Public Health and Communicable Diseases - SA Health - SA.Gov.au
Public Health and Communicable Diseases - SA Health - SA.Gov.au
Public Health and Communicable Diseases - SA Health - SA.Gov.au
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
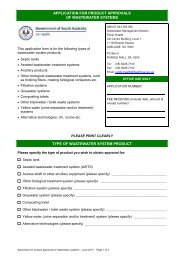
Emphasis on particular goals of public healthsurveillance may vary between different levels of publichealth responsibility. Some goals are achieved mosteffectively by a regional public health unit while othermore strategic aims are best managed by state-baseddisease surveillance units or the CommonwealthDepartment of <strong>Health</strong> <strong>and</strong> Ageing. In South Australia,data generated through communicable diseasesurveillance is most typically used as a prompt foroutbreak investigation, monitoring of disease trends <strong>and</strong>for initiating disease control initiatives. This does notpreclude the use of such data for other means includingepidemiological research <strong>and</strong> programme development.Table 1 lists the goals seen in effective public healthsurveillance.Table 1: Goals of effective public health surveillanceGoals of Surveillance• To detect cases or clusters of cases thereby enablinginterventions to be implemented that preventtransmission or reduce morbidity <strong>and</strong> mortality.• To assess the public health impact of a health eventor determinant <strong>and</strong> measure trends.• To demonstrate the need for public healthintervention programmes <strong>and</strong> resources.• To monitor the effectiveness of disease prevention<strong>and</strong> control measures <strong>and</strong> intervention strategies.• To identify high-risk populations or geographic areasto target interventions <strong>and</strong> guide analytical studies.• To develop hypotheses leading to analyticstudies about disease c<strong>au</strong>sation, transmission ordevelopment.Types of surveillance systems<strong>Public</strong> health surveillance systems have traditionallybeen classified as being passive, active or sentinel,<strong>and</strong> all three types are utilised in the surveillance ofcommunicable diseases in <strong>SA</strong>. 2Passive surveillancePassive disease surveillance usually refers tomonitoring of data supplied to health <strong>au</strong>thorities bydoctors <strong>and</strong> laboratories as a requirement under law.<strong>Communicable</strong> disease surveillance is heavily reliant onpassive surveillance, using both clinical <strong>and</strong> laboratorynotifications, however these systems are likely tounderestimate the true burden of illness as many peoplewith notifiable conditions may only have mild illness<strong>and</strong> do not seek care, while others may be incorrectlydiagnosed or may not receive laboratory testing toconfirm a diagnosis. For example Campylobactergastroenteritis, with over 15,000 notifications nationally,is the most common notifiable c<strong>au</strong>se of foodbornedisease in Australia, with <strong>SA</strong> having the highest statenotification rate (173 per 100,000). 2 Yet estimates ofits true prevalence in Australia are thought to exceed200,000 cases per year. 3 Nevertheless the patternsseen over time are informative <strong>and</strong> provide the basis forpublic health action.Active surveillanceTo preclude issues with under reporting, particularlyfor more serious conditions, more vigorous means ofdetection may be used. In <strong>SA</strong> additional laboratorytesting of all bloody stools for the presence of Shigatoxigenic Escherichia coli is undertaken, 4 as cases wouldnot be detected via routine microbiological examinationor a specific clinical diagnosis. This supplementarysurveillance was implemented in response to a largeoutbreak of Haemolytic Uraemic Syndrome (HUS)c<strong>au</strong>sed by fermented s<strong>au</strong>sage contaminated with E.Coli. 5 This type of surveillance is particularly useful inestablishing prevalence rates for conditions where theremay be a lack of data or where cases occur sporadically.Another illustration of active surveillance is theprocess of case ascertainment during an outbreakinvestigation. If a hospital intensive care doctornotified two cases of HUS a likely response would beto contact other intensive care unit <strong>and</strong> renal units toactively find more cases. Active systems can validatethe representativeness of passive systems, enablemore complete reporting of conditions or be used inconjunction with or part of specific epidemiological oroutbreak investigations.Sentinel surveillance systemsSentinel surveillance systems are established for thepurpose of enabling simple, early detection of disease.Animals are often used to provide this early warning. InAustralia, the Sentinel Chicken Surveillance Programmewas established to detect increases in flavivirus activity. 6The programme involves regular testing of a numberof chicken flocks across Australia for seroconversion toMurray Valley encephalitis virus <strong>and</strong> Kunjin virus in orderto determine levels of risk to human populations fromthese viruses.Sentinel healthcare providers are another example, withclinicians collecting data on selected indicators to assistin estimating the size of a problem among the generalpopulation. The Australian Sentinel Practice Research <strong>and</strong>Evaluation Network is one such example, with GeneralPractitioners (GP) collecting data on presentations forinfluenza-like illness (ILI). Such presentations couldpossibly represent an early expression of increasedinfluenza activity. In <strong>SA</strong> this data is combined withlaboratory reporting of influenza <strong>and</strong> ILI presentationsto emergency departments, to provide evidence of theimpact of seasonal influenza activity (Figure 1 next page).