Prevention of Heel Ulcers and Plantar Flexion Contractures
Prevention of Heel Ulcers and Plantar Flexion Contractures
Prevention of Heel Ulcers and Plantar Flexion Contractures
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
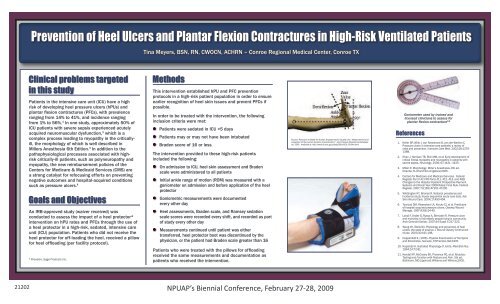
NPUAP’s Biennial Conference, February 27-28, 2009<strong>Prevention</strong> <strong>of</strong> <strong>Heel</strong> <strong>Ulcers</strong> <strong>and</strong> <strong>Plantar</strong> <strong>Flexion</strong> <strong>Contractures</strong> in High-Ris<strong>Prevention</strong> <strong>of</strong> <strong>Heel</strong> <strong>Ulcers</strong> <strong>and</strong> <strong>Plantar</strong> <strong>Flexion</strong> <strong>Contractures</strong> in High-Risk Ventilated PatientsTina Meyers, BSN, RN, CWOCN, ACHRN – Conroe Regional Medical Center, ConrTina Meyers, BSN, RN, CWOCN, ACHRN – Conroe Regional Medical Center, Conroe TXChange in <strong>Heel</strong>/Patient StatusPatients in the intensive care unit (ICU) have a highrisk <strong>of</strong> developing heel pressure ulcers (hPUs) <strong>and</strong>plantar flexion contractures (PFCs), with prevalenceranging from 14% to 41%, <strong>and</strong> incidence rangingfrom 1% to 56%. 1 In one study, approximately 50% <strong>of</strong>ICU patients with severe sepsis experienced acutelyacquired neuromuscular dysfunction, 2 which is acomplex process leading to myopathy in the criticallyill,the morphology <strong>of</strong> which is well described inMillers Anesthesia 6th Edition. 3 In addition to thepathophysiological processes associated with highriskcritically-ill patients, such as polyneuropathy <strong>and</strong>myopathy, the new reimbursement policies <strong>of</strong> theCenters for Medicare & Medicaid Services (CMS) area strong catalyst for refocusing efforts on preventingnegative outcomes <strong>and</strong> hospital-acquired conditionssuch as pressure ulcers. 4An IRB-approved study (waiver received) wasconducted to assess the impact <strong>of</strong> a heel protector*intervention on hPU rates <strong>and</strong> PFCs through the use <strong>of</strong>a heel protector in a high-risk, sedated, intensive careunit (ICU) population. Patients who did not receive theheel protector for <strong>of</strong>f-loading the heel, received a pillowfor heel <strong>of</strong>floading (per facility protocol).* Prevalon, Sage Products Inc.This intervention established hPU <strong>and</strong> PFC preventionprotocols in a high-risk patient population in order to ensureearlier recognition <strong>of</strong> heel skin issues <strong>and</strong> prevent PFCs ifpossible.In order to be treated with the intervention, the followinginclusion criteria were met:Patients were sedated in ICU >5 daysPatients may or may not have been intubatedBraden score <strong>of</strong> 16 or lessThe intervention provided to these high-risk patientsincluded the following:On admission to ICU, heel skin assessment <strong>and</strong> Bradenscale were administered to all patientsInitial ankle range <strong>of</strong> motion (ROM) was measured with aSource: Research Institute for Human Engineering for Quality Life, “Measurement <strong>and</strong>goniometer on evaluation admission <strong>of</strong> the human dynamic <strong>and</strong> characteristics,” before application Joint Passive Resistance <strong>of</strong> the Database heela4, 2000. Available at: http://www.dh.aist.go.jp/bodyDB/a/HQL-00-04e.htmlprotectorGoniometric measurements were documentedevery other day<strong>Heel</strong> assessments, Braden scale, <strong>and</strong> Ramsey sedationscale scores were recorded every shift, <strong>and</strong> recorded as part<strong>of</strong> study every other dayMeasurements continued until patient was eithertransferred, heel protector boot was discontinued by thephysician, or the patient had Braden scale greater than 16Patients who were treated with the pillows for <strong>of</strong>floadingreceived the same measurements <strong>and</strong> documentation aspatients who received the intervention.The study resulted in 100% prevention <strong>of</strong>hPU development, 100% prevention <strong>of</strong> PFCdevelopment, enhanced caregiver compliancewith existing protocols, <strong>and</strong> several surprisingsecondary findings:Source: Research Institute for Human Engineering for Quality Life, “Measurement <strong>and</strong>evaluation <strong>of</strong> the human dynamic characteristics,” Joint Passive Resistance Databasea4, 2000. Available at: http://www.dh.aist.go.jp/bodyDB/a/HQL-00-04e.html9.4% showed improvement in heel status fromentry to discharge11.3% <strong>of</strong> existing heel skin conditions stayedSource: Research Institute for Human Engineering for Quality Life, “Measurement <strong>and</strong>evaluation <strong>of</strong> the human dynamic characteristics,” Joint Passive Resistance Databasea4,the2000.sameAvailable at:withhttp://www.dh.aist.go.jp/bodyDB/a/HQL-00-04e.htmlno change <strong>and</strong> no worseningin status50% <strong>of</strong> abnormal heels showed improvement130130 120120 110110 100Ankle Ankle angle at at rest rest (in degrees)Ankle angle at rest100 9090 8080707060605050Secondary Goniometric Findings:Improvements in <strong>Plantar</strong> <strong>Flexion</strong> <strong>Contractures</strong>Improvements Secondary Goniometric in <strong>Plantar</strong> Findings:4.Improvements in <strong>Plantar</strong> <strong>Flexion</strong> <strong>Contractures</strong>Secondary Goniometric Findings:= improvementNeutral (normal)Goniometer used by trained <strong>and</strong>licensed clinicians to assess forplantar flexion contracture 6-8<strong>Flexion</strong> <strong>Contractures</strong>n = 106Individual anklesIndividual ankles*Individual anklesEntry MeasurementExit MeasurementEntry MeasurementExit Measurement* Of the 106 ankles measured with goniometer, 20 showed improvement from entry to exit..Goniometer used by trained <strong>and</strong>licensed clinicians to assess forplantar flexion contracture 6-8Goniometer used by trained <strong>and</strong>licensed clinicians to assess forplantar flexion contracture 6-8References1. Keller BP, Wille J, van Ramshorst B, van der Werken C.Pressure ulcers in intensive care patients: a review <strong>of</strong>risks <strong>and</strong> prevention. Intensive Care Med. 2002;28:1379-1388.2. Khan J, Harrison TB, Rich MM, et al: Early development <strong>of</strong>critical illness myopathy <strong>and</strong> neuropathy in patients withsevere sepsis. Neurology. 2006; 67:1421–1425.3. Miller R. Morphology. Miller’s Anesthesia, 6th ed.Orl<strong>and</strong>o, FL:Churchill-Livingstone;2005.Centers for Medicare <strong>and</strong> Medicaid Services. FederalRegister Part II 42 CFR Parts 411, 412, 413, <strong>and</strong> 489:Changes to the Hospital Inpatient Prospective PaymentSystems <strong>and</strong> Fiscal Year 2008 Rates; Final Rule. FederalNew hPUsFinancial Benefits <strong>of</strong> hPU PreventioRegister. 2007;72(162):47201-47205.5. Whittington KT, Briones R. National prevalence <strong>and</strong>incidence study: 6-year sequential acute care data. AdvSkin Wound Care. 2004;17:490-494.6. Tourtual DM, Riesenbert LA, Korutz CJ, et al. Predictors<strong>of</strong> hospital acquired pressure ulcers. Ostomy/WoundManage. 1997;43(9):24-40.7. L<strong>and</strong>i F, Onder G, Russo A, Bernabei R. Pressure ulcer<strong>and</strong> mortality in frail elderly people living in community.Arch Gerontol Geriatr. 2007;44 Suppl 1:217-223.8. Wong VK, Stolis NA. Physiology <strong>and</strong> prevention <strong>of</strong> heelulcers: the state <strong>of</strong> science. J Wound Ostomy ContinenceNurse. 2003;30:191-198.9. Hoppenfeld S. (1976). Physical Examination <strong>of</strong> the Spine<strong>and</strong> Extremities. Norwalk, CT:Prentice-Hall;1976.10. Kap<strong>and</strong>ji IA. Ilustrated Physiology <strong>of</strong> Joints. Med Biol Illus.1964;14:72-81.11. Kendall FP, McCreary EK, Provance PG, et al. Muscles:Testing <strong>and</strong> Function with Posture <strong>and</strong> Pain. 5th ed.Baltimore, MD:Lippincott Williams <strong>and</strong> Wilkens;2005.[Avg census 260; 7.3%4 may develop PUs = 19; 28%4 may develop hPUs = 5; total hPU days (365) = 1825;avg LOS 4.6 (NIS Data) = 397 actual hPU days; 93% stage 1 or 2 4 = 369; 7% stage 3 or 4 4 = 28]4 Whittington KT, Briones R. Adv Skin Wound Care. 2004;17:490-494;9 Young ZF, Evans A, Davis J. J Nurs Adm. 2003;33:380-383.21202• 100% prevention <strong>of</strong>NPUAP’s Biennial Conference, February 27-28, hospital-acquired 2009 hPUs• 100% prevention <strong>of</strong> plantarReferences1. Keller BP, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: a review<strong>of</strong> risks <strong>and</strong> prevention. Intensive Care Med. 2002;28:1379-1388.2. Khan J, Harrison TB, Rich MM, et al: Early development <strong>of</strong> critical illness myopathy <strong>and</strong> neuropathy in5.6.
CWOCN, ACHRN – Conroe Regional Medical Center, Center, Conroe Conroe TX TX<strong>Plantar</strong> <strong>Flexion</strong> <strong>Contractures</strong> in High-Risk Ventilated Patientsnsure ensureCs ififtientsth ae heelaheelonas sedation partcorded as parts partherthe ed by theater n 16 than 16effloadingn ntation 16as asgasN, CWOCN, ACHRN – Conroe Regional Medical Center, Conroe TXentionder ing to ensureent g PFCs iffollowingdd Bradenred with an <strong>of</strong> the heelThe study resulted in in 100% prevention <strong>of</strong> <strong>of</strong>hPU development, 100%100%preventionprevention<strong>of</strong><strong>of</strong>PFCPFCdevelopment, enhanced caregiver compliancedevelopment, enhanced caregiver complianceChange in <strong>Heel</strong>/Patient Statuswith existing protocols, <strong>and</strong> several surprisingwith The existing study resulted protocols, in 100% <strong>and</strong> prevention several surprising<strong>of</strong>secondary findings:hPUssecondary hPU development, findings: 100% prevention <strong>of</strong> PFC9.4%development,showedenhancedimprovementcaregiverin heelcompliancestatus from9.4% with existing showed protocols, improvement <strong>and</strong> several in surprisingentry heel status fromsecondaryto dischargefindings:entry to discharge11.3% 9.4% <strong>of</strong> showed existing improvement heel skin in conditions heel status stayed from11.3% the entry same <strong>of</strong> to with existing discharge no change heel skin <strong>and</strong> conditions no worsening stayedthe in status same with no change <strong>and</strong> no worsening11.3% <strong>of</strong> existing heel skin conditions stayedin status50% the <strong>of</strong> same abnormal with no heels change showed <strong>and</strong> no improvementworseningNew hPUsin status50% <strong>of</strong> abnormal heels showed improvementNew hPUsSecondary Goniometric Findings:Secondary 50% <strong>of</strong> abnormalImprovementsGoniometric heels showed improvementin <strong>Plantar</strong>Findings:New hPUs<strong>Flexion</strong> <strong>Contractures</strong>Secondary Goniometric Findings:Secondary Improvements Secondary Goniometric in <strong>Plantar</strong> Findings:Secondary GoniometricImprovements in <strong>Plantar</strong> Findings:Secondary <strong>Flexion</strong> <strong>Contractures</strong>130<strong>Flexion</strong> in <strong>Plantar</strong> <strong>Contractures</strong><strong>Flexion</strong> <strong>Contractures</strong>ImprovementsGoniometric in <strong>Plantar</strong>Findings:in <strong>Plantar</strong> Findings: <strong>Flexion</strong> <strong>Contractures</strong>Improvements Secondary Goniometric in <strong>Plantar</strong> Findings:Financial Benefits <strong>of</strong> hPU <strong>Prevention</strong>130130 120 Improvements 130 <strong>Flexion</strong> in <strong>Plantar</strong> <strong>Contractures</strong><strong>Flexion</strong> <strong>Contractures</strong>Financial Benefits <strong>of</strong> hPU <strong>Prevention</strong>120 110 130 120PFCs130 120110 100 120 110120 110100 110 10090110 100 10090908010090 80807090 8070 80 70607080 6060 705060507050 6050Ankle Ankle angle Ankle at at Ankle rest angle rest (in at at degrees) rest rest (in degrees)Ankle angle Ankle at angle rest at restAnkle Ankle angle at at rest rest (in degrees)Ankle angle at rest605050= improvementn = 106Individual anklesIndividual ankles*Individual ankles= improvementNeutral Neutral (normal) (normal)= improvementEntry MeasurementExit Exit MeasurementEntry Measurementankles Entry measured Measurement with goniometer,Exit Measurementshowed improvement from * Of the 106 20 entry to exit..* Of the 106 ankles measured with goniometer, 20 showed improvement from entry to exit..Neutral (normal)Exit Individual Measurement anklesIndividual ankles*Individual anklesEntry MeasurementEntry MeasurementExit Measurement• 100% prevention <strong>of</strong>n = 106n = 106Exit Measurement* Of the 106 ankles measured with goniometer, 20 showed improvement from entry to exit..• 100%hospital-acquiredprevention <strong>of</strong>hPUshospital-acquired hPUs• 100% prevention <strong>of</strong> <strong>of</strong> plantar• 100% flexion prevention contractures <strong>of</strong> plantarhospital-acquired hPUsflexion contractures• 100% prevention <strong>of</strong> plantarflexion contracturesChange Change in <strong>Heel</strong>/Patient in Status StatushPUs hPUsPFCsFinancial Benefits <strong>of</strong> hPU <strong>Prevention</strong>PFCs[Avg census 260; 7.3%4 may develop PUs = 19; 28%4 may develop hPUs = 5; total hPU days (365) = 1825;avg LOS 4.6 (NIS [Avg Data) census = 397260; actual 7.3%4 hPU days; may 93% develop stage PUs 1 or = 2 419; = 369; 28%4 7% may stage develop 3 or 4 4 = hPUs 28]5; total hPU days (365) = 1825;avg LOS 4.6 (NIS Data) = 397 actual hPU days; 93% stage 1 or 2 4 = 369; 7% stage 3 or 4 4 = 28]4 Whittington KT, Briones R. Adv Skin Wound Care. 2004;17:490-494;9 Young ZF, Evans 4 Whittington A, Davis J. KT, J Nurs Briones Adm. 2003;33:380-383.R. Adv Skin Wound Care. 2004;17:490-494;9 Young ZF, Evans A, Davis J. J Nurs Adm. 2003;33:380-383.ReferencesReferences[Avg census 260; 7.3%4 may develop PUs = 19; 28%4 may develop hPUs = 5; total hPU days (365) = 1825;avg LOS 4.6 (NIS Data) = 397 actual hPU days; 93% stage 1 or 2 4 = 369; 7% stage 3 or 4 4 = 28]4 Whittington KT, Briones R. Adv Skin Wound Care. 2004;17:490-494;9 Young ZF, Evans A, Davis J. J Nurs Adm. 2003;33:380-383.<strong>Heel</strong> PUs are the second most common pressure ulcer in the<strong>Heel</strong> PUs are the second most common pressure ulcer in theclinical setting,clinical 5 <strong>and</strong> cansetting, 5 result in serious complications such<strong>and</strong> can result in serious complications suchas osteomyelitis, cellulitis, septicemia, <strong>and</strong> limb amputation.as osteomyelitis, cellulitis, septicemia, <strong>and</strong> limb 6Septicemia is reported as the cause <strong>of</strong> death in 40% <strong>of</strong> pressureamputation. 6ulcer patients, Septicemia according is reported to national as multiple the cause cause-coded <strong>of</strong> death in death 40% <strong>of</strong> pressurerecords. 7 ulcer Fortunately, patients, with according appropriate to national preventative multiple measures, cause-coded hPUs deathcan be prevented, records. 78 Fortunately, <strong>and</strong> the clinical with implications appropriate <strong>of</strong> preventative a successful measures, hPUsprevention can protocol be prevented, for hPUs 8 in <strong>and</strong> high-risk the clinical sedated implications patients can <strong>of</strong> result a successfulin the following: prevention protocol for hPUs in high-risk sedated patients can resultin the following:Decreased morbidity <strong>and</strong> mortality related to hPU<strong>Prevention</strong> Decreased <strong>of</strong> possible morbidity pain <strong>and</strong> <strong>and</strong> discomfort mortality related related to hPUs to hPUPotential <strong>Prevention</strong> for indirect <strong>of</strong> cost possible savings pain (decreased <strong>and</strong> discomfort length <strong>of</strong> stay, related to hPUssavings on Potential cost <strong>of</strong> treatment, for indirect decreased cost savings nursing (decreased staff time, length etc.) <strong>of</strong> stay,<strong>Prevention</strong> savings <strong>of</strong> a hospital-acquired on cost <strong>of</strong> treatment, condition decreased nursing staff time, etc.)<strong>Prevention</strong> <strong>of</strong> a hospital-acquired condition<strong>Heel</strong> PUs are the second most common pressure ulcer in theclinical setting, 5 <strong>and</strong> can result in serious complications suchas osteomyelitis, cellulitis, septicemia, <strong>and</strong> limb amputation. 6Septicemia is reported as the cause <strong>of</strong> death in 40% <strong>of</strong> pressureulcer patients, according to national multiple cause-coded deathrecords. 7 Fortunately, with appropriate preventative measures, hPUscan be prevented, 8 <strong>and</strong> the clinical implications <strong>of</strong> a successfulprevention protocol for hPUs in high-risk sedated patients can resultin the following:Decreased morbidity <strong>and</strong> mortality related to hPU<strong>Prevention</strong> <strong>of</strong> possible pain <strong>and</strong> discomfort related to hPUsPotential for indirect cost savings (decreased length <strong>of</strong> stay,savings on cost <strong>of</strong> treatment, decreased nursing staff time, etc.)<strong>Prevention</strong> <strong>of</strong> a hospital-acquired conditionCentral nervous system disease or injury, <strong>and</strong>/or spinal corddisease or injury can lead to PFC. 9-11 Damage to the peronealnerve, myopathy Central nervous due to critical system illness, disease or immobility or injury, which <strong>and</strong>/or results spinal cordin shortening disease <strong>of</strong> the or Achilles injury can tendon lead (foot to PFC. drop 9-11 due Damage to contracture) to the peronealare all etiologic nerve, myopathy factors which due can to contribute critical illness, to PFCs. or immobility Risk factors which resultsfor PFCs include shortening pharmacologic <strong>of</strong> the Achilles sedation tendon or paralysis, (foot drop coma, due leg to contracture)weakness, are <strong>and</strong>/or all etiologic heavy <strong>and</strong> factors tight which bed linens can contribute which hold to the PFCs. foot in Risk factorsprolonged for plantar PFCs include flexion (extension). pharmacologic Physical sedation therapy or can paralysis, reverse coma, legtendon contracture, weakness, but <strong>and</strong>/or prevention heavy is <strong>and</strong> preferable tight bed as linens PFCs can which become hold the foot inpermanent prolonged deformities. plantar Clinical flexion implications (extension). <strong>of</strong> a Physical successful therapy PFC can reversepreventiontendonprotocolcontracture,include:but prevention is preferable as PFCs can becomeImproved permanent quality <strong>of</strong> deformities. life Clinical implications <strong>of</strong> a successful PFC<strong>Prevention</strong> prevention <strong>of</strong> potentially protocol permanent include: deformitiesPotential Improved for indirect quality cost savings <strong>of</strong> life (decreased length <strong>of</strong> stay,savings on<strong>Prevention</strong>rehabilitation<strong>of</strong> potentiallycosts for PFC,permanentetc.)deformities<strong>Prevention</strong> <strong>of</strong> a hospital-acquired conditionPotential for indirect cost savings (decreased length <strong>of</strong> stay,savings on rehabilitation costs for PFC, etc.)Central nervous system disease or injury, <strong>and</strong>/or spinal corddisease or injury can lead to PFC. 9-11 Damage to the peronealnerve, myopathy due to critical illness, or immobility which resultsin shortening <strong>of</strong> the Achilles tendon (foot drop due to contracture)are all etiologic factors which can contribute to PFCs. Risk factorsfor PFCs include pharmacologic sedation or paralysis, coma, legweakness, <strong>and</strong>/or heavy <strong>and</strong> tight bed linens which hold the foot inprolonged plantar flexion (extension). Physical therapy can reversetendon contracture, but prevention is preferable as PFCs can becomepermanent deformities. Clinical implications <strong>of</strong> a successful PFCprevention protocol include:Improved quality <strong>of</strong> life<strong>Prevention</strong> <strong>of</strong> potentially permanent deformitiesPotential for indirect cost savings (decreased length <strong>of</strong> stay,savings on rehabilitation costs for PFC, etc.)<strong>Prevention</strong> <strong>of</strong> a hospital-acquired condition1. Keller BP, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: a review 5. Whittington KT, Briones R. National prevalence <strong>and</strong> incidence study: 6-year sequential acute care data. 9. Hoppenfeld S. (1976). Physical Examination <strong>of</strong> the Spine <strong>and</strong> Extremities. Norwalk, CT:Prentice-Hall;1976.<strong>of</strong> risks <strong>and</strong> prevention. Intensive Care Med. 2002;28:1379-1388.Adv Skin Wound Care. 2004;17:490-494.10. Kap<strong>and</strong>ji IA. Ilustrated Physiology <strong>of</strong> Joints. Med Biol Illus. 1964;14:72-81.2. Khan J, 1. Harrison Keller TB, Rich BP, Wille MM, et J, al: van Early Ramshorst development B, van <strong>of</strong> critical der Werken illness myopathy C. Pressure <strong>and</strong> neuropathy ulcers in intensive care 6. patients: Tourtual a review DM, Riesenbert 5. LA, Korutz Whittington CJ, et al. Predictors KT, Briones <strong>of</strong> hospital R. National acquired prevalence pressure <strong>and</strong> ulcers. incidence Ostomy/ study: 6-year 11. sequential Kendall FP, acute McCreary care EK, data. Provance PG, et 9. al. Muscles: Hoppenfeld Testing S. <strong>and</strong> (1976). Function Physical with Posture Examination <strong>and</strong> Pain. <strong>of</strong> 5th the Spine <strong>and</strong> Extremities. Norwalk, CT:Prentice-Hall;1976.patients with severe sepsis. Neurology. 2006; 67:1421–1425.Wound Manage. 1997;43(9):24-40.<strong>of</strong> risks <strong>and</strong> prevention. Intensive Care Med. 2002;28:1379-1388.Adv Skin Wound Care. 2004;17:490-494.ed. Baltimore, MD:Lippincott Williams <strong>and</strong> Wilkens;2005.<strong>Prevention</strong> <strong>of</strong> a hospital-acquired 10. Kap<strong>and</strong>ji IA. Ilustrated Physiology <strong>of</strong> Joints. Med conditionBiol Illus. 1964;14:72-81.3. Miller R. Morphology. Miller’s Anesthesia, 6th ed. Orl<strong>and</strong>o, FL:Churchill-Livingstone;2005.7 . L<strong>and</strong>i F, Onder G, Russo A, Bernabei R. Pressure ulcer <strong>and</strong> mortality in frail elderly people living in2. Khan J, Harrison TB, Rich MM, et al: Early development <strong>of</strong> critical illness myopathy <strong>and</strong> neuropathy in6. Tourtual DM, Riesenbert LA, Korutz CJ, et al. Predictors <strong>of</strong> hospital acquired pressure ulcers. Ostomy/4. Centers for Medicare <strong>and</strong> Medicaid Services. Federal Register Part II 42 CFR Parts 411, 412, 413, <strong>and</strong>community. Arch Gerontol Geriatr. 2007;44 Suppl 1:217-223.11. Kendall FP, McCreary EK, Provance PG, et al. Muscles: Testing <strong>and</strong> Function with Posture <strong>and</strong> Pain. 5thpatients with severe sepsis. Neurology. 2006; 67:1421–1425.Wound Manage. 1997;43(9):24-40.489: Changes to the Hospital ReferencesInpatient Prospective Payment Systems <strong>and</strong> Fiscal Year 2008 Rates; Final 8. Wong VK, Stolis NA. Physiology <strong>and</strong> prevention <strong>of</strong> heel ulcers: the state <strong>of</strong> science. J Wound Ostomyed. Baltimore, MD:Lippincott Williams <strong>and</strong> Wilkens;2005.Rule. Federal 3. Register. Miller R. 2007;72(162):47201-47205.Morphology. Miller’s Anesthesia, 6th ed. Orl<strong>and</strong>o, FL:Churchill-Livingstone;2005. Continence Nurse. 2003;30:191-198. 7 . L<strong>and</strong>i F, Onder G, Russo A, Bernabei R. Pressure ulcer <strong>and</strong> mortality in frail elderly people living in4. Centers for Medicare <strong>and</strong> Medicaid Services. Federal Register Part II 42 CFR Parts 411, 412, 413, <strong>and</strong>community. Arch Gerontol Geriatr. 2007;44 Suppl 1:217-223.489: Changes1. Kellerto theBP,HospitalWille J,Inpatientvan RamshorstProspectiveB, vanPaymentder WerkenSystemsC.<strong>and</strong>PressureFiscal Yearulcers2008in intensiveRates; Finalcare patients:8.a reviewWong VK, Stolis5.NA. PhysiologyWhittington<strong>and</strong>KT,preventionBriones<strong>of</strong>R.heelNationalulcers:prevalencethe state <strong>of</strong><strong>and</strong>science.incidenceJ Woundstudy:Ostomy6-year sequential acute care data.Rule. Federal <strong>of</strong> Register. risks <strong>and</strong> 2007;72(162):47201-47205.prevention. Intensive Care Med. 2002;28:1379-1388.Continence Nurse. 2003;30:191-198.Adv Skin Wound Care. 2004;17:490-494.10. Kap<strong>and</strong>ji IA. Ilustrated Physiology <strong>of</strong> Joints. Med Biol Illus. 1964;14:72-81.2. Khan J, Harrison TB, Rich MM, et al: Early development <strong>of</strong> critical illness myopathy <strong>and</strong> neuropathy in6. Tourtual DM, Riesenbert LA, Korutz CJ, et al. Predictors <strong>of</strong> hospital acquired pressure ulcers. Ostomy/patients with severe sepsis. Neurology. 2006; 67:1421–1425.Wound Manage. 1997;43(9):24-40.3. Miller R. Morphology. Miller’s Anesthesia, 6th ed. Orl<strong>and</strong>o, FL:Churchill-Livingstone;2005.7 . L<strong>and</strong>i F, Onder G, Russo A, Bernabei R. Pressure ulcer <strong>and</strong> mortality in frail elderly people living incommunity. Arch Gerontol Geriatr. 2007;44 Suppl 1:217-223.9. Hoppenfeld S. (1976). Physical Examination <strong>of</strong> the Spine <strong>and</strong> Extremities. Norwalk, CT:Prentice-Hall;1976.11. Kendall FP, McCreary EK, Provance PG, et al. Muscles: Testing <strong>and</strong> Function with Posture <strong>and</strong> Pain. 5thed. Baltimore, MD:Lippincott Williams <strong>and</strong> Wilkens;2005.