<strong>ARVO</strong> 2013 Annual Meeting Abstracts by Scientific Section/Group - <strong>Cornea</strong>by measuring the area of NV, the level of opacification and thecornea thickness. The area of NV from the limbus into the graft wasmeasured by using corneal fluorescein angiography (FA) and digitalmeasurements. Persistence of opacification was assessed by slit-lampmicroscopy and graded on a 0 to 4+ scale. <strong>Cornea</strong> thickness andcornea astigmatism was measured by ocular coherence topography(OCT). At sacrifice (day 28) the cornea was fixed for histologicalanalysis of neovascularization, inflammation, and rejection.Results: <strong>Cornea</strong>l neovascularization, opacification, cornea thicknesswas significantly higher in the interrupted suture group compared tothe continuous suture group. (p = 0.006 or less). All corneas in thecontinuous suture group exhibited minimal neovascularization andgenerally presented with ≤ 1 opacification at each time point studied.A single running suture results in less postoperative astigmatismcompared with the interrupted sutures technique.Conclusions: <strong>Cornea</strong>s within the interrupted suture group wereassociated with a significant increased level of neovascularization,opacification and astigmatism followed by a higher rate of rejection.The suturing method appears to be a factor leading to the rate ofcornea rejection in a rabbit PK model and may be correlated tohuman surgical outcomes.Commercial Relationships: Maria A. Parker, None; Trevor J.McFarland, None; Winston Chamberlain, None; Scott Ellis,Oxford BioMedica (E); Kyriacos Mitrophanous, Oxford BioMedica(UK) Ltd (E); Tim Stout, Clayton Foundation (P), OxfordBiomedica (C), AGTC (F), Peregrine Pharmaceuticals Inc (C), StemCells Inc (C)Program Number: 3072 Poster Board Number: D0007Presentation Time: 8:30 AM - 10:15 AMMost frequent indications for keratoplasty at 2 academic centersover a 6-year periodKimberly Hsu 1 , Shu-Hong Chang 4, 1 , Whitney Brothers 2 , Sean L.Edelstein 2 , Hugo Y. Hsu 3, 2 , George J. Harocopos 1 . 1 Ophthalmology,Washington University in St. Louis, St. Louis, MO; 2 Ophthalmology,Saint Louis University, St. Louis, MO; 3 Ophthalmology, Universityof Southern California, Los Angeles, CA; 4 Ophthalmology,University of Washington, Seattle, WA.Purpose: To determine the most frequent indications for keratoplastyfrom 2002-2007 at 2 academic centers and to compare this data to themost common indications for keratoplasty nation-wide over this sametime period.Methods: A retrospective review was performed for the indicationsfor keratoplasty from 2002-2007 at Washington University in St.Louis (WUSTL) and St. Louis University (SLU). A pathologydatabase search was used to find all pathology reports of keratoplastyspecimens. The patients’ age, sex, right or left eye, type ofkeratoplasty, indication for keratoplasty, and ocular comorbiditieswere recorded. A total of 855 and 110 eyes underwent keratoplasty atWUSTL and SLU, respectively, during this time period. Statisticalreports were obtained from the Eye Bank Association of America(EBAA) for the corresponding years 2002-2007. The indications forkeratoplasty were reviewed and averaged for these 6 years andcompared to the data from our academic centers.Results: At WUSTL, the most common indication for keratoplastywas graft failure at 31.6%. This was followed by Fuchs cornealdystrophy at 22.1%, pseudophakic and aphakic bullous keratopathy at17.6%, and keratoconus at 6.9%. At SLU, the most commonindications for keratoplasty were PBK/ABK at 34.4% and graftfailure at 32.7%. This was followed by Fuchs corneal dystrophy(10%) and keratoconus (6.4%). Averaging the 2002-2007 EBAAdata, the most common indication for keratoplasty nation-wide wasPBK/ABK at 19.9%. This was followed by keratoconus at 15.9% andthen Fuchs dystrophy at 13.3%. Re-grafts accounted for only 13.2%of keratoplasties performed during this time period nation-wide.Conclusions: In our review of the indications for keratoplasties attwo academic centers in St. Louis, we found re-grafts to account forapproximately one third of all keratoplasties, which was more thandouble the proportion in the national data during this time period. Wepostulate that these higher percentages for re-grafting represent areferral bias of complex patients to academic centers who ultimatelyrequire multiple keratoplasties.Commercial Relationships: Kimberly Hsu, None; Shu-HongChang, None; Whitney Brothers, None; Sean L. Edelstein, None;Hugo Y. Hsu, Bausch & Lomb (R); George J. Harocopos, NoneProgram Number: 3073 Poster Board Number: D0008Presentation Time: 8:30 AM - 10:15 AMOutcome of Combined Penetrating Keratoplasty andVitreoretinal Surgery using Temporary EckardtKeratoprosthesis and Analysis for Factors affecting <strong>Cornea</strong>lAllograft SurvivalDae Seung Lee 1 , Jang won Heo 1 , Mee Kum Kim 1 , Hyuk Jin Choi 2 ,Won Ryang Wee 1 , Joo Youn Oh 1 . 1 Ophthalmology, Seoul NationalUniversity, Seoul, Republic of Korea; 2 Seoul National UniversityHospital Healthcare System Gangnam Center, Seoul, Republic ofKorea.Purpose: To evaluate the outcome of combined penetratingkeratoplasty and vitreoretinal surgery using temporary Eckardtkeratoprosthesis and to analyze the factors affecting the cornealallograft survival.Methods: We reviewed medical records of 11 patients whounderwent combined corneal allotransplantation and pars planavitrectomy using temporary Eckardt keratoprosthesis. Primaryoutcome measure was the survival rate of corneal grafts. Patientdemographics, clinical features of the cornea and retina such asdisease entities and preoperative status, or surgical methods werecompared between the group with graft rejection and the group withgraft survival.Results: The overall graft survival rate was 45.5 % (5/11 eyes).Retinal surgery was successful in 90.9 % (10/11 eyes). Rejectionoccurred in 5 patients (45.5 %, 5/11 eyes) with the mean survivaltime of 82.8 days during a follow up of 579 days. Four of 5 cases hadthe graft rejection within 2 months after surgery, and one patient hadrejection at 7 months. The presence of inflammation orvascularization in the cornea before surgery was a significant factoraffecting the occurrence of graft rejection (p value = 0.006). Activeinflammation was present preoperatively in the recipient cornea in allpatients with rejection. <strong>Cornea</strong>l neovascularization was present in therecipient cornea in 4 of 5 patients with rejection. In contrast, therewas no inflammation or vascularization in patients without rejection.The patient age, the presence of glaucoma, entities of corneal andretinal diseases, types of retinal surgery including the use of siliconeoil or gas tamponade had no significant correlation with the graftsurvival or rejection.Conclusions: Combined corneal allotransplantation and pars planavitrectomy using temporary Eckardt keratoprosthesis allowed forsuccessful surgical intervention of retinal diseases in patients withcoexisting corneal opacity. Although the retinal outcome wasexcellent in 90.9 %, corneal allografts survived in 45.5%, largelydepending on the preoperative status of the cornea including thepresence of active inflammation or vascularization.Commercial Relationships: Dae Seung Lee, None; Jang won Heo,None; Mee Kum Kim, None; Hyuk Jin Choi, None; Won RyangWee, None; Joo Youn Oh, NoneSupport: None in the Support field below©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permissionto reproduce any abstract, contact the <strong>ARVO</strong> Office at arvo@arvo.org.
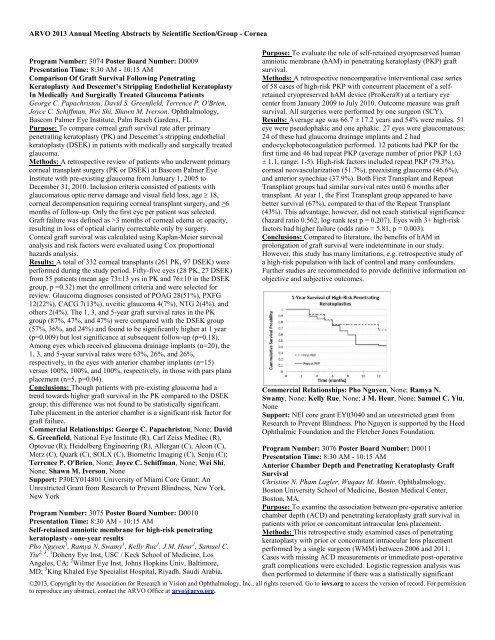
<strong>ARVO</strong> 2013 Annual Meeting Abstracts by Scientific Section/Group - <strong>Cornea</strong>Program Number: 3074 Poster Board Number: D0009Presentation Time: 8:30 AM - 10:15 AMComparison Of Graft Survival Following PenetratingKeratoplasty And Descemet’s Stripping Endothelial KeratoplastyIn Medically And Surgically Treated Glaucoma PatientsGeorge C. Papachristou, David S. Greenfield, Terrence P. O'Brien,Joyce C. Schiffman, Wei Shi, Shawn M. Iverson. Ophthalmology,Bascom Palmer Eye Institute, Palm Beach Gardens, FL.Purpose: To compare corneal graft survival rate after primarypenetrating keratoplasty (PK) and Descemet’s stripping endothelialkeratoplasty (DSEK) in patients with medically and surgically treatedglaucoma.Methods: A retrospective review of patients who underwent primarycorneal transplant surgery (PK or DSEK) at Bascom Palmer EyeInstitute with pre-existing glaucoma from January 1, 2005 toDecember 31, 2010. Inclusion criteria consisted of patients withglaucomatous optic nerve damage and visual field loss, age ≥ 18,corneal decompensation requiring corneal transplant surgery, and ≥6months of follow-up. Only the first eye per patient was selected.Graft failure was defined as >3 months of corneal edema or opacity,resulting in loss of optical clarity correctable only by surgery.<strong>Cornea</strong>l graft survival was calculated using Kaplan-Meier survivalanalysis and risk factors were evaluated using Cox proportionalhazards analysis.Results: A total of 332 corneal transplants (261 PK, 97 DSEK) wereperformed during the study period. Fifty-five eyes (28 PK, 27 DSEK)from 55 patients (mean age 73±13 yrs in PK and 76±10 in the DSEKgroup, p =0.32) met the enrollment criteria and were selected forreview. Glaucoma diagnoses consisted of POAG 28(51%), PXFG12(22%), CACG 7(13%), uveitic glaucoma 4(7%), NTG 2(4%), andothers 2(4%). The 1, 3, and 5-year graft survival rates in the PKgroup (87%, 47%, and 47%) were compared with the DSEK group(57%, 36%, and 24%) and found to be significantly higher at 1 year(p=0.009) but lost significance at subsequent follow-up (p=0.18).Among eyes which received glaucoma drainage implants (n=20), the1, 3, and 5-year survival rates were 63%, 26%, and 26%,respectively, in the eyes with anterior chamber implants (n=15)versus 100%, 100%, and 100%, respectively, in those with pars planaplacement (n=5, p=0.04).Conclusions: Though patients with pre-existing glaucoma had atrend towards higher graft survival in the PK compared to the DSEKgroup; this difference was not found to be statistically significant.Tube placement in the anterior chamber is a significant risk factor forgraft failure.Commercial Relationships: George C. Papachristou, None; DavidS. Greenfield, National Eye Institute (R), Carl Zeiss Meditec (R),Optovue (R), Heidelberg Engineering (R), Allergan (C), Alcon (C),Merz (C), Quark (C), SOLX (C), Biometric Imaging (C), Senju (C);Terrence P. O'Brien, None; Joyce C. Schiffman, None; Wei Shi,None; Shawn M. Iverson, NoneSupport: P30EY014801 University of Miami Core Grant: AnUnrestricted Grant from Research to Prevent Blindness, New York,New YorkProgram Number: 3075 Poster Board Number: D0010Presentation Time: 8:30 AM - 10:15 AMSelf-retained amniotic membrane for high-risk penetratingkeratoplasty - one-year resultsPho Nguyen 1 , Ramya N. Swamy 1 , Kelly Rue 1 , J M. Heur 1 , Samuel C.Yiu 2, 3 . 1 Doheny Eye Inst, USC / Keck School of Medicine, LosAngeles, CA; 2 Wilmer Eye Inst, Johns Hopkins Univ, Baltimore,MD; 3 King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia.Purpose: To evaluate the role of self-retained cryopreserved humanamniotic membrane (hAM) in penetrating keratoplasty (PKP) graftsurvival.Methods: A retrospective noncomparative interventional case seriesof 58 cases of high-risk PKP with concurrent placement of a selfretainedcryopreserved hAM device (ProKera®) at a tertiary eyecenter from January 2009 to July 2010. Outcome measure was graftsurvival. All surgeries were performed by one surgeon (SCY).Results: Average age was 66.7 ± 17.2 years and 54% were males. 51eye were pseudophakic and one aphakic. 27 eyes were glaucomatous;24 of these had glaucoma drainage implants and 2 hadendocyclophotocoagulation performed. 12 patients had PKP for thefirst time and 46 had repeat PKP (average number of prior PKP 1.63± 1.1, range: 1-5). High-risk factors included repeat PKP (79.3%),corneal neovascularization (51.7%), preexisting glaucoma (46.6%),and anterior synechiae (37.9%). Both First Transplant and RepeatTransplant groups had similar survival rates until 6 months aftertransplant. At year 1, the First Transplant group appeared to havebetter survival (67%), compared to that of the Repeat Transplant(43%). This advantage, however, did not reach statistical significance(hazard ratio 0.562, log-rank test p = 0.207). Eyes with 3+ high-riskfactors had higher failure (odds ratio = 5.81, p = 0.003).Conclusions: Compared to literature, the benefits of hAM inprolongation of graft survival were indeterminate in our study.However, this study has many limitations, e.g. retrospective study ofa high-risk population with lack of control and many confounders.Further studies are recommended to provide definitive information onobjective and subjective outcomes.Commercial Relationships: Pho Nguyen, None; Ramya N.Swamy, None; Kelly Rue, None; J M. Heur, None; Samuel C. Yiu,NoneSupport: NEI core grant EY03040 and an unrestricted grant fromResearch to Prevent Blindness. Pho Nguyen is supported by the HeedOphthalmic Foundation and the Fletcher Jones Foundation.Program Number: 3076 Poster Board Number: D0011Presentation Time: 8:30 AM - 10:15 AMAnterior Chamber Depth and Penetrating Keratoplasty GraftSurvivalChristine N. Pham Lagler, Wuqaas M. Munir. Ophthalmology,Boston University School of Medicine, Boston Medical Center,Boston, MA.Purpose: To examine the association between pre-operative anteriorchamber depth (ACD) and penetrating keratoplasty graft survival inpatients with prior or concomitant intraocular lens placement.Methods: This retrospective study examined cases of penetratingkeratoplasty with prior or concomitant intraocular lens placementperformed by a single surgeon (WMM) between 2006 and 2011.Cases with missing ACD measurements or immediate post-operativegraft complications were excluded. Logistic regression analysis wasthen performed to determine if there was a statistically significant©2013, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permissionto reproduce any abstract, contact the <strong>ARVO</strong> Office at arvo@arvo.org.
- Page 2 and 3:
ARVO 2013 Annual Meeting Abstracts
- Page 4 and 5:
ARVO 2013 Annual Meeting Abstracts
- Page 6 and 7:
ARVO 2013 Annual Meeting Abstracts
- Page 8 and 9:
ARVO 2013 Annual Meeting Abstracts
- Page 10:
ARVO 2013 Annual Meeting Abstracts
- Page 13 and 14:
ARVO 2013 Annual Meeting Abstracts
- Page 16 and 17:
ARVO 2013 Annual Meeting Abstracts
- Page 18 and 19:
ARVO 2013 Annual Meeting Abstracts
- Page 20 and 21:
ARVO 2013 Annual Meeting Abstracts
- Page 22 and 23:
ARVO 2013 Annual Meeting Abstracts
- Page 24 and 25:
ARVO 2013 Annual Meeting Abstracts
- Page 26 and 27:
ARVO 2013 Annual Meeting Abstracts
- Page 28 and 29:
ARVO 2013 Annual Meeting Abstracts
- Page 30 and 31:
ARVO 2013 Annual Meeting Abstracts
- Page 32 and 33:
ARVO 2013 Annual Meeting Abstracts
- Page 34 and 35:
ARVO 2013 Annual Meeting Abstracts
- Page 36 and 37:
ARVO 2013 Annual Meeting Abstracts
- Page 38 and 39:
ARVO 2013 Annual Meeting Abstracts
- Page 40 and 41:
ARVO 2013 Annual Meeting Abstracts
- Page 42 and 43:
ARVO 2013 Annual Meeting Abstracts
- Page 44 and 45:
ARVO 2013 Annual Meeting Abstracts
- Page 46 and 47:
ARVO 2013 Annual Meeting Abstracts
- Page 48 and 49:
ARVO 2013 Annual Meeting Abstracts
- Page 50 and 51:
ARVO 2013 Annual Meeting Abstracts
- Page 52 and 53:
ARVO 2013 Annual Meeting Abstracts
- Page 54 and 55:
ARVO 2013 Annual Meeting Abstracts
- Page 56 and 57:
ARVO 2013 Annual Meeting Abstracts
- Page 58 and 59:
ARVO 2013 Annual Meeting Abstracts
- Page 60 and 61:
ARVO 2013 Annual Meeting Abstracts
- Page 62 and 63:
ARVO 2013 Annual Meeting Abstracts
- Page 64 and 65:
ARVO 2013 Annual Meeting Abstracts
- Page 66 and 67:
ARVO 2013 Annual Meeting Abstracts
- Page 68 and 69:
ARVO 2013 Annual Meeting Abstracts
- Page 70 and 71:
ARVO 2013 Annual Meeting Abstracts
- Page 72 and 73:
ARVO 2013 Annual Meeting Abstracts
- Page 74 and 75:
ARVO 2013 Annual Meeting Abstracts
- Page 76 and 77:
ARVO 2013 Annual Meeting Abstracts
- Page 78 and 79:
ARVO 2013 Annual Meeting Abstracts
- Page 80 and 81:
ARVO 2013 Annual Meeting Abstracts
- Page 82 and 83:
ARVO 2013 Annual Meeting Abstracts
- Page 84 and 85:
ARVO 2013 Annual Meeting Abstracts
- Page 86 and 87:
ARVO 2013 Annual Meeting Abstracts
- Page 88 and 89:
ARVO 2013 Annual Meeting Abstracts
- Page 90 and 91:
ARVO 2013 Annual Meeting Abstracts
- Page 92 and 93:
ARVO 2013 Annual Meeting Abstracts
- Page 94 and 95:
ARVO 2013 Annual Meeting Abstracts
- Page 96 and 97:
ARVO 2013 Annual Meeting Abstracts
- Page 98 and 99:
ARVO 2013 Annual Meeting Abstracts
- Page 100 and 101:
ARVO 2013 Annual Meeting Abstracts
- Page 102 and 103:
ARVO 2013 Annual Meeting Abstracts
- Page 104 and 105:
ARVO 2013 Annual Meeting Abstracts
- Page 106 and 107:
ARVO 2013 Annual Meeting Abstracts
- Page 108 and 109:
ARVO 2013 Annual Meeting Abstracts
- Page 110 and 111:
ARVO 2013 Annual Meeting Abstracts
- Page 112 and 113:
ARVO 2013 Annual Meeting Abstracts
- Page 114 and 115:
ARVO 2013 Annual Meeting Abstracts
- Page 116 and 117:
ARVO 2013 Annual Meeting Abstracts
- Page 118 and 119:
ARVO 2013 Annual Meeting Abstracts
- Page 120 and 121:
ARVO 2013 Annual Meeting Abstracts
- Page 122 and 123:
ARVO 2013 Annual Meeting Abstracts
- Page 124 and 125:
ARVO 2013 Annual Meeting Abstracts
- Page 126 and 127:
ARVO 2013 Annual Meeting Abstracts
- Page 128 and 129:
ARVO 2013 Annual Meeting Abstracts
- Page 130 and 131:
ARVO 2013 Annual Meeting Abstracts
- Page 132 and 133:
ARVO 2013 Annual Meeting Abstracts
- Page 134 and 135:
ARVO 2013 Annual Meeting Abstracts
- Page 136 and 137:
ARVO 2013 Annual Meeting Abstracts
- Page 138 and 139: ARVO 2013 Annual Meeting Abstracts
- Page 140 and 141: ARVO 2013 Annual Meeting Abstracts
- Page 142 and 143: ARVO 2013 Annual Meeting Abstracts
- Page 144 and 145: ARVO 2013 Annual Meeting Abstracts
- Page 146 and 147: ARVO 2013 Annual Meeting Abstracts
- Page 148 and 149: ARVO 2013 Annual Meeting Abstracts
- Page 150 and 151: ARVO 2013 Annual Meeting Abstracts
- Page 152 and 153: ARVO 2013 Annual Meeting Abstracts
- Page 154 and 155: ARVO 2013 Annual Meeting Abstracts
- Page 156 and 157: ARVO 2013 Annual Meeting Abstracts
- Page 158 and 159: ARVO 2013 Annual Meeting Abstracts
- Page 160 and 161: ARVO 2013 Annual Meeting Abstracts
- Page 162 and 163: ARVO 2013 Annual Meeting Abstracts
- Page 164 and 165: ARVO 2013 Annual Meeting Abstracts
- Page 166 and 167: ARVO 2013 Annual Meeting Abstracts
- Page 168 and 169: ARVO 2013 Annual Meeting Abstracts
- Page 170 and 171: ARVO 2013 Annual Meeting Abstracts
- Page 172 and 173: ARVO 2013 Annual Meeting Abstracts
- Page 174 and 175: ARVO 2013 Annual Meeting Abstracts
- Page 176 and 177: ARVO 2013 Annual Meeting Abstracts
- Page 178 and 179: ARVO 2013 Annual Meeting Abstracts
- Page 180 and 181: ARVO 2013 Annual Meeting Abstracts
- Page 182 and 183: ARVO 2013 Annual Meeting Abstracts
- Page 184 and 185: ARVO 2013 Annual Meeting Abstracts
- Page 186 and 187: ARVO 2013 Annual Meeting Abstracts
- Page 190 and 191: ARVO 2013 Annual Meeting Abstracts
- Page 192 and 193: ARVO 2013 Annual Meeting Abstracts
- Page 194 and 195: ARVO 2013 Annual Meeting Abstracts
- Page 196 and 197: ARVO 2013 Annual Meeting Abstracts
- Page 198 and 199: ARVO 2013 Annual Meeting Abstracts
- Page 200 and 201: ARVO 2013 Annual Meeting Abstracts
- Page 202 and 203: ARVO 2013 Annual Meeting Abstracts
- Page 204 and 205: ARVO 2013 Annual Meeting Abstracts
- Page 206 and 207: ARVO 2013 Annual Meeting Abstracts
- Page 208 and 209: ARVO 2013 Annual Meeting Abstracts
- Page 210 and 211: ARVO 2013 Annual Meeting Abstracts
- Page 212 and 213: ARVO 2013 Annual Meeting Abstracts
- Page 214 and 215: ARVO 2013 Annual Meeting Abstracts
- Page 216 and 217: ARVO 2013 Annual Meeting Abstracts
- Page 218 and 219: ARVO 2013 Annual Meeting Abstracts
- Page 220 and 221: ARVO 2013 Annual Meeting Abstracts
- Page 222 and 223: ARVO 2013 Annual Meeting Abstracts
- Page 224 and 225: ARVO 2013 Annual Meeting Abstracts
- Page 226 and 227: ARVO 2013 Annual Meeting Abstracts
- Page 228 and 229: ARVO 2013 Annual Meeting Abstracts
- Page 230 and 231: ARVO 2013 Annual Meeting Abstracts
- Page 232 and 233: ARVO 2013 Annual Meeting Abstracts
- Page 234 and 235: ARVO 2013 Annual Meeting Abstracts
- Page 236 and 237: ARVO 2013 Annual Meeting Abstracts
- Page 238 and 239:
ARVO 2013 Annual Meeting Abstracts
- Page 240 and 241:
ARVO 2013 Annual Meeting Abstracts
- Page 242 and 243:
ARVO 2013 Annual Meeting Abstracts
- Page 244 and 245:
ARVO 2013 Annual Meeting Abstracts
- Page 246 and 247:
ARVO 2013 Annual Meeting Abstracts
- Page 248 and 249:
ARVO 2013 Annual Meeting Abstracts
- Page 250 and 251:
ARVO 2013 Annual Meeting Abstracts
- Page 252 and 253:
ARVO 2013 Annual Meeting Abstracts
- Page 254 and 255:
ARVO 2013 Annual Meeting Abstracts
- Page 256 and 257:
ARVO 2013 Annual Meeting Abstracts
- Page 258 and 259:
ARVO 2013 Annual Meeting Abstracts
- Page 260 and 261:
ARVO 2013 Annual Meeting Abstracts
- Page 262 and 263:
ARVO 2013 Annual Meeting Abstracts
- Page 264 and 265:
ARVO 2013 Annual Meeting Abstracts
- Page 266 and 267:
ARVO 2013 Annual Meeting Abstracts
- Page 268 and 269:
ARVO 2013 Annual Meeting Abstracts
- Page 270 and 271:
ARVO 2013 Annual Meeting Abstracts
- Page 272 and 273:
ARVO 2013 Annual Meeting Abstracts
- Page 274 and 275:
ARVO 2013 Annual Meeting Abstracts
- Page 276 and 277:
ARVO 2013 Annual Meeting Abstracts
- Page 278 and 279:
ARVO 2013 Annual Meeting Abstracts
- Page 280 and 281:
ARVO 2013 Annual Meeting Abstracts
- Page 282 and 283:
ARVO 2013 Annual Meeting Abstracts
- Page 284 and 285:
ARVO 2013 Annual Meeting Abstracts
- Page 286 and 287:
ARVO 2013 Annual Meeting Abstracts
- Page 288 and 289:
ARVO 2013 Annual Meeting Abstracts
- Page 290 and 291:
ARVO 2013 Annual Meeting Abstracts
- Page 292 and 293:
ARVO 2013 Annual Meeting Abstracts
- Page 294 and 295:
ARVO 2013 Annual Meeting Abstracts
- Page 296 and 297:
ARVO 2013 Annual Meeting Abstracts
- Page 298 and 299:
ARVO 2013 Annual Meeting Abstracts
- Page 300 and 301:
ARVO 2013 Annual Meeting Abstracts
- Page 302 and 303:
ARVO 2013 Annual Meeting Abstracts
- Page 304 and 305:
ARVO 2013 Annual Meeting Abstracts
- Page 306 and 307:
ARVO 2013 Annual Meeting Abstracts
- Page 308 and 309:
ARVO 2013 Annual Meeting Abstracts
- Page 310 and 311:
ARVO 2013 Annual Meeting Abstracts
- Page 312 and 313:
ARVO 2013 Annual Meeting Abstracts
- Page 314 and 315:
ARVO 2013 Annual Meeting Abstracts
- Page 316 and 317:
ARVO 2013 Annual Meeting Abstracts
- Page 318 and 319:
ARVO 2013 Annual Meeting Abstracts
- Page 320 and 321:
ARVO 2013 Annual Meeting Abstracts
- Page 322 and 323:
ARVO 2013 Annual Meeting Abstracts
- Page 324 and 325:
ARVO 2013 Annual Meeting Abstracts
- Page 326 and 327:
ARVO 2013 Annual Meeting Abstracts
- Page 328 and 329:
ARVO 2013 Annual Meeting Abstracts
- Page 330 and 331:
ARVO 2013 Annual Meeting Abstracts
- Page 332 and 333:
ARVO 2013 Annual Meeting Abstracts
- Page 334 and 335:
ARVO 2013 Annual Meeting Abstracts
- Page 336 and 337:
ARVO 2013 Annual Meeting Abstracts
- Page 338 and 339:
ARVO 2013 Annual Meeting Abstracts
- Page 340 and 341:
ARVO 2013 Annual Meeting Abstracts
- Page 342 and 343:
ARVO 2013 Annual Meeting Abstracts
- Page 344 and 345:
ARVO 2013 Annual Meeting Abstracts
- Page 346 and 347:
ARVO 2013 Annual Meeting Abstracts
- Page 348 and 349:
ARVO 2013 Annual Meeting Abstracts
- Page 350 and 351:
ARVO 2013 Annual Meeting Abstracts
- Page 352 and 353:
ARVO 2013 Annual Meeting Abstracts
- Page 354 and 355:
ARVO 2013 Annual Meeting Abstracts
- Page 356 and 357:
ARVO 2013 Annual Meeting Abstracts
- Page 358 and 359:
ARVO 2013 Annual Meeting Abstracts
- Page 360 and 361:
ARVO 2013 Annual Meeting Abstracts
- Page 362 and 363:
ARVO 2013 Annual Meeting Abstracts
- Page 364 and 365:
ARVO 2013 Annual Meeting Abstracts
- Page 366 and 367:
ARVO 2013 Annual Meeting Abstracts
- Page 368 and 369:
ARVO 2013 Annual Meeting Abstracts
- Page 370 and 371:
ARVO 2013 Annual Meeting Abstracts
- Page 372 and 373:
ARVO 2013 Annual Meeting Abstracts
- Page 374 and 375:
ARVO 2013 Annual Meeting Abstracts
- Page 376 and 377:
ARVO 2013 Annual Meeting Abstracts
- Page 378 and 379:
ARVO 2013 Annual Meeting Abstracts
- Page 380 and 381:
ARVO 2013 Annual Meeting Abstracts
- Page 382 and 383:
ARVO 2013 Annual Meeting Abstracts