Relationship between decile score of secondary school, the
Relationship between decile score of secondary school, the
Relationship between decile score of secondary school, the
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
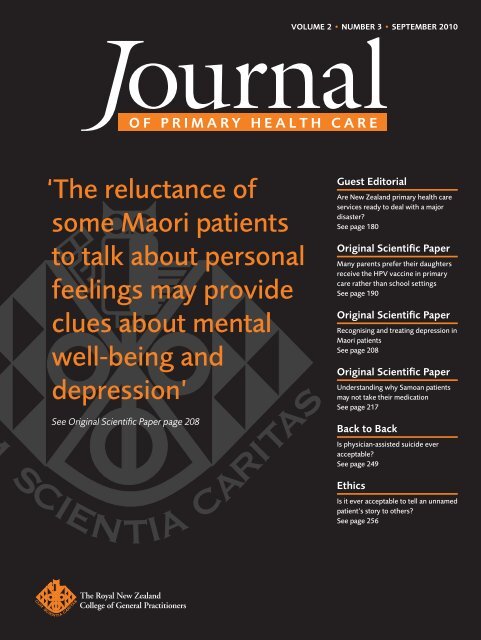
VOLUME 2 • NUMBER 3 • SEPTEMBER 2010OF PRIMARY HEALTH CARE‘The reluctance <strong>of</strong>some Maori patientsto talk about personalfeelings may provideclues about mentalwell-being anddepression’See Original Scientific Paper page 208Guest EditorialAre New Zealand primary health careservices ready to deal with a majordisaster?See page 180Original Scientific PaperMany parents prefer <strong>the</strong>ir daughtersreceive <strong>the</strong> HPV vaccine in primarycare ra<strong>the</strong>r than <strong>school</strong> settingsSee page 190Original Scientific PaperRecognising and treating depression inMaori patientsSee page 208Original Scientific PaperUnderstanding why Samoan patientsmay not take <strong>the</strong>ir medicationSee page 217Back to BackIs physician-assisted suicide everacceptable?See page 249EthicsIs it ever acceptable to tell an unnamedpatient’s story to o<strong>the</strong>rs?See page 256
EDITORIALsfrom <strong>the</strong> editorJPHC achieves MEDLINE statusFelicity Goodyear-Smith MBChB, MGP,FRNZCGP, EditorCorrespondence to:Felicity Goodyear-SmithPr<strong>of</strong>essor and GoodfellowPostgraduate Chair,Department <strong>of</strong> GeneralPractice and PrimaryHealth Care, TheUniversity <strong>of</strong> Auckland,PB 92019 Auckland,New Zealandf.goodyear-smith@auckland.ac.nzWe are delighted to announce that<strong>the</strong> Journal <strong>of</strong> Primary Health Care(JPHC) has been selected by <strong>the</strong> UnitedStates National Library <strong>of</strong> Medicine (NLM)for inclusion in Index Medicus and MEDLINE.The primary consideration in selecting journalsfor indexing is <strong>the</strong> scientific merit <strong>of</strong> a journal’scontent. The validity, importance, originality,and contribution to <strong>the</strong> coverage <strong>of</strong> <strong>the</strong> field <strong>of</strong><strong>the</strong> overall contents are key factors considered by<strong>the</strong> NLM’s selection panel in recommending ajournal for indexing.If a journal is published three or more times ayear, four issues are needed to apply for indexing.The application to NLM was made in January2010 based on <strong>the</strong> first four issues (2009, volume1, issues 1 to 4). MEDLINE indexing <strong>of</strong> <strong>the</strong> JPHChas <strong>the</strong>refore been achieved in <strong>the</strong> shortest possibletime. Throughout its 35 years <strong>of</strong> publication(1974 to 2008), <strong>the</strong> New Zealand Family Physicianwas unsuccessful in its bids to be indexed inMEDLINE. 1 One <strong>of</strong> <strong>the</strong> drivers for launching <strong>the</strong>JPHC was to create a flagship publication for <strong>the</strong>RNZCGP that would be internationally recognisedas a quality journal and obtain MEDLINEstatus.While <strong>the</strong> editor plays a substantial role, producinga journal is a team effort. This milestoneis a formal recognition <strong>of</strong> <strong>the</strong> contributionsmade by <strong>the</strong> many people who help create <strong>the</strong>journal—<strong>the</strong> authors who submit <strong>the</strong>ir work,peer reviewers who critique it, members <strong>of</strong> <strong>the</strong>editorial board who provide advice and guidance,<strong>the</strong> College staff who work to produce a firstrateprint and online journal and <strong>the</strong> readerswho provide thoughtful feedback. Many thanksto all who have played a part towards us reachingthis goal.MEDLINE is a bibliographic database containingover 18 million references to journal articles inlife sciences and biomedicine from about 5000 selectedjournals. Articles published in MEDLINEindexedjournals can be found using PubMed.Research published in non-MEDLINE journalshas little chance <strong>of</strong> being accessed and quoted byo<strong>the</strong>rs, hence it is <strong>of</strong> great value for journals tobe indexed in MEDLINE. Indexing will enablereaders to search and retrieve all JPHC articlesincluding our back issues.In 2009, Pr<strong>of</strong>essor Chris van Weel, past President<strong>of</strong> Wonca, was instrumental in <strong>the</strong> NLM introducinga new Subject Heading ‘Primary HealthCare’ (including Family Medicine) in IndexMedicus and reallocating <strong>the</strong> journals that focuson primary health care, family medicine andgeneral practice to this subject. 2 This means that<strong>the</strong> JPHC will be categorised alongside leadinggeneral practice journals such as Annals <strong>of</strong> FamilyMedicine, Family Practice and <strong>the</strong> British Journal<strong>of</strong> General Practice.Some <strong>of</strong> our readers still wish for a publicationby GPs for GPs, as attested in our Lettersto <strong>the</strong> Editor, while o<strong>the</strong>rs applaud <strong>the</strong> interdisciplinaryapproach adopted by <strong>the</strong> JPHC. Thisissue certainly continues with our cross-specialtyapproach. Authors include GPs and o<strong>the</strong>r medicalpractitioners, nurses, psychologists, pharmacists,epidemiologists and o<strong>the</strong>r assorted researchersand academics and cover a broad spectrum <strong>of</strong>primary health care issues.Mitchell and colleagues explore whe<strong>the</strong>r <strong>secondary</strong><strong>school</strong> <strong>decile</strong> rating and size <strong>of</strong> <strong>the</strong>ir town<strong>of</strong> origin has any impact on medical students’subsequent career choices such as rural generalpractice. 3 There are two studies from <strong>the</strong> team at178 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
EDITORIALsguest editorialWhile it is unlikely that <strong>the</strong>re will be a war here,recent international seismic events have raisedour awareness that, in NZ, we too are highlylikely to experience natural disasters by virtue <strong>of</strong>our geographic location on major, active tectonicplate intersections, volcanic zones and <strong>the</strong> oceanicand climatic impacts which bring tsunami, majorfloods and landslips. Climatic conditions mayalso generate circumstances for transport-relateddisasters, including road transport and aircraftcrashes as well as maritime disasters. Although<strong>the</strong>re are Civil Defence plans for immediateemergency disaster intervention, few, if any,resources appear to have been made available fortrauma treatment over <strong>the</strong> longer term.Any major disaster is accompanied by traumafor those upon whom it impacts ei<strong>the</strong>r directlyor indirectly, making <strong>the</strong>m susceptible to posttraumaticreactions <strong>of</strong> varying levels <strong>of</strong> severity.Estimates suggest PTSD will affect up to 30% <strong>of</strong>iour and academic performance <strong>of</strong> children andadolescents. 1,7 The Georgian experience has beenthat PTSD also has economic and social impactson adults, with observed increases in alcoholand drug abuse, depression and family violence.These impacts affected adults’ ability to care forchildren and also those normally expected towork with <strong>the</strong>m, such as teachers and communityhealth providers. 8There is an extensive body <strong>of</strong> evidence supportingtrauma-focussed CBT as <strong>the</strong> most effectiveintervention for post-traumatic symptoms. 4,5,9,10There is also evidence that such CBT is also<strong>the</strong> intervention <strong>of</strong> choice when working withtraumatised children, 11 including those as youngas two years old. 12Given that only a small proportion <strong>of</strong> NZ’smental health pr<strong>of</strong>essionals is trained to providetrauma-focussed CBT interventions, it is likelyHealth pr<strong>of</strong>essionals resident in a disaster area may be able toprovide an initial response, but it has to be recognised that, in anymajor disaster, locals are <strong>the</strong>mselves frequently traumatised andthus less well able to deliver an effective servicedisaster victims. 1 Because <strong>of</strong> delayed reactions andfactors associated with disruption <strong>of</strong> normal life,displacement from home, exposure to death orinjury <strong>of</strong> family members, loss <strong>of</strong> employment oro<strong>the</strong>r family stressors, PTSD symptoms may continueto emerge over periods as long as six monthsto two years post-disaster. 1,2 Research indicatesthat those most susceptible to development <strong>of</strong>PTSD are children, women and <strong>the</strong> elderly, whichis not to suggest that males are immune as <strong>the</strong>military data on male PTSD indicate. 4,5Post-disaster studies <strong>of</strong> children exposed to <strong>the</strong>effects <strong>of</strong> earthquakes, floods, tornados and <strong>the</strong>9/11 terror attack show that <strong>the</strong>y are particularlysusceptible to PTSD. 2,3,6,7 These effects aredurable, especially if untreated, being evidentfor at least three years afterwards. The impacts<strong>of</strong> PTSD are found to affect both <strong>school</strong> behavthateven fewer primary health care pr<strong>of</strong>essionalswill have had such training. As a result,provision <strong>of</strong> an effective response to moderateto severe trauma effects will be unlikely unlesssome consideration is given to training a cadre<strong>of</strong> pr<strong>of</strong>essionals who would <strong>the</strong>n be availableto respond to <strong>the</strong> traumatic aftermath <strong>of</strong> anymajor disaster. Health pr<strong>of</strong>essionals resident ina disaster area may be able to provide an initialresponse, but it has to be recognised that, in anymajor disaster, locals are <strong>the</strong>mselves frequentlytraumatised and thus less well able to deliver aneffective service.We identified a number <strong>of</strong> lessons for primaryhealth providers from <strong>the</strong> Russian–Georgianconflict and from <strong>the</strong> research literature thatcould be considered relevant to <strong>the</strong> NZ context inpreparing for a natural disaster.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 181
EDITORIALsguest editorialFirst, an initial emergency response, while helpful,is insufficient to provide significant benefitsfor persons suffering from moderate to severepost-traumatic effects, particularly as PTSD can,by definition, only be diagnosed at least fourweeks after exposure to <strong>the</strong> traumatic experience. 13Second, children and <strong>the</strong> elderly are <strong>the</strong> mostvulnerable to <strong>the</strong> development <strong>of</strong> post-traumaticsymptoms, females are more susceptible thanmales, and post-traumatic symptoms have amajor impact upon children’s academic performance,particularly concentration, memory, andclassroom demeanour and upon adults’ ability t<strong>of</strong>unction normally.Third, <strong>the</strong>re were cultural and gender differencesin symptom expression. In <strong>the</strong> cultural context,increases in somatic complaints (e.g. headaches,stomach pains) were noted, along with complaints<strong>of</strong> ‘illness’. Cultural beliefs around mental illnessmade somatic symptoms a more acceptable mode<strong>of</strong> expressing stress and trauma than reporting‘mental’ symptoms such as anxiety, phobias,panic reactions or re-experiencing. In terms <strong>of</strong>gender, boys tended to display post-traumaticproblems through increases in <strong>the</strong>ir aggressiveplay, disobedience and displays <strong>of</strong> anger, aggressionor anxiety (externalising), while girls tendedto become withdrawn, depressed or anxious andless able to focus on <strong>school</strong> work (internalising).Women <strong>of</strong>ten expressed concerns about <strong>the</strong> menand children ra<strong>the</strong>r than <strong>the</strong>ir own symptoms,and tried to avoid discussing <strong>the</strong> situation thatcaused <strong>the</strong> trauma. Men were more likely to denyany traumatic symptoms and to avoid treatment,while at <strong>the</strong> same time demonstrating increasesin drinking, smoking, anger and sleeplessness.Substance abuse and domestic violence increasedamongst displaced and unemployed males, affectingboth women and children in <strong>the</strong>ir familieswho already were living in very stressful circumstances.Males displaying trauma symptoms<strong>of</strong>ten denied trauma or avoided engaging withtreatment services. The emergency service andmilitary personnel exposed to <strong>the</strong> conflict werenot immune from trauma effects, but frequentlyfailed to seek assistance or be <strong>of</strong>fered it.Fourth, we found that, with our novice pr<strong>of</strong>essionals,key CBT trauma intervention skillscould be taught to a level <strong>of</strong> mastery relativelyeasily and in a short time (six weeks), whichmade effective intervention available for thosewho accepted treatment. Our trainee <strong>the</strong>rapistsfound that CBT produced rapid beneficial effectswith adults and children, even in cases <strong>of</strong> severePTSD symptoms and <strong>of</strong>ten after relatively briefexposure to treatment, so that symptoms such asavoidance, re-experiencing, insomnia and panicattacks became manageable, allowing normalfunctioning to be achieved.Our conclusion was that it would make sense totrain a cadre <strong>of</strong> primary health care personnelto deliver CBT for trauma so that NZ was wellprepared for <strong>the</strong> effects <strong>of</strong> any major disaster onits own shores and better able to <strong>of</strong>fer assistanceto nearby Pacific countries experiencing naturaldisasters.References1. Kruczek T, Salsman J. Prevention and treatment <strong>of</strong> posttraumaticstress disorder in <strong>the</strong> <strong>school</strong> setting. Psychol Sch.2006;43(4):461–470.2. Bal A. Post-traumatic stress disorder in Turkish child and adolescentsurvivors three years after <strong>the</strong> Marmara earthquake.Child Adolesc Ment Health. 2008;13(3):134–139.3. Bokszcanin A. PTSD symptoms in children and adolescents28 months after a flood: age and gender differences. J TraumaStress. 2007;20(3):347–351.4. Briere J, Scott C. Principles <strong>of</strong> trauma <strong>the</strong>rapy: symptoms,evaluation and treatment. New York: Sage Publications; 2006.5. Taylor S. Clinician’s guide to PTSD: a cognitive-behavioralapproach. New York: Guilford Press; 2006.6. Evans LG, Oehler-Stinnett J. Structure and prevalence <strong>of</strong> PTSDsymtomology in children who have experienced a severetornado. Psychol Sch. 2006;43(3):283–295.7. Sahin NH, Batigun AD, Yilmaz B. Psychological symptoms <strong>of</strong>Turkish children and adolescents after <strong>the</strong> 1999 earthquake:exposure, gender, location and time duration. J Trauma Stress.2007;20(3):335–345.8. World Health Organization. Unpublished report by <strong>the</strong> GeorgianWHO Mental Health Cluster Survey <strong>of</strong> IDP communitiesin conflict zones and collection centres in Georgia; 2009.9. Foa EB, Keane TM, Friedman MJ, editors. Effective treatmentsfor PTSD. New York: Guilford Press; 2000.10. Zayfert C, Becker CB. Cognitive-behavioral <strong>the</strong>rapy forPTSD: a case formulation approach. New York: GuilfordPress; 2007.11. Cohen J A, Mannarino AP, Deblinger E. Treating trauma andtraumatic grief in children and adolescents. New York: GuilfordPress; 2006.12. Scheeringa MS, Salloum A, Arnberger RA, Weems CF,Amaya-Jackson L, Cohen JA. Feasibility and effectiveness <strong>of</strong>cognitive-behavioral <strong>the</strong>rapy for post traumatic stress disorderin pre<strong>school</strong> children: Two case reports. J Trauma Stress.2007;20(4):631–636.13. American Psychiatric Association Diagnostic and StatisticalManual. 4th Ed. (Text Revision) (DSM-IV-TR). WashingtonDC; 2000.182 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPErSquantitative research<strong>Relationship</strong> <strong>between</strong> <strong>decile</strong> <strong>score</strong> <strong>of</strong><strong>secondary</strong> <strong>school</strong>, <strong>the</strong> size <strong>of</strong> town <strong>of</strong> originand career intentions <strong>of</strong> New Zealandmedical studentsClinton J Mitchell MBChB, Med;¹ Boaz Shulruf PhD,² Phillippa J Poole BSc, MBChB¹ABSTRACTintroduction: New Zealand is facing a general practice workforce crisis, especially in rural communities.Medical <strong>school</strong> entrants from low <strong>decile</strong> <strong>school</strong>s or rural locations may be more likely to chooserural general practice as <strong>the</strong>ir career path.1Medical Education Division,The University <strong>of</strong> Auckland,Auckland, New Zealand2Centre for Medical andHealth Sciences Education,The University <strong>of</strong> AucklandAim: To determine whe<strong>the</strong>r a relationship exists <strong>between</strong> <strong>secondary</strong> <strong>school</strong> <strong>decile</strong> rating, <strong>the</strong> size <strong>of</strong> <strong>the</strong>town <strong>of</strong> origin <strong>of</strong> medical students and <strong>the</strong>ir subsequent medical career intentions.Methods: University <strong>of</strong> Auckland medical students from 2006 to 2008 completed an entry questionnaireon a range <strong>of</strong> variables thought important in workforce determination. Analyses were performed ondata from <strong>the</strong> 346 students who had attended a high <strong>school</strong> in New Zealand.Results: There was a close relationship <strong>between</strong> size <strong>of</strong> town <strong>of</strong> origin and <strong>decile</strong> <strong>of</strong> <strong>secondary</strong> <strong>school</strong>.Most students expressed interests in a wide range <strong>of</strong> careers, with students from outside major citiesmaking slightly fewer choices on average.DISCUSSION: There is no strong signal from <strong>the</strong>se data that career speciality choices will be determinedby <strong>decile</strong> <strong>of</strong> <strong>secondary</strong> <strong>school</strong> or size <strong>of</strong> town <strong>of</strong> origin. An increase in <strong>the</strong> proportion <strong>of</strong> rural students inmedical programmes may increase <strong>the</strong> number <strong>of</strong> students from lower <strong>decile</strong> <strong>school</strong>s, without addingano<strong>the</strong>r affirmative action pathway.KEYWORDS: Education, medical; social class; career choiceBackgroundSome <strong>of</strong> <strong>the</strong> most important decisions in <strong>the</strong>shaping <strong>of</strong> <strong>the</strong> future medical workforce relate to<strong>the</strong> selection <strong>of</strong> medical students. There is a socialobligation on universities to facilitate <strong>the</strong> development<strong>of</strong> a wide range <strong>of</strong> medical practitioners tomeet <strong>the</strong> health needs <strong>of</strong> <strong>the</strong> population.It is likely that medical graduates from diversebackgrounds would address priority areas <strong>of</strong>need and result in <strong>the</strong> range <strong>of</strong> doctors needed. 1–3Diversification also allows equity <strong>of</strong> access forminority groups. For around 40 years, Maoriand Pacific medical student admission schemeshave been in place to redress <strong>the</strong> lack <strong>of</strong> minorityrepresentation within <strong>the</strong> medical workforce.Around 16% <strong>of</strong> <strong>the</strong> current Auckland studentbody identifies as Maori or Pacific (Medical ProgrammeDirectorate, The University <strong>of</strong> Auckland,personal communication). Since 2004, TheUniversity <strong>of</strong> Auckland has <strong>of</strong>fered places to 20students <strong>of</strong> rural origin. Evidence suggests <strong>the</strong>sestudents will be more likely to return to practisein rural settings. 4,5 In recent years in <strong>the</strong> UnitedKingdom, a number <strong>of</strong> efforts have been made togive students from lower socioeconomic backgrounds<strong>the</strong> opportunity to become doctors. 6 Fewstudies have reported on <strong>the</strong> career pathways andchoices <strong>of</strong> individuals from low socioeconomiccommunities.J PRIMARY HEALTH CARE2010;2(3):183–189.CORRESPONDENCE TO:Phillippa PooleAssociate Pr<strong>of</strong>essor,Medical EducationDivision, School <strong>of</strong>Medicine, Faculty <strong>of</strong>Medical and HealthSciences, The University<strong>of</strong> Auckland, PB 92019Auckland 1142,New Zealandp.poole@auckland.ac.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 183
ORIGINAL SCIENTIFIC PAPERSquantitative researchcould classify practising doctors. Although anopen field was also included, in all instancesresponses could be attributed to one <strong>of</strong> <strong>the</strong> 18options.The careers in which students indicated an interestin working were analysed by high <strong>school</strong><strong>decile</strong> and by size <strong>of</strong> town <strong>of</strong> origin. Odds ratios(OR) and 95% confidence intervals (CI) were calculated;instances where <strong>the</strong> OR value +/- 95% CIdid not cross 1.00 were deemed significant. O<strong>the</strong>rtechniques included logistic regression and crosstabulation.Statistical analyses were preparedusing SPSS for Windows Version 16.0.ResultsData were available from 397 medical studentsin <strong>the</strong> entry cohorts 2006 to 2008, which wasan 82% return rate. Of this cohort, 51 sets <strong>of</strong>data were excluded where <strong>the</strong> <strong>secondary</strong> <strong>school</strong>attended by <strong>the</strong> student was overseas or <strong>the</strong> NewZealand Correspondence School.There was a marked preponderance <strong>of</strong> studentsfrom <strong>decile</strong> 9 and 10 <strong>school</strong>s (see Figure 1). Itshould be noted that <strong>the</strong> number <strong>of</strong> year 13 studentsin each <strong>decile</strong> nationwide is not uniform;in fact <strong>decile</strong> 9 and 10 students make up 30%<strong>of</strong> year 13 students in New Zealand (Centre forMedical and Health Sciences Education, personalcommunication).The average <strong>decile</strong> <strong>of</strong> <strong>the</strong> <strong>school</strong>s for studentsfrom a major city was 8.1 compared with 6.4 and6.3 for provincial centre and small town respectively.By far, <strong>the</strong> largest number <strong>of</strong> city-origin studentscame from Auckland; Hamilton, Wellington andChristchurch were also represented. Over <strong>the</strong>three-year period <strong>of</strong> <strong>the</strong> study, students camefrom 120 <strong>school</strong>s throughout New Zealand.Students made a mean <strong>of</strong> 9.75 expressions <strong>of</strong>interest from <strong>the</strong> possible 18 career choices. Ingeneral, students from lower <strong>decile</strong> <strong>school</strong>s and/or smaller towns made fewer choices (Tables 2and 3), although this exceeded <strong>the</strong> significancelevel <strong>of</strong> 0.05 only for town size when analysis <strong>of</strong>variance was used.WHAT GAP THIS FILLSWhat we already know: Students from impoverished backgrounds arerare in medical student classes. The current retention crisis in New Zealand isuntenable, especially in rural communities.What this study adds: Seventy-two percent <strong>of</strong> students indicated aninterest in general practice on entry to medical <strong>school</strong>. An increase in <strong>the</strong>number <strong>of</strong> medical students from lower socioeconomic and rural areas mayhave <strong>the</strong> benefit <strong>of</strong> an added number <strong>of</strong> students choosing to practise incertain specialties, including general practice.When <strong>the</strong> data <strong>of</strong> students from small towns andprovincial centres were combined, students frommajor cities made more choices (10.20 (SD 5.4)versus 8.15 (SD 5.9); p
ORIGINAL SCIENTIFIC PAPErSquantitative researchNone<strong>the</strong>less, some differences were seen in <strong>the</strong>patterns <strong>of</strong> choice among students from differentbackgrounds.The major differences emerged in an analysiscomparing students who came from high <strong>decile</strong><strong>school</strong>s in major cities and those in <strong>the</strong> remaininggroups. Students from high <strong>decile</strong> <strong>school</strong>s weremore likely to signal an interest in most specialties(Figure 5) and <strong>the</strong>y were twice as likely aso<strong>the</strong>r students to signal an interest in medicineand surgery and respective subspecialties.DiscussionThere was a strong relationship <strong>between</strong> <strong>the</strong><strong>decile</strong> <strong>of</strong> a <strong>secondary</strong> <strong>school</strong> and <strong>the</strong> size <strong>of</strong> townFigure 2. Location <strong>of</strong> origin <strong>of</strong> University <strong>of</strong> Auckland medical students by regions <strong>of</strong>New Zealand and size <strong>of</strong> town.<strong>of</strong> origin. The average <strong>decile</strong> <strong>of</strong> <strong>the</strong> <strong>school</strong>s <strong>of</strong>‘major city’ students was two <strong>decile</strong> points higherthan <strong>the</strong>ir provincial/small town counterparts.These variables were associated with a relativelyminor effect on intended medical career choices.The majority <strong>of</strong> students came from <strong>the</strong> greaterAuckland region and <strong>the</strong> upper North Island.There was a very wide range <strong>of</strong> <strong>secondary</strong> <strong>school</strong><strong>of</strong> origin—this is in contrast to a common viewthat most students in <strong>the</strong> Auckland programmecome from a limited number <strong>of</strong> city <strong>school</strong>s inAuckland. We were encouraged to find over 11%came from areas with a population <strong>of</strong> 10 000 orless. To put <strong>the</strong>se findings in context, a studyfrom <strong>the</strong> University <strong>of</strong> Otago found that 84.5%came from main urban areas, while only 2.9%came from rural areas. 11 This observation may bean indication that <strong>the</strong> rural entry programmesintroduced in 2004 are having <strong>the</strong> desired effecton diversification.With <strong>the</strong> limitation that <strong>the</strong> <strong>decile</strong> <strong>of</strong> a high<strong>school</strong> can at most be an approximation <strong>of</strong> <strong>the</strong>socio economic status <strong>of</strong> an individual student,it was encouraging that 45% <strong>of</strong> students in <strong>the</strong>study reported <strong>the</strong>y did not attend <strong>decile</strong> 9 or10 <strong>school</strong>s. Traditionally, medical students havecome largely from upper socio economic groups. 12Even though students aiming for medical <strong>school</strong>are, by and large, capable students, it is stilllikely that <strong>the</strong> academic and personal preparationneeded during final years <strong>of</strong> high <strong>school</strong> and<strong>the</strong> admissions process unduly favour studentsfrom higher <strong>decile</strong> <strong>school</strong>s. Both universities nowselect students after at least one year at universityfor a number <strong>of</strong> reasons, one <strong>of</strong> which is thatthis may allow capable students who seek entryto medicine to compete on relatively level terms,regardless <strong>of</strong> socio economic status and location <strong>of</strong>high <strong>school</strong>.Thompson and Subich have recently discernedthat social status was predictive <strong>of</strong> ‘career decisionself-efficacy’, 13 and extended upon previousfindings that <strong>the</strong> range and implementation <strong>of</strong>choices was also affected by social status. 13,14At <strong>the</strong> opposite end <strong>of</strong> <strong>the</strong> spectrum, studentsperceiving <strong>the</strong>mselves as having greater economicresources compared with <strong>the</strong>ir peers reportedmore certainty in, and comfort with, career186 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSquantitative researchFigure 3. Odds ratio for students from low (left) or middle (right) <strong>decile</strong> <strong>school</strong>s choosing a particular specialty compared with those from high <strong>decile</strong> <strong>school</strong>s.Figure 4. Odds ratio for students from small towns (left) or provincial centres (right) choosing a particular specialty compared with those from major cities.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 187
ORIGINAL SCIENTIFIC PAPErSquantitative researchFigure 5. Odds ratio (OR) for students from high <strong>decile</strong> <strong>school</strong>s in major cities choosing aparticular specialty compared with those from all o<strong>the</strong>r areas and <strong>decile</strong>s.choices. 13 A different effect was seen with thiscohort <strong>of</strong> students. We found that NZ domesticstudents entering medical <strong>school</strong> in Aucklandare enthusiastic about <strong>the</strong> range open to <strong>the</strong>m; onaverage, students rate an interest in nearly 10 <strong>of</strong><strong>the</strong> 18 options available to <strong>the</strong>m. Students fromlower <strong>decile</strong> <strong>school</strong>s, provincial centres and smalltowns made fewer choices. The implication <strong>of</strong>this finding is not yet clear and <strong>the</strong>re are severalpossible explanations. There may be a lack <strong>of</strong>awareness in <strong>the</strong>se groups <strong>of</strong> <strong>the</strong> potential careerswithin medicines, or deliberate strategies used bystudents from larger towns/higher <strong>decile</strong>s to keepmany options open. An alternative hypo<strong>the</strong>sis isthat students from lower <strong>decile</strong>s or smaller townsmay be more definite about what <strong>the</strong>y do and donot want to do in medicine.Studies have shown that only a minority <strong>of</strong>students (45%) correctly identified <strong>the</strong>ir lateractual choice <strong>of</strong> specialty prior to <strong>the</strong>ir first day<strong>of</strong> lectures. 15 There were few strong and consistentpatterns in <strong>the</strong> intended careers <strong>of</strong> medicalstudents’ intention at entry due to <strong>the</strong> fact that<strong>the</strong>re were relatively small numbers <strong>of</strong> studentsin <strong>the</strong> survey and a wide range <strong>of</strong> choices available.However, we found that students from high<strong>decile</strong> <strong>school</strong>s in major cities were over twice aslikely to signal an interest in medicine and/orsurgery and <strong>the</strong>ir subspecialties. In five <strong>of</strong> <strong>the</strong>18 specialties, including <strong>the</strong> clinical specialties<strong>of</strong> geriatrics, general practice and obstetrics andgynaecology, <strong>the</strong>re was no significant differencein preferences <strong>between</strong> any <strong>of</strong> <strong>the</strong> student groupsin this study.A positive finding was that 250 <strong>of</strong> <strong>the</strong> 346students (72%) indicated an interest in generalpractice, a priority specialty area in NZ. Areasin NZ with high chronic disease burdens areover-represented by low <strong>decile</strong> <strong>school</strong>s and underservedby GPs. In Counties-Manukau, 65.5%<strong>of</strong> <strong>school</strong>s are <strong>decile</strong> 4 or below; 16 <strong>the</strong>re are 280general practitioners for every 100 000 population,compared with 425 for <strong>the</strong> same populationin Auckland DHB. 17 Vaglum found that studentsinterested in a career in family medicine at entryto medical <strong>school</strong> were motivated by status/security,more so than for any o<strong>the</strong>r career. They postulatedthat students coming from a lower ‘socialorigin’ may be more aware <strong>of</strong> a change in statusand/or security that accompanies being a doctor. 18This present study, however, does not supportthis notion—students from all groups signalledan interest in general practice similarly.Time will allow <strong>the</strong> testing <strong>of</strong> <strong>the</strong> <strong>secondary</strong>hypo<strong>the</strong>ses generated from this study that studentsfrom smaller centres/lower <strong>decile</strong> <strong>school</strong>sare more accurate in <strong>the</strong>ir predictions <strong>of</strong> careerchoices, and that students from high <strong>decile</strong> city<strong>school</strong>s are twice as likely to become NZ’s futurephysicians and surgeons.The students entering <strong>the</strong> programme now willnot be specialists until at least 2020. A strategy<strong>of</strong> seeking to ‘grow our own’ health pr<strong>of</strong>essionalsseems appropriate. Zayas opines that pr<strong>of</strong>essionalspractising in <strong>the</strong>ir home communities aremore cognisant <strong>of</strong>, and sensitive to, local needs. 19For us to achieve this will require overcoming<strong>the</strong> perception that students from lower socioeconomicgroups identify medical <strong>school</strong> as ‘culturallyalien and “posh”; few consider <strong>the</strong>y haveany chance <strong>of</strong> ever gaining a place’. 20 Selection188 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSquantitative researchprocesses and pathways must continue to enhance<strong>the</strong> prospects <strong>of</strong> a medical career for studentsfrom outer metropolitan areas and beyond, andfrom lower <strong>decile</strong> <strong>school</strong>s.The announcement <strong>of</strong> an imminent increase inmedical student numbers provides both medical<strong>school</strong>s with <strong>the</strong> impetus to review and possiblyamend admission policies. Given that half <strong>of</strong>NZ’s population live in <strong>the</strong> upper North Island,recruiting strategies for The University <strong>of</strong> Aucklandmight target outer metropolitan, regionaland rural <strong>school</strong>s in this region. Because <strong>of</strong> <strong>the</strong>strong relationship <strong>between</strong> <strong>the</strong> <strong>school</strong> <strong>decile</strong>and rurality identified in this study, an increasein <strong>the</strong> proportion <strong>of</strong> students from outside majorcities in <strong>the</strong> rural origin pathway would have <strong>the</strong>corollary <strong>of</strong> more students coming from lower<strong>decile</strong> <strong>school</strong>s. It might not be necessary to haveano<strong>the</strong>r specific pathway. Over time, we hope tohelp shed light on this debate.14. Blustein DL, Chaves AP, Diemer MA, Gallagher LA, et al.Voices <strong>of</strong> <strong>the</strong> forgotten half: <strong>the</strong> role <strong>of</strong> social class in <strong>the</strong><strong>school</strong>-to-work transition. J Couns Psychol. 2002;49:311–323.15. Zedlow PB, Preston RC, Daugherty SR. The decision toenter a medical specialty: timing and stability. Med Educ.1992;26:327–32.16. Big Cities. School <strong>decile</strong> ratings. [document on <strong>the</strong> Internet].Quality <strong>of</strong> Life ’08; 2008 [cited 19 December, 2008]. Availablefrom: http://www.bigcities.govt.nz/pdf2001/<strong>decile</strong>.pdf.17. Medical Council <strong>of</strong> New Zealand. The New Zealand medicalworkforce in 2007. Wellington: Medical Council <strong>of</strong> NewZealand; 2007.18. Valgum P, Wiers-Jenssen J, Ekeberg O. Motivation for medical<strong>school</strong>: <strong>the</strong> relationship to gender and specialty preferences ina nationwide sample. Med Educ. 1999;33:236–42.19. Zayas LE, McGuigan D. Experiences promoting healthcarecareer interest among high-<strong>school</strong> students from underservedcommunities. J Natl Med Assoc. 2006;98(9):1523–1531.20. Ma<strong>the</strong>rs J, Parry J. Why are <strong>the</strong>re so few working-class applicantsto medical <strong>school</strong>s? Learning from <strong>the</strong> success stories.Med Educ. 2009;43:21–228.References1. Angel CV, Johnson A. Broadening access to undergraduatemedical education. BMJ. 2000;321:1136–8.2. Lakhan SE. Diversification <strong>of</strong> U.S. medical <strong>school</strong>s via affirmativeaction implementation. BMC Med Educ. 2003;3:6.3. Komaromy M, Grumbach K, Drake M. The role <strong>of</strong> Black andHispanic physicians in providing health care for underservedpopulations. New Engl J Med. 1997;4:1305–1310.4. Easterbrook M, Godwin M, Wilson R, Hodgetts G et al. Ruralbackground and clinical rotations during medical training:effect on practice location. CMAJ. 1999;160:1159–63.5. Hsueh W, Wilkinson T, Bills J. What evidence-based undergraduateinterventions promote rural health? N Z Med J.2004;117(1204):U1117.6. Garlick PB, Brown G. Widening participation in medicine.BMJ. 2008;336:1111–1113.7. Medical Training Board. Collation <strong>of</strong> discussion papers released30 September 2008. Wellington: Government PublishingService; 2008.8. Ministry <strong>of</strong> Education. How <strong>the</strong> <strong>decile</strong> is calculated [documenton <strong>the</strong> Internet]. Wellington: MOH; 2008 [cited 19 December,2008]. Available from: http://www.minedu.govt.nz/educationSectors/Schools/SchoolOperations/Resourcing/OperationalFunding/Deciles/HowTheDecileIsCalculated.aspx.9. Roulston D. Educational policy change, newspapers andpublic opinion in New Zealand, 1988–1999. Victoria University<strong>of</strong> Wellington: Wellington; 2005.10. Shulruf B, Hattie J, Tumen S. Individual and <strong>school</strong> factorsaffecting students’ participation and success in higher education.J Higher Educ. 2008;56(5):613–632.11. Heath C, Stoddart C, Renwick J. Urban and rural origins <strong>of</strong>Otago Medical students. N Z Med J. 2002;115(1165).12. Heath C, Stoddart C, Green H. Parental backgrounds <strong>of</strong> Otagomedical students. N Z Med J. 2002;115(1165):U233.13. Thompson MN, Subich LM. The relation <strong>of</strong> social statusto <strong>the</strong> career decision-making process. J Vocat Behav.2006;96:289–301.COMPETING INTERESTSNone declared.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 189
ORIGINAL SCIENTIFIC PAPERSquantitative researchbegan at <strong>the</strong> start <strong>of</strong> <strong>the</strong> 2009 <strong>school</strong> year <strong>of</strong>feringvaccination to girls in Year 8 and above(12 years up). Administration <strong>of</strong> <strong>the</strong> Gardasil ®vaccine is recommended at an early age asyounger girls mount a greater antibody responseand <strong>the</strong>refore may be afforded better protectionagainst <strong>the</strong> virus, 3 and vaccination prior to sexualdebut ensures girls have not already been exposedto <strong>the</strong> virus. 4In NZ, Maori and Pacific women have <strong>the</strong> highestincidence <strong>of</strong> cervical cancer and a poorerprognosis once diagnosed. 5,6 Disparities have alsobeen reported in access to both screening (breastand cervical) and immunisation for Maori andPacific women. 5–7 The National HPV immunisationimplementation plan <strong>the</strong>refore recognisesMaori and Pacific as priority groups for vaccination,with additional funding provided to DHBsto address <strong>the</strong>se priority groups. 8 To achieve highuptake, and to minimise <strong>the</strong> risk <strong>of</strong> increasing inequalitiesfor both Maori and Pacific, we need anunderstanding <strong>of</strong> those factors that may increase,or conversely hinder, widespread coverage.Studies have been conducted overseas to exploreparental attitudes towards <strong>the</strong> new HPV/cervicalcancer vaccine. 9–19 NZ research has exploredparental views towards o<strong>the</strong>r childhood vaccines,and barriers to vaccination. 20–23 Place <strong>of</strong> vaccinationis an important factor when consideringaccess and uptake; <strong>the</strong> success <strong>of</strong> <strong>the</strong> MeNZB TMprogramme that was predominately <strong>school</strong>-based(for five- to 17-year-olds) played a role in <strong>the</strong>decision to deliver Gardasil ® via <strong>school</strong>s, despitedifferences in <strong>the</strong> nature <strong>of</strong> <strong>the</strong> disease targetedby <strong>the</strong>se vaccines. 8 Non-return <strong>of</strong> signed consentforms prohibits receipt <strong>of</strong> <strong>the</strong> vaccine. Analysis<strong>of</strong> data from one DHB region on receipt <strong>of</strong> <strong>the</strong>11-year-old vaccine (dip<strong>the</strong>ria/tetanus/whoopingcough) showed that Maori were significantly lesslikely to return consent forms than non-Maori. 23By contrast, consent form return rates were highfor Maori in <strong>the</strong> MeNZB TM programme. 8The cervical cancer vaccine differs from o<strong>the</strong>rson <strong>the</strong> immunisation schedule in a number<strong>of</strong> important ways. For example, it targets aninfection that is sexually transmitted and ismost effective when administered prior to sexualonset, it reduces likelihood <strong>of</strong> developing aWHAT GAP THIS FILLSWhat we already know: The HPV/cervical cancer vaccine has <strong>the</strong> potentialto reduce current disparities in cervical cancer incidence for Maori andPacific if high uptake is achieved. The vaccine will be delivered via a <strong>school</strong>basedprogramme in most areas <strong>of</strong> New Zealand to girls in Year 8 and above.What this study adds: Parents indicated a preference for <strong>the</strong>ir daughters’receipt <strong>of</strong> <strong>the</strong> HPV/cervical cancer vaccine in primary care, and many wouldseek <strong>the</strong> views <strong>of</strong> <strong>the</strong>ir GP before making a decision about vaccination for<strong>the</strong>ir daughter(s). The rationale for vaccination at a young age needs to be explainedclearly and information provided in a way that is accessible to parentsfrom all backgrounds.time-distant disease, and is currently only availablefor girls. Given <strong>the</strong> unique nature <strong>of</strong> thisvaccine, we aimed to explore factors that mightimpact on uptake, including: parents’ preferenceson where <strong>the</strong>ir daughter(s) receive <strong>the</strong> vaccineand at what age; age-appropriate informationfor girls; information needed to assist parentswith decision-making; parental contact regardingconsent and information-sharing <strong>between</strong> <strong>school</strong>and primary care.MethodsThe study was approved by <strong>the</strong> Central RegionEthics Committee on 17 June 2008(CEN/08/04/014). Surveys were distributed to<strong>school</strong>s in October and November in term 4 <strong>of</strong><strong>the</strong> 2008 <strong>school</strong> year. Return <strong>of</strong> a completedsurvey signified a parent’s consent to participate;surveys were received up until <strong>the</strong> end <strong>of</strong> January2009. Questions were developed based on findingsfrom key informant interviews conductedwith parents, similar work conducted overseasand local attitudinal research on immunisation.20–22 Surveys were piloted with 15 participants,and modified following feedback on clarityand ambiguity in question formatting.Recruitment and distribution <strong>of</strong> surveysEligibility criteria for <strong>school</strong>s included: locatedin Wellington, more than 100 pupils (with <strong>the</strong>exception <strong>of</strong> one Kura Kaupapa Maori languageimmersion <strong>school</strong> that had fewer than 100pupils), and attended by girls in Year 8 and above(intermediate and <strong>secondary</strong> <strong>school</strong>s). SchoolsVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 191
ORIGINAL SCIENTIFIC PAPErSquantitative researchwere stratified by <strong>decile</strong> rating into low (<strong>decile</strong>s1–3), medium (<strong>decile</strong>s 4–7) and high (<strong>decile</strong>s 8–10).Schools with lower ratings had higher proportions<strong>of</strong> Maori and Pacific students so were oversampledto achieve good representation <strong>of</strong> priority groups.The <strong>decile</strong> rating <strong>of</strong> a <strong>school</strong> is an indicator <strong>of</strong>socioeconomic status <strong>of</strong> <strong>the</strong> population within<strong>the</strong> <strong>school</strong>-defined area, where children attendinga <strong>decile</strong> 1 <strong>school</strong> are likely to be from a lowersocioeconomic background than those attending a<strong>decile</strong> 10 <strong>school</strong>. 24 All eligible <strong>school</strong>s in <strong>the</strong> Wellingtonarea with <strong>decile</strong> ratings <strong>between</strong> 1 and 5were invited to participate. Schools with <strong>decile</strong>ratings <strong>of</strong> 6 and above were randomly chosen (using<strong>the</strong> Excel RAND function).A letter <strong>of</strong> invitation was sent to <strong>the</strong> principal at22 <strong>of</strong> 41 eligible <strong>school</strong>s (10 low, six medium andsix high <strong>decile</strong>). Arrangements for administering<strong>the</strong> survey were made and a $50 book vouchergiven as a token <strong>of</strong> appreciation. Parents wereeligible for participation if <strong>the</strong>y had a daughterattending one <strong>of</strong> <strong>the</strong> participating <strong>school</strong>s.Surveys (with a brochure about cervical cancerand <strong>the</strong> HPV vaccine) 25 were distributed in one <strong>of</strong>two ways, as nominated by <strong>the</strong> <strong>school</strong>: girls took<strong>the</strong> survey home to <strong>the</strong>ir parents (10 <strong>school</strong>s),or <strong>the</strong> <strong>school</strong> posted <strong>the</strong> survey to parents (four<strong>school</strong>s). For three high-<strong>decile</strong> <strong>school</strong>s with largerolls, we asked <strong>school</strong>s to distribute surveys toparents <strong>of</strong> only half <strong>the</strong>ir students. Surveys werereturned directly to <strong>the</strong> researchers by freepostenvelope (eight <strong>school</strong>s), or students returned surveysto <strong>the</strong> <strong>school</strong> with small incentives <strong>of</strong>feredby <strong>the</strong> <strong>school</strong> (for example, entry into a draw towin vouchers) in an attempt to increase responserates. Reminder notices about completion andreturn <strong>of</strong> surveys were sent out by all <strong>school</strong>sin <strong>the</strong>ir newsletters and/or in daily notices. Theresearch team did not send reminders to nonrespondersas contact details for parents were notobtained due to privacy reasons.Data collection and analysisQuestionnaires collected demographic data andasked parents about <strong>the</strong>ir vaccination preferenceswith regards to age, venue and information needs,as well as <strong>the</strong> likelihood <strong>of</strong> seeking vaccinationfor <strong>the</strong>ir daughter(s). Ethnicity was collectedusing <strong>the</strong> 2001 NZ census question and wasrecoded to <strong>the</strong> following four groups: Maori, Pacific,New Zealand European (NZEu) and O<strong>the</strong>r.Assignment was based on prioritised ethnicity. 26‘Strongly agree’ and ‘agree’ responses were pooledfor analysis, as were ‘strongly disagree’ and ‘disagree’responses. Comments made to open-endedquestions were analysed for content and coded toallow for a frequency count (reason for preferenceon place <strong>of</strong> vaccination, format and content <strong>of</strong>fur<strong>the</strong>r information if desired). Kruskal-Wallistests followed by Wilcoxon pairwise comparisonswere performed in situations where data couldnot be assumed to follow a normal distribution.For <strong>the</strong>se pairwise comparisons, Bonferroni correctionswere applied to control for Type I errorresulting from multiple comparisons (significancelevel set at 0.05/n comparisons). Chi-square testswere performed to test for significant differences<strong>between</strong> categorical variables, and 95% confidenceintervals calculated where appropriate. Statisticalanalyses were performed using SAS (v9.2).ResultsFifteen <strong>of</strong> <strong>the</strong> 22 <strong>school</strong>s agreed to participate and,<strong>of</strong> those, 14 took part (six co-ed, two girls only,five intermediate and one full Kura Kaupapa Maori<strong>school</strong>) giving a population <strong>of</strong> 3123 girls in <strong>the</strong>age range. Five <strong>school</strong>s declined (all low <strong>decile</strong>) dueto ‘lack <strong>of</strong> time’, two were undecided (one highandone low-<strong>decile</strong> <strong>school</strong>) after several weeks sowere not fur<strong>the</strong>r pursued. The overall responserate from parents was 24.6% (769/3123). Co-education<strong>secondary</strong> <strong>school</strong>s had <strong>the</strong> lowest responserate (19.6%, 370/1889); followed by intermediate<strong>school</strong>s (30.5%, 215/704), <strong>the</strong> highest response ratewas parents <strong>of</strong> girls at girls-only <strong>secondary</strong> <strong>school</strong>s(35%,182/520). Participating <strong>school</strong>s were spreadacross <strong>decile</strong>s, with a response rate <strong>of</strong> 18.7% fromfour low-<strong>decile</strong> <strong>school</strong>s (157/838), 24.4% from sixmedium-<strong>decile</strong> <strong>school</strong>s (380/1560) and 32% fromfour high-<strong>decile</strong> <strong>school</strong>s (232/725).Table 1 presents <strong>the</strong> characteristics <strong>of</strong> participatingparents who returned completed surveys(n=769), with p-values denoting significantoverall differences <strong>between</strong> ethnic groups ondemographic variables using chi-square tests forsignificance. Pairwise comparisons showed thatMaori and Pacific parents were significantly more192 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSquantitative researchlikely to be younger (p
ORIGINAL SCIENTIFIC PAPErSquantitative researchTable 2. Likelihood <strong>of</strong> seeking vaccination for daughter and preferred venue and age at receipt <strong>of</strong> vaccinationWant daughter to receiveHPV vaccineTotal Maori Pacific NZEu ‘O<strong>the</strong>r’(n=769) (n=126) (n=57) (n=477) (n=109)n % n % n % n % n %(95% CI) (95% CI) (95% CI) (95% CI) (95% CI)514 66.8 84 66.7 36 63.2 323 67.7 71 65.1(63.4 – 70.2) (57.7 – 74.8) (49.3 - 75.6) (63.3 – 71.9) (55.4 – 74.0)Preferred venueClinic* 302 39.3 55 43.7 31 54.4 179 37.5 37 33.9(35.8 – 42.8) (34.8 – 52.8) (40.7 – 67.6) (33.2 – 42.0) (25.1 – 43.6)School 197 25.6 28 22.2 6 10.5 135 28.3 28 25.7(22.6 – 28.9) (15.3 – 30.5) (4.0 – 21.5) (24.3 – 32.6) (17.8 – 34.9)Clinic or <strong>school</strong> 89 11.6 17 13.5 5 8.8 56 11.7 11 10.1(9.4 – 14.0) (8.1 – 20.7) (2.9 – 19.3) (9.0 – 15.0) (5.1 – 17.3)Her choice 156 20.3 21 16.7 10 17.5 98 20.5 27 24.8(17.5 – 23.3) (10.6 – 24.3) (8.7 – 29.9) (17.0 – 24.5) (17.0 – 34.0)No preference /16 2.1 2 1.6 3 5.3 8 1.7 3 2.8Not having it(1.2 – 3.4) (0.2 – 5.6) (1.1 – 14.6) (0.7 – 3.3) (0.6 – 7.8)Preferred ageNever 22 2.9 1 0.8 4 7 12 2.5 5 4.6(1.8 – 4.3) (0.0 – 4.3) (1.9 – 17.0) (1.3 – 4.4) (1.5 – 10.4)Not sure 131 17 21 16.7 15 26.3 74 15.5 21 19.3(14.4 – 19.9) (10.6 – 24.3) (15.5 – 39.7) (12.4 – 19.1) (12.3 – 27.9)Median age 13 13 14 13 15(Interquartile range) (12 – 15) (12 – 14) (13 – 15) (12 – 15) (12.3 – 16)Age 10 years 25 3.3 12 9.5 2 3.5 11 2.3 0 0Age 11 years 24 3.1 7 5.6 1 1.8 11 2.3 5 4.6Age 12 years 167 21.7 31 24.6 5 8.8 115 24.1 16 14.7Age 13 years 121 15.7 18 14.3 5 8.8 89 18.7 9 8.3Age 14 years 88 11.4 15 11.9 7 12.3 59 12.4 7 6.4Age 15 years 76 9.9 9 7.1 9 15.8 42 8.8 16 14.7Age 16 or older 102 13.3 12 9.5 7 12.3 54 11.3 29 26.6* Includes GP or nurse clinic, Maori and Pacific health clinicsNon-return <strong>of</strong> consent formsand information-sharingThe majority <strong>of</strong> parents (87%) were happy to bephoned if <strong>the</strong>y had not returned a consent form(672/769). Few parents (8%) answered ‘no’ tobeing phoned (63/769) and only 3% were unsure.Maori (13%) and Pacific (14%) parents had aslightly higher proportion <strong>of</strong> ‘no’ responses thanNZEu (5.7%) parents (p
ORIGINAL SCIENTIFIC PAPERSquantitative researchyounger girls (causes and risks <strong>of</strong> cervical cancer,how HPV is passed on, abstinence, possible sideeffects <strong>of</strong> <strong>the</strong> vaccine, genital warts and STIs).Table 4 presents data relating to parents’ desirefor more information (o<strong>the</strong>r than <strong>the</strong> Ministry <strong>of</strong>Health brochure provided) to assist with decisionmakingabout <strong>the</strong> vaccine. Three-quarters <strong>of</strong><strong>the</strong>se parents (77%) responded to an open-endedquestion about <strong>the</strong> type <strong>of</strong> information <strong>the</strong>ywould want (184/236). Responses included: informationon side effects and risks (39/184); efficacyand long-term effects <strong>of</strong> vaccination (38/184);evidence-based research and scientific information(37/184); and safety (31/184). A few parentsalso noted <strong>the</strong>y would want ‘unbiased’ information,details about vaccine contents, updated informationabout <strong>the</strong> programme, and informationon whe<strong>the</strong>r a booster is needed at five years.DiscussionParents indicated a greater preference for delivery<strong>of</strong> <strong>the</strong> Gardasil ® vaccine in clinic ra<strong>the</strong>r than<strong>school</strong> settings. Reasons for clinic-based vaccinationwere, most frequently, that it would allowfor continuity <strong>of</strong> care (from <strong>the</strong> family GP),enable parental involvement and <strong>the</strong> opportunityfor parents to provide comfort and support to<strong>the</strong>ir daughter. Given that <strong>the</strong> HPV vaccinationprogramme will be run predominantly through<strong>school</strong>s, enabling girls to have whanau/familysupport on vaccination day at <strong>school</strong> might bebeneficial. Parents also need to be encouraged toseek vaccination for <strong>the</strong>ir daughter(s) through primarycare if that is <strong>the</strong>ir preference. Conveniencewas cited as a key reason for preferring <strong>school</strong>baseddelivery. In a previous study, parents expresseda preference for delivery <strong>of</strong> childhood immunisations(meningococcal disease and measles)in general practice, with <strong>the</strong> exception <strong>of</strong> Pacificparents who preferred <strong>school</strong>-based delivery 20 —afinding that differs from <strong>the</strong> current study.Just over a quarter <strong>of</strong> parents (28%) thought ages10–12 appropriate for receipt <strong>of</strong> <strong>the</strong> vaccine. Parents<strong>of</strong> Pacific and ‘O<strong>the</strong>r’ ethnicities were morelikely to indicate a preference for older age at re-Table 3. Information deemed appropriate for girls when discussing <strong>the</strong> HPV vaccineWhat should be discussed withgirls aged 12–15, and girls aged 16and older?*Topic (n responding to question)‘Yes’ responses presented by age groupBoth age groups 16 years and older only 12 to 15 years only Nei<strong>the</strong>r age groupn % n % n % n %(95% CI) (95% CI) (95% CI) (95% CI)Cervical cancer—causes and risks 615 95.3 28 4.3 1 0.2 1 0.2(645) (93.4 – 96.8) (2.9 – 6.2) (0.0 – 0.9) (0.0 – 0.9)HPV: What it is and how it’s passedon (during sexual contact) 587 92.2 47 7.4 2 0.3 1 0.2(637) (89.8 – 94.1) (5.5 – 9.7) (0.0 – 1.1) (0.0 – 0.9)Cervical screening and pap smears 545 86.6 78 12.4 1 0.2 5 0.8(629) (83.7 – 89.2) (9.9 – 15.2) (0.0 – 0.9) (0.3 – 1.8)Practising safe sex 545 86.6 78 12.4 1 0.2 5 0.8(629) (83.7 – 89.2) (9.9 – 15.2) (0.0 – 0.9) (0.3 – 1.8)Not having sex 490 78 26 4.1 42 6.7 69 11(628) (74.6 – 81.2) (2.7 – 6.0) (4.9 – 8.9) (8.6 – 13.7)Possible side effects <strong>of</strong> <strong>the</strong> vaccine 603 94.2 27 4.2 2 0.3 8 1.3(640) (92.1 – 95.9) (2.8 – 6.1) (0.0 – 1.1) (0.5 – 2.4)Genital warts and STIs 559 86.7 53 8.2 2 0.3 16 2.5(630) (86.0 – 91.1) (6.4 – 10.9) (0.0 – 1.1) (1.5 – 4.1)* Respondents were asked to answer for both age groups. A number <strong>of</strong> parents responded only for <strong>the</strong> age group in which <strong>the</strong>ir daughter fell, so <strong>the</strong>ir responses are notrecorded here to avoid skewing <strong>of</strong> <strong>the</strong> data.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 195
ORIGINAL SCIENTIFIC PAPErSquantitative researchTable 4. Desire for more information to assist decision about vaccinationInformation needsWant more informationbefore deciding on HPVvaccinationTotal Maori Pacific NZEu O<strong>the</strong>r(n=769) (n=126) (n=57) (n=477) (n=109)n % n % n % n % n %(95% CI) (95% CI) (95% CI) (95% CI) (95% CI)Yes 236 30.7 34 27 25 43.9 141 29.6 36 33(27.4 – 34.1) (19.5 – 35.6) (30.7 – 57.6) (25.5 – 33.9) (24.3 – 42.7)No 405 52.7 64 50.8 22 38.6 263 55.1 56 51.4(49.1 – 56.2) (41.7 – 59.8) (26.0 – 52.4) (50.5 – 59.7) (41.6 – 61.1)Don’t know 94 12.2 21 16.7 7 12.3 52 10.9 14 12.8Would seek o<strong>the</strong>r’s viewsabout <strong>the</strong> vaccine(10 – 14.7) (10.6 – 24.3) (5.1 – 23.7) (8.2 – 14.0) (7.2 – 20.6)Yes 582 75.7 96 76.2 47 82.5 358 75.1 81 74.3(72.5 – 78.7) (67.8 – 83.3) (70.1 – 91.3) (70.9 – 78.9) (65.1 – 82.2)No 137 17.8 19 15.1 4 7 96 20.1 18 16.5(15.2 – 20.7) (9.3 – 22.5) (1.9 – 17.0) (16.6 – 24.0) (10.1 – 24.8)Don’t know 41 5.3 7 5.6 3 5.3 22 4.6 9 8.3If Yes, would seek views <strong>of</strong>:(3.9 – 7.2) (2.3 – 11.1) (1.1 – 14.6) (2.9 – 6.9) (3.8 – 15.1)P-value*Extended family/whanau 231 39.7 48 50 18 38.3 143 39.9 22 27.2
ORIGINAL SCIENTIFIC PAPERSquantitative researchceipt <strong>of</strong> <strong>the</strong> vaccine. This might reflect characteristics<strong>of</strong> parents in <strong>the</strong>se groups; <strong>the</strong>y were morelikely to be immigrants (over 50% have English asa second language), and have a religious affiliationso might have different views on <strong>the</strong> appropriateage for vaccination. A recent NZ study reportedthat practice nurses would be more likely torecommend <strong>the</strong> vaccine to girls aged 16–26 (thanto younger girls), and that GPs would most likelyrecommend <strong>the</strong> vaccine to girls aged 13–15 yearsold, followed closely by 9–12-year-olds. 27 In <strong>the</strong>current programme, <strong>the</strong> vaccine will be <strong>of</strong>feredto girls in Year 8 (girls aged 12), <strong>the</strong>refore carefulexplanation will be needed for parents (andhealth providers) to understand <strong>the</strong> importantreasons for vaccination at this age.The majority <strong>of</strong> parents deemed informationrelating to HPV vaccination (presented in Table 3)suitable for girls <strong>of</strong> all vaccine-eligible ages.Cervical screening and pap smears, practisingsafe sex, genital warts and STIs were thoughtto be appropriate for discussion only with girlsaged 16 and older by 8–12% <strong>of</strong> parents. A third <strong>of</strong>parents wanted more information about Gardasil ®before making a decision about vaccination, andmany indicated that <strong>the</strong>y would seek <strong>the</strong> views<strong>of</strong> o<strong>the</strong>rs—most commonly those <strong>of</strong> <strong>the</strong> familydoctor (GP). A telephone survey <strong>of</strong> 1052parents conducted in 2009 also showed <strong>the</strong> GP/nurse/medical centre was <strong>the</strong> preferred place toget information on <strong>the</strong> vaccine. 28 As with o<strong>the</strong>rvaccines, health pr<strong>of</strong>essionals’ endorsement andsupport <strong>of</strong> <strong>the</strong> HPV vaccine will be important toensure <strong>the</strong> success <strong>of</strong> this programme. Henniger’ssurvey showed that GPs and practice nurses indicateda high level <strong>of</strong> willingness to recommend<strong>the</strong> vaccine to <strong>the</strong>ir patients. 27With parental or patient permission, receipt <strong>of</strong><strong>the</strong> HPV vaccine will be recorded on <strong>the</strong> NationalImmunisation Register (NIR), and authorisedhealth pr<strong>of</strong>essionals will be able to access thisinformation. Parents in this study were happy forinformation-sharing to occur <strong>between</strong> <strong>the</strong> NIRand primary care, stating that it was importantthat <strong>the</strong>ir daughter’s GP receive this informationfor <strong>the</strong>ir records. However, it appears that GPs/health providers are not routinely notified when<strong>the</strong>ir patients receive Gardasil ® at <strong>school</strong>, but canrequest information on <strong>the</strong>ir patients’ vaccinationstatus. This lack <strong>of</strong> information-sharing willpotentially limit opportunities for vaccination.Parents were also happy to be phoned if <strong>the</strong>yhad not returned a consent form to enable <strong>the</strong>irdaughter’s receipt <strong>of</strong> <strong>the</strong> vaccine. Resources t<strong>of</strong>ollow-up on consent forms will be particularlyimportant in <strong>school</strong>s or areas known to have lowreturn rates <strong>of</strong> (any) <strong>school</strong>-related paperworkfrom parents. The mass communicationcampaign, integrated information systems(<strong>school</strong>s and primary care) and <strong>the</strong> resources tosupport recall and follow-up have been cited askey to <strong>the</strong> success <strong>of</strong> <strong>the</strong> MeNZB TM programme.Our findings support <strong>the</strong> view <strong>of</strong> Grant etal. who advocated for an integrated systemto enable all opportunities for immunisationwith Gardasil ® to be utilised, 29 with vaccineadministration and information-sharing <strong>between</strong>primary care and education providers.This is <strong>the</strong> first NZ study to describe parents’preferences on where and when <strong>the</strong>ir daughters’receive <strong>the</strong> Gardasil ® vaccine. The inclusion <strong>of</strong>groups most at-risk for cervical cancer (Maori,Pacific and lower socioeconomic groups) is astrength <strong>of</strong> this research. By targeting <strong>school</strong>sknown to have a higher proportion <strong>of</strong> Maori andPacific students, we aimed to oversample parentsin <strong>the</strong>se ethnic groups, but response rates weregenerally lower from those <strong>school</strong>s. The distribution<strong>of</strong> our predominantly female participantsacross ethnic groups (62% European, 16.4% Maoriand 7.4% Pacific) closely reflects that <strong>of</strong> femalesaged 30–55 in <strong>the</strong> Wellington region where 70%are European, 11.7% Maori and 4.7% Pacific. Respondentsmay be more representative <strong>of</strong> parentswho have stronger views towards this vaccine.Pacific parents most <strong>of</strong>ten responded in waysthat differed from <strong>the</strong> three o<strong>the</strong>r groups, butfindings should be interpreted with caution dueto <strong>the</strong> smaller sample size (n=57). The responserate (25%) and recruitment <strong>of</strong> parents from onlyone region limits <strong>the</strong> generalisability <strong>of</strong> <strong>the</strong> findingsbeyond <strong>the</strong> study participants. However, <strong>the</strong>response rate is likely to be slightly higher thanthat reported, as we were generous in <strong>the</strong> number<strong>of</strong> surveys distributed to <strong>school</strong>s, having beengiven estimates <strong>of</strong> student numbers at participating<strong>school</strong>s. A survey <strong>of</strong> parent attitudes to HPVVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 197
ORIGINAL SCIENTIFIC PAPErSquantitative researchACKNOWLEDGEMENTSWe gratefully acknowledgeparticipation by 769parents and <strong>the</strong>irdaughters as well asprincipals and <strong>the</strong>ir<strong>school</strong>s for facilitatingdistribution and return<strong>of</strong> surveys. Thanks alsoto a small advisory groupfor early advice on <strong>the</strong>study, and to Dr JamesStanley (Biostatistician,Department <strong>of</strong> PublicHealth) for statisticaladvice and assistancewith analyses.FUNDINGThis study was fundedby a grant from <strong>the</strong>Health Research CouncilPartnership programme(REF 08/602).COMPETING INTERESTSNone declared.vaccination achieved a similar response rate (22%)in <strong>the</strong> United Kingdom, 30 and <strong>the</strong> Christchurchsurvey <strong>of</strong> GPs and practices nurses reached a 39%response rate. 27ConclusionsWe suggest that a programme jointly deliveredin primary care and <strong>school</strong> settings, that is appropriatelyresourced for follow-up and information-sharingwould increase vaccine coverage.The rationale for vaccination at age 12 needsto be made clear to parents and evidence-basedinformation needs to be delivered appropriately toparents and girls. As with o<strong>the</strong>r vaccines, healthpr<strong>of</strong>essionals’ endorsement <strong>of</strong> and support forthis new programme will be important to ensureits success.References1. Muñoz N, Bosch FX, Castellsagué X, Díaz M, Sanjose Sd,Hammouda D, et al. Against which human papillomavirustypes shall we vaccinate and screen? The international perspective.Int J Cancer. 2004;111(2):278–85.2. Wiley DJ, Douglas J, Beutner K, Cox T, Fife K, Moscicki AB, etal. External genital warts: diagnosis, treatment, and prevention.Clin Infect Dis. 2002;35:S210–S24.3. Block SL, Nolan T, Sattler C, Barr E, Giacoletti KE, MarchantCD, et al. Comparison <strong>of</strong> <strong>the</strong> immunogenicity and reactogenicity<strong>of</strong> a prophylactic quadrivalent human papillomavirus(types 6, 11, 16, and 18) L1 virus-like particle vaccine in maleand female adolescents and young adult women. Pediatrics.2006;118(5):2135–45.4. Villa LL, Costa RL, Petta CA, Andrade RP, Paavonen J, IversenOE, et al. High sustained efficacy <strong>of</strong> a prophylactic quadrivalenthuman papillomavirus types 6/11/16/18 L1 virus-likeparticle vaccine through five years <strong>of</strong> follow-up. Br J Cancer.2006;95(11):1459–66.5. Robson B, Purdie G, Cormack D. Unequal Impact: Maori andNon-Maori Cancer Statistics 1996–2001. Wellington: Ministry<strong>of</strong> Health Report; 2006. [Accessed Dec 2009]:Available from:http://www.moh.govt.nz/moh.nsf/pagesmh/4761/$File/unequal-impact-maori-nonmaori-cancer-statistics-96-01.pdf.6. Centre for Public Health Research. Annual monitoring report2004, National Cervical Screening Programme. Wellington:Massey University; 2007.7. Ministry <strong>of</strong> Health. Immunisation handbook 2006. Wellington,New Zealand: Ministry <strong>of</strong> Health; 2006.8. Ministry <strong>of</strong> Health HPV Project Team. The HPV (HumanPapillomavirus) Immunisation Programme: National ImplementationStrategic Overview. Population Health Directorate,Wellington: Ministry <strong>of</strong> Health; 2008. [Accessed Aug2009]:Available from: http://www.moh.govt.nz/moh.nsf/pagesmh/7893/$File/hpv-national-implementation-strategicoverview.pdf.9. Waller J, Marlow LAV, Wardle J. Mo<strong>the</strong>rs’ attitudes towardspreventing cervical cancer through human papillomavirusvaccination: a qualitative study. Cancer Epidemiol BiomarkersPrev. 2006;15(7):1257–61.10. Olshen E, Woods ER, Austin SB, Luskin M, Bauchner H. Parentalacceptance <strong>of</strong> <strong>the</strong> human papillomavirus vaccine. J AdolescHealth. 2005;37(3):248.11. Brabin L, Roberts SA, Kitchener HC. A semi-qualitativestudy <strong>of</strong> attitudes to vaccinating adolescents against humanpapillomavirus without parental consent. BMC Public Health.2007;7:20.12. Vallely LA, Roberts SA, Kitchener HC, Brabin L. Informingadolescents about human papillomavirus vaccination: whatwill parents allow? Vaccine. 2008;26(18):2203–10.13. Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that areassociated with parental acceptance <strong>of</strong> human papillomavirusvaccines: a randomized intervention study <strong>of</strong> written informationabout HPV. Pediatrics. 2006;117(5):1486–93.14. Chan SSC, Cheung TH, Lo WK, Chung TKH. Women’s attitudeson human papillomavirus vaccination to <strong>the</strong>ir daughters.J Adoles Health. 2007;41(2):204.15. Marshall H, Ryan P, Roberton D, Baghurst P. A cross-sectionalsurvey to assess community attitudes to introduction <strong>of</strong>human papillomavirus vaccine. Aust NZ J Public Health.2007;31(3):235–42.16. Constantine NA, Jerman P. Acceptance <strong>of</strong> human papillomavirusvaccination among Californian parents <strong>of</strong> daughters:a representative statewide analysis. J Adolesc Health.2007;40(2):108–15.17. Hausdorf K, Newman B, Whiteman D, Aitken J, Frazer I. HPVvaccination: what do Queensland parents think? Aust NZ JPublic Health. 2007;31(3):288–9.18. Marlow LAV, Waller J, Wardle J. Parental attitudes to prepubertalHPV vaccination. Vaccine. 2007;25(11):1945.19. Ogilvie GS, Remple VP, Marra F, McNeil SA, Naus M, PielakK, et al. Intention <strong>of</strong> parents to have male children vaccinatedwith <strong>the</strong> human papillomavirus vaccine. Sex Trans Infect.2008;84(4):318–23.20. Petousis-Harris H, Turner N, Soe B. Parent views on <strong>school</strong>based immunisation. NZ Fam Phys. 2004;31(4):222–28.21. Petousis-Harris H, Turner N, Kerse N. New Zealand mo<strong>the</strong>rs’knowledge <strong>of</strong> and attitudes towards immunisation. NZ FamPhys. 2002;29(4):240–46.22. Petousis-Harris H, Goodyear-Smith F, Godinet S, Turner N.Barriers to childhood immunisation among New Zealand mo<strong>the</strong>rs.NZ Fam Phys. 2002;29(6):396–401.23. Loring BJ, Curtis ET. Routine vaccination coverage <strong>of</strong> 11 yearolds, by ethnicity, through <strong>school</strong>-based vaccination in SouthAuckland. N Z Med J. 2009;122(1291):14–21.24. Ministry <strong>of</strong> Education. Frequently asked questions about<strong>decile</strong>s. Wellington: Ministry <strong>of</strong> Education; 2007. [AccessedJun 2009]: Available from: http://www.minedu.govt.nz/index.cfm?layout=document&documentid=7696&data=l25. Ministry <strong>of</strong> Health. Cervical cancer vaccine brochure—information for girls, young women and <strong>the</strong>ir familes. Ministry<strong>of</strong> Health website: HPV Immunisation programme 2008.[Accessed Aug 2008]:Available from: http://www.moh.govt.nz/moh.nsf/indexmh/immunisation-diseasesandvaccineshpv-programme#resources.26. Ministry <strong>of</strong> Health. Ethnicity data protocols for <strong>the</strong> health anddisability sector. Wellington: Ministry <strong>of</strong> Health; 2004. [AccessedFeb 2010]:Available from: http://www.nzhis.govt.nz/moh.nsf/pagesns/228/$File/ethnicity-data-protocols.pdf.27. Henninger J. Human papillomavirus and papillomavirusvaccines: knowledge, attitudes and intentions <strong>of</strong> general practitionersand practice nurses in Christchurch. J Primary HealthCare. 2009;1(4):278–85.28. Wyllie A, Brown R. HPV vaccine communications first trackingmonitor. Research report for GSL network on behalf <strong>of</strong> <strong>the</strong>Ministry <strong>of</strong> Health. 2009; October (Phoenix Research, Unpublished).29. Grant CC, Turner N, Jones R. Eliminating ethnic disparities inhealth through immunisation: New Zealand’s chance to earnglobal respect. N Z Med J. 2009;122(1291):10–13.30. Brabin L, Roberts SA, Farzaneh F, Kitchener HC. Future acceptance<strong>of</strong> adolescent human papillomavirus vaccination: Asurvey <strong>of</strong> parental attitudes. Vaccine. 2006;24(16):3087.198 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSquantitative researchIncreasing <strong>the</strong> uptake <strong>of</strong> opportunisticchlamydia screening: a pilot study in generalpracticeBeverley A Lawton ONZM, MBChB, FRNZCGP, DObst; 1 Sally B Rose PhD; 1 C Raina Elley MBChB, PhD; 2Collette Bromhead PhD; 3 E Jane MacDonald MBChB, FAChSHM, DTM&H; 4 Michael G Baker MBChB,FAFPHM, FRACMA, DComH, DObst 5ABSTRACTIntroduction: Genitourinary Chlamydia trachomatis infection is common and associated with considerablepersonal and public health cost. Effective detection strategies are needed.Aim: To assess feasibility <strong>of</strong> an opportunistic incentivised chlamydia screening programme in generalpractice over six months.MethodS: This study was designed as a pilot for a randomised controlled trial in primary care. Threegeneral practices were randomly allocated to intervention (two practices) and control groups. Theintervention involved practice education, self-sample collection and practice incentives (funding andfeedback) for a three-month ‘active’ intervention period. Feedback and education was discontinued during<strong>the</strong> second three-month period. Practice-specific nurse- or doctor-led strategies were developed foridentifying, testing, treating and recalling male and female patients aged 16–24 years. The main outcomemeasure was <strong>the</strong> difference <strong>between</strong> <strong>the</strong> practices’ chlamydia screening rates over <strong>the</strong> six months followingintroduction <strong>of</strong> <strong>the</strong> intervention, controlling for baseline rates from <strong>the</strong> previous year.Results: Chlamydia testing rates during <strong>the</strong> year prior to <strong>the</strong> intervention ranged from 2.9% to 7.0%<strong>of</strong> practice attendances by 16–24-year-olds. The intervention practices had higher rates <strong>of</strong> screeningcompared with <strong>the</strong> control practice (p
ORIGINAL SCIENTIFIC PAPErSquantitative research<strong>of</strong> pelvic inflammatory disease (PID), 5,6 demonstrating<strong>the</strong> individual benefit <strong>of</strong> diagnosing andtreating chlamydia. However, a chlamydia controlstrategy that aims to test and treat <strong>the</strong> widerpopulation is necessary to reduce <strong>the</strong> overallprevalence in <strong>the</strong> community. The US PreventiveServices Task Force recommends screening <strong>of</strong> allsexually-active women 24 years and younger. 2The challenge for any chlamydia control programmeis not only to increase testing in <strong>the</strong>primary care environment, but also to engagewith primary care.The general practice setting is an obvious choicefor opportunistic testing as a high proportion <strong>of</strong>under-25-year-olds attend in any one year (80%<strong>of</strong> females in Australia, 7 and 84% <strong>of</strong> females and70% <strong>of</strong> males in New Zealand). 8 In 2007 <strong>the</strong> annualrate <strong>of</strong> chlamydia infection in New Zealandis estimated to be 714 per 100 000 which is overtwice that <strong>of</strong> Australia (244.9/100 000). The highestrates occur in 15–19-year-olds with rates <strong>of</strong>2887 and 6382 per 100 000 respectively for <strong>the</strong>Waikato and Bay <strong>of</strong> Plenty regions. 9 Despite <strong>the</strong>sehigh rates <strong>of</strong> infection, good primary care systemsand <strong>the</strong> availability <strong>of</strong> testing and treatment, <strong>the</strong>reis currently no organised programme to reducechlamydia in Australia or in New Zealand. 10,11The question still remains about how to achievesustained control <strong>of</strong> <strong>the</strong> transmission <strong>of</strong> chlamydia.The aim <strong>of</strong> this study was to pilot an opportunisticchlamydia screening programme targetingmales and females aged 16–24 years. The programmeincorporates practice-specific screeningstrategies, incentives, and self-sample collectionwith feedback <strong>of</strong> testing rates over three months.MethodsThis study was approved by <strong>the</strong> Central RegionalEthics Committee in July 2006 (Ref.CEN/06/06/053), and carried out during 2007in Wellington. Three primary care practiceswere invited to participate by letter <strong>of</strong> invitationfollowed by a phone call and face-to-facemeeting. Written informed consent was obtainedfor participation. Eligibility criteria for practicesincluded: located in Wellington and attended byat least 300, 16–24-year-old patients in <strong>the</strong> previousyear. The three practices were selected basedon location—Practice A was located in an outercity suburb, Practice B in <strong>the</strong> central city, andPractice C in an inner city suburb. All three <strong>of</strong><strong>the</strong> invited practices were willing to participate,and were randomly allocated to <strong>the</strong> intervention(two practices) or control group (one practice), asdetermined by <strong>the</strong> flip <strong>of</strong> a coin.InterventionPrior to <strong>the</strong> start <strong>of</strong> data collection, <strong>the</strong> researchteam worked with practices in <strong>the</strong> interventiongroup over a six-week period to identify ways tobest achieve <strong>the</strong> goal <strong>of</strong> testing all 16–24-yearoldpatients attending for any reason. Thismethod was based on <strong>the</strong> ‘systems approach’used by Shafer to increase screening rates, andinvolved engaging <strong>the</strong> practice in <strong>the</strong> implementation<strong>of</strong> <strong>the</strong> programme, assembling a teamto champion <strong>the</strong> project, identifying <strong>the</strong> gap<strong>between</strong> best practice and current practice, andregular monitoring and feedback <strong>of</strong> progressover <strong>the</strong> trial period. 12 Sexual histories were nottaken prior to <strong>of</strong>fering screening. Practices wereencouraged to develop a system for identifyingappointments for patients in <strong>the</strong> age-group at<strong>the</strong> beginning <strong>of</strong> <strong>the</strong> day. Verbal scripts weredeveloped for use by practice staff in <strong>of</strong>feringchlamydia screening tests. Females were <strong>of</strong>feredself-taken swab or urine tests, while males were<strong>of</strong>fered urine tests. A brief instruction sheetwas provided for females as a guide to obtaininga vaginal swab. The active interventionphase ran for three months once opportunisticscreening began at intervention practices. Duringthis phase, practices were provided withregular feedback at face-to-face meetings with<strong>the</strong> programme team about <strong>the</strong>ir screening rates.During <strong>the</strong> second three months <strong>of</strong> <strong>the</strong> study(post-active intervention phase), <strong>the</strong> practices receivedno feedback, and no contact or meetingswith <strong>the</strong> programme team.The financial incentive provided to interventionpractices included a payment equivalent to twotenths<strong>of</strong> a nurse’s time over six months (paidin two instalments over six months) to ensure<strong>the</strong> programme was adequately resourced. Allgeneral practices in <strong>the</strong> study region can claimfor an already existent payment for a consultation(NZ$11 for a short consultation and NZ$40 for200 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSquantitative researcha long consultation) relating to sexual health in<strong>the</strong> under–25-year-olds. The control practice wasable to claim for this, but only <strong>the</strong> interventionpractices were reminded to claim.Intervention practices were asked to contactpatients about <strong>the</strong>ir results in <strong>the</strong> usual way(ei<strong>the</strong>r by telephone or in writing) and to <strong>of</strong>ferAzithromycin 1g stat as first-line treatment forpositive tests. Partner treatment was also recommended.A recall system was put in place to <strong>of</strong>fera repeat test at three months for patients whotested positive for chlamydia and at one year forpatients who tested negative. All chlamydia testingtook place at an ISO15189 accredited medicallaboratory using <strong>the</strong> Cobas TaqMan v2.0 PCRtest. This test has high sensitivity and specificityfor <strong>the</strong> detection <strong>of</strong> chlamydia from clinician orself-obtained specimens. 13 Laboratory results forpatients tested during <strong>the</strong> study period were fedback to requesting practices in <strong>the</strong> normal way(electronically).Outcome measuresData collection ran for six months from <strong>the</strong>start <strong>of</strong> <strong>the</strong> intervention. The primary outcomeWHAT GAP THIS FILLSWhat we already know: Chlamydia trachomatis is <strong>the</strong> most commonlydiagnosedbacterial sexually-transmitted infection in New Zealand andworldwide, and is responsible for considerable personal and public healthcost. There is a lack <strong>of</strong> evidence for effective chlamydia control programmes.What this study adds: Opportunistic screening in primary care can besignificantly increased by <strong>the</strong> use <strong>of</strong> incentives, practice education and feedback<strong>of</strong> screening rates.was change in rate <strong>of</strong> chlamydia testing in <strong>the</strong>intervention practices compared with <strong>the</strong> controlpractice over six months (including active andpost-active phases <strong>of</strong> <strong>the</strong> intervention). Monthlytest rates were calculated by taking laboratorytesting data as <strong>the</strong> numerator, and practice consultationsby 16–24-year-old patients during <strong>the</strong>assessment period as <strong>the</strong> denominator. Data ongender, age and ethnicity were also provided byWIPA (now Compass Health) who routinely collectpractice consultation data for <strong>the</strong>ir members.All data were de-identified so that no identifyingpatient details were provided to <strong>the</strong> researchteam. As consultation and testing rates werecollected electronically and automatically, <strong>the</strong>reFigure 1. Percentage <strong>of</strong> 16–24-year-olds screened for chlamydia in intervention compared with control practices before,during and after <strong>the</strong> interventionVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 201
ORIGINAL SCIENTIFIC PAPErSquantitative researchTable 1. Number and characteristics <strong>of</strong> 16–24-year-old patients attending study practices during <strong>the</strong> study periodCharacteristic Intervention ControlPractice ANurse-ledPractice BDoctor-ledPractice C(usual care)n % n % n %All patients 756 712 936Females 508 67.2 500 70.2 613 65.5Males 248 32.8 212 29.8 323 34.5Age-band16–19 years 363 48.0 107 15.0 344 36.820–24 years 393 52.0 605 85.0 592 63.2Ethnic groupNew Zealand European 362 47.9 514 72.2 688 73.5Maori 266 35.2 20 2.8 53 5.7Pacific 60 7.9 7 1.0 4 0.4Asian 25 3.3 35 4.9 58 6.2O<strong>the</strong>r/not known 43 5.7 136 19.1 133 14.2was no risk <strong>of</strong> assessor bias. Data relating to testresults were obtained from <strong>the</strong> laboratory.AnalysisTo assess <strong>the</strong> differences in changes in chlamydiascreening rates over time <strong>between</strong> <strong>the</strong> interventionand control practices (proportion tested), aregression model was used including baselinerates as a covariate. Analyses were also controlledfor gender proportions in each practice andscreening rates from <strong>the</strong> previous year. Percentagesscreened each month at each practice werearc-sine transformed to better satisfy <strong>the</strong> assumptions<strong>of</strong> normality. Two hypo<strong>the</strong>ses were testedusing contrasts. One a priori analysis assessedwhe<strong>the</strong>r <strong>the</strong>re was an effect <strong>of</strong> <strong>the</strong> interventionin general compared with no intervention, anda post hoc analysis assessed whe<strong>the</strong>r <strong>the</strong>re wasa significant difference in effect <strong>between</strong> <strong>the</strong>nurse-led and <strong>the</strong> doctor-led model interventionpractices. A p-value <strong>of</strong>
ORIGINAL SCIENTIFIC PAPERSquantitative researchTable 2. Description <strong>of</strong> intervention programme componentsComponentsFundingNurse-led interventionPractice ADoctor-led interventionPractice BControl (usual care)Practice C$11 payment* $11 payment* $11 payment*$400 study participation feeplus equivalent 2/10ths practicenurse time paid for six months$400 study participation feeplus equivalent 2/10ths practicenurse time paid for six months$400 study participationfeeProvided by <strong>the</strong>programme teamDocumentation22-page study manual customisedfor practice, covering all relevantaspects <strong>of</strong> chlamydia testing andtreatment22-page study manual customisedfor practice, covering all relevantaspects <strong>of</strong> chlamydia testing andtreatmentBest practice chlamydiamanagement guidelines(four pages) posted topracticeFeedbackFeedback on testing rates providedto practice team during <strong>the</strong> activeintervention phase (four face-to-facemeetings in weeks 2, 4, 6 and 10)Feedback on testing rates providedto practice team during activeintervention phase (two face-to-facemeetings in weeks 5 and 7; emailedfeedback in weeks 9 and 11)Method used toidentify eligiblepatientsSystematic identification <strong>of</strong> eligiblepatients by nurse at start <strong>of</strong> day,sometimes utilised Medtech † alertsOpportunistic identification <strong>of</strong>eligible patients by doctor duringday‘Usual practice’Information forpatients abouttestingPosters placed in waiting room andclinical roomsGP and nurses used brief ‘script’ to<strong>of</strong>fer testsOne page pamphlet <strong>of</strong> informationabout chlamydia <strong>of</strong>feredGP used brief ‘script’ to <strong>of</strong>fer testsOne page pamphlet <strong>of</strong> informationabout chlamydia <strong>of</strong>feredPractice-specificsystems developedin consultation withprogramme teamSample collectionFemales: urine; self-collected swab(instruction sheet <strong>of</strong>fered), clinicianswab with cervical smearsMales: urineFemales: urine; clinician swab withcervical smearsMales: urineNotification<strong>of</strong> results andtreatmentPatients asked to phone for results;positives phoned by nurseInvited partners to attend fortreatmentSent letter to patients regardless <strong>of</strong>whe<strong>the</strong>r result positive or negativeInvited partners to attend fortreatmentRecall <strong>of</strong> patientstestedAim to send letter to recall patientsPositive chlamydia—recall enteredinto Medtech for three monthsNegative chlamydia—recall enteredinto Medtech for 12 monthsAim to send letter to recall patientsPositive chlamydia—recall enteredinto Medtech for three monthsNegative chlamydia—recall enteredinto Medtech for 12 months* Available to all practices in <strong>the</strong> study region, payment can be claimed from <strong>the</strong> District Health Board for a short sexual health consult†Medtech is a computerised patient management system used in many general practices in New Zealand.proach (p=0.04). Screening rates declined at bothintervention practices after <strong>the</strong> three months <strong>of</strong><strong>the</strong> active intervention, with rates returning tobaseline by <strong>the</strong> end <strong>of</strong> <strong>the</strong> six-month period (Figure1). Screening rates tended to be similar formales and females at practice A, but were lowerfor males at practice B during <strong>the</strong> three months<strong>of</strong> active intervention (Table 4).In <strong>the</strong> 12 months prior to <strong>the</strong> intervention, <strong>the</strong>overall rate <strong>of</strong> chlamydia infection detectedat <strong>the</strong> three study practices (intervention andcontrol) was 10.5% (23/219). Practice A had <strong>the</strong>highest proportion <strong>of</strong> chlamydia-positive casesdetected at baseline with 20.3% (13/64), PracticeB detected chlamydia in 14.8% (4/27) <strong>of</strong> patientstested, and <strong>the</strong> control practice detected chlamy-VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 203
ORIGINAL SCIENTIFIC PAPErSquantitative researchTable 3. Number (percent) <strong>of</strong> attendances <strong>of</strong> 16–24-year-olds where screening for chlamydia occurred in interventioncompared with control practicesTimePre-interventionNurse-ledintervention (A)Doctor-ledintervention (B)A vs BControlpractice (C)n/N* % n/N % n/N %Previous 12-months 66/1304 5.1 27/924 2.9 137/1952 7.0Active interventionMonth 1 52/148 35.1 18/120 15.0 11/209 5.3Month 2 39/123 31.7 12/92 13.0 10/171 5.8Month 3 31/130 23.8 6/143 4.2 8/156 5.1Post active interventionMonth 4 20/125 16.0 6/112 5.4 5/127 3.9Month 5 13/103 12.6 4/115 3.5 9/133 6.8Month 6 7/127 5.5 2/127 1.6 6/140 4.3Interventionvs ControlP-value † 0.04
ORIGINAL SCIENTIFIC PAPERSquantitative researchDiscussionThis pilot study found that <strong>the</strong> three-monthintervention programme comprising practiceeducation, practice-specific screening strategies,self-sample collection, incentives and face-to-facefeedback on screening rates significantly increased<strong>the</strong> proportion <strong>of</strong> 16–24-year-old patientsscreened for chlamydia over six months.The rates <strong>of</strong> testing in <strong>the</strong> intervention practicesover three months (Practice A, 30.4%; Practice B,10.1%) compare favourably with those <strong>of</strong> <strong>the</strong>United Kingdom (UK) screening programmewhich had an average uptake <strong>of</strong> 9.5% by December2008. There was a return to pre-interventionscreening rates by <strong>the</strong> end <strong>of</strong> <strong>the</strong> six-monthdata-monitoring period. Interaction with <strong>the</strong> programmeteam and feedback <strong>of</strong> testing rates ceasedat <strong>the</strong> end <strong>of</strong> three months, which coincided with<strong>the</strong> gradual fall-<strong>of</strong>f in rates back to baseline testingrates at six months. Comments from partici-50% uptake <strong>of</strong> chlamydia testing by <strong>the</strong> eligiblefemale population was achieved. 15 General practitionersreceived a fee-for-service for chlamydiatesting in <strong>the</strong> pilot and 60% <strong>of</strong> positives weredetected through this setting. 16 Incentives werealso a component <strong>of</strong> an Australian randomisedcontrolled trial designed to increase chlamydiatesting in women presenting for Pap smears. Thisstudy found that women had a tw<strong>of</strong>old greaterchance <strong>of</strong> being tested in <strong>the</strong> intervention arm(6.9% vs 4.5% in <strong>the</strong> control). 17 The initial aim <strong>of</strong><strong>the</strong> UK National Chlamydia Screening Programme(NCSP) was to achieve <strong>the</strong> modest target<strong>of</strong> <strong>of</strong>fering testing to 15% <strong>of</strong> all 15–24-year-olds. 18The NCSP began roll-out in 2003 with <strong>the</strong>expectation <strong>of</strong> full national participation by allprimary care trusts by <strong>the</strong> end <strong>of</strong> 2007; howevertargets have not yet been met. 19The challenge for any chlamydia control programmeis not only to increase testing in <strong>the</strong>A strength <strong>of</strong> <strong>the</strong> present study was that testing was <strong>of</strong>fered to allmales and females in <strong>the</strong> eligible age group regardless <strong>of</strong> sexualactivity. Doctors in this study supported this approach suggesting itwas less threatening, and ‘normalised’ testingpating practice staff at <strong>the</strong> end <strong>of</strong> <strong>the</strong> six monthsindicated that <strong>the</strong>y stopped <strong>of</strong>fering tests because<strong>the</strong> study had stopped. This suggests that, as wellas incentives, being part <strong>of</strong> a broader programmemay assist in maintaining higher levels <strong>of</strong> screeningin general practice.Past research has also demonstrated that usinga ‘practice champion’ may be effective. 14 Thepresent study showed that <strong>the</strong> screening strategyled by a practice nurse champion was significantlymore effective than <strong>the</strong> doctor-led strategy,although this may have been due to o<strong>the</strong>rcharacteristics <strong>of</strong> <strong>the</strong> practices involved. Financialincentives, combined with practice educationand feedback <strong>of</strong> testing rates, have contributedto <strong>the</strong> increased testing rates seen in this study.Incentives were also used in a UK screeningpilot study in Wirral and Portsmouth in whichprimary care environment, but also to engagewith primary care. It has been suggested that <strong>the</strong>lack <strong>of</strong> engagement with general practitioners in<strong>the</strong> NCSP might be explained by <strong>the</strong> absence <strong>of</strong>any incentives. 20–23 The relative failure <strong>of</strong> pastor existing screening programmes to reduce <strong>the</strong>prevalence <strong>of</strong> chlamydia may also be related inpart to <strong>the</strong> failure to screen males, as well as factorssuch as failure to treat partners. 24Although males appear to have lower rates<strong>of</strong> chlamydia infection compared to females,it seems logical to screen and treat males toreduce <strong>the</strong> prevalence <strong>of</strong> chlamydia morbidityin females. 24,25 A strength <strong>of</strong> <strong>the</strong> present studywas that testing was <strong>of</strong>fered to all males andfemales in <strong>the</strong> eligible age group regardless <strong>of</strong>sexual activity. Doctors in this study supportedthis approach suggesting it was less threatening,VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 205
ORIGINAL SCIENTIFIC PAPErSquantitative researchand ‘normalised’ testing. This is consistent withqualitative research that concluded that womendid not want a sexual history taken and preferredtests to be <strong>of</strong>fered based on age ra<strong>the</strong>r than sexualhistory. 26,27 Rates <strong>of</strong> screening in this study weresimilar for males and females, suggesting thatthis approach was accepted by both genders andwas particularly effective in reaching males (43%tested in month 1 at Practice A). The UK screeningprogramme had achieved 4.5% coverage <strong>of</strong>males as <strong>of</strong> 2008. 19The use <strong>of</strong> self-sample collection in <strong>the</strong> practicemay also have increased acceptance rates,particularly for females who prefer self-collectionto traditional (more invasive) clinician-obtainedmethods. 19Detection <strong>of</strong> chlamydia cases in <strong>the</strong> presentstudy was significantly lower for interventionpractices during <strong>the</strong> three-month active interventionperiod (8.9%) compared with baseline(18.7%, p
ORIGINAL SCIENTIFIC PAPERSquantitative researchInstitute <strong>of</strong> Environmental Science and Research Limited; 2008April 2008 Contract No.: Document Number|.10. Hocking JS, Walker J, Regan D, Chen MY, Fairley CK. Chlamydiascreening—Australia should strive to achieve what o<strong>the</strong>rshave not. Med J Aust. 2008 21;188(2):106–8.11. Coughlan E, Bagshaw S. Chlamydia—<strong>the</strong> problem that justwon’t go away. N Z Med J. 2005 August; 118(1220). http://www.nzma.org.nz/journal/118-1220/605/.12. Shafer MA, Tebb KP, Pantell RH, Wibbelsman CJ, NeuhausJM, Tipton AC, et al. Effect <strong>of</strong> a clinical practice improvementintervention on chlamydial screening among adolescent girls.JAMA. 2002;288(22):2846–52.13. Skidmore S, Kaye M, Bayliss D, Devendra S. Validation <strong>of</strong> CO-BAS Taqman CT for <strong>the</strong> detection <strong>of</strong> Chlamydia trachomatis invulvo-vaginal swabs. Sex Transm Infect. 2008;84(4):277–8;discussion 8–9.14. McNulty CAM, Freeman E, Oliver I, Ford-Young W,Randall S. Strategies used to increase chlamydia screeningin general practice: a qualitative study. Public Health.2008;122(9):845-56.15. Pimenta JM, Catchpole M, Rogers PA, Perkins E, JacksonN, Carlisle C, et al. Opportunistic screening for genitalchlamydial infection. I: Acceptability <strong>of</strong> urine testing in primaryand <strong>secondary</strong> healthcare settings. Sex Transm Infect.2003;79(1):16–21.16. Pimenta JM, Catchpole M, Rogers PA, Hopwood J, Randall S,Mallinson H, et al. Opportunistic screening for genital chlamydialinfection. II: Prevalence among healthcare attenders,outcome, and evaluation <strong>of</strong> positive cases. Sex Transm Infect.20 03;79(1):22–7.17. Bowden FJ, Currie MJ, Toyne H, McGuiness C, Lim LL, ButlerJR, et al. Screening for Chlamydia trachomatis at <strong>the</strong> time <strong>of</strong>routine Pap smear in general practice: a cluster randomisedcontrolled trial. Med J Aust. 2008;188(2):76–80.18. Department <strong>of</strong> Health. National Chlamydia Screening Programme(NCSP) in England accessed 24th May 2010. http://www.chlamydiascreening.nhs.uk/ps/index.html 200419. National Chlamydia Screening Programme. National overviewApril–December 2008; 2008 [updated 2008; cited]. Availablefrom: http://www.chlamydiascreening.nhs.uk/ps/data/data_tables.html20. White C. Most trusts will not meet chlamydia screening target.Br Med J. 2007;335(7628):1010.21. Kalwij SA. Time for action on chlamydia. Br Med J.2007;334(7598):813–4.22. Ma R, Clark A. Chlamydia screening in general practice:views <strong>of</strong> pr<strong>of</strong>essionals on <strong>the</strong> key elements <strong>of</strong> a successfulprogramme. J Fam Plann Reprod Health Care. 2005;31:302–6.23. Ma R. With appropriate incentives, general practice canimprove <strong>the</strong> coverage <strong>of</strong> <strong>the</strong> National Chlamydia ScreeningProgramme. Br J Gen Pract. 2006 November;56(532):892–3.24. Greer AL, Fisman DN. Punching above <strong>the</strong>ir weight: males,reinfection, and <strong>the</strong> limited success <strong>of</strong> chlamydia screeningprograms. Sex Transm Dis. 2009;36(1):9–10.25. Dunne EF, Gift TL, Stamm WE. What about <strong>the</strong> men? SexTransm Dis. 2008;35(11 Suppl):S1–2.26. Pavlin N, Parker R, Fairley C, Gunn J, Hocking J. Take <strong>the</strong> sexout <strong>of</strong> STI screening! Views <strong>of</strong> young women on implementingchlamydia screening in general practice. BMC Infect Dis.2008;8(1):62.27. Hobbs MM, van der Pol B, Totten P, Gaydos CA, Wald A,Warren T, et al. From <strong>the</strong> NIH: proceedings <strong>of</strong> a workshop on<strong>the</strong> importance <strong>of</strong> self-obtained vaginal specimens for detection<strong>of</strong> sexually transmitted infections. Sex Transm Dis. 2008Jan;35(1):8–13.28. Low N. Screening programmes for chlamydial infection: whenwill we ever learn? Br Med J. 2007;334(7596):725–8.FUNDINGFunding was receivedfrom <strong>the</strong> University<strong>of</strong> Otago ResearchGrants Committee, <strong>the</strong>Ministry <strong>of</strong> Health and<strong>the</strong> Capital and CoastDistrict Health Board.COMPETING INTERESTSThe funding agencies hadno influence on <strong>the</strong> results<strong>of</strong> this study. All authorshave declared no directconflicts <strong>of</strong> interest. BLhas received grants andlecture honoraria, and SRgrants from a variety <strong>of</strong>industry sources includingRoche Diagnostics whomanufacture chlamydiatesting reagents.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 207
ORIGINAL SCIENTIFIC PAPErSqualitative researchGeneral practitioners’ views aboutdiagnosing and treating depression inMaori and non-Maori patientsDavid R Thomas BA, MA, PhD, FNZPsS; 1 Brooke Arlidge BA, MPH; 2 Bruce Arroll MBChB, PhD, FRNZCGP; 3Hinemoa Elder MBChB, RANZCP 41Emeritus Pr<strong>of</strong>essor, Socialand Community Health,School <strong>of</strong> Population Health,The University <strong>of</strong> Auckland,Auckland, New Zealand2Maori Health Researcher3Department <strong>of</strong> GeneralPractice and Primary HealthCare, Faculty <strong>of</strong> Medicaland Health Science, TheUniversity <strong>of</strong> Auckland,Auckland4Consultant Child andAdolescent Psychiatrist atHauora Waikato, Hamilton,New ZealandABSTRACTIntroduction: The study investigated general practitioners’ (GPs’) views about recognising andtreating depression among patients to establish possible reasons for reported lower levels <strong>of</strong> diagnosisand treatment <strong>of</strong> depression among Maori compared to non-Maori patients.MethodS: Semi-structured interviews with 23 GPs in <strong>the</strong> Auckland region, including both Maori andnon-Maori GPs, elicited GPs’ views about risk factors for depression, recognising depression and circumstancesin which GPs would prescribe medication or recommend o<strong>the</strong>r treatments for depression.Findings: A framework was developed which incorporated <strong>the</strong> strategies GPs reported using to diagnoseand treat depression. This consisted <strong>of</strong> three categories: (a) how depression is identified, (b) factorsinfluencing treatment decisions, and (c) treatment outcomes. Reasons reported by GPs as most likely tolead to ethnic differences in diagnosing depression were greater stigma relating to admitting depressionamong Maori patients, Maori patients being less likely to talk about being depressed, and <strong>the</strong> need for patientsto have effective communication with <strong>the</strong>ir GP. Effective communication, where Maori patients feltfree to talk about personal feelings, was more likely when <strong>the</strong>re was an established relationship <strong>between</strong><strong>the</strong> GP and patient.Conclusion: The findings are consistent with previous reports that depression is less likely to bediagnosed by GPs among Maori patients, compared to non-Maori patients. GPs who are able to establisheffective communication with patients, gain <strong>the</strong>ir trust and take account <strong>of</strong> <strong>the</strong> reluctance <strong>of</strong> some Maoripatients to talk about personal feelings, are more likely to diagnose and treat depression effectively.KEYWORDS: Depression; diagnosis; treatment; primary care; Maori; ethnicity; New ZealandJ PRIMARY HEALTH CARE2010;2(3):208–216.Correspondence to:David Thomas,Emeritus Pr<strong>of</strong>essorSocial and CommunityHealth, The University<strong>of</strong> Auckland, PB 92019,Auckland, New Zealand.dr.thomas@auckland.ac.nzIntroductionA study <strong>of</strong> depression in one general practice inAuckland noted that Maori patients were prescribedantidepressants at a much lower rate thannon-Maori patients. 1 A similar finding was reportedfrom <strong>the</strong> 2002 National Primary MedicalCare Survey (NatMedCa) on general practice inNew Zealand (NZ), which noted that antidepressantswere less commonly prescribed for Maoripatients. 2 In NatMedCa, antidepressant prescriptionsaccounted for 1.6% <strong>of</strong> all Maori prescriptionitems compared to 3.3% <strong>of</strong> prescription itemsamong non-Maori patients. The prescribing ratewas 2.1/100 visits by Maori patients compared to4.2/100 for non-Maori patients. In total, antidepressantsaccounted for 12.9% <strong>of</strong> <strong>the</strong> nervoussystem drug prescriptions for Maori compared to22.0% <strong>of</strong> non-Maori.Research on <strong>the</strong> prevalence <strong>of</strong> mental healthdisorders in NZ has indicated that Maori peopletend to have similar or somewhat higher prevalence<strong>of</strong> depression than non-Maori. 3,4 Given <strong>the</strong>apparent undertreatment <strong>of</strong> depression in Maori,208 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchwhat factors might be influential? A 2005 nationalsurvey noted that Maori respondents weresomewhat less likely to encourage someone withdepression to seek pr<strong>of</strong>essional help than non-Maori (48% vs 58%). 5 In relation to people who doseek primary health care, are general practitioners(GPs) less likely to diagnose depression in Maori?Are <strong>the</strong>y less likely to prescribe antidepressantmedication to Maori even when diagnosed, orboth? The study reported here addressed <strong>the</strong>question <strong>of</strong> why Maori patients seem to beprescribed antidepressants by primary health careproviders at a lower rate than non-Maori.To identify o<strong>the</strong>r demographic factors that mightbe related to <strong>the</strong> differences in prescribing antidepressantmedication to patients, we approached<strong>the</strong> authors <strong>of</strong> <strong>the</strong> NatMedCa study in June 2006to fur<strong>the</strong>r analyse <strong>the</strong>ir data. 2 In <strong>the</strong> NatMedCastudy data, <strong>the</strong> diagnosis rate for depression as apercentage <strong>of</strong> all visits and all ages was 0.7% forMaori men and 2.8% for non-Maori men, and 3.1%for Maori women and 4.5% for non-Maori women.The differences <strong>between</strong> Maori and non-Maori inboth diagnosis and prescribing were most evidentamong males 25–44 years <strong>of</strong> age. A key issue iswhe<strong>the</strong>r <strong>the</strong>se ethnic differences in diagnosingdepression and prescribing anti depressants are dueto doctor or patient effects, or both.A qualitative study <strong>of</strong> mental health consultationsin general practice in New Zealand reportedfour key features that had an impact on consultationswith GPs. 6 These included:• practice pressures (lack <strong>of</strong> time, a primaryfocus on physical conditions);• sociocultural factors (stigma attached topatients disclosing mental health problems,patient qualities <strong>of</strong> stoicism and self-reliance);• <strong>the</strong> medicolegal framework (e.g. patientaccess to medical notes, resistanceto mental health labels thatmight disadvantage patients); and• <strong>the</strong> consultation process (dealingwith physical problems first).GPs employed a number <strong>of</strong> strategies duringconsultations and do recognise mental healthproblems in patients. However practice pressuresand <strong>the</strong> o<strong>the</strong>r features noted above result inWHAT GAP THIS FILLSWhat we already know: Maori are prescribed antidepressant medicationin primary health care less frequently than non-Maori patients, even thoughprevalence surveys show high rates <strong>of</strong> depression among Maori. A likely reasonfor <strong>the</strong> difference is that general practitioners are less likely to diagnoseMaori patients as having depression.What this study adds: GPs reported that Maori patients tended to showgreater stigma relating to admitting depression and were less likely to talkabout being depressed compared to non-Maori patients. Effective communicationthat allows Maori patients to talk about personal feelings related todepression is more likely when <strong>the</strong>re is an established relationship <strong>between</strong><strong>the</strong> GP and patient.consultations not being given <strong>the</strong> label ‘mentalhealth’. 6 Previous studies have reported a generaltrend for depression to be underdiagnosed,or difficult to diagnose in primary health careservices 7–9 and that stigma associated with mentalhealth problems and depression is a majorfactor in lack <strong>of</strong> disclosure <strong>of</strong> relevant informationby patients. 10,11The aim <strong>of</strong> <strong>the</strong> current study was to explore processesrelated to diagnosis and treatment <strong>of</strong> depressionamong Maori and non-Maori patients. Thefocus was on <strong>the</strong> views and experiences <strong>of</strong> GPsin relation to patients who may have depression.The specific research objectives were to:1. Explore <strong>the</strong> views <strong>of</strong> GPs about causes,diagnosis and treatment <strong>of</strong> depression amongpatients.2. Develop a framework to describe <strong>the</strong> processesand procedures GPs typically use to diagnoseand treat depression.3. Document GPs’ views about possibledifferences <strong>between</strong> Maori and non-Maoripatients in <strong>the</strong> diagnosis and treatment <strong>of</strong>depression.The study reported here was part <strong>of</strong> a largerqualitative study examining <strong>the</strong> treatment <strong>of</strong>depression by GPs. Given that <strong>the</strong> New ZealandHealth Strategy includes a section on reducing<strong>the</strong> rate <strong>of</strong> suicide in New Zealanders 12 a betterunderstanding <strong>of</strong> depression should help in thisendeavour.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 209
ORIGINAL SCIENTIFIC PAPErSqualitative researchMethodsThe research design was a qualitative interviewstudy using face-to-face interviews with GPsworking in <strong>the</strong> Auckland region in NZ.Interview sampleTable 1. Questions used in interviews with GPs• How would you recognise depression in a patient?A total <strong>of</strong> 23 interviews were completed. BothMaori and non-Maori GPs were included toensure that Maori perspectives were representedin relation to diagnosis and treatment <strong>of</strong> Maoripatients and that <strong>the</strong> findings were based ona diverse sample. The study began by recruitingMaori practitioners identified through <strong>the</strong>networks <strong>of</strong> <strong>the</strong> research team. For each MaoriGP who agreed to participate, a non-Maori GPmatched by gender, approximate age and area<strong>of</strong> practice was recruited for interviewing. Thefinal sample consisted <strong>of</strong> 11 Maori GPs (sevenmale, four female) and 12 non-Maori GPs (sevenmale, five female). All were from practices in <strong>the</strong>greater Auckland area. Most worked in smallgroup or private practices. Seven worked for iwibased(Maori service provider) health clinics. Theinterviews were carried out by <strong>the</strong> second author(BA), a Maori public health researcher (a nonclinician).Ethics approval was obtained from <strong>the</strong>Nor<strong>the</strong>rn X Ethics Committee.• What kinds <strong>of</strong> people do you think might be more likely to get depression?• In your experience, what are <strong>the</strong> main causes <strong>of</strong> depression?• Are <strong>the</strong>re differences <strong>between</strong> your Maori and non-Maori patients?• When would you prescribe medication to treat depressed patients?• When would you prescribe o<strong>the</strong>r <strong>the</strong>rapies to depressed patients?• How effective do you think medication is to treat depression?• How effective do you think o<strong>the</strong>r <strong>the</strong>rapies are to treat depression?• What do you think would be ‘best practice’ treatment for depression?• Are <strong>the</strong>re differences in <strong>the</strong> way you would prescribe ei<strong>the</strong>r medication or ano<strong>the</strong>r<strong>the</strong>rapy to your Maori and non-Maori patients?• What, if any, do you think some <strong>of</strong> <strong>the</strong> barriers might be to adherence <strong>of</strong> treatmentfor patients?• Do you think <strong>the</strong>re are any differences in patient adherence?Interview questionsThe interview schedule included semi-structuredand open-ended questions (Table 1). Interviewswere conducted in a flexible manner that allowedGPs to share <strong>the</strong>ir experiences in relation to <strong>the</strong>topics covered by <strong>the</strong> questions.ProceduresFace-to-face interviews were conducted with 22GPs at <strong>the</strong>ir health practices. One was interviewedby phone. Most <strong>of</strong> <strong>the</strong> interviews tookapproximately half an hour and all were audiorecordedand transcribed verbatim, with <strong>the</strong>transcripts used for qualitative analysis.Data analysisThe analysis used an inductive approach 13 suitablefor <strong>the</strong> research objectives and <strong>the</strong> interview datacollected. An initial analysis was conducted by<strong>the</strong> interviewer to identify specific <strong>the</strong>mes andcategories. Subsequently text from <strong>the</strong> interviewtranscripts was imported into <strong>the</strong> qualitativeanalysis s<strong>of</strong>tware NVivo (v7) and analysed bya second team member (DRT). This confirmed<strong>the</strong> initial categories and constructed an overallframework that incorporated <strong>the</strong> specific categoriesand provided an overview <strong>of</strong> GPs’ strategiesfor identifying and treating depression. The finalset <strong>of</strong> categories was reviewed by <strong>the</strong> researchteam. A key focus <strong>of</strong> <strong>the</strong> analysis was on GPs’experiences in relation to potential differencesin identifying and treating depression <strong>between</strong>Maori and non-Maori patients, not to systematicallycompare Maori and non-Maori GPs.FindingsFindings from <strong>the</strong> reports <strong>of</strong> GPs were organisedinto two sections: (a) <strong>the</strong> framework incorporating<strong>the</strong> processes and procedures GPs reported usingto diagnose and treat depression and challenges<strong>the</strong>y faced, and (b) differences <strong>between</strong> Maoriand non-Maori patients.Diagnosing and treating depressionThree primary categories were constructedfrom <strong>the</strong> inductive analyses <strong>of</strong> <strong>the</strong> interviews.These were:210 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchTable 2. Categories constructed from GP interviewsPrimary categories Specific categories DescriptionsIdentifyingdepressionTreatmentdecisionsTreatmentoutcomesCommunication effectivenessRecognising depressionCauses and risks for depressionTreatment options and strategiesPatient expectations re treatmentFactors influencing treatment decisionsBarriers to effective treatmentPatient compliance with treatmentEffectiveness <strong>of</strong> treatmentsPatient responses to treatmentGood communication and a sense <strong>of</strong> trust<strong>between</strong> <strong>the</strong> GP and patient are important foridentifying depressionSigns or indicators used by GPs to recognisedepressionGP views about causes <strong>of</strong> depression and riskfactors for depressionGP options relating to pharmaceutical (medication)and non-pharmaceutical treatmentsPatients’ views about medication and o<strong>the</strong>rtreatmentsPatient factors affecting GP decisions abouttreatment, including age, treatment preferencesand availability <strong>of</strong> treatmentsBarriers relating to medication and counsellingtreatments, and stereotyping <strong>of</strong> mental illnessPatient characteristics related to compliance andreasons for non-complianceGP views about <strong>the</strong> effectiveness <strong>of</strong> treatments fordepressionGP reports about how patients responded totreatments• identifying depression—how GPs reportedidentifying depression;• treatment decisions—factors which influencedGPs’ treatment decisions; and• treatment outcomes—<strong>the</strong> outcomes<strong>of</strong> treatment for depression.Table 2 shows <strong>the</strong>se categories, <strong>the</strong> associatedsubcategories and <strong>the</strong>ir descriptions. These providea framework for understanding <strong>the</strong> strategiesGPs use to identify and treat depression, and acontext for <strong>the</strong> differences some GPs reported<strong>between</strong> Maori and non-Maori patients.enough to be able to recognise any significantchanges in <strong>the</strong>ir behaviour that might indicaterisk factors for depression. Some GPs emphasisedthat an adequate level <strong>of</strong> trust by <strong>the</strong>ir patientswas needed before patients would be comfortableenough to disclose personal issues.Unless your patient feels that <strong>the</strong>y have confidencein you <strong>the</strong>n <strong>the</strong>y’re not going to tell youanything. They’re <strong>of</strong>ten divulging very personal,private information and <strong>the</strong>y’re just not goingto tell you unless <strong>the</strong>y have confidence in you.[Maori GP11, female]Identifying depressionThree specific categories relating to identifyingdepression were evident in GPs’ accounts.1. Communication effectivenessHaving good communication and a sense <strong>of</strong> trust<strong>between</strong> <strong>the</strong> GP and patient were important indetecting signs <strong>of</strong> depression. Effective communicationrequires GPs knowing <strong>the</strong>ir patients well2. Recognising depressionMost GPs reported that patients with depressioncould present in several ways, with differentsymptoms. The most common ways <strong>of</strong> identifyingdepression were disclosure <strong>of</strong> depressiondirectly by <strong>the</strong> patient, <strong>the</strong> patient reportingsymptoms that were commonly associated withdepression and, less commonly, <strong>the</strong> use <strong>of</strong> screeningquestions or a checklist to assess depression.Some GPs noted that women appeared moreVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 211
ORIGINAL SCIENTIFIC PAPErSqualitative researchlikely to say <strong>the</strong>y were depressed. When patientsdid not directly disclose depression, GPs reportedo<strong>the</strong>r indications such as lack <strong>of</strong> motivation, notsleeping well or major negative events occurringin <strong>the</strong> patients’ lives and changes in behaviourpatterns. Patients might use phrases like feelinglow, down, wanting to give up, complaining <strong>of</strong>tiredness, or not being able to sleep.Quite <strong>of</strong>ten it’s <strong>the</strong>ir behaviour ra<strong>the</strong>r than necessarilywhat <strong>the</strong>y say. For instance I find if <strong>the</strong>ystart being difficult and a little bit aggressive anddemanding, or just different from how <strong>the</strong>y havebeen. And <strong>the</strong>n <strong>the</strong>re’s <strong>the</strong> obvious ways when <strong>the</strong>yactually tell you, which is easy. I guess I’m probablyalways looking for underlying reasons for why<strong>the</strong>y’re presenting, ra<strong>the</strong>r than just <strong>the</strong> symptomsthat <strong>the</strong>y come with. [Non-Maori GP3, female]3. Causes and risks for depressionThe most frequently mentioned cause <strong>of</strong> depressionfor <strong>the</strong>ir patients was related to life eventsand <strong>the</strong> patient’s social environment. GPs referredto reactive depression developing as a result <strong>of</strong> amajor traumatic life event. Some examples givenwere breakdown <strong>of</strong> a relationship, loss <strong>of</strong> a lovedone, or becoming chronically ill.Many GPs related depression to specific riskfactors. A personal or family history <strong>of</strong> depressionwas seen as a risk factor, as was havingexperienced abuse, including physical, sexual,and verbal abuse, as well as drug and alcoholabuse. Isolation was also seen as a majorcontributing risk factor for depression. Isolationincluded being separated from families, fromsocial groups, from work, geographical isolation,or emotional isolation.Treatment decisions1. Treatment options and strategiesThe GPs reported two main types <strong>of</strong> treatmentoptions, pharmaceutical (medication) and nonpharmaceuticaltreatments such as counselling.Within each treatment type, treatment decisionswere related to patient age, severity <strong>of</strong> depression,past history, duration <strong>of</strong> symptoms as well aspatient preference.All GPs spoke about <strong>of</strong>fering medication totreat patients with depression, most commonlyfor patients who had moderate to severe levels<strong>of</strong> depression. They reported choosing medication<strong>the</strong>y felt would work best for <strong>the</strong> level <strong>of</strong>severity or that would suit <strong>the</strong> patient. The mainnon-pharmaceutical treatment GPs mentionedwas counselling or psycho<strong>the</strong>rapy. This includedpsychological and psychiatric <strong>the</strong>rapies such ascognitive behavioural <strong>the</strong>rapy, as well as basiccounselling and group counselling.Some GPs mentioned <strong>the</strong>y preferred to <strong>of</strong>fer<strong>the</strong>ir patients counselling <strong>the</strong>rapies first before<strong>the</strong>y would prescribe antidepressant medication,particularly for mild depression. For <strong>the</strong> moreseverely depressed cases <strong>the</strong>y were more likely toconsider medication.I don’t like using medication for depression unlessI’m at a point <strong>of</strong> saying <strong>the</strong>se o<strong>the</strong>r things haven’tdone enough to help a person. They’re still reallydown to despite our own efforts. So I don’t go tomedication first. [Maori GP1, male]Many GPs noted that a combination <strong>of</strong> bothmedication and a counselling <strong>the</strong>rapy was <strong>the</strong>irrecommended ‘best-practice’ treatment for moderateto severely depressed patients. Some nonpharmaceuticaltreatments that were mentionedby <strong>the</strong> GPs included recommending a ‘GreenPrescription’ for physical exercise to help lift<strong>the</strong> mood <strong>of</strong> patients. As well as <strong>the</strong>se treatments,alternative <strong>the</strong>rapies were mentioned bya few GPs. These included rongoa Maori (Maoritraditional medicine), homeopathic remediesand acupuncture.2. Patient expectations regarding treatmentSeveral GPs talked about patients’ views about,and expectations <strong>of</strong>, treatment for depression.These <strong>of</strong>ten related to patients’ attitudesregarding antidepressant medication, which werereported to be diverse. Some mentioned patientswho did not want to be given antidepressantmedication, because <strong>the</strong>y were seen as beingaddictive or having negative side effects. Incontrast, some patients had no problems withtaking antidepressants—<strong>the</strong>y just wanted a‘quick fix’.212 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative research3. Factors influencing treatment decisionsGPs referred to multiple influences on <strong>the</strong>irchoice <strong>of</strong> treatments for depression. Treatmentchoices could be influenced by <strong>the</strong> patient’sage, personal preferences and <strong>the</strong> availability <strong>of</strong>specific treatments. Discussion with <strong>the</strong> patientsabout depression as an illness and <strong>the</strong> possibletreatment options was a priority for many GPs.I really talk to <strong>the</strong> person and it’s a discussion with<strong>the</strong>m and where <strong>the</strong>y’re at, you know… a lot <strong>of</strong>o<strong>the</strong>r people are like yeah I’m not into pills and youknow, you’ve just sort <strong>of</strong> got to leave it <strong>the</strong>re as anoption. [Maori GP9, female]During discussion with <strong>the</strong>ir patients, GPs wouldtalk through <strong>the</strong> treatment options that <strong>the</strong>y feltwere most appropriate for <strong>the</strong>ir patient. Theywere more likely to go ahead with a suggestedtreatment once <strong>the</strong> patient had agreed.I treat <strong>the</strong>m with medication when I feel that<strong>the</strong>y’re using all <strong>the</strong>ir energy to just control <strong>the</strong>irsymptoms and so <strong>the</strong>y’ve got no extra energy tomake changes in <strong>the</strong>ir lives. I give <strong>the</strong> similarity<strong>of</strong>, it’s like a Panadol for a headache. That you take<strong>the</strong> Panadol to get rid <strong>of</strong> <strong>the</strong> headache, but you’vestill got to work out why you’re getting <strong>the</strong> headaches.And I <strong>of</strong>ten say that as an idea to patients.[Non-Maori GP3, female]GPs’ decisions regarding treatment options for<strong>the</strong>ir patients were usually made after assessing<strong>the</strong> severity and duration <strong>of</strong> <strong>the</strong> depression. If <strong>the</strong>GP thought <strong>the</strong> patient’s level <strong>of</strong> depression wasmoderate or severe, <strong>the</strong>y might be more likely totry antidepressants, or antidepressants in conjunctionwith counselling <strong>the</strong>rapy.Well I think if someone, if someone is suicidalyou want to have <strong>the</strong>m on treatment and if <strong>the</strong>y’resuicidal, see a specialist, or a psychiatrist. I mean ifsomeone has had a chronic ongoing depression for,you know some months and <strong>the</strong>y’re just not gettingout <strong>of</strong> it, it’s worthwhile trying an antidepressant.Yeah it’s people generally with more serious symptoms,or with ongoing symptoms, consider tryingan antidepressant. [Non-Maori GP11, male]Access to counselling services was considered byGPs when considering this option. Some accessdifficulties mentioned were cost, lack <strong>of</strong> goodquality <strong>the</strong>rapists, or no <strong>the</strong>rapists being availablein some regions.4. Barriers to effective treatmentBarriers to effective treatment mentioned by GPsincluded patient concerns about taking medicationfor depression, views about counsellingtreatments, and negative stereotyping aroundmental illness. Many GPs felt that <strong>the</strong> stigmasurrounding antidepressant medication was asignificant barrier to patient acceptance and compliancewith treatment for depression.O<strong>the</strong>r barriers to treatment mentioned includedbeliefs about negative side effects from <strong>the</strong>drugs, having to take <strong>the</strong> medication regularlyand <strong>the</strong> lengthy duration <strong>of</strong> <strong>the</strong> treatment. Accessto counselling treatments was very difficultfor many patients due to cost, lengthy waitinglists to <strong>the</strong>rapists, and <strong>the</strong>rapists not being availablelocally.Treatment outcomesThree <strong>the</strong>mes were evident in GPs’ views about<strong>the</strong> factors affecting treatment outcomes.1. Patient compliance with treatmentPatient compliance or non-compliance with treatmentwas usually raised in relation to patients nottaking <strong>the</strong>ir prescribed medication. Some felt lack<strong>of</strong> compliance in taking antidepressant medicationwas related to <strong>the</strong> long course <strong>of</strong> treatment,or to side effects that some patients reported aftertaking medication.2. Effectiveness <strong>of</strong> treatmentsThere was a range <strong>of</strong> views among GPs about<strong>the</strong> effectiveness <strong>of</strong> treatments for depression.Some used observed improvements in <strong>the</strong>irpatients as a basis for assessing treatment effectivenessand some referred to research evidence<strong>the</strong>y had read. Most GPs felt that antidepressantmedication was in many cases an effective treatmentfor depression, especially in conjunctionwith o<strong>the</strong>r treatments. While noting benefitsfrom using medication with <strong>the</strong>ir patients, someVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 213
ORIGINAL SCIENTIFIC PAPErSqualitative researchGPs also emphasised <strong>the</strong> limitations and o<strong>the</strong>rfactors that needed to be considered. Medicationcould be ineffective or inappropriate forsome people. Some medication suited youngerpatients but were not suitable for elderly people.The uncertain nature <strong>of</strong> outcomes from takingmedication was pointed out.3. Patient responses to treatmentThe GPs interviewed commented that <strong>the</strong>re wasa wide range <strong>of</strong> patient responses to treatments.One response noted was patients stopping <strong>the</strong>irmedication. While patients had various reasonsfor ceasing <strong>the</strong>ir drug treatments, it was commonnot to notify or discuss <strong>the</strong> issue with<strong>the</strong>ir GP.… you see <strong>the</strong>m six months later and you ask, howis your depression? And <strong>the</strong>y say, <strong>the</strong>y’re a lot better.And you say, did you take <strong>the</strong> medication? And<strong>the</strong>y say, yeah I took it for a week or I took it for amonth, or I didn’t take it. So yeah <strong>the</strong>re certainlyare some people who don’t take it even though <strong>the</strong>yaccept it. [Non-Maori GP6, male]Differences <strong>between</strong> Maoriand non-Maori patientsDuring <strong>the</strong> interviews GPs were asked aboutdifferences among Maori and non-Maori patientsrelating to diagnosing and treating depression.The most common <strong>the</strong>me evident in <strong>the</strong> analysisrelated to ethnic differences was <strong>the</strong> difficultyin identifying or diagnosing depression in Maoridue to differences in communication styles.1. Identifying depressionSeveral GPs referred to <strong>the</strong> difficulties <strong>the</strong>yhad with diagnosing depression in some Maoripatients. Three specific features evident in <strong>the</strong>interviews were:i. A greater sense <strong>of</strong> stigma relating tomental illness generally and depressionamong Maori patients;ii. Maori patients being less likely to talkabout being depressed;i. Effective communication and anestablished relationship in which <strong>the</strong>patient trusted <strong>the</strong> GP being especiallyimportant for Maori patients before <strong>the</strong>yare likely to talk about personal feelingssuch as depression.The stigma attached to depression wasmentioned by several GPs. This was consistentwith <strong>the</strong> <strong>the</strong>mes that Maori patientswere less likely to talk about depression andneeded to develop a greater sense <strong>of</strong> trustwith GPs before <strong>the</strong>y were willing to talkabout personal feelings.My impression is that <strong>the</strong> Maori patients areperhaps less likely to be forthcoming… like certaingroups, you know <strong>the</strong>y’re always thinking aboutpsychological things. So your average middle-agedEuropean woman is going to come in and tell you Ithink I’m depressed, because… <strong>the</strong>y’d been readingit in a magazine. Your average Maori patient is notgoing to come in and say that as a general rule.Some do, some <strong>of</strong> <strong>the</strong> younger ones [but not] some<strong>of</strong> <strong>the</strong> older women, and hardly ever any <strong>of</strong> <strong>the</strong>men. [Maori GP4, female]Some GPs noted that it is more difficult todiagnose depression among Maori, particularlyMaori men. They are less likely to say <strong>the</strong>y aredepressed and more reluctant to accept a diagnosis<strong>of</strong> depression. Maori men tend to become lesscommunicative when depressed.Quite a few <strong>of</strong> <strong>the</strong>m [Maori males] might come inwith sort <strong>of</strong> funny o<strong>the</strong>r symptoms, physical symptomsand gradually <strong>the</strong>y might disclose that <strong>the</strong>y’redepressed as well. But <strong>of</strong>ten it can be quite hard toget that group <strong>of</strong> people to admit to depression inany sort <strong>of</strong> consultation type really. [Non-MaoriGP7, male]Several GPs reported that some Maori patientshave a different communication style from non-Maori. They take longer to get to know <strong>the</strong>ir GPand trust <strong>the</strong>m, particularly among older Maori.GPs may need to use culturally-specific communicationstyles with Maori patients and allowmore time for trust to develop.I think that sort <strong>of</strong> trust is more likely to be anestablished GP. They don’t want to bring it up withan A&E GP. That’s a problem with Maori people.214 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchThey’re worried about <strong>the</strong> trust… You can imaginewhat depression does to an uncommunicative Maorimale. It just makes <strong>the</strong>m less communicative. Andsometimes you need Maori doctors to be able tolink into that uncommunicative person. Like we’reused to it and don’t get frightened by it and canhandle it. [Maori GP3, female]A few GPs noted that Maori patients can presentdifferently from non-Maori. This meant depressionmay be diagnosed late.One <strong>of</strong> <strong>the</strong> things that you’re always meant to beaware <strong>of</strong>, that <strong>the</strong>y [Maori patients] may presentquite differently. And because <strong>of</strong> that, I guess ifwe’re not aware <strong>of</strong> it, we may not pick it up at <strong>the</strong>same point in time. We may be a bit late in diagnosingit. And so <strong>the</strong>re could be a consequence tothat… They may have progressed to a more seriousstage. [Maori GP5, male]2. Factors influencing treatmentMost <strong>of</strong> <strong>the</strong> GPs (14 out <strong>of</strong> 23) stated explicitlythat <strong>the</strong>ir antidepressant treatment wasnot related to <strong>the</strong> patient’s ethnicity and thattreatment was tailored to <strong>the</strong> specific needs <strong>of</strong>patients.…if I felt medication was indicated on <strong>the</strong> case Iwould <strong>of</strong>fer it to anyone, who was even, regardless<strong>of</strong> <strong>the</strong>ir ethnicity, I wouldn’t differentiate on thatbasis. [Non-Maori GP1, male]Whichever treatment option was recommended,consultation with <strong>the</strong> patient and <strong>the</strong>patient’s agreement were required. The likelycost <strong>of</strong> treatment and whe<strong>the</strong>r <strong>the</strong> GP thought<strong>the</strong> patient could afford a specific treatmentwere issues that were taken into considerationwhen recommending counselling or similar<strong>the</strong>rapies. The availability <strong>of</strong> suitable counsellorsand counsellors <strong>of</strong> <strong>the</strong> same ethnic backgroundas <strong>the</strong> patient were important factorsfor some GPs when considering counselling for<strong>the</strong>ir patients.The o<strong>the</strong>r thing is cognitive behavioural <strong>the</strong>rapy…Is it readily available? Not as much as I’d hoped. Imean counsellors are certainly around, you know,you can get hold <strong>of</strong> counsellors. They’ve beenthrough some difficulties like if you’re trying t<strong>of</strong>ind a Maori one, <strong>the</strong>y’re quite few and far <strong>between</strong>.So <strong>the</strong>re are difficulties trying to tailor your patient’sneeds to what’s available. [Maori GP12, male]A number <strong>of</strong> <strong>the</strong> GPs viewed Maori as generallyhaving better whanau support systems. Somerecognised whanau support as being an integralpart along <strong>the</strong> pathway <strong>of</strong> care to better healthfor patients.I think my Maori patients are more likely to havesupport structures in place that we can tap into,that I can say to <strong>the</strong>m, hey how about talking to soand so. [Maori GP1, male]Some GPs reported that Maori patients tend tobe less accepting <strong>of</strong> <strong>the</strong> idea <strong>of</strong> taking medication.Reasons for reluctance in taking medicationincluded being suspicious <strong>of</strong> pharmacologicalproducts, cost and cultural reasons.I think probably <strong>the</strong> Maori perhaps are a little bit[less] keen on taking anti-depressants than <strong>the</strong> Europeans…part <strong>of</strong> it may be cost, part <strong>of</strong> it just, youknow, perhaps a little bit fearful <strong>of</strong> perhaps a lot <strong>of</strong>medicine, or antidepressants. You know it may bepartly cultural, where some <strong>of</strong> <strong>the</strong> elders might say,you know, you don’t have to take those, or what areyou taking those for, that sort <strong>of</strong> thing. [Non-MaoriGP11, male]DiscussionThe present study investigated reasons whyMaori patients might appear to be less likely tobe diagnosed with depression and less likely tobe prescribed antidepressant medication. Themost likely contributing factor to <strong>the</strong> disparitywas <strong>the</strong> process <strong>of</strong> diagnosing depression.If depression was diagnosed, GPs reported thatMaori patients were <strong>of</strong>fered or recommended asimilar range <strong>of</strong> treatment options to non-Maoripatients. Processes most likely to lead to ethnicdifferences in diagnosing depression were agreater stigma relating to admitting depressionamong Maori patients, Maori patients being lesslikely to talk about being depressed, and <strong>the</strong>need to have effective communication with <strong>the</strong>irGP. Effective communication that allowed Maoripatients to talk about personal feelings, such asVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 215
ORIGINAL SCIENTIFIC PAPErSqualitative researchthose related to depression, was more likely when<strong>the</strong>re was an established relationship <strong>between</strong> <strong>the</strong>GP and patient.The findings <strong>of</strong> <strong>the</strong> present study were intendedto contribute to an understanding <strong>of</strong> <strong>the</strong> reasonswhy Maori patients are less likely to be prescribedantidepressants even though prevalencestudies show Maori to have similar rates <strong>of</strong> depressionto non-Maori. The findings are consistentwith previous reports that depression amongMaori patients is less likely to be diagnosed byGPs than among non-Maori. The implications <strong>of</strong><strong>the</strong>se findings point to <strong>the</strong> need for GPs to takespecial care in establishing effective communicationwith Maori patients, <strong>the</strong> need to gain <strong>the</strong>trust <strong>of</strong> Maori patients and note <strong>the</strong> reluctance<strong>of</strong> some Maori patients to talk about personalfeelings which may provide clues about mentalwell-being and depression.A previous study has suggested that Maori healthcare providers are better able to establish effectivecommunication with Maori who have experiencedcancer. 14 The pattern <strong>of</strong> findings we havereported is consistent with <strong>the</strong> view that bothpatient characteristics and health care providercharacteristics are influential in whe<strong>the</strong>r Maoripatients get effective treatment when <strong>the</strong>y aredepressed. 15 Compared to non-Maori, some Maoripatients may be reluctant seek pr<strong>of</strong>essional helpfor depression and to disclose information thatprovides GPs with clues about depression. Healthcare providers who are able to establish effectivecommunication with Maori patients are morelikely to diagnose depression among Maori and<strong>the</strong>n be able to treat it.References1. Arroll B, Goodyear-Smith F, Lloyd T. Depression inpatients in an Auckland general practice. N Z Med J.2002;115(1152):176–9.2. Crengle S, Lay Yee R, Davis P, Pearon JA. A comparison <strong>of</strong>Maori and non-Maori patient visits to doctors: <strong>the</strong> NationalPrimary Medical Care Survey (NatMedCa) 2001/2002. Wellington:Ministry <strong>of</strong> Health, Report 6; 2005.3. Arroll B, Goodyear-Smith F, Kerse N, Hwang M, Crengle S,Gunn S, et al. The prevalence <strong>of</strong> depression among Maoripatients in Auckland general practice. J Prim Health Care.2009;1(1):26–9.4. Oakley Browne MA, Wells JE, Scott KM, editors. Te RauHinengaro: The New Zealand Mental Health Survey. Wellington:Ministry <strong>of</strong> Health; 2006.5. Wyllie A, Goodman K, Akroyd S, Star L. Public health depressioninitiative benchmark survey. Wellington; Ministry <strong>of</strong>Health; October 2005.6. Dew K, Dowell A, McLeod D, Collings S, Bushnell J. ‘Thisglorious twilight zone <strong>of</strong> uncertainty’: mental health consultationsin general practice in New Zealand. Soc Sc Med.2005;61:1189–200.7. Henke R, Chou A, Chanin J, Zides A, Scholle S. Physicianattitude toward depression care interventions: implications forimplementation <strong>of</strong> quality improvement initiatives. ImplementationSci. 2008;3(1):40.8. Pollock K. Maintaining face in <strong>the</strong> presentation <strong>of</strong> depression:constraining <strong>the</strong> <strong>the</strong>rapeutic potential <strong>of</strong> <strong>the</strong> consultation.Health. 2007;11(2):163–80.9. Thomas-MacLean R, Stoppard J, Miedema BB, Tatemichi S.Diagnosing depression: <strong>the</strong>re is no blood test. Can Fam Physician.2005;51(August):1102–3.10. Barney, L, Griffiths, K, Jorm, A, Christensen, H. Stigma aboutdepression and its impact on help-seeking intentions. Aust NZJ Psychiatry. 2006;40(1):51–4.11. Brown, C, Conner, K, Copeland, V, Grote, N, Beach, S,Battista, D, et al. Depression stigma, race, and treatment seekingbehavior and attitudes. J Community Psychol. 2010;38(3):350–68.12. Ministry <strong>of</strong> Health. New Zealand Health Strategy. Wellington;2000.13. Thomas DR. A general inductive approach for analyzing qualitativeevaluation data. Am J Eval. 2006;27(2):237–46.14. Walker T, Signal L, Russell M, Smiler K, Tuhiwai-Ruru R, OtakiCommunity Health Centre, et al. The road we travel: Maoriexperience <strong>of</strong> cancer. N Z Med J. 2008;121(1279):27–35.15. Tapsell R, Mellsop, G. The contributions <strong>of</strong> culture and ethnicityto New Zealand mental health research findings. Int J SocPsychiatry. 2007;53(4):317–24.ACKNOWLEDGEMENTSWe wish to thank<strong>the</strong> GPs who agreedto be interviewedfor this project.FUNDINGThe project was fundedby a grant from <strong>the</strong>Health Research Council<strong>of</strong> New Zealand.COMPETING INTERESTSNone declared.A limitation <strong>of</strong> <strong>the</strong> present study is <strong>the</strong> relativelysmall number <strong>of</strong> GPs interviewed and <strong>the</strong>reliance on GPs’ accounts only. However, <strong>the</strong>findings do provide a lead for fur<strong>the</strong>r researchon possible reasons for <strong>the</strong> underdiagnosis <strong>of</strong>depression among Maori patients. A strength <strong>of</strong><strong>the</strong> study was <strong>the</strong> inclusion <strong>of</strong> both Maori andnon-Maori GPs. While <strong>the</strong> GPs interviewedworked in a range <strong>of</strong> different practices, we didnot have sufficient numbers to make comparisons<strong>between</strong> those working for Maori healthcare providers and GPs working in o<strong>the</strong>r healthcare settings.216 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchPerspectives on adherence to blood pressure–lowering medications among Samoan patients:qualitative interviewsKuinileti Chang Wai MBChB, MMedSci(Hons); C Raina Elley MBChB, PhD; Vili Nosa BA, MA (Hons), PhD;John Kennelly MBChB; Thusitha Mabotuwana BE (Hons); Jim Warren PhDABSTRACTSchool <strong>of</strong> Population HealthThe University <strong>of</strong> Auckland,Auckland, New ZealandAim: To explore influences on adherence to taking long-term medications among Samoan patients in anAuckland general practice.Methods: Twenty Samoan participants from an Auckland general practice were identified and interviewedabout <strong>the</strong>ir views on adherence or non-adherence to taking blood pressure–lowering medications.One-to-one semi-structured interviews using open-ended questions were undertaken in Samoanand English, recorded, transcribed and translated into English. Transcriptions were examined by tworesearchers to identify <strong>the</strong>mes.Findings: Patients with ‘high’ and ‘lower’ rates <strong>of</strong> adherence to taking usual medication were identifiedusing medication possession ratio cut-<strong>of</strong>fs from medical records <strong>of</strong> timely prescribing. Ten participantswith ‘high’ and 10 with ‘lower’ rates <strong>of</strong> adherence were interviewed, including 11 women and nine men.Themes identified for those with lower adherence included ‘lack <strong>of</strong> transport’, ‘family commitments’,‘forgetfulness’, ‘church activities’, ‘feeling well’ and ‘priorities’. Themes identified for those with highrates <strong>of</strong> adherence included ‘prioritising health’, ‘previous event’, ‘time management’, ‘supportive familymembers’ and ‘relationship with GP (language and trust)’. A <strong>the</strong>me common to both was ‘coping with <strong>the</strong>stress <strong>of</strong> multiple comorbidities’.Conclusion: Reasons for adherence and non-adherence to taking blood pressure–lowering medicationsamong <strong>the</strong> Samoan patients interviewed were multifactorial and encompass personal, social,cultural and environmental factors. Interdisciplinary teams to support treatment decisions (including Pacifichealth pr<strong>of</strong>essionals or community health workers), systematic identification <strong>of</strong> those with low rates<strong>of</strong> adherence, phone or text follow-up, use <strong>of</strong> church or family networks, provision <strong>of</strong> transport whereneeded and better tools and resources may help address this problem.Keywords: Medication adherence; New Zealand; Pacific Islands; ethnic groups; qualitative research;antihypertensive agentsJ PRIMARY HEALTH CARE2010;2(3):217–224.IntroductionRaised blood pressure is an important risk factorfor cardiovascular and renal disease. 1–7 There isstrong evidence that lowering blood pressure reducescardiovascular and renal events. 8,9 However,only about 30% <strong>of</strong> patients who take blood pressure–loweringmedication achieve adequate bloodpressure control. 10 According to <strong>the</strong> World HealthOrganization (WHO), at least 50% <strong>of</strong> patients donot take <strong>the</strong>ir blood pressure–lowering medicationsas prescribed. 11 Low adherence threatens <strong>the</strong>effectiveness <strong>of</strong> <strong>the</strong>se medications. Unfortunatelyfew interventions have been shown to improveadherence. 3,12,13 The WHO estimates that morehealth benefit could be achieved by successfulinterventions to improve adherence than fromnew medications. 11Correspondence to:C Raina ElleyDepartment <strong>of</strong> GeneralPractice and PrimaryHealth Care, School <strong>of</strong>Population Health, TheUniversity <strong>of</strong> Auckland,PB 92019, Auckland,New Zealandc.elley@auckland.ac.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 217
ORIGINAL SCIENTIFIC PAPErSqualitative researchTable 1. Participant characteristicsParticipant Age SexIt is known that Pacific Island people in NewZealand have high rates <strong>of</strong> coronary heart disease,hypertension, diabetes and renal disease,including dialysis, compared with Europeans. 14–19Fur<strong>the</strong>rmore, low rates <strong>of</strong> adherence have beendocumented in Pacific people. A recent audit <strong>of</strong>a largely Pacific clinic found that 38% <strong>of</strong> patientswith ‘hypertension’ routinely failed to collect<strong>the</strong>ir prescriptions in a timely fashion. 20 Some <strong>of</strong><strong>the</strong> factors that have been suggested to influenceadherence among Pacific people include socioeconomicfactors, cultural values and beliefs,attitudes towards taking medications, views surroundingtraditional healing practices comparedwith Western methods, and <strong>the</strong> side effects <strong>of</strong><strong>the</strong> medications in use. 21–24Years inNew ZealandYears diagnosed with‘hypertension’P1 60 Male 10 5P2 70 Female 11 20P3 70 Male 17 4P4 69 Female 44 10P5 46 Female 13 1P6 64 Female 21 12P7 45 Male 19 7P8 47 Male 3 9P9 81 Male 51 9P10 68 Male 36 10P11 61 Female 42 13P12 44 Female 21 5P13 63 Female 6 6P14 59 Female 33 4P15 59 Male 38 4P16 66 Male 45 5P17 41 Female 41 3P18 65 Female 7 22P19 63 Male 36 28P20 55 Female 9 7There are few studies that have investigated <strong>the</strong>reasons and no studies among Samoan people inNew Zealand primary care. Understanding <strong>the</strong>reasons and addressing <strong>the</strong>se directly may informinterventions to improve adherence and in turnimprove health outcomes for Pacific people inNew Zealand. The aim <strong>of</strong> this study was to exploreinfluences on adherence to taking long-termmedications among Samoan patients in an Aucklandgeneral practice. The study was a qualitativedescriptive study using one-to-one interviews.MethodsStudy populationThe study population included Samoan patientswithin one predominantly Pacific general practicein Auckland. An independent researcher randomlyselected 10 Samoan patients with ‘high rates <strong>of</strong>adherence’ and 10 Samoan patients with ‘lowerrates <strong>of</strong> adherence’ to taking blood pressure–lowering medications from 280 patients withhypertension, identified only by code numberin a recent audit <strong>of</strong> <strong>the</strong> practice. 20 ‘High rates <strong>of</strong>adherence’ was defined as a medication possessionratio (MPR) <strong>of</strong> at least 80%. 20,25 In o<strong>the</strong>r words,more than 80% <strong>of</strong> days from <strong>the</strong> previous 12months were covered by a prescription accordingto practice records. ‘Lower rates <strong>of</strong> adherence’ wasdefined as an MPR <strong>of</strong> less than 80%.The codes <strong>of</strong> <strong>the</strong> 20 selected patients were givento <strong>the</strong> principal author, a clinician at <strong>the</strong> practice,who <strong>the</strong>n matched codes with names and contacted<strong>the</strong> patients by phone to invite participation in<strong>the</strong> study. If <strong>the</strong>y were interested, patients weresent a participant information sheet in Samoan orEnglish. Informed consent was obtained prior tocommencement <strong>of</strong> <strong>the</strong> interview. Invited patientswere assured that <strong>the</strong>ir decision to participate ornot would not affect <strong>the</strong>ir care.InterviewsA semi-structured interview schedule was used.All interviews were one-to-one and recorded byaudiotape. The interviews were conducted inSamoan or English, according to <strong>the</strong> choice <strong>of</strong><strong>the</strong> participant, by <strong>the</strong> principal author who isfluent in both languages. The interview questionswere informed by a literature search and previousstudies addressing this specific area. 26 Allinterviews were conducted during 2008 at <strong>the</strong>usual general practice <strong>of</strong> <strong>the</strong> participant, althoughparticipants were given <strong>the</strong> choice <strong>of</strong> home orpractice venue. Interviews were approximately45 minutes in duration. Demographic informa-218 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchtion was also collected, as was information aboutusual medications and known medical conditions.AnalysisThe taped interviews were transcribed and transcriptionssent to <strong>the</strong> patients for final commentbefore completing analysis <strong>of</strong> <strong>the</strong> interviews.The principal author listened to <strong>the</strong> audiotapes,transcribed, interpreted and translated <strong>the</strong> interviewsfrom Samoan into English. The transcriptswere analysed separately by two researchers toidentify <strong>the</strong>mes.Ethical approvalExpedited ethical approval for <strong>the</strong> study wasgranted by <strong>the</strong> Nor<strong>the</strong>rn X Regional Ethics Committeein February 2008, Ministry <strong>of</strong> Health(NTX/08/17/EXP).FindingsAll 20 participants completed <strong>the</strong> interviews.Nineteen were undertaken in Samoan. One participantwas New Zealand–born and chose to have<strong>the</strong> interview conducted in English. Participantcharacteristics are included in Table 1. Elevenwere female and ranged in ages from 41 to 81years (mean 60 years). The time spent in New Zealandranged from three to 51 years (mean 25 years)and <strong>the</strong> duration <strong>of</strong> ‘diagnosed hypertension’varied from one to 28 years (mean nine years).Participants had <strong>between</strong> one and eight long-termconditions, such as obesity, hypertension, diabetes,gout, hyperlipidaemia, chronic obstructiveairways disease, bronchiectasis, cerebrovascularaccidents (strokes), myocardial infarction (heartattacks), aortic stenosis, hepatitis B carrier, Parkinson’sdisease, peptic ulcer and osteoarthritis.Themes from those with ‘lowerrates <strong>of</strong> adherence’Lack <strong>of</strong> transportA number <strong>of</strong> participants commented on <strong>the</strong> lack<strong>of</strong> transport as a problem for <strong>the</strong>m not attending<strong>the</strong>ir clinic appointments, <strong>the</strong>reby being unableto collect <strong>the</strong>ir prescriptions for <strong>the</strong>ir medicationWHAT GAP THIS FILLSWhat we already know: Adherence to taking long-term medications islow internationally, including among Pacific people. Pacific people have highrates <strong>of</strong> cardiovascular and renal morbidity and mortality. Little is knownabout <strong>the</strong> reasons for ‘high’ or ‘lower’ rates <strong>of</strong> medication adherence amongPacific patients. Rates <strong>of</strong> medication adherence can be estimated using medicationpossession ratio (MPR), or <strong>the</strong> percentage <strong>of</strong> days over <strong>the</strong> previous 12months that were covered by a prescription according to practice records.What this study adds: Factors contributing to lower rates <strong>of</strong> adherenceto taking antihypertensive medication by Samoan patients include lack <strong>of</strong>transport, family and church commitments and priorities, forgetfulness,time management issues and feeling ‘well’. Factors conducive to adherenceinclude family support, prioritising health, a previous cardiovascular event,and a good relationship with <strong>the</strong> health pr<strong>of</strong>essional. Common language andcultural understanding <strong>between</strong> patient and health pr<strong>of</strong>essional also assists inadherence to taking medication.supply. For example, participant 13 (female, aged63) commented:Everyone at home works, so <strong>the</strong>re is no one to bringme to <strong>the</strong> clinic when my appointment is due. Ihave to wait for someone to be free and that couldbe weeks, meanwhile, my tablets are finished. Idon’t want to be a pain to <strong>the</strong> workers, so I wait forone <strong>of</strong> <strong>the</strong>m to be free.Participant 20 (female, aged 55) commented:I take <strong>the</strong> bus because <strong>the</strong>re is no car at home, but ifit is a rainy day, <strong>the</strong>n I stay home, because <strong>the</strong> busstop is a little far from home.Family commitmentsFamily commitments were also highlighted asano<strong>the</strong>r factor for not taking high blood pressuremedication. This included being busy with lookingafter children for <strong>the</strong> women, and for <strong>the</strong> menit included <strong>the</strong>ir commitment to <strong>the</strong>ir work as part<strong>of</strong> being <strong>the</strong> main breadwinner, <strong>the</strong>reby showing<strong>the</strong>ir commitment to <strong>the</strong>ir family. For example,participant 6 (female, aged 64) commented:I <strong>of</strong>ten look after <strong>the</strong> grandchildren, so I am verybusy looking after <strong>the</strong>m, that I forget my tablets,until late in <strong>the</strong> night. By <strong>the</strong>n, it is too late totake <strong>the</strong>m.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 219
ORIGINAL SCIENTIFIC PAPErSqualitative researchParticipant 7 (male, aged 45) commented:I have a busy job and I work long hours <strong>of</strong>ten leavinghome very early in <strong>the</strong> morning and not returningtill very late at night, so I do forget my tablets alot <strong>of</strong> <strong>the</strong> time.ForgetfulnessSome <strong>of</strong> <strong>the</strong> participants mentioned that <strong>the</strong>y <strong>of</strong>tenforget to take <strong>the</strong>ir medications. For example,participant 17 (female, aged 41) commented:My day is usually very busy with taking childrento <strong>school</strong>, <strong>the</strong>n <strong>the</strong>re’s <strong>the</strong> shopping and houseworkand <strong>the</strong>n back at <strong>the</strong> <strong>school</strong> again in <strong>the</strong> afternoonto collect children and once we are home, <strong>the</strong>re’s<strong>the</strong> evening food to prepare, so I forget my tablets.On some days, like <strong>the</strong> weekends, even if I am notbusy, I just forget about <strong>the</strong> tablets, which I knowis bad, but I can’t help it, I am just forgetful.Church activitiesMany <strong>of</strong> <strong>the</strong> participants also spoke <strong>of</strong> <strong>the</strong>irresponsibilities within <strong>the</strong> church as ano<strong>the</strong>rfactor that contributed. For example, participant 1(male, aged 60) commented:There is always family responsibilities and churchactivities, like I am a deacon at church, so <strong>the</strong>responsibilities <strong>the</strong>re are a lot with all <strong>the</strong> meetingsyou have to go to, so it is easy to forget <strong>the</strong> tablets.Feeling wellSome <strong>of</strong> <strong>the</strong> participants stated that <strong>the</strong>y didnot take <strong>the</strong>ir medications when <strong>the</strong>y felt well.For example, participant 7 (male, aged 45) commented:When I feel well, I do not take my medication. Ionly take my tablets when I feel unwell like myhead is hurting. Sometimes I do not take my tabletsfor about three or more weeks.PrioritiesSome did not see taking <strong>the</strong>ir medications as apriority. For example, participant 10 (male, aged68) commented:I never liked taking tablets in my forties because Iwas too busy partying and drinking, but <strong>the</strong>n afterI had my stroke and now that I am getting older, Ineed to take my tablets, so I am better at taking <strong>the</strong>tablets now.Themes from those with ‘highrates <strong>of</strong> adherence’Prioritising healthMost knew that <strong>the</strong>ir medications were importantso <strong>the</strong>y prioritised taking <strong>the</strong>ir tablets over o<strong>the</strong>ractivities. This group <strong>of</strong> participants also knewexactly what kind <strong>of</strong> medication <strong>the</strong>y were taking,and if <strong>the</strong>y did not remember <strong>the</strong> names <strong>of</strong><strong>the</strong> tablets, <strong>the</strong>y knew <strong>the</strong> reasons why <strong>the</strong>y weretaking <strong>the</strong> tablets such as a description <strong>of</strong> <strong>the</strong>tablets as below:Participant 14 (female, aged 59) commented:If I don’t take my medication <strong>the</strong>n I don’t lovemyself at all, so yes, it’s important to me to take mymedication as instructed. For example, I take mybetaloc in <strong>the</strong> morning <strong>the</strong>n my cartia after food.At lunchtime, I take my next tablet. However, if Inotice that my medication bag is still on <strong>the</strong> fridge<strong>the</strong>n I know I have not taken my tablet.Previous eventSome <strong>of</strong> <strong>the</strong> patients had experienced events suchas stroke or heart attack and <strong>the</strong>y did not wantano<strong>the</strong>r event. So, <strong>the</strong>y made sure that <strong>the</strong>y took<strong>the</strong>ir medications.Participant 10 (male, aged 68) commented:I used to be very bad at taking my tablets in my youngerdays, but now, after my stroke, I make sure I takemy tablets everyday so I do not get ano<strong>the</strong>r stroke.Participant 8 (male, aged 47) commented:The day I had my stroke was a very bad day, so Idecided I needed to make some changes and listento my doctor and take <strong>the</strong> tablets. I still have someproblems with walking and my mind being slowafter <strong>the</strong> stroke, but it also reminds me that I needto continue taking my tablets.220 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchTime managementMany planned in advance to collect <strong>the</strong>ir medications.For example, participant 4 (female, aged 69)commented:I make sure I count how many <strong>of</strong> my tablets areleft and when <strong>the</strong>re is only two weeks left <strong>of</strong> mytablets, <strong>the</strong>n I make my appointment to come andsee you to get more tablets.Participant 2 (female, aged 70) commented:I try my best to keep an eye on my tablets, andwhen I see <strong>the</strong>re is only a few left, I tell my childrenthat I need to come and see <strong>the</strong> doctor to geta check-up and get more tablets. My children aregood like that; <strong>the</strong>y will bring me in to <strong>the</strong> doctorsbefore my tablets run out.Supportive family membersMany commented on a supportive family. Familymembers would <strong>of</strong>ten remind <strong>the</strong>m to take <strong>the</strong>irmedication. Participant 3 (male, aged 70) commented:I am lucky that I have my wife. She knows everythingand she reminds me when I need to take mytablets.Participant 18 (female, aged 65) commented:My husband is very good at reminding me aboutmy medications. O<strong>the</strong>rwise I forget. Sometimeswhen he reminds me, I get annoyed but <strong>the</strong>n Iknow that it is important to take my medications,o<strong>the</strong>rwise I would not be here.<strong>Relationship</strong> with <strong>the</strong> GP—languageThe majority <strong>of</strong> <strong>the</strong> participants commentedon <strong>the</strong> importance <strong>of</strong> language, whereby <strong>the</strong>yfelt comfortable communicating with a Samoandoctor.As participant 3 (male, aged 70) said:We went all <strong>the</strong> way to… to see Dr… because he wasSamoan and we wanted to talk to him in our ownlanguage so we can understand each o<strong>the</strong>r…and itwas good to be able to talk in Samoan. This helpedus understand <strong>the</strong> blood pressure problem and <strong>the</strong>need for medication plus diet changes and exercise.Participant 20 (female, aged 55) commented:It was <strong>the</strong> Samoan doctor, Dr… who explained hypertensionto me and so I really understood what he said.Participant 6 (female, aged 64) commented:I like coming here to see you since I can talk to youin Samoan and I know that you understand and Ican also understand what you say. Sometimes whenI come in and you are not here, I get shy since I donot have good English and so I prefer to wait until Ican get an appointment to see you.<strong>Relationship</strong> with <strong>the</strong> GP—trustAll participants had comorbid conditions andmultiple medications. The majority <strong>of</strong> <strong>the</strong> participantsthought that <strong>the</strong>y were coping well with<strong>the</strong> multi-medication regimes, although a few didmention that <strong>the</strong>ir families expressed concernabout <strong>the</strong> number <strong>of</strong> tablets <strong>the</strong>y were taking.Participant 6 (female, aged 64) commented:My children come home and look at my tablets.Then <strong>the</strong>y worry and ask why I am taking so manytablets and maybe I should stop some <strong>of</strong> <strong>the</strong>m. Ijust tell <strong>the</strong>m that I have to listen to my doctor andtake my medication, no matter how many <strong>the</strong>re are.Participant 16 (male, aged 66) commented:Even though I take a lot <strong>of</strong> tablets, I don’t mindsince I want to be well, and <strong>the</strong> doctors know what<strong>the</strong>y are doing, so I do my part and take my tablets.Coping with <strong>the</strong> stress <strong>of</strong>multiple comorbiditiesMany participants admitted that <strong>the</strong> multiplemedical conditions and medications were stressful.Some coped by having a positive attitude.Participant 16 (male, aged 66) commented:Even though my life is busy with being a builderand having to advise my children…, add to this<strong>the</strong> problem <strong>of</strong> pain in my back from arthritis plusVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 221
ORIGINAL SCIENTIFIC PAPErSqualitative researchblood pressure problem, <strong>the</strong>re are some days whenI have just had enough <strong>of</strong> all <strong>the</strong> stress. But, <strong>the</strong>n, Ithink <strong>of</strong> those who are less fortunate than me, <strong>the</strong>nI try and focus on <strong>the</strong> good things and cope thatway, so I do not feel sad.Participant 18 (female, aged 65) commented:If it was just <strong>the</strong> blood pressure problem, I wouldbe okay. But add to this <strong>the</strong> Parkinson’s plus <strong>the</strong>diabetes and all <strong>the</strong>se tablets I have to take, <strong>the</strong>nI sometimes feel sad. But, I am usually a positiveperson and I have a good sense <strong>of</strong> humour, so I donot feel sad for very long at all.Those who did not cope so well with <strong>the</strong> comorbiditiesplus <strong>the</strong> pressures <strong>of</strong> lack <strong>of</strong> finance andlack <strong>of</strong> support made <strong>the</strong> following remarks:Participant 17 (female, aged 41) commented:There are times when I feel all <strong>the</strong> pressure from financesand having no support, add to that all <strong>the</strong>semedical problems <strong>the</strong>n I feel down.When asked about suicide ideation, <strong>the</strong> sameparticipant said:When I look at my children, I know I cannot doanything like that, so <strong>the</strong>y help me get out <strong>of</strong> <strong>the</strong>bad place.Participant 20 (female, aged 55) denied that <strong>the</strong>yhad diabetes but accepted <strong>the</strong>y had hypertension:The diagnosis <strong>of</strong> diabetes made me angry since<strong>the</strong>re is no one in my family who has diabetes andso <strong>the</strong>refore I will not accept <strong>the</strong> diagnosis and I amnot going to take <strong>the</strong> tablets.DiscussionMain findingsThis is <strong>the</strong> first study to investigate reasonsfor high or lower rates <strong>of</strong> adherence to takinglong-term medications among Samoan people inNew Zealand primary health care. This studyhas highlighted that those with lower rates <strong>of</strong>adherence had a number <strong>of</strong> issues such as lack <strong>of</strong>transport, family commitments, forgetfulness,church activities, feeling well and o<strong>the</strong>r prioritiesthat contributed to <strong>the</strong> non-adherence to takingblood pressure medications. On <strong>the</strong> o<strong>the</strong>r hand,<strong>the</strong>mes from those with high rates <strong>of</strong> adherenceincluded: prioritising health; a previous cardiovascularevent; time management; supportivefamily members and <strong>the</strong> relationship with <strong>the</strong>irGP, both in terms <strong>of</strong> a common language andtrust. The majority <strong>of</strong> participants also had anumber <strong>of</strong> comorbid conditions and multiplemedication regimes, which <strong>the</strong>y found stressful.There was a range <strong>of</strong> coping mechanisms fromhaving a positive attitude to denial <strong>of</strong> <strong>the</strong> condition,and hence conscious non-adherence.Compared with <strong>the</strong> literatureThese findings reflect <strong>the</strong> Samoan model <strong>of</strong>health as described by <strong>the</strong> Fon<strong>of</strong>ale model,whereby health belief is viewed in <strong>the</strong> context <strong>of</strong>culture, language, and family, and encompassestime and <strong>the</strong> environment that surrounds aperson. 23 For example, <strong>the</strong> importance <strong>of</strong> cultureand language came through, where patients werewilling to travel long distances to see a doctor <strong>of</strong><strong>the</strong>ir own ethnicity because <strong>the</strong>y could understand<strong>the</strong> explanations about <strong>the</strong>ir medical condition,<strong>the</strong>refore encouraging adherence.A study by Barnes et al. in 2004 comparedillness beliefs and adherence in diabetes mellitus<strong>between</strong> Tongan and European patients.This study found that <strong>the</strong>re was a perceptionthat some <strong>of</strong> <strong>the</strong> medications were unnecessary,and higher levels <strong>of</strong> emotional distress relatedto <strong>the</strong>ir diabetes, among <strong>the</strong> Tongan participants,which were associated with lower rates<strong>of</strong> adherence to diet and medication taking. Thestudy highlighted <strong>the</strong> need for an assessment<strong>of</strong> patients’ personal and cultural beliefs about<strong>the</strong>ir illness and, most importantly, that <strong>the</strong>reis a need to understand <strong>the</strong> patients’ perceptionsabout illness and medication, and this mayprovide avenues for improving adherence to selfcareregimens. 27 The current study found similarbeliefs among some <strong>of</strong> <strong>the</strong> Samoan participantswith lower rates <strong>of</strong> adherence. However, whilesome did not think taking medications wasimportant, more commonly <strong>the</strong> beliefs were that<strong>the</strong> tablets were useful but that <strong>the</strong> ‘busyness’ <strong>of</strong>life took priority.222 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchThere are several factors that have been identifiedin previous studies that contribute to adherence.These include: ‘<strong>the</strong> specific condition beingtreated, <strong>the</strong> health care system and team delivering<strong>the</strong> intervention, <strong>the</strong> social and economicconditions <strong>of</strong> <strong>the</strong> patient and setting, characteristics<strong>of</strong> <strong>the</strong> <strong>the</strong>rapy itself and <strong>the</strong> contribution<strong>of</strong> <strong>the</strong> individual patient’. 1,11,28 In Burnier’s (2006)review, some <strong>of</strong> <strong>the</strong> potential reasons for lowerrates <strong>of</strong> adherence to taking blood pressure medicationscan be divided into physician and patientfactors or medication factors. 1 Physician andpatient factors included cost <strong>of</strong> medication andrelated care; unclear instructions to <strong>the</strong> patient;<strong>the</strong> primary caregivers not increasing <strong>the</strong> doses<strong>of</strong> medications or changing <strong>the</strong> medications; poorpatient education and lack <strong>of</strong> inclusion <strong>of</strong> <strong>the</strong> patientin <strong>the</strong>ir overall plan. Medication-related factorsincluded <strong>the</strong> side effects <strong>of</strong> <strong>the</strong> medicationsand, in addition to this, a complicated dosingregimen. In <strong>the</strong> current study, <strong>the</strong> issues involvingfamily, church and transport, relate both tosocioeconomic factors and cultural priorities.However, <strong>the</strong>re were few comments about <strong>the</strong>medications <strong>the</strong>mselves, potential or actual sideeffects or complicated medication regimes. With<strong>the</strong> problem <strong>of</strong> comorbidities, despite evidencefrom <strong>the</strong> literature that simplifying regimenswould help adherence, 29 none <strong>of</strong> <strong>the</strong> participantsin <strong>the</strong> current study commented on this as a factorfor <strong>the</strong>m.Medication adherence is only one part <strong>of</strong>‘self-management’ where <strong>the</strong> individual mustmanage symptoms, treatment, physical andpsychosocial consequences, and <strong>the</strong> lifestylechanges associated with having a long-termcondition. 30 Two literature reviews <strong>of</strong> selfmanagementinterventions found that diseasespecificinterventions improved knowledge,performance <strong>of</strong> self-management behaviourssuch as medication adherence, self-efficacy andaspects <strong>of</strong> health status compared with standardcare. 30,31 Such interventions included individualorgroup-based education or counselling led byhealth pr<strong>of</strong>essionals, peers or o<strong>the</strong>r lay people,addressing barriers to change or adherence, andsymptom management techniques. 30,31 Consequently,it was recommended that health careproviders focus on improving patients’ selfmanagementabilities, promote flexibility and apatient-centred approach in negotiated managementplans, and improve information provisionfor patients by making it relevant, accessible,while understandable yet evidence-based usingflexible modes <strong>of</strong> delivery. 30,32 Structuralchanges to improve access to services were alsorecommended.Strengths and limitationsThe fact that <strong>the</strong> researcher was also <strong>the</strong> doctor<strong>of</strong> several <strong>of</strong> <strong>the</strong> patients may have influencedparticipation or responses to <strong>the</strong> questions. Thismay limit validity <strong>of</strong> <strong>the</strong> findings. Use <strong>of</strong> anindependent interviewer may have avoided anyrisk <strong>of</strong> participants feeling obliged to participateor limiting responses to questions. On <strong>the</strong> o<strong>the</strong>rhand, <strong>the</strong> interviewer’s fluency in Samoan andMedication adherence is only one part <strong>of</strong> ‘selfmanagement’where <strong>the</strong> individual must managesymptoms, treatment, physical and psychosocialconsequences, and <strong>the</strong> lifestyle changesassociated with having a long-term conditionknowledge <strong>of</strong> and familiarity with <strong>the</strong> participantsmay have been more conducive to trustand disclosure <strong>of</strong> concerns than if interviewedby someone <strong>the</strong>y did not know. The study alsoassumed that patient and clinician initiallyagreed on <strong>the</strong> use <strong>of</strong> blood pressure–loweringmedication, but <strong>the</strong> validity <strong>of</strong> this assumptionwas not explored.Almost all participants were born in Samoa;hence <strong>the</strong> <strong>the</strong>mes may be different for Samoansborn in New Zealand. Fur<strong>the</strong>rmore,only Samoan patients were interviewed. Issuesaround adherence to taking medications maybe different within o<strong>the</strong>r Pacific groups. Thestudy was conducted in one Auckland practice,which again may be different from <strong>the</strong> experiences<strong>of</strong> Samoan people from o<strong>the</strong>r practices oro<strong>the</strong>r regions <strong>of</strong> New Zealand, or indeed in <strong>the</strong>Pacific Islands.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 223
ORIGINAL SCIENTIFIC PAPErSqualitative researchACKNOWLEDGEMENTSThanks to <strong>the</strong> patientsand practice staff <strong>of</strong> <strong>the</strong>participating practice.FUNDINGThanks to <strong>the</strong> PacificTeam at <strong>the</strong> HealthResearch Council for <strong>the</strong>financial award in 2008.COMPETING INTERESTSNone declared.RecommendationsInterdisciplinary teams to support treatmentdecisions (including Pacific health pr<strong>of</strong>essionalsor community health workers with a commonculture and language), systematic identification<strong>of</strong> those with low rates <strong>of</strong> adherence, phone ortext follow-up, use <strong>of</strong> church or family networks,provision <strong>of</strong> transport where needed to improveaccess to care, or use <strong>of</strong> community pharmacies,as well as better tools and resources, may helpaddress <strong>the</strong> problem <strong>of</strong> low rates <strong>of</strong> adherence totaking medications.References1. Burnier M. Medication adherence and persistence as <strong>the</strong>cornerstone <strong>of</strong> effective antihypertensive <strong>the</strong>rapy. Am JHypertens. 2006;19:1190–1196.2. Fahey T, Schroeder K, Ebrahim S, Glynn L. Interventions usedto improve control <strong>of</strong> blood pressure in patients with hypertension.Cochrane Database Syst Rev 2007.3. Schroeder K, Fahey T, Ebrahim S. Interventions for improvingadherence to treatment in patients with high blood pressurein ambulatory settings. Cochrane Database Syst Rev 2004:CD004804.4. Andersson K, Melander A, Svensson C, Lind O, Nilsson JL.Repeat prescriptions: refill adherence in relation to patient andprescriber characteristics, reimbursement level and type <strong>of</strong>medication. Eur J Public Health. 2005;15:621–626.5. Takiya LN, Peterson AM, Finley RS. Meta-analysis <strong>of</strong> interventionsfor medication adherence to antihypertensives. AnnPharmaco<strong>the</strong>r. 2004;38:1617–1624.6. MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J,et al. Blood pressure, stroke, and coronary heart disease.Part 1, Prolonged differences in blood pressure: prospectiveobservational studies corrected for <strong>the</strong> regression dilutionbias. Lancet. 1990;335:765–774.7. Stewart JH, McCredie MRE, Williams SM, Canadian OrganReplacement Register, Fenton SS, Trpeski L, et al. The enigma<strong>of</strong> hypertensive ESRD: observations on incidence and trendsin 18 European, Canadian, and Asian-Pacific populations, 1998to 2002. Am J Kidney Dis. 2006;48:183–191.8. de Galan B, Perkovic V, Ninomiya T, et al. Lowering bloodpressure reduces renal events in type 2 diabetes. J Am SocNephrol. 2009;20:883–892.9. Law M, Morris J, Wald N. Use <strong>of</strong> blood pressure loweringdrugs in <strong>the</strong> prevention <strong>of</strong> cardiovascular disease: meta-analysis<strong>of</strong> 147 randomised trials in <strong>the</strong> context <strong>of</strong> expectations fromprospective epidemiological studies. BMJ. 2009;338:1665.10. Wetzels GEC, Nelemans P, Schouten JS, Prins MH. Factsand fiction <strong>of</strong> poor compliance as a cause <strong>of</strong> inadequateblood pressure control: a systematic review. J Hypertens.2004;22:1849–1855.11. World Health Organization. Adherence to long-term <strong>the</strong>rapies:evidence for action 2003: Available from: http://www.emro.who.int/ncd/Publications/adherence_report.pdf:September 17 2007.12. Fahey T, Schroeder K, Ebrahim S. Interventions used to improvecontrol <strong>of</strong> blood pressure in patients with hypertension.Cochrane Database Syst Rev 2006: CD005182.13. Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonaldHP. Interventions for enhancing medication adherence.Cochrane Database Syst Rev 2007.14. Bell AC, Swinburn BA, Simmons D, Wang W, Amosa H,Gatland B. Heart disease and diabetes risk factors in PacificIslands communities and associations with measures <strong>of</strong> bodyfat. N Z Med J. 2001;114:208–213.15. Schaaf D, Scragg R, Metcalf P. Cardiovascular risk factors levels<strong>of</strong> Pacific people in a New Zealand multicultural workforce.N Z Med J. 2000;113:3–5.16. Scragg R, Baker J, Metcalf P, Dryson E. Prevalence <strong>of</strong> diabetesmellitus and impaired glucose tolerance in a New Zealandmultiracial workforce. N Z Med J. 1991;104:395–397.17. Bell C, Swinburn B, Stewart A, Jackson R, Tukuitonga C,Tipene-Leach D. Ethnic differences and recent trends incoronary heart disease incidence in New Zealand. N Z Med J.1996;109:66–68.18. Scragg R, Baker J, Metcalf P, Dryson E. Hypertension and itstreatment in a New Zealand multicultural workforce. N Z MedJ. 1993;106:147–150.19. Bathgate M. The health <strong>of</strong> Pacific Islands people in New Zealand.Public Health Commission Wellington; 1994.20. Mabotuwana T, Warren J, Gaikwad R, Kennelly J, Kenealy T.Analysis <strong>of</strong> medication possession ratio for improved bloodpressure control—towards a semantic web technology enabledworkbench. Health Care and Informatics Review Online2008;12:19–24.21. Ioasa-Martin I. Tulaga I Talitonuga Fa’aSamoa e Aafia ai letogafiti Ole Gasegase Ole Mafaufau.The role <strong>of</strong> traditionalSamoan beliefs in non-adherence amongst Samoan consumerswith psychotic disorders [Masters Thesis]. VictoriaUniversity; 2006.22. Macpherson C, Macpherson L. Samoan medical belief andpractice. Auckland: Auckland University Press; 1990.23. Pulotu-Endemann F, Spoonley P. Being Samoan: Samoanethnicity in New Zealand. Palmerston North: Massey University;1992.24. Ministry <strong>of</strong> Health. The Pacific Health and Disability ActionPlan. Wellington: Ministry <strong>of</strong> Health; 2002.25. Mabotuwana T, Warren J, Kennelly J. A computationalframework to identify patients with poor adherence toblood pressure lowering medication. Int J Med Inform.2009;78:745–756.26. Morecr<strong>of</strong>t C, Cantrill J, Tully MP. Patients’ evaluation <strong>of</strong> <strong>the</strong>appropriateness <strong>of</strong> <strong>the</strong>ir hypertension management—a qualitativestudy. Res Soc Admin Pharm. 2006;2:186–211.27. Barnes L, Moss-Morris R, Kaufusi M. Illness beliefs and adherencein diabetes mellitus: a comparison <strong>between</strong> Tongan andEuropean patients. N Z Med J. 2004;117:U743.28. Miller DB. Secondary prevention for ischemic heart disease.Relative numbers needed to treat with different <strong>the</strong>rapies.Arch Intern Med. 1997;157:2045–2052.29. van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R,Bensing J. Patient adherence to medical treatment: a review <strong>of</strong>reviews. BMC Health Serv Res. 2007;7:55.30. Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Selfmanagementapproaches for people with chronic conditions: areview. Patient Educ Couns. 2002;48:177–187.31. Newman S, Steed L, Mulligan K. Self-management interventionsfor chronic illness. Lancet. 2004;364:1523–1537.32. Kennedy A, Rogers A, Bower P. Support for self care forpatients with chronic disease. BMJ. 2007;335:968–970.224 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchGeneral practitioner perceptions <strong>of</strong>clinical medication reviews undertaken bycommunity pharmacistsLinda Bryant PhD; Gregor Coster PhD; Ross McCormick PhDABSTRACTIntroduction: Delivery <strong>of</strong> current health care services focuses on interdisciplinary teams andgreater involvement <strong>of</strong> health care providers such as nurses and pharmacists. This requires a change inrole perception and acceptance, usually with some resistance to changes. There are few studies investigating<strong>the</strong> perceptions <strong>of</strong> general practitioners (GPs) towards community pharmacists increasing <strong>the</strong>irparticipation in roles such as clinical medication reviews. There is an expectation that <strong>the</strong>se roles may beperceived as crossing a clinical boundary <strong>between</strong> <strong>the</strong> work <strong>of</strong> <strong>the</strong> GP and that <strong>of</strong> a pharmacist.Department <strong>of</strong> GeneralPractice and Primary HealthCare, The University <strong>of</strong>Auckland, Auckland,New ZealandMethodS: Thirty-eight GPs who participated in <strong>the</strong> General Practitioner–Pharmacists Collaboration(GPPC) study in New Zealand were interviewed at <strong>the</strong> study conclusion. The GPPC study investigatedoutcomes <strong>of</strong> a community pharmacist undertaking a clinical medication review in collaboration with aGP, and potential barriers. The GPs were exposed to one <strong>of</strong> 20 study pharmacists. The semi-structuredinterviews were recorded and transcribed verbatim <strong>the</strong>n analysed using a general inductive <strong>the</strong>maticapproach.Findings: The GP balanced two <strong>the</strong>mes, patient outcomes and resource utilisation, which determined<strong>the</strong> over-arching <strong>the</strong>me, value. This concept was a continuum, depending on <strong>the</strong> balance. Factors influencing<strong>the</strong> <strong>the</strong>me <strong>of</strong> patient outcomes included <strong>the</strong> clinical versus <strong>the</strong>oretical nature <strong>of</strong> <strong>the</strong> pharmacistrecommendations. Factors influencing resource utilisation for general practice were primarily time andfunding.conclusion: GPs attributed different values to community pharmacists undertaking clinical medicationreviews, but this value usually balanced <strong>the</strong> quality and usefulness <strong>of</strong> <strong>the</strong> pharmacist’s recommendationswith <strong>the</strong> efficiency <strong>of</strong> <strong>the</strong> system in terms <strong>of</strong> workload and funding.KEYWORDS: Family physicians; community pharmacy services; drug utilization review; primary healthcare;health plan implementation; qualitative research; interpr<strong>of</strong>essional relationsIntroductionDrug-related morbidity and mortality is a costlyproblem which cannot be resolved by one healthcare pr<strong>of</strong>ession in isolation. The numerous stepsinvolved in <strong>the</strong> generation and resolution <strong>of</strong> adrug <strong>the</strong>rapy problem requires coordination andcollaboration <strong>between</strong> pr<strong>of</strong>essions, usually withinan interdisciplinary team. This role expansion forhealth pr<strong>of</strong>essionals such as pharmacists and nurseshas not necessarily been a comfortable changefor all <strong>the</strong> health care workers ‘at <strong>the</strong> coalface’.Norris 1 reviewed <strong>the</strong> sociological development<strong>of</strong> community pharmacy in New Zealand (NZ)from 1930 to 1990, particularly focussing on <strong>the</strong>negotiation and renegotiation <strong>of</strong> occupationalcontrol, and <strong>the</strong> relationship <strong>between</strong> generalpractitioners (GPs) and pharmacists. Provision<strong>of</strong> health care was a division <strong>of</strong> labour usuallydecided by <strong>the</strong> medical practitioner. Nurseswere considered subordinate to medical practitionersand occupations such as optometryhad limited practice opportunities or required aJ PRIMARY HEALTH CARE2010;2(3):225–233.Correspondence to:Linda BryantDepartment <strong>of</strong> GeneralPractice and PrimaryHealth Care, TheUniversity <strong>of</strong> Auckland,PB 92019 Auckland,New Zealandlinda@cpsl.bizVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 225
ORIGINAL SCIENTIFIC PAPErSqualitative researchreferral system. Pharmacists were subordinate tomedical practitioners in terms <strong>of</strong> being requiredto dispense prescriptions written by <strong>the</strong> medicalpractitioner, but generally had commercialindependence and autonomy, unlike practicenurses who are seen as a core part <strong>of</strong> <strong>the</strong> healthcare team. The pharmacist’s place in <strong>the</strong> medicalmodel was ill-defined and marginal. Because<strong>the</strong>y were associated with shopkeeping, <strong>the</strong>rewas a perception that pharmacists were taintedas health pr<strong>of</strong>essionals. 1 This is a view shared by<strong>the</strong> British researchers Harding and Taylor. 2A small number <strong>of</strong> qualitative studies exploringgeneral practitioners’ views <strong>of</strong> community pharmacistshave helped identify barriers to collaborationwith community pharmacists. Early studiesindicated that GPs were unaware <strong>of</strong> pharmacists’pr<strong>of</strong>essional training and responsibilities, viewing<strong>the</strong>m as players in <strong>the</strong> commercial or retail environment.3,4 In o<strong>the</strong>r studies, medical practition<strong>of</strong><strong>the</strong> GPs saw <strong>the</strong> practice pharmacist as <strong>the</strong>preferred model because it removed <strong>the</strong> complicationsassociated with <strong>the</strong> shopkeeper image.Edmunds and Calnan 8 considered <strong>the</strong> medicalpr<strong>of</strong>ession’s status may be under threat in<strong>the</strong> United Kingdom, particularly from o<strong>the</strong>rhealth-related occupations such as communitypharmacy attempting to re-pr<strong>of</strong>essionalise.Their study explored community pharmacists’and GPs’ perceptions <strong>of</strong> an extended role forcommunity pharmacy using repeat dispensing,extended adherence support and pharmaceuticalcare focussing on ischaemic heart diseaseprovided from within a general practice, asexamples <strong>of</strong> extended services. The interviewees,26 GPs and 37 pharmacists, were selectedfrom extended services schemes and so likelyto be proactive. While <strong>the</strong> GPs had high regardfor pharmacists’ skills and were supportive <strong>of</strong><strong>the</strong> repeat dispensing schemes and pharmacistsWhile <strong>the</strong> GPs had high regard for pharmacists’ skills and weresupportive <strong>of</strong> <strong>the</strong> repeat dispensing schemes and pharmacistshelping patients’ manage <strong>the</strong>ir medicines, <strong>the</strong>y discriminated<strong>between</strong> those activities that were acceptable… and those thatencroached on <strong>the</strong>ir territoryers, usually in a hospital setting, who workedwith or more closely to pharmacists had morepositive perceptions for <strong>the</strong>ir expanding roles. 2,5,6This view apparently has not changed. A 2003British study 7 found that <strong>the</strong> image <strong>of</strong> a communitypharmacist as a shopkeeper was a superordinate<strong>the</strong>me that pervaded o<strong>the</strong>r <strong>the</strong>mes thatemerged—access, hierarchy and awareness. Theshopkeeper image was considered to generate conflict<strong>between</strong> health care and business, with someperverse incentives identified that might serveto increase <strong>the</strong> use <strong>of</strong> drugs. Lack <strong>of</strong> privacy in<strong>the</strong> shop was also noted. Issues <strong>of</strong> territory wereraised with a view <strong>of</strong> community pharmacistsas subordinate to doctors and considered to beon <strong>the</strong> periphery <strong>of</strong> <strong>the</strong> health care team. Manyhelping patients’ manage <strong>the</strong>ir medicines, <strong>the</strong>ydiscriminated <strong>between</strong> those activities that wereacceptable (delegated activities that reduced <strong>the</strong>general practitioner’s workload but didn’t removecontrol) and those that encroached on <strong>the</strong>ir territory.They were ambivalent about o<strong>the</strong>r patientcentredroles, being less keen on communitypharmacists screening for medical conditions ando<strong>the</strong>r clinical activities such as intervening inprescribing decisions, monitoring blood pressureor sharing medical records. The pharmacists werenot considered as equals. 8Ambler 9 noted <strong>the</strong> new initiatives occurring in<strong>the</strong> United Kingdom that impact on pharmacist–general practitioner relationships. Two questionswere discussed. The answer to, ‘Can a226 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchpharmacist currently undertake <strong>the</strong> main task<strong>of</strong> a general practitioner?’ was, ‘Obviously not,as diagnosis beyond minor, self-limiting conditionsis not part <strong>of</strong> <strong>the</strong> pharmacists’ knowledgeor skills base’. However, to <strong>the</strong> question ‘Cana community pharmacist work with a generalpractitioner to provide quality health care?’ itwas considered that <strong>the</strong> answer is ‘yes’, with <strong>the</strong>qualifier that <strong>the</strong> pharmacist is working within<strong>the</strong> general practice.In Australia, an independent report was commissionedby <strong>the</strong> Department <strong>of</strong> Health andAgeing into <strong>the</strong> Home Medicines ReviewProgramme (HMR), a programme similar to thatinvolved in <strong>the</strong> GPPC study with communitypharmacists undertaking patient medicationreviews. 10 Most <strong>of</strong> <strong>the</strong> 27 GPs interviewed wereambivalent about <strong>the</strong> HMRs, considering <strong>the</strong>mineffective in producing substantial improvementsin a patient’s health. The recommendationsincluded allowing direct referrals from <strong>the</strong>general practitioner to accredited pharmacists,without <strong>the</strong> need to go through a communitypharmacy, and allowing <strong>the</strong> accredited pharmaciststo claim fees directly, again without goingthrough <strong>the</strong> community pharmacy.When changing roles, <strong>the</strong> perceptions <strong>of</strong> <strong>the</strong>individuals involved are important because <strong>of</strong><strong>the</strong> barriers or facilitators generated. As pharmacistsmove towards more involvement in clinicalservices, <strong>the</strong> perceptions <strong>of</strong> GPs regarding <strong>the</strong>pharmacists’ shopkeeper image, <strong>the</strong> pharmacists’ability to perform clinical services and <strong>the</strong> pharmacists’role in <strong>the</strong> health care team, influences<strong>the</strong>ir acceptance <strong>of</strong> new pharmacist roles and <strong>the</strong>extent <strong>of</strong> collaboration that can occur.The General Practitioner–Pharmacist Collaboration(GPPC) study was a multi-centred randomised,controlled study conducted <strong>between</strong>2002 and 2004 comparing people older than 65years and on five or more medicines who receiveda clinical medication review with similar patientswho did not receive a consultation. The GPs wereinvited into <strong>the</strong> study by a participating pharmacistand <strong>the</strong>n identified and invited eligiblepatients consecutively until 12 patients wereenrolled. The community pharmacists had accessto patient medical records, met with <strong>the</strong> patientWHAT GAP THIS FILLSWhat we already know: Health care providers, including pharmacists,are under pressure to increase <strong>the</strong>ir input into direct patient care in what maybe traditionally considered general practitioner roles. There is little informationabout how appropriate general practitioners perceive <strong>the</strong> input <strong>of</strong> communitypharmacists into clinical medication reviews for patients.What this study adds: General practitioners who had been exposed tocommunity pharmacists undertaking clinical medication reviews for generalpractice patients, evaluated this service in terms <strong>of</strong> value. The value <strong>of</strong> <strong>the</strong> serviceswas arrived at by balancing <strong>the</strong> potential for improved patient outcomesagainst <strong>the</strong> resources required for <strong>the</strong> service, particularly time and funding.to review <strong>the</strong>ir medicines ei<strong>the</strong>r in <strong>the</strong> pharmacyor at home, and <strong>the</strong>n discussed potential medicationalterations with <strong>the</strong> general practitioner ina meeting that took approximately 10 minutesper patient. There were two to four patientsdiscussed per meeting. The general practitionerswere reimbursed NZ$50 from research funds foreach patient <strong>the</strong>y enrolled and <strong>the</strong> pharmacistsNZ$160 per patient through a government contractto provide medication reviews. The aim <strong>of</strong><strong>the</strong> GPPC study was to determine <strong>the</strong> impact <strong>of</strong>community pharmacy–based clinical medicationreviews on medicines-related health outcomes,and to investigate <strong>the</strong> potential barriers to <strong>the</strong>implementation <strong>of</strong> this service.The aim <strong>of</strong> this qualitative study is to explore <strong>the</strong>perceptions <strong>of</strong> GPs after working in this environmentto determine <strong>the</strong> barriers, if any, thatlimit community pharmacists and GPs workingtoge<strong>the</strong>r clinically. The perceptions <strong>of</strong> pharmacistsare discussed in a companion paper.MethodsAt <strong>the</strong> end <strong>of</strong> <strong>the</strong> GPPC study, face-to-face semistructuredinterviews <strong>of</strong> GPs and pharmacistswere undertaken by <strong>the</strong> pharmacist researcher.Ethical approval for <strong>the</strong> study was obtained from<strong>the</strong> regional ethics committees (ref: 99/207). AllGPs who participated in <strong>the</strong> GPPC study wereinvited to participate in an interview. The interviewswere up to 30 minutes and were audiotapedwith permission from <strong>the</strong> interviewee. Theprimary areas discussed with <strong>the</strong> GPs were:VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 227
ORIGINAL SCIENTIFIC PAPErSqualitative researchTable 1. Characteristics <strong>of</strong> <strong>the</strong> general practitioners interviewed.AgeGenderNationalityLocationGeneral practitioners% (no.)50 years old 22% (10)Range: 33–59 yearsMale 80% (30)Female 20% (8)New Zealand 71% (27)O<strong>the</strong>r29% (11)South African x6, UK x4, USA x1Town 24% (9)Peripheral city 47% (18)City 29% (11)Solo practice 21% (8)• Particularly useful aspects <strong>of</strong> <strong>the</strong>medication review service.• Their existing or envisaged problemswith <strong>the</strong> service.• Practicalities such as communicationissues, implementation issuesand location <strong>of</strong> <strong>the</strong> service.• The future <strong>the</strong>y envisaged for clinical medicationreviews by community pharmacists.The interviews were transcribed and analysedusing QSR NVivo v2.0. An analysis wasundertaken initially within six months <strong>of</strong> <strong>the</strong>interviews using a <strong>the</strong>matic approach, and <strong>the</strong>nre-analysed by <strong>the</strong> same researcher 18 monthslater to aid with consistency <strong>of</strong> interpretation.An inductive reasoning process was used, generatingideas or hypo<strong>the</strong>ses.FindingsThirty-eight <strong>of</strong> <strong>the</strong> 56 GPs who started <strong>the</strong>study were interviewed. Reasons for not beinginterviewed were, primarily, being on holidayat <strong>the</strong> time <strong>of</strong> <strong>the</strong> interview period or not beingable to make an appointment on <strong>the</strong> day <strong>the</strong>researcher was visiting. Of those interviewed,two had been invited by a pharmacist whowithdrew during <strong>the</strong> GPPC study. Overall <strong>the</strong>GPs interviewed had been exposed to one <strong>of</strong> 20study pharmacists, from <strong>the</strong> total <strong>of</strong> 27 studypharmacists. The characteristics <strong>of</strong> <strong>the</strong> GPs aredescribed in Table 1.OverviewThe overarching <strong>the</strong>me from <strong>the</strong> interviews was<strong>the</strong> concept <strong>of</strong> ‘value’, a balance <strong>of</strong> <strong>the</strong> <strong>the</strong>me <strong>of</strong>patient benefits against <strong>the</strong> <strong>the</strong>me <strong>of</strong> resourcessuch as general practitioner time and governmentfunding <strong>of</strong> <strong>the</strong> pharmacist required for <strong>the</strong>service. There was a continuum <strong>of</strong> how muchvalue <strong>the</strong> GPs placed on <strong>the</strong> service, but <strong>the</strong>yconsistently weighed up <strong>the</strong> perceived benefitsFigure 1. Summary <strong>of</strong> <strong>the</strong> <strong>the</strong>matic analysis from <strong>the</strong> general practitioner interviewsVALUEPatient healthoutcomesResourceutilisation• Clinical advice / recommendations– Usefulness / appropriateness– Reassurance• Patient view• Time• Funding• Practicalities– Communication– Location<strong>Relationship</strong>s / role perception228 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchand resources. Influencing this balance wereviews on relationships and territoriality. Thisprovides a complex model that balances twoseparate <strong>the</strong>mes with a range <strong>of</strong> perceptions togive a diverse stance on <strong>the</strong> overarching <strong>the</strong>me<strong>of</strong> ‘value’. An underlying third <strong>the</strong>me related torelationships and territoriality (Figure 1). Thisled to a continuum <strong>between</strong> positive and negativeresponses.The positive responders acknowledged <strong>the</strong> usefulness<strong>of</strong> an outside perspective on <strong>the</strong> patient’sviews and use <strong>of</strong> medicine, and included commentsabout creating an opportunity to stop orchange medicines. As <strong>the</strong> continuum changed tomore negative views, <strong>the</strong> value <strong>of</strong> <strong>the</strong> service wasreduced because some medication problems wereconsidered unsolvable or recommendations hadalready been tried, and so little changed despite<strong>the</strong> effort put in.I thought it was really invaluable because <strong>of</strong>ten,although we try, you know, sometimes you are justso busy you just don’t have a chance to review one’smedication and one <strong>of</strong> <strong>the</strong> problems that we have witholder people is <strong>the</strong>y tend to come in with complaintsabout certain drugs and you end up treating <strong>the</strong>m witha drug, and ano<strong>the</strong>r drug, and you end up chasing yourtail; and that is where it has been really good. [GP1]I suspect for <strong>the</strong> amount <strong>of</strong> time and effort and possibilityeven money that was put into it, I am notconvinced that we made a big difference. [GP3]Of <strong>the</strong> specific aspects that <strong>the</strong> GPs found useful,information on pharmacokinetic issues such asinteractions and dosing in renal impairment wereappreciated and considered important. The GPsconsidered that, with a heavy workload, this wasan area on which <strong>the</strong>y <strong>of</strong>ten found it difficult tomaintain up-to-date information. Similarly, identification<strong>of</strong> actual or potential adverse effectsand issues raised about compliance were useful.Patient health outcomesUsefulness <strong>of</strong> pharmacists’ recommendationsTo help determine <strong>the</strong> value <strong>of</strong> <strong>the</strong> service, GPsconsidered <strong>the</strong> usefulness and appropriateness<strong>of</strong> <strong>the</strong> pharmacist recommendations. The GPsgenerally found <strong>the</strong> recommendations usefulalthough at times <strong>the</strong>oretical. The overall value<strong>of</strong> <strong>the</strong> recommendations appeared to depend onhow frustrating <strong>the</strong> GPs found <strong>the</strong> provision <strong>of</strong>textbook-type advice. Conversely, reassurancethat <strong>the</strong> prescribed medicines were appropriatewas important to some GPs.Lots <strong>of</strong> good advice came out. Lots <strong>of</strong> changes happenedand I think almost 100% <strong>of</strong> <strong>the</strong>m would havedefinite benefits from it, not just in terms <strong>of</strong> drugsor whatever but actually <strong>the</strong>ir well-being improvednoticeably, which was great. [GP4]Medicine is a mixture <strong>of</strong> science and art whereas<strong>the</strong> medication review was purely science andsometimes <strong>the</strong> science doesn’t go with <strong>the</strong> person…The clinical implications versus <strong>the</strong> textbook is notalways <strong>the</strong> same and I think for a reviewer to go insimply from a scientific point <strong>of</strong> view it is not reallygoing to work as I think we have to deal with both<strong>the</strong> science and <strong>the</strong> person <strong>the</strong>mselves. [GP6]Resource utilisationTime and fundingBalanced against <strong>the</strong> <strong>the</strong>me <strong>of</strong> potential patien<strong>the</strong>alth outcomes was <strong>the</strong> <strong>the</strong>me <strong>of</strong> resourceutilisation, with time and funding being <strong>the</strong>primary domains. There was a strong view thatGPs should be funded for <strong>the</strong>ir time as <strong>the</strong>y arestill primarily a fee-for-service business, and notfully capitated. There was also consideration <strong>of</strong><strong>the</strong> expense <strong>of</strong> monitoring recommendations—laboratory time and nurses’ time.Approximately 10 minutes needed to be set asideto talk about each patient, although this was notnecessarily considered a negative if <strong>the</strong> time wasfunded. It was acknowledged that having someone(<strong>the</strong> pharmacist) able to spend time doingresearch or spend time with <strong>the</strong> patient to pick upon potential problems was usually useful.So, I mean, we don’t have <strong>the</strong> time and <strong>the</strong> facilitiesto sit and research. She had about X number<strong>of</strong> patients where she can really work. I don’t have<strong>the</strong> time to do that, so I thought, excellent. In fact,I told her we should really do some more over aperiod <strong>of</strong> time. [GP7]VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 229
ORIGINAL SCIENTIFIC PAPErSqualitative researchNo, in many ways, I mean, time is <strong>the</strong> biggest issue.In many ways it would be lovely if we could sitdown and discuss every third or fourth patient, youknow, and it would be learning for both but <strong>the</strong>reis just not that time or money for that. [GP1]Practical aspects <strong>of</strong> <strong>the</strong> serviceThere were some prompts provided for discussionon <strong>the</strong> practicalities <strong>of</strong> <strong>the</strong>se medication reviews,including <strong>the</strong> preferred communication method,any preference for location <strong>of</strong> <strong>the</strong> service and issueswith <strong>the</strong> implementation <strong>of</strong> recommendations.The preferred communication method forfeedback was face-to-face, with a small numberbelieving face-to-face was useful initially, butonce a relationship was established, a letter wouldbe adequate. Towards <strong>the</strong> end <strong>of</strong> <strong>the</strong> interview itwas asked whe<strong>the</strong>r <strong>the</strong>re would be any benefit inhaving <strong>the</strong> pharmacist work in <strong>the</strong> practice on asessional basis or whe<strong>the</strong>r it was better to have itWhen asked about difficulties in implementingsome <strong>of</strong> <strong>the</strong> recommendations a few admitted thatit was hard to remember who had been reviewed,and to not let <strong>the</strong> medicines review be supersededby o<strong>the</strong>r problems. Extra consultation time neededto be allocated to cover <strong>the</strong> medication review.Interpr<strong>of</strong>essional relationships<strong>Relationship</strong>s was an underlying <strong>the</strong>me thatpotentially influenced <strong>the</strong> balance <strong>between</strong> <strong>the</strong><strong>the</strong>mes <strong>of</strong> patient health outcomes and resourceutilisation. It incorporated views on <strong>the</strong> pharmacist’srole through concepts <strong>of</strong> trust and respect.Having a pr<strong>of</strong>essional relationship with <strong>the</strong> pharmacistwas very important to <strong>the</strong> GPs. Because<strong>the</strong> pharmacists enrolled <strong>the</strong> GPs into <strong>the</strong> study,and so in most situations some prior workingrelationship existed, this view was open to bias.Emerging through <strong>the</strong> <strong>the</strong>me <strong>of</strong> relationships<strong>the</strong>re appeared to be some traces <strong>of</strong> territoriality.Through many <strong>of</strong> <strong>the</strong> comments regarding <strong>the</strong> clinicalrecommendations and implementation, <strong>the</strong>re was an underlyingemphasis on <strong>the</strong> role <strong>of</strong> <strong>the</strong> general practitioner in controlling clinicaldecision-making, and that this was not <strong>the</strong> territory <strong>of</strong> <strong>the</strong> pharmacistprovided from a community pharmacy. A smallmajority <strong>of</strong> <strong>the</strong> GPs thought that having <strong>the</strong>pharmacist in <strong>the</strong> practice was reasonable because<strong>the</strong>y would be independent <strong>of</strong> <strong>the</strong> local pharmacistsand more part <strong>of</strong> <strong>the</strong> general practice team.I would prefer it to be a practice service, I think,yes… I think <strong>the</strong> independent side is quite important.I feel that quite strongly actually… I thinkwe have a different relationship with <strong>the</strong> localpharmacist. [GP8]I think it probably would be good to have <strong>the</strong>pharmacist in <strong>the</strong> practice because if you did have aquery you could go to <strong>the</strong>m and say why or what…plus from <strong>the</strong> point <strong>of</strong> view <strong>of</strong> <strong>the</strong> two way communication<strong>between</strong> <strong>the</strong> doctor and <strong>the</strong> pharmacistit would be better. [GP9]When <strong>the</strong> issue <strong>of</strong> territoriality was specificallyraised, <strong>the</strong> GPs generally commented that thiswas not an issue for <strong>the</strong>m and <strong>the</strong>y did not find<strong>the</strong> medication reviews threatening or encroachingon <strong>the</strong>ir territory, but <strong>the</strong>y could imaginethat it may be a problem for a number <strong>of</strong> <strong>the</strong>ircolleagues. However, through many <strong>of</strong> <strong>the</strong> commentsregarding <strong>the</strong> clinical recommendationsand implementation, <strong>the</strong>re was an underlyingemphasis on <strong>the</strong> role <strong>of</strong> <strong>the</strong> general practitioner incontrolling clinical decision-making, and that thiswas not <strong>the</strong> territory <strong>of</strong> <strong>the</strong> pharmacist.I think initially I was a wee bit sceptical. I supposewe all try to protect our patches a wee bit. Thereis certainly a feeling amongst <strong>the</strong> medical, some <strong>of</strong>my medical colleagues, that it is sort <strong>of</strong> an invasion<strong>of</strong> <strong>the</strong>ir right if you like. I don’t necessarily see it230 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchthat way. I think anything that will benefit us inwhat we do, looking at how we care for people, andalso for <strong>the</strong> people <strong>the</strong>mselves, is fine. I mean itis up to us whe<strong>the</strong>r we actually read that and say,yes, I will do this or do that, or whe<strong>the</strong>r we say,alright, that’s fine thank you and tend to ignore it.It is up to us I guess. [GP10]Well <strong>the</strong>, I think, <strong>the</strong> issue <strong>of</strong>, sort <strong>of</strong>, boundaries.Where was <strong>the</strong> line <strong>between</strong> pharmaceutical adviceand clinical decision-making? And I think that, Ithink, <strong>the</strong>re were one or two points where you justfelt sort <strong>of</strong>, maybe, hackles rising slightly, ‘well that’sour department’ sort <strong>of</strong> thing and I think that is probablyan issue; and that is an attitudinal thing I think,and it is very easy to fall into <strong>the</strong> sort <strong>of</strong>, ‘well, I knowmy individual patients so I don’t know what you aretalking about’, but that is not really <strong>the</strong> point. [GP8]Perceptions <strong>of</strong> a potential futurefor clinical medication reviewsIn response to direct questioning, GPs wereambivalent about whe<strong>the</strong>r <strong>the</strong>re was a future forcommunity pharmacists undertaking clinicalmedication reviews. A reflection <strong>of</strong> this ambivalencewas that over three-quarters <strong>of</strong> <strong>the</strong>m hadnot made a referral for a review since study initiation,although this was a service available outside<strong>of</strong> <strong>the</strong> study. Reasons for not referring includedthat it was not something that was in <strong>the</strong> front<strong>of</strong> <strong>the</strong>ir mind when <strong>the</strong>y were seeing patients,or <strong>the</strong>y were too rushed to refer even if <strong>the</strong>y didthink about it. There were comments that <strong>the</strong>reneeded to be a system to make <strong>the</strong> process more<strong>of</strong> a standard practice and that currently <strong>the</strong>system was not practical.Just over half <strong>the</strong> GPs appeared positive that<strong>the</strong>re was some future for <strong>the</strong> medication reviews.Hesitancy was focussed primarily on <strong>the</strong>funding and time issues, and <strong>the</strong> view that <strong>the</strong>rewould be only a limited number <strong>of</strong> patients whowould be suitable. There were comments that <strong>the</strong>reviews had to be done well if <strong>the</strong>y were going towork, and <strong>the</strong> pharmacist had to have credibility.A wide range <strong>of</strong> views were presented rangingfrom positive to more negative statements.I know how useful it was in <strong>the</strong> hospital, fantasticallyuseful in <strong>the</strong> hospital service, and it shouldbe useful in <strong>the</strong> community too, especially for <strong>the</strong>older people and to make sure that <strong>the</strong>y have goteverything straight because <strong>the</strong>y get so muddled.(Yes, I like <strong>the</strong> idea.) [GP11]From a clinical point <strong>of</strong> view I think it is excellentbut you are going to get back to a point <strong>of</strong> view <strong>of</strong>funding and what you are about to do, regardless <strong>of</strong>how excellent you think it is, will depend totallyon funding. (Sees value but funding issues.) [GP12]I suppose I am slightly guarded about that. I amsure <strong>the</strong>re is a role. I am sure <strong>the</strong>re is an extendedrole for pharmacists, put it that way, but we are stillfiguring out what that is and I guess some <strong>of</strong> us area bit nervous too about, I mean, <strong>the</strong>re are pharmacistswho are very commercially orientated and <strong>the</strong>yare already sort <strong>of</strong> pick around aspects <strong>of</strong> generalpractice which some <strong>of</strong> us tend to think might notbe really be <strong>the</strong>ir business. (No, not keen.) [GP13]DiscussionThe GPs interviewed evaluated <strong>the</strong> benefits topatient health outcomes against <strong>the</strong> resourcesrequired for <strong>the</strong> service to produce a concept <strong>of</strong>‘value’. The threshold for GPs to perceive <strong>the</strong> usefulness<strong>of</strong> <strong>the</strong> recommendations varied, with somefinding that reassurance that <strong>the</strong>y were prescribingappropriately was useful, o<strong>the</strong>rs finding <strong>the</strong>information and advice useful, even if not necessarilyacted upon, and o<strong>the</strong>rs being frustrated by<strong>the</strong> <strong>the</strong>oretical nature <strong>of</strong> some recommendations.GPs considered <strong>the</strong> time and money needed wasa large factor but despite <strong>the</strong> pressure <strong>of</strong> findingtime to spend with <strong>the</strong> pharmacist, most GPspreferred to have a face-to-face discussion with <strong>the</strong>pharmacist. Time and funding may be particularlyrelevant in NZ because <strong>of</strong> our fee-for-service systemand only partial capitation. Provided fundingbarriers can be met, it may be more efficient tohave a clinical pharmacist providing sessions from<strong>the</strong> practice and so be part <strong>of</strong> <strong>the</strong> practice team,with easier communication. In <strong>the</strong> USA and UKpostgraduate-qualified clinical pharmacists havebeen shown to have positive outcomes when workingin primary care clinics or general practices. 11–15GPs tended to distance <strong>the</strong>mselves from viewson territoriality, commenting on how <strong>the</strong>irVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 231
ORIGINAL SCIENTIFIC PAPErSqualitative researchcolleagues may perceive <strong>the</strong> service. While notseeing <strong>the</strong>mselves as territorial, <strong>the</strong>re was anunderlying impression from <strong>the</strong> comments thatcontrol <strong>of</strong> clinical decision-making was <strong>the</strong> roleand territory <strong>of</strong> <strong>the</strong> general practitioner. As longas <strong>the</strong> pharmacist did not encroach on this role,<strong>the</strong>re were no feelings <strong>of</strong> territoriality. Thistends to be similar to <strong>the</strong> work by Edmundsand Calnan. 8 The GPs had high regard for pharmacists’skills that focussed on <strong>the</strong>m helpingpatients ‘manage <strong>the</strong>ir medicines’, but were lessaccepting <strong>of</strong> a more clinical role such as interveningin prescribing decisions, monitoring orsharing patient records. Reebye et al. 16 identifieda suggestion that pharmacists undertaking rolessuch as dependent prescribing should be workingin primary care clinics, under <strong>the</strong> control <strong>of</strong>doctors. Hughes and McCann 7 found that GPsreferred to community pharmacists as ‘shopkeepers’,but a pharmacist located in generalpractices could be considered more part <strong>of</strong> <strong>the</strong>health care team (and under <strong>the</strong> control <strong>of</strong> <strong>the</strong>general practitioner). This greater acceptance <strong>of</strong> apharmacist in <strong>the</strong> general practice was similar to<strong>the</strong> current study.Hospitals have a strong focus on interdisciplinaryteams and continue to develop this conceptwith increasing pr<strong>of</strong>essional respect and trust<strong>between</strong> hospital doctors and pharmacists, allowingbetter teamwork, collaboration and decisionsharing. Within <strong>the</strong> hospital environment <strong>the</strong>reis more opportunity for medical practitioners tohave contact with clinical pharmacists and to beexposed to a new service. This exposure to aneffective service helps break down <strong>the</strong> stereotypicalperceptions as discussed by Adamick et al. 17and will enhance <strong>the</strong> opportunities for fur<strong>the</strong>rimplementation. A new service that is not donewell impedes any fur<strong>the</strong>r implementation.A limitation <strong>of</strong> this study was that <strong>the</strong> GPs generallyhad a prior relationship with <strong>the</strong> communitypharmacist before <strong>the</strong> GPPC study, were willingto participate in <strong>the</strong> study, and <strong>the</strong>refore werepossibly favourably predisposed to <strong>the</strong> concept.The GPs were aware that <strong>the</strong> researcher was apharmacist studying through <strong>the</strong> Department<strong>of</strong> General Practice and Primary Health Careat Auckland University, with a background inpharmacist facilitation, working with GPs in aPrimary Health Organisation. It did not appearthat <strong>the</strong> GPs were providing socially acceptableresponses because <strong>the</strong> researcher was a pharmacist,and some <strong>of</strong> <strong>the</strong> less favourable commentswould support this, although <strong>the</strong> intervieweesmay have responded differently to a general practitionerinterviewer.The lack <strong>of</strong> a second investigator checking <strong>the</strong>transcripts for <strong>the</strong>mes was a limitation.On reflection, it would have been useful toexplore whe<strong>the</strong>r <strong>the</strong> GPs would have useddiscretionary funding to employ a pharmacistto undertake this work. This concept wouldrequire more research on <strong>the</strong> cost-effectiveness<strong>of</strong> clinical pharmacist medication reviews. Theliterature is conflicting with some randomisedcontrolled trials suggesting a lack <strong>of</strong> impact <strong>of</strong>community pharmacists undertaking clinicalmedication reviews, 18–23 but o<strong>the</strong>r studies indicatingthat clinical pharmacists in clinics or generalpractices have a positive impact on patient healthoutcomes. 11,14,24,25 Clinical pharmacists in practicesor clinics occur in <strong>the</strong> United Kingdom and <strong>the</strong>USA, but are only starting in NZ and need fur<strong>the</strong>rresearch into <strong>the</strong> barriers and effectiveness.ConclusionGPs tended to balance <strong>the</strong> <strong>the</strong>mes <strong>of</strong> patientoutcomes against <strong>the</strong> resources required to determine<strong>the</strong> value <strong>of</strong> clinical medication reviewsby pharmacists. Pertinent factors involved <strong>the</strong>quality and usefulness <strong>of</strong> <strong>the</strong> recommendations,<strong>the</strong> efficiency <strong>of</strong> <strong>the</strong> system in terms <strong>of</strong> timeand funding required, and some issues <strong>of</strong> roleperception or territoriality. Taken in conjunctionwith o<strong>the</strong>r literature, it may be more suitable touse clinical pharmacists working within generalpractice to improve <strong>the</strong> efficiency <strong>of</strong> <strong>the</strong> clinicalmedication reviews and reduce drug-related morbidityand mortality. This system would createcloser association and communication with <strong>the</strong>practice team. It may also be preferable for <strong>the</strong>clinical pharmacist to have collaborative prescribingprivileges to implement recommendationsthat are agreed by <strong>the</strong> general practitioner toimprove efficiency, provided some <strong>of</strong> <strong>the</strong> generalpractice funding and territorial barriers are met.232 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchReferences1. Norris P. The negotiation and re-negotiation <strong>of</strong> occupationalcontrol. A study <strong>of</strong> retail pharmacy in New Zealand. 1930–1990.A PhD (Sociology) <strong>the</strong>sis submitted to <strong>the</strong> Victoria University <strong>of</strong>Wellington. Wellington: Victoria University; 1993.2. Harding G, Taylor KM. Pr<strong>of</strong>essional relationships <strong>between</strong>general practitioners and pharmacists in health centres. Br JGen Pract. 1990;40(340):464–6.3. Smith WE, Ray MD, Shannon DM. Physicians‘ expectations <strong>of</strong>pharmacists. Am J Health-Syst Pharm. 2002;59(1):50–7.4. Bleiker P, Lewis A. Extending <strong>the</strong> role <strong>of</strong> community pharmacists:The views <strong>of</strong> GPs. Int J Pharm Pract. 1998;6(3):140–144.5. Sulick JA, Pathak DS. The perceived influence <strong>of</strong> clinicalpharmacy services on physician prescribing behavior: amatched-pair comparison <strong>of</strong> pharmacists and physicians.Pharmaco<strong>the</strong>rapy. 1996;16(6):1133–41.6. Ritchey FJ, Raney MR. Effect <strong>of</strong> exposure on physicians‘attitudes toward clinical pharmacists. Am J Hosp Pharm.1981;38(10):1459–63.7. Hughes C, McCann S. Perceived interpr<strong>of</strong>essional barriers<strong>between</strong> community pharmacists and general practitioners: aqualitative assessment. Br J Gen Pract. 2003;53:600–06.8. Edmunds J, Calnan MW. The repr<strong>of</strong>essionalisation <strong>of</strong> communitypharmacy? An exploration <strong>of</strong> attitudes to extendedroles for community pharmacists amongst pharmacists andgeneral practitioners in <strong>the</strong> United Kingdom. Soc Sci Med.2001;53(7):943–55.9. Ambler S. General practitioners and community pharmacists:times <strong>the</strong>y are a-changing. Br J Gen Pract. 2003;53:594–95.10. Campbell Research & Consulting. Home Medicines ReviewProgram qualitative research project. Final report. http://www.health.gov.au/internet/main/publishing.nsf/Content/B2992EBF12BE7E1ECA2573D8007F91F3/$File/HMR%20Final%20Report.pdf. Canberra, ACT, Australia: Prepared for<strong>the</strong> Department <strong>of</strong> Health and Ageing; Dec 2008.11. Ellis SL, Carter BL, Malone DC, Billups SJ, Okano GJ, ValuckRJ, et al. Clinical and economic impact <strong>of</strong> ambulatory care clinicalpharmacists in management <strong>of</strong> dyslipidemia in older adults:<strong>the</strong> IMPROVE study. Impact <strong>of</strong> Managed Pharmaceutical Careon Resource Utilization and Outcomes in Veterans AffairsMedical Centers. Pharmaco<strong>the</strong>rapy. 2000;20(12):1508–16.12. Malone DC, Carter BL, Billups SJ, Valuck RJ, Barnette DJ,Sintek CD, et al. An economic analysis <strong>of</strong> a randomized, controlled,multicenter study <strong>of</strong> clinical pharmacist interventionsfor high-risk veterans: <strong>the</strong> IMPROVE study. Impact <strong>of</strong> ManagedPharmaceutical Care Resource Utilization and Outcomesin Veterans Affairs Medical Centers. Pharmaco<strong>the</strong>rapy.2000;20(10):1149–58.13. Rothman RL, Malone R, Bryant B, Shintani AK, Crigler B,Dewalt DA, et al. A randomized trial <strong>of</strong> a primary care-baseddisease management program to improve cardiovascular riskfactors and glycated hemoglobin levels in patients with diabetes.Am J Med. 2005;118(3):276–84.14. Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, SundaramV, Rushak<strong>of</strong>f RJ, et al. Effects <strong>of</strong> quality improvementstrategies for type 2 diabetes on glycemic control: a metaregressionanalysis. JAMA. 2006;296:427–40.15. Zermansky AG, Petty DR, Raynor DK, Freemantle N, Vail A,Lowe CJ. Randomised controlled trial <strong>of</strong> clinical medicationreview by a pharmacist <strong>of</strong> elderly patients receiving repeat prescriptionsin general practice. BMJ. 2001;323(7325):1340–3.16. Reebye RN, Avery AJ, Bissell P, Van Weel C. The issue <strong>of</strong> territoriality<strong>between</strong> pharmacists and physicians in primary care.Int J Pharm Pract. 2002;10(2):69–75.17. Adamcik BA, Ransford HE, Oppenheimer PR, Brown JF, EaganPA, Weissman FG. New clinical roles for pharmacists: a study<strong>of</strong> role expansion. Soc Sci Med. 1986;23(11):1187–1200.18. Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L.Systematic review <strong>of</strong> multidisciplinary interventions in heartfailure. Heart. 2005;91(7):899–906.19. Holland R, Brooksby I, Lenaghan E, Ashton K, Hay L, Smith R,et al. Effectiveness <strong>of</strong> visits from community pharmacists forpatients with heart failure: HeartMed randomised controlledtrial. BMJ. 2007. DOI:10.1136/bmj.39164.568183. AE (published23 April 2007).20. Holland R, Lenaghan E, Harvey I, Smith RB, Shepstone L,Lipp A, et al. Does home based medication review keep olderpeople out <strong>of</strong> hospital? The HOMER randomised controlledtrial. BMJ. 2005;330:293–97.21. Carter BL, Chrischilles E, Scales CJ, Hayase N, Bell N. Extent<strong>of</strong> services provided by pharmacists in <strong>the</strong> Iowa MedicaidPharmaceutical Case Management Program. J Am Pharm Assoc.2003;43:24–33.22. Community Pharmacy Medicines Management ProgrammeEvaluation Team. The MEDMAN study: a randomised controlledtrial <strong>of</strong> community pharmacist-led medication managementfor patients with coronary heart disease. Fam Pract.2007;24(2):189–200.23. RESPECT Trial Team. Effectiveness <strong>of</strong> shared pharmaceuticalcare for older patients: RESPECT trial findings. Br J Gen Pract.2010;60(570):10–19.24. Zermansky AG, Petty DR, Raynor DK, Freemantle N,Vail A, Lowe CJ. Randomised controlled trial <strong>of</strong> clinicalmedication review by a pharmacist <strong>of</strong> elderly patientsreceiving repeat prescriptions in general practice. BMJ.2001;323(7325):1340–3.25. Merenich J, Olson KL, Delate T, Rasmussen J, Helling DK,Ward D. Mortality reduction benefits in a comprehensive cardiaccare program for patients with occlusive coronary arterydisease. Pharmaco<strong>the</strong>rapy. 2007;27(10):1370–78.ACKNOWLEDGEMENTSWe wish to thank <strong>the</strong>general practitioners whoparticipated in <strong>the</strong> GPPCstudy, and showed anappreciated willingnessto participate in this newpharmacist service.FUNDINGFunding for <strong>the</strong> GPPCstudy, including <strong>the</strong>interviews, was providedthrough <strong>the</strong> governmentagency, <strong>the</strong> TransitionalHealth Authority(reimbursement <strong>of</strong>general practitioners)and <strong>the</strong> PharmaceuticalSociety Education andResearch Fund (printingand postage costs). Thesefunding bodies had noinfluence on <strong>the</strong> studydesign or any publication.The general practitionerswere funded $NZ150 for<strong>the</strong> for <strong>the</strong> interviews.COMPETING INTERESTSNone declared.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 233
ORIGINAL SCIENTIFIC PAPErSqualitative researchCommunity pharmacist perceptions <strong>of</strong>clinical medication reviewsLinda Bryant PhD; Gregor Coster PhD; Ross McCormick PhDDepartment <strong>of</strong> GeneralPractice and Primary HealthCare, Faculty <strong>of</strong> Medicineand Health Science, TheUniversity <strong>of</strong> Auckland,Auckland, New ZealandAbstractIntroduction: Changes in delivery <strong>of</strong> health care services has led to pressure for community pharmaciststo extend <strong>the</strong>ir traditional role and become more involved with patient-focussed services such asmedication reviews, in collaboration with general practitioners (GPs). This has not been generally implementedinto routine practice, and many barriers have been suggested that inhibit community pharmacistsextending <strong>the</strong>ir role. These have <strong>of</strong>ten focussed on physical or functional barriers. This study explorespossible attitudinal factors that prevent increased participation <strong>of</strong> community pharmacists in medicationreviews undertaken in collaboration with GPs.MethodS: Twenty community pharmacist participants who participated in <strong>the</strong> General Practitioner–Pharmacist Collaboration (GPPC) study were interviewed. The GPPC study investigated <strong>the</strong> outcomes <strong>of</strong>community pharmacists undertaking a clinical medication review in collaboration with GPs, and <strong>the</strong> potentialbarriers. Semi-structured interviews were analysed using a general inductive <strong>the</strong>matic approach.Findings: Emerging <strong>the</strong>mes were that community pharmacists perceived that <strong>the</strong>y were not mandatedto undertake this role, it was not a legitimate role, particularly from <strong>the</strong> business perceptive, and pharmacistswere concerned that <strong>the</strong>y lacked <strong>the</strong> skills and confidence to provide this level <strong>of</strong> input.Conclusion: While <strong>the</strong>re is concern that community pharmacists’ skills are underutilised, <strong>the</strong>reare probable attitudinal barriers inhibiting pharmacists from increasing <strong>the</strong>ir role in clinical medicationreviews. Perceived legitimacy <strong>of</strong> <strong>the</strong> service was a dominant <strong>the</strong>me, which appeared to be related to issuesin <strong>the</strong> business model. Fur<strong>the</strong>r investigation should consider <strong>the</strong> use <strong>of</strong> a clinical pharmacist workingwithin a general practice independent <strong>of</strong> a community pharmacy.KEYWORDS: Community pharmacy services; drug utilization review; primary healthcare; health planimplementationJ PRIMARY HEALTH CARE2010;2(3):234–242.Correspondence to:Linda BryantDepartment <strong>of</strong> GeneralPractice and PrimaryHealth Care, TheUniversity <strong>of</strong> Auckland,PB 92019 Auckland,New Zealandlinda@cpsl.bizIntroductionInternationally <strong>the</strong>re has been a drive for communitypharmacists to extend <strong>the</strong>ir practice froma product focus towards more patient-focussedservices, including involvement in medicationreviews. The term ‘medication review’ encompassesa wide range <strong>of</strong> review types—from a review<strong>of</strong> <strong>the</strong> person’s use <strong>of</strong> <strong>the</strong> medicine (adherencesupport, specific counselling or education) toclinical medication reviews involving collaborationwith <strong>the</strong> prescriber. These reviews have notbeen implemented from community pharmacy asuniversally as could be expected, and are not anintegral part <strong>of</strong> community pharmacy serviceseven though pharmacists appear enthusiastic. Anumber <strong>of</strong> published studies have indicated a lack<strong>of</strong> participation and high withdrawal rate, despitegood intentions by <strong>the</strong> community pharmacists. 1–5This is in contrast to clinical medication reviewsthat are undertaken by clinical pharmacists** In <strong>the</strong> literature, clinical pharmacists are generally those pharmacists who focus primarily on medication use by and for patients for <strong>the</strong> majority<strong>of</strong> <strong>the</strong>ir work, ra<strong>the</strong>r than supply and distribution (dispensing) roles. Previously <strong>the</strong> term was associated with hospital pharmacists workingwith medical teams and seeing patients on <strong>the</strong> wards. It now includes pharmacists in primary care who work closely with general practitioners,usually in general practice / physicians’ <strong>of</strong>fices or primary care clinics. These pharmacists usually have postgraduate qualifications.234 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchwithin a general practice in <strong>the</strong> UK 6 or in primarycare clinics / physicians’ <strong>of</strong>fices in <strong>the</strong> USA. 7–10The literature describes barriers to implementation<strong>of</strong> medicine management services, includingadherence support or medicine use reviews. Thebarriers include:11–18• Time/funding;13,14,19,20,21• Poor use <strong>of</strong> staff;• Lack <strong>of</strong> facilities, includingspace and privacy; 11,12,14,19• Lack <strong>of</strong> interpr<strong>of</strong>essional relationshipsand collaboration with general practitioners,17,18,20,22,23 although those pharmacistsin a non-community pharmacy setting(clinics, family physician <strong>of</strong>fices) were lesslikely to agree that this was a barrier; 18• Postgraduate training and skillsenhancement; 17,20,21• The type <strong>of</strong> role or type <strong>of</strong> communitypharmacy (e.g. managers versusstaff pharmacists; chain store versus independentcommunity pharmacy); 17,20• Concerns about <strong>the</strong> quality <strong>of</strong> <strong>the</strong> reviews,especially in chain store pharmacies; 1720• The attitudes <strong>of</strong> community pharmacists;• Access to documentation, althoughthis was not considered a barrier fornon–community pharmacy pharmacistsbased within physician <strong>of</strong>fices. 18Explorative work into why change is slow andhow change could be managed raises diverse concepts.In a USA study, 24 four consistent factorsemerged from four pharmacies that had successfullyimplemented innovative medication reviewprogrammes. These were:• Philosophy <strong>of</strong> practice—defining valuesthat guide pr<strong>of</strong>essional behaviours and settingpriorities when confronting challengingclinical decisions or ethical dilemmas• Patient care process—assuming responsibilityfor all <strong>the</strong> patient’s drug <strong>the</strong>rapy needs; developinga long-term <strong>the</strong>rapeutic relationshipwith <strong>the</strong> patient; collaborating with physiciansand o<strong>the</strong>r care providers to enhance care• Management system—including creating<strong>the</strong> physical environment <strong>of</strong> care areasWHAT GAP THIS FILLSWhat we already know: Community pharmacists are being encouragedto increase <strong>the</strong>ir participation in patient-focussed services such as medicationreviews. Implementation <strong>of</strong> <strong>the</strong>se services into routine practice have beenvery limited because <strong>of</strong> perceived physical or functional barriers.What this study adds: This study explored attitudes <strong>of</strong> community pharmacistswho participated in a study <strong>of</strong> clinical medication reviews in collaborationwith general practitioners. Barriers to this service were a perceived lack <strong>of</strong>mandate, a lack <strong>of</strong> perceived legitimacy <strong>of</strong> <strong>the</strong> service, and a perception that<strong>the</strong>re was a lack <strong>of</strong> adequacy to provide <strong>the</strong> service.and care rooms that are separate and distinctfrom <strong>the</strong> dispensing environment• Clinical knowledge—access to upto-dateand reliable clinical information;a desire to learn and keep up withcourses and continuing education.Along a similar <strong>the</strong>me, Latif 25 argued that <strong>the</strong>paradigm shift from a product-focussed pr<strong>of</strong>ession<strong>of</strong> dispensing to a more patient-focussedone with ‘shared’ responsibility for optimaldrug <strong>the</strong>rapy outcomes required <strong>the</strong> development<strong>of</strong> an ethical covenant <strong>between</strong> <strong>the</strong>pharmacist and patient. This was considered important,particularly in some organisational settings,e.g. chain drug stores, because <strong>the</strong>re wasan increased opportunity for ethical problems toarise where <strong>the</strong>re could be an inherent conflict<strong>between</strong> pr<strong>of</strong>essional values and organisationaldemands. For example, where <strong>the</strong> primaryreimbursement is from dispensing prescriptionsand selling retail products, a conflict may arisewhen more time is required for patient-focussedactivities such as counselling.Edmunds and Calnan 26 investigated issues evolvingfrom health-related occupations attemptingto re-pr<strong>of</strong>essionalise, including communitypharmacy, a group that <strong>the</strong> authors believed wasdeveloping strategies to enhance its pr<strong>of</strong>essionalstatus as a bid for survival, ra<strong>the</strong>r than tryingto usurp <strong>the</strong> general practitioner’s role per se.They recognised pharmacists were holding backchanges to community pharmacy. They reasonedthat this is because many community pharmacistsstill attribute ultimate authority to <strong>the</strong> generalpractitioner, and that <strong>the</strong>re are internal divisionsVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 235
ORIGINAL SCIENTIFIC PAPErSqualitative research<strong>between</strong> retail pharmacists and employee pharmacists,with pr<strong>of</strong>it-orientated versus health servicesconflicts. The pervasive view <strong>of</strong> pharmacy isdescribed as marginal, incomplete, limited, with‘quasi’ status due to reduced craftsman skillsrequired to compound medicines, and with occupationalor pr<strong>of</strong>essional limitations due to lack<strong>of</strong> control over clinical autonomy with respect toinvolvement with prescription medicines usage,and consequently lack <strong>of</strong> economic autonomybeyond <strong>the</strong> retail role.Edmunds and Calnan considered that pharmacywould remain viable only if full use <strong>of</strong> <strong>the</strong>pharmacists’ skills and qualifications were utilised,yet identified a basic dilemma <strong>of</strong> a conflict<strong>between</strong> community pharmacists as traders orhealth pr<strong>of</strong>essionals. Despite wishing to pursuemore patient-focussed roles, many pharmacistsdid not want to encroach on <strong>the</strong> general practitioner’sterritory, generally seeing <strong>the</strong>ir roleas reducing <strong>the</strong> general practitioner’s workload(delegatory roles) and helping with adherenceproblems and patients’ management <strong>of</strong> medicinesra<strong>the</strong>r than more clinical roles. They describedconflicting views about <strong>the</strong> management <strong>of</strong>long-term medical conditions by pharmacists.Basically, as perceived by <strong>the</strong> pharmacists, <strong>the</strong>reremained an entrenched division <strong>between</strong> generalpractitioners as prescribers and pharmacistsas dispensers. 26The GPPC study was a multi-centred randomised,controlled study conducted <strong>between</strong>2002 and 2004 comparing people older than65 years and on five or more medicines who receiveda clinical medication review, with similarpatients who did not receive a medication review.The trial used community pharmacists workingcollaboratively with general practitioners. Theintervention required <strong>the</strong> pharmacist to meetwith <strong>the</strong> patient, with access to patient medicalrecords, and <strong>the</strong>n meet with <strong>the</strong> general practitionerto discuss potential medication alterations.The pharmacists were funded NZ$160 permedication review. General practitioners werereimbursed for enrolling <strong>the</strong> patient at NZ$50per patient.The aim <strong>of</strong> <strong>the</strong> GPPC study was to determine <strong>the</strong>impact <strong>of</strong> community pharmacy–based clinicalmedication reviews on medicines-related healthoutcomes, and to investigate <strong>the</strong> potential barriersto <strong>the</strong> implementation <strong>of</strong> this service. A poorcompletion rate in <strong>the</strong> study, with only 39% <strong>of</strong>pharmacists who agreed to participate providingusable data, indicated significant barriers to implementation<strong>of</strong> such a service. This paper explores<strong>the</strong> perceptions <strong>of</strong> New Zealand community pharmacistsafter working in this environment andto determine <strong>the</strong> barriers that limit communitypharmacists and general practitioners workingtoge<strong>the</strong>r clinically. The perceptions <strong>of</strong> generalpractitioners are discussed in <strong>the</strong> previous paper. 27MethodsAt <strong>the</strong> end <strong>of</strong> <strong>the</strong> GPPC study face-to-facesemi-structured interviews <strong>of</strong> pharmacists wereundertaken by <strong>the</strong> researcher to determine what<strong>the</strong>y perceived as inhibitors to wider implementation<strong>of</strong> clinical medication reviews. Theinterviews were up to 30 minutes and wereaudiotaped with permission from <strong>the</strong> interviewee.The primary areas discussed with <strong>the</strong>pharmacists were:• Aspects <strong>of</strong> <strong>the</strong> medication reviewservice that went well.• Barriers to <strong>the</strong> provision <strong>of</strong> <strong>the</strong>medication review service.• Practicalities such as communicationprocesses, general practitioner acceptance,patient response, implementationproblems and location <strong>of</strong> <strong>the</strong> service.• The future <strong>the</strong>y envisaged for clinicalmedication reviews.The interviews continued until no fur<strong>the</strong>rinformation or concepts were forthcoming andwere transcribed and analysed using QSR NVivoversion 2.0. An analysis was undertaken by <strong>the</strong>researcher (LB) initially within six months <strong>of</strong><strong>the</strong> interviews. The transcriptions were <strong>the</strong>nre-analysed by <strong>the</strong> researcher using a general inductive<strong>the</strong>matic approach 18 months later to aidwith consistency <strong>of</strong> interpretation. It was on <strong>the</strong>second analysis that <strong>the</strong> <strong>the</strong>mes, beyond <strong>the</strong> basicresponses to <strong>the</strong> questions, emerged.Ethical approval for <strong>the</strong> study was obtained from<strong>the</strong> regional ethics committees (ref: 99/207).236 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchFindingsTwenty <strong>of</strong> <strong>the</strong> 26 pharmacists who started <strong>the</strong>GPPC study were interviewed. Of <strong>the</strong>se 20, twopharmacists had withdrawn during <strong>the</strong> study,two provided no clinical data and one providedclinical data only for <strong>the</strong> intervention arm. † Thesix pharmacists who were not interviewed wereunavailable for an interview at <strong>the</strong> time <strong>the</strong>researcher visited. The characteristics <strong>of</strong> <strong>the</strong> pharmacistsare noted in Table 1.OverviewThe <strong>the</strong>mes that emerged from <strong>the</strong> interviewswere whe<strong>the</strong>r <strong>the</strong> provision <strong>of</strong> clinical medicationreviews was mandated, had legitimacy, waseffective, and <strong>the</strong> adequacy <strong>of</strong> <strong>the</strong> pharmacistto provide <strong>the</strong> service. Views on governmentendorsement and <strong>the</strong> perceptions <strong>of</strong> o<strong>the</strong>rs suchas general practitioners and patients reflectedconcerns about a mandate. The concept <strong>of</strong> legitimacywas raised through comments relatingto time requirements and funding, suggestingthat medication reviews were not somethingthat had priority over traditional pharmacybusiness matters. Comments on lack <strong>of</strong> confidencein clinical and personal skills, plus aneed for peer support, indicated a perception <strong>of</strong>lack <strong>of</strong> adequacy.The <strong>the</strong>mes <strong>of</strong> mandate, legitimacy, effectivenessand adequacy are interrelated, with providersrequiring adequacy in order to achieve effectiveness,which <strong>the</strong>n gives legitimacy to <strong>the</strong> service,which should eventually become a role mandatedby <strong>the</strong> pr<strong>of</strong>ession and by o<strong>the</strong>rs external to <strong>the</strong>pr<strong>of</strong>ession. For <strong>the</strong> pharmacists <strong>the</strong> businessperspective was important to <strong>the</strong> <strong>the</strong>me <strong>of</strong> legitimacy,which became <strong>the</strong> major <strong>the</strong>me.The good aspects <strong>of</strong> medication reviewsIn response to <strong>the</strong> broad question about <strong>the</strong> goodaspects <strong>of</strong> <strong>the</strong> reviews, <strong>the</strong> pharmacists foundparticular satisfaction in building a better rapportwith customers, and making a difference or helpingpeople.Table 1. Characteristics <strong>of</strong> <strong>the</strong> pharmacists interviewed.Age (in 2002)GenderI think it builds a really good relationship withcustomers. [P1]I have really enjoyed <strong>the</strong>m because I have met differentpeople and got to know <strong>the</strong>m on a level that Iwouldn’t just in <strong>the</strong> shop. [P2]LegitimacyThere were some general comments about communitypharmacy as a business and <strong>the</strong> challenge<strong>of</strong> incorporating an extra service into <strong>the</strong> normaldispensing or supply and distribution priorities,particularly in times <strong>of</strong> staff shortages throughholidays, sickness, etc. The medication reviewservice was not seen as a priority or a part <strong>of</strong> <strong>the</strong>business, but more a ‘nice-to-do’. The majority<strong>of</strong> pharmacists commented that <strong>the</strong> medicationreviews were generally not done in routinework time, but in <strong>the</strong> pharmacist’s own time.The funding was paid to <strong>the</strong> pharmacy, not <strong>the</strong>pharmacist. This meant that it was not incorporatedinto <strong>the</strong> normal routine <strong>of</strong> <strong>the</strong> business andPharmacists(n=20)% (no.)50 years old 15% (3)Range: 27–57 yearsMale 30% (6)Female 70% (14)Ethnicity European 100% (20)LocationRolePostgraduate studyTown 15% (3)Peripheral city 60% (12)City 25% (5)Proprietor 35% (7)Employee 45% (9)Independent contractor 25% (4)Completed Masters or PG Diploma 30% (6)Completing Masters or PG 35% (7)No postgraduate study 35% (7)† In <strong>the</strong> GPPC study only 26 <strong>of</strong> <strong>the</strong> 44 pharmacists who agreed to participate started <strong>the</strong> study (59%); <strong>of</strong> <strong>the</strong>se, 21 completed <strong>the</strong> study(48%) and only 17 completed <strong>the</strong> study and provided useable data (39%).VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 237
ORIGINAL SCIENTIFIC PAPErSqualitative researcho<strong>the</strong>r tasks, such as dispensing and retail, wereconsidered a higher priority.The time spent on each <strong>of</strong> <strong>the</strong> patient medicationreviews was estimated by <strong>the</strong> pharmacists as fourto six hours generally, with a few estimating ashigh as eight hours, and one about one-and-a-halfto two hours.Because you start <strong>of</strong>f in <strong>the</strong> supply mode you gettrapped into that because that’s what, that’s kind <strong>of</strong><strong>the</strong> grind that you get into and it is really hard tobreak out and do something different, particularlywhen you are working for someone. [P3]I can’t do it. It needs a degree <strong>of</strong> dedicated time. Ipersonally find it too hard to do an interview, comeback to work, be a pharmacist dispensing <strong>the</strong>n gohome and write up <strong>the</strong> case studies, or try and findsome time out, because I don’t get space in <strong>the</strong> <strong>of</strong>fice…My head is in one place, and it has got to be inano<strong>the</strong>r because I have got a growing pharmacy. [P4]It is down time in <strong>the</strong> pharmacies. [P5]My impression from o<strong>the</strong>r community pharmaciststrying to do it is that <strong>the</strong> pressures <strong>of</strong> communitypharmacy impinge too much to allow <strong>the</strong>m to doCPC ®‡ [P6]Sometimes <strong>the</strong> shop detracts from <strong>the</strong> work <strong>of</strong>pharmacy. [P2]I mean that’s <strong>the</strong> o<strong>the</strong>r thing to reduce a person’smedicines, <strong>the</strong>y are actually taking away <strong>the</strong>ir business.I talked to a pharmacist in [NZ region] who ismy age who said, ‘why would you do CPC ® becauseyou are basically reducing my income’. [P7]MandateThe perception <strong>of</strong> whe<strong>the</strong>r <strong>the</strong>re is a mandate fora new service is an important aspect <strong>of</strong> acceptance<strong>of</strong> a service. The pharmacists perceived that<strong>the</strong>re was little mandate from general practitioners,although at times this seemed ambivalentand dependent on exposure. Despite governmentfunding for <strong>the</strong> service at <strong>the</strong> time <strong>of</strong> <strong>the</strong> study,<strong>the</strong> pharmacists did not think <strong>the</strong> government hadgiven <strong>the</strong>m a clear mandate to undertake this role.The biggest problem is I am actually, like, hitting abrick wall. It is whe<strong>the</strong>r you get doctors to buy into it. Whatever it takes to get <strong>the</strong>m to buy in, once<strong>the</strong>y are bought in I think <strong>the</strong>y are okay. [P4]There seems to be quite a demarcation line <strong>between</strong>medical things and pharmacy things and I think<strong>the</strong> Guild, <strong>the</strong> Doctors’ Guild, see us as just countingtablets and selling makeup. [P8]There needs to be clear guidance from <strong>the</strong> Ministryabout <strong>the</strong> implications and <strong>the</strong> realisation <strong>of</strong> whatCPC ® can give <strong>the</strong> country. [P4]AdequacyThe pharmacists need to feel <strong>the</strong>y have adequateclinical knowledge and skills to provide <strong>the</strong>clinical medication review service, or have <strong>the</strong>motivation to obtain <strong>the</strong> necessary skills. During<strong>the</strong> interviews <strong>the</strong>re were a number <strong>of</strong> commentsmade regarding clinical skills, personalconfidence and <strong>the</strong> desire for peer support, withan indication that a number <strong>of</strong> <strong>the</strong> pharmacistsfelt <strong>the</strong>y were working in isolation. The issue<strong>of</strong> funding is also relevant to <strong>the</strong> concept <strong>of</strong> adequacyto provide clinical medication reviews. Todo <strong>the</strong>se efficiently for <strong>the</strong> funding provided, <strong>the</strong>pharmacists require adequate skills and knowledgeto complete <strong>the</strong> review within <strong>the</strong> expected(funded) time frame.I probably need to up-skill to be able to be moreconfident and say, ‘okay this is <strong>the</strong> research that Iam talking about’, not just my gut feeling. [P9]I don’t have <strong>the</strong> confidence. [P10]I think it needs to be done properly, but havingsaid that, that is one <strong>of</strong> <strong>the</strong> reasons why <strong>the</strong>re aren’tenough people to actually do it now. [P6]That is one thing I do struggle with, I would prefer tobe able to discuss every care plan basically. It worriesme not having any backup, any double checking. [P11]‡ CPC ® is Comprehensive Pharmaceutical Care, a structured model used for <strong>the</strong> clinical medication reviews.238 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
Twelve months after <strong>the</strong> GPPC study ended, 44pharmacists who initially accepted <strong>the</strong> invitationto participate in <strong>the</strong> study were asked how manymedication reviews <strong>the</strong>y had done in <strong>the</strong> previousyear. Thirty-eight pharmacists (86%) responded.Of <strong>the</strong> 25 pharmacists who had not undertakenany medication reviews in <strong>the</strong> previous12 months, six no longer worked in communitypharmacy (two had moved to hospital, two to aPrimary Health Organisation (PHO) and two toa pr<strong>of</strong>essional organisation), three had sold <strong>the</strong>irpharmacy, and three were focussed on familycommitments. Of <strong>the</strong> 13 pharmacists who hadcompleted medication reviews in <strong>the</strong> previous 12months, six were rest home–based completingthree to 30 reviews over 12 months, and four haddone minimal numbers for ambulatory patients(two to eight). Three pharmacists who had under-ORIGINAL SCIENTIFIC PAPERSqualitative researchEffectivenessTo undertake a service <strong>the</strong>re must be a perceptionthat it is effective—for <strong>the</strong> patient, <strong>the</strong> generalpractitioner and <strong>the</strong> pharmacist. The pharmacist’sfocus on effectiveness also included an efficiencyand business perspective. This came through incomments relating to communication, feedback,implementation <strong>of</strong> recommendations, and potentiallocation <strong>of</strong> <strong>the</strong> service.Feedback on <strong>the</strong> acceptability <strong>of</strong> recommendationswas generally considered to be lacking, andso left <strong>the</strong> pharmacists not knowing whe<strong>the</strong>r<strong>the</strong>ir work had been useful. There were also someproblems with implementation, despite apparentacceptance <strong>of</strong> <strong>the</strong> recommendation in some cases.This seemed to be related to communication,with <strong>the</strong> preferred communication method <strong>between</strong><strong>the</strong> pharmacist and <strong>the</strong> general practitionerbeing face-to-face. It was recognised that this wasmore time consuming, but a written summaryplus a discussion appeared to be more productiveand assisted <strong>the</strong> pharmacist in understanding <strong>the</strong>general practitioner perspective.You do <strong>the</strong> first few and you don’t get any feedback.They are not good at giving feedback and how good<strong>the</strong>y found it. Actually that is probably <strong>the</strong> biggestdowner… if <strong>the</strong>y don’t refer o<strong>the</strong>r patients toyou for a while you think, oh, did I do somethingwrong? Did <strong>the</strong>y think it was a waste <strong>of</strong> time? [P12]Opinion on <strong>the</strong> best location <strong>of</strong> <strong>the</strong> service was divided.Home visits had recognised advantages butbecame a significant time factor in <strong>the</strong> total service,and problems with being in <strong>the</strong> pharmacy…I personally find it too hard to do an interview,come back to work, be a pharmacist dispensing <strong>the</strong>ngo home and write up <strong>the</strong> case studies or try andfind some time out because I don’t get space in <strong>the</strong><strong>of</strong>fice. [P4]If you are an independent person you can do it in<strong>the</strong> pharmacies, so long as you get yourself organisedand, like, have a morning a week to book inpatients and… I think it would be difficult to do itif you worked full-time in that pharmacy, and <strong>the</strong>nonce a week you were trying to do this because,when you go to write <strong>the</strong>m up, if you are trying todo it in work time and if you are trying to do it on<strong>the</strong> premises, it is very difficult to say to a member<strong>of</strong> <strong>the</strong> public why you are doing something in <strong>the</strong>dispensary one day and <strong>the</strong> next day you are ignoring<strong>the</strong>m. [P13]Feasibility <strong>of</strong> clinical medicationreviews in <strong>the</strong> futureAlthough <strong>the</strong> <strong>the</strong>mes <strong>of</strong> mandate, legitimacy,effectiveness and adequacy emerged, a final questionon whe<strong>the</strong>r <strong>the</strong> pharmacists believe <strong>the</strong>re is afuture for clinical medication reviews provided asummary <strong>of</strong> <strong>the</strong>ir overall view. All <strong>the</strong> pharmacistsconsidered that <strong>the</strong>se reviews should be part<strong>of</strong> <strong>the</strong> future for pharmacy, though two pharmacistsfelt that it was not something that <strong>the</strong>ywould pursue because <strong>of</strong> <strong>the</strong>ir perceived skilllevel and <strong>the</strong> stage <strong>the</strong>y were at in <strong>the</strong>ir career.No pharmacist could see <strong>the</strong>mselves providing<strong>the</strong> service full-time, but usually for one to twodays a week. The reasons for this varied: fittingit around children; having interests in o<strong>the</strong>rparts <strong>of</strong> <strong>the</strong> business; finding difficulty fittingit into <strong>the</strong> business staff-wise for more than oneday a week and finding <strong>the</strong> intensity difficult.This may also indicate a perceived lower priority<strong>of</strong> <strong>the</strong> service, and that it is merely an ‘add-on’service. A number <strong>of</strong> pharmacists commentedthat <strong>the</strong> standard <strong>of</strong> <strong>the</strong> reviews needed to bemaintained and <strong>the</strong> service needed to be doneproperly if <strong>the</strong>re was to be a future for clinicalmedication reviews.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 239
ORIGINAL SCIENTIFIC PAPErSqualitative researchtaken a substantial number <strong>of</strong> medication reviewsfor ambulatory patients had done so after movinginto a PHO environment and no longer workedin community pharmacy. (Figure 1) This demonstrates<strong>the</strong> lack <strong>of</strong> incorporation <strong>of</strong> <strong>the</strong> clinicalmedication reviews service into routine communitypharmacy services after <strong>the</strong> study, despitefunding being available at <strong>the</strong> time.DiscussionDespite <strong>the</strong> funding provided by <strong>the</strong> governmentfor clinical medication reviews, <strong>the</strong> communitypharmacists did not perceive that <strong>the</strong>y have amandate to provide <strong>the</strong> service, that it was alegitimate service or that <strong>the</strong>y had adequate skillsand experience to provide <strong>the</strong> service, despite anapparent desire to undertake <strong>the</strong>se services. If <strong>the</strong>Figure 1. Ongoing involvement in clinical medication reviews <strong>of</strong> <strong>the</strong> pharmacists who agreed to participate in <strong>the</strong> GPPC studySurvey sent to all pharmacists whoinitially agreed to participate in <strong>the</strong>GPPC studyN=44No responseN=6Responded to surveyN=38Had done no medication reviews in<strong>the</strong> previous 12 monthsN=25Had done at least one medical reviewin <strong>the</strong> last 12 monthsN=13No longerworking in <strong>the</strong>communitypharmacyN=6Sold <strong>the</strong>pharmacyN=3Focussingon familycommitmentsN=3No reason givenN=13Working in PHOenvironment(substantialnumbers)N=3Reviews forambulatorypatients (minimalnumbers)N=4Reviews done inrest home (range3 to 30 reviews)N=6240 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ORIGINAL SCIENTIFIC PAPERSqualitative researchreviews were perceived as a legitimate service,<strong>the</strong>n <strong>the</strong>y should receive reasonable priority interms <strong>of</strong> time.While o<strong>the</strong>r researchers identified a number <strong>of</strong>physical or system barriers, this study supports<strong>the</strong> findings that pharmacist attitudes contributeadditional barriers, 20 particularly <strong>the</strong> concept <strong>of</strong>whe<strong>the</strong>r this is a legitimate service from a communitypharmacy.The work <strong>of</strong> Edmunds and Calnan 26 suggest somereasons for this, including that, despite a viewthat <strong>the</strong>ir skills were underutilised and <strong>the</strong>irdesire for an extended role in patient health care,community pharmacists find it difficult to manage<strong>the</strong> conflict <strong>between</strong> being a trader and beinga health pr<strong>of</strong>essional. They believe that pharmacistssee <strong>the</strong>mselves as dispensers <strong>of</strong> <strong>the</strong> generalpractitioner’s prescriptions and wish to avoidconflict with general practitioners over clinicaldecisions. They feel unworthy to challenge <strong>the</strong>status quo, despite a perception that <strong>the</strong>y areknowledgeable about drug <strong>the</strong>rapy.In contrast, clinical pharmacists working withingeneral practice or primary care clinics appear tobe more integrated into <strong>the</strong> health care team andexperience fewer barriers to providing clinicalmedication reviews and o<strong>the</strong>r medicine managementservices independent <strong>of</strong> dispensing andsupply. 6–10 A fur<strong>the</strong>r area <strong>of</strong> research shouldinvolve <strong>the</strong> perceptions and acceptance <strong>of</strong> clinicalpharmacists working within PHOs and generalpractices, independent <strong>of</strong> a community pharmacy,as well as <strong>the</strong> influence this has on patientmedication–related health outcomes.The limitations <strong>of</strong> this study are that <strong>the</strong> pharmacistsgenerally already had a relationship with<strong>the</strong> general practitioners in <strong>the</strong> study, <strong>the</strong>reforereducing one barrier identified in previousresearch. 17,18,20,22,23 The nature <strong>of</strong> <strong>the</strong>se medicationreviews were clinical ra<strong>the</strong>r than just focussingon adherence support, which is <strong>the</strong> current fundedservice in New Zealand and likely to generateless hesitancy about adequacy. These findings alsorelate to pharmacists who were motivated, havingundertaken extra training to provide <strong>the</strong> clinicalmedication reviews. It would be <strong>of</strong> academicinterest to assess <strong>the</strong> views <strong>of</strong> less motivatedpharmacists. Presumably <strong>the</strong>y would be evenless accepting <strong>of</strong> <strong>the</strong>ir role in clinical medicationreviews. Conversely exploring <strong>the</strong> perceptions <strong>of</strong>clinical pharmacists working in PHOs may findthat <strong>the</strong>se pharmacists perceive a legitimate rolein clinical medication reviews and believe <strong>the</strong>yhave adequate knowledge and skills.ConclusionWhile <strong>the</strong> skills <strong>of</strong> community pharmacistsappear to be underutilised, <strong>the</strong>re are barriers toincreasing <strong>the</strong> role <strong>of</strong> community pharmacists inmedicines management services. One <strong>of</strong> <strong>the</strong> mainproblems that needs to be addressed is <strong>the</strong> perception<strong>of</strong> community pharmacists and <strong>the</strong>ir attitudetowards <strong>the</strong> new services, particularly <strong>the</strong> needto see <strong>the</strong>se services as a priority and a legitimateservice. It may be preferable to provide clinicalmedication reviews from within a PHO or generalpractice by a clinical pharmacist, independent<strong>of</strong> a community pharmacy.References1. Chrischilles E, Carter BL, Lund B, Rubenstein LZ, Chen-hardeeS, Voelker M, et al. Evaluation <strong>of</strong> <strong>the</strong> Iowa Medicaid PharmaceuticalCase Management Program. J Am Pharm Assoc.2004;44:337–49.2. Becker C, Bjornson DC, Kuhle J. Pharmacist care plansand documentation <strong>of</strong> follow-up before <strong>the</strong> Iowa PharmaceuticalCase Management Program. J Am Pharm Assoc.2004;44:350–7.3. Weinberger M, Murray MD, Marrero DG, Brewer N, LykensM, Harris LE, et al. Effectiveness <strong>of</strong> pharmacist care for patientswith reactive airways disease: a randomized controlledtrial. JAMA. 2002;288(13):1594–602.4. The Community Pharmacy Medicines Management ProjectEvaluation Team. The MEDMAN study: a randomised controlledtrial <strong>of</strong> community pharmacy-led medicines managementfor patients with coronary heart disease. Family Practice.2007;24:189–200.5. Stergachis A, Gardner JS, Anderson MT, Sullivan SD. Improvingpediatric asthma outcomes in <strong>the</strong> community setting: doespharmaceutical care make a difference? J Am Pharm Assoc.2002;42(5):743–52.6. Zermansky AG, Petty DR, Raynor DK, Freemantle N, Vail A,Lowe CJ. Randomised controlled trial <strong>of</strong> clinical medicationreview by a pharmacist <strong>of</strong> elderly patients receiving repeat prescriptionsin general practice. BMJ. 2001;323(7325):1340–3.7. Ellis SL, Carter BL, Malone DC, Billups SJ, Okano GJ, ValuckRJ, et al. Clinical and economic impact <strong>of</strong> ambulatory care clinicalpharmacists in management <strong>of</strong> dyslipidemia in older adults:<strong>the</strong> IMPROVE study. Impact <strong>of</strong> Managed Pharmaceutical Careon Resource Utilization and Outcomes in Veterans AffairsMedical Centers. Pharmaco<strong>the</strong>rapy. 2000;20(12):1508–16.8. Malone DC, Carter BL, Billups SJ, Valuck RJ, Barnette DJ,Sintek CD, et al. An economic analysis <strong>of</strong> a randomized, controlled,multicenter study <strong>of</strong> clinical pharmacist interventionsfor high-risk veterans: <strong>the</strong> IMPROVE study. Impact <strong>of</strong> ManagedPharmaceutical Care Resource Utilization and Outcomesin Veterans Affairs Medical Centers. Pharmaco<strong>the</strong>rapy.2000;20(10):1149–58.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 241
ORIGINAL SCIENTIFIC PAPErSqualitative researchACKNOWLEDGEMENTSWe wish to thank <strong>the</strong>dedicated pharmacistswho participated in <strong>the</strong>GPPC study, and showeda true pioneering spirit anda keen desire to improvepatient medicine-relatedhealth outcomes.FUNDINGFunding for <strong>the</strong> GPPCstudy was originallyprovided through <strong>the</strong>Transitional HealthAuthority (reimbursement<strong>of</strong> general practitioners)and <strong>the</strong> PharmaceuticalSociety Education andResearch Fund (printingand postage costs). Thesefunding bodies had noinfluence on <strong>the</strong> studydesign or any publication.COMPETING INTERESTSNone declared.9. Rothman RL, Malone R, Bryant B, Shintani AK, Crigler B,Dewalt DA, et al. A randomized trial <strong>of</strong> a primary care-baseddisease management program to improve cardiovascular riskfactors and glycated hemoglobin levels in patients with diabetes.Am J Med. 2005;118(3):276–84.10. Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, SundaramV, Rushak<strong>of</strong>f RJ, et al. Effects <strong>of</strong> quality improvementstrategies for type 2 diabetes on glycemic control: a metaregressionanalysis. JAMA. 2006;296:427–40.11. Amsler MR, Murray MD, Tierney WM, Brewer N, Harris LE,Marrero DG, et al. Pharmaceutical care in chain pharmacies:beliefs and attitudes <strong>of</strong> pharmacists and patients. J Am PharmAssoc. 2001;41(6):850–5.12. Dunlop JA, Shaw J. Community pharmacists’ perspectives onpharmaceutical care implementation in New Zealand. PharmWorld Sci. 2002;24:224–30.13. Rutter PR, Hunt AJ, Jones IF. Exploring <strong>the</strong> gap: Communitypharmacists’ perceptions <strong>of</strong> <strong>the</strong>ir current role compared with<strong>the</strong>ir aspirations. Int J Pharm Pract. 2000;8(3):204–208.14. Krska J, Veitch GBA. Perceived factors influencing <strong>the</strong>development <strong>of</strong> primary care-based pharmaceutical care inScotland. Int J Pharm Pract. 2001;9(4):243–252.15. van Mil F, de Boer W, Tromp T. European barriers toimplementation <strong>of</strong> pharmaceutical care. Int J Pharm Pract.2001;9:163–8.16. Lee E, Braund R, Tord<strong>of</strong>f J. Examining <strong>the</strong> first year <strong>of</strong> MedicinesUse Review services provided by pharmacists in NewZealand: 2008. NZMJ. 2009;122(1293):26–35.17. Bradley F, Wagner A, Elvey R, Noyce P, Ashcr<strong>of</strong>t DM. Determinants<strong>of</strong> <strong>the</strong> uptake <strong>of</strong> medicines use reviews (MURs) bycommunity pharmacies in England: A multi-method study.Health Policy. 2008;88:258–68.18. Lounsbery J, Green CF, Bennett MS, Pedersen CA. Evaluation<strong>of</strong> pharmacists’ barriers to <strong>the</strong> implementation <strong>of</strong> medication<strong>the</strong>rapy management services. J Am Pharm Assn.2009;49(1):51–8.19. Brown CM, Barner JC, Shepherd MD. Issues and barriersrelated to <strong>the</strong> provision <strong>of</strong> pharmaceutical care in communityhealth centers and migrant health centers. J Am Pharm Assoc.2003;43(1):75–7.20. Muijrers PE, Knottnerus JA, Sijbrandij J, Janknegt R, Grol RP.Pharmacists in primary care. Determinants <strong>of</strong> <strong>the</strong> care-providingfunction <strong>of</strong> Dutch community pharmacists in primary care.Pharm World Sci. 2004;26(5):256–62.21. Rossing C, Hansen E, Krass I, Traulsen J. Pharmaceutical Carein Denmark: perceived importance <strong>of</strong> medicine-related problemsand participation in postgraduate training. Pharm WorldSci. 2003(25):73–78.22. Rossing CH, E. Traulsen, J. Krass, I. Actual and perceivedprovision <strong>of</strong> pharmaceutical care in Danish communitypharmacies: <strong>the</strong> pharmacists’ opinion. Pharm World Sci.2005;27:175–81.23. Wilcock M, Harding G. General practitioner’s perceptions<strong>of</strong> medicines use reviews by pharmacists. Pharm J2007;279:501–03.24. Willink DP, Isetts BJ. Becoming ‘indispensable’: developinginnovative community pharmacy practices. J Am Pharm Assoc.2005;45(3):376–86.25. Latif DA. The relationship <strong>between</strong> pharmacists’ tenure in<strong>the</strong> community setting and moral reasoning. J Bus Ethics.2001;31(2):131–41.26. Edmunds J, Calnan MW. The repr<strong>of</strong>essionalisation <strong>of</strong> communitypharmacy? An exploration <strong>of</strong> attitudes to extendedroles for community pharmacists amongst pharmacists andGeneral Practitioners in <strong>the</strong> United Kingdom. Soc Sci Med.2001;53(7):943–55.27. Bryant L, Coster G, McCormick R. General practitionerperceptions <strong>of</strong> clinical medication reviews undertaken by communitypharmacists. J Primary Health Care. 2010;2(3):225–33.242 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
improving performanceReducing health disparities for low <strong>decile</strong>children and families: a nurse-led responseCatrina Riley RN, BN, MN (Child & Family); 1 Ruth Crawford RN, BA, PGCert. (Tertiary Teaching), M.Phil (Nursing) 2ABSTRACTBackground and context: Reducing health disparities for children living in deprived areas hasbeen difficult to achieve. This paper describes <strong>the</strong> implementation <strong>of</strong> a nurse-led, child-specific clinicwithin a general practice setting to improve health outcomes for high needs Maori/Pacific Island andNZDep96 quintile groups 4 and 5 children and <strong>the</strong>ir whanau/families.1The Doctors, Napier,Napier, New Zealand2Eastern Institute <strong>of</strong>Technology, Hawkes Bay,New ZealandAssessment <strong>of</strong> problem: The medical centre that implemented <strong>the</strong> clinic had a high number <strong>of</strong>enrolled children with chronic and recurrent morbidities. Children frequently did not attend clinic appointments,and <strong>the</strong>re was high use <strong>of</strong> after-hours services.Results: An outcome audit after 18 months demonstrated a significant (>30%) reduction in eczemaseverity, daily irritability, and daily occurrence <strong>of</strong> pain. Post-intervention fewer children were hospitalisedand <strong>the</strong>re was a 50% reduction in antibiotic use.Strategies for improvement: The aim <strong>of</strong> <strong>the</strong> nurse-led clinic was to improve health gains, facilitatemorbidity control <strong>of</strong> chronic conditions, and to <strong>of</strong>fer prevention strategies to promote wellness for<strong>the</strong> target population. The reduction <strong>of</strong> morbidity severity by 10% was measured with specific morbidityscoring systems for eczema, constipation and nocturnal enuresis. O<strong>the</strong>r outcome indicators measuredvomiting/reflux, wheezing/coughing, constipation/soiling, irritability, sleep disturbances, hospital admissions,and antibiotic use.Lessons: Nurse-led clinics facilitated by nurses with advanced skills can reduce health disparities for<strong>the</strong> target population. The amount <strong>of</strong> time <strong>the</strong> nurse is able to spend with <strong>the</strong> child and whanau/family,and <strong>the</strong> provision <strong>of</strong> opportunistic assessments as required, has effected positive change in thosechildren most in need.KEYWORDS: Child health; low <strong>decile</strong> families; Maori/Pacific families: chronic conditions; nurse-led clinicBackgroundReducing health disparities for Maori and Pacificchildren and for children living in areas <strong>of</strong> highdeprivation is a goal underpinning health provisionin New Zealand. These children have rates <strong>of</strong>common chronic health conditions two to six timeshigher than those not living in socioeconomicdeprivation. 1 This paper outlines an outcomeevaluation <strong>of</strong> a child health nurse-led clinic whichaimed to improve health gains, facilitate morbiditycontrol <strong>of</strong> chronic conditions, and <strong>of</strong>fer preventionstrategies to promote wellness in this population.Nurse-led clinics have become more commonplacein <strong>the</strong> provision <strong>of</strong> primary health care since<strong>the</strong> implementation <strong>of</strong> <strong>the</strong> Primary Health CareStrategy in 2001. 2 Government supported <strong>the</strong>development <strong>of</strong> innovative models <strong>of</strong> primaryhealth care nursing practice which would helpdeliver <strong>the</strong> objectives <strong>of</strong> <strong>the</strong> Primary HealthCare Strategy. 3 A more recent driver <strong>of</strong> nurse-ledclinics has been funding from Primary HealthOrganisations (PHOs) to meet <strong>the</strong> specific healthneeds <strong>of</strong> <strong>the</strong> population. 4 Services which arenurse-led are not merely replacing <strong>the</strong> doctorCorrespondence to:Ruth CrawfordSchool <strong>of</strong> Nursing, EITHawkes Bay, PB 1201Napier, New Zealandrcrawford@eit.ac.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 243
improving performancewith <strong>the</strong> nurse: nurses take <strong>the</strong> lead to add anenhanced quality <strong>of</strong> care. 5 Nurse-led clinics havebeen implemented successfully internationally 6–8and nationally. 9,10 Child health conditions suchas atopic eczema, asthma, functional constipation,urinary tract infections and iron deficiencyanaemia have been successfully managed within<strong>the</strong> nurse-led clinic model. 5,7–9,11–15 Benefits <strong>of</strong>nurse-led clinics include increased patientsatisfaction, longer consultations, and improvedpatient education. 5Hawkes Bay, a region on <strong>the</strong> east coast <strong>of</strong> NewZealand, has higher than <strong>the</strong> national averagenumbers <strong>of</strong> children and young people living in<strong>the</strong> most deprived (NZDep01 <strong>decile</strong> 10) areasaccording to <strong>the</strong> 2006 census. Thirty-five percent<strong>of</strong> children in Hawkes Bay live in deprivationareas 9 and 10 compared to 24% nationally. 16One <strong>of</strong> <strong>the</strong> authors (CR) works as a practice nurseat a general medical facility in Hawkes Bay. Thisfacility serves a culturally diverse urban area,with an enrolled child population (0–18 years)<strong>of</strong> 4968. The demographics <strong>of</strong> <strong>the</strong> enrolled childpopulation are shown in Table 1.PurposeThe purpose <strong>of</strong> this paper is to present an outcomeevaluation <strong>of</strong> a nurse-led clinic. An audit-basedapproach was used to evaluate <strong>the</strong> impact <strong>the</strong>clinic has had on children with chronic childhoodconditions with particular emphasis on highneeds Maori/Pacific Island children and NZDep96quintile groups 4 and 5 whanau/families.An application for ethical approval for thisoutcome evaluation was made to <strong>the</strong> Central RegionalHealth and Disability Ethics Committee.The Committee advised that this study does notrequire ethical approval, as it falls under exemptions11.8 and 11.9 <strong>of</strong> <strong>the</strong> Ethical Guidelines forObservational Studies: Observational Research,Audits and Related Activities (NEAC, December2006) and <strong>the</strong>refore requires no fur<strong>the</strong>r review.Assessment <strong>of</strong> problemSignificant numbers <strong>of</strong> <strong>the</strong> enrolled child populationin <strong>the</strong> practice experienced chronic and recurrentmorbidities. Nineteen percent <strong>of</strong> patientshad outstanding debts to <strong>the</strong> practice. Sixty-eightchildren (0–18 years) did not attend <strong>the</strong>ir bookedappointments over a two-month period. Over aone-year period, <strong>the</strong>re were 70 011 child presentationswithout a scheduled appointment (walkins),or after-hours, and 62% <strong>of</strong> <strong>the</strong>se childrenresided in NZDep96 quintile groups 4 and 5. 17In one year, 1644 children less than 18 yearswere identified as having a chronic condition.Repeat exacerbations were problematic¸ with<strong>the</strong> number <strong>of</strong> presentations ranging from twoto eight per child. Sixty-five percent <strong>of</strong> <strong>the</strong>sechildren lived in NZDep96 quintile groups 4and 5. 17Strategies for qualityimprovement/changeThe aim <strong>of</strong> <strong>the</strong> intervention was to improvehealth gains, facilitate morbidity control <strong>of</strong>chronic conditions, and <strong>of</strong>fer prevention strategiesto promote wellness to <strong>the</strong> target group <strong>of</strong>children. Chronic conditions included atopic eczema,asthma, food allergies/intolerances suspectedor actual, functional constipation, gastroesopha-Table 1. Demographics <strong>of</strong> enrolled children (n=4968) 0–18years. 17CharacteristicEthnicity n (%)NZ European 2807 (57%)Maori 1645 (33%)Pacific Island 167 (3%)Asian 68 (1%)Indian 23 (0.5%)African 18 (0.4%)Middle Eastern 10 (0.2%)O<strong>the</strong>r 230 (5%)NZDep96Quintile 1 278 (5.6%)Quintile 2 400 (8%)Quintile 3 854 (17%)Quintile 4 854 (17%)Quintile 5 2582 (52%)244 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
improving performancegeal reflux disease, nocturnal enuresis, and obesity.The clinic excluded children with complexcardiac, respiratory, renal, endocrinological, andneurological chronic morbidities. The service wasfunded by <strong>the</strong> Hawkes Bay Primary Health Organisation(HBPHO). All children under 18 yearswho were identified as having a chronic conditionwere sent a letter explaining <strong>the</strong> purpose <strong>of</strong> <strong>the</strong>clinic, and were <strong>of</strong>fered <strong>the</strong> opportunity to makean appointment.Each consultation was 45 minutes, which gavetime to discuss, educate, and <strong>of</strong>fer preventionstrategies. Within each consultation, wider socialissues affecting <strong>the</strong> child and <strong>the</strong>ir whanau/family were assessed, such as financial assistance,smoking cessation, transport issues, familyviolence screening, and housing concerns.Opportunistic assessments were <strong>of</strong>ten performedout <strong>of</strong> designated child health clinic hours, andafter hours (4pm to 7pm). Language barriers weremanaged with an interpreter service. The clinicrecognised and embraced <strong>the</strong> ‘Te Whare TapaWha’ concept as described by Durie. 18 Te WhareTapa Wha refers to <strong>the</strong> four walls <strong>of</strong> <strong>the</strong> whare(house), with each wall representing a dimension<strong>of</strong> health; taha wairua (spiritual), taha tinana(physical), taha hinengaro (mental/intellect),and taha whanau (extended family). 18 Followingreview <strong>of</strong> international best practice literatureregarding <strong>the</strong> impact <strong>of</strong> child-specific, nurseledclinics relating to eczema, constipation, andurinary tract infection, outcome indicators wereadopted. 5,11–14,20–22The nurse-led clinic had specific objectives withregard to assessment <strong>of</strong> particular childhoodchronic conditions. The reduction <strong>of</strong> morbidityseverity by 10% was measured with morbidityscoring systems, such as <strong>the</strong> Six Area, Six SignAtopic Dermatitis (SASSAD) severity <strong>score</strong> forchildren with eczema; <strong>the</strong> Bristol Stool Scalefor children with constipation; and number <strong>of</strong>wet nights per week for children with nocturnalenuresis. O<strong>the</strong>r child health outcome indicatorsmeasured vomiting/reflux, wheezing/coughing,constipation/soiling, irritability, sleep disturbances,hospital admissions, and antibiotic use. Anoutcome audit utilising <strong>the</strong> Medtech32 PatientManagement System Query Builder functionWHAT GAP THIS FILLSWhat we already know: Children from Maori and Pacific families, andlow <strong>decile</strong> groups have two to six times <strong>the</strong> rates <strong>of</strong> common chronic healthconditions than o<strong>the</strong>r children. Improving <strong>the</strong> health status <strong>of</strong> <strong>the</strong>se childrenhas been difficult to achieve. High incidences <strong>of</strong> families not attending clinicappointments, and reduced access to health care because <strong>of</strong> increasing waitingtimes for outpatient clinics have led to widening health disparities.What this study adds: A nurse-led, child-specific clinic for low-<strong>decile</strong>children with mild–moderate chronic conditions has been successfully implementedin New Zealand. Significant reductions in eczema severity, irritabilityand pain, alongside a decrease in hospital admissions and antibiotic use havebeen achieved by advanced nurses working with children and <strong>the</strong>ir whanau/families.extracted data for analysis. Baseline data was collectedat <strong>the</strong> time <strong>of</strong> <strong>the</strong> first visit from whanau/families, using direct questioning and observation.Post-intervention data was collected onemonth following <strong>the</strong> first clinic visit.The purpose <strong>of</strong> <strong>the</strong> intervention was to reduce<strong>the</strong> frequency <strong>of</strong> <strong>the</strong> indicator(s) from daily toevery second or third day, weekly, or none over aperiod <strong>of</strong> one month post-intervention.The children and <strong>the</strong>ir whanau/families were<strong>the</strong> major stakeholders in <strong>the</strong> intervention. Theywere <strong>of</strong>fered <strong>the</strong> choice <strong>of</strong> completing (or not)a consultation satisfaction survey (Appendix 1,available in <strong>the</strong> web version <strong>of</strong> this paper) postedto <strong>the</strong>m with a prepaid return addressed envelopewithin three months <strong>of</strong> <strong>the</strong>ir last visit to<strong>the</strong> child health clinic. Ano<strong>the</strong>r major group <strong>of</strong>stakeholders were <strong>the</strong> general practitioners (GPs)who worked within <strong>the</strong> practice. All GPs were<strong>of</strong>fered <strong>the</strong> opportunity to complete a survey <strong>of</strong><strong>the</strong> clinic (Appendix 2, available in <strong>the</strong> web version<strong>of</strong> this paper).Results <strong>of</strong> assessment/measurementTwo hundred and sixty-five consultations werecarried out over an 18-month period. Seventyfivepercent were from NZDep96 quintiles 4 and5. 19 Table 2 shows demographic data <strong>of</strong> childrenreviewed at <strong>the</strong> clinic. Results are reported undereach <strong>of</strong> <strong>the</strong> specific chronic conditions.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 245
improving performanceEczemaFifty-four children with eczema were included in<strong>the</strong> outcome audit. Children were excluded from<strong>the</strong> audit if follow-up did not occur one monthafter <strong>the</strong> first visit. The average SASSAD baseline<strong>score</strong> was 29, and <strong>the</strong> average post-interventionSASSAD <strong>score</strong> was 13. This demonstrates anaverage reduction <strong>of</strong> 16 in <strong>the</strong> SASSAD <strong>score</strong>s,and equates to a 32% reduction in eczema severity(Figure 1). 19A possible correlation may be noted <strong>between</strong> <strong>the</strong>increase in daily emollient utilisation, <strong>the</strong> reductionin daily topical corticosteroid use (TCS),<strong>the</strong> reduction in daily itching, and <strong>the</strong> reductionin eczema severity (Figure 1). Daily emollientuse increased by 51%, daily TCS reduced by15%, daily itching reduced by 32%, and eczemaseverity decreased by 32%. Similar findings werenoted in <strong>the</strong> United Kingdom in research whichassessed <strong>the</strong> efficacy <strong>of</strong> education and demonstration<strong>of</strong> topical <strong>the</strong>rapies for children with eczemain a nurse-led clinic environment. 12 Their resultsalso demonstrated a significant increase in dailyemollient utilisation and a significant reductionin eczema severity with no increase in <strong>the</strong> use <strong>of</strong>topical corticosteroids.ConstipationTen children who experienced constipationwere included in <strong>the</strong> audit; seven were excludedbecause <strong>the</strong>y did not attend <strong>the</strong>ir follow-up visitFigure 1.Comparison <strong>of</strong> baseline and post-intervention eczema outcome indicatorsTable 2. Demographics <strong>of</strong> children (n=265) 0–18 yearsreviewed in <strong>the</strong> child health clinicCharacteristic n (%)EthnicityNZ European 123 (46%)Maori 99 (37%)Pacific Island 24 (9%)Indian 8 (3%)Asian 3 (1%)O<strong>the</strong>r 8 (3%)Age in years
improving performancemonth, and post intervention 28% had received acourse <strong>of</strong> antibiotics within <strong>the</strong> month interval.Figure 2. Constipation outcomesO<strong>the</strong>r findings showed a 36% reduction in dailymood irritability; a 28% increase in childrensleeping throughout <strong>the</strong> night with 13% reductionin nightly sleep disturbances; a 22% reductionin <strong>the</strong> daily occurrence <strong>of</strong> pain; a 13% reduction<strong>of</strong> vomiting/reflux on a daily basis; a 12%reduction in daily occurrence <strong>of</strong> constipation/soiling;and an 11% reduction in children experiencingdaily, or every second/third day, wheezing/coughing symptoms. 19GP survey resultsTwelve GPs who worked within <strong>the</strong> practicegave feedback via a confidential survey (Appendix2, available in <strong>the</strong> web version <strong>of</strong> this paper).All agreed <strong>the</strong> nurse-led clinic was a usefulresource which had positively impacted upon<strong>the</strong>ir workload.Figure 3. Nocturnal enuresis outcomesFamily satisfaction resultsTwenty whanau/families <strong>of</strong> <strong>the</strong> 68 children whohad attended <strong>the</strong> nurse-led clinic gave feedbackvia a confidential consultation satisfaction survey(Appendix 2 in <strong>the</strong> web version). Findings showedall whanau/families strongly agreed or agreedthat <strong>the</strong>y were satisfied with <strong>the</strong> care received in<strong>the</strong> clinic; most whanau/families felt <strong>the</strong>y wereinvolved with goal setting; 85% felt <strong>the</strong> advice andeducation contributed to <strong>the</strong>ir child’s improvedTable 3. Comparison <strong>of</strong> baseline and post-intervention child health indicators (n=68)Indicator None Weekly Every 2 nd to 3 rd day DailyB PI B PI B PI B PISleep disturbance 22 (32%) 41 (60%) 12 (18%) 11 (16%) 13 (19%) 4 (6%) 21 (31%) 12 (18%)Pain 22 (32%) 46 (67%) 18 (26%) 15 (22%) 12 (18%) 6 (9%) 16 (24%) 1 (2%)Vomiting/reflux 53 (78%) 65 (96%) 5 (7%) 3 (4%) 1 (2%) 0 (0%) 9 (13%) 0 (0%)Wheeze/cough 47 (69%) 67 (98%) 14 (20%) 1 (2%) 6 (9%) 0 (0%) 1 (2%) 0 (0%)Irritability 22 (32%) 49 (72%) 5 (7%) 11 (16%) 12 (18%) 3 (4%) 29 (43%) 5 (7%)Constipation/soiling 53 (78%) 59 (87%) 3 (4%) 5 (7%) 3 (4%) 3 (4%) 10 (14%) 1 (2%)Antibiotic use 40 (59%) 49 (72%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 28 (41%) 19 (28%)Hospital admissions 64 (94%) 67 (98%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 4 (6%) 1 (2%)B = BaselinePI = Post interventionVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 247
improving performanceACKNOWLEDGEMENTSThe authors would liketo acknowledge <strong>the</strong>Hawkes Bay PrimaryHealth Organisation and<strong>the</strong> medical centre for<strong>the</strong>ir ongoing support<strong>of</strong> <strong>the</strong> nurse-led clinic.COMPETING INTERESTSNone declared.health, and felt more confident and motivated; andfinally, all whanau/families reported increasedunderstanding <strong>of</strong> <strong>the</strong>ir child’s diagnosis, medication,and treatment plan, and were satisfied with<strong>the</strong> amount <strong>of</strong> time <strong>the</strong> nurse spent with <strong>the</strong>m.Lessons and messagesPrimary health care is population- and patientfocussed.The introduction <strong>of</strong> <strong>the</strong> child healthnurse-led clinic provided a new resource for <strong>the</strong>medical practice. There were no primary healthchild-specific nursing services available to supportchildren with common chronic conditions in<strong>the</strong> region. The clinic was developed to meet <strong>the</strong>needs <strong>of</strong> a specific population within <strong>the</strong> medicalpractice. Over an 18-month period, 265 nurseledconsultations were undertaken. Seventy-fivepercent <strong>of</strong> children in <strong>the</strong> group were fromNZDep96 quintiles 4 and 5, and 46% were <strong>of</strong>Maori or Pacific Island descent.The clinic’s success could be attributed to earlyreview <strong>of</strong> children with mild to moderate forms<strong>of</strong> chronic conditions, and hence preventing <strong>the</strong>seconditions from becoming more severe. A fur<strong>the</strong>rachievement <strong>of</strong> <strong>the</strong> clinic was facilitating a shiftin service provision to primary health care in linewith government targets outlined in <strong>the</strong> PrimaryHealth Care Strategy.Intervening when morbidities are mild to moderate,and <strong>the</strong>n working closely with whanau/families with education and support, has enabledmore efficient condition control.Benefits for <strong>the</strong> practice have enabled nurses toundertake independent nurse-led clinics, thususing <strong>the</strong>ir knowledge and skills in ways notpreviously achieved. 23 The introduction <strong>of</strong> <strong>the</strong>child health nurse-led clinic did not require majorpractice change as all processes were acceptable andpracticable for nurses, GPs, and whanau/families.PHO, GP and practice nurse support has beenessential to <strong>the</strong> success <strong>of</strong> <strong>the</strong> child healthnurse-led clinic. It is anticipated that, with thisongoing support, <strong>the</strong> service will continue in <strong>the</strong>foreseeable future, addressing <strong>the</strong> health needs <strong>of</strong>children and young people in Hawkes Bay, and thusreducing <strong>the</strong> burden <strong>of</strong> ongoing chronic illness.References1. The Paediatric Society Monitoring <strong>the</strong> Health <strong>of</strong> New ZealandChildren and Young People: Indicator Handbook. 2007. RetrievedJanuary 10, 2008 from http://www.paediatrics.org.nz2. Ministry <strong>of</strong> Health. The Primary Health Care Strategy. Wellington;2001.3. Nelson K, Wright T, Connor M, Buckley S, Cumming J. Lessonsfrom eleven primary health care nursing innovations inNew Zealand. Int Nurs Rev. 2009;56(3)291–298.4. Hawkes Bay Primary Health Organisation. Nurse-led healthylifestyle clinics. Practice Nurse. 2008;7(3):20–21.5. Moore E, Williams A, Manias E, Varigos G. Nurse-led clinicsreduce severity <strong>of</strong> childhood atopic eczema: a review <strong>of</strong> <strong>the</strong>literature. B J Dermatol.2006;155:1242–1248.6. Hanson-Turton T, Miller ME. Nurses and nurse-managedhealth centers fill healthcare gaps. The Pennsylvania Nurse.2006; June, 18.7. Rance KS, Trent CA. Pr<strong>of</strong>ile <strong>of</strong> a primary care practice asthmaprogram: improved patient outcomes in a high-risk population.J Pediatr HealthCare. 2005;19(1):25–32.8. Wooler E. The role <strong>of</strong> <strong>the</strong> nurse in paediatric asthma management.Paediatric Respiratory Review. 2001;2:76–81.9. Bolitho S, Huntington A. Experiences <strong>of</strong> Maori families accessinghealth care for <strong>the</strong>ir unwell children: a pilot study. NursPrax NZ. 2006;22(1)23–32.10. Clendon J, White G. The feasibility <strong>of</strong> a nurse practitioner-ledprimary health care clinic in a <strong>school</strong> setting: a communityneeds analysis. J Adv Nurs. 2001;34(2)171–178.11. Burnett C, Juszczak E,Sullivan P. Nurse management <strong>of</strong> intractablefunctional constipation: A randomised controlled trial.Arch Dis Child. 2004;89(2)717–722.12. Cork M, Britton J, Butler L, Young S, Murphy R, Keohane S.Epidemiology and health services research: comparison <strong>of</strong>parent knowledge, <strong>the</strong>rapy utilisation and severity <strong>of</strong> atopiceczema before and after explanation and demonstration <strong>of</strong>topical <strong>the</strong>rapies by a specialist dermatology nurse. B J Dermatol.2003;149(8):582–589.13. Coulthard M, Vernon S, Lambert H, Mat<strong>the</strong>ws J. A nurse-lededucation and direct access service for <strong>the</strong> management <strong>of</strong>urinary tract infections in children: prospective controlled trial.BMJ. 2003;327(6):1346.14. Muir J, Burnett C. Setting up a nurse-led clinic for intractablechildhood constipation. Br J Community Nurs.1999;4(8):395–399.15. Bartle C. Developing a service for children with iron deficiencyanaemia. Nurs Stand. 2007;21(19):44–49.16. Hawkes Bay Primary Health Organisation. Strategic Plan2008–2011. Hastings; 2008.17. The Doctors Systems. Query builder. Retrieved March 12,2008 from The Doctors Systems.18. Durie M. Whaiora: Maori health development. 2nd ed.Oxford: Oxford University Press; 1999.19. The Doctors Systems. Query builder. Retrieved Feb 2010 fromThe Doctors Systems.20. Loening-Baucke,V. Constipation in early childhood: patientcharacteristics, treatment, and long-term follow up. BMJ.1993;34(1136):1400–1404.21. Fletcher M. Commentary: Nurse management <strong>of</strong> chronicconstipation. Paediatr Nurs. 2004;6(7):12.22. Wild S. (2006). Eczema clinics: Developing eczema experts.Retrieved January 20, 2008 from http://web.ebscohost.com.ezproxy.massey.ac.nz/ehost/detail.23. Henty C, Dickinson A. Practice nurses’ experience <strong>of</strong> <strong>the</strong> CarePlus programme: A qualitative descriptive study. NZ Fam Phys.2007;34(5):335–338.248 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
BACK TO BACKSometimes a case can be made forphysician-assisted suicideYESArguably this side <strong>of</strong> <strong>the</strong> moot is <strong>the</strong> easier;provide only one instance and <strong>the</strong> case is made,whilst arguing ‘no’ means anticipating all possiblecases. Moreover, <strong>the</strong> ethical principle <strong>of</strong>patient autonomy implies <strong>the</strong> need to providegood reasons for refusing. Indeed, given a defaultposition <strong>of</strong> autonomy, it is not actually necessaryto make a case, merely to refute any potentialobjections to physician-assisted suicide (PAS).Weak objectionsObjecting that <strong>the</strong> Hippocratic Oath forbidsPAS has little force, given <strong>the</strong> routine ignoring<strong>of</strong> o<strong>the</strong>r aspects <strong>of</strong> <strong>the</strong> oath (one could object toabortion on <strong>the</strong>se grounds) and <strong>the</strong> ludicrousness<strong>of</strong> imagining that ethical problems <strong>of</strong> <strong>the</strong> twentyfirstcentury should be solved by guidelines from<strong>the</strong> ancient Greeks. Similarly <strong>the</strong> objection that ‘adoctor’s job is to save life, not to end it’ is nei<strong>the</strong>rnecessarily true (fields like cosmetic surgery arerarely lifesaving) nor immutable.O<strong>the</strong>r objections might appear more compelling.It is certain that PAS would affect <strong>the</strong>doctor–patient relationship, but it is questionablewhe<strong>the</strong>r this would be a change for <strong>the</strong> worse.In countries where PAS and euthanasia areavailable, <strong>the</strong>re is no evidence <strong>of</strong> this, althoughthose whose enthusiasm outweighs <strong>the</strong>ir rigoursometimes produce apocryphal and unsubstantiatedscare stories <strong>of</strong> frightened people worryingthat <strong>the</strong>ir doctor will kill <strong>the</strong>m. Elsewhere <strong>the</strong>extension <strong>of</strong> autonomy appears to produce betterpatient well-being and relationships with pr<strong>of</strong>essionals,1 and <strong>the</strong>re seems little reason to believethat this would be any different for PAS.Perhaps <strong>the</strong> most persistent is <strong>the</strong> so-called‘slippery slope’ argument. 2 According to mostversions <strong>of</strong> this, a procedure such as PAS, whilstacceptable in itself, would later lead to someunacceptable future scenario such as <strong>the</strong> mass execution<strong>of</strong> <strong>the</strong> old and infirm. As a purely logicalargument it need not be taken seriously—indeedlogicians usually refer to <strong>the</strong> ‘slippery slopefallacy’, 3 only ceasing to be fallacious when <strong>the</strong>intervening steps are inevitable. Such steps could<strong>of</strong> course occur—for example, we may find thatdeaths through PAS are more peaceful, and thusmore opt for it, or maybe those who would havecommitted suicide alone may welcome assistance.If <strong>the</strong>se can be demonstrated, <strong>the</strong>n <strong>the</strong> argumentcan have real status, although one might questionwhe<strong>the</strong>r <strong>the</strong> examples given are undesirable.Unfortunately <strong>the</strong> data cited are typically correlationaland highly selected. 4 Rarely are counter-Glynn Owens PhDPr<strong>of</strong>essor, Department<strong>of</strong> Psychology, Faculty <strong>of</strong>Science, The University<strong>of</strong> Auckland, PB 92019,Auckland, New Zealandg.owens@auckland.ac.nzWhile evidence can help inform best practice, it needs to be placed in context.There may be no evidence available or applicable for a specific patient withhis or her own set <strong>of</strong> conditions, capabilities, beliefs, expectations and socialcircumstances. There are areas <strong>of</strong> uncertainty, ethics and aspects <strong>of</strong> care for which<strong>the</strong>re is no one right answer. General practice is an art as well as a science. Quality<strong>of</strong> care also lies with <strong>the</strong> nature <strong>of</strong> <strong>the</strong> clinical relationship, with communication andwith truly informed decision-making. The Back to Back section stimulatesdebate, with two pr<strong>of</strong>essionals presenting <strong>the</strong>ir opposing views regarding a clinical,ethical or political issue.Rod MacLeodGlynn OwenBACK TO BACK this issue:VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 249
BACK TO BACKexamples given—as with <strong>the</strong> United KingdomAbortion Act <strong>of</strong> 1967, which was introducedamong fears that <strong>the</strong> 28-week limit might ‘slip’ t<strong>of</strong>ull-term but in fact went in <strong>the</strong> o<strong>the</strong>r directionand later was reduced to 24 weeks.PAS and palliative care are not, as some claim,mutually exclusive. Like many working in end-<strong>of</strong>lifecare, I have heard, and accepted, claims thatwe are able to deal adequately with pain in around95–98% <strong>of</strong> cases, and have no argument with this.But even <strong>the</strong>se figures imply that around one in50 <strong>of</strong> our patients may suffer unacceptably andit is important to remember that pain may not be<strong>the</strong> only or even <strong>the</strong> main reason for wanting toend one’s life. 5 The suggestion that PAS is unnecessarywhere palliative care is available contrastswith our own New Zealand data showing illegaleuthanasia to be as likely when <strong>the</strong>re is access topalliative care services as not. PAS and palliativecare can peacefully coexist, and indeed liberalisationin Holland has been paralleled by a markedincrease in provision <strong>of</strong> palliative care. 6Potentially strong objectionsOne <strong>of</strong> <strong>the</strong> more compelling arguments concernsnot <strong>the</strong> patients but <strong>the</strong> practitioners. Typicallyfears are raised that providing PAS may lead toending life being seen as an easier or cheaper optionthan good palliative care, but Kay Mitchell’sinterviews with Dutch doctors performing euthanasiasuggest quite <strong>the</strong> opposite—doctors findingit extremely difficult and going to great lengthsto find alternatives. 7Also persuasive is <strong>the</strong> argument <strong>of</strong> ‘mistakes’;we might mistakenly allow PAS when someonecould be treated and allowed to enjoy <strong>the</strong>irlast days before dying naturally. Proponents,however, conveniently forget mistakes in <strong>the</strong>o<strong>the</strong>r direction—where someone is compelled tosuffer because <strong>the</strong> present systems cannot workproperly. Consider <strong>the</strong> following account <strong>of</strong> amyeloma patient in <strong>the</strong> USA who, saying that shedid not ‘have <strong>the</strong> energy to go ano<strong>the</strong>r round’ decidedto refuse food and drink from <strong>the</strong> Sundayevening ‘…only to find that <strong>the</strong> process wasn’t atall quick… by midnight Thursday she was alreadybeginning to choke on <strong>the</strong> liquid in her lungs…during <strong>the</strong> height <strong>of</strong> her struggles in <strong>the</strong> earlymorning hours <strong>of</strong> [Friday] she sweated, producedtears and manifested physical contortions whilemoaning… her body wri<strong>the</strong>d despite a displacedhip fracture and lack <strong>of</strong> bone definition in <strong>the</strong>long bone <strong>of</strong> one arm…’ (account from patient’shusband). Of course it could have been handledbetter—but mistakes happen under all policies,and, if comparing policies, we need to look at <strong>the</strong>mistakes on both sides.Finally <strong>the</strong>re is <strong>the</strong> argument that ‘many ask forhelp in dying, but typically only once’. Of coursemany patients may ask only once because <strong>the</strong> ‘no’is so resounding as to discourage repetition. But,in any event, no-one is suggesting legislationto permit PAS without evidence <strong>of</strong> an ‘enduringrequest’, as seen in such legislation in o<strong>the</strong>rcountries. For those who change <strong>the</strong>ir mind,this requirement provides safety and protection,whilst allowing those who do have an enduringwish to control <strong>the</strong>ir own lives.The picture that emerges, <strong>the</strong>n, is one <strong>of</strong> ourperpetuating <strong>the</strong> old ‘doctor knows best’ myth,depriving patients <strong>of</strong> control over <strong>the</strong>ir own liveswithout any sound justification. Perhaps <strong>the</strong> mosttelling argument comes from my colleague Pr<strong>of</strong>essorRod McLeod. After one <strong>of</strong> his very impressivelectures, a student said he’d been very impressedby Rod’s asking (and my apologies if he’s misquoted)‘Who are we to decide that someone else’s lifeisn’t worth living?’. Of course we have no right todo so, any more than we have <strong>the</strong> right to insistfor <strong>the</strong>m that it is when <strong>the</strong>y know o<strong>the</strong>rwise.References1. Deadman JM, Leinster SJ, Owens RG, Dewey ME, Slade PD.Taking responsibility for cancer treatment. Soc Sci Med.2001;53,669–677.2. Van Delden JJ. Slippery slopes in flat countries—a response. JMed Ethics. 1999;25:22–24.3. Enoch D. Once you start using slippery slope arguments you’reon a very slippery slope. Oxford J Leg Stud. 2001;4:629–647.4. Jochemsen H, Keown J. Voluntary euthanasia under control?Fur<strong>the</strong>r empirical evidence from <strong>the</strong> Ne<strong>the</strong>rlands. J Med Ethics.1999;25:16–215. Marquet RL, Bartelds A, Visser GJ, Spreeuwenberg P, Peters L.Twenty five years <strong>of</strong> requests for euthanasia and physician assistedsuicide in Dutch general practice: trend analysis.Br MedJ. 2003;327:201–202.6. Kuin A, Courtens AM, Deliens L, Vernooij-Dassen MJFJ, vanZuylen L, van der Linden B, van der Wal G. Palliative care consultationin <strong>the</strong> Ne<strong>the</strong>rlands; a nationwide evaluation study. JPain Symptom Manage. 2001;27:53–60.7. Mitchell K. Medical decisions at <strong>the</strong> end <strong>of</strong> life that hastendeath. PhD <strong>the</strong>sis. University <strong>of</strong> Auckland; 2002.250 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
BACK TO BACKSometimes a case can be made forphysician-assisted suicideNOWorking for most <strong>of</strong> my pr<strong>of</strong>essional lifetimewith people who are dying, it has been commonfor me to hear requests from individuals for<strong>the</strong>ir lives to be ended—mostly, I think, because<strong>of</strong> <strong>the</strong>ir sense <strong>of</strong> frustration, sadness, hopelessnessor fear. Some express <strong>the</strong>ir explicit opinionthat <strong>the</strong>y may be a burden on <strong>the</strong>ir family or onsociety and that is why <strong>the</strong>y are asking for <strong>the</strong>irlife to be ended.It is hard to imagine—even though I spend much<strong>of</strong> my clinical life with people who are desperatelyill—what it must be like to reach a stage where<strong>the</strong>y ask for death. Whatever it is that triggerssuch a request <strong>the</strong>y are rarely repeated overtime—once adequate palliative care is instituted,<strong>the</strong> request to die loses its urgency and <strong>the</strong> focusis once again on living. What I believe is thatmost, if not all, <strong>of</strong> <strong>the</strong>se requests are from peopletelling me <strong>the</strong>y ‘don’t want to live like this’,which is, <strong>of</strong> course, very different to wantingto die. The notion <strong>of</strong> real or potential sufferingthat cannot be relieved is a potent driverin some <strong>of</strong> <strong>the</strong>se requests. Some years ago <strong>the</strong>European Association for Palliative Care EthicsTask Force 1 produced a carefully constructed andwell thought out document that crystallised <strong>the</strong>thinking <strong>of</strong> many who are involved in end-<strong>of</strong>-lifecare. In that document <strong>the</strong>y suggested, amongo<strong>the</strong>r things, that: ‘Individual requests for euthanasiaand physician-assisted suicide are complexin origin and include personal, psychological, social,cultural, economic and demographic factors.Such requests require respect, careful attention,toge<strong>the</strong>r with open and sensitive communicationin <strong>the</strong> clinical setting.’They go on to suggest that ‘requests for euthanasiaand physician-assisted suicide are <strong>of</strong>ten alteredby <strong>the</strong> provision <strong>of</strong> comprehensive palliative care.Individuals requesting euthanasia or physicianassistedsuicide should <strong>the</strong>refore have access topalliative care expertise’. This is to say that weneed to explore, to our utmost abilities, what itis that is driving this request for <strong>the</strong> ending <strong>of</strong>a life and, in doing so, find ways to alleviate ormitigate suffering to such a degree that <strong>the</strong> desirefor death is diminished.The Task Force argues that ‘if euthanasia is legalisedin any society, <strong>the</strong>n <strong>the</strong> potential exists for:i. pressure on vulnerable persons;ii. <strong>the</strong> underdevelopment or devaluation <strong>of</strong>palliative care;iii. conflict <strong>between</strong> legal requirements and<strong>the</strong> personal and pr<strong>of</strong>essional values<strong>of</strong> physicians and o<strong>the</strong>r health carepr<strong>of</strong>essionals;iv. widening <strong>of</strong> <strong>the</strong> clinical criteria to includeo<strong>the</strong>r groups in society;v. an increase in <strong>the</strong> incidence <strong>of</strong> non-voluntary and involuntary medicalisedkilling;vi. killing to become accepted within society.’All <strong>of</strong> <strong>the</strong>se are real concerns that are met on aregular basis when caring for <strong>the</strong> most vulnerableand sick in our society and it is not unreasonable tosuppose that any intention to ‘permit’ assisted dyingwould put varying degrees <strong>of</strong> pressure on thosewho ask for <strong>the</strong> end <strong>of</strong> <strong>the</strong>ir life to be precipitated.Many who are receiving palliative care have afear <strong>of</strong> <strong>the</strong>ir life being prolonged unnecessarilyor for it to end in ‘unbearable’ distress. Clearlyno-one would want this, least <strong>of</strong> all for someone<strong>the</strong>y love, so it is incumbent upon us to ensurethat all who need it receive <strong>the</strong> best possiblephysical, psychological, spiritual and social care.In this way, assisted dying is not an option thatneeds be considered.Rod MacLeod MBChB,FRCGP, FAChPM, PhDHonorary Clinical Pr<strong>of</strong>essorand Associate Pr<strong>of</strong>essor,Department <strong>of</strong> GeneralPractice and Primary HealthCare, School <strong>of</strong> PopulationHealth, The University <strong>of</strong>Auckland, and Director<strong>of</strong> Palliative Care, NorthShore Hospice, Takapuna,Auckland, New Zealandrd.macleod@auckland.ac.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 251
BACK TO BACKEstablishing palliative care within mainstreamhealth care systems <strong>of</strong> all countries is essentialand this must be supported by appropriatefinance, education and research. In New Zealand,successive governments have demonstrated awillingness to support <strong>the</strong> provision <strong>of</strong> palliativecare through hospice programmes, but we stillfall behind many countries in <strong>the</strong> way in whichwe teach our health pr<strong>of</strong>essionals to deal withthis most challenging <strong>of</strong> health-related issues.Doctors have repeatedly reported being unpreparedto deal with end <strong>of</strong> life care on a practicallevel, let alone a legal or moral one. Repeatedly,<strong>the</strong> majority <strong>of</strong> doctors have voiced <strong>the</strong>ir viewsthat physician-assisted suicide is wrong. 2 Ano<strong>the</strong>rcompelling discussion is to be found in <strong>the</strong> writing<strong>of</strong> McLachlan 3 who asserts that one can ‘considerparticular actions to be contrary to appropricouldbe argued that, in palliative care, one <strong>of</strong><strong>the</strong> main things we have to <strong>of</strong>fer is that personalbond, but I would like to think that peoplewho are sick or dying should all be attended bythose who cared as well as attempted to cure,and nei<strong>the</strong>r <strong>of</strong> those aspects involves <strong>the</strong> ending<strong>of</strong> a life. When people consult <strong>the</strong>ir doctor it isbecause <strong>the</strong>y feel unwell, uncertain or <strong>the</strong>y aresuffering. It is hard enough to provide humanemedical care for <strong>the</strong>se people who seek helpwithout <strong>the</strong> added burden <strong>of</strong> an expectation thatsomewhere in that relationship <strong>between</strong> doctorand patient <strong>the</strong>re may be a tacit understandingthat this person, in whom <strong>the</strong>y have entrusted<strong>the</strong>ir life, <strong>the</strong>ir fears, <strong>the</strong>ir concerns, may be requiredultimately to end <strong>the</strong>ir life. There is nevera case to be made for physician-assisted suicide inany humane society.One <strong>of</strong> <strong>the</strong> many tensions in <strong>the</strong> doctor–patient relationship is <strong>the</strong>different perspective from which each party views <strong>the</strong> medicalencounter. Patients need caring as much as <strong>the</strong>y need curing and itis <strong>of</strong>ten caring that can be missingate pr<strong>of</strong>essional conduct even in <strong>the</strong> absence <strong>of</strong>legal and ethical objections to <strong>the</strong>m.’The major reason that physician-assisted suicideis so at odds with <strong>the</strong> rest <strong>of</strong> medical practiceis because <strong>of</strong> <strong>the</strong> unique bond that develops<strong>between</strong> doctor and patient. We need to ensurethat we strive to fully understand what it is that<strong>the</strong> patient is experiencing. Shimon Glick 4 writesthat one <strong>of</strong> <strong>the</strong> many tensions in <strong>the</strong> doctor–patient relationship is <strong>the</strong> different perspectivefrom which each party views <strong>the</strong> medicalencounter. Patients need caring as much as <strong>the</strong>yneed curing and it is <strong>of</strong>ten caring that can bemissing. 5 Francis Peabody, in <strong>the</strong> Journal <strong>of</strong> <strong>the</strong>American Medical Association in 1927 wrote:‘The reward is to be found in that personalbond which forms <strong>the</strong> greatest satisfaction in<strong>the</strong> practice <strong>of</strong> medicine.’ 6 Any situation wherephysician-assisted suicide is contemplated willirreparably damage that relationship or bond. ItReferences1. Materstvedt LJ, Clark D, Ellershaw J, Førde R, Boeck GravgaardA-M, Müller-Busch HC, Porta i Sales J, Rapin C-H.Euthanasia and physician-assisted suicide: a view from anEAPC Ethics Task Force. Palliat Med. 2003;17:97–101.2. Seale C. Legalisation <strong>of</strong> euthanasia or physician-assistedsuicide: survey <strong>of</strong> doctors’ attitudes. Palliat Med.2009;23:205–212.3. McLachlan HV. Assisted suicide and <strong>the</strong> killing <strong>of</strong> people?Maybe. Physician-assisted suicide and <strong>the</strong> killing <strong>of</strong> patients?No: <strong>the</strong> rejection <strong>of</strong> Shaw’s new perspective on euthanasia.J Med Ethics. 2010;36:306–309.4. Glick S. The empathic physician. In. Spiro H et al. (editors).Empathy and <strong>the</strong> practice <strong>of</strong> medicine. New Haven and London:Yale University; 1993.5. Janssen A, MacLeod RD What can people approaching deathteach us about how to care? Patient Education and Counseling.2010. In press.6. Peabody F. The care <strong>of</strong> <strong>the</strong> patient. JAMA (1927) 1984.(88:877–82) 252:813–18.252 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
continuing pr<strong>of</strong>essional developmentcochrane cornerTopical nasal decongestants: use up to 10 days maynot cause rhinitis medicamentosaBruce Arroll MBChB, PhD, FRNZCGPThe problem: The common cold affects almostevery human being at least once per year. Nasalcongestion is one <strong>of</strong> <strong>the</strong> most common symptoms<strong>of</strong> this condition and relief is sought from oralor topical decongestants. I was taught not to usetopical decongestants for more than three daysdue to concerns about rebound rhinitis known asRhinitis Medicamentosa, but have had patientswho have used topical decongestants for yearswith no such problem. Most <strong>of</strong> <strong>the</strong> literatureabout rhinitis medicamentosa comes from ENTclinics where patients have been using topicaldecongestants for many years. This CochraneCorner includes <strong>the</strong> Cochrane review 1 on nasaldecongestants for <strong>the</strong> common cold (now removedfrom <strong>the</strong> library, but available from Bruce Arrollvia email) and a randomised controlled trial byEccles (2008). 2More recently is <strong>the</strong> concern regarding illicit use<strong>of</strong> oral pseudoephedrine as a source <strong>of</strong> methamphetamine.Of medical concern may be <strong>the</strong> risk<strong>of</strong> increasing blood pressure and one oral decongestantphenylpropanolamine is no longer used.One case control study compared <strong>the</strong> use <strong>of</strong> coldpreparations containing phenylpropanolamine in702 people with a history <strong>of</strong> haemorrhagic strokeversus 1376 control people with no history <strong>of</strong>stroke. 3 The study found a non-significant trendtowards increased haemorrhagic stroke with phenylpropanolamine(RR 1.50, 95% CI 0.85 to 2.65).Clinical bottom line. The Cochrane reviewrecommended that topical nasal decongestantsseem to have an effect at least after <strong>the</strong> firstdose. The paper by Eccles found a similar benefitwhich persisted up to 10 days with three timesdaily use. The Cochrane review recommendednot using topical decongestants long-term andalso cautioned about using it in children asrhinitis medicamentosa has been reported after asingle dose in children. The Eccles paper foundno such problem in adults with three times dailyuse for 10 days.The University <strong>of</strong> Auckland,Auckland, New ZealandTopical nasal decongestants for <strong>the</strong> common coldTopical decongestants fornasal obstruction due to<strong>the</strong> common coldSuccess Evidence HarmsNNT <strong>of</strong> about 10 forimprovement in symptomsCochrane review 1RCT 2Possible risk <strong>of</strong> reboundcongestion with long-term useand in childrenNNT = numbers needed to treatReferences1. Taverner D, Latte GJ. Nasal decongestants for <strong>the</strong> common cold. Cochrane Database <strong>of</strong> Systematic Reviews 2007, Issue 1. Art. No:CD001953. DOI: 10.1002/14651858.CD001953.pub3.9 (now withdrawn but copy available from b.arroll@auckland.ac.nz)2. Eccles R, Eriksson M, Garreffa S, Chen SC. The nasal decongestant effect <strong>of</strong> xylometazoline in <strong>the</strong> common cold. Am J Rhinol.2008;22:491–496.3. Keman WN et al. Phenylpropanolamine and <strong>the</strong> risk <strong>of</strong> hemorrhagic stroke. N Engl J Med. 2000;343:1826–32.All people residing in New Zealand have access to <strong>the</strong> Cochrane Library via <strong>the</strong> Ministry websitewww.moh.govt.nz/cochranelibraryCorrespondence to:Bruce ArrollPr<strong>of</strong>essor <strong>of</strong> GeneralPractice and PrimaryHealth Care, TheUniversity <strong>of</strong> Auckland,PB 92019, Auckland,New Zealandb.arroll@auckland.ac.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 253
continuing pr<strong>of</strong>essional developmentcharms & harmsNoniMorinda citrifolia L.Also known as great morinda, Indian mulberry, nunaakai, dogdumpling, mengkudu, beach mulberry, vomit fruit and cheese fruitFelicity Goodyear-Smith MBChB, MGP,FRNZCGP; Pr<strong>of</strong>essor,Department <strong>of</strong> GeneralPractice and PrimaryHealth Care, School <strong>of</strong>Population Health, TheUniversity <strong>of</strong> Auckland,Auckland, New ZealandPreparations: The fruit is sometimes eaten asa food, especially in <strong>the</strong> Pacific Islands, althoughit has a strong smell and bitter taste. The seedsare edible if roasted. The root, leaves, bark, flowers,fruit and seed oil are all used medicinally.Roots, stem, bark, leaves and fruit may be appliedexternally as a poultice or consumed as an infusionor juice. Flowers and leaves may be taken astablets or teas and <strong>the</strong> fruit is <strong>of</strong>ten juiced.Active constituents: Approximately 200compounds have been isolated from noni, includinga number <strong>of</strong> anthraquinones and anthraquinoneglycosides, fatty acids and <strong>the</strong>ir derivatives,iridoids and iridoid glycosides, lignans, neolignans,flavonol glycosides, phenylpropanoids,saccharides, triterpenoids and fatty acids. 1 Thefruit provides a good source <strong>of</strong> vitamin C andpotassium. In vitro research is being conductedinto some <strong>of</strong> <strong>the</strong> anthraquinones and lignans butno ingredient has yet to be proven as a usefulbiologically active compound. Wide-rangingbenefits have been attributed to an alkaloid calledxeronine, which is reported to exist in noni as itsprecursor, proxeronine. However <strong>the</strong> presence <strong>of</strong>xeronine and proxeronine has not been confirmedin any peer-reviewed scientific publication norhave <strong>the</strong> structures <strong>of</strong> xeronine and proxeroninebeen provided. 1Main uses: Noni has been used as a medicinethroughout South East Asia, Polynesia and <strong>the</strong>Summary MessageEvidence for <strong>the</strong> efficacy <strong>of</strong> noni for <strong>the</strong> widerange <strong>of</strong> medicinal purposes for which it may beused is not available. Health pr<strong>of</strong>essionals shouldbe aware <strong>of</strong> <strong>the</strong> possibility <strong>of</strong> (undisclosed) use<strong>of</strong> noni and its use should be avoided, or at leastused only with caution, in patients on warfarin.Suspected adverse drug reactions should bereported to CARM. As with all herbal medicines,different noni products vary in <strong>the</strong>ir pharmaceuticalquality, and <strong>the</strong> implications <strong>of</strong> this forefficacy and safety should be considered.Caribbean for centuries. Externally it is appliedto cuts, sores and stings from poisonous fish.The green fruit, leaves and root traditionallyhave been used to treat menstrual cramps, bowelirregularities and urinary tract infections. Morerecently noni preparations have been promoted astreatment for cancer. Noni is purported to havea diverse range <strong>of</strong> effects including analgesic,anti-inflammatory, antimicrobial, anti-tubercular,antihypertensive and anticancer. 1 Its promotion asa panacea has led to a dramatic rise in its use inNorth America, Europe and Australasia and it isnow widely available in pharmacies, health foodstores, pharmacies and via <strong>the</strong> Internet.Herbal medicines are a popular health care choice, but few have been tested to contemporary standards.CHARMS & HARMS summarises <strong>the</strong> evidence for <strong>the</strong> potential benefits and possible harms <strong>of</strong> wellknownherbal medicines.254 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
continuing pr<strong>of</strong>essional developmentpearlsEvidence for efficacy: A number <strong>of</strong> invitro and animal studies involving noni extractshave been conducted, but <strong>the</strong>re has beenvery little research conducted under clinicaltrial conditions, and hence no Cochranesystematic review <strong>of</strong> trials <strong>of</strong> noni has beenundertaken.Adverse effects: Daily consumption <strong>of</strong>noni juice has led to hyperkalaemia in somepatients on potassium-restricted diets. Therehave also been reported cases <strong>of</strong> clinicallysignificant elevation in liver enzymes, includingtransaminases and lactate dehydrogenase,from daily noni juice, with return to normalonce <strong>the</strong> noni was discontinued. However,recent in vitro tests suggest that a normaldose <strong>of</strong> noni fruit juice is unlikely to induceadverse liver effects. 2Drug interactions: There is some evidencethat noni may interact with warfarin 3and that it may have an angiotensin I convertingenzyme (ACE) inhibiting effect. 1Key references1. Pawlus AD, Kinghorn DA. Review <strong>of</strong> <strong>the</strong> ethnobotany,chemistry, biological activity and safety <strong>of</strong> <strong>the</strong> botanicaldietary supplement Morinda citrifolia (noni). J PharmPharmacol. 2007 Dec;59(12):1587–609.2. West BJ, Su CX, Jensen CJ. Hepatotoxicity and subchronictoxicity tests <strong>of</strong> Morinda citrifolia (noni) fruit. J Toxicol Sci.2009 Oct;34(5):581–5.3. Carr ME, Klotz J, Bergeron M. Coumadin resistanceand <strong>the</strong> vitamin supplement ‘Noni’. Am J Hematol. 2004Sep;77(1):103.String <strong>of</strong> PEARLSPractical Evidence About Real Life SituationsPEARLS are succinct summaries <strong>of</strong> Cochrane Systematic Reviewsfor primary care practitioners—developed by Pr<strong>of</strong>. Brian McAvoyfor <strong>the</strong> Cochrane Primary Care Field (www.cochraneprimarycare.org), New Zealand Branch <strong>of</strong> <strong>the</strong> Australasian Cochrane Centre at <strong>the</strong>Department <strong>of</strong> General Practice and Primary Health Care, University<strong>of</strong> Auckland (www.auckland.ac.nz/uoa), funded by <strong>the</strong> New ZealandGuidelines Group (www.nzgg.org.nz) and published in NZ Doctor(www.nzdoctor.co.nz.).Watch and wait is usually as effective as antibiotics inchildren over six months <strong>of</strong> age with acute otitis mediaAntihistamines and/or decongestants are notrecommended for children with otitis media wi<strong>the</strong>ffusionGrommets are effective for recurrent acute otitis mediaAutoinflation for otitis media with effusion is helpful in<strong>the</strong> short-termTopical treatments are better than systemic antibioticsfor chronically discharging earsIntranasal corticosteroids may improve nasalobstruction symptoms in children with adenoidalhypertrophyTonsillectomy or adeno-tonsillectomy are effective forchronic and recurrent acute tonsillitisDisclaimer: PEARLS are for educational use only and are not meantto guide clinical activity, nor are <strong>the</strong>y a clinical guideline.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 255
ETHICSWork storiesVanya Kovach PhDIn 2006, <strong>the</strong> New Zealand Policelaunched its now long-runningrecruitment campaign based on <strong>the</strong>slogan ‘Better Work Stories’, and manymight have wondered what duties <strong>of</strong>confidentiality should constrain <strong>of</strong>ficerswhen talking about what happens to<strong>the</strong>m at work.* But we must acknowledgethat talking to our partners and friendsabout significant events has undeniablevalue, because storytelling is a centralpart <strong>of</strong> human life, connecting us too<strong>the</strong>rs and revealing us to ourselves.However, when <strong>the</strong>se events occur inpr<strong>of</strong>essional life, this very natural aspect<strong>of</strong> life is curtailed by obligations <strong>of</strong>confidentiality. The aim in what followsis to raise some questions about workstories and to explore one argument forallowing <strong>the</strong>m, under certain circumstances,and with certain limitations.The telling <strong>of</strong> work stories in <strong>the</strong> pr<strong>of</strong>essionsis not much studied or <strong>the</strong> ethics<strong>of</strong> it <strong>of</strong>ten addressed. † However, one1982 study in <strong>the</strong> USA reported thatwhile 17% <strong>of</strong> patients had <strong>the</strong> expectationthat <strong>the</strong>ir case would be discussedwith <strong>the</strong> medical staff members’ spouseor partner, 70% <strong>of</strong> medical staff admittedthat this was a common practice.Only 9% <strong>of</strong> patients thought it likelythat medical staff would use <strong>the</strong>ir caseas an interesting story to tell to nonmedicalfriends at a party, and yet 45%<strong>of</strong> medical staff reported that <strong>the</strong>y didthis. Interestingly, only 2% <strong>of</strong> patientsexpected that <strong>the</strong>y might be identifiedby name to non-medical personnel, andonly 8% <strong>of</strong> medical staff acknowledgedthat <strong>the</strong>y had done this. 1 No studieshave been done in New Zealand, so asyet we have no information about <strong>the</strong>expectations <strong>of</strong> patients here.What telling <strong>of</strong> stories is allowable bylaw? The Health Information PrivacyCode (2008) Rule 10, 1(e) allows that patientinformation may be used ‘in a formin which <strong>the</strong> individual concerned is notidentified’, and this is clarified as use‘within <strong>the</strong> agency’ or by students writingcase histories <strong>of</strong> patients who haveconsented to be seen by that student.Note, though, that <strong>the</strong>se restrictions on<strong>the</strong> use <strong>of</strong> anonymised information arein <strong>the</strong> non-binding commentary section<strong>of</strong> <strong>the</strong> Code. It seems <strong>the</strong> law does notclearly determine, at least in this Code,whe<strong>the</strong>r anonymised information canbe used for o<strong>the</strong>r purposes, though <strong>the</strong>implication is that any use should beconnected with health care. Just whatthis might encompass is a matter forethical debate.The pr<strong>of</strong>essional obligation to keepinformation about patients confidentialis grounded on a number <strong>of</strong> differentvalues or principles: respect for patients’autonomous control over <strong>the</strong>mselves;promises made by pr<strong>of</strong>essionals to<strong>the</strong>ir clients; benefits that can only begained when a client is assured that<strong>the</strong> information <strong>the</strong>y provide is keptsecret, and <strong>the</strong> relationship <strong>of</strong> trust<strong>between</strong> clients and pr<strong>of</strong>essionals. ‡ Thegeneral requirements <strong>of</strong> <strong>the</strong> obligation<strong>of</strong> confidentiality in health care, as setout in numerous codes <strong>of</strong> ethics, arethat information given by patients to* At <strong>the</strong> time, <strong>the</strong> police had no formal code <strong>of</strong> ethics, but <strong>the</strong> vulnerability <strong>of</strong> <strong>the</strong> people <strong>the</strong>y come in contact with should suffice to ground an obligation <strong>of</strong> confidentiality.Many <strong>of</strong> <strong>the</strong> work stories recorded on <strong>the</strong> police website are general and innocuous, but one worrying one is posted, entitled ‘Pregnant’.† A number <strong>of</strong> empirical studies have been published about patient expectations <strong>of</strong> confidentiality, but <strong>the</strong> ethical issue <strong>of</strong> works stories in particular has not been muchexamined. One exception is: James S. Gossip, stories and friendship: confidentiality in midwifery practice. Nursing Ethics. 1995;2(4):295–302. The issue is mentioned,but not discussed, in <strong>the</strong> canonical text Beauchamp TL and Childress JF. Principles <strong>of</strong> biomedical ethics. 6th edition. New York: Oxford University Press; 2008, p 305.‡ An excellent (and classic) paper on <strong>the</strong> justification and limits <strong>of</strong> confidentiality is: Bok S. The limits <strong>of</strong> confidentiality. Hastings Center Report. 1983;13(1):24–31.Correspondence to:Vanya KovachDepartment <strong>of</strong> Philosophy, Faculty<strong>of</strong> Arts, The University <strong>of</strong> Auckland,PB 92019 Auckland, New Zealandv.kovach@auckland.ac.nzThe ethics column explores issues around practising ethically in primary health careand aims to encourage thoughtfulness about ethical dilemmas that we may face.THIS ISSUE: Vanya Kovach, ethicist with <strong>the</strong> Philosophy Department at The University<strong>of</strong> Auckland, explores <strong>the</strong> morality and legality <strong>of</strong> health pr<strong>of</strong>essionals’ sharedanonymous stories about <strong>the</strong>ir patients.256 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ethicshealth pr<strong>of</strong>essionals is to be used onlyfor <strong>the</strong> purposes for which it was given,and that this information, and any factsabout <strong>the</strong> patient’s condition, be sharedonly with those who have an institutionally-recognisedrole in <strong>the</strong> care <strong>of</strong><strong>the</strong> patient, unless <strong>the</strong> patient gives permissionfor o<strong>the</strong>rs to have access. Legitimateexceptions to <strong>the</strong>se requirementsare made when serious and imminentharm to <strong>the</strong> patient or third partiesthreatens or when <strong>the</strong> court orders,and when <strong>the</strong> use <strong>of</strong> statistics based onpatient information is allowed for auditand service provision planning. All <strong>of</strong>this is familiar, and accepted. Concernshave been raised about <strong>the</strong> debasement<strong>of</strong> confidentiality, given <strong>the</strong> number <strong>of</strong>staff who might have electronic accessto a patient’s information, 2 and no-onebelieves that bedside curtains in wardsare soundpro<strong>of</strong>, but <strong>the</strong> expectation <strong>of</strong>patients persists that only a few willknow <strong>the</strong> intimate details <strong>of</strong> <strong>the</strong>irmedical conditions, and <strong>the</strong>ir familialand social circumstances.However, we know that work storiesabound, and that <strong>the</strong>re are a variety <strong>of</strong>motives for telling <strong>the</strong>m. Stories aretold to provide entertainment, for socialself-promotion, to establish commonality,to unwind and unload at <strong>the</strong> end <strong>of</strong><strong>the</strong> day, to warn <strong>of</strong> health dangers orto stimulate reflection and gain counseland comfort. O<strong>the</strong>r factors may havesignificance in evaluating <strong>the</strong> recounting<strong>of</strong> a story which involves informationabout patients, and <strong>the</strong>se includewho is speaking, who is listening, <strong>the</strong>level <strong>of</strong> detail which is disclosed, <strong>the</strong>context in which <strong>the</strong> information wasga<strong>the</strong>red and recounted, and <strong>the</strong> expectations<strong>of</strong> <strong>the</strong> people whose informationis being disclosed. Some <strong>of</strong> <strong>the</strong>se factorswill be explored in <strong>the</strong> followingthree scenarios.1A doctor is regaling her friends withstories at a dinner party, and describesan unnamed patient in a way thatmakes <strong>the</strong>m seem ridiculous.There are a number <strong>of</strong> reasons why thismight be unacceptable. Even if it is arguedthat this is not a breach <strong>of</strong> confidentiality,because <strong>the</strong> information is anonymised,this behaviour is in conflict with o<strong>the</strong>rpr<strong>of</strong>essional obligations: to treat one’spatients with dignity, and to respect<strong>the</strong>m. Although <strong>the</strong> doctor may not beable to show disrespect to a particularperson if <strong>the</strong>ir name is not mentioned,she can herself fail to respect <strong>the</strong>m—andalso encourage disrespect to o<strong>the</strong>rs whoshare characteristics with <strong>the</strong> person in<strong>the</strong> story. There is no direct harm to <strong>the</strong>patient, but <strong>the</strong>re may be harm to <strong>the</strong>doctor’s character and to <strong>the</strong> reputation<strong>of</strong> her pr<strong>of</strong>ession in <strong>the</strong> minds <strong>of</strong> <strong>the</strong>hearers. Perhaps it could be said that notrust <strong>between</strong> patient and doctor is lost, as<strong>the</strong> patient is unaware that <strong>the</strong>y have beenused in this way. But <strong>the</strong> obligation is to betrustworthy, not trusted. Trustworthinessis a disposition which can be understood asconsisting <strong>of</strong> a collection <strong>of</strong> conditionals:…If I was asked to lie…If someone <strong>of</strong>feredme money… (and, most relevantly here)if my patients did hear me talking about<strong>the</strong>m… But what <strong>of</strong> telling an unnamedpatient’s story without disrespect?2A nurse is concerned about <strong>the</strong>unhealthy habits and risky behaviour<strong>of</strong> her young relatives. Motivated by herlove for <strong>the</strong>m, and, she thinks, a properpr<strong>of</strong>essional desire to educate and inform,she tells <strong>the</strong>m some stories about unnamedpast patients who have suffered seriouslyfrom <strong>the</strong> effects <strong>of</strong> those behaviours.In this case <strong>the</strong>re is no disrespect topatients and no attack on <strong>the</strong>ir dignity.This is not a case <strong>of</strong> using patient informationfor <strong>the</strong> purposes for which it wasgiven, and yet <strong>the</strong> motive for telling <strong>the</strong>stories is consistent with <strong>the</strong> wider aims<strong>of</strong> health care. We accept <strong>the</strong> use <strong>of</strong> anonymisedpatient information for medicaleducation, so is its use for education <strong>of</strong><strong>the</strong> wider public any different? First,patients usually do have an expectationthat <strong>the</strong>ir cases will be used for teaching;§ second, such teaching takes place ina formal context where only medical pr<strong>of</strong>essionalsattend, and third, <strong>the</strong> hearerstake <strong>the</strong>mselves to be under obligations<strong>of</strong> confidentiality and respect. (Note thatif medical students discuss cases in bars,<strong>the</strong> latter two conditions are not met.)One fur<strong>the</strong>r difference is that <strong>the</strong> use<strong>of</strong> detailed cases is necessary for medicaleducation, but not for passing on healthadvice, though <strong>the</strong>re seems little doubtthat stories do lodge in <strong>the</strong> minds <strong>of</strong> hearersmore firmly than do generalisationsand statistics. If we do think that <strong>the</strong> necessityfor telling <strong>the</strong> story is importantin its justification, <strong>the</strong>n this might showthat even respectful recounting <strong>of</strong> cases,as interesting stories, is unacceptable.A pharmacist has encountered a3 troubling situation, which raises anumber <strong>of</strong> ethical and clinical issues andhe is unsure about how to respond. He hasdiscussed it with a colleague, but reachedno conclusion. He spends <strong>the</strong> eveningtalking about <strong>the</strong> case with his partner, ||(mentioning no names or identifyingcharacteristics), framing and reframing<strong>the</strong> facts, constructing and evaluating differentsolutions, struggling to find a goodway to proceed. He is tense and unhappy,and feels responsible for things outside<strong>of</strong> his control. His partner listens, asksquestions, suggests alternative points <strong>of</strong>view, and tries to get him to see that he isdoing all that he can. Is this apparentlycommon occurrence acceptable in <strong>the</strong> light<strong>of</strong> obligations <strong>of</strong> confidentiality?§ If patient expectations are relevant to <strong>the</strong> justification <strong>of</strong> what we do, <strong>the</strong>n research into what <strong>the</strong>y are is essential, as is public acknowledgement <strong>of</strong> what medical pr<strong>of</strong>essionalsactually do with stories.|| What follows might apply to close friends, or relatives, as well as partners.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 257
ETHICSIn this case, again, no lack <strong>of</strong> respect orattack on dignity is involved. But, again,<strong>the</strong> information has been disclosed tosomeone who has no formal role in <strong>the</strong>care <strong>of</strong> <strong>the</strong> patient, and who is <strong>the</strong>reforenot under any formal obligations tokeep <strong>the</strong> information confidential. Is itsafe to disclose, in <strong>the</strong>se circumstances?This might depend on a number <strong>of</strong> factors.Although no names are mentioned,will <strong>the</strong> partner know who <strong>the</strong> patientis? In small communities, it mightbe hard to avoid this. Is <strong>the</strong> partnersomeone who takes seriously <strong>the</strong> trustreposed in him or her, when <strong>the</strong>sestories are shared? Or are <strong>the</strong>y likelyto pass <strong>the</strong> stories on, for entertainment,self-promotion or even spite? Twopositions are possible here; first, that allsuch discussions are to be prohibited,because safety from identification orfrom misuse cannot be fully assured orenforced, or second, that such discussionsare acceptable to <strong>the</strong> extent thatit can be reasonably predicted that <strong>the</strong>information is safe, given <strong>the</strong> degree <strong>of</strong>detail disclosed, <strong>the</strong> social context <strong>of</strong><strong>the</strong> people involved and <strong>the</strong> character <strong>of</strong><strong>the</strong> partner.<strong>the</strong> relevant knowledge and experienceneeded for assisting decision-making,though <strong>the</strong>y may be able to contributeastute questions and useful perspectives.Decision-making might be aided bydiscussion with a partner, but it cannotbe claimed that <strong>the</strong>y have a necessaryrole in <strong>the</strong> process. The o<strong>the</strong>r purposefor telling <strong>the</strong> story is more personal.The pharmacist may need to vent emotions,explore psychological issues, orseek comfort. He may need to talk overhis responses to challenges, sad outcomesand mistakes in order integrate<strong>the</strong>m into his life and <strong>the</strong> way he thinksabout himself, both personally andpr<strong>of</strong>essionally. This second purpose isconsistent with <strong>the</strong> goals <strong>of</strong> health care,in that it provides significant support fortrue <strong>of</strong> a partner, though in most caseswe can assume that <strong>the</strong> partner hasat least that capacity for close attentionand sympa<strong>the</strong>tic concern that a<strong>the</strong>rapist <strong>of</strong>fers. One important limitto what is told is suggested by identifyingthis purpose <strong>of</strong> telling workstories—what is talked about must be‘about me’, and that <strong>the</strong> detail disclosedshould be only enough to provide <strong>the</strong>necessary context for understanding<strong>the</strong> personal difficulties and distressexperienced.Perhaps what this shows is that allhealth care workers should have regularpr<strong>of</strong>essional counselling, and thismay be so. However, <strong>the</strong>re is a deeperpurpose to sharing work stories withWhereas social workers and counsellors have formalsupervisory relationships within which <strong>the</strong>y can reflecton how <strong>the</strong>y have been affected personally by incidentsin <strong>the</strong>ir practice, most health pr<strong>of</strong>essionals do notIn <strong>the</strong> situation described, <strong>the</strong>re are twopurposes for telling <strong>the</strong> story. One isto seek assistance in making a decisionabout how to act. Should this take placeoutside <strong>the</strong> health care team? Reasonsfor maintaining that it shouldn’t includenot just confidentiality but efficacy, asnon-medical partners are likely to lackAcknowledgementsMy thanks to Allen Fraser,Christine Johannis, RobynBennitt, Peter Hoar, StephenKovacevich and students in<strong>the</strong> Diploma in Pr<strong>of</strong>essionalEthics at <strong>the</strong> University <strong>of</strong>Auckland for helping clarifymy thoughts on this issue.a pr<strong>of</strong>essional to perform his or her role.But is this sufficient to satisfy <strong>the</strong> intent<strong>of</strong> <strong>the</strong> Health Information PrivacyCode, and <strong>the</strong> ethical basis <strong>of</strong> promises<strong>of</strong> confidentiality?How necessary is it for <strong>the</strong> pharmacistto seek this support from his partner?Whereas social workers and counsellorshave formal supervisory relationshipswithin which <strong>the</strong>y can reflect on how<strong>the</strong>y have been affected personally byincidents in <strong>the</strong>ir practice, most healthpr<strong>of</strong>essionals do not. Colleagues mayperform this supervisory and counsellingrole, though <strong>the</strong>y might havelimited time, and lack <strong>the</strong> skills or <strong>the</strong>intimacy <strong>of</strong> relationship required forsuch ‘counselling’ to be effective andsafe. Of course, this could be equallypartners, and that is to meet <strong>the</strong> needto be known intimately, and to shareour lives fully with our life companions.Pr<strong>of</strong>essional life requires that weabjure many quite natural things—including always applying our ownmorality to <strong>the</strong> work that we do. It isnot too much to ask that in joining apr<strong>of</strong>ession we give up <strong>the</strong> freedom touse our work stories to gossip, preenand entertain, but is it too much toask that we give up sharing our wholeselves with our partners?References1. Weiss B. Confidentiality expectations <strong>of</strong> patients,physicians and medical students. JAMA. 1982;247(19):2695–97.2. Siegler M. Confidentiality in medicine—a decrepit concept. New Eng J Med.1982;307(24):1518–21.258 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
ook reviewsHerbs and Natural Supplements: An Evidence-based Guide3rd editionEdited by L. Braun and M. CohenReviewed by Felicity Goodyear-SmithThe University <strong>of</strong> AucklandThis reference book is written for anAustralian and New Zealand audience<strong>of</strong> health practitioners fromvarious disciplines to provide a comprehensiveguide to <strong>the</strong> evidence base <strong>of</strong>commonly-used herbs and supplements.The first section covers discussion oncomplementary medicine in general,and herbal medicine, clinical nutrition,aroma<strong>the</strong>rapy and food as medicine inparticular. This is followed by severalchapters on <strong>the</strong>ir use in clinical practice.However, <strong>the</strong> bulk <strong>of</strong> <strong>the</strong> book is analphabetical compendium <strong>of</strong> evidencebasedreviews <strong>of</strong> 130 popular herbs andnatural supplements available over <strong>the</strong>counter in Australia and New Zealand.The final section is appendices <strong>of</strong> summarisedtables.The book is well set out and indexed. Themonographs follow a standard formatwith headings such as chemical components,main actions, clinical use, adversereactions, interactions, contraindicationsand precautions, pregnancy use and answersto frequently asked questions. They<strong>of</strong>ten include a box <strong>of</strong> ‘practice points’.The reviews are generally well referenced.However, on careful examination <strong>of</strong>some <strong>of</strong> <strong>the</strong> reviews, <strong>the</strong>re is a tendencyto overemphasise <strong>the</strong> effectiveness <strong>of</strong><strong>the</strong> remedies and downplay <strong>the</strong> potentialharms. For example, <strong>the</strong> monograph onsaw palmetto claims <strong>the</strong>re is substantialscientific evidence that it is an effectivetreatment for benign prostatic hypertrophy,whereas a 2009 Cochrane reviewfound it no more effective than placebo.Similarly, <strong>the</strong> book concludes that clinicaltrials support <strong>the</strong> use <strong>of</strong> black cohoshfor menopausal symptoms, whereas <strong>the</strong>evidence for effectiveness is inconclusive,and <strong>the</strong>re is a small but serious risk<strong>of</strong> liver reactions to this compound.While this book is a systematic andcomprehensive approach to documenting<strong>the</strong> evidence for herbs and natural supplements,<strong>the</strong> interpretation tends to beslanted in favour <strong>of</strong> <strong>the</strong>ir use. I wouldadvise caution in following all <strong>the</strong>irrecommendations.Publisher: Churchill LivingstoneDate <strong>of</strong> publication: 2010No. <strong>of</strong> pages: 1221Evidence-based Practice across <strong>the</strong> Health Pr<strong>of</strong>essionsBy Tammy H<strong>of</strong>fmann, Sally Bennett and Chris Del MarReviewed by Gill Robb, Epidemiology andBiostatistics, School <strong>of</strong> Population Health,The University <strong>of</strong> AucklandAs <strong>the</strong> authors suggest in <strong>the</strong> preface:why ano<strong>the</strong>r book about evidence-basedpractice? The value<strong>of</strong> this book about evidence-based practiceis that it does indeed target a wide range<strong>of</strong> health pr<strong>of</strong>essionals. For each studydesign (including qualitative research),worked examples are provided that relateto each <strong>of</strong> <strong>the</strong> major pr<strong>of</strong>essional groups,including occupational <strong>the</strong>rapy, physio<strong>the</strong>rapy,speech pathology, podiatry,medicine, nursing, nutrition, radiationand complementary and alternative <strong>the</strong>rapies.Using a wide range <strong>of</strong> examples givesan opportunity to illustrate many <strong>of</strong> <strong>the</strong>key concepts and challenges in appraisingevidence. This provides a rich source <strong>of</strong>information for all health pr<strong>of</strong>essionals.The book is clearly written and usessimple, non-technical language, makingit easy to read. The content is well structuredand organised, making good use <strong>of</strong>headings, tables and figures to navigate<strong>the</strong> reader through <strong>the</strong> text and understand<strong>the</strong> material. There are 16 chapters,which follow logically through <strong>the</strong> fivesteps <strong>of</strong> evidence-based practice (EBP).Each chapter starts with an outline <strong>of</strong><strong>the</strong> key learning objectives and concludeswith summary points and references.The first chapter introduces <strong>the</strong> concept<strong>of</strong> evidence-based practice, its rationale,origins and scope. The second chapterdescribes how to translate informationneeds into answerable questions, andwhich study design is most suited toVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 259
BOOK REVIEWSanswer each type <strong>of</strong> question. Readersare introduced to some <strong>of</strong> <strong>the</strong> importantconcepts for EBP, such as chance, biasand confounding, statistical and clinicalsignificance. Chapter three is an excellentresource for people who find searchingfor <strong>the</strong> evidence a challenging exercise.After describing <strong>the</strong> basics <strong>of</strong> searching,readers are guided through <strong>the</strong> searchprocess, starting with <strong>the</strong> top layer <strong>of</strong> <strong>the</strong>Evidence Pyramid described by Haynes(<strong>the</strong> higher up <strong>the</strong> pyramid, <strong>the</strong> morereliable <strong>the</strong> information) and workingdown. For each ‘layer’, a comprehensivelist <strong>of</strong> sources <strong>of</strong> evidence is supplied. Forlocating individual studies (bottom layer)<strong>the</strong> common databases are explained andmore detailed instruction is given onhow to undertake an effective search,including how to used <strong>the</strong> ‘Clinical Queries’function in PubMed and Medline.Worked examples are provided for searchesfocussed around clinical questions.Chapters 4–11 deal with <strong>the</strong> core material<strong>of</strong> <strong>the</strong> book. Two chapters are devotedto each type <strong>of</strong> evidence (intervention,diagnosis, prognosis and client’s experiencesand concerns). Using a clinicalscenario for each, <strong>the</strong> initial chapter worksthrough <strong>the</strong> five steps <strong>of</strong> EBP, explainingkey concepts. Of particular value are <strong>the</strong>explanations <strong>of</strong> <strong>the</strong> meaning <strong>of</strong> <strong>the</strong> results,which <strong>of</strong>ten present a barrier whenappraising evidence. The second chapterprovides worked examples for each <strong>of</strong><strong>the</strong> major pr<strong>of</strong>essional groups.Systematic reviews and meta-analyses aredealt with in Chapter 12, and guidelinesin Chapter 13. Chapter 14 focuses on howto communicate evidence to patients andincludes an eloquent discussion on <strong>the</strong>complex issue <strong>of</strong> shared decision-making.Several simple ways <strong>of</strong> communicatingstatistical information to patients arepresented, and a tool ‘Discern’ is providedto help practitioners evaluate any writteninformation patients may have locatedon <strong>the</strong> Internet. The chapter on clinicalreasoning provides an interesting insightinto <strong>the</strong> complexities <strong>of</strong> pr<strong>of</strong>essionalpractice—a topic not <strong>of</strong>ten covered inmany EBP texts. The inherent difficulties<strong>of</strong> integrating <strong>the</strong> many sources <strong>of</strong> ‘evidence’,while at <strong>the</strong> same time fulfillingrole expectations and delivering a service,are acknowledged. The final chapter covers<strong>the</strong> last and probably <strong>the</strong> most challengingstep in <strong>the</strong> EBP process—closing<strong>the</strong> evidence–practice gap. A number <strong>of</strong>methods are described, along with <strong>the</strong>barriers and enablers. The importance <strong>of</strong>using a <strong>the</strong>oretical framework to addressfactors that influence getting evidenceinto practice is emphasised.In summary, this book is an excellentresource for all health practitioners. Theway it has been structured and writtenwill encourage readers to ‘dip into’ <strong>the</strong>book frequently as <strong>the</strong>y embark on <strong>the</strong>irjourney <strong>of</strong> lifelong learning.Publisher: Churchill Livingstone, AustraliaDate <strong>of</strong> publication: 2010No. <strong>of</strong> pages: 349A History <strong>of</strong> <strong>the</strong> ‘Unfortunate Experiment’at National Women’s Hospital—by Linda Bryderand The Cartwright Papers: Essays on <strong>the</strong> CervicalCancer Inquiry <strong>of</strong> 1987–88—edited by Joanna ManningReviewed by Jane Gunn, Pr<strong>of</strong>essor, Chair<strong>of</strong> Primary Care Research and Head <strong>of</strong> <strong>the</strong>Department <strong>of</strong> General Practice, University<strong>of</strong> Melbourne, AustraliaMore than 20 years have passedsince Sandra Coney and PhillidaBunkle published an articlein Auckland’s Metro magazine titled‘An unfortunate experiment at NationalWomen’s’. The article claimed that DrHerbert Green, an associate pr<strong>of</strong>essorand gynaecologist, had withheld treatmentfrom women at risk <strong>of</strong> developingcervical cancer. The response to <strong>the</strong>article was alarming and unprecedented,resulting in <strong>the</strong> now famous ‘CartwrightInquiry into Cervical Cancer’ whichhad important and lasting ramificationson health care provision, especially forwomen—ramifications that spread farbeyond <strong>the</strong> shores <strong>of</strong> New Zealand.Now, two decades later, <strong>the</strong> controversyhas been reignited by <strong>the</strong> publication <strong>of</strong>two books presenting opposing views. InA History <strong>of</strong> <strong>the</strong> ‘Unfortunate Experiment’at National Women’s Hospital, <strong>the</strong>medical historian Linda Bryder, fromThe University <strong>of</strong> Auckland, arguesthat Dr Herbert Green was in manyways ahead <strong>of</strong> his time—‘a thinkinggynaecologist’—a reflexive practitionerwho questioned <strong>the</strong> level <strong>of</strong> interventionand radical treatments delivered towomen with precancerous and carcinomain situ lesions. She makes a convincingargument that Green was a scapegoatwho was outwitted by a passionate andactive feminist movement. If one wasto read only Bryder’s book one wouldbe convinced that Green was dealt a260 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
BOOK REVIEWSWith regards to <strong>the</strong> Back to Back in <strong>the</strong> last issue <strong>of</strong> <strong>the</strong>JPHC on population-based screening for ADHD, 1 Iwish to support Ross Lawrenson’s objections to Tony Hanne’sproposal for population-based screening for attention deficithyperactivity disorder (ADHD) from a non-medical perspective.The problem with viewing behaviours <strong>of</strong> concern from amedical viewpoint is that <strong>the</strong> process <strong>of</strong> diagnosis, assignment<strong>of</strong> cause and <strong>the</strong> mode <strong>of</strong> intervention are all regarded primarilyfrom a physiological or organismic position. The contexsevereinjustice. Yet, here enters JoannaManning, an associate pr<strong>of</strong>essor <strong>of</strong> law,also from The University <strong>of</strong> Auckland,who responded to Bryder’s book with anedited series on The Cartwright Papers.Manning and colleagues appear to haveproduced <strong>the</strong>ir book with <strong>the</strong> mainpurpose <strong>of</strong> discrediting Bryder’s account.It is not made clear whe<strong>the</strong>r Bryder andManning (both from The University <strong>of</strong>Auckland) know each o<strong>the</strong>r, or have hadpast disputes. I would have found thisdeclaration a useful piece <strong>of</strong> information.For anyone interested in how one storycan be portrayed in two completely opposingways, <strong>the</strong>n I recommend reading<strong>the</strong>se two books as a pair. Every medicaland nursing student would benefit fromreading and discussing <strong>the</strong>se bookstoge<strong>the</strong>r—<strong>the</strong>re are just so many lessonsto be learned. I would start with Bryder.Here you will get to know Dr HerbertGreen and see his actions in <strong>the</strong> bestpossible light. Moving on to <strong>the</strong> essaysedited by Manning, you will find yourselfquestioning Bryder’s view. In <strong>the</strong>end you will have to decide for yourself.Personally, I could never condone <strong>the</strong>way in which Dr Green changed previousdiagnostic categories—this is justbad and unethical research. Yet, on <strong>the</strong>o<strong>the</strong>r hand, I agree with Bryder that inmany ways he was ahead <strong>of</strong> his time and<strong>the</strong> way he thought about cervical dysplasiawas potentially groundbreaking.The outcome could have been so differentif only he could have had betterresearch training and maintained a moreobjective view. His lack <strong>of</strong> communicationwith colleagues and patients is, inmy mind, his great undoing. Bryder’sdefense <strong>of</strong> Green’s behaviour as beingtypical <strong>of</strong> <strong>the</strong> time, makes for worthyreflection. Yet in both books, Green,<strong>the</strong> somewhat intimidating gynaecologist,is a familiar character to anyonetrained prior to <strong>the</strong> late eighties. Thereis certainly a feeling that this storycould have been found in any number <strong>of</strong>institutions. The medical pr<strong>of</strong>ession andwider health care system has changeddramatically since <strong>the</strong> days when DrGreen was a presiding power at <strong>the</strong> NationalWomen’s. Whe<strong>the</strong>r you remember<strong>the</strong> Cartwright Inquiry, whe<strong>the</strong>r youwere taught or treated by Dr HerbertGreen (or someone remarkably similar),<strong>the</strong>se two books make excellent reading.Most <strong>of</strong> all, <strong>the</strong>y make you think. Theinclusion <strong>of</strong> a chapter by Clare Ma<strong>the</strong>son(<strong>the</strong> patient at <strong>the</strong> centre <strong>of</strong> initial controversy)in <strong>the</strong> Manning book makes forpowerful reading. The view that such adebacle could happen again somewherein our health care system is put forwardas a chilling warning—ano<strong>the</strong>r reason toget <strong>the</strong>se books and read <strong>the</strong>m!A History <strong>of</strong> <strong>the</strong> ‘Unfortunate Experiment’at National Women’s HospitalPublisher: Auckland University PressDate <strong>of</strong> publication: 2009No. <strong>of</strong> pages: 264The Cartwright Papers: Essays on <strong>the</strong>Cervical Cancer Inquiry <strong>of</strong> 1987–88Publisher: Bridget Williams BooksDate <strong>of</strong> publication: 2010No. <strong>of</strong> pages: 223LETTERS TO THE EDITORWe should not screen for ADHDtual and ecological contributors which may generate, maintainand elaborate such behaviours thus remain ignored or, at best,poorly analysed and consequently go unresolved. Fur<strong>the</strong>r,screening instruments are notoriously coarse-grained, <strong>of</strong>ten<strong>of</strong> poor validity, and are likely to provide, at best, numbers <strong>of</strong>false positives and negatives. Asking parents and teachers tomake appropriate judgments in a questionnaire upon whicha diagnosis is <strong>the</strong>n based exposes <strong>the</strong> process to bias becauseboth may simply be seeking a solution which does not involveei<strong>the</strong>r party to examine or modify <strong>the</strong>ir behaviour managementmethods, even though <strong>the</strong>se may be major contributorsto <strong>the</strong> behaviours <strong>of</strong> which <strong>the</strong>y complain.Letters may respond to published papers, briefly report original research or case reports, or raise matters <strong>of</strong> interest relevant toprimary health care. The best letters are succinct and stimulating. Letters <strong>of</strong> no more than 400 words may be emailed to:editor@rnzcgp.org.nz. All letters are subject to editing and may be shortened.VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 261
LETTERS TO THE EDITORA one-<strong>of</strong>f screen and a consulting room assessment cannotprovide an adequate basis for diagnosis or intervention. Working,as I do, with families and in <strong>school</strong>s with children whoare deemed problematic by parents and teachers emphasises <strong>the</strong>role <strong>of</strong> adults in mismanaging children’s behaviour. Teachersfrequently identify children as ‘hyperactive’ when <strong>the</strong>ycannot manage <strong>the</strong>m or find <strong>the</strong>m disruptive. Closer analysiscan reveal that <strong>the</strong> teacher provides high rates <strong>of</strong> attentionfor disruption and little encouragement for desired behaviourwhen it occurs. Sometimes <strong>the</strong> child lacks <strong>the</strong> entry skills into<strong>the</strong> academic programme or comes to <strong>school</strong> troubled and/orhungry from a dysfunctional family and so engages in alternativeactivities which attract adult attention. Failure to identifyand deal with <strong>the</strong>se ecological factors or simply masking <strong>the</strong>mwith methylphenidate begins to verge on <strong>the</strong> irresponsible inmy opinion. I have systematically observed <strong>the</strong> classroom behaviour<strong>of</strong> children diagnosed as ADHD by paediatricians andpsychiatrists. Some have remained non-medicated by parentalrequest and my data have shown <strong>the</strong>m to be functioning aswell as, if not better than, peers in terms <strong>of</strong> on-task behaviour,compliance and disruption. Such data raise questions <strong>of</strong> <strong>the</strong>validity <strong>of</strong> diagnosis by those currently assigned <strong>the</strong> role and,consequently, questions about <strong>the</strong> utility <strong>of</strong> population-basedscreening and treatment <strong>of</strong> ADHD by GPs.Barry S Parsonson MA(Hons), PGDipClinPsychPhD FNZPsS MICP, Registered PsychologistReferences1. Hanne T, Lawrenson R. Back to Back: New Zealand general practice shouldadopt population-based screening for attention deficit hyperactivity disorder. JPrimary Health Care. 2009;2(2):155–8.Too many articles by nursesThank you for <strong>the</strong> last edition <strong>of</strong> Journal <strong>of</strong> Primary HealthCare (better to be named ‘Journal <strong>of</strong> RNZCGP’). I enjoyreading <strong>the</strong> articles in every issue. The last edition was hugelychanged in format. There were so many articles by nurses Iwondered whe<strong>the</strong>r I was reading a nursing journal?Why don’t you encourage and stimulate young doctors todo research and write some learning and educational articleswhich will be useful for GPs? If you advertise in <strong>the</strong> NZ Doctormagazine and primary health journals inviting <strong>the</strong> doctorsand registrars to write, definitely all will get <strong>the</strong> message.Also you could give <strong>the</strong>m awards or certificates for doing suchresearch activities and writings.Hope you welcome our comments in a positive way.Dr Mrs M RamanathanA well designed journal for <strong>the</strong> primary care sectorAs Editor <strong>of</strong> <strong>the</strong> Journal <strong>of</strong> Primary Health Care, we applaudyou for re-launching <strong>the</strong> traditional GP journal(New Zealand Family Physician) as a primary care, ra<strong>the</strong>r thansolely GP-orientated publication. Likewise, we believe that bysupporting <strong>the</strong> Journal <strong>of</strong> Primary Health Care, <strong>the</strong> Royal NewZealand College <strong>of</strong> General Practitioners (RNZCGP) demonstratesa commitment to <strong>the</strong> wider view <strong>of</strong> <strong>the</strong> primary carelandscape. There is an expectation by health policy-makersthat <strong>the</strong> primary care sector delivers high quality health carethrough <strong>the</strong> development <strong>of</strong> effective multidisciplinary teams.Patients also assume this happens but, sadly, it is not always<strong>the</strong> case. Your journal supports a step in <strong>the</strong> right direction.In terms <strong>of</strong> ‘usability’ as a resource, this new look journalhas a lot to <strong>of</strong>fer <strong>the</strong> primary care sector. There is clinical materialwhich will assist general practitioners, practice nurses,community pharmacists and PHO-based clinical advisorypharmacists to stay current. The Back to Back section engagesspecialists into <strong>the</strong> primary care arena and allows informeddebate to be facilitated in peer group sessions. For academicsand applied health services researchers, <strong>the</strong> Journal <strong>of</strong> PrimaryHealth Care provides a platform for publishing robust researchwhich is locally relevant and interesting. There is a Gems sectionwhich refers us back to <strong>the</strong> good work that New Zealandprimary care researchers are publishing abroad. Finally, for <strong>the</strong>more political amongst us <strong>the</strong>re is a commentary/essay/viewpointssection.In addition to <strong>the</strong> vigorous, multidisciplinary nature <strong>of</strong> <strong>the</strong>journal, we really like <strong>the</strong> multiple categories under which wecan publish. There is no need for <strong>the</strong>med issues as <strong>the</strong> regularcategories within <strong>the</strong> journal cater for a myriad <strong>of</strong> topics. Asresearchers we don’t need to wait any longer than we should tohave our papers reviewed and accepted, but can feel reassuredthat speed <strong>of</strong> publication is not at <strong>the</strong> expense <strong>of</strong> thoughtfuland robust review from experts in <strong>the</strong> field, as well as practicebasedacademics.Based on our experience <strong>of</strong> reading, reviewing and publishingin local and international journals over <strong>the</strong> past few yearswe think that <strong>the</strong> Journal <strong>of</strong> Primary Health Care fulfils animportant role in bringing toge<strong>the</strong>r primary care researchersfrom a range <strong>of</strong> disciplines to publish and comment on <strong>the</strong>issues that are relevant to primary care practitioners and policymakers alike. We would like to thank you and <strong>the</strong> RNZCGPfor <strong>the</strong> energy and insight in bringing us <strong>the</strong> Journal <strong>of</strong> PrimaryHealth Care.Shane Scahill (Doctoral candidate, School <strong>of</strong> Pharmacy andClinical Advisory Pharmacist), Dr Jeff Harrison (School <strong>of</strong>Pharmacy), Dr Peter Carswell (School <strong>of</strong> Population Health—Division Health Systems), Pr<strong>of</strong>. John Shaw (School <strong>of</strong> Pharmacy)262 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE
RESEARCH GEMSGems <strong>of</strong> New ZealandPrimary Health Care ResearchWhich anticonvulsant drug is effectivefor which types <strong>of</strong> neuropathic pain?Anticonvulsant drugs are used fortreating neuropathic pain. This paperreviewed all <strong>the</strong> evidence for <strong>the</strong> efficacy<strong>of</strong> different anticonvulsants for specificconditions. It includes a table whichsummarises which drugs have been assessedfor which conditions and whe<strong>the</strong>r<strong>the</strong> evidence supports <strong>the</strong>ir use or not.Gaps in <strong>the</strong> evidence are striking.Goodyear-Smith F, Halliwell J. Anticonvulsantsfor neuropathic pain: gaps in <strong>the</strong> evidence.Clin J Pain. 2009;25(6):528–536. DOI:10.1097/AJP.0b013e318197d4cc.Corresponding author: F. Goodyear-Smith.Email: f.goodyear-smith@auckland.ac.nzUse <strong>of</strong> antidepressants fordepression in primary carePrevious reviews have looked at <strong>the</strong> use<strong>of</strong> antidepressant treatment in <strong>secondary</strong>care settings, but <strong>the</strong>re has been doubtabout <strong>the</strong> effectiveness <strong>of</strong> antidepressantsin primary care. This Cochranereview included 14 studies conducted inadults (not <strong>the</strong> elderly) in primary caresettings, in which tricyclic antidepressants(TCAs) or selective serotonin reupdateinhibitors (SSRIs) were comparedagainst placebo controls in <strong>the</strong> treatment<strong>of</strong> depression. The results showed thatboth types <strong>of</strong> antidepressants were effectivefor depression. There appearedto be more adverse effects with TCAsthan with SSRIs, although <strong>the</strong> rates <strong>of</strong>withdrawal from <strong>the</strong> study medicationdue to adverse effects were very similar<strong>between</strong> <strong>the</strong> two classes <strong>of</strong> drugs.Arroll B, Elley CR, Fishman T, Goodyear-Smith FA, Kenealy T, Blashki G, Kerse N,MacGillivray S. Antidepressants versusplacebo for depression in primary care(review), The Cochrane Library, pp 61,Issue 3, 2009. ID 692702053115360884.Corresponding author: B. Arroll.Email: b.arroll@auckland.ac.nzStopping smoking early in pregnancymay prevent pre-term birthsA cohort study <strong>of</strong> 2500 women foundthat current smokers had higher rates <strong>of</strong>spontaneous pre-term birth and smallfor gestational age infants than stoppedsmokers. Women who stopped smokingbefore 15 weeks’ gestation had <strong>the</strong> samerates <strong>of</strong> spontaneous preterm birth andsmall-for-dates babies as non-smokers,indicating that <strong>the</strong>se severe adverseeffects <strong>of</strong> smoking may be reversible ifsmoking is stopped early in pregnancy.McCowan L, Dekker G, Chan E, StewartA,Chappell L, Misty Hunter M, Moss-Morris R, North R On behalf <strong>of</strong> <strong>the</strong> SCOPEconsortium. Spontaneous preterm birthand small for gestational age infantsin women who stop smoking early inpregnancy: prospective cohort study. BMJ.2009;338:b1081. doi:10.1136/bmj.b1081.Corresponding author: L. McCowan.Email: l.mccowan@auckland.ac.nzAcclimatisation by aeroplaneIt is generally accepted that <strong>the</strong> performance<strong>of</strong> athletes participating in aerobicendurance events is adversely affectedby altitude, whereas athletes involvedin speed and anaerobic events are ei<strong>the</strong>runaffected or perform even better ataltitude than at sea level. Athletes travellingoverseas in long-haul flights areeffectively spending up to 13 hours atelevated altitude, because aircraft cabinsare pressurised to maximum effectivealtitudes <strong>of</strong> 2440 metres. This studyshowed that oxygen saturation declinedsignificantly in athletes during longhaulcommercial flights, in response toreduced cabin pressure. Athletes <strong>of</strong>tenneed to compete at altitudes similar to<strong>the</strong> effective altitudes experienced inairliner cabins. The exact timing andimpact <strong>of</strong> <strong>the</strong>se changes on performanceis still unclear but has implicationsfor altitude acclimatisation planning byathletes.Geertsema C, Williams AB, Dzendrowskyj P,Hanna C. Effect <strong>of</strong> commercial airline travelon oxygen saturation in athletes. Br J SportsMed. 2008;42(11):577–81.Corresponding author: C. Geertsema.Email: celeste.g@ihug.co.nzGEMS are short précis <strong>of</strong> original papers published by NZ researchers. For a copy <strong>of</strong> a full paper pleaseemail <strong>the</strong> corresponding author. Researchers, to have your work included please send a 100word summary <strong>of</strong> your paper and <strong>the</strong> full reference details to: editor@rnzcgp.org.nzVOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE 263
about <strong>the</strong> journal <strong>of</strong> primary health careThe Journal <strong>of</strong> Primary Health Care(JPHC) is a peer-reviewed journalwhich has replaced <strong>the</strong> New ZealandFamily Physician. It is a interdisciplinarypublication aimed at moving research intoprimary health care practice and practice intoresearch. This includes <strong>the</strong> fields <strong>of</strong> familypractice, primary health care nursing andcommunity pharmacy as well as areas suchas health care delivery, health promotion,epidemiology, public health and medicalsociology <strong>of</strong> interest to a primary health careprovider audience.The journal publishes peer-reviewed quantitativeand qualitative original research,systematic reviews, papers on improving performanceand short reports that are relevantto its primary health care practitioners. For<strong>the</strong> aim, scope, instructions to authors andtemplates for publications see www.rnzcgp.org.nz/journal-<strong>of</strong>-primary-health-care/.JPHC acts as a knowledge refinery to providebusy practitioners with up-to-date knowledgeabout <strong>the</strong> latest evidence and best practice.Continuing pr<strong>of</strong>essional developmentincludes pithy summaries <strong>of</strong> <strong>the</strong> latest evidencesuch as Cochrane Corner, a String <strong>of</strong>PEARLS (Practical Evidence About Real LifeSituations) and Charms & Harms (evidence <strong>of</strong>effectiveness and safety <strong>of</strong> complementaryand alternative medicines). JPHC includesPoumanu (treasures <strong>of</strong> Maori wisdom) andGems <strong>of</strong> NZ Primary Health Care Researchpublished at home and internationally.Evidence can help inform best practice. Howeversometimes <strong>the</strong>re is no evidence availableor applicable for a specific patient with hisor her own set <strong>of</strong> conditions, capabilities,beliefs, expectations and social circumstances.Evidence needs to be placed in context.General practice is an art as well as a science.Quality <strong>of</strong> care lies also with <strong>the</strong> nature <strong>of</strong> <strong>the</strong>clinical relationship, with communication andwith truly informed decision-making. JPHCpublishes viewpoints, commentaries and reflectionsthat explore areas <strong>of</strong> uncertainty onaspects <strong>of</strong> care for which <strong>the</strong>re is no one rightanswer. Debate is stimulated by <strong>the</strong> Back toBack section where two pr<strong>of</strong>essionals present<strong>the</strong>ir opposing views on a topic. There is aregular Ethics column. Letters to <strong>the</strong> Editorare welcomed.While published in New Zealand by <strong>the</strong> RoyalNew Zealand College <strong>of</strong> General Practitioners,much <strong>of</strong> this research has genericimplications. Our Editorial Board comprisesrenowned and active primary care clinicians,clinical and scientific academics and healthpolicy experts with both New Zealand andinternational representation.EditorDr Felicity Goodyear-Smith: Pr<strong>of</strong>essor andGoodfellow Postgraduate Chair, Department<strong>of</strong> General Practice and Primary HealthCare, University <strong>of</strong> Auckland, Auckland, NewZealand; editor@rnzcgp.org.nzDeputy EditorsDr Derelie Mangin: Associate Pr<strong>of</strong>essor,Department <strong>of</strong> Public Health and GeneralPractice, University <strong>of</strong> Otago, Christchurch, NZDr Tony Dowell: Pr<strong>of</strong>essor and Head <strong>of</strong> <strong>the</strong>Department <strong>of</strong> Primary Health Care and GeneralPractice, Wellington School <strong>of</strong> Medicine,University <strong>of</strong> Otago, NZEditorial BoardDr Bruce Arroll: Pr<strong>of</strong>essor and Head <strong>of</strong> <strong>the</strong>Department <strong>of</strong> General Practice & PrimaryHealth Care, University <strong>of</strong> Auckland, NZDr Jo Barnes: Associate Pr<strong>of</strong>essor <strong>of</strong>Pharmacy, School <strong>of</strong> Pharmacy, University <strong>of</strong>Auckland, NZDr Jenny Carryer: Pr<strong>of</strong>essor <strong>of</strong> Nursing,School <strong>of</strong> Health and Social Services, MasseyUniversity, Palmerston North, NZDr Peter Crampton: Dean and Head <strong>of</strong>Campus, Wellington School <strong>of</strong> Medicine andHealth Sciences, University <strong>of</strong> Otago, NZMs Eileen McKinlay: Senior Lecturer inPrimary Health Care, Department <strong>of</strong> PrimaryHealth Care and General Practice, University<strong>of</strong> Otago Wellington, NZDr Barry Parsonson: Psychologist for NZ Ministry<strong>of</strong> Education and International Consultant,UNICEF (Georgia) Training Project for InstitutionalStaff working with disabled childrenDr Shane Reti: Assistant Pr<strong>of</strong>essor, InternationalProgram Director Clinical Informaticsand CEO <strong>of</strong> Clinical Informatics IndustrialResearch, Harvard Medical School, USADr Kurt Stange: Pr<strong>of</strong>essor <strong>of</strong> FamilyMedicine, Case Western Reserve University,Cleveland, OH, USA and Editor, Annals <strong>of</strong>Family MedicineDr Colin Tukuitonga: Associate Pr<strong>of</strong>essorand CEO <strong>of</strong> <strong>the</strong> Ministry <strong>of</strong> Pacific Island Affairs,Wellington, NZSubmissionsPlease send all submissions to:The Editor: editor@rnzcgp.org.nz, or to:The Editorial Assistant—Cherylyn Borlase: editorialassistant@rnzcgp.org.nzaccompanied by a covering letter as outlined at:http://www.rnzcgp.org.nz/journal-<strong>of</strong>-primary-health-care/#coverSubscription and advertising queriesCherylyn Borlase, Publications CoordinatorRNZCGP, PO Box 10440, Wellington 6143, New Zealand; jphcnz@rnzcgp.org.nzJPHC is printed on uncoated, acid-free paper which meets <strong>the</strong> archival requirements <strong>of</strong> ANSI/NISO Z39.48-1992 (Permanence <strong>of</strong> Paper) and is Forest Stewardship Council (FSC)–certifiedwhich meets <strong>the</strong> highest environmentally responsible standards.The Journal <strong>of</strong> Primary Health Care is <strong>the</strong> <strong>of</strong>ficial journal <strong>of</strong> <strong>the</strong> RNZCGP. However, views expressed are not necessarily those <strong>of</strong> <strong>the</strong> College,<strong>the</strong> Editor, or <strong>the</strong> Editorial Board. ©The Royal New Zealand College <strong>of</strong> General Practitioners 2010. All Rights Reserved.264 VOLUME 2 • NUMBER 3 • SEPTEMBER 2010 J OURNAL OF PRIMARY HEALTH CARE