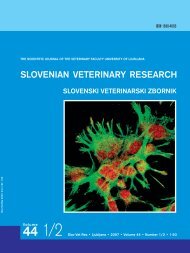
Advanced periodontal disease in a Yorkshire terrier with concurrent nasal cavity malignancy105though <strong>the</strong> mon<strong>of</strong>ilament resorbable suture material(Biosyn 5-0; United States Surgical, USA) wasstill present. After thorough oral cleaning (scalingand polishing), <strong>the</strong> left maxillary canine tooth,left mandibular canine tooth and left mandibularfirst premolar tooth were extracted using <strong>the</strong> techniquesdescribed previously, <strong>the</strong> oronasal fistulabeing closed with a single layer mucogingival flap.A thorough examination <strong>of</strong> <strong>the</strong> larynx, pharynx,s<strong>of</strong>t palate and caudal nasal cavity using a dentalspeculum, mirror and retractor was performed, butno additional abnormalities were found. Due to <strong>the</strong>presence <strong>of</strong> <strong>the</strong> oronasal fistula <strong>the</strong> dog was maintainedon amoxicillin and clavulanic acid (20 mg/kg/12 hours p.o.) for 10 days following <strong>the</strong> dentaltreatment, with carpr<strong>of</strong>en (4 mg/kg/day) also beinggiven for <strong>the</strong> first 4 days.Fur<strong>the</strong>r presentations and diagnosticproceduresOne month after <strong>the</strong> second dental treatment(April 2007) <strong>the</strong> owner reported reappearance <strong>of</strong> <strong>the</strong>serous nasal discharge from <strong>the</strong> left nostril, it havingstopped shortly after <strong>the</strong> previous treatment, andmild difficulties breathing. As no recurrence <strong>of</strong> <strong>the</strong>oronasal fistula was detected on clinical examination,<strong>the</strong> owner agreed to have ano<strong>the</strong>r examinationunder general anaes<strong>the</strong>sia, but <strong>the</strong> owner scheduledthis for 1 month later (May 2007). At this time allCBC values, urea, creatinine, alkaline phosphataseand alanine aminotransferase were still within normallimits. Examination under general anaes<strong>the</strong>sia(induced and maintained as previously, but withoutantibiotics and carpr<strong>of</strong>en) revealed no abnormalitiesin <strong>the</strong> oral cavity. Radiographs <strong>of</strong> <strong>the</strong> head (lateral,open-mouth and intra-oral occlusal dorsoventralprojections) were obtained but were not diagnostic.Rhinoscopy with a 2.7 mm rigid endoscope passedvia <strong>the</strong> nostrils was performed revealing no abnormalitiesin <strong>the</strong> right nasal cavity, however, in <strong>the</strong> leftnasal cavity at a depth <strong>of</strong> approximately 3 cm <strong>the</strong>rewas a mass estimated to be 1 cm 3 in size, appearingto be based caudally. The surrounding nasal tissueswere visibly inflamed. Nasal flush was performed toclear any discharge before biopsy to obtain materialfor histopathology. As <strong>the</strong> drainage lymph nodes weresmall no attempt was made to perform fine needle aspirationat this stage, invasive biopsy remaining anoption if <strong>the</strong> nasal biopsy confirmed neoplasia. Thedog was discharged with a course <strong>of</strong> meloxicam foranalgesia (Metacam; Boehringer Ingelheim VetmedicaGmbH, Germany; 0.1 mg/kg/day p.o.).Histopathology results and fur<strong>the</strong>rtreatmentHistopathology results revealed an inflamed lowgrademalignant nasal tumour, composed <strong>of</strong> twodistinct subtypes predominant papillary and cysticadenocarcinoma with mucus secretion and formation<strong>of</strong> small cysts (Figure 1) and a smaller part <strong>of</strong><strong>the</strong> transitional carcinoma, which is also referredto as respiratory epi<strong>the</strong>lial carcinoma or nonkeratinizingsquamous cell carcinoma (Figure 2) (4). Theadenocarcinomatous part was mostly composed <strong>of</strong>Figure 1: Papillary cystic adenocarcinoma. Part <strong>of</strong> <strong>the</strong> tumourshows a less well differentiated tall columnar epi<strong>the</strong>liumwith mild cellular and nuclear pleomorphism. Agroup <strong>of</strong> pleomorphic epi<strong>the</strong>lial cells can be seen in <strong>the</strong>middle (arrow) and a mitotic figure in <strong>the</strong> left lower corner(arrow). There is abundant lymphocytic infiltrate and neutrophilsin <strong>the</strong> stroma. HE staining, x200Figure 2: Transitional carcinoma. Cellular and nuclearpleomorphism is clearly evident. Abundant lymphocyticinfiltration can be seen in <strong>the</strong> stroma. HE staining, x200
106 A. Nemec, Z. Pavlica, P. Juntes, D. A. Crossleywell differentiated cuboidal or tall columnar epi<strong>the</strong>lialcells with mild pleomorphism, only limited areasshowing greater pleomorphism. The cells <strong>of</strong> a transitionalcarcinoma subtype revealed greater variability<strong>of</strong> cell shape and size, from smaller basaloidcells to larger tall columnar and spindle-shaped orpolygonal cells with moderate amount <strong>of</strong> pale eosinophiliccytoplasm and hyperchromatic nuclei containingone or two, and rarely several, small nucleoli.Mitotic figures were rare in both parts.The dog was much better while on meloxicamand <strong>the</strong> owner was advised to proceed with staging.In view <strong>of</strong> <strong>the</strong> final diagnosis <strong>the</strong> owner was <strong>of</strong>feredreferral for a CT scan prior (3, 5) to possible radiation<strong>the</strong>rapy.DiscussionPeriodontal disease is <strong>the</strong> most common chronicinfectious disease in dogs affecting a majority <strong>of</strong> <strong>the</strong>mature population (6, 7), with small breeds beingpredisposed to it (8). Tumours <strong>of</strong> <strong>the</strong> nasal and paranasalsinuses are rare in most domestic species butare recognised most frequently in dogs. The prevalence,however, is only 0.3 to 2.4%, with medium tolarge dolichocephalic breeds being more <strong>of</strong>ten affected.The higher risk associated with a long nosemay be related to <strong>the</strong> larger surface area <strong>of</strong> nasal epi<strong>the</strong>liumand with <strong>the</strong> filtering capability, althougha genetic basis in some breeds is also suspected (9).Incidence <strong>of</strong> nasal tumours also increases with age<strong>of</strong> <strong>the</strong> dog, <strong>the</strong> mean age being reported as 9 to 10years (10, 11). Despite <strong>the</strong> low prevalence, however,Tasker (12) reports that neoplasia is <strong>the</strong> most commondiagnosis in dogs with persistent nasal disease(one third <strong>of</strong> cases), where as periodontal disease isonly recognized as <strong>the</strong> cause in 10% <strong>of</strong> cases. Adenocarcinomais <strong>the</strong> most frequent malignant nasaltumour recognized in dogs (9, 10) with transitionalcarcinoma being <strong>the</strong> second most common, both beingrare or not reported in o<strong>the</strong>r animal species (4).Acinic cell carcinoma or even neuroendocrine carcinomacan not been ruled out completely in this caseas differentiation requires immunohistochemistry,which was not performed. As neuroendocrine carcinomais an uncommon sinonasal tract neoplasmwith aggressive clinical behaviour (13, 14) this differentialdiagnosis was not consistent with clinicaland histomorphological findings in <strong>the</strong> presentedcase.The diagnostic approach to a patient with nasaldischarge includes obtaining a complete historysupported by thorough physical examination androutine blood tests to rule out systemic disease (1).If <strong>the</strong> results are normal as in <strong>the</strong> presented case,complete oral examination is <strong>the</strong> next step as wellas nasal swabs for cytology and culture if fungal diseaseis suspected, before proceeding to imaging andrhinoscopy with biopsy sampling (1). However, bloodtest results may be normal in dogs with nasal neoplasiaas paraneoplastic disorders associated withnasal tumours are rare in dogs (10).As advanced periodontal disease with oronasalfistulae at <strong>the</strong> maxillary canine teeth was detectedin this case, <strong>the</strong> chronic serous bilateral nasal dischargewas suspected to be <strong>of</strong> dental origin, especiallywhen <strong>the</strong> nasal discharge completely disappearedon <strong>the</strong> right side after <strong>the</strong> first dental treatment (extraction<strong>of</strong> <strong>the</strong> right maxillary canine tooth and closure<strong>of</strong> <strong>the</strong> fistula at that site), but remained on <strong>the</strong>untreated site. As <strong>the</strong> discharge from <strong>the</strong> left nostrilalso temporarily disappeared after extraction <strong>of</strong> <strong>the</strong>left maxillary canine tooth and antibiotic and antiinflammatorytreatment, dental disease must havehad an influence on <strong>the</strong> nasal discharge, though<strong>the</strong> improvement may have been due to suppression<strong>of</strong> secondary bacterial infection in <strong>the</strong> nasalcavity with <strong>the</strong> use <strong>of</strong> antibiotics (11). After unilateralrecurrence <strong>of</strong> <strong>the</strong> signs, inadequate healing <strong>of</strong><strong>the</strong> oronasal fistula was considered <strong>the</strong> most likelydifferential diagnosis (15). Once this was ruled outfur<strong>the</strong>r investigation was required to identify <strong>the</strong>cause. Nasal neoplasia most <strong>of</strong>ten presents initiallywith unilateral nasal discharge, epistaxis, epiphoraand facial deformity occurring in more advancedcases (11). When <strong>the</strong>re is only serous discharge andexpiratory stertor, as our case, chronic rhinitis andnasopharyngeal dysfunction have also to be considered.It is impossible to say, what <strong>the</strong> primary diseasewas or if <strong>the</strong>re is any link between <strong>the</strong> two diseasesin <strong>the</strong> present case as periodontal disease isextremely common in older small breed dogs andadenocarcinoma, although not a common condition,is seen most <strong>of</strong>ten in older dogs. Both conditionshave chronic courses, clinical signs persistingfor months (1, 6, 10, 11). It is well established thatchronic inflammation and/or infection with certainorganisms (particularly toxin producing spirochetes)prediposes to carcinoma in certain sites but <strong>the</strong>rehave not been any reports suggesting a link betweenperiodontitis and nasal carcinoma (16, 17). Oral lichenplanus, a chronic inflammatory disease seenin man is reported to be clinically associated with