best practice for the management of lymphoedema ... - EWMA
best practice for the management of lymphoedema ... - EWMA
best practice for the management of lymphoedema ... - EWMA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ASSESSMENT<br />
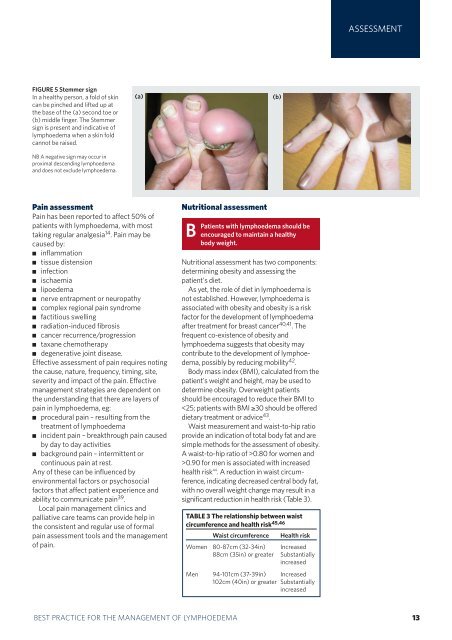
FIGURE 5 Stemmer sign<br />
In a healthy person, a fold <strong>of</strong> skin<br />
can be pinched and lifted up at<br />
<strong>the</strong> base <strong>of</strong> <strong>the</strong> (a) second toe or<br />
(b) middle finger. The Stemmer<br />
sign is present and indicative <strong>of</strong><br />
<strong>lymphoedema</strong> when a skin fold<br />
cannot be raised.<br />
NB A negative sign may occur in<br />
proximal descending <strong>lymphoedema</strong><br />
and does not exclude <strong>lymphoedema</strong>.<br />
(a)<br />
Pain assessment<br />
Pain has been reported to affect 50% <strong>of</strong><br />
patients with <strong>lymphoedema</strong>, with most<br />
taking regular analgesia 14 . Pain may be<br />
caused by:<br />
■ inflammation<br />
■ tissue distension<br />
■ infection<br />
■ ischaemia<br />
■ lipoedema<br />
■ nerve entrapment or neuropathy<br />
■ complex regional pain syndrome<br />
■ factitious swelling<br />
■ radiation-induced fibrosis<br />
■ cancer recurrence/progression<br />
■ taxane chemo<strong>the</strong>rapy<br />
■ degenerative joint disease.<br />
Effective assessment <strong>of</strong> pain requires noting<br />
<strong>the</strong> cause, nature, frequency, timing, site,<br />
severity and impact <strong>of</strong> <strong>the</strong> pain. Effective<br />
<strong>management</strong> strategies are dependent on<br />
<strong>the</strong> understanding that <strong>the</strong>re are layers <strong>of</strong><br />
pain in <strong>lymphoedema</strong>, eg:<br />
■ procedural pain – resulting from <strong>the</strong><br />
treatment <strong>of</strong> <strong>lymphoedema</strong><br />
■ incident pain – breakthrough pain caused<br />
by day to day activities<br />
■ background pain – intermittent or<br />
continuous pain at rest.<br />
Any <strong>of</strong> <strong>the</strong>se can be influenced by<br />
environmental factors or psychosocial<br />
factors that affect patient experience and<br />
ability to communicate pain 39 .<br />
Local pain <strong>management</strong> clinics and<br />
palliative care teams can provide help in<br />
<strong>the</strong> consistent and regular use <strong>of</strong> <strong>for</strong>mal<br />
pain assessment tools and <strong>the</strong> <strong>management</strong><br />
<strong>of</strong> pain.<br />
Nutritional assessment<br />
B Patients<br />
with <strong>lymphoedema</strong> should be<br />
encouraged to maintain a healthy<br />
body weight.<br />
Nutritional assessment has two components:<br />
determining obesity and assessing <strong>the</strong><br />
patient's diet.<br />
As yet, <strong>the</strong> role <strong>of</strong> diet in <strong>lymphoedema</strong> is<br />
not established. However, <strong>lymphoedema</strong> is<br />
associated with obesity and obesity is a risk<br />
factor <strong>for</strong> <strong>the</strong> development <strong>of</strong> <strong>lymphoedema</strong><br />
after treatment <strong>for</strong> breast cancer 40,41 . The<br />
frequent co-existence <strong>of</strong> obesity and<br />
<strong>lymphoedema</strong> suggests that obesity may<br />
contribute to <strong>the</strong> development <strong>of</strong> <strong>lymphoedema</strong>,<br />
possibly by reducing mobility 42 .<br />
Body mass index (BMI), calculated from <strong>the</strong><br />
patient's weight and height, may be used to<br />
determine obesity. Overweight patients<br />
should be encouraged to reduce <strong>the</strong>ir BMI to<br />
0.80 <strong>for</strong> women and<br />
>0.90 <strong>for</strong> men is associated with increased<br />
health risk 44 . A reduction in waist circumference,<br />
indicating decreased central body fat,<br />
with no overall weight change may result in a<br />
significant reduction in health risk (Table 3).<br />
TABLE 3 The relationship between waist<br />
circumference and health risk45,46 Waist circumference Health risk<br />
Women 80-87cm (32-34in) Increased<br />
88cm (35in) or greater Substantially<br />
increased<br />
Men 94-101cm (37-39in) Increased<br />
102cm (40in) or greater Substantially<br />
increased<br />
ASSESSMENT<br />
BEST PRACTICE FOR THE MANAGEMENT OF LYMPHOEDEMA 13<br />
(b)