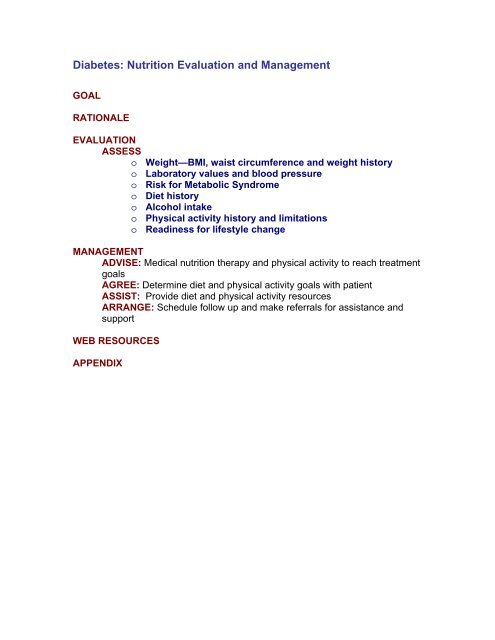
Nutrition: Diabetes Evaluation and Management
Nutrition: Diabetes Evaluation and Management
Nutrition: Diabetes Evaluation and Management
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
DIABETES GOALHelp patients with pre-diabetes decrease their risk for cardiovascular disease<strong>and</strong> diabetes by adopting a healthy lifestyle which includes:• Healthy food choices with emphasis on decreased fat <strong>and</strong> calories• Increased physical activity• Moderate weight lossHelp patients with diabetes achieve the following:• Blood glucose levels as close to normal range as safely possible• Calorie levels to attain <strong>and</strong> maintain reasonable weight• Lipid profile levels that reduce the risk for macrovascular disease• Blood pressure levels that reduce the risk for vascular disease• Optimal health through healthy food choices <strong>and</strong> physical activity• Diet alterations to prevent <strong>and</strong> treat acute <strong>and</strong> chronic complicationsGoals for nutrition therapy for individual patients will vary with age, type ofdiabetes, treatment regimen, co-morbidities, personal <strong>and</strong> cultural preferences,<strong>and</strong> willingness to change behavior.Source: <strong>Nutrition</strong> recommendations <strong>and</strong> interventions for diabetes. <strong>Diabetes</strong>Care 2007;30, Supl 1:S48-S65.
DIABETES RATIONALE<strong>Diabetes</strong> is widely recognized as one of the leading causes of death <strong>and</strong>disability in the United States. The rapid increase in diabetes parallels theincrease in obesity <strong>and</strong> overweight. According to data from the Centers forDisease Control, 20.8 million people (7% of population) have diabetes <strong>and</strong> thenumbers are expected to rise (Centers for Disease Control, 2005).<strong>Diabetes</strong> is expensive with an annual cost to the United States of $132 billionannually, including both indirect <strong>and</strong> direct costs (American <strong>Diabetes</strong> Association,2003).Long-term complications of diabetes affect almost every part of the body. Thedisease often leads to blindness, heart <strong>and</strong> blood vessel disease, stroke, kidneyfailure, amputations, <strong>and</strong> nerve damage. Uncontrolled diabetes can complicatepregnancy, <strong>and</strong> birth defects are more common in babies born to women withdiabetes. About 65% of deaths among those with diabetes are attributed to heartdisease <strong>and</strong> stroke. (Centers for Disease Control <strong>Diabetes</strong> Fact Sheet, 2005http://www.cdc.gov/diabetes/pubs/estimates05.htm#prev)Many patients with diabetes fit the criteria for Metabolic Syndrome, aconstellation of risk factors for heart disease, which include hypertension,abnormal blood lipids, elevated blood sugars, <strong>and</strong> abdominal obesity. SeeMetabolic Syndrome: <strong>Nutrition</strong> <strong>Evaluation</strong> <strong>and</strong> <strong>Management</strong>(http://www.medicine.wisc.edu/mainweb/DOMPages.php?section=naa&page=metabolic)The American <strong>Diabetes</strong> Association includes nutrition therapy as an integralcomponent of diabetes management to prevent <strong>and</strong> treat diabetes, <strong>and</strong> preventor, at least, delay onset of diabetes complications <strong>and</strong> heart disease. (<strong>Diabetes</strong>Care 2007; 30, Supl 1:S4-S41). Numerous studies have shown nutritionintervention has a positive impact on diabetes control <strong>and</strong> reduces the cost ofdiabetes care by decreasing the amount of medication required.• <strong>Nutrition</strong> therapy based on practice guidelines from the American DieteticAssociation has been shown to improve patient outcomes for both Type 1<strong>and</strong> Type 2 diabetes (<strong>Diabetes</strong> Care 2002; 25:608-613 <strong>and</strong> J Am DietAssoc 2003; 103:827-831).• Moderate weight loss with reduced calorie intake <strong>and</strong> increased physicalactivity in obese patients with Type 2 diabetes decreases insulinresistance, decreases fasting blood sugar, <strong>and</strong> reduces the need formedications (<strong>Diabetes</strong> Care 2004; 27:2067-2073).• In the Improving Control with Activity <strong>and</strong> <strong>Nutrition</strong> (ICAN) study, obeseparticipants with Type 2 diabetes in the dietitian-led case managementgroup achieved greater weight loss, needed fewer medications <strong>and</strong> hadgreater improvement in health-related quality of life than patients receivingusual care (<strong>Diabetes</strong> Care 2004;27:1570-1576).
• In the <strong>Diabetes</strong> Prevention Program, obese patients with impaired glucosetolerance achieved a 58% relative reduction in new onset diabetes withintensive lifestyle intervention—a 5-7% weight loss <strong>and</strong> increased physicalactivity (NEJM 2002; 346:393-403). The Finnish <strong>Diabetes</strong> PreventionStudy showed similar results (NEJM 2001; 344:1343-1350).
DIABETES EVALUATIONASSESSo Weight—BMI, waist circumference <strong>and</strong> weight historyo Laboratory values <strong>and</strong> blood pressureo Risk for Metabolic Syndromeo Diet historyo Alcohol intakeo Physical activity history <strong>and</strong> limitationso Readiness for lifestyle changeWeight—BMI, waist circumference <strong>and</strong> weight history• Use Body Mass Index (BMI) to determine if patient is overweight or obese.• Consider measuring waist circumference to assess abdominal obesity.• Assess recent weight changes, <strong>and</strong> if BMI>25, assess history of obesity, i.e.,age of onset, <strong>and</strong> previous weight loss attempts <strong>and</strong> successes.BMI is used to determine obesity• BMI=Weight divided by height squared (Wt kg/Ht m 2 )• St<strong>and</strong>ards are the same for both adult men <strong>and</strong> adult women• Correlates with body fat• Determines degree of obesity <strong>and</strong> health risk• Can be used to track treatment results for obesity• May overestimate body fat in athletes <strong>and</strong> others who have a muscular build• May underestimate body fat in older persons <strong>and</strong> others who have lostmuscle mass• May be inaccurate for patients with edemaThe US Preventive Services Task Force recommends including BMI as a vitalsign.BMI tables http://www.nhlbi.nih.gov/guidelines/obesity/bmi_tbl.htmBMI calculator http://www.nhlbisupport.com/bmi/bmicalc.htmBMI calculator to download to PDA http://hin.nhlbi.nih.gov/bmi_palm.htmBMI ClassificationUnderweight 30Extreme obesity =>40Classification of Overweight <strong>and</strong> Obesityhttp://www.nhlbi.nih.gov/guidelines/obesity/e_txtbk/txgd/414.htm
Waist circumference predicts health risk• Measures excess abdominal fat• Predicts abdominal fat better than waist:hip ratio• Independently predicts health risk when BMI not markedly increased (IfBMI>35, no need to measure waist circumference.)• Is important in diagnosing Metabolic Syndrome• Measure waist circumference correctly for accurate assessment. MeasuringTape Position for Waist (Abdominal) Circumferencehttp://www.nhlbi.nih.gov/guidelines/obesity/e_txtbk/txgd/4142.htmHigh Risk Waist CircumferenceMen>40 in (102 cm)Women >88 cm (>35 in)Measuring Waist Circumferencehttp://www.nhlbi.nih.gov/guidelines/obesity/e_txtbk/txgd/4142.htmLaboratory values <strong>and</strong> blood pressure• HgbA1C• Blood pressure• Fasting lipid profile• Urine for microalbuminuria
Risk for Metabolic SyndromeAssess patient’s risk for Metabolic Syndrome.Risk FactorAbdominal obesity*MenWomenTriglyceridesHDL cholesterolMenWomenBlood pressureFasting glucoseCriteria for Metabolic SyndromeThree or More of the Following Risk FactorsDefining LevelWaist circumference+>102 cm (>40 in)>88 cm (>35 in)>150 mg/dL or drug treatment forelevated triglycerides 100 mg/dL or drug treatment forelevated glucose*Abdominal obesity is more highly correlated with metabolic risk factors than isan elevated BMI.+Guidelines for measuring waist circumference are available athttp://www.nhlbi.nih.gov/guidelines/obesity/e_txtbk/txgd/4142.htmSource: Diagnosis & <strong>Management</strong> of the Metabolic Syndrome: AHA/NHLBIScientific Statement. Circulation. 2005;112:2735-52.http://circ.ahajournals.org/cgi/content/full/112/17/2735Diet historyThe diet history should include what, when <strong>and</strong> how much:• Meals <strong>and</strong> snacking patterns (number/day <strong>and</strong> time of day)• Portion sizes—See Appendix, Table 1: Seven Ways to Size Up YourServings.• Saturated <strong>and</strong> trans fat from dairy products <strong>and</strong> fatty meats, commercialsnack foods <strong>and</strong> pastries, fried foods <strong>and</strong> added fats <strong>and</strong> oils• Refined carbohydrates from baked products, desserts, cookies <strong>and</strong> othersweets• Fiber <strong>and</strong> protective nutrients (potassium, magnesium <strong>and</strong> calcium) fromfruits, vegetables, legumes, nuts <strong>and</strong> whole grains• Sweetened beverages (juice drinks, soda) <strong>and</strong> alcohol• Major sources of sodium from processed foods, eating out <strong>and</strong> added salt• Frequency of restaurant meals, fast food, take out food (Eating away fromhome 4 or more times/week is correlated with obesity.)
• Over-the-counter products—vitamin/mineral supplements, herbs <strong>and</strong> otherdietary supplements. See NIH Office of Dietary Supplements (http://dietarysupplements.info.nih.gov/index.aspx)<strong>and</strong> NIH Medline Plus Drugs <strong>and</strong>Supplements (http://www.nlm.nih.gov/medlineplus/druginformation.html ) forinformation on supplements patients are taking• Use a patient questionnaire to quickly assess dietary habits: REAP (RapidEating Assessment for Patients) with answer key for diet assessment <strong>and</strong>counseling.REAP http://bms.brown.edu/nutrition/acrobat/REAP%206.pdfAnswer key http://bms.brown.edu/nutrition/acrobat/reapmdkey.pdfAlcohol intake• Assess usual intake (frequency <strong>and</strong> quantity).• Use CAGE or other screening tools (Screening for Alcohol Use <strong>and</strong> OtherRelated Problems, NIAAA, April 2005(http://pubs.niaaa.nih.gov/publications/aa65/AA65.pdf) to screen for alcoholabuse if intake appears to be greater than 1 drink/day for women <strong>and</strong> 2drinks/day for men.• Alcohol intake exceeding these levels contributes to high blood pressure <strong>and</strong>elevated triglycerides, <strong>and</strong> is not cardioprotective.• Alcoholic beverages can be a hidden source of calories (alcohol=7calories/gram) <strong>and</strong> contribute to excess body weight.• Can cause hypoglycemia in Type 1 diabetics who drink without eating.What is a “Drink”Serving SizeCalories12 oz regular beer 1505 oz wine 1001.5 oz 80-proof distilled spirits, 100not including mixersPhysical activity history <strong>and</strong> limitations• Physical activity:o Contributes to weight losso Improves lipid profileo Reduces blood pressureo Improves blood sugar <strong>and</strong> decreases insulin resistanceo Reduces risk of cardiovascular disease <strong>and</strong> overall mortalityo May contribute to blood sugar fluctuations in Type 1 diabetes if activity issporadic• Assess limitations with PAR-Q. Physical Activity Readiness Questionnairehttp://www.csep.ca/communities/c574/files/hidden/pdfs/par-q.pdf is a patientquestionnaire used to screen for potential problems with exercise.• Assess current physical activity—frequency, type of activity, <strong>and</strong> amount of
time per session.• How Physically Active Are You?”(http://depts.washington.edu/hprc/publications/rapa.htm) is an easy to readrapid assessment questionnaire of the level <strong>and</strong> intensity of physical activityfor older adults. (Preventing Chronic Disease October 2006http://www.cdc.gov/pcd/issues/2006/oct/06_0001.htm• Ask about inactivity—number of hours per day with television or computer.More than 2 hours per day has been associated with higher risk of obesity inchildren (JAMA 1999;282,1561).Readiness for lifestyle change• Assess patient’s stage of behavior change <strong>and</strong> match intervention to patient’sstage of readiness. See Appendix, Table 2: Stages of Readiness forBehavior Change <strong>and</strong> Recommended Intervention for Each Stage.• Assess availability of social support <strong>and</strong> potential barriers, such asdepression, financial problems or stress.
DIABETES MANAGEMENTADVISE: Medical <strong>Nutrition</strong> Therapy <strong>and</strong> increased physical activity to reachtreatment goalso Medical <strong>Nutrition</strong> Therapyo Meal planning—major dietary componentso Meal planning—other factors to considero Increased physical activityMedical <strong>Nutrition</strong> TherapyDiet strategies to achieve blood sugar control include use of carbohydratecounting, food group exchange lists, <strong>and</strong> individualized carbohydrate goalsbased on analysis of pre- <strong>and</strong> postpr<strong>and</strong>ial blood glucose values.Medical <strong>Nutrition</strong> Therapy for patients who take insulin• These guidelines apply to both Type 1 <strong>and</strong> Type 2 patients who requireinsulin.• To match food with timing <strong>and</strong> peak action of insulin, patients with fixedinsulin dose should have:o Consistent meal times each dayo Consistent carbohydrate at each meal.o Note: Fixed insulin doses are often given as “split <strong>and</strong> mixed insulin,”which means rapid <strong>and</strong> long acting insulin mixed together <strong>and</strong> givenusually with 2 injections/day, pre-breakfast <strong>and</strong> pre-supper. 70/30premixed insulin is not appropriate for patients unwilling or unable `toeat 3 meals daily at consistent times which match the timing <strong>and</strong> peakaction of the 70/30 insulin.• For multiple daily injections (basal bolus insulin, i.e., basal or background <strong>and</strong>bolus or rapid acting insulin taken before meals in 4 injections/day) orcontinuous infusion insulin pump:o Bolus (meal) insulin dose for each patient is determined byindividualized carbohydrate to insulin ratios.o Using their personal carbohydrate to insulin ratio, such as 1 unit rapidacting insulin for every 10 g carbohydrate, patients determine their premealinsulin dose based on carbohydrate content of the upcomingmeal.o Meal times <strong>and</strong> carbohydrate content can be more flexible than withfixed insulin dose.o Multiple daily injections or insulin pump therapy most closely mimicphysiologic insulin secretion in response to meals or hepatic glucoserelease.• To determine insulin regimen, consider individual diet <strong>and</strong> activitypreferences, glycemic goals, functional status, <strong>and</strong> lifestyle.• When reviewing blood sugar records to make adjustments in insulin, considerpatient’s diet, physical activity, usual schedule, insulin action time <strong>and</strong> dose.• Adjust nutrition therapy for Type 2 patients who require insulin to addressMetabolic Syndrome risk factors.
Medical <strong>Nutrition</strong> Therapy for patients who do not take insulin• <strong>Nutrition</strong> therapy is based on the individual patient’s metabolic profile <strong>and</strong>diagnoses related to Metabolic Syndrome (presence of obesity, lipidmetabolism disorder, hypertension <strong>and</strong>/or diabetes).• The focus of diet <strong>and</strong> activity changes will vary depending upon the individualpatient’s risk factors.Diet <strong>and</strong> Physical Activity for Metabolic SyndromeIncrease physical activity150 minutes minimum/weekLose weight At least 7% of initial body weight if BMI >25Decrease total & saturated fat Total fat not >25-35% caloriesSaturated fat 50-60% total calorieswith emphasis on whole grains, fruits &vegetablesNot >2400 mg/dayUp to 25-30 gm/dayUp to 9 servings fruits & vegetables/dayPer 2000 caloriesMg 500 mgCa 1200 mgK 4700 mgDiet for Metabolic Syndrome• When translated to food, the diet for Metabolic Syndrome is similar to theMediterranean diet <strong>and</strong> contains:o An abundance of whole grains, fruits <strong>and</strong> vegetableso Legumes (dried beans, soy, split peas, lentils), low fat dairyproducts, fish <strong>and</strong> poultry as primary protein sourceso Moderate amounts of fat from canola or olive oils <strong>and</strong> nutso Reduced amounts of red meats <strong>and</strong> refined carbohydrates,especially sweets <strong>and</strong> high sugar beverageso Reduced sodium from processed foods• See patient information about Metabolic Syndrome, Insulin Resistance <strong>and</strong>Pre-<strong>Diabetes</strong> http://diabetes.niddk.nih.gov/dm/pubs/insulinresistance/ fromthe National <strong>Diabetes</strong> Information Clearinghouse.
Meal planning—major dietary componentsCarbohydrate—sugars, starches <strong>and</strong> fiber• Dietary carbohydrate primarily determines post pr<strong>and</strong>ial glucose levels.• Major carbohydrate sources are grains, breads, cereals, dry beans <strong>and</strong> otherlegumes, starchy vegetables, fruit <strong>and</strong> fruit juice, milk <strong>and</strong> yogurt, sweetenedbeverages, sweets <strong>and</strong> desserts.• Both the amount <strong>and</strong> type of carbohydrate <strong>and</strong> a host of other factors havesome influence over post pr<strong>and</strong>ial blood sugar. Some examples of factorsthat influence post pr<strong>and</strong>ial blood sugar are cooking methods, the mix ofprotein, carbohydrate, fat in the meal <strong>and</strong> the degree of insulin resistance.• Low carbohydrate diets, lower than the RDA of60% calories from carbohydrate) can increaseinsulin resistance, raise triglycerides <strong>and</strong> reduce HDL-cholesterol.• No evidence exists to support the use of diets based on “no concentratedsweets” <strong>and</strong> “no added sugar.”• Clinical studies show sucrose does not increase blood sugar more than equalcaloric amounts of starch. Although sucrose <strong>and</strong> sucrose containing foodsneed not be totally eliminated, they should be included in the totalcarbohydrate allotment <strong>and</strong> eaten in the context of a healthy diet. Smallportions will be required to stay within dietary carbohydrate <strong>and</strong> calorie goals.Most of the carbohydrate should come from fruits, vegetables, whole grains,<strong>and</strong> legumes.• Very high fiber diets of up to 50 gm fiber/day may reduce glycemia,hyperinsulinemia, <strong>and</strong> lipids, but are not practical or palatable for Americantastes. The ADA recommendation for dietary fiber is the same as for thegeneral population of 14 gm/1000 calories, or about 25-35 gm/day. Diets ofmost Americans are very low in fiber.
FoodFOOD SOURCES OF FIBERSolubleFiber,gmTotalFiber, gmCEREAL GRAINS(½ cup cooked)Barley 1 4Oatmeal 1 2FRUIT(1 medium)Apple 1 4Banana 1 3Citrus (orange, grapefruit) 2 2-3Pear 2 4BEANS/LENTILS(½ cup cooked)Black, kidney, navy beans 2-3 5-7Lentils 1 8Peas, green
• 15%-20% of calories from protein for an1800 calorie diet is 65-90 gm/day.Protein in 1800 Calorie DietFood GroupProtein, gm6 grains, breads, starches 186 oz meat 423 8-oz servings milk 24Total 84• Dietary protein has minimal effect on plasma glucose concentration but doesstimulate insulin secretion.• High protein, low carbohydrate diets (e.g., Atkins Diet) are not recommendedfor weight loss:o Long term safety <strong>and</strong> efficacy for patients with diabetes not knowno High protein diets lack antioxidant-rich, high fiber fruits <strong>and</strong> vegetables<strong>and</strong> contain high amounts of saturated fato Do not produce significantly more weight loss than other low caloriediets after 12 monthsFat• Saturated fat in the diet should be limited to less than 7% of total calories.• Higher percent of calories from monounsaturated fat (with total fat up to 40%calories) can decrease postpr<strong>and</strong>ial glycemia <strong>and</strong> triglycerides, <strong>and</strong> mayincrease HDL-cholesterol levels.• High fat diets may lead to excessive calorie intake that can promote weightgain <strong>and</strong> increase insulin resistance.• Trans fatty acids should be minimized in the diet as they raise LDLcholesterol<strong>and</strong> reduce HDL-cholesterol. Trans fats are formed during thehydrogenation process to convert liquid oil to a solid fat when makingmargarine or shorteningoMajor food sources of trans fats:• Stick margarine• Shortening <strong>and</strong> foods made with shortening• Commercially prepared fried foods• Baked products such as pastries, donuts <strong>and</strong> crackers whichcontain hydrogenated fats• Most microwave <strong>and</strong> movie theatre popcorno Minimize intake by using liquid oils <strong>and</strong> soft margarine <strong>and</strong> avoidingfoods fried in restaurants <strong>and</strong> commercial foods prepared withhydrogenated fats.• Margarines with added plant stanol/sterol esters (Trade names Benecol <strong>and</strong>Take Control):o 2 -4 tablespoons/day provide 2-3 gm plant stanol/sterol <strong>and</strong> lower LDLcholesterol6-15%o Have little effect on triglycerides or HDL-cholesterol
o Provide 40-80 calories/tablespoon. Calories from other foods mayneed to be decreased to prevent weight gain.Meal planning—other factors to considerThe glycemic index• The glycemic index (GI) is a relative ranking of postpr<strong>and</strong>ial blood glucoseresponse to constant amounts of carbohydrate from various foods. Each foodis assigned a GI from 0 to 100 according to the extent that food raises bloodglucose levels when compared to the blood glucose response of a referencefood assigned a GI of 100 (Am J Clin Nutr 2002; 76:5-56).• Foods with a lower GI raise blood glucose levels less than those with a higherGI, when amounts providing the same amount of carbohydrate are compared.• For example, the GI of lentils is 40 when compared to glucose with a GI of100.Glycemic IndexTwo Hour Blood Sugar Response of Lentils Compared to GlucoseSt<strong>and</strong>ard-GlucoseGI Glucose=100Test food-LentilsGI Lentils=40• Tests to determine GI are conducted in a fasting state <strong>and</strong> with only a singlefood.• The GI of a food can be significantly changed by food preparation methods(degree of cooking, combination with acids, etc) <strong>and</strong> by the food combinationsthat are part of a typical meal that includes fiber, fat <strong>and</strong> protein.• For more information, see Home of the Glycemic Indexhttp://www.glycemicindex.com , a database maintained by the University ofSidney, Australia.
Foods with Higher <strong>and</strong> Lower Glycemic IndexHigher Glycemic FoodsLower Glycemic FoodsBreads, baked products made with white flour Whole grain cereals & breadsWhite riceBrown riceRefined breakfast cerealsWhole fruitsWhite spaghetti, cooked until very softLegumesSoft drinks <strong>and</strong> juiceOatsSugarBarleyPotatoesDairy productsHigh GI =70 or greater, Medium GI=56-69, Low GI =55 or lessUse of the glycemic index for diabetes meal planning• The American <strong>Diabetes</strong> Association’s position is that monitoring total gramsof carbohydrate in the diet should be the primary method for meal planning,but that a low GI diet may provide a modest additional benefit (<strong>Diabetes</strong> Care2004 27; 2266-2271).• Reports from the Nurses’ Health Study indicate that the risks of Type 2diabetes <strong>and</strong> coronary heart disease are decreased in women with dietarypatterns having a lower overall GI <strong>and</strong> higher total fiber content (NEJM 2000;343:16-22).• The World Health Organization <strong>and</strong> the Food <strong>and</strong> Agriculture Organizationhave recommended diets based on low GI foods to reduce the risk ofcoronary heart disease, diabetes <strong>and</strong> obesity.• Foods with low GI (e.g., dairy products, legumes, certain fruits, unprocessedgrains) may reduce postpr<strong>and</strong>ial blood sugar <strong>and</strong> help prevent obesity <strong>and</strong>cardiovascular disease (JAMA 2002; 287:2414-2423 <strong>and</strong> <strong>Diabetes</strong> Care2003; 26:2261-2267).• Several popular diet books for weight loss are based on the GI concept.These diets require complicated counting of glycemic index <strong>and</strong> calculatingglycemic load which is a measure of the total amount of carbohydrate in ameal. However, the benefits can be obtained by choosing a variety of low GIfoods <strong>and</strong> by decreasing high GI foods without a lot of counting. Low GI foodsgenerally have fewer calories <strong>and</strong> more fiber, antioxidants, <strong>and</strong> other nutrientsthan high GI foods.Non-nutritive sweeteners <strong>and</strong> sugar alcohols• Do not raise blood sugar• Are safe when consumed in amounts within levels established as safe by theFood <strong>and</strong> Drug Administration• The following sweeteners with no calories are currently available <strong>and</strong>approved by the Food <strong>and</strong> Drug Administration:o Saccharin (Sweet n Low)o Aspartame (Nutrasweet or Equal)—Most widely used in foods <strong>and</strong>beverages
o Acesulfame potassium (Sunette)o Sucralose (Splenda)o Neotame• Food products often contain both nutritive <strong>and</strong> non-nutritive sweeteners.• Sugar alcohols (mannitol, sorbitol, xylitol) <strong>and</strong> hydrogenated starchhydrolysates are nutritive sweeteners used in commercial c<strong>and</strong>y. They have aslower glycemic response. Large amounts can cause an osmotic diarrhea<strong>and</strong> can increase blood sugar. Sugar alcohols have about 2 calories/gmcompared to sucrose at 4 calories/gm, but the total calories may be high insugar free c<strong>and</strong>y due to high fat content. Patients should be cautioned to limitthe amount to 1-2 small pieces.Alcohol• Can be hidden source of calories (1 gm alcohol has 7 calories)• Moderate amount of alcohol with calorie free mixers has no acute effect onglucose or insulin concentration.• Patients on insulin should consume alcohol with food to reduce risk ofhypoglycemia. Alcohol is preferentially metabolized by the liver <strong>and</strong> caninterfere with gluconeogenesis.• Patients taking glucophage or thiazolidinediones should avoid alcohol.• Limit daily intake to not more than 1 drink/day for women <strong>and</strong> 2 drinks/day formen.What is a “Drink”Serving SizeCalories12 oz regular beer 1505 oz wine 1001.5 oz 80-proof distilled 100spirits, without added mixerSupplements: botanicals/herbs/vitamins/minerals• Surveys show people do not mention over-the-counter supplements whenasked about medications, <strong>and</strong> need to be asked directly.• Most supplements have little evidence available for either help or harm. TheAmerican <strong>Diabetes</strong> Association has no specific recommendations for the useof herb or vitamin/mineral supplements in people with diabetes other thanwhat is recommended for the general population without diabetes, such as inpregnancy, for elders, people on calorie restricted diets, etc.• ADA advises that chromium <strong>and</strong> magnesium supplements, which are oftenrecommended in the popular press for patients with diabetes or obesity, arenot recommended due to lack of evidence of long term safety <strong>and</strong> efficacy.• Supplements can be dangerous, especially for patients taking multiplemedications <strong>and</strong> with multiple co-morbidities. For example, ephedra (a.k.a.ma huang), which was recently banned by the FDA, can increase heart rate<strong>and</strong> blood pressure, especially when combined with caffeine.• Information about dietary supplements is available from NIH Office of Dietary
Supplements (http://dietary-supplements.info.nih.gov/index.aspx), NIHMedlinePlus Drugs <strong>and</strong> Supplements(http://www.nlm.nih.gov/medlineplus/druginformation.html) <strong>and</strong> ConsumerLab (http://www.consumerlab.com).Acute illnessAdvise patients about carbohydrate intake <strong>and</strong> liquids when unable to tolerateregular meals:• Test blood sugar every 2-4 hours <strong>and</strong> urine for ketones if blood sugar>240.• Drink 8 oz of calorie free fluids/hour while awake, i.e., water, diet softdrinks, sugar-free Kool-Aid.• For nausea, vomiting or intolerance to food or fluids, sip on 15-20 gmcarbohydrate containing liquid every hour. Example: Drink 12 -16 oz ofGatorade or non-diet soft drink over a 4 hour period.• To prevent ketosis, at least 150 gm carbohydrate/day is needed.• If blood sugar>300, usual carbohydrate intake may not be needed.Diet for chronic complications• Nephropathy: Protein intake should be limited to the RDA 0.8 g/kg bodyweight/day for patients with any degree of kidney disease.• Gastroparesiso Diet varies depending upon frequency <strong>and</strong> severity of nausea <strong>and</strong>vomiting <strong>and</strong> delayed gastric emptying.o Advise 6 small meals instead of 3 larger ones <strong>and</strong> avoidance of fatty<strong>and</strong> high fiber foods that prolong gastric emptying.o Use liquid meal replacements during periods of exacerbation ofdelayed gastric emptying.o Bolus insulin may be taken after meals if needed. Measuring bloodsugar 2-4 hours after meals will help decide the best time to takeinsulin.o During severe exacerbation, consider enteral feeding with jejunostomytube.o See Gastroparesis <strong>and</strong> <strong>Diabetes</strong> for patient information.(http://digestive.niddk.nih.gov/ddiseases/pubs/gastroparesis/)Diet Rx for hospital <strong>and</strong> long term care• Hospital—The term “ADA diet” to order hospital diets based on calorie level isno longer used. Consult with the nutrition services department for protocol forwriting diet prescriptions for hospitalized patients with diabetes.• Long-term care—Order “Consistent Carbohydrate.” Liberalized regular dietswith consistent mealtimes <strong>and</strong> consistent carbohydrate intake may promoteadequate intake, decrease risk of malnutrition <strong>and</strong> improve quality of lifewithout exacerbating blood sugar control.
Increased physical activity• The American <strong>Diabetes</strong> Association recommends both aerobic exercise <strong>and</strong>resistance training for patients with diabetes, unless contraindicated:(<strong>Diabetes</strong> Care 2007;30, Supl 1:S4-S41)• At least 150 minutes/week of moderate-intensity aerobic physicalactivity or at least 90 minutes/week of vigorous aerobic exercise, <strong>and</strong>distributed over at least 3 days/week with no more than 2 consecutivedays between exercise sessions• People with Type 2 diabetes are advised to perform resistance trainingat lease 3 days/week, targeting all major muscle groups.• Both aerobic activity <strong>and</strong> resistance training improve insulin sensitivity.• Patients who participate in structured exercise programs of =>8 weeks havesignificantly lower A1C values than control groups, independent of weightloss.• Previously sedentary patients with diabetes who plan to start physical activityof greater intensity than brisk walking should have a medical evaluation forcardiac risk <strong>and</strong> other potential contradictions such as severe neuropathy orretinopathy.• Regular exercise may prevent diabetes in individuals at high risk for diabetes.• Obese sedentary individuals need encouragement <strong>and</strong> realistic goals toincrease physical activity. Obese individuals may achieve a moderateintensity at lower levels due to the work load of excess weight <strong>and</strong> lowcardiorespiratory fitness.Examples of Moderate IntensityPhysical Activity*Walking 1 ¾ miles in 35 minutes (20 minute mile)Bicycling 5 miles in 30 minutesWater aerobics for 30 minutesSwimming laps for 20 minutesDancing fast for 30 minutesShoveling snow for 15 minutesGardening 30-45 minutesRaking leaves for 30 minutesWashing windows or floors for 45-60 minutes*Roughly equivalent to expending 150 caloriesThe Practical Guide to Identification, <strong>Evaluation</strong>, <strong>and</strong>Treatment of Overweight <strong>and</strong> Obesity in Adults, 2000.http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_b.pdf• An hour a day is necessary for significant weight loss but is unrealistic formany patients. See Institute of Medicine report, Dietary Reference Intakes for
Macronutrients http://www.iom.edu/report.asp?id=4340.• A more realistic goal for physically unfit patents is to start with 10 minutesevery other day <strong>and</strong> increase to 30-45 minutes on most, <strong>and</strong> preferably all,days to expend 100-200 calories. Walking is practical because of safety <strong>and</strong>accessibility.• Physical activity may be intermittent throughout the day or all at one time.• Limit sedentary time (screen time with TV, computer) to
AGREE: Determine diet <strong>and</strong> physical activity goals with patiento Match your intervention to the patient’s stage of behavior changeo What to say to patient not ready to make diet or physical activitychangeso Goals for patient ready to make diet changeso Goals for patient ready to increase physical activityMatch your intervention to patient’s stage of behavior change• See Appendix Table 2, Stages of Readiness for Behavior Change <strong>and</strong>Recommended Intervention at Each Stage• For physical activity counseling to match stages of behavior change, seeCenter for Chronic Illness Prevention <strong>and</strong> Health Promotion, PhysicalActivity—Getting Startedhttp://www.cdc.gov/nccdphp/dnpa/physical/starting/index.htmWhat to say to patient not ready to make diet or physical activity changesDiscuss personal risks <strong>and</strong> benefits of change. You might say:“Eating a healthy diet for diabetes <strong>and</strong> becoming morephysically active are very important things you can do toimprove your blood sugars. This will reduce your risk ofcomplications of diabetes.”“Even small changes would help <strong>and</strong> you might be able tocut down on the amount of medicine you take. I’d like tohelp you when you are ready.”Goals for patient ready to make diet changesEvaluate diet for variety from food groups <strong>and</strong> portion sizes. See WAVE (Weight,Activity, Variety, <strong>and</strong> Excess) <strong>Nutrition</strong> Assessment <strong>and</strong> Counseling toolhttp://bms.brown.edu/nutrition/acrobat/wave.pdf.Review diet history with patient <strong>and</strong> collaboratively determine one or two goals:• Drink only diet soda• Limit portion size of high carbohydrate foods, especially cereals, pasta,mashed potatoes to not more than 1 fist size portion• Add fruit or vegetable at every meal• Eat leaner meats, like loin <strong>and</strong> round cuts, low fat hamburger• Try 1% or skim milk• Eat more soluble fiber from beans, oats, fruits• Eat 1 oz nuts daily• Read <strong>Nutrition</strong> Facts labels to determine carbohydrate choices• Take lunch to work instead of eating fast food
Goals for patient ready to increase physical activityCollaboratively agree on one or two specific goals to increase physical activity:• Walk on treadmill for 30 minutes during the 6 o’clock TV news• Go to water exercise class 3 times/week at fitness club• Walk dog Monday, Wednesday, Friday after work with my spouse for 20minutes• Make a date with myself to exercise—put on the calendar just like anyother appointment
ASSIST: Provide diet <strong>and</strong> physical activity resourceso Diet resources for diabetes meal planningo Physical activity resourcesDiet resources for diabetes meal planningDiet complexity varies with diabetes treatment regimen, functional level of patient<strong>and</strong> co-morbidities such as Metabolic Syndrome. Individualized meal planstailored to specific patients have replaced the st<strong>and</strong>ardized one-size-fits-all“ADA” diets. All meal plans should help patients work toward:• Calorie level to reach desirable weight or at least not gain• Decreased refined carbohydrate <strong>and</strong> sugars• Decreased total, saturated <strong>and</strong> trans fats with emphasis onmonounsaturated fats• Low fat dairy products, low fat meats <strong>and</strong> non-meat protein sources• Increased fiber from fruits, vegetables, legumes, <strong>and</strong> whole grainsMeal planning with diabetes food pyramid—simplified approach• What I Need to Know about Eating <strong>and</strong> <strong>Diabetes</strong>, based on the diabetes foodpyramid, is an easy to read resource useful when working with low literacy orlow functioning patients. (http://diabetes.niddk.nih.gov/dm/pubs/eating_ez/)• Visual images which compare serving size to common objects help estimateportions. See Appendix, Table 1: Seven Ways to Size Up Your Servings orWhat Size is Your Serving?http://www.kidsnutrition.org/images/pdfs_nyc/USDAposters/servingsize_poster.pdf• Use the “Plate Method” to visualize food groups for simplified meal planning.(http://www.cdc.gov/pcd/issues/2007/jan/06_0050.htm)
Meal Planning with the Plate MethodLunch/DinnerMilkFruitVegetablesMeat &OtherProteinStarch &BreadStarch & Bread, Fruit, <strong>and</strong> Milk food groups raise blood sugarLow carbohydrate Vegetables raise blood sugar in negligible amountsMeat/Protein foods raise blood sugar very little with moderate portions
Meal planning with basic carbohydrate counting• A specific number of carbohydrate choices is assigned for meals <strong>and</strong> snacksbased on calorie needs.• A carbohydrate choice is the amount of food that contains 15 gramscarbohydrate.Carbohydrate Choices for Common Foods1 serving = 1 carbohydrate choice or ~15 gm carbohydrateGrains/Starches Fruits Milk Other CarbohydratesBread, 1 sliceCereal,unsweetened,¾ cupCorn, ½ cupCrackers, snack,4-5Hamburger orhot dog bun, ½Banana,½ mediumBerries, 1 cupCanned fruit injuice or water,½ cupFresh fruit,1 mediumApple, Orange,Peach, PearFruit juice,1/3 to ½ cupButtermilk, 1 cupLow fat or non fat,1 cupYogurt, lowfat,plain, 1 cupYogurt, artificiallysweetened, 1 cupCake, no icing,2 inch square, 1Casserole or hot dish,½ cupChili, ½ cupCookie, 3 inch, 1Donut, plain, ½ smallPasta, ½ cup Grapes 12-15 Granola bar, 1 smallPeas, ½ cup Kiwi, 1 Pizza, thin crust,1 slicePopcorn, plain, Melon, 1 cupPasta sauce, ½ cup3 cupsPotato, 1 small or Raisins, 2 TbspPotato chips, 1 oz½ cupRice, 1/3 cup Plums, 2 small Soup, broth, milk orbean, 1 cupTortilla, 6 inch, 1 Vanilla wafers, 5
• Most adults with moderate activity need 3-5 carbohydrate choices (45-75 gmcarbohydrate) per meal. The Sample Meal Plan shows the carbohydratechoices <strong>and</strong> other food group servings for an approximate 1800 calorie mealplan.MealSample Meal Plan ~ 1800 CALORIESCARBOHYDRATE COUNTING1 CARB CHOICE =15 GM CARBOHYDRATETotalCarbChoicesStarch Fruit Milk MoreCarbLowCarbVegMeatBreakfast 4 2 1 1 0-1ozFatsSnackAsdesiredLunch 4 3 1 AsdesiredSnack 1 1 AsdesiredSupper 4 3 1 AsdesiredSnack 2 1-2 Asdesired3 oz3-4 ozEatlowfatfoodsTotal 15 8 3 2 2 7-8 oz
• Many patients with diabetes say, “I just avoid sugar.” But carbohydratechoices can be excessive even in a meal that appears “healthy” <strong>and</strong> does nothave foods with added sugar. Compare the foods, portion sizes <strong>and</strong> totalcarbohydrate choices in the two lunch menus.Comparison of Carbohydrate Choices in 2 Lunch MenusMenu 11 cup beefstew/potatoes1 slice bread withmargarine1 apple (tennis ballsize)CarbChoice Menu 2CarbChoice2 1 cup pasta salad 21 1 large bagel with tuna 41 1 large apple 21 can diet soda 0 12 oz unsweetened 3orange juiceTotal 4 Total 11• To use carbohydrate counting, patients need to know:o Food groups that contain carbohydrateo Portion sizeo How to read a <strong>Nutrition</strong> Facts label• Food groups that contain carbohydrate:o Food groups with carbohydrate are starch/bread, fruit, milk, desserts <strong>and</strong>sweets. White potatoes, sweet potatoes, peas, corn, <strong>and</strong> winter squashare starchy vegetables that are high in carbohydrates.o Food groups with limited or no carbohydrate are nonstarchy vegetables(such as green beans, lettuce, peppers, broccoli, etc.), meat/meatsubstitutes, fats <strong>and</strong> free foods, i.e., foods with
o Patients can measure food portions or use visual aids to help estimateportions.:• See Appendix, Table 1: Seven Ways to Size Up Your Servings.• See What Size is Your Serving, a colorful poster comparingserving size to common objects.http://www.kidsnutrition.org/images/pdfs_nyc/USDAposters/servingsize_poster.pdfo Restaurant portions have become larger <strong>and</strong> larger in recent years.Patients need special strategies to rein in portions when eating out. SeeCalorie cost of Supersizing.Calorie Cost of SupersizingLocation Item Size Ounces Calories Fat, gmCinnabon Minibon 3 300 11Cinnabon 8 670 34BaskinRobbinsStarbucksTaco BellBurger KingMcDonald’s7-ElevenChocolatechip icecreamCafé lattewith wholemilkNachosKidsScoop2.5 150 10Double8 540 34ScoopTall 12 210 11Venti 20 350 18Supreme 7 440 24Mucho18 1320 82Gr<strong>and</strong>eWhopper 10 680 39Whopper1710 69Value MealFrench friesSnickersCokeClassicKing sizefries <strong>and</strong>cokeSmall 2.4 210 10Supersize 7 610 29Regular 2.1 280 14“Big One” 3.7 510 24Gulp 16 150 0Double64 600 0GulpFrom Wallet to Waistline: The Hidden Costs of Supersizing. The NationalAlliance for <strong>Nutrition</strong> <strong>and</strong> Activity, Center for Science in the Public Interesthttp://www.cspinet.org/
• How to read a <strong>Nutrition</strong> Facts label for carbohydrate choices:o For example: a 1 cup serving of a food that has 31 gm carbohydrate onthe <strong>Nutrition</strong> Facts label below is 2 carbohydrate choices (15 gm=1carbohydrate choice). A 2 cup portion (2 servings as defined by the<strong>Nutrition</strong> Facts label) is 4 carbohydrate choices.o A common mistake patients make when reading the <strong>Nutrition</strong> Factslabel is to consider only the sugars instead of the total carbohydrate.
CAUTION!Check the <strong>Nutrition</strong> Facts Label for Total Carbohydrate6 oz yogurt no-sugar-added 16 gm total carbohydrate6 oz yogurt with sugar <strong>and</strong> 34 gm total carbohydratehigh fructose corn syrupRead the label for total carbohydrate instead of sugar as thesugar is included in the total carbohydrate.Advanced carbohydrate counting• For patients using multiple daily injections or continuous insulin infusionpumps:o Multiple daily injections—background long-acting insulin plus bolusrapid-acting insulin with mealso Insulin pump with continuous insulin—pump programmed by patient todeliver insulin bolus prior to meals <strong>and</strong> continuous background insulin• Bolus or meal insulin dose is based on individually determined carbohydrateto-insulinratio from diet <strong>and</strong> blood sugar logs—approximately 8-20 gmcarbohydrate/unit rapid acting insulin.• Using their carbohydrate to insulin ratio, patients determine the amount ofbolus or meal insulin to take based on the carbohydrate content of the meal.For example, a patient who takes 1 unit of rapid acting insulin for every 10 gmcarbohydrate would take 5 units rapid acting insulin for a meal with 50 gmcarbohydrate.• Supplements of rapid acting insulin or delayed food intake can be used tocorrect high pre-meal blood glucose.• This approach offers more flexibility to accommodate irregular mealschedules, variable carbohydrate intake at meals, <strong>and</strong> variable activity.Appropriate role of snacks• A common misperception by patients about diet for diabetes is that frequenteating, i.e., snacking or up to 6 small meals, is necessary. Historically, thisbelief is likely due to the need for snacks for patients taking split <strong>and</strong> mixeddoses of NPH <strong>and</strong> Regular insulin twice daily.• Snacks are not necessary for obese type 2 patients who are diet controlled,who take insulin sensitizer oral hypoglycemic agents, or who use long-actinginsulin (glargine or detemir) <strong>and</strong> rapid acting insulin (aspart, lispro orglulisine).• Rapid acting insulin supplements may be needed for large snacks with morethan 2 carbohydrate choices. For example, a teen boy who eats a peanutbutter s<strong>and</strong>wich <strong>and</strong> a 16 oz glass of milk as an after school snack has used4 carbohydrate choices <strong>and</strong> should administer additional insulin.• Patients may need help choosing low or no carbohydrate snacks.
Low or No Carbohydrate SnacksCarbFoodChoicesTriscuit crackers, 5 1Fudgsicle, 1 bar 1Popcorn, 3 cups 1Teddy Grahams,15 1Small piece fruit (tennis ball size) 1Fruit juice bar 1Light yogurt, 6 oz 1Peanuts, 1 oz (ping pong ball size) 0Low fat string cheese 0Treating hypoglycemia• 15 -15 Rule for Treatment of Hypoglycemia:o If blood sugar is under 70, take 15 gm carbohydrateo Wait 15 minutes <strong>and</strong> re-test blood sugaroIf blood sugar still
Physical activity resourcesA useful tool to motivate some patients is a pedometer that counts steps.• Short term goal: Measure my usual daily steps with a pedometer <strong>and</strong>increase by 1,000 steps.• Long term goal: Slowly increase steps to 10,000 steps per day orapproximately 5 miles.• For information about ordering a pedometer <strong>and</strong> to Take the 10,000 StepsChallenge! see http://www.new-lifestyles.com/challenge.html.Web-based physical activity resources:• Physical Activity http://www.cdc.gov/nccdphp/dnpa/physical/index.htm, acomprehensive Website on physical activity with information ranging fromGetting Started to defining the Components of Physical Activity from theCenter for Chronic Disease Prevention <strong>and</strong> Health Promotion• NIH Senior Health exercise information for older adultshttp://nihseniorhealth.gov/exercise/toc.html• America on the Move—Web-based program to encourage people to move2,000 steps more <strong>and</strong> eat 100 calories less/day to prevent the 2 lb/yeargained by most Americans http://www.americaonthemove.org/
ARRANGE: Schedule follow-up appointments <strong>and</strong> make referrals forassistance <strong>and</strong> supportLong-term success is more likely with regular follow-up via office visits, groupsupport or encouragement by telephone. Consider referrals to:• Medical nutrition therapy, registered dietitians http://www.eatright.org• Personal trainers <strong>and</strong> exercise programs at YMCA or fitness clubs
WEB RESOURCESFor patientsAmerican <strong>Diabetes</strong> Associationwww.diabetes.org<strong>Diabetes</strong> Prevention Program, George Washington Universityhttp://www.bsc.gwu.edu/dpp/index.htmlvdocNational <strong>Diabetes</strong> Education Programhttp://ndep.nih.gov/National Institute of <strong>Diabetes</strong> <strong>and</strong> Digestive <strong>and</strong> Kidney Diseases-<strong>Nutrition</strong>www.niddk.nih.gov/health/nutrition.htmThe <strong>Nutrition</strong> Source: Knowledge for Healthy Eating, Department of<strong>Nutrition</strong>, Harvard School of Public Healthhttp://www.hsph.harvard.edu/nutritionsource/For cliniciansWisconsin Essential <strong>Diabetes</strong> Mellitus Care Guidelineshttp://dhfs.wisconsin.gov/Health/diabetes/DBMCGuidelns.htmAmerican <strong>Diabetes</strong> Associationwww.diabetes.orgCenter for Disease Control: Division of <strong>Diabetes</strong> Translationwww.cdc.gov/diabetes/index.htm<strong>Nutrition</strong> history form. Hark L <strong>and</strong> Deen D. Taking a nutrition history: Apractical approach for family practice physicians. Amer Fam Phy March15,1999, pp 1521-1537. http://www.aafp.org/afp/990315ap/1521.html<strong>Nutrition</strong> principles <strong>and</strong> recommendations in diabetes. <strong>Nutrition</strong>recommendations <strong>and</strong> interventions for diabetes. <strong>Diabetes</strong> Care 2007;30,Supl 1:S48-S65.http://care.diabetesjournals.org/cgi/content/full/30/suppl_1/S48WAVE (Weight, Activity, Variety, Excess) <strong>Nutrition</strong> assessment <strong>and</strong>recommendations tool from Brown University, Rhode Isl<strong>and</strong>.http://bms.brown.edu/nutrition/acrobat/wave.pdf
APPENDIXTable 1. Seven Ways to Size Up Your ServingsTable 2. Stages of Readiness for Behavior Change <strong>and</strong> RecommendedIntervention for Each Stage
Table 1. Seven Ways to Size Up Your ServingsSeven Ways to Size Up Your ServingsMeasure food portions several times so you can learn to estimate your portion or use thepictures below as a guide.13 ounces of meat is about the size <strong>and</strong>thickness of a deck of playing cards or anaudiotape cassette.234567A medium apple or peach is about the sizeof a tennis ball.1 ounce of cheese is about the size of 4stacked dice.1/2 cup of ice cream is about the size of aracquetball or tennis ball.1 cup of mashed potatoes or broccoli isabout the size of your fist.1 teaspoon of butter or peanut butter isabout the size of the tip of your thumb.1 ounce of nuts or small c<strong>and</strong>ies equals oneh<strong>and</strong>ful.
Table 2. Stages of Readiness for Behavior Change <strong>and</strong> RecommendedIntervention for Each StageStages of Readiness for Behavior Change <strong>and</strong>Recommended Intervention for Each StageStage Patient ClinicianPrecontemplationGoal: Patient willbegin thinkingabout changeContemplationGoal: Patient willexamine benefits<strong>and</strong> barriers tochange• Not thinking aboutchange• May be resigned• Feeling of nocontrol• Denial; does notbelieve it applies toself• Believesconsequences arenot serious• Weighing benefits<strong>and</strong> costs ofbehavior, proposedchange• Use relationship-buildingskills• Personalize risk factors• Give data about patient’svitals, lab results, etc.compared with norm• Rather than use scaretactics, express your caringconcern• Use teachable moments (thesymptom as a message)• Educate in small bits,repeatedly, over time• Ask “How would you know ifyour ___ was a problem foryou?”• Ask “If you were to decide tochange, what do you imaginemight be some advantages?”• Elicit from patient thereasons to change <strong>and</strong> theconsequences of notchanging• Explore ambivalence; praisethe patient for consideringthe difficulties of change• Restate both sides ofambivalence• Question possible solutionsfor one barrier at a time• Pose advice gently as “asolution that has beeneffective for some patientsmight be adaptable to you” toavoid patient’s naturalresistance
Table 2, continuedPreparationGoal: Patient willdiscover theelementsnecessary fordecisive actionActionGoal: Patient willtake decisiveactionMaintenanceGoal: Patient willincorporatechange into dailylifestyleRelapseGoal: Learn fromthe temporarysuccess <strong>and</strong> reengagepatient inthe changeprocess• Experimenting withsmall changes• Taking a definitiveaction to change• Maintaining newbehavior over time• Experiencing normalpart of the processof change• Usually feelsdemoralized• Encourage the patient’sefforts• Ask which strategies thepatient has decided on forrisk situations• Ask for a change date• Reinforce the decision• Delight in even smallsuccesses• View problems as helpfulinformation• Ask what else is needed forsuccess• Continue reinforcement• Ask what strategies havebeen helpful <strong>and</strong> whatsituations problematic(provides physician withmore information to use withother patients as well)• Reframe from “failure” tosuccessful for a while plusnew lessons for continued“success”• Remind the patient thatchange is a process, thatmost people “recycle”Zimmerman G, Olson C, & Bosworth M. A ‘stages of change’ approach to helpingpatients change behavior. Amer Fam Phys March 1, 2000, pp 1409-1422(http://www.aafp.org/afp/20000301/1409.html).Prochaska JO, DiClemente CC, Norcross JC. In search of how people change.Am Psychol 1992; 47:1102-1114.Miller WR, Rollnick S. Motivational interviewing: preparing people to changeaddictive behavior. New York: Guilford, 1991:191-202.