Premise Indirect - przewodnik kliniczny - Kerr Hawe
Premise Indirect - przewodnik kliniczny - Kerr Hawe
Premise Indirect - przewodnik kliniczny - Kerr Hawe
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Bio... what?<br />
<strong>Premise</strong> <strong>Indirect</strong> | Biomimetic nanotechnology<br />
<strong>Premise</strong> <strong>Indirect</strong>. The new biomimetic nanotechnology tempered composite<br />
programme which uniquely offers restorations that look, feel, mature and<br />
perform just like natural teeth... just as nature intended.<br />
For more information, log on to www.kerrhawe.com or call 00800 41 05 05 05<br />
©2008 <strong>Kerr</strong> Corporation<br />
Lab for life.
Press Release<br />
Biomimetic Story<br />
Product Presentation: The strength of <strong>Premise</strong> <strong>Indirect</strong> is the long history<br />
with belleGlass<br />
Historical and Provisional Studies<br />
Frequently Asked Questions
INDIRECTaddressesallthemodernrequirementsofprofessionalsseekingtheultimateinatempered compositeprogrammethatmostcloselyresemblesnaturaltoothstructurebothintermsofformand function. TheresultofsciencebornfromthesuccessofHerculiteXRV,belleGlassNGand<strong>Premise</strong>-newPREMISE<br />
<strong>Indirect</strong>withanalmostceramiclikeappearancethankstoprovenoptimisedtriomodalpolymerisation butwithalltheadditionaladvantagesof<strong>Kerr</strong>’suniqueheatandpressurecuringsystem;thepresenceof nitrogenreplacesairtouniquelyannihilatetheinhibitionlayerandproducewhatiseffectivelya98% Continuousimprovementsintermsofhandling,aestheticsandpolishabilityprovidesnew<strong>Premise</strong><br />
totallypolymerisedrestoration.Marginalintegrityandcolourstabilityaremaximisedwithbothwear<br />
terminlay,onlay,crown,bridgeandveneerrestorations.WhenincorporatedwithCONSTRUCTfibre matrix,unprecedentedopportunitiesmayalsoberealised. andflexuralratesmimickingnaturaltoothstructureunsurpassedbyanycompetitivesystemforlong<br />
‘forgiving’proprioceptiverestorativealternativeispreferredandtimeisoftheessence. Thefulllineof<strong>Kerr</strong>productsisavailablefromauthorizeddentaldistributors.Formoredetailed NewPREMISEINDIRECTisespeciallysuitedforimmediateloadimplantpatientswhereamore<br />
www.<strong>Kerr</strong>Dental.com,contactyourlocal<strong>Kerr</strong>representative,orcall<strong>Kerr</strong>InternationalFreephone informationonPREMISEINDIRECToranyother<strong>Kerr</strong>dentalproducts,pleasevisitourwebsiteat<br />
KERR (00800)41050505.<br />
ViaStrecce4 6934Bioggio Switzerland <strong>Kerr</strong><strong>Hawe</strong>SA<br />
InternationalFreephone:(00800)41050505<br />
www.<strong>Kerr</strong>Dental.com www.<strong>Kerr</strong><strong>Hawe</strong>.com
BIOMIMETICS<br />
Biomimeticsistheapplicationofbiologicalmethodsandsystemsfoundinnaturetothestudyand dentistandtechnicianwhoareconcernedwithproviding‘virtuallylife-longaestheticrestorations’.<br />
thatmostofuswouldreadilyappreciate. Twoeasilyrecognisedexamplesofthistransferfrombiologytotechnologyaretheintroductionof designofengineeringsystemsandmoderntechnology:‘life-like’wouldbeapopularinterpretation<br />
certainanimals(GeorgedeMestral,SwissEngineer,1948)andofcoursetheUK’sveryownPercy Shaw‘s‘cat’seye’reflectorfornighttimeroaddelineation:his1935inventionwasbasedonthefact thatthemakeupofacat’seyeincorporatesasystemofreflectingcells(tapetumlicidum)capable theVelcrofasteningfollowingresearchintothewayburrhooksfromsomeplantsclungtothefurof<br />
Nelumbolotusleafhasbeensimilarlymimickedbysomemanufacturersofself-cleaningpaints,roof tilesandevensheetglass,isanothercleveradaptationofman’sharbouringofnaturalphenomena ofreflectingthetiniestamountoflight.The‘Lotuseffect,’wherebytheselfcleaningnatureofthe<br />
Thebiomimeticprocessisofcourseatwowayaffairandtheflowofideasandsolutions,especially thosewithmedicalpositivesenhancingalongerandbetterqualityoflifeforushumans,bringsus forapplicationinatotallynovelway.<br />
hypeconcerningceramicrestorations,notablyCAD/CAMmilling,itisalltooeasytoforgetthegreat synergisticqualitiesthatalaboratorytemperedCOMPOSITEcrown,bridge,inlay,veneeroronlaycan provideforthepatient.<strong>Kerr</strong>’sbelleGlassNGsystem,constantlyratedNo1initsclassby’Reality’, neatlytodentistryingeneralandanextendedstorylinefrom<strong>Kerr</strong>inparticular.Withallthecurrent<br />
forindirectresinmaterial:itsuniqueformulaandspecialtri-modalcuringprocess(heat,pressure andlight)hashelpedsecureitsfavouredpositionwiththousandsofrestorationssuccessfullyplaced representswithoutdoubttheindustrystandardandhasstoodthetestoftimeasproductofchoice<br />
TheclinicalandtechnicalexcellenceofbelleGlassNGisbeyonddoubtwithcountlessin-vitroandinvivostudiessupportingitsheritagepositionstatus.Restorationsthathavealmostthesamewear<br />
overa13yearhistory.<br />
naturaldentitionisasadirectresultofbelleGlass‘uniqueandpatentedmaterialpropertiesand curingprocess.<strong>Kerr</strong>’sambitionistocontinuetoprovidepatientswithrestorationsthatwillgive countlessyearsofaestheticfunctionandanew,improvedbellleGlassunderthenamePREMISE rateashumanteethandcombinecoefficientofthermalexpansionresultswhichvirtuallymirror<br />
New<strong>Premise</strong><strong>Indirect</strong>sharesalltheyears’ofheritagestatusgainedfrombelleGlass,HerculiteXRV INDIRECTisthecompany’swayofcontinuingtofulfilthisintention.<br />
evenbetterceramiclikeaesthetics,minimumplaqueattractionandsuperbplacementhandlingfor effortlessfabrication.AswithbelleGlassCONSTRUCTpolyethylenefibremayalsobeaddedto <strong>Premise</strong><strong>Indirect</strong>restorationsespeciallyforbridgeworkorcrownswheretrulyexceptionalstrengthis and<strong>Premise</strong>chairsidecompositeswiththeaddedbonusoflongtermglossespeciallyintheanterior,<br />
required.Allinalllongtermcolourstabilitywithlowwaterabsorptioncombinetomakepossible<br />
MartinLindsay<strong>Kerr</strong>LabProductManagerEuropediscussesanewperspectiveofinteresttoboth
thiswiththehugegrowthinimplantworksundertakenandthenecessitytouseamoreforgiving proprioceptiverestorativesuperstructurematerialotherthanceramic,thenthereareevenmore reasonstobeexcitedaboutnew<strong>Premise</strong><strong>Indirect</strong>.Addtothesefactstheuseof<strong>Kerr</strong>’sawardwinning trulylife-likebiomimeticrestorationsthatwear,feel,lookandagejustlikenaturalteeth.Combine<br />
trulyharmonised,scientificallybalancedandlong-livedrestorativeapproach. NX3dualcureresincementthenwinningcombinationsarecertainlytheorderofthedaywitha<br />
toshowofftheirinnateartisticskillsbyprovidingbespokeandaestheticallypleasingyetalone Fabricating<strong>Premise</strong><strong>Indirect</strong>restorationsextra-orallygivesbothtechniciansanddentistsachance<br />
oftime.Withmuchdentistryalsoconcernedwith‘repairandmaintenance’itiscomfortingtoknow thatintheunlikelyeventofchippingorfracture,<strong>Premise</strong><strong>Indirect</strong>restorationscanbeswiftly repairedintra-orallywiththeminimumofstressfordentistorpatient. functionalandlonglivedpatientfriendlyrestorativesolutionssimplyandinarelativelyshortperiod<br />
contactyourlocal<strong>Kerr</strong>representativeorcall<strong>Kerr</strong>InternationalFreephone(00800)41050505. Tofindoutmoreregarding<strong>Kerr</strong>’snewPREMISEINDIRECTbiomimeticnanotechnologyrestorative
Lab for Life. <br />
<strong>Premise</strong> <strong>Indirect</strong> | Biomimetic nanotechnolgy
History<br />
• 1891, <strong>Kerr</strong> Brothers founded Detroit Dental Manufacturing<br />
Company Only Product, Gas Fired Porcelain Furnace<br />
• 1920’s, Impression Compounds & Waxes<br />
• 1950’s Investments, Denture Base Material<br />
• ‘60s & 80’s, Division of Sybron Corporation, market leader in<br />
alloys, endo, impression material, composite, bonding<br />
& amalgamators.<br />
• 1993 - Sybron Dental Specialties, acquisitions; Demetron,<br />
Metrex, E&D, belle de st. Claire, Precision Rotary<br />
Instruments<br />
• 2000 SDS spins off from Sybron International<br />
.06% Camphoroquinone + .01% Aromatic or .04%<br />
Aliphatic Tertiary Amine + 450 nm Light Source =<br />
Higher Conversion
Benzoyl Peroxide + Heat = FREE RADICALS<br />
Allows higher curing temperature<br />
= higher conversion - 98.5%
Chemistry<br />
Conversion of Heat and Pressure Cured Composite<br />
Bennet ME, Puckett AD, Parsall DE, Roberts SB, J Dent Res 1996:<br />
75-291. Abstr #2188<br />
5 min 10 min 15 min 20 min<br />
Hardness (V) 69.5 (6.8) 79.7 (4.4) 81.6 (4.4) 90.7 (2.4)<br />
Diametral<br />
Tensile 34.7 (7.3) 53.9 (10.9) 62.5 (11.2) 65.8 (4.9)<br />
Strength<br />
% Conversion 86.5 92.8 96.2 98.5<br />
Eliminate The<br />
oxygen-inhibited<br />
layer = conversion to<br />
the surface and<br />
any voids that may<br />
remain after<br />
pressure curing.
Features<br />
Result:<br />
Heat & Pressure Processed Polymer-Glass Restorative<br />
• Increased Productivity<br />
• Improved Aesthetics<br />
• Physical properties more closely matching that of human dentin<br />
Features<br />
History:<br />
• Based on 19 Years of HerculiteXRV Technology<br />
• Leader in Resin & Composite Technology (Herculite, Prodigy, Point 4)
Indications<br />
Anterior Veneers<br />
Opalescent particles<br />
within enamel layer<br />
exhibits a natural vitality<br />
Indications<br />
Opalescence<br />
Definition:<br />
Opalescence is the<br />
reflection of an iridescent<br />
light.
Indications<br />
Single Crowns<br />
• Metal Understructure or<br />
• Construct<br />
Polyethylene<br />
Reinforcement<br />
Indications<br />
Implant Restorations<br />
• Kind and forgiving to<br />
opposing dentin<br />
• Simulation of lost<br />
periodontal ligament
Indications<br />
Metal Free Bonded Bridges &<br />
Perio Splints<br />
• Connect / Construct Polyethylene Fiber Reinforcement<br />
Features<br />
<strong>Premise</strong> <strong>Indirect</strong> / Biomimetics<br />
“Clinicians now have a restorative material available that alleviates<br />
our concerns about abrasion to opposing dentition, and one that<br />
matches if not surpasses the aesthetic level of porcelain.”<br />
Gregg A. Helvey, DDS
Features<br />
Advantages of <strong>Indirect</strong><br />
Composites over Ceramics<br />
• Simple Fabrication<br />
• Margins when finished are impeccable<br />
• Restoration/Luting Cement: same type of material<br />
• Less than 1% Shrinkage<br />
• Can be repaired at Chairside<br />
• Kind to the opposing teeth<br />
Features<br />
Vs. Porcelain<br />
belleGlass Intra-oral Repair:<br />
· Freshen restoration<br />
· Silane surface<br />
· Apply modeling resin<br />
· Repair w/ <strong>Kerr</strong> resin<br />
· Trim & Polish<br />
· Dismiss patient<br />
· 1 Hour<br />
Porcelain Intra-oral Repair:<br />
· Remove restoration<br />
· Re-appoint patient<br />
· Mail restoration to<br />
lab<br />
· Wait 7 to 10 days<br />
· Anesthetize patient<br />
· Re-cement<br />
restoration<br />
· 10 Days
Developments<br />
Coefficient of Thermal Expansion of<br />
Restorative Materials<br />
MATERIAL<br />
CTE (ppm/°C)<br />
AMALGAM 25<br />
PORCELAIN 7.8<br />
GOLD 14.4<br />
BG OPACEOUS DENTIN 13.1<br />
Natural Enamel 12<br />
Natural Dentin 11.4<br />
COMPOSITE RESIN 30<br />
GLASS IONOMER CEMENT 5.7*<br />
Skinner, E.W. and Phillips, R.W. The Science of Dental Materials; W.B.<br />
Saunders, Co. Phil. 1967.<br />
* Puckett, A.D. et al, Quint. Int. 26 (8), p577-581, 1996.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Biomimetics<br />
Biomimetic refers to human-made processes,<br />
substances, devices or systems that imitate nature.<br />
Burs on a dog’s coat<br />
led to the invention of<br />
Velcro.
<strong>Premise</strong> <strong>Indirect</strong> / Biomimetics<br />
The art and science of designing and building<br />
biomimetic apparatus is called biomimetics.<br />
Replicating the water<br />
repellant nature of<br />
certain leaves in the<br />
manufacturing of paint.<br />
Picture Courtesy of David Zielinski RDT, USA
<strong>Premise</strong> <strong>Indirect</strong> / Nanotechnology<br />
Nanotechnology involves the creation and<br />
manipulation of complex structures on the scale of<br />
nanometers – something organisms have done for<br />
about 3.8 billion years.<br />
The ideal nanohybrid<br />
restorative that ages,<br />
feels, wears, functions<br />
and looks like a natural<br />
tooth.<br />
Picture Courtesy of Ronnie van Eeden RDT, South Africa
Picture Courtesy of Gabriel Palazzi RDT, Switzerland<br />
<strong>Premise</strong> <strong>Indirect</strong> / Features<br />
The result of science born from the<br />
success of Heruculite XRV,<br />
belleGlassNG and <strong>Premise</strong>.<br />
<strong>Premise</strong> <strong>Indirect</strong> utilizes the same<br />
optimized trimodal polymerization as<br />
belleGlass NG, the most respected<br />
indirect restorative of its kind.<br />
Indications: Inlays, onlays, crowns,<br />
veneers, bridges, splints and ideal for<br />
implant restorations with proprioceptive<br />
tooth-like response.
<strong>Premise</strong> <strong>Indirect</strong> / Features<br />
Natural look and wear. Closely matches<br />
natural dentition in wear characteristics,<br />
as well as an opalescent appearance that<br />
virtually replicates natural enamel like no<br />
other restorative material.<br />
Performance. Trimodal curing (light, heat<br />
and pressure) achieves over 98% material<br />
conversion, as compared to 60 – 70%<br />
achieved with light-cure only materials.<br />
Proven History. Twelve years of positive<br />
clinical history, and tens of thousands of<br />
successful restorations placed since 1996.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Research<br />
Nanohybrid technology. The combination of large prepolymerized filler<br />
(PPF) particles, 0.4 micron structural filler and small silica nanoparticles<br />
allows higher filler loading, improved physical properties, optimal handling,<br />
higher surface gloss and reduced polymerization shrinkage.<br />
Prepolymerized filler<br />
Point 4 filler<br />
Silica nanoparticles
<strong>Premise</strong> <strong>Indirect</strong> / Research<br />
High gloss retention. The particle size of fillers in PPF particles is below<br />
the wavelength of visible light and light-scattering effects are minimal.<br />
Plucking of PPF particles is reduced because mechanical properties are<br />
more similar to the cured paste number rather than ceramic particles.<br />
Cured traditional composites wear<br />
unevenly causing a loss of luster and<br />
gloss.<br />
<strong>Premise</strong> <strong>Indirect</strong> PPF particles wear<br />
more uniformly, wear resistance is<br />
improved and surface remains<br />
smoother and glossier with time.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Research<br />
In-vivo measurements of wear over a<br />
In-vivo measurements of wear over a<br />
five year period shows an average of<br />
1.2 microns a year – closer to the wear<br />
of natural teeth than any other material<br />
tested.
<strong>Premise</strong> <strong>Indirect</strong> / Research<br />
<strong>Premise</strong> <strong>Indirect</strong> more closely<br />
matches the coefficient of<br />
thermal expansion (CTE) of<br />
natural dentin – resulting in a<br />
material that looks and acts<br />
virtually the same as natural<br />
tooth structure.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Systems<br />
Intro System<br />
Starter system offering everything<br />
needed for Inlays and Onlays.<br />
Master System<br />
Complete system offering<br />
everything needed for Inlays to<br />
full bridges.
<strong>Premise</strong> <strong>Indirect</strong> / Materials<br />
Primary Dentins are used for foundation<br />
and coping layers and improve strength.<br />
Facial Dentins cover all foundation and<br />
coping layers to produce a stable long<br />
lived polished surface.<br />
Incisals are placed onto the incisal /<br />
cuspal area and are designed to match the<br />
vitality of tooth enamel.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Materials<br />
Modeling Resin is an unfilled<br />
universal wetting agent used for<br />
sculpturing.<br />
Rubber Sep is a removable<br />
latex release agent and spacer<br />
applied to all dies and contact<br />
areas creating a 20 micron<br />
space.<br />
Opaques are applied after metal<br />
prep and block out any<br />
underlying metal color.<br />
Silane Primer is applied to the<br />
fitting surface of any metal free<br />
restoration prior to bonding.<br />
Cervicals simulate root and<br />
cervical color,<br />
Kolor Plus is applied<br />
internally to add effect on<br />
occlusal and interproximal<br />
surfaces.
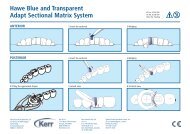
<strong>Premise</strong> <strong>Indirect</strong> / Inlays & Onlays<br />
When layering note that maximum Facial Dentin<br />
thickness should not exceed 1.5 mm.<br />
Primary Facial Incisal<br />
<strong>Premise</strong> <strong>Indirect</strong> / Inlays & Onlays<br />
If desired, duplicate the working die and<br />
articulate. Isolate adjacent tooth contact<br />
points and opposing dentition with Rubber<br />
Sep.<br />
Prepare the model and working die. Block<br />
out all undercuts.<br />
Apply a thin layer of Primary Dentin into<br />
the floor and axial walls and adapt to the<br />
desired contour. Finish slightly short of the<br />
marginal periphery. Apply Kolor Plus to<br />
modify the occlusal color if needed. Light<br />
cure all aspects for 20 seconds.
<strong>Premise</strong> <strong>Indirect</strong> / Inlays & Onlays<br />
Adapt Facial Dentin in small increments to<br />
desired contour. Continuously verify<br />
occlusal clearance. Work one cusp at a<br />
time. Apply Kolor Plus modifier to simulate<br />
occlusal staining. Light cure each<br />
increment for 10 seconds.<br />
Finalize the occlusal scheme with Cuspal /<br />
Incisal to desired contour. Remove the die<br />
from the working model. Add contact areas<br />
if needed. Light cure all aspects for 20<br />
seconds. Polymerize for 20 minutes in the<br />
curing unit. Remove the restoration from<br />
the die as soon as possible after full<br />
polymerization.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Inlays & Onlays<br />
The completed restoration after polishing.
<strong>Premise</strong> <strong>Indirect</strong> / Crowns & Veneers<br />
When layering note that maximum Facial Dentin<br />
thickness should not exceed 1.5 mm.<br />
Primary Facial Incisal<br />
<strong>Premise</strong> <strong>Indirect</strong> / Crowns & Veneers<br />
If desired, duplicate the working die and<br />
articulate. Isolate adjacent tooth contact<br />
points with Rubber Sep.<br />
Prepare the model and working die.<br />
Apply Primary Dentin and contour to the<br />
desired shape. Finish slightly short of the<br />
marginal periphery. Light cure each aspect<br />
for 20 seconds.
<strong>Premise</strong> <strong>Indirect</strong> / Crowns & Veneers<br />
Adapt Facial Dentin onto the margin for<br />
precision fit.<br />
Adapt Facial Dentin to the desired contour.<br />
Repeat on all aspects. Light cure at<br />
frequent intervals. Once final contour has<br />
been achieved, light cure all aspects for 20<br />
seconds.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Crowns & Veneers<br />
Adapt Incisal material in small increments.<br />
Light cure each increment for 10 seconds.<br />
Finalize contour at the incisal edge. Create<br />
a restoration that is slightly longer than the<br />
tooth being replicated. (This allows for<br />
correct morphology after polishing<br />
procedures). Remove the die from the<br />
working model. Add contact areas. Light<br />
cure all aspects for 20 seconds.
<strong>Premise</strong> <strong>Indirect</strong> / Crowns & Veneers<br />
Polymerize for 20 minutes in the curing unit.<br />
Remove the restoration from the die as<br />
soon as possible after full polymerization.<br />
The completed restoration after polishing.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
<strong>Premise</strong> <strong>Indirect</strong> can be incorporated onto<br />
any recommended dental alloy. Use of<br />
mechanical retention is recommended.<br />
Metal frameworks should incorporate<br />
smooth rounded edges especially for incisal<br />
and occlusal areas. Produce a framework<br />
thickness of 0.3 – 0.5 mm. For bridges,<br />
design the framework for correct placement<br />
of pontics and connectors. Ensure adequate<br />
space for veneering material.<br />
Primary Facial Incisal Metal Opaque
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
Wax to full contour.<br />
Remove waxed crown.<br />
Assess available space.<br />
Trim framework to desired shape.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
Ideal margin space.<br />
Rounded and smoothed.<br />
Trim and polish backings<br />
before applying material.<br />
Rounded and smoothed.
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
To achieve maximum bond strength, it is<br />
essential to ensure cleanliness of the metal.<br />
Sandblast all veneering areas with 50 micron<br />
Aluminum Oxide at no more than 2 bar (30<br />
PSI) pressure.<br />
After cleaning, apply Metal Prep with an<br />
applicator brush or directly from the bottle.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
All veneering areas are covered with Metal<br />
Prep. Allow to fully dry approximately 1<br />
minute. Blast excess metal prep off with<br />
compressed air at 1 bar (15 PSI) pressure.<br />
Apply Opaque to a final thickness of 0.1 –<br />
0.2 mm. Ensure that there are no visible grey<br />
areas. This may require 2 – 3 applications.<br />
Light cure each opaque layer for 40 seconds<br />
per surface. Create a first wash Opaque. If<br />
desired, mix a small amount of Modeling<br />
Resin with Opaque.
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
If desired, modify Opaque shades with Kolor<br />
Plus.<br />
Orange modifier is ideal for cervical areas or<br />
for producing a warmer color.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Metal Restorations<br />
Wash application of Opaque with cervical<br />
area completed. Light cure each layer for 40<br />
seconds.<br />
Complete masking of the underlying metal<br />
framework. Note a slight surface shine.
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Construct reinforcing braid is the ideal<br />
“building block”. It has a patented weave<br />
designed for more complete resin wetting.<br />
• Delivers superior strength and toughness<br />
• Made from polyethylene fiber<br />
• Cold gas plasma treated<br />
• Three widths available<br />
• Three times stronger than steel<br />
• Impregnated with Silane and Resin<br />
• Available in three shades, one neutral<br />
and two opaque shades designed to<br />
eliminate “shine through”.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Indications<br />
• Single-unit posterior crowns<br />
• Posterior bridges<br />
• Anterior bridges<br />
• Selected anterior single crowns<br />
• Selected Inlays and Onlays<br />
Guidelines<br />
• Assess all prescribed cases to ensure a successful outcome.<br />
• Always use the largest width of Construct fiber available.<br />
• Ensure complete wetting of the fiber with Construct Resin.<br />
• Keep the design of frameworks as simple as possible.
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Prepare the model and working die.<br />
Asses size and area of the preparation.<br />
Forma a flat disc of Primary Dentin 0.5 – 0.6<br />
mm thick.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Apply the disc to the occlusal surface and adapt<br />
excess material over the axial walls to form a<br />
coping. Finish short of the margin periphery.<br />
Light cure each aspect for 20 seconds. The<br />
ideal coping thickness is 0.2 mm.<br />
Construct needs to be wrapped around the<br />
periphery of the preparation. Apply to the<br />
occlusal surface if space permits. Follow the<br />
preparations contour for optimal placement.<br />
Using Construct scissors, cut a length of<br />
fiber. Wet one end of the fiber with Construct<br />
Resin. Apply to the proximal axial walls into<br />
its desired position. After full adaptation and<br />
saturation, light cure for 3 – 5 seconds.
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Apply Construct Resin in small increments 1<br />
– 2 mm at a time. Wrap around the<br />
periphery. After each adaptation and<br />
saturation of the fiber, light cure for 3 – 5<br />
seconds.<br />
Wrap around the entire periphery. Light cure<br />
little and often.<br />
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
After full adaptation overlay by 0.1 – 0.2 mm<br />
and cut the fiber. Light cure 3 – 5 seconds.<br />
Measure a length of Construct for the<br />
occlusal surface.
<strong>Premise</strong> <strong>Indirect</strong> / Construct<br />
Apply Construct as before and light cure 3 –<br />
5 seconds. Once completed light cure all<br />
aspects for 20 seconds.<br />
Continue layering of the crown to final<br />
completed restoration.<br />
<strong>Premise</strong> <strong>Indirect</strong><br />
Continued improvements over the years<br />
with our indirect restorative line has resulted<br />
in superior handling characteristics as well<br />
as exceptional polishability.<br />
Please refer to the complete Directions for<br />
Use for more information.<br />
Visit www.kerrlab.com for more information.
Historical and Provisional<br />
Studies
Primary research information courtesy of<br />
Prof. D Watts,<br />
Dr. Nick Silikas (BSc, MPhil, PhD, FADM),<br />
The University of Manchester<br />
Higher Cambridge Street<br />
Manchester M15 6FH
Dental Materials 19 (2003) 393–398<br />
www.elsevier.com/locate/dental<br />
In vitro characterization of two laboratory-processed resin composites<br />
A. Kakaboura a, *, C. Rahiotis a , S. Zinelis b , Y.A. Al-Dhamadi c , N. Silikas c , D.C. Watts c<br />
a Department of Operative Dentistry, University of Athens, Thivon 2, 115 27, Goudi, Athens, Greece<br />
b Biomaterials Laboratory, University of Athens, Greece<br />
c Dental School, University of Manchester, Manchester, UK<br />
Received 15 January 2002; revised 20 May 2002; accepted 11 June 2002<br />
Abstract<br />
Purpose. To compare various characteristics of two new-generation laboratory-processed resin composites (BelleGlass HP/SDS-<strong>Kerr</strong> and<br />
Sinfony/3M-ESPE). The properties evaluated were degree of CyC conversion, microhardness, roughness, biaxial flexural strength and<br />
polymerization shrinkage-strain.<br />
Materials and methods. All specimens were subjected to a first and a second polymerization cycle according to the manufacturers’<br />
instructions. The degree of CyC conversion (DC) was recorded on rectangular (3 £ 2 £ 0.5 mm 3 ) specimens (n ¼ 3) by FT-IR<br />
micromultiple internal reflectance spectroscopy immediately after each of the two polymerization cycles. Twenty cylindrical specimens<br />
(10 £ 2mm 2 ) of each material were prepared for surface microhardness (n ¼ 10, VHN, 200 g load, 20 s) and surface roughness (n ¼ 10, Ra)<br />
measurements. The biaxial flexural strength and stiffness were determined on disk-shaped (n ¼ 8, 15 £ 0.7 mm 2 ) specimens loaded to<br />
fracture at 1 mm/min crosshead speed. The polymerization shrinkage-strain was calculated with the bonded-disk method. All values were<br />
statistically analyzed by Student’s unpaired t-test ( p , 0.05).<br />
Results. The second polymerization cycle significantly increased the degree of CyC conversion for both materials ( p , 0.05). BelleGlass<br />
HP exhibited significantly higher degree of CyC conversion, surface microhardness, surface roughness, biaxial flexural strength and stiffness<br />
values compared to Sinfony ( p , 0.05).<br />
Significance. Several differences exist between the materials although both products are recommended for the same clinical applications.<br />
q 2003 Academy of Dental Materials. Published by Elsevier Science Ltd. All rights reserved.<br />
Keywords: Belleglass HP; Sinfony; Degree of cure; Microhardness; Roughness; Biaxial flexural strength; Shrinkage-strain; Load-to-failure rates<br />
1. Introduction<br />
Although porcelain is a well-accepted esthetic material<br />
for prosthodontic applications, the metal–ceramic and allceramic<br />
restorations show some undesirable characteristics.<br />
The opaque nature of metal substructure does not simulate<br />
natural translucency; fabrication is time-consuming and<br />
technically demanding and the abrasiveness of porcelain is<br />
destructive to the opposing natural tooth structure [1].<br />
Moreover, in all ceramic restorations, the absence of a metal<br />
framework gives the potential for low fracture resistance,<br />
limiting the clinical application in high stress areas.<br />
In an effort to overcome some of these disadvantages, the<br />
manufacturers, even in the early 1980s, introduced numerous<br />
products of laboratory-processed resin composites [2].<br />
These materials provided alternative ways for clinicians to<br />
* Corresponding author. Tel.: þ30-317788575; fax: þ30-31-8033129.<br />
E-mail address: afrodite1@otenet.gr (A. Kakaboura).<br />
overcome some inherent deficiencies of direct composites<br />
restorations, including polymerization shrinkage,<br />
inadequate polymerization in deep interproximal areas and<br />
restoration of proximal contacts and contour [3].<br />
However, these resin composites were microfill materials<br />
which demonstrated poor clinical performance due to low<br />
flexural strength and wear characteristics attributed to the<br />
low inorganic filler content [4]. In the early 1990s a second<br />
generation of laboratory-processed resin composites was<br />
developed, advocated for a wide range of fixed prosthodontic<br />
applications such as inlays, onlays, veneering, metal-free<br />
single unit crowns and short span anterior bridges [4]. A<br />
variety of materials with remarkable differences in composition,<br />
polymerization modes and curing conditions comprise<br />
the second generation of the laboratory-processed<br />
resin composites. Ultra-small filler particles and polyfunctional<br />
methacrylate monomers are used in these composites.<br />
They are processed by different laboratory techniques based<br />
on combinations of heat, pressure, vacuum and light<br />
0109-5641/03/$ - see front matter q 2003 Academy of Dental Materials. Published by Elsevier Science Ltd. All rights reserved.<br />
doi:10.1016/S0109-5641(02)00082-9
394<br />
A. Kakaboura et al. / Dental Materials 19 (2003) 393–398<br />
Table 1<br />
Composition and polymerization modes of the materials tested<br />
Materials Batch number # Composition Polymerization mode<br />
First cycle: photopolymerization (Light<br />
Teklite) 650 mW/cm 2 ,40s;<br />
Second cycle: heat 140 8C, pressure 60 psi, N 2<br />
(BelleGlass HP curing unit), 20 min<br />
BelleGlass HP shade: enamel natural 808B93 Aliphatic urethane dimethacrylate, aliphatic<br />
dimethacrylate oligomers, fillers: 74 wt% barium<br />
silicate glasses and SiO 2 , mean size: 0.6 mm<br />
First cycle: photopolymerization (Visio<br />
Alpha), 400 mW/cm 2 ,15s;<br />
Second cycle: photopolymerization<br />
(Visio Beta) up to 40 8C, vacuum, 15 min<br />
Sinfony shade: enamel natural FW0059863 Aliphatic and cycloaliphatic monomers,<br />
fillers: 50 wt% aluminum glass and SiO2<br />
mean size: 0.6 mm<br />
polymerization. Although, second generation products<br />
became available in 1995, their characteristics and clinical<br />
performance have not been adequately investigated [2,<br />
5–10]. Additional products, such as Sinfony (3M-ESPE<br />
Dental AG, Germany), were introduced claiming improved<br />
performance and esthetics. The purpose of this study was to<br />
evaluate the in vitro performance of two second-generation<br />
laboratory-processed resin composites. Properties to be<br />
examined include: the degree of CyC conversion, surface<br />
microhardness, surface roughness, biaxial flexural strength<br />
and polymerization shrinkage-strain which are acknowledged<br />
to be related to the clinical performance of composite<br />
restorations.<br />
The null hypothesis to be tested, was that no significant<br />
differences would be found in the properties examined,<br />
between the two materials.<br />
2. Materials and methods<br />
The resin composites examined were BelleGlass HP<br />
(SDS-<strong>Kerr</strong>, Orange, CA, USA) and Sinfony (3M-ESPE<br />
Seefeld, Germany). The composition of each material and<br />
their required polymerization mode are shown in Table 1.<br />
The degree of CyC conversion (DC) was evaluated after the<br />
first and second polymerization cycles with a reflectance<br />
FT-IR spectroscopy (Perkin–Elmer, Norwalk, CT, USA).<br />
Three rectangular specimens (3 £ 2 £ 0.5 mm 3 ) were prepared<br />
per material. Spectra of the original pastes and of the<br />
directly irradiated surfaces were acquired after the first and<br />
second polymerization cycle under the following conditions:<br />
4000–400 cm 21 range, 4 cm 21 resolution, 458 para<br />
edge KRS-5 minicrystal of seven internal reflections, 40<br />
scans coaddition at 35 ^ 1 8C. The quantitative measurements<br />
of DC were performed based on the two-frequency<br />
method [11,12].<br />
For surface microhardness measurements, the resin<br />
composite pastes were packed into disk-shaped Teflon<br />
molds (10 mm diameter, 2 mm height), pressed against<br />
transparent polyester matrix strips and subjected to the two<br />
polymerization cycles. Ten specimens per material were<br />
prepared. After the second polymerization cycle the specimens<br />
were stored in water under dark conditions at 37 8C for<br />
24 h, the flat surfaces were ground slightly with 1000 grit<br />
size wet silicon carbide (SiC) papers and the microhardness<br />
values were obtained after application of 200 g load for 20 s<br />
using a Microhardness instrument (HMV 2000, Shimadzu<br />
Corp., Tokyo, Japan) equipped with a Vickers diamond<br />
indenter.<br />
For surface roughness measurements, 10 disk-shaped<br />
specimens per material were prepared, as described above.<br />
Mean roughness values (Ra) were measured using an<br />
electronic profilometer (Diavite DH-5, Asmeto AG, Richterswill,<br />
Germany) operated with a 5 mm diamond stylus,<br />
908 reading angle and 0.80 mm cut-off length. Six<br />
recordings per specimen surface were recorded.
A. Kakaboura et al. / Dental Materials 19 (2003) 393–398 395<br />
Fig. 1. Schematic representation of the biaxial flexural method of fracture.<br />
Eight disk-shaped specimens (15 mm diameter,<br />
0.7 mm height) per material were prepared for the<br />
biaxial flexural strength test, which were subjected to the<br />
two individual polymerization cycles. The specimens<br />
were ground, as described earlier and were immersed in<br />
water at 37 ^ 1 8C for 24 h. Then, each specimen was<br />
transferred on a biaxial flexure device consisting of three<br />
stainless steel balls (3.2 mm in diameter) equally spaced<br />
along the periphery of 10 mm diameter supporting circle<br />
(Fig. 1). The specimens of each group were loaded at<br />
the center with a stainless steel ball of 3.2 mm diameter<br />
until fracture, in a universal testing machine (Model<br />
6022, Instron Corp, Canton MA, USA) operating in<br />
compression at 1 mm/min crosshead speed. The biaxial<br />
flexural strength was calculated according to the<br />
equation [13]<br />
BS ¼ AP=h 2 and<br />
A ¼ð3=4pÞ½2ð1 þ nÞlnða=r p 0Þþð1 þ nÞð2a 2 2 r p2<br />
0 Þ=2b 2<br />
þð1 þ nÞŠ<br />
r p 0 ¼ð1:6r 2 0 þ h 2 Þ 1=2 2 0:675h<br />
where BS is the biaxial flexural strength, P the load at<br />
failure, n the Poisson’s ratio (0.24) [14], a the radius of<br />
supporting circle, b the radius of the specimen disk, h<br />
the thickness of the sample and r 0 the ball radius.<br />
The load-to-failure rate was determined directly from the<br />
load versus time graphs plotted as the ratio of the fractured<br />
load to the failure time.<br />
The polymerization shrinkage-strain during the primary<br />
cure cycle was measured with the bonded-disk<br />
method [15,16].<br />
Statistical analysis was performed by unpaired Student’s<br />
t-test to define any significant differences in the properties<br />
tested between the two resin composites for each testing<br />
condition. A 95% confidence level was chosen ( p ¼ 0.05).<br />
3. Results<br />
The mean values of all the properties are shown in<br />
Table 2. The second polymerization cycle significantly<br />
improved the percentage degree of CyC conversion (DC) in<br />
both materials ( p , 0.05). BelleGlass HP showed significantly<br />
higher final DC values, higher surface microhardness<br />
and higher roughness (Ra) values, compared to Sinfony<br />
( p , 0.05). BelleGlass HP exhibited lower final shrinkagestrain<br />
values compared to Sinfony during the primary cure<br />
cycle, and also had remarkably lower shrinkage-strain<br />
values in the early stages of the polymerization, 10–40 s<br />
(Tables 3 and 4). No statistically significant differences<br />
were detected between the two materials regarding the<br />
biaxial flexural strength. Nevertheless, BelleGlass HP
396<br />
A. Kakaboura et al. / Dental Materials 19 (2003) 393–398<br />
Table 2<br />
Results (mean ^ SD) of all characteristics evaluated. The properties were measured after the second cure cycle<br />
Material<br />
Degree of CyC<br />
conversion, first cycle<br />
Degree of CyC<br />
conversion, second cycle<br />
Micro-hardness<br />
(VHN)<br />
Roughness<br />
(Ra, mm)<br />
Biaxial flexural strength<br />
(MPa)<br />
Load-to-failure rate<br />
(MPa/s)<br />
BelleGlass HP 60 (7.2) 80 (10.4) 174 (22.1) 0.31 (0.05) 49.4 (9.4) 5.5 (0.4)<br />
Sinfony 50 (5.1) 66 (6.8) 77.8 (16.5) 0.16 (0.03) 53.4 (8.1) 2.6 (0.3)<br />
exhibited a significantly higher load-to-failure rate compared<br />
to Sinfony ( p , 0.05), an indication of higher<br />
material stiffness.<br />
4. Discussion<br />
The null hypothesis was rejected. The two materials<br />
exhibited significant differences in most of the properties<br />
studied. The degree of CyC conversion for direct resin<br />
composites has been reported to vary from 50 to 75% [17,<br />
18]. The results of the present study indicate that after the<br />
second polymerization, Sinfony reached a value within this<br />
range, whereas BelleGlass HP demonstrated an even higher<br />
degree of CyC conversion (80%), which is in accordance<br />
with the results reported by Knobloch et al. [2]. Differences<br />
in monomer composition and polymerization conditions<br />
may explain the higher degree of CyC conversion provided<br />
by BelleGlass HP. BelleGlass HP contains aliphatic<br />
urethane monomers, which are known to provide an<br />
increased degree of CyC conversion [18]. However, the<br />
main differences are expected to arise from the temperatures<br />
used in the second cure cycle. The polymerization of<br />
BelleGlass HP during the second cycle was performed at a<br />
higher temperature (140 8C) than for Sinfony (40 8C).<br />
In general, the additional cure-cycle and photothermal<br />
annealing enhance the DC of the resin composites. Thus, the<br />
physicomechanical properties of the materials can be<br />
improved [19,20] and an increase in polymerization rate<br />
can be achieved which yields and promotes an annealing<br />
effect in the polymer. The high pressure (60 psi) applied<br />
during BelleGlass HP polymerization may also increase the<br />
extent of polymerization.<br />
The positive influence of the additional cure on DC found<br />
in this study has been noted in previous studies [21–23].<br />
The second polymerization cycle will increase the molecular<br />
mobility of the residual monomer and the chain segments<br />
after initial photopolymerization. However, an inherent<br />
drawback of the increased CyC conversion may be the<br />
reduction of remaining CyC bonds available for copolymerization<br />
with the resin luting cements. Jordan [24]<br />
reported that the lack of air-inhibited layer and the limited<br />
unsaturation of the laboratory-processed resins negatively<br />
affect the composite-luting cement interfacial strength.<br />
The proportional increase in DC after the second<br />
polymerization cycle was found to be essentially equivalent<br />
for both materials.<br />
The volume fraction and type of inorganic fillers as well as<br />
the DC of the organic matrix are important contributory<br />
factors to the microhardness of composite materials [19,25,<br />
26]. The higher inorganic volume fraction of BelleGlass HP,<br />
the harder type of glasses contained [27] and the higher density<br />
of the organic matrix, as a result of the enhanced conversion,<br />
can explain the higher microhardness values obtained. Surface<br />
microhardness is considered as an indicative factor of the<br />
mechanical strength of a resin [28]. A positive correlation<br />
between the hardness of a resin material and the wear<br />
resistance has been reported [7,28,29] although such a<br />
correlation has not been confirmed in other studies [30,31].<br />
Resin composite restorations with smooth outer surfaces<br />
lead to reduced plaque retention, surface staining and<br />
secondary caries incidence [32,33]. The higher roughness<br />
value obtained for BelleGlass HP may be partly explained<br />
by the higher filler volume loading and the harder type of<br />
fillers incorporated into the material. Moreover, curing of<br />
BelleGlass HP under nitrogen pressure may provide<br />
nitrogen entrapment, which may increase the porosity at<br />
the surface region. On the other hand, polymerization of<br />
Sinfony under vacuum eliminates such surface porosity.<br />
Nevertheless, both materials investigated showed initial<br />
roughness lower than the roughness values of<br />
0.64 ^ 0.25 mm reported for enamel. Enamel roughness<br />
of 0.64 mm at enamel-to-enamel occlusal contact areas is<br />
considered as a standard for roughness measurements of<br />
resin composites [34]. Plaque accumulation preferentially<br />
occurs on composite surfaces with a roughness range of<br />
Table 3<br />
Mean shrinkage-strain values for Sinfony, at three different temperatures during the first cure cycle, SD in parentheses (n ¼ 5)<br />
Temperature (8C)<br />
Sinfony<br />
10 s 20 s 40 s 30 min 60 min<br />
23 2.60 (0.15) 3.30 (0.04) 3.50 (0.03) 4.30 (0.05) 4.34 (0.06)<br />
37 2.90 (0.10) 3.55 (0.16) 3.80 (0.16) 4.40 (0.19) 4.44 (0.20)<br />
60 3.34 (0.30) 3.94 (0.35) 4.10 (0.39) 4.66 (0.47) 4.73 (0.46)
A. Kakaboura et al. / Dental Materials 19 (2003) 393–398 397<br />
Table 4<br />
Mean shrinkage-strain values for BelleGlass HP, at three different temperatures during the first cure cycle, SD in parentheses (n ¼ 5)<br />
Temperature (8C)<br />
BelleGlass HP<br />
10 s 20 s 40 s 30 min 60 min<br />
23 0.28 (0.11) 0.96 (0.10) 1.85 (0.10) 2.67 (0.12) 2.90 (0.10)<br />
37 0.24 (0.03) 1.27 (0.08) 2.30 (0.08) 3.18 (0.10) 3.28 (0.10)<br />
60 0.34 (0.10) 1.96 (0.34) 2.93 (0.32) 3.56 (0.35) 3.70 (0.40)<br />
0.7–1.4 mm [32]. The lower roughness of Sinfony compared<br />
to BelleGlass HP may be a contributory factor to the<br />
higher reported color stability of Sinfony [6]. The roughness<br />
of BelleGlass HP recorded by Soeno et al. [35] cannot be<br />
compared with the results of the present study since a<br />
different polishing procedure of the specimens was used.<br />
Mechanical strength is an important factor in the<br />
clinical success of a restoration. Resin composites are<br />
much weaker in tension than in compression. Therefore,<br />
tensile strength is generally considered as a more<br />
meaningful property for assessment of the clinical failure<br />
potential of resin materials [36]. The traditional tensile<br />
test has rarely been used for resins because of the<br />
difficulty associated with gripping and aligning of the<br />
specimens. Recently, the biaxial flexural test has been<br />
used to determine the tensile strength of composite<br />
materials [36]. In the present study, although BelleGlass<br />
HP exhibited a higher DC and a higher filler volume<br />
than Sinfony, similar biaxial flexural strength values were<br />
recorded from both materials. It is well recognized that<br />
several structural parameters, such as inclusions of voids,<br />
cracks, flaws and stress gradients influence the fracture<br />
strength of brittle materials [36]. A value of n ¼ 0.24<br />
was taken as a selected value of Poisson’s ratio which is<br />
consistent with previous measurements [14]. Other<br />
restorative materials, such as glass-ionomer cements,<br />
exhibited higher values of 0.30 [37]. If such a larger<br />
value had been selected it would have enhanced the<br />
values by 4.7%. Hence, even if the values for the<br />
materials varied widely 0.24–0.30, this would not have<br />
produced a very significant effect on the resultant<br />
strength values. It is not known whether nitrogen<br />
entrapment into BelleGlass HP during the second<br />
polymerization cycle may induce flaws, which in<br />
sequence may affect the material strength. So, despite<br />
the fact BelleGlass HP presented a higher DC than<br />
Sinfony, this cannot predict their relative strengths.<br />
The load-to-failure rates measured show that Sinfony<br />
is a more flexible material than BelleGlass HP. The<br />
lower DC in Sinfony may generate a less stiff organic<br />
network, which along with the lower filler volume<br />
content may explain the more flexible nature of Sinfony.<br />
The latter may permit higher energy absorption capacity<br />
under loading, which may appear as plastic deformation.<br />
This effectively blunts the crack tip, which then requires<br />
more energy to propagate.<br />
The polymerization shrinkage-strain during the primary<br />
cure cycle showed that Sinfony had consistently higher<br />
shrinkage values compared to Belleglass HP, despite its<br />
lower DC. This could be attributed to the higher filler<br />
percentage of Belleglass HP (74%), compared to that of<br />
Sinfony (50%). The slower shrinkage response of Belleglass<br />
HP is consistent with a lower concentration of the<br />
photosensitizer. The rate of propagation R p is proportional<br />
to the photosensitizer concentration C s [38]. This probably<br />
accounts for the slower start in the polymerization of<br />
Belleglass HP.<br />
In conclusion, significant differences were determined<br />
between the two second-generation laboratory-processed<br />
resin composites evaluated in terms of DC, surface<br />
microhardness, surface roughness, biaxial flexural strength<br />
and stiffness, which may affect the clinical behavior of each<br />
material. Nevertheless, controlled long-term clinical studies<br />
are needed to confirm the clinical significance of these<br />
differences. It is not known whether the greater compliance<br />
of Sinfony may provide a better stress distribution pattern<br />
and more efficiently preserve adjacent tissue integrity in<br />
intracoronal restorations. However, the mechanical properties<br />
of these materials may be modified when veneering<br />
metal frameworks, as the bonding capacity of the composite-metal<br />
interface may strongly influence the mechanical<br />
performance of the complex. Consequently, although the in<br />
vitro characterization of material properties cannot yet<br />
establish sound criteria for the prediction of their clinical<br />
efficacy, it provides a basis for understanding the laboratory<br />
and clinical performance of these materials and for the<br />
development of new materials.<br />
References<br />
[1] McLean JW. The science and art of dental ceramics. Oper Dent 1991;<br />
16:149–56.<br />
[2] Knobloch LA, Kerby RE, Seghi R, Van Putten M. Two body wear<br />
resistance and degree of conversion of laboratory processed<br />
composite materials. Int J Prosthodont 1999;12:432–8.<br />
[3] Roulet JF. Benefits and disadvantages of tooth coloured alternatives to<br />
amalgam. J Dent 1997;25:459–73.<br />
[4] Touati B, Aidan N. Second generation laboratory composite resins for<br />
indirect restorations. J Esthet Dent 1997;9:108–18.<br />
[5] Freiberg RS, Ferracane JL. Evaluation of cure, properties and wear<br />
resistance of Artglass dental composites. Am J Dent 1998;11:214–8.<br />
[6] Stober T, Gilbe H, Lenz P. Color stability of highly filled composite<br />
resin materials for facings. Dent Mater 2001;17:87–94.
398<br />
A. Kakaboura et al. / Dental Materials 19 (2003) 393–398<br />
[7] Mandikos MN, McGivney GP, Davis E, Bush PJ, Carter MJ. A<br />
comparison of the wear resistance and hardness of indirect composite<br />
resins. J Prosthet Dent 2001;85:386–95.<br />
[8] Douglass RD. Color stability of new-generation indirect resins for<br />
prosthodontic application. J Prosthet Dent 2000;83:166–70.<br />
[9] Kallio TT, Lastumaki TM, Vallittu PK. Bonding of restorative and<br />
veneering composite resin to some polymeric composites. Dent Mater<br />
2001;17:80–6.<br />
[10] Bouschlicher MR, Cobb DS, Vargas MA. Effect of two abrasive<br />
systems on resin bonding to laboratory-processed indirect resin<br />
composite restorations. J Esthet Dent 1999;11:185–96.<br />
[11] Ferracane JL, Greener EH. Fourier transform infrared analysis of<br />
degree of polymerization in unfilled resins-methods comparison.<br />
J Dent Res 1984;63:1093–5.<br />
[12] Urbanski J, Czerwinski W, Janicka K, Majewska F, Zowall H.<br />
Hanbook of analysis of synthetic polymers and plastics. Chichester,<br />
UK: Ellis Horwood; 1977. p. 403–13.<br />
[13] Marshall DB. An improved biaxial flexural strength test for ceramics.<br />
Am Ceram Soc Bull 1980;59:551–3.<br />
[14] O’Brien WJ. Dental materials and their selection, 2nd ed. London,<br />
England: Quintessence Publishing Co; 1997.<br />
[15] Watts DC, Cash AJ. Determination of polymerization kinetics in<br />
visible-light cured materials: methods development. Dent Mater 1991;<br />
7:281–7.<br />
[16] Watts DC, Marouf AS. Optimal specimen geometry in bonded-disk<br />
shrinkage-strain measurements on light-cured biomaterials. Dent<br />
Mater 2000;16:447–51.<br />
[17] Ruyter IE. Monomer systems and photopolymerization. In: Vanherle<br />
G, Smith DC, editors. Imternational symposium on posterior<br />
composite resin dental restorative materials. Minnesota Mining and<br />
Manufacturing Co. The Netherlands: Peter Sculz Publishing Company;<br />
1985. p. 109–35.<br />
[18] Ferracane JL, Greener EH. The effect of resin formulation on the<br />
degree of conversion and mechanical properties of dental restorative<br />
resins. J Biomed Mater Res 1986;20:121–31.<br />
[19] Wendt SL. The effect of heat as a secondary cure upon the physical<br />
properties of three composite resins: I. Diametral tensile strength,<br />
compressive strength and marginal dimensional stability. II. Wear,<br />
hardness and color stability. Quint Int 1987;18:265–71.<br />
[20] Mc Cabe JF, Kagi S. Mechanical properties of a composite inlay<br />
material following post curing. Br Dent J 1991;171:246–8.<br />
[21] Eliades GC, Vougiouklakis GL, Caputo AA. Degree of double bond<br />
conversion in light cured composites. Dent Mater 1987;3:19–25.<br />
[22] Ferracane JL, Condon JR. Post-cure heat treatments for composites:<br />
properties and fractography. Dent Mater 1992;8:290–3.<br />
[23] Park SH. Comparison of degree of conversion for light-cured and<br />
additionally heat-cured composites. J Prosthet Dent 1996;76:613–8.<br />
[24] Jordan RE. Esthetic composite bonding: techniques and materials, 2nd<br />
ed. St Louis: Mosby; 1993. p. 23–33.<br />
[25] Wassel RW, McCabe JF, Walls AWG. Subsurface deformation<br />
associated with hardness measurements of composites. Dent Mater<br />
1992;8:218–23.<br />
[26] Peutzfeldt A, Asmussen E. Mechanical properties of three composite<br />
resins for the inlay/onlay technique. J Prosthet Dent 1991;66:322–4.<br />
[27] Ferrance JL. Status of research on new fillers and new resins for dental<br />
composites. In: Tagami J, Toledano M, Prati C, editors. Advanced<br />
adhesive dentistry. Third International Kuraray Symposium. Cirimido<br />
(Como), Italy by Erredue G; 1999. p. 3–29.<br />
[28] Ferracane JL, Mitchem JC, Condon JR, Todd R. Wear and marginal<br />
breakdown of composites with various degrees of cure. J Dent Res<br />
1997;76:1508–16.<br />
[29] McCabe JF. Applied dental materials, 7th ed. Oxford, England:<br />
Blackwell; 1990. p. 78–86.<br />
[30] Lappalainen R, Yli-Upro A, Seppa L. Wear of dental restorative and<br />
prosthetic materials in vitro. Dent Mater 1989;5:35–7.<br />
[31] Kawai K, Iwami Y, Ebisu S. Effect of resin monomer composition on<br />
toothbrush wear resistance. J Oral Rehabil 1998;25:264–8.<br />
[32] Weitman RT, Eames WB. Plaque accumulation on composite surfaces<br />
after various finishing procedures. JADA 1975;91:101–6.<br />
[33] Chan KC, Fuller JL, Hormati AA. The ability of foods to stain two<br />
composite resins. J Prosthet Dent 1980;43:542–5.<br />
[34] Williams PT, Johnson LN. Composite resins revisited. J Can Dent<br />
Assoc 1993;59:538–43.<br />
[35] Soeno K, Matsamura H, Atsuta M, Kawasaki K. Effect of acidulated<br />
phosphate fluoride on veneering particulate filler composites. Int J<br />
Prosthodont 2001;14:127–32.<br />
[36] Ban S, Anusavice KL. Influence of test method on failure stress of<br />
brittle dental materials. J Dent Res 1990;69:1791–9.<br />
[37] Akinmade AO, Nicholson JW. Poisson’s ratio of glass-polyalkenoate<br />
(‘glass-ionomer’) cements determined by an ultrasonic pulse method.<br />
J Mater Sci Mater Med 1995;6:483–5.<br />
[38] Watts DC. Dental restorative materials. In: Cahn RW, Haasen P,<br />
Kramer EJ, editors. Materials science and technology: a<br />
comprehensive treatment, vol. 14. Germany: Weinheim; 1992. p.<br />
209–58.
KERR - PROJECT<br />
1) GLOSS
Material<br />
<strong>Premise</strong> <strong>Indirect</strong> - Facial<br />
Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> <strong>Indirect</strong> - Primary<br />
Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> Direct - Dentin<br />
Light-cure – 40 sec<br />
<strong>Premise</strong> Direct - Enamel<br />
Light-cure – 40 sec<br />
24 h – After<br />
cure<br />
24 h –<br />
Ethanol<br />
100%<br />
% of Gloss<br />
retention<br />
Δ Gloss<br />
75.6 (1.1) 65.1 (3.9) 86.1 (4.2) 10.5 (3.0)<br />
33.7 (9.3) 17.1 (4.9) 50.7 (0.8) 16.5 (4.3)<br />
45.9 (2.9) 27.9 (14.0) 59.8 (0.8) 18.0 (11.7)<br />
66.6 (2.0) 55.5 (10.4) 83.1 (13.3) 11.1 (8.6)
2) KNOOP HARDNESS NUMBER
Material<br />
<strong>Premise</strong> <strong>Indirect</strong> - Facial Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> <strong>Indirect</strong> - Primary Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> Direct - Dentin<br />
Light-cure – 40 sec<br />
<strong>Premise</strong> Direct - Enamel<br />
Light-cure – 40 sec<br />
24 h – After cure<br />
24 h – Ethanol<br />
100%<br />
% KHN<br />
51.8 (6.4) 34.2 (6.6) 34.4 (5.4)<br />
54.7 (4.7) 39.2 (5.3) 28.1 (9.3)<br />
44.8 (2.3) 28.3 (0.8) 36.8 (4.7)<br />
43.6 (2.6) 24.2 (1.9) 44.4 (3.0)
3) COLOUR STABILITY<br />
Material<br />
<strong>Premise</strong> <strong>Indirect</strong> - Facial Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> <strong>Indirect</strong> - Primary Dentin<br />
(3 steps cure)<br />
<strong>Premise</strong> Direct - Dentin<br />
Light-cure – 40 sec<br />
<strong>Premise</strong> Direct - Enamel<br />
Light-cure – 40 sec<br />
ΔE<br />
0.89 (0.08)<br />
2.15 (0.60)<br />
1.88 (0.49)<br />
1.01 (0.18)
(InternalData) PHYSICALPROPERTIESINDIRECTCOMPOSITERESINS(Ref.139AK74)<br />
Dia.Tens. Comp. Flex.Str. Flex.Mod. Rockwell X-RayOp. Wt.%Filler Vol% CTE K1C Str.,MPa(sd)Str.,MPa(sd) MPa(sd) MPa(sd) 15THard. (%Al) (Vol.%) shrink.(sd)ppm/Deg.C.(sd)MPam1/2(sd) BelleGlassHP TranslucentDentin 63(4) 417(34) 142(10)13100(700) 87(1.0) 78(56) 3.0(0.1) 30.2(0.8) 1.04(0.04) Product<br />
56(4) 370(28) 158(11)21,000(1400) 89.1(1.0) 300 87.1(72.5) 0.94(0.1) 13.1(0.7) 1.48(0.09) Enamels 63(2) 460(50) 167(21)10,700(200) 89.6(0.4) 100 72.9(59.5) 3.1(0.03) 26.4(0.3) 0.96(0.07) BelleglassNG Trans.Dent.306-167,131-192 450(60) 150(30)11,100(200) 84.0(0.7 2.3(0.2) 28.6(1.4) OpaceousDentin<br />
50(10) 510(10) 150(10)10,900(300) 87(0.8) 100 77(70) 2.3(0.3) 33.9(0.8) MetalPlus,Op.Dent. 63(5) 450(40) 130(14)11,500(300) 82(0.5) 200 78(63) 1.9(0.1) 25.1(1.7) 1.1(0.1) <strong>Premise</strong><strong>Indirect</strong> Enamel313-79,329-5<br />
56(4) 370(28) 158(11)21,000(1400) 89.1(1.0) 300 87.1(72.5) 0.94(0.1) 13.1(0.7) 1.48(0.09) FacialDentin 450(60) 150(30)11,100(200) 84.0(0.7 200 78(63) 2.3(0.2) 28.6(1.4) Incisal 50(10) 510(10) 150(10)10,900(300) 87(0.8) 100 77(70) 2.3(0.3) 33.9(0.8) 1.1(0.1) Artglass PrimaryDentin<br />
67(4) 351(28) 109(10)8,300(400) 80(1.0) 69 3.4(0.1) 33.3(1.0) 1.17(0.05) Enamel 67(2) 365(14) 114(10)7,800(400) 79(1.0) 500 67 Targis Dentin 58(8) 415(25) 142(23)10,300(600) 84.6(1) 74 3.0(0.1) 28.2(0.6) 0.77(0.09) Dentin<br />
107(16)6,300(460) Sculpture Dentin 48(8) 395(20) 136(9)12,700(400) 84.6(1) 78.7 2.62(1.4) 24.0(1.4) 1.13(0.16) Enamel<br />
126(21)10,500(300) Cristobal+ OpaceousDentin 49(6) 450(38) 179(11)13,000(400) 87.8(0.2) 216 75.1 3.26(0.3) 27.0(1.0) 1.14(0.27) Incisal 66(10) 473(19) 156(20)12,000(200) 86.4(1.0) 200 73 2.91(0.10) 1.22(0.09) Enamel<br />
Dentin 60(9) 441(60) 155(13)16,129(601) 93(0.4) 86.8(72.4) 1.55(0.15) 15.3(2.8) 1.27(0.2) Enamel 66(4) >500 136(18)17,980(715) 93.9(0.2) 300 88.2 1.62(0.07) 13.7(1.1) 1.19(0.09) Sinfony Estenia<br />
63(3) 430(18) 89(8)3,557(338) 51.5(1.3) 83 4.53(0.04) 62.6(3.0) 1.12(0.05) Enamel 63(4) 457(43) 89(3)3,219(228) 56.6(1.2) 100 44.7 4.62(0.3) 68.6(1.5) 1.31(0.08) Dentin<br />
Dentin 54(8) 420(34) 128(17)9,700(460) 83.5(1.5) 77.9 2.4(0.2) 34.3(0.3) Enamel 59(6) 409(27) 140(8) 9700(500) 83.1(0.7) 73.5 3.2(0.2) 33.5(0.3) Ceramics DiamondCrown<br />
Feldspathic 80 In-Ceram 450 Nature 70 393 45 600
elleGlassNGTM2003TECHNICALSUMMARY 2. Eight-yearclinicalperformanceofheatandpressurecuredindirectcomposite.D.A.Givan,S.J. O’NEALandS.SUZUKI.(Univ.ofAlabamaSchoolofDentistry,Birmingham,Alabama,USA) 1.<br />
<strong>Indirect</strong>PosteriorCompositeResins;KarlFLeinfelderDDS,MS,July2005 AdjunctProfessor,UniversityofNorthCarolina,ChapelHill,NorthCarolina ProfessorEmeritus,UniversityofAlabama,Birmingham,Alabama 3.<br />
<strong>Indirect</strong>Composites:Dentistry'sBestKeptSecret,DamonC.Adams,DDS,May6,2007,Spring ScientificSession 4.<br />
AnteriorApplicationofan<strong>Indirect</strong>Composite,aDoctor/TechnicianLiaison’sPerspective,Dr. DamonC.Adams,DDS;DentistryToday,April2005 6. Wearofcompositeresinveneeringmaterialsandenamelinachewingsimulator 5.<br />
andDentalMaterials,DentalSchool,Christian-Albrechts-UniversityatKiel,Germany SoerenScheibnerb,PrivatePractice,Neuburg,Germany Publishedondentalmaterials23(2007) ChristianMehla,KlausLudwiga,MatthiasKerna,DepartmentofProsthodontics,Propaedeutics<br />
SuccesswithbelleGlass–StepbyStep-CompositeisProgress ByAxelMühlhäuser(DT),Germany,publishedondental-labinternational,Vol.3,No.1/2007 7.<br />
ClinicalPerformanceofBondedCeramicandResin-BasedCompositeInlaysandOnlaysUsinga Self-EtchBondingSystem:a51-MonthReport Jose-LuisRuiz,DDS;GordonJ.Christensen,DDS,MSD,PhD;AbdiSameni,DDS;LuisVargas,DDS PublishedonINSIDEDENTISTRY—MAY2007 8.<br />
SupplementalOneAppointmentInlay/OnlayProcedure(ForDentists) 10. Protocol–ConservativeOneAppointmentBelleglassNGOnlayProcedure–MAY2007 9.<br />
10-yearClinicalEvaluationofaSelf-etchingAdhesiveSystem-ClinicalResearch NAkimoto,MTakamizu,YMomoi 11.<br />
12. EvaluationofClinicalandInVitroWearforResinComposites. ShiroSuzuki,KarlLeinfelder,UniversityofAlabamaatBirmingham OperativeDentistry,2007,32-1,3-10<br />
AlvinKobashigawa,EdwardShellard-Sybron/<strong>Kerr</strong>
A.I.KobashigawaandE.Shellard;“CrackArrestingPropertiesofaFiberReinforcedComposite ResinLaminate.”;J.Dent.Res.V.79SpecialIssueAbst.#289,Apr.2000 14. EffectOfFiberReinforcementOnTheBreakingStrengthOfCrowns,C.A.Munoz-Viveros,etal., 13.<br />
15. CrackArrestingPropertiesOfafiberReinforcedCompositeResinLaminateA.I.Kobashigawaand E.Shellard,KERRCorporation,Orange,California,USA Abst.#1177J.Dent.Res.77SpecialIssueB,June,1998.<br />
ClinicalEvaluationofaDentinAdhesiveSystem:13YearResults;A.A.BoghosianandJ.L. DrummondandE.P.Lautenschlager,NorthwesternUniversityFeinbergSchoolofMedicine 16.<br />
W.D.Roe*,M.H.Ramp:“WearofenamelOpposingThreeEstheticMaterialsandOneAlloy”.;J. Dent.Res.V.79SpecialIssueAbst.#1090,Apr.2000 18. ALL-IN-ONEADHESIVE-NEXUS3DENTINBONDSTRENGTH:INDIRECTPROCEDURE 17.
BGNG-belleGlassNGNextGeneration BGHP-belleGlassHPHeatandPressure<br />
•<br />
PI–<strong>Premise</strong><strong>Indirect</strong><br />
Newcompositenames?<br />
•<br />
belleGlassNGEnamelsNOW<strong>Premise</strong><strong>Indirect</strong>Incisal belleGlassNGOpaceousDentineNOW<strong>Premise</strong><strong>Indirect</strong>PrimaryDentine belleGlassNGTranslucentDentineNOW<strong>Premise</strong><strong>Indirect</strong>FacialDentin<br />
Yes-thenewovenisexactlythesameastheoldoneexceptithasamoremodernfasciaand CantheoldBGNGovenbeusedtocure<strong>Premise</strong><strong>Indirect</strong>?<br />
•<br />
Isnitrogenabsolutelynecessary? CuringrestorationsinthePIovenwithoutnitrogenmeanstheywillbecoveredinthesticky touchcontrolpanel.<br />
finalrestorationwheneitherusingornotusingnitrogenbutourpreferenceisofcourseto useit. airinhibitedlayer.Thiscanbeeasilyremoved.Thereisverylittleclinicaldifferenceinthe<br />
WhatarethemajorimprovementswiththenewPIcomposite? – Evenbetterhandling(nonstickytexture,easytocarveandcondensewithminimum<br />
anterior.<br />
Closershadematchtotheshadeguide.<br />
EvenmoretoothlikeappearanceespeciallywiththeIncisal. slump)withsuperbceramic-likeappearanceandlongerlivedglossespeciallyinthe<br />
AbilitytobuilduptheentirerestorationwithpolishablePIFacialifspacedoesnot permitforPrimary,FacialandIncisal. – FacialcontainsahigherchromavaluethanbelleGlassOpaciousDentinsoismore effectiveatmaskingmetalworkssoidealforimplantsuperstructureandothermetal<br />
work.
•<br />
Simplythetransferoftechnologytobiologyorbiologytotechnologyandtheenhancement ofeitherbyboth.Thecat’seyeinthemiddleoftheroadclearlyvisibleatnightreflecting Explainbiomimetic<br />
bornwithwhichhelpsthemseebetteratnight.PIisatransferoftechnologytobiology wherebyvirtuallytoothlikerestorationsinallsensesofthewordarefabricated. surroundinglightisanearexactcopyoftheinternalsightstructuremechanismthatcatsare<br />
•<br />
•<br />
manufacture. Isitpossibletomixbotholdandnewmaterials? Yeabutcareshouldbetakentoestablishfinalshadematchespriortorestoration<br />
OursuggestionistouseMetalPrepfromGCintheinterimperiod. Nothisproducthasbeendiscontinuedandwearecurrentlyworkingonanewformulation. Is<strong>Kerr</strong>MetalPrepavailable?<br />
•<br />
•<br />
highsmilelinecases.Thecervicalred/brownshaderemainsavailable. Whataboutawiderrangeofshadesforcervicalcolouring? Thisisinhandtomanufactureabroaderrangeofpinkcoloursespeciallyforimplantand<br />
-TheFacialDentinbuildupshouldbenomorethan1.5mminthickness. Howtoachieveoptimumaesthetics? -UseA-1PrimarydentinforalloftheshadesexceptB-1forextralightshades. -Properincisalshadeselectionisimportant.Monochromaticlayeringdoesnotwork.<br />
-Usethe40secondruletomakesurethattheCQinbleached. -ProperuseofthePrimaryDentinbuildupwilldecreasethechromaonthickbuildups. -Carrytheincisalbuilduptonomorethan1/4ofthefacialbuildup.