>for</strong> crime,evidence-based parenting programmesmay be a cost-effective intervention thatcould have longitudinal benefits. The <strong>Centre</strong>(Sainsbury <strong>Centre</strong>, 2009b) estimates that <strong>the</strong>seprogrammes cost as little as £600-£900 perperson <strong>for</strong> group-based <strong>the</strong>rapies and up to£4,000 per person <strong>for</strong> individual interventions.The brevity of parenting programmes alsomeans that <strong>the</strong>y could potentially be delivered<strong>for</strong> women who are serving short sentences.RecommendationsRecommendation 1: Where appropriate,alternatives to custody should be sought at allstages of <strong>the</strong> criminal justice system <strong>for</strong> womenwith a diagnosis of borderline personalitydisorder.Prison can be especially traumatic <strong>for</strong> womenwith a diagnosis of borderline personalitydisorder, due to <strong>the</strong>ir personal histories of abuseand victimisation.Staff should be vigilant to symptoms of BPDat all stages of <strong>the</strong> criminal justice pathway,leading to professional assessment anddiversion to appropriate services.Recommendation 2: Prison staff shouldbe aware of self-harm as a key symptomof borderline personality disorder. This isconsistent with <strong>the</strong> NICE guidelines <strong>for</strong> thiscondition (NICE, 2009).Prison staff should be given training torecognise <strong>the</strong> symptoms of borderlinepersonality disorder, and equipped with <strong>the</strong>basic understanding and skills to managesensitively those who self-harm.8
Recommendation 3: Where possible,interventions consistent with NICE guidelinesshould be offered to women with BPD in <strong>the</strong>criminal justice system.The NICE guidelines recommend that evidencebasedpsychological <strong>the</strong>rapies are used in<strong>the</strong> treatment of people with a diagnosis ofborderline personality disorder. The minimumperiod of treatment suggested in <strong>the</strong> guidelinesis three months.Women with a diagnosis of borderlinepersonality disorder who are servinglong sentences should be given access topsychological <strong>the</strong>rapies to help <strong>the</strong>m to manage<strong>the</strong>ir condition.Where women are on shorter sentences,<strong>the</strong>rapies should still be offered and continuedafter release. Adequately provisioned mentalhealth in-reach services may provide an effectivesolution.Recommendation 4: ‘Meet and greet’ careshould be provided on discharge to improvelinks between prison and community services.People with a borderline personality disorderdiagnosis benefit greatly from well-managedtransitions between different health careproviders. A ‘meet and greet’ procedure wouldavoid disruption in <strong>the</strong> provision of services.This is often ignored due to <strong>the</strong> absence ofadequate hand-over procedures betweencommunity mental health teams and prisonhealth care.Prison health care staff should liaise withprisoners’ local community mental health teamsto prepare <strong>for</strong> release.Recommendation 5: An adequate number oftrained <strong>the</strong>rapists with dialectical behavioural<strong>the</strong>rapy (DBT) skills should be commissioned.The Government is committed to deliveringan increase in access to evidence-basedpsychological <strong>the</strong>rapies (Department of<strong>Health</strong>, 2010). Currently, Improving Access toPsychological Therapy (IAPT) services are beingintroduced across England. This roll-out includes<strong>the</strong> provision of training <strong>for</strong> psychological<strong>the</strong>rapists. This training should be expanded toinclude dialectical behavioural <strong>the</strong>rapy.Recommendation 6: More research needs tobe undertaken to understand <strong>the</strong> impact ofcustody and family separation on women with adiagnosis of borderline personality disorder.The lack of contact with <strong>the</strong>ir children and<strong>the</strong> uncertainty surrounding <strong>the</strong>ir custodyarrangements is a source of great distress to allparents in prison, but particularly <strong>for</strong> women.There is little specific research available in <strong>the</strong>context of women with this diagnosis.Recommendation 7: Family-based and parentinginterventions should be provided to incarceratedwomen with a borderline personality disorder.Children of incarcerated women with a borderlinepersonality disorder diagnosis are particularlyat risk of conduct problems and future offendingbehaviour.Women with a borderline personality disorderdiagnosis tend to have more disrupted families,and so require greater support to maintain astable family unit.By seeking suitable diversion at an earlier stagewithin <strong>the</strong> criminal justice pathway, family unitscan be maintained and <strong>the</strong> risk of disruption tochildren’s lives can be minimised.Where incarceration is <strong>the</strong> only option, socialservices should be sensitive to <strong>the</strong> beneficialeffects of family interventions. All options shouldbe sought to maintain <strong>the</strong> integrity of <strong>the</strong> familyunit. This may include <strong>the</strong> provision of parentingand lifestyle interventions both in prison and onrelease into <strong>the</strong> community.AcknowledgementsThis paper was written by Matt Fossey, <strong>Centre</strong><strong>for</strong> <strong>Mental</strong> <strong>Health</strong> and Georgia Black, Institute ofPsychiatry.The authors would like to thank:The women who agreed to share <strong>the</strong>irexperiences and stories of living with adiagnosis of borderline personality disorder inprison.All of <strong>the</strong> professionals who participated in<strong>the</strong> drafting of this report and contributed<strong>the</strong>ir views and experiences. In particular,Michael Parsonage, Dr Chiara Samele, ClaireWarrington, Lorraine Khan, Dr Graham Durcanand Max Ru<strong>the</strong>r<strong>for</strong>d.<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>9
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>ReferencesBarnow, S., Spitzer, C. et al. (2006) Individualcharacteristics, familial experience, andpsychopathology in children of mo<strong>the</strong>rs withborderline personality disorder. Journal ofAmerican Academy of Child & AdolescentPsychiatry, 45 (8) 965.Barrett, B., By<strong>for</strong>d, S. et al. (2009) Theassessment of dangerous and severepersonality disorder: service use, cost, andconsequences. Journal of Forensic Psychiatry &Psychology, 20 (1) 120-131.Binks, C. A., Fenton, M., McCarthy, L., Lee, T.,Adams, C.E. & Duggan, C. (2006) Psychological<strong>the</strong>rapies <strong>for</strong> people with borderline personalitydisorder. Cochrane Database of SystematicReviews (Issue 1), Art. No: CD005652.DOI:10.1002 / 14651858.CD005652.Birmingham L., Mason, D. & Grubin, D. (1997)<strong>Health</strong> screening at first reception into prison.Journal of Forensic Psychiatry & Psychology, 8(2) 435-439.Birmingham, L., Wilson, S. et al. (2006) Prisonmedicine: ethics and equivalence. The BritishJournal of Psychiatry 188 (1) 4-6.Black, D., Gunter, T. et al. (2007) Borderlinepersonality disorder in male and femaleoffenders newly committed to prison.Comprehensive Psychiatry, 48 (5) 400-405.Bowers, L., Callaghan, P., Nijman, H., Paton, J.,Carr-Walker, P., Allan, T. & Simpson, A. (2003)The Right People <strong>for</strong> <strong>the</strong> Job: Choosing staffthat will adjust positively and productively toworking in <strong>the</strong> new personality disorder (PD)services. Report to <strong>the</strong> Home Office.Bowers, L., Carr-Walker, P. et al. (2006) Attitudeto personality disorder among prison officersworking in a dangerous and severe personalitydisorder unit. International Journal of Law andPsychiatry, 29 (5) 333-342.Bradley, K. (2009) The Bradley Report: LordBradley’s review of people with mental healthproblems or learning disabilities in <strong>the</strong> criminaljustice system. London: Ministry of Justice.Buchanan, A. & Leese, M. (2001) Detentionof people with dangerous severe personalitydisorders: a systematic review. The Lancet, 358(9297) 1955-1959.Caddle, D. & Crisp, D. (1997) Imprisoned Womenand Mo<strong>the</strong>rs. Home Office Research Study No.162. London: Home Office.Corston, J. (2007) The Corston report: A reviewof women with particular vulnerabilities in <strong>the</strong>criminal justice system. London: Home Office.Councell, R. (2003) The Prison Population in2002: A statistical review. Home Office Findings228. London: Home Office.Cunningham, A. & Baker, L. (2004) InvisibleVictims: The children of women in prison.Ontario, Canada: <strong>Centre</strong> <strong>for</strong> Children & Familiesin <strong>the</strong> Justice System.Department of <strong>Health</strong> (2010) Press Release23 June 2010 Psychological <strong>the</strong>rapies offeredacross <strong>the</strong> NHS. (http://www.dh.gov.uk/en/Media<strong>Centre</strong>/Pressreleases/DH_116919)Department of <strong>Health</strong> (2009) Improving <strong>Health</strong>,Supporting Justice: The national delivery planof <strong>the</strong> <strong>Health</strong> and Criminal Justice ProgrammeBoard. London: Department of <strong>Health</strong>.Department of <strong>Health</strong> (2006) Planning andDelivery Guide <strong>for</strong> Women’s DSPD Services(Primrose Programme). Home Office DSPDprogramme. London: Department of <strong>Health</strong> andHM Prison Service.Department of <strong>Health</strong> (2005) Offender <strong>Mental</strong><strong>Health</strong> Care Pathway. London: Department of<strong>Health</strong>.Department of <strong>Health</strong> (2003) PersonalityDisorder: No longer a diagnosis of exclusion– policy implementation guidance <strong>for</strong> <strong>the</strong>development of services <strong>for</strong> people withpersonality disorder. London: Department of<strong>Health</strong>.Dirks, D. (2004) Sexual revictimization andretraumatization of women in prison. Women’sStudies Quarterly, 32 (3) 102-115.Douglas, N. & Plugge, E. (2006) A <strong>Health</strong>Needs Assessment <strong>for</strong> Young Women in YoungOffender Institutions. London: Youth JusticeBoard/University of Ox<strong>for</strong>d.DSM-IV (1994) DSM-IV: Diagnostic andstatistical manual of mental disorders. ArlingtonVA: American Psychiatric Association.Duff, A. (2003) Managing personality disorders:making positive connections. NursingManagement (Harrow), 10 (3) 27-30.10
Fawcett Society (2008) Women and <strong>the</strong> CriminalJustice System: The facts. London: FawcettSociety.Feldman, R., Zelkowitz, P. et al. (1995) Acomparison of <strong>the</strong> families of mo<strong>the</strong>rs withborderline and non-borderline personalitydisorders. Comprehensive Psychiatry, 36 (2)157-163.Greene, S., Haney, C. et al. (2000) Cycles of pain:risk factors in <strong>the</strong> lives of incarcerated mo<strong>the</strong>rsand <strong>the</strong>ir children. The Prison Journal, 80 (1) 3.Heney, J. & Kristiansen, C. (1998) An analysisof <strong>the</strong> impact of prison on women survivors ofchildhood sexual abuse. Women and <strong>the</strong>rapy,20 (4) 29-44.Herman, J., Perry, J. et al. (1989) Childhoodtrauma in borderline personality disorder.American Journal of Psychiatry, 146 (4) 490.HM Chief Inspector of Prisons (2009) RaceRelations in Prison: Responding to adult womenfrom black and minority ethnic backgrounds.London: HM Inspectorate of Prisons.Hobson, R. P., Patrick, M. et al. (2005) Personalrelatedness and attachment in infants ofmo<strong>the</strong>rs with borderline personality disorder.Development and Psychopathology, 17 (02)329-347.Home Office (2010) Statistics on Women and<strong>the</strong> Criminal Justice System: A Ministry of Justicepublication under Section 95 of <strong>the</strong> CriminalJustice Act 1991. London: Ministry of Justice.Home Office (2009) Statistics on Women and <strong>the</strong>Criminal Justice System. London: Home Office.Home Office (2004) Women’s OffendingReduction Programme (WORP) Action Plan.London: Home Office.Hunter, G., Boyce, I. & Smith, L. (2005) CriminalJustice Liaison and Diversion Schemes: A focuson women offenders. <strong>Mental</strong> <strong>Health</strong> Briefing.NACRO. London: NACRO.Jordan, B.K., Schlenger, W.E., Fairbank, J.A. &Caddell, J.M. (1996) Prevalence of psychiatricdisorders among incarcerated women part II.Convicted felons entering prison. Arch GenPsychiatry, 53 (6) 513-519.Lyons-Ruth, K. (1996) Attachment relationshipsamong children with aggressive behaviorproblems: The role of disorganized earlyattachment patterns. Journal of Consulting andClinical Psychology, 64 (1) 64-72.Ministry of Justice (2007) Monthly Bulletin: April2007. Population in Custody. London: Ministryof Justice / NOMS.Moloney, K., van den Bergh, B. et al. (2009)Women in prison: <strong>the</strong> central issues of gendercharacteristics and trauma history. Public<strong>Health</strong>, 123 (6) 426-430Nehls, N. (1999) Borderline personality disorder:The voice of patients. Research in Nursing &<strong>Health</strong>, 22 (4) 285-293.NICE (2009) Borderline Personality Disorder:Treatment and management. London: NICE.Niveau, G. (2007) Relevance and limits of <strong>the</strong>principle of ‘equivalence of care’ in prisonmedicine. British Medical Journal, 33 (10) 610.Perseius, K., Ekdahl, S. et al. (2005) To tame avolcano: patients with borderline personalitydisorder and <strong>the</strong>ir perceptions of suffering.Archives of Psychiatric Nursing, 19 (4) 160-168.Prison Service (2010) March 2010. Populationin Custody: Monthly Bulletin. London: PrisonService.Rendu, A., Moran, P. et al. (2002) Economicimpact of personality disorders in UK primarycare attenders. The British Journal of Psychiatry,181 (1) 62.Ru<strong>the</strong>r<strong>for</strong>d, M. (2010) Blurring <strong>the</strong> boundaries:The convergence of mental health and criminaljustice policy, legislation, systems and practice.London: Sainsbury <strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong>.Sainsbury <strong>Centre</strong> (2009a) Personality Disorder:A briefing <strong>for</strong> people working in <strong>the</strong> criminaljustice system. London: Sainsbury <strong>Centre</strong> <strong>for</strong><strong>Mental</strong> <strong>Health</strong>.Sainsbury <strong>Centre</strong> (2009b) The Chance of aLifetime: Preventing early conduct problems andreducing crime. London: Sainsbury <strong>Centre</strong> <strong>for</strong><strong>Mental</strong> <strong>Health</strong>.Shaw, J., Creed, F. et al. (1999) Prevalence anddetection of serious psychiatric disorder indefendants attending court. Lancet (Britishedition), 353 (9158) 1053-1056.Shaw, J. & Humber, N. (2007) Prison mentalhealth services. Psychiatry, 6 (11) 465-469.<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>11
<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>Silk, K., Lee, S., et al. (1995) Borderlinepersonality disorder symptoms and severity ofsexual abuse. American Journal of Psychiatry,152 (7) 1059-1064.Singleton, N., Meltzer, H. & Gatward, R. (1998)Psychiatric Morbidity among Prisoners inEngland and Wales. London: Office <strong>for</strong> NationalStatistics.Social Exclusion Task Force (2009) Short Studyon Women Offenders. London: Cabinet Office.Social Exclusion Unit (2002) Reducing Reoffendingby Ex-prisoners. London: SocialExclusion Unit.Taylor, R. (2004) Women in Prison and Childrenof Imprisoned Mo<strong>the</strong>rs: Preliminary researchpaper. Geneva, Switzerland: Quaker UnitedNations Office.Travers, R. & Reeves, S. (2005) Breaking barriersand building connections. International Journalof Prisoner <strong>Health</strong>, 1 (2) 199-205.Trull, T., Sher, K. et al. (2000) Borderlinepersonality disorder and substance usedisorders: A review and integration. ClinicalPsychology Review, 20 (2) 235-253.Warren, J. & South, S. (2009) A symptomlevel examination of <strong>the</strong> relationship betweenCluster B personality disorders and patterns ofcriminality and violence in women. InternationalJournal of Law and Psychiatry, 32 (1) 10-17.Weiss, M., Zelkowitz, P. et al. (1996)Psychopathology in offspring of mo<strong>the</strong>rs withborderline personality disorder: a pilot study.Canadian Journal of Psychiatry, 41 (5) 285-290.Whisman, M. & Schonbrun, Y. (2009) Socialconsequences of borderline personality disordersymptoms in a population-based survey:marital distress, marital violence, and maritaldisruption. Journal of Personality Disorders, 23(4) 410-415.Wolff, N. & Shi, J. (2009) Victimisation andfeelings of safety among male and femaleinmates with behavioural health problems.Journal of Forensic Psychiatry & Psychology, 20,56-77.Zlotnick, C. (1997) Post traumatic stress disorder(PTSD), PTSD co-morbidity and childhood abuseamong incarcerated women. Journal of Nervous& <strong>Mental</strong> Disease, 185 (12) 761-763.12
More from a better waya better way is our campaign to highlight our concerns and provoke political, media andpublic debate about <strong>the</strong> approach we take to mental health in <strong>the</strong> criminal justice system.We want to change <strong>the</strong> way people think about mental health and criminal justice and setout a better way of working.Our campaign includes <strong>the</strong> following publications:Public <strong>Health</strong> and Criminal Justice: Promoting and protecting offenders’ mental healthand wellbeing (July 2010)Blurring <strong>the</strong> Boundaries: The convergence of mental health and criminal justice policy,legislation, systems and practice (March 2010)The Chance of a Lifetime: Preventing early conduct problems and reducing crime(November 2009)Securing Employment <strong>for</strong> Offenders with <strong>Mental</strong> <strong>Health</strong> Problems: Towards a better way(September 2009)The Bradley Report and <strong>the</strong> Government’s Response: The implications <strong>for</strong> mental healthservices <strong>for</strong> offenders (July 2009)Commissioning <strong>Mental</strong> <strong>Health</strong> Care in <strong>the</strong> Criminal Justice System: 10 top tips <strong>for</strong> PCTBoards (June 2009)A Missed Opportunity: Community Sentences and <strong>the</strong> <strong>Mental</strong> <strong>Health</strong> TreatmentRequirement (March 2009)Diversion: A better way <strong>for</strong> criminal justice and mental health (February 2009)On <strong>the</strong> Outside: Continuity of care <strong>for</strong> people leaving prison (December 2008)The Police and <strong>Mental</strong> <strong>Health</strong>: A briefing (September 2008)From <strong>the</strong> Inside: Experiences of prison mental health care (June 2008)Short-changed: Spending on prison mental health care (May 2008)Visit www.centre<strong>for</strong>mentalhealth.org.uk to find out more about our work and to downloadcopies of <strong>the</strong>se publications.<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong> POLICY PAPER <strong>Under</strong> <strong>the</strong> <strong>radar</strong>13
<strong>Under</strong> <strong>the</strong> <strong>radar</strong>Women with borderline personalitydisorder in prisonMatt Fossey and Georgia Black© <strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong>,September 2010Recipients (journals excepted) are free tocopy or use <strong>the</strong> material from this paper,provided that <strong>the</strong> source is appropriatelyacknowledged.Register <strong>for</strong> our monthly email bulletinsand copies of new briefing papers atwww.centre<strong>for</strong>mentalhealth.org.ukPOLICY<strong>Under</strong> <strong>the</strong> <strong>radar</strong>Women with borderlinepersonality disorder in prisonMatt Fossey and Georgia Blacka better way<strong>Centre</strong> <strong>for</strong><strong>Mental</strong> <strong>Health</strong>Realising a better future<strong>Centre</strong> <strong>for</strong> <strong>Mental</strong> <strong>Health</strong>134–138 Borough High Street, London SE1 1LBT 020 7827 8300F 020 7827 8369www.centre<strong>for</strong>mentalhealth.org.ukCharity registration no. 1091156. A Company limited by guaranteeregistered in England and Wales no. 4373019.