Child Health Check-Up (formerly EPSDT) - Herman & Associates ...
Child Health Check-Up (formerly EPSDT) - Herman & Associates ...
Child Health Check-Up (formerly EPSDT) - Herman & Associates ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
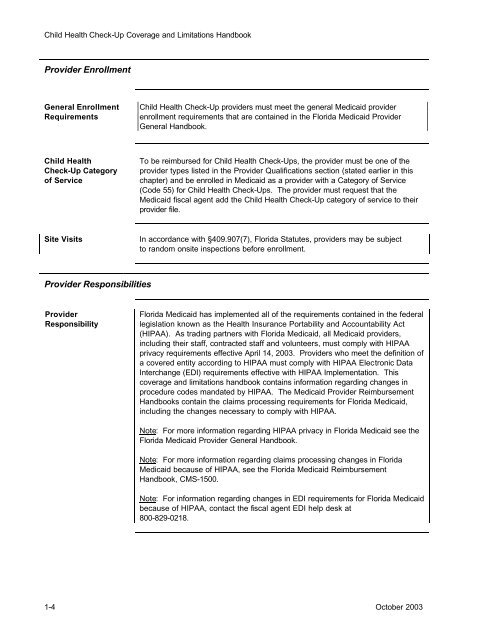
<strong>Child</strong> <strong>Health</strong> <strong>Check</strong>-<strong>Up</strong> Coverage and Limitations HandbookProvider EnrollmentGeneral EnrollmentRequirements<strong>Child</strong> <strong>Health</strong> <strong>Check</strong>-<strong>Up</strong> providers must meet the general Medicaid providerenrollment requirements that are contained in the Florida Medicaid ProviderGeneral Handbook.<strong>Child</strong> <strong>Health</strong><strong>Check</strong>-<strong>Up</strong> Categoryof ServiceTo be reimbursed for <strong>Child</strong> <strong>Health</strong> <strong>Check</strong>-<strong>Up</strong>s, the provider must be one of theprovider types listed in the Provider Qualifications section (stated earlier in thischapter) and be enrolled in Medicaid as a provider with a Category of Service(Code 55) for <strong>Child</strong> <strong>Health</strong> <strong>Check</strong>-<strong>Up</strong>s. The provider must request that theMedicaid fiscal agent add the <strong>Child</strong> <strong>Health</strong> <strong>Check</strong>-<strong>Up</strong> category of service to theirprovider file.Site VisitsIn accordance with §409.907(7), Florida Statutes, providers may be subjectto random onsite inspections before enrollment.Provider ResponsibilitiesProviderResponsibilityFlorida Medicaid has implemented all of the requirements contained in the federallegislation known as the <strong>Health</strong> Insurance Portability and Accountability Act(HIPAA). As trading partners with Florida Medicaid, all Medicaid providers,including their staff, contracted staff and volunteers, must comply with HIPAAprivacy requirements effective April 14, 2003. Providers who meet the definition ofa covered entity according to HIPAA must comply with HIPAA Electronic DataInterchange (EDI) requirements effective with HIPAA Implementation. Thiscoverage and limitations handbook contains information regarding changes inprocedure codes mandated by HIPAA. The Medicaid Provider ReimbursementHandbooks contain the claims processing requirements for Florida Medicaid,including the changes necessary to comply with HIPAA.Note: For more information regarding HIPAA privacy in Florida Medicaid see theFlorida Medicaid Provider General Handbook.Note: For more information regarding claims processing changes in FloridaMedicaid because of HIPAA, see the Florida Medicaid ReimbursementHandbook, CMS-1500.Note: For information regarding changes in EDI requirements for Florida Medicaidbecause of HIPAA, contact the fiscal agent EDI help desk at800-829-0218.1-4 October 2003