Georgia ems patient care report 2000 pcr scan - NHTSA
Georgia ems patient care report 2000 pcr scan - NHTSA
Georgia ems patient care report 2000 pcr scan - NHTSA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
GEORGIA EMS PATIENT CAREREPORT <strong>2000</strong>PCR SCAN SHEETINSTRUCTION BOOK1
PCRs are to be completed for each response made by a licensedvehicle (ambulance, first responder unit, neonatal transport unit, etc.)even if the <strong>patient</strong> is not transported, it was a false call, no <strong>patient</strong> foundor call was cancelled. On round-trip calls (from point A to point B andback to point A) the local service may decide whether one or two <strong>report</strong>swill be completed for the response. If only one <strong>report</strong> is completed, thetime of completion of the entire round trip is to be entered in the “InService” time area. On calls that have two destinations, one of which is abrief stop (such as from a nursing home to the doctor’s office and then tothe hospital) point A to point B to point C, only one <strong>report</strong> is necessary.FREQUENTLY ASKED QUESTIONSDo I use a pen or a pencil to fill out the <strong>report</strong>?Use ink (blue or black only) to enter your information on page 2. You can use ink (blueor black) on page 1, the <strong>scan</strong> part. A gel medium ink pen may be best.. Do not useerasable ink on either copy.Do I “X” in my choices in the boxes?NO! You must blacken in the appropriate boxes. Try to stay within the box and fill itascompletely as possible. Do not put an “x” or “check mark” in the box.If a section is “Not Applicable” should I mark “N/A” in that section?NO! Do not make any marks other than those called for by your <strong>patient</strong> information.“N/A” or a line through a section will give false data.2
FREQUENTLY ASKED QUESTIONS-CONTINUEDWhat if I make a mistake on the form?The local service should establish a policy on how to handle mistakes on the<strong>scan</strong> form. You may correct the top copy of page one with a white pigmentmarker (not “white out”) and then correct the copies of the <strong>scan</strong> sheet. Theproper method on the page 2 narrative section is to mark a line through theerror and write the word “error” above the mistake along with the date andyour initials.What if there is not enough space on page 2 in the “narrative” and “vitalsigns” sections to finish my documentation? What should I do?Use a supplemental <strong>report</strong>.Will I always have to fill in every section?Fill in ALL that apply to your call. If there is an N/A in a field that is notapplicable to your call please mark that. If there is no N/A and the field is notapplicable to your call you should leave it blank.There’s no Refusal area on either page. How do I do a refusal?The Refusal area on the old PCR was inadequate without extensive backupdocumentation. It is suggested that your service adopts one or have an attorneydraw up a separate Refusal Form. REMEMBER…All Refusals requireadditional documentation to be valid.3
FREQUENTLY ASKED QUESTIONS-CONTINUEDShould I use “leading zeros”?YES! Use “leading zeros” as indicated in the PCR Instruction Booklet.Basically you can use a “leading zero” in any field that has a “zero” in it if thenumbers you need to enter don’t fill up the space provided. The exception tothis might be in the “Miscellaneous” or “Study 1” or “Study 2” areas.I don’t understand some of the abbreviations on the Scan form.All abbreviations except the common or obvious ones are explained later inthis document. If you have further questions contact your Regional EMSoffice.Where do the signatures go?All signatures go on the Narrative page. Receiving nurse and M.D. on the leftand Medics on the right.4
Additional InformationWho gets which copies?The top copy of Page 1, the <strong>scan</strong> page, goes either to your Regional EMSOffice or whoever <strong>scan</strong>s your <strong>report</strong>s for data. This original <strong>scan</strong> copy does notneed a narrative page attachment. The top copy of Page 2, the narrative page,goes to your service for a record of the call along with the third page of the<strong>scan</strong> form and any attachments such as supplemental <strong>report</strong>s or ECG strips. Acopy of the <strong>scan</strong> form, the narrative page, and copies of any attachments go tothe hospital. Do not staple forms submitted to the state.The State of <strong>Georgia</strong> code lists are available online athttps://g<strong>ems</strong>is.dhr.state.ga.us. The lists will be periodically updated.If there is no code or the code is invalid for Agency, Date or UnitResponse Time the <strong>report</strong> will be rejected and not included in the databasebecause it cannot be properly counted as a single unique EMS run.5
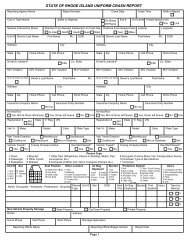
Row 1AGENCY UNIT EMS VIDAGENCY:UNIT:0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9 9 9Enter the agencys state ID number and mark thecorresponding boxes. This number should also be enteredat the top of page 2.Enter the agencys state ID number and mark thecorresponding boxes. This number should also be enteredat the top of page 2.Enter the EMS unit number. If only 2 digits use zero as thefirst digit then mark the corresponding boxes.Enter the EMS agency unit number. If only 1 or 2 digits usezero as the first digits then mark the corresponding boxes.CENSUS TRACT:Enter the Census tract for the location of the call. (If yourcounty is not broken into census tracts then you could useFire Districts as your location codes. Such as in Fire Stations territory your number might be 10200. This will help youtrack the location of your calls.) Then mark the correspondingboxes.EMS VID: Enter the state assigned 5-digit vehicle number.6
Row 1-ContinuedSERV REQ VEH TYPELOCATION TYPESceneGrndHomeRes/InstiUnschedRotorFarmEduca InstiSchedFixedMine/QuarryHospitalStandbyOtherIndustryPhys/ClinicRendezvOtherNoneRecreationStreet/HwyOther911 USED Y NRESPONSE MODEOut In Out In Out InRLSUpdgradeWALK/DRIVENo RLSDwn GradeSERVICEREQUEST:Fill in the appropriate box to describe why you were called.911: Fill in the appropriate box whether 911 was used or not.VEHICLE TYPE:Fill in the appropriate box for the type of vehicle you areusing.LOCATION TYPE: Mark the appropriate box for the location you respond to.RESP. MODE:(Response Mode)Mark the appropriate box for OUT To Scene and IN FromScene RLS=Red lights and siren. Walk-Drive means a<strong>patient</strong> comes to your unit or station. For instance, if you areapproached by a <strong>patient</strong> while you are at a restaurant or ifsomeone comes to your station and requests <strong>care</strong> thesewould be in the Walk-Drive category.7
COUNTYRow 1-ContinuedRESPONSE NUMBER0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9COUNTY:RESPONSERESPONSENUMBER:NUMBER:Enter your county ID number and mark the appropriateboxes.Enter the county ID number where the call originated andmark the appropriate boxes.Enter your county assigned Response or Incident NumberEnter your agency assigned Response or Incident Numberand mark the appropriate boxes. This number should alsoand mark the appropriate boxes. This number should alsobe entered at the top of page 2.be entered at the top of page 2.8
Row 1-ContinuedDRV/MEDIC T MEDIC 1TMEDIC 20 0 0 0 0 0 F 0 0 0 0 0 F 0 0 0 0 01 1 1 1 1 1 E 1 1 1 1 1 E 1 1 1 1 12 2 2 2 2 2 I 2 2 2 2 2 I 2 2 2 2 23 3 3 3 3 3 C 3 3 3 3 3 C 3 3 3 3 34 4 4 4 4 4 P 4 4 4 4 4 P 4 4 4 4 45 5 5 5 5 5 O 5 5 5 5 5 O 5 5 5 5 56 6 6 6 6 6 6 6 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9 9 9 9 9 9 9 9DRV/MEDIC:Enter the Driver/Medics state ID number and mark thecorresponding boxes.T: Mark the level of certification for each crew member.(TRAINING)= First Responder,= Basic EMT,= EMT Intermediate(ALL Ga. EMTs are this level.)= Cardiac Tech= Paramedic= Other, RN, MD, Resp. Therapist, LPN, anything thatdoes not fit. Document exact level in in your narrative.MEDIC 1:MEDIC 2:Enter the primary <strong>care</strong> Medics state county ID number and mark thethe corresponding boxes. boxes. Mark Mark as as appropriate.Enter the the secondary <strong>care</strong> <strong>care</strong> Medics Medics (if county any) state number number and and markmark the corresponding boxes. Mark as appropriate.the corresponding boxes. Mark as appropriate.9
Row 2JANFEBMARAPRMAYJUNJULAUGSEPOCTNOVDECCALL DATED D Y Y0 0 0 01 1 1 12 2 2 23 3 3 34 4 45 5 56 6 67 7 78 8 89 9 9MONTH:Mark the appropriate box to designate the month to go withthe CALL DATE area.CALL DATE:Enter the numeric day of the call and the last two digits ofthe year and mark the corresponding boxes for each.10
Row 2-ContinuedREPORT 911 DISP NOTIFIED UNIT NOTIFIED0 0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9REPORT 911:Enter the time 911 or your dispatch center received thecall from the public and mark the corresponding boxes.DISP. NOTIFIED:Enter the time Dispatch was notified of the call and mark thecorresponding boxes. Note this time may be the same asREPORT 911 time.UNIT NOTIFIED:Enter the time your unit was notified to respond to the calland mark the corresponding boxes.Use 24 hour clock for all times.11
UNIT RESPONSERow 2-ContinuedAT SCENEAT PATIENT0 0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9UNIT UNIT RESPONSE: Enter the the time time your your unit unit responded responded (actually (actually begins beginsmovement) to the to the call call and mark and mark the corresponding the corresponding boxes. boxes.AT SCENE:AT SCENE:AT PATIENT:AT PATIENT:Enter the the time time you you arrived arrived at the at scene the of scene the call of and the mark call and markthe corresponding boxes.boxes.Enter the the time time you you arrived arrived at the at <strong>patient</strong>s the <strong>patient</strong>s side and side mark and the mark thecorresponding boxes. boxes.Use 24 hour clock for all times.12
Row 2-Continued1ST SHCK/EXTRIC ENROUTE DESTINATION IN SERVICE0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 4 4 4 4E 5 5 5 5 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 6 6 6 6D 7 7 7 7 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9 9 9 91 ST 1DEFIB/EXTRIC: ST SHCK/EXTRIC: Enter the time of the first defibrillation, if any, if any, or when or whenextrication was completed, if if any, any, and and mark mark the thecorresponding boxes. Please note note the the 1 st Defib 1 st Defib time time may maybe be before your arrival. ALSO mark mark the the if it if is it anis anextrication time or or the the if if it it is is a defibrillation a defibrillation time. time.Leave this area blank if it is not applicable.Leave this area blank if it is not applicable.ENROUTE:DESTINATION:IN IN SERVICE: SERVICE:Enter the time time you you go go enroute enroute to your to your destination destination and mark and markthe corresponding boxes.the corresponding boxes.Enter the time you you arrive arrive at your at your destination destination and mark and mark the thecorresponding boxes. boxes.Enter Enter the the time time you you are are available available for your for your next next call and call mark and markthe corresponding boxes. boxes.Use 24 hour clock for all times.13
Row 3GENDER JanDOBMALE M Feb D D Y YFEMALE F Mar 0 0 0 0Unkwn U Apr 1 1 1 1RACE May 2 2 2 2Afr Am Jun 3 3 3 3Asian Jul 4 4 4Cauc Aug cent 5 5 5Hispan Sep 18 6 6 6NatAm Oct 19 7 7 7Other Nov 20 8 8 8Unkn Dec 9 9 9GENDER:RACE:Mark the appropriate box for your <strong>patient</strong>s gender. The is for the <strong>patient</strong> who is so disfigured that the genderis unidentifiable.Mark the appropriate box for the <strong>patient</strong>s race.The next date fields are for the <strong>patient</strong>s age. Mark the appropriate Month.DAY:CENT.:(CENTURY)YEAR:Enter the day of the month the <strong>patient</strong> was born andmark the corresponding boxes.This area is for the Century of the <strong>patient</strong>s birth.18 is for 1800s, 19 is for the 1900s and ofcourse 20 is for <strong>2000</strong>s. Mark the right box.Enter the last 2 digits of the <strong>patient</strong>s year of birthand mark the corresponding boxes.14
Row 3-ContinuedPATIENT ID NUMBERCLIN AREA0 0 0 0 0 0 0 0 0CARDIACMEDICAL1 1 1 1 1 1 1 1 1 NEONATE2 2 2 2 2 2 2 2 2 OB/GYN3 3 3 3 3 3 3 3 3 PSYCH4 4 4 4 4 4 4 4 4 TRAUMA5 5 5 5 5 5 5 5 5 TRAUMA6 6 6 6 6 6 6 6 6 TRIAGE7 7 7 7 7 7 7 7 7 PHYSIO8 8 8 8 8 8 8 8 8 ANAT9 9 9 9 9 9 9 9 9 MECHPATIENT ID NUMBER-This field is no longer in use. Agency may use thisfor its own pt identification and use.CLIN. AREA:Mark the appropriate box to indicate the Clinical Area ofthe <strong>patient</strong>s primary problem. Mark only one.TRAUMA TRIAGE: Mark the appropriate box. See the explanation of theTrauma Triage Criteria on the next pages.15
Prehospital Trauma TriagePrehospital management of the injured <strong>patient</strong> consists of assessment,extrication, initiation of resuscitation, and rapid transportation to theclosest appropriate facility. Early identification of the injured <strong>patient</strong>sthat would most likely benefit from a trauma center is important.Prehospital Trauma Triage criteria provides for objective andconsistent field identification of major trauma according to theguidelines by the American College of Surgeons Committee onTrauma (Resources for Optimal Care of the Injured Patient: 1999).The use of consistent criteria with injured <strong>patient</strong>s detects physiologicparameters, identifies specific anatomic injuries and considers themechanism of forces that could lead to severe injury. The use of thesecriteria may guide destination decisions, protocols, and <strong>care</strong> at thereceiving facility. Additionally, the use of consistent criteria buildstrust relationships between prehospital and hospital providers since thesame language is being used and strong professional relationships leadto better <strong>patient</strong> outcomes.As <strong>patient</strong> <strong>report</strong>s are called in to medical control and /or receivingfacilities, use the criteria as part of <strong>report</strong>. For example, “…2 <strong>patient</strong>sfrom a motor vehicle crash – 1 that meets physiologic criteria and 1that meets mechanism, high speed” is much more descriptive than “2<strong>patient</strong>s from a motor vehicle crash”. Concise, consistent informationallows the facility to be better prepared to receive the injured <strong>patient</strong>.16
TRAUMA TRIAGE CRITERIAThe 1999 prehospital triage criteria in the Resources for Optimal Care of theInjured Patient are:Physiologic: These are the simplest to perform and provide an accurate basis forfield triage.• Systolic BP
TRAUMA TRIAGE CRITERIAMechanism: Indications that significant forces were applied to the body.• Ejection from automobile• Falls >20 feet (>15 in reality or any ‘significant’ fall)• Rollover• Death in same passenger compartment• Extrication time >20 minutes• Auto/Pedestrian with significant (>5 mph) impact or pedestrian thrown on• run over• Auto/Bicycle with significant (>5 mph) impact• Motorcycle crash >20 mph or with separation of rider from bike• High speed motor vehicle crash with initial speed >40 mph or major• deformity of >20 inches or passenger compartment intrusion of >12 inchesDocumentation of the criteria on the Patient Care Report is important becauseit allows tracking of specific injuries or mechanisms and can be utilized bytraining departments to identify training needs or opportunities forimprovement. At a regional or state level, documentation of prehospitalcriteria will provide “hard data” as to the number and severity of major trauma<strong>patient</strong>s. This may be useful for services and communities applying for grantsand funding and is invaluable for epidemiological purposes.18
TRAUMA TRIAGE CRITERIA GUIDELINES1. PHYSIOLOGIC CRITERIA:A. Systolic BP < 90 (no radial pulses)B. GCS 29 or respiratory compromise or impendingcompromise.YES♦ Transport to Trauma Center if available.♦ Notify hospital of Physiologic Criteria assoon as possible.♦ Mark Physiologic Criteria on PCR2. ANATOMIC CRITERIA:A. Penetrating wound to the head, torso or long bones.B. Flail chest.C. Pelvic fracture.D. Two or more proximal long bone fractures.E. Paralysis (related to current event)F. Amputations (excluding fingers and toes)G. Combination trauma with burnsH. Open and depressed skull fractures.YES♦ Transport to Trauma Center if available.♦ Notify Hospital of Anatomic Criteria assoon as possible.♦ Mark Anatomic Criteria on PCR.3. MECHANISM CRITERIA:A. Ejection from automobileB. Death in same passenger compartmentC. Extrication time > 20 minutes.D. Falls > 15 feetE. RolloverF. High speed MVC: initial speed > 40 mph or major auto deformity > 20 inches or intrusion intopassenger compartment > 12 inches.G. Auto pedestrian/ auto bicycle injury with impact > 5 mph.H. Pedestrian thrown or run over.I. Motorcycle crash > 20 mph or with separation of rider from bike.YES♦ Transport to Trauma Center if available.♦ Notify Hospital of Mechanism Criteria assoon as possible.♦ Mark Mechanism Criteria on PCR.19
Row 3-ContinuedAcc HitAircraftAssaultBicycleBiteChem-ExpCold ExDrwningElectricFallFall ObjCAUSE OF INJURYFireGSW-AccGSW-asltGSW-selfHeat ExLghtningMachineMcycleMVCOff RoadOtherPedestRadiationRapeRx ODSmokeStabbingStingsSuffocatUnknownWatercftCAUSE OF INJURY: Mark the appropriate boxes. More than one box can bemarked. Listed below are the explanations for theabbreviations in this area.Acc. Hit=Accidently hit bysomething or someone.Fire=Injured by fire Pedest=Pedestrianstruck by a vehicle.Aircraft=Any type aircraft GSW-acc=AccidentalGSWRadiation=Radiationexposure.Assault=Physically GSW-aslt=GSW by Rape=Physical rape.assaulted by another. assault.Bicycle=Injured on bicycle GSW-self=Self inflicted Rx OD=Drug overdose.GSW.Bite=Human or animal Heat Ex=Heat exposure Smoke=SmokeinhalationChem Ex=Chemical Lghtning=Struck by Stabbing=Stabbedexposurelightning.Cold Exp.=Cold exposure Machine=Injured bymachinery.Stings=Bee, Wasp, JellyFish, etc.Drwning=Drowning or Mcycle=Injured on a Suffocat=Suffocationnear drowning.motorcycle.Electric=Injured by MVC=Injured in a motor Unknown=Unknownelectric shock.Fall=Injured in a fall.Fall Obj.=Injured by afalling object.vehicle crash.Off Road=Injured ridingan Off Road Vehicle.Other=Fits no otherinjury cause category.cause of injury.Watercrft=Injured on aboat or jet ski.20
Row 3-ContinuedAbd PainAir ObstAllergicAlt LOCApp DeathBack PainBleedingBurn/OtherBurn/ThermCard ArrChokingPROVIDER IMPRESSIONS/SIGNS AND SYMPTOMSChst PainCrush InjDiarrheaDizzinessDysrhythmEar PainEye PainFeverGI BleedHeadacheHyperglycHypertenHyperthermHypoglycHypothermHypovolemInhalationRash/BlisterN/VOB DelivPalpitationParalysisPoisoningPsychResp ArrResp DistSeizuresSex AsltStrokeSyncopeUnresponVag BleedWeaknessPROVIDER IMPRESSIONS/SIGNS AND SYMPTOMS:Mark your impressions and/orthe <strong>patient</strong>s Signs andSymptoms.More than one box can bemarked.The explanations of theabbreviations in this area areto the right.ABD Pn=Abdominal painAir Obst.=AirwayObstructionAllergic=Allergicor AnaphylacticAlt LOC=AlteredLevel ofConsciousnessApp DeathChst Pain=ChestPain.Crush Inj.DiarrheaDizzinessDysrhythm=Abnormal heartrhythmHyperten=HBPHypertherm=HyperthermiaHypoglyc=LowBlood Sugar.Hypotherm=HypothermiaHypovolem=HypovolemiaPoisoningPsychResp Arr.=RespArrest.Resp Dist=Respiratorydistress.SeizuresBack Pain Ear Pain Inhalation Sex Aslt=SexualAssaultBleeding Eye Pain Rash/Blister StrokeBurn-Other Fever N/V=Nausea and SyncopevomitingBurn/Therm= GI Bleed OB Deliv Unrespon.Thermal BurnCard Arr Headache Palpitations Vag. BleedChoking Hyperglyc=HighBlood Sugar.Paralysis Weakness21
Row 4SAFETY EQUIPNot UsedShoulderLap OnlyLap/ShldrChild SeatAirbag DepHelmetEye ProtFloat DevProt ClothUnkwnFACTORSWeatherRoad CondVeh ProbUnsafe ScnLanguageExt> 20Haz MatCrowdOtherN/AHeadFaceNeckThoraxAbdomenBackPelvisU ExtremL ExtremAMPTINJURY SITE & TYPEBURNDFXGSWLACPAINPUNCSOFTSAFETY EQUIP:FACTORS:INJURY SITE& TYPEThis is for safety equipment used by the <strong>patient</strong>.Mark theappropriate box. Use N/A if not applicable.This is for Factors affecting the call. Mark the appropriateboxes. Use N/A if not applicable.Mark all appropriate boxes. NOTE: DFX Means:Dislocation/Fracture.22
Row 4-ContinuedPULSE RESP SYS B/P DIAS B/PPULSE:RESP:SYS B/P:DIAS B/P:0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 34 4 4 4 P 4 4 4 45 5 5 5 A 5 5 5 56 6 6 6 L 6 6 6 67 7 7 7 P 7 7 7 78 8 8 8 8 8 8 89 9 9 9 9 9 9 9Mark the appropriate boxes. USE LEADING ZEROS.For example for a pulse of 80 mark 0-8-0. PLEASENOTETHIS IS FOR THE ACTUAL PALPATED PULSERATE, NOT THE READING ON THE PULSE OX.Mark the appropriate boxes. USE LEADING ZEROS IFNEEDED.Mark the appropriate boxes. USE LEADING ZEROS IFNEEDED. Mark PALP if appropriate.Mark the appropriate boxes. USE LEADING ZEROS IFNEEDED. If B/P is palpated leave blank.23
Row 4-ContinuedPULSE OX Resp GLASCOW COMA SCOREEffort EYEMOTOR0 0 0 N Spontan 4 Obedient 61 1 1 L To Voice 3 Localize 52 2 S To Pain 2 Withdrwl 43 3 A None 1 Flexion 3RA4 4 Skin VERBAL Extension 25 5 Perf Oriented 5 None 16 6 N Confused 4O2 7 7 D Inapprop 3 GCS Total8 8 Incompre 29 9 None 1TREATMENT AUTH. BYStand OrdOn-lineOn-sceneWrittenCLINICAL COURSEImprovMaintainDeteriorExpiredPULSE OX:RESP EFFORT:GCS EYE:Mark the appropriate boxes. USE LEADING ZEROS IFNEEDED. Mark R/A if initial O2 saturation is on Room AirMark O2 if initial saturation is with the <strong>patient</strong> on oxygen.= Normal, = Labored, = Shallow, = Absent.Mark the appropriate box.Mark the appropriate boxGCS VERBAL:GCS MOTOR:SKIN PERF:Mark the appropriate box.Mark the appropriate box. Add EYE, VERBAL and MOTORFor GCS TOTAL.Mark the appropriate box.TREAT AUTH BY: Mark the appropriate box. (If by Protocol mark StandingOrder.)CLINICAL COURSE:What happened to the <strong>patient</strong> while in your <strong>care</strong>?24
Row 5ENV. CAUSEAbuseAlcoholHousingNeglectNutritionSubstanceN/AUnintentIntent-selfIntent-otherINJURY INTENTUnknownN/AENV. CAUSE: This is for identifying an environmental cause thatcontributed to the <strong>patient</strong>s present condition. You should make an objectiveobservation and back it up in your narrative. Mark the appropriate box. Use N/Aif not applicable.INJURY INTENT:Choices are: Intent-self=Intentional by self,Intent-oth=Intentional by another person,Unintent=Unintentional by any means,Unknown and N/A. Mark the appropriate box.SinusS. BradyS.TachRHYTHMI D Narrow Complex Tach I D Vtach I D PEA I D 2nd Deg Type 2 I DI D Wide Complex Tach I D Vfib I D Atrial Fib I D 3rd Deg Block I DI D PVC,PAC,PJC I D Asystole I D 2nd Deg Type 1 I D Paced I DRHYTHM:Mark ONE box to indicate the <strong>patient</strong>s initial rhythm.Mark initial rhythm in the box.Mark ONE box to indicate the <strong>patient</strong>s rhythm whenarriving at your destination. Mark destination rhythm in the box.25
Row 6CARE RENDERED MEDIC PROCEDURE MEDIC ATTEMPT SUCCESS12 Lead EKG D 1 2 AED D 1 2 1 2 3 Y NAssist Delivery D 1 2 Sync Cardvrt D 1 2 1 2 3 Y NAuto Ventilation D 1 2 Manual Defib D 1 2 1 2 3 Y NBag-Valve-Mask D 1 2 Chest Decomp D 1 2 1 2 3 Y NBleed Control D 1 2 Oral/Nas Airway D 1 2 1 2 3 Y NCardiac Monitor D 1 2 Combitube D 1 2 1 2 3 Y NCPRD 1 2 ET/NT Intub D 1 2 1 2 3 Y NC-Spine Mgmt D 1 2 Intraosseous D 1 2 1 2 3 Y NGlucose Monitor D 1 2 IV #1 D 1 2 1 2 3 Y NMASTD 1 2 IV #2 D 1 2 1 2 3 Y NOxygen D 1 2 IV #3 D 1 2 1 2 3 Y NSplintsD 1 2 Needle Cric D 1 2 1 2 3 Y NSuctionD 1 2 Pacing D 1 2 1 2 3 Y NTraction Splint D 1 2 Vagal Manvr D 1 2 1 2 3 Y NCARE RENDERED:PROCEDURE:Mark all appropriate boxes under medic by whorendered the <strong>care</strong>. = Drv/Medic, = Medic 1, = Medic 2.Mark all appropriate boxes under Medic.ATTEMPT:SUCC:(SUCCESSFUL)Mark the single appropriate number per procedure. Mark all that areapplicable.Mark or for successful or unsuccessful procedure.26
Row 6-ContinuedMED 1 MED 2 MED 3 MED 4 MED 5 MED 6 MED 70 0 0 0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9 9 9 9 9 9ROSCY N N/AMED 1-MED 7:Fill in the proper code for each med given and mark thecorresponding boxes to match. Medication codes are listed in theeducation book. If you use a medication not included in the list usecode 99 and explain in your narrative. Use the proper area onthe Narrative Page to list your medications by name, dose,route, time, and who gave the medication. PLEASE NOTETHERE ARE EXTRA BLANK CODES ON THE MEDICATIONLIST FOR MEDS THAT MIGHT BE SPECIFIC TO YOUR EMSSERVICE. YOUR SERVICE SHOULD DEFINE THE CODE FORTHESE MEDS.ROSC:Return Of Spontaneous Circulation. Mark the box to indicate thereturn of a pulse, or the box to indicate no return of a pulse in thecardiac arrest <strong>patient</strong>. Mark N/A if not applicable.27
DEST CODERow 6-ContinuedMILES OUTMILES IN0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8PRE-EXISTINGAsthmaDiabetesTuberculosisEmphysemaChronic RenalCardiacHypertensionMR/Dev DelayPremature BabyPsychiatric9 9 9 9 9 9 9 9 9 Seizure DisorderTracheostomyTraumatic Brain Inj.DEST.:Enter the Destination/Hospital number here and mark the correspondingboxes.MILES OUT:Write in the appropriate number of miles to the scene and mark thecorresponding boxes. Use leading zeros.MILES IN:Write in the appropriate number of miles to your destination and mark thecorresponding boxes. Use leading zeros.PRE-EXISTING: Mark the appropriate box to indicate a pre-existing condition or pertinentmedical history. More than one box can be marked. NOTE: M/R Dev. Delay means MentalRetardation with developmental delay. You also need to list these and other history onthe Narrative Page in the Past Medical Hx area.28
INCIDENT/PATIENT DISPOSITIONCancelledTreated, TransportedNo Patient Found Treated, Xfer CareFalse CallTreated, POVRefused AllTreated, ReleasedAssist at Home Treated, Refused TransportDead at SceneNo Treat RequiredRow 7Transport OnlyN/AINCIDENT/PATIENT DISPOSITION: Mark the appropriate box to indicate what happened on theincident and /or to the <strong>patient</strong>.Cancelled=Cancelled prior to arrival orcancelled on the scene.No Patient Found=No <strong>patient</strong> on thescene.False Call=Bogus call or false alarmRefused All=Patient refuses all EMStreatment and transport.Assist at home=Assist a <strong>patient</strong> to bedor do home <strong>care</strong>, etc.Dead at sceneNo Treatment Required=Patientneeds no treatment by EMS.Treated, Transported=Treated andTransported by your unit.Treated, Xfer Care=Treated and transfer <strong>care</strong> toanother unit. For example you turn over your<strong>patient</strong> to a helicopter crew or an ALS unit.Treated, POV=Treated by you but transported byPOV.Treated, Released=Treated and released,transport by EMS is not needed.Treated, Refused Transport=Patient treated butrefuses transport.Transport Only=No treatment given. Such as areturn call to a skilled <strong>care</strong> facility.N/A=Use this category for a standby at a sportsevent or doing Rehab at a fire scene where youdont actually do <strong>patient</strong> <strong>care</strong>.29
DEST CHOICEClosestPt/Fam ChoicePt Phys ChoiceManag CareLaw EnforceProtocolSpecialtyOn-Line MedDiversionTraumaRow 7-ContinuedMISCELLANEOUSSTUDY 1 STUDY 20 0 0 0 0 0 0 0 0 0 0 01 1 1 1 1 1 1 1 1 1 1 12 2 2 2 2 2 2 2 2 2 2 23 3 3 3 3 3 3 3 3 3 3 34 4 4 4 4 4 4 4 4 4 4 45 5 5 5 5 5 5 5 5 5 5 56 6 6 6 6 6 6 6 6 6 6 67 7 7 7 7 7 7 7 7 7 7 78 8 8 8 8 8 8 8 8 8 8 89 9 9 9 9 9 9 9 9 9 9 9DEST. CHOICE:Mark the appropriate box to indicate WHY you transportedthe <strong>patient</strong> to a particular destination.MISCELLANEOUS: This box is to be used and defined by the individual service.Write in and mark as directed by your service.STUDY 1:STUDY 2:This box is for special study data to be designated by the state, region or individualservice.This box is for special study data to be designated by the state, region or individualservice.30
Row 7-ContinuedTECH ASSISTEDHomeVentilatorsCPAPCent IVCahteterPacemakerFeedingCatheterCSF ShuntColostomiesTHIS IS A SECTION SPECIFICALLY DESIGNED ANDREQUESTED BY EMSC. ITS PURPOSE IS TO COLLECTDATA ON CHILDREN WHO HAVE SPECIAL PROBLEMS ANDARE TAKEN CARE OF AT HOME.Home Ventilators:CPAP:Cent. IV Catheter:Pacemaker:MARK ALL AREAS THAT APPLYMark this area for children on home ventilators.Mark this area if your pediatric <strong>patient</strong> is on ContinuousPositive Air Pressure.Mark this area if your pediatric <strong>patient</strong> has a central line.Mark this area if your pediatric <strong>patient</strong> has a pacemaker.Feeding Catheter:Mark this area if your pediatric <strong>patient</strong> has a feedingcatheter.CSF Shunt:Mark this area if your pediatric <strong>patient</strong> has a CerebralSpinal Fluid Shunt.Colostomies:Mark this area if your pediatric <strong>patient</strong> has a colostomy3122
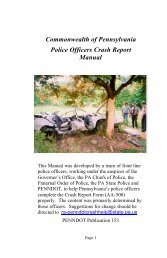
PCR Page 2 OverviewPage 2 of the PCR is for written information only. The top part of the formis designed to supply minimal <strong>patient</strong> information to the hospital and theindividual EMS service. It is not designed to take the place of a billing form.Just below the Patient Information area is a line for Chief Complaint. TheChief Complaint should be the primary problem voiced by the <strong>patient</strong> or bybystanders if the <strong>patient</strong> cant communicate. Your diagnosis of the <strong>patient</strong>scondition does not go on this line. For instance if the <strong>patient</strong> is in cardiac arrestthe chief complaint from the bystanders or family might be unconscious perbystanders or if a qualified first responder is there prior to your arrival it might becardiac arrest per Engine 12 crew. Chief complaint for a motor vehicle crashwill not be MVC but whatever complaint the <strong>patient</strong> expresses to you such asMy neck hurts. Or Neck pain.The next three lines are for Current Medications, Allergies and PastMedical History. If there are None Known mark that spot. Past Medical Historyalso has a spot on the <strong>scan</strong> sheet.In response to many requests for more narrative space the next 12 linesare for your narrative. This should, in conjunction with the next area, be morethan enough narrative/vital sign information area on a large percentage of your<strong>patient</strong>s.The next 13 lines are for vital signs, orders, treatment, response totreatment and medications given. The first set of vital signs should match thoseon your <strong>scan</strong> sheet.Receiving person, MD signature and crew signatures are at the bottom ofthe form. Crew signatures should include level of certification and state number.The original copy of page two goes to the EMS service, the second copygoes to the hospital along with the second copy of the <strong>scan</strong> sheet. Yourpharmacy copy should come from the third copy of the narrative page.32
Use Blue/Black Ink - Press FirmlyService Name Service # Response #Today's DateIncident LocationTransported ToPATIENTINFOPatient Last Name First MIStreet AddressCity State Zip CodePhone Age DOB GenderSocial Security # Hosp. Record #Personal MDTreating MDResponsible PartyPhoneStreet AddressCity State Zip<strong>Georgia</strong>CHIEF COMPLAINTCURRENT MEDICATIONSALLERGIES (MEDS)PAST MEDICAL HXNARRATIVENone KnownNone KnownNone KnownPCRPage 2TIMEEMT# Pulse Resp B/P SaO2 Neuro/////////////ORDERS - TREATMENT - RESPONSE - RxPatient Received By Drv /Medic Certification and NumberPhysicians Signature Medic1 Certification and NumberBar CodeMedic2Certification and Number33