Stroke thrombolysis guideline extended age and treatment window
Stroke thrombolysis guideline extended age and treatment window
Stroke thrombolysis guideline extended age and treatment window
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
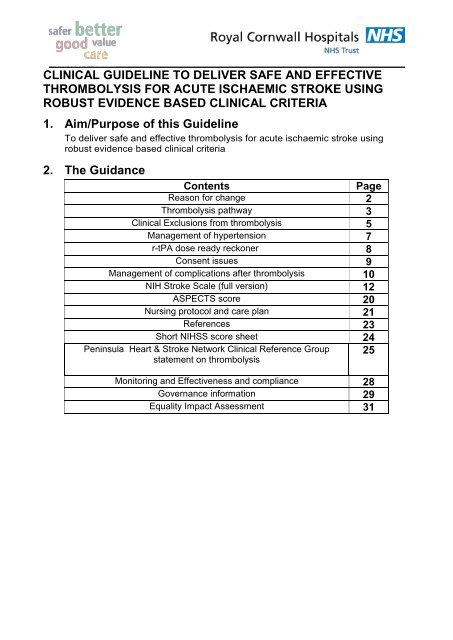
CLINICAL GUIDELINE TO DELIVER SAFE AND EFFECTIVETHROMBOLYSIS FOR ACUTE ISCHAEMIC STROKE USINGROBUST EVIDENCE BASED CLINICAL CRITERIA1. Aim/Purpose of this GuidelineTo deliver safe <strong>and</strong> effective <strong>thrombolysis</strong> for acute ischaemic stroke usingrobust evidence based clinical criteria2. The GuidanceContentsP<strong>age</strong>Reason for change 2Thrombolysis pathway 3Clinical Exclusions from <strong>thrombolysis</strong> 5Man<strong>age</strong>ment of hypertension 7r-tPA dose ready reckoner 8Consent issues 9Man<strong>age</strong>ment of complications after <strong>thrombolysis</strong> 10NIH <strong>Stroke</strong> Scale (full version) 12ASPECTS score 20Nursing protocol <strong>and</strong> care plan 21References 23Short NIHSS score sheet 24Peninsula Heart & <strong>Stroke</strong> Network Clinical Reference Groupstatement on <strong>thrombolysis</strong>Monitoring <strong>and</strong> Effectiveness <strong>and</strong> compliance 28Governance information 29Equality Impact Assessment 3125
Reason for changeECAS III AND IST-3 <strong>and</strong> an updated Cochrane review (available at www.ist3.com) haveled to a change in guidance across all hospitals in the SW peninsula (see Peninsula Heart& <strong>Stroke</strong> Network Clinical Reference Group statement on <strong>thrombolysis</strong>, appendix 2)The main changes are:1. NO UPPER AGE LIMIT FOR PATIENTS PRESENTING WITHIN 3 HOURS.2. PATIENTS 18-80y CAN BE TREATED UP TO 4.5 HOURS3. PATIENTS UNDER 80 PRESENTING WITHIN 4.5-6 HOURS ARE LIKELY TO HAVEA SMALLER BENEFIT BUT UNLIKELY TO HAVE GREATER RISK OFDEATH/BLEEDING– THESE DECISIONS SHOULD BE MADE ON CASE-BY-CASEBASIS BY THROMBOLYSING DOCTOR4. PATIENTS OVER 80 DO NOT BENEFIT IF TREATED AFTER 3 HOURS5. LARGER STROKES (ie HIGHER NIHSS AND EARLY ISCHAEMIC CHANGES) MAYALSO BENEFIT IF TREATED WITHIN 3 HOURSIn summary18-80y Over 80yWithin 3h YES YES3-4.5h YES NO4.5-6h MAY BENEFIT NOThe number needed to treat declines rapidly over time. Patients benefit the most if treatedwithin the first hour.DO NOT DELAY TREATMENT BECAUSE THE TIME WINDOW HAS BEENEXTENDED.6. PATIENTS ON WARFARIN CAN NOW BE LYSED IF INR ≤1.77. DIABETES MELLITUS AND OLD STROKE IS NO LONGER A CONTRA-INDICATION<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 2 of 31
RCHT STROKE THROMBOLYSIS PATHWAYPRE-HOSPITAL<strong>Stroke</strong> eligible for <strong>thrombolysis</strong>:• Positive FAST (Face, Arm <strong>and</strong> Speech Test)• Age 18 or older• Symptoms noted on waking exclude <strong>thrombolysis</strong>• Symptom onset to <strong>thrombolysis</strong> within 6h• No seizure at onsetCheck BM, confirm time of onset, transport to ED RCHT, with NOK <strong>and</strong> list of pills ifavailable. Pre-alert ED – ensure name, DOB <strong>and</strong> AFFECTED SIDE includedEMERGENCY DEPARTMENT• Confirm stroke using ROSIER scale• Book CT on MAXIMS – ensure side affected is clear on request• P<strong>age</strong> acute stroke doctor (In hours bleep 2866, out of hours Geriatrician on call)• Ring 4444 to alert radiographer/stroke nurse/stroke ward• Transport patient straight to CT on arrival for urgent CT head• Confirm time of onset• Brief medical history <strong>and</strong> examination, estimate weight• BP both arms, repeat higher arm BP after 15 minutes (manual cuff not dynamap)• iv access x2• Urgent bloods = FBC, U&E, clotting, G&S (INR if on warfarin), lipids, glucose• ECG (<strong>and</strong> CXR if needed)ACUTE STROKE DOCTOR (In hours bleep 2866,out of hours Geriatrician on call)• Confirm inclusion <strong>and</strong> exclusion criteria• Perform NIHSS examination (National Institute Health <strong>Stroke</strong> Scale)• Man<strong>age</strong> high BP as per protocol• Inform clinical site coordinator of need for critical care bed (bleep 2634)• Keep record of timesCT SCANNERRadiographer performs scan <strong>and</strong> informs on call radiologist to report scan usingASPECTS score<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 3 of 31
DECISION TO THROMBOLYSE• Repeat NIHSS to ensure not rapidly improving• Do not delay while waiting for bloods (unless on warfarin or on chemo or knownhaematological disorder)• Decision to thrombolyse taken by thrombolysing doctor• Obtain verbal consent if possible• Calculate dose using ready reckoner, give bolus in 10ml syringe over 1-2minutes then infusion over 1 hour using 50ml syringe driver• Start <strong>treatment</strong> in ED <strong>and</strong> organise bed on HDUMONITOR FOR COMPLICATIONS• Watch for signs of neurological deterioration, bleeding, anaphylaxis• Repeat NIHSS at 2h• Manual BP, pulse, GCS, respiratory rate, temperature, SaO2 every 15 min for2h, then every 30 min for 6 h, then every hour for 18h• Maintain BP Systolic
CLINICAL EXCLUSIONS FROM THROMBOLYSISDo not give <strong>thrombolysis</strong> if you have ticked any ‘YES’ boxesFROM THE HISTORYYESNOTime of onset unknownAwoke with symptomsSeizure at onsetKnown bleeding diathesisArterial puncture at a non-compressible site, or lumbarpuncture, within the last 7 daysMajor surgery within the last 14 daysGastrointestinal or urinary tract haemorrh<strong>age</strong> within 21 daysHead injury, intracranial surgery or stroke within the last 3monthsAny history of intracranial haemorrh<strong>age</strong>, brain tumour,intracranial AVM or aneurysmTIME OF ONSETWithin 3h – no upper <strong>age</strong> limit3 to 4.5h – can treat if 18-80, patients over 80y do not benefit4.5 to 6h – patients 18-80 may benefit – needs decision by thrombolysing doctorANTICOAGULANTSCurrent warfarin <strong>treatment</strong> is not an exclusion if the INR ≤1.7Current heparin <strong>treatment</strong> is not an exclusion if the APTT ratio is less than 1.2Full dose (but not low dose/prophylactic) LMWH is an exclusionRivaroxaban/Dabigatran – if a patient is on these <strong>treatment</strong>s, 24h or 12h respectivelyshould elapse before a parenteral anticoagulant is given. This excludes these patientsfrom <strong>thrombolysis</strong> for stroke.PREGNANCYPregnancy or women who are post-partum – r-tPa is unlicensed for use in pregnancy.It should not be withheld in pregnant patients with ischaemic stroke, but becauseexperience is limited, risks <strong>and</strong> benefits must be carefully weighed <strong>and</strong> should bediscussed with on-call obstetricianCHEMOTHERAPYSome chemotherapy <strong>age</strong>nts may be relative contra-indications to <strong>thrombolysis</strong>. Orpatients may be cytopaenic. If patient on chemotherapy drugs please ensure bloodsnormal first <strong>and</strong> check with oncology or haematology before giving lysisCHILDRENAlteplase is not licensed for
ON INITIAL ASSESSMENT YES NOComa (GCS 140or BP>180/105 having received more than 2 doseslabetolol (see man<strong>age</strong>ment of hypertension p<strong>age</strong> 7)Capillary glucose
MANAGEMENT OF HYPERTENSION IN POTENTIAL THROMBOLYSIS PATIENTSBP should be recorded in both arms initially to exclude aortic dissection <strong>and</strong> CT thoraxconsidered. The arm with the highest reading should be used thereafter. Take anotherBP in this arm after 15 minutes.USE MANUAL CUFF NOT DYNAMAP1. If diastolic BP >140 on both readingsPatient is NOT eligible for <strong>thrombolysis</strong> even if other inclusion criteria met2. If systolic BP >220 <strong>and</strong>/or diastolic BP 121-140 on both readingsGive labetolol 10mg iv over 1-2 minutesRepeat as necessary at same or double dose at 10 minute intervals to bring BP below180/105 (maximum dose cumulative dose is 200mg, labetolol can be given 6 hourlythereafter as needed)Alternatively, after the bolus of labetolol an infusion of 2-8 mg/min can be initiated. If morethan 2 doses of labetolol required to control BP, patient is NOT eligible for <strong>thrombolysis</strong>even if other inclusion criteria met.If asthma, cardiac failure or > 1 st degree heart block, use isoket infusion (2-10 mg/hr)3. If systolic BP 180-220 or diastolic BP 105-120 on both readingsIf patient is otherwise not eligible for <strong>thrombolysis</strong> monitor BP but do not interveneIf patient is otherwise eligible for <strong>thrombolysis</strong>, man<strong>age</strong> as per (2)4. If systolic BP
RtPA DOSE READY RECKONERAlteplase, Recombinant tissue plasminogen activator(Actilyse® Boehringer Ingelheim)• Unless the patient or companion knows their recent weight, estimate it to thenearest 5 kg• The total dose of rt-PA is 0.9 mg/kg or 90 mg, whichever is the lesser (Column 3)• Make up one or two vials of rt-PA using the 50 ml diluent in each drug pack, makinga solution of 1 mg/ml rt-PA• Draw up <strong>and</strong> give 10% as a bolus over 1-2 minutes (Column 4), using a 10 mlsyringe• Draw up the remaining 90% (the ‘infusion dose’, Column 5) into 1 or 2 50mlsyringes <strong>and</strong> set up the 50ml syringe driver (IVAC) with the corresponding infusionrate in mls/hr.• Do not give the cardiac dose• Do not give more than 90 mg1 2 3 4 5Estimate ofpatientsweight (kg)EquivalentImperialweightBolus dose(mls)given over 1-2minutesInfusiondose (mls) =infusion ratein mls/hrTotal dose(mg at 1mg/ml)OnevialTwovials45 7 st 1 lb 4 36 4050 7 st 12 lb 5 40 4555 8 st 9 lb 5 44 4960 9 st 6 lb 5 49 5465 10 st 3 lb 6 52 5870 11 st 0 lb 6 57 6375 11 st 11 lb 7 60 6780 12 st 8 lb 7 65 7285 13 st 5 lb 7 69 7690 14 st 2 lb 8 73 8195 14 st 13 lb 8 77 85≥100 15 st 10 lb 9 81 90<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 8 of 31
ISSUES AROUND CONSENTInformation for patients / relatives before giving <strong>thrombolysis</strong>Thrombolysis with r-tPA is a licensed <strong>treatment</strong> for acute ischaemic stroke, sowritten consent is not required. If possible there should be agreement from the patient <strong>and</strong>/ or relative.When the patient cannot agree because of their impairments <strong>and</strong> no relative is available,then <strong>treatment</strong> can still be given if it is judged to be in the best interests of the patient. Anyexplanation might include:• There has been a significant stroke caused by a blocked artery preventing bloodfrom getting to a part of the brain <strong>and</strong> causing permanent dam<strong>age</strong>. With or without<strong>treatment</strong> there may be some recovery or things could get worse. <strong>Stroke</strong> is fatal inabout a third of people.• Only one <strong>treatment</strong> has been shown to prevent dam<strong>age</strong> to the brain. This <strong>treatment</strong>dissolves the blood clot blocking the artery <strong>and</strong> allows blood to get back to the brain.It only works if given quickly after the stroke starting <strong>and</strong> the benefit is greater thesooner it is given• There is a slight increased risk of death within the first week (8.9 vs 6.4%), mostlydue to fatal intracranial bleeding (3.6 vs 0.6%). But after the first week there is alower chance of death (11.5 vs 13.6%), so several months later there is nodifference in chance of death overall.• The chances of being alive <strong>and</strong> independent (Rankin score 0-2) several months laterare higher,% chance of thisoutcome if lysed% chance ofthis outcome ifnot lysedAbsolute benefit –number of extrapatients with thisgood outcome per1000 patientstreatedif treated within 6h 46.3% 42.1% 42if treated within 3h 40.7% 31.7% 90If treated 3-6h 47.5% 45.7% 18<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 9 of 31
MANAGEMENT OF COMPLICATIONS AFTER THROMBOLYSISBP commonly drops after initiation of <strong>thrombolysis</strong>, not necessarily due to bleeding. If thishappens give iv fluid bolus.Bleeding, by process of de-fibrination, is more common than with heparin (around 3%)Intracranial bleedingShould be suspected if there is neurological deterioration, new headache, fall in consciouslevel, acute hypertension, seizure, nausea or vomitingInitial actionStop infusion of r-tPA, repeat NIHSS, commence iv saline if neededArrange urgent CT scanCheck FBC, full coagulation screen, check blood sent for G&SIf CT scan shows bleeding• Is haemorrh<strong>age</strong> petechial? If so it is unlikely anything other than stopping r-tPA will beneeded. Continue to observe patient closely• Is haemorrh<strong>age</strong> parenchymal?Give 20% mannitol 200ml stat (dose may be repeated)Consider tranexamic acid 10 mg/kg IV <strong>and</strong> 10 units cryoprecipitateFurther advice is available via the intranet anti-coagulation <strong>guideline</strong>s <strong>and</strong> from the on-callgeriatrician <strong>and</strong> Consultant HaematologistConsult neurosurgeon regarding possible transfer for haematoma evacuationIf CT scan shows no bleedingRecheck patient for other causes of deterioration eg recurrent ischaemic stroke, sepsis,seizure, metabolic derangement, extracranial bleedingExtracranial bleedingShould be suspected if there is shock, drop in BP, evidence of blood loss – although ahigh index of suspicion is needed as blood loss may not be obvious.Initial actionStop infusion of r-tPACheck FBC, full coagulation screen, check blood sent for G&S <strong>and</strong>/or arrange cross matchdepending on situationCommence iv saline or blood transfusion depending on situationIf patient fails to respond to simple measures or there is severe haemorrh<strong>age</strong>, considertranexamic acid 10 mg/kg IV <strong>and</strong> 10 units cryoprecipitateFurther advice is available from intranet, on call geriatrician <strong>and</strong> haematologist as above.AnaphylaxisAnaphylactic reactions to r-tPA can occur but are rare. If an urticarial rash, peri-orbitalswelling or tongue swelling occur, the r-tPA should be stopped <strong>and</strong> the patient reviewed bya doctor urgently.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 10 of 31
NIH STROKE SCALE – full version <strong>and</strong> master copy – please record patient scores on quick version(see p<strong>age</strong> 23)INSTRUCTION SCALE DEFINITION SCORE11a. Level of Consciousness:The investigator must choose a response,even if a full evaluation is prevented bysuch obstacles as an endotracheal tube,langu<strong>age</strong> barrier, orotracheal trauma/b<strong>and</strong><strong>age</strong>s. A 3 is scored only if the patientmakes no movement (other than reflexiveposturing) in response to noxiousstimulation.1b. LOC Questions:The patient is asked the month <strong>and</strong> his/her<strong>age</strong>. The answer must be correct - there isno partial credit for being close. Aphasic<strong>and</strong> stuporous patients who do notcomprehend the questions will score 2.Patients unable to speak because ofendotracheal intubation, orotrachealtrauma, severe dysarthria from any cause,langu<strong>age</strong> barrier or any other problem notsecondary to aphasia are scored 1. It isimportant that only the initial answer begraded <strong>and</strong> that the examiner not “help” thepatient with verbal or non-verbal cues.1c. LOC Comm<strong>and</strong>s:The patient is asked to open <strong>and</strong> close theeyes <strong>and</strong> then to grip <strong>and</strong> release thenonparetic h<strong>and</strong>. Substitute another onestep comm<strong>and</strong> if the h<strong>and</strong>s cannot be used.Credit is given if an unequivocal attempt ismade but not completed due to weakness.If the patient does not respond tocomm<strong>and</strong>, the task should be demonstratedto them (pantomime) <strong>and</strong> score the result(i.e., follows none, one, or two comm<strong>and</strong>s).Patients with trauma, amputation, or otherphysical impediments should be givensuitable one-step comm<strong>and</strong>s. Only the firstattempt is scored.2. Best Gaze:Only horizontal eye movements will betested. Voluntary or reflexive(oculocephalic) eye movements will bescored but caloric testing is not done. If thepatient has a conjugate deviation of theeyes that can be overcome by voluntary orreflexive activity, the score will be 1. If apatient has an isolated peripheral nerveparesis (CN III, IV, OR VI) score a 1. Gazeis testable in all aphasic patients. Patientswith ocular trauma, b<strong>and</strong><strong>age</strong>s, preexistingblindness or other disorder of visual acuityor fields should be tested with reflexivemovements <strong>and</strong> a choice made by the<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 11 of 310 = Alert; keenly responsive.1 = Not alert, but rousable by minorstimulation to obey, answer, or respond.2 = Not alert, requires repeatedstimulation to attend, or is obtunded <strong>and</strong>requires strong or painful stimulation tomake movements (not stereotyped).3 = Coma; Responds only with reflexmotor or autonomic effects, or totallyunresponsive, flaccid, areflexic.0 = Answers both questions correctly.1 = Answers one question correctly.2 = Answers neither question correctly.0 = Performs both tasks correctly.1 = Performs one task correctly.2 = Performs neither task correctly.0 = Normal1 = Partial gaze palsy. This score isgiven when gaze is abnormal in one orboth eyes, but where forced deviation ortotal gaze paresis are not present.2 = Forced deviation, or total gazeparesis not overcome by theoculocephalic manoeuvreSCORE2----------- ---------------------- ---------------------- ---------------------- -----------
investigator. Establishing eye contact <strong>and</strong>then moving about the patient from side toside will occasionally clarify the presence ofa gaze palsy.3. Visual:Visual fields (upper <strong>and</strong> lower quadrants)are tested by confrontation, using fingercounting or visual threat as appropriate.Patient must be encour<strong>age</strong>d, but if theylook at the side of the moving fingersappropriately, this can be scored as normal.If there is unilateral blindness orenucleation, visual fields in the remainingeye are scored. Score 1 only if a clear-cutasymmetry, including quadrantanopia isfound. If patient is blind from any causescore 3. Double simultaneous stimulationis performed at this point. If there isextinction patient receives a 1 <strong>and</strong> theresults are used to answer question 11.4. Facial Palsy:Ask, or use pantomime to encour<strong>age</strong> thepatient to show teeth or raise eyebrows orclose eyes. Score symmetry of grimace inresponse to noxious stimuli in the poorlyresponsive or non-comprehending patient.If facial trauma/b<strong>and</strong><strong>age</strong>s, orotracheal tube,tape, or other physical barrier obscures theface, these should be removed to the extentpossible.5&6. Motor Arm <strong>and</strong> Leg:The limb is placed in the appropriateposition: extend the arms 90 degrees (ifsitting) or 45 degrees (if supine) <strong>and</strong> the leg30 degrees (always tested supine). Drift isscored if the arm falls before 10 seconds orthe leg before 5 seconds. The aphasicpatient is encour<strong>age</strong>d using urgency in thevoice <strong>and</strong> pantomime but not noxiousstimulation. Each limb is tested in turn,beginning with the nonparetic arm. Only inthe case of amputation or joint fusion at theshoulder or hip may the score be “9” <strong>and</strong>the examiner must clearly write theexplanation for scoring as a “9”.0 = No visual loss.1 = Partial hemianopia.2 = Complete hemianopia.3 = Bilateral hemianopia (blind includingcortical blindness). ----------- -----------0 = Normal symmetrical movement.1 = Minor paralysis (flattened nasolabialfold, asymmetry on smiling).2 = Partial paralysis (total or near totalparalysis of lower face).3 = Complete paralysis (absence of facialmovement in the upper <strong>and</strong> lower face).Arm0 = No drift, arm holds 90 (or 45) degreesfor full 10 seconds.1 = Drift, arm holds 90 (45) degrees, butdrifts down before full 10 seconds; doesnot hit bed or other support.2 = Some effort against gravity, limbcannot get to or maintain (if cued) 90 (or45) degrees, drifts down to bed, but hassome effort against gravity.3 = No effort against gravity, arm falls.4 = No movement.9 = Amputation, joint fusion -explain:5a = Right Arm----------- ---------------------------------<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 12 of 315b = Left ArmLeg0 = No drift, leg holds 30 degrees positionfor full 5 seconds.1 = Drift, leg falls by the end of the 5second period but does not hit bed.2 = Some effort against gravity, leg fallsto bed by 5 seconds, but has some effortagainst gravity.3 = No effort against gravity, leg falls tobedimmediately.4 = No movement.9 = Amputation, joint fusion -explain:----------------------
6a = Right Leg6b = Left Leg--------------------------------------------7. Limb Ataxia:This item is aimed at finding evidence of aunilateral cerebellar lesion. Test with eyesopen. In case of visual defect, ensuretesting is done in intact visual field. Thefinger-nose-finger <strong>and</strong> heel-shin tests areperformed on both sides, <strong>and</strong> ataxia isscored only if present out of proportion toweakness. Ataxia is absent in the patientwho cannot underst<strong>and</strong> or is hemiplegic.Only in the case of amputation or jointfusion may the item be scored “9”, <strong>and</strong> theexaminer must clearly write the explanationfor not scoring. In case of blindness, testby touching nose from <strong>extended</strong> armposition.8. Sensory:Sensation or grimace to pinprick whentested, or withdrawal from noxious stimulusin the obtunded or aphasic patient. Onlysensory loss attributed to stroke is scoredas abnormal <strong>and</strong> the examiner should testas many body areas [arms (not h<strong>and</strong>s),legs, trunk, face] as needed to accuratelycheck for hemisensory loss. A score of 2,“severe or total”, should only be given whena severe or total loss of sensation can beclearly demonstrated. Stuporous <strong>and</strong>aphasic patients will therefore probablyscore 1 or 0. The patient with brainstemstroke who has bilateral loss of sensation isscored 2. If the patient does not respond<strong>and</strong> is quadriplegic, score 2. Patients incoma (item 1a=3) are arbitrarily given a 2on this item.0 = Absent.1 = Present in one limb.2 = Present in two limbs.0 = Normal; no sensory loss.1 = Mild to moderate sensory loss; patientfeels pinprick is less sharp or is dull onthe affected side; or there is a loss ofsuperficial pain with pinprick but patient isaware he/she is being touched.2 = Severe to total sensory loss; patient isnot aware of being touched.----------- -----------9. Best Langu<strong>age</strong>:A great deal of information aboutcomprehension will be obtained during thepreceding sections of the examination. Thepatient is asked to describe what ishappening in the attached picture, to namethe items on the attached list of sentences.Comprehension is judged from responseshere as well as to all of the comm<strong>and</strong>s inthe preceding general neurological exam. Ifvisual loss interferes with the tests, ask thepatient to identify objects placed in theh<strong>and</strong>, repeat, <strong>and</strong> produce speech. Theintubated patient should be asked to write.The patient in coma (question 1a = 3) willarbitrarily score 3 on this item. The<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 13 of 310 = No aphasia, normal.1 = Mild to moderate aphasia; someobvious loss of fluency or facility ofcomprehension, without significantlimitation on ideas expressed or form ofexpression. Reduction of speech <strong>and</strong>/orcomprehension, however, makesconversation about provided materialdifficult or impossible. For example, inconversation about provided materialsexaminer can identify picture or namingcard from patient’s response.2 = Severe aphasia; all communication isthrough fragmentary expression; greatneed for inference, questioning, <strong>and</strong>guessing by the listener. Range of----------- -----------
examiner must choose a score in thepatient with stupor or limited cooperationbut a score of 3 should be used only if thepatient is mute <strong>and</strong> follows no one stepcomm<strong>and</strong>s.10. Dysarthria:If the patient is thought to be normal, anadequate sample of speech must beobtained by asking patient to read or repeatwords from the attached list. If the patienthas severe aphasia, the clarity ofarticulation of spontaneous speech can berated. Only if the patient is intubated or hasother physical barrier to producing speechmay the item be scored “9", <strong>and</strong> theexaminer must clearly write an explanationfor not scoring. Do not tell the patient whyhe/she is being tested.11. Extinction <strong>and</strong> Inattention(formerly Neglect)Sufficient information to identify neglectmay be obtained during the prior testing. Ifthe patient has severe visual losspreventing visual double simultaneousstimulation, <strong>and</strong> the cutaneous stimuli arenormal, the score is normal. If the patienthas aphasia but does appear to attend toboth sides, the score is normal. Thepresence of visual spatial neglect oranosagnosia may also be taken asevidence of neglect. Since neglect isscored only if present, the item is neveruntestable.information that can be exchanged islimited; listener carries burden ofcommunication. Examiner cannot identifymaterials provided from patient response.3 = Mute, global aphasia; no usablespeech or auditory comprehension.0 = Normal.1 = Mild to moderate; patient slurs at leastsome words <strong>and</strong>, at worst, can beunderstood with some difficulty.2 = Severe; patient’s speech is so slurredas to be unintelligible in the absence of orout of proportion to any dysphasia, or ismute/anarthric.9 = Intubated or other physical barrier -explain:0 = No abnormality.1 = Visual, tactile, auditory, spatial, orpersonal inattention or extinction tobilateralsimultaneous stimulation in one of thesensory modalities.2 = Profound hemi-inattention or hemiinattentionto more than one modality.Does not recognize own h<strong>and</strong> or orientsto only one side of space.----------- ---------------------- -----------TotalMaxscore 42TotalMaxscore 42<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 14 of 31
<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 15 of 31
<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 16 of 31
<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 17 of 31
ASPECTS scoreThis is a topographic score for dividing middle cerebral artery territory into 10 regions. It iscalculated from 2 st<strong>and</strong>ard axial CT cuts, one at the level of the basal ganglia <strong>and</strong> one atthe corona radiate / centrum semiovale level. Subcortical structures are allotted 3 points<strong>and</strong> cortical structures 7 points.For each of these 10 areas a point is subtracted if there is evidence of ischemic dam<strong>age</strong>there (eg reduced attenuation, loss of grey-white matter differentiation, focal swelling).A scan with no ischaemia in the MCA territory would score 10 <strong>and</strong> a scan with diffuseinvolvement of all MCA territory would score 0.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 18 of 31
An ASPECTS score 7 or less is a relative contra-indication to <strong>thrombolysis</strong>, with increasedrisk of haemorrh<strong>age</strong>; in this instance consider carefully other factors that may influence thedecision to treat or not to treatM1 = anterior MCA cortex, M2 = MCA cortex lateral to insular ribbonM3 = posterior MCA cortex, M4, M5, M6 are anterior, lateral <strong>and</strong> posterior MCA territoriesimmediately superior to M1, M2, M3C = caudate, L = lentiform, IC = internal capsule, I = insular ribbon<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 19 of 31
Nursing ProtocolNursing Care Following Thrombolysis for <strong>Stroke</strong>1. Patient to be nursed in identified bed space that allows for continuous observation.2. Oxygen, Suction, Cardiac Monitor, Sphygmomanometer, O2 Saturation machine should beavailable at the bed side. Capillary blood glucose machine, Anaphylaxis box should beeasily accessible.3. Initiate post administration <strong>thrombolysis</strong> care plan on arrival4. Perform patient observations as indicated <strong>and</strong> record a baseline ECG5. If there are any concerns, medical review is essential. Report, review, document <strong>and</strong>increase frequency of observations accordingly.6. Pyrexia > 37°C should be treated with PR or PO Paracetamol (1g 4-6 hourly. No morethan 4g in 24 hours)7. If haemorrh<strong>age</strong> is suspected, report immediately <strong>and</strong> arrange for urgent medicalreview. Send urgent FBC, clotting <strong>and</strong> group <strong>and</strong> save8. If anaphylaxis is suspected (Tachypnoea, dyspnoea, tachycardia, swelling, rash) Stopinfusion <strong>and</strong> employ anaphylaxis protocol. Arrange for urgent medical review orperform a crash call (2222)if required9. Avoid catheterisation for 24 hours following <strong>thrombolysis</strong> infusion to minimise the risk oftrauma <strong>and</strong> bleeding. If essential, consult with medical team.10. Do not insert naso gastric tubes for 24 hours post <strong>thrombolysis</strong> infusion to minimise therisk of trauma <strong>and</strong> bleeding11. IM injections should be avoided for 48 hours post <strong>thrombolysis</strong> infusion to minimise therisk of excessive bruising12. Avoid giving heparin / warfarin. Refer to medical staff before commencing any anticoagulant or antiplatelet therapy (only given if CT at 24h shows no bleeding).<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 20 of 31
Observations following administration of<strong>thrombolysis</strong> for strokeManual BP, Pulse, Temperature, Respirations,GCS <strong>and</strong> Oxygen Saturations (MEWS Score – Refer to localGuidelines)Every 15 minutes for 2 hoursEvery 30 minutes for 6 hoursHourly for 18 hoursMaintain BP < Systolic 180 / Diastolic 105Temperature not to exceed 37°C.Observe for signs of raised intracranial pressure or intracranialbleeding• Unequal pupils• Sudden drop in GCS• Onset of drowsiness• Onset of nausea, vomiting (photophobia)• Rising BP <strong>and</strong> falling pulse<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 21 of 31
ReferencesThrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic <strong>Stroke</strong>NEJM 2008; 359: 3517-29The benefits <strong>and</strong> harms of intravenous <strong>thrombolysis</strong> with recombinant tissue plasminogenactivator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): ar<strong>and</strong>omised controlled trialLancet 2012 ;379 :2352-63Recombinant tissue plasminogen activator for acute ischaemic stroke: an updatedsystematic review <strong>and</strong> meta-analysisLancet 2012; 379: 2364-72NICE Guidance TA 122 - Alteplase for the <strong>treatment</strong> of acute ischaemic strokeNational <strong>Stroke</strong> Strategy, Department of Health 2007Validity <strong>and</strong> reliability of a quantitative computed tomography score in predicting outcomeof hyperacute stroke before thrombolytic therapyLancet 2000; 355:1670-1674Use of the Alberta <strong>Stroke</strong> Program Early CT Score (ASPECTS) for Assessing CT Scans inPatients with Acute <strong>Stroke</strong>Am J Neuroradiol 2001; 22:1534–42Importance of Early Ischemic Computed Tomography Changes Using ASPECTS inNINDS rtPA <strong>Stroke</strong> Study<strong>Stroke</strong> 2005; 36:2110-15<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 22 of 31
Short NIHSS scoring sheetThis is master copy – patient packsinclude this sheet which should be filedin medical notes with completedinclusion/exclusion checklistNational Institute for Health <strong>Stroke</strong> Scale (NIHSS)REFER TO LAMINATED FULL GUIDANCE FOR SCORINGDate <strong>and</strong> Time1a. LOCScore 0-31b. LOC – Response to QuestionsScore 0-21c. LOC – Response to Comm<strong>and</strong>sScore 0-22. Best gazeScore 0-23. Visual fieldsScore 0-34. Facial palsyScore 0-35. Right Arm motorScore 0-4 or X if untestable6. Left Arm motorScore 0-4 or X if untestable7. Right Leg motorScore 0-4 or X if untestable8. Left leg motorScore 0-4 or X if untestable9. AtaxiaScore 0-2 or X if untestable10. SensoryScore 0-211. Best langu<strong>age</strong>Score 0-312. DysarthriaScore 0-2 or X if untestable13. Neglect/InattentionScore 0-2Total Score (0-42)Score Score Score Score<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 23 of 31
Peninsula Heart & <strong>Stroke</strong> Network Clinical Reference GroupAugust 2012Statement on Thrombolysis for Acute Ischaemic <strong>Stroke</strong>1. Intravenous AlteplaseWith the publication of IST3 in May 2012, linked to an updated Cochrane Review (both available atwww.ist3.com) the indications for rtPA (alteplase) <strong>treatment</strong> for acute ischaemic stroke within 6hours of known onset were considered at the June PH&SN Clinical Reference Group (CRG)meeting. The updated 4 th Edition of the RCP’s National Clinical Guidelines for <strong>Stroke</strong> will bepublished in September 2012 also taking account of the new evidence <strong>and</strong> systematic review.Summary of main IST3 findings3035 patients were r<strong>and</strong>omised between rtPA or control at up to 6 hours after onset. 95% ofpatients were outside the prevailing EU licence at the time, <strong>and</strong> 53% were above the <strong>age</strong> of 80.Within 3 hours, the large majority of patients were over 80, whereas beyond 4.5 hours the majoritywere younger than 80. 30% of patients had atrial fibrillation, 43% had a TACI syndrome.Safety: the overall incidence of symptomatic intracranial haemorrh<strong>age</strong> (ICH) in IST3 was 7%, verysimilar to the reported incidence in the SITS-MOST audit dataset. The risk of intracerebralhaemorrh<strong>age</strong> did not increase with time from onset, or with <strong>age</strong>. The excess of ICH wasresponsible for an excess early mortality with rtPA (within 7 days) of 11% versus 7% with control.Between 7 days <strong>and</strong> 6 months there was an excess of deaths in the control group such that by 6months, mortality between the two groups was entirely equivalent at 27%.Efficacy: the trial’s primary endpoint was the proportion of patients ‘alive <strong>and</strong> independent’ at 6months (an Oxford H<strong>and</strong>icap Scale score [OHS; roughly equivalent to the modified Rankin Scale]of 0-2). This proportion was higher with rtPA, but not statistically significant – 37% with rtPAversus 35% with control. Shift analysis of the probability of a better outcome as determined by thefinal category of the OHS indicated a 27% higher chance of a better outcome with rtPA, <strong>and</strong> thiswas statistically significant (95% CI 1.10-1.47; p=0.001).Subgroups: the benefit from rtPA was at least as great for patients over the <strong>age</strong> of 80 as foryounger patients. Patients with severe stroke benefitted at least as much as those with lesssevere stroke. The benefit was greatest in patients treated within 3 hours of onset, bearing in mindthat these patients tended to be older <strong>and</strong> more severe. The presence of acute ischaemicchanges on baseline CT scan did not appear to prejudice the benefit from <strong>treatment</strong>.Updated Cochrane ReviewThe data from IST3 were added to the 11 existing trials of rtPA, with the numbers of patientstreated up to 6 hours from onset almost doubling to over 7000. Almost all the data in patients overthe <strong>age</strong> of 80 comes from IST3. The review confirms an excess risk of fatal ICH (four-foldincreased risk) <strong>and</strong> a 44% relative increase in risk of death within 7 days to 8.9%. At six months,total mortality was the same with or without rtPA <strong>treatment</strong>, with an overall absolute increase inpatients with reduced or absent disability of 5.5% with <strong>treatment</strong>. Early <strong>treatment</strong> (within 3 hours)was definitely beneficial, increasing the relative odds of a good outcome by 53%. The magnitudeof the benefit of <strong>treatment</strong> within 3 hours was very similar for patients above or below the <strong>age</strong> of 80(a 9.5% absolute increase in the chance of a good outcome), but beyond 3 hours there was nobenefit for patients over 80, <strong>and</strong> a lesser benefit for younger patients.Clinical ImplicationsThe European licence for rtPA in acute ischaemic stroke has recently been amended to licence<strong>treatment</strong> in patients <strong>age</strong>d 80 or younger up to 4.5 hours after known onset, based on the results of<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 24 of 31
the ECASS III trial <strong>and</strong> the updated individual patient meta-analysis of Lees et al (2010). The moststraightforward conclusion the CRG drew from the additional IST3 data was that the benefits of<strong>thrombolysis</strong> can be immediately <strong>extended</strong> to those patients previously excluded by <strong>age</strong>, by strokeseverity or by the presence of early ischaemic changes on CT scan. The relation to time to<strong>treatment</strong> is more complex, although IST3 adds further emphasis to the importance of treating allpatients as early as possible to maximise the chances of benefit. Subdividing the Cochrane reviewby <strong>age</strong> (above or below 80 years) <strong>and</strong> time to <strong>treatment</strong> (before 3 hours or between 3-6 hours)indicates clear benefit below 3 hours regardless of <strong>age</strong>, but no clear evidence of benefit forpatients over 80 beyond 3 hours. Thus the extension to include older patients within 3 hours isstraightforward, but beyond 3 hours probably requires the results of other current or planned trialsfor a clearer answer. The Cochrane review provides reassurance regarding the risks of ICH, whichare not higher than previously reported even among patients with severe stroke or those treated upto 6 hours, <strong>and</strong> so may provide justification for patients below the <strong>age</strong> of 80 with severe stroke <strong>and</strong>a lot to lose being treated up to 6 hours after symptom onset.The <strong>Stroke</strong> CRG thus concluded that:1. Any patient, regardless of <strong>age</strong> or stroke severity, where <strong>treatment</strong> can be started within 3 hoursof known symptom onset <strong>and</strong> who has been shown not to have an intracerebral haemorrh<strong>age</strong>or other contraindications should be considered for <strong>treatment</strong> using alteplase.2. Between 3 <strong>and</strong> 4.5 hours of known symptom onset, patients under 80 who have been shownnot to have an intracerebral haemorrh<strong>age</strong> or other contraindication should be considered for<strong>treatment</strong> with alteplase.3. Between 3 hours <strong>and</strong> 6 hours of known symptom onset patients should be considered for<strong>treatment</strong> with alteplase on an individual basis recognising that the benefits of <strong>treatment</strong> arelikely to be smaller than those treated earlier, but that the risks of a worse outcome, includingdeath, will on aver<strong>age</strong> not be increased.4. To permit these decisions to be considered in every case in a timely fashion, the South WesternAmbulance Service should deliver every patient with suspected stroke within 6 hours of onset tothe nearest ED as fast as possible with a pre-alert (according to local arrangements) <strong>and</strong> a ‘bluelight’ transfer, without further pre-selection.2. Intra-arterial interventions for acute ischaemic strokeThe other main development in acute stroke <strong>thrombolysis</strong> is the suspension of the IMS III trial bythe National Institutes of Health in May 2012. IMS III was planned to compare outcomes in 900patients r<strong>and</strong>omised to intravenous rtPA or to an IV/IA regimen, using mechanical clot retrieval orintra-arterial rtPA within 7 hours of known onset. The trial was suspended after 656 patients werer<strong>and</strong>omised on the grounds of futility, given that the trial had a very low likelihood of demonstratinga clinically significant difference in benefit between the <strong>treatment</strong> arms of the study. Other<strong>treatment</strong> regimens are being studied in the US <strong>and</strong> elsewhere (including with tenectaplase ordesmoteplase), but at present the data supporting an IV/IA rescue strategy are not sufficient toadvocate a major change in man<strong>age</strong>ment approach. This is in keeping with the upcoming NationalClinical Guidelines recommendation that intra-arterial interventions should only be used in thecontext of a clinical trial.The approach to intra-arterial interventions within the Peninsula Heart & <strong>Stroke</strong> Network willtherefore be based on the consensus statements from the <strong>Stroke</strong> Improvement Programmemeeting of October 2011, as follows:1. The widespread adoption of intra-arterial interventions in acute stroke could not berecommended at the present time, on the grounds that the available r<strong>and</strong>omised controlled trialevidence was insufficient.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 25 of 31
2. A number of trials are in progress that may help clarify the appropriate role of such therapies<strong>and</strong> devices <strong>and</strong> it is strongly recommended that further research is conducted.3. Intra-arterial interventions in acute stroke should only be undertaken within the context of a trialor national/international registry <strong>and</strong> at specialist stroke centres that fulfil agreed st<strong>and</strong>ards ofcare.4. Further work at a national level should be undertaken to agree <strong>and</strong> describe the requiredst<strong>and</strong>ards of care for both staff <strong>and</strong> processes at such centres: st<strong>and</strong>ards that would includedemonstrable research capability <strong>and</strong> activity in trials of interventional <strong>treatment</strong>s.Implications for the Peninsula Heart & <strong>Stroke</strong> NetworkFollowing the results of IST3 <strong>and</strong> the updated Cochrane Review, the Clinical Reference Groupaimed for a consistent approach to eligibility for intravenous alteplase <strong>treatment</strong> across thePeninsula. This will include the need for <strong>thrombolysis</strong> protocols to be amended, <strong>and</strong> to liaise withthe South Western Ambulance Services Trust to achieve a consistent approach to pre-hospitalcare. At the same time, SINAP data for the first full year (2011-12) continue to show very low ratesof <strong>thrombolysis</strong> across the Peninsula (from less than 2% to 6%) when the comparative nationalSINAP aver<strong>age</strong> for the first quarter of 2012-13 is now 11%. Removing the upper <strong>age</strong> limit for<strong>treatment</strong> will have an immediate effect on the proportion of patients eligible for <strong>treatment</strong>, butfurther efforts are needed to increase the disability benefit for patients through the eradication ofdelays to <strong>treatment</strong> in all centres.3. Monitoring compliance <strong>and</strong> effectivenessElement to be Outcome of <strong>thrombolysis</strong> for individual patientsmonitoredLeadDr Katja AdieToolFrequencyReportingarrangementsActing onrecommendations<strong>and</strong> Lead(s)Change inpractice <strong>and</strong>lessons to besharedSITS(MOST) -Safe implementation of Thrombolysis in <strong>Stroke</strong>Monitoring Study – an international monitoring studySentinel <strong>Stroke</strong> National Audit Programme (SSNAP) from the RoyalCollege of PhysiciansEach thrombolysed patients details <strong>and</strong> outcomes are entered onto the SITS MOST database <strong>and</strong> the SSNAP Audit ProgrammeDr Adie reports outcome locally to the eldercare governancemeeting six monthlySSNAP data is collected as part of the Trust Clinical Audit &Outcomes Programme on an ongoing basisSSNAP data is reported <strong>and</strong> published nationally <strong>and</strong> monitored bythe Strategic Health AuthorityDr Adie, Dr HarringtonRequired changes to practice will be identified <strong>and</strong> actioned withinsix months. Dr Adie <strong>and</strong> Dr Harrington as lead members of theteam will take each change forward where appropriate.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 26 of 31
4. Equality <strong>and</strong> Diversity4.1 This document complies with the Royal Cornwall Hospitals NHS Trust serviceEquality <strong>and</strong> Diversity statement.4.2 Equality Impact AssessmentThe Initial Equality Impact Assessment Screening Form is at Appendix 2.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 27 of 31
Appendix 1. Governance InformationDocument TitleDate Issued/Approved: 3/9/12Date Valid From: 3/9/12Date Valid To: 1/9/15<strong>Stroke</strong> Thrombolysis Guideline Version 3Extended Age <strong>and</strong> Treatment WindowDirectorate / Department responsible(author/owner):Dr Frances Harrington, ConsultantPhysician, Eldercare RCHTContact details: 01872 253290Brief summary of contentsGuideline for the administration of<strong>thrombolysis</strong> for acute ischaemic stroke –upper <strong>age</strong> limit removed, time <strong>window</strong><strong>extended</strong> for some patients from 3h to 6hSuggested Keywords:Target AudienceExecutive Director responsible forPolicy:Date revised: 22/8/12This document replaces (exact title ofprevious version):Approval route (names ofcommittees)/consultation:Divisional Man<strong>age</strong>r confirmingapproval processesName <strong>and</strong> Post Title of additionalsignatoriesSignature of Executive Director givingapprovalPublication Location (refer to Policyon Policies – Approvals <strong>and</strong>Ratification):Document Library Folder/Sub FolderLinks to key external st<strong>and</strong>ardsRelated Documents:<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 28 of 31<strong>Stroke</strong>, Thrombolysis, AlteplaseRCHT PCT CFTMedical Director<strong>Stroke</strong> Thrombolysis 24/7 ProtocolAcute <strong>Stroke</strong> Group, SERCO, SWASTDr Duncan BrowneNot RequiredInternet & Intranet Intranet OnlyClinical / Neurology <strong>and</strong> <strong>Stroke</strong>NICE Guidance TA122 - Alteplase for the<strong>treatment</strong> of acute ischaemic strokeAdvanced <strong>Stroke</strong> Man<strong>age</strong>ment PathwayAcute <strong>Stroke</strong> Man<strong>age</strong>ment<strong>Stroke</strong> <strong>and</strong> TIA Multidisciplinary CarePathwaySecondary Prevention after <strong>Stroke</strong> or TIA
Training Need Identified?Yes. Learning <strong>and</strong> Developmentdepartment have been informed.Version Control TableDateVersionNoJuly 2008 V1.0Initial IssueSummary of ChangesChanges Made by(Name <strong>and</strong> Job Title)Dr F HarringtonDecember2010V2.0 Amendment to 24/7 service Dr F Harrington3/9/12 V3.0 Extended <strong>age</strong> <strong>and</strong> <strong>treatment</strong> <strong>window</strong> Dr F HarringtonAll or part of this document can be released under the Freedom of InformationAct 2000This document is to be retained for 10 years from the date of expiry.This document is only valid on the day of printingControlled DocumentThis document has been created following the Royal Cornwall Hospitals NHS TrustPolicy on Document Production. It should not be altered in any way without theexpress permission of the author or their Line Man<strong>age</strong>r.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 29 of 31
Appendix 2. Initial Equality Impact Assessment ScreeningFormName of service, strategy, policy or project (hereafter referred to as policy) to beassessed: <strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowDirectorate <strong>and</strong> service area:Is this a new or existing Procedure? existingName of individual completingTelephone:assessment: Dr F Harrington01872 2532901. Policy Aim* To safely administer thrombolytic <strong>age</strong>nt to acute ischaemicstroke patients using updated, clearly defined criteria2. Policy Objectives* Safe administration of emergency drug therapyClear advice <strong>and</strong> guidance for staff involved in theadministration of emergency <strong>treatment</strong> <strong>and</strong> aftercare ofpatients who have undergone <strong>thrombolysis</strong> for stroke3. Policy – intended As aboveOutcomes*4. How will you measurethe outcome?5. Who is intended tobenefit from the Policy?6a. Is consultationrequired with theworkforce, equalitygroups, local interestgroups etc. around thispolicy?b. If yes, have thesegroups been consulted?c. Please list any groupswho have been consultedabout this procedure.Patient response to <strong>treatment</strong>Audit – ongoing local <strong>and</strong> RCP National Sentinel <strong>Stroke</strong>AuditInclusion in international SITS-MOST register (Safeimplementation of <strong>thrombolysis</strong> in stroke)Patients: through the promotion of safe, effective, evidencebased practiceYesYesAcute <strong>Stroke</strong> Group, SERCO, SWAST*Please see Glossary7. The ImpactPlease complete the following table using ticks. You should refer to the EA guidance notesfor areas of possible impact <strong>and</strong> also the Glossary if needed.• Where you think that the policy could have a positive impact on any of the equalitygroup(s) like promoting equality <strong>and</strong> equal opportunities or improving relationswithin equality groups, tick the ‘Positive impact’ box.<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 30 of 31
• Where you think that the policy could have a negative impact on any of the equalitygroup(s) i.e. it could disadvant<strong>age</strong> them, tick the ‘Negative impact’ box.• Where you think that the policy has no impact on any of the equality group(s) listedbelow i.e. it has no effect currently on equality groups, tick the ‘No impact’ box.Equality Positive Negative No Reasons for decisionGroup Impact Impact ImpactAge X Removal of upper <strong>age</strong> limit forstroke <strong>thrombolysis</strong> based onrecent r<strong>and</strong>omised controlled trialsDisabilityXReligion orbeliefGenderTransgenderPregnancy/MaternityRaceSexualOrientationMarri<strong>age</strong> / CivilPartnershipXXXXXXXYou will need to continue to a full Equality Impact Assessment if the following havebeen highlighted:• A negative impact <strong>and</strong>• No consultation (this excludes any policies which have been identified as notrequiring consultation).8. If there is no evidence that the policypromotes equality, equal opportunitiesor improved relations - could it beadapted so that it does? How?Full statement of commitment to policy ofequal opportunities is included in the policyPlease sign <strong>and</strong> date this form.Keep one copy <strong>and</strong> send a copy to Matron, Equality, Diversity <strong>and</strong> Human Rights,c/o Royal Cornwall Hospitals NHS Trust, Human Resources Department, ChyveanHouse, Penventinnie Lane, Truro, Cornwall, TR1 3LJA summary of the results will be published on the Trust’s web site.Signed ________________________________________Date _________________________________________<strong>Stroke</strong> Thrombolysis Guideline Extended Age <strong>and</strong> Treatment WindowP<strong>age</strong> 31 of 31