Perioperative Management of the Diabetic Patient: [Print ...
Perioperative Management of the Diabetic Patient: [Print ...
Perioperative Management of the Diabetic Patient: [Print ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Perioperative</strong> <strong>Management</strong> <strong>of</strong> <strong>the</strong> <strong>Diabetic</strong> <strong>Patient</strong>: [<strong>Print</strong>] - eMedicine Pe... http://emedicine.medscape.com/article/284451-print<br />
type 1 diabetes mellitus (DM) usually demand intravenous insulin <strong>the</strong>rapy depending on <strong>the</strong> nature <strong>of</strong> surgery and are more<br />
predisposed to end-organ complications than patients with type 2 diabetes mellitus. <strong>Patient</strong>s with type 2 diabetes will need to have <strong>the</strong>ir<br />
oral hypoglycemic drugs discontinued preoperatively, with intravenous insulin administered if dictated by <strong>the</strong> extent <strong>of</strong> <strong>the</strong> procedure.<br />
Even nondiabetic patients, because <strong>of</strong> <strong>the</strong> considerable stress response, may become hyperglycemic perioperatively. Multiple<br />
randomized controlled studies have shown that controlling serum glucose levels in all patients, not merely those with diabetes mellitus<br />
(DM), impacts <strong>the</strong> outcome <strong>of</strong> surgical patients who are critically ill. This effect does not appear to be related to <strong>the</strong> dose <strong>of</strong> insulin but<br />
ra<strong>the</strong>r to <strong>the</strong> absolute level <strong>of</strong> serum glucose achieved.<br />
Anes<strong>the</strong>tic agents can affect glucose metabolism through <strong>the</strong> modulation <strong>of</strong> sympa<strong>the</strong>tic tone; in vitro data suggest that inhalational<br />
agents suppress insulin secretion. [19 ] The resulting relative insulin deficiency <strong>of</strong>ten leads to glucose dysregulation and hyperglycemia.<br />
This deficiency is compounded in diabetic patients, particularly those with insulin resistance, raising <strong>the</strong> risk <strong>of</strong> ketoacidosis. The use <strong>of</strong><br />
regional anes<strong>the</strong>sia or peripheral nerve blocks may mitigate <strong>the</strong>se concerns, but no data suggest that <strong>the</strong>se forms <strong>of</strong> anes<strong>the</strong>sia<br />
improve postoperative survival in patients with diabetes mellitus (DM).<br />
Goals <strong>of</strong> <strong>Perioperative</strong> Glycemic Control<br />
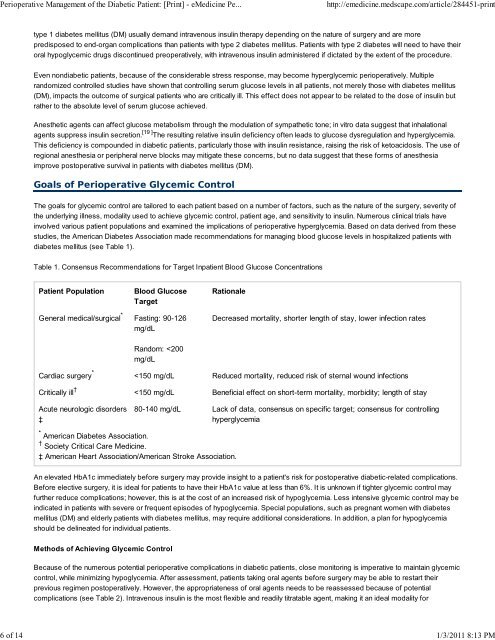
The goals for glycemic control are tailored to each patient based on a number <strong>of</strong> factors, such as <strong>the</strong> nature <strong>of</strong> <strong>the</strong> surgery, severity <strong>of</strong><br />
<strong>the</strong> underlying illness, modality used to achieve glycemic control, patient age, and sensitivity to insulin. Numerous clinical trials have<br />
involved various patient populations and examined <strong>the</strong> implications <strong>of</strong> perioperative hyperglycemia. Based on data derived from <strong>the</strong>se<br />
studies, <strong>the</strong> American Diabetes Association made recommendations for managing blood glucose levels in hospitalized patients with<br />
diabetes mellitus (see Table 1).<br />
Table 1. Consensus Recommendations for Target Inpatient Blood Glucose Concentrations<br />
<strong>Patient</strong> Population Blood Glucose<br />
Target<br />
General medical/surgical *<br />
Cardiac surgery *<br />
Critically ill †<br />
Acute neurologic disorders<br />
‡<br />
Fasting: 90-126<br />
mg/dL<br />
Random: