Web-economic-crisis-health-systems-and-health-web
Web-economic-crisis-health-systems-and-health-web Web-economic-crisis-health-systems-and-health-web
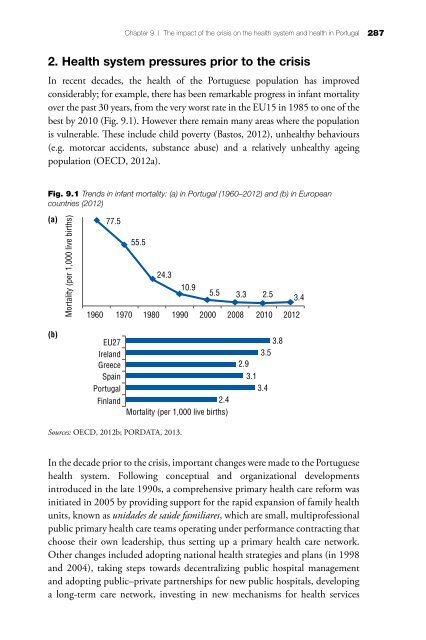
Chapter 9 | The impact of the crisis on the health system and health in Portugal 287 2. Health system pressures prior to the crisis In recent decades, the health of the Portuguese population has improved considerably; for example, there has been remarkable progress in infant mortality over the past 30 years, from the very worst rate in the EU15 in 1985 to one of the best by 2010 (Fig. 9.1). However there remain many areas where the population is vulnerable. These include child poverty (Bastos, 2012), unhealthy behaviours (e.g. motorcar accidents, substance abuse) and a relatively unhealthy ageing population (OECD, 2012a). Fig. 9.1 Trends in infant mortality: (a) in Portugal (1960–2012) and (b) in European countries (2012) (a) Mortality (per 1,000 live births) 77.5 55.5 24.3 10.9 5.5 3.3 2.5 3.4 1960 1970 1980 1990 2000 2008 2010 2012 (b) EU27 Ireland Greece Spain Portugal Finland 2.4 Mortality (per 1,000 live births) 3.8 3.5 2.9 3.1 3.4 Sources: OECD, 2012b; PORDATA, 2013. In the decade prior to the crisis, important changes were made to the Portuguese health system. Following conceptual and organizational developments introduced in the late 1990s, a comprehensive primary health care reform was initiated in 2005 by providing support for the rapid expansion of family health units, known as unidades de saúde familiares, which are small, multiprofessional public primary health care teams operating under performance contracting that choose their own leadership, thus setting up a primary health care network. Other changes included adopting national health strategies and plans (in 1998 and 2004), taking steps towards decentralizing public hospital management and adopting public–private partnerships for new public hospitals, developing a long-term care network, investing in new mechanisms for health services
288 Economic crisis, health systems and health in Europe: country experience contracting, advances in pharmaceutical policy such as the introduction of generic drugs, improvements to waiting list management, rationalizing emergency and maternity services, and investment in more human resources for health services, particularly physicians and nurses. Although the Portuguese NHS is considered to be better performing than many of the country's other public sectors, and a “Portuguese health cluster” bringing together health services, research institutions and industry to promote the economic value of the health sector was created in the 2000s, concerns about the sustainability of the NHS have been voiced repeatedly since the mid-1990s. In 2007, a Commission on the Financial Sustainability of the NHS established by the Ministry of Health reported its main findings and recommendations (Simões, Barros & Pereira, 2007). These included: • maintaining the principle of basic, mandatory and universal health insurance, financed through taxation; • reducing the tax credits for private health care expenditures; • making public subsystems that finance health care expenditures for public servants financially self-sustainable (i.e. discontinuing subsidies from the general state budget); and • under exceptional circumstances, temporarily establish an earmarked tax to complement NHS financing. These recommendations were not implemented at the time, but most of them were included in the AP by mid-2011. By 2008, notable challenges included high OOP payments, relatively high expenditure on pharmaceuticals and low nurse-to-physician and GP-tospecialist ratios. There were also difficulties accessing primary health care services in some parts of the country. Although surgical waiting times were still high, some progress had been achieved, although less so for outpatient waiting times. Lastly, local public health infrastructure still required modernization. 3. Health system responses to the crisis Specific to the health system, the objectives of the AP were to improve efficiency and effectiveness, encourage more rational use of services, control expenditure, reduce public spending on pharmaceuticals (to 1.25% of GDP by the end of 2012 and about 1% of GDP in 2013) and reduce hospital operating costs. More rational use of services and cost-containment were expected to generate savings of 0.3% of GDP in 2013, of which two-thirds of savings were expected from pharmaceuticals (Table 9.2). The Ministry of Health was actively committed to implementing the AP, particularly those on pharmaceutical policies.
- Page 270 and 271: Chapter 7 | The impact of the crisi
- Page 272 and 273: Chapter 7 | The impact of the crisi
- Page 274 and 275: Chapter 7 | The impact of the crisi
- Page 276 and 277: Chapter 7 | The impact of the crisi
- Page 278: Chapter 7 | The impact of the crisi
- Page 281 and 282: 248 Economic crisis, health systems
- Page 283 and 284: 250 Economic crisis, health systems
- Page 285 and 286: 252 Economic crisis, health systems
- Page 287 and 288: 254 Economic crisis, health systems
- Page 289 and 290: 256 Economic crisis, health systems
- Page 291 and 292: 258 Economic crisis, health systems
- Page 293 and 294: 260 Economic crisis, health systems
- Page 295 and 296: 262 Economic crisis, health systems
- Page 297 and 298: 264 Economic crisis, health systems
- Page 299 and 300: 266 Economic crisis, health systems
- Page 301 and 302: 268 Economic crisis, health systems
- Page 303 and 304: 270 Economic crisis, health systems
- Page 305 and 306: 272 Economic crisis, health systems
- Page 307 and 308: 274 Economic crisis, health systems
- Page 309 and 310: 276 Economic crisis, health systems
- Page 311 and 312: 278 Economic crisis, health systems
- Page 313 and 314: 280 Economic crisis, health systems
- Page 316 and 317: Chapter 9 The impact of the crisis
- Page 318 and 319: Chapter 9 | The impact of the crisi
- Page 322 and 323: Chapter 9 | The impact of the crisi
- Page 324 and 325: Chapter 9 | The impact of the crisi
- Page 326 and 327: Chapter 9 | The impact of the crisi
- Page 328 and 329: Chapter 9 | The impact of the crisi
- Page 330 and 331: Chapter 9 | The impact of the crisi
- Page 332 and 333: Chapter 9 | The impact of the crisi
- Page 334 and 335: Chapter 9 | The impact of the crisi
- Page 336 and 337: Chapter 9 | The impact of the crisi
- Page 338 and 339: Chapter 9 | The impact of the crisi
- Page 340 and 341: Chapter 9 | The impact of the crisi
- Page 342 and 343: Chapter 9 | The impact of the crisi
- Page 344 and 345: Chapter 9 | The impact of the crisi
- Page 346 and 347: Chapter 9 | The impact of the crisi
- Page 348 and 349: Chapter 9 | The impact of the crisi
- Page 350 and 351: Chapter 9 | The impact of the crisi
- Page 352: Chapter 9 | The impact of the crisi
- Page 356 and 357: Albania Genc Burazeri and Enver Ros
- Page 358 and 359: Country profiles of health system r
- Page 360 and 361: Country profiles of health system r
- Page 362 and 363: Austria Thomas Czypionka and Maria
- Page 364 and 365: Country profiles of health system r
- Page 366 and 367: Azerbaijan Fuad Ibrahimov Economic
- Page 368 and 369: Country profiles of health system r
Chapter 9 | The impact of the <strong>crisis</strong> on the <strong>health</strong> system <strong>and</strong> <strong>health</strong> in Portugal<br />
287<br />
2. Health system pressures prior to the <strong>crisis</strong><br />
In recent decades, the <strong>health</strong> of the Portuguese population has improved<br />
considerably; for example, there has been remarkable progress in infant mortality<br />
over the past 30 years, from the very worst rate in the EU15 in 1985 to one of the<br />
best by 2010 (Fig. 9.1). However there remain many areas where the population<br />
is vulnerable. These include child poverty (Bastos, 2012), un<strong>health</strong>y behaviours<br />
(e.g. motorcar accidents, substance abuse) <strong>and</strong> a relatively un<strong>health</strong>y ageing<br />
population (OECD, 2012a).<br />
Fig. 9.1 Trends in infant mortality: (a) in Portugal (1960–2012) <strong>and</strong> (b) in European<br />
countries (2012)<br />
(a)<br />
Mortality (per 1,000 live births)<br />
77.5<br />
55.5<br />
24.3<br />
10.9<br />
5.5 3.3 2.5 3.4<br />
1960 1970 1980 1990 2000 2008 2010 2012<br />
(b)<br />
EU27<br />
Irel<strong>and</strong><br />
Greece<br />
Spain<br />
Portugal<br />
Finl<strong>and</strong><br />
2.4<br />
Mortality (per 1,000 live births)<br />
3.8<br />
3.5<br />
2.9<br />
3.1<br />
3.4<br />
Sources: OECD, 2012b; PORDATA, 2013.<br />
In the decade prior to the <strong>crisis</strong>, important changes were made to the Portuguese<br />
<strong>health</strong> system. Following conceptual <strong>and</strong> organizational developments<br />
introduced in the late 1990s, a comprehensive primary <strong>health</strong> care reform was<br />
initiated in 2005 by providing support for the rapid expansion of family <strong>health</strong><br />
units, known as unidades de saúde familiares, which are small, multiprofessional<br />
public primary <strong>health</strong> care teams operating under performance contracting that<br />
choose their own leadership, thus setting up a primary <strong>health</strong> care network.<br />
Other changes included adopting national <strong>health</strong> strategies <strong>and</strong> plans (in 1998<br />
<strong>and</strong> 2004), taking steps towards decentralizing public hospital management<br />
<strong>and</strong> adopting public–private partnerships for new public hospitals, developing<br />
a long-term care network, investing in new mechanisms for <strong>health</strong> services