Quiz topic 1 - General Practice and Primary Health Care Academic ...
Quiz topic 1 - General Practice and Primary Health Care Academic ...
Quiz topic 1 - General Practice and Primary Health Care Academic ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
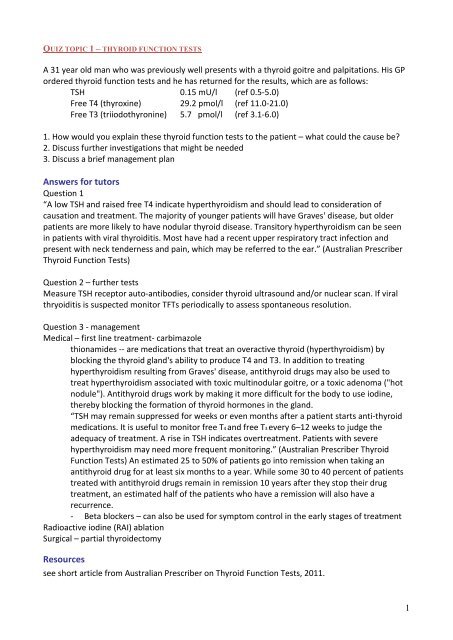
QUIZ TOPIC 1 – THYROID FUNCTION TESTS<br />
A 31 year old man who was previously well presents with a thyroid goitre <strong>and</strong> palpitations. His GP<br />
ordered thyroid function tests <strong>and</strong> he has returned for the results, which are as follows:<br />
TSH 0.15 mU/l (ref 0.5-5.0)<br />
Free T4 (thyroxine) 29.2 pmol/l (ref 11.0-21.0)<br />
Free T3 (triiodothyronine) 5.7 pmol/l (ref 3.1-6.0)<br />
1. How would you explain these thyroid function tests to the patient – what could the cause be?<br />
2. Discuss further investigations that might be needed<br />
3. Discuss a brief management plan<br />
Answers for tutors<br />
Question 1<br />
“A low TSH <strong>and</strong> raised free T4 indicate hyperthyroidism <strong>and</strong> should lead to consideration of<br />
causation <strong>and</strong> treatment. The majority of younger patients will have Graves' disease, but older<br />
patients are more likely to have nodular thyroid disease. Transitory hyperthyroidism can be seen<br />
in patients with viral thyroiditis. Most have had a recent upper respiratory tract infection <strong>and</strong><br />
present with neck tenderness <strong>and</strong> pain, which may be referred to the ear.” (Australian Prescriber<br />
Thyroid Function Tests)<br />
Question 2 – further tests<br />
Measure TSH receptor auto-antibodies, consider thyroid ultrasound <strong>and</strong>/or nuclear scan. If viral<br />
thryoiditis is suspected monitor TFTs periodically to assess spontaneous resolution.<br />
Question 3 - management<br />
Medical – first line treatment- carbimazole<br />
thionamides -- are medications that treat an overactive thyroid (hyperthyroidism) by<br />
blocking the thyroid gl<strong>and</strong>'s ability to produce T4 <strong>and</strong> T3. In addition to treating<br />
hyperthyroidism resulting from Graves' disease, antithyroid drugs may also be used to<br />
treat hyperthyroidism associated with toxic multinodular goitre, or a toxic adenoma ("hot<br />
nodule"). Antithyroid drugs work by making it more difficult for the body to use iodine,<br />
thereby blocking the formation of thyroid hormones in the gl<strong>and</strong>.<br />
“TSH may remain suppressed for weeks or even months after a patient starts anti-thyroid<br />
medications. It is useful to monitor free T4 <strong>and</strong> free T3 every 6–12 weeks to judge the<br />
adequacy of treatment. A rise in TSH indicates overtreatment. Patients with severe<br />
hyperthyroidism may need more frequent monitoring.” (Australian Prescriber Thyroid<br />
Function Tests) An estimated 25 to 50% of patients go into remission when taking an<br />
antithyroid drug for at least six months to a year. While some 30 to 40 percent of patients<br />
treated with antithyroid drugs remain in remission 10 years after they stop their drug<br />
treatment, an estimated half of the patients who have a remission will also have a<br />
recurrence.<br />
- Beta blockers – can also be used for symptom control in the early stages of treatment<br />
Radioactive iodine (RAI) ablation<br />
Surgical – partial thyroidectomy<br />
Resources<br />
see short article from Australian Prescriber on Thyroid Function Tests, 2011.<br />
1
QUIZ TOPIC 2 – BOWEL CANCER SCREENING<br />
A 45 year old woman comes to your general practice to ask you about bowel cancer screening.<br />
1. What questions would you ask her to determine her risk of bowel cancer?<br />
2. She has no personal history <strong>and</strong> is currently asymptomatic, but based on the answers to her<br />
family history the following genogram is developed. Based on this, what screening, if any, would<br />
you recommend?<br />
3. When is FOBT recommended for the general population?<br />
4. The patient wants you to describe what is involved in having a colonoscopy performed. What<br />
would you advise her? What are the risks?<br />
Answers for tutors<br />
Question 1<br />
a. Personal history -Bowel cancer, colorectal adenomas, inflammatory bowel<br />
disease of 8 years or more<br />
b. Family history -History of multiple large adenomas, other cancers eg<br />
endometrial, ovarian, stomach, small bowel, renal pelvis or ureter, biliary tract,<br />
brain; <strong>and</strong> age at which family members affected<br />
c. Symptoms -Rectal bleeding, symptoms of anaemia, change in bowel habit,<br />
abdominal pain, weight loss<br />
Question 2<br />
She is at moderately increased risk because she has one first degree relative with bowel cancer<br />
diagnosed before age 55. She has 3-6 times greater than the average risk, however should be<br />
advised that 70-90% of people in this risk bracket will never develop bowel cancer. However she<br />
should be offered the following screening:<br />
• Colonoscopy every 5 years (you would start this at age 50 or 10 years younger than the age<br />
of first diagnosis bowel cancer in the family) – starting now<br />
• Consider offering FOBT in the intervening years.<br />
2
Question 3<br />
FOBT recommended at least every 2 years for all people over 50.<br />
Note regarding the Government funded FOBT program:<br />
Currently only those turning 50, 55, or 65 years of age, who hold a Medicare card or DVA<br />
gold card, are currently being invited to take part in the program. Next year it will be<br />
exp<strong>and</strong>ed to 60 year olds <strong>and</strong> to 70 year olds in 2015. It is not until 2017-18 that biennial<br />
screening will be commenced – this will be for 72 year olds only initially. Hence it will not<br />
be for many years all Australians aged between 50 <strong>and</strong> 74 years will be offered free<br />
screening every two years, consistent with the recommendations of the National <strong>Health</strong><br />
<strong>and</strong> Medical Research Council. This can currently be arranged by patients through<br />
pharmacies <strong>and</strong> GPs.<br />
Question 4<br />
Before the test clear fluids <strong>and</strong> a liquid medication are used to empty the bowel. The<br />
doctor uses a long flexible tube instrument called a colonoscope to examine the lining of<br />
the rectum <strong>and</strong> colon. You will be sedated during this procedure. If any polyps (growths)<br />
are found, the doctor will remove these <strong>and</strong> send them away to be analysed under a<br />
microscope. You may be given some preliminary results after the procedure <strong>and</strong> will be<br />
asked to come back <strong>and</strong> see the doctor or your GP for the final results <strong>and</strong> the results of<br />
any biopsies taken.<br />
Risks of colonoscopy (from Flinders Medical Centre)<br />
• Incomplete colonoscopy: occurs in 5-20% of cases depending on age <strong>and</strong> if there<br />
has been previous pelvic/abdominal surgery. Would need to have followup with<br />
virtual endoscopy or barium enema<br />
• Missed lesions: Can occur in 2-8% of cases. This is why important to have FOBT in<br />
intervening years.<br />
• Perforation of colon: This will vary by centre but may be between 1 in 400 <strong>and</strong> 1 in<br />
800<br />
• Bleeding from bowel: this is more common after polypectomy – In 1 in 100 cases of<br />
polypectomy the bleeding may be sufficient enough to require transfusion.<br />
• Dehydration with acute renal failure – is related to the bowel preparation<br />
Resources<br />
Familial aspects of bowel cancer – Cancer Council<br />
3
QUIZ TOPIC 3 – RHEUMATOLOGY<br />
A 66 year old woman comes to your general practice with 6 months of gradually worsening<br />
bilateral shoulder pain <strong>and</strong> stiffness <strong>and</strong> has lost 4kg. There is pain <strong>and</strong> stiffness in both shoulders<br />
<strong>and</strong> some pain in her hips. The pain is worse in the morning <strong>and</strong> can be so severe that she finds it<br />
difficult to wash/comb her hair. There is no history of antecedent injury or different activity at the<br />
time of onset. She has trialled NSAIDs with mild benefit.<br />
She has no personal history of prior joint pains <strong>and</strong> there is no history of rheumatological disease<br />
in the family. She has been on statin therapy for 3 years for hypercholesterolaemia (but no recent<br />
changes to her medication).<br />
<strong>General</strong> appearance: fatigued BMI 23, no pallor, pink conjunctivae; Vitals: BP 130/80 HR 72 reg<br />
Shoulder: restricted ROM in all movements, restricted to 60 degrees abduction/flexion (bilateral).<br />
Hips: restricted ROM in all movements (bilateral)<br />
Cardio: Normal S1-S2, nil added; Resp: nad; Abdo: nad; Neuro: nad<br />
No visual changes, no scalp tenderness or tenderness over temporal arteries<br />
1. What are the differential diagnoses?<br />
2. What tests would you order?<br />
3. What are some appropriate management options for this patient?<br />
Answers for tutors<br />
Question 1 - differentials<br />
• Polymyalgia Rheumatica (PMR)<br />
• Seronegative arthritis<br />
• Rheumatoid Arthritis<br />
• Other inflammatory arthritis (SLE, Psoriatic arthritis)<br />
• OA<br />
• Malignancy<br />
• Fibromyalgia<br />
• Viral myalgias<br />
Question 2 - tests<br />
• FBE<br />
• E/LFTs<br />
• ESR/CRP<br />
• TFTs<br />
• Rheumatoid factor/anti-CCP<br />
• (second line inflammatory markers could be ordered – if specific conditions are suspected<br />
ANA/ANCA/dsDNA/anti-Ro)<br />
• Consider imaging: if so, of what?<br />
4
Investigation findings:<br />
FBE: nad<br />
UEC: nad<br />
LFTs: nad<br />
TFTs: nad<br />
ESR: 95<br />
CRP: 30<br />
Antibody screen: nad<br />
Question 3 – management Polymyalgia Rheumatica<br />
1) Look for temporal arteritis (giant cell arteritis) which occurs in 20% of people with PMR.<br />
2) Corticosteroids (explain weaning dose); requires monitoring <strong>and</strong> review.<br />
3) Osteoporosis screening with DEXA scan if on steroids >5mg for > 3/12<br />
4) Non-pharmacological (including Smoking, nutrition, alcohol, physical activity -SNAP):<br />
a. Education<br />
b. Active; low impact exercise (e.g. swimming, walking)<br />
c. Well-balanced diet (maintain healthy weight; avoid risk of other health problems)<br />
d. Physiotherapist<br />
e. Rheumatologist<br />
5
QUIZ TOPIC 4 – BREAST LUMP<br />
A 37 year old female presents to you with a left breast lump that she has just noticed in the<br />
shower yesterday for the first time. It is not painful. She is very anxious because she is worried<br />
about cancer. She has no past medical history. She has a 3 year old son who she breast fed for 6<br />
months <strong>and</strong> then went back to work. She has just finished her menstrual period. She is using<br />
condoms for contraception at present although used the combined oral contraceptive pill for<br />
many years prior to conceiving. She smoked for 5 years until she gave up at the age of 23.<br />
Family history: Maternal aunt diagnosed with breast cancer aged 55years <strong>and</strong> is still alive.<br />
Paternal Gr<strong>and</strong>mother breast cancer aged 70 years <strong>and</strong> survived until the age of 80 years. No<br />
family history of any other cancer including ovarian, bowel, prostate, pancreas etc.<br />
1. What would you do on examination?<br />
2. What would the differential diagnosis be for a woman with a discrete lump at this age?<br />
3. Would you do any investigations? What is the triple test?<br />
4. Assuming a benign result now, when should she commence mammogram screening?<br />
Answers for tutors<br />
Question 1 - examination<br />
• Expose both breasts – patient to take top <strong>and</strong> bra off.<br />
• Inspect breasts with arms by sides, arms above head <strong>and</strong> arms pressing on hips.<br />
• Palpate breasts sitting up <strong>and</strong> lying down.<br />
• Palpate cervical, supraclavicular <strong>and</strong> axillary lymph nodes.<br />
On examination you find there is nothing of significance on inspection. On palpation, a 20mm X<br />
20mm smooth, firm, non tender round lump palpable in the left breast in the 3 o’clock position<br />
just 20mm lateral to the nipple. The lump is mobile <strong>and</strong> not tethered to any surrounding<br />
structures. The right breast is unremarkable. There is no associated cervical, supraclavicular or<br />
axillary lymphadenopathy.<br />
Question 2 – differential diagnoses<br />
• Benign: fibroadenoma, cyst, abscess, fibrocystic change, gl<strong>and</strong>ular parenchyma,<br />
phyllodes tumour,<br />
• Malignant: Breast carcinoma, malignant phyllodes tumour,<br />
Most likely diagnosis: Fibroadenoma.<br />
Cyst would be softer <strong>and</strong> very mobile, abscess would be associated with signs of inflammation<br />
including erythema, warmth <strong>and</strong> tenderness. Phyllodes tumour presents similar to a fibroadenoma<br />
but usually presents much larger e.g. > 30-40mm in size.<br />
6
Question 3 – investigations - the triple test<br />
Any new breast lump should be investigated using the triple test.<br />
The triple test involves:<br />
- History <strong>and</strong> examination.<br />
- Imaging e.g. with an ultrasound <strong>and</strong>/or mammogram.<br />
- Non-excisional biopsy: Fine needle aspirate cytology <strong>and</strong>/or core biopsy.<br />
In 99.6% of breast cancers, the triple test is positive. A positive triple test is defined by any of the 3<br />
components being suspicious. A negative triple test is defined by all 3 components being either<br />
negative or benign. If triple test is positive you need to do a surgical excision/biopsy.<br />
You would now proceed to doing an Ultrasound. If there were any suspicious signs on the<br />
Ultrasound then you would do a mammogram.<br />
Ultrasound shows a hyperechoic lesion with a 25mm diameter.<br />
A core biopsy would be arranged under ultrasound control for this type of lesion – most commonly<br />
a fibroadenoma would be found.<br />
If time permits – could discuss management of a fibroadenoma<br />
You need to take into consideration patient’s age, lump size, symptoms the patient is experiencing<br />
<strong>and</strong> imaging/biopsy results.<br />
There are essentially 2 options:<br />
• Conservative: if the lump is not bothering the patient <strong>and</strong> there are no indications<br />
for surgery (see below) you can monitor it with ultrasound every 6-12 months <strong>and</strong><br />
refer again to a specialist if there are any changes to the lump.<br />
• Surgical excision: if the lump is bothering the patient or there are suspicious<br />
features. Surgery is recommended if lump > 40mm, age of patient > 40, biopsy<br />
results concering, the lump is bothering the patient e.g. painful, the fibroadenoma<br />
is increasing in size while being monitored.<br />
There is no evidence that fibroadenoma increases the risk of developing breast cancer.<br />
Fibroadenoma cells are just as likely as normal breast tissue cells to develop cancer.<br />
Question 4: - screening<br />
Breastscreening Victoria provides free mammograms to all women over the age of 40 years.<br />
Screening is generally recommended every 2 years for women aged 50 to 69 years.<br />
BRCA 1 <strong>and</strong> 2 genetic testing – appropriate for women with strong family history in 1 st degree<br />
relatives – refer to genetic counselling service first.<br />
Resource<br />
National Breast Cancer Centre – Investigation of a new breast symptom, 2006<br />
7
QUIZ TOPIC 5 – DIABETES<br />
A 55 year old man presents worried he may have diabetes, as he has developed a fungal groin rash over the<br />
last few weeks <strong>and</strong> is very tired. He has searched the internet <strong>and</strong> feels that he has several of the diabetes<br />
risk factors.<br />
1. How would you determine his risk of type 2 diabetes? Are there any online tools that you can use to<br />
assist?<br />
2. What tests would you order to determine whether he has diabetes?<br />
After testing you determine he does have type 2 diabetes.<br />
3. What are the key management points in managing type 2 diabetes? Include in your answer issues around<br />
monitoring, drug <strong>and</strong> non-drug treatments, health promotion etc.<br />
Answers for tutors<br />
Question 1 – risk factors<br />
AUSDRISK is a great tool for this: http://www.ausdrisk.com.au/<br />
• Family history of diabetes<br />
• Obesity – particularly central<br />
• Symptoms – polyuria/polydipsia, fungal infections, tiredness, blurred vision<br />
• Symptoms or history of complications – e.g. retinopathy, nephropathy, neuropathy,<br />
cardiovascular disease<br />
• Examination: BMI & waist circumference, Acanthosis nigrens, evidence of neuropathy<br />
• Urine testing in the clinic - glycosuria or proteinuria – although a formal urine<br />
microalbuminuria test is more accurate<br />
• R<strong>and</strong>om finger prick for blood sugar<br />
Question 2 – diagnostic tests<br />
• Fasting glucose > 5.5<br />
• Proceed to GTT<br />
• HbA1c is now approved for diagnosis of T2 diabetes >=6.5%. Currently not Medicare<br />
rebateable, but likely will be in 2013. If diabetes present, may order HbA1c (if not done<br />
previously)<br />
• Tests for complications - EUC/Urine Microalbumin<br />
Question 3 - management<br />
a. Lifestyle modification is the key first line therapy, involves no side effects, <strong>and</strong> if<br />
adhered to may reverse diabetes in up to 60-70% cases. Education relating to<br />
carbohydrate intake is key. 150min/wk of moderately strenuous exercise is highly<br />
8
advised; healthy dietary changes including moving from highly refined to less processed<br />
low GI foods, adequate intake of vegetables <strong>and</strong> wholegrains <strong>and</strong> care with<br />
carbohydrate intake; decrease or cease alcohol consumption; cease smoking; weight<br />
reduction aiming initially for 10% weight reduction.<br />
b. Management involving other allied health professionals such as diabetic educator,<br />
dietician, exercise physiologist will often greatly assist the GP in achieving lifestyle goals<br />
with a willing patient.<br />
c. Education around finger prick BGL monitoring <strong>and</strong> goals of BGLs should be given<br />
(roughly aiming BGL 4-8 fasting <strong>and</strong> 6-10 post pr<strong>and</strong>ial depending on the person),<br />
although there is little evidence that this is effective at improving control in people who<br />
are not requiring insulin.<br />
d. Annual review at least with the patient’s GP will be important for follow up of HbA1c<br />
<strong>and</strong> consideration of other risk factors, monitoring BP, weight, lipids, microalbumin,<br />
feet, eyes.<br />
e. Medications that may be considered if along with or if lifestyle therapy is not enough<br />
Metformin is first line, then possibly a sulphonylurea e.g. Glicazide. There are a range of<br />
other medications that may be considered <strong>and</strong> are probably beyond the scope of this<br />
quiz. Eventually insulin therapy may be needed if inadequate control.<br />
Resource<br />
For more information about the management of T2 diabetes in general practice, see:<br />
http://www.diabetesaustralia.com.au/Documents/DA/What%27s%20New/12.10.02%2<br />
0Diabetes%20Management%20in%20<strong>General</strong>%20<strong>Practice</strong>.pdf<br />
9