Care and Maintenance to Reduce Vascular Access Complications
Care and Maintenance to Reduce Vascular Access Complications
Care and Maintenance to Reduce Vascular Access Complications
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
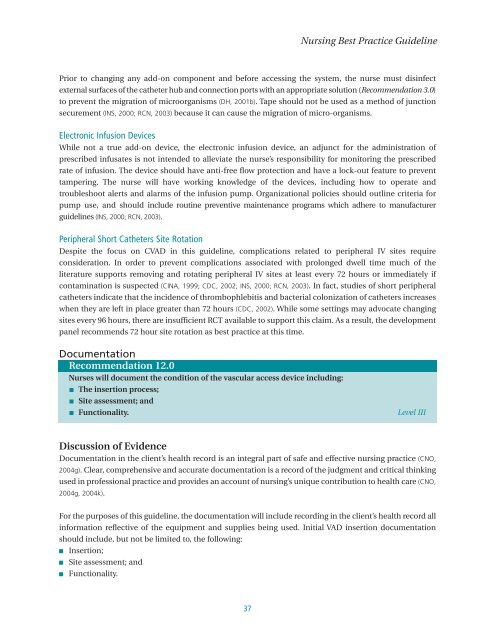
Nursing Best Practice GuidelinePrior <strong>to</strong> changing any add-on component <strong>and</strong> before accessing the system, the nurse must disinfectexternal surfaces of the catheter hub <strong>and</strong> connection ports with an appropriate solution (Recommendation 3.0)<strong>to</strong> prevent the migration of microorganisms (DH, 2001b). Tape should not be used as a method of junctionsecurement (INS, 2000; RCN, 2003) because it can cause the migration of micro-organisms.Electronic Infusion DevicesWhile not a true add-on device, the electronic infusion device, an adjunct for the administration ofprescribed infusates is not intended <strong>to</strong> alleviate the nurse’s responsibility for moni<strong>to</strong>ring the prescribedrate of infusion. The device should have anti-free flow protection <strong>and</strong> have a lock-out feature <strong>to</strong> preventtampering. The nurse will have working knowledge of the devices, including how <strong>to</strong> operate <strong>and</strong>troubleshoot alerts <strong>and</strong> alarms of the infusion pump. Organizational policies should outline criteria forpump use, <strong>and</strong> should include routine preventive maintenance programs which adhere <strong>to</strong> manufacturerguidelines (INS, 2000; RCN, 2003).Peripheral Short Catheters Site RotationDespite the focus on CVAD in this guideline, complications related <strong>to</strong> peripheral IV sites requireconsideration. In order <strong>to</strong> prevent complications associated with prolonged dwell time much of theliterature supports removing <strong>and</strong> rotating peripheral IV sites at least every 72 hours or immediately ifcontamination is suspected (CINA, 1999; CDC, 2002; INS, 2000; RCN, 2003). In fact, studies of short peripheralcatheters indicate that the incidence of thrombophlebitis <strong>and</strong> bacterial colonization of catheters increaseswhen they are left in place greater than 72 hours (CDC, 2002). While some settings may advocate changingsites every 96 hours, there are insufficient RCT available <strong>to</strong> support this claim. As a result, the developmentpanel recommends 72 hour site rotation as best practice at this time.DocumentationRecommendation 12.0Nurses will document the condition of the vascular access device including:■ The insertion process;■ Site assessment; <strong>and</strong>■ Functionality. Level IIIDiscussion of EvidenceDocumentation in the client’s health record is an integral part of safe <strong>and</strong> effective nursing practice (CNO,2004g). Clear, comprehensive <strong>and</strong> accurate documentation is a record of the judgment <strong>and</strong> critical thinkingused in professional practice <strong>and</strong> provides an account of nursing’s unique contribution <strong>to</strong> health care (CNO,2004g, 2004k).For the purposes of this guideline, the documentation will include recording in the client’s health record allinformation reflective of the equipment <strong>and</strong> supplies being used. Initial VAD insertion documentationshould include, but not be limited <strong>to</strong>, the following:■■■Insertion;Site assessment; <strong>and</strong>Functionality.37