Download PDF here - Macmillan Cancer Support
Download PDF here - Macmillan Cancer Support
Download PDF here - Macmillan Cancer Support
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
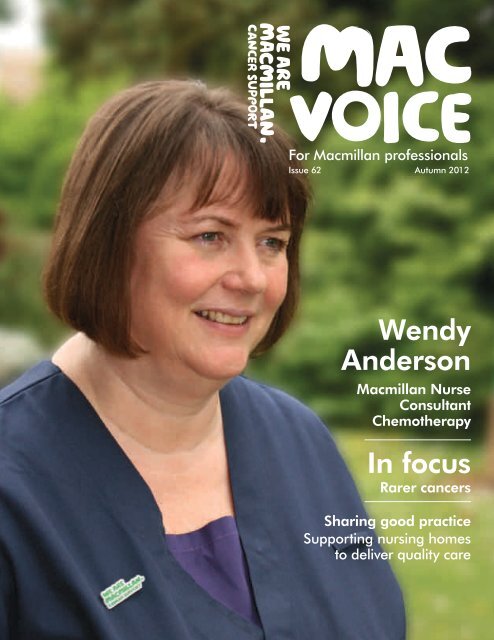
For <strong>Macmillan</strong> professionalsIssue 62Autumn 2012WendyAnderson<strong>Macmillan</strong> NurseConsultantChemotherapyIn focusRarer cancersSharing good practice<strong>Support</strong>ing nursing homesto deliver quality care
Visit our websiteAll the great news stories and featuresfrom this issue are now available atmacmillan.org.uk/macvoice If you’d liketo stop getting a paper copy of Mac Voice,please email macvoice@macmillan.org.ukWriters wantedMac Voice is for you. You can write aboutthe issues that matter to you and share yourknowledge with others. You don’t haveto be an experienced writer to get involved –simply email rcotter@macmillan.org.ukor call 020 7091 2219ContributorsWendy Anderson • Kathy Blythe • Sarah BurtonMichelle Binnion • David Cook • Penny CoyleRhian Davies • Kathy Gorman • SarahHenderson • Geoff Heyes • Trish HughesClifford Jones • Erica Lucero • Karen ParkinsonClaire Savage • Andrew Wilcock • Ruth WilsonEditorial boardCharlotte Argyle, Carers <strong>Support</strong> ManagerKathy Blythe, <strong>Macmillan</strong> DevelopmentManager • Alison Foster, <strong>Macmillan</strong> ClinicalNurse Manager & Lead Clinician for SpecialistPalliative Care • Alison Hill, Nurse Director,South West London <strong>Cancer</strong> Network • BeverlyHurst, <strong>Macmillan</strong> Gynaecology/Oncology CNSSusan Llewelyn, <strong>Macmillan</strong> Information FacilitatorYvonne McKenna, <strong>Macmillan</strong> Lead <strong>Cancer</strong> NurseBarry McVeigh, <strong>Macmillan</strong> DevelopmentManager • Heather Nicklin, <strong>Macmillan</strong> SpecialistPalliative Care Social Worker • Terry Priestman,Consultant Clinical Oncologist • Debbie Provan,<strong>Macmillan</strong> Project Lead Dietitian • Helen Tyler,Therapies Service Manager • Tracy Williams,Senior Information Development NurseEditorial teamRosie Cotter • Genevieve Osei-KuffuorGraham Pembrey • Sajjad ShahContentsNews4–11 New evidence to support multidisciplinary teams;how <strong>Macmillan</strong> can support you during a post orservice change; and changes to <strong>Macmillan</strong>'s onlineinformation for teenagers and young peopleQ&A12–13 Wendy Anderson, <strong>Macmillan</strong> Nurse ConsultantChemotherapy, talks about her role and developingbetter chemotherapy servicesFeatures14 Seamless support15 Piloting a nurse-led survivorship clinic16–17 Setting international standards18 Shaping local services19 Awareness training20–21 Primary care development22 Early diagnosisSharing good practice pull-out<strong>Support</strong>ing nursing homes to deliver quality careIn focus: Rarer cancers23–27 Features about accessing treatment, penile cancer,germ cell tumours of the ovary and Hodgkinlymphoma in young peopleThe views expressed in Mac Voice do not necessarilyrepresent the views and policies of <strong>Macmillan</strong> <strong>Cancer</strong><strong>Support</strong>. Any references to websites, books andjournals do not necessarily imply endorsement from<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>. Although we do ourbest to make sure that all of the information in themagazine is accurate and up-to-date, neither we, norany other party involved in producing the magazinewill be liable for your use of its content.Resources28 New and updated information from <strong>Macmillan</strong>© <strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>, registered charity inEngland and Wales (261017), Scotland (SC039907)and the Isle of Man (604). MAC5772_09_12Printed using sustainable material. Please recycle.2 Mac Voice Autumn 2012
EditorialRarer cancersA cancer may be defined as ‘rarer’ if it affects anunusual site in the body, or because the cancer itselfis of an unusual type or requires special treatment. [1]Further informationGeoff Heyes, Senior PublicAffairs Officer<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>020 7840 4843gheyes@macmillan.org.ukReference1Rarer <strong>Cancer</strong>sFoundation. What isa rarer cancer? www.rarercancers.org.uk/index.php?option=com_content&view=article&id=1&Itemid=2(accessed 5 July 2012).<strong>Download</strong>Improving access? Reporton the implementation ofthe <strong>Cancer</strong> Drugs Fundand the development of avalue-based pricing system.December 2011. <strong>Macmillan</strong><strong>Cancer</strong> <strong>Support</strong>.Visit macmillan.org.uk/improvingaccessPeople with rarer cancers often feelisolated. They may have never heardof their illness or not know anyone elsewith it. Health professionals may alsolack knowledge about their type ofcancer. This issue of Mac Voice focuseson treatment and support for peoplewith rarer cancers.One of the key difficulties peoplewith rarer cancers face is securingaccess to drugs and treatment.Because t<strong>here</strong> will only be a smallnumber of people who need aparticular drug, they are oftenexpensive to develop and produce.As a result, the drugs are often notapproved for NHS funding.The <strong>Cancer</strong> Drugs Fund waslaunched in England last yearfollowing a successful campaign by<strong>Macmillan</strong>. The fund was created toimprove access to cancer drugs thataren’t routinely available on the NHS.However, the fund comes to an endin 2014. <strong>Macmillan</strong> believes it hasprovided some important lessons forthe future, which are set out in t<strong>here</strong>port, Improving access?. Crucially,we argue that the drugs currentlyavailable through the fund mustcontinue to be funded by the NHSonce it ends.The Westminster government isin the process of developing a new‘value-based’ system for the pricingof drugs. <strong>Macmillan</strong> is working withthe Department of Health on what‘value’ means for people with cancer,but it's essential that any new systemimproves access to drugs for peoplewith rarer cancers.For more about access to treatmentin the UK, visit macmillan.org.uk/accesstotreatmentLooking for an articlefrom last year?You can now accessissues of MacVoice from spring2011 onwards atmacmillan.org.uk/macvoicewww.macmillan.org.uk/macvoice 3
NewsStudy backsmultidisciplinaryteamsA study by NHS Greater Glasgow and Clydesuggests that introducing multidisciplinaryteams to the area has improved the survivalrates of women who have undergone surgeryfor breast cancer.Multidisciplinary teams were introduced toGlasgow in 1995. Before their introduction,mortality from breast cancer was 11% higher inGlasgow than in surrounding health board areasin the west of Scotland.The study, which was published in the BMJ inApril, shows that after multidisciplinary teamswere adopted, mortality from breast cancer was18% lower than in other areas w<strong>here</strong> individualhealth professionals were responsible for the samedecisions. Survival improved in all areas throughoutthe 1990s, but even more in Glasgow aftermultidisciplinary teams were introduced.Project manager Eileen Kesso, who carried outthe study, says the introduction of multidisciplinaryteams, ‘marked a new development in the deliveryof cancer services, but until now t<strong>here</strong> has not beenany strong evidence that they made a differenceto a patient’s survival’.Many of you have asked us for a resource to helpyou communicate with your stakeholders about<strong>Macmillan</strong>. So, we have created a presentationshowcasing <strong>Macmillan</strong>'s organisational successes.It explains w<strong>here</strong> <strong>Macmillan</strong> has come from,who we are and what we do. It also illustratesw<strong>here</strong> <strong>Macmillan</strong> is going and its strategy to meetthe future demands of cancer care.You can download the presentation slides atmacmillan.org.uk/professionalresourcesWe also have a handy guide to giving presentationsat macmillan.org.uk/presentationsThursday 8 and Friday 9 NovemberPark Inn, London HeathrowThe event will provide opportunities todevelop new skills and share experiencesof self-management. We will also belaunching the new <strong>Macmillan</strong> professionalsawards with a prestigious ceremony.<strong>Support</strong>ed self-management in cancer careFor more information and toregister, visit macmillan.org.uk/professionalsevent4 Mac Voice Autumn 2012
Survival variationsTwo separate reports havesuggested that both w<strong>here</strong> aperson lives, and their level ofwealth, may affect their chancesof surviving certain cancers.One report from the Office forNational Statistics, Geographicpatterns of cancer survival inEngland, patients followed to 2010,revealed wide variations in oneyearsurvival estimates betweencancer networks. The largestdiscrepancy was for people withstomach cancer, with one-yearsurvival varying between 28.6%and 45.5% across networks.Mike Hobday, <strong>Macmillan</strong>Director of Policy and Research,says, ‘It is clear that every personwith cancer should expect the verybest chances of survival – nomatter w<strong>here</strong> they live. Moremoney needs to be put intoNewsunderstanding and reducing thesevariations in order to end thiscancer survival postcode lottery.’Another study, which waspresented at the National <strong>Cancer</strong>Intelligence Network conference inBirmingham this year, found thatsurvival rates for bowel cancerwere lower in more economicallydeprivedareas. The researcherslooked at nearly 4,300 people whohad surgery for bowel cancer, andcompared those of the same ageat diagnosis and sex across varioussocioeconomic groups.The findings showed that peoplewith bowel cancer living in poorerareas were 24% less likely tosurvive than more affluent patients.Researchers said that peoplepresenting with symptoms ata later stage in these areaswas a factor in this.In briefOff-labelThe Rarer <strong>Cancer</strong>s Foundationestimates that the <strong>Cancer</strong> DrugsFund has led to an increase in accessto off-label treatments of between39% and 51%, representing theextent of unmet need in the oldsystem. Read its new report, Rarebut common, at bit.ly/MA2lZ6<strong>Cancer</strong> statsBetween 1971 and 2010, the annualnumber of new cancer cases inEngland almost doubled from 138,436to 268,758, according to the Officeof National Statistics. Visit tinyurl.com/7r7bdzb to read its report.Green DealFrom October, a new UK-widescheme will help homeowners tomake energy-saving changes to theirhome at no upfront cost. It is hopedthat the Green Deal will benefit themany people affected by cancer whoare affected by fuel poverty. In 2011,<strong>Macmillan</strong> gave £2.68 million to13,691 people to help with theirfuel bills. Visit tinyurl.com/d2qswu37 yearsCatherine Skinner, who has spent37 years fundraising for <strong>Macmillan</strong>,was highly commended in theVolunteer of the Year categoryof the Third Sector ExcellenceAwards. Her achievements includeraising £106,000 from a Highlandcattle market to help fund a newchemotherapy unit in Inverness.www.macmillan.org.uk/macvoice 5
NewsInaugural laryngectomyconference a successMore than 100 people who had undergonea laryngectomy met with professionals nearCambridge earlier this year for the area’sfirst laryngectomy conference.September28 SeptemberWorld’s Biggest Coffee Morningwww.macmillan.org.uk/coffeeOctoberBreast <strong>Cancer</strong> Awareness Monthwww.breastcancercare.org.uk1 OctoberInternational Day of Older Personswww.macmillan.org.uk/ageoldexcuseNovemberLung <strong>Cancer</strong> Awareness Monthwww.macmillan.org.uk/lungcancer8–9 November<strong>Macmillan</strong> professionals eventwww.macmillan.org.uk/professionalsevent30 NovemberCarers Rights Daywww.macmillan.org.uk/carersThe aim of the day was to discusstreatment and survivorship issuesand to enable attendees to sharetheir own experiences followingthis life-changing surgery.Relatives, friends and carersalso attended.The event had originallybeen the idea of BarbaraBlagnys, former Speech andLanguage Therapist at Norfolkand Norwich Hospital, and cametogether after 10 months ofcareful planning.The morning includedpresentations about swimmingafter laryngectomy, physiotherapyfor laryngectomees and thefuture of laryngeal cancertreatment. These proved to bethought-provoking, inspiring andgenerated lots of discussion andquestions for the speakers.Lunch and refreshments wereprovided and t<strong>here</strong> was timefor the attendees to browse thestalls, which included stands fromover 15 companies and charitiesinvolved in laryngectomy care.Discussion tables were setup in the afternoon to allow forsmaller, group sessions on topicssuch as nutrition, voice prosthesesand communication. Delegateschatted, shared experiences andstories, and the feedback fromthe attendees was very positive.The event was made possibleby a grant from <strong>Macmillan</strong>and through sponsorship fromcompanies involved in healthand laryngectomy care. Wehope the conference will becomean annual event and we havealready received suggestions forfuture topics and speakers.More InformationContact Sarah Pilsworth,<strong>Macmillan</strong> Senior Specialist SLT(H&N/ENT) at Addenbrooke'sHospital on 01223 216 200.DecemberChildhood <strong>Cancer</strong> Awareness Monthwww.clicsargent.org.uk6 Mac Voice Autumn 2012
NewsBoots and <strong>Macmillan</strong>broaden local supportWe know that t<strong>here</strong> are peopleaffected by cancer who find it difficultto seek out help and support. Theymay not know w<strong>here</strong> to turn forprofessional advice, be unsure aboutwhat local services are available ormay not be comfortable seeking help.The Boots <strong>Macmillan</strong> informationpharmacist role seeks to address andbreakdown these barriers. It was bornout of <strong>Macmillan</strong> and Boots’ visionthat everyone, w<strong>here</strong>ver they are inthe UK, has access to the best cancerinformation and support in theirlocal area.Connecting servicesThe pharmacist role will signpostpeople affected by cancer to expertise,and set out the services available tothem in their local community. Thecreation of the role provides anotherchannel people can choose to accessthe information they need locally. Boots<strong>Macmillan</strong> information pharmacists willoffer advice in Boots stores, which forlots of people is a trusted, informaland familiar environment. Theywill also raise awareness of wider<strong>Macmillan</strong> services.Working with other professionalsAs well as supporting people living withcancer, the pharmacist role is designedto support <strong>Macmillan</strong> professionalsand assist the work of local informationservices. Boots <strong>Macmillan</strong> informationpharmacists are encouraged to buildlinks and raise the profile of local<strong>Macmillan</strong> services.To complement the work of<strong>Macmillan</strong> information professionals,Boots <strong>Macmillan</strong> informationpharmacists will deliver cancerinformation at the <strong>Macmillan</strong> InteractionLevels 1–2 for information and supportservices. These will enable Boots<strong>Macmillan</strong> information pharmacists tounderstand and identify that peoplehave a variety of information needs,and signpost them to more specialisedsupport, both locally and nationally.PreparationTo become a Boots <strong>Macmillan</strong>information pharmacist, allpharmacists need to complete ane-learning programme, which wasdeveloped in consultation withBoots and <strong>Macmillan</strong>’s Learningand Development Team. It includescompulsory sign up to a Charter ofCommitment in which pharmacistsagree to seek out ongoing CPDopportunities to improve customercare for people affected by cancer.Becoming a Boots <strong>Macmillan</strong>information pharmacist is voluntary,but over 100 pharmacists havesigned up so far. It is anticipated thatt<strong>here</strong> will be at least 250 trainedpharmacists in Boots stores across theUK by the end of September.Speaking about her role as a Boots<strong>Macmillan</strong> information pharmacist,Kim Baker said, ‘I like to be on hand togive advice to people on the high streetand be that first port of call if anyonehas any questions. You get regularcustomers who really benefit from theadvice you’ve given them. It’s alsogreat to be more linked to <strong>Macmillan</strong>.The training has helped me becomethe pharmacist I wanted to become.’Want to know more?Visit macmillan.org.uk/bootsor call 020 7840 4901.www.macmillan.org.uk/macvoice 7
NewsLegacy givingWhile 74% of the UK populationgives financial support to charities,only 7% leave a legacy to them.Remember A Charity Week runsfrom 17–23 September and aims toencourage people to consider leavinga gift to charity in their will.At <strong>Macmillan</strong>, legacies and gifts inwills account for more than a third ofour total income – without these, wewouldn’t be able to fund the amazingwork you do in supporting peopleaffected by cancer.Gifts in wills don’t have to be large;they come in all shapes and sizes.In 2011, our legacies ranged from£50–£3.4 million. We’ve also been lefta fish and chip shop, a carousel horseand even a herd of cows.Sarah Lee, Legacies Managersays, ’Legacy giving is surrounded bymyths that stop people from activelyconsidering supporting charities in thisway. The main misunderstandings arethat it’s expensive and complicated towrite a will, and that you need to bevery wealthy to leave a gift in yourwill to a charity.‘We want to raise awareness of theimportance of writing a will to ensurepeople's family and personal causesare cared for.’Want to know more?If you or your patients have anyquestions about legacies or wills, callthe team on 0800 107 4448, emailleavealegacy@macmillan.org.ukor visit rememberacharity.org.uk74%of people inthe UK givefinancialsupport tocharities7%leave a legacyto charities intheir willSource: Remember A Charity. About us.Accessed at: rememberacharity.org.uk/pages/about-us-.htmlThanks for sharingKaren Aylward,<strong>Macmillan</strong> Family<strong>Support</strong> Worker<strong>Macmillan</strong>’s fundraising team wouldlike to thank the professionals whohave helped with its campaignsover the last year. Stories fromprofessionals like Karen Aylward,<strong>Macmillan</strong> Family <strong>Support</strong> Worker,allow the team to breathe life intoits fundraising asks, and lend a faceto the work we do.Karen was featured in the Februarycash appeal this year alongside theFitzpatrick family who received helpand support following their Dad’sdiagnosis of a brain tumour. By gettinginvolved in sharing the Fitzpatrick’sstory, Karen has helped <strong>Macmillan</strong>raise over £90,000. This moneycould help fund almost two additional<strong>Macmillan</strong> professionals like Karen,for a whole year.‘I am always happy to support<strong>Macmillan</strong> in whatever way I can ...to me it is really important to get involvedand be part of the team. It's also been aninteresting learning experience to see justa small part of what the fundraising sideof <strong>Macmillan</strong> does.’Many of <strong>Macmillan</strong>’s supporterschoose to make a financial gift becausethey or their family have been helped bya <strong>Macmillan</strong> professional. By telling thestories of <strong>Macmillan</strong> professionals, itreminds supporters of just how vital<strong>Macmillan</strong>’s services are, and what adifference they can make topeoples’ lives.Want to get involved?If you would like to be featuredin some of <strong>Macmillan</strong>’s fundraisingmaterials, please contact Bengu Shail,Case Studies Officer, atbshail@macmillan.org.ukor call 020 7840 4891.
NewsChanges to onlineinformation for teensThis month sees somechanges to <strong>Macmillan</strong>’sinformation for teenagersand young people affectedby cancer.Visitors to click4tic.org.uk – <strong>Macmillan</strong>’s websitefor teenagers and youngpeople (TIC), will beredirected to a new sectionof the main website atmacmillan.org.uk/teensandyoungadultsThe move will ensure thatvaluable information forpeople affected by cancer‘Content will beavailable in moreflexible ways, includingon mobile devices‘of all ages is accessible onour main site and includedin <strong>Macmillan</strong>’s exciting webdevelopment plans. It alsomeans content will beavailable in more flexibleways, including on mobiledevices and in printfriendlydownloads.TIC was originally setup in 2005 to supportteenagers and youngpeople affected by cancer,as t<strong>here</strong> was very littleinformation about canceravailable for this age group.We really appreciate all theinput the site had fromcharities and individuals,and will continue towork with a range ofstakeholders, includingyoung people, as we reviewthe main website.A new online communitygroup for 16–24 year oldswas also launched on themain <strong>Macmillan</strong> site earlierthis year. The group allowsyoung people to talk to eachother and to get supportfrom <strong>Macmillan</strong>. Pleasesignpost 16–24 year oldsto our main website andnew community groups forinformation and support.At the moment, wecan’t provide the levelof moderation requiredto offer a safe, onlineenvironment for under16s, so we signpost themto websites such as theTeenage <strong>Cancer</strong> Trust's atteenagecancertrust.org‘The community groupallows young peopleto talk to each otherand to get supportfrom <strong>Macmillan</strong>‘Under 16s will still be ableto access our informationand can contact us onFacebook (facebook.com/macmillancancer)or Twitter (twitter.com/macmillancancer).Financialguidance nowon the <strong>Macmillan</strong><strong>Support</strong> LineTo make it easier for people affected bycancer to get the financial information andsupport they need, <strong>Macmillan</strong> has integratedits Financial Guidance service into the<strong>Macmillan</strong> <strong>Support</strong> Line on 0808 808 00 00.This means people can now make one phonecall for free, independent and tailored guidanceon financial matters, and to access <strong>Macmillan</strong>'sother services.<strong>Support</strong>ed by the Royal Bank of ScotlandGroup, the service can help with issues suchas financial planning, pensions and insurancematters and explaining financial jargon.If you know someone affected by cancer thatcould benefit from financial information andsupport, please direct them to the service. Theycan contact the Financial Guidance team onthe number above or at macmillan.org.uk/financialguidanceThe Financial Guidance service is availableMonday to Thursday, 9am–5pm, and Friday,9am–4.30pm. You can also order <strong>Macmillan</strong>'sfinancial information for people affected bycancer at be.macmillan.org.uk or byphoning 0800 500 800.www.macmillan.org.uk/macvoice 9
NCSI updateThe National <strong>Cancer</strong> Survivorship Initiative (NCSI) was launched in 2008as a partnership between the Department of Health and <strong>Macmillan</strong>, withsupport from NHS Improvement. It set a vision to help people living withcancer to lead an active and healthy lifestyle for as long as possible.Four years on, the partnershiphas a much greater understandingof the needs and numbers of peopleliving with cancer; w<strong>here</strong> they arein the cancer care pathway; theprofessional cultural shifts required;and what evidence-based serviceswill be necessary for the future.NCSI 2012 next steps documentThis document looks at whathas been achieved; what we nowknow; and what needs to happennext. It will be available this autumnat ncsi.org.ukThe NCSI's next steps will be to:• share learning around managingdiagnosis, treatment, recoveryconsequences of treatment andactive and advanced disease• describe the necessary changesto the cancer care pathway,and the proposed changesto enable implementation• emphasize the importanceof a ‘recovery package’for every person finishingtreatment, consisting of a holisticassessment, care planning,a Treatment Summary, anda transition event such as a<strong>Macmillan</strong> Health andWellbeing clinic• set the direction for survivorshipwork in England to 2015.<strong>Cancer</strong> Care ReviewA full evaluation report of the NCSI’sIT templates for <strong>Cancer</strong> Care Review(CCR) is now available on theNCSI website.The Quality and OutcomesFramework (QOF) requires everyonediagnosed with cancer to receive aCCR by their GP within six months oftheir diagnosis. However, the QOFlacks clarity on what the CCR shouldconsist of and what is helpful andnecessary to include.To help GPs conduct high-qualityCCRs, <strong>Macmillan</strong> worked with themain GP IT system providers – INPSand EMIS – to develop and test settemplates with GPs.The evaluation of these templatesidentified that 79% of GPs found thetemplate ‘fairly useful’ or ‘very useful’and that they appreciated the promptsfor reviewing medication or noting thecarers’ details. Work is now underwayto encourage widespread adoptionof the templates.Active and advanced diseaseThis work stream has looked at issuesfaced by people living with advancedcancer. These include: keeping well,accessing other support services,re-entering the healthcare system(eg at a time of recurrence), and theprogression of illness to palliativecare and end of life.Part of the group’s work has includedtesting a new model of care forpeople affected by lung cancer inBrighton and Hull. Themodel includes:• having a structured assessmentprocess and a personal careplan that offers support andinformation to enableself-management• rehabilitation and support throughsocial and emotional care, aswell as physical care with servicesclearly signposted• survivors and health professionalshaving access to prompt specialistcare and treatment on recurrenceor when encountering problems• the early introduction of palliativespecialists so that palliative andend-of-life care decisions can bemade in a timely way by patientsand professionals.The data is currently being analysed,however initial reports suggest thatpatients who receive early support andinformation show an improvementin their quality of life. For moreinformation, visit the NCSI website.Coming up ...We'll be including updates on otherareas of the NCSI in future editionsof Mac Voice.10 Mac Voice Autumn 2012
NewsDemonstrating impactHow <strong>Macmillan</strong>’s Service Development Teamscan support you during a post or service changeThe current health and social careclimate continues to be challenging.Many organisations are undertakingreviews and service reconfigurationto support the changing demands ofservices. As a result, some <strong>Macmillan</strong>posts are at risk. <strong>Macmillan</strong> believesit is important that any changescontinue to improve care and supportfor people affected by cancer, andare not short-term actions to achieveefficiency targets.Providing evidence<strong>Macmillan</strong> services need to show thatthey are of a high quality and arecost effective. To support <strong>Macmillan</strong>professionals to do this, we havedeveloped a series of ‘impactdocuments’ that summarise the best,current evidence relating to various<strong>Macmillan</strong> roles and services. Thesewill support you in communicating thevalue and benefits of the service youprovide. It's a good idea to gat<strong>here</strong>vidence to support your role as earlyas possible, regardless of its status.Working togetherMDMs will monitor posts that havebeen identified as ‘at risk’. The MDMwill work with the partner organisationto identify the issues and providesupport and evidence around theproposed changes. T<strong>here</strong> may be avariety of solutions, but whatever thecircumstances, MDMs and ServiceDevelopment Teams work on a caseby-casebasis to achieve the bestpossible outcome.You can find details of yourlocal MDM and <strong>Macmillan</strong>'s impactdocuments at macmillan.org.uk/serviceimpactKeeping <strong>Macmillan</strong> involved<strong>Macmillan</strong> aims to ensure thatservices for people affected by cancercontinue to be delivered to the higheststandard, by professionals with theright skills and training. It is importantthat we are involved in discussionsabout any changes to a <strong>Macmillan</strong>post or service. We can only providesupport when we are made aware ofpotential plans to change a service.T<strong>here</strong>fore it is essential that you makeyour local <strong>Macmillan</strong> DevelopmentManager (MDM) aware of:1 Changes to yourmanagement structure.2 Organisation reviews that includeyour service or post.3 <strong>Macmillan</strong> post(s) within yourservice that are frozen whena colleague leaves.4 Discussions relating to the use ofthe <strong>Macmillan</strong> title.5 Discussions relating to achange in working conditionsor service agreement.6 Discussions relating to thesustainability of a post or service.Case studyA team of three <strong>Macmillan</strong>professionals were under review ina trust facing financial challenges.<strong>Macmillan</strong> provided support in anumber of ways:• The local MDM was involvedin the review process withthe trust.• Discussions were held betweenthe MDM and the director ofservices to ensure the trust wasfully informed of the impactthe service had for peopleaffected by cancer, the extentof <strong>Macmillan</strong>’s prior servicesupport, and the originalservice agreement.• Evidence of the service impactwas presented by the team withsupport from the MDM.• The trust, <strong>Macmillan</strong> and theteam worked together to lookat new ways of working toincrease Quality, Innovation,Productivity and Prevention(QUIPP) within the service,and how the service mightcontribute to the TrustCQUIN (Commissioningfor Quality and Innovationpayment framework) andQUIPP agenda.• The MDM advised the team onhow to collect comprehensiveevidence of user experienceand service quality and presentit in a compelling way.OutcomeTwo of the three posts kept thesame grades at the end of t<strong>here</strong>view. However, the professionalshad accepted new ways of workingthat they felt would improve servicedelivery in the future. The thirdpost, which was vacant, underwenta grade change to provide a teamwith mixed skills.www.macmillan.org.uk/macvoice 11
for the patients because they getdirect access to a medicines expert,continuity of care and a key contactfor problems and advice. The clinicshave also improved waiting times,increased capacity in oncology clinics,contributed to role development,and improved team working andjob satisfaction.NameWendy Anderson<strong>Macmillan</strong> Nurse ConsultantChemotherapyIn postSince February 2010LocationJames Cook University Hospital,South Tees Hospitals NHSFoundation TrustContactwendy.anderson@stees.nhs.uk01642 850850 ext 53665What does your role involve?I provide clinical expertise, adviceand nursing leadership to develop,promote and coordinate a multiprofessionalchemotherapy service.This includes the delivery ofchemotherapy, care of patientsexperiencing complications fromsuch treatments, and a 50% clinicalworkload. The chemotherapyservice has around 10,000 patientattendances each year.Tell us about the joint nurseand pharmacist-led clinicsI introduced these clinics for peoplereceiving chemotherapy for urologyor colorectal cancers, and they havebeen well-received. They are beneficialWhat other service developmentshave you led?Prior to 2010, the amount ofchemotherapy drugs wasted was inexcess of in excess of £8,000 amonth. In a project led by myself,we have been able to reduce thatwaste to around £200 a monththrough several different initiatives.These included: increasing staffawareness of the waste issue; askingprescribers to account for wastageof high cost items (£800 or above);implementing a more effectivesystem for obtaining and actingon results of bloods taken priorto treatments; and providing moreguidance and training for clinicianson the prescribing and managementsystem. We also used telemedicineto check each patient’s fitness andwillingness to proceed on the allottedday. A waste reduction culture is nowembedded into the service and wecelebrated this success.And you have also standardisedpolicies and procedures?The Trust now has one anti-cancermedicines policy for both malignantand non-malignant chemotherapydelivery. The aim of this is to supportthe delivery of high-quality, evidencebased care, and minimise the risksassociated with the delivery ofcytotoxic chemotherapy and otheranti-cancer medicines to patients. Thepolicy also addresses the governanceissues associated with chemotherapy12 Mac Voice Autumn 2012
delivery, such as ensuring compliancewith safety updates and alerts.What is your experience of usingelectronic prescribing?I have used electronic prescribingfor chemotherapy since I cameinto post. It has improved patientsafety and complies with cancerpeer review measures. Mistakes andmisunderstanding are less frequent.What are the biggest challengesof the role?Caring for patients when theyhave a recurrence can be difficult,especially when you have builtup a relationship with them andtheir relatives. Keeping cancerand chemotherapy on the agendaalongside other priorities in healthcareis also an ongoing challenge.What is your greatest success?Personally, my greatest successhas been ensuring continuity ofcare for my patients. I have receivedpositive feedback from manypatients and relatives, and this aspectof my service has been well-evaluated.How would you like the serviceto develop?I would like to ensure the Trustconsolidates and continues to developas a specialist treatment provider ofhigh-quality, patient focused care. Iwant the Trust to become known as anemployer of choice for chemotherapyand oncology expertise in nursing.‘Patients get direct accessto a medicines expert,continuity of care anda key contact forproblems and advice’Why did you go into cancer care?My interest started early on when I wasworking as a staff nurse on a generalward with some patients being treatedfor cancer. I really enjoyed caring forthem and when a job came up to carefor these patients in a specialist role, Iapplied and was lucky enough to get it.Who inspires you?T<strong>here</strong>’s no one individual, but I havea husband, son, many patients andseveral friends and work colleagueswho are pretty amazing. I draw ontheir positive aspects. They are vibrant,energetic, make positive thingshappen, and are not afraid to takerisks and rise to a challenge.What’s the most unusual jobyou’ve had?Well, I was a chef before I becamea nurse. But the most unusual partof my current job was learning howto curtsey properly. This was inpreparation for being introduced toPrincess Alexandra, who opened thenew chemotherapy and radiotherapycentre at the hospital earlier this year.It’s now even easier to get hold of our large range of brandedmerchandise and promotional items on be.<strong>Macmillan</strong>. You can browseby type or use our improved search function to find everything fromclothing to stationery, signage to promotional giveaways.Order these for free at be.<strong>Macmillan</strong>.org.uk/profmerchandiseThese branded items show people that you’re part of our team,which helps inspire them to get involved with <strong>Macmillan</strong>.www.macmillan.org.uk/macvoice 13
Feature Holistic careFurther informationDr Andrew Wilcock DM FRCP<strong>Macmillan</strong> Reader inPalliative Medicine andMedical OncologyHayward House <strong>Macmillan</strong>Specialist Palliative Care<strong>Cancer</strong> UnitNottingham UniversityHospitals NHS Trust0115 9627 778Reference1Nottingham <strong>Macmillan</strong>Lung <strong>Cancer</strong> CAREservice. Final report. 2011’I have the highestpraise for thisteam, being helpful,courteous andreadily availableat all times’The CARE team: Andrew Wilcock;Asmah Hussain, Data Manager;Helena Alvey, Physiotherapist;Cheryl Percival, Dietitian; RachelBentley, Occupational TherapistSeamless supportDr Andrew Wilcock shares the achievements of theaward-winning <strong>Macmillan</strong> Lung <strong>Cancer</strong> CARE teamOver the past two years, the CAREteam has helped over 540 peoplewith thoracic cancer through itsmultidisciplinary approach. Based atNottingham University Hospitals NHS Trust,the team works with existing cancer andspecialist palliative care services to provideholistic support to people with lung cancerand mesothelioma. T<strong>here</strong> is a particularfocus on the cachexia-anorexia syndrome.The team was named team of the year at the2011 Excellence in Oncology Awards.Our serviceAll people recently diagnosed with thoraciccancer are invited to complete the SheffieldProfile for Assessment and Referral toCare (SPARC) questionnaire to identifytheir holistic supportive and palliative careneeds. The results are then discussed at amultidisciplinary meeting, which includesthe lung cancer nurse specialists and aconsultant in palliative medicine. This closeintegration is one of the most successfulaspects of the service as it facilitates goodcommunication and seamless support forpatients and carers. Based on the needsuncovered, the appropriate team membersvisit the patient at home or at their nexthospital appointment to carry out a moredetailed assessment and provide therapy.All patients are assessed by the dietitian.AchievementsThe team has provided around 3,200 faceto-faceappointments and 2,800 phonereviews. 80% of new, and 12% of follow-upassessments, take place in the patient’s home.The team has also:• undertaken user satisfaction surveys,which show the team is held in veryhigh regard• evaluated contributions of individualteam members, for example, dietetic data(poster presentation and submitted forpublication), and occupational therapydata (forming the basis of an MSc)• increased the number of people withthoracic cancer able to die at home (33to 49%), reduced the number dying inhospital (46 to 36%) and the number ofhospital days utilised (6,778 to 5,696) [1]• disseminated data through conferences,journals and linked with national initiatives• provided teaching and training to a widerange of disciplines.W<strong>here</strong> do we go next?Despite these achievements, we were unableto secure ongoing funding for the servicedue to the economic climate. Subsequently,the team was reconfigured last year as aspecialist palliative care rehabilitation service,applying the same principles of assessmentand support to a wider group of patients.We recently won a tender to provide such aservice to patients within the community. Thiswill ensure patients and their families continueto benefit from this type of care.14 Mac Voice Autumn 2012
Follow-up FeaturePiloting a nurse-ledsurvivorship clinic<strong>Macmillan</strong> Lead Gynae Oncology CNS Sarah Burton onsetting up a clinic for women affected by ovarian cancerLast year, my colleague ClareChurcher, Gynae Oncology CNSand I piloted a nurse-led survivorshipclinic for women with ovarian cancer at theVelindre <strong>Cancer</strong> Centre in Cardiff.Gynaecological referrals to the centrehave increased over the last five yearsand are expected to continue increasing.Based on this, and the fact that women withovarian cancer are living longer, we felt itwas necessary to deliver alternative followupcare. Women being cared for at thecentre also felt they couldn't take up theirconsultant's time with survivorship issues.Having previously run a nurse-ledchemotherapy clinic alongside doctors, webelieved we could apply a similar model,and that the nurse-led and consultant-ledservices would complement each other.Individual needsWe set up the survivorship clinic to discussindividual health needs and any associatedproblems. Common survivorship issuesfor ovarian cancer include psychosexualproblems, altered body image and fertilityissues. Some younger women experiencepost-menopausal symptoms following theirtreatment and say they do not feel feminineanymore. They can be tearful, have moodswings and loss of libido.Pilot clinicOur first clinic ran for three hours,with a 20 minutes slot for each patient.It became clear that 20 minutes was notenough, as each person took 30–45minutes to discuss their concerns in detail.We now allocate 30 minutes, which isadequate for most women, but we arelooking to review this. We also offertelephone follow-up.Many of the women attending the firstclinic had issues such as weight gain,exercise and diet, and concerns aboutfinances and employment rights. Wediscussed a variety of coping mechanisms.For many, it is about learning to live withtheir diagnosis and trying to live a ‘normal’life again.Women attending the clinic may havehad intensive treatment, involving visitsto the centre for clinic appointments andchemotherapy for 18 weeks or longer.To then be faced with being told, ‘we’llsee you in two to three months’ can bevery daunting. For some, facing life againwithout having the security of appointmentsat the centre is very frightening. Clare and Ioften find our patients need a lot of supportfollowing completion of their treatment. It’sall about adapting and tailoring the serviceto the individual.Positive evaluationA patient satisfaction questionnaire wassent out to 30 women in February and 25forms were returned. Responses showedthat patients were very satisfied withthe clinics. We also started a monthlypsychosexual treatment clinic for womenwith gynaecological cancers and somepeople living with colorectal cancers lastSeptember. We are looking to audit it soon.Further informationSarah Burton<strong>Macmillan</strong> Lead GynaeOncology Clinical NurseSpecialistVelindre <strong>Cancer</strong> Centre,Cardiffsarah.burton@wales.nhs.uk029 2061 5888’The nurses arealways happyto discuss anyproblems you have,Sarah inspiresconfidence’www.macmillan.org.uk/macvoice 15
Feature LymphoedemaFurther informationRhian Davies, Grad.Dip.Phys,PgD (Adv.Prac.)<strong>Macmillan</strong> University TeacherNursing & Health CareSchool, College of Medical,Veterinary & Life Sciences,University of Glasgow0141 330 2972rhian.davies@glasgow.ac.ukSetting internationalstandardsRhian Davies, <strong>Macmillan</strong> University Teacher, writes aboutthe development of the <strong>Macmillan</strong> Lymphoedema AcademyReferences1Lymphoedema <strong>Support</strong>Network website. www.lymphoedema.org(accessed 4December 2011).2<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>.Specialist lymphoedemaservices: An evidencereview. 2011.3Lam R, Wallace A, BurbidgeB, Franks PJ. and Moffatt CJ. Experiences of patientswith lymphoedema. Journalof Lymphoedema. 2006.1(1):16–21.4Davies R. An Investigationof the Education Needs ofHealth Care Professionalsin Scotland in relation toLymphoedema Care. 2012.Available at nes.scot.nhs.uk/education-and-training/by-discipline/nursingand-midwifery/resources/publications/lymphoedemaexecutive-summary-andlearning-needs-analysis.aspx5Sneddon M, Pearson J andFranks P. Lymphoedema:Service Provision andNeeds in Scotland. 2008.University of Glasgow and<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>.Lymphoedema affects around100,000 people in the UK. [1]It is a swelling in an arm, leg orother body part because of a buildup of fluid in the body's tissues. It canoccur as a result of cancer treatmentor because of cancer itself.While the availability of services hasimproved in the last 20 years, peoplewith cancer have told <strong>Macmillan</strong> thataccess to help and support remainsvaried. [2] Services for those affectedby non-cancer related lymphoedemaare even more patchy. [3,4,5] Mostpeople at risk of, or affected bylymphoedema, could be helped torecognise signs and symptoms and toself-manage. However, once peoplehave lymphoedema, they are likelyto require specialist support at somepoint in their care pathway.Education projectBetween 2006 and 2009, <strong>Macmillan</strong>spent around £1.7 million onlymphoedema initiatives for bothcancer and non-cancer relatedlymphoedema. [2] One such initiativewas the <strong>Macmillan</strong> LymphoedemaEducation Project (MLEP), which startedin 2003. The Peacock Charitable Trustfunded the project with <strong>Macmillan</strong>'ssupport. The overall aim was todevelop teachers in lymphoedemamanagement, with a focus onmanual lymphatic drainage (MLD) –a specialised, gentle type of massage.MLD training had been difficult toaccess as t<strong>here</strong> were very few teachersbased in the UK. It was anticipated thatby increasing the number of trainingopportunities for NHS and hospicestaff, it would be possible to increasethe number of lymphoedema-trainedhealthcare professionals in the UK.The three-year project was ledby Dr Jacquelyne Todd, ConsultantPhysiotherapist (Lymphoedema), whowas trained by Drs John and JudithCasley-Smith to teach the Modernmanagement of lymphoedema course.She was assisted by Catherine Groom,MLD Therapist and teacher of theCasley-Smith technique. The techniqueis an approach to decongestivelymphatic therapy, which involvesspecialised massage, compression,exercise and skin care.Ten healthcare professionalsincluding nurses, physiotherapists andan occupational therapist, took partin the teacher training programme,during which the curriculum wasstandardised and teaching materialswere developed. After completingthe programme in 2006, theseprofessionals developed the <strong>Macmillan</strong>Lymphoedema Academy (MLA),which offers registered healthcareprofessionals accredited and nonaccreditedcourses across the UK.The group also peer reviews teachersto maintain standards.Over 500 professionals havesuccessfully completed one of themany courses offered. T<strong>here</strong> is the16 Mac Voice Autumn 2012
added benefit that someone trainedto this level may be supporting threeor four others, teaching lymphoedemacare locally, and managing a caseloadof patients who would otherwise not bemanaged adequately.Working with <strong>Macmillan</strong> to extend thework of the group has been rewardingfor the teachers, and has improved theskills of many professionals who haveattended the courses. Patients withinand beyond the UK are now feeling thebenefits of this work.Rhian demonstrateslymphoedemabandagingCasley-Smith techniqueThe influence of the MLA now extendsbeyond the UK. Two members representthe MLA on the board of Casley-SmithInternational, a collective of internationalteachers of Casley-Smith technique.Dr Todd has been key to writing thecurriculum for training future Casley-Smith teachers anyw<strong>here</strong> in the worldso that t<strong>here</strong> are consistent standardsof Casley-Smith MLD educationinternationally. Casley-Smith Internationaland the MLA will continue to update andmodernise learning materials through itswebsite – casleysmithinternational.orgCommunity of practiceIn 2010, the MLA broadened its remitbeyond education and has since becomethe <strong>Macmillan</strong> Lymphoedema AcademyCommunity of Practice. The communityhas reviewed patient informationresources and developed:• a 3D educational tool to demonstratelymphotomes and watersheds tolymphoedema students (available atmacmillan.org.uk/learnzone)• genital and lower limb prostheticmodels to teach lymphoedemastudents, patients and their carers theskills of bandaging genital oedema.Related informationVisit macmillan-lymphoedemaacademy.org.ukwww.macmillan.org.uk/macvoice 17University of Glasgow, Nursing & Health Care
Feature Primary carePrimary care developmentDr Penny Coyle and Dr Clifford Jones reflect on their firstyear as <strong>Macmillan</strong> GP FacilitatorsFurther informationDr Penny Coyle<strong>Macmillan</strong> GP Facilitator,Aneurin Bevan HealthBoardpenny.coyle@wales.nhs.ukAs <strong>Macmillan</strong> GP facilitators,we aim to improve the quality ofcancer and palliative care providedby primary healthcare teams within the localhealth economy, in line with national and<strong>Macmillan</strong> priorities. We represent peoplewho are chronically ill by embedding theirneeds in the health system, empoweringthem to make informed choices abouttheir treatment, and providing professionalswith the right information to supportthese decisions.Our first year in post has been bothbusy and challenging – not everything hasgone perfectly, but we have found the rolehugely rewarding and the early resultsencouraging. Our work has been supportedand guided by two clinical mentors and asteering group of healthcare professionals,and <strong>Macmillan</strong> and patient representatives.AssessmentOur first challenge was to assess existingservices. We began by circulating aquestionnaire to all GP surgeries in the Trustarea to understand what palliative careprovision was available to the community.The results allowed us to map currentpractice, strengths, weaknesses and identifyareas for improvement. We intend to revisitthe questionnaire at regular points duringour post to track the improvements inthese community services.We have also spent time meetingdifferent team members to understandtheir experience of providing care to the20 Mac Voice Autumn 2012
Primary care Featurechronically ill. Such patients arelikely to be treated by many differentprofessionals. Understanding theseroles and referral pathways hasprovided us with an insight into whysystems don’t always work efficientlyand helped us identify w<strong>here</strong>improvements could be made.Meeting different team membershas also given us the opportunityto share information and providetraining. We have facilitated interactiveteaching sessions for GPs in each ofthe five localities that make up theAneurin Bevan Health Board (ABHB).The sessions were run jointly withpalliative care consultants, basedaround the key theme of ‘qualitystandards for end-of-life care’.We used these sessions to discusshow to:• identify patients – what are the keysigns of deterioration, what factorspredict prognosis• use the integrated care priorities• control symptoms• discuss sensitive topics with peoplewho are chronically ill.We have supported these sessionswith the production of templates tohelp professionals capture relevantinformation in palliative care meetings.Such information is invaluable intracking and monitoring patients,particularly if their symptoms requirefurther treatment.Access to careWe have complemented our trainingscheme with specific projects in theABHB area aimed at improvingaccess to appropriate care andpromoting advance care planning.Our objective is to ensure health andsocial care professionals are wellinformedabout the patients’ historiesand current situations, so patients donot need to repeat this informationwhen encountering someone new.For example, we have initiated aproject to enable people to be caredfor in their preferred place of care andto reduce unnecessary admissions tohospital at the end of life. The projectfocuses on understanding why hospitaladmissions occur and on developingprotocols to enable people to accessappropriate care. In particular, wewill focus on people in residential andnursing homes to emphasise how theyshould be offered every opportunity tobe involved in planning for their futureregardless of diagnosis.‘Our first year in posthas been both busy andchallenging – not everythinghas gone perfectly, but wehave found the role hugelyrewarding and the earlyresults encouraging’Care at homeA second project has focused onthe care of people at home. Wehave looked at improving two criticalareas – ensuring people have accessto the right medicine at any time ofthe day and that medical professionalscan be quickly brought up to speedon a patient’s history should anemergency occur.With the first area, we recognisethat the needs of people in palliativecare change very quickly and theymay require immediate access tonew medicines outside of the normalworking day, when these are leastlikely to be available. We haveworked with other professionalsto launch ‘Just in case’ boxes, whichprovide medicine in anticipation ofa prescription being written, avoidingthe need to visit pharmacies lateat night.The second area is based on theneed to share important information.We have designed an advance careplanning communication tool. This isa simple document that can be usedto record important information aboutthe patient and their future wishesand decisions. It is then stored inthe patients’ notes and also faxed todoctors working in different sectors,eg hospital and out-of-hours service.We have also been helping topromote the ‘Message in a bottle’scheme. This specially designed bottleis stored in the fridge and containsvital information for any healthprofessionals visiting the home. Thiscould be about medicines, medicalnotes or in some cases resuscitativepreference. A sticker on or near thefront door alerts visitors of the bottlein the fridge, which can be particularlyimportant in an emergency situationor when the patient may not beable to respond.Moving forwardWhile our first year has presentedmany challenges, it has also provedthat although the health service iscomplex, improvements to patientcare can be made by simple, smallchanges. We are excited to move onto different projects that will involveassisting in the development of cancerservices and cancer survivorship.These roles would not exist without<strong>Macmillan</strong>’s invaluable supportand funding.Related informationFor more about <strong>Macmillan</strong>'sprimary care community, visitmacmillan.org.uk/pcclwww.macmillan.org.uk/macvoice 21
Feature Improving outcomesEarly diagnosisKaren Parkinson shares how she and colleagues are raisingawareness of the signs and symptoms of cancerFurther informationKaren ParkinsonEPOC DevelopmentWorker (Sleaford Area)karen.parkinson@developmentplus.org.ukepoc@developmentplus.org.uk01522 533510The EPOC programmeis delivered by t<strong>here</strong>gistered charitydevelopmentplus andis funded by NHSLincolnshire and<strong>Macmillan</strong> <strong>Cancer</strong><strong>Support</strong>. The EPOCDevelopment Workersare Karen Parkinson,Louise Irving, KasiaPisarska Hopkins andBonney Cottrell.The Early Presentationof <strong>Cancer</strong> Programme(EPOC) was setup in 2009 to lowercancer mortality rates inLincolnshire’s growing andageing population.It aims to:• raise awareness of theimportance of earlydetection of cancerthrough recognition ofsigns and symptoms.• promote the earlypresentation of cancersymptoms to GPs• work with GPs to raisetheir awareness and useof early diagnostic tools• promote better uptakeand attendance ofscreening services• work in the heartof communities,developing volunteeringand social marketing.EPOC was establishedby NHS Lincolnshirein response to actionpoints identified in the<strong>Cancer</strong> Reform Strategy.[1]The strategy sets outa programme of actionacross ten areas, includingsix areas to improve canceroutcomes and four areas toensure delivery.Spreading the wordEPOC spreads cancerprevention and healthylifestyle messages to peoplefrom all walks of life. Theteam visit schools, colleges,universities, communitygroups and local events,and volunteers hold amonthly market stall.During the first sixmonths of 2012, the teamdelivered more than 300events and workshops.Volunteers receivetraining from <strong>Macmillan</strong>about the signs andsymptoms of cancer,confidence buildingand talking to membersof the public. One ofthe volunteers found acancerous breast tumourafter joining the programmeand she now uses her storyto show that early diagnosiscan save lives.EPOC has also runa successful ‘Boobs andBalls’ campaign to educateyoung people about theimportance of getting toknow their breasts andtesticles from an early ageand reporting any changesto their GP. Over 6,150young people have beenreached by the campaignthis year.ScreeningAs part of the second phaseof EPOC’s development, theteam is raising awarenessof the NHS <strong>Cancer</strong>Screening Programmesto improve uptake. Theteam development workersliaise with local breast andbowel screening units tofind out w<strong>here</strong> and whentheir screening sessionsare taking place andpromote the sessions withincommunities with the helpof volunteers.The team discussspecific queries and fearswith individuals and haveaddressed these withvery encouraging results.The Lincolnshire breastscreening unit has reportedan increase in womenattending for screening inthe targeted areas.EPOC has beenpromoting the nationalbowel screeningprogramme by encouragingpeople to use their postalkits and we promoted theservice at Lincolnshire'sagricultural show. The teamare currently devising acervical cancer campaign toincrease uptake of cervicalscreening invitations by allage groups.An evaluation of theprogramme will beginin October and we'll beincluding updates on ourwork in future editions ofMac Voice.22 Mac Voice Autumn 2012
In this section24 Access to treatmentDavid Cook25 Penile cancerSarah Henderson, <strong>Macmillan</strong>Urology Nurse Specialist26 Germ cell tumoursErica Lucero, <strong>Macmillan</strong>Gynae-Oncology ClinicalNurse Specialist27 Hodgkin lymphomaTrish Hughes, <strong>Macmillan</strong>Haematology ClinicalNurse Specialistwww.macmillan.org.uk/macvoice 23
Access to treatmentDavid Cook, 52, was diagnosed with kidney cancer in 2004– he says it's more difficult for people with a rarer cancer toaccess information, support and treatmentFurther informationDavid CookDavid was awardeda <strong>Macmillan</strong> <strong>Cancer</strong>Champion award in2010. This is given tovolunteers who haveused their experience ofcancer to help others.Kidney <strong>Cancer</strong> <strong>Support</strong>Networkwww.kidneycancersupportnetwork.co.ukRarer <strong>Cancer</strong>sFoundationwww.rarercancers.org.ukReference<strong>Cancer</strong> Research UKwebsite. Kidney cancerstatistics. http://info.cancerresearchuk.org/cancerstats/types/kidney/uk-kidney-cancerstatistics(accessed 8August 2012).‘The biggestimpact ofthe postcodelottery is onrarer cancers’When David was first diagnosed,he didn’t know anything aboutkidney cancer.‘I found it difficult to get information.With more common types of cancer, t<strong>here</strong>is almost an overload of information, butfor kidney cancer t<strong>here</strong> isn’t much at all.’Kidney cancer affects around 9,000people in the UK each year. [1] It is morecommon in men than women and incidenceincreases as people get older.David had surgery to remove his leftkidney, but t<strong>here</strong> was no adjuvant therapyavailable at that time. He says the surgeonhe saw was ‘fantastic and positive’.Appealing for treatmentIn December 2006, two years after his firstdiagnosis, David was told that the cancerhad spread to his lungs and lymph nodes.His specialist wanted to prescribe himsorafenib (Nexavar ® ), a drug that had beenproven effective in treating advanced kidneycancer. However, his primary care trust(PCT) prohibited this, so David had to applyfor exceptional funding. His first applicationwas rejected, but he appealed and the PCToverturned its decision. In the meantime,David had gone three months withouttreatment. During this time, David’s wifediscovered that she also had cancer.Campaigning for changeIn a speech to an All Party ParliamentaryGroup on <strong>Cancer</strong> at the Houses ofParliament in 2009, David said, ‘You canimagine how devastating this was for myfamily. My children were burdened withthe knowledge that both of their parentshad cancer, and one was being deniedtreatment. Luckily, their mother is okayand I am still <strong>here</strong>.’David is a strong advocate of the<strong>Cancer</strong> Drugs Fund and points out thatit has helped 11,400 people since it wasestablished last year. ‘However, t<strong>here</strong> arestill areas of the UK w<strong>here</strong> it is much harderto get approval for new cancer drugs. Thebiggest impact of the postcode lotteryis on rarer cancers.’Living with cancerBefore David won his appeal in 2007,he was told that he only had a year to live,for some of which he would be bedridden.Since that time, the cancer hasn't spreadsignificantly. David has also been takingpart in a trial for everolimus (Afinitor ® )since 2009.David admits that he has difficult days.‘I’ve had fantastic treatment, and supportfrom my family and work. But t<strong>here</strong> arepsychological issues. Every three monthsI have to go for a CT scan and I neverknow what the result is going to be. A lotof the other people I’ve met with kidneycancer have now died or are in a very poorcondition. It’s difficult to come to terms withthe fact that, at some point, that’s going tobe me. But I do think that t<strong>here</strong>’s now<strong>here</strong>better than the NHS when you’re seriouslyill. And working with <strong>Macmillan</strong> hasbeen fantastic.'Related information<strong>Macmillan</strong> has information aboutkidney cancer and the <strong>Cancer</strong> Drugs Fund.Order free from be.macmillan.org.ukor call 0800 500 800.24 Mac Voice Autumn 2012
Penile cancerSarah Henderson, <strong>Macmillan</strong> Urology Nurse Specialist,discusses this rare and devastating tumourPenile cancer affects about 400 meneach year in the UK. Although it ismainly seen in men over 60, 20% ofcases will be diagnosed in men under 40.Symptoms can vary widely from a small,reddened area on the glans, to a largefungating mass with enlarged groin lymphnodes. Diagnosis may be delayed eitherdue to the man not seeking help or lack ofknowledge from healthcare professionals.TreatmentTreatment can vary from topicalchemotherapy to a variety of surgicaltechniques. Radiotherapy to the penis israrely used as a primary treatment now.Treatments have changed dramaticallyin the last decade with penile preservingsurgery now being the most commonprimary management. Radical penectomymay be necessary for more advancedtumours. The first place this cancer willspread to is the groin lymph nodes, sostaging of lymph nodes is important.Specialist centresPenile cancer is managed in supra regionalcentres. T<strong>here</strong> are about 10 such centresspread across the UK. The purpose behindthis is to consolidate expertise into specialistcentres w<strong>here</strong> clinicians work in teamsthat see this problem on a regular basis.This unfortunately means that patientsmay have to travel long distances for theirtreatment. Management can be streamlinedto a certain degree if scans and outpatientappointments are booked on the same day.Treatment so far from home can beisolating and although hospital stays havebeen reduced, it is important to considerlocal accommodation for partners or familymembers. Travel and accommodation costscan also be significant so <strong>Macmillan</strong> Grantsand referral to a local benefits service canbe very helpful. Communication with thepatient’s local team is key to a smoothtransition of care.Subsequent oncological treatments, suchas chemotherapy or radiotherapy, are morelikely to be carried out closer to the patient’shome. T<strong>here</strong> is a key oncologist in each ofthe referring centres who will coordinatethese treatments.Prognosis depends on the stage of thecancer and those with lymph nodes thathave extracapsular spread will have thepoorest chance of survival.<strong>Support</strong>Psychological intervention is important formen affected by penile cancer and theirpartners. All penile cancer centres shouldhave access to psychological services.The effect of treatments for penile cancercan be significant and if more radicalsurgery is necessary it may impact not onlyon sexual function but urination as well.Sitting down to pass urine may have botha psychological and social impact.It is difficult to provide support groupsbecause of the nature of the disease andthe wide area from which patients travel.Patient surveys have shown that web-basedsupport is preferred. T<strong>here</strong> are a coupleof online groups, including <strong>Macmillan</strong>’sOnline Community, and details of theseare provided at diagnosis. This method ofsupport is not suitable for everybody solocal cancer support centres may be helpful.This can be a devastating cancer, butgood communication and team work canimprove the patient experience.Further informationSarah Henderson<strong>Macmillan</strong> UrologyNurse SpecialistSt. George’s HealthcareNHS Trust, Londonsarah.henderson@stgeorges.nhs.uk020 8725 0393Relatedinformation<strong>Macmillan</strong> has a factsheet about penilecancer. Order free frombe.macmillan.org.uk or call 0800 500800. Visit <strong>Macmillan</strong>’sOnline Community atmacmillan.org.uk/communitywww.macmillan.org.uk/macvoice 25
Further informationErica Lucero<strong>Macmillan</strong> GynaeOncology Clinical NurseSpecialistCroydon HealthcareServices NHS Trust,Croydon UniversityHospital020 8401 3000 Ext3967 or Bleep 227erica.lucero@mayday.nhs.ukThe factsGerm cell tumours of theovary are a rare type ofovarian cancer. Fewer than1,500 women are diagnosedwith this type of cancer in theUK each year.SymptomsMany woman with early stageovarian cancer do not haveany symptoms. If symptomsare present, they can includeabdominal pain, a feeling offullness or abdominal swelling,Germ cell tumoursErica Lucero, <strong>Macmillan</strong> Gynae Oncology CNS, writes aboutthe discovery of a germ cell tumour during a pregnancy scanMary* was 22 weeks pregnantwith her first child when anultrasound scan detected anovarian mass. Her scan and tumourmarkers raised a high suspicion ofmalignancy or ovarian cancer.Ovarian cancer occurs in around1 in 18,000 pregnancies and thecombination of a germ cell tumourduring pregnancy is even rarer. Aswith many early stage ovarian cancers,Mary did not have any symptoms.Mary’s case was discussed at amultidisciplinary team meeting andMary subsequently chose to have herovary surgically removed at 26 weeks,rather than wait until after herpregnancy. The team ensured that theunborn baby was considered in alldiscussions of care.Before Mary had the procedure,she was counselled by the gynaecologyconsultant about possibleand sometimes an increasedneed to pass urine. Somewomen may have irregularvaginal bleeding.DiagnosisSeveral tests may be usedincluding blood tests, ultrasoundand CT scans, and laparoscopy.TreatmentTreatment will usually involve acombination of surgeryand chemotherapy.complications during and aftersurgery, and the possibility ofmiscarriage during surgery. I was alsoon hand to provide psychologicalsupport and to answer Mary’squestions. She was worried about herbaby and did not say or ask much,which is not unusual after receivingbad news. I gave her a pack withinformation about ovarian cancer,contact details and some informationand support websites. Before Maryleft, I emphasised that she could callme if she had any queries or neededany psychological support. Mary’spartner was included in the discussionsabout her diagnosis and treatment.After a few days, she rang with alist of questions related to the cancerand her pregnancy. At the end of ourconversation, she said she felt betterand reassured. I also referred her tothe <strong>Macmillan</strong> cancer support centre.Following the operation, she wastold that the ovary that was taken outhad an early stage of ovarian cancer.She was speechless and teary.At her follow-up appointment, shewas well and fully recovered from theoperation. She has had monthly MRIscans and blood tests following hertreatment. The rest of her pregnancywent well and she is expecting a babygirl in few weeks. Mary was gratefulthat a routine scan detected the cancerand that it was investigated promptly.Related information<strong>Macmillan</strong> has informationabout germ cell tumours of the ovaryat macmillan.org.uk/gcto* Name has been changed.26 Mac Voice Autumn 2012
Hodgkin lymphomaTrish Hughes, <strong>Macmillan</strong> Haematology CNS, ontreating young people with Hodgkin lymphomaLucy* was 19 when she wasdiagnosed with Hodgkinlymphoma. It was August andshe was due to go to university thefollowing month to study biomedicalscience. Lucy and her parents werenaturally very distressed.A diagnosis of cancer in this agegroup is the last thing people expect.Young people are often at universityor college or may even have youngfamilies, so this has a huge impacton their lives. They are often veryfrightened and it is my role to supportthem through this experience.As a key worker for young peoplelike Lucy, I provide psychologicalsupport and information for the youngperson and their parents. This includesspending time explaining the diagnosisand treatment options.Ongoing supportI kept in regular telephone contact withLucy while she was undergoing testsbefore commencing treatment. I alsocontacted her tutor to organise for herplace at university to be deferred.Lucy was given chemotherapy byhaematology clinic staff, who alsoplayed a part in providing holistic carefor Lucy. At the end of treatment Isupported Lucy with her transition backto university by organising some workexperience for her with our laboratorystaff. Lucy did this for a few monthsafter completing treatment andthoroughly enjoyed the experience.I saw Lucy in clinic recently and shehas just completed her first year ofuniversity and remains very well.SurvivorshipWhen a young person has finishedtreatment for Hodgkin lymphomat<strong>here</strong> is regular follow-up throughthe haematology department. Inthe past I have had an informalchat with patients, however I amabout to commence a holistic needsassessment clinic for people at the endof treatment, w<strong>here</strong> we will discussconcerns and make a care plan.Related information<strong>Macmillan</strong> has a booklet aboutHodgkin lymphoma. It also has abooklet written especially for youngpeople with cancer called I'm still me.You can order these for free frombe.macmillan.org.uk or call0800 500 800.* Name has been changed.The factsHodgkin lymphoma is a cancerof the lymphatic system. Around1,870 people are diagnosed withit in the UK each year.SymptomsThese can include a painlessswelling of a lymph node(lymphadenopathy) night sweats,fevers, fatigue and weight loss anditching. In some cases t<strong>here</strong> is novisible swelling and a young personmay present at the GP with vaguesymptoms such as itching.Further informationTrish Hughes, <strong>Macmillan</strong>Haematology CNSNorthampton GeneralHospital NHS Trusttrish.hughes@ngh.nhs.ukReferencesLymphoma Association.Frequently asked questions.(Accessed at www.lymphomas.org.uk/information-andsupport/information-aboutlymphoma/frequently-askedquestions#What%20is%20Hodgkin%20lymphoma).Improving supportive andpalliative care for adults withcancer. 2004 London, NICE.Improving outcomes in childrenand young people with cancer.2005. London, NICE.DiagnosisA lymph node biopsy is neededto confirm the diagnosis. Otherstaging tests include a CT scan ora PET scan, a bone marrow testand blood tests.TreatmentDepending on the stage of thelymphoma, treatment is usuallychemotherapy. If the lymphomais localised to one group of lymphnodes radiotherapy can be given.www.macmillan.org.uk/macvoice 27
ResourcesNewUpdatedUnderstanding the consequencesof cancer treatment – top 10 tipsMAC13615This leaflet aims to help people to getthe support they need following cancertreatment and to help them monitortheir own health and well-being.Bowel symptoms and headand neck symptomsMAC13793 and MAC13792These two flyers encourage people toget cancer symptoms checked at anearly stage.Having tests for prostate cancerand Having tests for bowel cancerMAC13704 and MAC13679How are you feeling? Theemotional effects of cancerMAC11593Understanding breast cancer in menMAC11915, 2 nd editionI’m still meMAC6706, 6 th editionA guide for 12–25 year olds livingwith cancer.Recipes for people affectedby cancerMAC11668, 4 th editionRedesigned and updated, this bookletcontains recipes that are appropriatefor people living with cancer. We alsohave three new booklets about dietand cancer: Healthy eating and cancer(MAC13612); The building up diet(MAC13614); and Eating problems andcancer (MAC13613).Relationships, sex and fertility foryoung people affected by cancerMAC11679, 4 th editionTo order free copiesVisit be.macmillan.org.ukor call 0800 500 800. Some of ourresources are also available on CD.Can we talk about work?New e-learning course aboutcancer and its impact on workThis bite-sized, online coursefor health and social careprofessionals can help you toimprove your understanding ofwork and cancer issues, anddevelop your confidence indiscussing them with peopleliving with cancer and theircarers. It includes modules aboutemployment rights, financialissues, referrals and advice,and <strong>Macmillan</strong> resources. Visitmacmillan.org.uk/learnzoneCrossword123 456Clues acrossClues down7911 1216 17192181318410142051561 Small informal party (3-8)7 Grows old8 Japanese unarmed fightingsport (2-5)9 Have power of vision10 Surrender or submit11 Large rounded wine glass13 Roused into action16 Speak … complete ortotal nonsense?18 Deuce19 Middling or so-so20 Track for trains21 Scented climbing shrub1 A kept toy-boy2 Dangly furnishingsdecoration3 Speak out againstsomething4 Get pleasure from5 Impetuous person6 Curved11 Hungarian stew12 Amongst13 Rich cream cake14 Hooded waterproof jacket15 Locomotive17 Immediately availableAnswers across 1 Get-together 7 Ages 8 Ju-jitsu 9 See 10 Yield 11 Goblet 13 Goaded 16 Utter 18 Two 19 Average 20 Rail 21 HoneysuckleAnswers down 1 Gigolo 2 Tassel 3 Object 4 Enjoy 5 Hothead 6 Rounded 11 Goulash 12 Between 13 Gateau 14 Anorak 15 Engine 17 Ready