INTERACT SBAR for Assisted Living Nurses
INTERACT SBAR for Assisted Living Nurses
INTERACT SBAR for Assisted Living Nurses
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
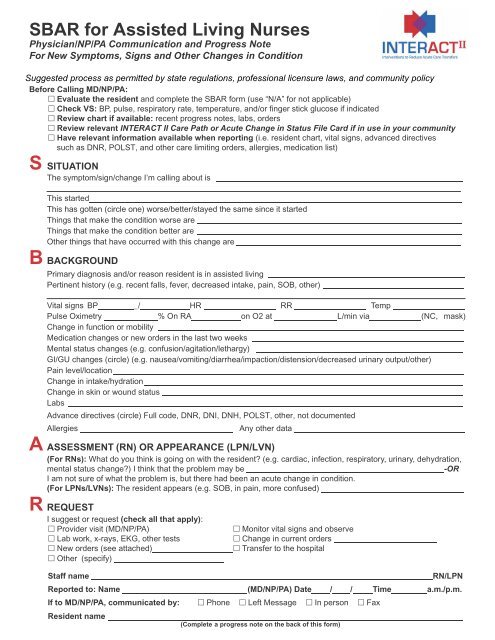
<strong>SBAR</strong> <strong>for</strong> <strong>Assisted</strong> <strong>Living</strong> <strong>Nurses</strong>Physician/NP/PA Communication and Progress NoteFor New Symptoms, Signs and Other Changes in ConditionSuggested process as permitted by state regulations, professional licensure laws, and community policyBe<strong>for</strong>e Calling MD/NP/PA: Evaluate the resident and complete the <strong>SBAR</strong> <strong>for</strong>m (use “N/A” <strong>for</strong> not applicable) Check VS: BP, pulse, respiratory rate, temperature, and/or finger stick glucose if indicated Review chart if available: recent progress notes, labs, orders Review relevant <strong>INTERACT</strong> II Care Path or Acute Change in Status File Card if in use in your community Have relevant in<strong>for</strong>mation available when reporting (i.e. resident chart, vital signs, advanced directivessuch as DNR, POLST, and other care limiting orders, allergies, medication list)S SITUATIONThe symptom/sign/change I’m calling about isThis startedThis has gotten (circle one) worse/better/stayed the same since it startedThings that make the condition worse areThings that make the condition better areOther things that have occurred with this change areB BACKGROUNDPrimary diagnosis and/or reason resident is in assisted livingPertinent history (e.g. recent falls, fever, decreased intake, pain, SOB, other)Vital signs BP _/ HR RR TempPulse Oximetry % On RA on O2 at L/min via (NC, mask)Change in function or mobilityMedication changes or new orders in the last two weeksMental status changes (e.g. confusion/agitation/lethargy)GI/GU changes (circle) (e.g. nausea/vomiting/diarrhea/impaction/distension/decreased urinary output/other)Pain level/locationChange in intake/hydrationChange in skin or wound statusLabsAdvance directives (circle) Full code, DNR, DNI, DNH, POLST, other, not documentedAllergiesAny other dataA ASSESSMENT (RN) OR APPEARANCE (LPN/LVN)(For RNs): What do you think is going on with the resident? (e.g. cardiac, infection, respiratory, urinary, dehydration,mental status change?) I think that the problem may be-ORI am not sure of what the problem is, but there had been an acute change in condition.(For LPNs/LVNs): The resident appears (e.g. SOB, in pain, more confused)R REQUESTI suggest or request (check all that apply): Provider visit (MD/NP/PA) Monitor vital signs and observe Lab work, x-rays, EKG, other tests Change in current orders New orders (see attached) Transfer to the hospital Other (specify)Staff nameRN/LPNReported to: Name (MD/NP/PA) Date / / Time a.m./p.m.If to MD/NP/PA, communicated by: Phone Left Message In person FaxResident name(Complete a progress note on the back of this <strong>for</strong>m)
©2010 FAU Updated June 2012 Family or health care proxy notifiedName Date / / / Time / AM/PMProgress NoteReturn call/message new orders from MD/NP/PA Date / / / Time / AM/PMSignature RN/LPN/LVN Date / / / Time / AM/PMResident Name©2010 FAU Updated June 2012