here - International Trauma Anesthesia and Critical Care Society
here - International Trauma Anesthesia and Critical Care Society
here - International Trauma Anesthesia and Critical Care Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Trauma</strong><strong>Care</strong>ITACCS Summer 2002I N T E R N A T I O N A LT R A U M AC A R EVolume 12 Number 1Summer 2002The Official Publication of ITACCS<strong>International</strong> <strong>Trauma</strong> <strong>Care</strong><strong>Trauma</strong><strong>Care</strong>now available atwww.ITACCS.com➤ Hypertonic SolutionsSee Clinical Issues,page 6CMEQuestions!See Pages22 & 23➤ Abdominal AorticTransection in anAbused ChildSee Clinical Issues,page 12➤ ED Thoracotomy<strong>and</strong> ECLSSee Clinical Issues,page 15SOCÍETÉ INTERNATIONALE D ANESTHÉSIE - REANIMATION EN TRAUMATOLOGIE➤ Field Hospital inNorthern IndiaSee Military Medicine,page 18INTERNATIONALE GESELLSCHAFT FÜR ANÄSTHESIE UND INTENSIVMEDIZIN IM TRAUMASOCIEDAD INTERNACIONAL DE ANESTHESIE Y REANIMACION EN TRAUMATOLOGIA1
ITACCS Summer 20022
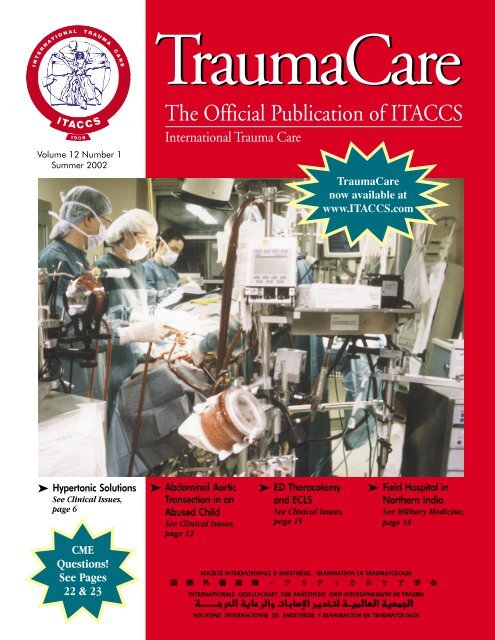
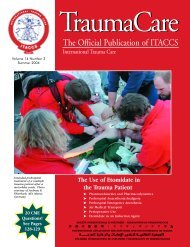
ITACCS<strong>Trauma</strong><strong>Care</strong>Volume 12 Number 1 Summer 2002I N T E R N A T I O N A LT R A U M AC A R EPRESIDENT’S REPORT5 • Opportunities for Interaction<strong>and</strong> EducationMichael J. A. Parr, MB, BS, FRCA, FANZCACLINICAL ISSUES6 • Hypertonic Solutions: An UpdateChrister H. Svensén, MD, PhD12 • Blunt Abdominal AorticTransection in an Abused Child:A Case Report <strong>and</strong> Literature ReviewRoya Yumul, MD, PhD, Zoreh Steffens,MD, Stephen N. Steen, ScD, MD,Calvin Johnson, MD15 • A Case of Multiple Blunt InjuriesTreated with EmergencyDepartment Thoracotomy <strong>and</strong>Extracorporeal Life SupportTaichi Takeda, MD, Yutaka Taira, MD,Itaru Takara, MD, Kazuhiro Sugahara,MD, Yoshihiko Yoshii, MDMILITARY MEDICINE18 • Provision of a <strong>Trauma</strong>Resuscitation <strong>and</strong> AnaesthesiaService in an Advance FieldMilitary Hospital in Northern IndiaMajor Manish Mehrotra, MD, <strong>and</strong>Lt. Col. S<strong>and</strong>eep Mehrotra, MS, DNBCME QUESTIONS22 • 20 Questions for 10 Credit Hoursin AMA Category 1Publication Date: October 2002Credit Expiration Date: October 2003The Official Publication of ITACCS<strong>International</strong> <strong>Trauma</strong> <strong>Care</strong>Cover PhotoUse of extracorporeal life support circuitfor a patient with severe respiratory failurein the R Adams Cowley Shock <strong>Trauma</strong>Center, Baltimore, Maryl<strong>and</strong>. Left to right:H. Neal Reynolds, MD, Maureen McCunn,MD, Victor Gustina, RN.CONTENTSCopyright 2002 © by the <strong>International</strong><strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> <strong>Society</strong>ISSN 1094-1126Co-Editors-in-ChiefAdolph H. Giesecke, MDDepartment of AnesthesiologyUT Southwestern Medical CenterDallas, TX 75390-9068 USATel: 214-590-7254; Fax: 214-590-6945e-mail: Adolph.Giesecke@UTSouthwestern.eduJohn K. Stene, MD, PhDDepartment of AnesthesiologyMilton S. Hershey Medical CenterHershey, PA 17033 USATel: 717-531-8434; Fax: 717-531-4110e-mail: jstene@psu.eduManaging EditorLinda J. Kesselring, MS, ELSNational Study Center for <strong>Trauma</strong>/EMS701 W. Pratt Street, Fifth FloorBaltimore, MD 21201 USATel: 410-328-7449; Fax: 410-328-3699e-mail: lkessel112@aol.comGuidelines for Authors available atwww.ITACCS.comSend address changes <strong>and</strong> generalinquiries to <strong>Trauma</strong><strong>Care</strong>Mail@aol.comITACCS World HeadquartersP.O. Box 4826, Baltimore, MD 21211 USAFax: 410-235-8084 • www.ITACCS.comThe opinions expressed in <strong>Trauma</strong><strong>Care</strong>are those of the authors <strong>and</strong> not necessarilythose of ITACCS.The drug <strong>and</strong> dosage information presentedin this publication is believed to beaccurate. However, the reader is urged toconsult the full prescribing information onany product mentioned in this publicationfor recommended dosage, indications,contraindications, warning, precautions,<strong>and</strong> adverse effects. This is particularlyimportant for drugs that are new orprescribed infrequently.3BOARD OF DIRECTORSPRESIDENTMichael J. A. Parr, MB, BS, MRCP, FRCA, FANZCAVICE PRESIDENTSWalter Mauritz, MD, PhDColin F. Mackenzie, MDJorge G. Plaza, MDEXECUTIVE DIRECTORChristopher M. Gr<strong>and</strong>e, MD, MPHGENERAL MEMBERSJeffrey M. Berman, MDPierre A. Carli, MDYves Lambert, MDJerry P. Nolan, MB, BS FRCAKeiichi Tanaka, MD, PhDPAST PRESIDENTSEnrico M. Camporesi, MDElizabeth A.M. Frost, MDPeter J. F. Baskett, MB, BCh, FRCA, MRCPJohn K. Stene, MD, PhDAdolph H. Giesecke, MDCOMMITTEE CHAIRPERSONSEDUCATION AND TRAININGChristopher M. Gr<strong>and</strong>e, MD, MPHRESEARCHColin F. Mackenzie, MDJOURNAL: TRAUMACAREAdolph H. Giesecke, MD (Co-Editor)John K. Stene, MD, PhD (Co-Editor)CQI/TQM/RISK MANAGEMENTRichard P. Dutton, MDDISASTER/MASS CASUALTYAndreas Thierbach, MDPEDIATRIC TRAUMAGail E. Rasmussen, MDGERIATRIC TRAUMAJeffrey H. Silverstein, MDPREHOSPITAL/EMSCharles Deakin, MDCRITICAL CAREMaureen McCunn, MDSPECIAL EQUIPMENT/TECHNIQUESCharles E. Smith, MD, FRCPCFINANCE OF TRAUMA CAREAnne J. Sutcliffe, MB, BCh, FRCABIOTECHNOLOGY IN TRAUMALouis M. Guzzi, MDPAIN MANAGEMENT/REGIONAL ANESTHESIAAndrew D. Rosenberg, MDTOXIC TRAUMA/HAZMATDavid J. Baker, M. Phil, DM FRCAMILITARY TRAUMAMatthias Helm, MDADVISORY COMMITTEE ON TRAINEESPaul R. Barach, MD, MPHTRAUMA SURGERY LIAISONLewis J. Kaplan, MD, FACSEMERGENCY MEDICINE LIAISONDario Gonzalez, MD, FACEPCRNA LIAISONCharles R. Barton, CRNA, MEdRESPIRATORY THERAPIST LIAISONRusty Reid, RRTOPERATIONAL PROJECTSDEVELOPING NATIONS PROGRAM (DNP)Christopher M. Gr<strong>and</strong>e, MD, MPHCOMPREHENSIVE APPROACH TO TRAUMATOLOGY (CAT)Peter J. F. Baskett, MB, BCh, FRCA, MRCPTRAUMA/EMS TERMINOLOGYWolfgang F. Dick, MD, PhDLOTAS: LEVEL ONE TRAUMA SIMULATIONSColin F. Mackenzie, MDJOURNAL: TRAUMACARELinda J. Kesselring, MS, ELS, Managing EditorREFRESHER COURSES/WORKSHOPSPaul Hilliard, CRNA, ManagerSPECIAL AD HOC ADVISORSBruce F. Cullen, MDRobert L. Fila, Esq.Ake N. A. Grenvik, MD, PhDDouglas G. Hicks, CPAIrene H. Impellizzeri, PhDRonald M. Kropp, MHSJohn D. Lupiano, MD, MHPeter Safar, MD
ITACCS Summer 20024
ITACCS Summer 2002PRESIDENT’S REPORTOpportunities forInteraction <strong>and</strong> EducationMichael J.A. Parr, MB, BS,MRCP, FRCA, FANZCAIntensive <strong>Care</strong> UnitLiverpool HospitalSydney, AustraliaMichael.Parr@swsahs.nsw.gov.auThe overall aim of<strong>Trauma</strong><strong>Care</strong> <strong>International</strong>(ITACCS) is to facilitate traumaeducation <strong>and</strong> t<strong>here</strong>by improvetrauma management at alllevels <strong>and</strong> by all disciplines.The international membershipof the society provides aunique resource with firsth<strong>and</strong>insight <strong>and</strong> experience in the global management oftrauma. Increasingly we recognize we all share the same issuesin trauma management but local factors of resource, education,<strong>and</strong> experience dictate what is achievable.This issue of the journal <strong>Trauma</strong><strong>Care</strong> provides a peerreviewedresource to aid this education process. Svensen fromGalveston, Texas, USA, provides us with a concise review of thehistory, effects, <strong>and</strong> adverse effects of hypertonic solutions usedfor resuscitation. The role of these solutions in fluid managementof trauma victims continues to be defined. Their effectsare diverse <strong>and</strong> incompletely understood but it appears that formany countries they have established roles in trauma management.However, their true role will be clearly defined only byappropriate clinical trials. A r<strong>and</strong>omised prehospital trial of theuse of hypertonic saline is due for completion later this year inMelbourne, Australia, <strong>and</strong>, it is hoped, will clarify the role.Also in this issue are two case reports — the first from Yumul<strong>and</strong> colleagues from Los Angeles, California, USA, <strong>and</strong> the secondfrom Takeda <strong>and</strong> colleagues in Okinawa, Japan — which demonstratewhat a well-resourced trauma service can provide indeveloped nations. In contrast, Mehrotra <strong>and</strong> Mehrotra provide uswith an article that demonstrates the reality of providing a traumaservice in a developing nation in the difficult environment of farnorth India. We can certainly learn from each other <strong>and</strong> assistothers in the development of their trauma systems. With theanniversary of September the 11th just passing, it is appropriate toreflect on how we can share our knowledge on a global scale.The management of trauma is a rapidly changing field ofmedical practice, <strong>and</strong> the Internet provides many attractiveopportunities for interaction <strong>and</strong> education. A leading resource inthis goal is the <strong>Trauma</strong>-List mailing list <strong>and</strong> discussion groupbased at www.trauma.org, which carries a link to the ITACCS Website <strong>and</strong> which regularly receives input from <strong>Trauma</strong><strong>Care</strong> <strong>International</strong>(ITACCS) members from around the world. With increasingglobalisation <strong>and</strong> ease of access to electronic media, the Internetprovides a great opportunity to share trauma knowledge throughoutthe world. <strong>Trauma</strong><strong>Care</strong> <strong>International</strong> (ITACCS) will becollaborating widely <strong>and</strong> exp<strong>and</strong>ing its own Web-based resourcesto achieve our goals. As a society we are open to membershipfrom all disciplines involved in trauma care <strong>and</strong> we are alwayshappy to hear from individuals with ideas on how to achieve ourgoals. The annual <strong>Trauma</strong><strong>Care</strong> meetings provide an ideal forumfor national <strong>and</strong> international collaboration. The planning for<strong>Trauma</strong><strong>Care</strong> 2003 in Dallas <strong>and</strong> <strong>Trauma</strong><strong>Care</strong> 2004 in Sydney isnow in advanced stages of preparation.Editorial Board for <strong>Trauma</strong><strong>Care</strong>Co-Editors-in-ChiefAdolph H. Giesecke, MD (USA) • John K. Stene, MD, PhD (USA)Prehospital <strong>Care</strong>Dario Gonzalez, MD, FACEP (USA) • David LaCombe, NREMT-P (USA)Eldar Søreide, MD, PhD (Norway)Emergency Department <strong>Care</strong>Dale M. Carrison, DO, FACEP (USA) • Marvin Wayne, MD, FACEP (USA)OR <strong>and</strong> Intensive <strong>Care</strong>Paul Barach, MD (USA) • James G. Cain, MD (USA) • Richard P. Dutton, MD (USA)William F. Fallon, Jr., MD, FACS (USA) • Maureen McCunn, MD (USA)Pediatric <strong>Trauma</strong>James Fletcher, MD (USA) • Calvin Johnson, MD (USA)Thomas Long, MD (USA) • Gail E. Rasmussen, MD (USA)Original ResearchLewis Kaplan, MD, FACS (USA) • Colin F. Mackenzie, MD (USA)Charles E. Smith, MD, FRCPC (USA)CRNA SectionCharles R. Barton, MEd, CRNA (USA) • James M. Rich, MA, CRNA (USA)<strong>International</strong> Advisory BoardWolfgang F. Dick, MD, PhD (Germany) • C.M. Gr<strong>and</strong>e, MD, MPH (USA)Louis M. Guzzi, MD (USA) • Yves Lambert, MD (France)Walter Mauritz, MD, PhD (Austria) • Jerry Nolan, MB, ChB, FFARCS (Engl<strong>and</strong>)Michael J.A. Parr, MB, BS, MRCP(UK), FRCA (Australia) • Anne J. Sutcliffe, FRCA (Engl<strong>and</strong>)Keiichi Tanaka, MD (Japan)Educational ObjectivesThis activity is designed to provide trauma care professionalsinterested in the treatment of critically ill trauma patients with aregular overview <strong>and</strong> critical analysis of the most current, clinicallyuseful information available, covering strategies <strong>and</strong> advances in thediagnosis of traumatic injuries <strong>and</strong> the treatment of trauma patients.Controversies, advantages, <strong>and</strong> disadvantages of diagnosis <strong>and</strong> treatmentplans are emphasized. T<strong>here</strong> are no prerequisites for participationin this activity.After reading each issue, participants should have a workingfamiliarity with the most significant information <strong>and</strong> perspectivespresented <strong>and</strong> apply what they have learned promptly in clinicalpractice. Specific learning objectives are printed at the opening ofeach article.5
ITACCS Summer 2002in those capillaries that have a swollen endothelium. 21 Increasingconcentrations of sodium thus have a positive inotropiceffect 23 at an osmolality range of 240 to 320 mOsm, w<strong>here</strong>asconcentrations higher than 320 mOsm have a negative effect.This could explain why too rapid infusion of HS could lead to adecrease in blood pressure.Renal Effects. Renal physiologists have infused 5% to 10%salt solutions to determine how the kidneys h<strong>and</strong>le an acutesalt load <strong>and</strong> increased serum osmolality. 24 Administration ofhypertonic solutions is associated with an increased urineoutput, which in turn is associated with a natriuresis, to which,in hypovolemic conditions, rectification of renal blood flow25, 26<strong>and</strong> glomerular filtration are contributing factors.The improvement in diuresis, which occurs even duringhypovolemia, is the result of an osmotic diuresis.Coagulation Effects. The administration of hypertonicsolutions affects coagulation by the extent of hemodilution. 27The slight effect of prolongation of prothrombin <strong>and</strong> decreasedhuman platelet aggregation when diluting human blood withHSD is attributed to the HS component. 28 Since dextran 70 is apart of HSD, t<strong>here</strong> have been concerns about combined causesof impaired hemostasis. 29 In fact, the doses of dextran neededto impair hemostasis must be much higher, 30 <strong>and</strong> t<strong>here</strong> is nointeraction between the HS component <strong>and</strong> the dextrancomponent. Furthermore, t<strong>here</strong> are no effects on typing orcross-matching when using clinical doses of HSD. 31Immunologic Effects. The physiologic responses totrauma <strong>and</strong> hemorrhage are manifestations of complexcellular <strong>and</strong> molecular events. Inflammatory cells, includingmacrophages, polymorphonuclear cells, <strong>and</strong> lymphocytes, arerecruited to the site of injury <strong>and</strong> secrete inflammatorymediators. The inflammatory response to injury involves aninterplay between hormones (e.g., catecholamines, adrenocorticotropichormone, cortisol, <strong>and</strong> glucagon), cytokines(e.g., tumor necrosis factor-alpha), interleukins (e.g., IL-6, IL-8, IL-10, IL1-beta), <strong>and</strong> other cellular products such asproteases, free radicals, eicosanoids, acute-phase reactants,<strong>and</strong> growth factors. 32-35Posttraumatic immunosuppression is thus a well-documentedphenomenon that has been implicated in the pathogenesisof posttraumatic complications such as acute respiratorydistress syndrome, sepsis, <strong>and</strong> multiple organ failure.Therapeutic approaches to counter these threats have been thefocus of numerous investigations for many years. Traditionaltherapies have concentrated on antibiotics, mechanicalventilation, <strong>and</strong> fluid therapy toward endpoints such as bloodpressure <strong>and</strong> urine output. 36 Current fluid regimens use largevolumes of both crystalloids <strong>and</strong> colloids. 36 Recent research hasshown that lactated Ringer’s solution has inflammatory33, 37properties.Efforts to use hypertonic solutions in animal models as avolume exp<strong>and</strong>er have shown some promising results (i.e., lessvolume used, improved cardiac support). 38, 39 In addition, HShas been shown to enhance T-cell function in vitro <strong>and</strong> cellmediatedimmune function in vivo. 38 It has been suggested thatthese capabilities of HS are the result of the ability of the fluid’shypertonicity to co-stimulate the T cells in proliferation. Thus,HS replaces the abundant signal pathway for activating T cellsin immune-compromised patients 38, 39 —a concept that researchershave suggested might protect patients from septicchallenge, 39 improve intestinal mucosal blood flow, 40 <strong>and</strong>reduce the onset of late complications in trauma patients. 1 Asin the prehospital scenario, 41 investigations have shown that HSshould be given as early as possible to a patient if it is to beused to enhance that patient’s immune response. 1, 42, 43 It hasalso been shown that hypertonic solutions are associated withthe attenuation of the neuroendocrine response to surgery <strong>and</strong>hemorrhage. 41, 44 Infusion of HS was associated with attenuationof the cortisol, aldosterone, <strong>and</strong> angiotensin II responsesto surgery.Clinical UsePrehospital Use. Effective resuscitation of the patientsuffering from hemorrhagic hypotension is an attractiveproposition to both military <strong>and</strong> civilian health care professionals.In warfare, wounds from bullets <strong>and</strong> shrapnel causebleeding, hypotension, <strong>and</strong> ultimately hemorrhagic shock. 45More often than not, the battlefield setting is plagued by longtransport times <strong>and</strong> difficult logistics. Added to these problemsis the fact that medics can carry only a limited amount of fluids.From the civilian perspective, conditions are quite different.Typically, transport times are much shorter <strong>and</strong> logisticalpreparations allow ambulances <strong>and</strong> rescue personnel to carrysubstantial amounts of fluids.The types of trauma encountered in each setting alsodiffer. While military medical personnel most often have to dealwith penetrating trauma, civilian health care professionalsencounter both penetrating <strong>and</strong> blunt trauma. The importanceof early intervention has been debated, 45-51 but t<strong>here</strong> is nowwidespread consensus to initially stabilize a traumatized victimby securing the airway, stabilizing the neck, <strong>and</strong> stoppingexternal bleeding. When it comes to intravenous infusiontherapy, the mainstay of prehospital management of postinjuryhypotension has been to immediately replace the lost intravascularvolume. 52 This concept originates from animal studiesperformed during the 1950s <strong>and</strong> 1960s, which formed the basisfor treatment of wounded soldiers in the Vietnam War. Thistreatment eventually was transferred to the streets of theUnited States in the 1970s. With the advent of rapid transportationsystems <strong>and</strong> trauma centers, however, the type, volume,time of initiation, <strong>and</strong> even the value of prehospital fluid49, 50, 53, 54resuscitation have been challenged in the past 20 years.The reluctance of certain providers to start intravenous fluidtherapy in the field has been associated primarily with the lackof sufficient education among rescue personnel, the risk ofrebleeding, 53,55 <strong>and</strong> the delay of transportation to definitive caresites. 53 Since the development of these new technologies, noconsensus has been reached as to how to initially treat traumapatients, <strong>and</strong> different trauma protocols have been launcheddepending on the different types of trauma <strong>and</strong> the differentsettings in which they occur.Although promising, clinical trials have not provided56, 57definitive data as to the efficacy of hypertonic solutions.This has been in part due to the limited numbers of enrolledpatients <strong>and</strong> the diversity of the underlying trauma responsiblefor the injuries. Wade et al 56 in 1997 conducted an extensivemeta-analysis of all r<strong>and</strong>omized prospective clinical trials usinghypertonic 7.5% saline solutions to determine whether7
ITACCS Summer 2002hypertonic solutions improved survival in patients withhypotension associated with traumatic injury. They separatedthe analysis into the effects of a 250-mL bolus of HS alone <strong>and</strong>/or in combination with HSD. The two hypertonic groups werecompared with matched groups receiving a 250-mL bolus ofisotonic solution. In all cases, additional isotonic solution wasadministered to continue the hypertonic solution started. Aftera meticulous search for available studies, the authors found sixeligible studies using HS <strong>and</strong> eight studies using HSD. A totalof 615 patients were treated with HSD <strong>and</strong> 340 patients weretreated with HS. All individual studies were r<strong>and</strong>omized,included a control group, <strong>and</strong> had as endpoints survival atdischarge or after 30 days. In the meta-analysis for studiesusing HS, no difference in outcome was found. In the HSDgroup, all studies 1, 58-64 except one showed an improvement insurvival, but again, differences reached statistical significance inonly one of the individual studies 62 <strong>and</strong> only in specificsubpopulations—patients with head injuries <strong>and</strong> those withpenetrating injuries requiring surgery. 1 The mean difference ofsurvival calculated for all studies favoring treatment with HSDover controls was 3.5% (P=0.07, one-tailed). The conclusionwas that HSD might be beneficial in improving survival inpatients with hypotension associated with traumatic injury.Subsequently, a meta-analysis using individual data from sixof the eight studies containing data with HSD was performed, 65which showed a significantly lowered mortality for HSD inpatients for whom HSD was infused as the first fluid (incontrast to isotonic therapy).The lesson to be learned from these studies is that thenumber of patients in individual trauma trials generally hasbeen insufficient to establish statistically significantly improvedsurvival <strong>and</strong> that aggregate data from these same trials areencouraging but not fully significant. Moreover, meta-analysisstudies can be criticized 66 because t<strong>here</strong> are difficulties associatedwith comparing the underlying studies. Since metaanalysesare not generally considered sufficient evidence forregulatory approval, HSD has not been approved for use in theUnited States. Interestingly, no other intravenous fluid orvolume exp<strong>and</strong>er has been required to improve survival inorder to be used in the clinical setting. Current fluids are usedmainly because they have shown volume-expansion properties.When established rules of obtaining consent for participatingin clinical studies in the United States appeared in the first halfof the 1990s, prehospital studies became difficult to perform.This development, coupled with concerns raised amongsurgeons when Bickell et al 53 reported that conventional fluidtherapy might be inferior to delayed prehospital fluid resuscitationin hypotensive <strong>and</strong> penetrating trauma patients, resultedin a general reduction of interest in prehospital resuscitationwith hypertonic solutions in the United States.In Europe, however, the situation is different. In Austria,HS colloid solution has been in use since 1991. Austria <strong>and</strong>Brazil were the first countries in which this type of solutionwas used routinely for resuscitation from severe trauma <strong>and</strong>shock. In Austria, HS is mixed with hetastarch (Osmohes—7.2%sodium chloride + 10% hetastarch 200/0.5—is now replacedby Hyperhes—7.2% sodium chloride + 6% hydroxyethyl starch200/0.62). In the past decade, more than 50,000 units havebeen administered safely. Sweden was the first country toregister Rescueflow® (7.5% sodium chloride + 6% dextran 70),in 1998. 67 Now this solution is registered in 14 countries inEurope. Finally, Germany in 2000 approved HyperHAES (7.2%sodium chloride + 6% hetastarch 200/0.5). In the majority ofthese cases, the st<strong>and</strong>ard amount of hypertonic solutions givenwas 250 ml.Head <strong>Trauma</strong>. Closed head injury is a common feature ofsevere blunt trauma. The outcome from closed head injury isdetermined primarily by the severity of the injury <strong>and</strong> the ageof the patient. Additional important factors are the presence ofhypoxia <strong>and</strong> hypotension, 68 making the brain vulnerable tosecondary brain injury. This condition, however, can bereversed. Prehospital care of patients should t<strong>here</strong>fore focus onminimizing the effects of secondary insults to the brain. 69 Manypatients with severe head injury have hypoxemia upon arrivalat hospital, with PaO 2values
ITACCS Summer 2002to 10 minutes. Do not start intravenous fluid earlier than15 minutes after trauma.3. For other types of trauma, if prehospital time is ≤30minutes:• Give no fluid.In all these scenarios, one should continue treatment withthe st<strong>and</strong>ard fluid of care (crystalloids or colloids as needed)after the administration of the hypertonic solution. If HSD isgiven, hapten dextran (Promit) to prevent immune complexformation when dextran 70 is given is not recommended asnecessary in the trauma setting. 67 If the patient deteriorates,one should suspect rebleeding, stop infusion of the hypertonicsolution, <strong>and</strong> give a slow crystalloid infusion (1000 ml over thecourse of 30 minutes). 81Adverse EffectsDose <strong>and</strong> Rate of Administration. Hypertonic solutionswere originally developed for prehospital use <strong>and</strong> designed toreplace larger volumes of isotonic solutions. The reasons forusing a st<strong>and</strong>ard dose of 4 ml/kg or 250 ml of HS, HSD, or HHSseem to be based more on practicality rather than on any truephysiologic concept. Although it may be reasonable even in theprehospital area to titrate the solutions toward an endpoint, 82t<strong>here</strong> is still support among some clinicians for using ast<strong>and</strong>ard dose for reasons of simplicity. The rate of infusionshould be rapid in order to establish the desired effects. Thegreatest concern regarding rate of infusion has been derivedfrom the hypothesis that fluid resuscitation of prehospital55, 81,trauma can exacerbate uncontrolled internal hemorrhage.83, 84A controlled bleed (1 L implies asituation in which fluids need to be given, but if intravenousline insertion will be difficult <strong>and</strong> transport time will be short,it is probably better to go to the hospital immediately. In thescenario in which major penetrating injury to the heart or largevessels has created an uncontrolled bleed that has not stopped,immediate transport to the proper surgical center is the onlything that will save the patient.Uncontrolled bleeding that has stopped is seen in somevictims of penetrating trauma but also at times in cases of blunttrauma. 85 In such cases, an increased risk of rebleeding shouldbe considered. Since hypertonic solutions tend to increaseblood pressure more than isotonic solutions, this could be apotential risk. Consequently, decreasing the rate of infusion<strong>and</strong> reducing the infused volume to patients with presumptive“uncontrolled bleeding” is recommended. 82 However, thisrecommendation is disputed, since the clinical data do notshow that the administration of hypertonic solutions increasesmortality in the clinical setting. 63 The results of experimentalstudies suggesting that administration of HS exacerbatesbleeding from injured vessels <strong>and</strong> leads to early death inanesthetized animals with lacerations in the aorta or cut tailsare probably not relevant to the clinical setting in mostpatients. 60, 63 Nevertheless, since the beneficial properties ofhypertonic solutions are obtained anyway, it seems reasonableto slow the dose from the recommended 2 to 5 minutes to 5 to10 minutes. Furthermore, the timing of the infusion must beconsidered. In an urban setting with short transport times, it ismost likely best to transfer the patient to an emergencydepartment immediately. In a longer transport scenario, it isunlikely that any intravenous infusion will be started earlierthan 15 minutes after trauma, when the risk of rebleeding isless likely.Hypernatremia. Hypernatremia is common with theinfusion of hypertonic solutions. Levels of hypernatremia inexcess of 165 mmoL have been reported without any adverseeffects. 1 The levels of sodium <strong>and</strong> raised osmolality usually go up9 to 12 mmoL <strong>and</strong> return to baseline within 4 to 6 hours. Theinfusion of hypertonic solutions causes an increased diuresis,increased natriuresis, <strong>and</strong> subsequent kaluresis. As a result, it isrecommended that clinicians monitor electrolytes closely.Anaphylaxis. It has been suggested that HSD can causeanaphylactic reactions because of the dextran contained in thesolution. Patients with hypersensitivity have high plasma titersof dextran-reactive antibodies, particularly of the IgG-class.Infusion of dextran in a patient with such antibodies may causethe formation of large immune complexes with ensuingactivation of plasma enzyme cascades <strong>and</strong> an anaphylacticreaction. HSD contains a small amount of dextran; nevertheless,only a few drops of dextran can cause an adverse reaction<strong>and</strong> pretreatment with hapten dextran (Promit) is normallynecessary. <strong>Trauma</strong> patients, however, seem to be protected in away that is different from other patients. This may be becauseof large amounts of circulating catecholamines. Hapten dextranwas not given in any of the prehospital studies mentioned inthis review. 1, 59-61, 63, 64 T<strong>here</strong> were no anaphylactic reactions inany of these clinical studies. The Swedish Physician’s DeskReference (FASS) makes no recommendation for using haptendextran for trauma patients.As for dextran, previous exposure to hetastarch can triggerreactive antibodies that cause anaphylactoid or anaphylacticreactions. T<strong>here</strong> is, in contrast to dextran, no existing pretreatment,but again this seems not necessary for trauma patients. 9ConclusionPerhaps what can most easily be ascertained from thevoluminous amount of work on hypertonic solutions is that itseems to be very safe to give them. In 35 clinical trials, morethan 1,400 patients have received HS, HSD, or HSS without anycomplications. 9, 86 Furthermore, in the prehospital scenario,patients suffering from severe head trauma seem to be thegroup that benefits most from receiving hypertonic solutions.References1. Mattox KL, Maningas PA, Moore EE, Mateer JR, Marx JA,Aprahamian C, Burch JM, Pepe PE. Prehospital hypertonicsaline/dextran infusion for post-traumatic hypotension.The U.S.A. Multicenter Trial. Ann Surg 1991; 213:482–91.2. Committee on Fluid Resuscitation for Combat Casualties.Executive summary. In Pope A, French G, Longnecker DE,eds. Fluid Resuscitation. Washington, DC, NationalAcademy Press, 1999, pp 1–7.9
ITACCS Summer 20023. Silbert S. The treatment of tromboangiitis obliterans byintravenous injection of hypertonic salt solution. JAMA1926; 86:1759–61.4. Monafo WW. The treatment of burn shock by the intravenous<strong>and</strong> oral administration of hypertonic lactated salinesolution. J <strong>Trauma</strong> 1970; 10:575–86.5. Velasco IT, Pontieri V, Rocha e Silva, Lopes OU.Hyperosmotic NaCl <strong>and</strong> severe hemorrhagic shock. Am JPhysiol 1980; 239:H664–73.6. de FJ Jr, Timoner J, Velasco IT, Lopes OU, Rocha-e-Silva.Treatment of refractory hypovolaemic shock by 7.5%sodium chloride injections. Lancet 1980; 2:1002–4.7. Kramer GC, Perron PR, Lindsey DC, Ho HS, Gunther RA,Boyle WA, Holcroft JW. Small-volume resuscitation withhypertonic saline dextran solution. Surgery 1986;100:239–47.8. Kreimeier U, Frey L, Messmer K. Small-volume resuscitation.Anaesthesiology 1993; 6:400–8.9. Schmietta W, Schöchl H, Kröll W, Pölz W, Mauritz W. Safetyof hypertonic hyperoncotic solutions—survey fromAustria. Wien Klin Wochenschr 2002; 114:89–95.10. Frey L, Kesel K, Pruckner S, Pacheco A, Welte M, MessmerK. Is sodium acetate dextran superior to sodium chloridedextran for small volume resuscitation from traumatichemorrhagic shock? Anesth Analg 1994; 79:517–24.11. Wolf MB. Plasma volume dynamics after hypertonic fluidinfusions in nephrectomized dogs. Am J Physiol 1971;221:1392–5.12. Kramer G, Elgjo GI, Poli de Figueiredo L, Wade C.Hyperosmotic-hyperoncotic solutions. Baillieres ClinicalAnaesthesiology 1997; 11:143–61.13. Lopes OU, Pontieri V, Rocha e Silva, Velasco IT.Hyperosmotic NaCl <strong>and</strong> severe hemorrhagic shock: role ofthe innervated lung. Am J Physiol 1981; 241:H883–90.14. Allen DA, Schertel ER, Schmall LM, Muir WW. Lung innervation<strong>and</strong> the hemodynamic response to 7% sodium chloridein hypovolemic dogs. Circ Shock 1992; 38:189–94.15. Hjelmqvist H, Gunnarsson U. Comparison between theeffects of central <strong>and</strong> systemic hypertonic NaCl onhemodynamic responses to hemorrhage in sheep. Shock1995; 3:355–61.16. Mazzoni MC, Borgstrom P, Arfors KE, Intaglietta M.Dynamic fluid redistribution in hyperosmotic resuscitationof hypovolemic hemorrhage. Am J Physiol 1988;255:H629–37.17. Vassar MJ, Holcroft JW. Use of hypertonic-hyeroncoticfluids for resuscitation of trauma patients. J Intensive <strong>Care</strong>Med 1992; 7:189–98.18. Svensen C, Hahn RG. Volume kinetics of Ringer solution,dextran 70, <strong>and</strong> hypertonic saline in male volunteers.Anesthesiology 1997; 87:204–12.19. Drobin D, Hahn RG. Kinetics of isotonic <strong>and</strong> hypertonic plasmavolume exp<strong>and</strong>ers. Anesthesiology 2002; 96:1371–80.20. Drobin D, Hahn RG. Volume kinetics of Ringer’s solution inhypovolemic volunteers. Anesthesiology 1999; 90:81–91.21. Mazzoni MC, Intaglietta M, Cragoe EJ Jr, Arfors KE.Amiloride-sensitive Na+ pathways in capillary endothelialcell swelling during hemorrhagic shock. J Appl Physiol1992; 73:1467–73.22. Nolte D, Bayer M, Lehr HA, Becker M, Krombach F,Kreimeier U, Messmer K. Attenuation of postischemicmicrovascular disturbances in striated muscle byhyperosmolar saline dextran. Am J Physiol 1992;263:H1411–6.23. Ben Haim SA, Edoute Y, Hayam G, Better OS. Sodium modulatesinotropic response to hyperosmolarity in isolated workingrat heart. Am J Physiol 1992; 263:H1154–60.24. Selkurt EE, Post RS. Renal clearance of sodium in the dog:effect of increasing sodium load on reabsorptive mechanism.Am J Physiol 1950; 162:639–48.25. Shackford SR, Norton CH, Todd MM. Renal, cerebral, <strong>and</strong>pulmonary effects of hypertonic resuscitation in a porcinemodel of hemorrhagic shock. Surgery 1988; 104:553–60.26. Sondeen JL, Gonzaludo GA, Loveday JA, Rodkey WG, WadeCE. Hypertonic saline/dextran improves renal functionafter hemorrhage in conscious swine. Resuscitation 1990;20:231–41.27. Sc<strong>here</strong>r R, Giebler R, Kampe S, Kox WJ. Effects of hypertonicsaline hydroxyethyl starch solution on collageninducedplatelet aggregation <strong>and</strong> ATP secretion.Infusionsther Transfusionsmed 1994; 21:310–4.28. Hess JR, Dubick MA, Summary JJ, Bangal NR, Wade CE. Theeffects of 7.5% NaCl/6% dextran 70 on coagulation <strong>and</strong> plateletaggregation in humans. J <strong>Trauma</strong> 1992; 32:40–4.29. Reed RL, Johnston TD, Chen Y, Fischer RP. Hypertonicsaline alters plasma clotting times <strong>and</strong> platelet aggregation.J <strong>Trauma</strong> 1991; 31:8–14.30. Bergman A, Andreen M, Blomback M. Plasma substitutionwith 3% dextran-60 in orthopaedic surgery: influence onplasma colloid osmotic pressure, coagulation parameters,immunoglobulins <strong>and</strong> other plasma constituents. ActaAnaesthesiol Sc<strong>and</strong> 1990; 34:21–9.31. Moore GL, Summary JJ, Dubick MA, Ledford ME, Ryan BA,Gonzales A, Wade CE. Effects of hypertonic saline (7.5%)/dextran 70 on human red cell typing, lysis, <strong>and</strong> metabolismin vitro. Vox Sang 1990; 59:227–31.32. Keane RM, Birmingham W, Shatney CM, Winchurch RA,Munster AM. Prediction of sepsis in the multitraumaticpatient by assays of lymphocyte responsiveness. SurgGynecol Obstet 1983; 156:163–7.33. Napolitano LM, Faist E, Wichmann MW, Coimbra R.Immune dysfunction in trauma. Surg Clin North Am 1999;79:1385–416.34. Kim PK, Deutschman CS. Inflammatory responses <strong>and</strong>mediators. Surg Clin North Am 2000; 80:885–94.35. Rackow EC, Astiz ME. Mechanisms <strong>and</strong> management ofseptic shock. Crit <strong>Care</strong> Clin 1993; 9:219–37.36. Shoemaker WC, Kvetan V, Fyodorov V, Kram HB. Clinicalalgorithm for initial fluid resuscitation in disasters. Crit<strong>Care</strong> Clin 1991; 7:363–81.37. Rhee P, Burris D, Kaufmann C, Pikoulis M, Austin B, LingG, Harviel D, Waxman K. Lactated Ringer’s solutionresuscitation causes neutrophil activation after hemorrhagicshock. J <strong>Trauma</strong> 1998; 44:313–9.38. Junger WG, Coimbra R, Liu FC, Herdon-Remelius C, JungerW, Junger H, Loomis W, Hoyt DB, Altman A. Hypertonic salineresuscitation: a tool to modulate immune function intrauma patients? Shock 1997; 8:235–41.39. Coimbra R, Junger WG, Hoyt DB, Liu FC, Loomis WH, EversMF. Hypertonic saline resuscitation restores hemorrhage-in-10
ITACCS Summer 2002duced immunosuppression by decreasing prostagl<strong>and</strong>in E2<strong>and</strong> interleukin-4 production. J Surg Res 1996; 64:203–9.40. Oi Y, Aneman A, Svensson M, Ewert S, Dahlqvist M,Haljamae H. Hypertonic saline-dextran improves intestinalperfusion <strong>and</strong> survival in porcine endotoxin shock. Crit<strong>Care</strong> Med 2000; 28:2843–50.41. Wade CE, Hannon JP, Bossone CA, Hunt MM, Loveday JA,Coppes RI Jr, Gildengorin VL. Neuroendocrine responsesto hypertonic saline/dextran resuscitation followinghemorrhage. Circ Shock 1991;35:37–43.42. Somell A, Suneson A, Riddez L, Sollevi A, Hjelmqvist H.Effect of rescue flow (HSD) on oxygen-related variables inLPS-induced endotoxin shock in pigs. Acta Anaesth Sc<strong>and</strong>2001; 45(115):63.43. Somell A, Suneson A, Riddez L, Sollevi A, Hjelmqvist H.Treatment with rescue flow (hypertonic saline/dextran) onLPS-induced septic shock in anaesthetized pigs. Intensive<strong>Care</strong> Med 2000; 26:S258.44. Cross JS, Gruber DP, Gann DS, Singh AK, Moran JM,Burchard KW. Hypertonic saline attenuates the hormonalresponse to injury. Ann Surg 1989; 209:684–91.45. Bellamy RF. The causes of death in conventional l<strong>and</strong>warfare: implications for combat casualty care research.Mil Med 1984; 149:55–62.46. Smith JP, Bodai BI, Hill AS, Frey CF. Prehospital stabilizationof critically injured patients: a failed concept. J<strong>Trauma</strong> 1985; 25:65–70.47. Lewis FR, Jr.. Prehospital intravenous fluid therapy: physiologiccomputer modelling. J <strong>Trauma</strong> 1986; 26:804–11.48. Border JR, Lewis FR, Aprahamian C, Haller JA, Jacobs LM,Luterman A. Panel: prehospital trauma care—stabilize orscoop <strong>and</strong> run. J <strong>Trauma</strong> 1983; 23:708–11.49. Kaweski SM, Sise MJ, Virgilio RW. The effect of prehospitalfluids on survival in trauma patients. J <strong>Trauma</strong> 1990;30:1215–8.50. Chudnofsky CR, Dronen SC, Syverud SA, Hedges JR, ZinkBJ. Early versus late fluid resuscitation: lack of effect inporcine hemorrhagic shock. Ann Emerg Med 1989;18:122–6.51. Pepe PE, Eckstein M. Reappraising the prehospital care ofthe patient with major trauma. Emerg Med Clin North Am1998; 16:1–15.52. American College of Surgeons Committee on <strong>Trauma</strong>.Chapter 3: Shock, In Advanced <strong>Trauma</strong> Life Support® forDoctors: Instructor Course Manual. Chicago, AmericanCollege of Surgeons, 1997, pp 97–146.53. Bickell WH, Wall MJ Jr, Pepe PE, Martin RR, Ginger VF,Allen MK, Mattox KL. Immediate versus delayed fluidresuscitation for hypotensive patients with penetratingtorso injuries. N Engl J Med 1994; 331:1105–9.54. Dalton AM. Prehospital intravenous fluid replacement intrauma: an outmoded concept? J R Soc Med 1995;88:213P–6P.55. Bickell WH, Bruttig SP, Millnamow GA, O’Benar J, WadeCE. Use of hypertonic saline/dextran versus lactatedRinger’s solution as a resuscitation fluid after uncontrolledaortic hemorrhage in anesthetized swine. Ann Emerg Med1992; 21:1077–85.56. Wade CE, Kramer GC, Grady JJ, Fabian TC, Younes RN.Efficacy of hypertonic 7.5% saline <strong>and</strong> 6% dextran-70 intreating trauma: a meta-analysis of controlled clinicalstudies. Surgery 1997; 122:609–16.57. Bunn F, Roberts I, Tasker R, Akpa E. Hypertonic versusisotonic crystalloid for fluid resuscitation in critically illpatients. Cochrane Database Syst Rev 2000; CD002045.58. Younes RN, Aun F, Accioly CQ, Casale LP, Szajnbok I,Birolini D. Hypertonic solutions in the treatment ofhypovolemic shock: a prospective, r<strong>and</strong>omized study inpatients admitted to the emergency room. Surgery 1992;111:380–5.59. Maningas PA, Mattox KL, Pepe PE, Jones RL, Feliciano DV,Burch JM. Hypertonic saline-dextran solutions for theprehospital management of traumatic hypotension. Am JSurg 1989; 157:528–33.60. Vassar MJ, Perry CA, Gannaway WL, Holcroft JW. 7.5%sodium chloride/dextran for resuscitation of traumapatients undergoing helicopter transport. Arch Surg 1991;126:1065–72.61. Vassar MJ, Perry CA, Holcroft JW. Prehospital resuscitationof hypotensive trauma patients with 7.5% NaCl versus7.5% NaCl with added dextran: a controlled trial. J <strong>Trauma</strong>1993; 34:622–32.62. Younes RN, Aun F, Ching CT, Goldenberg DC, Franco MH,Miura FK, Santos SS, Sequeiros IM, Rocha e Silva, FujimuraI, Birolini D. Prognostic factors to predict outcomefollowing the administration of hypertonic/hyperoncoticsolution in hypovolemic patients. Shock 1997; 7:79–83.63. Vassar MJ, Fischer RP, O’Brien PE, Bachulis BL, ChambersJA, Hoyt DB, Holcroft JW. A multicenter trial for resuscitationof injured patients with 7.5% sodium chloride. Theeffect of added dextran 70. The Multicenter Group for theStudy of Hypertonic Saline in <strong>Trauma</strong> Patients. Arch Surg1993; 128:1003–11.64. Vassar MJ, Perry CA, Holcroft JW. Analysis of potential risksassociated with 7.5% sodium chloride resuscitation oftraumatic shock. Arch Surg 1990; 125:1309–15.65. Wade C, Grady J, Kramer G. Efficacy of hypertonic salinedextran (HSD) in patients with traumatic hypotension:meta-analysis of individual patient data. Acta AnaesthesiolSc<strong>and</strong> Suppl 1997; 110:77–9.66. LeLorier J, Gregoire G, Benhaddad A, Lapierre J, DerderianF. Discrepancies between meta-analyses <strong>and</strong> subsequentlarge r<strong>and</strong>omized, controlled trials. N Engl J Med 1997;337:536–42.67. Olsson J, Svensen CH. The use of hypertonic-salinedextran in the prehospital setting. <strong>Trauma</strong><strong>Care</strong> Fall/Winter2001; 11(2):85.68. Chesnut RM, Marshall LF, Klauber MR, Blunt BA, BaldwinN, Eisenberg HM, Jane JA, Marmarou A, Foulkes MA. Therole of secondary brain injury in determining outcomefrom severe head injury. J <strong>Trauma</strong> 1993; 34:216–22.69. Cooper DJ. Hypertonic saline resuscitation for headinjured patients. <strong>Critical</strong> <strong>Care</strong> <strong>and</strong> Resuscitation 1999;1:157–61.70. Chesnut RM. Secondary brain insults after head injury:clinical perspectives. New Horiz 1995; 3:366–75.71. Fearnside MR, Cook RJ, McDougall P, McNeil RJ. TheWestmead Head Injury Project outcome in severe headinjury: a comparative analysis of pre-hospital, clinical <strong>and</strong>CT variables. Br J Neurosurg 1993; 7:267–79.11
ITACCS Summer 200272. Wade CE, Grady JJ, Kramer GC, Younes RN, Gehlsen K,Holcroft JW. Individual patient cohort analysis of theefficacy of hypertonic saline/dextran in patients withtraumatic brain injury <strong>and</strong> hypotension. J <strong>Trauma</strong> 1997;42:S61–5.73. Bouma GJ, Muizelaar JP, B<strong>and</strong>oh K, Marmarou A. Bloodpressure <strong>and</strong> intracranial pressure-volume dynamics insevere head injury: relationship with cerebral blood flow. JNeurosurg 1992; 77:15–9.74. Hamilton SM, Breakey P. Fluid resuscitation of the traumapatient: how much is enough? Can J Surg 1996; 1:11–6.75. Shackford SR, Bourguignon PR, Wald SL, Rogers FB, OslerTM, Clark DE. Hypertonic saline resuscitation of patientswith head injury: a prospective, r<strong>and</strong>omized clinical trial. J<strong>Trauma</strong> 1998; 44:50–8.76. Bourguignon PR, Shackford SR, Shiffer C, Nichols P, NeesAV. Delayed fluid resuscitation of head injury <strong>and</strong> uncontrolledhemorrhagic shock. Arch Surg 1998; 133:390–8.77. Prough DS, Johnson JC, Stump DA, Stullken EH, Poole GV,Jr., Howard G. Effects of hypertonic saline versus lactatedRinger’s solution on cerebral oxygen transport duringresuscitation from hemorrhagic shock. J Neurosurg 1986;64:627–32.78. Schmoker JD, Zhuang J, Shackford SR. Hypertonic fluidresuscitation improves cerebral oxygen delivery <strong>and</strong>reduces intracranial pressure after hemorrhagic shock. J<strong>Trauma</strong> 1991; 31:1607–13.79. Prough DS, Whitley JM, Taylor CL, Deal DD, DeWitt DS.Rebound intracranial hypertension in dogs after resuscitationwith hypertonic solutions from hemorrhagic shockaccompanied by an intracranial mass lesion. J NeurosurgAnesthesiol 1999; 11:102–11.80. Khanna S, Davis D, Peterson B, Fisher B, Tung H,O’Quigley J, Deutsch R. Use of hypertonic saline in thetreatment of severe refractory posttraumatic intracranialhypertension in pediatric traumatic brain injury. Crit <strong>Care</strong>Med 2000; 28:1144–51.81. Riddez L, Hahn RG, Suneson A, Hjelmqvist H. Central <strong>and</strong>regional hemodynamics during uncontrolled bleedingusing hypertonic saline dextran for resuscitation. Shock1998; 10:176–81.82. Riddez L, Drobin D, Sjostr<strong>and</strong> F, Svensen CH, Hahn RG.Lower dose of hypertonic saline dextran reduces the riskof lethal rebleeding in uncontrolled hemorrhage. Shock2002; 17(5): 377–82.83. Bickell WH, Bruttig SP, Millnamow GA, O’Benar J, WadeCE. The detrimental effects of intravenous crystalloid afteraortotomy in swine. Surgery 1991; 110:529–36.84. Kowalenko T, Stern S, Dronen S, Wang X. Improvedoutcome with hypotensive resuscitation of uncontrolledhemorrhagic shock in a swine model. J <strong>Trauma</strong> 1992;33:349–53.85. Lechleuthner A, Lefering R, Bouillon B, Lentke E, VorwegM, Tiling T. Prehospital detection of uncontrolledhaemorrhage in blunt trauma. Eur J Emerg Med 1994;1:13–8.86. Kramer GC, Poli de Figueiredo LF. Hypertonic 7.5% saline:evaluations of efficacy <strong>and</strong> safety from human trials. InOkada K, Ogata H, eds. Third <strong>International</strong> ShockCongress. Amsterdam, Elsevier Science, 1996, pp 363–8.Blunt Abdominal AorticTransection in an Abused Child:A Case Report <strong>and</strong> a LiteratureReviewRoya Yumul, MD, PhDZoreh Steffens, MDStephen N. Steen, ScD, MDCalvin Johnson, MDDepartment of AnesthesiologyMartin Luther King, Jr., HospitalCharles R. Drew University of Medicine & ScienceLos Angeles CA 90059 USAe-mail: ryumul@dhs.co.la.ca.usLearning Objectives: 1) To identify the indicators ofabdominal aortic injury in children after blunttrauma, 2) to review diagnostic options for pediatricpatients with blunt abdominal trauma, <strong>and</strong> 3) toappreciate the advantages/disadvantages of clamp<strong>and</strong>-sewversus intraoperative bypass techniques.AbstractBlunt abdominal aortic trauma is most frequentlycaused by motor vehicle crashes. We report thesecond successful management, to our knowledge, ofa case of pediatric abdominal aortic trauma caused byknown child abuse <strong>and</strong> resulting in almost completetransection of the abdominal aorta.Case ReportA 2 1 ⁄2-year-old girl (16 kg, 65 cm) was brought to theemergency department by paramedics, who stated that she hadreportedly been thrown against a couch by her mother’sboyfriend. The child was lethargic at the scene with bleedingfrom a scalp laceration <strong>and</strong> had not lost consciousness.Upon arrival in the trauma emergency department, thechild was lethargic with a Glasgow Coma Scale (GSC) score of6 (E4, M1, V1). She was not crying; slow movement of theupper extremities <strong>and</strong> no movement of the lower extremitieswere observed. She presented with the following vital signs:blood pressure, 67/41 mmHg; heart rate, 120/150 beats/min;respiratory rate, 20 to 32 breaths/min; <strong>and</strong> temperature, 33 o C;O 2saturation was 90%. Physical examination revealed adistended, tense abdomen, with no bowel sounds. The lowerextremities were bluish <strong>and</strong> cold with no palpable pulsesbelow the femoral vessels. Two intravenous lines (18 gauge)were placed in the upper extremities. A blood sample was sentfor type <strong>and</strong> crossmatch. The patient was intubated with a 4.5endotracheal tube <strong>and</strong> was resuscitated using fluids. Radiographsof the chest, pelvis, <strong>and</strong> C-spine were normal with nosign of fractures. Hemoglobin concentration was 6.0 g/dL.12
ITACCS Summer 2002A computed tomography (CT) scan of the head showedbilateral occipital subdural effusion (hygroma), no intracranialhemorrhage, no fractures, <strong>and</strong> no shifting or mass effect; CT ofthe abdomen showed a hematoma (right>left). The hematomaappeared to involve the right kidney as well as possible injuriesof the liver, spleen, <strong>and</strong> aorta. The patient was taken to theoperating room suite for exploratory laparotomy. On admissionto the operating room, the patient was profoundly acidotic:arterial blood gas analysis showed a pH of 7.19, PaCO 2of 21mmHg, PaO 2of 180 mmHg, HCO 3of 8.0 mEq/L, base deficit of19.1 mEq/L, O 2saturation of 97.7%, <strong>and</strong> Hgb of 5.5 g/dL.St<strong>and</strong>ard monitoring was used. A right 20-gauge arterialline <strong>and</strong> a right internal jugular double-lumen catheter wereplaced. Fluid warmer, Bair hugger, warming blanket, <strong>and</strong>autologous red blood cell salvage machine were used. Fluidresuscitation with crystalloids, albumin, <strong>and</strong> blood transfusionwas started prior to incision. Sodium bicarbonate was administeredfor normalization of profound acidemia. Laparotomydemonstrated a massive central hematoma extending all theway from the liver down to the pelvis. Two hundred millilitersof free blood were found in the abdomen. The spleen <strong>and</strong> liverappeared to be normal.A quick mesenteric surgical approach was used. Furt<strong>here</strong>xploration of the retroperitoneal hematoma revealed almostcomplete transection of the aorta approximately 3 cm belowthe infrarenal artery, which was tamponaded by the massiveretroperitoneal hematoma. When clamps were placedsuprarenally <strong>and</strong> infrarenally <strong>and</strong> on both renal arteries, it wasnoted that the aorta was 98% transected below the renal artery<strong>and</strong> was being held together by only a few millimeters ofadventitia. A right kidney contusion with parenchymal damage<strong>and</strong> a right renal artery laceration were observed. A primaryend-to-end anastomosis (clamp-<strong>and</strong>-sew technique) <strong>and</strong> a rightrenal artery repair were performed.During the 6-hour procedure, aortic cross clamp time was1.5 hours, with an estimated blood loss of 2,500 ml <strong>and</strong> a urineoutput of 20 ml. During the anesthetic course, 3 units of packedred blood cells; 10 units of platelets; 1 unit of fresh frozenplasma; 250 ml blood from the red cell saver; 300 ml normalsaline, 9%; 1,200 ml lactated Ringer’s solution, 500 ml; <strong>and</strong> 5%albumin were given. Prior to exit from the operating room thepatient had a hemoglobin concentration of 13 g/dL, hematocritof 38%, <strong>and</strong> platelet count of 98,000/mm 3 . Electrolytes werewithin normal limits, except for a blood urea nitrogen of 26mg/dL <strong>and</strong> a creatinine concentration of 1.4 mg/dL.Following the operative procedure, biphasic Dopplersignals on both right <strong>and</strong> left posterior tibial <strong>and</strong> dorsalis pedisarteries were normal. After surgery, the patient was admitted tothe pediatric intensive care unit (ICU). She was extubated on the6th postoperative day, discharged from the ICU on the 10thpostoperative day, <strong>and</strong> sent home on the 21st postoperative day.DiscussionBlunt abdominal aortic trauma, a rarely reported injury, ismost frequently caused by motor vehicle crashes. 1 It carries ahigh mortality rate <strong>and</strong> significant morbidity for those patientswho survive. Most reported injuries have occurred in adults oradolescents <strong>and</strong> include intimal disruption (with or withoutthrombosis), pseudoaneurysm, stenosis, <strong>and</strong> distal embolizationof atheromatous debris. Of all aortic injuries, only 4% to8% occur below the diaphragm. 2The hallmark of abdominal aortic injury is the triad of bluntabdominal trauma, acute arterial insufficiency, <strong>and</strong> lowerextremityparalysis. In patients with lower extremity sensorymotor deficits, spinal cord injury is to be suspected. However,pulses may be present distal to an arterial injury. Griffen 3 emphasizedthe importance of bilateral femoral bruits in association withunexplained shock <strong>and</strong> flank ecchymosis as being diagnostic,although the latter sign is not commonly reported. In this case,the child presented in similar fashion to other children asreported in the literature (i.e., in shock with cold, pulseless lowerextremities but no lower-extremity flaccid paralysis).Abdominal aortic aneurysms were first described by Vesaliusin the sixteenth century, 4 but aortic injuries secondary to blunttrauma have been reported infrequently in the literature. <strong>Trauma</strong>ticaortic rupture (TAR) in the pediatric age group (
ITACCS Summer 2002namically unstable patient who requires emergency operation.Transesophageal echocardiography (TEE) can be performedrapidly in the operating room, allowing expeditious diagnosisof thoracic aortic injury <strong>and</strong> selection of the required operativeapproach. TEE <strong>and</strong> aortography were not indicated in our casebecause the diagnosis was confirmed intraoperatively.It is possible to perform this operation <strong>and</strong> repair this injurywith a clamp-<strong>and</strong>-sew technique <strong>and</strong> achieve good results. 10 Themajority of adults undergo graft interpositions or bypass. Aorticcross clamp time beyond 30 minutes is associated with paraplegia.In our case (the patient being hemodynamically stable), theclamp-<strong>and</strong>-sew approach was used. The advantages of clamp <strong>and</strong>sew are simplicity <strong>and</strong> the lack of need for heparin. Thisapproach has received significant support in recent literature. Asignificant controversy has developed over whether t<strong>here</strong> aredifferences in result comparing direct repair (clamp <strong>and</strong> sew)with techniques that provide distal aortic perfusion duringrepair. Specifically, is the risk of paraplegia, the most significantcomplication of repair, lowered by distal aortic perfusiontechniques? An advantage of bypass techniques is that the distalaorta is perfused, which may decrease the rate of paraplegia aswell as reduce ischemia <strong>and</strong> reperfusion injuries associated withsacrifice of hepatic, renal, <strong>and</strong> mesenteric flow during clamp<strong>and</strong>-sewrepair. Disadvantages of partial <strong>and</strong> full bypass are theneed for systemic heparinization, which may increase the risk ofbleeding complications. Our patient, with an aortic clamp timeof 1.5 hr, did not show any sign of spinal cord injury.The preference for operative repair remains the clamp-<strong>and</strong>sewtechnique in the child with multiple trauma. It is interestingthat children with spinal myelopathy have demonstrated bothshort- <strong>and</strong> long-term recovery from the deficits. T<strong>here</strong> have beenlimited reports of neurologic <strong>and</strong> functional improvement inpatients who have sustained postoperative paraplegia or paraparesis.It remains to be shown whether children can sustainspinal cord ischemia longer than adults or whether the pediatricspinal cord has more protective or regenerative capabilities. 11Reisman <strong>and</strong> Morgan 7 reported a case involving a 17-yearoldmale, a passenger wearing a seat belt, who sustained an abdominalaortic injury during a motor vehicle crash. At operation,the patient was noted to have a complete transection of the intimafrom a point 2 cm below the renal artery to about 1.5 cmabove the bifurcation. Unfortunately, he had a complicated postoperativecourse, remaining paraplegic with minimal return ofsensitivity <strong>and</strong> ultimately being transferred to a rehabilitationhospital. The authors believed this was a case of anterior spinalartery syndrome (characterized by incontinence <strong>and</strong> paraplegia).It appears that the first successful repair of abdominalaortic disruption caused by blunt trauma was reported byLevien <strong>and</strong> Chleboun in 1983. 12 Their patient was a 17-year-oldwho fell from his motorcycle while crossing an elevation in thetrack. The cycle l<strong>and</strong>ed on his abdomen. If this case is consideredin the pediatric category, then this would be the firstreported pediatric TAR. Kyösola <strong>and</strong> Järvinen 13 reported thesecond case, a 13-year-old boy who was trapped <strong>and</strong> crushedbetween a lorry <strong>and</strong> a trailer. Since the event occurred 11 yearsbefore the report was published, it would be the first descriptionof a pediatric survivor of TAR.In a relatively recent autopsy case review of 142 fatal casesof blunt injuries of the aorta, Feczko et al 2 listed only 9 cases ofabdominal aortic laceration (6%) <strong>and</strong> one of child abuse.Unfortunately, the report does not indicate whether the abusedchild had a TAR nor the age of the child.In 1999, Urwin <strong>and</strong> Ridley 14 stated that survival of patientsafter emergency repair of abdominal aortic aneurysm is poorthough such aneurysms are common. The authors cited anincidence of 17 to 64 per 100,000 population in the UnitedKingdom. It should be noted that this figure was not inrelation to blunt injury of the abdominal aorta.The question as to whether outcome is better if bluntinjury of the abdominal aorta is treated in specialized vascularsurgical services 15 than in nonspecialized general units 16 is notparticularly germane when we consider the pediatric patient.However, for very young patients with this injury, pediatrictrauma surgeons would be required.Many more children are abused than official statisticsshow. The majority of children victimized are younger than 7years of age, <strong>and</strong> deaths occur most often in children aged 3<strong>and</strong> under. The article by Fox et al 6 <strong>and</strong> ours add to the small,but growing, number of reports of pediatric TAR.References1. Cox EF. Blunt abdominal trauma: a 5-year analysis of 870patients requiring celiotomy. Ann Surg 1984; 149:467–74.2. Feczko JD, Lynch L, Pless JE, et al. An autopsy case reviewof 142 nonpenetrating (blunt) injuries of the aorta. J<strong>Trauma</strong> 1992; 33:8–16.3. Griffen WO Jr, Belin RP, Walder AI. <strong>Trauma</strong>tic aneurysm ofthe abdominal aorta. Surgery 1960; 60:817.4. http://rev’g-rad.rwjuh.edu/rad web/aa.ht <strong>and</strong> Welborn MBJr, Sawyers JL. Acute abdominal aortic occlusion due tonon-penetrating trauma. Am J Surg 1969; 118:112–6.5. Trachiotis GD, Sell JF, Pearson ED, et al. <strong>Trauma</strong>tic thoracicaortic rupture in the pediatric patient. Ann Thorac Surg1996; 62:724–32.6. Fox JT, Huang YC, Bereia PI, et al. Blunt abdominal aortic transectionin a child: case report. J <strong>Trauma</strong> 1996; 41:1051–3.7. Reisman JD, Morgan AS. Analysis of 46 intra-abdominalaortic injuries from blunt trauma: case reports <strong>and</strong>literature review. J <strong>Trauma</strong> 1990; 30:1294–7.8. Blute R, Ray F. <strong>Trauma</strong>tic dissecting aneurysm of theabdominal aorta. J Maine Med Assoc 1973; 64:164–6.9. Brathwaite CEM, Rodriguez A. Injuries of the abdominalaorta from blunt trauma. Am Surg 1992; 58:350–2.10. Sweeney MS, Young JD, Frazier OH, et al. <strong>Trauma</strong>tic aortictransections: eight-year experience with the “clamp-sew”technique. Ann Thorac Surg 1997; 64:384–9.11. Von Oppell UO, Dunne TT, De Groot CM, et al. <strong>Trauma</strong>ticaortic rupture: a twenty-year metaanalysis of mortality <strong>and</strong>risk of paraplegia. Ann Thorac Surg 1994; 8:585–93.12. Levien LJ, Chleboun JO. Survival after blunt traumatic ruptureof the abdominal aorta. S Afr J Surg 1983; 21:251–4.13. Kyösola K, Järvinen A. Abdominal aortic aneurysm <strong>and</strong> dissectionafter blunt trauma. J Cardiovasc Surg 1987; 28:737–9.14. Urwin SC, Ridley SA. Prognostic indicators following emergencyaortic aneurysm repair. <strong>Anesthesia</strong> 1999; 54:739–44.15. Nathens AB, Turkovich GJ, Maier RV, et al. Relationshipbetween trauma center volume <strong>and</strong> outcomes. JAMA 2001;285:1164–71.16. Dudley RA, Johansen KL, Br<strong>and</strong> R, et al. Selective referralto high volume hospitals: estimating potential avoidabledeaths. JAMA 2000; 283:1159–66.14
ITACCS Summer 2002A Case of Multiple Blunt InjuriesTreated with EmergencyDepartment Thoracotomy <strong>and</strong>Extracorporeal Life SupportTaichi Takeda, MD*Yutaka Taira, MD*Itaru Takara, MD†Kazuhiro Sugahara, MD†Yoshihiko Yoshii, MD*Emergency Unit* <strong>and</strong> Intensive <strong>Care</strong> Unit†Ryukyu University HospitalUniversity of the Ryukyus School of MedicineUehara 207, Nishihara-choOkinawa 903-0215, Japane-mail: taictake-da@umin.ac.jpLearning Objectives: 1) To underst<strong>and</strong> the indicationsfor thoracotomy during resuscitation of trauma patientsin the emergency department <strong>and</strong> 2) to appreciate therole of extracorporeal life support in the managementof posttraumatic acute respiratory failure.AbstractA 7-year-old girl was run over on her chest <strong>and</strong> abdomenby a tank truck. She sustained cardiac arrest in theemergency department due to hemorrhagic shock <strong>and</strong> bilateraltension hemopneumothorax, despite no apparentthoracic surface injury. Resuscitation was achieved withemergency department thoracotomy <strong>and</strong> internal cardiacmassage. The patient was also noted to have brain concussion,m<strong>and</strong>ibular fracture, <strong>and</strong> dorsal degloving injury. Laparotomyrevealed hepatic <strong>and</strong> mesenteric injuries, intestinallacerations, <strong>and</strong> pancreatic transection. Once bleedingwas controlled, a distal pancreatectomy was performed.Massive intrabronchial bleeding from left bronchial <strong>and</strong>pulmonary injuries was controlled by a bronchial balloontamponade technique. Respiratory insufficiency caused bybilateral pulmonary contusions <strong>and</strong> a left intrabronchial clotwas managed by conventional ventilation strategies. However,the respiratory index deteriorated, <strong>and</strong> extracorporeallife support (ECLS) was begun on the second hospital day.After 18 days of ECLS, pulmonary function was recovered<strong>and</strong> periodic suctioning successfully removed clots in theleft lower lobular bronchus with further improvement inoxygenation. The patient was extubated on the 30th hospitalday <strong>and</strong> suffered posttraumatic epilepsy, which becamewell controlled with antiepileptic agents. She eventually returnedto her elementary school activities in 6 months.We describe the assessment <strong>and</strong> treatment of this 7-year-old patient following a motor vehicle incident resultingin severe blunt trauma <strong>and</strong> cardiopulmonary arrest,who survived <strong>and</strong> fully recovered a rare scenario of pediatricmultiple injuries. In particular, the application of emergencydepartment thoracotomy <strong>and</strong> ECLS played a criticalrole in supporting this child with multisystem trauma.The value of emergency department thoracotomy for blunttrauma has been questioned because of its poor prognosis;however, the technique could be beneficial for pediatricpatients who demonstrate “salvageability” on arrival. Thepliability of a child’s chest wall may result in heart <strong>and</strong> pulmonarydamage without overlying injury, in which case resuscitativethoracotomy may reveal reparable internal injury.The management of severe pulmonary contusions isextremely challenging when complicated with bronchial injuryin multisystem trauma patients. The adjunctive use of extracorporeallife support (ECLS) for lethal acute respiratory failurehas played a critical role in supporting such patients.In this case report, we describe a child with multiple bluntinjuries, including brain concussion, m<strong>and</strong>ibular fracture,severe bilateral pulmonary contusions, injury of the left mainbronchus, blunt cardiac injury, liver injury, pancreatic transection,mesenteric injuries, intestinal lacerations, <strong>and</strong> a dorsaldegloving injury. The patient was resuscitated successfully withemergency department thoracotomy <strong>and</strong> managed on ECLS for2 weeks for posttraumatic acute respiratory failure.Case ReportA 7-year-old girl was run over on her chest <strong>and</strong> abdomen by atank truck. External bleeding was not noted at the scene. She waslethargic <strong>and</strong> brought to our hospital by an emergency medicalteam. On arrival, during the primary survey, she sustained a witnessedcardiac arrest. Resuscitation was achieved with tracheal intubation,left thoracotomy, internal cardiac massage, right pleuraldrainage, <strong>and</strong> intravenous epinephrine infusion in the emergencydepartment. Tension hemopneumothorax <strong>and</strong> pulmonary contusionswere recognized when the thoracotomy was performed.After the resuscitation, on an FiO 2of 1.0, blood gas analysisresulted a PaCO 2of 61.8 mmHg, a PaO 2of 116.4 mmHg, <strong>and</strong> pH of6.97. Since she had demonstrated guarding during earlier abdominalexaminations, she underwent laparotomy, which revealed gradeIV liver injuries, mesenteric injuries, intestinal lacerations, <strong>and</strong> agrade III pancreatic transection. Peritoneal bleeding was controlledsurgically <strong>and</strong> distal pancreatectomy was performed. During theoperation, increased bronchial bleeding from coagulopathy due tohemorrhage, dilution, <strong>and</strong> hypothermia was noted. Left bronchialrupture at the division of upper <strong>and</strong> lower lobe bronchus wasdiagnosed by fiberoptic bronchoscopy. Since a size-appropriatedouble-lumen endotracheal tube was not available for isolation ofthe lung, massive intrabronchial bleeding from the left bronchial<strong>and</strong> pulmonary injury was controlled by a bronchial balloontamponade technique using a Fogarty catheter placed in the leftmain bronchus proximal to the injury for 4 hours (Figure 1). Totalbleeding from the time of incident to the end of operation wasestimated at 3,000 ml, <strong>and</strong> resuscitation included the infusion of2,100 ml of crystalloid <strong>and</strong> 2,800 ml of blood.After surgical hemostasis was achieved, the patient was admittedto the intensive care unit. Management of respiratoryinsufficiency resulting from bilateral pulmonary contusions <strong>and</strong>a left intrabronchial clot was attempted by increased FiO 2, positiveend-expiratory pressure ventilation, pressure-controlledinverse-ratio ventilation, prone ventilation, <strong>and</strong> permissive hypercapnia.However, a hemopneumopericardium developed,<strong>and</strong> the patient’s subcutaneous <strong>and</strong> mediastinal emphysemaworsened. Although the pericardium was opened <strong>and</strong> drainedthrough a subxiphoid window <strong>and</strong> bilateral pleural drainage15
ITACCS Summer 2002bleeding complication was noted as a right hemothorax, <strong>and</strong>surgical hemostasis <strong>and</strong> drainage were performed throughright thoracotomy. Considering the balance between improvedpulmonary function <strong>and</strong> the added risk of coagulopathy, shewas weaned from ECLS over 2 days; ECLS was terminated onthe 18th day of its course. Right femoral cannulas wereremoved <strong>and</strong> vessels were surgically reconstructed. On the22nd hospital day, the clot obstructing the left lower lobularbronchus cleared <strong>and</strong> respiratory function improved drastically.The patient was extubated successfully after 30 days of intensivecare therapy <strong>and</strong> transferred to a general ward. Shesuffered posttraumatic epilepsy, which was well controlled withantiepileptic agents. She left the hospital for home with fullrecovery in 4 months after the incident <strong>and</strong> returned to <strong>here</strong>lementary school activities in 6 months.Figure 1. Chest radiograph immediately after surgery. Left mainbronchus was blocked by balloon catheter, <strong>and</strong> the left lungshowed intrabronchial hemorrhage <strong>and</strong> atelectasis. Since the leftlung was not exp<strong>and</strong>ed, the left pleural fluid has not drainedsufficiently. In the right lung, pulmonary contusion <strong>and</strong>overexpansion were observed.was doubled <strong>and</strong> secured, her respiratory function deteriorated.On an FiO 2of 1.0, a respiratory rate of 30 breaths/min, a positiveend-expiratory pressure of 15 cm H 2O, <strong>and</strong> peak inspiratorypressure of 30 cmH 2O, blood gas analysis revealed a PaCO 2of 42.3 mmHg <strong>and</strong> a PaO 2of 32.4 mmHg.Although a pulmonary artery catheter was not inserted tomeasure transpulmonary shunt, in response to this deterioratingoxygenation, ECLS was initiated on the second hospital day.ECLS flow via the right femoral vein <strong>and</strong> artery was established at2.0 L/min, contributing about 50% of cardiac output. Theextracorporeal circuit consisted of a centrifugal pump <strong>and</strong> ahollow-fiber oxygenator (Terumo Corporation, Tokyo, Japan);the entire extracorporeal system was heparin coated. The wholeblood activated clotting time was kept between 180 <strong>and</strong> 220 secwith continuous infusions of heparin sodium, 300 to 400 IU/hr,<strong>and</strong> nafamostat mesilate, 2.0 to 2.5 mg/hr (Futhan®, ToriiPharmaceutical Co., Ltd, Tokyo, Japan) (a protease inhibitor).The circuit was replaced every 3 days to maintain oxygenativeability of the hollow fibers. During ECLS, ventilatory settingswere reduced to an FiO 2of 0.35, a respiratory rate of 17 breaths/min, a positive end-expiratory pressure of 5 cm H 2O, <strong>and</strong> tidalvolume of 100 ml in order to minimize barotrauma <strong>and</strong> oxygentoxicity. Meticulous pulmonary toilet <strong>and</strong> positional drainage ofairway secretions were maintained throughout the course ofECLS. Vigorous lavage <strong>and</strong> suctioning were performed periodicallyif secretions were copious. Liquid ventilation was notavailable in our institute. The patient was sedated with continuousinfusion of morphine, midazolam, <strong>and</strong> propofol. Systemicantibiotics were given to prevent surgical wound infection.Central hyperalimentation <strong>and</strong> enteral feedings via nasogastrictube were provided, <strong>and</strong> optimization of oxygen delivery bytransfusion, selective use of inotropic agents, <strong>and</strong> carefulintravascular volume management was achieved.After 2 weeks of ECLS, the patient’s pulmonary functionrecovered gradually. Sixteen days into the ECLS course, aDiscussionEnthusiasm for emergency department thoracotomy haswaned over the past several years. The survival of patientsreceiving emergency department thoracotomy is less than 5%,<strong>and</strong> the mortality rate is significantly higher when it is performedfor blunt injury. 1 T<strong>here</strong>fore, it is reported that thoracotomy isindicated only in select patients who have vital signs at the sceneor upon arrival in the emergency department, or if the patient isexperiencing witnessed deterioration or cardiac arrest. 2Our pediatric patient was awake but agitated at the scene<strong>and</strong> deteriorated during transport to our hospital. The cardiacarrest was witnessed by a trauma surgeon on arrival at theemergency department, <strong>and</strong> thoracotomy <strong>and</strong> internal cardiacmassage were performed immediately. Tension hemopneumothoraxwas not apparent before the arrest despite carefulphysical examination, done while awaiting the results of imagingstudies. The flexibility of a child’s chest wall might result inorgan damage without overlying injury, <strong>and</strong> the mobility ofmediastinal structures might predispose a child to tensionpneumothorax. In these situations, resuscitative thoracotomymay reveal reparable thoracic injury of lung, heart, aorta,esophagus, or diaphragm, as in this case, in which tensionhemopneumothorax <strong>and</strong> pulmonary contusions were found.Left thoracotomy also allows immediate access for clampocclusion of thoracic aorta if it were indicated for uncontrolledperitoneal bleeding. Although median sternotomy is anotheroption to allow superior exposure to the mediastinum, weprioritized the immediate access through left anterolateralthoracotomy using simple instruments for resuscitation.The technique of balloon tamponade (using the Fogartycatheter) to control endobronchial bleeding has been reportedpreviously. 3 In our case, this technique was effective for hemostasis<strong>and</strong> one-lung ventilation. However, this blockage resulted inleft endobronchial occlusion with clotted blood, which, togetherwith severe pulmonary contusion, led to severe respiratoryfailure. During the postoperative course, ECLS was initiatedsince conventional ventilatory support was failing.Accepted criteria for ECLS include patients with potentiallylethal respiratory failure with a transpulmonary shunt greaterthan 30%, who are unresponsive to conventional management<strong>and</strong> whose primary condition is reversible. 4–6 The therapeuticprinciple of ECLS is to ensure adequate oxygenation bypartially replacing pulmonary gas exchange. The lungs are notexposed to potential barotrauma <strong>and</strong> volutrauma from16
ITACCS Summer 2002mechanical ventilation or to oxygen toxicity from exposure totoxic FiO 2levels. T<strong>here</strong>fore, the lung is better able to healduring this period of rest <strong>and</strong> support. Furthermore, ECLSallows a margin of minutes for broncho-alveolar lavage, whichis particularly useful in a small pediatric airway.Hill et al reported the first adult case of trauma managed successfullywith prolonged ECLS in 1972. 7 A subsequent NationalInstitutes of Health-sponsored r<strong>and</strong>omized, multicenter, prospectivetrial failed to demonstrate improvement of survival in adultswith acute respiratory distress syndrome managed with ECLS. 8However, technology has changed considerably, <strong>and</strong> more recentstudies in adults suggest better survival. 5,9 An adult with multipleinjuries successfully treated with open heart massage in the operatingroom <strong>and</strong> ECLS was reported. 6 However, to our knowledge,survival <strong>and</strong> full recovery of a child with multiple injuries treatedwith combination of emergency department thoracotomy <strong>and</strong> ECLShave not been reported previously. In a retrospective review ofpediatric blunt trauma patients, Steiner et al 10 reported survival in4 of 6 cases treated with ECLS for respiratory failure. Althoughsignificant conclusions cannot be drawn from a limited experience,ECLS may prove useful in the treatment of posttraumatic acuterespiratory failure. Further evaluation will be necessary to determineselection criteria for this invasive technique.AcknowledgmentsPart of this report was presented at the 5th AnnualMeeting of Kyusyu Regional Association for Acute Medicine,Beppu, Ooita, Japan, May 12, 2001, <strong>and</strong> the 14th Annual<strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> Symposium <strong>and</strong> WorldExposition, San Diego, California, USA, May 17–19, 2001.This work was supported by University of the RyukyusSchool of Medicine.The authors thank institutional staff that care for patientsfor their professional assistance.References1. Branney SW, Moore EE, Feldhaus KM, Wolf RE. <strong>Critical</strong>analysis of two decades of experience with postinjury<strong>Trauma</strong><strong>Care</strong>200316th Annual <strong>Trauma</strong> <strong>Anesthesia</strong>& <strong>Critical</strong> <strong>Care</strong> SymposiumMay 15-17, 2003Dallas, Texashttp://www.itaccs.comemergency department thoracotomy in a regional traumacenter. J <strong>Trauma</strong> 1988; 45(1):87–94.2. Powell MA, McMahon D, Peitzman AB. Thoracic injury. InPeitzman AB, Rhodes M, Schwab CW, Yealy DM, eds. The<strong>Trauma</strong> Manual. Philadelphia, Lippincott-Raven Publishers,1998, pp 199–225.3. Kshettry VR, Bassett HF. The Fogarty balloon technique forthe control of endobronchial bleeding. Thorax 1983;38(8):640.4. Germann P, Ullrich R, Donner A, et al. Extracorporeal lungassist (ELA) in adults: indications <strong>and</strong> application. ActaAnaesthesiol Sc<strong>and</strong> Suppl 1997; 111:132–5.5. Michaels AJ, Schriener RJ, Kolla S, et al. Extracorporeal lifesupport in pulmonary failure after trauma. J <strong>Trauma</strong> 1999;46(4):638–45.6. Sasadeusz KJ, Long WB III, Kemalyan N, et al. Successfultreatment of a patient with multiple injuries using extracorporealmembrane oxygenation <strong>and</strong> inhaled nitric oxide.J <strong>Trauma</strong> 2000; 49:1126–8.7. Hill JD, O’Brien TG, Murray JJ, et al. Prolonged extracorporealoxygenation for acute post-traumatic respiratory failure(shock-lung syndrome): use of the Bramson membranelung. N Engl J Med 1972; 286(12):629–34.8. Zapol WM, Snider MT, Hill JG, et al. Extracorporeal membraneoxygenation in severe acute respiratory failure: a r<strong>and</strong>omizedprospective study. JAMA 1979; 242(20):2193–6.9. Anderson H 3rd, Shapiro MB, Delius RE, et al. Extracorporeallife support for respiratory failure after multiple trauma.J <strong>Trauma</strong> 1993; 37(2):266–72.10. Steiner RB, Adolph VR, Heaton JF, et al. Pediatric extracorporealmembrane oxygenation in posttraumatic respiratoryfailure. J Pediatr Surg 1991; 26(9):1011–5.SLAM Express One Day WorkshopEmergency & Rescue Airway ManagementAn intensive one-day workshop on all aspectsof emergency airway management:lectures, cricothyrotomy lab using medical specimens,<strong>and</strong> h<strong>and</strong>s-on workshop covering rescue ventilation<strong>and</strong> strategies for difficult intubation.Sponsored by ITACCS. Founded <strong>and</strong> managed byAirway Education & Research Foundation.Featuring the SLAM EmergencyIntubation Algorithm10 CEUs <strong>and</strong> CMEs available forPhysicians, RNs, CRNAs, EMT-Ps, LPs,<strong>and</strong> other health care workers.More information on pricing, workshop dates<strong>and</strong> locations available at www.AirwayEducation.com.JRofDallas@aol.com or call 972.463.0845Learn Street Level Airway Management - SLAM -<strong>and</strong> more, because if your patient can’t breathe,Nothing Else Matters!!17
ITACCS Summer 2002MILITARY MEDICINEProvision of a <strong>Trauma</strong> Resuscitation<strong>and</strong> <strong>Anesthesia</strong> Service in anAdvance Field Military Hospitalin Northern IndiaMajor (Dr.) Manish Mehrotra, MDAnaesthesiologist, Indian Army56/7, Manekshaw Officers EnclaveManekshaw MargDelhi CanttNew Delhi – 110010 Indiamannil10@satyam.net.inmannil10@rediffmail.comLt. Col. (Dr.) S<strong>and</strong>eep Mehrotra, MS, DNBGeneral Surgeon, Indian ArmyComm<strong>and</strong> HospitalCh<strong>and</strong>im<strong>and</strong>irCh<strong>and</strong>igarh, Indias<strong>and</strong>eepshraddha@hotmail.comLearning Objectives: 1) To underst<strong>and</strong> the challengesin<strong>here</strong>nt in the provision of trauma care,specifically anesthesia services, in remote areas ofmilitary operations <strong>and</strong> 2) to compare the anesthesiaequipment <strong>and</strong> drugs that have been adopted for usein remote medical facilities.<strong>Trauma</strong> is a leading cause of death <strong>and</strong> debility in India.Anaesthesiologists are commonly involved in providing acutemanagement of such patients. A trauma anaesthesiologist as aresuscitation specialist, as a part of mobile resuscitation team, 1or as a member of a critical care transportation team 2 willensure the optimal clinical state of the patient on his arrival atthe trauma centre. While provision of anaesthesia <strong>and</strong> criticalcare for such victims is always a challenge, the requirementsdictated by a patient’s medical condition do not vary withlocation. However, difficult environments restrict the ability toprovide high quality care. All trauma patients require anorganized prehospital response <strong>and</strong> definitive care followed byrehabilitation to achieve the best outcome. 3 In an ideal world,intensive care management of the seriously injured patientwould start in the prehospital setting <strong>and</strong> continue until nolonger necessary or considered to be futile. 4The development of military anesthesia dates back to thediscovery of anaesthesia itself. Morton administered ether tothe wounded close to the field of battle in 1864 during theAmerican Civil War. 5 Each war <strong>and</strong> conflict has requiredanaesthesiologists to adapt to new challenges in differentenvironments. Whether the terrain is a snowbound area alongthe line of control (LOC) or counter insurgency operations(CIOPS) in jungles, all present unique problems.A complex military conflict has continued in Northern Indiasince 1989, causing numerous military <strong>and</strong> civilian casualties.The cross-border terrorism turned into war in mid-1999. Liberaluse of small arms as well as artillery shelling <strong>and</strong> air raidsfollowed. During military operations in Kargil, more than 400Indian soldiers died <strong>and</strong> about 600 suffered serious injuries. 6Though the conflict officially ended in July 1999, hostileexchanges have continued, with morbidity <strong>and</strong> mortality oftroops. In addition, this sector is faced with harsh climate,difficult terrain, <strong>and</strong> inadequate logistic support. In this environment,field resuscitation <strong>and</strong> anaesthesia aim at minimizing delay<strong>and</strong> preserving life <strong>and</strong> limb. This can be accomplished only withmeticulous planning <strong>and</strong> rehearsed protocols. This articleprovides an insight into the working of a forward military traumacare centre located in the conflict area of northern India.<strong>Trauma</strong> <strong>Care</strong> Set Up of the Armed Forces Medical ServicesIn contrast to civilian counterpart organizations, theIndian Armed Forces Medical Services has a well-evolvedsystem of trauma care, 7 which features• Level III facilities: Forward Surgical Centre (FSC), fieldhospital, or static border hospital• Level II facilities: Base hospitals or zonal hospitalswith multidisciplinary surgical care• Level I facilities: Comm<strong>and</strong> hospitals/Army hospitalwith tertiary rehabilitative surgical careThe most remote surgical service in the Indian army is aFSC with a single anaesthesiologist, a surgeon, <strong>and</strong> ancillarystaff, including operating room assistants <strong>and</strong> radiology <strong>and</strong>laboratory technicians.Key Problems EncounteredThe importance of teamwork is critical in the managementof trauma victims with limited resources. Resuscitation,analgesia, <strong>and</strong> anaesthesia may need to be practiced simultaneously,requiring coordination between anaesthesiologists,surgeons, operating room assistants (ORA), <strong>and</strong> other ancillarystaff. Anaesthesiologists working in a FSC dealing with battlecasualties assume the responsibility of guiding all members ofthe team. Individuals must clearly underst<strong>and</strong> the importantrole that each plays. Adaptability is the key to achieving optimalresults.The main challenge in this harsh environment is completingessential tasks in a timely manner. Of particular concern forresuscitation <strong>and</strong> anaesthesia are the following:• Loss of the “Golden Hour” due to location <strong>and</strong> difficultiesin evacuation• Hostile weather conditions <strong>and</strong> inadequate warmingequipment• Non-availability of blood products <strong>and</strong> radiology facilities• Compromise in sterility <strong>and</strong> asepsis• Lack of conventional anaesthesia <strong>and</strong> surgical equipment• Lack of facilities for equipment repair• Lack of manpower <strong>and</strong> difficulties with staff turnoverEvacuation. Evacuation of the injured is a difficult task.Northern India is at high altitude, with extreme cold <strong>and</strong> high18
ITACCS Summer 2002Figure 1. Difficult terrain of far North India.wind velocity (Fig. 1). Soldiers are assessed for fitness <strong>and</strong>undergo very strict acclimatization before deployment. Postsare provided with high altitude pulmonary oedema (HAPO)bags <strong>and</strong> special equipment to counter cold injuries. Besidesthe altitude <strong>and</strong> cold, the steep gradient <strong>and</strong> loose rockysurface make the region prone to avalanche. In addition to thethreat of shelling <strong>and</strong> mortar attack, much of the area is heavilymined.Selected soldiers are trained by medical units on a regularbasis to provide battlefield first aid. These soldiers are calledbattlefield-nursing assistants (BFNA). The BFNAs provide firstaid <strong>and</strong> cardiopulmonary resuscitation <strong>and</strong> help with evacuationof casualties to the FSC, w<strong>here</strong> the medical officer nearestthe site of action provides care.Before evacuation, rapid dressing of wounds <strong>and</strong> splintingof fractures site are usually done. Because of the terrain, rapidevacuation of the casualties is often not possible. A roadopening party (ROP) checks every inch of vehicle routes eachmorning before movement of vehicles is allowed. Soldiers arethen placed every 10 to 15 metres along the route to ensuresecurity. Ambulances <strong>and</strong> helicopters are used for evacuations.The mode of evacuation depends largely on the time ofoccurrence, number of casualties, <strong>and</strong> access to the site.Ambulances are generally used, but in the afternoons helicoptersare available until 1600 hours. Later in the day, victims canbe transported only by road accompanied by a Quick ReactionForce (QRF), which consists of a minimum of 50 heavily armedmen, who move on mine-prone roads at risk of ambush. Inwinter, when forward bases are cut off by snow, helicopters arealso unable to l<strong>and</strong>. It may take up to 16 hours to bring apatient to the nearest road head or helipad. Six-memberstretcher-bearer squads carry the injured. Soldiers in their 16-piece winter gear move through waist-deep snow to reach apoint from which patients can be evacuated. This is a challengingjob on a steep climb, even with scoop stretchers incorporatinglocal modifications with bamboo <strong>and</strong> blankets.Golden Hour. Speed is vital in all cases; however, the goalof reaching the FSC within the Golden Hour is rarely achieved. 8Despite the enormous difficulties outlined above, the majorityof the wounded do receive medical attention within the first 60minutes. Ambulances are equipped with resuscitation equipmentto provide care, which during evacuation shortens delays<strong>and</strong> improves patient condition on arrival. With these resources,we managed 574 casualties over a 2-year period(November 1999 to August 2001) (discussed below).Initial Management. The trauma centre organizationrecognizes that trauma care requires highly trained resuscitation<strong>and</strong> anaesthesia personnel to achieve optimal outcomes.In our advance field surgical hospital, w<strong>here</strong> a singleanaesthesiologist is available, the job of the anaesthesiologiststarts with prehospital care. A team of three ORAs <strong>and</strong> thenurses serve as assistants. The anaesthesiologist secures theairway; ensures adequate ventilation; gives appropriate fluidmanagement, sedation, <strong>and</strong> anaesthesia; <strong>and</strong> looks after thesafe transport of patients.Obtaining a history <strong>and</strong> physical examination is difficultwithin the time constraints. Communication with othersoldiers, stretcher bearers, <strong>and</strong> surgeon helps to gatherinformation. A general trauma survey is conducted to identifyor exclude all injuries. The mechanism of injury determines thepattern of associated injuries, <strong>and</strong> this knowledge focusestreatment priorities. For example, effects of blunt trauma oftenevolve with time <strong>and</strong> require re-evaluation, w<strong>here</strong>as penetratingthoracic trauma resulting from shrapnel, missiles, or bulletsrequires immediate intervention. Penetrating injures in theneck region can seriously jeopardize the airway, so earlyintubation is essential <strong>and</strong> the best protection against aspiration.Securing the airway can be very difficult if a fibreopticbrochoscope <strong>and</strong> laryngeal mask airway are not available.Intubation can be facilitated with the use of improvised devicessuch as a spoon or torchlight. In difficult cases, awake intubationafter superior laryngeal nerve block <strong>and</strong> transtrachealinjection of local anaesthetic is our preferred method. Surgicalairway is reserved for patients who cannot be intubated orallyor nasally. Cricothyrotomy is the preferred technique. Theanaesthesiologist needs to be comfortable with both needlecricothyroidotomy <strong>and</strong> cricothyroidotomy with insertion of atracheostomy tube.Great debate continues on the subject of how much <strong>and</strong>which fluid should be used in multi trauma patients. 9,10 At ourcentre, all staff follows a fluid administration protocol thatinvolves insertion of two 14G intravenous (IV) cannulae in theupper extremity if possible <strong>and</strong> may involve venous cutdown.Warmed IV colloids <strong>and</strong> crystalloids are administered to allcasualties to avoid precipitating or worsening hypothermia.Warm water baths are used in the absence of heat-exchangerdevices. An inflated blood pressure cuff around the IV fluidbags facilitates rapid administration. Following assessment ofblood loss, the anaesthesiologist monitors the patient’sresponse to therapy to guide further fluid <strong>and</strong> blood administration.A list of blood donors is kept in the hospital at alltimes; t<strong>here</strong>fore, fresh whole blood is readily available fortransfusion.Definitive TreatmentLife- <strong>and</strong> limb-saving surgery with cardiovascular <strong>and</strong>respiratory stabilisation are the primary concerns. Variousadaptations have been made to meet these goals.Operating Facility. The main operating theatre is insidean underground bunker. The bunker contains a preoperativeresuscitation room; an instrument room with an autoclave; apostoperative room; <strong>and</strong> a storeroom, which is also used as a19
ITACCS Summer 2002Figure 2. Foot-operated suction apparatus. Figure 3. Resuscitation area. Figure 4. Boyles machine.rely on a generator. Casualties are also kept warm by beingcovered with blankets. Irrigation of body cavities is performedwith warmed saline solution.We managed a total of 574 casualties between November1999 <strong>and</strong> August 2001. This included all battle casualties <strong>and</strong>accidents as well as weather-related injuries, mountain sickness,<strong>and</strong> HAPO. Of these, 487 patients underwent surgicalintervention at our centre (Table 1). Primary wound debridement<strong>and</strong> foreign body removal accounted for 77% (375 of437) of the procedures.Figure 5. Surgical ward beds.Table 1. Mode of InjuriesMode of Injury No. of Cases (%)Shrapnel 183 (37.5)Gunshot wounds 160 (32.8)L<strong>and</strong>mine blast 105 (21.5)Grenade blast 39 (8)changing room. The floor has a polyvinyl covering. T<strong>here</strong> is anadjustable operating table <strong>and</strong> portable operating light. Bothelectrical <strong>and</strong> foot-operated suction is available (Fig. 2) <strong>and</strong> avehicle battery system is kept as st<strong>and</strong>by in case of generatorfailure.The cold climate, high wind velocity, <strong>and</strong> high wind chillfactor may lower the temperature of operation theatre to aslow as –25 o C (Fig. 3). Hypothermia correlates with a very pooroutcome. T<strong>here</strong>fore, warming the theatre is a major priority<strong>and</strong> is accomplished with blower-type heat convectors, whichAnaesthesia Equipment. Military anaesthesia requiressmall, lightweight, versatile, <strong>and</strong> easily transportable anaesthesiamachines for use in a frontline field surgical unit. A portableBoyles machine with a backup cylinder supply system isavailable in our hospital (Fig. 4). It is a rugged <strong>and</strong> robustmachine that has withstood the test of time despite problemswith a lack of safety features, gas leaks, <strong>and</strong> the inability to usea closed circuit. A Goldman vaporiser, which is a variablebypass, flow over without wick, out of circuit,nonthermocompensated vapouriser, is used for the administrationof halothane. An Epstein-Macintosh-Oxford (EMO)vaporiser is also available but is seldom used.While total intravenous anaesthesia (TIVA) has a role indifficult environments, we are unable to use this techniquebecause infusion pumps <strong>and</strong> suitable IV anaesthetic agents arenot available. However, ketamine has been used increasingly,with satisfactory results. Dissociative anaesthesia was used in40% of cases, general anaesthesia induced by halothane in 30%,<strong>and</strong> regional local anaesthetic techniques in 30%. Over aperiod of 22 months, 141 cases of isolated extremity traumawere managed with regional local anaesthetic techniques withgood results. Despite numerous advantages of regionaltechniques over general anaesthesia, they are probably stillunderutilised.Patients requiring postoperative ventilation are moved toan acute surgical ward for further management (Fig. 5). TheEast Radcliffe, the Drager Evita, <strong>and</strong> the Compaq ventilators areavailable <strong>and</strong> sufficiently robust <strong>and</strong> versatile for use in ourdifficult environment.T<strong>here</strong> are limitations to the monitoring devices available.20
ITACCS Summer 2002The best monitor is clinical assessment, with frequent conventionalblood pressure measurement <strong>and</strong> pulse measurements. Apulse oximeter <strong>and</strong> a defibrillator electrocardiography monitorare available. Bladder catheterisation <strong>and</strong> urine production areused as indicators of fluid balance <strong>and</strong> renal perfusion. Centralvenous lines are not available. Some patients require transfer toa tertiary level centre. Patients are monitored during transport<strong>and</strong> a portable ventilator provides ventilation. As the monitorsare generally single items in each FSC, their absence from theoperating theatre during transfer can seriously hinder themanagement of patients <strong>and</strong> their surgery.Conclusion<strong>Trauma</strong> care continues to be an important part of medicalpractice. With improved resuscitation <strong>and</strong> definitive care,military experience has seen a reduction in mortality <strong>and</strong>morbidity of soldiers. Despite enormous difficulties, in t<strong>here</strong>cent conflict in India, Army doctors working in advancesurgical units have saved innumerable lives. The presence ofexpert care at a forward post is a major moral boost for troops,who recognize that prompt optimal care gives the best chanceof recovery. T<strong>here</strong> are numerous challenges foranaesthesiologists involved in trauma care in an advance fieldsurgical unit. Improving the available level of care with thelimited resources <strong>and</strong> minimization of morbidity <strong>and</strong> mortalitycontinue to be our goals.References1. Gr<strong>and</strong>e CM, Stene JK, Bernhard WN, Barton CR. <strong>Trauma</strong>anesthesia <strong>and</strong> critical care: the concept <strong>and</strong> rationale for anew subspecialty. Crit <strong>Care</strong> Clin 1989; 6(1):1–11.2. Campbell D. Immediate hospital care of the injured. Br JAnaesth 1977; 49:673–9.3. Kochar SK. Opinion of the professionals: <strong>Trauma</strong> whoshould be the first responder? General surgeon, orthopedicsurgeon or anaesthesiologist ? Journal of <strong>Trauma</strong><strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> 2000; 1(1):1–3.4. Parr MJA, Nolan JP. Intensive care for trauma patients: thefirst 24 hours. Journal of <strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong><strong>Care</strong> 2000; 1(1):3–13.5. Morton WTG. The first use of ether as an anesthetic. At theBattle of Wilderness in the Civil War. JAMA 1904; 42:1068–72.6. Mohanty SN. True experiences of Kargil <strong>and</strong> other warinjuries. Journal of <strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong>2000; 1(1):20–26.7. Suri YV. Prehospital trauma <strong>and</strong> primary resuscitation inpolytrauma. Journal of <strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong><strong>Care</strong> 2000; 1(1):14–20.8. Malhotra SK. Management of disasters <strong>and</strong> mass casualties.Journal of <strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> 2000;1(1):34–41.9. Hambly PR, Dutton RP. Excess mortality associated withthe use of rapid infusion system at level 1 trauma center.Resuscitation 1996; 31:127–33.10. Schierhout G, Roberts I. Fluid resuscitation with colloid orcrystalloid solution in critically ill patients: a systemicreview of r<strong>and</strong>omised trials. BMJ 1998; 316:961–4.Join the worldwiderevolution in trauma care!JOIN ITACCS!Membership Form:Name:______________________________________________________________■ MD ■ DO ■ PhD ■ CRNA■ RN ■ CCRN ■ Other(s)_____________Mailing Address:____________________________________________________________________________________________________________________________________________________________________________________________________________________________________________City/State: _______________________________________Zip/Country Code: _______________________________Country:_________________________________________Hospital Affiliation:_______________________________Academic/Clinical Position:________________________________________________Telephone Number:______________________________Fax Number: ____________________________________E-mail Address: __________________________________Membership Category:■ Corporate Member (US$1000)■ Full Member (US$100)■ Professional in Training (US$40) (a letter verifyingtraining status is required)Method of Payment:■ US Check (US residents only) - Make checkpayable to ITACCS.■ <strong>International</strong> Draft - Make payable to ITACCSthrough a US bank in US dollars.■ Bank Transfer - Must be written in US dollars.Verification of transfer from financial institutionmust accompany this form. Please have fundstransferred to ITACCS Account Number 169-8133-3 with First National Bank of Maryl<strong>and</strong>,Route Number 052000113.■ Credit Card: ■ MasterCard ■ VISACard No.:___________________________________Expiration Date:_____________________________Name as it appears on card:_______________________________________________Signature: ______________________________________Return membership form <strong>and</strong> dues toITACCS World Headquarters,PO Box 4826, Baltimore MD 21211 USA21
ITACCS Summer 2002CONTINUING MEDICAL EDUCATIONThis issue of <strong>Trauma</strong><strong>Care</strong> can be used to earn 10 CME credit hours.Accreditation StatementThis activity has been planned <strong>and</strong> produced in accordance with the Essential Areas <strong>and</strong> Policies of the Accreditation Council for ContinuingMedical Education (ACCME) through the sponsorship of the <strong>International</strong> <strong>Trauma</strong> <strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> <strong>Society</strong> (ITACCS). ITACCS isaccredited by the ACCME to sponsor continuing medical education (CME) for physicians <strong>and</strong> takes responsibility for the content, quality, <strong>and</strong>scientific integrity of this CME activity.Credit Designation StatementITACCS designates this educational activity for a maximum of 10 hours per issue in category 1 credit toward the AMA Physician’s Recognition Award.Faculty Disclosure StatementIt is the policy of ITACCS that faculty members disclose real or apparent conflict of interest relating to the topics of this educational activity <strong>and</strong> alsodisclose discussions of unlabeled/unapproved uses of drugs or devices in their presentations. Dr. Christer Svensen has received travel support fromBiophausia, Inc. Hypertonic saline dextran, the topic of his article, is not approved by the Food <strong>and</strong> Drug Administration for use in the United States.None of the other contributors to this issue of <strong>Trauma</strong><strong>Care</strong> reports a financial relationship that might constitute conflict of interest <strong>and</strong> none hassuggested off-label use of any other product. The authors’ completed disclosure forms are on file in the managing editor’s office.INSTRUCTIONS• On the answer form at the bottom of page 23, circle only one response next to each number.• Complete the evaluation form.• Cut out or copy your completed answer form <strong>and</strong> evaluation form.• Write a check for $100 (or $50 accompanied by verification of current ITACCS membership), payable to the <strong>International</strong> <strong>Trauma</strong><strong>Anesthesia</strong> <strong>and</strong> <strong>Critical</strong> <strong>Care</strong> <strong>Society</strong>.• Mail the forms <strong>and</strong> your check (<strong>and</strong> membership verification, if applicable) to ITACCS, Department of CME Credit, PO Box 4826,Baltimore, MD 21211.• The completed test will be accepted for grading if received by October 1, 2003.• Please allow 4 to 6 weeks for processing.CME QUESTIONS1. Hypertonic solutions were initially used to treata. prehospital patients. b. burn patients. c. septic patients. d. patients with vascular diseases.2. Cardiovascular effects of administration of hypertonic solutions result ina. recruitment of endothelial fluid. b. lowered preload.c. lowered heart rate. d. lowered contractility of the heart.3. In the clinical setting, patients who benefit most from the administration of hypertonic solutions area. penetrating trauma patients. b. head trauma patients.c. patients with blunt trauma. d. multitrauma patients.4. The recommended infusion time of hypertonic solutions in the prehospital setting isa. 20 min.5. Administration of clinically appropriate doses of hypertonic saline has no effect on blood typing or cross-matching.a. True b. False6. Infusion of hypertonic solutions causesa. increased diuresis. b. increased natriuresis. c. kaluresis. d. all of the above.7. The hallmark of abdominal aortic injury is the triad of blunt abdominal trauma, acute aortic insufficiency,<strong>and</strong> lower-extremity paralysis.a. True b. False8. Among children who sustain complete aortic transection in vehicular crashes, what percentage of the injuriesoccur at the aortic isthmus?a. 5%–10% b. 20%–25% c. 75%–80% d. 100%9. Simplicity <strong>and</strong> lack of the need for heparin administration are advantages of which technique for repair ofabdominal aortic rupture?a. clamp <strong>and</strong> sew b. distal aortic perfusion during surgical repair10. In children with blunt abdominal trauma aortic rupture should be suspected based ona. mechanism of injury. b. chest film abnormalities.c. pseudocoarctation. d. all of the above.11. A c<strong>and</strong>idate for emergency department thoracotomy will havea. cardiac arrest <strong>and</strong> loss of vital signs at the scene.b. loss of consciousness at the scene after blunt trauma.c. vital signs at the scene of injury <strong>and</strong> subsequent witnessed cardiac arrest.d. hypotension upon arrival in the emergency department.Questions continue on page 2322
ITACCS Summer 200212. After a child sustains blunt chest trauma, reparable internal organ damage will always be suggested by an externalsign such as ecchymosis or hematoma.a. True b. False13. Extracorporeal life support is a well-established technique for the treatment of respiratory failure in children whohave sustained blunt chest trauma.a. True b. False14. The use of balloon tamponade to control endobronchial bleeding carries the risk ofa. rupture of the bronchus. b. endobronchial occlusion with clotted blood.c. occlusion of the endotracheal tube. d. sudden deflation of the balloon.15. A patient with potentially lethal respiratory failure <strong>and</strong> a transpulmonary shunt >30%, who is unresponsive toconventional management <strong>and</strong> whose primary condition is reversible is a c<strong>and</strong>idate fora. chaplain’s consult. b. extracorporeal life support.c. lung transplantation. d. high-frequency ventilation.16. The development of military anesthesia dates back to the discovery of anesthesia itself.a. True b. False17. Which of the following anesthesia problems were encountered on the Northern Indian battlefield?a. Hostile weather conditions <strong>and</strong> lack of warming equipment. b. Loss of the “Golden Hour” due to remote locations.c. Lack of conventional anesthesia <strong>and</strong> surgical equipment. d. All of the above.e. None of the above.18. Initial airway management in the forward surgical center involvesa. Only an oxygen mask. b. Early extubation.c. Facilitating intubation with improvised devices such as a spoon <strong>and</strong> torch. d. Doing nothing.19. The most common injuries treated in the Northern Indian forward surgical center were those caused by l<strong>and</strong> mine explosions.a. True b. False20. Fluid administration in the forward surgical center includesa. Rescueflow. b. Fresh whole blood. c. Oral electrolyte solutions. d. Packed red blood cells.Evaluation Form: Please rate this self-study activity by marking one response for each statement.Did the articles meet their stated objectives? ___Yes ___NoHow do you rank the quality of this educational activity? ___5 (high) ____4 ___3 ___2 ___1 (low)Comments: __________________________________________________________________________________________________________Did you perceive any evidence of bias for or against any commercial products? ___Yes ___No If yes, please explain.Comments: __________________________________________________________________________________________________________How do you rank the effectiveness of this activity as it pertains to your practice? ___5 (high) ____4 ___3 ___2 ___1 (low)Did this material stimulate your intellectual curiosity? ___5 (high) ____4 ___3 ___2 ___1 (low)Additional comments about this activity: ______________________________________________________________________________________________________________________________________________________________________________________________________Answer Form: Please circle the one best answer for each question.<strong>Trauma</strong><strong>Care</strong> Summer 2002 issueName: ________________________________________________________Address: ________________________________________________________________________________________________________________City: ________________________________________________________State:_______________Zip: _________ Phone:______________________I certify that I have completed the “<strong>Trauma</strong><strong>Care</strong>/Summer 2002” activity as designed <strong>and</strong> claim 10credit hours in Category 1 of the Physicians Recognition Award of the American Medical Association.____________________________________________________________________________ _______________________________________SignatureDateMail answer form <strong>and</strong> check ($50, members; $100, nonmembers) to ITACCS Departmentof CME Credit, P.O. Box 4826, Baltimore, MD 21211. Allow 4 to 6 weeks for processing.1. a b c d2. a b c d3. a b c d4. a b c d5. a b6. a b c d7. a b8. a b c d9. a b10. a b c d11. a b c d12. a b13. a b14. a b c d15. a b c d16. a b17. a b c d e18. a b c d19. a b20. a b c dCredit for this activity is offered until October 1, 2003.23