Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT)
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
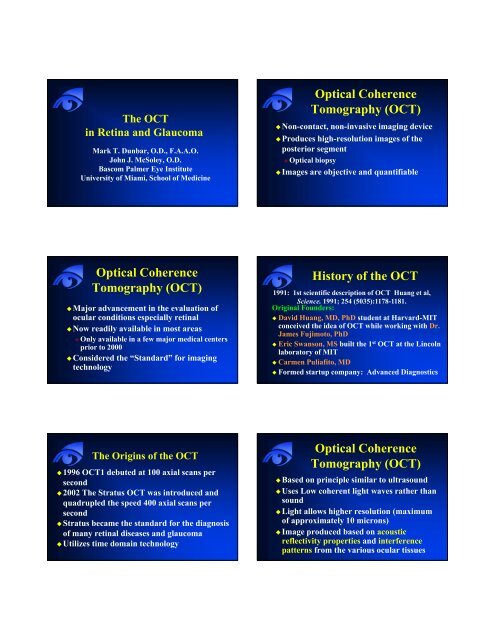
The <strong>OCT</strong>in Retina and GlaucomaMark T. Dunbar, O.D., F.A.A.O.John J. McSoley, O.D.Bascom Palmer Eye InstituteUniversity of Miami, School of Medicine<strong>Optical</strong> <strong>Coherence</strong><strong>Tomography</strong> (<strong>OCT</strong>)Non-contact, non-invasive imaging deviceProduces high-resolution images of theposterior segment <strong>Optical</strong> biopsyImages are objective and quantifiable<strong>Optical</strong> <strong>Coherence</strong><strong>Tomography</strong> (<strong>OCT</strong>)Major advancement in the evaluation ofocular conditions especially retinalNow readily available in most areas Only available in a few major medical centersprior to 2000Considered the “Standard” for imagingtechnologyHistory of the <strong>OCT</strong>1991: 1st scientific description of <strong>OCT</strong> Huang et al,Science. 1991; 254 (5035):1178-1181.Original Founders: David Huang, MD, PhD student at Harvard-MITconceived the idea of <strong>OCT</strong> while working with Dr.James Fujimoto, PhD Eric Swanson, MS built the 1 st <strong>OCT</strong> at the Lincolnlaboratory of MIT Carmen Puliafito, MD Formed startup company: Advanced DiagnosticsThe Origins of the <strong>OCT</strong>1996 <strong>OCT</strong>1 debuted at 100 axial scans persecond2002 The Stratus <strong>OCT</strong> was introduced andquadrupled the speed 400 axial scans persecondStratus became the standard for the diagnosisof many retinal diseases and glaucomaUtilizes time domain technology<strong>Optical</strong> <strong>Coherence</strong><strong>Tomography</strong> (<strong>OCT</strong>)Based on principle similar to ultrasoundUses Low coherent light waves rather thansoundLight allows higher resolution (maximumof approximately 10 microns)Image produced based on acousticreflectivity properties and interferencepatterns from the various ocular tissues
Advantages of <strong>OCT</strong>Quick – takes less than five minutes toobtain images of both eyesNon-invasive and well tolerated by ypatients No injection No biohazard or blood-related risk No medication reactionsMore readily interpreted and understoodby patientsNormal Retinal AnatomySchuman JS, Puliafito CA,Fujimoto JG eds. <strong>Optical</strong> <strong>Coherence</strong><strong>Tomography</strong> of Ocular Disease.Thorofare, NJ: Slack Inc.; 2004.Main Clinical Utilitiesof <strong>OCT</strong> High resolution evaluation of retinal anatomy Diagnosis of macular conditions difficult toestablish with biomicroscopy Quantitative assessment of retinal anatomicalterations Quantitative assessment of vitreoretinalinterface Objective means for monitoring diseaseprogression and/or therapeutic responseDiagnosis of macular conditionsdifficult to establish withbiomicroscopy
50 y/o Creole Female50 y/o Creole Female20/20020/60 20/200Decreased vision OU L > R X 6 monthsFull Thickness Macular Hole20/60Vitreomacular TractionImpending Macular HoleAMD with CNV
VA = 20/300CNV withassociated CMEMacular EdemaInferiorSuperiorClassic ChoroidalNeovascularizationPost-Operative CystoidMacular EdemaVA = 20/100EarlyCMEVA = 20/100LateTemporalNasalIdiopathic CentralSerous ChorioretinopathyVA = 20/400EarlyIdiopathic Central SerousRetinopathyLate
InferiorICSCVA = 20/400SuperiorBreakthroughs with <strong>OCT</strong>Provided New Perspectives in theUnderstanding of Vitreoretinal Macular DiseaseIt has redefined our understanding of thepathogenesis of macular hole formationandExpanded the spectrum of vitreomaculartractionIdiopathic Macular Holes Females 70% 6th to 7th decade No predisposingfactors Blurred VA Metamorphopsia Develops fromperifoveal vitreousdetachment Macular Hole Formation (Arch Ophthalmol. 1999;117:744-751)Stages ofMacular Holes
Stages of Macular Holes0: Stage “0” macular holeI: Pseudocyst associated with traction IA: Yellow spot or ring in macula IB: Loss of foveal depressionII: Partial tear in the sensory retinaIII: Full thickness macular holeIV: Macular hole with PVDVitreomacular TractionOriginally described as a “syndrome”Incomplete or partial PVD at the ONResults in traction at the macula Often in a “dumbbell” shaped configurationProduces macular edema – CMENecessitates pars plana vitrectomyRareSmiddy, Green, Michaels AJO, 1989Vitreomacular Tractionin the Era of <strong>OCT</strong>Not rare!A group of disorders caused by incompletePVDLeads to persistent traction on the maculaProduces in most cases CME anddecreased visual acuityCan be idiopathicCan occur with ERM and macular hole<strong>Optical</strong> <strong>Coherence</strong><strong>Tomography</strong> (<strong>OCT</strong>)Greatly enhances our ability to identifyvitreomacular traction Represents traction at the macula fromincomplete PVD VMT is more common than previously suspected Improved understanding of the pathogenesis ofmacular holes Excellent clinical tool for the evaluation andmanagement of these conditions
Next Generation <strong>OCT</strong>Spectral-Domain <strong>OCT</strong> (Fourier Domain <strong>OCT</strong>) Does not utilize a mirror Analyzes data using a spectrometere e‣ Allows the ability to determine various depthssimultaneously – current <strong>OCT</strong> does this serially Very fast acquisition speed -> 100 X > acquisitionspeed (1.28 for current vs milliseconds) Very high resolution – 3.5 to 6 µ 3-D imagingTime Domain <strong>OCT</strong>• Sequential•1pixelatatime• 1024 pixels per A-scan• .0025 seconds per A scan• 512 A-scans in 1.28 sec• Slower than eye movementsMotion artifact512 A-scans in 1.28 secSlide courtesy of Dr. David Huang, USCFourier Domain <strong>OCT</strong>• Simultaneous• Entire A-scan at once• 2048 pixels per A scan• .00000385 sec per A scan• 1024 A-scans in 0.04 sec• Faster than eye movementsSmall blood vesselsIS/OSChoroidal vessels1024 A-scans in 0.04 secHigher speed, higher definition and higher signal.Spectral Domain <strong>OCT</strong>The CompetitionCarl Zeiss: CirrusOptiVue: p RTvueHeidelberg: SpectralisTopcon26,000Speed(A‐scansper sec)400100The evolution of <strong>OCT</strong>Zeiss <strong>OCT</strong> 1 and2, 1996Fourier domain <strong>OCT</strong>Time domain <strong>OCT</strong>Zeiss Stratus200216 10 5Resolution(μm)OptiVueCerriusSpectralisTopcon 65 x faster 2 x resolutionCirrus HD-<strong>OCT</strong>Time Domain <strong>OCT</strong> & Spectral Domain <strong>OCT</strong> A new member of the Zeiss <strong>OCT</strong> family of products Spectral domain <strong>OCT</strong> technology Capable of volumetric (3D) & high definition linescanning of the retina• Received FDA 510K clearanceFebruary 2007• Available in the fall of 2007
Time Domain and Spectral DomainNormal MaleYellow square on LSLO fundusimage represents the 6mm x 6mmmargins of the scanned macularcubeAdjustable cross hair on fundusimage shows precise location ofthe horizontal and vertical scansselected.Stratus <strong>OCT</strong>Healthy RetinaHealthy RetinaVertical B-scancomprised of 128A-scansStratus <strong>OCT</strong> high-resolution line scan and the Cirrus HD-<strong>OCT</strong> scanreveal details of retinal structureHorizontal B-scancomprised of 512A-scansHigh Definition and High ResolutionAxial resolution,ordefinitiondetermines whichretinal layers can bedistinguished. Axialresolution isdetermined by thelight source.Normal MalePrecise location of raster linesindicated on LSLO fundus imageTransverse resolution determines accuracy with which size and separation offeatures (such as drusen) can be identified. Transverse resolution is determined byoptics of the eye, as limited by pupil size, and as corrected by the scanner.Normal MaleLSLO fundus image with overlay ofretinal thickness mapCirrus HD-<strong>OCT</strong> Image of Schisis3D layer segmentation maps provide detailedvisualization i of histology and pathology3D retinal thickness map3D segmentation of RPE layer3D segmentation of ILM and RPE layers
AMD with DrusenAMD with Drusen38 Year-Old Male, High Myopia with ICSC38 Year-Old Male, High Myopia with ICSCYellow square on LSLO fundus imagerepresents the 6mm x 6mm marginsof the scanned macular cubePrecise location of raster linesindicated on LSLO fundus imageAdjustable cross hair on fundusimage shows precise location of thehorizontal and vertical scansselected.Vertical B-scancomprised of 128A-scansHorizontal B-scan comprisedof 512 A-scans38 Year-Old Male, High Myopia with ICSCScan alignment to previous visitLSLO fundus image with overlayof retinal thickness map3D layer segmentation maps provide detailedvisualization i of histology and pathology3D retinal thickness map3D segmentation of RPE layer3D segmentation of ILM and RPE layers
What is AdvancedVisualization? Visualization of cube data in 3 dimensions beyond dynamic 3Dcube analysis Averaging/Mean imaging of user-defined C-Scan groupingsreferred to as “Slabs” With “Slab” analysis, user can image 2D en face representations ofcommon retinal layers/disorders:Choroidal VasculatureRPE/NSRVitreoretinal InterfaceEpiretinal MembraneChoroidal NeovascularizationPigment Epithelial DetachmentIntraretinal Cystic formations3D Volume RenderingAdvanced VisualizationAdvanced VisualizationAdvanced Visualization3D Volume Rendering withRPE layer exposed•The Tissue Layer image allows you to isolateand visualize a layer of the retina.•The thickness and placement of the layer areadjustable.•This provides a virtual dissection of the retinaby extracting the layer of interestAdvanced VisualizationEn face view of RPE layerThe RTVue 100High Speed, High Resolution <strong>OCT</strong>
Fourier Domain <strong>OCT</strong> – RTVue 100High Speed allows 3-D scanning•<strong>Optical</strong> <strong>Coherence</strong> <strong>Tomography</strong> providescross sectional imaging of the retina•Spectrometry and Fourier Domainmethods allow high h speed data capture(26,000 A scans per second)•Broad-band light source provides highdepth resolution (5 microns)B-scans provide high resolution detailMacula thickness map reveals edemaCystoid Macula EdemaClassic CNVCourtesy: Michael Turano, CRAColumbia University.Courtesy: Michael Turano, CRAColumbia University.horizontalverticalImages courtesy of Dr. Tano, Osaka University
Spectralis HRA+<strong>OCT</strong>The Fusion of Imaging TechnologiesSPECTRALIS TechnologyCombined confocal scanning laserophthalmoscope and spectral domain <strong>OCT</strong>Built on a fundus imaging platformCombines high resolution cSLO C-scan withhigh resolution SD-<strong>OCT</strong> B-scanScans with TruTrack Eye TrackingIncorporates Heidelberg Noise Reduction Eye Tracking using TruTrack ®Eye Tracking Stops 3D Motion ArtifactWithout Eye TrackerWith Eye TrackerArtificial ripplesdue to eye movementsTrue anatomic structureScan does not follow eyeScan tracks with eyeTopcon 3D-<strong>OCT</strong>No glaucoma data base<strong>OCT</strong> in Glaucoma
Traditional Methods ofAssessing GlaucomaIOP monitoring Major risk factorSubjective S evaluationof the optic nerveVisual field testingThere is a need for objectivetesting that can reliably detectthose patients who may haveglaucoma and/or are at risk ofdeveloping glaucomaStructural AssessmentInstruments“According to the AIGS, there is limited butconsistent evidence that automated imagingsystems can detect early to moderate glaucomaequally as well as standardized, expertqualitative assessment of stereoscopic optic discand RNFL photographs in clinical researchsettings.”AIGS Consensus Statements<strong>OCT</strong>: Glaucoma and NFLAnalysisMultiple studies show that <strong>OCT</strong> has theability to detect early glaucoma change bymeasuring NFL thicknessOften before visual field lossWhat is the science that supports this?Value of <strong>OCT</strong> in GlaucomaRNFL analysisOptic p nerve head topographyp Bilateral comparisonsSerial comparisonNormative databaseRetinal Nerve Fiber (RNFL)AnalysisCircular scans aroundthe ONH at radius of1.73 mmScans begin temporal3 scans are acquiredand data is averaged
StandardStandard or Fast More scans more data points 512 scans 1536 data pointsFast Fewer scans - as good sensitivity 256 scans 768 datapoints Normative databaseRNFL MeasurementMeasures differences in delay of thebackscattering of light from the RNFLRNFL is differentiated by an algorithmthat detects anterior edge of the RPE andthe photoreceptor layer positionRNFL Thickness Analysis WithNormative DataAnalysis resultsdisplayed in tabulardisplay and graphsRNFL thicknessgraph in TSNITorientation ti withnormative datadisplayAsymmetrydemonstrated in OUTSNIT graphOD RNFL thicknesswithin normal limits(green)Scan imageScan signalstrength andqualityOS areas of RNFLoutside normallimits (red)Normative Database Provides age-matched reference values forretinal nerve fiber layer thickness measurements FDA approved July 2003 Fast RNFL thickness scans 256 points > 350 subjects; age 20-80, mean age 47 6 sites in US Broad representation of ethnic group No correlation for other demographic factorssuch as ethnicity or gender, right/left eyeStratus <strong>OCT</strong>Stop Light Display ofRNFL Normative Range95% of normal population falls inor below green band; 90% fallswithin green band5% of normal population fallswithin or below yellow band: 4%falls within the yellow band1% falls within red band;considered outside normal limits5%90%4%1%100%95%5%1%0%
RNFL in Glaucoma“False” Positive and Negatives High Myopia Optic nerve tilt Peripapillary atrophy Disc drusen Sectoral pigmentarychanges Retinal edema Retinal cystic changes Retinal traction ERM Mylinated nervefibers Optic nerve pitAssessing Data PointsInferior and SuperiorRNFL AveragesSuperior RNFL Ave = 142.7µ Early Glaucoma = 104.8µAny change repeatable > 12µIs statistically significant**Inferior RNFL Ave = 138.6µ Early Glaucoma = 103.9µGuedes V, Shuman JC, Ophthalmol 2003; 110 (1):77,177-189Normal PatientGlaucoma PatientHow good is <strong>OCT</strong> as DiagnosingGlaucoma….…or Detecting Progression
RNFL Sensitivity and Specificity ofthe <strong>OCT</strong> for Diagnosing GlaucomaBudenz et al Ophthalmology. January 2005;112:3-9 109 normal and 63 glaucoma subjects 18 mild, 21 moderate, 24 severe (VF) Avg RNFL < 5% 84% sensitivity;98% specificity 1 or more quad 1 Quad with Ave RNFLThickness < 1%> 1 Clock Hr with Ave RNFLThickness < 5%> 1 Clock Hr with Ave RNFLThickness < 1%83% (73-92%) 100%89% (81-97%) 92% (87-97%)83% (73-92%) 100%Budenz DL et al. Ophthalmology. January 2005;112:3-9RNFL Sensitivity and Specificity ofthe <strong>OCT</strong> for Diagnosing GlaucomaBudenz et al Ophthalmology. January 2005;112:3-9 Excellent sensitivity andspecificity of RNFLmeasurements using Stratus <strong>OCT</strong>for glaucoma with manifest VFdefects The best parameters seem to be≥1 quadrants abnormal at the≤5% level or ≥1 clock hoursabnormal at the ≤5% levelCorrelation of RNFL Thicknessto Having GlaucomaInferior Quadrant 0.971Mean 0.966Inferior Temporal 0.959Superior Quad 0.952Budenz DL et al. Ophthalmology. January 2005;112:3-9Rogelia 62 y/o Hispanic FemaleCC -> pain/burning in the both eyes c/wdry eyeVA: 20/20 OUAnt Segment unremarkableTA: 12 OUFundusRogelia - Summary63 y/o Hispanic Female presents with dryeye complaintsSuspicious Cups RE inferior thinning anda superior nasal field defect RE (NormalLE), consistent with <strong>OCT</strong> RNFL findings,IOP 12Diagnosis -> NTG RE, No GL LEManagement…initial observation untildocumented progression…then Tx
Ability of <strong>OCT</strong> to DetectLocalized RNFL DefectsJeoung JW et al. Ophthalmology. December 2005; 112; 2157-216355 Patients – 43 NTG, 12 POAG withvisible wedge-shaped RNFL Defects andcorresponding VF defectsThe <strong>OCT</strong> showed good diagnosticagreement with red-free RNFL photosSensitivity of 85.9%; Specificity of 97.4%with normative data baseAbility of <strong>OCT</strong> to DetectLocalized RNFL DefectsJeoung JW et al. Ophthalmology. December 2005; 112; 2157-2163 Sensitivity in inferiorquadrant = 91.3% Sensitivity in superiorquadrant =76% Smaller RNFL defectssuperior Good agreement withlocation of the RNFLdefectReproducibility of <strong>OCT</strong> RNFL MeasurementsBudenz DL et al. Invest Ophthal Vis Sci 2005; 46: 2440-2443Same day reproducibility of RNFLmeasurements of glaucoma andnonglaucomatous eyes using <strong>OCT</strong>Excellent reproducibility in both groups Normal range was 3.5µ-4.7µ Glaucoma range was 5.2µ-6.6µNasal quadrant has most variability 10.2µ-13.0µ Normals vs. 10.2µ-13.8µ glaucomaReproducibilityIntraTest VariabilityUsing Serial Analysis ProgramDocumenting Progression with <strong>OCT</strong>Serial AnalysisExcellent ReproducibilityOn Both VisitsRELE
Documenting Progression with <strong>OCT</strong>Serial AnalysisSensitivity/Specificity BetweenInstrumentsMedeiros FA et al. Arch of Ophthal 2004; 122:82775 pts with glaucoma, 66 normals 70% had early GL visual field lossNo Statistical difference b/w the 3 machinesStratus <strong>OCT</strong> 0.92GDX 0.91HRT II 0.86Agreement BetweenInstrumentsMedeiros FA et al. Arch of Ophthal 2004; 122:827<strong>OCT</strong> and GDX VCC: 89% agreementGDX G VCC HRT II: 81% agreementHRT II and <strong>OCT</strong>: 81% agreementCirrus HD-<strong>OCT</strong>Software Version 3.0†HRT measures optic disc topography and provides indirectmeasurement of RNFL as a secondaryCirrus Software Version 3.0‣ RNFL Thickness Analysis‣ RNFL Normative Data‣ 3D Volume Rendering‣ Custom 5-line Raster Scan‣ High Definition Cross Scan‣ Segmentation Editing Tool‣ Precise registrationRNFL Thickness Analysis
Glaucoma – RNFL Thickness Analysis• Center of disc is automatically identified for precise registration andrepeatability• RNFL thickness display is of a 1.73mm radius circle around the disc• TSNIT graph is compared to normative database of about 300patientsGlaucoma – RNFL Thickness AnalysisThe LSO fundus image is shown with an<strong>OCT</strong> fundus overlay. The red circleindicates the location of the RNFL TNSITcircleThe <strong>OCT</strong> image is a cross section ofthe TSNIT circleRNFL thickness is displayed ingraphic format and compared tonormative dataGlaucoma – RNFLThickness AnalysisThe RNFL thickness map shows thepatterns and thickness of the nerve fiberlayerGlaucoma – RNFL Thickness AnalysisAn OU analysis example (1)The RNFL deviation map is overlaid on the<strong>OCT</strong> fundus image to illustrate preciselywhere RNFL thickness deviates from anormal rangeGlaucoma – RNFL Thickness AnalysisAn OU analysis example (2)Glaucoma PackagegHeidelberg Spectralis
Basic Glaucoma - Circle Scan AnalysisSpectralis: Samples 1536 A-Scans vs. 256 with Cirrus and StratusPhase 1 Glaucoma PackagePosterior 30° Pole AnalysisPosterior Pole Assessment Full thickness Grids correspond toVF Hemisphere analysisGlaucoma Analysis with the RTVue: Nerve Head MapRTVue Glaucoma PackageProvides• Cup Area• Rim Area• RNFL Map16 sector analysiscompares sector values tonormative database andcolor codes result basedon probability values (pvalues)TSNIT graphColor shaded regionsrepresent normativedatabase ranges basedon p‐values
RNFL ParametersGlaucoma Analysis with the RTVue:Nerve Head Map ParametersOptic Disc ParametersThe ganglion cell complex (ILM – IPL)Inner retinal layers provide complete Ganglion cellassessment:• Nerve fiber layer (g‐cell axons)• Ganglion cell layer (g-cell body)• Inner plexiform layer (g-cell dendrites)All parameters color‐coded based oncomparison to normative databaseImages courtesy of Dr. Ou Tan, USCBorderlineSector results inSuperiortemporalregionEarly GlaucomaGCC Analysis may detectdamage before RNFLAbnormalOS NormalparametersTSNIT dipsbelow normalTSNIT showssignificantAsymmetryGCC and RNFL analysis will be correlated, however GCCanalysis may be more sensitive for detecting early damage<strong>OCT</strong> Glaucoma Summary <strong>OCT</strong> is able to accurately detected earlyglaucoma with good reliability Also very good with already establishedglaucoma Determining same day reliability is critical Corroborate your findings To be to accurately utilize serial analysis in futurescans <strong>OCT</strong> is as good as other ON imaging devices<strong>OCT</strong> Retina: Summary“New” technology allows for cross-sectionalimaging of retina structuresAllows detailed imaging of retinal pathologyAllows detailed imaging of retinal pathologyRedefined our understanding of a numberof disease processesThe next generation of imaging - Spectral-Domain <strong>OCT</strong> is already here