Hoffa's Posterior Fat Pad Syndrome (Liposynovitis ... - Knee Surgeon
Hoffa's Posterior Fat Pad Syndrome (Liposynovitis ... - Knee Surgeon
Hoffa's Posterior Fat Pad Syndrome (Liposynovitis ... - Knee Surgeon
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
The process begins in the patient's room withmarking the leg to be operated on and in particularthe exact point on the knee where the patient feelsthe pain. Then, following a description of theoperation offered the risks, benefits andalternatives a formal consent for the surgery andtype of anaesthesia is obtained.Once the patient is blissfully snoring away atemporary tourniquet is placed at the top of thethigh. The skin is covered with an antisepticsolution and the rest of the patient draped so thatonly the knee is exposed. This is to reduce the risksof postoperative infection. Two small holes aremade either side of the fat pad and a narrowtelescope with the latest high definition HDcamera is placed through one portal and evensmaller instruments placed through the other.Pictures are taken and a video is made for thepatient of the state of the knee before theprocedure, during the procedure and after removalof the fibrosed synovial tag has been achieved.The patient is woken and returned to theatrerecovery for a chat with the recovery nurse. Theythen return to their room and have lunch, get upand walk around. Before being taken home thedressing from theatre is changed and thephysiotherapist on the team checks the patient isself caring, can mobilise and walk up and downstairs.WHAT ELSE SHOULD I KNOW?Patients are reviewed back at the hospital 2 weeksafter surgery to remove sutures, check the wound,show them the pictures of the fibrosed synovial tagand its removal and advise on whether furtherphysiotherapy is necessary. Usually it is not. You arethen seen six weeks after surgery to assess yourprogress.After you go home you should continue exercising tostrengthen and improve the range of motion of yourknee. Although you should be able to get back tolight work (such as a desk job) in about a week, itmay take longer (2 to 3 weeks) to start doing moreactive work..Don't engage in strenuous activities like jogging,running, or active sports until your surgeon says so.Avoid twisting your knee - if you have to turn whilestanding, do so by stepping with your feet and notsimply by turning at the waist.Hoffa’s <strong>Posterior</strong><strong>Fat</strong> <strong>Pad</strong><strong>Syndrome</strong>(<strong>Liposynovitis</strong>Prepatellaris)Your surgeon should see you after surgery to discussthe findings and confirm what you can and cannotdo following the treatment.Further copies of this brochure can be found at:www.JohnHardy.co.ukPhone 0044 (0)117 3171793Fax 0044 (0)117 973 8676
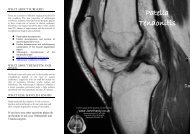
HOFFA’SPOSTERIOR FATPAD SYNDROMEINTRODUCTIONThe knee joint is formed by the lower end of thethigh bone (femur) and the upper end of the shinbone (tibia). The knee cap (patella) sits in the tendonof the quadriceps muscle which is connected to thetibia by the patella tendon. The fat pad of Hoffa liesbehind the patella tendon suspended by theinfrapatella ligament. A medial and a lateral extensionof fat lay either side of the base of the anteriorcruciate ligament (Gallagher J et al. 2005). Thecondition goes frequently unrecognised by manydoctors. It is called variously <strong>Hoffa's</strong> <strong>Posterior</strong> <strong>Fat</strong><strong>Pad</strong> <strong>Syndrome</strong> (HPFPS), <strong>Hoffa's</strong> <strong>Syndrome</strong> or<strong>Liposynovitis</strong> Prepatellaris. It is one of the causes ofthe umbrella diagnosis “anterior knee pain”.WHAT CAUSES IT?The condition is caused by chronicimpingement of the one of the extensions of fatpad either side of the base of the anteriorcruciate ligament in the knee (yellow arrow).After a time the fat becomes scarred by thispinching (green arrow) leading to high pressurebetween the viscoelastic hyaline cartilage thatcovers the joint surfaces of the bone. Theanalogy is a stone in the shoe causing a painthen a blister then an ulcer as the patient walkson with the stone under the heel. Once thescarred fat flips into the joint the patientexperiences a sharp catch in the front of theknee. Patients are good at pin pointing the placewhere this happens. This causes slow degeneratechanges to the hyaline cartilage of the tibia andfemur (blue arrow) leading to a localisedosteoarthritis in the knee.The Consultant in Orthopaedics and Trauma withexperience in arthroscopic surgery of the kneeshould have taken a history, examined you,performed investigations like MRI and helped youcome to a decision on the best treatment for youunder the circumstances of your current medicalcondition. MRI helps determine the presence of atear of the ligamentum mucosum (Saddik D et al2004), oedema or fibrosis in the fat pad and thepresence or absence of chondromalacia orosteoarthritis (Magi M et al. 1991).The purpose of this leaflet is to explain theconservative treatments and surgical options torelieve your symptoms. The treatment aim is toget the fibrosed synovial tag out of thearticulating surfaces of the joint to relieve thepain and prevent the degenerative change.CONSERVATIVE TREATMENTIf your condition is acute (six weeks) with noevidence of cartilage damage (chondromalacia) thena course of pain killers physical therapy, patellataping and orthotics should be considered. Thepatella taping works by either changing the forcesinduced by the muscles (Cowan SM et al. 2002), byoff loading the extension of the fat pad or by anothermechanism yet unknown. Patella taping once taughtwill be repeatable if the patient takes a digitalphotograph of the pattern of taping that has workedin their case. Taping paradoxically works in differentdirections for different people.SURGICAL TREATMENTIf at least six weeks of conservative treatment hasfailed to cause improvement then surgery should beconsidered. This is Day Case key hole surgery.“My advice to patients is that they should notaccept an operation from a surgeon who has notbeen through this extensive process of assessmentand consent of the individual”.PREASSESSMENTDepending on other underlying conditions you mayrequire other types of tests before surgery such as anECG (electrocardiogram), blood tests and tests toexclude MRSATHE OPERATIONThe operation is arthroscopy of the knee (keyholesurgery) and partial excision of the fat pad(removing only the scarred bit) with or withoutchondroplasty (repairing or removing any looseflaps of cartilage).